User login
Two novel approaches for infected ventral hernia mesh
BOSTON – Deep according to Cleveland Clinic investigators.
When infected mesh is removed, however, there’s a novel approach that avoids the pitfalls of both immediate and staged abdominal wall reconstruction, according to a second team from the Georgetown University, Washington.
The two approaches were offered at the annual clinical congress of the American College of Surgery as alternatives to usual care. Infected ventral hernia mesh is a well-known headache for general surgeons, and management isn’t standardized. Surgeons are keenly alert for new approaches to improve outcomes; the presenters said they hoped their talks would help.
The work “is really pushing this forward, and giving us new data to manage a really vexing problem,” said an audience member.
Almost 80% salvageable
Infected meshes are usually removed, but the Cleveland Clinic investigators found that that’s often not necessary.
They reviewed 905 elective ventral hernia repairs at the clinic with synthetic sublay mesh in the retrorectus space. The median hernia width was about 15 cm, and the implanted mesh – usually medium- or heavy-weight polypropylene – had a mean area of 900 cm2, “so these were big hernias with a lot of mesh. [Patients] often come to us as a last resort because they’ve been told no elsewhere,” said lead investigator Dominykas Burneikis, MD.
Twenty-four patients (2.7%) developed deep surgical site infections below the anterior rectus fascia. Instead of returning to the OR for new mesh, the team opened, drained, and debrided the wounds, and patients received antibiotics plus negative pressure wound therapy.
Those measures were enough for all but one patient. Mesh was generally found to be granulating well into surrounding tissue, so it was left completely intact in 19 cases (79%), and just trimmed a bit in four others. One man had an excision after his skin flap died and the hernia recurred. At 8 months, 11 patients were completely healed, and 12 had granulating wounds with no visible mesh. There were no cutaneous fistulas.
In short, “we had an 80% mesh salvage rate at 8 months, [which] led us to conclude that most synthetic mesh infections after retrorectus sublay repair do not require explanation,” Dr. Burneikis said.
A hybrid approach
When infected mesh does need to come out, abdominal wall reconstruction is either done in the same procedure or months later. Immediate reconstruction generally means operating in a contaminated field, with subsequent rates of wound infection of up to 48%. Delayed closure, meanwhile, means long-term wound care and temporary hernia recurrence, among other problems.
The Georgetown team reported good outcomes with a hybrid approach that combines the benefits of both procedures while avoiding their pitfalls. In the first step, mesh is removed, the abdominal wall debrided, fistulas taken down, and cultures obtained, explained lead investigator and surgery resident Kieranjeet Nijhar, MD.
The wound is temporarily closed with a sterile plastic liner under negative pressure, and patients are taken to the floor for IV antibiotics based on culture results. Three days later, after the infection has been knocked down, the patient is returned to the OR for debridement to healthy tissue and definitive reconstruction with biologic mesh. It’s all done during the same hospitalization.
Dr. Nijhar reviewed 53 cases at Georgetown since 2009. Patients were a mean age of 58 years, with an average body mass index of 35.1 kg/m2. Infected mesh was most commonly underlain or retrorectus; mean defect size was 206 cm2. Patients spent an average of 11 days in the hospital.
During a mean follow-up of about 9 months, 17 patients (32%) had surgical site problems – infection, dehiscence, hematoma, or seroma – and hernia recurred in six (11.3%); the results compare favorably with especially immediate reconstruction. As in prior studies, higher age and bridge repair were associated with recurrence and methicillin-resistant Staphylococcus aureus (MRSA) infection with surgical site problems.
“We propose this as a potential alternative for” repairs of ventral hernias with infected mesh, Dr. Nijhar said.
Dr. Nijhar and Dr. Burneikis had no relevant disclosures. There was no external funding for the work.
BOSTON – Deep according to Cleveland Clinic investigators.
When infected mesh is removed, however, there’s a novel approach that avoids the pitfalls of both immediate and staged abdominal wall reconstruction, according to a second team from the Georgetown University, Washington.
The two approaches were offered at the annual clinical congress of the American College of Surgery as alternatives to usual care. Infected ventral hernia mesh is a well-known headache for general surgeons, and management isn’t standardized. Surgeons are keenly alert for new approaches to improve outcomes; the presenters said they hoped their talks would help.
The work “is really pushing this forward, and giving us new data to manage a really vexing problem,” said an audience member.
Almost 80% salvageable
Infected meshes are usually removed, but the Cleveland Clinic investigators found that that’s often not necessary.
They reviewed 905 elective ventral hernia repairs at the clinic with synthetic sublay mesh in the retrorectus space. The median hernia width was about 15 cm, and the implanted mesh – usually medium- or heavy-weight polypropylene – had a mean area of 900 cm2, “so these were big hernias with a lot of mesh. [Patients] often come to us as a last resort because they’ve been told no elsewhere,” said lead investigator Dominykas Burneikis, MD.
Twenty-four patients (2.7%) developed deep surgical site infections below the anterior rectus fascia. Instead of returning to the OR for new mesh, the team opened, drained, and debrided the wounds, and patients received antibiotics plus negative pressure wound therapy.
Those measures were enough for all but one patient. Mesh was generally found to be granulating well into surrounding tissue, so it was left completely intact in 19 cases (79%), and just trimmed a bit in four others. One man had an excision after his skin flap died and the hernia recurred. At 8 months, 11 patients were completely healed, and 12 had granulating wounds with no visible mesh. There were no cutaneous fistulas.
In short, “we had an 80% mesh salvage rate at 8 months, [which] led us to conclude that most synthetic mesh infections after retrorectus sublay repair do not require explanation,” Dr. Burneikis said.
A hybrid approach
When infected mesh does need to come out, abdominal wall reconstruction is either done in the same procedure or months later. Immediate reconstruction generally means operating in a contaminated field, with subsequent rates of wound infection of up to 48%. Delayed closure, meanwhile, means long-term wound care and temporary hernia recurrence, among other problems.
The Georgetown team reported good outcomes with a hybrid approach that combines the benefits of both procedures while avoiding their pitfalls. In the first step, mesh is removed, the abdominal wall debrided, fistulas taken down, and cultures obtained, explained lead investigator and surgery resident Kieranjeet Nijhar, MD.
The wound is temporarily closed with a sterile plastic liner under negative pressure, and patients are taken to the floor for IV antibiotics based on culture results. Three days later, after the infection has been knocked down, the patient is returned to the OR for debridement to healthy tissue and definitive reconstruction with biologic mesh. It’s all done during the same hospitalization.
Dr. Nijhar reviewed 53 cases at Georgetown since 2009. Patients were a mean age of 58 years, with an average body mass index of 35.1 kg/m2. Infected mesh was most commonly underlain or retrorectus; mean defect size was 206 cm2. Patients spent an average of 11 days in the hospital.
During a mean follow-up of about 9 months, 17 patients (32%) had surgical site problems – infection, dehiscence, hematoma, or seroma – and hernia recurred in six (11.3%); the results compare favorably with especially immediate reconstruction. As in prior studies, higher age and bridge repair were associated with recurrence and methicillin-resistant Staphylococcus aureus (MRSA) infection with surgical site problems.
“We propose this as a potential alternative for” repairs of ventral hernias with infected mesh, Dr. Nijhar said.
Dr. Nijhar and Dr. Burneikis had no relevant disclosures. There was no external funding for the work.
BOSTON – Deep according to Cleveland Clinic investigators.
When infected mesh is removed, however, there’s a novel approach that avoids the pitfalls of both immediate and staged abdominal wall reconstruction, according to a second team from the Georgetown University, Washington.
The two approaches were offered at the annual clinical congress of the American College of Surgery as alternatives to usual care. Infected ventral hernia mesh is a well-known headache for general surgeons, and management isn’t standardized. Surgeons are keenly alert for new approaches to improve outcomes; the presenters said they hoped their talks would help.
The work “is really pushing this forward, and giving us new data to manage a really vexing problem,” said an audience member.
Almost 80% salvageable
Infected meshes are usually removed, but the Cleveland Clinic investigators found that that’s often not necessary.
They reviewed 905 elective ventral hernia repairs at the clinic with synthetic sublay mesh in the retrorectus space. The median hernia width was about 15 cm, and the implanted mesh – usually medium- or heavy-weight polypropylene – had a mean area of 900 cm2, “so these were big hernias with a lot of mesh. [Patients] often come to us as a last resort because they’ve been told no elsewhere,” said lead investigator Dominykas Burneikis, MD.
Twenty-four patients (2.7%) developed deep surgical site infections below the anterior rectus fascia. Instead of returning to the OR for new mesh, the team opened, drained, and debrided the wounds, and patients received antibiotics plus negative pressure wound therapy.
Those measures were enough for all but one patient. Mesh was generally found to be granulating well into surrounding tissue, so it was left completely intact in 19 cases (79%), and just trimmed a bit in four others. One man had an excision after his skin flap died and the hernia recurred. At 8 months, 11 patients were completely healed, and 12 had granulating wounds with no visible mesh. There were no cutaneous fistulas.
In short, “we had an 80% mesh salvage rate at 8 months, [which] led us to conclude that most synthetic mesh infections after retrorectus sublay repair do not require explanation,” Dr. Burneikis said.
A hybrid approach
When infected mesh does need to come out, abdominal wall reconstruction is either done in the same procedure or months later. Immediate reconstruction generally means operating in a contaminated field, with subsequent rates of wound infection of up to 48%. Delayed closure, meanwhile, means long-term wound care and temporary hernia recurrence, among other problems.
The Georgetown team reported good outcomes with a hybrid approach that combines the benefits of both procedures while avoiding their pitfalls. In the first step, mesh is removed, the abdominal wall debrided, fistulas taken down, and cultures obtained, explained lead investigator and surgery resident Kieranjeet Nijhar, MD.
The wound is temporarily closed with a sterile plastic liner under negative pressure, and patients are taken to the floor for IV antibiotics based on culture results. Three days later, after the infection has been knocked down, the patient is returned to the OR for debridement to healthy tissue and definitive reconstruction with biologic mesh. It’s all done during the same hospitalization.
Dr. Nijhar reviewed 53 cases at Georgetown since 2009. Patients were a mean age of 58 years, with an average body mass index of 35.1 kg/m2. Infected mesh was most commonly underlain or retrorectus; mean defect size was 206 cm2. Patients spent an average of 11 days in the hospital.
During a mean follow-up of about 9 months, 17 patients (32%) had surgical site problems – infection, dehiscence, hematoma, or seroma – and hernia recurred in six (11.3%); the results compare favorably with especially immediate reconstruction. As in prior studies, higher age and bridge repair were associated with recurrence and methicillin-resistant Staphylococcus aureus (MRSA) infection with surgical site problems.
“We propose this as a potential alternative for” repairs of ventral hernias with infected mesh, Dr. Nijhar said.
Dr. Nijhar and Dr. Burneikis had no relevant disclosures. There was no external funding for the work.
REPORTING FROM THE ACS CLINICAL CONGRESS
Key clinical point: Infected mesh can sometimes be left in place, and a new surgical approach splits the difference between immediate and staged reconstruction.
Major finding: The salvage rate for infected ventral hernia mesh was almost 80% at 8 months, and the recurrence rate was 11.3% with hybrid reconstruction at 9 months.
Study details: Reviews of 24 infected mesh cases and 53 hybrid repairs
Disclosures: The study leads didn’t have any disclosures, and there was no external funding.
Endoscopy-related infections found higher than expected, prophylaxis overused
ATLANTA – The risk of infection from flexible endoscopes is far greater than generally believed, despite the excessive use of prophylactic antimicrobials in patients undergoing endoscopy, recent studies show.
Many gastroenterologists and guidelines from professional organizations use a reference point of “less than one per million” regarding the risk of infection from scopes, but a Johns Hopkins University study of more than 2.3 million patients in 6 states showed that the infection risk with colonoscopy is about 1 per 1,000, the risk for upper gastrointestinal endoscopy is about 3 per 1,000, and the risk with cystoscopy is about 4 per 1,000, Cori Ofstead said at the International Conference on Emerging Infectious Diseases.
“For bronchoscopy [the infection risk] was 15.6 in 1,000, which is 1.6% – not anywhere in the 1 in a million range,” said Ms. Ofstead, president and chief executive officer of Ofstead & Associates, a St. Paul, Minn. health care research firm.
It also turns out that prophylactic antibiotics are frequently given to patients undergoing routine endoscopy procedures, she said, noting that four major associations – two gastroenterology associations and two urology associations in the United States and Europe – recommend that prophylactic antimicrobials be given with routine endoscopies for certain patients undergoing certain types of procedures.
One U.S. organization is recommending prophylactic antimicrobials for every patient undergoing ureteroscopy, she added.
A Cleveland Clinic study looking at the impact of those American Urological Association guidelines for prophylactic antimicrobials showed that in a subset of patients with negative urine cultures before ureteroscopy, 100% received the prophylaxis, and 68% were also given other antimicrobials to take home.
“So the question, of course, is how well does this work...,” Ms. Ofstead said. “They found 3%-4% infection, with the rates exactly the same – no statistically significant differences – between patients who got prophylaxis just in the hospital or who went home with prophylactic meds, and they concluded that there was no benefit to the extra take-home antimicrobials.”
Others studies in multiple countries show either no impact or only minor impact of this prophylaxis on infection rates, and yet all show infection rates after endoscopy that are not one in a million, but in “the percentage point range,” she said.
“As we move toward more of these minimally invasive procedures, we need to be aware that we’re using extremely complex instruments that are very difficult to clean and disinfect or sterilize,” she said, adding that “in the field we’re seeing that improper reprocessing is actually business as usual.”
Infections have been seen with all kinds of scopes, Ms. Ofstead noted.
“The potential for this becoming a bit of a monster is enhanced by the widespread use of prophylactic antimicrobials during endoscopy, and I’m also troubled by the quick reaction of giving people antimicrobials when they have a positive culture from a scope rather than making sure the scope is clean,” she said, explaining that while most scopes have microbes and patients could be getting infections, they also may be reacting to soil and endotoxins in the scope rather than microbes.
“In any case, to reduce risks there are a number of things people can do,” she said. When using reusable scopes, proper cleaning is essential. “I think we should be moving toward scopes that can be disassembled so we can see inside and get those channels clean,” adding that efforts should also be made to move toward single-use scopes.
“Particularly in these outbreak situations where we’re using bronchoscopy on multiple patients, there’s just no excuse for reusing bronchoscopes and not sterilizing them between uses and making darn sure that they’re not full of whatever our outbreak pathogen is,” Ms. Ofstead said. “And lastly, I’m hoping that some folks here can talk some sense into people at the professional associations who are recommending prophylactic antimicrobial use, because if we don’t get some stewardship going, we’re going to be in big trouble.”
The guidelines create a conundrum for doctors who are torn between that stewardship and a failure to follow the recommendations.
“Their professional organization is telling them to give prophylactic antimicrobials. If they don’t do it and a patients gets an infection, that’s a malpractice issue. So we’ve got to go through those associations and get them to stop recommending prophylactic antimicrobials when there is no evidence of their effectiveness,” she said.
Ms. Ofstead has been a consultant for 3M Company, Ambu, Auris, Boston Scientific, Cogentix, Convergascent, Healthmark, Invendo Medical, Nanosonics, and Advanced Sterilization Products, and has received grant/research support from 3M Company, Advanced Sterilization Products, Ambu, Boston Scientific, Cogentix, Healthmark, Invendo Medical, Medivators, and Steris.
SOURCE: Ofstead C., ICEID 2018 Presentation.
ATLANTA – The risk of infection from flexible endoscopes is far greater than generally believed, despite the excessive use of prophylactic antimicrobials in patients undergoing endoscopy, recent studies show.
Many gastroenterologists and guidelines from professional organizations use a reference point of “less than one per million” regarding the risk of infection from scopes, but a Johns Hopkins University study of more than 2.3 million patients in 6 states showed that the infection risk with colonoscopy is about 1 per 1,000, the risk for upper gastrointestinal endoscopy is about 3 per 1,000, and the risk with cystoscopy is about 4 per 1,000, Cori Ofstead said at the International Conference on Emerging Infectious Diseases.
“For bronchoscopy [the infection risk] was 15.6 in 1,000, which is 1.6% – not anywhere in the 1 in a million range,” said Ms. Ofstead, president and chief executive officer of Ofstead & Associates, a St. Paul, Minn. health care research firm.
It also turns out that prophylactic antibiotics are frequently given to patients undergoing routine endoscopy procedures, she said, noting that four major associations – two gastroenterology associations and two urology associations in the United States and Europe – recommend that prophylactic antimicrobials be given with routine endoscopies for certain patients undergoing certain types of procedures.
One U.S. organization is recommending prophylactic antimicrobials for every patient undergoing ureteroscopy, she added.
A Cleveland Clinic study looking at the impact of those American Urological Association guidelines for prophylactic antimicrobials showed that in a subset of patients with negative urine cultures before ureteroscopy, 100% received the prophylaxis, and 68% were also given other antimicrobials to take home.
“So the question, of course, is how well does this work...,” Ms. Ofstead said. “They found 3%-4% infection, with the rates exactly the same – no statistically significant differences – between patients who got prophylaxis just in the hospital or who went home with prophylactic meds, and they concluded that there was no benefit to the extra take-home antimicrobials.”
Others studies in multiple countries show either no impact or only minor impact of this prophylaxis on infection rates, and yet all show infection rates after endoscopy that are not one in a million, but in “the percentage point range,” she said.
“As we move toward more of these minimally invasive procedures, we need to be aware that we’re using extremely complex instruments that are very difficult to clean and disinfect or sterilize,” she said, adding that “in the field we’re seeing that improper reprocessing is actually business as usual.”
Infections have been seen with all kinds of scopes, Ms. Ofstead noted.
“The potential for this becoming a bit of a monster is enhanced by the widespread use of prophylactic antimicrobials during endoscopy, and I’m also troubled by the quick reaction of giving people antimicrobials when they have a positive culture from a scope rather than making sure the scope is clean,” she said, explaining that while most scopes have microbes and patients could be getting infections, they also may be reacting to soil and endotoxins in the scope rather than microbes.
“In any case, to reduce risks there are a number of things people can do,” she said. When using reusable scopes, proper cleaning is essential. “I think we should be moving toward scopes that can be disassembled so we can see inside and get those channels clean,” adding that efforts should also be made to move toward single-use scopes.
“Particularly in these outbreak situations where we’re using bronchoscopy on multiple patients, there’s just no excuse for reusing bronchoscopes and not sterilizing them between uses and making darn sure that they’re not full of whatever our outbreak pathogen is,” Ms. Ofstead said. “And lastly, I’m hoping that some folks here can talk some sense into people at the professional associations who are recommending prophylactic antimicrobial use, because if we don’t get some stewardship going, we’re going to be in big trouble.”
The guidelines create a conundrum for doctors who are torn between that stewardship and a failure to follow the recommendations.
“Their professional organization is telling them to give prophylactic antimicrobials. If they don’t do it and a patients gets an infection, that’s a malpractice issue. So we’ve got to go through those associations and get them to stop recommending prophylactic antimicrobials when there is no evidence of their effectiveness,” she said.
Ms. Ofstead has been a consultant for 3M Company, Ambu, Auris, Boston Scientific, Cogentix, Convergascent, Healthmark, Invendo Medical, Nanosonics, and Advanced Sterilization Products, and has received grant/research support from 3M Company, Advanced Sterilization Products, Ambu, Boston Scientific, Cogentix, Healthmark, Invendo Medical, Medivators, and Steris.
SOURCE: Ofstead C., ICEID 2018 Presentation.
ATLANTA – The risk of infection from flexible endoscopes is far greater than generally believed, despite the excessive use of prophylactic antimicrobials in patients undergoing endoscopy, recent studies show.
Many gastroenterologists and guidelines from professional organizations use a reference point of “less than one per million” regarding the risk of infection from scopes, but a Johns Hopkins University study of more than 2.3 million patients in 6 states showed that the infection risk with colonoscopy is about 1 per 1,000, the risk for upper gastrointestinal endoscopy is about 3 per 1,000, and the risk with cystoscopy is about 4 per 1,000, Cori Ofstead said at the International Conference on Emerging Infectious Diseases.
“For bronchoscopy [the infection risk] was 15.6 in 1,000, which is 1.6% – not anywhere in the 1 in a million range,” said Ms. Ofstead, president and chief executive officer of Ofstead & Associates, a St. Paul, Minn. health care research firm.
It also turns out that prophylactic antibiotics are frequently given to patients undergoing routine endoscopy procedures, she said, noting that four major associations – two gastroenterology associations and two urology associations in the United States and Europe – recommend that prophylactic antimicrobials be given with routine endoscopies for certain patients undergoing certain types of procedures.
One U.S. organization is recommending prophylactic antimicrobials for every patient undergoing ureteroscopy, she added.
A Cleveland Clinic study looking at the impact of those American Urological Association guidelines for prophylactic antimicrobials showed that in a subset of patients with negative urine cultures before ureteroscopy, 100% received the prophylaxis, and 68% were also given other antimicrobials to take home.
“So the question, of course, is how well does this work...,” Ms. Ofstead said. “They found 3%-4% infection, with the rates exactly the same – no statistically significant differences – between patients who got prophylaxis just in the hospital or who went home with prophylactic meds, and they concluded that there was no benefit to the extra take-home antimicrobials.”
Others studies in multiple countries show either no impact or only minor impact of this prophylaxis on infection rates, and yet all show infection rates after endoscopy that are not one in a million, but in “the percentage point range,” she said.
“As we move toward more of these minimally invasive procedures, we need to be aware that we’re using extremely complex instruments that are very difficult to clean and disinfect or sterilize,” she said, adding that “in the field we’re seeing that improper reprocessing is actually business as usual.”
Infections have been seen with all kinds of scopes, Ms. Ofstead noted.
“The potential for this becoming a bit of a monster is enhanced by the widespread use of prophylactic antimicrobials during endoscopy, and I’m also troubled by the quick reaction of giving people antimicrobials when they have a positive culture from a scope rather than making sure the scope is clean,” she said, explaining that while most scopes have microbes and patients could be getting infections, they also may be reacting to soil and endotoxins in the scope rather than microbes.
“In any case, to reduce risks there are a number of things people can do,” she said. When using reusable scopes, proper cleaning is essential. “I think we should be moving toward scopes that can be disassembled so we can see inside and get those channels clean,” adding that efforts should also be made to move toward single-use scopes.
“Particularly in these outbreak situations where we’re using bronchoscopy on multiple patients, there’s just no excuse for reusing bronchoscopes and not sterilizing them between uses and making darn sure that they’re not full of whatever our outbreak pathogen is,” Ms. Ofstead said. “And lastly, I’m hoping that some folks here can talk some sense into people at the professional associations who are recommending prophylactic antimicrobial use, because if we don’t get some stewardship going, we’re going to be in big trouble.”
The guidelines create a conundrum for doctors who are torn between that stewardship and a failure to follow the recommendations.
“Their professional organization is telling them to give prophylactic antimicrobials. If they don’t do it and a patients gets an infection, that’s a malpractice issue. So we’ve got to go through those associations and get them to stop recommending prophylactic antimicrobials when there is no evidence of their effectiveness,” she said.
Ms. Ofstead has been a consultant for 3M Company, Ambu, Auris, Boston Scientific, Cogentix, Convergascent, Healthmark, Invendo Medical, Nanosonics, and Advanced Sterilization Products, and has received grant/research support from 3M Company, Advanced Sterilization Products, Ambu, Boston Scientific, Cogentix, Healthmark, Invendo Medical, Medivators, and Steris.
SOURCE: Ofstead C., ICEID 2018 Presentation.
REPORTING FROM ICEID 2018
Key clinical point:
Major finding: Infection risk is about 1 per 1,000 with colonoscopy; 3 per 1,000 with upper gastrointestinal endoscopy; and 4 per 1,000 with cystoscopy.
Study details: Endoscopic procedures performed at ASCs in 2014 all-payer claims data from 6 U.S. states.
Disclosures: Ms. Ofstead has been a consultant for 3M Company, Ambu, Auris, Boston Scientific, Cogentix, Convergascent, Healthmark, Invendo Medical, Nanosonics, and Advanced Sterilization Products, and has received grant/research support from 3M Company, Advanced Sterilization Products, Ambu, Boston Scientific, Cogentix, Healthmark, Invendo Medical, Medivators, and Steris.
Source: Ofstead C et al. ICEID 2018 Presentation.
Vancomycin loading boost yields better C. diff outcomes
SAN FRANCISCO – A heightened loading dose of vancomycin may lead to faster recovery and greater efficacy in Clostridium difficile infections, according to the results of a quasi-experimental study presented at an annual scientific meeting on infectious diseases.
The study looked at a loading dose of 500 mg of vancomycin delivered four times per day for the first 48 hours, followed by a step down to 125 mg every 6 hours. It came on the heels of an attempted randomized, clinical trial that was inconclusive because of insufficient recruitment. Still, the results were promising enough to convince the Yale New Haven Hospital to make it standard practice in C. difficile patients.
Samad Tirmizi, PharmD, an infectious disease pharmacist at Stony Brook University (N.Y.), shares the results of a comparison of outcomes before and after the initiation of this treatment protocol in a video interview.
The approach grew out of concerns that vancomycin may not achieve sufficient concentrations in the colon early in treatment. A pharmacokinetics study published in 2010 suggested that a high initial loading led to higher fecal vancomycin levels, even in patients with increased stool frequency (BMC Infect Dis. 2010 Dec 30;10:363).
SOURCE: Tirmizi S et al. IDWeek 2018, Abstract 1980.
SAN FRANCISCO – A heightened loading dose of vancomycin may lead to faster recovery and greater efficacy in Clostridium difficile infections, according to the results of a quasi-experimental study presented at an annual scientific meeting on infectious diseases.
The study looked at a loading dose of 500 mg of vancomycin delivered four times per day for the first 48 hours, followed by a step down to 125 mg every 6 hours. It came on the heels of an attempted randomized, clinical trial that was inconclusive because of insufficient recruitment. Still, the results were promising enough to convince the Yale New Haven Hospital to make it standard practice in C. difficile patients.
Samad Tirmizi, PharmD, an infectious disease pharmacist at Stony Brook University (N.Y.), shares the results of a comparison of outcomes before and after the initiation of this treatment protocol in a video interview.
The approach grew out of concerns that vancomycin may not achieve sufficient concentrations in the colon early in treatment. A pharmacokinetics study published in 2010 suggested that a high initial loading led to higher fecal vancomycin levels, even in patients with increased stool frequency (BMC Infect Dis. 2010 Dec 30;10:363).
SOURCE: Tirmizi S et al. IDWeek 2018, Abstract 1980.
SAN FRANCISCO – A heightened loading dose of vancomycin may lead to faster recovery and greater efficacy in Clostridium difficile infections, according to the results of a quasi-experimental study presented at an annual scientific meeting on infectious diseases.
The study looked at a loading dose of 500 mg of vancomycin delivered four times per day for the first 48 hours, followed by a step down to 125 mg every 6 hours. It came on the heels of an attempted randomized, clinical trial that was inconclusive because of insufficient recruitment. Still, the results were promising enough to convince the Yale New Haven Hospital to make it standard practice in C. difficile patients.
Samad Tirmizi, PharmD, an infectious disease pharmacist at Stony Brook University (N.Y.), shares the results of a comparison of outcomes before and after the initiation of this treatment protocol in a video interview.
The approach grew out of concerns that vancomycin may not achieve sufficient concentrations in the colon early in treatment. A pharmacokinetics study published in 2010 suggested that a high initial loading led to higher fecal vancomycin levels, even in patients with increased stool frequency (BMC Infect Dis. 2010 Dec 30;10:363).
SOURCE: Tirmizi S et al. IDWeek 2018, Abstract 1980.
REPORTING FROM IDWEEK 2018
Discharge trends for septic shock survivors remain steady
SAN ANTONIO – While septic shock mortality has decreased since the Surviving Sepsis Campaign guidelines were introduced, discharge trends for survivors have not changed significantly over time, a recent analysis suggests.
The percentage of survivors discharged to subacute rehab or long-term facilities did not change appreciably over time, according to the 10-year retrospective analysis, presented at the annual meeting of the American College of Chest Physicians.
However, average length of stay did significantly trend downward over the decade analyzed, while total charge per septic shock admission significantly increased, according to investigator Di Pan, DO, Icahn School of Medicine at Mount Sinai, New York, and his colleagues.
This is one of few studies looking at outcomes in survivors of septic shock, as most analyses have primarily focused on mortality outcomes, the investigators said.
Their analysis was based on the 2004 to 2014 National (Nationwide) Inpatient Sample databases and included patients with a primary diagnosis of septic shock at discharge.
Out of nearly 1.8 million patients with septic shock in that cohort, about 1 million survived, according to data Dr. Pan and colleagues provided in an abstract of the presentation.
In-hospital mortality decreased from 51.7% in 2004 to 39.3% in 2014 (P less than .001), the investigators reported.
The proportion of survivors discharged to subacute rehab or long-term acute care facilities was 61.9% in 2004, and similarly, 62.4% in 2014 (P = .1), while the percentage discharged home was 17.1% in 2004 and 15.1% in 2014 (P = 0.55).
However, there was a small but statistically significant downtick in mean length of stay, from 12.6 days in 2004 to 11.05 days in 2014, the investigators said. Meanwhile, total hospitalization charges surged from $105,776 in 2004 to $134,394 over the same time period.
The first edition of the Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock was published in March 2004 in Critical Care Medicine.
Future studies and clinical trials should look beyond mortality outcomes to additionally evaluate morbidity outcomes in septic shock survivors, Dr. Pan and coauthors said in their report.
The researchers had no relationships to disclose relevant to the presented study.
SOURCE: Pan D et al. CHEST 2018. doi: 10.1016/j.chest.2018.08.339.
SAN ANTONIO – While septic shock mortality has decreased since the Surviving Sepsis Campaign guidelines were introduced, discharge trends for survivors have not changed significantly over time, a recent analysis suggests.
The percentage of survivors discharged to subacute rehab or long-term facilities did not change appreciably over time, according to the 10-year retrospective analysis, presented at the annual meeting of the American College of Chest Physicians.
However, average length of stay did significantly trend downward over the decade analyzed, while total charge per septic shock admission significantly increased, according to investigator Di Pan, DO, Icahn School of Medicine at Mount Sinai, New York, and his colleagues.
This is one of few studies looking at outcomes in survivors of septic shock, as most analyses have primarily focused on mortality outcomes, the investigators said.
Their analysis was based on the 2004 to 2014 National (Nationwide) Inpatient Sample databases and included patients with a primary diagnosis of septic shock at discharge.
Out of nearly 1.8 million patients with septic shock in that cohort, about 1 million survived, according to data Dr. Pan and colleagues provided in an abstract of the presentation.
In-hospital mortality decreased from 51.7% in 2004 to 39.3% in 2014 (P less than .001), the investigators reported.
The proportion of survivors discharged to subacute rehab or long-term acute care facilities was 61.9% in 2004, and similarly, 62.4% in 2014 (P = .1), while the percentage discharged home was 17.1% in 2004 and 15.1% in 2014 (P = 0.55).
However, there was a small but statistically significant downtick in mean length of stay, from 12.6 days in 2004 to 11.05 days in 2014, the investigators said. Meanwhile, total hospitalization charges surged from $105,776 in 2004 to $134,394 over the same time period.
The first edition of the Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock was published in March 2004 in Critical Care Medicine.
Future studies and clinical trials should look beyond mortality outcomes to additionally evaluate morbidity outcomes in septic shock survivors, Dr. Pan and coauthors said in their report.
The researchers had no relationships to disclose relevant to the presented study.
SOURCE: Pan D et al. CHEST 2018. doi: 10.1016/j.chest.2018.08.339.
SAN ANTONIO – While septic shock mortality has decreased since the Surviving Sepsis Campaign guidelines were introduced, discharge trends for survivors have not changed significantly over time, a recent analysis suggests.
The percentage of survivors discharged to subacute rehab or long-term facilities did not change appreciably over time, according to the 10-year retrospective analysis, presented at the annual meeting of the American College of Chest Physicians.
However, average length of stay did significantly trend downward over the decade analyzed, while total charge per septic shock admission significantly increased, according to investigator Di Pan, DO, Icahn School of Medicine at Mount Sinai, New York, and his colleagues.
This is one of few studies looking at outcomes in survivors of septic shock, as most analyses have primarily focused on mortality outcomes, the investigators said.
Their analysis was based on the 2004 to 2014 National (Nationwide) Inpatient Sample databases and included patients with a primary diagnosis of septic shock at discharge.
Out of nearly 1.8 million patients with septic shock in that cohort, about 1 million survived, according to data Dr. Pan and colleagues provided in an abstract of the presentation.
In-hospital mortality decreased from 51.7% in 2004 to 39.3% in 2014 (P less than .001), the investigators reported.
The proportion of survivors discharged to subacute rehab or long-term acute care facilities was 61.9% in 2004, and similarly, 62.4% in 2014 (P = .1), while the percentage discharged home was 17.1% in 2004 and 15.1% in 2014 (P = 0.55).
However, there was a small but statistically significant downtick in mean length of stay, from 12.6 days in 2004 to 11.05 days in 2014, the investigators said. Meanwhile, total hospitalization charges surged from $105,776 in 2004 to $134,394 over the same time period.
The first edition of the Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock was published in March 2004 in Critical Care Medicine.
Future studies and clinical trials should look beyond mortality outcomes to additionally evaluate morbidity outcomes in septic shock survivors, Dr. Pan and coauthors said in their report.
The researchers had no relationships to disclose relevant to the presented study.
SOURCE: Pan D et al. CHEST 2018. doi: 10.1016/j.chest.2018.08.339.
REPORTING FROM CHEST 2018
Key clinical point: While septic shock mortality has decreased over time, discharge trends for survivors have remained steady.
Major finding: In-hospital mortality dropped from about 52% to 39% over the 2004-2014 period, while discharges to subacute rehab or long-term facilities stayed around 62%.
Study details: Retrospective analysis of nearly 1.8 million patients with septic shock, of whom about 1 million survived.
Disclosures: The authors had no relationships to disclose relevant to the presented study.
Source: Pan D et al. CHEST 2018.
NYC outbreak of Candida auris linked to 45% mortality
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
FROM EMERGING INFECTIOUS DISEASES
Review protocols, follow reprocessing guidelines to cut device-related HAIs
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
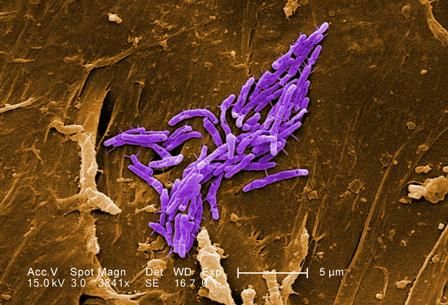
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
[email protected]
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
[email protected]
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
[email protected]
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
REPORTING FROM ICEID 2018
Key clinical point: Medical devices can be reservoirs and transmission vectors for health care–associated infections.
Major finding: Of 285 consultations, 48 involved medical devices or device reprocessing.
Study details: A review of records from 285 consultations
Disclosures: Dr. Benowitz reported having no disclosures
Source: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
United Kingdom experience provides important lessons for controlling C. auris outbreaks
ATLANTA – The persistence and transmission of Candida auris in health care settings appears to be dependent on environmental survival, underscoring the need for careful investigation of the environment – and, in particular, multiuse patient equipment.
That’s the key lesson from one of the largest outbreaks of the emerging, multidrug-resistant pathogen to date, David Eyre, DPhil, said at the International Conference on Emerging Infectious Diseases.
“Our experience at Oxford began with a Public Health England alert, which closely followed a similar alert from the [Centers for Disease Control and Prevention] in the summer of 2016,” Dr. Eyre of the University of Oxford (England) said during an update on the epidemiology of the outbreak and the successful, multipronged effort to control it.
The outbreak, which occurred in the neurosciences intensive care unit of Oxford University Hospitals beginning in early 2015, was detected in 2016 when a cluster of C. auris infections was identified and traced to the unit. An intensive patient and environmental screening program was established, isolation protocols were used for patients who tested positive, enhanced cleaning processes were initiated, and equipment was removed and replaced with single-use equipment when possible.
“We also worked quite closely with our staff to raise awareness,” he said, adding that colonized patients who were undergoing a surgical procedure received single-dose antifungal prophylaxis prior to the procedure.
A case-control study was conducted, and after the researchers used multivariate logistic regression to control for length of stay, patient physiology, and biomarkers, exposure to multiuse skin surface axillary temperature monitoring was shown to be one of the strongest independent predictors of C. auris colonization and infection (odds ratio 6.80), he said, adding that antifungal exposure was also a significant risk factor, but only 5% of patients had received antifungals.
The axillary probes were then removed from the environment. As of April 2017 (when the probes were removed), 66 patients had been colonized or infected, and an additional 10 cases occurred after the probes were removed, with the last case occurring in November 2017.
Seven of the 76 cases involved invasive infection, and 1 patient died several months after hospital discharge, Dr. Eyre said.
The patient screening processes allowed for estimation of colonization time (approximately 2 months), and also allowed for whole-genome sequencing of 79 samples from 43 patients, 6 environmental isolates, and 2 isolates from regional surveillance, Dr. Eyre said.
All outbreak sequences formed a single genetic cluster within the C. auris South African clade, and were found to have been introduced to Oxford around 2012 or 2013, with about six mutations per year, or “roughly 12 million base pairs in total,” he said, adding that both patients and temperature probes were colonized with multiple strains, and there was “close mixing” between the two.
This pattern changed following removal of the temperature probes, but it took some time.
“However, from November [2017] onward – so that’s now 291 days ... we’ve not had another new patient isolate, and that’s not only no invasive infection, but also no colonization despite continuing the screening program,” he said.
According to the CDC, C. auris is “an emerging fungus that presents a serious global health threat” because of its often multidrug-resistant nature, difficulty identifying the pathogen using standard laboratory methods, and the risk for misidentification in labs without specific technology, which could lead to inappropriate management.
“It has caused outbreaks in health care settings. For this reason, it is important to quickly identify C. auris in a hospitalized patient so that health care facilities can take special precautions to stop its spread,” a CDC page on C. auris states. “CDC encourages all U.S. laboratory staff who identify C. auris to notify their state or local public health authorities and CDC at [email protected].”
Dr. Eyre reported having no disclosures.
SOURCE: Eyre D et al. ICEID 2018 Oral Abstract Presentation.
ATLANTA – The persistence and transmission of Candida auris in health care settings appears to be dependent on environmental survival, underscoring the need for careful investigation of the environment – and, in particular, multiuse patient equipment.
That’s the key lesson from one of the largest outbreaks of the emerging, multidrug-resistant pathogen to date, David Eyre, DPhil, said at the International Conference on Emerging Infectious Diseases.
“Our experience at Oxford began with a Public Health England alert, which closely followed a similar alert from the [Centers for Disease Control and Prevention] in the summer of 2016,” Dr. Eyre of the University of Oxford (England) said during an update on the epidemiology of the outbreak and the successful, multipronged effort to control it.
The outbreak, which occurred in the neurosciences intensive care unit of Oxford University Hospitals beginning in early 2015, was detected in 2016 when a cluster of C. auris infections was identified and traced to the unit. An intensive patient and environmental screening program was established, isolation protocols were used for patients who tested positive, enhanced cleaning processes were initiated, and equipment was removed and replaced with single-use equipment when possible.
“We also worked quite closely with our staff to raise awareness,” he said, adding that colonized patients who were undergoing a surgical procedure received single-dose antifungal prophylaxis prior to the procedure.
A case-control study was conducted, and after the researchers used multivariate logistic regression to control for length of stay, patient physiology, and biomarkers, exposure to multiuse skin surface axillary temperature monitoring was shown to be one of the strongest independent predictors of C. auris colonization and infection (odds ratio 6.80), he said, adding that antifungal exposure was also a significant risk factor, but only 5% of patients had received antifungals.
The axillary probes were then removed from the environment. As of April 2017 (when the probes were removed), 66 patients had been colonized or infected, and an additional 10 cases occurred after the probes were removed, with the last case occurring in November 2017.
Seven of the 76 cases involved invasive infection, and 1 patient died several months after hospital discharge, Dr. Eyre said.
The patient screening processes allowed for estimation of colonization time (approximately 2 months), and also allowed for whole-genome sequencing of 79 samples from 43 patients, 6 environmental isolates, and 2 isolates from regional surveillance, Dr. Eyre said.
All outbreak sequences formed a single genetic cluster within the C. auris South African clade, and were found to have been introduced to Oxford around 2012 or 2013, with about six mutations per year, or “roughly 12 million base pairs in total,” he said, adding that both patients and temperature probes were colonized with multiple strains, and there was “close mixing” between the two.
This pattern changed following removal of the temperature probes, but it took some time.
“However, from November [2017] onward – so that’s now 291 days ... we’ve not had another new patient isolate, and that’s not only no invasive infection, but also no colonization despite continuing the screening program,” he said.
According to the CDC, C. auris is “an emerging fungus that presents a serious global health threat” because of its often multidrug-resistant nature, difficulty identifying the pathogen using standard laboratory methods, and the risk for misidentification in labs without specific technology, which could lead to inappropriate management.
“It has caused outbreaks in health care settings. For this reason, it is important to quickly identify C. auris in a hospitalized patient so that health care facilities can take special precautions to stop its spread,” a CDC page on C. auris states. “CDC encourages all U.S. laboratory staff who identify C. auris to notify their state or local public health authorities and CDC at [email protected].”
Dr. Eyre reported having no disclosures.
SOURCE: Eyre D et al. ICEID 2018 Oral Abstract Presentation.
ATLANTA – The persistence and transmission of Candida auris in health care settings appears to be dependent on environmental survival, underscoring the need for careful investigation of the environment – and, in particular, multiuse patient equipment.
That’s the key lesson from one of the largest outbreaks of the emerging, multidrug-resistant pathogen to date, David Eyre, DPhil, said at the International Conference on Emerging Infectious Diseases.
“Our experience at Oxford began with a Public Health England alert, which closely followed a similar alert from the [Centers for Disease Control and Prevention] in the summer of 2016,” Dr. Eyre of the University of Oxford (England) said during an update on the epidemiology of the outbreak and the successful, multipronged effort to control it.
The outbreak, which occurred in the neurosciences intensive care unit of Oxford University Hospitals beginning in early 2015, was detected in 2016 when a cluster of C. auris infections was identified and traced to the unit. An intensive patient and environmental screening program was established, isolation protocols were used for patients who tested positive, enhanced cleaning processes were initiated, and equipment was removed and replaced with single-use equipment when possible.
“We also worked quite closely with our staff to raise awareness,” he said, adding that colonized patients who were undergoing a surgical procedure received single-dose antifungal prophylaxis prior to the procedure.
A case-control study was conducted, and after the researchers used multivariate logistic regression to control for length of stay, patient physiology, and biomarkers, exposure to multiuse skin surface axillary temperature monitoring was shown to be one of the strongest independent predictors of C. auris colonization and infection (odds ratio 6.80), he said, adding that antifungal exposure was also a significant risk factor, but only 5% of patients had received antifungals.
The axillary probes were then removed from the environment. As of April 2017 (when the probes were removed), 66 patients had been colonized or infected, and an additional 10 cases occurred after the probes were removed, with the last case occurring in November 2017.
Seven of the 76 cases involved invasive infection, and 1 patient died several months after hospital discharge, Dr. Eyre said.
The patient screening processes allowed for estimation of colonization time (approximately 2 months), and also allowed for whole-genome sequencing of 79 samples from 43 patients, 6 environmental isolates, and 2 isolates from regional surveillance, Dr. Eyre said.
All outbreak sequences formed a single genetic cluster within the C. auris South African clade, and were found to have been introduced to Oxford around 2012 or 2013, with about six mutations per year, or “roughly 12 million base pairs in total,” he said, adding that both patients and temperature probes were colonized with multiple strains, and there was “close mixing” between the two.
This pattern changed following removal of the temperature probes, but it took some time.
“However, from November [2017] onward – so that’s now 291 days ... we’ve not had another new patient isolate, and that’s not only no invasive infection, but also no colonization despite continuing the screening program,” he said.
According to the CDC, C. auris is “an emerging fungus that presents a serious global health threat” because of its often multidrug-resistant nature, difficulty identifying the pathogen using standard laboratory methods, and the risk for misidentification in labs without specific technology, which could lead to inappropriate management.
“It has caused outbreaks in health care settings. For this reason, it is important to quickly identify C. auris in a hospitalized patient so that health care facilities can take special precautions to stop its spread,” a CDC page on C. auris states. “CDC encourages all U.S. laboratory staff who identify C. auris to notify their state or local public health authorities and CDC at [email protected].”
Dr. Eyre reported having no disclosures.
SOURCE: Eyre D et al. ICEID 2018 Oral Abstract Presentation.
REPORTING FROM ICEID 2018
Key clinical point:
Major finding: Ten additional cases occurred in the 7 months after the axillary probes were removed from the environment.
Study details: A review of the epidemiology and control of a C. auris outbreak affecting 76 patients.
Disclosures: Dr. Eyre reported having no disclosures.
Source: Eyre D et al. ICEID 2018 Oral Abstract Presentation.
Patient transfers between hospitals contribute substantially to CDI burden
ATLANTA – Patient sharing among hospital facilities contributed substantially to the overall Clostridium difficile infection rate, an analysis of interhospital contamination effects showed.
In fact, 7.6% of all Clostridium difficile infection (CDI) cases at the nearly 400 California hospitals included in the study were directly attributable to the patient-sharing network, Daniel Sewell, PhD, reported at the International Conference on Emerging Infectious Diseases.
“The methods that we employed allowed us to estimate the expected increase in CDI cases due to transfers as a function of the CDI rate at the hospital from which those patients were brought. These transfer patients were responsible for about 3.06 times the number of CDI cases as a normal patient,” said Dr. Sewell, a biostatistician at the University of Iowa, Iowa City.
The findings, which underscored the importance of regional (rather than local) efforts to minimize the spread of health care–associated infections, are based on an analysis of 27,200,873 hospital admissions and 532,320 same-day patient transfers identified from the Healthcare Cost and Utilization Project California State Inpatient Database for 2005-2011.
Transfer networks based on the monthly average number of patients discharged from one hospital and admitted to another on the same day were constructed, and the monthly average number of CDI cases per hospital were considered, along with hospital-level characteristics such as patient length of stay, age, and number of diagnoses. Network autocorrelation models that help eliminate bias were then used to assess the contamination effects between hospitals, he explained.
This led to development of an equation that can be used to determine the expected number of CDI cases in a hospital as a function of the number of transfers coming in and the contamination level of the source hospitals. The ability to calculate the expected number of CDI cases in this fashion is an important factor for the success of regional versus local intervention efforts, which are increasingly thought to be important for reducing health care–associated infections.
“If we want to design a coordinated or regional approach, we’ve got to have a much better understanding of the role that patient transfers have in these diseases,” Dr. Sewell said.
As most hospitals included in the study had a low CDI rate and a low transfer rate, the CDIs attributable to transfers represent a minority of cases, but they are a substantial minority, he said, noting that the main concern is with the “perfect storm” of high CDI rate plus high transfer rate.
The methodological approach used in this study to estimate CDI rates can be used for any health care–associated infection of interest, he added.
Dr. Sewell reported that he had no disclosures.
ATLANTA – Patient sharing among hospital facilities contributed substantially to the overall Clostridium difficile infection rate, an analysis of interhospital contamination effects showed.
In fact, 7.6% of all Clostridium difficile infection (CDI) cases at the nearly 400 California hospitals included in the study were directly attributable to the patient-sharing network, Daniel Sewell, PhD, reported at the International Conference on Emerging Infectious Diseases.
“The methods that we employed allowed us to estimate the expected increase in CDI cases due to transfers as a function of the CDI rate at the hospital from which those patients were brought. These transfer patients were responsible for about 3.06 times the number of CDI cases as a normal patient,” said Dr. Sewell, a biostatistician at the University of Iowa, Iowa City.
The findings, which underscored the importance of regional (rather than local) efforts to minimize the spread of health care–associated infections, are based on an analysis of 27,200,873 hospital admissions and 532,320 same-day patient transfers identified from the Healthcare Cost and Utilization Project California State Inpatient Database for 2005-2011.
Transfer networks based on the monthly average number of patients discharged from one hospital and admitted to another on the same day were constructed, and the monthly average number of CDI cases per hospital were considered, along with hospital-level characteristics such as patient length of stay, age, and number of diagnoses. Network autocorrelation models that help eliminate bias were then used to assess the contamination effects between hospitals, he explained.
This led to development of an equation that can be used to determine the expected number of CDI cases in a hospital as a function of the number of transfers coming in and the contamination level of the source hospitals. The ability to calculate the expected number of CDI cases in this fashion is an important factor for the success of regional versus local intervention efforts, which are increasingly thought to be important for reducing health care–associated infections.
“If we want to design a coordinated or regional approach, we’ve got to have a much better understanding of the role that patient transfers have in these diseases,” Dr. Sewell said.
As most hospitals included in the study had a low CDI rate and a low transfer rate, the CDIs attributable to transfers represent a minority of cases, but they are a substantial minority, he said, noting that the main concern is with the “perfect storm” of high CDI rate plus high transfer rate.
The methodological approach used in this study to estimate CDI rates can be used for any health care–associated infection of interest, he added.
Dr. Sewell reported that he had no disclosures.
ATLANTA – Patient sharing among hospital facilities contributed substantially to the overall Clostridium difficile infection rate, an analysis of interhospital contamination effects showed.
In fact, 7.6% of all Clostridium difficile infection (CDI) cases at the nearly 400 California hospitals included in the study were directly attributable to the patient-sharing network, Daniel Sewell, PhD, reported at the International Conference on Emerging Infectious Diseases.
“The methods that we employed allowed us to estimate the expected increase in CDI cases due to transfers as a function of the CDI rate at the hospital from which those patients were brought. These transfer patients were responsible for about 3.06 times the number of CDI cases as a normal patient,” said Dr. Sewell, a biostatistician at the University of Iowa, Iowa City.
The findings, which underscored the importance of regional (rather than local) efforts to minimize the spread of health care–associated infections, are based on an analysis of 27,200,873 hospital admissions and 532,320 same-day patient transfers identified from the Healthcare Cost and Utilization Project California State Inpatient Database for 2005-2011.
Transfer networks based on the monthly average number of patients discharged from one hospital and admitted to another on the same day were constructed, and the monthly average number of CDI cases per hospital were considered, along with hospital-level characteristics such as patient length of stay, age, and number of diagnoses. Network autocorrelation models that help eliminate bias were then used to assess the contamination effects between hospitals, he explained.
This led to development of an equation that can be used to determine the expected number of CDI cases in a hospital as a function of the number of transfers coming in and the contamination level of the source hospitals. The ability to calculate the expected number of CDI cases in this fashion is an important factor for the success of regional versus local intervention efforts, which are increasingly thought to be important for reducing health care–associated infections.
“If we want to design a coordinated or regional approach, we’ve got to have a much better understanding of the role that patient transfers have in these diseases,” Dr. Sewell said.
As most hospitals included in the study had a low CDI rate and a low transfer rate, the CDIs attributable to transfers represent a minority of cases, but they are a substantial minority, he said, noting that the main concern is with the “perfect storm” of high CDI rate plus high transfer rate.
The methodological approach used in this study to estimate CDI rates can be used for any health care–associated infection of interest, he added.
Dr. Sewell reported that he had no disclosures.
REPORTING FROM ICEID 2018
Key clinical point: Patient sharing among hospitals contributes substantially to Clostridium difficile infection (CDI) rates.
Major finding: Patient transfers account for 7.6% of the overall CDI burden.
Study details: A statistical analysis to estimate interhospital CDI transmissions.
Disclosures: Dr. Sewell reported that he had no disclosures.
Hand hygiene linked to reduced ICU health care–associated infections
A hospital-wide infection control program (ICP) was found to be associated with reduced health care-associated severe sepsis/septic shock or death in the ICU, but it was not clear whether this decrease was a consequence of the ICP or because of a concomitant improvement in HAI case management, according to a the results of a prospective analysis.
In addition, there was no significant decrease in overall HAIs seen despite implementation of the program, according to the report published online in Clinical Microbiology and Infection (doi: 10.1016/j.cmi.2018.07.010), according to Stefan Hagel, MD, of the Institute for Infectious Diseases and Infection Control, Jena (Germany) University Hospital, and his colleagues.
They assessed two surveillance periods (September 2011 to August 2012 and May 2013 to August 2014). The ICP started in October 2012, and included hand-hygiene promotion and bundle implementation for common HAIs.
The data were analyzed by segmented mixed-effects Poisson regression and multi-state models and reported as adjusted incidence rate ratios (aIRR) and 50 adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
In the first period, 62,154 patients were under surveillance, with 1,568 HAIs identified in 1,170 patients (4.3/100 admissions) and 2,336 HAIs identified in 1,711 patients (4.9/100 admissions) in the second surveillance period. No differences were found in the overall HAI incidence rates between the periods in the general wards and ICUs. There was only a slight decline in the incidence rate of HAIs in the ICUs (aIRR 0.98 [0.97, 1.00] per 1-week increment), compared with the general wards (aIRR 1.01 [1.00, 1.02]).
However, a reduction in severe HAIs (aIRR 0.13 [0.05, 0.32]) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56 [0.31, 0.99]) were observed in the second period in the ICUs.
In attempting to explain the variance seen between the results for general wards and the ICU, an analysis of alcohol-based handrub solution consumption as a marker of hand-hygiene behavior indicated that a remarkable increase in consumption occurred in the ICUs while a less pronounced increase occurred in the general wards. “This finding might explain the observed decline in the HAI incidence after starting the campaign in the ICUs, which was not observed on the general wards.” Dr. Hagel and his colleagues suggested.
The authors discussed how several confounding factors that influenced the incidence of HAIs needed to be considered. As a consequence of the improvement in HAI management, the number of collected blood culture sets nearly doubled hospital-wide from 13,126 to 25,805 per year between 2011 and 2014, which likely undermined the study objective, they stated. The increase in cultures may have impacted the number of overall HAIs found.
“Although the primary aim of the study of reducing the overall incidence of HAIs was not achieved, the study demonstrated a decline of severe HAIs in patients in ICUs in the second surveillance period. Whether this result was a consequence of the ICP or a general improvement in HAI management remains unclear,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010].
A hospital-wide infection control program (ICP) was found to be associated with reduced health care-associated severe sepsis/septic shock or death in the ICU, but it was not clear whether this decrease was a consequence of the ICP or because of a concomitant improvement in HAI case management, according to a the results of a prospective analysis.
In addition, there was no significant decrease in overall HAIs seen despite implementation of the program, according to the report published online in Clinical Microbiology and Infection (doi: 10.1016/j.cmi.2018.07.010), according to Stefan Hagel, MD, of the Institute for Infectious Diseases and Infection Control, Jena (Germany) University Hospital, and his colleagues.
They assessed two surveillance periods (September 2011 to August 2012 and May 2013 to August 2014). The ICP started in October 2012, and included hand-hygiene promotion and bundle implementation for common HAIs.
The data were analyzed by segmented mixed-effects Poisson regression and multi-state models and reported as adjusted incidence rate ratios (aIRR) and 50 adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
In the first period, 62,154 patients were under surveillance, with 1,568 HAIs identified in 1,170 patients (4.3/100 admissions) and 2,336 HAIs identified in 1,711 patients (4.9/100 admissions) in the second surveillance period. No differences were found in the overall HAI incidence rates between the periods in the general wards and ICUs. There was only a slight decline in the incidence rate of HAIs in the ICUs (aIRR 0.98 [0.97, 1.00] per 1-week increment), compared with the general wards (aIRR 1.01 [1.00, 1.02]).
However, a reduction in severe HAIs (aIRR 0.13 [0.05, 0.32]) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56 [0.31, 0.99]) were observed in the second period in the ICUs.
In attempting to explain the variance seen between the results for general wards and the ICU, an analysis of alcohol-based handrub solution consumption as a marker of hand-hygiene behavior indicated that a remarkable increase in consumption occurred in the ICUs while a less pronounced increase occurred in the general wards. “This finding might explain the observed decline in the HAI incidence after starting the campaign in the ICUs, which was not observed on the general wards.” Dr. Hagel and his colleagues suggested.
The authors discussed how several confounding factors that influenced the incidence of HAIs needed to be considered. As a consequence of the improvement in HAI management, the number of collected blood culture sets nearly doubled hospital-wide from 13,126 to 25,805 per year between 2011 and 2014, which likely undermined the study objective, they stated. The increase in cultures may have impacted the number of overall HAIs found.
“Although the primary aim of the study of reducing the overall incidence of HAIs was not achieved, the study demonstrated a decline of severe HAIs in patients in ICUs in the second surveillance period. Whether this result was a consequence of the ICP or a general improvement in HAI management remains unclear,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010].
A hospital-wide infection control program (ICP) was found to be associated with reduced health care-associated severe sepsis/septic shock or death in the ICU, but it was not clear whether this decrease was a consequence of the ICP or because of a concomitant improvement in HAI case management, according to a the results of a prospective analysis.
In addition, there was no significant decrease in overall HAIs seen despite implementation of the program, according to the report published online in Clinical Microbiology and Infection (doi: 10.1016/j.cmi.2018.07.010), according to Stefan Hagel, MD, of the Institute for Infectious Diseases and Infection Control, Jena (Germany) University Hospital, and his colleagues.
They assessed two surveillance periods (September 2011 to August 2012 and May 2013 to August 2014). The ICP started in October 2012, and included hand-hygiene promotion and bundle implementation for common HAIs.
The data were analyzed by segmented mixed-effects Poisson regression and multi-state models and reported as adjusted incidence rate ratios (aIRR) and 50 adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
In the first period, 62,154 patients were under surveillance, with 1,568 HAIs identified in 1,170 patients (4.3/100 admissions) and 2,336 HAIs identified in 1,711 patients (4.9/100 admissions) in the second surveillance period. No differences were found in the overall HAI incidence rates between the periods in the general wards and ICUs. There was only a slight decline in the incidence rate of HAIs in the ICUs (aIRR 0.98 [0.97, 1.00] per 1-week increment), compared with the general wards (aIRR 1.01 [1.00, 1.02]).
However, a reduction in severe HAIs (aIRR 0.13 [0.05, 0.32]) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56 [0.31, 0.99]) were observed in the second period in the ICUs.
In attempting to explain the variance seen between the results for general wards and the ICU, an analysis of alcohol-based handrub solution consumption as a marker of hand-hygiene behavior indicated that a remarkable increase in consumption occurred in the ICUs while a less pronounced increase occurred in the general wards. “This finding might explain the observed decline in the HAI incidence after starting the campaign in the ICUs, which was not observed on the general wards.” Dr. Hagel and his colleagues suggested.
The authors discussed how several confounding factors that influenced the incidence of HAIs needed to be considered. As a consequence of the improvement in HAI management, the number of collected blood culture sets nearly doubled hospital-wide from 13,126 to 25,805 per year between 2011 and 2014, which likely undermined the study objective, they stated. The increase in cultures may have impacted the number of overall HAIs found.
“Although the primary aim of the study of reducing the overall incidence of HAIs was not achieved, the study demonstrated a decline of severe HAIs in patients in ICUs in the second surveillance period. Whether this result was a consequence of the ICP or a general improvement in HAI management remains unclear,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010].
FROM CLINICAL MICROBIOLOGY AND INFECTION
Key clinical point: Hand hygiene was the key factor associated with a decrease in severe HAIs.
Major finding: A reduction in severe HAIs (aIRR 0.13) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56]) were observed.
Study details: A prospective database analysis of more nearly 65,000 hospitalized patients.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010.
Fewer groin infections with closed incision negative pressure therapy after vascular surgery
Closed incision negative pressure therapy (ciNPT) was found to reduce surgical site infections (SSI) in vascular surgery, according to the results of a prospective, randomized, industry-sponsored trial of patients who underwent vascular surgery for peripheral artery disease (PAD) published online in the European Journal of Vascular and Endovascular Surgery.
The investigator-initiated Reduction of Groin Wound Infections After Vascular Surgery by Using an Incision Management System trial (NCT02395159) included 204 patients who underwent vascular surgery involving longitudinal groin incision to treat the lower extremity or the iliac arteries between July 2015 and May 2017 at two study centers.
The primary endpoint was the occurrence of SSI assessed by the Szilagyi classification (grades I-III). The mean patient age was nearly 67 years and 70% were men. In terms of PAD staging, 52% were stage 2B, 28% were stage 3, and 19% were stage 4. Among the patients, 45% had a previous groin incision and 42% had diabetes.
All patients underwent similar preoperative treatment: hair shaving and preparation with Poly Alcohol (Antiseptica, Pulheim, Germany) and Braunoderm (Braun, Melsungen, Germany). At 30 minutes preincision, patients received intravenous antibiotic treatment (1.5 g cefuroxime or 600 mg clindamycin, if allergic to penicillin). After closure, the incision and surrounding skin area was cleaned and dried using sterile gauze. In the control group, a sterile adhesive wound dressing was applied to the wound, which was changed daily. In the treatment group, ciNPT was applied under sterile conditions in the operating room using the Prevena device, which exerts a continuous negative pressure of 125 mm Hg on the closed incision during the time of application. The device was removed at 5-7 days postoperatively, and no further wound dressings were used in the treatment group unless an SSI occurred.
The control group experienced more frequent SSIs (33.3%) than the intervention group (13.2%) (P =.0015). This difference was based on an increased rate of Szilagyi grade I SSI in the control group (24.6% vs. 8.1%, P = .0012), according to Alexander Gombert, MD, of the University Hospital Aachen (Germany), and his colleagues. The absolute risk difference based on the Szilagyi classification was –20.1 per 100 (95% confidence interval, –31.9 to –8.2).
In addition, there was a statistically significantly lower rate of SSI when using ciNPT within the subgroups at greater risk of infection, compared with controls: PAD stage greater than or equal to 3 (P less than .001), body mass index greater than 25 kg/m2 (P less than .001), and previous groin incision (P = .016).
There were no statistical differences between the two groups in Szilagyi grade II and III SSIs (which occurred in 5.8% of all procedures).
No potentially device-related complications were observed in the trial and there were no failures of the device seen.
“The use of ciNPT rather than standard wound dressing after groin incision as access for vascular surgery was associated with a reduced rate of superficial SSI classified by Szilagyi, suggesting that ciNPT may be useful for reducing the SSI rate among high-risk patients,” the researchers concluded.
The trial was funded by Acelity. Dr. Gombert received travel grants from Acelity.
SOURCE: Gombert A et al. Eur J Vasc Surg. 2018 Jul 2. doi: 10.1016/j.ejvs.2018.05.018.
Closed incision negative pressure therapy (ciNPT) was found to reduce surgical site infections (SSI) in vascular surgery, according to the results of a prospective, randomized, industry-sponsored trial of patients who underwent vascular surgery for peripheral artery disease (PAD) published online in the European Journal of Vascular and Endovascular Surgery.
The investigator-initiated Reduction of Groin Wound Infections After Vascular Surgery by Using an Incision Management System trial (NCT02395159) included 204 patients who underwent vascular surgery involving longitudinal groin incision to treat the lower extremity or the iliac arteries between July 2015 and May 2017 at two study centers.
The primary endpoint was the occurrence of SSI assessed by the Szilagyi classification (grades I-III). The mean patient age was nearly 67 years and 70% were men. In terms of PAD staging, 52% were stage 2B, 28% were stage 3, and 19% were stage 4. Among the patients, 45% had a previous groin incision and 42% had diabetes.
All patients underwent similar preoperative treatment: hair shaving and preparation with Poly Alcohol (Antiseptica, Pulheim, Germany) and Braunoderm (Braun, Melsungen, Germany). At 30 minutes preincision, patients received intravenous antibiotic treatment (1.5 g cefuroxime or 600 mg clindamycin, if allergic to penicillin). After closure, the incision and surrounding skin area was cleaned and dried using sterile gauze. In the control group, a sterile adhesive wound dressing was applied to the wound, which was changed daily. In the treatment group, ciNPT was applied under sterile conditions in the operating room using the Prevena device, which exerts a continuous negative pressure of 125 mm Hg on the closed incision during the time of application. The device was removed at 5-7 days postoperatively, and no further wound dressings were used in the treatment group unless an SSI occurred.
The control group experienced more frequent SSIs (33.3%) than the intervention group (13.2%) (P =.0015). This difference was based on an increased rate of Szilagyi grade I SSI in the control group (24.6% vs. 8.1%, P = .0012), according to Alexander Gombert, MD, of the University Hospital Aachen (Germany), and his colleagues. The absolute risk difference based on the Szilagyi classification was –20.1 per 100 (95% confidence interval, –31.9 to –8.2).
In addition, there was a statistically significantly lower rate of SSI when using ciNPT within the subgroups at greater risk of infection, compared with controls: PAD stage greater than or equal to 3 (P less than .001), body mass index greater than 25 kg/m2 (P less than .001), and previous groin incision (P = .016).
There were no statistical differences between the two groups in Szilagyi grade II and III SSIs (which occurred in 5.8% of all procedures).
No potentially device-related complications were observed in the trial and there were no failures of the device seen.
“The use of ciNPT rather than standard wound dressing after groin incision as access for vascular surgery was associated with a reduced rate of superficial SSI classified by Szilagyi, suggesting that ciNPT may be useful for reducing the SSI rate among high-risk patients,” the researchers concluded.
The trial was funded by Acelity. Dr. Gombert received travel grants from Acelity.
SOURCE: Gombert A et al. Eur J Vasc Surg. 2018 Jul 2. doi: 10.1016/j.ejvs.2018.05.018.
Closed incision negative pressure therapy (ciNPT) was found to reduce surgical site infections (SSI) in vascular surgery, according to the results of a prospective, randomized, industry-sponsored trial of patients who underwent vascular surgery for peripheral artery disease (PAD) published online in the European Journal of Vascular and Endovascular Surgery.
The investigator-initiated Reduction of Groin Wound Infections After Vascular Surgery by Using an Incision Management System trial (NCT02395159) included 204 patients who underwent vascular surgery involving longitudinal groin incision to treat the lower extremity or the iliac arteries between July 2015 and May 2017 at two study centers.
The primary endpoint was the occurrence of SSI assessed by the Szilagyi classification (grades I-III). The mean patient age was nearly 67 years and 70% were men. In terms of PAD staging, 52% were stage 2B, 28% were stage 3, and 19% were stage 4. Among the patients, 45% had a previous groin incision and 42% had diabetes.
All patients underwent similar preoperative treatment: hair shaving and preparation with Poly Alcohol (Antiseptica, Pulheim, Germany) and Braunoderm (Braun, Melsungen, Germany). At 30 minutes preincision, patients received intravenous antibiotic treatment (1.5 g cefuroxime or 600 mg clindamycin, if allergic to penicillin). After closure, the incision and surrounding skin area was cleaned and dried using sterile gauze. In the control group, a sterile adhesive wound dressing was applied to the wound, which was changed daily. In the treatment group, ciNPT was applied under sterile conditions in the operating room using the Prevena device, which exerts a continuous negative pressure of 125 mm Hg on the closed incision during the time of application. The device was removed at 5-7 days postoperatively, and no further wound dressings were used in the treatment group unless an SSI occurred.
The control group experienced more frequent SSIs (33.3%) than the intervention group (13.2%) (P =.0015). This difference was based on an increased rate of Szilagyi grade I SSI in the control group (24.6% vs. 8.1%, P = .0012), according to Alexander Gombert, MD, of the University Hospital Aachen (Germany), and his colleagues. The absolute risk difference based on the Szilagyi classification was –20.1 per 100 (95% confidence interval, –31.9 to –8.2).
In addition, there was a statistically significantly lower rate of SSI when using ciNPT within the subgroups at greater risk of infection, compared with controls: PAD stage greater than or equal to 3 (P less than .001), body mass index greater than 25 kg/m2 (P less than .001), and previous groin incision (P = .016).
There were no statistical differences between the two groups in Szilagyi grade II and III SSIs (which occurred in 5.8% of all procedures).
No potentially device-related complications were observed in the trial and there were no failures of the device seen.
“The use of ciNPT rather than standard wound dressing after groin incision as access for vascular surgery was associated with a reduced rate of superficial SSI classified by Szilagyi, suggesting that ciNPT may be useful for reducing the SSI rate among high-risk patients,” the researchers concluded.
The trial was funded by Acelity. Dr. Gombert received travel grants from Acelity.
SOURCE: Gombert A et al. Eur J Vasc Surg. 2018 Jul 2. doi: 10.1016/j.ejvs.2018.05.018.
FROM THE EUROPEAN JOURNAL OF VASCULAR AND ENDOVASCULAR SURGERY
Key clinical point: Closed incision negative pressure therapy lessened the incidence of groin infection after vascular surgery.
Major finding: The control group experienced more frequent surgical site infections (33.3%) than the intervention group (13.2%) (P =.0015).
Study details: A randomized, controlled trial of 204 patients with peripheral artery disease who underwent vascular surgery.
Disclosures: The trial was funded by Acelity. Dr. Gombert received travel grants from Acelity.
Source: Gombert A et al. Eur J Vasc Surg. 2018 Jul 2. doi: 10.1016/j.ejvs.2018.05.018.