User login
Nerve growth factor therapy speeds gastric ulcer healing
a recent study found.
Compared with young individuals, elderly people have significantly lower levels of NGF in gastric endothelial cells (GECs), a finding that is associated with impaired angiogenesis and delayed gastric ulcer healing.
“Our previous studies have shown that the gastric mucosa of aging individuals ... has increased susceptibility to injury and delayed healing owing to impaired angiogenesis, but the mechanisms are not fully elucidated,” wrote Amrita Ahluwalia, PhD, of Medical and Research Services at the Veterans Affairs Long Beach (Calif.) Healthcare System and her coauthors.
Mapping the drivers of angiogenesis in the gastric mucosa could lead to treatment options for elderly patients with injured or ulcerated gastric tissue. In prior trials (with rats), “treatment with VEGF [vascular endothelial growth factor] only partly reversed impaired angiogenesis in aging [GECs], indicating an essential role for other factor(s) in addition to VEGF,” the investigators wrote in the September issue of Cellular and Molecular Gastroenterology and Hepatology. They looked to NGF as another possible factor because recent studies had shown it could improve angiogenesis in the brain.
The present study measured NGF expression in rats and humans of varying ages, with NGF treatment and gene therapy performed in rats (in vitro and in vivo).
In vitro angiogenesis was 4.1-fold lower in GECs from aging rats (24 months of age) than it was in GECs from young rats (3 months of age; P less than .001). NGF protein and NGF mRNA levels were also significantly lower in aging GECs than they were with young GECs (NGF protein, 3.0-fold lower; NGF mRNA, 4.2-fold lower; P less than .001).
Treatment of aging rat GECs with exogenous NGF increased angiogenesis by 1.5-fold (P less than .001). Pretreatment with a PI3 kinase inhibitor or an mTOR inhibitor abolished this improvement, suggesting that the PI3 kinase/Akt and mTOR pathways are involved.
When NGF gene therapy was performed in aging GECs, NGF levels rose to the level of that in young GECs, with an accompanying restoration of angiogenesis (threefold increase; P less than .001). Proliferation of aging GECs also increased with gene therapy (P less than .001).
In vivo studies revealed that NGF expression and cell proliferation in aging rat gastric mucosa were lower than in younger rats. Of note, older rats treated with local NGF protein showed increased gastric mucosa angiogenesis and faster ulcer healing, compared with phosphate-buffered saline treatment.
Similar age-related NGF declines were found in humans. When gastric mucosa biopsies were collected from younger individuals (younger than 40 years old; n = 10) and compared with samples from an older population (at least 70 years old; n = 10), the investigators found that NGF expression was 5.5-fold lower in the older people (P less than .001).
“This clearly indicates human relevance of our experimental findings and also can explain impaired angiogenesis and delayed healing of injured gastric mucosa in aging individuals,” the investigators wrote.
“Aging gastropathy and its consequences are clinically critical issues,” the investigators noted, “especially because the aging U.S. population is growing rapidly and it is estimated that, by the year 2030, approximately 70 million Americans will be older than 65 years of age.” Gastric ulcers become more common with age, and individuals 70 years or older have an eightfold increased risk of associated complications, compared with people under 50 years.
The investigators noted that multiple growth factors likely play a role in stimulation of angiogenesis, including NGF, VEGF, epidermal growth factor, and basic fibroblast growth factor. “Further studies are necessary to investigate the role of other growth factors and cytokines in angiogenesis, [gastric ulcer] healing, and their impairment in aging,” the investigators concluded.
The study was funded by the Department of Veterans Affairs Biomedical Laboratory Research and Development Service. The authors declared no conflicts of interest.
SOURCE: Ahluwalia A et al. CMGH. 2018 May 17. doi: 10.1016/j.jcmgh.2018.05.003
Although the incidence of gastric ulcers has been declining in the general population, hospitalization and mortality linked to gastric ulcers remains high in the elderly population. One of the major risk factors for gastric ulceration is the use of NSAIDs. It is estimated that 40% of individuals aged 65 years and older fill at least one prescription for an NSAID each year. Given that the elderly population (those aged 65 years and older) is anticipated to more than double by the year 2050, reaching 84 million, understanding the pathogenesis of gastric ulceration is increasingly relevant.
This study described a new role for nerve growth factor (NGF) in promoting angiogenesis during gastric ulcer repair. The authors observed that aged rats exhibited low NGF levels in gastric endothelial cells that corresponded with impaired ulcer healing of the gastric mucosa following injury. Local NGF treatment to aged rats significantly increased angiogenesis and gastric regeneration. Consistent with their in vivo rat model, analysis of human gastric biopsy specimens showed that individuals more than 70 years of age had decreased expression of NGF in gastric endothelial cells, compared with individuals younger than 40 years.
Ahluwalia and colleagues are the first to demonstrate the role of NGF in aging gastropathy, and their work highlights a key mechanism of angiogenesis during gastric repair that may inform future therapeutic strategies.
Amy Christine Engevik, PhD, is a postdoctoral fellow in the division of surgical sciences at Vanderbilt University Medical Center, Nashville, Tenn. She has no conflicts of interest.
Although the incidence of gastric ulcers has been declining in the general population, hospitalization and mortality linked to gastric ulcers remains high in the elderly population. One of the major risk factors for gastric ulceration is the use of NSAIDs. It is estimated that 40% of individuals aged 65 years and older fill at least one prescription for an NSAID each year. Given that the elderly population (those aged 65 years and older) is anticipated to more than double by the year 2050, reaching 84 million, understanding the pathogenesis of gastric ulceration is increasingly relevant.
This study described a new role for nerve growth factor (NGF) in promoting angiogenesis during gastric ulcer repair. The authors observed that aged rats exhibited low NGF levels in gastric endothelial cells that corresponded with impaired ulcer healing of the gastric mucosa following injury. Local NGF treatment to aged rats significantly increased angiogenesis and gastric regeneration. Consistent with their in vivo rat model, analysis of human gastric biopsy specimens showed that individuals more than 70 years of age had decreased expression of NGF in gastric endothelial cells, compared with individuals younger than 40 years.
Ahluwalia and colleagues are the first to demonstrate the role of NGF in aging gastropathy, and their work highlights a key mechanism of angiogenesis during gastric repair that may inform future therapeutic strategies.
Amy Christine Engevik, PhD, is a postdoctoral fellow in the division of surgical sciences at Vanderbilt University Medical Center, Nashville, Tenn. She has no conflicts of interest.
Although the incidence of gastric ulcers has been declining in the general population, hospitalization and mortality linked to gastric ulcers remains high in the elderly population. One of the major risk factors for gastric ulceration is the use of NSAIDs. It is estimated that 40% of individuals aged 65 years and older fill at least one prescription for an NSAID each year. Given that the elderly population (those aged 65 years and older) is anticipated to more than double by the year 2050, reaching 84 million, understanding the pathogenesis of gastric ulceration is increasingly relevant.
This study described a new role for nerve growth factor (NGF) in promoting angiogenesis during gastric ulcer repair. The authors observed that aged rats exhibited low NGF levels in gastric endothelial cells that corresponded with impaired ulcer healing of the gastric mucosa following injury. Local NGF treatment to aged rats significantly increased angiogenesis and gastric regeneration. Consistent with their in vivo rat model, analysis of human gastric biopsy specimens showed that individuals more than 70 years of age had decreased expression of NGF in gastric endothelial cells, compared with individuals younger than 40 years.
Ahluwalia and colleagues are the first to demonstrate the role of NGF in aging gastropathy, and their work highlights a key mechanism of angiogenesis during gastric repair that may inform future therapeutic strategies.
Amy Christine Engevik, PhD, is a postdoctoral fellow in the division of surgical sciences at Vanderbilt University Medical Center, Nashville, Tenn. She has no conflicts of interest.
a recent study found.
Compared with young individuals, elderly people have significantly lower levels of NGF in gastric endothelial cells (GECs), a finding that is associated with impaired angiogenesis and delayed gastric ulcer healing.
“Our previous studies have shown that the gastric mucosa of aging individuals ... has increased susceptibility to injury and delayed healing owing to impaired angiogenesis, but the mechanisms are not fully elucidated,” wrote Amrita Ahluwalia, PhD, of Medical and Research Services at the Veterans Affairs Long Beach (Calif.) Healthcare System and her coauthors.
Mapping the drivers of angiogenesis in the gastric mucosa could lead to treatment options for elderly patients with injured or ulcerated gastric tissue. In prior trials (with rats), “treatment with VEGF [vascular endothelial growth factor] only partly reversed impaired angiogenesis in aging [GECs], indicating an essential role for other factor(s) in addition to VEGF,” the investigators wrote in the September issue of Cellular and Molecular Gastroenterology and Hepatology. They looked to NGF as another possible factor because recent studies had shown it could improve angiogenesis in the brain.
The present study measured NGF expression in rats and humans of varying ages, with NGF treatment and gene therapy performed in rats (in vitro and in vivo).
In vitro angiogenesis was 4.1-fold lower in GECs from aging rats (24 months of age) than it was in GECs from young rats (3 months of age; P less than .001). NGF protein and NGF mRNA levels were also significantly lower in aging GECs than they were with young GECs (NGF protein, 3.0-fold lower; NGF mRNA, 4.2-fold lower; P less than .001).
Treatment of aging rat GECs with exogenous NGF increased angiogenesis by 1.5-fold (P less than .001). Pretreatment with a PI3 kinase inhibitor or an mTOR inhibitor abolished this improvement, suggesting that the PI3 kinase/Akt and mTOR pathways are involved.
When NGF gene therapy was performed in aging GECs, NGF levels rose to the level of that in young GECs, with an accompanying restoration of angiogenesis (threefold increase; P less than .001). Proliferation of aging GECs also increased with gene therapy (P less than .001).
In vivo studies revealed that NGF expression and cell proliferation in aging rat gastric mucosa were lower than in younger rats. Of note, older rats treated with local NGF protein showed increased gastric mucosa angiogenesis and faster ulcer healing, compared with phosphate-buffered saline treatment.
Similar age-related NGF declines were found in humans. When gastric mucosa biopsies were collected from younger individuals (younger than 40 years old; n = 10) and compared with samples from an older population (at least 70 years old; n = 10), the investigators found that NGF expression was 5.5-fold lower in the older people (P less than .001).
“This clearly indicates human relevance of our experimental findings and also can explain impaired angiogenesis and delayed healing of injured gastric mucosa in aging individuals,” the investigators wrote.
“Aging gastropathy and its consequences are clinically critical issues,” the investigators noted, “especially because the aging U.S. population is growing rapidly and it is estimated that, by the year 2030, approximately 70 million Americans will be older than 65 years of age.” Gastric ulcers become more common with age, and individuals 70 years or older have an eightfold increased risk of associated complications, compared with people under 50 years.
The investigators noted that multiple growth factors likely play a role in stimulation of angiogenesis, including NGF, VEGF, epidermal growth factor, and basic fibroblast growth factor. “Further studies are necessary to investigate the role of other growth factors and cytokines in angiogenesis, [gastric ulcer] healing, and their impairment in aging,” the investigators concluded.
The study was funded by the Department of Veterans Affairs Biomedical Laboratory Research and Development Service. The authors declared no conflicts of interest.
SOURCE: Ahluwalia A et al. CMGH. 2018 May 17. doi: 10.1016/j.jcmgh.2018.05.003
a recent study found.
Compared with young individuals, elderly people have significantly lower levels of NGF in gastric endothelial cells (GECs), a finding that is associated with impaired angiogenesis and delayed gastric ulcer healing.
“Our previous studies have shown that the gastric mucosa of aging individuals ... has increased susceptibility to injury and delayed healing owing to impaired angiogenesis, but the mechanisms are not fully elucidated,” wrote Amrita Ahluwalia, PhD, of Medical and Research Services at the Veterans Affairs Long Beach (Calif.) Healthcare System and her coauthors.
Mapping the drivers of angiogenesis in the gastric mucosa could lead to treatment options for elderly patients with injured or ulcerated gastric tissue. In prior trials (with rats), “treatment with VEGF [vascular endothelial growth factor] only partly reversed impaired angiogenesis in aging [GECs], indicating an essential role for other factor(s) in addition to VEGF,” the investigators wrote in the September issue of Cellular and Molecular Gastroenterology and Hepatology. They looked to NGF as another possible factor because recent studies had shown it could improve angiogenesis in the brain.
The present study measured NGF expression in rats and humans of varying ages, with NGF treatment and gene therapy performed in rats (in vitro and in vivo).
In vitro angiogenesis was 4.1-fold lower in GECs from aging rats (24 months of age) than it was in GECs from young rats (3 months of age; P less than .001). NGF protein and NGF mRNA levels were also significantly lower in aging GECs than they were with young GECs (NGF protein, 3.0-fold lower; NGF mRNA, 4.2-fold lower; P less than .001).
Treatment of aging rat GECs with exogenous NGF increased angiogenesis by 1.5-fold (P less than .001). Pretreatment with a PI3 kinase inhibitor or an mTOR inhibitor abolished this improvement, suggesting that the PI3 kinase/Akt and mTOR pathways are involved.
When NGF gene therapy was performed in aging GECs, NGF levels rose to the level of that in young GECs, with an accompanying restoration of angiogenesis (threefold increase; P less than .001). Proliferation of aging GECs also increased with gene therapy (P less than .001).
In vivo studies revealed that NGF expression and cell proliferation in aging rat gastric mucosa were lower than in younger rats. Of note, older rats treated with local NGF protein showed increased gastric mucosa angiogenesis and faster ulcer healing, compared with phosphate-buffered saline treatment.
Similar age-related NGF declines were found in humans. When gastric mucosa biopsies were collected from younger individuals (younger than 40 years old; n = 10) and compared with samples from an older population (at least 70 years old; n = 10), the investigators found that NGF expression was 5.5-fold lower in the older people (P less than .001).
“This clearly indicates human relevance of our experimental findings and also can explain impaired angiogenesis and delayed healing of injured gastric mucosa in aging individuals,” the investigators wrote.
“Aging gastropathy and its consequences are clinically critical issues,” the investigators noted, “especially because the aging U.S. population is growing rapidly and it is estimated that, by the year 2030, approximately 70 million Americans will be older than 65 years of age.” Gastric ulcers become more common with age, and individuals 70 years or older have an eightfold increased risk of associated complications, compared with people under 50 years.
The investigators noted that multiple growth factors likely play a role in stimulation of angiogenesis, including NGF, VEGF, epidermal growth factor, and basic fibroblast growth factor. “Further studies are necessary to investigate the role of other growth factors and cytokines in angiogenesis, [gastric ulcer] healing, and their impairment in aging,” the investigators concluded.
The study was funded by the Department of Veterans Affairs Biomedical Laboratory Research and Development Service. The authors declared no conflicts of interest.
SOURCE: Ahluwalia A et al. CMGH. 2018 May 17. doi: 10.1016/j.jcmgh.2018.05.003
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Nerve growth factor (NGF) therapy in aging rats improves angiogenesis and speeds gastric ulcer (GU) healing, suggesting possible applications in human medicine.
Major finding: Compared with young individuals, elderly people have 5.5-fold lower NGF expression in their gastric mucosa.
Study details: A prospective study involving rats and humans, with NGF therapy performed in rats.
Disclosures: The study was funded by the Department of Veterans Affairs Biomedical Laboratory Research and Development Service. The authors declared no conflicts of interest.
Source: Ahluwalia et al. CMGH. 2018 May 17. doi: 10.1016/j.jcmgh.2018.05.003
Patient transfers between hospitals contribute substantially to CDI burden
ATLANTA – Patient sharing among hospital facilities contributed substantially to the overall Clostridium difficile infection rate, an analysis of interhospital contamination effects showed.
In fact, 7.6% of all Clostridium difficile infection (CDI) cases at the nearly 400 California hospitals included in the study were directly attributable to the patient-sharing network, Daniel Sewell, PhD, reported at the International Conference on Emerging Infectious Diseases.
“The methods that we employed allowed us to estimate the expected increase in CDI cases due to transfers as a function of the CDI rate at the hospital from which those patients were brought. These transfer patients were responsible for about 3.06 times the number of CDI cases as a normal patient,” said Dr. Sewell, a biostatistician at the University of Iowa, Iowa City.
The findings, which underscored the importance of regional (rather than local) efforts to minimize the spread of health care–associated infections, are based on an analysis of 27,200,873 hospital admissions and 532,320 same-day patient transfers identified from the Healthcare Cost and Utilization Project California State Inpatient Database for 2005-2011.
Transfer networks based on the monthly average number of patients discharged from one hospital and admitted to another on the same day were constructed, and the monthly average number of CDI cases per hospital were considered, along with hospital-level characteristics such as patient length of stay, age, and number of diagnoses. Network autocorrelation models that help eliminate bias were then used to assess the contamination effects between hospitals, he explained.
This led to development of an equation that can be used to determine the expected number of CDI cases in a hospital as a function of the number of transfers coming in and the contamination level of the source hospitals. The ability to calculate the expected number of CDI cases in this fashion is an important factor for the success of regional versus local intervention efforts, which are increasingly thought to be important for reducing health care–associated infections.
“If we want to design a coordinated or regional approach, we’ve got to have a much better understanding of the role that patient transfers have in these diseases,” Dr. Sewell said.
As most hospitals included in the study had a low CDI rate and a low transfer rate, the CDIs attributable to transfers represent a minority of cases, but they are a substantial minority, he said, noting that the main concern is with the “perfect storm” of high CDI rate plus high transfer rate.
The methodological approach used in this study to estimate CDI rates can be used for any health care–associated infection of interest, he added.
Dr. Sewell reported that he had no disclosures.
The AGA Fecal Microbiota Transplantation (FMT) National Registry will assess short- and long-term patient outcomes associated with FMT. Learn more at http://ow.ly/WdQE30lBuSu
ATLANTA – Patient sharing among hospital facilities contributed substantially to the overall Clostridium difficile infection rate, an analysis of interhospital contamination effects showed.
In fact, 7.6% of all Clostridium difficile infection (CDI) cases at the nearly 400 California hospitals included in the study were directly attributable to the patient-sharing network, Daniel Sewell, PhD, reported at the International Conference on Emerging Infectious Diseases.
“The methods that we employed allowed us to estimate the expected increase in CDI cases due to transfers as a function of the CDI rate at the hospital from which those patients were brought. These transfer patients were responsible for about 3.06 times the number of CDI cases as a normal patient,” said Dr. Sewell, a biostatistician at the University of Iowa, Iowa City.
The findings, which underscored the importance of regional (rather than local) efforts to minimize the spread of health care–associated infections, are based on an analysis of 27,200,873 hospital admissions and 532,320 same-day patient transfers identified from the Healthcare Cost and Utilization Project California State Inpatient Database for 2005-2011.
Transfer networks based on the monthly average number of patients discharged from one hospital and admitted to another on the same day were constructed, and the monthly average number of CDI cases per hospital were considered, along with hospital-level characteristics such as patient length of stay, age, and number of diagnoses. Network autocorrelation models that help eliminate bias were then used to assess the contamination effects between hospitals, he explained.
This led to development of an equation that can be used to determine the expected number of CDI cases in a hospital as a function of the number of transfers coming in and the contamination level of the source hospitals. The ability to calculate the expected number of CDI cases in this fashion is an important factor for the success of regional versus local intervention efforts, which are increasingly thought to be important for reducing health care–associated infections.
“If we want to design a coordinated or regional approach, we’ve got to have a much better understanding of the role that patient transfers have in these diseases,” Dr. Sewell said.
As most hospitals included in the study had a low CDI rate and a low transfer rate, the CDIs attributable to transfers represent a minority of cases, but they are a substantial minority, he said, noting that the main concern is with the “perfect storm” of high CDI rate plus high transfer rate.
The methodological approach used in this study to estimate CDI rates can be used for any health care–associated infection of interest, he added.
Dr. Sewell reported that he had no disclosures.
The AGA Fecal Microbiota Transplantation (FMT) National Registry will assess short- and long-term patient outcomes associated with FMT. Learn more at http://ow.ly/WdQE30lBuSu
ATLANTA – Patient sharing among hospital facilities contributed substantially to the overall Clostridium difficile infection rate, an analysis of interhospital contamination effects showed.
In fact, 7.6% of all Clostridium difficile infection (CDI) cases at the nearly 400 California hospitals included in the study were directly attributable to the patient-sharing network, Daniel Sewell, PhD, reported at the International Conference on Emerging Infectious Diseases.
“The methods that we employed allowed us to estimate the expected increase in CDI cases due to transfers as a function of the CDI rate at the hospital from which those patients were brought. These transfer patients were responsible for about 3.06 times the number of CDI cases as a normal patient,” said Dr. Sewell, a biostatistician at the University of Iowa, Iowa City.
The findings, which underscored the importance of regional (rather than local) efforts to minimize the spread of health care–associated infections, are based on an analysis of 27,200,873 hospital admissions and 532,320 same-day patient transfers identified from the Healthcare Cost and Utilization Project California State Inpatient Database for 2005-2011.
Transfer networks based on the monthly average number of patients discharged from one hospital and admitted to another on the same day were constructed, and the monthly average number of CDI cases per hospital were considered, along with hospital-level characteristics such as patient length of stay, age, and number of diagnoses. Network autocorrelation models that help eliminate bias were then used to assess the contamination effects between hospitals, he explained.
This led to development of an equation that can be used to determine the expected number of CDI cases in a hospital as a function of the number of transfers coming in and the contamination level of the source hospitals. The ability to calculate the expected number of CDI cases in this fashion is an important factor for the success of regional versus local intervention efforts, which are increasingly thought to be important for reducing health care–associated infections.
“If we want to design a coordinated or regional approach, we’ve got to have a much better understanding of the role that patient transfers have in these diseases,” Dr. Sewell said.
As most hospitals included in the study had a low CDI rate and a low transfer rate, the CDIs attributable to transfers represent a minority of cases, but they are a substantial minority, he said, noting that the main concern is with the “perfect storm” of high CDI rate plus high transfer rate.
The methodological approach used in this study to estimate CDI rates can be used for any health care–associated infection of interest, he added.
Dr. Sewell reported that he had no disclosures.
The AGA Fecal Microbiota Transplantation (FMT) National Registry will assess short- and long-term patient outcomes associated with FMT. Learn more at http://ow.ly/WdQE30lBuSu
REPORTING FROM ICEID 2018
Key clinical point: Patient sharing among hospitals contributes substantially to Clostridium difficile infection (CDI) rates.
Major finding: Patient transfers account for 7.6% of the overall CDI burden.
Study details: A statistical analysis to estimate interhospital CDI transmissions.
Disclosures: Dr. Sewell reported that he had no disclosures.
Eosinophils could be a marker for nonceliac gluten or wheat sensitivity
.
NCGWS could be considered an inflammatory condition of the entire intestinal track and the eosinophil infiltration “may represent a key candidate player” in its pathogenesis, wrote the authors, led by Antonio Carroccio, MD, of Giovanni Paolo II Hospital, Sciacca, and DiBiMIS University of Palermo, Italy. The report is in Clinical Gastroenterology and Hepatology.
The research team noted that duodenal histology, a lack of villous atrophy, and evaluation of intraepithelial infiltration of the duodenal mucosa were the usual steps involved in the diagnostic work-up of NCGWS.
Many people with NCGWS had symptoms that overlapped with irritable bowel syndrome but no studies had evaluated histologic features of duodenal and rectal biopsies from these patients.
“Alterations of the mucosal immune system are believed to play a role in IBS and some patients may indeed have inflammation of the colonic mucosa. Consequently, it would be logical to study the colon of NCGWS patients for possible inflammation in this site,” they wrote.
The current study involved 78 consecutive adult patients attending two tertiary referral centers in Italy. The average age of the patients was 36.4 years and they were diagnosed with NCGWS through a double-blind wheat challenge. A non-NCGWS control group of 55 patients had either celiac disease (n = 16) or self-reported NCGWS but with negative results from the wheat challenge (n = 39).
Both duodenal and rectal biopsies were performed in both groups of patients after they had consumed a wheat-containing diet (a minimum of 100 g) for at least 4 weeks.
The researchers then analyzed intraepithelial CD3+T cells, lamina propria CD45+ cells, CD4+ and CD8+ T cells, mast cells, and eosinophils as well as the presence and size of lymphoid nodules.
Histologic evaluation of the duodenal mucosa showed that none of the NCGWS patients or non-NCGWS controls had a villus/crypt ratio less than 3, whereas all the controls with celiac disease (CD) had villous atrophy.
Mucosal inflammation both in the duodenum and the rectal mucosa was common in patients with NCGWS. For example, intraepithelial CD3+ lymphocytes progressively increased from the non-NCGWS controls (14.3 ± 4.2) to NCGWS patients (19.6 ± 10.7; P less than .03) and CD controls (47.7 ± 23.3; P less than .001 vs. NCGWS patients).
Lamina propria CD45+ cells, which the authors said represented the “total immunocyte” infiltration were significantly higher in NCGWS patients than in the non-NCGWS controls at both sites.
In patients with NCGWS, the mean eosinophil infiltration was more than 2.5-fold the upper normal limit in the rectum and nearly twice the upper normal limit in the duodenum (P less than .0001).
Eosinophil numbers in the duodenal mucosa were also higher in the NCGWS patients with dyspepsia than in the NCGWS patients without upper digestive tract symptoms.
For example, in 33 patients who reported upper digestive tract symptoms, the number of lamina propria eosinophils was significantly higher than in the remaining NCGWS patients who did not report symptoms (8.6 ± 2.6 vs. 6.8 ± 3.6; P less than .01).
“Functional dyspepsia is frequently associated with IBS [irritable bowel syndrome], suggesting that these two diseases have a shared pathogenesis,” the researchers speculated.
The researchers suggested that in the absence of endoscopic findings, eosinophil infiltration of the rectal mucosa could be a marker of NCGWS, noting that it could not be considered a specific marker as eosinophils were found in the colon and rectal mucosa in several clinical conditions, such as inflammatory bowel diseases and celiac disease.
“However, these clinical conditions have clinical, endoscopic, serologic, and histologic aspects markedly different from NCGWS. ... We would suggest that in clinical practice, subjects showing an IBS clinical presentation and mucosa eosinophil infiltration should be recommended to commence an elimination diet with a subsequent wheat challenge,” they said.
The authors said another noteworthy finding from their study was that about 95% of patients had lymphoid follicles that were significantly larger than those of the control group. Although this can be considered a “normal” finding in rectal mucosa, they said in their experience the presence of large follicles was associated with non-IgE mediated food allergy.
“It can be hypothesized that not only eosinophils could play a pathogenetic role in NCGWS, and that a complex immunologic response involving both innate and acquired immunity may be responsible for this disease,” they said.
A study limitation was selection bias stemming from the fact that the cohort included patients referred to tertiary centers, they noted. “Our results must not be extended to all self-treated or diagnosed NCGWS patients,” they cautioned.
SOURCE: Clin Gastroenterol Hepatol. 2018 Aug 20. doi: 10.1016/j.cgh.2018.08.043.
.
NCGWS could be considered an inflammatory condition of the entire intestinal track and the eosinophil infiltration “may represent a key candidate player” in its pathogenesis, wrote the authors, led by Antonio Carroccio, MD, of Giovanni Paolo II Hospital, Sciacca, and DiBiMIS University of Palermo, Italy. The report is in Clinical Gastroenterology and Hepatology.
The research team noted that duodenal histology, a lack of villous atrophy, and evaluation of intraepithelial infiltration of the duodenal mucosa were the usual steps involved in the diagnostic work-up of NCGWS.
Many people with NCGWS had symptoms that overlapped with irritable bowel syndrome but no studies had evaluated histologic features of duodenal and rectal biopsies from these patients.
“Alterations of the mucosal immune system are believed to play a role in IBS and some patients may indeed have inflammation of the colonic mucosa. Consequently, it would be logical to study the colon of NCGWS patients for possible inflammation in this site,” they wrote.
The current study involved 78 consecutive adult patients attending two tertiary referral centers in Italy. The average age of the patients was 36.4 years and they were diagnosed with NCGWS through a double-blind wheat challenge. A non-NCGWS control group of 55 patients had either celiac disease (n = 16) or self-reported NCGWS but with negative results from the wheat challenge (n = 39).
Both duodenal and rectal biopsies were performed in both groups of patients after they had consumed a wheat-containing diet (a minimum of 100 g) for at least 4 weeks.
The researchers then analyzed intraepithelial CD3+T cells, lamina propria CD45+ cells, CD4+ and CD8+ T cells, mast cells, and eosinophils as well as the presence and size of lymphoid nodules.
Histologic evaluation of the duodenal mucosa showed that none of the NCGWS patients or non-NCGWS controls had a villus/crypt ratio less than 3, whereas all the controls with celiac disease (CD) had villous atrophy.
Mucosal inflammation both in the duodenum and the rectal mucosa was common in patients with NCGWS. For example, intraepithelial CD3+ lymphocytes progressively increased from the non-NCGWS controls (14.3 ± 4.2) to NCGWS patients (19.6 ± 10.7; P less than .03) and CD controls (47.7 ± 23.3; P less than .001 vs. NCGWS patients).
Lamina propria CD45+ cells, which the authors said represented the “total immunocyte” infiltration were significantly higher in NCGWS patients than in the non-NCGWS controls at both sites.
In patients with NCGWS, the mean eosinophil infiltration was more than 2.5-fold the upper normal limit in the rectum and nearly twice the upper normal limit in the duodenum (P less than .0001).
Eosinophil numbers in the duodenal mucosa were also higher in the NCGWS patients with dyspepsia than in the NCGWS patients without upper digestive tract symptoms.
For example, in 33 patients who reported upper digestive tract symptoms, the number of lamina propria eosinophils was significantly higher than in the remaining NCGWS patients who did not report symptoms (8.6 ± 2.6 vs. 6.8 ± 3.6; P less than .01).
“Functional dyspepsia is frequently associated with IBS [irritable bowel syndrome], suggesting that these two diseases have a shared pathogenesis,” the researchers speculated.
The researchers suggested that in the absence of endoscopic findings, eosinophil infiltration of the rectal mucosa could be a marker of NCGWS, noting that it could not be considered a specific marker as eosinophils were found in the colon and rectal mucosa in several clinical conditions, such as inflammatory bowel diseases and celiac disease.
“However, these clinical conditions have clinical, endoscopic, serologic, and histologic aspects markedly different from NCGWS. ... We would suggest that in clinical practice, subjects showing an IBS clinical presentation and mucosa eosinophil infiltration should be recommended to commence an elimination diet with a subsequent wheat challenge,” they said.
The authors said another noteworthy finding from their study was that about 95% of patients had lymphoid follicles that were significantly larger than those of the control group. Although this can be considered a “normal” finding in rectal mucosa, they said in their experience the presence of large follicles was associated with non-IgE mediated food allergy.
“It can be hypothesized that not only eosinophils could play a pathogenetic role in NCGWS, and that a complex immunologic response involving both innate and acquired immunity may be responsible for this disease,” they said.
A study limitation was selection bias stemming from the fact that the cohort included patients referred to tertiary centers, they noted. “Our results must not be extended to all self-treated or diagnosed NCGWS patients,” they cautioned.
SOURCE: Clin Gastroenterol Hepatol. 2018 Aug 20. doi: 10.1016/j.cgh.2018.08.043.
.
NCGWS could be considered an inflammatory condition of the entire intestinal track and the eosinophil infiltration “may represent a key candidate player” in its pathogenesis, wrote the authors, led by Antonio Carroccio, MD, of Giovanni Paolo II Hospital, Sciacca, and DiBiMIS University of Palermo, Italy. The report is in Clinical Gastroenterology and Hepatology.
The research team noted that duodenal histology, a lack of villous atrophy, and evaluation of intraepithelial infiltration of the duodenal mucosa were the usual steps involved in the diagnostic work-up of NCGWS.
Many people with NCGWS had symptoms that overlapped with irritable bowel syndrome but no studies had evaluated histologic features of duodenal and rectal biopsies from these patients.
“Alterations of the mucosal immune system are believed to play a role in IBS and some patients may indeed have inflammation of the colonic mucosa. Consequently, it would be logical to study the colon of NCGWS patients for possible inflammation in this site,” they wrote.
The current study involved 78 consecutive adult patients attending two tertiary referral centers in Italy. The average age of the patients was 36.4 years and they were diagnosed with NCGWS through a double-blind wheat challenge. A non-NCGWS control group of 55 patients had either celiac disease (n = 16) or self-reported NCGWS but with negative results from the wheat challenge (n = 39).
Both duodenal and rectal biopsies were performed in both groups of patients after they had consumed a wheat-containing diet (a minimum of 100 g) for at least 4 weeks.
The researchers then analyzed intraepithelial CD3+T cells, lamina propria CD45+ cells, CD4+ and CD8+ T cells, mast cells, and eosinophils as well as the presence and size of lymphoid nodules.
Histologic evaluation of the duodenal mucosa showed that none of the NCGWS patients or non-NCGWS controls had a villus/crypt ratio less than 3, whereas all the controls with celiac disease (CD) had villous atrophy.
Mucosal inflammation both in the duodenum and the rectal mucosa was common in patients with NCGWS. For example, intraepithelial CD3+ lymphocytes progressively increased from the non-NCGWS controls (14.3 ± 4.2) to NCGWS patients (19.6 ± 10.7; P less than .03) and CD controls (47.7 ± 23.3; P less than .001 vs. NCGWS patients).
Lamina propria CD45+ cells, which the authors said represented the “total immunocyte” infiltration were significantly higher in NCGWS patients than in the non-NCGWS controls at both sites.
In patients with NCGWS, the mean eosinophil infiltration was more than 2.5-fold the upper normal limit in the rectum and nearly twice the upper normal limit in the duodenum (P less than .0001).
Eosinophil numbers in the duodenal mucosa were also higher in the NCGWS patients with dyspepsia than in the NCGWS patients without upper digestive tract symptoms.
For example, in 33 patients who reported upper digestive tract symptoms, the number of lamina propria eosinophils was significantly higher than in the remaining NCGWS patients who did not report symptoms (8.6 ± 2.6 vs. 6.8 ± 3.6; P less than .01).
“Functional dyspepsia is frequently associated with IBS [irritable bowel syndrome], suggesting that these two diseases have a shared pathogenesis,” the researchers speculated.
The researchers suggested that in the absence of endoscopic findings, eosinophil infiltration of the rectal mucosa could be a marker of NCGWS, noting that it could not be considered a specific marker as eosinophils were found in the colon and rectal mucosa in several clinical conditions, such as inflammatory bowel diseases and celiac disease.
“However, these clinical conditions have clinical, endoscopic, serologic, and histologic aspects markedly different from NCGWS. ... We would suggest that in clinical practice, subjects showing an IBS clinical presentation and mucosa eosinophil infiltration should be recommended to commence an elimination diet with a subsequent wheat challenge,” they said.
The authors said another noteworthy finding from their study was that about 95% of patients had lymphoid follicles that were significantly larger than those of the control group. Although this can be considered a “normal” finding in rectal mucosa, they said in their experience the presence of large follicles was associated with non-IgE mediated food allergy.
“It can be hypothesized that not only eosinophils could play a pathogenetic role in NCGWS, and that a complex immunologic response involving both innate and acquired immunity may be responsible for this disease,” they said.
A study limitation was selection bias stemming from the fact that the cohort included patients referred to tertiary centers, they noted. “Our results must not be extended to all self-treated or diagnosed NCGWS patients,” they cautioned.
SOURCE: Clin Gastroenterol Hepatol. 2018 Aug 20. doi: 10.1016/j.cgh.2018.08.043.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: The evaluation of patients for nonceliac gluten or wheat sensitivity should include histologic analysis of rectal biopsies.
Major finding: Mucosal inflammation in the duodenum and in the rectal mucosa was common in patients with NCGWS. In these patients the mean eosinophil infiltration was more than 2.5-fold the upper normal limit in the rectum and nearly twice the upper normal limit in the duodenum (P less than .0001).
Study details: A prospective study of 78 patients with NCGWS and 55 controls with either celiac disease or self-reported NCGWS but negative wheat challenge results.
Disclosures: The Italian Foundation for Celiac Disease funded the study. The authors declared no conflicts of interest.
Source: Clin Gastroenterol Hepatol. 2018 Aug 20. doi: 10.1016/j.cgh.2018.08.043.
Three Clinical Studies Demonstrating Safety and Efficacy of Treatment for Diarrhea-Predominant Irritable Bowel Syndrome (IBS-D) in Adults
In this supplement to GI & Hepatology news, Christine Frissora, MD, provides an overview of the burdens that patients with IBS-D experience. Three clinical efficacy and safety studies surrounding an FDA-approved treatment are also examined.
Topics include:
- IBS-D diagnosis and treatment challenges
- The role of microbial imbalance and altered gut microbiota
- A treatment option for relief of IBS-D symptoms
XIFI.0273.USA.18
In this supplement to GI & Hepatology news, Christine Frissora, MD, provides an overview of the burdens that patients with IBS-D experience. Three clinical efficacy and safety studies surrounding an FDA-approved treatment are also examined.
Topics include:
- IBS-D diagnosis and treatment challenges
- The role of microbial imbalance and altered gut microbiota
- A treatment option for relief of IBS-D symptoms
XIFI.0273.USA.18
In this supplement to GI & Hepatology news, Christine Frissora, MD, provides an overview of the burdens that patients with IBS-D experience. Three clinical efficacy and safety studies surrounding an FDA-approved treatment are also examined.
Topics include:
- IBS-D diagnosis and treatment challenges
- The role of microbial imbalance and altered gut microbiota
- A treatment option for relief of IBS-D symptoms
XIFI.0273.USA.18
Surgical outcomes for UC worse since introduction of biologics
Since the approval of more UC patients are having multiple operations to manage their disease and their surgical outcomes tend to be worse, according to a study published in Annals of Surgery.
“Encouragingly, early randomized controlled trials demonstrated that infliximab may reduce the short-term need for surgery,” wrote Jonathan Abelson, MD, of the department of surgery, Cornell University, New York, and his coauthors. “However, even after the development and approval of several other biologic agents to treat UC, 30%-66% of patients treated with biologic agents still ultimately require surgical intervention.”
The study reviewed records of 7,070 patients with UC in a New York State Department of Health database who had colorectal surgery in two comparative time periods: 3,803 from 1995 to 2005, before biologics were available, and 3,267 from 2006 to 2013, after infliximab was approved. Dr. Abelson and coauthors said this is the first study to look at long-term surgical outcomes in a large group of patients with UC over an extended time period. Previous studies have reported conflicting results of how biologic agents for UC can impact surgical outcomes. The researchers set out to explore two hypotheses: whether staged procedures increased after 2005 and whether UC patients had worse outcomes over the past decade. The study results validated both hypotheses. Up until 2005, the proportion of patients who underwent at least three procedures after the index hospitalization was 9%; after 2006, that proportion was 14% (P less than .01).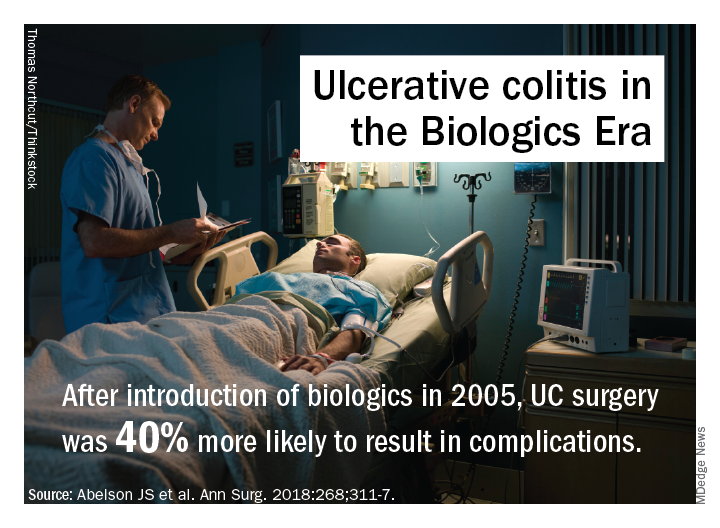
A potential explanation for trends in postsurgery death may be higher rates of Clostridium difficile after 2005 (10.6% vs. 5.8%; P less than .01), but that was accounted for in the adjusted analysis and is probably not a major factor, the researchers said. After 2006 patients were slightly older and more likely to be on Medicare and nonwhite; they also were sicker, with 28% having two or more comorbidities vs. 10% before 2006.
The investigators offered another explanation: “It is also possible that the immunosuppressive effect of biologic agents ... predisposes patients to worse postoperative outcomes. In addition, it is possible that patients are referred for surgery too late in their disease course because of prolonged medical therapy.”
Dr. Abelson and coauthors reported having no financial relationships.
SOURCE: Abelson JS et al. Ann Surg. 2018:268;311-7.
Since the approval of more UC patients are having multiple operations to manage their disease and their surgical outcomes tend to be worse, according to a study published in Annals of Surgery.
“Encouragingly, early randomized controlled trials demonstrated that infliximab may reduce the short-term need for surgery,” wrote Jonathan Abelson, MD, of the department of surgery, Cornell University, New York, and his coauthors. “However, even after the development and approval of several other biologic agents to treat UC, 30%-66% of patients treated with biologic agents still ultimately require surgical intervention.”
The study reviewed records of 7,070 patients with UC in a New York State Department of Health database who had colorectal surgery in two comparative time periods: 3,803 from 1995 to 2005, before biologics were available, and 3,267 from 2006 to 2013, after infliximab was approved. Dr. Abelson and coauthors said this is the first study to look at long-term surgical outcomes in a large group of patients with UC over an extended time period. Previous studies have reported conflicting results of how biologic agents for UC can impact surgical outcomes. The researchers set out to explore two hypotheses: whether staged procedures increased after 2005 and whether UC patients had worse outcomes over the past decade. The study results validated both hypotheses. Up until 2005, the proportion of patients who underwent at least three procedures after the index hospitalization was 9%; after 2006, that proportion was 14% (P less than .01).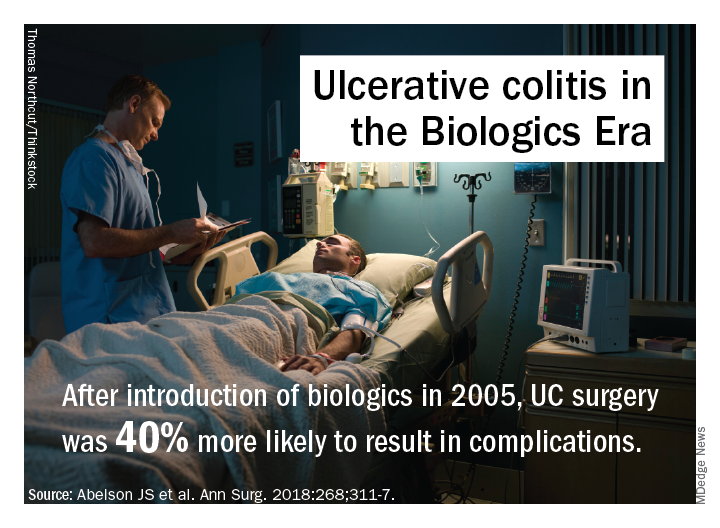
A potential explanation for trends in postsurgery death may be higher rates of Clostridium difficile after 2005 (10.6% vs. 5.8%; P less than .01), but that was accounted for in the adjusted analysis and is probably not a major factor, the researchers said. After 2006 patients were slightly older and more likely to be on Medicare and nonwhite; they also were sicker, with 28% having two or more comorbidities vs. 10% before 2006.
The investigators offered another explanation: “It is also possible that the immunosuppressive effect of biologic agents ... predisposes patients to worse postoperative outcomes. In addition, it is possible that patients are referred for surgery too late in their disease course because of prolonged medical therapy.”
Dr. Abelson and coauthors reported having no financial relationships.
SOURCE: Abelson JS et al. Ann Surg. 2018:268;311-7.
Since the approval of more UC patients are having multiple operations to manage their disease and their surgical outcomes tend to be worse, according to a study published in Annals of Surgery.
“Encouragingly, early randomized controlled trials demonstrated that infliximab may reduce the short-term need for surgery,” wrote Jonathan Abelson, MD, of the department of surgery, Cornell University, New York, and his coauthors. “However, even after the development and approval of several other biologic agents to treat UC, 30%-66% of patients treated with biologic agents still ultimately require surgical intervention.”
The study reviewed records of 7,070 patients with UC in a New York State Department of Health database who had colorectal surgery in two comparative time periods: 3,803 from 1995 to 2005, before biologics were available, and 3,267 from 2006 to 2013, after infliximab was approved. Dr. Abelson and coauthors said this is the first study to look at long-term surgical outcomes in a large group of patients with UC over an extended time period. Previous studies have reported conflicting results of how biologic agents for UC can impact surgical outcomes. The researchers set out to explore two hypotheses: whether staged procedures increased after 2005 and whether UC patients had worse outcomes over the past decade. The study results validated both hypotheses. Up until 2005, the proportion of patients who underwent at least three procedures after the index hospitalization was 9%; after 2006, that proportion was 14% (P less than .01).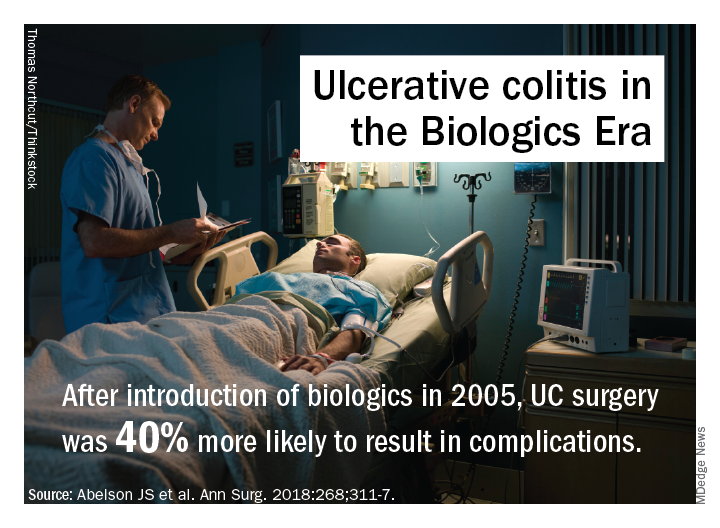
A potential explanation for trends in postsurgery death may be higher rates of Clostridium difficile after 2005 (10.6% vs. 5.8%; P less than .01), but that was accounted for in the adjusted analysis and is probably not a major factor, the researchers said. After 2006 patients were slightly older and more likely to be on Medicare and nonwhite; they also were sicker, with 28% having two or more comorbidities vs. 10% before 2006.
The investigators offered another explanation: “It is also possible that the immunosuppressive effect of biologic agents ... predisposes patients to worse postoperative outcomes. In addition, it is possible that patients are referred for surgery too late in their disease course because of prolonged medical therapy.”
Dr. Abelson and coauthors reported having no financial relationships.
SOURCE: Abelson JS et al. Ann Surg. 2018:268;311-7.
FROM ANNALS OF SURGERY
Key clinical point: Rates of multiple surgeries for ulcerative colitis have increased since biologic agents were introduced.
Major finding: Fourteen percent of patients have had multiple operations since 2006 vs. 9% before that.
Study details: A longitudinal analysis of 7,070 patients in the New York State Department of Health of Health Statewide Planning and Research Cooperative System database who had surgery for UC from 1995 to 2013.
Disclosures: Dr. Abelson and coauthors reported having no financial relationships.
Source: Abelson JS et al. Ann Surg. 2018;268:311-7.
‘Game of Crohn’s ... and colitis’
Here is an update on the rapidly moving field of inflammatory bowel disease (IBD), from the power of the microbiome to the prediction of IBD and new ways to use established drugs.
Regarding the microbiome, we now understand that, while the healthy microbiome is diverse and able to produce short-chain fatty acids, such as butyrate, the dysbiotic IBD microbiome is less diverse and characterized by expansion of proinflammatory pathobionts (such as Fusobacterium), the proliferation of sulfate-reducing bacteria, and a decrease in anti-inflammatory butyrate production.
There have now been several promising trials of fecal microbial transplant (FMT) for the treatment of ulcerative colitis (UC). The most effective strategies have involved colonic delivery of FMT, pooled donors, and repeated stool enemas to solidify the response. Following FMT, patients’ microbial diversity increases. The hope is that we can use diet as a complement to maintain the diversity and generation of beneficial metabolites, as well as deliver the therapy orally.
Predicting IBD
Although we have made advances in therapy, we continue to miss opportunities to prevent long-term complications. At Digestive Disease Week,® Jean-Frederic Colombel, MD, a professor of medicine at the Icahn School of Medicine at Mount Sinai, New York, presented data on the PREDICTS study (Aliment Pharacol Ther. 2016 Jun;43[12]:1300-10), in which serum samples collected from military recruits prior to development of IBD was used to identify serologic markers that could predict those who ultimately developed Crohn’s disease but not UC.
The pediatric medical community, meanwhile, has studied an inception cohort of newly diagnosed, untreated children – the RISK cohort ( Lancet. 2017 Apr 29;389[10080]:1710-8 ) – to define some of the risk factors that predict more aggressive disease. By using biopsy tissue from the time of diagnosis, investigators could predict who would develop stricturing disease versus penetrating disease. Patients who would develop penetrating disease had up-regulation of inflammatory pathways and responded to anti–tumor necrosis factor therapy, while those who developed a stricturing phenotype had increased expression of extracellular matrix pathways and were significantly less likely to respond to anti-TNF therapy ( Lancet. 2017 Apr 29;389[10080]:1710-8 ). These studies provide a proof of concept that we might someday be able to use for personalized approaches to treating IBD.
Using new drugs, targeting new pathways
The recently published CALM study tested the hypothesis that treating to a target of no biochemical inflammation (elevated C reactive protein or fecal calprotectin) would be better than symptom-driven treatment alone. Treatment escalation for active disease included adalimumab every other week, then weekly adalimumab, and finally the addition of azathioprine. At the end of the study, patients whose medical therapy was based on both symptoms and biochemical inflammation had a higher degree of mucosal healing than did patients in the clinical management group (Lancet. 2018 Dec 23;390[10114]:2779-89).
Ustekinumab is a monoclonal antibody that targets the p40 subunit of interleukin-12 and interleukin-23 and is approved for Crohn’s disease. Various pharmaceutical companies are now developing anti-p19 antibodies, which block IL-23 only; at DDW 2018, the anti–IL-23 mirikizumab was shown to be effective in UC. We are also seeing the availability of oral medications for IBD. Just prior to DDW, tofacitinib ( N Engl J Med. 2017 May 4;376:1723-36 ), a Janus kinase (JAK) 1/3 inhibitor, which has an effect on multiple different cytokine pathways, received approval for UC. Other JAK inhibitors with different specificities are being tested in trials of UC and Crohn’s disease.
Dr. Abreu is a professor of medicine, a professor of microbiology and immunology, and the director of the Crohn’s & Colitis Center at the University of Miami Miller School of Medicine. She has no conflicts of interest. Dr. Abreu made her comments during the AGA Institute Presidential Plenary at the Annual Digestive Disease Week.
Here is an update on the rapidly moving field of inflammatory bowel disease (IBD), from the power of the microbiome to the prediction of IBD and new ways to use established drugs.
Regarding the microbiome, we now understand that, while the healthy microbiome is diverse and able to produce short-chain fatty acids, such as butyrate, the dysbiotic IBD microbiome is less diverse and characterized by expansion of proinflammatory pathobionts (such as Fusobacterium), the proliferation of sulfate-reducing bacteria, and a decrease in anti-inflammatory butyrate production.
There have now been several promising trials of fecal microbial transplant (FMT) for the treatment of ulcerative colitis (UC). The most effective strategies have involved colonic delivery of FMT, pooled donors, and repeated stool enemas to solidify the response. Following FMT, patients’ microbial diversity increases. The hope is that we can use diet as a complement to maintain the diversity and generation of beneficial metabolites, as well as deliver the therapy orally.
Predicting IBD
Although we have made advances in therapy, we continue to miss opportunities to prevent long-term complications. At Digestive Disease Week,® Jean-Frederic Colombel, MD, a professor of medicine at the Icahn School of Medicine at Mount Sinai, New York, presented data on the PREDICTS study (Aliment Pharacol Ther. 2016 Jun;43[12]:1300-10), in which serum samples collected from military recruits prior to development of IBD was used to identify serologic markers that could predict those who ultimately developed Crohn’s disease but not UC.
The pediatric medical community, meanwhile, has studied an inception cohort of newly diagnosed, untreated children – the RISK cohort ( Lancet. 2017 Apr 29;389[10080]:1710-8 ) – to define some of the risk factors that predict more aggressive disease. By using biopsy tissue from the time of diagnosis, investigators could predict who would develop stricturing disease versus penetrating disease. Patients who would develop penetrating disease had up-regulation of inflammatory pathways and responded to anti–tumor necrosis factor therapy, while those who developed a stricturing phenotype had increased expression of extracellular matrix pathways and were significantly less likely to respond to anti-TNF therapy ( Lancet. 2017 Apr 29;389[10080]:1710-8 ). These studies provide a proof of concept that we might someday be able to use for personalized approaches to treating IBD.
Using new drugs, targeting new pathways
The recently published CALM study tested the hypothesis that treating to a target of no biochemical inflammation (elevated C reactive protein or fecal calprotectin) would be better than symptom-driven treatment alone. Treatment escalation for active disease included adalimumab every other week, then weekly adalimumab, and finally the addition of azathioprine. At the end of the study, patients whose medical therapy was based on both symptoms and biochemical inflammation had a higher degree of mucosal healing than did patients in the clinical management group (Lancet. 2018 Dec 23;390[10114]:2779-89).
Ustekinumab is a monoclonal antibody that targets the p40 subunit of interleukin-12 and interleukin-23 and is approved for Crohn’s disease. Various pharmaceutical companies are now developing anti-p19 antibodies, which block IL-23 only; at DDW 2018, the anti–IL-23 mirikizumab was shown to be effective in UC. We are also seeing the availability of oral medications for IBD. Just prior to DDW, tofacitinib ( N Engl J Med. 2017 May 4;376:1723-36 ), a Janus kinase (JAK) 1/3 inhibitor, which has an effect on multiple different cytokine pathways, received approval for UC. Other JAK inhibitors with different specificities are being tested in trials of UC and Crohn’s disease.
Dr. Abreu is a professor of medicine, a professor of microbiology and immunology, and the director of the Crohn’s & Colitis Center at the University of Miami Miller School of Medicine. She has no conflicts of interest. Dr. Abreu made her comments during the AGA Institute Presidential Plenary at the Annual Digestive Disease Week.
Here is an update on the rapidly moving field of inflammatory bowel disease (IBD), from the power of the microbiome to the prediction of IBD and new ways to use established drugs.
Regarding the microbiome, we now understand that, while the healthy microbiome is diverse and able to produce short-chain fatty acids, such as butyrate, the dysbiotic IBD microbiome is less diverse and characterized by expansion of proinflammatory pathobionts (such as Fusobacterium), the proliferation of sulfate-reducing bacteria, and a decrease in anti-inflammatory butyrate production.
There have now been several promising trials of fecal microbial transplant (FMT) for the treatment of ulcerative colitis (UC). The most effective strategies have involved colonic delivery of FMT, pooled donors, and repeated stool enemas to solidify the response. Following FMT, patients’ microbial diversity increases. The hope is that we can use diet as a complement to maintain the diversity and generation of beneficial metabolites, as well as deliver the therapy orally.
Predicting IBD
Although we have made advances in therapy, we continue to miss opportunities to prevent long-term complications. At Digestive Disease Week,® Jean-Frederic Colombel, MD, a professor of medicine at the Icahn School of Medicine at Mount Sinai, New York, presented data on the PREDICTS study (Aliment Pharacol Ther. 2016 Jun;43[12]:1300-10), in which serum samples collected from military recruits prior to development of IBD was used to identify serologic markers that could predict those who ultimately developed Crohn’s disease but not UC.
The pediatric medical community, meanwhile, has studied an inception cohort of newly diagnosed, untreated children – the RISK cohort ( Lancet. 2017 Apr 29;389[10080]:1710-8 ) – to define some of the risk factors that predict more aggressive disease. By using biopsy tissue from the time of diagnosis, investigators could predict who would develop stricturing disease versus penetrating disease. Patients who would develop penetrating disease had up-regulation of inflammatory pathways and responded to anti–tumor necrosis factor therapy, while those who developed a stricturing phenotype had increased expression of extracellular matrix pathways and were significantly less likely to respond to anti-TNF therapy ( Lancet. 2017 Apr 29;389[10080]:1710-8 ). These studies provide a proof of concept that we might someday be able to use for personalized approaches to treating IBD.
Using new drugs, targeting new pathways
The recently published CALM study tested the hypothesis that treating to a target of no biochemical inflammation (elevated C reactive protein or fecal calprotectin) would be better than symptom-driven treatment alone. Treatment escalation for active disease included adalimumab every other week, then weekly adalimumab, and finally the addition of azathioprine. At the end of the study, patients whose medical therapy was based on both symptoms and biochemical inflammation had a higher degree of mucosal healing than did patients in the clinical management group (Lancet. 2018 Dec 23;390[10114]:2779-89).
Ustekinumab is a monoclonal antibody that targets the p40 subunit of interleukin-12 and interleukin-23 and is approved for Crohn’s disease. Various pharmaceutical companies are now developing anti-p19 antibodies, which block IL-23 only; at DDW 2018, the anti–IL-23 mirikizumab was shown to be effective in UC. We are also seeing the availability of oral medications for IBD. Just prior to DDW, tofacitinib ( N Engl J Med. 2017 May 4;376:1723-36 ), a Janus kinase (JAK) 1/3 inhibitor, which has an effect on multiple different cytokine pathways, received approval for UC. Other JAK inhibitors with different specificities are being tested in trials of UC and Crohn’s disease.
Dr. Abreu is a professor of medicine, a professor of microbiology and immunology, and the director of the Crohn’s & Colitis Center at the University of Miami Miller School of Medicine. She has no conflicts of interest. Dr. Abreu made her comments during the AGA Institute Presidential Plenary at the Annual Digestive Disease Week.
Simplified formula validated for MRI Crohn’s disease assessment
WASHINGTON – The same Spanish research team who introduced an MRI-based formula for scoring the activity of luminal Crohn’s disease in 2011 have developed and validated a new, simplified version of their MRI score that speeds assessment.
“The simplified version of the MaRIA [Magnetic Resonance Index of Activity] score allows a faster and easier assessment of inflammation and quantification of severity in Crohn’s disease by keeping high accuracy for diagnosis and therapeutic response,” Ingrid Ordás, MD, said at the annual Digestive Disease Week®. The main advantage of the simplified MaRIA is that it is a “less time-consuming calculation that is not confounded by missing segments,” said Dr. Ordás, a gastroenterologist at the Hospital Clinic of Barcelona.
Although the data reported by Dr. Ordás included the derivation results, which used 98 patients enrolled in two separate prospective studies, and a separate prospective validation cohort of 37 patients, all these patients were evaluated by clinicians at the Hospital Clinic of Barcelona, and hence further validation with patients enrolled at other sites is now needed, Dr. Ordás said in an interview. Further accumulation of evidence for high sensitivity and specificity of Crohn’s disease assessment using the simplified MaRIA could allow it to replace endoscopy as the standard tool for assessing disease activity and severity in patients with luminal Crohn’s disease.
The derivation phase of the study identified four features that significantly correlated with disease activity and severity: bowel wall thickening to more than 3 mm, mural edema, perienteric fat stranding, and mucosal ulcerations. Limiting assessment to these four features cut in half the elements in the original MaRIA (Inflamm Bowel Dis. 2011 Aug;17[8];1759-68). Fat stranding – loss of the usual sharp interface between the wall and mesentery because of fluid – is a new parameter in the simplified MaRIA. The other three elements had been in the original index, but several other elements are now gone, including relative contrast enhancement wall signal intensity and consideration of lymph nodes.
In the validation phase, the researchers compared the MaRIA findings of the validation cohort with endoscopy findings both at baseline and then after they had received treatment. The sensitivity and specificity of the simplified MaRIA depended on the cutoff used, but as an example, a patient with a simplified MaRIA of 1 or greater as having active disease had a sensitivity of 90%, specificity of 81%, and an area under the receiver operator characteristic curve of 0.91. Using a simplified MaRIA of at least 2 as indicative of severe disease had a sensitivity of 85%, a specificity of 92%, and an AUROC of 0.94, Dr. Ordás reported.
Further assessment in patients who underwent treatment showed that reductions in the simplified MaRIA significantly correlated with treatment responses and remained essentially unchanged in patients who did not have clinical response to treatment. The analysis also showed a strong, positive correlation coefficient of 0.83 when the simplified MaRIA of an individual patient, compared with the patient’s Crohn’s disease endoscopy index of severity, and a correlation coefficient of 0.94 when a patient’s simplified MaRIA determined by one clinician, compared with the index score calculated by a second clinician.
Dr. Ordás had no disclosures to report.
SOURCE: Ordás I et al. DDW 2018, Presentation 437.
WASHINGTON – The same Spanish research team who introduced an MRI-based formula for scoring the activity of luminal Crohn’s disease in 2011 have developed and validated a new, simplified version of their MRI score that speeds assessment.
“The simplified version of the MaRIA [Magnetic Resonance Index of Activity] score allows a faster and easier assessment of inflammation and quantification of severity in Crohn’s disease by keeping high accuracy for diagnosis and therapeutic response,” Ingrid Ordás, MD, said at the annual Digestive Disease Week®. The main advantage of the simplified MaRIA is that it is a “less time-consuming calculation that is not confounded by missing segments,” said Dr. Ordás, a gastroenterologist at the Hospital Clinic of Barcelona.
Although the data reported by Dr. Ordás included the derivation results, which used 98 patients enrolled in two separate prospective studies, and a separate prospective validation cohort of 37 patients, all these patients were evaluated by clinicians at the Hospital Clinic of Barcelona, and hence further validation with patients enrolled at other sites is now needed, Dr. Ordás said in an interview. Further accumulation of evidence for high sensitivity and specificity of Crohn’s disease assessment using the simplified MaRIA could allow it to replace endoscopy as the standard tool for assessing disease activity and severity in patients with luminal Crohn’s disease.
The derivation phase of the study identified four features that significantly correlated with disease activity and severity: bowel wall thickening to more than 3 mm, mural edema, perienteric fat stranding, and mucosal ulcerations. Limiting assessment to these four features cut in half the elements in the original MaRIA (Inflamm Bowel Dis. 2011 Aug;17[8];1759-68). Fat stranding – loss of the usual sharp interface between the wall and mesentery because of fluid – is a new parameter in the simplified MaRIA. The other three elements had been in the original index, but several other elements are now gone, including relative contrast enhancement wall signal intensity and consideration of lymph nodes.
In the validation phase, the researchers compared the MaRIA findings of the validation cohort with endoscopy findings both at baseline and then after they had received treatment. The sensitivity and specificity of the simplified MaRIA depended on the cutoff used, but as an example, a patient with a simplified MaRIA of 1 or greater as having active disease had a sensitivity of 90%, specificity of 81%, and an area under the receiver operator characteristic curve of 0.91. Using a simplified MaRIA of at least 2 as indicative of severe disease had a sensitivity of 85%, a specificity of 92%, and an AUROC of 0.94, Dr. Ordás reported.
Further assessment in patients who underwent treatment showed that reductions in the simplified MaRIA significantly correlated with treatment responses and remained essentially unchanged in patients who did not have clinical response to treatment. The analysis also showed a strong, positive correlation coefficient of 0.83 when the simplified MaRIA of an individual patient, compared with the patient’s Crohn’s disease endoscopy index of severity, and a correlation coefficient of 0.94 when a patient’s simplified MaRIA determined by one clinician, compared with the index score calculated by a second clinician.
Dr. Ordás had no disclosures to report.
SOURCE: Ordás I et al. DDW 2018, Presentation 437.
WASHINGTON – The same Spanish research team who introduced an MRI-based formula for scoring the activity of luminal Crohn’s disease in 2011 have developed and validated a new, simplified version of their MRI score that speeds assessment.
“The simplified version of the MaRIA [Magnetic Resonance Index of Activity] score allows a faster and easier assessment of inflammation and quantification of severity in Crohn’s disease by keeping high accuracy for diagnosis and therapeutic response,” Ingrid Ordás, MD, said at the annual Digestive Disease Week®. The main advantage of the simplified MaRIA is that it is a “less time-consuming calculation that is not confounded by missing segments,” said Dr. Ordás, a gastroenterologist at the Hospital Clinic of Barcelona.
Although the data reported by Dr. Ordás included the derivation results, which used 98 patients enrolled in two separate prospective studies, and a separate prospective validation cohort of 37 patients, all these patients were evaluated by clinicians at the Hospital Clinic of Barcelona, and hence further validation with patients enrolled at other sites is now needed, Dr. Ordás said in an interview. Further accumulation of evidence for high sensitivity and specificity of Crohn’s disease assessment using the simplified MaRIA could allow it to replace endoscopy as the standard tool for assessing disease activity and severity in patients with luminal Crohn’s disease.
The derivation phase of the study identified four features that significantly correlated with disease activity and severity: bowel wall thickening to more than 3 mm, mural edema, perienteric fat stranding, and mucosal ulcerations. Limiting assessment to these four features cut in half the elements in the original MaRIA (Inflamm Bowel Dis. 2011 Aug;17[8];1759-68). Fat stranding – loss of the usual sharp interface between the wall and mesentery because of fluid – is a new parameter in the simplified MaRIA. The other three elements had been in the original index, but several other elements are now gone, including relative contrast enhancement wall signal intensity and consideration of lymph nodes.
In the validation phase, the researchers compared the MaRIA findings of the validation cohort with endoscopy findings both at baseline and then after they had received treatment. The sensitivity and specificity of the simplified MaRIA depended on the cutoff used, but as an example, a patient with a simplified MaRIA of 1 or greater as having active disease had a sensitivity of 90%, specificity of 81%, and an area under the receiver operator characteristic curve of 0.91. Using a simplified MaRIA of at least 2 as indicative of severe disease had a sensitivity of 85%, a specificity of 92%, and an AUROC of 0.94, Dr. Ordás reported.
Further assessment in patients who underwent treatment showed that reductions in the simplified MaRIA significantly correlated with treatment responses and remained essentially unchanged in patients who did not have clinical response to treatment. The analysis also showed a strong, positive correlation coefficient of 0.83 when the simplified MaRIA of an individual patient, compared with the patient’s Crohn’s disease endoscopy index of severity, and a correlation coefficient of 0.94 when a patient’s simplified MaRIA determined by one clinician, compared with the index score calculated by a second clinician.
Dr. Ordás had no disclosures to report.
SOURCE: Ordás I et al. DDW 2018, Presentation 437.
REPORTING FROM DDW 2018
Key clinical point: Researchers devised a simplified way to use MRI to noninvasively assess Crohn’s disease activity.
Major finding: The simplified, MRI-based formula identified Crohn’s disease activity with 90% sensitivity and 81% specificity.
Study details: The validation study included 37 patients with luminal Crohn’s disease at a single center in Barcelona.
Disclosures: Dr. Ordás had no disclosures to report.
Source: Ordás I et al. DDW 2018, Presentation 437.
Prolonged opioid use among U.S. IBD patients doubled during 2002-2016
WASHINGTON – based on statistics gathered in a database that included medical records from more than 40 million American patients.
Prolonged opioid treatment, defined as filling at least two prescriptions for an opioid at least 90 days apart in a calendar year, rose among patients diagnosed with either Crohn’s disease or ulcerative colitis from a low of 14% in 2002 to 26% in 2016, reaching a peak during the period of 29% in 2014, Marc Landsman, MD, said at the annual Digestive Disease Week.®
The sharpest rise during the 15-year period examined was an increase in this level of opioid use from 15% in 2004 to 21% in 2005. Prolonged opioid use remained at or above 26% of all U.S. patients identified with IBD in the database during each year from 2011 to 2016, said Dr. Landsman, a gastroenterologist at the MetroHealth Medical Center in Cleveland. He suggested that a multidisciplinary approach to pain relief including alternative approaches to pain management, “will be vital” for pain management in IBD patients.
“Pain is a very important symptom of IBD. Opioids have been easy to prescribe, but they may not be the correct drug to prescribe,” commented Gil Y. Melmed, MD, director of clinical inflammatory bowel disease at Cedars-Sinai Medical Center in Los Angeles. He agreed with Dr. Landsman that a more multidisciplinary approach to pain management, including behavioral interventions, might reduce reliance on opioids in these patients. In addition, good control of an IBD patient’s inflammatory disease with, for example, a tumor necrosis factor inhibitor often produces substantial pain reduction, although some patients may also need surgery to relieve obstructive pain, Dr. Melmed said in an interview.The analysis run by Dr. Landsman and his associates used data in the Explorys database that included 276,340 unique patients with a diagnosis in their insurance record of IBD who also underwent either flexible sigmoidoscopy or colonoscopy during the year when they first received the diagnosis.
The study also analyzed the type of medical insurance used by patients who received prolonged opioid treatment. During 2002, 43% of patients who received an opioid for a prolonged period had Medicare coverage, 35% had private insurance, and 20% had Medicaid coverage. The prevalence of Medicare and private insurance coverage among opioid recipients steadily shifted during the next 14 years, so that in 2016 private insurance was the most prevalent coverage among the IBD patients on prolonged opioid use, at 46%, with 33% on Medicare coverage and 15% covered by Medicaid. The changes in the prevalence of Medicare and private insurance coverage from 2002 to 2016 were statistically significant, Dr. Landsman said.
Dr. Landsman and Dr. Melmed had no relevant disclosures.
SOURCE: Landsman M et al. DDW 2018. Presentation 14.
WASHINGTON – based on statistics gathered in a database that included medical records from more than 40 million American patients.
Prolonged opioid treatment, defined as filling at least two prescriptions for an opioid at least 90 days apart in a calendar year, rose among patients diagnosed with either Crohn’s disease or ulcerative colitis from a low of 14% in 2002 to 26% in 2016, reaching a peak during the period of 29% in 2014, Marc Landsman, MD, said at the annual Digestive Disease Week.®
The sharpest rise during the 15-year period examined was an increase in this level of opioid use from 15% in 2004 to 21% in 2005. Prolonged opioid use remained at or above 26% of all U.S. patients identified with IBD in the database during each year from 2011 to 2016, said Dr. Landsman, a gastroenterologist at the MetroHealth Medical Center in Cleveland. He suggested that a multidisciplinary approach to pain relief including alternative approaches to pain management, “will be vital” for pain management in IBD patients.
“Pain is a very important symptom of IBD. Opioids have been easy to prescribe, but they may not be the correct drug to prescribe,” commented Gil Y. Melmed, MD, director of clinical inflammatory bowel disease at Cedars-Sinai Medical Center in Los Angeles. He agreed with Dr. Landsman that a more multidisciplinary approach to pain management, including behavioral interventions, might reduce reliance on opioids in these patients. In addition, good control of an IBD patient’s inflammatory disease with, for example, a tumor necrosis factor inhibitor often produces substantial pain reduction, although some patients may also need surgery to relieve obstructive pain, Dr. Melmed said in an interview.The analysis run by Dr. Landsman and his associates used data in the Explorys database that included 276,340 unique patients with a diagnosis in their insurance record of IBD who also underwent either flexible sigmoidoscopy or colonoscopy during the year when they first received the diagnosis.
The study also analyzed the type of medical insurance used by patients who received prolonged opioid treatment. During 2002, 43% of patients who received an opioid for a prolonged period had Medicare coverage, 35% had private insurance, and 20% had Medicaid coverage. The prevalence of Medicare and private insurance coverage among opioid recipients steadily shifted during the next 14 years, so that in 2016 private insurance was the most prevalent coverage among the IBD patients on prolonged opioid use, at 46%, with 33% on Medicare coverage and 15% covered by Medicaid. The changes in the prevalence of Medicare and private insurance coverage from 2002 to 2016 were statistically significant, Dr. Landsman said.
Dr. Landsman and Dr. Melmed had no relevant disclosures.
SOURCE: Landsman M et al. DDW 2018. Presentation 14.
WASHINGTON – based on statistics gathered in a database that included medical records from more than 40 million American patients.
Prolonged opioid treatment, defined as filling at least two prescriptions for an opioid at least 90 days apart in a calendar year, rose among patients diagnosed with either Crohn’s disease or ulcerative colitis from a low of 14% in 2002 to 26% in 2016, reaching a peak during the period of 29% in 2014, Marc Landsman, MD, said at the annual Digestive Disease Week.®
The sharpest rise during the 15-year period examined was an increase in this level of opioid use from 15% in 2004 to 21% in 2005. Prolonged opioid use remained at or above 26% of all U.S. patients identified with IBD in the database during each year from 2011 to 2016, said Dr. Landsman, a gastroenterologist at the MetroHealth Medical Center in Cleveland. He suggested that a multidisciplinary approach to pain relief including alternative approaches to pain management, “will be vital” for pain management in IBD patients.
“Pain is a very important symptom of IBD. Opioids have been easy to prescribe, but they may not be the correct drug to prescribe,” commented Gil Y. Melmed, MD, director of clinical inflammatory bowel disease at Cedars-Sinai Medical Center in Los Angeles. He agreed with Dr. Landsman that a more multidisciplinary approach to pain management, including behavioral interventions, might reduce reliance on opioids in these patients. In addition, good control of an IBD patient’s inflammatory disease with, for example, a tumor necrosis factor inhibitor often produces substantial pain reduction, although some patients may also need surgery to relieve obstructive pain, Dr. Melmed said in an interview.The analysis run by Dr. Landsman and his associates used data in the Explorys database that included 276,340 unique patients with a diagnosis in their insurance record of IBD who also underwent either flexible sigmoidoscopy or colonoscopy during the year when they first received the diagnosis.
The study also analyzed the type of medical insurance used by patients who received prolonged opioid treatment. During 2002, 43% of patients who received an opioid for a prolonged period had Medicare coverage, 35% had private insurance, and 20% had Medicaid coverage. The prevalence of Medicare and private insurance coverage among opioid recipients steadily shifted during the next 14 years, so that in 2016 private insurance was the most prevalent coverage among the IBD patients on prolonged opioid use, at 46%, with 33% on Medicare coverage and 15% covered by Medicaid. The changes in the prevalence of Medicare and private insurance coverage from 2002 to 2016 were statistically significant, Dr. Landsman said.
Dr. Landsman and Dr. Melmed had no relevant disclosures.
SOURCE: Landsman M et al. DDW 2018. Presentation 14.
REPORTING FROM DDW 2018
Key clinical point: Prolonged opioid use by IBD patients increased substantially during 2002-2016.
Major finding: The incidence of prolonged opioid use among U.S. IBD patients rose from 14% in 2002 to 26% in 2016.
Study details: Review of 276,340 U.S. patients diagnosed with IBD contained in a large insurance database.
Disclosures: Dr. Landsman and Dr. Melmed had no relevant disclosures.
Source: Landsman M et al. DDW 2018. Presentation 14.
Fecal transplantation suggests IBS efficacy in small, randomized studies
WASHINGTON –
In the more positive of the two studies, patients with “bloating-predominant” IBS received a freshly prepared FMT from either a selected donor or from their own stool as a placebo control. After 12 weeks, the percentage of patients reporting clinically meaningful improvements in both abdominal bloating and in IBS symptoms was roughly twice as high, about 56%, among the 43 actively treated patients as the 26% rate of patients reporting these changes among 19 controls, Tom Holvoet, MD, said at the annual Digestive Disease Week.®Further follow-up of 22 patients who had significant improvement of their IBS symptoms at 12 weeks after treatment showed that, 1 year later, 6 of the 22 (27%) maintained their improved state while the other 73% of patients relapsed, suggesting that retreatment may be necessary for many, said Dr. Holvoet, a gastroenterologist at Ghent (Belgium) University. Five of the six patients who showed a prolonged response had received a donor FMT, while the sixth patient was from the control group that received a transplant of material prepared from the patient’s own stool.
“I think some patients would be willing to have multiple treatments,” Dr. Holvoet said in an interview. “These are highly motivated patients; you need to be highly motivated to undergo this treatment, and if they see an effect they’ll be motivated for retreatment,” he predicted.
The single-center study enrolled patients 18-75 years old with refractory IBS, based on the Rome III criteria, with intermittent diarrhea and severe bloating. Each patient received a single FMT. Patients in the active-treatment arm received their FMT from either of two donors selected for their “rich microbial diversity,” and demonstrated efficacy in an earlier pilot study with 12 patients (Gut. 2017 May;66[5]:980-2). In addition to a higher rate of improvement of abdominal bloating and IBS symptoms, the donor FMT also led to a significantly better improvement in IBS-related quality of life. Preliminary analysis of the intestinal microbiome profile of patients in the study suggested that specific changes to the microbiome were linked with treatment success.
Dr. Holvoet highlighted that more research is needed to identify ideal patients to treat this way, and to simplify and streamline the FMT process.
“Our study is a good first step, but we need to figure out what is happening in these patients,” Dr. Holvoet said in an interview.
Results from the second study failed to show a statistically significant benefit from FMT, compared with placebo, for the primary endpoint, but it did show benefit in one secondary endpoint.
This study enrolled 48 patients 19-65 years old with moderate to severe, diarrhea-predominant IBS, based on the Rome III definitions, at any of three U.S. centers. The researchers randomized patients to either immediate treatment for 3 days with an encapsulated, frozen fecal preparation obtained from the OpenBiome stool bank or placebo capsules. After 12 weeks, the average change from baseline in the IBS–Symptom Severity Score (SSS), the study’s primary endpoint, was virtually identical in both arms of the study. In both treatment groups the average baseline IBS-SSS was nearly 300, and in both treatment groups the SSS dropped sharply after 1 week into the study and then remained stable at this lower level in both groups during the next 11 weeks. Patients then underwent a second round of treatment in a crossover design. During a second 12 weeks of follow-up the average IBS-SSS remained steady among the patients who received placebo as their second treatment, but the patients who received active treatment as their second dose showed a further significant decline in their SSS, so that after the second 12-week follow-up the average score was 76 points lower in patients who recently had active treatment than those who recently received placebo, a statistically significant difference for this clinically meaningful point difference, reported Lawrence J. Brandt, MD, professor of medicine and surgery at Albert Einstein College of Medicine in New York.
In addition, the 12 patients in the study who had postinfection IBS showed the most dramatic reduction from baseline in their IBS-SSS 12 weeks after active treatment, compared with placebo. In contrast, 33 other patients in the study with noninfectious IBS etiologies showed on average no difference between active and placebo treatment in their 12-week change in SSS.
Preliminary findings in this study also showed some correlations between certain microbiome changes and better clinical responses to FMT, Dr. Brandt noted.
Dr. Holvoet and Dr. Brandt had no disclosures.
SOURCE: Holvoet T et al. DDW 2018. Presentation 617; Aroniadis OC et al. Presentation 742.
WASHINGTON –
In the more positive of the two studies, patients with “bloating-predominant” IBS received a freshly prepared FMT from either a selected donor or from their own stool as a placebo control. After 12 weeks, the percentage of patients reporting clinically meaningful improvements in both abdominal bloating and in IBS symptoms was roughly twice as high, about 56%, among the 43 actively treated patients as the 26% rate of patients reporting these changes among 19 controls, Tom Holvoet, MD, said at the annual Digestive Disease Week.®Further follow-up of 22 patients who had significant improvement of their IBS symptoms at 12 weeks after treatment showed that, 1 year later, 6 of the 22 (27%) maintained their improved state while the other 73% of patients relapsed, suggesting that retreatment may be necessary for many, said Dr. Holvoet, a gastroenterologist at Ghent (Belgium) University. Five of the six patients who showed a prolonged response had received a donor FMT, while the sixth patient was from the control group that received a transplant of material prepared from the patient’s own stool.
“I think some patients would be willing to have multiple treatments,” Dr. Holvoet said in an interview. “These are highly motivated patients; you need to be highly motivated to undergo this treatment, and if they see an effect they’ll be motivated for retreatment,” he predicted.
The single-center study enrolled patients 18-75 years old with refractory IBS, based on the Rome III criteria, with intermittent diarrhea and severe bloating. Each patient received a single FMT. Patients in the active-treatment arm received their FMT from either of two donors selected for their “rich microbial diversity,” and demonstrated efficacy in an earlier pilot study with 12 patients (Gut. 2017 May;66[5]:980-2). In addition to a higher rate of improvement of abdominal bloating and IBS symptoms, the donor FMT also led to a significantly better improvement in IBS-related quality of life. Preliminary analysis of the intestinal microbiome profile of patients in the study suggested that specific changes to the microbiome were linked with treatment success.
Dr. Holvoet highlighted that more research is needed to identify ideal patients to treat this way, and to simplify and streamline the FMT process.
“Our study is a good first step, but we need to figure out what is happening in these patients,” Dr. Holvoet said in an interview.
Results from the second study failed to show a statistically significant benefit from FMT, compared with placebo, for the primary endpoint, but it did show benefit in one secondary endpoint.
This study enrolled 48 patients 19-65 years old with moderate to severe, diarrhea-predominant IBS, based on the Rome III definitions, at any of three U.S. centers. The researchers randomized patients to either immediate treatment for 3 days with an encapsulated, frozen fecal preparation obtained from the OpenBiome stool bank or placebo capsules. After 12 weeks, the average change from baseline in the IBS–Symptom Severity Score (SSS), the study’s primary endpoint, was virtually identical in both arms of the study. In both treatment groups the average baseline IBS-SSS was nearly 300, and in both treatment groups the SSS dropped sharply after 1 week into the study and then remained stable at this lower level in both groups during the next 11 weeks. Patients then underwent a second round of treatment in a crossover design. During a second 12 weeks of follow-up the average IBS-SSS remained steady among the patients who received placebo as their second treatment, but the patients who received active treatment as their second dose showed a further significant decline in their SSS, so that after the second 12-week follow-up the average score was 76 points lower in patients who recently had active treatment than those who recently received placebo, a statistically significant difference for this clinically meaningful point difference, reported Lawrence J. Brandt, MD, professor of medicine and surgery at Albert Einstein College of Medicine in New York.
In addition, the 12 patients in the study who had postinfection IBS showed the most dramatic reduction from baseline in their IBS-SSS 12 weeks after active treatment, compared with placebo. In contrast, 33 other patients in the study with noninfectious IBS etiologies showed on average no difference between active and placebo treatment in their 12-week change in SSS.
Preliminary findings in this study also showed some correlations between certain microbiome changes and better clinical responses to FMT, Dr. Brandt noted.
Dr. Holvoet and Dr. Brandt had no disclosures.
SOURCE: Holvoet T et al. DDW 2018. Presentation 617; Aroniadis OC et al. Presentation 742.
WASHINGTON –
In the more positive of the two studies, patients with “bloating-predominant” IBS received a freshly prepared FMT from either a selected donor or from their own stool as a placebo control. After 12 weeks, the percentage of patients reporting clinically meaningful improvements in both abdominal bloating and in IBS symptoms was roughly twice as high, about 56%, among the 43 actively treated patients as the 26% rate of patients reporting these changes among 19 controls, Tom Holvoet, MD, said at the annual Digestive Disease Week.®Further follow-up of 22 patients who had significant improvement of their IBS symptoms at 12 weeks after treatment showed that, 1 year later, 6 of the 22 (27%) maintained their improved state while the other 73% of patients relapsed, suggesting that retreatment may be necessary for many, said Dr. Holvoet, a gastroenterologist at Ghent (Belgium) University. Five of the six patients who showed a prolonged response had received a donor FMT, while the sixth patient was from the control group that received a transplant of material prepared from the patient’s own stool.
“I think some patients would be willing to have multiple treatments,” Dr. Holvoet said in an interview. “These are highly motivated patients; you need to be highly motivated to undergo this treatment, and if they see an effect they’ll be motivated for retreatment,” he predicted.
The single-center study enrolled patients 18-75 years old with refractory IBS, based on the Rome III criteria, with intermittent diarrhea and severe bloating. Each patient received a single FMT. Patients in the active-treatment arm received their FMT from either of two donors selected for their “rich microbial diversity,” and demonstrated efficacy in an earlier pilot study with 12 patients (Gut. 2017 May;66[5]:980-2). In addition to a higher rate of improvement of abdominal bloating and IBS symptoms, the donor FMT also led to a significantly better improvement in IBS-related quality of life. Preliminary analysis of the intestinal microbiome profile of patients in the study suggested that specific changes to the microbiome were linked with treatment success.
Dr. Holvoet highlighted that more research is needed to identify ideal patients to treat this way, and to simplify and streamline the FMT process.
“Our study is a good first step, but we need to figure out what is happening in these patients,” Dr. Holvoet said in an interview.
Results from the second study failed to show a statistically significant benefit from FMT, compared with placebo, for the primary endpoint, but it did show benefit in one secondary endpoint.
This study enrolled 48 patients 19-65 years old with moderate to severe, diarrhea-predominant IBS, based on the Rome III definitions, at any of three U.S. centers. The researchers randomized patients to either immediate treatment for 3 days with an encapsulated, frozen fecal preparation obtained from the OpenBiome stool bank or placebo capsules. After 12 weeks, the average change from baseline in the IBS–Symptom Severity Score (SSS), the study’s primary endpoint, was virtually identical in both arms of the study. In both treatment groups the average baseline IBS-SSS was nearly 300, and in both treatment groups the SSS dropped sharply after 1 week into the study and then remained stable at this lower level in both groups during the next 11 weeks. Patients then underwent a second round of treatment in a crossover design. During a second 12 weeks of follow-up the average IBS-SSS remained steady among the patients who received placebo as their second treatment, but the patients who received active treatment as their second dose showed a further significant decline in their SSS, so that after the second 12-week follow-up the average score was 76 points lower in patients who recently had active treatment than those who recently received placebo, a statistically significant difference for this clinically meaningful point difference, reported Lawrence J. Brandt, MD, professor of medicine and surgery at Albert Einstein College of Medicine in New York.
In addition, the 12 patients in the study who had postinfection IBS showed the most dramatic reduction from baseline in their IBS-SSS 12 weeks after active treatment, compared with placebo. In contrast, 33 other patients in the study with noninfectious IBS etiologies showed on average no difference between active and placebo treatment in their 12-week change in SSS.
Preliminary findings in this study also showed some correlations between certain microbiome changes and better clinical responses to FMT, Dr. Brandt noted.
Dr. Holvoet and Dr. Brandt had no disclosures.
SOURCE: Holvoet T et al. DDW 2018. Presentation 617; Aroniadis OC et al. Presentation 742.
REPORTING FROM DDW 2018
Key clinical point: Results from two small randomized studies suggest that fecal microbiome transplantation may help some IBS patients.
Major finding: In one study, fecal transplantation linked with a doubling of patients having reduced IBS symptoms, compared with placebo, .
Study details: A single-center randomized study with 62 patients and a multicenter randomized crossover study with 48 patients.
Disclosures: Dr. Holvoet and Dr. Brandt had no disclosures.
Source: Holvoet T et al. DDW 2018. Presentation 617; Aroniadis OC et al. Presentation 742.
Home-based CBT significantly improved IBS symptoms
Primarily home-based cognitive-behavioral therapy improved irritable bowel syndrome symptoms at least as much as conventional CBT, cut clinician time by 60%, and significantly outperformed educational sessions in a multicenter clinical trial reported in the July issue of Gastroenterology.
Acutely, primarily home-based CBT produced a mean 61% improvement in self-reported symptoms on the IBS version of the Clinical Global Impressions Scale, versus 44% for the educational control group (P less than .05), wrote Jeffrey M. Lackner, PsyD, of the State University of New York at Buffalo and his associates. Blinded gastroenterologists reported improvements of 56% and 40%, respectively (P less than .05). The superiority of the minimal-contact CBT program held up at 6 months and equivalence tests found it “at least as effective as standard CBT,” the researchers wrote.
IBS is a major area of unmet clinical need that costs the United States some $28 billion annually. Clinicians and patients lack both reliable biomarkers and “uniformly effective” therapies, the investigators noted. In recent years, severe adverse events have greatly restricted the availability of otherwise promising Food and Drug Administration–approved therapies, such as Lotronex (alosetron hydrochlorine), which has been linked to ischemic colitis and fatal cases of ruptured bowel, and Zelnorm (tegaserod maleate), which has been associated with myocardial infarction, stroke, and unstable angina.
In contrast, face-to-face CBT is safe, efficacious, and guideline recommended for IBS. However, uptake is limited by cost, stigma, geography, and a shortage of certified providers, the researchers noted. They enrolled 436 patients with IBS based on Rome III criteria and randomly assigned them to one of three interventions. The standard CBT group received 10 weekly, 60-minute, face-to-face CBT sessions on brain-gut interactions, symptom triggers and monitoring, muscle relaxation, worry control, problem-solving, and relapse prevention. The primarily home-based CBT group covered the same topics but attended only four clinic sessions and was provided home study materials. Finally, the education group attended four sessions with background information on IBS and the role of stress, diet, and exercise.
Baseline characteristics were comparable among groups, as were dropout rates (9% overall). In all, 89% of patients completed at least 8 of 10 standard cognitive-behavioral therapy sessions or at least three of four home-based CBT or educational sessions. Six months after the interventions ended, primarily home-based CBT continued to outperform education (blinded gastroenterologist-reported improvements, 58.4% and 44.8%, respectively; P = .05 for difference between groups).
Equivalence tests indicated that the minimal-CBT intervention was at least as effective as standard CBT, and improvements were not primarily the result of concomitant medications, according to the researchers. Nonetheless, only 42% of patients who benefited from CBT achieved remission, defined as no or mild IBS symptoms on the gastroenterologist-administered Clinical Global Impressions Scale. Unremitted patients might benefit from combining CBT with medical therapies that target both “central and peripheral mechanisms of IBS,” the investigators said.
The three interventions produced comparable acute and longer-term improvements on the IBS Symptom Severity Scale, which emphasizes sensory symptoms and therefore might be a less sensitive endpoint than the Clinical Global Impressions Scale, the researchers noted. Nonetheless, CBT produced some of the strongest absolute symptomatic improvements ever reported for IBS. “To put these data in context, treatment response of FDA-approved pharmacological agents using global IBS symptom improvement scales range from 17% to 40%,” the researchers wrote.
The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
SOURCE: Lackner JM et al. Gastroenterology. 2018 Apr 24. doi: 10.1053/j.gastro.2018.03.063.
Treating the myriad symptoms of irritable bowel syndrome (IBS) patients remains a great challenge in clinical practice. A bigger challenge is the management of IBS patients who are refractory to medical therapy, which commonly includes a combination of pain, bowel, and psychiatric medications. In this very well designed and executed study, Lackner and his colleagues randomized refractory IBS patients with moderate to severe symptoms to three therapeutic arms: standard cognitive-behavioral therapy (CBT), minimal-contact home-based CBT, and IBS education. The authors demonstrated that 4-session home-based CBT was as efficacious as 10 sessions of standard CBT and both were significantly more efficacious than IBS education in global improvement of IBS symptoms. The superior effect of both types of CBT was maintained over a period of 6 months post treatment.
There are several important conclusions from this pivotal trial. First, the study further cemented the therapeutic value of CBT in the management of IBS patients, especially for those patients who are refractory to the currently available medical therapy. Because of the size of the study and the rigorous design, it is probably the best evidence we currently have about the value of CBT in IBS. Second, minimal-contact home-based CBT is as effective as standard CBT in controlling the full range of IBS symptoms. The former may be preferred by IBS patients, who are not available or may not be compliant with repeated clinic visits for standard CBT sessions. Standard CBT is typically lengthy and expensive. The minimal-contact home-based CBT option has the benefit of being more accessible and less costly, and most importantly, it does so in a way that does not compromise the therapeutic value of symptom relief.
The exact duration of symptom control that can be achieved post CBT and the value of other psychological interventions in IBS patients remain to be elucidated.
Ronnie Fass, MD, is a professor of medicine at Case Western Reserve University, Cleveland, as well as the medical director of the Digestive Health Center and director of the division of gastroenterology and hepatology, head, esophageal and swallowing center at MetroHealth Medical Center, also in Cleveland. He has no conflicts of interest.
Treating the myriad symptoms of irritable bowel syndrome (IBS) patients remains a great challenge in clinical practice. A bigger challenge is the management of IBS patients who are refractory to medical therapy, which commonly includes a combination of pain, bowel, and psychiatric medications. In this very well designed and executed study, Lackner and his colleagues randomized refractory IBS patients with moderate to severe symptoms to three therapeutic arms: standard cognitive-behavioral therapy (CBT), minimal-contact home-based CBT, and IBS education. The authors demonstrated that 4-session home-based CBT was as efficacious as 10 sessions of standard CBT and both were significantly more efficacious than IBS education in global improvement of IBS symptoms. The superior effect of both types of CBT was maintained over a period of 6 months post treatment.
There are several important conclusions from this pivotal trial. First, the study further cemented the therapeutic value of CBT in the management of IBS patients, especially for those patients who are refractory to the currently available medical therapy. Because of the size of the study and the rigorous design, it is probably the best evidence we currently have about the value of CBT in IBS. Second, minimal-contact home-based CBT is as effective as standard CBT in controlling the full range of IBS symptoms. The former may be preferred by IBS patients, who are not available or may not be compliant with repeated clinic visits for standard CBT sessions. Standard CBT is typically lengthy and expensive. The minimal-contact home-based CBT option has the benefit of being more accessible and less costly, and most importantly, it does so in a way that does not compromise the therapeutic value of symptom relief.
The exact duration of symptom control that can be achieved post CBT and the value of other psychological interventions in IBS patients remain to be elucidated.
Ronnie Fass, MD, is a professor of medicine at Case Western Reserve University, Cleveland, as well as the medical director of the Digestive Health Center and director of the division of gastroenterology and hepatology, head, esophageal and swallowing center at MetroHealth Medical Center, also in Cleveland. He has no conflicts of interest.
Treating the myriad symptoms of irritable bowel syndrome (IBS) patients remains a great challenge in clinical practice. A bigger challenge is the management of IBS patients who are refractory to medical therapy, which commonly includes a combination of pain, bowel, and psychiatric medications. In this very well designed and executed study, Lackner and his colleagues randomized refractory IBS patients with moderate to severe symptoms to three therapeutic arms: standard cognitive-behavioral therapy (CBT), minimal-contact home-based CBT, and IBS education. The authors demonstrated that 4-session home-based CBT was as efficacious as 10 sessions of standard CBT and both were significantly more efficacious than IBS education in global improvement of IBS symptoms. The superior effect of both types of CBT was maintained over a period of 6 months post treatment.
There are several important conclusions from this pivotal trial. First, the study further cemented the therapeutic value of CBT in the management of IBS patients, especially for those patients who are refractory to the currently available medical therapy. Because of the size of the study and the rigorous design, it is probably the best evidence we currently have about the value of CBT in IBS. Second, minimal-contact home-based CBT is as effective as standard CBT in controlling the full range of IBS symptoms. The former may be preferred by IBS patients, who are not available or may not be compliant with repeated clinic visits for standard CBT sessions. Standard CBT is typically lengthy and expensive. The minimal-contact home-based CBT option has the benefit of being more accessible and less costly, and most importantly, it does so in a way that does not compromise the therapeutic value of symptom relief.
The exact duration of symptom control that can be achieved post CBT and the value of other psychological interventions in IBS patients remain to be elucidated.
Ronnie Fass, MD, is a professor of medicine at Case Western Reserve University, Cleveland, as well as the medical director of the Digestive Health Center and director of the division of gastroenterology and hepatology, head, esophageal and swallowing center at MetroHealth Medical Center, also in Cleveland. He has no conflicts of interest.
Primarily home-based cognitive-behavioral therapy improved irritable bowel syndrome symptoms at least as much as conventional CBT, cut clinician time by 60%, and significantly outperformed educational sessions in a multicenter clinical trial reported in the July issue of Gastroenterology.
Acutely, primarily home-based CBT produced a mean 61% improvement in self-reported symptoms on the IBS version of the Clinical Global Impressions Scale, versus 44% for the educational control group (P less than .05), wrote Jeffrey M. Lackner, PsyD, of the State University of New York at Buffalo and his associates. Blinded gastroenterologists reported improvements of 56% and 40%, respectively (P less than .05). The superiority of the minimal-contact CBT program held up at 6 months and equivalence tests found it “at least as effective as standard CBT,” the researchers wrote.
IBS is a major area of unmet clinical need that costs the United States some $28 billion annually. Clinicians and patients lack both reliable biomarkers and “uniformly effective” therapies, the investigators noted. In recent years, severe adverse events have greatly restricted the availability of otherwise promising Food and Drug Administration–approved therapies, such as Lotronex (alosetron hydrochlorine), which has been linked to ischemic colitis and fatal cases of ruptured bowel, and Zelnorm (tegaserod maleate), which has been associated with myocardial infarction, stroke, and unstable angina.
In contrast, face-to-face CBT is safe, efficacious, and guideline recommended for IBS. However, uptake is limited by cost, stigma, geography, and a shortage of certified providers, the researchers noted. They enrolled 436 patients with IBS based on Rome III criteria and randomly assigned them to one of three interventions. The standard CBT group received 10 weekly, 60-minute, face-to-face CBT sessions on brain-gut interactions, symptom triggers and monitoring, muscle relaxation, worry control, problem-solving, and relapse prevention. The primarily home-based CBT group covered the same topics but attended only four clinic sessions and was provided home study materials. Finally, the education group attended four sessions with background information on IBS and the role of stress, diet, and exercise.
Baseline characteristics were comparable among groups, as were dropout rates (9% overall). In all, 89% of patients completed at least 8 of 10 standard cognitive-behavioral therapy sessions or at least three of four home-based CBT or educational sessions. Six months after the interventions ended, primarily home-based CBT continued to outperform education (blinded gastroenterologist-reported improvements, 58.4% and 44.8%, respectively; P = .05 for difference between groups).
Equivalence tests indicated that the minimal-CBT intervention was at least as effective as standard CBT, and improvements were not primarily the result of concomitant medications, according to the researchers. Nonetheless, only 42% of patients who benefited from CBT achieved remission, defined as no or mild IBS symptoms on the gastroenterologist-administered Clinical Global Impressions Scale. Unremitted patients might benefit from combining CBT with medical therapies that target both “central and peripheral mechanisms of IBS,” the investigators said.
The three interventions produced comparable acute and longer-term improvements on the IBS Symptom Severity Scale, which emphasizes sensory symptoms and therefore might be a less sensitive endpoint than the Clinical Global Impressions Scale, the researchers noted. Nonetheless, CBT produced some of the strongest absolute symptomatic improvements ever reported for IBS. “To put these data in context, treatment response of FDA-approved pharmacological agents using global IBS symptom improvement scales range from 17% to 40%,” the researchers wrote.
The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
SOURCE: Lackner JM et al. Gastroenterology. 2018 Apr 24. doi: 10.1053/j.gastro.2018.03.063.
Primarily home-based cognitive-behavioral therapy improved irritable bowel syndrome symptoms at least as much as conventional CBT, cut clinician time by 60%, and significantly outperformed educational sessions in a multicenter clinical trial reported in the July issue of Gastroenterology.
Acutely, primarily home-based CBT produced a mean 61% improvement in self-reported symptoms on the IBS version of the Clinical Global Impressions Scale, versus 44% for the educational control group (P less than .05), wrote Jeffrey M. Lackner, PsyD, of the State University of New York at Buffalo and his associates. Blinded gastroenterologists reported improvements of 56% and 40%, respectively (P less than .05). The superiority of the minimal-contact CBT program held up at 6 months and equivalence tests found it “at least as effective as standard CBT,” the researchers wrote.
IBS is a major area of unmet clinical need that costs the United States some $28 billion annually. Clinicians and patients lack both reliable biomarkers and “uniformly effective” therapies, the investigators noted. In recent years, severe adverse events have greatly restricted the availability of otherwise promising Food and Drug Administration–approved therapies, such as Lotronex (alosetron hydrochlorine), which has been linked to ischemic colitis and fatal cases of ruptured bowel, and Zelnorm (tegaserod maleate), which has been associated with myocardial infarction, stroke, and unstable angina.
In contrast, face-to-face CBT is safe, efficacious, and guideline recommended for IBS. However, uptake is limited by cost, stigma, geography, and a shortage of certified providers, the researchers noted. They enrolled 436 patients with IBS based on Rome III criteria and randomly assigned them to one of three interventions. The standard CBT group received 10 weekly, 60-minute, face-to-face CBT sessions on brain-gut interactions, symptom triggers and monitoring, muscle relaxation, worry control, problem-solving, and relapse prevention. The primarily home-based CBT group covered the same topics but attended only four clinic sessions and was provided home study materials. Finally, the education group attended four sessions with background information on IBS and the role of stress, diet, and exercise.
Baseline characteristics were comparable among groups, as were dropout rates (9% overall). In all, 89% of patients completed at least 8 of 10 standard cognitive-behavioral therapy sessions or at least three of four home-based CBT or educational sessions. Six months after the interventions ended, primarily home-based CBT continued to outperform education (blinded gastroenterologist-reported improvements, 58.4% and 44.8%, respectively; P = .05 for difference between groups).
Equivalence tests indicated that the minimal-CBT intervention was at least as effective as standard CBT, and improvements were not primarily the result of concomitant medications, according to the researchers. Nonetheless, only 42% of patients who benefited from CBT achieved remission, defined as no or mild IBS symptoms on the gastroenterologist-administered Clinical Global Impressions Scale. Unremitted patients might benefit from combining CBT with medical therapies that target both “central and peripheral mechanisms of IBS,” the investigators said.
The three interventions produced comparable acute and longer-term improvements on the IBS Symptom Severity Scale, which emphasizes sensory symptoms and therefore might be a less sensitive endpoint than the Clinical Global Impressions Scale, the researchers noted. Nonetheless, CBT produced some of the strongest absolute symptomatic improvements ever reported for IBS. “To put these data in context, treatment response of FDA-approved pharmacological agents using global IBS symptom improvement scales range from 17% to 40%,” the researchers wrote.
The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
SOURCE: Lackner JM et al. Gastroenterology. 2018 Apr 24. doi: 10.1053/j.gastro.2018.03.063.
FROM GASTROENTEROLOGY
Key clinical point: Primarily home-based CBT significantly reduced self-reported and gastroenterologist-assessed symptoms of IBS.
Major finding: The intervention required 60% less clinician time and was at least as effective as 10 sessions of conventional CBT, according to responses to the Clinical Global Impressions Improvement Scale. CBT also significantly outperformed the education control (P less than .05).
Study details: Two-center, single-blinded randomized trial of 436 patients with IBS per Rome III criteria.
Disclosures: The National Institutes of Health provided funding. The researchers reported having no conflicts of interest.
Source: Lackner JM et al. Gastroenterology. 2018 Apr 24. doi: 10.1053/j.gastro.2018.03.063.