User login
PD-1 inhibitor granted accelerated approval for cHL

Photo courtesy of Business Wire
The US Food and Drug Administration (FDA) has granted accelerated approval for the PD-1 inhibitor nivolumab (Opdivo) to treat classical Hodgkin lymphoma (cHL).
The drug is approved to treat patients with relapsed or refractory cHL who have received an autologous hematopoietic stem cell transplant (HSCT) and post-transplant brentuximab vedotin.
Nivolumab received accelerated approval because it has not yet shown a clinical benefit in these patients. The FDA’s accelerated approval program allows conditional approval of a drug that fills an unmet medical need for a serious condition.
Accelerated approval is based on a surrogate or intermediate endpoint—in this case, overall response rate—that is reasonably likely to predict clinical benefit. Continued approval of nivolumab for the aforementioned indication may be contingent upon verification of clinical benefit in confirmatory trials.
The FDA previously granted nivolumab breakthrough therapy designation, priority review status, and orphan drug designation.
Dosing and precautions
The recommended dose and schedule of nivolumab for cHL patients is 3 mg/kg intravenously every 2 weeks until disease progression or unacceptable toxicity.
The FDA added a new “Warning and Precaution” to the label for nivolumab, regarding complications of allogeneic HSCT after nivolumab.
Transplant-related deaths have occurred. So the FDA said healthcare professionals should follow patients closely for early evidence of transplant-related complications, such as hyperacute graft-versus-host disease (GVHD), severe acute GVHD, steroid-requiring febrile syndrome, hepatic veno-occlusive disease, and other immune-mediated adverse reactions.
The FDA has required the manufacturer of nivolumab, Bristol-Myers Squibb, to further study the safety of allogeneic HSCT after nivolumab.
Full prescribing information for the drug is available here.
Trials of nivolumab
The FDA granted nivolumab accelerated approval in cHL patients based on the results of 2 single-arm, multicenter trials—the phase 1 Checkmate 039 trial (presented at ICML last year) and the phase 2 CheckMate 205 trial (to be presented at ASCO 2016).
Efficacy
Thus far, researchers have evaluated the efficacy of nivolumab in 95 cHL patients from both trials. All of these patients previously received an autologous HSCT and post-transplant brentuximab vedotin. They received a median of 5 prior systemic regimens (range, 3 to 15).
The patients received a median of 17 doses of nivolumab (range, 3 to 48). The overall response rate was 65%, and the complete response rate was 7%.
The median time to response was 2.1 months (range, 0.7 to 5.7), and the estimated median duration of response was 8.7 months (range, 0+ to 23.1+).
Safety
Researchers evaluated the safety of nivolumab in 263 patients with relapsed or refractory cHL. Ninety-eight percent of these patients had received an autologous HSCT. The patients received a median of 10 doses of nivolumab (range, 1 to 48) at the approved dose and schedule.
The most common (≥20%) adverse events (AEs) of any grade were fatigue, upper respiratory tract infection, cough, pyrexia, and diarrhea.
Additional common (≥10%) AEs included rash, pruritus, musculoskeletal pain, nausea, vomiting, abdominal pain, headache, peripheral neuropathy, arthralgia, dyspnea, infusion-related reactions, and hypothyroidism or thyroiditis.
Serious AEs were reported in 21% of patients. The most common, reported in 1% to 3% of patients, were pneumonia, pleural effusion, pneumonitis, pyrexia, infusion-related reaction, and rash. ![]()

Photo courtesy of Business Wire
The US Food and Drug Administration (FDA) has granted accelerated approval for the PD-1 inhibitor nivolumab (Opdivo) to treat classical Hodgkin lymphoma (cHL).
The drug is approved to treat patients with relapsed or refractory cHL who have received an autologous hematopoietic stem cell transplant (HSCT) and post-transplant brentuximab vedotin.
Nivolumab received accelerated approval because it has not yet shown a clinical benefit in these patients. The FDA’s accelerated approval program allows conditional approval of a drug that fills an unmet medical need for a serious condition.
Accelerated approval is based on a surrogate or intermediate endpoint—in this case, overall response rate—that is reasonably likely to predict clinical benefit. Continued approval of nivolumab for the aforementioned indication may be contingent upon verification of clinical benefit in confirmatory trials.
The FDA previously granted nivolumab breakthrough therapy designation, priority review status, and orphan drug designation.
Dosing and precautions
The recommended dose and schedule of nivolumab for cHL patients is 3 mg/kg intravenously every 2 weeks until disease progression or unacceptable toxicity.
The FDA added a new “Warning and Precaution” to the label for nivolumab, regarding complications of allogeneic HSCT after nivolumab.
Transplant-related deaths have occurred. So the FDA said healthcare professionals should follow patients closely for early evidence of transplant-related complications, such as hyperacute graft-versus-host disease (GVHD), severe acute GVHD, steroid-requiring febrile syndrome, hepatic veno-occlusive disease, and other immune-mediated adverse reactions.
The FDA has required the manufacturer of nivolumab, Bristol-Myers Squibb, to further study the safety of allogeneic HSCT after nivolumab.
Full prescribing information for the drug is available here.
Trials of nivolumab
The FDA granted nivolumab accelerated approval in cHL patients based on the results of 2 single-arm, multicenter trials—the phase 1 Checkmate 039 trial (presented at ICML last year) and the phase 2 CheckMate 205 trial (to be presented at ASCO 2016).
Efficacy
Thus far, researchers have evaluated the efficacy of nivolumab in 95 cHL patients from both trials. All of these patients previously received an autologous HSCT and post-transplant brentuximab vedotin. They received a median of 5 prior systemic regimens (range, 3 to 15).
The patients received a median of 17 doses of nivolumab (range, 3 to 48). The overall response rate was 65%, and the complete response rate was 7%.
The median time to response was 2.1 months (range, 0.7 to 5.7), and the estimated median duration of response was 8.7 months (range, 0+ to 23.1+).
Safety
Researchers evaluated the safety of nivolumab in 263 patients with relapsed or refractory cHL. Ninety-eight percent of these patients had received an autologous HSCT. The patients received a median of 10 doses of nivolumab (range, 1 to 48) at the approved dose and schedule.
The most common (≥20%) adverse events (AEs) of any grade were fatigue, upper respiratory tract infection, cough, pyrexia, and diarrhea.
Additional common (≥10%) AEs included rash, pruritus, musculoskeletal pain, nausea, vomiting, abdominal pain, headache, peripheral neuropathy, arthralgia, dyspnea, infusion-related reactions, and hypothyroidism or thyroiditis.
Serious AEs were reported in 21% of patients. The most common, reported in 1% to 3% of patients, were pneumonia, pleural effusion, pneumonitis, pyrexia, infusion-related reaction, and rash. ![]()

Photo courtesy of Business Wire
The US Food and Drug Administration (FDA) has granted accelerated approval for the PD-1 inhibitor nivolumab (Opdivo) to treat classical Hodgkin lymphoma (cHL).
The drug is approved to treat patients with relapsed or refractory cHL who have received an autologous hematopoietic stem cell transplant (HSCT) and post-transplant brentuximab vedotin.
Nivolumab received accelerated approval because it has not yet shown a clinical benefit in these patients. The FDA’s accelerated approval program allows conditional approval of a drug that fills an unmet medical need for a serious condition.
Accelerated approval is based on a surrogate or intermediate endpoint—in this case, overall response rate—that is reasonably likely to predict clinical benefit. Continued approval of nivolumab for the aforementioned indication may be contingent upon verification of clinical benefit in confirmatory trials.
The FDA previously granted nivolumab breakthrough therapy designation, priority review status, and orphan drug designation.
Dosing and precautions
The recommended dose and schedule of nivolumab for cHL patients is 3 mg/kg intravenously every 2 weeks until disease progression or unacceptable toxicity.
The FDA added a new “Warning and Precaution” to the label for nivolumab, regarding complications of allogeneic HSCT after nivolumab.
Transplant-related deaths have occurred. So the FDA said healthcare professionals should follow patients closely for early evidence of transplant-related complications, such as hyperacute graft-versus-host disease (GVHD), severe acute GVHD, steroid-requiring febrile syndrome, hepatic veno-occlusive disease, and other immune-mediated adverse reactions.
The FDA has required the manufacturer of nivolumab, Bristol-Myers Squibb, to further study the safety of allogeneic HSCT after nivolumab.
Full prescribing information for the drug is available here.
Trials of nivolumab
The FDA granted nivolumab accelerated approval in cHL patients based on the results of 2 single-arm, multicenter trials—the phase 1 Checkmate 039 trial (presented at ICML last year) and the phase 2 CheckMate 205 trial (to be presented at ASCO 2016).
Efficacy
Thus far, researchers have evaluated the efficacy of nivolumab in 95 cHL patients from both trials. All of these patients previously received an autologous HSCT and post-transplant brentuximab vedotin. They received a median of 5 prior systemic regimens (range, 3 to 15).
The patients received a median of 17 doses of nivolumab (range, 3 to 48). The overall response rate was 65%, and the complete response rate was 7%.
The median time to response was 2.1 months (range, 0.7 to 5.7), and the estimated median duration of response was 8.7 months (range, 0+ to 23.1+).
Safety
Researchers evaluated the safety of nivolumab in 263 patients with relapsed or refractory cHL. Ninety-eight percent of these patients had received an autologous HSCT. The patients received a median of 10 doses of nivolumab (range, 1 to 48) at the approved dose and schedule.
The most common (≥20%) adverse events (AEs) of any grade were fatigue, upper respiratory tract infection, cough, pyrexia, and diarrhea.
Additional common (≥10%) AEs included rash, pruritus, musculoskeletal pain, nausea, vomiting, abdominal pain, headache, peripheral neuropathy, arthralgia, dyspnea, infusion-related reactions, and hypothyroidism or thyroiditis.
Serious AEs were reported in 21% of patients. The most common, reported in 1% to 3% of patients, were pneumonia, pleural effusion, pneumonitis, pyrexia, infusion-related reaction, and rash. ![]()
FDA grants accelerated approval to nivolumab for Hodgkin lymphoma
The Food and Drug Administration has granted accelerated approval to nivolumab for the treatment of patients with classical Hodgkin lymphoma (cHL) that has relapsed or progressed after autologous hematopoietic stem cell transplantation (HSCT) and posttransplantation brentuximab vedotin.
Approval was based on a 65% objective response rate in 95 patients treated with nivolumab following autologous HSCT and posttransplantation brentuximab vedotin. All patients in the single-arm, multicenter trial had relapsed or refractory cHL and were enrolled regardless of PD-L1 expression status. Patients received a median of 17 doses of nivolumab, the FDA said in a written statement.
The median time to response was 2.1 months (range, 0.7-5.7 months). The estimated median duration of response was 8.7 months.
The FDA also issued a warning for complications of allogeneic HSCT after nivolumab, reporting that transplant-related deaths have occurred. Health care professionals should follow patients closely for early evidence of transplant-related complications, such as hyperacute graft-versus-host disease (GVHD), severe acute GVHD, steroid-requiring febrile syndrome, hepatic veno-occlusive disease, and other immune-mediated adverse reactions, they said.
The most common adverse reactions in a second single-arm study used to evaluate safety (n = 263) were upper respiratory tract infection, cough, pyrexia, and diarrhea. Other immune-mediated adverse reactions, occurring in 1%-5% of patients, included rash, pneumonitis, hepatitis, hyperthyroidism, and colitis. The most common serious adverse reactions, which were reported in 1%-3% of patients, were pneumonia, pleural effusion, pneumonitis, pyrexia, infusion-related reaction, and rash.
Nivolumab is marketed as Opdivo by Bristol-Myers Squibb and has been previously approved to treat advanced renal cell carcinoma, lung cancer, and melanoma.
On Twitter @NikolaidesLaura
The Food and Drug Administration has granted accelerated approval to nivolumab for the treatment of patients with classical Hodgkin lymphoma (cHL) that has relapsed or progressed after autologous hematopoietic stem cell transplantation (HSCT) and posttransplantation brentuximab vedotin.
Approval was based on a 65% objective response rate in 95 patients treated with nivolumab following autologous HSCT and posttransplantation brentuximab vedotin. All patients in the single-arm, multicenter trial had relapsed or refractory cHL and were enrolled regardless of PD-L1 expression status. Patients received a median of 17 doses of nivolumab, the FDA said in a written statement.
The median time to response was 2.1 months (range, 0.7-5.7 months). The estimated median duration of response was 8.7 months.
The FDA also issued a warning for complications of allogeneic HSCT after nivolumab, reporting that transplant-related deaths have occurred. Health care professionals should follow patients closely for early evidence of transplant-related complications, such as hyperacute graft-versus-host disease (GVHD), severe acute GVHD, steroid-requiring febrile syndrome, hepatic veno-occlusive disease, and other immune-mediated adverse reactions, they said.
The most common adverse reactions in a second single-arm study used to evaluate safety (n = 263) were upper respiratory tract infection, cough, pyrexia, and diarrhea. Other immune-mediated adverse reactions, occurring in 1%-5% of patients, included rash, pneumonitis, hepatitis, hyperthyroidism, and colitis. The most common serious adverse reactions, which were reported in 1%-3% of patients, were pneumonia, pleural effusion, pneumonitis, pyrexia, infusion-related reaction, and rash.
Nivolumab is marketed as Opdivo by Bristol-Myers Squibb and has been previously approved to treat advanced renal cell carcinoma, lung cancer, and melanoma.
On Twitter @NikolaidesLaura
The Food and Drug Administration has granted accelerated approval to nivolumab for the treatment of patients with classical Hodgkin lymphoma (cHL) that has relapsed or progressed after autologous hematopoietic stem cell transplantation (HSCT) and posttransplantation brentuximab vedotin.
Approval was based on a 65% objective response rate in 95 patients treated with nivolumab following autologous HSCT and posttransplantation brentuximab vedotin. All patients in the single-arm, multicenter trial had relapsed or refractory cHL and were enrolled regardless of PD-L1 expression status. Patients received a median of 17 doses of nivolumab, the FDA said in a written statement.
The median time to response was 2.1 months (range, 0.7-5.7 months). The estimated median duration of response was 8.7 months.
The FDA also issued a warning for complications of allogeneic HSCT after nivolumab, reporting that transplant-related deaths have occurred. Health care professionals should follow patients closely for early evidence of transplant-related complications, such as hyperacute graft-versus-host disease (GVHD), severe acute GVHD, steroid-requiring febrile syndrome, hepatic veno-occlusive disease, and other immune-mediated adverse reactions, they said.
The most common adverse reactions in a second single-arm study used to evaluate safety (n = 263) were upper respiratory tract infection, cough, pyrexia, and diarrhea. Other immune-mediated adverse reactions, occurring in 1%-5% of patients, included rash, pneumonitis, hepatitis, hyperthyroidism, and colitis. The most common serious adverse reactions, which were reported in 1%-3% of patients, were pneumonia, pleural effusion, pneumonitis, pyrexia, infusion-related reaction, and rash.
Nivolumab is marketed as Opdivo by Bristol-Myers Squibb and has been previously approved to treat advanced renal cell carcinoma, lung cancer, and melanoma.
On Twitter @NikolaidesLaura
Low transformation rate in nodular lymphocyte–predominant Hodgkin lymphoma
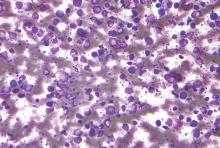
Fewer than 8% of cases of nodular lymphocyte–predominant Hodgkin lymphoma (NLPHL) transformed to diffuse large B-cell lymphoma (DLBCL), based on a large prospective single-center study with long-term follow-up.
This rate was lower than the risk of transformation reported for transformed follicular lymphoma or chronic lymphocytic leukemia, according to Dr. Saad Kenderian and his associates at the Mayo Clinic, Rochester, Minn. Transformation was significantly associated with splenic involvement at presentation and with prior chemotherapy exposure, but did not worsen overall survival, they added.
“To our knowledge, this cohort represents the largest analysis to date of consecutive patients with NLPHL,” they said.
The study comprised 222 patients with newly diagnosed NLPHL who were treated at Mayo Clinic between 1970 and 2011. Median age at diagnosis was 40 years, and two-thirds of patients were men. The median follow-up period was 16 years (Blood 2016;12:1960-6. doi: 10.1182/blood-2015-08-665505).
During follow up, 17 cases (7.6%) transformed to DLBCL, for a transformation rate of 0.74 cases for every 100 patient-years, the investigators said. Median time to transformation was 35 months (range, 6-268 months). Predictors of transformation included any prior chemotherapy exposure (P = .04) and splenic involvement (P = .03). The rates of 40-year freedom from transformation were 87% when there was no splenic involvement and 21% when the spleen was involved, and were 87% if radiation therapy was used as a single modality compared with 77% in patients treated with prior chemotherapy or chemoradiation.
Five-year overall survival was 76% in patients with transformed disease, which was similar to overall survival among patients whose disease did not transform to DLBCL, the researchers noted.
Other studies of NLPHL have reported anywhere from a 2% to a 17% transformation rate, but those studies had smaller sample sizes, shorter follow-up periods, and less rigorous enrollment criteria and methods to confirm transformation, the investigators noted. “The finding of splenic involvement as a risk factor for transformation was reported by previous investigators. Interestingly, the association between exposure to prior chemotherapy and reduced freedom from transformation has not been reported in the past, but it has been observed in other low-grade lymphoma studies,” they added. “In contrast to follicular lymphoma, transformed NLPHL is not associated with an adverse impact on OS, suggesting a possibly different biology of transformation.”
The research was partially supported by Lymphoma SPORE and the Predolin Foundation. The investigators had no disclosures.
Kenderian et al. report a lower rate of transformation (7.6%) to diffuse large B-cell lymphoma for patients with nodular lymphocyte–predominant Hodgkin lymphoma compared with other series and found that transformation did not have a negative impact on overall survival. Reassuringly, even if transformation occurs, it is generally at a low rate. Also, these patients do well with additional treatment and do not have worse overall survival. At the MD Anderson Cancer Center, we have used a regimen based on R-CHOP and have not seen transformations. But only through large cooperative clinical trials can we determine whether R-CHOP or other more novel regimens are actually superior to ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) or rituximab (R)-ABVD for patients at high risk of transformation.
Dr. Michelle Fanale is at the University of Texas MD Anderson Cancer Center, Houston. She had no disclosures. These comments are from her editorial (Blood 2016;1927:1946-7 doi: 10.1182/blood-2016-03-699108).
Kenderian et al. report a lower rate of transformation (7.6%) to diffuse large B-cell lymphoma for patients with nodular lymphocyte–predominant Hodgkin lymphoma compared with other series and found that transformation did not have a negative impact on overall survival. Reassuringly, even if transformation occurs, it is generally at a low rate. Also, these patients do well with additional treatment and do not have worse overall survival. At the MD Anderson Cancer Center, we have used a regimen based on R-CHOP and have not seen transformations. But only through large cooperative clinical trials can we determine whether R-CHOP or other more novel regimens are actually superior to ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) or rituximab (R)-ABVD for patients at high risk of transformation.
Dr. Michelle Fanale is at the University of Texas MD Anderson Cancer Center, Houston. She had no disclosures. These comments are from her editorial (Blood 2016;1927:1946-7 doi: 10.1182/blood-2016-03-699108).
Kenderian et al. report a lower rate of transformation (7.6%) to diffuse large B-cell lymphoma for patients with nodular lymphocyte–predominant Hodgkin lymphoma compared with other series and found that transformation did not have a negative impact on overall survival. Reassuringly, even if transformation occurs, it is generally at a low rate. Also, these patients do well with additional treatment and do not have worse overall survival. At the MD Anderson Cancer Center, we have used a regimen based on R-CHOP and have not seen transformations. But only through large cooperative clinical trials can we determine whether R-CHOP or other more novel regimens are actually superior to ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) or rituximab (R)-ABVD for patients at high risk of transformation.
Dr. Michelle Fanale is at the University of Texas MD Anderson Cancer Center, Houston. She had no disclosures. These comments are from her editorial (Blood 2016;1927:1946-7 doi: 10.1182/blood-2016-03-699108).
Fewer than 8% of cases of nodular lymphocyte–predominant Hodgkin lymphoma (NLPHL) transformed to diffuse large B-cell lymphoma (DLBCL), based on a large prospective single-center study with long-term follow-up.
This rate was lower than the risk of transformation reported for transformed follicular lymphoma or chronic lymphocytic leukemia, according to Dr. Saad Kenderian and his associates at the Mayo Clinic, Rochester, Minn. Transformation was significantly associated with splenic involvement at presentation and with prior chemotherapy exposure, but did not worsen overall survival, they added.
“To our knowledge, this cohort represents the largest analysis to date of consecutive patients with NLPHL,” they said.
The study comprised 222 patients with newly diagnosed NLPHL who were treated at Mayo Clinic between 1970 and 2011. Median age at diagnosis was 40 years, and two-thirds of patients were men. The median follow-up period was 16 years (Blood 2016;12:1960-6. doi: 10.1182/blood-2015-08-665505).
During follow up, 17 cases (7.6%) transformed to DLBCL, for a transformation rate of 0.74 cases for every 100 patient-years, the investigators said. Median time to transformation was 35 months (range, 6-268 months). Predictors of transformation included any prior chemotherapy exposure (P = .04) and splenic involvement (P = .03). The rates of 40-year freedom from transformation were 87% when there was no splenic involvement and 21% when the spleen was involved, and were 87% if radiation therapy was used as a single modality compared with 77% in patients treated with prior chemotherapy or chemoradiation.
Five-year overall survival was 76% in patients with transformed disease, which was similar to overall survival among patients whose disease did not transform to DLBCL, the researchers noted.
Other studies of NLPHL have reported anywhere from a 2% to a 17% transformation rate, but those studies had smaller sample sizes, shorter follow-up periods, and less rigorous enrollment criteria and methods to confirm transformation, the investigators noted. “The finding of splenic involvement as a risk factor for transformation was reported by previous investigators. Interestingly, the association between exposure to prior chemotherapy and reduced freedom from transformation has not been reported in the past, but it has been observed in other low-grade lymphoma studies,” they added. “In contrast to follicular lymphoma, transformed NLPHL is not associated with an adverse impact on OS, suggesting a possibly different biology of transformation.”
The research was partially supported by Lymphoma SPORE and the Predolin Foundation. The investigators had no disclosures.
Fewer than 8% of cases of nodular lymphocyte–predominant Hodgkin lymphoma (NLPHL) transformed to diffuse large B-cell lymphoma (DLBCL), based on a large prospective single-center study with long-term follow-up.
This rate was lower than the risk of transformation reported for transformed follicular lymphoma or chronic lymphocytic leukemia, according to Dr. Saad Kenderian and his associates at the Mayo Clinic, Rochester, Minn. Transformation was significantly associated with splenic involvement at presentation and with prior chemotherapy exposure, but did not worsen overall survival, they added.
“To our knowledge, this cohort represents the largest analysis to date of consecutive patients with NLPHL,” they said.
The study comprised 222 patients with newly diagnosed NLPHL who were treated at Mayo Clinic between 1970 and 2011. Median age at diagnosis was 40 years, and two-thirds of patients were men. The median follow-up period was 16 years (Blood 2016;12:1960-6. doi: 10.1182/blood-2015-08-665505).
During follow up, 17 cases (7.6%) transformed to DLBCL, for a transformation rate of 0.74 cases for every 100 patient-years, the investigators said. Median time to transformation was 35 months (range, 6-268 months). Predictors of transformation included any prior chemotherapy exposure (P = .04) and splenic involvement (P = .03). The rates of 40-year freedom from transformation were 87% when there was no splenic involvement and 21% when the spleen was involved, and were 87% if radiation therapy was used as a single modality compared with 77% in patients treated with prior chemotherapy or chemoradiation.
Five-year overall survival was 76% in patients with transformed disease, which was similar to overall survival among patients whose disease did not transform to DLBCL, the researchers noted.
Other studies of NLPHL have reported anywhere from a 2% to a 17% transformation rate, but those studies had smaller sample sizes, shorter follow-up periods, and less rigorous enrollment criteria and methods to confirm transformation, the investigators noted. “The finding of splenic involvement as a risk factor for transformation was reported by previous investigators. Interestingly, the association between exposure to prior chemotherapy and reduced freedom from transformation has not been reported in the past, but it has been observed in other low-grade lymphoma studies,” they added. “In contrast to follicular lymphoma, transformed NLPHL is not associated with an adverse impact on OS, suggesting a possibly different biology of transformation.”
The research was partially supported by Lymphoma SPORE and the Predolin Foundation. The investigators had no disclosures.
FROM BLOOD
Key clinical point: The risk of transformation to diffuse large B-cell lymphoma is low in patients with nodular lymphocyte–predominant Hodgkin lymphoma.
Major finding: Only 7.6% of cases transformed over a median of 16 years of follow-up, and transformation did not worsen overall survival.
Data source: A prospective single-center study of 222 consecutive adults with NLPHL.
Disclosures: The research was partially supported by Lymphoma SPORE and the Predolin Foundation. The investigators had no disclosures.
Childhood cancer risk linked to mother’s birthplace

Photo by Nina Matthews
New research suggests a mother’s birthplace may affect the risk of certain cancers for Hispanic children.
The study showed that children of Hispanic mothers who were not born in the US had lower risks of brain cancers, neuroblastoma, and Wilms tumor, when compared to children of US-born Hispanic mothers and non-Hispanic white mothers born in the US.
However, all Hispanic children, regardless of where their mothers were born, had higher risks of acute leukemias and Hodgkin lymphoma but a lower risk of non-Hodgkin lymphoma (NHL).
Julia E. Heck, PhD, of the University of California, Los Angeles, and her colleagues reported these findings in JAMA Pediatrics.
The researchers used California birth records to identify children born from 1983 through 2011. Information on cancer cases came from California Cancer Registry records from 1988 to 2012.
The team restricted their analysis to children of US-born white, US-born Hispanic, and non-US-born Hispanic mothers. The study included 13,666 cases of children diagnosed with cancer before the age of 6 and 15,513,718 children who served as control subjects.
To assess the hazard ratios (HRs) for various cancers, the researchers used children of non-Hispanic white mothers as a reference (HR=1.00) and compared them to the children of non-US-born Hispanic mothers and US-born Hispanic mothers.
For children of non-US-born Hispanic mothers, the HR was 0.50 for glioma, 0.43 for astrocytoma, 0.47 for neuroblastoma, and 0.70 for Wilms tumor. For children of US-born Hispanic mothers, the HR was 0.71 for glioma, 0.62 for astrocytoma, 0.66 for neuroblastoma, and 0.88 for Wilms tumor.
When compared to non-Hispanic white children, Hispanic children had an increased risk of acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), and Hodgkin lymphoma but lower risks of NHL and Burkitt lymphoma.
For children of US-born Hispanic mothers, the HR was 1.20 for ALL, 1.28 for AML, 2.49 for Hodgkin lymphoma, 0.79 for NHL, and 0.69 for Burkitt lymphoma.
For children of non-US-born Hispanic mothers, the HR was 1.06 for ALL, 1.05 for AML, 2.35 for Hodgkin lymphoma, 0.76 for NHL, and 0.73 for Burkitt lymphoma.
The researchers said the differences observed between children of US-born and non-US-born Hispanic mothers may be explained by lifestyle differences and varying environmental exposures.
These factors may explain the differences in cancer incidence between Hispanic children and white children as well, but the differences may also be a result of genetic variation and infection exposures early in life. ![]()

Photo by Nina Matthews
New research suggests a mother’s birthplace may affect the risk of certain cancers for Hispanic children.
The study showed that children of Hispanic mothers who were not born in the US had lower risks of brain cancers, neuroblastoma, and Wilms tumor, when compared to children of US-born Hispanic mothers and non-Hispanic white mothers born in the US.
However, all Hispanic children, regardless of where their mothers were born, had higher risks of acute leukemias and Hodgkin lymphoma but a lower risk of non-Hodgkin lymphoma (NHL).
Julia E. Heck, PhD, of the University of California, Los Angeles, and her colleagues reported these findings in JAMA Pediatrics.
The researchers used California birth records to identify children born from 1983 through 2011. Information on cancer cases came from California Cancer Registry records from 1988 to 2012.
The team restricted their analysis to children of US-born white, US-born Hispanic, and non-US-born Hispanic mothers. The study included 13,666 cases of children diagnosed with cancer before the age of 6 and 15,513,718 children who served as control subjects.
To assess the hazard ratios (HRs) for various cancers, the researchers used children of non-Hispanic white mothers as a reference (HR=1.00) and compared them to the children of non-US-born Hispanic mothers and US-born Hispanic mothers.
For children of non-US-born Hispanic mothers, the HR was 0.50 for glioma, 0.43 for astrocytoma, 0.47 for neuroblastoma, and 0.70 for Wilms tumor. For children of US-born Hispanic mothers, the HR was 0.71 for glioma, 0.62 for astrocytoma, 0.66 for neuroblastoma, and 0.88 for Wilms tumor.
When compared to non-Hispanic white children, Hispanic children had an increased risk of acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), and Hodgkin lymphoma but lower risks of NHL and Burkitt lymphoma.
For children of US-born Hispanic mothers, the HR was 1.20 for ALL, 1.28 for AML, 2.49 for Hodgkin lymphoma, 0.79 for NHL, and 0.69 for Burkitt lymphoma.
For children of non-US-born Hispanic mothers, the HR was 1.06 for ALL, 1.05 for AML, 2.35 for Hodgkin lymphoma, 0.76 for NHL, and 0.73 for Burkitt lymphoma.
The researchers said the differences observed between children of US-born and non-US-born Hispanic mothers may be explained by lifestyle differences and varying environmental exposures.
These factors may explain the differences in cancer incidence between Hispanic children and white children as well, but the differences may also be a result of genetic variation and infection exposures early in life. ![]()

Photo by Nina Matthews
New research suggests a mother’s birthplace may affect the risk of certain cancers for Hispanic children.
The study showed that children of Hispanic mothers who were not born in the US had lower risks of brain cancers, neuroblastoma, and Wilms tumor, when compared to children of US-born Hispanic mothers and non-Hispanic white mothers born in the US.
However, all Hispanic children, regardless of where their mothers were born, had higher risks of acute leukemias and Hodgkin lymphoma but a lower risk of non-Hodgkin lymphoma (NHL).
Julia E. Heck, PhD, of the University of California, Los Angeles, and her colleagues reported these findings in JAMA Pediatrics.
The researchers used California birth records to identify children born from 1983 through 2011. Information on cancer cases came from California Cancer Registry records from 1988 to 2012.
The team restricted their analysis to children of US-born white, US-born Hispanic, and non-US-born Hispanic mothers. The study included 13,666 cases of children diagnosed with cancer before the age of 6 and 15,513,718 children who served as control subjects.
To assess the hazard ratios (HRs) for various cancers, the researchers used children of non-Hispanic white mothers as a reference (HR=1.00) and compared them to the children of non-US-born Hispanic mothers and US-born Hispanic mothers.
For children of non-US-born Hispanic mothers, the HR was 0.50 for glioma, 0.43 for astrocytoma, 0.47 for neuroblastoma, and 0.70 for Wilms tumor. For children of US-born Hispanic mothers, the HR was 0.71 for glioma, 0.62 for astrocytoma, 0.66 for neuroblastoma, and 0.88 for Wilms tumor.
When compared to non-Hispanic white children, Hispanic children had an increased risk of acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), and Hodgkin lymphoma but lower risks of NHL and Burkitt lymphoma.
For children of US-born Hispanic mothers, the HR was 1.20 for ALL, 1.28 for AML, 2.49 for Hodgkin lymphoma, 0.79 for NHL, and 0.69 for Burkitt lymphoma.
For children of non-US-born Hispanic mothers, the HR was 1.06 for ALL, 1.05 for AML, 2.35 for Hodgkin lymphoma, 0.76 for NHL, and 0.73 for Burkitt lymphoma.
The researchers said the differences observed between children of US-born and non-US-born Hispanic mothers may be explained by lifestyle differences and varying environmental exposures.
These factors may explain the differences in cancer incidence between Hispanic children and white children as well, but the differences may also be a result of genetic variation and infection exposures early in life. ![]()
Drug granted breakthrough designation for cHL

Photo courtesy of Merck
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation for pembrolizumab (Keytruda) to treat patients with relapsed or refractory classical Hodgkin lymphoma (cHL).
Pembrolizumab is a monoclonal antibody that binds to the PD-1 receptor and blocks its interaction with PD-L1 and PD-L2, releasing PD-1 pathway-mediated inhibition of the immune response, including the antitumor immune response.
The FDA’s breakthrough therapy designation is intended to expedite the development and review of new therapies for serious or life threatening conditions, which have shown encouraging early clinical results demonstrating substantial improvement on a clinically significant endpoint over available therapies.
The breakthrough designation for pembrolizumab in cHL is based on data from the phase 1b KEYNOTE-013 trial and the phase 2 KEYNOTE-087 trial.
Findings from the KEYNOTE-013 study were presented at ASH 2014 (in patients with cHL) and ASH 2015 (in primary mediastinal large B-cell lymphoma).
Data from KEYNOTE-087 will be presented at an upcoming medical meeting, according to Merck, the company developing pembrolizumab.
Pembrolizumab also has breakthrough designation from the FDA as a treatment for advanced melanoma, advanced non-small cell lung cancer, and advanced colorectal cancer.
The drug is already FDA-approved to treat melanoma and non-small cell lung cancer. Pembrolizumab is administered at a dose of 2 mg/kg as an intravenous infusion over 30 minutes every 3 weeks for the approved indications. ![]()

Photo courtesy of Merck
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation for pembrolizumab (Keytruda) to treat patients with relapsed or refractory classical Hodgkin lymphoma (cHL).
Pembrolizumab is a monoclonal antibody that binds to the PD-1 receptor and blocks its interaction with PD-L1 and PD-L2, releasing PD-1 pathway-mediated inhibition of the immune response, including the antitumor immune response.
The FDA’s breakthrough therapy designation is intended to expedite the development and review of new therapies for serious or life threatening conditions, which have shown encouraging early clinical results demonstrating substantial improvement on a clinically significant endpoint over available therapies.
The breakthrough designation for pembrolizumab in cHL is based on data from the phase 1b KEYNOTE-013 trial and the phase 2 KEYNOTE-087 trial.
Findings from the KEYNOTE-013 study were presented at ASH 2014 (in patients with cHL) and ASH 2015 (in primary mediastinal large B-cell lymphoma).
Data from KEYNOTE-087 will be presented at an upcoming medical meeting, according to Merck, the company developing pembrolizumab.
Pembrolizumab also has breakthrough designation from the FDA as a treatment for advanced melanoma, advanced non-small cell lung cancer, and advanced colorectal cancer.
The drug is already FDA-approved to treat melanoma and non-small cell lung cancer. Pembrolizumab is administered at a dose of 2 mg/kg as an intravenous infusion over 30 minutes every 3 weeks for the approved indications. ![]()

Photo courtesy of Merck
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation for pembrolizumab (Keytruda) to treat patients with relapsed or refractory classical Hodgkin lymphoma (cHL).
Pembrolizumab is a monoclonal antibody that binds to the PD-1 receptor and blocks its interaction with PD-L1 and PD-L2, releasing PD-1 pathway-mediated inhibition of the immune response, including the antitumor immune response.
The FDA’s breakthrough therapy designation is intended to expedite the development and review of new therapies for serious or life threatening conditions, which have shown encouraging early clinical results demonstrating substantial improvement on a clinically significant endpoint over available therapies.
The breakthrough designation for pembrolizumab in cHL is based on data from the phase 1b KEYNOTE-013 trial and the phase 2 KEYNOTE-087 trial.
Findings from the KEYNOTE-013 study were presented at ASH 2014 (in patients with cHL) and ASH 2015 (in primary mediastinal large B-cell lymphoma).
Data from KEYNOTE-087 will be presented at an upcoming medical meeting, according to Merck, the company developing pembrolizumab.
Pembrolizumab also has breakthrough designation from the FDA as a treatment for advanced melanoma, advanced non-small cell lung cancer, and advanced colorectal cancer.
The drug is already FDA-approved to treat melanoma and non-small cell lung cancer. Pembrolizumab is administered at a dose of 2 mg/kg as an intravenous infusion over 30 minutes every 3 weeks for the approved indications. ![]()
PD-1 inhibitor granted priority review for cHL

Photo courtesy of Business Wire
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application seeking to expand use of the PD-1 inhibitor nivolumab (Opdivo) to patients with previously treated classical Hodgkin lymphoma (cHL).
A priority review designation means the FDA’s goal is to take action on an application within 6 months, rather than the 10 months typically taken for a standard review.
To grant an application priority review, the FDA must believe the drug would provide a significant improvement in the treatment, diagnosis, or prevention of a serious condition.
About nivolumab
Nivolumab is an inhibitor that binds to the checkpoint receptor PD-1, which is expressed on activated T cells. The drug prevents PD-L1 and PD-L2 from binding, thereby preventing the PD-1 pathway’s suppressive signaling on the immune system, including interference with an anti-tumor immune response.
Nivolumab is being developed by Bristol-Myers Squibb. The drug currently has regulatory approval in 48 countries.
In the US, nivolumab is approved—both as a single agent and in combination—to treat certain patients with melanoma, non-small-cell lung cancer, or advanced renal cell carcinoma.
According to Bristol-Myers Squibb, nivolumab has the potential to become first PD-1 inhibitor approved for a hematologic malignancy in the US.
The supplemental biologics license application for nivolumab included data from the phase 2 trial CheckMate 205. In this ongoing trial, researchers are evaluating nivolumab in patients with relapsed or refractory cHL who have received an autologous stem cell transplant and brentuximab vedotin.
Data from this trial are expected to be presented at a medical meeting later this year.
The FDA previously granted nivolumab breakthrough therapy designation for cHL. The FDA’s breakthrough therapy designation is intended to expedite the development and review of drugs for serious or life-threatening conditions. ![]()

Photo courtesy of Business Wire
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application seeking to expand use of the PD-1 inhibitor nivolumab (Opdivo) to patients with previously treated classical Hodgkin lymphoma (cHL).
A priority review designation means the FDA’s goal is to take action on an application within 6 months, rather than the 10 months typically taken for a standard review.
To grant an application priority review, the FDA must believe the drug would provide a significant improvement in the treatment, diagnosis, or prevention of a serious condition.
About nivolumab
Nivolumab is an inhibitor that binds to the checkpoint receptor PD-1, which is expressed on activated T cells. The drug prevents PD-L1 and PD-L2 from binding, thereby preventing the PD-1 pathway’s suppressive signaling on the immune system, including interference with an anti-tumor immune response.
Nivolumab is being developed by Bristol-Myers Squibb. The drug currently has regulatory approval in 48 countries.
In the US, nivolumab is approved—both as a single agent and in combination—to treat certain patients with melanoma, non-small-cell lung cancer, or advanced renal cell carcinoma.
According to Bristol-Myers Squibb, nivolumab has the potential to become first PD-1 inhibitor approved for a hematologic malignancy in the US.
The supplemental biologics license application for nivolumab included data from the phase 2 trial CheckMate 205. In this ongoing trial, researchers are evaluating nivolumab in patients with relapsed or refractory cHL who have received an autologous stem cell transplant and brentuximab vedotin.
Data from this trial are expected to be presented at a medical meeting later this year.
The FDA previously granted nivolumab breakthrough therapy designation for cHL. The FDA’s breakthrough therapy designation is intended to expedite the development and review of drugs for serious or life-threatening conditions. ![]()

Photo courtesy of Business Wire
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application seeking to expand use of the PD-1 inhibitor nivolumab (Opdivo) to patients with previously treated classical Hodgkin lymphoma (cHL).
A priority review designation means the FDA’s goal is to take action on an application within 6 months, rather than the 10 months typically taken for a standard review.
To grant an application priority review, the FDA must believe the drug would provide a significant improvement in the treatment, diagnosis, or prevention of a serious condition.
About nivolumab
Nivolumab is an inhibitor that binds to the checkpoint receptor PD-1, which is expressed on activated T cells. The drug prevents PD-L1 and PD-L2 from binding, thereby preventing the PD-1 pathway’s suppressive signaling on the immune system, including interference with an anti-tumor immune response.
Nivolumab is being developed by Bristol-Myers Squibb. The drug currently has regulatory approval in 48 countries.
In the US, nivolumab is approved—both as a single agent and in combination—to treat certain patients with melanoma, non-small-cell lung cancer, or advanced renal cell carcinoma.
According to Bristol-Myers Squibb, nivolumab has the potential to become first PD-1 inhibitor approved for a hematologic malignancy in the US.
The supplemental biologics license application for nivolumab included data from the phase 2 trial CheckMate 205. In this ongoing trial, researchers are evaluating nivolumab in patients with relapsed or refractory cHL who have received an autologous stem cell transplant and brentuximab vedotin.
Data from this trial are expected to be presented at a medical meeting later this year.
The FDA previously granted nivolumab breakthrough therapy designation for cHL. The FDA’s breakthrough therapy designation is intended to expedite the development and review of drugs for serious or life-threatening conditions. ![]()
FDG-PET guides need for eBEACOPP in advanced Hodgkin’s
Using FDG-PET (fluorodeoxyglucose positron emission tomography) imaging to gauge treatment response after the first two rounds of ABVD therapy helps to determine which patients with advanced Hodgkin’s lymphoma should be switched to a more aggressive eBEACOPP regimen, according to the results of the Southwest Oncology Group (SWOG) S0816 study.
In this large U.S. trial of PET scanning to guide treatment approach in people with high-risk stage II or stage III-IV Hodgkin’s lymphoma, progression-free survival at 2 years for those with early interim positive PET scans was 64%, which is much higher than the expected progression-free survival of 15%-30%, according to Dr. Oliver Press, a SWOG member at Fred Hutchinson Cancer Research Center and the lead author of study, which was published ahead of print in the Journal of Clinical Oncology (2016 April 11. doi: 10.1200/JCO.2015.63.1119).
In addition, just 20% of patients in the trial were exposed to eBEACOPP, which usually results in infertility, can cause sustained heart or lung damage, and increases the risk of secondary cancers.
Researchers recruited 358 Hodgkin’s patients to the trial and were able to evaluate 331 of them. All trial volunteers were given two rounds of standard ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine) chemotherapy, followed by a PET scan. If the scan was negative, patients received four more cycles of ABVD. If the scan was positive, with a Deauville score of 4-5, they were advised to switch to eBEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone), a seven-drug combination used in Europe. Of 60 patients with positive interim PET scans, 11 patients declined to switch, and 49 switched as planned to six cycles of eBEACOPP.
With a median follow-up of nearly 40 months, the Kaplan-Meier estimate for 2-year overall survival was 98%, and the 2-year estimate for progression-free survival was 79%. In the subset of patients who had positive PET scans after two cycles of ABVD, the 2-year estimate for progression-free survival was 64%, more than double the expected remission rate.
At least seven phase II and III cooperative group studies are underway testing this approach in advanced-stage Hodgkin’s lymphoma, the researchers wrote. “We hope that in the future, molecular biomarker studies at initial diagnosis, or the combination of biomarkers and molecular imaging, may define patients who require more intense therapy with eBEACOPP or other novel targeted drugs with greater accuracy than is achievable with current technology.”
The study was funded by the National Cancer Institute, the David and Patricia Giuliani Family Foundation, the Lymphoma Foundation, the Adam Spector Fund for Hodgkin Research, and the Ernest & Jeanette Dicker Charitable Foundation.
On Twitter @maryjodales
Using FDG-PET (fluorodeoxyglucose positron emission tomography) imaging to gauge treatment response after the first two rounds of ABVD therapy helps to determine which patients with advanced Hodgkin’s lymphoma should be switched to a more aggressive eBEACOPP regimen, according to the results of the Southwest Oncology Group (SWOG) S0816 study.
In this large U.S. trial of PET scanning to guide treatment approach in people with high-risk stage II or stage III-IV Hodgkin’s lymphoma, progression-free survival at 2 years for those with early interim positive PET scans was 64%, which is much higher than the expected progression-free survival of 15%-30%, according to Dr. Oliver Press, a SWOG member at Fred Hutchinson Cancer Research Center and the lead author of study, which was published ahead of print in the Journal of Clinical Oncology (2016 April 11. doi: 10.1200/JCO.2015.63.1119).
In addition, just 20% of patients in the trial were exposed to eBEACOPP, which usually results in infertility, can cause sustained heart or lung damage, and increases the risk of secondary cancers.
Researchers recruited 358 Hodgkin’s patients to the trial and were able to evaluate 331 of them. All trial volunteers were given two rounds of standard ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine) chemotherapy, followed by a PET scan. If the scan was negative, patients received four more cycles of ABVD. If the scan was positive, with a Deauville score of 4-5, they were advised to switch to eBEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone), a seven-drug combination used in Europe. Of 60 patients with positive interim PET scans, 11 patients declined to switch, and 49 switched as planned to six cycles of eBEACOPP.
With a median follow-up of nearly 40 months, the Kaplan-Meier estimate for 2-year overall survival was 98%, and the 2-year estimate for progression-free survival was 79%. In the subset of patients who had positive PET scans after two cycles of ABVD, the 2-year estimate for progression-free survival was 64%, more than double the expected remission rate.
At least seven phase II and III cooperative group studies are underway testing this approach in advanced-stage Hodgkin’s lymphoma, the researchers wrote. “We hope that in the future, molecular biomarker studies at initial diagnosis, or the combination of biomarkers and molecular imaging, may define patients who require more intense therapy with eBEACOPP or other novel targeted drugs with greater accuracy than is achievable with current technology.”
The study was funded by the National Cancer Institute, the David and Patricia Giuliani Family Foundation, the Lymphoma Foundation, the Adam Spector Fund for Hodgkin Research, and the Ernest & Jeanette Dicker Charitable Foundation.
On Twitter @maryjodales
Using FDG-PET (fluorodeoxyglucose positron emission tomography) imaging to gauge treatment response after the first two rounds of ABVD therapy helps to determine which patients with advanced Hodgkin’s lymphoma should be switched to a more aggressive eBEACOPP regimen, according to the results of the Southwest Oncology Group (SWOG) S0816 study.
In this large U.S. trial of PET scanning to guide treatment approach in people with high-risk stage II or stage III-IV Hodgkin’s lymphoma, progression-free survival at 2 years for those with early interim positive PET scans was 64%, which is much higher than the expected progression-free survival of 15%-30%, according to Dr. Oliver Press, a SWOG member at Fred Hutchinson Cancer Research Center and the lead author of study, which was published ahead of print in the Journal of Clinical Oncology (2016 April 11. doi: 10.1200/JCO.2015.63.1119).
In addition, just 20% of patients in the trial were exposed to eBEACOPP, which usually results in infertility, can cause sustained heart or lung damage, and increases the risk of secondary cancers.
Researchers recruited 358 Hodgkin’s patients to the trial and were able to evaluate 331 of them. All trial volunteers were given two rounds of standard ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine) chemotherapy, followed by a PET scan. If the scan was negative, patients received four more cycles of ABVD. If the scan was positive, with a Deauville score of 4-5, they were advised to switch to eBEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone), a seven-drug combination used in Europe. Of 60 patients with positive interim PET scans, 11 patients declined to switch, and 49 switched as planned to six cycles of eBEACOPP.
With a median follow-up of nearly 40 months, the Kaplan-Meier estimate for 2-year overall survival was 98%, and the 2-year estimate for progression-free survival was 79%. In the subset of patients who had positive PET scans after two cycles of ABVD, the 2-year estimate for progression-free survival was 64%, more than double the expected remission rate.
At least seven phase II and III cooperative group studies are underway testing this approach in advanced-stage Hodgkin’s lymphoma, the researchers wrote. “We hope that in the future, molecular biomarker studies at initial diagnosis, or the combination of biomarkers and molecular imaging, may define patients who require more intense therapy with eBEACOPP or other novel targeted drugs with greater accuracy than is achievable with current technology.”
The study was funded by the National Cancer Institute, the David and Patricia Giuliani Family Foundation, the Lymphoma Foundation, the Adam Spector Fund for Hodgkin Research, and the Ernest & Jeanette Dicker Charitable Foundation.
On Twitter @maryjodales
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Using FDG-PET imaging to gauge treatment response after the first two rounds of ABVD therapy helps to determine which patients with advanced Hodgkin’s lymphoma should be switched to the eBEACOPP regimen.
Major finding: Progression-free survival at 2 years for those with early interim positive PET scans was 64%; the historical progression-free survival for this group is 15%-30%.
Data source: Evaluations of 331 patients in the Southwest Oncology Group S0816 study.
Disclosures: The study was funded by the National Cancer Institute, the David and Patricia Giuliani Family Foundation, the Lymphoma Foundation, the Adam Spector Fund for Hodgkin Research, and the Ernest & Jeanette Dicker Charitable Foundation.
PET-guided chemo improves PFS in advanced HL

Image by Jens Langner
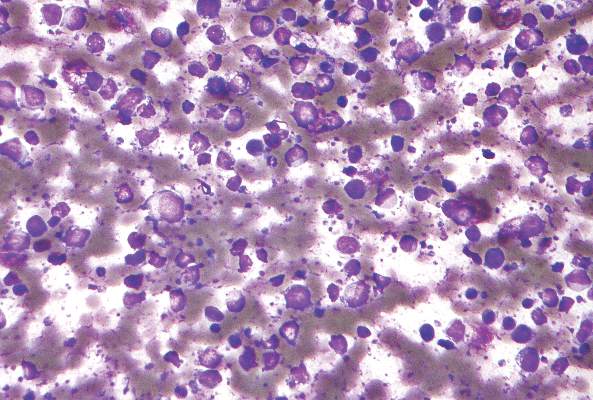
Using PET imaging to guide chemotherapy can improve outcomes for patients with advanced Hodgkin lymphoma (HL), according to research published in the Journal of Clinical Oncology.
The study indicated that PET-guided treatment can improve progression-free survival (PFS) among patients who do not achieve remission with 2 cycles of ABVD.
The results also suggested the approach can spare some patients unnecessary toxicity.
“The goal of cancer treatment is to cure as many people as possible with as little toxicity as possible,” said study author Oliver Press, MD, PhD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington.
“We found a promising way to do that by tailoring treatment to Hodgkin patients, an approach which could lead to a new standard of care.”
Dr Press and his colleagues began this study with 358 HIV-negative patients with advanced HL, but only 336 of them were eligible and evaluable at baseline.
The patients’ median age was 32 (range, 18 to 60). Fifty-two percent had stage III disease, 48% had stage IV, 49% had an International Prognostic Score of 0 to 2, and 51% had a score of 3 to 7.
All of the patients received ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine) and underwent a PET scan to gauge their response after 2 cycles (PET2).
If the scan was negative, patients received a final 4 cycles of ABVD. If the scan was positive, patients received 6 cycles of eBEACOPP (escalated bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisolone).
Central review of the PET2 scan was performed in 331 patients. Most (82%, n=271) had a negative scan.
Forty-nine of the 60 PET2-positive patients went on to receive eBEACOPP as planned, but 11 patients declined.
The median follow-up was 39.7 months. For the entire study cohort, the estimated 2-year overall survival was 98%, and the estimated 2-year PFS was 79%.
The 2-year estimated PFS was 82% for PET2-negative patients and 64% for PET2-positive patients. The researchers noted that, typically, if HL patients have a positive PET scan after 2 rounds of ABVD, their expected 2-year PFS ranges from about 15% to 30%.
The researchers also pointed out that eBEACOPP was significantly more toxic than ABVD. The incidence of grade 4/5 toxicities was 85.7% and 36.7%, respectively (P<0.001).
There were 3 treatment-related deaths—1 in the ABVD group and 2 in the eBEACOPP group. And 6 patients developed secondary malignancies—3 in each group—including 2 non-Hodgkin lymphomas, 2 kidney cancers, 1 melanoma, and 1 skin cancer.
“[O]nly 20% of the patients in our trial were exposed to eBEACOPP, which means [most patients] weren’t exposed to its bad effects,” said Jonathan Friedberg, MD, of the University of Rochester Medical Center in Rochester, New York.
“That’s important because many people diagnosed with Hodgkin lymphoma are in their 20s and 30s and want to have children. This response-adapted therapy would ensure that the people who need the more toxic drugs receive them and would spare others from infertility and serious toxicities.” ![]()

Image by Jens Langner
Using PET imaging to guide chemotherapy can improve outcomes for patients with advanced Hodgkin lymphoma (HL), according to research published in the Journal of Clinical Oncology.
The study indicated that PET-guided treatment can improve progression-free survival (PFS) among patients who do not achieve remission with 2 cycles of ABVD.
The results also suggested the approach can spare some patients unnecessary toxicity.
“The goal of cancer treatment is to cure as many people as possible with as little toxicity as possible,” said study author Oliver Press, MD, PhD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington.
“We found a promising way to do that by tailoring treatment to Hodgkin patients, an approach which could lead to a new standard of care.”
Dr Press and his colleagues began this study with 358 HIV-negative patients with advanced HL, but only 336 of them were eligible and evaluable at baseline.
The patients’ median age was 32 (range, 18 to 60). Fifty-two percent had stage III disease, 48% had stage IV, 49% had an International Prognostic Score of 0 to 2, and 51% had a score of 3 to 7.
All of the patients received ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine) and underwent a PET scan to gauge their response after 2 cycles (PET2).
If the scan was negative, patients received a final 4 cycles of ABVD. If the scan was positive, patients received 6 cycles of eBEACOPP (escalated bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisolone).
Central review of the PET2 scan was performed in 331 patients. Most (82%, n=271) had a negative scan.
Forty-nine of the 60 PET2-positive patients went on to receive eBEACOPP as planned, but 11 patients declined.
The median follow-up was 39.7 months. For the entire study cohort, the estimated 2-year overall survival was 98%, and the estimated 2-year PFS was 79%.
The 2-year estimated PFS was 82% for PET2-negative patients and 64% for PET2-positive patients. The researchers noted that, typically, if HL patients have a positive PET scan after 2 rounds of ABVD, their expected 2-year PFS ranges from about 15% to 30%.
The researchers also pointed out that eBEACOPP was significantly more toxic than ABVD. The incidence of grade 4/5 toxicities was 85.7% and 36.7%, respectively (P<0.001).
There were 3 treatment-related deaths—1 in the ABVD group and 2 in the eBEACOPP group. And 6 patients developed secondary malignancies—3 in each group—including 2 non-Hodgkin lymphomas, 2 kidney cancers, 1 melanoma, and 1 skin cancer.
“[O]nly 20% of the patients in our trial were exposed to eBEACOPP, which means [most patients] weren’t exposed to its bad effects,” said Jonathan Friedberg, MD, of the University of Rochester Medical Center in Rochester, New York.
“That’s important because many people diagnosed with Hodgkin lymphoma are in their 20s and 30s and want to have children. This response-adapted therapy would ensure that the people who need the more toxic drugs receive them and would spare others from infertility and serious toxicities.” ![]()

Image by Jens Langner
Using PET imaging to guide chemotherapy can improve outcomes for patients with advanced Hodgkin lymphoma (HL), according to research published in the Journal of Clinical Oncology.
The study indicated that PET-guided treatment can improve progression-free survival (PFS) among patients who do not achieve remission with 2 cycles of ABVD.
The results also suggested the approach can spare some patients unnecessary toxicity.
“The goal of cancer treatment is to cure as many people as possible with as little toxicity as possible,” said study author Oliver Press, MD, PhD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington.
“We found a promising way to do that by tailoring treatment to Hodgkin patients, an approach which could lead to a new standard of care.”
Dr Press and his colleagues began this study with 358 HIV-negative patients with advanced HL, but only 336 of them were eligible and evaluable at baseline.
The patients’ median age was 32 (range, 18 to 60). Fifty-two percent had stage III disease, 48% had stage IV, 49% had an International Prognostic Score of 0 to 2, and 51% had a score of 3 to 7.
All of the patients received ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine) and underwent a PET scan to gauge their response after 2 cycles (PET2).
If the scan was negative, patients received a final 4 cycles of ABVD. If the scan was positive, patients received 6 cycles of eBEACOPP (escalated bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisolone).
Central review of the PET2 scan was performed in 331 patients. Most (82%, n=271) had a negative scan.
Forty-nine of the 60 PET2-positive patients went on to receive eBEACOPP as planned, but 11 patients declined.
The median follow-up was 39.7 months. For the entire study cohort, the estimated 2-year overall survival was 98%, and the estimated 2-year PFS was 79%.
The 2-year estimated PFS was 82% for PET2-negative patients and 64% for PET2-positive patients. The researchers noted that, typically, if HL patients have a positive PET scan after 2 rounds of ABVD, their expected 2-year PFS ranges from about 15% to 30%.
The researchers also pointed out that eBEACOPP was significantly more toxic than ABVD. The incidence of grade 4/5 toxicities was 85.7% and 36.7%, respectively (P<0.001).
There were 3 treatment-related deaths—1 in the ABVD group and 2 in the eBEACOPP group. And 6 patients developed secondary malignancies—3 in each group—including 2 non-Hodgkin lymphomas, 2 kidney cancers, 1 melanoma, and 1 skin cancer.
“[O]nly 20% of the patients in our trial were exposed to eBEACOPP, which means [most patients] weren’t exposed to its bad effects,” said Jonathan Friedberg, MD, of the University of Rochester Medical Center in Rochester, New York.
“That’s important because many people diagnosed with Hodgkin lymphoma are in their 20s and 30s and want to have children. This response-adapted therapy would ensure that the people who need the more toxic drugs receive them and would spare others from infertility and serious toxicities.” ![]()
Combos produce similar 10-year OS, PFS in HL

Photo by Bill Branson
Long-term results of the HD2000 trial reveal similar survival rates in patients with previously untreated, aggressive Hodgkin lymphoma (HL) who received 3 different combination treatment regimens.
At 10 years of follow-up, there was no significant difference in overall survival (OS) or progression-free survival (PFS) whether patients received ABVD, BEACOPP, or CEC.
However, patients who received ABVD were significantly less likely than those who received BEACOPP or CEC to develop second malignancies.
Francesco Merli, MD, of Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) in Italy, and his colleagues reported these results in the Journal of Clinical Oncology.
The trial enrolled 307 patients with advanced-stage HL. Patients were randomized to receive 1 of 3 treatment regimens:
- Six cycles of ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine)
- Four escalated plus 2 standard cycles of BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone)
- Six cycles of CEC (cyclophosphamide, lomustine, vindesine, melphalan, prednisone, epidoxorubicin, vincristine, procarbazine, vinblastine, and bleomycin).
Some patients also received radiotherapy, but there was no significant difference in the proportion of patients receiving radiotherapy across the treatment arms—46% in the ABVD arm, 44% in the BEACOPP arm, and 43% in the CEC arm (P=0.871).
Results
At the end of all therapy, the complete response rate was 84% with ABVD, 91% with BEACOPP, and 83% with CEC.
There were 84 patients who did not achieve a complete response, and salvage data were available for 73 of these patients. Three patients (4%) died before salvage therapy could begin, 26 (36%) received conventional chemotherapy, 40 (55%) received a hematopoietic stem cell transplant, and 4 (5%) received radiotherapy.
The median follow-up was 120 months (range, 4 to 169 months), and 295 patients were evaluable.
In a previous analysis, at a median follow-up of 42 months, patients who received BEACOPP had superior PFS compared to patients who received ABVD.
However, in the current analysis, there was no significant difference in PFS between the 3 treatment arms. The 10-year PFS was 69% in the ABVD arm, 75% in the BEACOPP arm, and 76% in the CEC arm (P=0.471).
Likewise, there was no significant difference in OS between the treatment arms. The 10-year OS was 85% in the ABVD arm, 84% in the BEACOPP arm, and 86% in the CEC arm (P=0.892).
There were a total of 13 second malignancies—1 in the ABVD arm and 6 each in the BEACOPP and CEC arms.
The cumulative risk of developing a second malignancy at 10 years was 0.9% in the ABVD arm, 6.6% in the BEACOPP arm, and 6% in the CEC arm. So the risk with either BEACOPP or CEC was significantly higher than with ABVD (P=0.027 and 0.02, respectively).
The researchers said these results suggest BEACOPP provides better disease control than ABVD, but this benefit is counterbalanced by a higher rate of late major events with BEACOPP, particularly second malignancies, which resulted in patient deaths.
So the team concluded that BEACOPP is a viable treatment option for advanced HL, but it should not be considered the standard for all patients because 70% of these patients may be cured with ABVD and limited radiotherapy. A careful assessment of the risk-benefit ratio of the initial treatment choice is warranted. ![]()

Photo by Bill Branson
Long-term results of the HD2000 trial reveal similar survival rates in patients with previously untreated, aggressive Hodgkin lymphoma (HL) who received 3 different combination treatment regimens.
At 10 years of follow-up, there was no significant difference in overall survival (OS) or progression-free survival (PFS) whether patients received ABVD, BEACOPP, or CEC.
However, patients who received ABVD were significantly less likely than those who received BEACOPP or CEC to develop second malignancies.
Francesco Merli, MD, of Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) in Italy, and his colleagues reported these results in the Journal of Clinical Oncology.
The trial enrolled 307 patients with advanced-stage HL. Patients were randomized to receive 1 of 3 treatment regimens:
- Six cycles of ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine)
- Four escalated plus 2 standard cycles of BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone)
- Six cycles of CEC (cyclophosphamide, lomustine, vindesine, melphalan, prednisone, epidoxorubicin, vincristine, procarbazine, vinblastine, and bleomycin).
Some patients also received radiotherapy, but there was no significant difference in the proportion of patients receiving radiotherapy across the treatment arms—46% in the ABVD arm, 44% in the BEACOPP arm, and 43% in the CEC arm (P=0.871).
Results
At the end of all therapy, the complete response rate was 84% with ABVD, 91% with BEACOPP, and 83% with CEC.
There were 84 patients who did not achieve a complete response, and salvage data were available for 73 of these patients. Three patients (4%) died before salvage therapy could begin, 26 (36%) received conventional chemotherapy, 40 (55%) received a hematopoietic stem cell transplant, and 4 (5%) received radiotherapy.
The median follow-up was 120 months (range, 4 to 169 months), and 295 patients were evaluable.
In a previous analysis, at a median follow-up of 42 months, patients who received BEACOPP had superior PFS compared to patients who received ABVD.
However, in the current analysis, there was no significant difference in PFS between the 3 treatment arms. The 10-year PFS was 69% in the ABVD arm, 75% in the BEACOPP arm, and 76% in the CEC arm (P=0.471).
Likewise, there was no significant difference in OS between the treatment arms. The 10-year OS was 85% in the ABVD arm, 84% in the BEACOPP arm, and 86% in the CEC arm (P=0.892).
There were a total of 13 second malignancies—1 in the ABVD arm and 6 each in the BEACOPP and CEC arms.
The cumulative risk of developing a second malignancy at 10 years was 0.9% in the ABVD arm, 6.6% in the BEACOPP arm, and 6% in the CEC arm. So the risk with either BEACOPP or CEC was significantly higher than with ABVD (P=0.027 and 0.02, respectively).
The researchers said these results suggest BEACOPP provides better disease control than ABVD, but this benefit is counterbalanced by a higher rate of late major events with BEACOPP, particularly second malignancies, which resulted in patient deaths.
So the team concluded that BEACOPP is a viable treatment option for advanced HL, but it should not be considered the standard for all patients because 70% of these patients may be cured with ABVD and limited radiotherapy. A careful assessment of the risk-benefit ratio of the initial treatment choice is warranted. ![]()

Photo by Bill Branson
Long-term results of the HD2000 trial reveal similar survival rates in patients with previously untreated, aggressive Hodgkin lymphoma (HL) who received 3 different combination treatment regimens.
At 10 years of follow-up, there was no significant difference in overall survival (OS) or progression-free survival (PFS) whether patients received ABVD, BEACOPP, or CEC.
However, patients who received ABVD were significantly less likely than those who received BEACOPP or CEC to develop second malignancies.
Francesco Merli, MD, of Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) in Italy, and his colleagues reported these results in the Journal of Clinical Oncology.
The trial enrolled 307 patients with advanced-stage HL. Patients were randomized to receive 1 of 3 treatment regimens:
- Six cycles of ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine)
- Four escalated plus 2 standard cycles of BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone)
- Six cycles of CEC (cyclophosphamide, lomustine, vindesine, melphalan, prednisone, epidoxorubicin, vincristine, procarbazine, vinblastine, and bleomycin).
Some patients also received radiotherapy, but there was no significant difference in the proportion of patients receiving radiotherapy across the treatment arms—46% in the ABVD arm, 44% in the BEACOPP arm, and 43% in the CEC arm (P=0.871).
Results
At the end of all therapy, the complete response rate was 84% with ABVD, 91% with BEACOPP, and 83% with CEC.
There were 84 patients who did not achieve a complete response, and salvage data were available for 73 of these patients. Three patients (4%) died before salvage therapy could begin, 26 (36%) received conventional chemotherapy, 40 (55%) received a hematopoietic stem cell transplant, and 4 (5%) received radiotherapy.
The median follow-up was 120 months (range, 4 to 169 months), and 295 patients were evaluable.
In a previous analysis, at a median follow-up of 42 months, patients who received BEACOPP had superior PFS compared to patients who received ABVD.
However, in the current analysis, there was no significant difference in PFS between the 3 treatment arms. The 10-year PFS was 69% in the ABVD arm, 75% in the BEACOPP arm, and 76% in the CEC arm (P=0.471).
Likewise, there was no significant difference in OS between the treatment arms. The 10-year OS was 85% in the ABVD arm, 84% in the BEACOPP arm, and 86% in the CEC arm (P=0.892).
There were a total of 13 second malignancies—1 in the ABVD arm and 6 each in the BEACOPP and CEC arms.
The cumulative risk of developing a second malignancy at 10 years was 0.9% in the ABVD arm, 6.6% in the BEACOPP arm, and 6% in the CEC arm. So the risk with either BEACOPP or CEC was significantly higher than with ABVD (P=0.027 and 0.02, respectively).
The researchers said these results suggest BEACOPP provides better disease control than ABVD, but this benefit is counterbalanced by a higher rate of late major events with BEACOPP, particularly second malignancies, which resulted in patient deaths.
So the team concluded that BEACOPP is a viable treatment option for advanced HL, but it should not be considered the standard for all patients because 70% of these patients may be cured with ABVD and limited radiotherapy. A careful assessment of the risk-benefit ratio of the initial treatment choice is warranted. ![]()
Dual inhibitor shows early promise for DLBCL

The small-molecule inhibitor CUDC-907 can provide disease control in patients with relapsed or refractory lymphoma and multiple myeloma (MM), according to researchers.
In a phase 1 trial, CUDC-907 produced responses in a small number of patients with diffuse large B-cell lymphoma (DLBCL).
And more than half of patients had stable disease while on CUDC-907, including those with MM, DLBCL, Hodgkin lymphoma (HL), and other lymphomas.
However, a majority of patients in this trial—84%—discontinued treatment due to confirmed progressive disease or signs of progression.
These results were published in The Lancet. The trial was sponsored by Curis, Inc., the company developing CUDC-907, and the Leukemia and Lymphoma Society.
“The data from the phase 1 monotherapy trial for CUDC-907, especially in heavily pretreated patients with relapsed/refractory DLBCL are very encouraging, and we look forward to data emerging from the current phase 2 trial in patients with MYC-altered DLBCL,” said study author Anas Younes, MD, of the Memorial Sloan Kettering Cancer Center in New York, New York.
CUDC-907 is an oral, dual inhibitor of class I and II histone deacetylases (HDACs), as well as class I PI3K enzymes. Specifically, CUDC-907 is designed to inhibit HDACs 1, 2, 3, 6, and 10 and PI3K-alpha, delta, and beta isoforms.
Between Jan 23, 2013, and July 27, 2015, the phase 1 trial of CUDC-907 enrolled 44 patients who were refractory to or had relapsed after 2 or more previous regimens. The patients’ median age was 63 (range, 22-83), and they had received a median of 5 prior treatments (range, 2-10).
Four patients had MM, 12 had HL, and 12 had DLBCL. The remaining 16 patients had other types of lymphoma, including lymphoplasmacytic lymphoma (n=3), small lymphocytic lymphoma (n=3), mantle cell lymphoma (n=3), follicular lymphoma (n=2), T-cell lymphoma (n=2), marginal zone lymphoma (n=1), Burkitt lymphoma (n=1), and gray zone lymphoma (n=1).
Treatment
CUDC-907 was given in a standard 3 + 3 dose-escalation design at 4 different dosing schedules—once daily, twice weekly, 3 times weekly, and daily for 5 days followed by a 2-day break (5/2)—in 21-day cycles.
Patients continued to receive CUDC-907 until disease progression or other treatment discontinuation criteria were met. The primary objective was to determine the maximum tolerated dose (MTD) and recommended phase 2 dose.
Ten patients were sequentially assigned to CUDC-907 once-daily (MTD 60 mg), 12 to twice-weekly (MTD 150 mg), 15 to 3-times-weekly (MTD 150 mg), and 7 to the 5/2 dosing schedule (MTD 60 mg).
Safety
Four dose-limiting toxicities (DLTs) occurred in 3 of 40 DLT-evaluable patients. The DLTs were diarrhea and hyperglycemia in 1 patient on 60 mg once daily, hyperglycemia in 1 patient on 150 mg twice weekly, and diarrhea in 1 patient on 150 mg 3 times weekly. There were no DLTs in patients on the 5/2 schedule.
The incidence of grade 3 or higher adverse events (AEs) was 43% (19/44). The most common of these AEs were thrombocytopenia (20%, n=9), neutropenia (7%, n=3), and hyperglycemia (7%, n=3).
Twenty-five percent of patients (11/44) had serious AEs. Three of these events were considered treatment-related. They were epistaxis and the DLTs of diarrhea and hyperglycemia.
AEs led to dose reductions in 6 patients (14%) and treatment discontinuation in 7 patients (16%).
Efficacy
Thirty-seven patients were evaluable for response, and 5 of these patients responded (14%). All responses—2 complete and 3 partial responses—occurred in patients with DLBCL.
Twenty-one of the response-evaluable patients (57%) had stable disease. This included 1 patient with DLBCL, 2 with MM, 8 with HL, and 10 with the “other” types of lymphoma.
The remaining 11 patients progressed (30%)—3 with DLBCL, 2 with MM, 2 with HL, and 4 with other lymphomas.
Thirty-seven patients (84%) discontinued CUDC-907 because of progressive disease or clinical signs of progressive disease at the data cutoff.
Based on the clinical activity of CUDC-907 in patients with relapsed/refractory DLBCL, particularly those with MYC alterations, Curis has initiated a phase 2 trial of the drug in these patients. The recommended phase 2 dose is 60 mg on the 5/2 dosing schedule. ![]()

The small-molecule inhibitor CUDC-907 can provide disease control in patients with relapsed or refractory lymphoma and multiple myeloma (MM), according to researchers.
In a phase 1 trial, CUDC-907 produced responses in a small number of patients with diffuse large B-cell lymphoma (DLBCL).
And more than half of patients had stable disease while on CUDC-907, including those with MM, DLBCL, Hodgkin lymphoma (HL), and other lymphomas.
However, a majority of patients in this trial—84%—discontinued treatment due to confirmed progressive disease or signs of progression.
These results were published in The Lancet. The trial was sponsored by Curis, Inc., the company developing CUDC-907, and the Leukemia and Lymphoma Society.
“The data from the phase 1 monotherapy trial for CUDC-907, especially in heavily pretreated patients with relapsed/refractory DLBCL are very encouraging, and we look forward to data emerging from the current phase 2 trial in patients with MYC-altered DLBCL,” said study author Anas Younes, MD, of the Memorial Sloan Kettering Cancer Center in New York, New York.
CUDC-907 is an oral, dual inhibitor of class I and II histone deacetylases (HDACs), as well as class I PI3K enzymes. Specifically, CUDC-907 is designed to inhibit HDACs 1, 2, 3, 6, and 10 and PI3K-alpha, delta, and beta isoforms.
Between Jan 23, 2013, and July 27, 2015, the phase 1 trial of CUDC-907 enrolled 44 patients who were refractory to or had relapsed after 2 or more previous regimens. The patients’ median age was 63 (range, 22-83), and they had received a median of 5 prior treatments (range, 2-10).
Four patients had MM, 12 had HL, and 12 had DLBCL. The remaining 16 patients had other types of lymphoma, including lymphoplasmacytic lymphoma (n=3), small lymphocytic lymphoma (n=3), mantle cell lymphoma (n=3), follicular lymphoma (n=2), T-cell lymphoma (n=2), marginal zone lymphoma (n=1), Burkitt lymphoma (n=1), and gray zone lymphoma (n=1).
Treatment
CUDC-907 was given in a standard 3 + 3 dose-escalation design at 4 different dosing schedules—once daily, twice weekly, 3 times weekly, and daily for 5 days followed by a 2-day break (5/2)—in 21-day cycles.
Patients continued to receive CUDC-907 until disease progression or other treatment discontinuation criteria were met. The primary objective was to determine the maximum tolerated dose (MTD) and recommended phase 2 dose.
Ten patients were sequentially assigned to CUDC-907 once-daily (MTD 60 mg), 12 to twice-weekly (MTD 150 mg), 15 to 3-times-weekly (MTD 150 mg), and 7 to the 5/2 dosing schedule (MTD 60 mg).
Safety
Four dose-limiting toxicities (DLTs) occurred in 3 of 40 DLT-evaluable patients. The DLTs were diarrhea and hyperglycemia in 1 patient on 60 mg once daily, hyperglycemia in 1 patient on 150 mg twice weekly, and diarrhea in 1 patient on 150 mg 3 times weekly. There were no DLTs in patients on the 5/2 schedule.
The incidence of grade 3 or higher adverse events (AEs) was 43% (19/44). The most common of these AEs were thrombocytopenia (20%, n=9), neutropenia (7%, n=3), and hyperglycemia (7%, n=3).
Twenty-five percent of patients (11/44) had serious AEs. Three of these events were considered treatment-related. They were epistaxis and the DLTs of diarrhea and hyperglycemia.
AEs led to dose reductions in 6 patients (14%) and treatment discontinuation in 7 patients (16%).
Efficacy
Thirty-seven patients were evaluable for response, and 5 of these patients responded (14%). All responses—2 complete and 3 partial responses—occurred in patients with DLBCL.
Twenty-one of the response-evaluable patients (57%) had stable disease. This included 1 patient with DLBCL, 2 with MM, 8 with HL, and 10 with the “other” types of lymphoma.
The remaining 11 patients progressed (30%)—3 with DLBCL, 2 with MM, 2 with HL, and 4 with other lymphomas.
Thirty-seven patients (84%) discontinued CUDC-907 because of progressive disease or clinical signs of progressive disease at the data cutoff.
Based on the clinical activity of CUDC-907 in patients with relapsed/refractory DLBCL, particularly those with MYC alterations, Curis has initiated a phase 2 trial of the drug in these patients. The recommended phase 2 dose is 60 mg on the 5/2 dosing schedule. ![]()

The small-molecule inhibitor CUDC-907 can provide disease control in patients with relapsed or refractory lymphoma and multiple myeloma (MM), according to researchers.
In a phase 1 trial, CUDC-907 produced responses in a small number of patients with diffuse large B-cell lymphoma (DLBCL).
And more than half of patients had stable disease while on CUDC-907, including those with MM, DLBCL, Hodgkin lymphoma (HL), and other lymphomas.
However, a majority of patients in this trial—84%—discontinued treatment due to confirmed progressive disease or signs of progression.
These results were published in The Lancet. The trial was sponsored by Curis, Inc., the company developing CUDC-907, and the Leukemia and Lymphoma Society.
“The data from the phase 1 monotherapy trial for CUDC-907, especially in heavily pretreated patients with relapsed/refractory DLBCL are very encouraging, and we look forward to data emerging from the current phase 2 trial in patients with MYC-altered DLBCL,” said study author Anas Younes, MD, of the Memorial Sloan Kettering Cancer Center in New York, New York.
CUDC-907 is an oral, dual inhibitor of class I and II histone deacetylases (HDACs), as well as class I PI3K enzymes. Specifically, CUDC-907 is designed to inhibit HDACs 1, 2, 3, 6, and 10 and PI3K-alpha, delta, and beta isoforms.
Between Jan 23, 2013, and July 27, 2015, the phase 1 trial of CUDC-907 enrolled 44 patients who were refractory to or had relapsed after 2 or more previous regimens. The patients’ median age was 63 (range, 22-83), and they had received a median of 5 prior treatments (range, 2-10).
Four patients had MM, 12 had HL, and 12 had DLBCL. The remaining 16 patients had other types of lymphoma, including lymphoplasmacytic lymphoma (n=3), small lymphocytic lymphoma (n=3), mantle cell lymphoma (n=3), follicular lymphoma (n=2), T-cell lymphoma (n=2), marginal zone lymphoma (n=1), Burkitt lymphoma (n=1), and gray zone lymphoma (n=1).
Treatment
CUDC-907 was given in a standard 3 + 3 dose-escalation design at 4 different dosing schedules—once daily, twice weekly, 3 times weekly, and daily for 5 days followed by a 2-day break (5/2)—in 21-day cycles.
Patients continued to receive CUDC-907 until disease progression or other treatment discontinuation criteria were met. The primary objective was to determine the maximum tolerated dose (MTD) and recommended phase 2 dose.
Ten patients were sequentially assigned to CUDC-907 once-daily (MTD 60 mg), 12 to twice-weekly (MTD 150 mg), 15 to 3-times-weekly (MTD 150 mg), and 7 to the 5/2 dosing schedule (MTD 60 mg).
Safety
Four dose-limiting toxicities (DLTs) occurred in 3 of 40 DLT-evaluable patients. The DLTs were diarrhea and hyperglycemia in 1 patient on 60 mg once daily, hyperglycemia in 1 patient on 150 mg twice weekly, and diarrhea in 1 patient on 150 mg 3 times weekly. There were no DLTs in patients on the 5/2 schedule.
The incidence of grade 3 or higher adverse events (AEs) was 43% (19/44). The most common of these AEs were thrombocytopenia (20%, n=9), neutropenia (7%, n=3), and hyperglycemia (7%, n=3).
Twenty-five percent of patients (11/44) had serious AEs. Three of these events were considered treatment-related. They were epistaxis and the DLTs of diarrhea and hyperglycemia.
AEs led to dose reductions in 6 patients (14%) and treatment discontinuation in 7 patients (16%).
Efficacy
Thirty-seven patients were evaluable for response, and 5 of these patients responded (14%). All responses—2 complete and 3 partial responses—occurred in patients with DLBCL.
Twenty-one of the response-evaluable patients (57%) had stable disease. This included 1 patient with DLBCL, 2 with MM, 8 with HL, and 10 with the “other” types of lymphoma.
The remaining 11 patients progressed (30%)—3 with DLBCL, 2 with MM, 2 with HL, and 4 with other lymphomas.
Thirty-seven patients (84%) discontinued CUDC-907 because of progressive disease or clinical signs of progressive disease at the data cutoff.
Based on the clinical activity of CUDC-907 in patients with relapsed/refractory DLBCL, particularly those with MYC alterations, Curis has initiated a phase 2 trial of the drug in these patients. The recommended phase 2 dose is 60 mg on the 5/2 dosing schedule.