User login
Ribavirin boosts HCV genotype 3 eradication in compensated cirrhotic patients
VIENNA – In patients with compensated cirrhosis infected with genotype 3 hepatitis C virus, adding ribavirin to a usual antiviral regimen of sofosbuvir and velpatasvir significantly boosted the rate of sustained virologic response in a review of more than 14,000 English residents entered in a national registry starting in 2017.
With ribavirin added to a sofosbuvir plus velpatasvir regimen for 12 weeks of treatment, the three-drug combination produced a 98% rate of sustained virologic response after 12 weeks (SVR12) in 196 treated patients, Kate Drysdale, MBBCh, said at the meeting sponsored by the European Association for the Study of the Liver. In contrast, 218 compensated cirrhosis patients who received a 12-week regimen of sofosbuvir plus velpatasvir (Epclusa) but without ribavirin had an SVR12 rate of just under 92%, a statistically significant difference, compared with the rate among patients who also received ribavirin, said Dr. Drysdale, a gastroenterologist at Bart’s Health and Queen Mary University of London. The SVR12 rate among 167 compensated cirrhotic patients treated for 12 weeks with the combination of glecaprevir plus pibrentasvir (Mavyret) was 96%, and not statistically different from the patients who received three drugs including ribavirin. The sofosbuvir, velpatasvir, ribavirin combination also outperformed the combination of sofosbuvir plus daclatasvir (Daklinza) and ribavirin, which produced an SVR12 of 92% in 868 patients. The SVR12 rate is the percentage of patients with undetectable hepatitis C virus (HCV) 12 or more weeks after the end of treatment.
Dr. Drysdale cautioned that the data have not yet been put through a multivariate analysis, but the results so far provide “a strong indication that ribavirin may not be as insignificant” as many have recently presumed. “Ribavirin has been set aside because it was thought not to add to the SVR12, but if patients get only one go at treatment, we must be sure their first treatment is the best one,” Dr. Drysdale said in an interview. If ribavirin can be shown to make a significant contribution to treatment efficacy “then we should think more widely about using it when patients tolerate it.”
The analysis included too few patients with either current decompensated cirrhosis or a history of decompensated cirrhosis to make any statistically meaningful comparisons of the treatment subgroups among these patients. And among patients with genotype 3 HCV infection and without cirrhosis, none of the treatments used in practice showed any statistically significant differences in the SVR12 rates they produced. Among patients without cirrhosis the most commonly used regimens by far were an 8-week course of glecaprevir plus pibrentasvir in 731 patients or a 12-week course of sofosbuvir plus velpatasvir in 1,184 patients. Both regimens had SVR12 rates in noncirrhotic patients of 97%, regardless of whether patients had no, mild, or moderate liver fibrosis.
The study used data collected in an English national registry of HCV-infected patients treated with direct-acting antiviral drugs starting in 2017. Dr. Drysdale and her associates narrowed down the total database of more than 37,000 English adults who received some HCV therapy during the period to 14,603 who received a complete, valid regimen and had follow-up SVR12 information available. The overall SVR12 rate among all these patients was 95.59%, and among the patients infected by genotype 3 virus the SVR12 rate was 95.03%. Dr. Drysdale’s analysis focused primarily on the roughly one-third of patients in the study group infected with genotype 3 HCV, the genotype that historically has presented unique treatment challenges (Drugs. 2017 Feb;77[2]:131-44).
Another finding Dr. Drysdale reported was that as liver disease severity worsened from no fibrosis to mild or moderate fibrosis, and then to compensated cirrhosis or decompensation, the SVR12 rate steadily diminished. Among genotype 3 patients, the SVR12 rate fell from about 97% among patients without any fibrosis to about 87% among those with decompensated cirrhosis. Although this observation had been made before, this finding in such a large number of treated patients adds significant new evidence to support this pattern. It also adds further support to the idea of screening for HCV infection among higher-risk, asymptomatic people to optimize their prospects for virus eradication with treatment.
“If patients get much better treatment outcomes before they become cirrhotic then we should try to find these HCV-infected people before they develop symptoms,” Dr. Drysdale said.
Dr. Drysdale reported no disclosures.
SOURCE: Drysdale K et al. J Hepatol. 2019 April;70(1):e131.
The results from Dr. Drysdale’s analysis confirm what had previously been proposed by other investigators that, in a subgroup of patients with cirrhosis and infected with hepatitis C virus (HCV) genotype 3, adding ribavirin to a regimen of direct-acting antiviral drugs can increase efficacy. But the new study included no data to address the prevalence of HCV genetic variants with resistance mutations that necessitate adding ribavirin. We have known that, in patients with cirrhosis and infected with resistant genotype 3 HCV, adding ribavirin is necessary. In many locations resistance testing is not possible; in those circumstances, adding ribavirin to the treatment should be routinely done.
Thomas Berg, MD, is professor and head of hepatology at University Hospital in Leipzig, Germany. He has received personal fees and research support from several companies. He made these comments in an interview.
The results from Dr. Drysdale’s analysis confirm what had previously been proposed by other investigators that, in a subgroup of patients with cirrhosis and infected with hepatitis C virus (HCV) genotype 3, adding ribavirin to a regimen of direct-acting antiviral drugs can increase efficacy. But the new study included no data to address the prevalence of HCV genetic variants with resistance mutations that necessitate adding ribavirin. We have known that, in patients with cirrhosis and infected with resistant genotype 3 HCV, adding ribavirin is necessary. In many locations resistance testing is not possible; in those circumstances, adding ribavirin to the treatment should be routinely done.
Thomas Berg, MD, is professor and head of hepatology at University Hospital in Leipzig, Germany. He has received personal fees and research support from several companies. He made these comments in an interview.
The results from Dr. Drysdale’s analysis confirm what had previously been proposed by other investigators that, in a subgroup of patients with cirrhosis and infected with hepatitis C virus (HCV) genotype 3, adding ribavirin to a regimen of direct-acting antiviral drugs can increase efficacy. But the new study included no data to address the prevalence of HCV genetic variants with resistance mutations that necessitate adding ribavirin. We have known that, in patients with cirrhosis and infected with resistant genotype 3 HCV, adding ribavirin is necessary. In many locations resistance testing is not possible; in those circumstances, adding ribavirin to the treatment should be routinely done.
Thomas Berg, MD, is professor and head of hepatology at University Hospital in Leipzig, Germany. He has received personal fees and research support from several companies. He made these comments in an interview.
VIENNA – In patients with compensated cirrhosis infected with genotype 3 hepatitis C virus, adding ribavirin to a usual antiviral regimen of sofosbuvir and velpatasvir significantly boosted the rate of sustained virologic response in a review of more than 14,000 English residents entered in a national registry starting in 2017.
With ribavirin added to a sofosbuvir plus velpatasvir regimen for 12 weeks of treatment, the three-drug combination produced a 98% rate of sustained virologic response after 12 weeks (SVR12) in 196 treated patients, Kate Drysdale, MBBCh, said at the meeting sponsored by the European Association for the Study of the Liver. In contrast, 218 compensated cirrhosis patients who received a 12-week regimen of sofosbuvir plus velpatasvir (Epclusa) but without ribavirin had an SVR12 rate of just under 92%, a statistically significant difference, compared with the rate among patients who also received ribavirin, said Dr. Drysdale, a gastroenterologist at Bart’s Health and Queen Mary University of London. The SVR12 rate among 167 compensated cirrhotic patients treated for 12 weeks with the combination of glecaprevir plus pibrentasvir (Mavyret) was 96%, and not statistically different from the patients who received three drugs including ribavirin. The sofosbuvir, velpatasvir, ribavirin combination also outperformed the combination of sofosbuvir plus daclatasvir (Daklinza) and ribavirin, which produced an SVR12 of 92% in 868 patients. The SVR12 rate is the percentage of patients with undetectable hepatitis C virus (HCV) 12 or more weeks after the end of treatment.
Dr. Drysdale cautioned that the data have not yet been put through a multivariate analysis, but the results so far provide “a strong indication that ribavirin may not be as insignificant” as many have recently presumed. “Ribavirin has been set aside because it was thought not to add to the SVR12, but if patients get only one go at treatment, we must be sure their first treatment is the best one,” Dr. Drysdale said in an interview. If ribavirin can be shown to make a significant contribution to treatment efficacy “then we should think more widely about using it when patients tolerate it.”
The analysis included too few patients with either current decompensated cirrhosis or a history of decompensated cirrhosis to make any statistically meaningful comparisons of the treatment subgroups among these patients. And among patients with genotype 3 HCV infection and without cirrhosis, none of the treatments used in practice showed any statistically significant differences in the SVR12 rates they produced. Among patients without cirrhosis the most commonly used regimens by far were an 8-week course of glecaprevir plus pibrentasvir in 731 patients or a 12-week course of sofosbuvir plus velpatasvir in 1,184 patients. Both regimens had SVR12 rates in noncirrhotic patients of 97%, regardless of whether patients had no, mild, or moderate liver fibrosis.
The study used data collected in an English national registry of HCV-infected patients treated with direct-acting antiviral drugs starting in 2017. Dr. Drysdale and her associates narrowed down the total database of more than 37,000 English adults who received some HCV therapy during the period to 14,603 who received a complete, valid regimen and had follow-up SVR12 information available. The overall SVR12 rate among all these patients was 95.59%, and among the patients infected by genotype 3 virus the SVR12 rate was 95.03%. Dr. Drysdale’s analysis focused primarily on the roughly one-third of patients in the study group infected with genotype 3 HCV, the genotype that historically has presented unique treatment challenges (Drugs. 2017 Feb;77[2]:131-44).
Another finding Dr. Drysdale reported was that as liver disease severity worsened from no fibrosis to mild or moderate fibrosis, and then to compensated cirrhosis or decompensation, the SVR12 rate steadily diminished. Among genotype 3 patients, the SVR12 rate fell from about 97% among patients without any fibrosis to about 87% among those with decompensated cirrhosis. Although this observation had been made before, this finding in such a large number of treated patients adds significant new evidence to support this pattern. It also adds further support to the idea of screening for HCV infection among higher-risk, asymptomatic people to optimize their prospects for virus eradication with treatment.
“If patients get much better treatment outcomes before they become cirrhotic then we should try to find these HCV-infected people before they develop symptoms,” Dr. Drysdale said.
Dr. Drysdale reported no disclosures.
SOURCE: Drysdale K et al. J Hepatol. 2019 April;70(1):e131.
VIENNA – In patients with compensated cirrhosis infected with genotype 3 hepatitis C virus, adding ribavirin to a usual antiviral regimen of sofosbuvir and velpatasvir significantly boosted the rate of sustained virologic response in a review of more than 14,000 English residents entered in a national registry starting in 2017.
With ribavirin added to a sofosbuvir plus velpatasvir regimen for 12 weeks of treatment, the three-drug combination produced a 98% rate of sustained virologic response after 12 weeks (SVR12) in 196 treated patients, Kate Drysdale, MBBCh, said at the meeting sponsored by the European Association for the Study of the Liver. In contrast, 218 compensated cirrhosis patients who received a 12-week regimen of sofosbuvir plus velpatasvir (Epclusa) but without ribavirin had an SVR12 rate of just under 92%, a statistically significant difference, compared with the rate among patients who also received ribavirin, said Dr. Drysdale, a gastroenterologist at Bart’s Health and Queen Mary University of London. The SVR12 rate among 167 compensated cirrhotic patients treated for 12 weeks with the combination of glecaprevir plus pibrentasvir (Mavyret) was 96%, and not statistically different from the patients who received three drugs including ribavirin. The sofosbuvir, velpatasvir, ribavirin combination also outperformed the combination of sofosbuvir plus daclatasvir (Daklinza) and ribavirin, which produced an SVR12 of 92% in 868 patients. The SVR12 rate is the percentage of patients with undetectable hepatitis C virus (HCV) 12 or more weeks after the end of treatment.
Dr. Drysdale cautioned that the data have not yet been put through a multivariate analysis, but the results so far provide “a strong indication that ribavirin may not be as insignificant” as many have recently presumed. “Ribavirin has been set aside because it was thought not to add to the SVR12, but if patients get only one go at treatment, we must be sure their first treatment is the best one,” Dr. Drysdale said in an interview. If ribavirin can be shown to make a significant contribution to treatment efficacy “then we should think more widely about using it when patients tolerate it.”
The analysis included too few patients with either current decompensated cirrhosis or a history of decompensated cirrhosis to make any statistically meaningful comparisons of the treatment subgroups among these patients. And among patients with genotype 3 HCV infection and without cirrhosis, none of the treatments used in practice showed any statistically significant differences in the SVR12 rates they produced. Among patients without cirrhosis the most commonly used regimens by far were an 8-week course of glecaprevir plus pibrentasvir in 731 patients or a 12-week course of sofosbuvir plus velpatasvir in 1,184 patients. Both regimens had SVR12 rates in noncirrhotic patients of 97%, regardless of whether patients had no, mild, or moderate liver fibrosis.
The study used data collected in an English national registry of HCV-infected patients treated with direct-acting antiviral drugs starting in 2017. Dr. Drysdale and her associates narrowed down the total database of more than 37,000 English adults who received some HCV therapy during the period to 14,603 who received a complete, valid regimen and had follow-up SVR12 information available. The overall SVR12 rate among all these patients was 95.59%, and among the patients infected by genotype 3 virus the SVR12 rate was 95.03%. Dr. Drysdale’s analysis focused primarily on the roughly one-third of patients in the study group infected with genotype 3 HCV, the genotype that historically has presented unique treatment challenges (Drugs. 2017 Feb;77[2]:131-44).
Another finding Dr. Drysdale reported was that as liver disease severity worsened from no fibrosis to mild or moderate fibrosis, and then to compensated cirrhosis or decompensation, the SVR12 rate steadily diminished. Among genotype 3 patients, the SVR12 rate fell from about 97% among patients without any fibrosis to about 87% among those with decompensated cirrhosis. Although this observation had been made before, this finding in such a large number of treated patients adds significant new evidence to support this pattern. It also adds further support to the idea of screening for HCV infection among higher-risk, asymptomatic people to optimize their prospects for virus eradication with treatment.
“If patients get much better treatment outcomes before they become cirrhotic then we should try to find these HCV-infected people before they develop symptoms,” Dr. Drysdale said.
Dr. Drysdale reported no disclosures.
SOURCE: Drysdale K et al. J Hepatol. 2019 April;70(1):e131.
REPORTING FROM ILC 2019
Tailoring the Mediterranean diet for NAFLD
Adults with nonalcoholic fatty liver disease (NAFLD) were more likely to implement the Mediterranean diet when they had greater nutritional knowledge and skills, family support, nutritional care, and positive reinforcement in the media, according to an in-depth study of 19 patients.
Barriers to adopting the diet included “an obesogenic environment, life stressors, and demand for convenience. Poor understanding of the causes and significance of NAFLD adversely affected readiness to change dietary habits,” wrote Laura Haigh of Newcastle University in Newcastle Upon Tyne, England, and associates. The study, which included both standard quantitative methods and semistructured interviews, was published in Clinical Gastroenterology and Hepatology.
The Mediterranean diet emphasizes vegetables, legumes, fish, fruits, whole grains, nuts, and olive oil in lieu of processed foods, sweets, saturated fats, and red meat. This diet has been definitively shown to improve insulin sensitivity and steatosis, even when patients do not lose weight. This has sparked interest in its use for NAFLD disease, but keys to its successful adoption in Northern Europe are not well understood.
Therefore, the researchers recruited 19 NAFLD patients from a tertiary care center in the United Kingdom for a 12-week Mediterranean diet intervention. Most were female, white, in their late 50s, obese, and had type 2 diabetes. “Participants were taught behavioral strategies through the provision of shopping lists, meal planners, and recipes. No advice was given on calorie allowances or physical activities,” the investigators noted.
By using a 14-point assessment tool, they found that dietary adherence rose significantly at 12 weeks, compared with baseline (P = .006). In all, 79% of patients lost weight (mean, 2.4 kg; P = .001 versus baseline), and 72% significantly increased their serum level of HDL cholesterol. Interviews linked successful adoption of the diet with diverse factors, such as believing that NAFLD is lifestyle associated, realizing that healthier nutrition can improve health outcomes, and having access to transportation and budget grocery stories. Patients generally saw the Mediterranean diet as flexible and affordable, but they struggled to adopt it if they worked irregular hours, experienced substantial life stress or were very busy, or tended to eat for self-reward or self-comfort.
Other cited barriers included “diet saboteurs” (including spouses), the plethora of unhealthy foods available in patients’ environments, low nutritional or medical knowledge, and cultural, social, or taste incompatibility, the researchers reported. Taken together, the findings underscore “the futility of a one-size-fits-all approach” when implementing the Mediterranean diet in this population, they concluded. Instead, their patients valued a collaborative, tailored approach – ideally one that incorporated in-person and group-based treatment, as well as online support.
Funders included the North East of England hub of the Allied Health Professions Research Network, the Elucidating Pathways of Steatohepatitis consortium, the Horizon 2020 Framework Program of the European Union, and the Newcastle NIHR Biomedical Research Centre. The researchers reported having no conflicts of interest.
SOURCE: Haigh L et al. Clin Gastroenterol Hepatol. 2018 Oct 31. doi: 10.1016/j.cgh.2018.10.044.
Adults with nonalcoholic fatty liver disease (NAFLD) were more likely to implement the Mediterranean diet when they had greater nutritional knowledge and skills, family support, nutritional care, and positive reinforcement in the media, according to an in-depth study of 19 patients.
Barriers to adopting the diet included “an obesogenic environment, life stressors, and demand for convenience. Poor understanding of the causes and significance of NAFLD adversely affected readiness to change dietary habits,” wrote Laura Haigh of Newcastle University in Newcastle Upon Tyne, England, and associates. The study, which included both standard quantitative methods and semistructured interviews, was published in Clinical Gastroenterology and Hepatology.
The Mediterranean diet emphasizes vegetables, legumes, fish, fruits, whole grains, nuts, and olive oil in lieu of processed foods, sweets, saturated fats, and red meat. This diet has been definitively shown to improve insulin sensitivity and steatosis, even when patients do not lose weight. This has sparked interest in its use for NAFLD disease, but keys to its successful adoption in Northern Europe are not well understood.
Therefore, the researchers recruited 19 NAFLD patients from a tertiary care center in the United Kingdom for a 12-week Mediterranean diet intervention. Most were female, white, in their late 50s, obese, and had type 2 diabetes. “Participants were taught behavioral strategies through the provision of shopping lists, meal planners, and recipes. No advice was given on calorie allowances or physical activities,” the investigators noted.
By using a 14-point assessment tool, they found that dietary adherence rose significantly at 12 weeks, compared with baseline (P = .006). In all, 79% of patients lost weight (mean, 2.4 kg; P = .001 versus baseline), and 72% significantly increased their serum level of HDL cholesterol. Interviews linked successful adoption of the diet with diverse factors, such as believing that NAFLD is lifestyle associated, realizing that healthier nutrition can improve health outcomes, and having access to transportation and budget grocery stories. Patients generally saw the Mediterranean diet as flexible and affordable, but they struggled to adopt it if they worked irregular hours, experienced substantial life stress or were very busy, or tended to eat for self-reward or self-comfort.
Other cited barriers included “diet saboteurs” (including spouses), the plethora of unhealthy foods available in patients’ environments, low nutritional or medical knowledge, and cultural, social, or taste incompatibility, the researchers reported. Taken together, the findings underscore “the futility of a one-size-fits-all approach” when implementing the Mediterranean diet in this population, they concluded. Instead, their patients valued a collaborative, tailored approach – ideally one that incorporated in-person and group-based treatment, as well as online support.
Funders included the North East of England hub of the Allied Health Professions Research Network, the Elucidating Pathways of Steatohepatitis consortium, the Horizon 2020 Framework Program of the European Union, and the Newcastle NIHR Biomedical Research Centre. The researchers reported having no conflicts of interest.
SOURCE: Haigh L et al. Clin Gastroenterol Hepatol. 2018 Oct 31. doi: 10.1016/j.cgh.2018.10.044.
Adults with nonalcoholic fatty liver disease (NAFLD) were more likely to implement the Mediterranean diet when they had greater nutritional knowledge and skills, family support, nutritional care, and positive reinforcement in the media, according to an in-depth study of 19 patients.
Barriers to adopting the diet included “an obesogenic environment, life stressors, and demand for convenience. Poor understanding of the causes and significance of NAFLD adversely affected readiness to change dietary habits,” wrote Laura Haigh of Newcastle University in Newcastle Upon Tyne, England, and associates. The study, which included both standard quantitative methods and semistructured interviews, was published in Clinical Gastroenterology and Hepatology.
The Mediterranean diet emphasizes vegetables, legumes, fish, fruits, whole grains, nuts, and olive oil in lieu of processed foods, sweets, saturated fats, and red meat. This diet has been definitively shown to improve insulin sensitivity and steatosis, even when patients do not lose weight. This has sparked interest in its use for NAFLD disease, but keys to its successful adoption in Northern Europe are not well understood.
Therefore, the researchers recruited 19 NAFLD patients from a tertiary care center in the United Kingdom for a 12-week Mediterranean diet intervention. Most were female, white, in their late 50s, obese, and had type 2 diabetes. “Participants were taught behavioral strategies through the provision of shopping lists, meal planners, and recipes. No advice was given on calorie allowances or physical activities,” the investigators noted.
By using a 14-point assessment tool, they found that dietary adherence rose significantly at 12 weeks, compared with baseline (P = .006). In all, 79% of patients lost weight (mean, 2.4 kg; P = .001 versus baseline), and 72% significantly increased their serum level of HDL cholesterol. Interviews linked successful adoption of the diet with diverse factors, such as believing that NAFLD is lifestyle associated, realizing that healthier nutrition can improve health outcomes, and having access to transportation and budget grocery stories. Patients generally saw the Mediterranean diet as flexible and affordable, but they struggled to adopt it if they worked irregular hours, experienced substantial life stress or were very busy, or tended to eat for self-reward or self-comfort.
Other cited barriers included “diet saboteurs” (including spouses), the plethora of unhealthy foods available in patients’ environments, low nutritional or medical knowledge, and cultural, social, or taste incompatibility, the researchers reported. Taken together, the findings underscore “the futility of a one-size-fits-all approach” when implementing the Mediterranean diet in this population, they concluded. Instead, their patients valued a collaborative, tailored approach – ideally one that incorporated in-person and group-based treatment, as well as online support.
Funders included the North East of England hub of the Allied Health Professions Research Network, the Elucidating Pathways of Steatohepatitis consortium, the Horizon 2020 Framework Program of the European Union, and the Newcastle NIHR Biomedical Research Centre. The researchers reported having no conflicts of interest.
SOURCE: Haigh L et al. Clin Gastroenterol Hepatol. 2018 Oct 31. doi: 10.1016/j.cgh.2018.10.044.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Fecal microbiota transplant shows promise for hepatic encephalopathy
VIENNA –
The oral fecal microbiota transplant (FMT), modeled on guideline-directed treatment for Clostridium difficile (Clin Infect Dis. 2018 April 1;66[7]:e1-48), was linked with a cut in hospitalizations and serious adverse events, as well as a clinically meaningful improvement in a cognitive measure specific for hepatic encephalopathy, Jasmohan S. Bajaj, MD, said at the meeting sponsored by the European Association for the Study of the Liver. Given the preliminary scope of the study, the next step is to assess the treatment in more patients and to evaluate delivery of the FMT specifically to the upper or lower gastrointestinal tract, said Dr. Bajaj, a hepatologist at Virginia Commonwealth University and McGuire VA Medical Center, both in Richmond.
The study included 20 patients with recurrent hepatic encephalopathy (RHE) and a history of at least two encephalopathy episodes despite treatment with lactulose and rifaximin (Xifaxan). After a baseline assessment, 10 patients received a single, oral dose of FMT contained in 15 capsules and composed of fecal material from the OpenBiome collection, and 10 patients received placebo capsules. All of the FMT material came from a single donor and contained a high level of beneficial microbial types, specifically Lachnospiraceae and Ruminococcaceae species. Patients averaged 64 years of age.
During 5 months of follow-up, 6 of the 10 placebo patients had a serious adverse event versus 1 of the 10 patients treated with an active FMT; altogether, there were 11 serious adverse events among the placebo patients versus only 1 event among the FMT patients, Dr. Bajaj reported. Three patients in the control arm had a total of seven hepatic encephalopathy events, compared with a single patient with one event in the intervention arm.
Enrolled patients also underwent two cognitive tests at baseline and during follow-up. Using a Stroop smartphone app (EncephalApp) designed to assess patients with RHE (Hepatology. 2013 Sept;58[3]:1122-32), the researchers found an average 51-second improvement in OffTime+OnTime, a statistically significant and clinically meaningful improvement in the patients treated with FMT, whereas the control patients showed no statistically significant change in this parameter. The second cognitive measure was the average performance by patients using the Psychometric Hepatic Encephalopathy Score (Curr Gastroenterol Rep. 2014 Jan;16[1]:362), which showed no significant change after treatment in either study arm. The actively treated patients also showed favorable changes in the microbial composition of their stool and mucosa, as well as an enhanced small intestinal barrier, following treatment, Dr. Bajaj said.
SOURCE: Bajaj JS et al. J Hepatol. 2019 April;70[1]:e55.
VIENNA –
The oral fecal microbiota transplant (FMT), modeled on guideline-directed treatment for Clostridium difficile (Clin Infect Dis. 2018 April 1;66[7]:e1-48), was linked with a cut in hospitalizations and serious adverse events, as well as a clinically meaningful improvement in a cognitive measure specific for hepatic encephalopathy, Jasmohan S. Bajaj, MD, said at the meeting sponsored by the European Association for the Study of the Liver. Given the preliminary scope of the study, the next step is to assess the treatment in more patients and to evaluate delivery of the FMT specifically to the upper or lower gastrointestinal tract, said Dr. Bajaj, a hepatologist at Virginia Commonwealth University and McGuire VA Medical Center, both in Richmond.
The study included 20 patients with recurrent hepatic encephalopathy (RHE) and a history of at least two encephalopathy episodes despite treatment with lactulose and rifaximin (Xifaxan). After a baseline assessment, 10 patients received a single, oral dose of FMT contained in 15 capsules and composed of fecal material from the OpenBiome collection, and 10 patients received placebo capsules. All of the FMT material came from a single donor and contained a high level of beneficial microbial types, specifically Lachnospiraceae and Ruminococcaceae species. Patients averaged 64 years of age.
During 5 months of follow-up, 6 of the 10 placebo patients had a serious adverse event versus 1 of the 10 patients treated with an active FMT; altogether, there were 11 serious adverse events among the placebo patients versus only 1 event among the FMT patients, Dr. Bajaj reported. Three patients in the control arm had a total of seven hepatic encephalopathy events, compared with a single patient with one event in the intervention arm.
Enrolled patients also underwent two cognitive tests at baseline and during follow-up. Using a Stroop smartphone app (EncephalApp) designed to assess patients with RHE (Hepatology. 2013 Sept;58[3]:1122-32), the researchers found an average 51-second improvement in OffTime+OnTime, a statistically significant and clinically meaningful improvement in the patients treated with FMT, whereas the control patients showed no statistically significant change in this parameter. The second cognitive measure was the average performance by patients using the Psychometric Hepatic Encephalopathy Score (Curr Gastroenterol Rep. 2014 Jan;16[1]:362), which showed no significant change after treatment in either study arm. The actively treated patients also showed favorable changes in the microbial composition of their stool and mucosa, as well as an enhanced small intestinal barrier, following treatment, Dr. Bajaj said.
SOURCE: Bajaj JS et al. J Hepatol. 2019 April;70[1]:e55.
VIENNA –
The oral fecal microbiota transplant (FMT), modeled on guideline-directed treatment for Clostridium difficile (Clin Infect Dis. 2018 April 1;66[7]:e1-48), was linked with a cut in hospitalizations and serious adverse events, as well as a clinically meaningful improvement in a cognitive measure specific for hepatic encephalopathy, Jasmohan S. Bajaj, MD, said at the meeting sponsored by the European Association for the Study of the Liver. Given the preliminary scope of the study, the next step is to assess the treatment in more patients and to evaluate delivery of the FMT specifically to the upper or lower gastrointestinal tract, said Dr. Bajaj, a hepatologist at Virginia Commonwealth University and McGuire VA Medical Center, both in Richmond.
The study included 20 patients with recurrent hepatic encephalopathy (RHE) and a history of at least two encephalopathy episodes despite treatment with lactulose and rifaximin (Xifaxan). After a baseline assessment, 10 patients received a single, oral dose of FMT contained in 15 capsules and composed of fecal material from the OpenBiome collection, and 10 patients received placebo capsules. All of the FMT material came from a single donor and contained a high level of beneficial microbial types, specifically Lachnospiraceae and Ruminococcaceae species. Patients averaged 64 years of age.
During 5 months of follow-up, 6 of the 10 placebo patients had a serious adverse event versus 1 of the 10 patients treated with an active FMT; altogether, there were 11 serious adverse events among the placebo patients versus only 1 event among the FMT patients, Dr. Bajaj reported. Three patients in the control arm had a total of seven hepatic encephalopathy events, compared with a single patient with one event in the intervention arm.
Enrolled patients also underwent two cognitive tests at baseline and during follow-up. Using a Stroop smartphone app (EncephalApp) designed to assess patients with RHE (Hepatology. 2013 Sept;58[3]:1122-32), the researchers found an average 51-second improvement in OffTime+OnTime, a statistically significant and clinically meaningful improvement in the patients treated with FMT, whereas the control patients showed no statistically significant change in this parameter. The second cognitive measure was the average performance by patients using the Psychometric Hepatic Encephalopathy Score (Curr Gastroenterol Rep. 2014 Jan;16[1]:362), which showed no significant change after treatment in either study arm. The actively treated patients also showed favorable changes in the microbial composition of their stool and mucosa, as well as an enhanced small intestinal barrier, following treatment, Dr. Bajaj said.
SOURCE: Bajaj JS et al. J Hepatol. 2019 April;70[1]:e55.
REPORTING FROM ILC 2019
VIDEO: Givosiran cuts acute intermittent porphyria attacks in pivotal trial
VIENNA – A .

Although the study also identified some safety issues with givosiran, an RNA-inhibitor molecule delivered by subcutaneous injection once a month, the increases in liver enzyme levels it produced in some patients as well as decreased renal function did not seem severe or frequent enough to counterbalance the benefits to treated patients, who often have significant comorbidities and adverse effects because of their disease, Manisha Balwani, MD, said at the meeting sponsored by the European Association for the Study of the Liver. Among the 48 patients assigned to the givosiran group, one patient dropped out because of an adverse effect of treatment.
The results put givosiran on track to become the first Food and Drug Administration–approved treatment for acute hepatic porphyria, a set of similar, rare genetic diseases that produce symptoms in about 1 in every 10,000 people, although asymptomatic disease is likely more common (Hepatol Commun. 2019 Feb;3[2]:193-206). The trial outcomes were also notable for the dramatic improvements in life-disrupting symptoms like pain, nausea, and fatigue that many treated patients experienced.
Patients’ lives were “completely transformed” by givosiran treatment, Dr. Balwani said in a video interview. Patients also had a reduced need for analgesics, including opioids, said Dr. Balwani, a medical geneticist at the Icahn School of Medicine at Mount Sinai in New York.
The ENVISION (A Study to Evaluate the Efficacy and Safety of Givosiran [ALN-AS1] in Patients With Acute Hepatic Porphyrias) study randomized 94 patients who were at least 12 years old and diagnosed with an acute hepatic porphyria, and had experienced at least two porphyria attacks during the prior 6 months. The study ran at 36 sites in 18 countries. Enrolled patients averaged about 39 years old, and had been diagnosed with a hepatic porphyria for an average of about 6 years. During the study, patients did not receive hemin (Panhematin) prophylaxis.
The study’s primary endpoint was the average annualized rate of porphyria attacks during 6 months of treatment, which was 3.2 attacks in 46 patients evaluable for efficacy on givosiran treatment and 12.5 attacks in 43 patients evaluable for efficacy in the control group, a 74% reduction in attacks with givosiran that was statistically significant, Dr. Balwani reported. The percentage of patients with no attacks during the study was 16% among control patients and 50% among those on givosiran. Future analysis of the study data will attempt to identify the patients with the best responses to givosiran.
Among the full cohort of 94 patients enrolled in the study, 21% of the givosiran-treated patients had a adverse reaction, and 17% had a severe adverse reaction, compared with rates of 9% and 11%, respectively, among controls. Three of the serious adverse reactions were judged related to givosiran treatment: one patient with pyrexia, one with abnormal liver function test results, and one patient who developed chronic kidney disease. A total of two patients in the givosiran group developed chronic kidney disease that warranted elective hospitalization for diagnostic evaluation, and an additional three patients on the drug developed chronic kidney disease that did not require hospitalization. Nausea affected 27% of patients on givosiran and 11% of the control patients. Injection-site reactions occurred in 17% of those on givosiran and in none of the placebo patients. An elevation in the serum level of alanine aminotransferase to more than three times the upper limit of normal of baseline occurred in 15% of the givosiran-treated patients and in 2% of the placebo patients.
Givosiran’s small RNA molecule inhibits production of 5‐aminolevulinic acid synthase 1 (ALAS‐1), the rate-limiting enzyme that drives production of the heme precursor molecules that are pathophysiologic in patients with acute hepatic porphyria.
SOURCE: Balwani M et al. J Hepatol. 2019 April 70(1):e81-2.
VIENNA – A .

Although the study also identified some safety issues with givosiran, an RNA-inhibitor molecule delivered by subcutaneous injection once a month, the increases in liver enzyme levels it produced in some patients as well as decreased renal function did not seem severe or frequent enough to counterbalance the benefits to treated patients, who often have significant comorbidities and adverse effects because of their disease, Manisha Balwani, MD, said at the meeting sponsored by the European Association for the Study of the Liver. Among the 48 patients assigned to the givosiran group, one patient dropped out because of an adverse effect of treatment.
The results put givosiran on track to become the first Food and Drug Administration–approved treatment for acute hepatic porphyria, a set of similar, rare genetic diseases that produce symptoms in about 1 in every 10,000 people, although asymptomatic disease is likely more common (Hepatol Commun. 2019 Feb;3[2]:193-206). The trial outcomes were also notable for the dramatic improvements in life-disrupting symptoms like pain, nausea, and fatigue that many treated patients experienced.
Patients’ lives were “completely transformed” by givosiran treatment, Dr. Balwani said in a video interview. Patients also had a reduced need for analgesics, including opioids, said Dr. Balwani, a medical geneticist at the Icahn School of Medicine at Mount Sinai in New York.
The ENVISION (A Study to Evaluate the Efficacy and Safety of Givosiran [ALN-AS1] in Patients With Acute Hepatic Porphyrias) study randomized 94 patients who were at least 12 years old and diagnosed with an acute hepatic porphyria, and had experienced at least two porphyria attacks during the prior 6 months. The study ran at 36 sites in 18 countries. Enrolled patients averaged about 39 years old, and had been diagnosed with a hepatic porphyria for an average of about 6 years. During the study, patients did not receive hemin (Panhematin) prophylaxis.
The study’s primary endpoint was the average annualized rate of porphyria attacks during 6 months of treatment, which was 3.2 attacks in 46 patients evaluable for efficacy on givosiran treatment and 12.5 attacks in 43 patients evaluable for efficacy in the control group, a 74% reduction in attacks with givosiran that was statistically significant, Dr. Balwani reported. The percentage of patients with no attacks during the study was 16% among control patients and 50% among those on givosiran. Future analysis of the study data will attempt to identify the patients with the best responses to givosiran.
Among the full cohort of 94 patients enrolled in the study, 21% of the givosiran-treated patients had a adverse reaction, and 17% had a severe adverse reaction, compared with rates of 9% and 11%, respectively, among controls. Three of the serious adverse reactions were judged related to givosiran treatment: one patient with pyrexia, one with abnormal liver function test results, and one patient who developed chronic kidney disease. A total of two patients in the givosiran group developed chronic kidney disease that warranted elective hospitalization for diagnostic evaluation, and an additional three patients on the drug developed chronic kidney disease that did not require hospitalization. Nausea affected 27% of patients on givosiran and 11% of the control patients. Injection-site reactions occurred in 17% of those on givosiran and in none of the placebo patients. An elevation in the serum level of alanine aminotransferase to more than three times the upper limit of normal of baseline occurred in 15% of the givosiran-treated patients and in 2% of the placebo patients.
Givosiran’s small RNA molecule inhibits production of 5‐aminolevulinic acid synthase 1 (ALAS‐1), the rate-limiting enzyme that drives production of the heme precursor molecules that are pathophysiologic in patients with acute hepatic porphyria.
SOURCE: Balwani M et al. J Hepatol. 2019 April 70(1):e81-2.
VIENNA – A .

Although the study also identified some safety issues with givosiran, an RNA-inhibitor molecule delivered by subcutaneous injection once a month, the increases in liver enzyme levels it produced in some patients as well as decreased renal function did not seem severe or frequent enough to counterbalance the benefits to treated patients, who often have significant comorbidities and adverse effects because of their disease, Manisha Balwani, MD, said at the meeting sponsored by the European Association for the Study of the Liver. Among the 48 patients assigned to the givosiran group, one patient dropped out because of an adverse effect of treatment.
The results put givosiran on track to become the first Food and Drug Administration–approved treatment for acute hepatic porphyria, a set of similar, rare genetic diseases that produce symptoms in about 1 in every 10,000 people, although asymptomatic disease is likely more common (Hepatol Commun. 2019 Feb;3[2]:193-206). The trial outcomes were also notable for the dramatic improvements in life-disrupting symptoms like pain, nausea, and fatigue that many treated patients experienced.
Patients’ lives were “completely transformed” by givosiran treatment, Dr. Balwani said in a video interview. Patients also had a reduced need for analgesics, including opioids, said Dr. Balwani, a medical geneticist at the Icahn School of Medicine at Mount Sinai in New York.
The ENVISION (A Study to Evaluate the Efficacy and Safety of Givosiran [ALN-AS1] in Patients With Acute Hepatic Porphyrias) study randomized 94 patients who were at least 12 years old and diagnosed with an acute hepatic porphyria, and had experienced at least two porphyria attacks during the prior 6 months. The study ran at 36 sites in 18 countries. Enrolled patients averaged about 39 years old, and had been diagnosed with a hepatic porphyria for an average of about 6 years. During the study, patients did not receive hemin (Panhematin) prophylaxis.
The study’s primary endpoint was the average annualized rate of porphyria attacks during 6 months of treatment, which was 3.2 attacks in 46 patients evaluable for efficacy on givosiran treatment and 12.5 attacks in 43 patients evaluable for efficacy in the control group, a 74% reduction in attacks with givosiran that was statistically significant, Dr. Balwani reported. The percentage of patients with no attacks during the study was 16% among control patients and 50% among those on givosiran. Future analysis of the study data will attempt to identify the patients with the best responses to givosiran.
Among the full cohort of 94 patients enrolled in the study, 21% of the givosiran-treated patients had a adverse reaction, and 17% had a severe adverse reaction, compared with rates of 9% and 11%, respectively, among controls. Three of the serious adverse reactions were judged related to givosiran treatment: one patient with pyrexia, one with abnormal liver function test results, and one patient who developed chronic kidney disease. A total of two patients in the givosiran group developed chronic kidney disease that warranted elective hospitalization for diagnostic evaluation, and an additional three patients on the drug developed chronic kidney disease that did not require hospitalization. Nausea affected 27% of patients on givosiran and 11% of the control patients. Injection-site reactions occurred in 17% of those on givosiran and in none of the placebo patients. An elevation in the serum level of alanine aminotransferase to more than three times the upper limit of normal of baseline occurred in 15% of the givosiran-treated patients and in 2% of the placebo patients.
Givosiran’s small RNA molecule inhibits production of 5‐aminolevulinic acid synthase 1 (ALAS‐1), the rate-limiting enzyme that drives production of the heme precursor molecules that are pathophysiologic in patients with acute hepatic porphyria.
SOURCE: Balwani M et al. J Hepatol. 2019 April 70(1):e81-2.
REPORTING FROM ILC 2019
Key clinical point: Givosiran cut acute hepatic porphyria attacks in its pivotal trial.
Major finding: Patients treated with givosiran had 74% fewer acute porphyria attacks, compared with patients on placebo.
Study details: ENVISION, an international pivotal trial with 94 patients.
Disclosures: ENVISION was funded by Alnylam, the company developing givosiran. Dr. Balwani has been an advisor to and has received research funding from Alnylam. The center where Dr. Balwani works, the Icahn School of Medicine at Mount Sinai, in New York, holds patents related to givosiran that it has licensed to Amnylam.
Source: Balwani M et al. J Hepatol. 2019 April 70(1):e81-2.
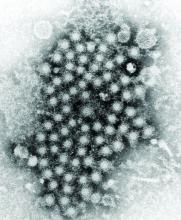
Tenofovir disoproxil treated HBV with fewer future HCCs
VIENNA – Treatment of individuals chronically infected with hepatitis B virus (HBV) with the nucleotide analog tenofovir disoproxil fumarate significantly linked with a substantial cut in the incidence of hepatocellular carcinoma (HCC) compared with those who received the nucleoside analog entecavir, according to a review of more than 29,000 Hong Kong patients.
This is the second reported study to find that association. In January 2019, a study of more than 24,000 Korean residents chronically infected with HBV showed a similar, statistically significant link between treatment with tenofovir disoproxil fumarate (Viread) and a lower incidence of HCC compared with patients treated with entecavir (Baraclude) (JAMA Oncol. 2019 Jan;5[1]:30-6), Grace L.H. Wong, MD, said at the meeting, sponsored by the European Association for the Study of the Liver (EASL).
However, another report published just a few days before Dr. Wong spoke failed to find an association between tenofovir disoproxil treatment of HBV and the subsequent rate of HCC compared with patients treated with entecavir. That study comprised nearly 2,900 HBV patients treated at any of four Korean medical centers (J Hepatol. 2019 Apr. doi: 10.1016/j.jhep.2019.03.028).
Dr. Wong noted that although current guidelines from EASL cite both tenofovir disoproxil and entecavir (as well as tenofovir alafenamide [Vemlidy]) as first-line treatments for chronic HBV infection (J Hepatol. 2017 Aug;67[2]:370-98), some evidence suggests that tenofovir disoproxil might produce effects subtly different from those of entecavir.
At the meeting in Vienna, for example, a report on 176 Japanese patients with chronic HBV showed that those who were treated with a nucleotide analog such as tenofovir disoproxil produced higher serum levels of interferon-lamda3 compared with patients treated with entecavir, and increased levels of this interferon could improve clearance of HBV surface antigen (J Hepatol. 2019 April;70[1]:e477). The most recent EASL guidelines for treatment of chronic hepatitis B infection also list tenofovir disoproxil, entecavir, and tenofovir alafenamide as preferred agents (Hepatology. 2018 April;67[4]:1560-99).
The data Dr. Wong and her associates analyzed came from health records kept for about 80% of Hong Kong’s population in the Clinical Data Analysis and Recording System of the Hospital Authority of Hong Kong. From January 2010 to June 2018, this database included 28,041 consecutive patients chronically infected with HBV and treated with entecavir, and 1,309 consecutive patients treated with tenofovir disoproxil. These numbers excluded patients treated for less than 6 months, patients coinfected with hepatitis C or D virus, patients with cancer diagnosed or a liver transplanted before or during their first 6 months on treatment, and patients previously treated with an interferon or nucleos(t)ide.
During an average follow-up of 2.8 years of tenofovir disoproxil treatment, 8 patients developed HCC, and during an average follow-up of 3.7 years of entecavir treatment, 1,386 patients developed HCC, reported Dr. Wong, a hepatologist and professor of medicine at the Chinese University of Hong Kong.
In a multivariate analysis that adjusted for demographic and clinical differences, treatment with tenofovir disoproxil linked with a statistically significant 68% reduced rate of HCC development compared with the entecavir-treated patients, she said. In a propensity score–weighted analysis, tenofovir disoproxil linked with a statistically significant 64% reduced rate of incident HCC, and in a propensity score–matched analysis tenofovir disoproxil linked with a 58% reduced rate of HCC, although in this analysis, which excluded many of the entecavir-treated patients and hence had less statistical power, the difference just missed statistical significance.
As an additional step to try to rule out the possible effect of unadjusted confounders, Dr. Wong and associates analyzed the links between tenofovir disoproxil and entecavir treatment and two negative-control outcomes, the incidence of lung cancer and the incidence of acute myocardial infarction. Neither of these outcomes showed a statistically significant link with one of the HBV treatments, suggesting that the link between treatment and HCC incidence did not appear because of an unadjusted confounding bias, Dr. Wong said. The Hong Kong database did not include enough patients treated with tenofovir alafenamide to allow assessment of this drug, she added.
Dr. Wong has been an adviser to Gilead and a speaker for Abbott, AbbVie, Bristol-Myers Squibb, Gilead, Janssen, and Roche. Tenofovir disoproxil fumarate is marketed by Gilead, and entecavir is marketed by Bristol-Myers Squibb.
SOURCE: Wong GL et al. J Hepatol. 2019 April;70[1]:e128.
VIENNA – Treatment of individuals chronically infected with hepatitis B virus (HBV) with the nucleotide analog tenofovir disoproxil fumarate significantly linked with a substantial cut in the incidence of hepatocellular carcinoma (HCC) compared with those who received the nucleoside analog entecavir, according to a review of more than 29,000 Hong Kong patients.
This is the second reported study to find that association. In January 2019, a study of more than 24,000 Korean residents chronically infected with HBV showed a similar, statistically significant link between treatment with tenofovir disoproxil fumarate (Viread) and a lower incidence of HCC compared with patients treated with entecavir (Baraclude) (JAMA Oncol. 2019 Jan;5[1]:30-6), Grace L.H. Wong, MD, said at the meeting, sponsored by the European Association for the Study of the Liver (EASL).
However, another report published just a few days before Dr. Wong spoke failed to find an association between tenofovir disoproxil treatment of HBV and the subsequent rate of HCC compared with patients treated with entecavir. That study comprised nearly 2,900 HBV patients treated at any of four Korean medical centers (J Hepatol. 2019 Apr. doi: 10.1016/j.jhep.2019.03.028).
Dr. Wong noted that although current guidelines from EASL cite both tenofovir disoproxil and entecavir (as well as tenofovir alafenamide [Vemlidy]) as first-line treatments for chronic HBV infection (J Hepatol. 2017 Aug;67[2]:370-98), some evidence suggests that tenofovir disoproxil might produce effects subtly different from those of entecavir.
At the meeting in Vienna, for example, a report on 176 Japanese patients with chronic HBV showed that those who were treated with a nucleotide analog such as tenofovir disoproxil produced higher serum levels of interferon-lamda3 compared with patients treated with entecavir, and increased levels of this interferon could improve clearance of HBV surface antigen (J Hepatol. 2019 April;70[1]:e477). The most recent EASL guidelines for treatment of chronic hepatitis B infection also list tenofovir disoproxil, entecavir, and tenofovir alafenamide as preferred agents (Hepatology. 2018 April;67[4]:1560-99).
The data Dr. Wong and her associates analyzed came from health records kept for about 80% of Hong Kong’s population in the Clinical Data Analysis and Recording System of the Hospital Authority of Hong Kong. From January 2010 to June 2018, this database included 28,041 consecutive patients chronically infected with HBV and treated with entecavir, and 1,309 consecutive patients treated with tenofovir disoproxil. These numbers excluded patients treated for less than 6 months, patients coinfected with hepatitis C or D virus, patients with cancer diagnosed or a liver transplanted before or during their first 6 months on treatment, and patients previously treated with an interferon or nucleos(t)ide.
During an average follow-up of 2.8 years of tenofovir disoproxil treatment, 8 patients developed HCC, and during an average follow-up of 3.7 years of entecavir treatment, 1,386 patients developed HCC, reported Dr. Wong, a hepatologist and professor of medicine at the Chinese University of Hong Kong.
In a multivariate analysis that adjusted for demographic and clinical differences, treatment with tenofovir disoproxil linked with a statistically significant 68% reduced rate of HCC development compared with the entecavir-treated patients, she said. In a propensity score–weighted analysis, tenofovir disoproxil linked with a statistically significant 64% reduced rate of incident HCC, and in a propensity score–matched analysis tenofovir disoproxil linked with a 58% reduced rate of HCC, although in this analysis, which excluded many of the entecavir-treated patients and hence had less statistical power, the difference just missed statistical significance.
As an additional step to try to rule out the possible effect of unadjusted confounders, Dr. Wong and associates analyzed the links between tenofovir disoproxil and entecavir treatment and two negative-control outcomes, the incidence of lung cancer and the incidence of acute myocardial infarction. Neither of these outcomes showed a statistically significant link with one of the HBV treatments, suggesting that the link between treatment and HCC incidence did not appear because of an unadjusted confounding bias, Dr. Wong said. The Hong Kong database did not include enough patients treated with tenofovir alafenamide to allow assessment of this drug, she added.
Dr. Wong has been an adviser to Gilead and a speaker for Abbott, AbbVie, Bristol-Myers Squibb, Gilead, Janssen, and Roche. Tenofovir disoproxil fumarate is marketed by Gilead, and entecavir is marketed by Bristol-Myers Squibb.
SOURCE: Wong GL et al. J Hepatol. 2019 April;70[1]:e128.
VIENNA – Treatment of individuals chronically infected with hepatitis B virus (HBV) with the nucleotide analog tenofovir disoproxil fumarate significantly linked with a substantial cut in the incidence of hepatocellular carcinoma (HCC) compared with those who received the nucleoside analog entecavir, according to a review of more than 29,000 Hong Kong patients.
This is the second reported study to find that association. In January 2019, a study of more than 24,000 Korean residents chronically infected with HBV showed a similar, statistically significant link between treatment with tenofovir disoproxil fumarate (Viread) and a lower incidence of HCC compared with patients treated with entecavir (Baraclude) (JAMA Oncol. 2019 Jan;5[1]:30-6), Grace L.H. Wong, MD, said at the meeting, sponsored by the European Association for the Study of the Liver (EASL).
However, another report published just a few days before Dr. Wong spoke failed to find an association between tenofovir disoproxil treatment of HBV and the subsequent rate of HCC compared with patients treated with entecavir. That study comprised nearly 2,900 HBV patients treated at any of four Korean medical centers (J Hepatol. 2019 Apr. doi: 10.1016/j.jhep.2019.03.028).
Dr. Wong noted that although current guidelines from EASL cite both tenofovir disoproxil and entecavir (as well as tenofovir alafenamide [Vemlidy]) as first-line treatments for chronic HBV infection (J Hepatol. 2017 Aug;67[2]:370-98), some evidence suggests that tenofovir disoproxil might produce effects subtly different from those of entecavir.
At the meeting in Vienna, for example, a report on 176 Japanese patients with chronic HBV showed that those who were treated with a nucleotide analog such as tenofovir disoproxil produced higher serum levels of interferon-lamda3 compared with patients treated with entecavir, and increased levels of this interferon could improve clearance of HBV surface antigen (J Hepatol. 2019 April;70[1]:e477). The most recent EASL guidelines for treatment of chronic hepatitis B infection also list tenofovir disoproxil, entecavir, and tenofovir alafenamide as preferred agents (Hepatology. 2018 April;67[4]:1560-99).
The data Dr. Wong and her associates analyzed came from health records kept for about 80% of Hong Kong’s population in the Clinical Data Analysis and Recording System of the Hospital Authority of Hong Kong. From January 2010 to June 2018, this database included 28,041 consecutive patients chronically infected with HBV and treated with entecavir, and 1,309 consecutive patients treated with tenofovir disoproxil. These numbers excluded patients treated for less than 6 months, patients coinfected with hepatitis C or D virus, patients with cancer diagnosed or a liver transplanted before or during their first 6 months on treatment, and patients previously treated with an interferon or nucleos(t)ide.
During an average follow-up of 2.8 years of tenofovir disoproxil treatment, 8 patients developed HCC, and during an average follow-up of 3.7 years of entecavir treatment, 1,386 patients developed HCC, reported Dr. Wong, a hepatologist and professor of medicine at the Chinese University of Hong Kong.
In a multivariate analysis that adjusted for demographic and clinical differences, treatment with tenofovir disoproxil linked with a statistically significant 68% reduced rate of HCC development compared with the entecavir-treated patients, she said. In a propensity score–weighted analysis, tenofovir disoproxil linked with a statistically significant 64% reduced rate of incident HCC, and in a propensity score–matched analysis tenofovir disoproxil linked with a 58% reduced rate of HCC, although in this analysis, which excluded many of the entecavir-treated patients and hence had less statistical power, the difference just missed statistical significance.
As an additional step to try to rule out the possible effect of unadjusted confounders, Dr. Wong and associates analyzed the links between tenofovir disoproxil and entecavir treatment and two negative-control outcomes, the incidence of lung cancer and the incidence of acute myocardial infarction. Neither of these outcomes showed a statistically significant link with one of the HBV treatments, suggesting that the link between treatment and HCC incidence did not appear because of an unadjusted confounding bias, Dr. Wong said. The Hong Kong database did not include enough patients treated with tenofovir alafenamide to allow assessment of this drug, she added.
Dr. Wong has been an adviser to Gilead and a speaker for Abbott, AbbVie, Bristol-Myers Squibb, Gilead, Janssen, and Roche. Tenofovir disoproxil fumarate is marketed by Gilead, and entecavir is marketed by Bristol-Myers Squibb.
SOURCE: Wong GL et al. J Hepatol. 2019 April;70[1]:e128.
REPORTING FROM ILC 2019
Three-drug regimen shows promise for refractory primary biliary cholangitis
VIENNA –
In addition to producing drops in levels of alkaline phosphatase and bilirubin, key surrogate markers for ultimate clinical benefit, the addition of bezafibrate also led to reduced pruritis among five of eight patients who had this symptom when they started on bezafibrate, Lena Smets said at the meeting, sponsored by the European Association for the Study of the Liver. Pruritis is a bothersome adverse effect from obeticholic acid (OCA) treatment that also occurs in patients with untreated primary biliary cholangitis (PBC), so the drop in pruritis in patients who started bezafibrate was notable. Overall, the triple regimen of ursodeoxycholic acid (UDCA), OCA, and bezafibrate was “well tolerated,” said Ms. Smets, a researcher at KU Leuven, Belgium.
Bezafibrate is available in Europe as a lipid-lowering treatment, especially for lowering triglycerides, so there might be a temptation to use it off label in routine practice as an add-on to UDCA and OCA in PBC patients who are not fully responsive to this dual therapy, Ms. Smets acknowledged. But she stressed that what’s needed now is a multicenter, randomized trial of bezafibrate as part of triple-therapy regimen with many more than the 10 patients included in her review.
Both UDCA and OCA have Food and Drug Administration approval for U.S. treatment of PBC. Bezafibrate is not approved for U.S. marketing, but the related agent fenofibrate has FDA approval and has shown preliminary evidence of acting like bezafibrate in PBC patients in small pilot studies or case reports, showing that “growing evidence supports the use of fibrates, but their safety has not been firmly established, and caution should be used,” according to a recent review by clinicians from the University of California, Davis (Gastroenterol Hepatol [NY]. 2018 March;14[3]:154-63).
The series of 10 PBC patients who received triple therapy at KU Leuven began as part of a cohort of 16 PBC patients treated at that center with UDCA monotherapy for an average of 6 years before entering the POISE (Phase 3 Study of Obeticholic Acid in Patients With Primary Biliary Cirrhosis) phase 3 trial that ran at KU Leuven and 57 other sites in 13 countries. POISE randomized 216 PBC patients with persistently elevated alkaline phosphatase and bilirubin levels despite UDCA treatment to added treatment with OCA. The results showed incremental benefit to these patients from a tolerable OCA acid regimen (N Engl J Med. 2016 Aug 18;375[7]631-43). The findings helped OCA (Ocaliva) get FDA marketing approval in 2016 for treatment of PBC when added to UDCA in patients not fully responsive to UDCA monotherapy.
The case for bezafibrate as an add-on to UDCA for refractory PBC patients was documented by a 2018 report from the BEZURSO (Phase 3 Study of Bezafibrate in Combination With Ursodeoxycholic Acid in Primary Biliary Cirrhosis) trial. Run at multiple centers in France, the trial randomized 100 patients on UDCA treatment to added bezafibrate or placebo, and showed that bezafibrate produced significant incremental decreases in and normalizations of alkaline phosphatase and bilirubin levels. It also had the expected effect of increasing serum creatinine level by an average of 5% (N Engl J Med. 2018 June 7;378[23]:2171-81).
Among the 16 participants in the POISE trial at KU Leuven, 13 completed that trial and then agreed to start on a triple regimen with bezafibrate added because of persistent elevations in alkaline phosphatase, and 10 patients completed 6 months on triple treatment. After 6 months, alkaline phosphatase levels reached the normal range in 5 of these 10 patients, Ms. Smets reported. Bilirubin levels also decreased in each of the 10 patients, although bilirubin had already been at a normal level in 9 of the 10 patients at the start of bezafibrate treatment, and this rate remained at 9 of 10 after 6 months. Eight of the 10 had pruritis when they started bezafibrate, and five of these eight reported decreased symptoms on treatment. Patients also showed no biochemical evidence of hepatotoxicity on the triple regimen, Ms. Smets said.
Guidelines published in 2017 from the European Association for the Study of the Liver cited evidence from small studies showing possible efficacy of fibrates as an add-on for PBC patients refractory to UDCA monotherapy, but stopped short of any endorsement of their use (J Hepatol. 2017 July;67[1]:145-72). However, guidelines from the American Association for the Study of Liver Diseases, released several months later and after publication of the BEZURSO results, said that “fibrates can be considered as off-label alternatives for patients with PBC and inadequate response to UDCA,” but also warned that “use of OCA and fibrates is discouraged in patients with decompensated liver disease (Child Pugh–Turcotte B or C)” (Hepatology. 2018 Jan;69[1]:394-419).
SOURCE: Smets L et al. J Hepatol. 2019 April;70[1]:e130.
Clinicians in Europe already use this triple therapy in appropriate patients. Bezafibrate is cheap, it has been used since the 1970s to lower triglyceride levels, and it is generally safe. Following the report of results from the BEZURSO trial in 2018, guidelines changed to accept the option of adding a fibrate to ursodeoxycholic acid and obeticholic acid.
Thomas Berg, MD, is professor and head of hepatology at University Hospital in Leipzig, Germany. He has received personal fees and research support from several companies including Intercept, the company that markets obeticholic acid (Ocaliva). He made these comments in an interview.
Clinicians in Europe already use this triple therapy in appropriate patients. Bezafibrate is cheap, it has been used since the 1970s to lower triglyceride levels, and it is generally safe. Following the report of results from the BEZURSO trial in 2018, guidelines changed to accept the option of adding a fibrate to ursodeoxycholic acid and obeticholic acid.
Thomas Berg, MD, is professor and head of hepatology at University Hospital in Leipzig, Germany. He has received personal fees and research support from several companies including Intercept, the company that markets obeticholic acid (Ocaliva). He made these comments in an interview.
Clinicians in Europe already use this triple therapy in appropriate patients. Bezafibrate is cheap, it has been used since the 1970s to lower triglyceride levels, and it is generally safe. Following the report of results from the BEZURSO trial in 2018, guidelines changed to accept the option of adding a fibrate to ursodeoxycholic acid and obeticholic acid.
Thomas Berg, MD, is professor and head of hepatology at University Hospital in Leipzig, Germany. He has received personal fees and research support from several companies including Intercept, the company that markets obeticholic acid (Ocaliva). He made these comments in an interview.
VIENNA –
In addition to producing drops in levels of alkaline phosphatase and bilirubin, key surrogate markers for ultimate clinical benefit, the addition of bezafibrate also led to reduced pruritis among five of eight patients who had this symptom when they started on bezafibrate, Lena Smets said at the meeting, sponsored by the European Association for the Study of the Liver. Pruritis is a bothersome adverse effect from obeticholic acid (OCA) treatment that also occurs in patients with untreated primary biliary cholangitis (PBC), so the drop in pruritis in patients who started bezafibrate was notable. Overall, the triple regimen of ursodeoxycholic acid (UDCA), OCA, and bezafibrate was “well tolerated,” said Ms. Smets, a researcher at KU Leuven, Belgium.
Bezafibrate is available in Europe as a lipid-lowering treatment, especially for lowering triglycerides, so there might be a temptation to use it off label in routine practice as an add-on to UDCA and OCA in PBC patients who are not fully responsive to this dual therapy, Ms. Smets acknowledged. But she stressed that what’s needed now is a multicenter, randomized trial of bezafibrate as part of triple-therapy regimen with many more than the 10 patients included in her review.
Both UDCA and OCA have Food and Drug Administration approval for U.S. treatment of PBC. Bezafibrate is not approved for U.S. marketing, but the related agent fenofibrate has FDA approval and has shown preliminary evidence of acting like bezafibrate in PBC patients in small pilot studies or case reports, showing that “growing evidence supports the use of fibrates, but their safety has not been firmly established, and caution should be used,” according to a recent review by clinicians from the University of California, Davis (Gastroenterol Hepatol [NY]. 2018 March;14[3]:154-63).
The series of 10 PBC patients who received triple therapy at KU Leuven began as part of a cohort of 16 PBC patients treated at that center with UDCA monotherapy for an average of 6 years before entering the POISE (Phase 3 Study of Obeticholic Acid in Patients With Primary Biliary Cirrhosis) phase 3 trial that ran at KU Leuven and 57 other sites in 13 countries. POISE randomized 216 PBC patients with persistently elevated alkaline phosphatase and bilirubin levels despite UDCA treatment to added treatment with OCA. The results showed incremental benefit to these patients from a tolerable OCA acid regimen (N Engl J Med. 2016 Aug 18;375[7]631-43). The findings helped OCA (Ocaliva) get FDA marketing approval in 2016 for treatment of PBC when added to UDCA in patients not fully responsive to UDCA monotherapy.
The case for bezafibrate as an add-on to UDCA for refractory PBC patients was documented by a 2018 report from the BEZURSO (Phase 3 Study of Bezafibrate in Combination With Ursodeoxycholic Acid in Primary Biliary Cirrhosis) trial. Run at multiple centers in France, the trial randomized 100 patients on UDCA treatment to added bezafibrate or placebo, and showed that bezafibrate produced significant incremental decreases in and normalizations of alkaline phosphatase and bilirubin levels. It also had the expected effect of increasing serum creatinine level by an average of 5% (N Engl J Med. 2018 June 7;378[23]:2171-81).
Among the 16 participants in the POISE trial at KU Leuven, 13 completed that trial and then agreed to start on a triple regimen with bezafibrate added because of persistent elevations in alkaline phosphatase, and 10 patients completed 6 months on triple treatment. After 6 months, alkaline phosphatase levels reached the normal range in 5 of these 10 patients, Ms. Smets reported. Bilirubin levels also decreased in each of the 10 patients, although bilirubin had already been at a normal level in 9 of the 10 patients at the start of bezafibrate treatment, and this rate remained at 9 of 10 after 6 months. Eight of the 10 had pruritis when they started bezafibrate, and five of these eight reported decreased symptoms on treatment. Patients also showed no biochemical evidence of hepatotoxicity on the triple regimen, Ms. Smets said.
Guidelines published in 2017 from the European Association for the Study of the Liver cited evidence from small studies showing possible efficacy of fibrates as an add-on for PBC patients refractory to UDCA monotherapy, but stopped short of any endorsement of their use (J Hepatol. 2017 July;67[1]:145-72). However, guidelines from the American Association for the Study of Liver Diseases, released several months later and after publication of the BEZURSO results, said that “fibrates can be considered as off-label alternatives for patients with PBC and inadequate response to UDCA,” but also warned that “use of OCA and fibrates is discouraged in patients with decompensated liver disease (Child Pugh–Turcotte B or C)” (Hepatology. 2018 Jan;69[1]:394-419).
SOURCE: Smets L et al. J Hepatol. 2019 April;70[1]:e130.
VIENNA –
In addition to producing drops in levels of alkaline phosphatase and bilirubin, key surrogate markers for ultimate clinical benefit, the addition of bezafibrate also led to reduced pruritis among five of eight patients who had this symptom when they started on bezafibrate, Lena Smets said at the meeting, sponsored by the European Association for the Study of the Liver. Pruritis is a bothersome adverse effect from obeticholic acid (OCA) treatment that also occurs in patients with untreated primary biliary cholangitis (PBC), so the drop in pruritis in patients who started bezafibrate was notable. Overall, the triple regimen of ursodeoxycholic acid (UDCA), OCA, and bezafibrate was “well tolerated,” said Ms. Smets, a researcher at KU Leuven, Belgium.
Bezafibrate is available in Europe as a lipid-lowering treatment, especially for lowering triglycerides, so there might be a temptation to use it off label in routine practice as an add-on to UDCA and OCA in PBC patients who are not fully responsive to this dual therapy, Ms. Smets acknowledged. But she stressed that what’s needed now is a multicenter, randomized trial of bezafibrate as part of triple-therapy regimen with many more than the 10 patients included in her review.
Both UDCA and OCA have Food and Drug Administration approval for U.S. treatment of PBC. Bezafibrate is not approved for U.S. marketing, but the related agent fenofibrate has FDA approval and has shown preliminary evidence of acting like bezafibrate in PBC patients in small pilot studies or case reports, showing that “growing evidence supports the use of fibrates, but their safety has not been firmly established, and caution should be used,” according to a recent review by clinicians from the University of California, Davis (Gastroenterol Hepatol [NY]. 2018 March;14[3]:154-63).
The series of 10 PBC patients who received triple therapy at KU Leuven began as part of a cohort of 16 PBC patients treated at that center with UDCA monotherapy for an average of 6 years before entering the POISE (Phase 3 Study of Obeticholic Acid in Patients With Primary Biliary Cirrhosis) phase 3 trial that ran at KU Leuven and 57 other sites in 13 countries. POISE randomized 216 PBC patients with persistently elevated alkaline phosphatase and bilirubin levels despite UDCA treatment to added treatment with OCA. The results showed incremental benefit to these patients from a tolerable OCA acid regimen (N Engl J Med. 2016 Aug 18;375[7]631-43). The findings helped OCA (Ocaliva) get FDA marketing approval in 2016 for treatment of PBC when added to UDCA in patients not fully responsive to UDCA monotherapy.
The case for bezafibrate as an add-on to UDCA for refractory PBC patients was documented by a 2018 report from the BEZURSO (Phase 3 Study of Bezafibrate in Combination With Ursodeoxycholic Acid in Primary Biliary Cirrhosis) trial. Run at multiple centers in France, the trial randomized 100 patients on UDCA treatment to added bezafibrate or placebo, and showed that bezafibrate produced significant incremental decreases in and normalizations of alkaline phosphatase and bilirubin levels. It also had the expected effect of increasing serum creatinine level by an average of 5% (N Engl J Med. 2018 June 7;378[23]:2171-81).
Among the 16 participants in the POISE trial at KU Leuven, 13 completed that trial and then agreed to start on a triple regimen with bezafibrate added because of persistent elevations in alkaline phosphatase, and 10 patients completed 6 months on triple treatment. After 6 months, alkaline phosphatase levels reached the normal range in 5 of these 10 patients, Ms. Smets reported. Bilirubin levels also decreased in each of the 10 patients, although bilirubin had already been at a normal level in 9 of the 10 patients at the start of bezafibrate treatment, and this rate remained at 9 of 10 after 6 months. Eight of the 10 had pruritis when they started bezafibrate, and five of these eight reported decreased symptoms on treatment. Patients also showed no biochemical evidence of hepatotoxicity on the triple regimen, Ms. Smets said.
Guidelines published in 2017 from the European Association for the Study of the Liver cited evidence from small studies showing possible efficacy of fibrates as an add-on for PBC patients refractory to UDCA monotherapy, but stopped short of any endorsement of their use (J Hepatol. 2017 July;67[1]:145-72). However, guidelines from the American Association for the Study of Liver Diseases, released several months later and after publication of the BEZURSO results, said that “fibrates can be considered as off-label alternatives for patients with PBC and inadequate response to UDCA,” but also warned that “use of OCA and fibrates is discouraged in patients with decompensated liver disease (Child Pugh–Turcotte B or C)” (Hepatology. 2018 Jan;69[1]:394-419).
SOURCE: Smets L et al. J Hepatol. 2019 April;70[1]:e130.
REPORTING FROM ILC 2019
HCC linked to mitochondrial damage, iron accumulation from HCV
according to an extensive literature review.
Although the mechanisms underlying the hepatocellular carcinoma development are not fully understood, it is known that oxidative stress exists to a greater degree in hepatitis C virus (HCV) infection, compared with other inflammatory liver diseases. Such stress has been proposed as a major mechanism of liver injury in patients with chronic HCV, the authors reported in Free Radical Biology and Medicine.
Patients with HCV have significant hepatocellular mitochondrial alterations, and iron accumulation is also a well-known characteristic in patients with chronic HCV. Such alterations in mitochondria and iron accumulation are closely related to oxidative stress, since the mitochondria are the main site of reactive oxygen species generation, and iron produces hydroxy radicals via the Fenton reaction, according to the review.
“The greatest concern is whether mitochondrial damage and iron metabolic dysregulation persist even after HCV eradication and to what extent such pathological conditions affect the development of HCC. Determining the molecular signaling that underlies the mitophagy induced by iron depletion is another topic of interest and is expected to lead to potential therapeutic approaches for multiple diseases,” the researchers concluded.
Support was from the Research Program on Hepatitis from the Japan Agency for Medical Research and Development. The authors reported no disclosures.
SOURCE: Keisuke H et al. Free Radic Biol Med. 2019;133:193-9.
according to an extensive literature review.
Although the mechanisms underlying the hepatocellular carcinoma development are not fully understood, it is known that oxidative stress exists to a greater degree in hepatitis C virus (HCV) infection, compared with other inflammatory liver diseases. Such stress has been proposed as a major mechanism of liver injury in patients with chronic HCV, the authors reported in Free Radical Biology and Medicine.
Patients with HCV have significant hepatocellular mitochondrial alterations, and iron accumulation is also a well-known characteristic in patients with chronic HCV. Such alterations in mitochondria and iron accumulation are closely related to oxidative stress, since the mitochondria are the main site of reactive oxygen species generation, and iron produces hydroxy radicals via the Fenton reaction, according to the review.
“The greatest concern is whether mitochondrial damage and iron metabolic dysregulation persist even after HCV eradication and to what extent such pathological conditions affect the development of HCC. Determining the molecular signaling that underlies the mitophagy induced by iron depletion is another topic of interest and is expected to lead to potential therapeutic approaches for multiple diseases,” the researchers concluded.
Support was from the Research Program on Hepatitis from the Japan Agency for Medical Research and Development. The authors reported no disclosures.
SOURCE: Keisuke H et al. Free Radic Biol Med. 2019;133:193-9.
according to an extensive literature review.
Although the mechanisms underlying the hepatocellular carcinoma development are not fully understood, it is known that oxidative stress exists to a greater degree in hepatitis C virus (HCV) infection, compared with other inflammatory liver diseases. Such stress has been proposed as a major mechanism of liver injury in patients with chronic HCV, the authors reported in Free Radical Biology and Medicine.
Patients with HCV have significant hepatocellular mitochondrial alterations, and iron accumulation is also a well-known characteristic in patients with chronic HCV. Such alterations in mitochondria and iron accumulation are closely related to oxidative stress, since the mitochondria are the main site of reactive oxygen species generation, and iron produces hydroxy radicals via the Fenton reaction, according to the review.
“The greatest concern is whether mitochondrial damage and iron metabolic dysregulation persist even after HCV eradication and to what extent such pathological conditions affect the development of HCC. Determining the molecular signaling that underlies the mitophagy induced by iron depletion is another topic of interest and is expected to lead to potential therapeutic approaches for multiple diseases,” the researchers concluded.
Support was from the Research Program on Hepatitis from the Japan Agency for Medical Research and Development. The authors reported no disclosures.
SOURCE: Keisuke H et al. Free Radic Biol Med. 2019;133:193-9.
FROM FREE RADICAL BIOLOGY AND MEDICINE
Blunted cardiac reserve strongly predicts incident hepatorenal syndrome
VIENNA – Patients with cirrhosis and undergoing work-up for a possible liver transplant who had low cardiac reserve had a nearly fourfold increased rate of developing hepatorenal syndrome (HRS) during an average 17 months of follow-up, compared with patients with normal cardiac reserve, in a review of 560 Australian patients assessed for a possible liver transplant.
The findings suggest that patients with advanced liver disease should routinely undergo assessment for low cardiac reserve, Anoop N. Koshy, MBBS, said at the meeting sponsored by the European Association for the Study of the Liver.
said Dr. Koshy, a cardiologist with Austin Health in Melbourne. “We propose that it’s not low cardiac output that leads to HRS, but an inability of patients to increase their cardiac output” in response to usual stimuli.
The findings also add to the concerns about using nonselective beta-blocker drugs in patients with cirrhosis because of the potential of these drugs to further blunt increases in cardiac output; they also suggest that noninvasive measurement of cardiac reserve could identify patients with low cardiac reserve who could benefit from closer monitoring and new approaches to treatment, he suggested. About 10%-30% of patients with cirrhosis develop HRS, and the new finding suggests a noninvasive way to identify patients with the highest risk for this complication.
The study included 560 consecutive patients with cirrhosis and end-stage liver disease who were awaiting a liver transplant at the Victoria Liver Transplant Unit in Melbourne and underwent assessment by stress echocardiography using low-dose dobutamine (10 mcg/kg per min) during 2010-2017 as part of their standard pretransplant work-up. Exclusion of patients with known cardiac disease prior to their stress echo examination or incomplete measurement left 488 patients, of whom 424 were free from HRS at baseline. Patients with HRS at the time of their stress echo assessment had on average a cardiac output that was about 25% higher than patients without HRS, a statistically significant difference driven by both a significantly increased heart rate and stroke volume.
Among the 424 patients free from HRS at baseline, 85 developed HRS during an average 17-month follow-up. Patients with low cardiac reserve after dobutamine challenge, defined as an increase in cardiac output of less than 25%, had a 3.9-fold increased rate of incident HRS during follow-up, compared with patients who had a larger rise in their cardiac output after adjustment for several clinical and echocardiographic baseline variables, Dr. Koshy reported. In this analysis low cardiac reserve was the strongest predictor of subsequent HRS, he said.
Dr. Koshy had no disclosures.
SOURCE: Koshy AN et al. J Hepatol. 2019 April;70(1):e56.
Cardiovascular abnormalities develop in patients with advanced chronic liver disease to produce a hyperdynamic systemic circulation with splanchnic vasodilation, decreased systemic vascular resistance, and increased cardiac output (J Hepatol. 2018;69[4]:958-60). The term cirrhotic cardiomyopathy has also been used for the changes of systolic dysfunction with impaired cardiac contractile response to stress and altered diastolic relaxation that develops in patients with cirrhosis (J Hepatol. 2010;53[1]:179-90).
In this study by Dr. Koshy and colleagues, the inability to increase cardiac output during dobutamine stress echo (DSE) was associated with a greater subsequent risk for hepatorenal syndrome (J Hepatol. 2019;70:e56).
All patients in the study were undergoing pretransplant liver evaluation. Those who developed hepatorenal syndrome (HRS) in follow-up had a higher mean cardiac output with a reduction of the increase in cardiac output that follows dobutamine administration when compared with those who did not develop HRS. A multivariate analysis that adjusted for age, gender, MELD score, and Child-Pugh score found that “impaired contractile response was the strongest predictor of hepatorenal syndrome” as defined by a less than 22% increase in cardiac output following dobutamine. Overall, 40% of those with impaired contractile reserve developed hepatorenal syndrome, compared with 25% of those with normal contractile reserve following dobutamine (P = .006). It is of interest that cirrhotic patients with HRS at the time of initial dobutamine stress echo had a 25% higher average cardiac output than those without HRS. Patients who subsequently developed hepatorenal syndrome also had higher average cardiac output at initial evaluation than those who did not.
This study continues to raise important questions about the role of cardiovascular dysfunction and the risk of hepatorenal syndrome. Additional studies seem warranted to evaluate progression of cardiac changes and dobutamine response throughout follow-up of end-stage liver disease patients, including at the development of hepatorenal syndrome. Studies of HRS patients with specific associations such as sepsis, spontaneous bacterial peritonitis, and gastrointestinal bleeding may also provide information on the role of systolic and diastolic dysfunction during such events.
This article also draws attention to “concerns about using nonselective beta-blocker drugs in patients with cirrhosis.” Current data indicate that nonselective beta-blockers reduce all-cause mortality and the risk of first variceal hemorrhage in patients with advanced liver disease (Hepatology. 2019;69[4]:1657-75). Until we have studies that reveal a clear association between beta-blockers and development of hepatorenal syndrome, I will continue to recommend the use of beta-blockers in cirrhotic patients at risk for first variceal hemorrhage.
Rowen K. Zetterman, MD, is dean emeritus of the Creighton University School of Medicine in Omaha, Neb. He serves as the Associate Vice Chancellor for Academic Affairs and the Associate Vice Chancellor for Planning at the University of Nebraska Medical Center in Omaha. Dr. Zetterman, a gastroenterologist and hepatologist, is also a member of the editorial advisory board of Internal Medicine News.
Cardiovascular abnormalities develop in patients with advanced chronic liver disease to produce a hyperdynamic systemic circulation with splanchnic vasodilation, decreased systemic vascular resistance, and increased cardiac output (J Hepatol. 2018;69[4]:958-60). The term cirrhotic cardiomyopathy has also been used for the changes of systolic dysfunction with impaired cardiac contractile response to stress and altered diastolic relaxation that develops in patients with cirrhosis (J Hepatol. 2010;53[1]:179-90).
In this study by Dr. Koshy and colleagues, the inability to increase cardiac output during dobutamine stress echo (DSE) was associated with a greater subsequent risk for hepatorenal syndrome (J Hepatol. 2019;70:e56).
All patients in the study were undergoing pretransplant liver evaluation. Those who developed hepatorenal syndrome (HRS) in follow-up had a higher mean cardiac output with a reduction of the increase in cardiac output that follows dobutamine administration when compared with those who did not develop HRS. A multivariate analysis that adjusted for age, gender, MELD score, and Child-Pugh score found that “impaired contractile response was the strongest predictor of hepatorenal syndrome” as defined by a less than 22% increase in cardiac output following dobutamine. Overall, 40% of those with impaired contractile reserve developed hepatorenal syndrome, compared with 25% of those with normal contractile reserve following dobutamine (P = .006). It is of interest that cirrhotic patients with HRS at the time of initial dobutamine stress echo had a 25% higher average cardiac output than those without HRS. Patients who subsequently developed hepatorenal syndrome also had higher average cardiac output at initial evaluation than those who did not.
This study continues to raise important questions about the role of cardiovascular dysfunction and the risk of hepatorenal syndrome. Additional studies seem warranted to evaluate progression of cardiac changes and dobutamine response throughout follow-up of end-stage liver disease patients, including at the development of hepatorenal syndrome. Studies of HRS patients with specific associations such as sepsis, spontaneous bacterial peritonitis, and gastrointestinal bleeding may also provide information on the role of systolic and diastolic dysfunction during such events.
This article also draws attention to “concerns about using nonselective beta-blocker drugs in patients with cirrhosis.” Current data indicate that nonselective beta-blockers reduce all-cause mortality and the risk of first variceal hemorrhage in patients with advanced liver disease (Hepatology. 2019;69[4]:1657-75). Until we have studies that reveal a clear association between beta-blockers and development of hepatorenal syndrome, I will continue to recommend the use of beta-blockers in cirrhotic patients at risk for first variceal hemorrhage.
Rowen K. Zetterman, MD, is dean emeritus of the Creighton University School of Medicine in Omaha, Neb. He serves as the Associate Vice Chancellor for Academic Affairs and the Associate Vice Chancellor for Planning at the University of Nebraska Medical Center in Omaha. Dr. Zetterman, a gastroenterologist and hepatologist, is also a member of the editorial advisory board of Internal Medicine News.
Cardiovascular abnormalities develop in patients with advanced chronic liver disease to produce a hyperdynamic systemic circulation with splanchnic vasodilation, decreased systemic vascular resistance, and increased cardiac output (J Hepatol. 2018;69[4]:958-60). The term cirrhotic cardiomyopathy has also been used for the changes of systolic dysfunction with impaired cardiac contractile response to stress and altered diastolic relaxation that develops in patients with cirrhosis (J Hepatol. 2010;53[1]:179-90).
In this study by Dr. Koshy and colleagues, the inability to increase cardiac output during dobutamine stress echo (DSE) was associated with a greater subsequent risk for hepatorenal syndrome (J Hepatol. 2019;70:e56).
All patients in the study were undergoing pretransplant liver evaluation. Those who developed hepatorenal syndrome (HRS) in follow-up had a higher mean cardiac output with a reduction of the increase in cardiac output that follows dobutamine administration when compared with those who did not develop HRS. A multivariate analysis that adjusted for age, gender, MELD score, and Child-Pugh score found that “impaired contractile response was the strongest predictor of hepatorenal syndrome” as defined by a less than 22% increase in cardiac output following dobutamine. Overall, 40% of those with impaired contractile reserve developed hepatorenal syndrome, compared with 25% of those with normal contractile reserve following dobutamine (P = .006). It is of interest that cirrhotic patients with HRS at the time of initial dobutamine stress echo had a 25% higher average cardiac output than those without HRS. Patients who subsequently developed hepatorenal syndrome also had higher average cardiac output at initial evaluation than those who did not.
This study continues to raise important questions about the role of cardiovascular dysfunction and the risk of hepatorenal syndrome. Additional studies seem warranted to evaluate progression of cardiac changes and dobutamine response throughout follow-up of end-stage liver disease patients, including at the development of hepatorenal syndrome. Studies of HRS patients with specific associations such as sepsis, spontaneous bacterial peritonitis, and gastrointestinal bleeding may also provide information on the role of systolic and diastolic dysfunction during such events.
This article also draws attention to “concerns about using nonselective beta-blocker drugs in patients with cirrhosis.” Current data indicate that nonselective beta-blockers reduce all-cause mortality and the risk of first variceal hemorrhage in patients with advanced liver disease (Hepatology. 2019;69[4]:1657-75). Until we have studies that reveal a clear association between beta-blockers and development of hepatorenal syndrome, I will continue to recommend the use of beta-blockers in cirrhotic patients at risk for first variceal hemorrhage.
Rowen K. Zetterman, MD, is dean emeritus of the Creighton University School of Medicine in Omaha, Neb. He serves as the Associate Vice Chancellor for Academic Affairs and the Associate Vice Chancellor for Planning at the University of Nebraska Medical Center in Omaha. Dr. Zetterman, a gastroenterologist and hepatologist, is also a member of the editorial advisory board of Internal Medicine News.
VIENNA – Patients with cirrhosis and undergoing work-up for a possible liver transplant who had low cardiac reserve had a nearly fourfold increased rate of developing hepatorenal syndrome (HRS) during an average 17 months of follow-up, compared with patients with normal cardiac reserve, in a review of 560 Australian patients assessed for a possible liver transplant.
The findings suggest that patients with advanced liver disease should routinely undergo assessment for low cardiac reserve, Anoop N. Koshy, MBBS, said at the meeting sponsored by the European Association for the Study of the Liver.
said Dr. Koshy, a cardiologist with Austin Health in Melbourne. “We propose that it’s not low cardiac output that leads to HRS, but an inability of patients to increase their cardiac output” in response to usual stimuli.
The findings also add to the concerns about using nonselective beta-blocker drugs in patients with cirrhosis because of the potential of these drugs to further blunt increases in cardiac output; they also suggest that noninvasive measurement of cardiac reserve could identify patients with low cardiac reserve who could benefit from closer monitoring and new approaches to treatment, he suggested. About 10%-30% of patients with cirrhosis develop HRS, and the new finding suggests a noninvasive way to identify patients with the highest risk for this complication.
The study included 560 consecutive patients with cirrhosis and end-stage liver disease who were awaiting a liver transplant at the Victoria Liver Transplant Unit in Melbourne and underwent assessment by stress echocardiography using low-dose dobutamine (10 mcg/kg per min) during 2010-2017 as part of their standard pretransplant work-up. Exclusion of patients with known cardiac disease prior to their stress echo examination or incomplete measurement left 488 patients, of whom 424 were free from HRS at baseline. Patients with HRS at the time of their stress echo assessment had on average a cardiac output that was about 25% higher than patients without HRS, a statistically significant difference driven by both a significantly increased heart rate and stroke volume.
Among the 424 patients free from HRS at baseline, 85 developed HRS during an average 17-month follow-up. Patients with low cardiac reserve after dobutamine challenge, defined as an increase in cardiac output of less than 25%, had a 3.9-fold increased rate of incident HRS during follow-up, compared with patients who had a larger rise in their cardiac output after adjustment for several clinical and echocardiographic baseline variables, Dr. Koshy reported. In this analysis low cardiac reserve was the strongest predictor of subsequent HRS, he said.
Dr. Koshy had no disclosures.
SOURCE: Koshy AN et al. J Hepatol. 2019 April;70(1):e56.
VIENNA – Patients with cirrhosis and undergoing work-up for a possible liver transplant who had low cardiac reserve had a nearly fourfold increased rate of developing hepatorenal syndrome (HRS) during an average 17 months of follow-up, compared with patients with normal cardiac reserve, in a review of 560 Australian patients assessed for a possible liver transplant.
The findings suggest that patients with advanced liver disease should routinely undergo assessment for low cardiac reserve, Anoop N. Koshy, MBBS, said at the meeting sponsored by the European Association for the Study of the Liver.
said Dr. Koshy, a cardiologist with Austin Health in Melbourne. “We propose that it’s not low cardiac output that leads to HRS, but an inability of patients to increase their cardiac output” in response to usual stimuli.
The findings also add to the concerns about using nonselective beta-blocker drugs in patients with cirrhosis because of the potential of these drugs to further blunt increases in cardiac output; they also suggest that noninvasive measurement of cardiac reserve could identify patients with low cardiac reserve who could benefit from closer monitoring and new approaches to treatment, he suggested. About 10%-30% of patients with cirrhosis develop HRS, and the new finding suggests a noninvasive way to identify patients with the highest risk for this complication.
The study included 560 consecutive patients with cirrhosis and end-stage liver disease who were awaiting a liver transplant at the Victoria Liver Transplant Unit in Melbourne and underwent assessment by stress echocardiography using low-dose dobutamine (10 mcg/kg per min) during 2010-2017 as part of their standard pretransplant work-up. Exclusion of patients with known cardiac disease prior to their stress echo examination or incomplete measurement left 488 patients, of whom 424 were free from HRS at baseline. Patients with HRS at the time of their stress echo assessment had on average a cardiac output that was about 25% higher than patients without HRS, a statistically significant difference driven by both a significantly increased heart rate and stroke volume.
Among the 424 patients free from HRS at baseline, 85 developed HRS during an average 17-month follow-up. Patients with low cardiac reserve after dobutamine challenge, defined as an increase in cardiac output of less than 25%, had a 3.9-fold increased rate of incident HRS during follow-up, compared with patients who had a larger rise in their cardiac output after adjustment for several clinical and echocardiographic baseline variables, Dr. Koshy reported. In this analysis low cardiac reserve was the strongest predictor of subsequent HRS, he said.
Dr. Koshy had no disclosures.
SOURCE: Koshy AN et al. J Hepatol. 2019 April;70(1):e56.
REPORTING FROM ILC 2019
MicroRNA-375 may be key to fibrolamellar carcinoma
Up-regulation of microRNA-375 may be a future therapeutic strategy for patients with fibrolamellar carcinoma (FLC), according to investigators.
Analysis of primary FLC tumors showed that microRNA-375 was the most abnormal microRNA, down-regulated 27-fold, reported lead author Timothy A. Dinh, MD, of the University of North Carolina at Chapel Hill and his colleagues. Overexpression of microRNA-375 in an FLC cell line suppressed cell migration and proliferation, hinting at therapeutic potential.
“Overall, our results show that miR-375 [microRNA-375] functions as a tumor suppressor in FLC and points toward future therapies based on miR-375 mimics that may provide a viable option for patients,” the investigators wrote in a Cellular and Molecular Gastroenterology and Hepatology.
FLC is an uncommon liver cancer in adolescents and young adults. Currently, surgery is the only effective treatment; unfortunately, many patients have metastatic disease at the time of diagnosis, disallowing surgical cure.
“The lack of knowledge of underlying disease mechanisms has hindered our understanding of this cancer and the development of novel therapeutics for FLC patients,” the investigators wrote.
Previous research has shown that almost all patients with FLC (80%-100%) have a heterozygous deletion mutation on chromosome 19. However, it is not a loss of genetic information that incites neoplasia; instead, the deletion causes a fusion of genes DNAJB1 and PRKACA. This fusion is capable of triggering liver tumors, a phenomenon confirmed through mouse models. The present study built on these findings, along with recent awareness that several microRNAs are dysregulated in FLC, compared with normal liver tissue.
First, the investigators performed small RNA-sequencing in six primary FLC tumors from The Cancer Genome Atlas (TCGA). They found that 30 microRNAs were up-regulated and 46 microRNAs were down-regulated. Among these, microRNA-375 was the most significantly down-regulated, at 27-fold (P = .009). To confirm these findings, the same process was repeated in 18 independent samples, with the same result.
The investigators explained that, in addition to magnitude of down-regulation, microRNA-375 deserved attention for at least three other reasons: It is down-regulated in numerous cancer types, it directly targets known oncogenes, and it is suppressed by the cyclic adenosine monophosphate (cAMP)/protein kinase A (PKA) signaling axis, which is overactive in FLC.
Further testing confirmed that microRNA-375 was consistently more down-regulated in samples of FLC, by up to 20-fold, than it was in nonmalignant liver tissue. To confirm that loss of microRNA-375 expression occurred in FLC tumor cells instead of other cell types, such as stromal cells, a patient-derived xenograft of FLC was compared with liver lineage cells, including adult hepatocytes, hepatoblasts, hepatic stem cells, and biliary tree stem cells. Again, microRNA-375 was down-regulated most in the FLC cells. Additional comparisons within the TCGA showed that microRNA-375 was more down-regulated in FLC than 21 out of 22 other tumor types (second only to melanoma).
“Taken together with our findings from primary tumor tissue, our results strongly suggest that miR-375 may function as a tumor suppressor in FLC,” the investigators wrote.
Having confirmed the ubiquity of microRNA-375 down-regulation in FLC, the investigators turned to the relationship between the DNAJB1-PRKACA fusion and microRNA-375. Using two methods – gene deletion with CRISPR/Cas9 and transposon injection – the investigators found that creating the DNAJB1-PRKACA fusion in cells of mice was sufficient to suppress microRNA-375 expression, which supports a downstream relationship.
Finally, the investigators showed that treating an FLC cell line with an microRNA-375 mimic suppressed the Hippo signaling pathway, including connective tissue growth factor (CTGF) and yes-associated protein 1 (YAP1). These events translated to reduced cellular activity, which suggests that up-regulating microRNA-375 could, indeed, control FLC.
“Importantly, introduction of a miR-375 mimic significantly reduced colony formation, EdU incorporation, and migration, indicative of reduced survival, proliferation, and metastatic potential, respectively,” the investigators wrote.
“With RNA-based therapies showing increasing promise, miR-375–based therapies merit future consideration for FLC therapeutics,” they concluded.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute on Alcohol Abuse and Alcoholism, and the Fibrolamellar Cancer Foundation. The investigators declared no conflicts of interest.
SOURCE: Dinh TA et al. Cell Mol Gastroenterol Hepatol. 2019 Feb 11. doi: 10.1016/j.jcmgh.2019.01.008.
For several decades, fibrolamellar carcinoma was the enigmatic liver cancer. Neither etiology nor molecular causes were known. The breakthrough came when tumor sequencing identified a hitherto undescribed fusion gene in 15 out of 15 patients analyzed: A small portion of the heat shock protein DNAJB1 was fused to the catalytic subunit of protein kinase A (PKA, or PRKACA), which retained full kinase activity.
Underscoring the significance of this finding, the DNAJB1-PRKACA fusion gene was shown to be sufficient to elicit tumors similar to human fibrolamellar carcinoma when engineered in mice. The absence of conspicuous codriver genes makes DNAJB1-PRKACA a primary candidate for therapeutic target. However, PKA inhibitors would be problematic in the clinic because of the vital physiological functions of PKA. Consequently, the hunt is on to decipher the oncogenic signaling pathways emanating from DNAJB1-PRKACA with the hope to identify alternative targets among its downstream mediators.
In this work, the Sethupathy lab performed a thorough study on abnormally regulated microRNAs in fibrolamellar carcinoma tumors. Intriguingly, they identified several microRNAs controlled by DNAJB1-PRKACA that have oncogenic or tumor suppressor function in other cancers. In particular, the tumor suppressor microRNA-375 was massively down-regulated by DNAJB1-PRKACA. Furthermore, introducing a microRNA-375 mimic in fibrolamellar cancer cells suppressed proliferation and motility. Important studies like this open up new avenues aiming to manipulate cancer microRNAs as alternative or complementary approaches for targeting DNAJB1-PRKACA signaling in the highly fatal fibrolamellar carcinoma.
Morten Frödin, MSc, PhD, is an associate professor and group leader of the Biotech Research and Innovation Centre, University of Copenhagen.
For several decades, fibrolamellar carcinoma was the enigmatic liver cancer. Neither etiology nor molecular causes were known. The breakthrough came when tumor sequencing identified a hitherto undescribed fusion gene in 15 out of 15 patients analyzed: A small portion of the heat shock protein DNAJB1 was fused to the catalytic subunit of protein kinase A (PKA, or PRKACA), which retained full kinase activity.
Underscoring the significance of this finding, the DNAJB1-PRKACA fusion gene was shown to be sufficient to elicit tumors similar to human fibrolamellar carcinoma when engineered in mice. The absence of conspicuous codriver genes makes DNAJB1-PRKACA a primary candidate for therapeutic target. However, PKA inhibitors would be problematic in the clinic because of the vital physiological functions of PKA. Consequently, the hunt is on to decipher the oncogenic signaling pathways emanating from DNAJB1-PRKACA with the hope to identify alternative targets among its downstream mediators.
In this work, the Sethupathy lab performed a thorough study on abnormally regulated microRNAs in fibrolamellar carcinoma tumors. Intriguingly, they identified several microRNAs controlled by DNAJB1-PRKACA that have oncogenic or tumor suppressor function in other cancers. In particular, the tumor suppressor microRNA-375 was massively down-regulated by DNAJB1-PRKACA. Furthermore, introducing a microRNA-375 mimic in fibrolamellar cancer cells suppressed proliferation and motility. Important studies like this open up new avenues aiming to manipulate cancer microRNAs as alternative or complementary approaches for targeting DNAJB1-PRKACA signaling in the highly fatal fibrolamellar carcinoma.
Morten Frödin, MSc, PhD, is an associate professor and group leader of the Biotech Research and Innovation Centre, University of Copenhagen.
For several decades, fibrolamellar carcinoma was the enigmatic liver cancer. Neither etiology nor molecular causes were known. The breakthrough came when tumor sequencing identified a hitherto undescribed fusion gene in 15 out of 15 patients analyzed: A small portion of the heat shock protein DNAJB1 was fused to the catalytic subunit of protein kinase A (PKA, or PRKACA), which retained full kinase activity.
Underscoring the significance of this finding, the DNAJB1-PRKACA fusion gene was shown to be sufficient to elicit tumors similar to human fibrolamellar carcinoma when engineered in mice. The absence of conspicuous codriver genes makes DNAJB1-PRKACA a primary candidate for therapeutic target. However, PKA inhibitors would be problematic in the clinic because of the vital physiological functions of PKA. Consequently, the hunt is on to decipher the oncogenic signaling pathways emanating from DNAJB1-PRKACA with the hope to identify alternative targets among its downstream mediators.
In this work, the Sethupathy lab performed a thorough study on abnormally regulated microRNAs in fibrolamellar carcinoma tumors. Intriguingly, they identified several microRNAs controlled by DNAJB1-PRKACA that have oncogenic or tumor suppressor function in other cancers. In particular, the tumor suppressor microRNA-375 was massively down-regulated by DNAJB1-PRKACA. Furthermore, introducing a microRNA-375 mimic in fibrolamellar cancer cells suppressed proliferation and motility. Important studies like this open up new avenues aiming to manipulate cancer microRNAs as alternative or complementary approaches for targeting DNAJB1-PRKACA signaling in the highly fatal fibrolamellar carcinoma.
Morten Frödin, MSc, PhD, is an associate professor and group leader of the Biotech Research and Innovation Centre, University of Copenhagen.
Up-regulation of microRNA-375 may be a future therapeutic strategy for patients with fibrolamellar carcinoma (FLC), according to investigators.
Analysis of primary FLC tumors showed that microRNA-375 was the most abnormal microRNA, down-regulated 27-fold, reported lead author Timothy A. Dinh, MD, of the University of North Carolina at Chapel Hill and his colleagues. Overexpression of microRNA-375 in an FLC cell line suppressed cell migration and proliferation, hinting at therapeutic potential.
“Overall, our results show that miR-375 [microRNA-375] functions as a tumor suppressor in FLC and points toward future therapies based on miR-375 mimics that may provide a viable option for patients,” the investigators wrote in a Cellular and Molecular Gastroenterology and Hepatology.
FLC is an uncommon liver cancer in adolescents and young adults. Currently, surgery is the only effective treatment; unfortunately, many patients have metastatic disease at the time of diagnosis, disallowing surgical cure.
“The lack of knowledge of underlying disease mechanisms has hindered our understanding of this cancer and the development of novel therapeutics for FLC patients,” the investigators wrote.
Previous research has shown that almost all patients with FLC (80%-100%) have a heterozygous deletion mutation on chromosome 19. However, it is not a loss of genetic information that incites neoplasia; instead, the deletion causes a fusion of genes DNAJB1 and PRKACA. This fusion is capable of triggering liver tumors, a phenomenon confirmed through mouse models. The present study built on these findings, along with recent awareness that several microRNAs are dysregulated in FLC, compared with normal liver tissue.
First, the investigators performed small RNA-sequencing in six primary FLC tumors from The Cancer Genome Atlas (TCGA). They found that 30 microRNAs were up-regulated and 46 microRNAs were down-regulated. Among these, microRNA-375 was the most significantly down-regulated, at 27-fold (P = .009). To confirm these findings, the same process was repeated in 18 independent samples, with the same result.
The investigators explained that, in addition to magnitude of down-regulation, microRNA-375 deserved attention for at least three other reasons: It is down-regulated in numerous cancer types, it directly targets known oncogenes, and it is suppressed by the cyclic adenosine monophosphate (cAMP)/protein kinase A (PKA) signaling axis, which is overactive in FLC.
Further testing confirmed that microRNA-375 was consistently more down-regulated in samples of FLC, by up to 20-fold, than it was in nonmalignant liver tissue. To confirm that loss of microRNA-375 expression occurred in FLC tumor cells instead of other cell types, such as stromal cells, a patient-derived xenograft of FLC was compared with liver lineage cells, including adult hepatocytes, hepatoblasts, hepatic stem cells, and biliary tree stem cells. Again, microRNA-375 was down-regulated most in the FLC cells. Additional comparisons within the TCGA showed that microRNA-375 was more down-regulated in FLC than 21 out of 22 other tumor types (second only to melanoma).
“Taken together with our findings from primary tumor tissue, our results strongly suggest that miR-375 may function as a tumor suppressor in FLC,” the investigators wrote.
Having confirmed the ubiquity of microRNA-375 down-regulation in FLC, the investigators turned to the relationship between the DNAJB1-PRKACA fusion and microRNA-375. Using two methods – gene deletion with CRISPR/Cas9 and transposon injection – the investigators found that creating the DNAJB1-PRKACA fusion in cells of mice was sufficient to suppress microRNA-375 expression, which supports a downstream relationship.
Finally, the investigators showed that treating an FLC cell line with an microRNA-375 mimic suppressed the Hippo signaling pathway, including connective tissue growth factor (CTGF) and yes-associated protein 1 (YAP1). These events translated to reduced cellular activity, which suggests that up-regulating microRNA-375 could, indeed, control FLC.
“Importantly, introduction of a miR-375 mimic significantly reduced colony formation, EdU incorporation, and migration, indicative of reduced survival, proliferation, and metastatic potential, respectively,” the investigators wrote.
“With RNA-based therapies showing increasing promise, miR-375–based therapies merit future consideration for FLC therapeutics,” they concluded.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute on Alcohol Abuse and Alcoholism, and the Fibrolamellar Cancer Foundation. The investigators declared no conflicts of interest.
SOURCE: Dinh TA et al. Cell Mol Gastroenterol Hepatol. 2019 Feb 11. doi: 10.1016/j.jcmgh.2019.01.008.
Up-regulation of microRNA-375 may be a future therapeutic strategy for patients with fibrolamellar carcinoma (FLC), according to investigators.
Analysis of primary FLC tumors showed that microRNA-375 was the most abnormal microRNA, down-regulated 27-fold, reported lead author Timothy A. Dinh, MD, of the University of North Carolina at Chapel Hill and his colleagues. Overexpression of microRNA-375 in an FLC cell line suppressed cell migration and proliferation, hinting at therapeutic potential.
“Overall, our results show that miR-375 [microRNA-375] functions as a tumor suppressor in FLC and points toward future therapies based on miR-375 mimics that may provide a viable option for patients,” the investigators wrote in a Cellular and Molecular Gastroenterology and Hepatology.
FLC is an uncommon liver cancer in adolescents and young adults. Currently, surgery is the only effective treatment; unfortunately, many patients have metastatic disease at the time of diagnosis, disallowing surgical cure.
“The lack of knowledge of underlying disease mechanisms has hindered our understanding of this cancer and the development of novel therapeutics for FLC patients,” the investigators wrote.
Previous research has shown that almost all patients with FLC (80%-100%) have a heterozygous deletion mutation on chromosome 19. However, it is not a loss of genetic information that incites neoplasia; instead, the deletion causes a fusion of genes DNAJB1 and PRKACA. This fusion is capable of triggering liver tumors, a phenomenon confirmed through mouse models. The present study built on these findings, along with recent awareness that several microRNAs are dysregulated in FLC, compared with normal liver tissue.
First, the investigators performed small RNA-sequencing in six primary FLC tumors from The Cancer Genome Atlas (TCGA). They found that 30 microRNAs were up-regulated and 46 microRNAs were down-regulated. Among these, microRNA-375 was the most significantly down-regulated, at 27-fold (P = .009). To confirm these findings, the same process was repeated in 18 independent samples, with the same result.
The investigators explained that, in addition to magnitude of down-regulation, microRNA-375 deserved attention for at least three other reasons: It is down-regulated in numerous cancer types, it directly targets known oncogenes, and it is suppressed by the cyclic adenosine monophosphate (cAMP)/protein kinase A (PKA) signaling axis, which is overactive in FLC.
Further testing confirmed that microRNA-375 was consistently more down-regulated in samples of FLC, by up to 20-fold, than it was in nonmalignant liver tissue. To confirm that loss of microRNA-375 expression occurred in FLC tumor cells instead of other cell types, such as stromal cells, a patient-derived xenograft of FLC was compared with liver lineage cells, including adult hepatocytes, hepatoblasts, hepatic stem cells, and biliary tree stem cells. Again, microRNA-375 was down-regulated most in the FLC cells. Additional comparisons within the TCGA showed that microRNA-375 was more down-regulated in FLC than 21 out of 22 other tumor types (second only to melanoma).
“Taken together with our findings from primary tumor tissue, our results strongly suggest that miR-375 may function as a tumor suppressor in FLC,” the investigators wrote.
Having confirmed the ubiquity of microRNA-375 down-regulation in FLC, the investigators turned to the relationship between the DNAJB1-PRKACA fusion and microRNA-375. Using two methods – gene deletion with CRISPR/Cas9 and transposon injection – the investigators found that creating the DNAJB1-PRKACA fusion in cells of mice was sufficient to suppress microRNA-375 expression, which supports a downstream relationship.
Finally, the investigators showed that treating an FLC cell line with an microRNA-375 mimic suppressed the Hippo signaling pathway, including connective tissue growth factor (CTGF) and yes-associated protein 1 (YAP1). These events translated to reduced cellular activity, which suggests that up-regulating microRNA-375 could, indeed, control FLC.
“Importantly, introduction of a miR-375 mimic significantly reduced colony formation, EdU incorporation, and migration, indicative of reduced survival, proliferation, and metastatic potential, respectively,” the investigators wrote.
“With RNA-based therapies showing increasing promise, miR-375–based therapies merit future consideration for FLC therapeutics,” they concluded.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute on Alcohol Abuse and Alcoholism, and the Fibrolamellar Cancer Foundation. The investigators declared no conflicts of interest.
SOURCE: Dinh TA et al. Cell Mol Gastroenterol Hepatol. 2019 Feb 11. doi: 10.1016/j.jcmgh.2019.01.008.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Liver steatosis common in English young adults
VIENNA – The prevalence of liver steatosis among unselected English young adults was 21% in a study of just over 4,000 people. The prevalence of apparent liver fibrosis was 2.4%, and among the 21% with steatosis, nearly half – 10% of the studied cohort – had severe, S3 steatosis.
The prevalence of steatosis, a marker of nonalcoholic fatty liver disease (NAFLD), seemed to be linked with obesity. Among the 79% of the study group who had no steatosis the obesity prevalence was 6%, compared with a 26% prevalence among those with S1 steatosis, a 33% obesity rate among those with S2 steatosis, and a 57% obesity prevalence among those with S3 steatosis, Kushala Abeysekera, MBBS, said at the meeting sponsored by the European Association for the Study of the Liver.
He and his associates determined these prevalence rates in a population that excluded people who reported consuming what was deemed “excessive” alcohol use.
Another notable finding was that 1,874 of the same people had undergone ultrasound assessment for NAFLD when they were 18 years old, and that assessment found a prevalence of 2.5% (J Clin Endocrinol Metab. 2014 March;99[3]:e410-7), which meant that during the subsequent 6 years prevalence of NAFLD jumped nearly 900%.
Both the 2014 report and the current study used people who had been enrolled in the Avon Longitudinal Study of Parents and Children, a prospective population-based study that began by recruiting a cohort of more than 14,000 pregnant women during 1991-1992, and then followed the more than 13,000 children who resulted from those pregnancies. The study reported by Dr. Abeysekera focused on 4,021 of these children – now young adults – who responded to an invitation to participate in this follow-up, a number that then reduced to 3,600 with informative transient elastography results that quantified fibrosis, and 3,768 with valid Controlled Attenuated Parameter scores from elastography that reflected steatosis extent. Transient elastography is a noninvasive method of measuring liver stiffness using ultrasound and an elastic shear wave (Clin Mol Hepatol. 2012 June;18[2]:163-73).
“To the best of my knowledge, this is the only study that has assessed NAFLD in young adults using transient elastography,” said Dr. Abeysekera, an epidemiologist at the University of Bristol (England).
After subtracting from the study cohort people with excessive alcohol use, the study had transient elastography data from 3,277 24-year-olds that could calculate steatosis severity, and data from 3,128 that could quantify fibrosis.
The analysis also showed a statistically significant link between sex and the presence and severity of steatosis. Among women, 18% had steatosis, including 7% with S3 steatosis, defined as involving at least two-thirds of the liver. Among men, 26% had some degree of steatosis and 14% had the most severe form.
The presence of more severe liver fibrosis also showed a strong link to obesity. The eight people identified with F4 fibrosis (with cirrhosis) had a median body mass index of 32 kg/m2, compared with a median body mass index of 25 kg/m2 or less among those either without fibrosis or with a milder form of F1, F2, or F3 fibrosis.
Dr. Abeysekera reported no disclosures.
VIENNA – The prevalence of liver steatosis among unselected English young adults was 21% in a study of just over 4,000 people. The prevalence of apparent liver fibrosis was 2.4%, and among the 21% with steatosis, nearly half – 10% of the studied cohort – had severe, S3 steatosis.
The prevalence of steatosis, a marker of nonalcoholic fatty liver disease (NAFLD), seemed to be linked with obesity. Among the 79% of the study group who had no steatosis the obesity prevalence was 6%, compared with a 26% prevalence among those with S1 steatosis, a 33% obesity rate among those with S2 steatosis, and a 57% obesity prevalence among those with S3 steatosis, Kushala Abeysekera, MBBS, said at the meeting sponsored by the European Association for the Study of the Liver.
He and his associates determined these prevalence rates in a population that excluded people who reported consuming what was deemed “excessive” alcohol use.
Another notable finding was that 1,874 of the same people had undergone ultrasound assessment for NAFLD when they were 18 years old, and that assessment found a prevalence of 2.5% (J Clin Endocrinol Metab. 2014 March;99[3]:e410-7), which meant that during the subsequent 6 years prevalence of NAFLD jumped nearly 900%.
Both the 2014 report and the current study used people who had been enrolled in the Avon Longitudinal Study of Parents and Children, a prospective population-based study that began by recruiting a cohort of more than 14,000 pregnant women during 1991-1992, and then followed the more than 13,000 children who resulted from those pregnancies. The study reported by Dr. Abeysekera focused on 4,021 of these children – now young adults – who responded to an invitation to participate in this follow-up, a number that then reduced to 3,600 with informative transient elastography results that quantified fibrosis, and 3,768 with valid Controlled Attenuated Parameter scores from elastography that reflected steatosis extent. Transient elastography is a noninvasive method of measuring liver stiffness using ultrasound and an elastic shear wave (Clin Mol Hepatol. 2012 June;18[2]:163-73).
“To the best of my knowledge, this is the only study that has assessed NAFLD in young adults using transient elastography,” said Dr. Abeysekera, an epidemiologist at the University of Bristol (England).
After subtracting from the study cohort people with excessive alcohol use, the study had transient elastography data from 3,277 24-year-olds that could calculate steatosis severity, and data from 3,128 that could quantify fibrosis.
The analysis also showed a statistically significant link between sex and the presence and severity of steatosis. Among women, 18% had steatosis, including 7% with S3 steatosis, defined as involving at least two-thirds of the liver. Among men, 26% had some degree of steatosis and 14% had the most severe form.
The presence of more severe liver fibrosis also showed a strong link to obesity. The eight people identified with F4 fibrosis (with cirrhosis) had a median body mass index of 32 kg/m2, compared with a median body mass index of 25 kg/m2 or less among those either without fibrosis or with a milder form of F1, F2, or F3 fibrosis.
Dr. Abeysekera reported no disclosures.
VIENNA – The prevalence of liver steatosis among unselected English young adults was 21% in a study of just over 4,000 people. The prevalence of apparent liver fibrosis was 2.4%, and among the 21% with steatosis, nearly half – 10% of the studied cohort – had severe, S3 steatosis.
The prevalence of steatosis, a marker of nonalcoholic fatty liver disease (NAFLD), seemed to be linked with obesity. Among the 79% of the study group who had no steatosis the obesity prevalence was 6%, compared with a 26% prevalence among those with S1 steatosis, a 33% obesity rate among those with S2 steatosis, and a 57% obesity prevalence among those with S3 steatosis, Kushala Abeysekera, MBBS, said at the meeting sponsored by the European Association for the Study of the Liver.
He and his associates determined these prevalence rates in a population that excluded people who reported consuming what was deemed “excessive” alcohol use.
Another notable finding was that 1,874 of the same people had undergone ultrasound assessment for NAFLD when they were 18 years old, and that assessment found a prevalence of 2.5% (J Clin Endocrinol Metab. 2014 March;99[3]:e410-7), which meant that during the subsequent 6 years prevalence of NAFLD jumped nearly 900%.
Both the 2014 report and the current study used people who had been enrolled in the Avon Longitudinal Study of Parents and Children, a prospective population-based study that began by recruiting a cohort of more than 14,000 pregnant women during 1991-1992, and then followed the more than 13,000 children who resulted from those pregnancies. The study reported by Dr. Abeysekera focused on 4,021 of these children – now young adults – who responded to an invitation to participate in this follow-up, a number that then reduced to 3,600 with informative transient elastography results that quantified fibrosis, and 3,768 with valid Controlled Attenuated Parameter scores from elastography that reflected steatosis extent. Transient elastography is a noninvasive method of measuring liver stiffness using ultrasound and an elastic shear wave (Clin Mol Hepatol. 2012 June;18[2]:163-73).
“To the best of my knowledge, this is the only study that has assessed NAFLD in young adults using transient elastography,” said Dr. Abeysekera, an epidemiologist at the University of Bristol (England).
After subtracting from the study cohort people with excessive alcohol use, the study had transient elastography data from 3,277 24-year-olds that could calculate steatosis severity, and data from 3,128 that could quantify fibrosis.
The analysis also showed a statistically significant link between sex and the presence and severity of steatosis. Among women, 18% had steatosis, including 7% with S3 steatosis, defined as involving at least two-thirds of the liver. Among men, 26% had some degree of steatosis and 14% had the most severe form.
The presence of more severe liver fibrosis also showed a strong link to obesity. The eight people identified with F4 fibrosis (with cirrhosis) had a median body mass index of 32 kg/m2, compared with a median body mass index of 25 kg/m2 or less among those either without fibrosis or with a milder form of F1, F2, or F3 fibrosis.
Dr. Abeysekera reported no disclosures.
REPORTING FROM ILC 2019