User login
Hospital Medicine Leaders Flock to HM13 for Answers, Encouragement
Ibe Mbanu, MD, MBA, MPH, became medical director of the adult hospitalist department at Bon Secours St. Mary’s Hospital in Richmond, Va., about six months ago. Since then, he’s been besieged by a torrent of reform-based challenges he says make his job exponentially more difficult than that of medical directors just a few years ago.
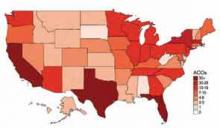
Accountable-care organizations (ACOs), value-based purchasing, and discussions about bundled payments for episodic care are changing rapidly, and as a new administrator in a group with 24 hospitalists and three nonphysician providers (NPPs), he felt he needed to attend his first SHM annual meeting to keep up.
“The landscape in health care is rapidly evolving, at a frantic pace,” Dr. Mbanu says. “I essentially came here to just try to get a condensed source of information on how to manage the changes that are coming through the pipeline, and how to effectively run my department.”
Managing a practice is a challenge, and many of the more than 2,700 attendees at HM13 said the four-day confab’s focus on the topic was a major draw. From a rebooted continuing medical education (CME) pre-course appropriately named “What Keeps You Awake at Night? Hot Topics in Hospitalist Practice Management” to dozens of breakout sessions on the topic, it’s clear that successful practice management is a concern for many hospitalists.
“Before, the drivers were pretty clear,” Dr. Mbanu says. “Volume, productivity. Now we’re switching more toward a business model that’s changing from volume to value. Trying to adapt to that change is pretty challenging.
“Now it’s critical to really understand the environment.”
Comanagement Conundrum
One particularly hot topic this year was the trend of hospitalists taking on more comanagement responsibilities for patients previously managed by other specialties, including neurology, surgery, and others. Frank Volpicelli, MD, a first-year hospitalist and instructor at New York University (NYU) Langone Medical Center in New York, was one of three members of his HM group that attended the “Perioperative Medicine: Medical Consultation and Co-Management” pre-course. This summer, his group is going to establish a presence in the preoperative clinic.
“We hope very strongly that we can prevent some complications, identify patients that we should be following when they come into the hospital, and help the surgeons out,” he says. “No. 1, keep them in the [operating room] more, and No. 2, get in front of some of the complications that they are less comfortable managing.”
Ralph Velazquez, MD, senior vice president of care management for OSF Healthcare System in Peoria, Ill., isn’t so sure comanagement of more and more patients is the best practice-management model moving forward. For example, as physician compensation is tied more to how much their care costs to deliver, a hospitalist comanaging a surgical patient’s elective knee replacement could be financially penalized for the cost of that person’s stay, despite having nothing to do with the most expensive portion of the bill.
“You have a financial model that says do more billings, but as you start developing analytics … you may see there is no difference between the model that’s doing more billing, in terms of improving quality, and the one that is doing less,” Dr. Velazquez says. “So if you’re getting the same amount of quality, and the only thing you’re doing is generating more cost by doing more billing, you need to reevaluate your strategy.”
He believes some patients benefit from comanagement, but HM groups have to be diligent in seeking them out.
“We look for simple solutions and one-size-fits-all,” he adds. “Comanagement in complex patients—definitely there’s a need for that. Comanagement in noncomplex patients, elective patients—there’s no need for that. It’s just additional cost. I don’t think it’s going to produce any value.”
Startup Academy
John Colombo, MD, FACP, a 30-year veteran of internal medicine who moved to HM a few years ago when one of the hospitals he worked at asked him to launch a hospitalist group, thinks bundled payments might alleviate that value conundrum. Then again, he’s not quite sure. That’s why attended his first annual meeting.
“I found it difficult starting a new program from scratch,” says Dr. Colombo, of Crozer Keystone Health System in Drexel Hill, Pa. “Even with the materials available, there’s not a lot of ‘how to do it’ out there. There’s no ‘Starting Hospitals for Dummies’ book.”
Dr. Colombo spent much of his meeting focused on recruiting, compensation, bonus structures, and scheduling concerns. He said all are important in the hospital-heavy metropolitan Philadelphia region where he works. Plus, with departures and retirements at other programs in his health system, Dr. Colombo went from no HM experience three years ago to being in charge of four HM programs.
“The biggest thing is, I wanted to make sure I hadn’t stepped in something that I shouldn’t have already,” he adds. “There’s many different ways to do things. So I’ve learned a few different ways. I found value.”
Demonstrate Value
Another way to discover value in running a practice is looking at the business side of the house, says Denice Cora-Bramble, MD, MBA, chief medical officer and executive vice president of Ambulatory & Community Health Services at the Children’s National Medical Center in Washington, D.C.
Dr. Bramble says many hospitalists need to understand that while clinical care is what brought them to medicine, their future paychecks depend on recognizing how to provide that care in a way that demonstrates business value.
“When you finish residency, if you have not intentionally sought out those courses or those seminars, you need to recognize that as a blind spot,” she says. “You need to fill that toolkit as it relates to the business side of medicine.
“You don’t necessarily have to know all the answers, but you need to know the right questions to ask,” she says.
Dr. Bramble adds that hospitalist leaders should take advantage of certificate programs, leadership courses, basic budgeting classes, or anything that gives them added education about the economics of healthcare.
“It all comes down to demonstrating your outcomes, demonstrating the value that you bring to that institution,” she says. “And with health-care reform, I think hospitalists are uniquely positioned to be able to partner with other areas of the hospital to look at this value-based approach.”
Gary Gammon, MD, FHM, the newly named medical director of the Hospitalist Service at FirstHealth Moore Regional Hospital in Pinehurst, N.C., is doing his part to demonstrate value to his administrators. While his group does multidisciplinary rounds on patients, one of his questions for the pre-course faculty was to make sure that system of rounding is an evidence-based practice. He’s also looking for ways to establish more hegemony to his practice to ensure the rounds are effective, regardless of which physicians and others are participating.
The feedback he received was that most people view multidisciplinary rounds as a best practice. Now, Dr. Gammon can feel more authoritative that he and his 32 hospitalists and 12 extenders are practicing HM the way it should be practiced.
“I wanted to hear just what I heard, which is the leaders in the community feel that it’s helping, feel that it’s the right thing to do, feel that there’s objective data,” he says. “This is the stuff that makes me say, ‘OK, I’ve got the same problems everybody else has.’”
Richard Quinn is a freelance writer in New Jersey.
Ibe Mbanu, MD, MBA, MPH, became medical director of the adult hospitalist department at Bon Secours St. Mary’s Hospital in Richmond, Va., about six months ago. Since then, he’s been besieged by a torrent of reform-based challenges he says make his job exponentially more difficult than that of medical directors just a few years ago.
Accountable-care organizations (ACOs), value-based purchasing, and discussions about bundled payments for episodic care are changing rapidly, and as a new administrator in a group with 24 hospitalists and three nonphysician providers (NPPs), he felt he needed to attend his first SHM annual meeting to keep up.
“The landscape in health care is rapidly evolving, at a frantic pace,” Dr. Mbanu says. “I essentially came here to just try to get a condensed source of information on how to manage the changes that are coming through the pipeline, and how to effectively run my department.”
Managing a practice is a challenge, and many of the more than 2,700 attendees at HM13 said the four-day confab’s focus on the topic was a major draw. From a rebooted continuing medical education (CME) pre-course appropriately named “What Keeps You Awake at Night? Hot Topics in Hospitalist Practice Management” to dozens of breakout sessions on the topic, it’s clear that successful practice management is a concern for many hospitalists.
“Before, the drivers were pretty clear,” Dr. Mbanu says. “Volume, productivity. Now we’re switching more toward a business model that’s changing from volume to value. Trying to adapt to that change is pretty challenging.
“Now it’s critical to really understand the environment.”
Comanagement Conundrum
One particularly hot topic this year was the trend of hospitalists taking on more comanagement responsibilities for patients previously managed by other specialties, including neurology, surgery, and others. Frank Volpicelli, MD, a first-year hospitalist and instructor at New York University (NYU) Langone Medical Center in New York, was one of three members of his HM group that attended the “Perioperative Medicine: Medical Consultation and Co-Management” pre-course. This summer, his group is going to establish a presence in the preoperative clinic.
“We hope very strongly that we can prevent some complications, identify patients that we should be following when they come into the hospital, and help the surgeons out,” he says. “No. 1, keep them in the [operating room] more, and No. 2, get in front of some of the complications that they are less comfortable managing.”
Ralph Velazquez, MD, senior vice president of care management for OSF Healthcare System in Peoria, Ill., isn’t so sure comanagement of more and more patients is the best practice-management model moving forward. For example, as physician compensation is tied more to how much their care costs to deliver, a hospitalist comanaging a surgical patient’s elective knee replacement could be financially penalized for the cost of that person’s stay, despite having nothing to do with the most expensive portion of the bill.
“You have a financial model that says do more billings, but as you start developing analytics … you may see there is no difference between the model that’s doing more billing, in terms of improving quality, and the one that is doing less,” Dr. Velazquez says. “So if you’re getting the same amount of quality, and the only thing you’re doing is generating more cost by doing more billing, you need to reevaluate your strategy.”
He believes some patients benefit from comanagement, but HM groups have to be diligent in seeking them out.
“We look for simple solutions and one-size-fits-all,” he adds. “Comanagement in complex patients—definitely there’s a need for that. Comanagement in noncomplex patients, elective patients—there’s no need for that. It’s just additional cost. I don’t think it’s going to produce any value.”
Startup Academy
John Colombo, MD, FACP, a 30-year veteran of internal medicine who moved to HM a few years ago when one of the hospitals he worked at asked him to launch a hospitalist group, thinks bundled payments might alleviate that value conundrum. Then again, he’s not quite sure. That’s why attended his first annual meeting.
“I found it difficult starting a new program from scratch,” says Dr. Colombo, of Crozer Keystone Health System in Drexel Hill, Pa. “Even with the materials available, there’s not a lot of ‘how to do it’ out there. There’s no ‘Starting Hospitals for Dummies’ book.”
Dr. Colombo spent much of his meeting focused on recruiting, compensation, bonus structures, and scheduling concerns. He said all are important in the hospital-heavy metropolitan Philadelphia region where he works. Plus, with departures and retirements at other programs in his health system, Dr. Colombo went from no HM experience three years ago to being in charge of four HM programs.
“The biggest thing is, I wanted to make sure I hadn’t stepped in something that I shouldn’t have already,” he adds. “There’s many different ways to do things. So I’ve learned a few different ways. I found value.”
Demonstrate Value
Another way to discover value in running a practice is looking at the business side of the house, says Denice Cora-Bramble, MD, MBA, chief medical officer and executive vice president of Ambulatory & Community Health Services at the Children’s National Medical Center in Washington, D.C.
Dr. Bramble says many hospitalists need to understand that while clinical care is what brought them to medicine, their future paychecks depend on recognizing how to provide that care in a way that demonstrates business value.
“When you finish residency, if you have not intentionally sought out those courses or those seminars, you need to recognize that as a blind spot,” she says. “You need to fill that toolkit as it relates to the business side of medicine.
“You don’t necessarily have to know all the answers, but you need to know the right questions to ask,” she says.
Dr. Bramble adds that hospitalist leaders should take advantage of certificate programs, leadership courses, basic budgeting classes, or anything that gives them added education about the economics of healthcare.
“It all comes down to demonstrating your outcomes, demonstrating the value that you bring to that institution,” she says. “And with health-care reform, I think hospitalists are uniquely positioned to be able to partner with other areas of the hospital to look at this value-based approach.”
Gary Gammon, MD, FHM, the newly named medical director of the Hospitalist Service at FirstHealth Moore Regional Hospital in Pinehurst, N.C., is doing his part to demonstrate value to his administrators. While his group does multidisciplinary rounds on patients, one of his questions for the pre-course faculty was to make sure that system of rounding is an evidence-based practice. He’s also looking for ways to establish more hegemony to his practice to ensure the rounds are effective, regardless of which physicians and others are participating.
The feedback he received was that most people view multidisciplinary rounds as a best practice. Now, Dr. Gammon can feel more authoritative that he and his 32 hospitalists and 12 extenders are practicing HM the way it should be practiced.
“I wanted to hear just what I heard, which is the leaders in the community feel that it’s helping, feel that it’s the right thing to do, feel that there’s objective data,” he says. “This is the stuff that makes me say, ‘OK, I’ve got the same problems everybody else has.’”
Richard Quinn is a freelance writer in New Jersey.
Ibe Mbanu, MD, MBA, MPH, became medical director of the adult hospitalist department at Bon Secours St. Mary’s Hospital in Richmond, Va., about six months ago. Since then, he’s been besieged by a torrent of reform-based challenges he says make his job exponentially more difficult than that of medical directors just a few years ago.
Accountable-care organizations (ACOs), value-based purchasing, and discussions about bundled payments for episodic care are changing rapidly, and as a new administrator in a group with 24 hospitalists and three nonphysician providers (NPPs), he felt he needed to attend his first SHM annual meeting to keep up.
“The landscape in health care is rapidly evolving, at a frantic pace,” Dr. Mbanu says. “I essentially came here to just try to get a condensed source of information on how to manage the changes that are coming through the pipeline, and how to effectively run my department.”
Managing a practice is a challenge, and many of the more than 2,700 attendees at HM13 said the four-day confab’s focus on the topic was a major draw. From a rebooted continuing medical education (CME) pre-course appropriately named “What Keeps You Awake at Night? Hot Topics in Hospitalist Practice Management” to dozens of breakout sessions on the topic, it’s clear that successful practice management is a concern for many hospitalists.
“Before, the drivers were pretty clear,” Dr. Mbanu says. “Volume, productivity. Now we’re switching more toward a business model that’s changing from volume to value. Trying to adapt to that change is pretty challenging.
“Now it’s critical to really understand the environment.”
Comanagement Conundrum
One particularly hot topic this year was the trend of hospitalists taking on more comanagement responsibilities for patients previously managed by other specialties, including neurology, surgery, and others. Frank Volpicelli, MD, a first-year hospitalist and instructor at New York University (NYU) Langone Medical Center in New York, was one of three members of his HM group that attended the “Perioperative Medicine: Medical Consultation and Co-Management” pre-course. This summer, his group is going to establish a presence in the preoperative clinic.
“We hope very strongly that we can prevent some complications, identify patients that we should be following when they come into the hospital, and help the surgeons out,” he says. “No. 1, keep them in the [operating room] more, and No. 2, get in front of some of the complications that they are less comfortable managing.”
Ralph Velazquez, MD, senior vice president of care management for OSF Healthcare System in Peoria, Ill., isn’t so sure comanagement of more and more patients is the best practice-management model moving forward. For example, as physician compensation is tied more to how much their care costs to deliver, a hospitalist comanaging a surgical patient’s elective knee replacement could be financially penalized for the cost of that person’s stay, despite having nothing to do with the most expensive portion of the bill.
“You have a financial model that says do more billings, but as you start developing analytics … you may see there is no difference between the model that’s doing more billing, in terms of improving quality, and the one that is doing less,” Dr. Velazquez says. “So if you’re getting the same amount of quality, and the only thing you’re doing is generating more cost by doing more billing, you need to reevaluate your strategy.”
He believes some patients benefit from comanagement, but HM groups have to be diligent in seeking them out.
“We look for simple solutions and one-size-fits-all,” he adds. “Comanagement in complex patients—definitely there’s a need for that. Comanagement in noncomplex patients, elective patients—there’s no need for that. It’s just additional cost. I don’t think it’s going to produce any value.”
Startup Academy
John Colombo, MD, FACP, a 30-year veteran of internal medicine who moved to HM a few years ago when one of the hospitals he worked at asked him to launch a hospitalist group, thinks bundled payments might alleviate that value conundrum. Then again, he’s not quite sure. That’s why attended his first annual meeting.
“I found it difficult starting a new program from scratch,” says Dr. Colombo, of Crozer Keystone Health System in Drexel Hill, Pa. “Even with the materials available, there’s not a lot of ‘how to do it’ out there. There’s no ‘Starting Hospitals for Dummies’ book.”
Dr. Colombo spent much of his meeting focused on recruiting, compensation, bonus structures, and scheduling concerns. He said all are important in the hospital-heavy metropolitan Philadelphia region where he works. Plus, with departures and retirements at other programs in his health system, Dr. Colombo went from no HM experience three years ago to being in charge of four HM programs.
“The biggest thing is, I wanted to make sure I hadn’t stepped in something that I shouldn’t have already,” he adds. “There’s many different ways to do things. So I’ve learned a few different ways. I found value.”
Demonstrate Value
Another way to discover value in running a practice is looking at the business side of the house, says Denice Cora-Bramble, MD, MBA, chief medical officer and executive vice president of Ambulatory & Community Health Services at the Children’s National Medical Center in Washington, D.C.
Dr. Bramble says many hospitalists need to understand that while clinical care is what brought them to medicine, their future paychecks depend on recognizing how to provide that care in a way that demonstrates business value.
“When you finish residency, if you have not intentionally sought out those courses or those seminars, you need to recognize that as a blind spot,” she says. “You need to fill that toolkit as it relates to the business side of medicine.
“You don’t necessarily have to know all the answers, but you need to know the right questions to ask,” she says.
Dr. Bramble adds that hospitalist leaders should take advantage of certificate programs, leadership courses, basic budgeting classes, or anything that gives them added education about the economics of healthcare.
“It all comes down to demonstrating your outcomes, demonstrating the value that you bring to that institution,” she says. “And with health-care reform, I think hospitalists are uniquely positioned to be able to partner with other areas of the hospital to look at this value-based approach.”
Gary Gammon, MD, FHM, the newly named medical director of the Hospitalist Service at FirstHealth Moore Regional Hospital in Pinehurst, N.C., is doing his part to demonstrate value to his administrators. While his group does multidisciplinary rounds on patients, one of his questions for the pre-course faculty was to make sure that system of rounding is an evidence-based practice. He’s also looking for ways to establish more hegemony to his practice to ensure the rounds are effective, regardless of which physicians and others are participating.
The feedback he received was that most people view multidisciplinary rounds as a best practice. Now, Dr. Gammon can feel more authoritative that he and his 32 hospitalists and 12 extenders are practicing HM the way it should be practiced.
“I wanted to hear just what I heard, which is the leaders in the community feel that it’s helping, feel that it’s the right thing to do, feel that there’s objective data,” he says. “This is the stuff that makes me say, ‘OK, I’ve got the same problems everybody else has.’”
Richard Quinn is a freelance writer in New Jersey.
Health-Care Journalists Tackle Barriers to Hospital Safety Records
The Association of Health Care Journalists, a professional association that includes 1,400 journalists, is tackling some of the barriers consumers and advocates face when trying to access such information as hospital safety records. AHCJ’s www.HospitalInfections.org is a free, searchable news application that went live in March with detailed reports of deficiencies cited in federal inspection visits for acute- and critical-access hospitals nationwide.
Through years of advocacy, AHCJ has filed Freedom of Information Act requests and negotiated with the Centers for Medicare & Medicaid Services (CMS) to get access to hospital safety information in electronic form.
CMS’ Hospital Compare website (www.medicare.gov/hospitalcompare) and the Joint Commission’s Quality Check (www.qualitycheck.org) program both publicly report hospital quality data, but they have significant time lags and data that are difficult for the average consumer to understand, according to AHCJ. The association touts its new site as an “early attempt by an advocacy group to make hospital safety information easier to access and more consumer-driven.”
“Being able to easily review the performance of your local hospital is vital for health-care journalists and for the public,” AHCJ president Charles Ornstein, a senior reporter at ProPublica in New York, said in a statement.
Larry Beresford is a freelance writer in San Francisco
References
- Weigel C, Suen W, Gupta G. Using Lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013 Feb 4 [Epub ahead of print].
- Morganti KG, Lovejoy S, Beckjord EB, Haviland AM, Haas AC, Farley DO. A retrospective evaluation of the Perfecting Patient Care University training program for health care organizations. Am J Med Qual. 2013 Apr 9 [Epub ahead of print].
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators’ Academy: fulfilling an unmet need for faculty development. Am J Med Qual. 2013 Apr 11 [Epub ahead of print].
- Dong XQ, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 Apr 8:1-7. doi: 10.1001/jamainternmed.2013.238 [Epub ahead of print].
- Cisco mConcierge. 90% American workers use their own smartphones for work. Cisco mConcierge website. Available at: http://www.ciscomcon.com/sw/swchannel/registration/internet/registrationcfm?SWAPPID=91&RegPageID=350200&SWTHEMEID=12949. Accessed
The Association of Health Care Journalists, a professional association that includes 1,400 journalists, is tackling some of the barriers consumers and advocates face when trying to access such information as hospital safety records. AHCJ’s www.HospitalInfections.org is a free, searchable news application that went live in March with detailed reports of deficiencies cited in federal inspection visits for acute- and critical-access hospitals nationwide.
Through years of advocacy, AHCJ has filed Freedom of Information Act requests and negotiated with the Centers for Medicare & Medicaid Services (CMS) to get access to hospital safety information in electronic form.
CMS’ Hospital Compare website (www.medicare.gov/hospitalcompare) and the Joint Commission’s Quality Check (www.qualitycheck.org) program both publicly report hospital quality data, but they have significant time lags and data that are difficult for the average consumer to understand, according to AHCJ. The association touts its new site as an “early attempt by an advocacy group to make hospital safety information easier to access and more consumer-driven.”
“Being able to easily review the performance of your local hospital is vital for health-care journalists and for the public,” AHCJ president Charles Ornstein, a senior reporter at ProPublica in New York, said in a statement.
Larry Beresford is a freelance writer in San Francisco
References
- Weigel C, Suen W, Gupta G. Using Lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013 Feb 4 [Epub ahead of print].
- Morganti KG, Lovejoy S, Beckjord EB, Haviland AM, Haas AC, Farley DO. A retrospective evaluation of the Perfecting Patient Care University training program for health care organizations. Am J Med Qual. 2013 Apr 9 [Epub ahead of print].
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators’ Academy: fulfilling an unmet need for faculty development. Am J Med Qual. 2013 Apr 11 [Epub ahead of print].
- Dong XQ, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 Apr 8:1-7. doi: 10.1001/jamainternmed.2013.238 [Epub ahead of print].
- Cisco mConcierge. 90% American workers use their own smartphones for work. Cisco mConcierge website. Available at: http://www.ciscomcon.com/sw/swchannel/registration/internet/registrationcfm?SWAPPID=91&RegPageID=350200&SWTHEMEID=12949. Accessed
The Association of Health Care Journalists, a professional association that includes 1,400 journalists, is tackling some of the barriers consumers and advocates face when trying to access such information as hospital safety records. AHCJ’s www.HospitalInfections.org is a free, searchable news application that went live in March with detailed reports of deficiencies cited in federal inspection visits for acute- and critical-access hospitals nationwide.
Through years of advocacy, AHCJ has filed Freedom of Information Act requests and negotiated with the Centers for Medicare & Medicaid Services (CMS) to get access to hospital safety information in electronic form.
CMS’ Hospital Compare website (www.medicare.gov/hospitalcompare) and the Joint Commission’s Quality Check (www.qualitycheck.org) program both publicly report hospital quality data, but they have significant time lags and data that are difficult for the average consumer to understand, according to AHCJ. The association touts its new site as an “early attempt by an advocacy group to make hospital safety information easier to access and more consumer-driven.”
“Being able to easily review the performance of your local hospital is vital for health-care journalists and for the public,” AHCJ president Charles Ornstein, a senior reporter at ProPublica in New York, said in a statement.
Larry Beresford is a freelance writer in San Francisco
References
- Weigel C, Suen W, Gupta G. Using Lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013 Feb 4 [Epub ahead of print].
- Morganti KG, Lovejoy S, Beckjord EB, Haviland AM, Haas AC, Farley DO. A retrospective evaluation of the Perfecting Patient Care University training program for health care organizations. Am J Med Qual. 2013 Apr 9 [Epub ahead of print].
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators’ Academy: fulfilling an unmet need for faculty development. Am J Med Qual. 2013 Apr 11 [Epub ahead of print].
- Dong XQ, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 Apr 8:1-7. doi: 10.1001/jamainternmed.2013.238 [Epub ahead of print].
- Cisco mConcierge. 90% American workers use their own smartphones for work. Cisco mConcierge website. Available at: http://www.ciscomcon.com/sw/swchannel/registration/internet/registrationcfm?SWAPPID=91&RegPageID=350200&SWTHEMEID=12949. Accessed
‘Hill Trip’ Connects Legislators to Hospitalists, Health Care Issues
A veritable perfect storm of relationships brought hospitalist Jairy Hunter, MD, MBA, SFHM, to “Hospitalists on the Hill 2013,” a daylong advocacy affair that preceded HM13 last month.
First, Dr. Hunter was born and bred—and now lives—in South Carolina, a close-knit state where leaders across industries tend to run in the same circles, or at least have relatives who do. Second, Dr. Hunter’s father, Jairy Hunter Jr., is the longtime president of Charleston Southern University, where Sen. Tim Scott (R-S.C.) earned his undergraduate degree when it was still called Baptist College at Charleston. And three, Dr. Hunter is associate executive medical director of one of the state’s flagship health-care institutions, Medical University of South Carolina in Charleston.
So it was that SHM set Dr. Hunter up in meetings with the offices of Scott, Sen. Lindsey Graham (R-S.C.), and Rep. Jim Clyburn (D-S.C.), and—for the day at least—made Dr. Hunter the voice of hospital medicine.
“It was a little bit demystifying of an experience to be able to know there’s actually people you can talk to and you can develop a relationship with,” says Dr. Hunter, who also serves on Team Hospitalist. “I thought that was very rewarding.”
The connections made by Dr. Hunter are the point of the annual trek made by SHM leaders and members to lobby legislators and federal staffers “on the way policies affect your practice and your patients,” SHM says on its website (www.hospitalmedicine.org/advocacy). This year’s volunteer effort was by far the largest ever, says Public Policy Committee chair Ron Greeno, MD, FCCP, MHM. More than 150 hospitalists participated in training, 113 hospitalists visited Capitol Hill, and scores more had to be turned away. All told, hospitalists held 409 individual meetings with legislators and staff members.
“Quite frankly, if we’d have had the budget, we could have had another 100 to 150 people come,” Dr. Greeno says. “That’s how many people wanted to go.”
Dr. Greeno attributes the interest to two factors. One, having the annual meeting at the Gaylord National Resort & Convention Center, just outside Washington, D.C, makes the Hill trip a natural extension. Two, the current landscape of health-care reform has motivated many physicians to become more involved than they might otherwise be. One challenge of having so many first-timers making this year’s trip was making sure they were properly prepared. To hone the message, SHM gave the group a few hours of education by former legislative staffer Stephanie Vance of Advocacy Associates, a communications firm that helps organizations, such as medical societies, tailor their message to policymakers. Vance told hospitalists a personal visit with a constituent often becomes the most influential type of advocacy.
“That’s why it was easy to make an initial connection, because these staffers are from where I’m from, friends with people that I’m friends with,” Dr. Hunter says.
Unique Approach
SHM CEO Larry Wellikson, MD, SFHM, says the society tries to differentiate itself from other organizations through its grassroots approach to advocacy. More important, the society refrains from giving a long list of legislative requests that are self-serving.
“We’re someone they want to talk to because we’re not coming there to just say, ‘Here’s a power play for hospitalists,’” Dr. Wellikson says. “We come and try to provide solutions.”
To that end, this year’s lobbying effort was targeted to topics important both to HM and the health-care system:
- Repealing the sustainable growth rate (SGR) formula for Medicare payments, specifically via the proposed Medicare Physician Payment Innovation Act of 2013 (H.R. 574);
- Solving the quagmire of observation status time not counting toward the required three consecutive overnights as an inpatient needed to qualify for Medicare benefits at a skilled nursing facility, by supporting the Improving Access to Medicare Coverage Act of 2013 (H.R. 1179, S. 569); and
- Getting the federal government to commit to providing $434 million in funding for the Agency for Healthcare Research and Quality (AHRQ) in fiscal 2014.
“The message that we’re sending resonated with the people we met with on both sides of the aisle,” Dr. Greeno says. “The SGR, for instance, they know there needs to be a fix. We want to serve as a resource for them as they start to figure out the answer to the question: What are we going to replace it with?
“What we want to do is make everybody on the Hill understand that we can be relied upon as a resource when they’re looking for solutions,” he says.
Focused on Follow-Up
And that’s where rank-and-filers, such as Dr. Hunter, have to take charge. So for his Hill Day visits, he tried to stand out. Everyone he met with got a lapel pin in the shape of a South Carolina state flag, which has become a popular fashion statement in recent years. And Scott also got a pin from Charleston Southern University, his alma mater. The gestures were small, but they served as icebreakers and reminders that Dr. Hunter and the people he met are bound by service to the residents of the Palmetto State.
Dr. Hunter also hopes the small token will be that little extra that makes him memorable enough that the next time a Congressional staffer has an SGR question, they’ll ask him and not a doctor from another specialty.
“I’m interested to see how much feedback I get back from them,” he says. “I can feed them all day long, but I don’t want to be that crazy guy bugging them. If they respond back to me, I can hopefully make more inroads.”
He certainly would if Dr. Greeno gets his way. Moving forward, SHM hopes to be able to rely more on local advocates pushing for reform than just a once-a-year major event and formal positions drafted by SHM’s staffers or the Public Policy Committee. Dr. Greeno says the physicians who participated in this year’s Hill trip are likely to find they will be asked to be the first cohort of a grassroots initiative meant to deliver the society’s message more routinely.
“These are not easy things to change because there are not easy solutions,” Dr. Greeno adds. “If you have just one meeting on the Hill, you’ll have no impact at all. You have to follow up. You have to do it consistently. And you have to have a consistent message. And we will.”
Richard Quinn is a freelance writer in New Jersey.
A veritable perfect storm of relationships brought hospitalist Jairy Hunter, MD, MBA, SFHM, to “Hospitalists on the Hill 2013,” a daylong advocacy affair that preceded HM13 last month.
First, Dr. Hunter was born and bred—and now lives—in South Carolina, a close-knit state where leaders across industries tend to run in the same circles, or at least have relatives who do. Second, Dr. Hunter’s father, Jairy Hunter Jr., is the longtime president of Charleston Southern University, where Sen. Tim Scott (R-S.C.) earned his undergraduate degree when it was still called Baptist College at Charleston. And three, Dr. Hunter is associate executive medical director of one of the state’s flagship health-care institutions, Medical University of South Carolina in Charleston.
So it was that SHM set Dr. Hunter up in meetings with the offices of Scott, Sen. Lindsey Graham (R-S.C.), and Rep. Jim Clyburn (D-S.C.), and—for the day at least—made Dr. Hunter the voice of hospital medicine.
“It was a little bit demystifying of an experience to be able to know there’s actually people you can talk to and you can develop a relationship with,” says Dr. Hunter, who also serves on Team Hospitalist. “I thought that was very rewarding.”
The connections made by Dr. Hunter are the point of the annual trek made by SHM leaders and members to lobby legislators and federal staffers “on the way policies affect your practice and your patients,” SHM says on its website (www.hospitalmedicine.org/advocacy). This year’s volunteer effort was by far the largest ever, says Public Policy Committee chair Ron Greeno, MD, FCCP, MHM. More than 150 hospitalists participated in training, 113 hospitalists visited Capitol Hill, and scores more had to be turned away. All told, hospitalists held 409 individual meetings with legislators and staff members.
“Quite frankly, if we’d have had the budget, we could have had another 100 to 150 people come,” Dr. Greeno says. “That’s how many people wanted to go.”
Dr. Greeno attributes the interest to two factors. One, having the annual meeting at the Gaylord National Resort & Convention Center, just outside Washington, D.C, makes the Hill trip a natural extension. Two, the current landscape of health-care reform has motivated many physicians to become more involved than they might otherwise be. One challenge of having so many first-timers making this year’s trip was making sure they were properly prepared. To hone the message, SHM gave the group a few hours of education by former legislative staffer Stephanie Vance of Advocacy Associates, a communications firm that helps organizations, such as medical societies, tailor their message to policymakers. Vance told hospitalists a personal visit with a constituent often becomes the most influential type of advocacy.
“That’s why it was easy to make an initial connection, because these staffers are from where I’m from, friends with people that I’m friends with,” Dr. Hunter says.
Unique Approach
SHM CEO Larry Wellikson, MD, SFHM, says the society tries to differentiate itself from other organizations through its grassroots approach to advocacy. More important, the society refrains from giving a long list of legislative requests that are self-serving.
“We’re someone they want to talk to because we’re not coming there to just say, ‘Here’s a power play for hospitalists,’” Dr. Wellikson says. “We come and try to provide solutions.”
To that end, this year’s lobbying effort was targeted to topics important both to HM and the health-care system:
- Repealing the sustainable growth rate (SGR) formula for Medicare payments, specifically via the proposed Medicare Physician Payment Innovation Act of 2013 (H.R. 574);
- Solving the quagmire of observation status time not counting toward the required three consecutive overnights as an inpatient needed to qualify for Medicare benefits at a skilled nursing facility, by supporting the Improving Access to Medicare Coverage Act of 2013 (H.R. 1179, S. 569); and
- Getting the federal government to commit to providing $434 million in funding for the Agency for Healthcare Research and Quality (AHRQ) in fiscal 2014.
“The message that we’re sending resonated with the people we met with on both sides of the aisle,” Dr. Greeno says. “The SGR, for instance, they know there needs to be a fix. We want to serve as a resource for them as they start to figure out the answer to the question: What are we going to replace it with?
“What we want to do is make everybody on the Hill understand that we can be relied upon as a resource when they’re looking for solutions,” he says.
Focused on Follow-Up
And that’s where rank-and-filers, such as Dr. Hunter, have to take charge. So for his Hill Day visits, he tried to stand out. Everyone he met with got a lapel pin in the shape of a South Carolina state flag, which has become a popular fashion statement in recent years. And Scott also got a pin from Charleston Southern University, his alma mater. The gestures were small, but they served as icebreakers and reminders that Dr. Hunter and the people he met are bound by service to the residents of the Palmetto State.
Dr. Hunter also hopes the small token will be that little extra that makes him memorable enough that the next time a Congressional staffer has an SGR question, they’ll ask him and not a doctor from another specialty.
“I’m interested to see how much feedback I get back from them,” he says. “I can feed them all day long, but I don’t want to be that crazy guy bugging them. If they respond back to me, I can hopefully make more inroads.”
He certainly would if Dr. Greeno gets his way. Moving forward, SHM hopes to be able to rely more on local advocates pushing for reform than just a once-a-year major event and formal positions drafted by SHM’s staffers or the Public Policy Committee. Dr. Greeno says the physicians who participated in this year’s Hill trip are likely to find they will be asked to be the first cohort of a grassroots initiative meant to deliver the society’s message more routinely.
“These are not easy things to change because there are not easy solutions,” Dr. Greeno adds. “If you have just one meeting on the Hill, you’ll have no impact at all. You have to follow up. You have to do it consistently. And you have to have a consistent message. And we will.”
Richard Quinn is a freelance writer in New Jersey.
A veritable perfect storm of relationships brought hospitalist Jairy Hunter, MD, MBA, SFHM, to “Hospitalists on the Hill 2013,” a daylong advocacy affair that preceded HM13 last month.
First, Dr. Hunter was born and bred—and now lives—in South Carolina, a close-knit state where leaders across industries tend to run in the same circles, or at least have relatives who do. Second, Dr. Hunter’s father, Jairy Hunter Jr., is the longtime president of Charleston Southern University, where Sen. Tim Scott (R-S.C.) earned his undergraduate degree when it was still called Baptist College at Charleston. And three, Dr. Hunter is associate executive medical director of one of the state’s flagship health-care institutions, Medical University of South Carolina in Charleston.
So it was that SHM set Dr. Hunter up in meetings with the offices of Scott, Sen. Lindsey Graham (R-S.C.), and Rep. Jim Clyburn (D-S.C.), and—for the day at least—made Dr. Hunter the voice of hospital medicine.
“It was a little bit demystifying of an experience to be able to know there’s actually people you can talk to and you can develop a relationship with,” says Dr. Hunter, who also serves on Team Hospitalist. “I thought that was very rewarding.”
The connections made by Dr. Hunter are the point of the annual trek made by SHM leaders and members to lobby legislators and federal staffers “on the way policies affect your practice and your patients,” SHM says on its website (www.hospitalmedicine.org/advocacy). This year’s volunteer effort was by far the largest ever, says Public Policy Committee chair Ron Greeno, MD, FCCP, MHM. More than 150 hospitalists participated in training, 113 hospitalists visited Capitol Hill, and scores more had to be turned away. All told, hospitalists held 409 individual meetings with legislators and staff members.
“Quite frankly, if we’d have had the budget, we could have had another 100 to 150 people come,” Dr. Greeno says. “That’s how many people wanted to go.”
Dr. Greeno attributes the interest to two factors. One, having the annual meeting at the Gaylord National Resort & Convention Center, just outside Washington, D.C, makes the Hill trip a natural extension. Two, the current landscape of health-care reform has motivated many physicians to become more involved than they might otherwise be. One challenge of having so many first-timers making this year’s trip was making sure they were properly prepared. To hone the message, SHM gave the group a few hours of education by former legislative staffer Stephanie Vance of Advocacy Associates, a communications firm that helps organizations, such as medical societies, tailor their message to policymakers. Vance told hospitalists a personal visit with a constituent often becomes the most influential type of advocacy.
“That’s why it was easy to make an initial connection, because these staffers are from where I’m from, friends with people that I’m friends with,” Dr. Hunter says.
Unique Approach
SHM CEO Larry Wellikson, MD, SFHM, says the society tries to differentiate itself from other organizations through its grassroots approach to advocacy. More important, the society refrains from giving a long list of legislative requests that are self-serving.
“We’re someone they want to talk to because we’re not coming there to just say, ‘Here’s a power play for hospitalists,’” Dr. Wellikson says. “We come and try to provide solutions.”
To that end, this year’s lobbying effort was targeted to topics important both to HM and the health-care system:
- Repealing the sustainable growth rate (SGR) formula for Medicare payments, specifically via the proposed Medicare Physician Payment Innovation Act of 2013 (H.R. 574);
- Solving the quagmire of observation status time not counting toward the required three consecutive overnights as an inpatient needed to qualify for Medicare benefits at a skilled nursing facility, by supporting the Improving Access to Medicare Coverage Act of 2013 (H.R. 1179, S. 569); and
- Getting the federal government to commit to providing $434 million in funding for the Agency for Healthcare Research and Quality (AHRQ) in fiscal 2014.
“The message that we’re sending resonated with the people we met with on both sides of the aisle,” Dr. Greeno says. “The SGR, for instance, they know there needs to be a fix. We want to serve as a resource for them as they start to figure out the answer to the question: What are we going to replace it with?
“What we want to do is make everybody on the Hill understand that we can be relied upon as a resource when they’re looking for solutions,” he says.
Focused on Follow-Up
And that’s where rank-and-filers, such as Dr. Hunter, have to take charge. So for his Hill Day visits, he tried to stand out. Everyone he met with got a lapel pin in the shape of a South Carolina state flag, which has become a popular fashion statement in recent years. And Scott also got a pin from Charleston Southern University, his alma mater. The gestures were small, but they served as icebreakers and reminders that Dr. Hunter and the people he met are bound by service to the residents of the Palmetto State.
Dr. Hunter also hopes the small token will be that little extra that makes him memorable enough that the next time a Congressional staffer has an SGR question, they’ll ask him and not a doctor from another specialty.
“I’m interested to see how much feedback I get back from them,” he says. “I can feed them all day long, but I don’t want to be that crazy guy bugging them. If they respond back to me, I can hopefully make more inroads.”
He certainly would if Dr. Greeno gets his way. Moving forward, SHM hopes to be able to rely more on local advocates pushing for reform than just a once-a-year major event and formal positions drafted by SHM’s staffers or the Public Policy Committee. Dr. Greeno says the physicians who participated in this year’s Hill trip are likely to find they will be asked to be the first cohort of a grassroots initiative meant to deliver the society’s message more routinely.
“These are not easy things to change because there are not easy solutions,” Dr. Greeno adds. “If you have just one meeting on the Hill, you’ll have no impact at all. You have to follow up. You have to do it consistently. And you have to have a consistent message. And we will.”
Richard Quinn is a freelance writer in New Jersey.
Rival Hospitalists Can Bring Havoc, or Healthy Competition to Hospitals
In November 2011, the board of directors of Lee Memorial Health System in Fort Myers, Fla., voted to close access at its four hospitals to any hospitalist who didn’t already practice there or wasn’t affiliated with private practices that contracted with the health system. According to a report in a local newspaper, the proliferation of competing hospitalist practices at Lee Memorial was contributing to high rates of patient and referring physician dissatisfaction and hospitalist turnover.1 As a result, the board limited new hospitalists from entering practice in their facilities until they could develop “rules of engagement” for the existing hospitalists through new contracts and standards of practice.
The Lee Memorial example of multiple, competing hospitalist groups—and individuals practicing hospital medicine, also known as “lone wolf” hospitalists—causing havoc is atypical of the fledgling medical specialty, which has seen rapid growth the past two decades. Even so, veteran hospitalists confirm that nowadays, with nearly 40,000 hospitalists practicing in a majority of U.S. hospitals, it’s not uncommon to have multiple groups or individuals working under the same hospital roof. What is concerning to some in the specialty is how the competition can turn ugly, especially considering SHM espouses such virtues as teamwork, leadership, and quality improvement (QI).
Even so, situations arise when multiple HM groups under one roof don’t get along. Sometimes those groups or individual practitioners compete, head to head, for new admissions. Some hospitals have patient populations carved out by capitated medical groups or staff/group model HMOs. Some specialty groups, cardiology or orthopedics, for example, choose to contract hospitalist groups for their patients, setting up potential conflicts with new admissions. Other hospitals have “lone wolf” hospitalists, basically a practice of one.
No matter the dynamic, hospital administrators are frustrated with their inability to control competitive situations, especially when competing groups or individuals do not act in conjunction with their strategic goals.
Depending on hospital bylaws and state regulations, it might be difficult to exclude hospitalists from practicing in the hospital or to cut off competition. Some hospitals even welcome competition—as a prime virtue in its own right, a way to advance quality, or to guard against staffing shortages. The challenge, hospitalists and administrators say, is to encourage multiple groups to work amicably alongside each other, cooperating on the hospital’s larger mission and working toward its quality targets—and to make sure clinicians focus less on competition and more on patients (see “The Magic Bullet: Communication,”).

—Lowell Palmer, MD, FHM, hospitalist, Southwest Washington Medical Center, Vancouver
Purposeful, Team-Based Medicine
Scott Nygaard, MD, Lee Memorial’s chief medical officer for physician services, announced on Aug. 29, 2012, that the health system was contracting with a newly formed medical group called Inpatient Specialists of Southwest Florida (ISSF), a partnership between Cape Coral, Fla.-based Hospitalist Group of Southwest Florida (HGSF) and national management company Cogent HMG based in Brentwood, Tenn. HGSF and Cogent HMG already had established practices in two of Lee’s four hospitals.
Other existing hospitalist groups are permitted to continue practicing in these hospitals, although only a contracted group will be able to recruit or add new physicians, Dr. Nygaard says.
“The bylaws did not allow us to formally close access for staff already in practice,” he said. Physicians have the option of joining ISSF, and eventually, he says, the other groups dwindled in numbers through attrition. As Lee Memorial’s sole provider of hospitalist care, ISSF’s long-term goal is to put HM on a similar footing with other hospital-based specialties, such as emergency medicine and anesthesiology.
As of late 2012, six hospitalist groups and more than 80 hospitalists practice at Lee Memorial hospitals; 40 of those hospitalists belong to ISSF. “The other groups were all offered an opportunity to discuss a contractual relationship with the system, but they declined,” Dr. Nygaard says.
The remaining groups had worked amicably alongside each other but in an atmosphere Dr. Nygaard likens to a flea market, with each group practicing its own separate business and business model.
A standardized approach conducive to achieving the hospital’s quality and performance targets was lacking, however. As a result, Lee Memorial implemented an HM standard of care within the system. It helped somewhat, Dr. Nygaard says, but it didn’t fix all of the competition problems.
“We have learned that variation is the enemy of quality, especially in the highly complex environment of an acute-care hospital, trying to generate the kinds of measurable results we are now being asked to provide,” he explains. “We need to be more organized, structured, and purposeful in an era of team-based medicine. You need committed, aligned partnerships offering appropriate incentives.”
The ISSF contract contains such performance incentives.
“The joint venture formalizes an informal, long-standing, collaborative relationship” between the two participating HM groups, says Joseph Daley, MD, co-founder and director of quality services for Hospitalist Group of Southwest Florida. “We bring substantial, local expertise to the table, and have been quality partners with both Lee Memorial and Cogent HMG.”
And, as of April, Lee Memorial spokesperson Mary Briggs reported patient satisfaction scores for hospitalists are improving. “We believe the changes put in place were the right ones,” she emailed The Hospitalist.

—Scott Nygaard, MD, chief medical officer for physician services, Lee Memorial Health System, Fort Myers, Fla.
Supply and Demand
Every local hospital environment is different, with HM group arrangements shaped to a large degree by supply and demand for physicians, says Brian Hazen, MD, chief of hospital medicine at Inova Fairfax Hospital in Falls Church, Va., one of five hospitals in the Inova system. Inova Fairfax employs the hospitalists in Dr. Hazen’s group but is also home to other groups, including a neurohospitalist service and about a half dozen solo practitioners. Dr. Hazen’s group receives administrative support from the hospital and primarily is assigned patients through the ED. Some of the private hospitalists don’t want to take ED call, he says, instead preferring to get referrals of insured patients from primary-care-physician groups.
“Here in the D.C. area, we’re reasonably well staffed by hospitalists, but we’re not fighting over patients. In fact, if it weren’t for the private physicians, we’d have trouble meeting current staffing needs,” Dr. Hazen says. “I have also seen competition in other hospital settings, but I haven’t been in a situation where the doctors were fighting over patients.”
The “lone wolf” hospitalists at Inova Fairfax work very hard, Dr. Hazen adds. “A lot of them have private practices, see patients in the hospital, and also take call. If one of them has to leave town on short notice, we can help them out. On the flip side, if we’re busy in the emergency department, we’ll call on them,” he says.
The ED receives instruction on which hospitalist group admits which patient, but sometimes referral mistakes are made.
“If we accidently admit a patient who should have gone to one of the private people, who depend on these admissions for their income, I let them choose whether we should continue to see that patient or do a transfer,” Dr. Hazen says. “For the most part, we all try to be nice people.”
In the current health-care environment, hospital administrators might be reluctant to erect barriers to multiple hospitalist practices under one roof for fear of restraining trade, just as they don’t stand in the way of primary-care physicians who want to follow their own patients into the hospital. It might be easier to enact equally enforced requirements for the credentialing and privileging of all hospitalists who want to practice at the hospital, spelling out expectations in such areas as following protocols. (In 2011, SHM issued a position paper on hospitalist credentialing that addressed the appropriate time to institute a credentialing category with privileging criteria for hospitalists, and how to preserve maximum flexibility within this process.)2
Hospitals can limit who they contract with, who gets administrative support—and how much—using financial and quality performance to shape contracting decisions. In many communities, that could serve as an excluder of multiple groups in the same building, but in other locales, the payor mix might be attractive enough for physicians to survive on billing alone, says Leslie Flores, MPH, of Nelson Flores Hospital Medicine Consultants. If the hospital isn’t providing financial support, it will have less influence over how that group does things.
Dr. Hazen says his employed hospitalist group at Inova Fairfax is represented on more than 20 hospital committees and quality initiatives in the hospital, and has demonstrated its alignment with the hospital’s goals. Recently, in response to the administration’s concerns about throughput, his group initiated geographic, multidisciplinary rounding.
“I can do this because I have elite physicians, and because I protect them from unreasonable expectations,” he says. “Everyone needs to understand that the hospital needs to survive, so the hospital has a right to expect certain things from its hospitalists, such as performance on length of stay, throughput, other core measures, and promptly answering pages. Everyone should understand that those are the rules. Being fair, honest, and transparent about expectations is not an unreasonable expectation.”
Competition among hospitalists should be on a professional basis, experts emphasize, and cooperation is in everyone’s best interests. But Lowell Palmer, MD, FHM, a hospitalist at Southwest Washington Medical Center in Vancouver, Wash., thinks competition can be a healthy thing for hospitalist groups.
“It forces us to make sure the services we provide are meeting the customer’s expectations,” says Dr. Palmer, who works with Cogent Physician Services, one of the three HM groups at Southwest Washington. “We can and do learn from each other.”
Impact of Health-Care Reform
Beware the transformation health-care reform is having on the dynamics of hospital-based practice and the competitive landscape facing more hospitalist groups, says Roger Heroux, MHA, PhD, CHE, consultant with Hospitalist Management Resources LLC. Reforms mean hospitalists are seeing an increased emphasis on coordinating with post-acute-care providers, improving care transitions, preventing readmissions, and meeting hospital targets for quality and patient safety.
Primary-care groups, accountable-care organizations (ACOs), and health plans could choose specific hospitalist practices they want to partner with to manage the care of their hospitalized members, but they will have clear performance expectations that those groups will need to meet, spelled out in benchmarks. Or, as some experts believe, they might opt to bring in their own hospitalist group.
“We’re spending our time working with existing hospitalist programs to help them be more efficient and effective, to manage risk, and to become aggressive about meeting the clinical benchmarks,” Heroux says. Hospitals, ACOs, and capitated groups can’t afford not to have a high-performing hospitalist program, so this will become a hallmark of survival for hospitalist programs as well. “In a highly managed environment, patients will be managed by a hospitalist group that is responsive to these expectations,” he says.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Gluck F. Lee Memorial Health Systems’ hospitalists under new controls. Fort Myers News Press. Dec. 1, 2011.
- Society of Hospital Medicine Position Statement on Hospitalist Credentialing and Medical Staff Privileges. SHM website. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Where_We_Stand&Template=/CM/HTMLDisplay.cfm&ContentID=28262. Accessed April 1, 2013.
In November 2011, the board of directors of Lee Memorial Health System in Fort Myers, Fla., voted to close access at its four hospitals to any hospitalist who didn’t already practice there or wasn’t affiliated with private practices that contracted with the health system. According to a report in a local newspaper, the proliferation of competing hospitalist practices at Lee Memorial was contributing to high rates of patient and referring physician dissatisfaction and hospitalist turnover.1 As a result, the board limited new hospitalists from entering practice in their facilities until they could develop “rules of engagement” for the existing hospitalists through new contracts and standards of practice.
The Lee Memorial example of multiple, competing hospitalist groups—and individuals practicing hospital medicine, also known as “lone wolf” hospitalists—causing havoc is atypical of the fledgling medical specialty, which has seen rapid growth the past two decades. Even so, veteran hospitalists confirm that nowadays, with nearly 40,000 hospitalists practicing in a majority of U.S. hospitals, it’s not uncommon to have multiple groups or individuals working under the same hospital roof. What is concerning to some in the specialty is how the competition can turn ugly, especially considering SHM espouses such virtues as teamwork, leadership, and quality improvement (QI).
Even so, situations arise when multiple HM groups under one roof don’t get along. Sometimes those groups or individual practitioners compete, head to head, for new admissions. Some hospitals have patient populations carved out by capitated medical groups or staff/group model HMOs. Some specialty groups, cardiology or orthopedics, for example, choose to contract hospitalist groups for their patients, setting up potential conflicts with new admissions. Other hospitals have “lone wolf” hospitalists, basically a practice of one.
No matter the dynamic, hospital administrators are frustrated with their inability to control competitive situations, especially when competing groups or individuals do not act in conjunction with their strategic goals.
Depending on hospital bylaws and state regulations, it might be difficult to exclude hospitalists from practicing in the hospital or to cut off competition. Some hospitals even welcome competition—as a prime virtue in its own right, a way to advance quality, or to guard against staffing shortages. The challenge, hospitalists and administrators say, is to encourage multiple groups to work amicably alongside each other, cooperating on the hospital’s larger mission and working toward its quality targets—and to make sure clinicians focus less on competition and more on patients (see “The Magic Bullet: Communication,”).

—Lowell Palmer, MD, FHM, hospitalist, Southwest Washington Medical Center, Vancouver
Purposeful, Team-Based Medicine
Scott Nygaard, MD, Lee Memorial’s chief medical officer for physician services, announced on Aug. 29, 2012, that the health system was contracting with a newly formed medical group called Inpatient Specialists of Southwest Florida (ISSF), a partnership between Cape Coral, Fla.-based Hospitalist Group of Southwest Florida (HGSF) and national management company Cogent HMG based in Brentwood, Tenn. HGSF and Cogent HMG already had established practices in two of Lee’s four hospitals.
Other existing hospitalist groups are permitted to continue practicing in these hospitals, although only a contracted group will be able to recruit or add new physicians, Dr. Nygaard says.
“The bylaws did not allow us to formally close access for staff already in practice,” he said. Physicians have the option of joining ISSF, and eventually, he says, the other groups dwindled in numbers through attrition. As Lee Memorial’s sole provider of hospitalist care, ISSF’s long-term goal is to put HM on a similar footing with other hospital-based specialties, such as emergency medicine and anesthesiology.
As of late 2012, six hospitalist groups and more than 80 hospitalists practice at Lee Memorial hospitals; 40 of those hospitalists belong to ISSF. “The other groups were all offered an opportunity to discuss a contractual relationship with the system, but they declined,” Dr. Nygaard says.
The remaining groups had worked amicably alongside each other but in an atmosphere Dr. Nygaard likens to a flea market, with each group practicing its own separate business and business model.
A standardized approach conducive to achieving the hospital’s quality and performance targets was lacking, however. As a result, Lee Memorial implemented an HM standard of care within the system. It helped somewhat, Dr. Nygaard says, but it didn’t fix all of the competition problems.
“We have learned that variation is the enemy of quality, especially in the highly complex environment of an acute-care hospital, trying to generate the kinds of measurable results we are now being asked to provide,” he explains. “We need to be more organized, structured, and purposeful in an era of team-based medicine. You need committed, aligned partnerships offering appropriate incentives.”
The ISSF contract contains such performance incentives.
“The joint venture formalizes an informal, long-standing, collaborative relationship” between the two participating HM groups, says Joseph Daley, MD, co-founder and director of quality services for Hospitalist Group of Southwest Florida. “We bring substantial, local expertise to the table, and have been quality partners with both Lee Memorial and Cogent HMG.”
And, as of April, Lee Memorial spokesperson Mary Briggs reported patient satisfaction scores for hospitalists are improving. “We believe the changes put in place were the right ones,” she emailed The Hospitalist.

—Scott Nygaard, MD, chief medical officer for physician services, Lee Memorial Health System, Fort Myers, Fla.
Supply and Demand
Every local hospital environment is different, with HM group arrangements shaped to a large degree by supply and demand for physicians, says Brian Hazen, MD, chief of hospital medicine at Inova Fairfax Hospital in Falls Church, Va., one of five hospitals in the Inova system. Inova Fairfax employs the hospitalists in Dr. Hazen’s group but is also home to other groups, including a neurohospitalist service and about a half dozen solo practitioners. Dr. Hazen’s group receives administrative support from the hospital and primarily is assigned patients through the ED. Some of the private hospitalists don’t want to take ED call, he says, instead preferring to get referrals of insured patients from primary-care-physician groups.
“Here in the D.C. area, we’re reasonably well staffed by hospitalists, but we’re not fighting over patients. In fact, if it weren’t for the private physicians, we’d have trouble meeting current staffing needs,” Dr. Hazen says. “I have also seen competition in other hospital settings, but I haven’t been in a situation where the doctors were fighting over patients.”
The “lone wolf” hospitalists at Inova Fairfax work very hard, Dr. Hazen adds. “A lot of them have private practices, see patients in the hospital, and also take call. If one of them has to leave town on short notice, we can help them out. On the flip side, if we’re busy in the emergency department, we’ll call on them,” he says.
The ED receives instruction on which hospitalist group admits which patient, but sometimes referral mistakes are made.
“If we accidently admit a patient who should have gone to one of the private people, who depend on these admissions for their income, I let them choose whether we should continue to see that patient or do a transfer,” Dr. Hazen says. “For the most part, we all try to be nice people.”
In the current health-care environment, hospital administrators might be reluctant to erect barriers to multiple hospitalist practices under one roof for fear of restraining trade, just as they don’t stand in the way of primary-care physicians who want to follow their own patients into the hospital. It might be easier to enact equally enforced requirements for the credentialing and privileging of all hospitalists who want to practice at the hospital, spelling out expectations in such areas as following protocols. (In 2011, SHM issued a position paper on hospitalist credentialing that addressed the appropriate time to institute a credentialing category with privileging criteria for hospitalists, and how to preserve maximum flexibility within this process.)2
Hospitals can limit who they contract with, who gets administrative support—and how much—using financial and quality performance to shape contracting decisions. In many communities, that could serve as an excluder of multiple groups in the same building, but in other locales, the payor mix might be attractive enough for physicians to survive on billing alone, says Leslie Flores, MPH, of Nelson Flores Hospital Medicine Consultants. If the hospital isn’t providing financial support, it will have less influence over how that group does things.
Dr. Hazen says his employed hospitalist group at Inova Fairfax is represented on more than 20 hospital committees and quality initiatives in the hospital, and has demonstrated its alignment with the hospital’s goals. Recently, in response to the administration’s concerns about throughput, his group initiated geographic, multidisciplinary rounding.
“I can do this because I have elite physicians, and because I protect them from unreasonable expectations,” he says. “Everyone needs to understand that the hospital needs to survive, so the hospital has a right to expect certain things from its hospitalists, such as performance on length of stay, throughput, other core measures, and promptly answering pages. Everyone should understand that those are the rules. Being fair, honest, and transparent about expectations is not an unreasonable expectation.”
Competition among hospitalists should be on a professional basis, experts emphasize, and cooperation is in everyone’s best interests. But Lowell Palmer, MD, FHM, a hospitalist at Southwest Washington Medical Center in Vancouver, Wash., thinks competition can be a healthy thing for hospitalist groups.
“It forces us to make sure the services we provide are meeting the customer’s expectations,” says Dr. Palmer, who works with Cogent Physician Services, one of the three HM groups at Southwest Washington. “We can and do learn from each other.”
Impact of Health-Care Reform
Beware the transformation health-care reform is having on the dynamics of hospital-based practice and the competitive landscape facing more hospitalist groups, says Roger Heroux, MHA, PhD, CHE, consultant with Hospitalist Management Resources LLC. Reforms mean hospitalists are seeing an increased emphasis on coordinating with post-acute-care providers, improving care transitions, preventing readmissions, and meeting hospital targets for quality and patient safety.
Primary-care groups, accountable-care organizations (ACOs), and health plans could choose specific hospitalist practices they want to partner with to manage the care of their hospitalized members, but they will have clear performance expectations that those groups will need to meet, spelled out in benchmarks. Or, as some experts believe, they might opt to bring in their own hospitalist group.
“We’re spending our time working with existing hospitalist programs to help them be more efficient and effective, to manage risk, and to become aggressive about meeting the clinical benchmarks,” Heroux says. Hospitals, ACOs, and capitated groups can’t afford not to have a high-performing hospitalist program, so this will become a hallmark of survival for hospitalist programs as well. “In a highly managed environment, patients will be managed by a hospitalist group that is responsive to these expectations,” he says.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Gluck F. Lee Memorial Health Systems’ hospitalists under new controls. Fort Myers News Press. Dec. 1, 2011.
- Society of Hospital Medicine Position Statement on Hospitalist Credentialing and Medical Staff Privileges. SHM website. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Where_We_Stand&Template=/CM/HTMLDisplay.cfm&ContentID=28262. Accessed April 1, 2013.
In November 2011, the board of directors of Lee Memorial Health System in Fort Myers, Fla., voted to close access at its four hospitals to any hospitalist who didn’t already practice there or wasn’t affiliated with private practices that contracted with the health system. According to a report in a local newspaper, the proliferation of competing hospitalist practices at Lee Memorial was contributing to high rates of patient and referring physician dissatisfaction and hospitalist turnover.1 As a result, the board limited new hospitalists from entering practice in their facilities until they could develop “rules of engagement” for the existing hospitalists through new contracts and standards of practice.
The Lee Memorial example of multiple, competing hospitalist groups—and individuals practicing hospital medicine, also known as “lone wolf” hospitalists—causing havoc is atypical of the fledgling medical specialty, which has seen rapid growth the past two decades. Even so, veteran hospitalists confirm that nowadays, with nearly 40,000 hospitalists practicing in a majority of U.S. hospitals, it’s not uncommon to have multiple groups or individuals working under the same hospital roof. What is concerning to some in the specialty is how the competition can turn ugly, especially considering SHM espouses such virtues as teamwork, leadership, and quality improvement (QI).
Even so, situations arise when multiple HM groups under one roof don’t get along. Sometimes those groups or individual practitioners compete, head to head, for new admissions. Some hospitals have patient populations carved out by capitated medical groups or staff/group model HMOs. Some specialty groups, cardiology or orthopedics, for example, choose to contract hospitalist groups for their patients, setting up potential conflicts with new admissions. Other hospitals have “lone wolf” hospitalists, basically a practice of one.
No matter the dynamic, hospital administrators are frustrated with their inability to control competitive situations, especially when competing groups or individuals do not act in conjunction with their strategic goals.
Depending on hospital bylaws and state regulations, it might be difficult to exclude hospitalists from practicing in the hospital or to cut off competition. Some hospitals even welcome competition—as a prime virtue in its own right, a way to advance quality, or to guard against staffing shortages. The challenge, hospitalists and administrators say, is to encourage multiple groups to work amicably alongside each other, cooperating on the hospital’s larger mission and working toward its quality targets—and to make sure clinicians focus less on competition and more on patients (see “The Magic Bullet: Communication,”).

—Lowell Palmer, MD, FHM, hospitalist, Southwest Washington Medical Center, Vancouver
Purposeful, Team-Based Medicine
Scott Nygaard, MD, Lee Memorial’s chief medical officer for physician services, announced on Aug. 29, 2012, that the health system was contracting with a newly formed medical group called Inpatient Specialists of Southwest Florida (ISSF), a partnership between Cape Coral, Fla.-based Hospitalist Group of Southwest Florida (HGSF) and national management company Cogent HMG based in Brentwood, Tenn. HGSF and Cogent HMG already had established practices in two of Lee’s four hospitals.
Other existing hospitalist groups are permitted to continue practicing in these hospitals, although only a contracted group will be able to recruit or add new physicians, Dr. Nygaard says.
“The bylaws did not allow us to formally close access for staff already in practice,” he said. Physicians have the option of joining ISSF, and eventually, he says, the other groups dwindled in numbers through attrition. As Lee Memorial’s sole provider of hospitalist care, ISSF’s long-term goal is to put HM on a similar footing with other hospital-based specialties, such as emergency medicine and anesthesiology.
As of late 2012, six hospitalist groups and more than 80 hospitalists practice at Lee Memorial hospitals; 40 of those hospitalists belong to ISSF. “The other groups were all offered an opportunity to discuss a contractual relationship with the system, but they declined,” Dr. Nygaard says.
The remaining groups had worked amicably alongside each other but in an atmosphere Dr. Nygaard likens to a flea market, with each group practicing its own separate business and business model.
A standardized approach conducive to achieving the hospital’s quality and performance targets was lacking, however. As a result, Lee Memorial implemented an HM standard of care within the system. It helped somewhat, Dr. Nygaard says, but it didn’t fix all of the competition problems.
“We have learned that variation is the enemy of quality, especially in the highly complex environment of an acute-care hospital, trying to generate the kinds of measurable results we are now being asked to provide,” he explains. “We need to be more organized, structured, and purposeful in an era of team-based medicine. You need committed, aligned partnerships offering appropriate incentives.”
The ISSF contract contains such performance incentives.
“The joint venture formalizes an informal, long-standing, collaborative relationship” between the two participating HM groups, says Joseph Daley, MD, co-founder and director of quality services for Hospitalist Group of Southwest Florida. “We bring substantial, local expertise to the table, and have been quality partners with both Lee Memorial and Cogent HMG.”
And, as of April, Lee Memorial spokesperson Mary Briggs reported patient satisfaction scores for hospitalists are improving. “We believe the changes put in place were the right ones,” she emailed The Hospitalist.

—Scott Nygaard, MD, chief medical officer for physician services, Lee Memorial Health System, Fort Myers, Fla.
Supply and Demand
Every local hospital environment is different, with HM group arrangements shaped to a large degree by supply and demand for physicians, says Brian Hazen, MD, chief of hospital medicine at Inova Fairfax Hospital in Falls Church, Va., one of five hospitals in the Inova system. Inova Fairfax employs the hospitalists in Dr. Hazen’s group but is also home to other groups, including a neurohospitalist service and about a half dozen solo practitioners. Dr. Hazen’s group receives administrative support from the hospital and primarily is assigned patients through the ED. Some of the private hospitalists don’t want to take ED call, he says, instead preferring to get referrals of insured patients from primary-care-physician groups.
“Here in the D.C. area, we’re reasonably well staffed by hospitalists, but we’re not fighting over patients. In fact, if it weren’t for the private physicians, we’d have trouble meeting current staffing needs,” Dr. Hazen says. “I have also seen competition in other hospital settings, but I haven’t been in a situation where the doctors were fighting over patients.”
The “lone wolf” hospitalists at Inova Fairfax work very hard, Dr. Hazen adds. “A lot of them have private practices, see patients in the hospital, and also take call. If one of them has to leave town on short notice, we can help them out. On the flip side, if we’re busy in the emergency department, we’ll call on them,” he says.
The ED receives instruction on which hospitalist group admits which patient, but sometimes referral mistakes are made.
“If we accidently admit a patient who should have gone to one of the private people, who depend on these admissions for their income, I let them choose whether we should continue to see that patient or do a transfer,” Dr. Hazen says. “For the most part, we all try to be nice people.”
In the current health-care environment, hospital administrators might be reluctant to erect barriers to multiple hospitalist practices under one roof for fear of restraining trade, just as they don’t stand in the way of primary-care physicians who want to follow their own patients into the hospital. It might be easier to enact equally enforced requirements for the credentialing and privileging of all hospitalists who want to practice at the hospital, spelling out expectations in such areas as following protocols. (In 2011, SHM issued a position paper on hospitalist credentialing that addressed the appropriate time to institute a credentialing category with privileging criteria for hospitalists, and how to preserve maximum flexibility within this process.)2
Hospitals can limit who they contract with, who gets administrative support—and how much—using financial and quality performance to shape contracting decisions. In many communities, that could serve as an excluder of multiple groups in the same building, but in other locales, the payor mix might be attractive enough for physicians to survive on billing alone, says Leslie Flores, MPH, of Nelson Flores Hospital Medicine Consultants. If the hospital isn’t providing financial support, it will have less influence over how that group does things.
Dr. Hazen says his employed hospitalist group at Inova Fairfax is represented on more than 20 hospital committees and quality initiatives in the hospital, and has demonstrated its alignment with the hospital’s goals. Recently, in response to the administration’s concerns about throughput, his group initiated geographic, multidisciplinary rounding.
“I can do this because I have elite physicians, and because I protect them from unreasonable expectations,” he says. “Everyone needs to understand that the hospital needs to survive, so the hospital has a right to expect certain things from its hospitalists, such as performance on length of stay, throughput, other core measures, and promptly answering pages. Everyone should understand that those are the rules. Being fair, honest, and transparent about expectations is not an unreasonable expectation.”
Competition among hospitalists should be on a professional basis, experts emphasize, and cooperation is in everyone’s best interests. But Lowell Palmer, MD, FHM, a hospitalist at Southwest Washington Medical Center in Vancouver, Wash., thinks competition can be a healthy thing for hospitalist groups.
“It forces us to make sure the services we provide are meeting the customer’s expectations,” says Dr. Palmer, who works with Cogent Physician Services, one of the three HM groups at Southwest Washington. “We can and do learn from each other.”
Impact of Health-Care Reform
Beware the transformation health-care reform is having on the dynamics of hospital-based practice and the competitive landscape facing more hospitalist groups, says Roger Heroux, MHA, PhD, CHE, consultant with Hospitalist Management Resources LLC. Reforms mean hospitalists are seeing an increased emphasis on coordinating with post-acute-care providers, improving care transitions, preventing readmissions, and meeting hospital targets for quality and patient safety.
Primary-care groups, accountable-care organizations (ACOs), and health plans could choose specific hospitalist practices they want to partner with to manage the care of their hospitalized members, but they will have clear performance expectations that those groups will need to meet, spelled out in benchmarks. Or, as some experts believe, they might opt to bring in their own hospitalist group.
“We’re spending our time working with existing hospitalist programs to help them be more efficient and effective, to manage risk, and to become aggressive about meeting the clinical benchmarks,” Heroux says. Hospitals, ACOs, and capitated groups can’t afford not to have a high-performing hospitalist program, so this will become a hallmark of survival for hospitalist programs as well. “In a highly managed environment, patients will be managed by a hospitalist group that is responsive to these expectations,” he says.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Gluck F. Lee Memorial Health Systems’ hospitalists under new controls. Fort Myers News Press. Dec. 1, 2011.
- Society of Hospital Medicine Position Statement on Hospitalist Credentialing and Medical Staff Privileges. SHM website. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Where_We_Stand&Template=/CM/HTMLDisplay.cfm&ContentID=28262. Accessed April 1, 2013.
UCSF Engages Hospitalists to Improve Patient Communication
In a poster presented at HM12, Kathryn Quinn, MPH, CPPS, FACHE, described how her quality team at the University of California at San Francisco (UCSF) developed a checklist to improve physician communication with patients, then taught it to the attending hospitalist faculty.1 The project began with a list of 29 best practices for patient-physician interaction, as identified in medical literature. Hospitalists then voted for the elements they felt were most important to their practice, as well as those best able to be measured, and a top-10 list was created.
Quinn, the program manager for quality and safety in the division of hospital medicine at UCSF, says the communication best practices were “chosen by the people whose practices we are trying to change.”
The quality team presented the best practices in one-hour training sessions that included small-group role plays, explains co-investigator and UCSF hospitalist Diane Sliwka, MD. The training extended to outpatient physicians, medical specialists, and chief residents. Participants also were provided a laminated pocket card listing the interventions. They also received feedback from structured observations with patients on service.
Quinn says UCSF hospitalists have improved at knocking and asking permission to enter patient rooms, introducing themselves by name and role, and encouraging questions at the end of the interaction. They have been less successful at inquiring about the patient’s concerns early in the interview and at discussing duration of treatment and next steps.
“We learned that it takes more than just talk,” Quinn says. “Just telling physicians how to improve communication doesn’t mean it’s easy to do.”
Still to be determined is the project’s impact on patient satisfaction scores, although the hospitalists reported that they found the training and feedback helpful.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
In a poster presented at HM12, Kathryn Quinn, MPH, CPPS, FACHE, described how her quality team at the University of California at San Francisco (UCSF) developed a checklist to improve physician communication with patients, then taught it to the attending hospitalist faculty.1 The project began with a list of 29 best practices for patient-physician interaction, as identified in medical literature. Hospitalists then voted for the elements they felt were most important to their practice, as well as those best able to be measured, and a top-10 list was created.
Quinn, the program manager for quality and safety in the division of hospital medicine at UCSF, says the communication best practices were “chosen by the people whose practices we are trying to change.”
The quality team presented the best practices in one-hour training sessions that included small-group role plays, explains co-investigator and UCSF hospitalist Diane Sliwka, MD. The training extended to outpatient physicians, medical specialists, and chief residents. Participants also were provided a laminated pocket card listing the interventions. They also received feedback from structured observations with patients on service.
Quinn says UCSF hospitalists have improved at knocking and asking permission to enter patient rooms, introducing themselves by name and role, and encouraging questions at the end of the interaction. They have been less successful at inquiring about the patient’s concerns early in the interview and at discussing duration of treatment and next steps.
“We learned that it takes more than just talk,” Quinn says. “Just telling physicians how to improve communication doesn’t mean it’s easy to do.”
Still to be determined is the project’s impact on patient satisfaction scores, although the hospitalists reported that they found the training and feedback helpful.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
In a poster presented at HM12, Kathryn Quinn, MPH, CPPS, FACHE, described how her quality team at the University of California at San Francisco (UCSF) developed a checklist to improve physician communication with patients, then taught it to the attending hospitalist faculty.1 The project began with a list of 29 best practices for patient-physician interaction, as identified in medical literature. Hospitalists then voted for the elements they felt were most important to their practice, as well as those best able to be measured, and a top-10 list was created.
Quinn, the program manager for quality and safety in the division of hospital medicine at UCSF, says the communication best practices were “chosen by the people whose practices we are trying to change.”
The quality team presented the best practices in one-hour training sessions that included small-group role plays, explains co-investigator and UCSF hospitalist Diane Sliwka, MD. The training extended to outpatient physicians, medical specialists, and chief residents. Participants also were provided a laminated pocket card listing the interventions. They also received feedback from structured observations with patients on service.
Quinn says UCSF hospitalists have improved at knocking and asking permission to enter patient rooms, introducing themselves by name and role, and encouraging questions at the end of the interaction. They have been less successful at inquiring about the patient’s concerns early in the interview and at discussing duration of treatment and next steps.
“We learned that it takes more than just talk,” Quinn says. “Just telling physicians how to improve communication doesn’t mean it’s easy to do.”
Still to be determined is the project’s impact on patient satisfaction scores, although the hospitalists reported that they found the training and feedback helpful.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
Hospitalists Can Get Ahead Through Quality and Patient Safety Initiatives
Are you a hospitalist who, on daily rounds, often thinks, “There’s got to be a better way to do this”? You might be just the type of person who can carve a niche for yourself in hospital quality and patient safety—and advance your career in the process.
Successful navigation of the quality-improvement (QI) and patient-safety domains, according to three veteran hospitalists, requires an initial passion and an incremental approach. Now is an especially good time, they agree, for young hospitalists to engage in these types of initiatives.
Why Do It?
In her capacity as president of the Mid-Atlantic Business Unit for Brentwood, Tenn.-based CogentHMG, Julia Wright, MD, SFHM, FACP, often encourages young recruits to consider participation in QI and patient-safety initiatives. She admits that the transition from residency to a busy HM practice, with its higher patient volumes and a faster pace, can be daunting at first. Still, she tries to cultivate interest in initiatives and establish a realistic timeframe for involvement.
There are many reasons to consider this as a career step. Dr. Wright says that quality and patient safety dovetail with hospitalists’ initial reasons for choosing medicine: to improve patients’ lives.
Janet Nagamine, RN, MD, SFHM, former patient safety officer and assistant chief of quality at Kaiser Permanente in Santa Clara, Calif., describes the fit this way: “I might be a good doctor, but as a hospitalist, I rely on many others within the system to deliver, so my patients can’t get good care until the entire system is running well,” she says. “There are all kinds of opportunities to fix our [hospital] system, and I really believe that hospitalists cannot separate themselves from that engagement.”
Elizabeth Gundersen, MD, FHM, of Fort Lauderdale, Fla., agrees that it’s a natural step to think about the ways to make a difference on a larger level. At her former institution, the University of Massachusetts (UMass) Medical School in Worcester, she parlayed her interest in QI to work her way up from ground-level hospitalist to associate chief of her division and quality officer for the hospital. “Physicians get a lot of satisfaction from helping individual patients,” she says. “One thing I really liked about getting involved with quality improvement was being able to make a difference for patients on a systems level.”
An Incremental Path
The path to her current position began with a very specific issue for Dr. Nagamine, an SHM board member who also serves as a Project BOOST co-investigator. “Although I have been doing patient safety since before they had a name for it, I didn’t start out saying that I wanted a career in quality and safety,” she says. “I was trying to take better care of my patients with diabetes, but controlling their glucose was extremely challenging because all the related variables—timing and amount of their insulin dosage, when and how much they had eaten—were charted in different places. This made it hard to adjust their insulin appropriately.”
It quickly became clear to Dr. Nagamine that the solution had to be systemic. She realized that something as basic as taking care of her patients with diabetes required multiple departments (i.e. dietary, nursing, and pharmacy) to furnish information in an integrated manner. So she joined the diabetes committee and went to work on the issue. She helped devise a flow chart that could be used by all relevant departments. A further evolution on the path emanated from one of her patients receiving the wrong medication. She joined the medication safety committee, became chair, “and the next thing you know, I’m in charge of patient safety, and an assistant chief of quality.”
Training Is Necessary
QI and patient-safety methodologies have become sophisticated disciplines in the past two decades, Dr. Wright says. Access to training in QI basics now is readily available to early-career hospitalists. For example, CogentHMG offers program support for QI so that anyone interested “doesn’t have to start from scratch anymore; we can help show them the way and support them in doing it.”
This month, HM13 (www.hospital medicine2013.org)—just outside Washington, D.C.—will offer multiple sessions on quality, as well as the “Initiating Quality Improvement Projects with Built-In Sustainment” workshop, led by Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) core investigator Peter Kaboli, MD, MS, who will address sustainability.
Beyond methodological tools, success in quality and patient safety requires the ability to motivate people, often across multiple disciplines, Dr. Nagamine says. “If you want things to work better, you must invite the right people to the table. For example, we often forget to include key nonclinical stakeholders,” she adds.
When working with hospitals across the country to implement rapid-response tTeams, Dr. Nagamine often reminds them to invite the operators, or “key people,” in the process.
“If you put patient safety at the core of your initiative and create the context for that, most people will agree that it’s the right thing to do and will get on board, even if it’s an extra step for them,” she says. “Know your audience, listen to their perspective, and learn what matters to them. And to most people, it matters that they give good patient care.”
Gretchen Henkel is a freelance writer in California.
Are you a hospitalist who, on daily rounds, often thinks, “There’s got to be a better way to do this”? You might be just the type of person who can carve a niche for yourself in hospital quality and patient safety—and advance your career in the process.
Successful navigation of the quality-improvement (QI) and patient-safety domains, according to three veteran hospitalists, requires an initial passion and an incremental approach. Now is an especially good time, they agree, for young hospitalists to engage in these types of initiatives.
Why Do It?
In her capacity as president of the Mid-Atlantic Business Unit for Brentwood, Tenn.-based CogentHMG, Julia Wright, MD, SFHM, FACP, often encourages young recruits to consider participation in QI and patient-safety initiatives. She admits that the transition from residency to a busy HM practice, with its higher patient volumes and a faster pace, can be daunting at first. Still, she tries to cultivate interest in initiatives and establish a realistic timeframe for involvement.
There are many reasons to consider this as a career step. Dr. Wright says that quality and patient safety dovetail with hospitalists’ initial reasons for choosing medicine: to improve patients’ lives.
Janet Nagamine, RN, MD, SFHM, former patient safety officer and assistant chief of quality at Kaiser Permanente in Santa Clara, Calif., describes the fit this way: “I might be a good doctor, but as a hospitalist, I rely on many others within the system to deliver, so my patients can’t get good care until the entire system is running well,” she says. “There are all kinds of opportunities to fix our [hospital] system, and I really believe that hospitalists cannot separate themselves from that engagement.”
Elizabeth Gundersen, MD, FHM, of Fort Lauderdale, Fla., agrees that it’s a natural step to think about the ways to make a difference on a larger level. At her former institution, the University of Massachusetts (UMass) Medical School in Worcester, she parlayed her interest in QI to work her way up from ground-level hospitalist to associate chief of her division and quality officer for the hospital. “Physicians get a lot of satisfaction from helping individual patients,” she says. “One thing I really liked about getting involved with quality improvement was being able to make a difference for patients on a systems level.”
An Incremental Path
The path to her current position began with a very specific issue for Dr. Nagamine, an SHM board member who also serves as a Project BOOST co-investigator. “Although I have been doing patient safety since before they had a name for it, I didn’t start out saying that I wanted a career in quality and safety,” she says. “I was trying to take better care of my patients with diabetes, but controlling their glucose was extremely challenging because all the related variables—timing and amount of their insulin dosage, when and how much they had eaten—were charted in different places. This made it hard to adjust their insulin appropriately.”
It quickly became clear to Dr. Nagamine that the solution had to be systemic. She realized that something as basic as taking care of her patients with diabetes required multiple departments (i.e. dietary, nursing, and pharmacy) to furnish information in an integrated manner. So she joined the diabetes committee and went to work on the issue. She helped devise a flow chart that could be used by all relevant departments. A further evolution on the path emanated from one of her patients receiving the wrong medication. She joined the medication safety committee, became chair, “and the next thing you know, I’m in charge of patient safety, and an assistant chief of quality.”
Training Is Necessary
QI and patient-safety methodologies have become sophisticated disciplines in the past two decades, Dr. Wright says. Access to training in QI basics now is readily available to early-career hospitalists. For example, CogentHMG offers program support for QI so that anyone interested “doesn’t have to start from scratch anymore; we can help show them the way and support them in doing it.”
This month, HM13 (www.hospital medicine2013.org)—just outside Washington, D.C.—will offer multiple sessions on quality, as well as the “Initiating Quality Improvement Projects with Built-In Sustainment” workshop, led by Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) core investigator Peter Kaboli, MD, MS, who will address sustainability.
Beyond methodological tools, success in quality and patient safety requires the ability to motivate people, often across multiple disciplines, Dr. Nagamine says. “If you want things to work better, you must invite the right people to the table. For example, we often forget to include key nonclinical stakeholders,” she adds.
When working with hospitals across the country to implement rapid-response tTeams, Dr. Nagamine often reminds them to invite the operators, or “key people,” in the process.
“If you put patient safety at the core of your initiative and create the context for that, most people will agree that it’s the right thing to do and will get on board, even if it’s an extra step for them,” she says. “Know your audience, listen to their perspective, and learn what matters to them. And to most people, it matters that they give good patient care.”
Gretchen Henkel is a freelance writer in California.
Are you a hospitalist who, on daily rounds, often thinks, “There’s got to be a better way to do this”? You might be just the type of person who can carve a niche for yourself in hospital quality and patient safety—and advance your career in the process.
Successful navigation of the quality-improvement (QI) and patient-safety domains, according to three veteran hospitalists, requires an initial passion and an incremental approach. Now is an especially good time, they agree, for young hospitalists to engage in these types of initiatives.
Why Do It?
In her capacity as president of the Mid-Atlantic Business Unit for Brentwood, Tenn.-based CogentHMG, Julia Wright, MD, SFHM, FACP, often encourages young recruits to consider participation in QI and patient-safety initiatives. She admits that the transition from residency to a busy HM practice, with its higher patient volumes and a faster pace, can be daunting at first. Still, she tries to cultivate interest in initiatives and establish a realistic timeframe for involvement.
There are many reasons to consider this as a career step. Dr. Wright says that quality and patient safety dovetail with hospitalists’ initial reasons for choosing medicine: to improve patients’ lives.
Janet Nagamine, RN, MD, SFHM, former patient safety officer and assistant chief of quality at Kaiser Permanente in Santa Clara, Calif., describes the fit this way: “I might be a good doctor, but as a hospitalist, I rely on many others within the system to deliver, so my patients can’t get good care until the entire system is running well,” she says. “There are all kinds of opportunities to fix our [hospital] system, and I really believe that hospitalists cannot separate themselves from that engagement.”
Elizabeth Gundersen, MD, FHM, of Fort Lauderdale, Fla., agrees that it’s a natural step to think about the ways to make a difference on a larger level. At her former institution, the University of Massachusetts (UMass) Medical School in Worcester, she parlayed her interest in QI to work her way up from ground-level hospitalist to associate chief of her division and quality officer for the hospital. “Physicians get a lot of satisfaction from helping individual patients,” she says. “One thing I really liked about getting involved with quality improvement was being able to make a difference for patients on a systems level.”
An Incremental Path
The path to her current position began with a very specific issue for Dr. Nagamine, an SHM board member who also serves as a Project BOOST co-investigator. “Although I have been doing patient safety since before they had a name for it, I didn’t start out saying that I wanted a career in quality and safety,” she says. “I was trying to take better care of my patients with diabetes, but controlling their glucose was extremely challenging because all the related variables—timing and amount of their insulin dosage, when and how much they had eaten—were charted in different places. This made it hard to adjust their insulin appropriately.”
It quickly became clear to Dr. Nagamine that the solution had to be systemic. She realized that something as basic as taking care of her patients with diabetes required multiple departments (i.e. dietary, nursing, and pharmacy) to furnish information in an integrated manner. So she joined the diabetes committee and went to work on the issue. She helped devise a flow chart that could be used by all relevant departments. A further evolution on the path emanated from one of her patients receiving the wrong medication. She joined the medication safety committee, became chair, “and the next thing you know, I’m in charge of patient safety, and an assistant chief of quality.”
Training Is Necessary
QI and patient-safety methodologies have become sophisticated disciplines in the past two decades, Dr. Wright says. Access to training in QI basics now is readily available to early-career hospitalists. For example, CogentHMG offers program support for QI so that anyone interested “doesn’t have to start from scratch anymore; we can help show them the way and support them in doing it.”
This month, HM13 (www.hospital medicine2013.org)—just outside Washington, D.C.—will offer multiple sessions on quality, as well as the “Initiating Quality Improvement Projects with Built-In Sustainment” workshop, led by Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) core investigator Peter Kaboli, MD, MS, who will address sustainability.
Beyond methodological tools, success in quality and patient safety requires the ability to motivate people, often across multiple disciplines, Dr. Nagamine says. “If you want things to work better, you must invite the right people to the table. For example, we often forget to include key nonclinical stakeholders,” she adds.
When working with hospitals across the country to implement rapid-response tTeams, Dr. Nagamine often reminds them to invite the operators, or “key people,” in the process.
“If you put patient safety at the core of your initiative and create the context for that, most people will agree that it’s the right thing to do and will get on board, even if it’s an extra step for them,” she says. “Know your audience, listen to their perspective, and learn what matters to them. And to most people, it matters that they give good patient care.”
Gretchen Henkel is a freelance writer in California.
Drive Change in an ACO
From informal polls I’ve recently conducted of hospitalists, many are not even aware they are part of an accountable-care organization (ACO). And if they are aware, they might not be engaging in meaningful dialogue with ACO leaders about their role in these organizations. But, in the long term, ACOs will need to bring hospitalists to the table in order to be successful.
Are You Part of an ACO?
David Muhlestein, who blogs for Health Affairs, tracks the growth of ACOs around the country. He states that, as of Jan. 31, there were 428 ACOs in the U.S. (see Figure 1).1 In terms of numbers, Florida, Texas, and California lead the nation with 42, 33, and 46 ACOs, respectively. So it is likely that you are part of an ACO. If you are unsure, ask your chief medical officer or president of the medical staff.
How ACOs Work
All ACOs seek to manage a group, or population, of patients as efficiently as possible while maintaining or improving quality of care. For Medicare ACOs, the goal is to bring together hospitals and physicians in order to share savings derived from efficiencies in care. But before any savings can be shared, the Medicare ACO must demonstrate that it achieved high-quality care across four domains, totaling 33 individual quality measures. (see Table 1)
Main Flavors of ACOs
There are two types of ACOs: private ACOs and Medicare ACOs. Prior to Medicare ACOs, which were launched in January 2012, there were 150 private-sector ACOs, and this number continues to grow. Private ACOs represent a heterogeneous group in terms of reimbursement model. Some operate under shared savings programs; others use full or partial capitation, bundled payments, and/or other types of arrangements. But nearly all ACOs operate under the premise that the incentives used to make care more efficient and less costly can only be applied if measurable quality is maintained or improved. ACOs do not pay doctors or hospitals more unless high quality is demonstrated.
ACO Quality Measures and Hospitalists
Most of the 33 quality measures required by Medicare ACOs are based in ambulatory practice. These include measures related to blood pressure, immunizations, cancer, and fall-risk screening, and measures for diabetics, such as lipids and hemoglobin A1C. However, there are a few measures for which hospitalists should share in accountability, including:
- All-cause hospital readmission rate—risk-standardized;
- Ambulatory sensitive condition hospital admission rates (CHF, COPD); and
- Medication reconciliation after discharge from an inpatient facility.
Four Key Actions for Hospitalists
Hospitalists make a significant contribution to the quality and the financial performance of ACOs. In addition to the quality metrics cited above, hospitalists impact the inpatient portion of the overall population’s cost of care. Furthermore, hospitalists are vital partners in the care coordination required for an ACO to be successful.
Here are four actions I suggest taking in order for your hospitalist group to be effective as participants in an ACO:
- Have a representative from your group participate in ACO committees that address hospital utilization and related matters, such as care coordination impacting pre- and post-hospital care.
- Learn how to work with ACO case managers on care transitions, including post-discharge follow-up and information transfer.
- Understand an ACO’s approach to engagement of and coordination with post-acute-care facilities. The ability of a post-acute facility, such a skilled nursing facility, to accept patients who have complex care needs, to manage changes in condition in the facility when appropriate, and to send complete information upon transfer to the hospital are important strategies for an ACO’s success.
- Understand how an ACO reports quality and cost performance and how savings will be shared among participants.
Mindset Change
If hospitalists are part of the chain of ACO physicians and providers held accountable for the health of a population of patients, we must work more closely with the medical home/neighborhood, post-acute-care facilities, and home-care providers. The change in mindset will occur only if we have a set of tools to get the job done, such as case managers and information technology, and the appropriate incentives to support better care coordination. I encourage my fellow hospitalists to make things happen, instead of taking a passive role in this monumental transformation.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
From informal polls I’ve recently conducted of hospitalists, many are not even aware they are part of an accountable-care organization (ACO). And if they are aware, they might not be engaging in meaningful dialogue with ACO leaders about their role in these organizations. But, in the long term, ACOs will need to bring hospitalists to the table in order to be successful.
Are You Part of an ACO?
David Muhlestein, who blogs for Health Affairs, tracks the growth of ACOs around the country. He states that, as of Jan. 31, there were 428 ACOs in the U.S. (see Figure 1).1 In terms of numbers, Florida, Texas, and California lead the nation with 42, 33, and 46 ACOs, respectively. So it is likely that you are part of an ACO. If you are unsure, ask your chief medical officer or president of the medical staff.
How ACOs Work
All ACOs seek to manage a group, or population, of patients as efficiently as possible while maintaining or improving quality of care. For Medicare ACOs, the goal is to bring together hospitals and physicians in order to share savings derived from efficiencies in care. But before any savings can be shared, the Medicare ACO must demonstrate that it achieved high-quality care across four domains, totaling 33 individual quality measures. (see Table 1)
Main Flavors of ACOs
There are two types of ACOs: private ACOs and Medicare ACOs. Prior to Medicare ACOs, which were launched in January 2012, there were 150 private-sector ACOs, and this number continues to grow. Private ACOs represent a heterogeneous group in terms of reimbursement model. Some operate under shared savings programs; others use full or partial capitation, bundled payments, and/or other types of arrangements. But nearly all ACOs operate under the premise that the incentives used to make care more efficient and less costly can only be applied if measurable quality is maintained or improved. ACOs do not pay doctors or hospitals more unless high quality is demonstrated.
ACO Quality Measures and Hospitalists
Most of the 33 quality measures required by Medicare ACOs are based in ambulatory practice. These include measures related to blood pressure, immunizations, cancer, and fall-risk screening, and measures for diabetics, such as lipids and hemoglobin A1C. However, there are a few measures for which hospitalists should share in accountability, including:
- All-cause hospital readmission rate—risk-standardized;
- Ambulatory sensitive condition hospital admission rates (CHF, COPD); and
- Medication reconciliation after discharge from an inpatient facility.
Four Key Actions for Hospitalists
Hospitalists make a significant contribution to the quality and the financial performance of ACOs. In addition to the quality metrics cited above, hospitalists impact the inpatient portion of the overall population’s cost of care. Furthermore, hospitalists are vital partners in the care coordination required for an ACO to be successful.
Here are four actions I suggest taking in order for your hospitalist group to be effective as participants in an ACO:
- Have a representative from your group participate in ACO committees that address hospital utilization and related matters, such as care coordination impacting pre- and post-hospital care.
- Learn how to work with ACO case managers on care transitions, including post-discharge follow-up and information transfer.
- Understand an ACO’s approach to engagement of and coordination with post-acute-care facilities. The ability of a post-acute facility, such a skilled nursing facility, to accept patients who have complex care needs, to manage changes in condition in the facility when appropriate, and to send complete information upon transfer to the hospital are important strategies for an ACO’s success.
- Understand how an ACO reports quality and cost performance and how savings will be shared among participants.
Mindset Change
If hospitalists are part of the chain of ACO physicians and providers held accountable for the health of a population of patients, we must work more closely with the medical home/neighborhood, post-acute-care facilities, and home-care providers. The change in mindset will occur only if we have a set of tools to get the job done, such as case managers and information technology, and the appropriate incentives to support better care coordination. I encourage my fellow hospitalists to make things happen, instead of taking a passive role in this monumental transformation.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
From informal polls I’ve recently conducted of hospitalists, many are not even aware they are part of an accountable-care organization (ACO). And if they are aware, they might not be engaging in meaningful dialogue with ACO leaders about their role in these organizations. But, in the long term, ACOs will need to bring hospitalists to the table in order to be successful.
Are You Part of an ACO?
David Muhlestein, who blogs for Health Affairs, tracks the growth of ACOs around the country. He states that, as of Jan. 31, there were 428 ACOs in the U.S. (see Figure 1).1 In terms of numbers, Florida, Texas, and California lead the nation with 42, 33, and 46 ACOs, respectively. So it is likely that you are part of an ACO. If you are unsure, ask your chief medical officer or president of the medical staff.
How ACOs Work
All ACOs seek to manage a group, or population, of patients as efficiently as possible while maintaining or improving quality of care. For Medicare ACOs, the goal is to bring together hospitals and physicians in order to share savings derived from efficiencies in care. But before any savings can be shared, the Medicare ACO must demonstrate that it achieved high-quality care across four domains, totaling 33 individual quality measures. (see Table 1)
Main Flavors of ACOs
There are two types of ACOs: private ACOs and Medicare ACOs. Prior to Medicare ACOs, which were launched in January 2012, there were 150 private-sector ACOs, and this number continues to grow. Private ACOs represent a heterogeneous group in terms of reimbursement model. Some operate under shared savings programs; others use full or partial capitation, bundled payments, and/or other types of arrangements. But nearly all ACOs operate under the premise that the incentives used to make care more efficient and less costly can only be applied if measurable quality is maintained or improved. ACOs do not pay doctors or hospitals more unless high quality is demonstrated.
ACO Quality Measures and Hospitalists
Most of the 33 quality measures required by Medicare ACOs are based in ambulatory practice. These include measures related to blood pressure, immunizations, cancer, and fall-risk screening, and measures for diabetics, such as lipids and hemoglobin A1C. However, there are a few measures for which hospitalists should share in accountability, including:
- All-cause hospital readmission rate—risk-standardized;
- Ambulatory sensitive condition hospital admission rates (CHF, COPD); and
- Medication reconciliation after discharge from an inpatient facility.
Four Key Actions for Hospitalists
Hospitalists make a significant contribution to the quality and the financial performance of ACOs. In addition to the quality metrics cited above, hospitalists impact the inpatient portion of the overall population’s cost of care. Furthermore, hospitalists are vital partners in the care coordination required for an ACO to be successful.
Here are four actions I suggest taking in order for your hospitalist group to be effective as participants in an ACO:
- Have a representative from your group participate in ACO committees that address hospital utilization and related matters, such as care coordination impacting pre- and post-hospital care.
- Learn how to work with ACO case managers on care transitions, including post-discharge follow-up and information transfer.
- Understand an ACO’s approach to engagement of and coordination with post-acute-care facilities. The ability of a post-acute facility, such a skilled nursing facility, to accept patients who have complex care needs, to manage changes in condition in the facility when appropriate, and to send complete information upon transfer to the hospital are important strategies for an ACO’s success.
- Understand how an ACO reports quality and cost performance and how savings will be shared among participants.
Mindset Change
If hospitalists are part of the chain of ACO physicians and providers held accountable for the health of a population of patients, we must work more closely with the medical home/neighborhood, post-acute-care facilities, and home-care providers. The change in mindset will occur only if we have a set of tools to get the job done, such as case managers and information technology, and the appropriate incentives to support better care coordination. I encourage my fellow hospitalists to make things happen, instead of taking a passive role in this monumental transformation.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Larry Wellikson: Exceptional Hospitalists Bring Positive Change to Health Care Industry
Even though hospital medicine and SHM are still relatively young, we can be very proud of what our specialty already has brought to changing our nation’s health care for the better. Many of these accomplishments, from winning the prestigious Eisenberg Award to our change leadership by SHM’s Center for Healthcare Innovation and Improvement at more 300 hospitals to the extraordinary growth of our specialty, have been well chronicled in The Hospitalist and elsewhere the last few years.
I wanted to use this month’s column to highlight the unique career directions of a few SHM members to shine a bright light on the influence hospitalists are making nationwide. Certainly, there are many more hospitalists beyond this group of five that I have selected, but this small cadre should serve as an example of the talent and reach of our specialty—with only more and greater things ahead to come in the future.
Chief Medical Officer of CMS
Pat Conway, MD, SFHM, is a pediatric hospitalist and the former chair of SHM’s Public Policy Committee. He left his pediatric academic practice to become a White House fellow, then returned to Cincinnati Children’s Hospital to serve as chief medical officer (CMO). When Don Berwick was in charge of the Centers for Medicare & Medicaid Services (CMS), he reached out to Pat and asked him to come to Washington to be part of Medicare’s senior team as the CMO for CMS. In this role, Pat has been a nationally recognized leader in performance improvement and patient safety, and he has been instrumental in bringing about evolutionary changes to the largest healthcare program in the world. Pat will be sharing his perspectives as a keynote speaker at HM13 (check out our 10-page HM13 preview starting on p. 45).
Resident Fellow at the American Enterprise Institute
Scott Gottlieb, MD, is a practicing hospitalist in New York City, but he is better known as a leading expert in healthcare policy, most recently acting as an advisor to presidential candidate Mitt Romney. From 2005 to 2007, Scott was a deputy commissioner at the FDA. He has worked as a senior advisor to the administrator at CMS, where he played an instrumental role in the implementation of the Medicare Drug Benefit in 2004.
Scott is best known for his frequent contributions to The Wall Street Journal, The New York Times, USA Today, and Forbes. He has held editorial positions at the British Medical Journal and the Journal of the American Medical Association, regularly appears as a guest commentator on CNBC, and is a frequent contributor to Politico.
At SHM, Scott has brought his national viewpoint to the Public Policy Committee. He proudly touts his experience as a practicing hospitalist as bringing a front-line reality to his national recognition and much-sought-after critical thinking about healthcare policy.
Chairman of the American Board of Internal Medicine
Bob Wachter, MD, MHM, was a thought leader in HM before our specialty even had a name, writing the initial peer-reviewed articles and coining the term “hospitalist.” Bob has built a pre-eminent hospitalist program at the University of California at San Francisco and helped influence and populate much of academic HM. His Wachter’s World blog (www.wachtersworld.com) is one of the most widely read medical blogs, reaching an audience well beyond our specialty.
Bob was one of the first presidents of SHM—back when we were known as NAIP, or the National Association of Inpatient Physicians—and set SHM on its strong growth and innovative direction that has made us the envy of other medical specialty societies. Last year, Modern Healthcare hailed Bob as the 14th most influential physician executive in the entire country.
On the ABIM board, Bob has represented the best of HM and brought our innovative spirit and our commitment to improvement, safety, and change leadership, culminating this year in the ABIM chairmanship. Bob will offer his unique insights into HM and the national healthcare agenda at HM13 (www.hospitalmedicine 2013.org).
CEO: Telemedicine for the ICU
Mary Jo Gorman, MD, MHM, is a hospitalist and intensivist who made her mark on HM as the chief medical officer (CMO) of IPC: The Hospitalist Company. As she offered her talents to SHM, she became chairman of SHM’s Public Policy Committee and eventually SHM president.
For the last few years, Mary Jo has been the CEO of ICUMedicine. In this role, she has been active around the country, bringing ICU competencies to many community hospitals by offering a telemedicine solution for critically ill patients. This unconventional approach to meeting a glaring need fits into Mary Jo’s career history of looking for new and different ways to bring better healthcare solutions to the front lines of patient care. Last year, Modern Healthcare recognized Mary Jo as one of the most influential female physician executives in the country.
CEO, Medical University of South Carolina (MUSC) Hospitals
After leaving Duke University, Pat Cawley, MD, MBA, MHM, started his career as a community-based hospitalist leader. After a number of leadership roles at SHM, Pat served as SHM president and was elected a Master in Hospital Medicine in 2012.
Pat initially was recruited to MUSC to build and manage their HM group. Soon he was tapped to be the CMO at MUSC. Earlier this year, Pat became the first hospitalist to be chosen to run a major academic medical center when he was promoted to CEO at MUSC.
In recent years, Pat has been a leading voice as the American Hospital Association looks to involve physician leaders. He is a rising star at AHA, helping to merge the cultures of hospital administrators and physicians to create the hospital of the future.
Hospitalists Contribute at the Highest Level
Obviously, I could go on and on, adding other hospitalists who are making unique and important contributions at the local and national level. It is interesting that at a time when many are still trying to get their heads around just what HM is, we already can recognize the immense talent that resides in hospitalist groups across the country. At a time when the U.S. healthcare system is being reshaped, hospitalists, such as those mentioned above and oh-so-many more, are already making large and small steps forward. We are helping to create a new healthcare enterprise, based on value, efficiency, effectiveness, and putting the patient first.
SHM wants to continue to be the place where the innovators and thought leaders of today and tomorrow can come together to multiply their efforts. The challenges are daunting, but the results can be rewarding, and the members of SHM are ready to bring our talents, energies, and commitments to do our part in this great American journey.
Even though hospital medicine and SHM are still relatively young, we can be very proud of what our specialty already has brought to changing our nation’s health care for the better. Many of these accomplishments, from winning the prestigious Eisenberg Award to our change leadership by SHM’s Center for Healthcare Innovation and Improvement at more 300 hospitals to the extraordinary growth of our specialty, have been well chronicled in The Hospitalist and elsewhere the last few years.
I wanted to use this month’s column to highlight the unique career directions of a few SHM members to shine a bright light on the influence hospitalists are making nationwide. Certainly, there are many more hospitalists beyond this group of five that I have selected, but this small cadre should serve as an example of the talent and reach of our specialty—with only more and greater things ahead to come in the future.
Chief Medical Officer of CMS
Pat Conway, MD, SFHM, is a pediatric hospitalist and the former chair of SHM’s Public Policy Committee. He left his pediatric academic practice to become a White House fellow, then returned to Cincinnati Children’s Hospital to serve as chief medical officer (CMO). When Don Berwick was in charge of the Centers for Medicare & Medicaid Services (CMS), he reached out to Pat and asked him to come to Washington to be part of Medicare’s senior team as the CMO for CMS. In this role, Pat has been a nationally recognized leader in performance improvement and patient safety, and he has been instrumental in bringing about evolutionary changes to the largest healthcare program in the world. Pat will be sharing his perspectives as a keynote speaker at HM13 (check out our 10-page HM13 preview starting on p. 45).
Resident Fellow at the American Enterprise Institute
Scott Gottlieb, MD, is a practicing hospitalist in New York City, but he is better known as a leading expert in healthcare policy, most recently acting as an advisor to presidential candidate Mitt Romney. From 2005 to 2007, Scott was a deputy commissioner at the FDA. He has worked as a senior advisor to the administrator at CMS, where he played an instrumental role in the implementation of the Medicare Drug Benefit in 2004.
Scott is best known for his frequent contributions to The Wall Street Journal, The New York Times, USA Today, and Forbes. He has held editorial positions at the British Medical Journal and the Journal of the American Medical Association, regularly appears as a guest commentator on CNBC, and is a frequent contributor to Politico.
At SHM, Scott has brought his national viewpoint to the Public Policy Committee. He proudly touts his experience as a practicing hospitalist as bringing a front-line reality to his national recognition and much-sought-after critical thinking about healthcare policy.
Chairman of the American Board of Internal Medicine
Bob Wachter, MD, MHM, was a thought leader in HM before our specialty even had a name, writing the initial peer-reviewed articles and coining the term “hospitalist.” Bob has built a pre-eminent hospitalist program at the University of California at San Francisco and helped influence and populate much of academic HM. His Wachter’s World blog (www.wachtersworld.com) is one of the most widely read medical blogs, reaching an audience well beyond our specialty.
Bob was one of the first presidents of SHM—back when we were known as NAIP, or the National Association of Inpatient Physicians—and set SHM on its strong growth and innovative direction that has made us the envy of other medical specialty societies. Last year, Modern Healthcare hailed Bob as the 14th most influential physician executive in the entire country.
On the ABIM board, Bob has represented the best of HM and brought our innovative spirit and our commitment to improvement, safety, and change leadership, culminating this year in the ABIM chairmanship. Bob will offer his unique insights into HM and the national healthcare agenda at HM13 (www.hospitalmedicine 2013.org).
CEO: Telemedicine for the ICU
Mary Jo Gorman, MD, MHM, is a hospitalist and intensivist who made her mark on HM as the chief medical officer (CMO) of IPC: The Hospitalist Company. As she offered her talents to SHM, she became chairman of SHM’s Public Policy Committee and eventually SHM president.
For the last few years, Mary Jo has been the CEO of ICUMedicine. In this role, she has been active around the country, bringing ICU competencies to many community hospitals by offering a telemedicine solution for critically ill patients. This unconventional approach to meeting a glaring need fits into Mary Jo’s career history of looking for new and different ways to bring better healthcare solutions to the front lines of patient care. Last year, Modern Healthcare recognized Mary Jo as one of the most influential female physician executives in the country.
CEO, Medical University of South Carolina (MUSC) Hospitals
After leaving Duke University, Pat Cawley, MD, MBA, MHM, started his career as a community-based hospitalist leader. After a number of leadership roles at SHM, Pat served as SHM president and was elected a Master in Hospital Medicine in 2012.
Pat initially was recruited to MUSC to build and manage their HM group. Soon he was tapped to be the CMO at MUSC. Earlier this year, Pat became the first hospitalist to be chosen to run a major academic medical center when he was promoted to CEO at MUSC.
In recent years, Pat has been a leading voice as the American Hospital Association looks to involve physician leaders. He is a rising star at AHA, helping to merge the cultures of hospital administrators and physicians to create the hospital of the future.
Hospitalists Contribute at the Highest Level
Obviously, I could go on and on, adding other hospitalists who are making unique and important contributions at the local and national level. It is interesting that at a time when many are still trying to get their heads around just what HM is, we already can recognize the immense talent that resides in hospitalist groups across the country. At a time when the U.S. healthcare system is being reshaped, hospitalists, such as those mentioned above and oh-so-many more, are already making large and small steps forward. We are helping to create a new healthcare enterprise, based on value, efficiency, effectiveness, and putting the patient first.
SHM wants to continue to be the place where the innovators and thought leaders of today and tomorrow can come together to multiply their efforts. The challenges are daunting, but the results can be rewarding, and the members of SHM are ready to bring our talents, energies, and commitments to do our part in this great American journey.
Even though hospital medicine and SHM are still relatively young, we can be very proud of what our specialty already has brought to changing our nation’s health care for the better. Many of these accomplishments, from winning the prestigious Eisenberg Award to our change leadership by SHM’s Center for Healthcare Innovation and Improvement at more 300 hospitals to the extraordinary growth of our specialty, have been well chronicled in The Hospitalist and elsewhere the last few years.
I wanted to use this month’s column to highlight the unique career directions of a few SHM members to shine a bright light on the influence hospitalists are making nationwide. Certainly, there are many more hospitalists beyond this group of five that I have selected, but this small cadre should serve as an example of the talent and reach of our specialty—with only more and greater things ahead to come in the future.
Chief Medical Officer of CMS
Pat Conway, MD, SFHM, is a pediatric hospitalist and the former chair of SHM’s Public Policy Committee. He left his pediatric academic practice to become a White House fellow, then returned to Cincinnati Children’s Hospital to serve as chief medical officer (CMO). When Don Berwick was in charge of the Centers for Medicare & Medicaid Services (CMS), he reached out to Pat and asked him to come to Washington to be part of Medicare’s senior team as the CMO for CMS. In this role, Pat has been a nationally recognized leader in performance improvement and patient safety, and he has been instrumental in bringing about evolutionary changes to the largest healthcare program in the world. Pat will be sharing his perspectives as a keynote speaker at HM13 (check out our 10-page HM13 preview starting on p. 45).
Resident Fellow at the American Enterprise Institute
Scott Gottlieb, MD, is a practicing hospitalist in New York City, but he is better known as a leading expert in healthcare policy, most recently acting as an advisor to presidential candidate Mitt Romney. From 2005 to 2007, Scott was a deputy commissioner at the FDA. He has worked as a senior advisor to the administrator at CMS, where he played an instrumental role in the implementation of the Medicare Drug Benefit in 2004.
Scott is best known for his frequent contributions to The Wall Street Journal, The New York Times, USA Today, and Forbes. He has held editorial positions at the British Medical Journal and the Journal of the American Medical Association, regularly appears as a guest commentator on CNBC, and is a frequent contributor to Politico.
At SHM, Scott has brought his national viewpoint to the Public Policy Committee. He proudly touts his experience as a practicing hospitalist as bringing a front-line reality to his national recognition and much-sought-after critical thinking about healthcare policy.
Chairman of the American Board of Internal Medicine
Bob Wachter, MD, MHM, was a thought leader in HM before our specialty even had a name, writing the initial peer-reviewed articles and coining the term “hospitalist.” Bob has built a pre-eminent hospitalist program at the University of California at San Francisco and helped influence and populate much of academic HM. His Wachter’s World blog (www.wachtersworld.com) is one of the most widely read medical blogs, reaching an audience well beyond our specialty.
Bob was one of the first presidents of SHM—back when we were known as NAIP, or the National Association of Inpatient Physicians—and set SHM on its strong growth and innovative direction that has made us the envy of other medical specialty societies. Last year, Modern Healthcare hailed Bob as the 14th most influential physician executive in the entire country.
On the ABIM board, Bob has represented the best of HM and brought our innovative spirit and our commitment to improvement, safety, and change leadership, culminating this year in the ABIM chairmanship. Bob will offer his unique insights into HM and the national healthcare agenda at HM13 (www.hospitalmedicine 2013.org).
CEO: Telemedicine for the ICU
Mary Jo Gorman, MD, MHM, is a hospitalist and intensivist who made her mark on HM as the chief medical officer (CMO) of IPC: The Hospitalist Company. As she offered her talents to SHM, she became chairman of SHM’s Public Policy Committee and eventually SHM president.
For the last few years, Mary Jo has been the CEO of ICUMedicine. In this role, she has been active around the country, bringing ICU competencies to many community hospitals by offering a telemedicine solution for critically ill patients. This unconventional approach to meeting a glaring need fits into Mary Jo’s career history of looking for new and different ways to bring better healthcare solutions to the front lines of patient care. Last year, Modern Healthcare recognized Mary Jo as one of the most influential female physician executives in the country.
CEO, Medical University of South Carolina (MUSC) Hospitals
After leaving Duke University, Pat Cawley, MD, MBA, MHM, started his career as a community-based hospitalist leader. After a number of leadership roles at SHM, Pat served as SHM president and was elected a Master in Hospital Medicine in 2012.
Pat initially was recruited to MUSC to build and manage their HM group. Soon he was tapped to be the CMO at MUSC. Earlier this year, Pat became the first hospitalist to be chosen to run a major academic medical center when he was promoted to CEO at MUSC.
In recent years, Pat has been a leading voice as the American Hospital Association looks to involve physician leaders. He is a rising star at AHA, helping to merge the cultures of hospital administrators and physicians to create the hospital of the future.
Hospitalists Contribute at the Highest Level
Obviously, I could go on and on, adding other hospitalists who are making unique and important contributions at the local and national level. It is interesting that at a time when many are still trying to get their heads around just what HM is, we already can recognize the immense talent that resides in hospitalist groups across the country. At a time when the U.S. healthcare system is being reshaped, hospitalists, such as those mentioned above and oh-so-many more, are already making large and small steps forward. We are helping to create a new healthcare enterprise, based on value, efficiency, effectiveness, and putting the patient first.
SHM wants to continue to be the place where the innovators and thought leaders of today and tomorrow can come together to multiply their efforts. The challenges are daunting, but the results can be rewarding, and the members of SHM are ready to bring our talents, energies, and commitments to do our part in this great American journey.
UCLA Exec: Patient-Centered Approach Essential to Quality of Hospital Care

–David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles
Patient satisfaction is a buzzword in HM circles, as compensation is increasingly tied to performance in keeping inpatients happy. David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles, could be called a guru of patient satisfaction.
Just don’t tell him that.
“I hope I’m not seen as ‘patient satisfaction,’” he says. “I hope I’m seen as ‘patient centeredness.’ And patient satisfaction is a key piece of patient centeredness.”
Dr. Feinberg, who assumed his current role UCLA Health System in 2011, is a national voice for pushing a patient-centric model of care delivery. To wit, he will be one of the keynote speakers at HM13 next month at the Gaylord National Resort & Convention Center in National Harbor, Md. His address is fittingly titled “Healing Humankind One Patient at a Time.”
The Hospitalist spoke to Dr. Feinberg about his message to hospitalists.
Question: What do you think is the evolution of patient centeredness, as that becomes more of a focus for others?
Answer: Patient centeredness to me is the true north, and I think everything else that we’ve done that isn’t patient-centered has been a distraction. … It’s why we signed up to get into healthcare. It’s what we should be doing today and tonight, and it should guide our future tomorrow. It would be like me saying to the restaurateur, “How important is the food?”
Q: Is it something that hasn’t always been done?
A: It’s pathetic. You’re totally right. We’ve lost our way.
Q: If it’s so common-sense, how did we lose our way?
A: It really became, to me, the coin of the realm in medicine was how much the doctor made, how great their reputation was. It even got to the point of: You were a good doctor if your waiting room was packed. … I keep saying the waiting room should be for the doctors. The patient shouldn’t have to wait. You should be back in the exam room and the doctor should be waiting to see you. So we’ve got to completely change the paradigm. … It’s really the patient who’s at the top of the pyramid. And I just think we’ve lost that completely.
Q: How does a hospitalist engage quickly to ensure that they’re trying to accomplish patient centeredness and manage outcomes properly?
A: Hospitalists have a unique opportunity there, because everybody remembers when they got put in the hospital. It is a big deal when you’re hospitalized. Your family is in a vulnerable state, everybody is in a heightened sense of alertness and focus. Think about how important those four days are around education, around myths and demystifying, around beliefs and disbelief.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Q: So what is the one thing you want hospitalists to take away from your address?
A: That they should join with all of us who want to heal humankind; that they are healers, above all.
Q: How do you translate “I want to be a healer” to the grind of daily work?
A: Well, I don’t think this is a grind. I think that when you’re in this healing profession, that you come here with a purpose. I think if we asked them to look at their personal statements of why they went into med school, every single one of them has something to do with, “I was sick as a kid, my grandmother got sick, I had had this doctor who was a role model, I like to help people, I was a volunteer and I met this patient.” Everyone says that. So this is different than trying to inspire the workers at Costco. These are people that, by definition, have gone and chosen this. We know they’re all smart. They could have all become investment bankers, they could have all become schoolteachers, but what they chose was to go into this field that’s about healing others, and that’s what I think we need to and what I would want them to do, is to get back in touch with themselves because I know it’s there. By definition, it’s there.
Q: Then why don’t more people just make that connection? What is the hurdle?
A: There are a lot of distractions. There are a lot of things coming your way. Worrying about your own life; doctors have lives at home. Worrying about the pressures of making a living. Some of this stuff is really, really hard. There are a million things going on. I believe, and I hope at UCLA, that we believe the strategy to make all of that stuff work is to get it right with the patient. And if you get it right with the patient, then all of that other stuff seems to fall into place and starts to make sense. The finances work out. The market share works out. The healthcare reform works out. I think it is the answer.
Richard Quinn is a freelance writer in New Jersey.

–David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles
Patient satisfaction is a buzzword in HM circles, as compensation is increasingly tied to performance in keeping inpatients happy. David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles, could be called a guru of patient satisfaction.
Just don’t tell him that.
“I hope I’m not seen as ‘patient satisfaction,’” he says. “I hope I’m seen as ‘patient centeredness.’ And patient satisfaction is a key piece of patient centeredness.”
Dr. Feinberg, who assumed his current role UCLA Health System in 2011, is a national voice for pushing a patient-centric model of care delivery. To wit, he will be one of the keynote speakers at HM13 next month at the Gaylord National Resort & Convention Center in National Harbor, Md. His address is fittingly titled “Healing Humankind One Patient at a Time.”
The Hospitalist spoke to Dr. Feinberg about his message to hospitalists.
Question: What do you think is the evolution of patient centeredness, as that becomes more of a focus for others?
Answer: Patient centeredness to me is the true north, and I think everything else that we’ve done that isn’t patient-centered has been a distraction. … It’s why we signed up to get into healthcare. It’s what we should be doing today and tonight, and it should guide our future tomorrow. It would be like me saying to the restaurateur, “How important is the food?”
Q: Is it something that hasn’t always been done?
A: It’s pathetic. You’re totally right. We’ve lost our way.
Q: If it’s so common-sense, how did we lose our way?
A: It really became, to me, the coin of the realm in medicine was how much the doctor made, how great their reputation was. It even got to the point of: You were a good doctor if your waiting room was packed. … I keep saying the waiting room should be for the doctors. The patient shouldn’t have to wait. You should be back in the exam room and the doctor should be waiting to see you. So we’ve got to completely change the paradigm. … It’s really the patient who’s at the top of the pyramid. And I just think we’ve lost that completely.
Q: How does a hospitalist engage quickly to ensure that they’re trying to accomplish patient centeredness and manage outcomes properly?
A: Hospitalists have a unique opportunity there, because everybody remembers when they got put in the hospital. It is a big deal when you’re hospitalized. Your family is in a vulnerable state, everybody is in a heightened sense of alertness and focus. Think about how important those four days are around education, around myths and demystifying, around beliefs and disbelief.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Q: So what is the one thing you want hospitalists to take away from your address?
A: That they should join with all of us who want to heal humankind; that they are healers, above all.
Q: How do you translate “I want to be a healer” to the grind of daily work?
A: Well, I don’t think this is a grind. I think that when you’re in this healing profession, that you come here with a purpose. I think if we asked them to look at their personal statements of why they went into med school, every single one of them has something to do with, “I was sick as a kid, my grandmother got sick, I had had this doctor who was a role model, I like to help people, I was a volunteer and I met this patient.” Everyone says that. So this is different than trying to inspire the workers at Costco. These are people that, by definition, have gone and chosen this. We know they’re all smart. They could have all become investment bankers, they could have all become schoolteachers, but what they chose was to go into this field that’s about healing others, and that’s what I think we need to and what I would want them to do, is to get back in touch with themselves because I know it’s there. By definition, it’s there.
Q: Then why don’t more people just make that connection? What is the hurdle?
A: There are a lot of distractions. There are a lot of things coming your way. Worrying about your own life; doctors have lives at home. Worrying about the pressures of making a living. Some of this stuff is really, really hard. There are a million things going on. I believe, and I hope at UCLA, that we believe the strategy to make all of that stuff work is to get it right with the patient. And if you get it right with the patient, then all of that other stuff seems to fall into place and starts to make sense. The finances work out. The market share works out. The healthcare reform works out. I think it is the answer.
Richard Quinn is a freelance writer in New Jersey.

–David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles
Patient satisfaction is a buzzword in HM circles, as compensation is increasingly tied to performance in keeping inpatients happy. David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles, could be called a guru of patient satisfaction.
Just don’t tell him that.
“I hope I’m not seen as ‘patient satisfaction,’” he says. “I hope I’m seen as ‘patient centeredness.’ And patient satisfaction is a key piece of patient centeredness.”
Dr. Feinberg, who assumed his current role UCLA Health System in 2011, is a national voice for pushing a patient-centric model of care delivery. To wit, he will be one of the keynote speakers at HM13 next month at the Gaylord National Resort & Convention Center in National Harbor, Md. His address is fittingly titled “Healing Humankind One Patient at a Time.”
The Hospitalist spoke to Dr. Feinberg about his message to hospitalists.
Question: What do you think is the evolution of patient centeredness, as that becomes more of a focus for others?
Answer: Patient centeredness to me is the true north, and I think everything else that we’ve done that isn’t patient-centered has been a distraction. … It’s why we signed up to get into healthcare. It’s what we should be doing today and tonight, and it should guide our future tomorrow. It would be like me saying to the restaurateur, “How important is the food?”
Q: Is it something that hasn’t always been done?
A: It’s pathetic. You’re totally right. We’ve lost our way.
Q: If it’s so common-sense, how did we lose our way?
A: It really became, to me, the coin of the realm in medicine was how much the doctor made, how great their reputation was. It even got to the point of: You were a good doctor if your waiting room was packed. … I keep saying the waiting room should be for the doctors. The patient shouldn’t have to wait. You should be back in the exam room and the doctor should be waiting to see you. So we’ve got to completely change the paradigm. … It’s really the patient who’s at the top of the pyramid. And I just think we’ve lost that completely.
Q: How does a hospitalist engage quickly to ensure that they’re trying to accomplish patient centeredness and manage outcomes properly?
A: Hospitalists have a unique opportunity there, because everybody remembers when they got put in the hospital. It is a big deal when you’re hospitalized. Your family is in a vulnerable state, everybody is in a heightened sense of alertness and focus. Think about how important those four days are around education, around myths and demystifying, around beliefs and disbelief.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Q: So what is the one thing you want hospitalists to take away from your address?
A: That they should join with all of us who want to heal humankind; that they are healers, above all.
Q: How do you translate “I want to be a healer” to the grind of daily work?
A: Well, I don’t think this is a grind. I think that when you’re in this healing profession, that you come here with a purpose. I think if we asked them to look at their personal statements of why they went into med school, every single one of them has something to do with, “I was sick as a kid, my grandmother got sick, I had had this doctor who was a role model, I like to help people, I was a volunteer and I met this patient.” Everyone says that. So this is different than trying to inspire the workers at Costco. These are people that, by definition, have gone and chosen this. We know they’re all smart. They could have all become investment bankers, they could have all become schoolteachers, but what they chose was to go into this field that’s about healing others, and that’s what I think we need to and what I would want them to do, is to get back in touch with themselves because I know it’s there. By definition, it’s there.
Q: Then why don’t more people just make that connection? What is the hurdle?
A: There are a lot of distractions. There are a lot of things coming your way. Worrying about your own life; doctors have lives at home. Worrying about the pressures of making a living. Some of this stuff is really, really hard. There are a million things going on. I believe, and I hope at UCLA, that we believe the strategy to make all of that stuff work is to get it right with the patient. And if you get it right with the patient, then all of that other stuff seems to fall into place and starts to make sense. The finances work out. The market share works out. The healthcare reform works out. I think it is the answer.
Richard Quinn is a freelance writer in New Jersey.
Medicare CMO Encourages Hospitalists to Become Experts in Managing Quality Patient Care

–Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer, Centers for Medicaid & Medicare Service
Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer of the Centers for Medicaid & Medicare Services (CMS), often says that physicians need to come to the proverbial table to tell CMS what they think is best. So it’s fitting that at HM13 at the Gaylord National Resort & Convention Center in National Harbor, Md., Dr. Conway will be a keynote speaker who can deliver his message of quality through teamwork to more than 2,500 hospitalists.
A pediatric hospitalist who also serves as director of the Office of Clinical Standards and Quality at the U.S. Department of Health and Human Services in Washington, D.C., Dr. Conway will paint a picture of what hospitalists can do to become the quality-improvement (QI) leaders healthcare needs in the coming years in a presentation titled “The Ideal Hospitalist in 2014 and Beyond: Active Change Agent.”
“Are hospitalists going to accept that challenge?” he asks. “I hope they are.”
This is the second year in a row that Dr. Conway will be a plenary speaker. Last year in San Diego, he told a packed room that CMS had to move from a “passive payor to an active facilitator and catalyst for quality improvement,” says Danielle Scheurer, MD, MSCR, SFHM, physician editor of The Hospitalist. Or, in his own words: “better health, better care, and lower cost.”
But many of the issues in his 2012 commentary were in flux. The Affordable Care Act (ACA), now moving through the slow process of implementation, was then still a law very much in doubt. It wasn’t until last summer that the law was upheld by a bitterly divided U.S. Supreme Court and it became clear much of the proposed reforms would move forward.
This year, he will urge hospitalists to step up their focus on patient-centered outcomes and stop questioning whether that should be the way the HM and other physicians should be judged.
“Given the changing context of payment, hospitalists are going to have to become true experts in managing the quality of care,” Dr. Conway says. “The days of you just graduating residency, seeing as many patients as you can, and you go home at the end of the day—that’s gone for hospital medicine.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Hospitalists can take charge of quality initiatives via involvement with accountable-care organizations (ACOs), health exchanges, and CMS’ value-based purchasing modifier (VBPM). In part, HM is perfectly positioned to assume leadership roles over the next few years because hospitalists already work across multiple departments.
“Hospital medicine is already ahead of a lot of specialties,” Dr. Conway says. “Hospital medicine physicians are already taking on much larger roles in their systems. I think you’re going to see an increasing trend.”
Richard Quinn is a freelance writer in New Jersey.

–Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer, Centers for Medicaid & Medicare Service
Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer of the Centers for Medicaid & Medicare Services (CMS), often says that physicians need to come to the proverbial table to tell CMS what they think is best. So it’s fitting that at HM13 at the Gaylord National Resort & Convention Center in National Harbor, Md., Dr. Conway will be a keynote speaker who can deliver his message of quality through teamwork to more than 2,500 hospitalists.
A pediatric hospitalist who also serves as director of the Office of Clinical Standards and Quality at the U.S. Department of Health and Human Services in Washington, D.C., Dr. Conway will paint a picture of what hospitalists can do to become the quality-improvement (QI) leaders healthcare needs in the coming years in a presentation titled “The Ideal Hospitalist in 2014 and Beyond: Active Change Agent.”
“Are hospitalists going to accept that challenge?” he asks. “I hope they are.”
This is the second year in a row that Dr. Conway will be a plenary speaker. Last year in San Diego, he told a packed room that CMS had to move from a “passive payor to an active facilitator and catalyst for quality improvement,” says Danielle Scheurer, MD, MSCR, SFHM, physician editor of The Hospitalist. Or, in his own words: “better health, better care, and lower cost.”
But many of the issues in his 2012 commentary were in flux. The Affordable Care Act (ACA), now moving through the slow process of implementation, was then still a law very much in doubt. It wasn’t until last summer that the law was upheld by a bitterly divided U.S. Supreme Court and it became clear much of the proposed reforms would move forward.
This year, he will urge hospitalists to step up their focus on patient-centered outcomes and stop questioning whether that should be the way the HM and other physicians should be judged.
“Given the changing context of payment, hospitalists are going to have to become true experts in managing the quality of care,” Dr. Conway says. “The days of you just graduating residency, seeing as many patients as you can, and you go home at the end of the day—that’s gone for hospital medicine.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Hospitalists can take charge of quality initiatives via involvement with accountable-care organizations (ACOs), health exchanges, and CMS’ value-based purchasing modifier (VBPM). In part, HM is perfectly positioned to assume leadership roles over the next few years because hospitalists already work across multiple departments.
“Hospital medicine is already ahead of a lot of specialties,” Dr. Conway says. “Hospital medicine physicians are already taking on much larger roles in their systems. I think you’re going to see an increasing trend.”
Richard Quinn is a freelance writer in New Jersey.

–Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer, Centers for Medicaid & Medicare Service
Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer of the Centers for Medicaid & Medicare Services (CMS), often says that physicians need to come to the proverbial table to tell CMS what they think is best. So it’s fitting that at HM13 at the Gaylord National Resort & Convention Center in National Harbor, Md., Dr. Conway will be a keynote speaker who can deliver his message of quality through teamwork to more than 2,500 hospitalists.
A pediatric hospitalist who also serves as director of the Office of Clinical Standards and Quality at the U.S. Department of Health and Human Services in Washington, D.C., Dr. Conway will paint a picture of what hospitalists can do to become the quality-improvement (QI) leaders healthcare needs in the coming years in a presentation titled “The Ideal Hospitalist in 2014 and Beyond: Active Change Agent.”
“Are hospitalists going to accept that challenge?” he asks. “I hope they are.”
This is the second year in a row that Dr. Conway will be a plenary speaker. Last year in San Diego, he told a packed room that CMS had to move from a “passive payor to an active facilitator and catalyst for quality improvement,” says Danielle Scheurer, MD, MSCR, SFHM, physician editor of The Hospitalist. Or, in his own words: “better health, better care, and lower cost.”
But many of the issues in his 2012 commentary were in flux. The Affordable Care Act (ACA), now moving through the slow process of implementation, was then still a law very much in doubt. It wasn’t until last summer that the law was upheld by a bitterly divided U.S. Supreme Court and it became clear much of the proposed reforms would move forward.
This year, he will urge hospitalists to step up their focus on patient-centered outcomes and stop questioning whether that should be the way the HM and other physicians should be judged.
“Given the changing context of payment, hospitalists are going to have to become true experts in managing the quality of care,” Dr. Conway says. “The days of you just graduating residency, seeing as many patients as you can, and you go home at the end of the day—that’s gone for hospital medicine.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Hospitalists can take charge of quality initiatives via involvement with accountable-care organizations (ACOs), health exchanges, and CMS’ value-based purchasing modifier (VBPM). In part, HM is perfectly positioned to assume leadership roles over the next few years because hospitalists already work across multiple departments.
“Hospital medicine is already ahead of a lot of specialties,” Dr. Conway says. “Hospital medicine physicians are already taking on much larger roles in their systems. I think you’re going to see an increasing trend.”
Richard Quinn is a freelance writer in New Jersey.