User login
Obeticholic acid reversed NASH liver fibrosis in phase 3 trial
VIENNA – making obeticholic acid the first agent proven to improve the course of this disease.
“There is no doubt that with these data we have changed the treatment” of nonalcoholic steatohepatitis (NASH), Zobair M. Younossi, MD, of Inova Fairfax Medical Campus in Falls Church, Va., said at the meeting sponsored by the European Association for the Study of the Liver. “We are at a watershed moment” in NASH treatment, Dr. Younossi added in a video interview.
Until now “we have had no effective treatments for NASH. This is the first success in a phase 3 trial; obeticholic acid looks very promising,” commented Philip N. Newsome, PhD, professor of experimental hepatology at the University of Birmingham (England).
Obeticholic acid (OCA), an agonist of the farnesoid X receptor, already has Food and Drug Administration marketing approval for the indication of primary biliary cholangitis, a much rarer disease than NASH.
The REGENERATE (Randomized Global Phase 3 Study to Evaluate the Impact on NASH With Fibrosis of Obeticholic Acid Treatment) trial has so far enrolled 931 patients at about 350 sites in 20 countries, including the United States, and followed them during 18 months of treatment, the prespecified time for an interim analysis. The study enrolled adults with biopsy-proven NASH and generally focused on patients with either stage 2 or 3 liver fibrosis and a nonalcoholic fatty liver disease activity score of at least 4. Enrolled patients averaged about 55 years old, slightly more than half the enrolled patients had type 2 diabetes, and more than half had stage 3 fibrosis.
The study design included two coprimary endpoints, and specified that a statistically significant finding for either outcome meant a positive trial result, but the design also prespecified that the benefit would need to meet a stringent definition of statistical significance, compared with placebo patients, with a P value of no more than .01. REGENERATE tested two different OCA dosages, 10 mg or 25 mg, once daily. The results showed a trend for benefit from the smaller dosage, but these effects did not achieve statistical significance.
For the primary endpoint of regression of liver fibrosis by at least one stage with no worsening of NASH the intention-to-treat analysis showed after 18 months a 13% rate with placebo, a 21% rate with the 10-mg dosage, and a 23% rate with the 25-mg dosage, a statistically significant improvement over placebo for the higher dosage.
The second primary endpoint was resolution of NASH without worsening liver fibrosis, which occurred in 8% of placebo patients, 11% of patients on 10 mg OCA/day and 12% of those on 25 mg/day. The differences between each of the active groups and the controls were not statistically significant for this endpoint.
Among the 931 enrolled patients 668 (72%) actually received treatment fully consistent with the study protocol, and among these per-protocol patients the benefit from 25 mg/day OCA was even more striking: a 28% rate of fibrosis regression, compared with 13% in the control patients. Regression by at least two fibrotic stages occurred in 5% of placebo patients and 13% of those on 25 mg/day OCA. Many treated patients also showed normalizations of liver enzyme levels.
Adverse events on OCA were mostly mild or moderate, with similar rates of serious adverse events in the OCA groups and in control patients. The most common adverse effect on OCA treatment was pruritus, a previously described effect, reported by 51% of patients on the 25 mg/day dosage and by 19% of control patients.
REGENERATE will continue until a goal level of endpoint events occur, and may eventually enroll as many as 2,400 patients and extend for a few more years. By then, Dr. Younossi said, he hopes that an analysis will be possible of “harder” endpoints than fibrosis, such as development of cirrhosis. He noted, however, that the FDA has designated fibrosis regression as a valid surrogate endpoint for assessing treatment efficacy for NASH.
Already on the U.S. market, a single 10-mg OCA pill currently retails for almost $230; a 25-mg formulation is not currently marketed. Dr. Younossi said that subsequent studies will assess the cost-effectiveness of OCA treatment for NASH. He also hopes that further study of patient characteristics will identify which NASH patients are most likely to respond to OCA. Eventually, OCA may be part of a multidrug strategy for treating this disease, Dr. Younossi said.
REGENERATE was sponsored by Intercept, the company that markets obeticholic acid (Ocaliva). Dr. Younossi is a consultant to and has received research funding from Intercept. He has also been a consultant to Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Novartis, Novo Nordisk, Quest, Siemens, Terns Pharmaceutical, and Viking Therapeutics. Dr. Newsome has been a consultant or speaker for Intercept as well as Boehringer Ingelheim, Dignity Sciences, Johnson & Johnson, Novo Nordisk, and Shire, and he has received research funding from Pharmaxis and Boehringer Ingelheim.
VIENNA – making obeticholic acid the first agent proven to improve the course of this disease.
“There is no doubt that with these data we have changed the treatment” of nonalcoholic steatohepatitis (NASH), Zobair M. Younossi, MD, of Inova Fairfax Medical Campus in Falls Church, Va., said at the meeting sponsored by the European Association for the Study of the Liver. “We are at a watershed moment” in NASH treatment, Dr. Younossi added in a video interview.
Until now “we have had no effective treatments for NASH. This is the first success in a phase 3 trial; obeticholic acid looks very promising,” commented Philip N. Newsome, PhD, professor of experimental hepatology at the University of Birmingham (England).
Obeticholic acid (OCA), an agonist of the farnesoid X receptor, already has Food and Drug Administration marketing approval for the indication of primary biliary cholangitis, a much rarer disease than NASH.
The REGENERATE (Randomized Global Phase 3 Study to Evaluate the Impact on NASH With Fibrosis of Obeticholic Acid Treatment) trial has so far enrolled 931 patients at about 350 sites in 20 countries, including the United States, and followed them during 18 months of treatment, the prespecified time for an interim analysis. The study enrolled adults with biopsy-proven NASH and generally focused on patients with either stage 2 or 3 liver fibrosis and a nonalcoholic fatty liver disease activity score of at least 4. Enrolled patients averaged about 55 years old, slightly more than half the enrolled patients had type 2 diabetes, and more than half had stage 3 fibrosis.
The study design included two coprimary endpoints, and specified that a statistically significant finding for either outcome meant a positive trial result, but the design also prespecified that the benefit would need to meet a stringent definition of statistical significance, compared with placebo patients, with a P value of no more than .01. REGENERATE tested two different OCA dosages, 10 mg or 25 mg, once daily. The results showed a trend for benefit from the smaller dosage, but these effects did not achieve statistical significance.
For the primary endpoint of regression of liver fibrosis by at least one stage with no worsening of NASH the intention-to-treat analysis showed after 18 months a 13% rate with placebo, a 21% rate with the 10-mg dosage, and a 23% rate with the 25-mg dosage, a statistically significant improvement over placebo for the higher dosage.
The second primary endpoint was resolution of NASH without worsening liver fibrosis, which occurred in 8% of placebo patients, 11% of patients on 10 mg OCA/day and 12% of those on 25 mg/day. The differences between each of the active groups and the controls were not statistically significant for this endpoint.
Among the 931 enrolled patients 668 (72%) actually received treatment fully consistent with the study protocol, and among these per-protocol patients the benefit from 25 mg/day OCA was even more striking: a 28% rate of fibrosis regression, compared with 13% in the control patients. Regression by at least two fibrotic stages occurred in 5% of placebo patients and 13% of those on 25 mg/day OCA. Many treated patients also showed normalizations of liver enzyme levels.
Adverse events on OCA were mostly mild or moderate, with similar rates of serious adverse events in the OCA groups and in control patients. The most common adverse effect on OCA treatment was pruritus, a previously described effect, reported by 51% of patients on the 25 mg/day dosage and by 19% of control patients.
REGENERATE will continue until a goal level of endpoint events occur, and may eventually enroll as many as 2,400 patients and extend for a few more years. By then, Dr. Younossi said, he hopes that an analysis will be possible of “harder” endpoints than fibrosis, such as development of cirrhosis. He noted, however, that the FDA has designated fibrosis regression as a valid surrogate endpoint for assessing treatment efficacy for NASH.
Already on the U.S. market, a single 10-mg OCA pill currently retails for almost $230; a 25-mg formulation is not currently marketed. Dr. Younossi said that subsequent studies will assess the cost-effectiveness of OCA treatment for NASH. He also hopes that further study of patient characteristics will identify which NASH patients are most likely to respond to OCA. Eventually, OCA may be part of a multidrug strategy for treating this disease, Dr. Younossi said.
REGENERATE was sponsored by Intercept, the company that markets obeticholic acid (Ocaliva). Dr. Younossi is a consultant to and has received research funding from Intercept. He has also been a consultant to Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Novartis, Novo Nordisk, Quest, Siemens, Terns Pharmaceutical, and Viking Therapeutics. Dr. Newsome has been a consultant or speaker for Intercept as well as Boehringer Ingelheim, Dignity Sciences, Johnson & Johnson, Novo Nordisk, and Shire, and he has received research funding from Pharmaxis and Boehringer Ingelheim.
VIENNA – making obeticholic acid the first agent proven to improve the course of this disease.
“There is no doubt that with these data we have changed the treatment” of nonalcoholic steatohepatitis (NASH), Zobair M. Younossi, MD, of Inova Fairfax Medical Campus in Falls Church, Va., said at the meeting sponsored by the European Association for the Study of the Liver. “We are at a watershed moment” in NASH treatment, Dr. Younossi added in a video interview.
Until now “we have had no effective treatments for NASH. This is the first success in a phase 3 trial; obeticholic acid looks very promising,” commented Philip N. Newsome, PhD, professor of experimental hepatology at the University of Birmingham (England).
Obeticholic acid (OCA), an agonist of the farnesoid X receptor, already has Food and Drug Administration marketing approval for the indication of primary biliary cholangitis, a much rarer disease than NASH.
The REGENERATE (Randomized Global Phase 3 Study to Evaluate the Impact on NASH With Fibrosis of Obeticholic Acid Treatment) trial has so far enrolled 931 patients at about 350 sites in 20 countries, including the United States, and followed them during 18 months of treatment, the prespecified time for an interim analysis. The study enrolled adults with biopsy-proven NASH and generally focused on patients with either stage 2 or 3 liver fibrosis and a nonalcoholic fatty liver disease activity score of at least 4. Enrolled patients averaged about 55 years old, slightly more than half the enrolled patients had type 2 diabetes, and more than half had stage 3 fibrosis.
The study design included two coprimary endpoints, and specified that a statistically significant finding for either outcome meant a positive trial result, but the design also prespecified that the benefit would need to meet a stringent definition of statistical significance, compared with placebo patients, with a P value of no more than .01. REGENERATE tested two different OCA dosages, 10 mg or 25 mg, once daily. The results showed a trend for benefit from the smaller dosage, but these effects did not achieve statistical significance.
For the primary endpoint of regression of liver fibrosis by at least one stage with no worsening of NASH the intention-to-treat analysis showed after 18 months a 13% rate with placebo, a 21% rate with the 10-mg dosage, and a 23% rate with the 25-mg dosage, a statistically significant improvement over placebo for the higher dosage.
The second primary endpoint was resolution of NASH without worsening liver fibrosis, which occurred in 8% of placebo patients, 11% of patients on 10 mg OCA/day and 12% of those on 25 mg/day. The differences between each of the active groups and the controls were not statistically significant for this endpoint.
Among the 931 enrolled patients 668 (72%) actually received treatment fully consistent with the study protocol, and among these per-protocol patients the benefit from 25 mg/day OCA was even more striking: a 28% rate of fibrosis regression, compared with 13% in the control patients. Regression by at least two fibrotic stages occurred in 5% of placebo patients and 13% of those on 25 mg/day OCA. Many treated patients also showed normalizations of liver enzyme levels.
Adverse events on OCA were mostly mild or moderate, with similar rates of serious adverse events in the OCA groups and in control patients. The most common adverse effect on OCA treatment was pruritus, a previously described effect, reported by 51% of patients on the 25 mg/day dosage and by 19% of control patients.
REGENERATE will continue until a goal level of endpoint events occur, and may eventually enroll as many as 2,400 patients and extend for a few more years. By then, Dr. Younossi said, he hopes that an analysis will be possible of “harder” endpoints than fibrosis, such as development of cirrhosis. He noted, however, that the FDA has designated fibrosis regression as a valid surrogate endpoint for assessing treatment efficacy for NASH.
Already on the U.S. market, a single 10-mg OCA pill currently retails for almost $230; a 25-mg formulation is not currently marketed. Dr. Younossi said that subsequent studies will assess the cost-effectiveness of OCA treatment for NASH. He also hopes that further study of patient characteristics will identify which NASH patients are most likely to respond to OCA. Eventually, OCA may be part of a multidrug strategy for treating this disease, Dr. Younossi said.
REGENERATE was sponsored by Intercept, the company that markets obeticholic acid (Ocaliva). Dr. Younossi is a consultant to and has received research funding from Intercept. He has also been a consultant to Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Novartis, Novo Nordisk, Quest, Siemens, Terns Pharmaceutical, and Viking Therapeutics. Dr. Newsome has been a consultant or speaker for Intercept as well as Boehringer Ingelheim, Dignity Sciences, Johnson & Johnson, Novo Nordisk, and Shire, and he has received research funding from Pharmaxis and Boehringer Ingelheim.
REPORTING FROM ILC 2019
Research coalition issues plan for curing hepatitis B virus
VIENNA – They hope either to have a cure or to have made substantial progress toward this goal over the next 10 years.
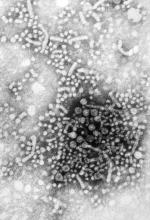
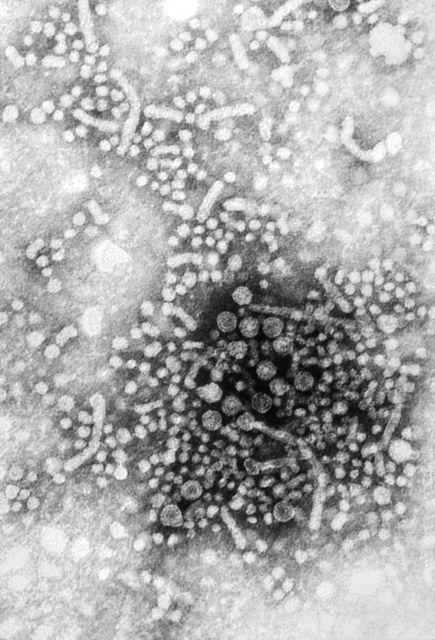
Treatments already are on the market that effectively inhibit hepatitis B replication in infected patients (and an effective preventive vaccine also exists). Still, these treatments are not curative, and for the vast majority of patients treatment must continue indefinitely, while their risk for liver cancer and their virally induced immune system abnormalities remain, Peter A. Revill, PhD, said during a press briefing that introduced a strategy for hepatitis B virus (HBV) cure development from the International Coalition to Eliminate HBV. Concurrently with the briefing session, the strategy appeared in an article published online (Lancet Gastroenterol Hepatol. 2019 Apr 10. doi: 10.1016/s2468-1253(19)30119-0).
The way forward will likely be a “two-pronged approach or restoring immune responses and targeting the virus,” Dr. Revill, head of molecular virology at the Doherty Institute in Melbourne, said in a video interview.
The new strategy recognizes the huge challenge of devising a treatment that produces a total cure that includes elimination of all traces of viral DNA from patients and for the immediate future focuses on the goal of functional cure. The term functional cure means a sustained period without detectable HBV surface antigen or HBV DNA in a patient’s serum, as well as suppressed virus release. Another feature of a functional cure would be a halt to progression of liver disease, replaced by liver regeneration, said Anna S. Lok, MD, professor of medicine and director of clinical hepatology at the University of Michigan, Ann Arbor, and a member of the strategy-writing group. She and her colleagues who wrote the strategy foresee the need for drug combinations with agents that can hit multiple viral targets as well as agents that restore normal immune function.
Several novel drug classes aimed at new viral targets, such as capsid inhibitors, are in various stages of clinical development, said Fabien Zoulim, MD, head of the gastroenterology and hepatology service at the Red Cross Hospital in Lyon, France, and another member of the writing panel. “We have many drug candidates” that use novel approaches to further restrict viral growth, roughly 50 agents in phase 1 and 2 studies, he said during the press briefing, held during the meeting sponsored by the European Association for the Study of the Liver. The other, immunologic aspect of the two-part cure strategy – restoring the “exhausted” HBV-specific T-cell population and stimulating production of neutralizing antibody to HBV – remains hypothetical right now, however. “It’s a concept that needs development,” Dr. Zoulim said.
A reason members of the coalition are optimistic about eventual prospects for a cure is that currently about 1% of patients on HBV antiviral treatments have a functional cure after relatively brief treatment, and the percentage of cured patients plateaus at about 10% among those who remain on current HBV antiviral drugs for several years. In addition, a substantial fraction of patients spontaneously resolve their HBV infection without any treatment. Experts estimate that more than 1 billion people worldwide have been infected by HBV and then later had their infection clear “naturally,” said Dr. Revill. But the mechanism by which this happens is currently a mystery. “We don’t know how or why” so many infected people are “cured” naturally, Dr. Revill admitted, but it gives him and his colleagues hope that the numbers can expand once more and better treatments for HBV infection are available.
VIENNA – They hope either to have a cure or to have made substantial progress toward this goal over the next 10 years.
Treatments already are on the market that effectively inhibit hepatitis B replication in infected patients (and an effective preventive vaccine also exists). Still, these treatments are not curative, and for the vast majority of patients treatment must continue indefinitely, while their risk for liver cancer and their virally induced immune system abnormalities remain, Peter A. Revill, PhD, said during a press briefing that introduced a strategy for hepatitis B virus (HBV) cure development from the International Coalition to Eliminate HBV. Concurrently with the briefing session, the strategy appeared in an article published online (Lancet Gastroenterol Hepatol. 2019 Apr 10. doi: 10.1016/s2468-1253(19)30119-0).
The way forward will likely be a “two-pronged approach or restoring immune responses and targeting the virus,” Dr. Revill, head of molecular virology at the Doherty Institute in Melbourne, said in a video interview.
The new strategy recognizes the huge challenge of devising a treatment that produces a total cure that includes elimination of all traces of viral DNA from patients and for the immediate future focuses on the goal of functional cure. The term functional cure means a sustained period without detectable HBV surface antigen or HBV DNA in a patient’s serum, as well as suppressed virus release. Another feature of a functional cure would be a halt to progression of liver disease, replaced by liver regeneration, said Anna S. Lok, MD, professor of medicine and director of clinical hepatology at the University of Michigan, Ann Arbor, and a member of the strategy-writing group. She and her colleagues who wrote the strategy foresee the need for drug combinations with agents that can hit multiple viral targets as well as agents that restore normal immune function.
Several novel drug classes aimed at new viral targets, such as capsid inhibitors, are in various stages of clinical development, said Fabien Zoulim, MD, head of the gastroenterology and hepatology service at the Red Cross Hospital in Lyon, France, and another member of the writing panel. “We have many drug candidates” that use novel approaches to further restrict viral growth, roughly 50 agents in phase 1 and 2 studies, he said during the press briefing, held during the meeting sponsored by the European Association for the Study of the Liver. The other, immunologic aspect of the two-part cure strategy – restoring the “exhausted” HBV-specific T-cell population and stimulating production of neutralizing antibody to HBV – remains hypothetical right now, however. “It’s a concept that needs development,” Dr. Zoulim said.
A reason members of the coalition are optimistic about eventual prospects for a cure is that currently about 1% of patients on HBV antiviral treatments have a functional cure after relatively brief treatment, and the percentage of cured patients plateaus at about 10% among those who remain on current HBV antiviral drugs for several years. In addition, a substantial fraction of patients spontaneously resolve their HBV infection without any treatment. Experts estimate that more than 1 billion people worldwide have been infected by HBV and then later had their infection clear “naturally,” said Dr. Revill. But the mechanism by which this happens is currently a mystery. “We don’t know how or why” so many infected people are “cured” naturally, Dr. Revill admitted, but it gives him and his colleagues hope that the numbers can expand once more and better treatments for HBV infection are available.
VIENNA – They hope either to have a cure or to have made substantial progress toward this goal over the next 10 years.
Treatments already are on the market that effectively inhibit hepatitis B replication in infected patients (and an effective preventive vaccine also exists). Still, these treatments are not curative, and for the vast majority of patients treatment must continue indefinitely, while their risk for liver cancer and their virally induced immune system abnormalities remain, Peter A. Revill, PhD, said during a press briefing that introduced a strategy for hepatitis B virus (HBV) cure development from the International Coalition to Eliminate HBV. Concurrently with the briefing session, the strategy appeared in an article published online (Lancet Gastroenterol Hepatol. 2019 Apr 10. doi: 10.1016/s2468-1253(19)30119-0).
The way forward will likely be a “two-pronged approach or restoring immune responses and targeting the virus,” Dr. Revill, head of molecular virology at the Doherty Institute in Melbourne, said in a video interview.
The new strategy recognizes the huge challenge of devising a treatment that produces a total cure that includes elimination of all traces of viral DNA from patients and for the immediate future focuses on the goal of functional cure. The term functional cure means a sustained period without detectable HBV surface antigen or HBV DNA in a patient’s serum, as well as suppressed virus release. Another feature of a functional cure would be a halt to progression of liver disease, replaced by liver regeneration, said Anna S. Lok, MD, professor of medicine and director of clinical hepatology at the University of Michigan, Ann Arbor, and a member of the strategy-writing group. She and her colleagues who wrote the strategy foresee the need for drug combinations with agents that can hit multiple viral targets as well as agents that restore normal immune function.
Several novel drug classes aimed at new viral targets, such as capsid inhibitors, are in various stages of clinical development, said Fabien Zoulim, MD, head of the gastroenterology and hepatology service at the Red Cross Hospital in Lyon, France, and another member of the writing panel. “We have many drug candidates” that use novel approaches to further restrict viral growth, roughly 50 agents in phase 1 and 2 studies, he said during the press briefing, held during the meeting sponsored by the European Association for the Study of the Liver. The other, immunologic aspect of the two-part cure strategy – restoring the “exhausted” HBV-specific T-cell population and stimulating production of neutralizing antibody to HBV – remains hypothetical right now, however. “It’s a concept that needs development,” Dr. Zoulim said.
A reason members of the coalition are optimistic about eventual prospects for a cure is that currently about 1% of patients on HBV antiviral treatments have a functional cure after relatively brief treatment, and the percentage of cured patients plateaus at about 10% among those who remain on current HBV antiviral drugs for several years. In addition, a substantial fraction of patients spontaneously resolve their HBV infection without any treatment. Experts estimate that more than 1 billion people worldwide have been infected by HBV and then later had their infection clear “naturally,” said Dr. Revill. But the mechanism by which this happens is currently a mystery. “We don’t know how or why” so many infected people are “cured” naturally, Dr. Revill admitted, but it gives him and his colleagues hope that the numbers can expand once more and better treatments for HBV infection are available.
REPORTING FROM ILC 2019
An HCV-infected population showed gaps in HBV testing, vaccination, and care
Assessment of a large cohort of hepatitis C virus (HCV)–infected patients revealed a high prevalence of current or past hepatitis B virus. However, within this cohort, there were notable gaps in HBV testing, directed care, and vaccination, according to Aaron M. Harris, MD, of the Centers for Disease Control and Prevention.
Dr. Harris and his colleagues abstracted patient-level data from the Grady Health System EHR in August 2016 to create an HCV patient registry. They found that, among 4,224 HCV-infected patients, 3,629 (86%) had test results for the hepatitis B surface antigen (HBsAg), with 43 (1.2%) being HBsAg positive.
“Our results identified a gap in care as a minority of HBsAg-positive patients with HCV coinfection received HBV DNA and/or e-antigen [HBeAg] testing,” the researchers stated.
Overall, only 2,342 (55.4%) patients had test results for all three HBV serologic markers. Among these, 789 (33.7%) were anti-HBc positive only, 678 (28.9%) were anti-HBc/anti-HBs positive, 190 (8.1%) were anti-HBs positive only, and 642 (27.4%) were HBV susceptible. In addition, only 50% of the HBV-susceptible patients received at least one dose of hepatitis B vaccine, according to the report published in Vaccine.
“Strategies are needed to increase hepatitis B testing, linkage to hepatitis B–directed care of HBV/HCV-coinfected patients, and to increase uptake in hepatitis B vaccination for HCV-infected patients within the Grady Health System,” the researchers concluded.
The study was funded by the CDC and the authors reported that they had no conflicts.
SOURCE: Harris AM et al. Vaccine. 2019;37:2188-93.
Assessment of a large cohort of hepatitis C virus (HCV)–infected patients revealed a high prevalence of current or past hepatitis B virus. However, within this cohort, there were notable gaps in HBV testing, directed care, and vaccination, according to Aaron M. Harris, MD, of the Centers for Disease Control and Prevention.
Dr. Harris and his colleagues abstracted patient-level data from the Grady Health System EHR in August 2016 to create an HCV patient registry. They found that, among 4,224 HCV-infected patients, 3,629 (86%) had test results for the hepatitis B surface antigen (HBsAg), with 43 (1.2%) being HBsAg positive.
“Our results identified a gap in care as a minority of HBsAg-positive patients with HCV coinfection received HBV DNA and/or e-antigen [HBeAg] testing,” the researchers stated.
Overall, only 2,342 (55.4%) patients had test results for all three HBV serologic markers. Among these, 789 (33.7%) were anti-HBc positive only, 678 (28.9%) were anti-HBc/anti-HBs positive, 190 (8.1%) were anti-HBs positive only, and 642 (27.4%) were HBV susceptible. In addition, only 50% of the HBV-susceptible patients received at least one dose of hepatitis B vaccine, according to the report published in Vaccine.
“Strategies are needed to increase hepatitis B testing, linkage to hepatitis B–directed care of HBV/HCV-coinfected patients, and to increase uptake in hepatitis B vaccination for HCV-infected patients within the Grady Health System,” the researchers concluded.
The study was funded by the CDC and the authors reported that they had no conflicts.
SOURCE: Harris AM et al. Vaccine. 2019;37:2188-93.
Assessment of a large cohort of hepatitis C virus (HCV)–infected patients revealed a high prevalence of current or past hepatitis B virus. However, within this cohort, there were notable gaps in HBV testing, directed care, and vaccination, according to Aaron M. Harris, MD, of the Centers for Disease Control and Prevention.
Dr. Harris and his colleagues abstracted patient-level data from the Grady Health System EHR in August 2016 to create an HCV patient registry. They found that, among 4,224 HCV-infected patients, 3,629 (86%) had test results for the hepatitis B surface antigen (HBsAg), with 43 (1.2%) being HBsAg positive.
“Our results identified a gap in care as a minority of HBsAg-positive patients with HCV coinfection received HBV DNA and/or e-antigen [HBeAg] testing,” the researchers stated.
Overall, only 2,342 (55.4%) patients had test results for all three HBV serologic markers. Among these, 789 (33.7%) were anti-HBc positive only, 678 (28.9%) were anti-HBc/anti-HBs positive, 190 (8.1%) were anti-HBs positive only, and 642 (27.4%) were HBV susceptible. In addition, only 50% of the HBV-susceptible patients received at least one dose of hepatitis B vaccine, according to the report published in Vaccine.
“Strategies are needed to increase hepatitis B testing, linkage to hepatitis B–directed care of HBV/HCV-coinfected patients, and to increase uptake in hepatitis B vaccination for HCV-infected patients within the Grady Health System,” the researchers concluded.
The study was funded by the CDC and the authors reported that they had no conflicts.
SOURCE: Harris AM et al. Vaccine. 2019;37:2188-93.
FROM VACCINE
Future of NASH care means multiple targets, multiple providers, expert says
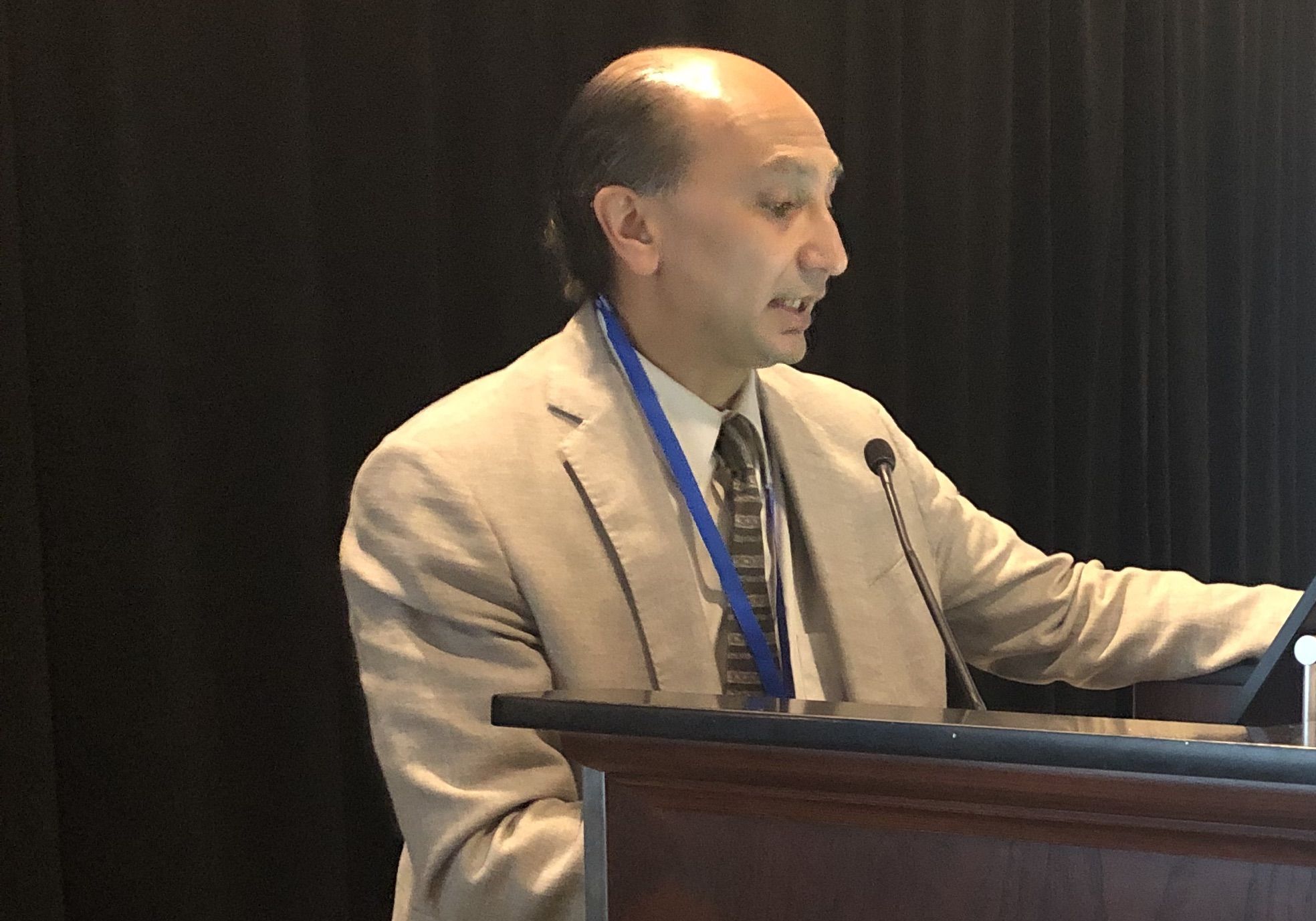
PHILADELPHIA – While current treatment options are limited for patients with nonalcoholic steatohepatitis (NASH), a number of potential agents in clinical trials, Zobair M. Younossi, MD, MPH, said here at the 6th annual Digestive Diseases: New Advances conference.
With agents currently available and those to come, the future will be focused on long-term management of NASH as a chronic disease in specialized centers, according to Dr. Younossi, chairman in the department of medicine at Inova Fairfax Hospital and vice president for research at Inova Health System, both in Falls Church, Va.
“We are not going to be able to cure NASH – we need to manage it,” Dr. Younossi said in a podium presentation. “NASH will be managed like type 2 diabetes. It’s not going to be treated like hepatitis C.”
Current treatment options are limited, with no Food and Drug Administration–approved options, and just two agents, vitamin E and pioglitazone, supported by guidance from the American Association for the Study of Liver Diseases (AASLD), Dr. Younossi said.
Public health interventions are needed to address the obesity and type 2 diabetes that are “the root of this disease,” Dr. Younossi said at the meeting, which was jointly provided by Rutgers and Global Academy for Medical Education.
Current AASLD guidance is based on studies suggesting that weight loss in the 3%-5% range may improve steatosis, and a 7%-10% weight loss can improve most histologic features of NASH, including fibrosis.
“The problem is that this is very hard to achieve,” Dr. Younossi said, adding that it is also hard to maintain. In a 2011 meta-analysis of clinical trials for reduction in nonalcoholic fatty liver disease, only a small minority of patients were able to maintain weight loss.
Bariatric surgery may be “very effective” for weight loss in the right patients, with some trials showing a proportion of patients maintaining improvement at 5-year follow-up, he said.
Exercise alone might prevent or reduce steatosis, but its effects on other aspects of liver histology, such as fibrosis, remain unknown, Dr. Younossi said.
Pioglitazone improves liver histology in patients with biopsy-proven NASH, although the benefits and risks, including potential adverse effects such as bone loss, diastolic dysfunction, or weight gain, should be discussed with each individual patient, he said.
Dr. Younossi highlighted randomized phase 3 trials for several agents that could figure into the treatment paradigm of NASH in the future by targeting different promoters of NASH and fibrosis progression. One of those was elafibranor, which targets the PPAR alpha/gamma pathways and is being evaluated versus placebo in NASH patients in the phase 3 RESOLVE-IT study. In a post hoc analysis of a previous randomized trial, the treatment resolved NASH without fibrosis worsening.
Other agents being evaluated in phase 3 trials include the CCR2/CCR5 receptor blocker cenicriviroc, the FXR agonist obeticholic acid, and the ASK-1 inhibitor selonsertib, Dr. Younossi said.
Optimal NASH care in the future may be based on targeting multiple such pathways, with patients increasingly treated at specialized centers that incorporate not only hepatologists, but also diabetes experts, dietitians, and exercise specialists.
“My own belief is that you have to treat this in the long term and also in a multidisciplinary sort of approach,” he said.
Dr. Younossi indicated that he is a consultant for Gilead, Intercept, Bristol-Myers Squibb, Novo Nordisk, Viking, Terms, Shionogi, AbbVie, Merck, and Novartis.
Global Academy and this news organization are owned by the same parent company.
PHILADELPHIA – While current treatment options are limited for patients with nonalcoholic steatohepatitis (NASH), a number of potential agents in clinical trials, Zobair M. Younossi, MD, MPH, said here at the 6th annual Digestive Diseases: New Advances conference.
With agents currently available and those to come, the future will be focused on long-term management of NASH as a chronic disease in specialized centers, according to Dr. Younossi, chairman in the department of medicine at Inova Fairfax Hospital and vice president for research at Inova Health System, both in Falls Church, Va.
“We are not going to be able to cure NASH – we need to manage it,” Dr. Younossi said in a podium presentation. “NASH will be managed like type 2 diabetes. It’s not going to be treated like hepatitis C.”
Current treatment options are limited, with no Food and Drug Administration–approved options, and just two agents, vitamin E and pioglitazone, supported by guidance from the American Association for the Study of Liver Diseases (AASLD), Dr. Younossi said.
Public health interventions are needed to address the obesity and type 2 diabetes that are “the root of this disease,” Dr. Younossi said at the meeting, which was jointly provided by Rutgers and Global Academy for Medical Education.
Current AASLD guidance is based on studies suggesting that weight loss in the 3%-5% range may improve steatosis, and a 7%-10% weight loss can improve most histologic features of NASH, including fibrosis.
“The problem is that this is very hard to achieve,” Dr. Younossi said, adding that it is also hard to maintain. In a 2011 meta-analysis of clinical trials for reduction in nonalcoholic fatty liver disease, only a small minority of patients were able to maintain weight loss.
Bariatric surgery may be “very effective” for weight loss in the right patients, with some trials showing a proportion of patients maintaining improvement at 5-year follow-up, he said.
Exercise alone might prevent or reduce steatosis, but its effects on other aspects of liver histology, such as fibrosis, remain unknown, Dr. Younossi said.
Pioglitazone improves liver histology in patients with biopsy-proven NASH, although the benefits and risks, including potential adverse effects such as bone loss, diastolic dysfunction, or weight gain, should be discussed with each individual patient, he said.
Dr. Younossi highlighted randomized phase 3 trials for several agents that could figure into the treatment paradigm of NASH in the future by targeting different promoters of NASH and fibrosis progression. One of those was elafibranor, which targets the PPAR alpha/gamma pathways and is being evaluated versus placebo in NASH patients in the phase 3 RESOLVE-IT study. In a post hoc analysis of a previous randomized trial, the treatment resolved NASH without fibrosis worsening.
Other agents being evaluated in phase 3 trials include the CCR2/CCR5 receptor blocker cenicriviroc, the FXR agonist obeticholic acid, and the ASK-1 inhibitor selonsertib, Dr. Younossi said.
Optimal NASH care in the future may be based on targeting multiple such pathways, with patients increasingly treated at specialized centers that incorporate not only hepatologists, but also diabetes experts, dietitians, and exercise specialists.
“My own belief is that you have to treat this in the long term and also in a multidisciplinary sort of approach,” he said.
Dr. Younossi indicated that he is a consultant for Gilead, Intercept, Bristol-Myers Squibb, Novo Nordisk, Viking, Terms, Shionogi, AbbVie, Merck, and Novartis.
Global Academy and this news organization are owned by the same parent company.
PHILADELPHIA – While current treatment options are limited for patients with nonalcoholic steatohepatitis (NASH), a number of potential agents in clinical trials, Zobair M. Younossi, MD, MPH, said here at the 6th annual Digestive Diseases: New Advances conference.
With agents currently available and those to come, the future will be focused on long-term management of NASH as a chronic disease in specialized centers, according to Dr. Younossi, chairman in the department of medicine at Inova Fairfax Hospital and vice president for research at Inova Health System, both in Falls Church, Va.
“We are not going to be able to cure NASH – we need to manage it,” Dr. Younossi said in a podium presentation. “NASH will be managed like type 2 diabetes. It’s not going to be treated like hepatitis C.”
Current treatment options are limited, with no Food and Drug Administration–approved options, and just two agents, vitamin E and pioglitazone, supported by guidance from the American Association for the Study of Liver Diseases (AASLD), Dr. Younossi said.
Public health interventions are needed to address the obesity and type 2 diabetes that are “the root of this disease,” Dr. Younossi said at the meeting, which was jointly provided by Rutgers and Global Academy for Medical Education.
Current AASLD guidance is based on studies suggesting that weight loss in the 3%-5% range may improve steatosis, and a 7%-10% weight loss can improve most histologic features of NASH, including fibrosis.
“The problem is that this is very hard to achieve,” Dr. Younossi said, adding that it is also hard to maintain. In a 2011 meta-analysis of clinical trials for reduction in nonalcoholic fatty liver disease, only a small minority of patients were able to maintain weight loss.
Bariatric surgery may be “very effective” for weight loss in the right patients, with some trials showing a proportion of patients maintaining improvement at 5-year follow-up, he said.
Exercise alone might prevent or reduce steatosis, but its effects on other aspects of liver histology, such as fibrosis, remain unknown, Dr. Younossi said.
Pioglitazone improves liver histology in patients with biopsy-proven NASH, although the benefits and risks, including potential adverse effects such as bone loss, diastolic dysfunction, or weight gain, should be discussed with each individual patient, he said.
Dr. Younossi highlighted randomized phase 3 trials for several agents that could figure into the treatment paradigm of NASH in the future by targeting different promoters of NASH and fibrosis progression. One of those was elafibranor, which targets the PPAR alpha/gamma pathways and is being evaluated versus placebo in NASH patients in the phase 3 RESOLVE-IT study. In a post hoc analysis of a previous randomized trial, the treatment resolved NASH without fibrosis worsening.
Other agents being evaluated in phase 3 trials include the CCR2/CCR5 receptor blocker cenicriviroc, the FXR agonist obeticholic acid, and the ASK-1 inhibitor selonsertib, Dr. Younossi said.
Optimal NASH care in the future may be based on targeting multiple such pathways, with patients increasingly treated at specialized centers that incorporate not only hepatologists, but also diabetes experts, dietitians, and exercise specialists.
“My own belief is that you have to treat this in the long term and also in a multidisciplinary sort of approach,” he said.
Dr. Younossi indicated that he is a consultant for Gilead, Intercept, Bristol-Myers Squibb, Novo Nordisk, Viking, Terms, Shionogi, AbbVie, Merck, and Novartis.
Global Academy and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM DIGESTIVE DISEASES: NEW ADVANCES
Novel microbiome signature may detect NAFLD-cirrhosis
according to results from a study published in Nature Communications.
“Limited data exist concerning the diagnostic accuracy of gut microbiome–derived signatures for detecting NAFLD-cirrhosis,” wrote Cyrielle Caussy, MD, PhD, of the University of California, San Diego, along with her colleagues.
The researchers conducted a cross-sectional analysis of 203 patients with NAFLD. Data was collected from a twin and family cohort with a total of 98 probands that included the complete spectrum of the disease. In addition, 105 first-degree relatives of the probands were also included.
The team analyzed stool samples of participants using MRI and assessed whether the novel signature could accurately identify cirrhosis in NAFLD.
After analysis, the researchers found that in a specific cohort of probands, the microbial biomarker showed strong diagnostic accuracy for identifying cirrhosis in patients with NAFLD (area under the ROC curve, 0.92). These findings were validated in another cohort of first-degree relatives of the proband group (AUROC, 0.87).
The authors acknowledged that a key limitation of the analysis was that it was only a single-center study. As a result, the widespread generalizability of the findings could be restricted.
“This conveniently assessed microbial biomarker could present an adjunct tool to current invasive approaches to determine stage of liver disease,” they concluded.
The study was supported by funding from the National Institutes of Health and Janssen. The authors reported financial affiliations with the American Gastroenterological Association, Atlantic Philanthropies, the John A. Hartford Foundation, and the Association of Specialty Professors.
SOURCE: Caussy C et al. Nat Commun. 2019 Mar 29. doi: 10.1038/s41467-019-09455-9.
according to results from a study published in Nature Communications.
“Limited data exist concerning the diagnostic accuracy of gut microbiome–derived signatures for detecting NAFLD-cirrhosis,” wrote Cyrielle Caussy, MD, PhD, of the University of California, San Diego, along with her colleagues.
The researchers conducted a cross-sectional analysis of 203 patients with NAFLD. Data was collected from a twin and family cohort with a total of 98 probands that included the complete spectrum of the disease. In addition, 105 first-degree relatives of the probands were also included.
The team analyzed stool samples of participants using MRI and assessed whether the novel signature could accurately identify cirrhosis in NAFLD.
After analysis, the researchers found that in a specific cohort of probands, the microbial biomarker showed strong diagnostic accuracy for identifying cirrhosis in patients with NAFLD (area under the ROC curve, 0.92). These findings were validated in another cohort of first-degree relatives of the proband group (AUROC, 0.87).
The authors acknowledged that a key limitation of the analysis was that it was only a single-center study. As a result, the widespread generalizability of the findings could be restricted.
“This conveniently assessed microbial biomarker could present an adjunct tool to current invasive approaches to determine stage of liver disease,” they concluded.
The study was supported by funding from the National Institutes of Health and Janssen. The authors reported financial affiliations with the American Gastroenterological Association, Atlantic Philanthropies, the John A. Hartford Foundation, and the Association of Specialty Professors.
SOURCE: Caussy C et al. Nat Commun. 2019 Mar 29. doi: 10.1038/s41467-019-09455-9.
according to results from a study published in Nature Communications.
“Limited data exist concerning the diagnostic accuracy of gut microbiome–derived signatures for detecting NAFLD-cirrhosis,” wrote Cyrielle Caussy, MD, PhD, of the University of California, San Diego, along with her colleagues.
The researchers conducted a cross-sectional analysis of 203 patients with NAFLD. Data was collected from a twin and family cohort with a total of 98 probands that included the complete spectrum of the disease. In addition, 105 first-degree relatives of the probands were also included.
The team analyzed stool samples of participants using MRI and assessed whether the novel signature could accurately identify cirrhosis in NAFLD.
After analysis, the researchers found that in a specific cohort of probands, the microbial biomarker showed strong diagnostic accuracy for identifying cirrhosis in patients with NAFLD (area under the ROC curve, 0.92). These findings were validated in another cohort of first-degree relatives of the proband group (AUROC, 0.87).
The authors acknowledged that a key limitation of the analysis was that it was only a single-center study. As a result, the widespread generalizability of the findings could be restricted.
“This conveniently assessed microbial biomarker could present an adjunct tool to current invasive approaches to determine stage of liver disease,” they concluded.
The study was supported by funding from the National Institutes of Health and Janssen. The authors reported financial affiliations with the American Gastroenterological Association, Atlantic Philanthropies, the John A. Hartford Foundation, and the Association of Specialty Professors.
SOURCE: Caussy C et al. Nat Commun. 2019 Mar 29. doi: 10.1038/s41467-019-09455-9.
FROM NATURE COMMUNICATIONS
Study eyes biomarkers of regorafenib response in hepatocellular carcinoma
.
“In the absence of established or predefined biomarkers for regorafenib, we performed a broad exploratory biomarker analyses at the DNA, RNA, and protein level that represents a much more comprehensive approach than previous studies of regorafenib or sorafenib,” wrote Michael Teufel, PhD, of Bayer Healthcare Pharmaceuticals in Whippany, N.J., and his associates. The preplanned, retrospective analysis of data from the phase 3 RESOURCE trial was reported in Gastroenterology.
The randomized trial included 567 patients whose hepatocellular carcinoma had progressed on sorafenib. Regorafenib significantly outperformed placebo with regard to overall survival (OS). Dr. Teufel and his associates performed next-generation sequencing on 17 archived tumor samples containing sufficient tissue (all from regorafenib recipients). They also performed immune profiling on 46 tumor samples (32 from regorafenib recipients and 14 from placebo recipients), protein analysis on 499 plasma samples (332 from regorafenib recipients and 167 from placebo recipients), and microRNA analysis on 343 plasma samples (234 regorafenib recipients and 109 placebo recipients).
Among 266 proteins tested, decreased levels of 5 proteins correlated with significantly longer OS on regorafenib therapy. These proteins are involved in inflammation or hepatocellular carcinogenesis, the researchers noted. Importantly, none were associated with survival independent of treatment. These five proteins included angiopoietin 1 (hazard ratio for OS, 0.53; 95% confidence interval, 0.38-0.73), cystatin B (hazard ratio, 0.47; 95% CI, 0.34-0.64); the latency-associated peptide of transforming growth factor beta (HR, 0.46; 95% CI, 0.33-0.64), oxidized low-density lipoprotein receptor 1 (HR, 0.54; 95% CI, 0.41-0.72), and C-C motif chemokine ligand 3 (HR, 0.54; 95% CI, 0.39-0.74).
Additionally, baseline concentrations of 47 of the 266 proteins correlated with a time to progression (TPP) benefit on regorafenib therapy (adjusted P less than or equal to .05 for each). The 47 proteins included all 5 that predicted an OS benefit. All but two proteins (calbindin and gelsolin) showed the same directional effect as for OS (that is, low expression predicted response).
Nine plasma microRNA’s levels correlated with improved OS on regorafenib (adjusted P less than or equal to .05): MIR30A, MIR122, MIR125B, MIR200A, MIR374B, MIR15B, MIR107, MIR320, and MIR645. Notably, expression was linked to longer OS specifically among patients with the Hoshida S3 subtype of hepatocellular carcinoma. Next-generation sequencing of tumor samples also identified 49 variants in 27 oncogenes or tumor-suppressor genes. Mutations in CTNNB1 were found in 3 of 10 patients who progressed on regorafenib, and VEGFA amplification was found in 1 of 7 regorafenib responders.
“Thus far, rational biomarker selection has been unsuccessful in identifying predictive markers for regorafenib in colorectal cancer and gastrointestinal stromal tumors,” the researchers commented. “The broader approach used in this study is not only biologically warranted considering the heterogeneity of hepatocellular carcinoma tumors, but is also needed due to the multiple targets and pathways affected by MKIs such as regorafenib. Levels of these circulating biomarkers and genetic features of tumors might be used to identify patients with hepatocellular carcinoma most likely to respond to regorafenib.”
Bayer funded the study, provided the study drug, and was involved in all aspects of the study. Dr. Teufel and three coinvestigators are Bayer employees. Dr. Teufel and two coinvestigators own stock in Bayer. Three other coinvestigators disclosed ties to Bayer and other pharmaceutical companies.
SOURCE: Teufel M et al. Gastroenterology. 2019 Jan 30. doi: 10.1053/j.gastro.2019.01.261.
.
“In the absence of established or predefined biomarkers for regorafenib, we performed a broad exploratory biomarker analyses at the DNA, RNA, and protein level that represents a much more comprehensive approach than previous studies of regorafenib or sorafenib,” wrote Michael Teufel, PhD, of Bayer Healthcare Pharmaceuticals in Whippany, N.J., and his associates. The preplanned, retrospective analysis of data from the phase 3 RESOURCE trial was reported in Gastroenterology.
The randomized trial included 567 patients whose hepatocellular carcinoma had progressed on sorafenib. Regorafenib significantly outperformed placebo with regard to overall survival (OS). Dr. Teufel and his associates performed next-generation sequencing on 17 archived tumor samples containing sufficient tissue (all from regorafenib recipients). They also performed immune profiling on 46 tumor samples (32 from regorafenib recipients and 14 from placebo recipients), protein analysis on 499 plasma samples (332 from regorafenib recipients and 167 from placebo recipients), and microRNA analysis on 343 plasma samples (234 regorafenib recipients and 109 placebo recipients).
Among 266 proteins tested, decreased levels of 5 proteins correlated with significantly longer OS on regorafenib therapy. These proteins are involved in inflammation or hepatocellular carcinogenesis, the researchers noted. Importantly, none were associated with survival independent of treatment. These five proteins included angiopoietin 1 (hazard ratio for OS, 0.53; 95% confidence interval, 0.38-0.73), cystatin B (hazard ratio, 0.47; 95% CI, 0.34-0.64); the latency-associated peptide of transforming growth factor beta (HR, 0.46; 95% CI, 0.33-0.64), oxidized low-density lipoprotein receptor 1 (HR, 0.54; 95% CI, 0.41-0.72), and C-C motif chemokine ligand 3 (HR, 0.54; 95% CI, 0.39-0.74).
Additionally, baseline concentrations of 47 of the 266 proteins correlated with a time to progression (TPP) benefit on regorafenib therapy (adjusted P less than or equal to .05 for each). The 47 proteins included all 5 that predicted an OS benefit. All but two proteins (calbindin and gelsolin) showed the same directional effect as for OS (that is, low expression predicted response).
Nine plasma microRNA’s levels correlated with improved OS on regorafenib (adjusted P less than or equal to .05): MIR30A, MIR122, MIR125B, MIR200A, MIR374B, MIR15B, MIR107, MIR320, and MIR645. Notably, expression was linked to longer OS specifically among patients with the Hoshida S3 subtype of hepatocellular carcinoma. Next-generation sequencing of tumor samples also identified 49 variants in 27 oncogenes or tumor-suppressor genes. Mutations in CTNNB1 were found in 3 of 10 patients who progressed on regorafenib, and VEGFA amplification was found in 1 of 7 regorafenib responders.
“Thus far, rational biomarker selection has been unsuccessful in identifying predictive markers for regorafenib in colorectal cancer and gastrointestinal stromal tumors,” the researchers commented. “The broader approach used in this study is not only biologically warranted considering the heterogeneity of hepatocellular carcinoma tumors, but is also needed due to the multiple targets and pathways affected by MKIs such as regorafenib. Levels of these circulating biomarkers and genetic features of tumors might be used to identify patients with hepatocellular carcinoma most likely to respond to regorafenib.”
Bayer funded the study, provided the study drug, and was involved in all aspects of the study. Dr. Teufel and three coinvestigators are Bayer employees. Dr. Teufel and two coinvestigators own stock in Bayer. Three other coinvestigators disclosed ties to Bayer and other pharmaceutical companies.
SOURCE: Teufel M et al. Gastroenterology. 2019 Jan 30. doi: 10.1053/j.gastro.2019.01.261.
.
“In the absence of established or predefined biomarkers for regorafenib, we performed a broad exploratory biomarker analyses at the DNA, RNA, and protein level that represents a much more comprehensive approach than previous studies of regorafenib or sorafenib,” wrote Michael Teufel, PhD, of Bayer Healthcare Pharmaceuticals in Whippany, N.J., and his associates. The preplanned, retrospective analysis of data from the phase 3 RESOURCE trial was reported in Gastroenterology.
The randomized trial included 567 patients whose hepatocellular carcinoma had progressed on sorafenib. Regorafenib significantly outperformed placebo with regard to overall survival (OS). Dr. Teufel and his associates performed next-generation sequencing on 17 archived tumor samples containing sufficient tissue (all from regorafenib recipients). They also performed immune profiling on 46 tumor samples (32 from regorafenib recipients and 14 from placebo recipients), protein analysis on 499 plasma samples (332 from regorafenib recipients and 167 from placebo recipients), and microRNA analysis on 343 plasma samples (234 regorafenib recipients and 109 placebo recipients).
Among 266 proteins tested, decreased levels of 5 proteins correlated with significantly longer OS on regorafenib therapy. These proteins are involved in inflammation or hepatocellular carcinogenesis, the researchers noted. Importantly, none were associated with survival independent of treatment. These five proteins included angiopoietin 1 (hazard ratio for OS, 0.53; 95% confidence interval, 0.38-0.73), cystatin B (hazard ratio, 0.47; 95% CI, 0.34-0.64); the latency-associated peptide of transforming growth factor beta (HR, 0.46; 95% CI, 0.33-0.64), oxidized low-density lipoprotein receptor 1 (HR, 0.54; 95% CI, 0.41-0.72), and C-C motif chemokine ligand 3 (HR, 0.54; 95% CI, 0.39-0.74).
Additionally, baseline concentrations of 47 of the 266 proteins correlated with a time to progression (TPP) benefit on regorafenib therapy (adjusted P less than or equal to .05 for each). The 47 proteins included all 5 that predicted an OS benefit. All but two proteins (calbindin and gelsolin) showed the same directional effect as for OS (that is, low expression predicted response).
Nine plasma microRNA’s levels correlated with improved OS on regorafenib (adjusted P less than or equal to .05): MIR30A, MIR122, MIR125B, MIR200A, MIR374B, MIR15B, MIR107, MIR320, and MIR645. Notably, expression was linked to longer OS specifically among patients with the Hoshida S3 subtype of hepatocellular carcinoma. Next-generation sequencing of tumor samples also identified 49 variants in 27 oncogenes or tumor-suppressor genes. Mutations in CTNNB1 were found in 3 of 10 patients who progressed on regorafenib, and VEGFA amplification was found in 1 of 7 regorafenib responders.
“Thus far, rational biomarker selection has been unsuccessful in identifying predictive markers for regorafenib in colorectal cancer and gastrointestinal stromal tumors,” the researchers commented. “The broader approach used in this study is not only biologically warranted considering the heterogeneity of hepatocellular carcinoma tumors, but is also needed due to the multiple targets and pathways affected by MKIs such as regorafenib. Levels of these circulating biomarkers and genetic features of tumors might be used to identify patients with hepatocellular carcinoma most likely to respond to regorafenib.”
Bayer funded the study, provided the study drug, and was involved in all aspects of the study. Dr. Teufel and three coinvestigators are Bayer employees. Dr. Teufel and two coinvestigators own stock in Bayer. Three other coinvestigators disclosed ties to Bayer and other pharmaceutical companies.
SOURCE: Teufel M et al. Gastroenterology. 2019 Jan 30. doi: 10.1053/j.gastro.2019.01.261.
FROM GASTROENTEROLOGY
For patients with HBV, daily aspirin may reduce risk of liver cancer
Sixteen years of data showed that daily aspirin therapy reduced the risk of HBV-related HCC by 29%, reported lead author Teng-Yu Lee, MD, PhD, of Taichung (Taiwan) Veterans General Hospital and his colleagues. Analysis also showed that antiviral nucleos(t)ide analogue therapy and statin use were independently associated with reduced risk of HCC, whereas older age, cirrhosis, and male sex increased risk.
“Therapy with [nucleos(t)ide analogues] is associated with reductions in HCC risk, but the risk is not erased,” the investigators wrote in JAMA Internal Medicine. “Therefore, using only [nucleos(t)ide analogue] therapy may not be enough for HCC prevention. Antiviral therapy is not indicated in most HBV carriers, so another effective way of reducing HCC risk needs to be developed.”
Previous studies have shown that aspirin can reduce the risk of colorectal cancer; however, data supporting aspirin for HCC prevention are limited to a few animal models and human studies, the latter of which are statistically unreliable.
“Therefore, we conducted a nationwide cohort study to evaluate the association of daily aspirin therapy with HBV-related HCC,” the investigators wrote.
They screened 204,507 patients with HBV included in the Taiwanese National Health Insurance Research Database (NHIRD) between 1997 and 2012, first excluding any with confounding conditions, such as hepatitis C infection or alcoholic liver disease. Next, 2,123 patients were identified who had taken aspirin for 90 days or longer. Finally, these cases were randomly matched with 8,492 control patients with HBV who had never received antiplatelet therapy. The main measured outcome was diagnosis with HCC. Patients were followed until this diagnosis was made, death occurred, or the end of the study period.
Analysis showed that most patients were male (72.4%) and took aspirin for about 4 years, usually prescribed for cardiovascular disease risk factors. Almost all patients in the treatment group (98%) received an aspirin dose of 100 mg or less.
After 5 years, the cumulative incidence of HCC in the aspirin group was 5.20% versus 7.87% in the control group (P less than .001). Multivariable analysis revealed that daily aspirin was associated with a significant risk reduction of 29% (HR 0.71; P less than .001), as were nucleos(t)ide analogues and statins, which lowered risk by 46% and 38%, respectively. In contrast, risk increased with older age at the rate of 1% per year, male sex carried an additional risk of 75%, and liver cirrhosis was associated with a 2.89-fold risk increase.
“In the present study, we report that daily aspirin therapy was associated with a reduced incidence of HCC in patients with [chronic hepatitis B],” the investigators wrote. “Our findings may be of help in future efforts to further improve the chemoprevention of HBV-related HCC, and a proof-of-concept study is thus warranted.”
The investigators described several mechanisms that may have contribute to the possible risk reduction provided by aspirin. For one, aspirin inhibits platelet activation, which is associated with development of HBV-related liver disease. Additional benefit may come from induction of HCC cell apoptosis, control of tumor growth, reduced liver fibrosis, and increased liver regeneration, all of which have been associated with aspirin in rodent models.
“Hepatitis B virus–related HCC is generally a consequence of chronic inflammation due to hepatitis, fibrosis, dysplasia, and tumor growth,” the investigators wrote, suggesting that aspirin-related reductions in inflammation could also explain reduced neoplastic activity.
To assess for increased risk of peptic ulcers secondary to aspirin, the investigators performed a subanalysis of peptic ulcer bleeding. These results showed that rates of peptic ulcer bleeding, at around 5%-6%, were similar between the aspirin group and the control group. Among other variables, cirrhosis didn’t significantly affect rates of peptic ulcer bleeding, and aspirin users had similar rates of peptic ulcer bleeding regardless of HBV status. Because of the study design, however, the investigators cautioned that these analyses could underestimate ulcer risk because patients who could not tolerate aspirin for at least 90 days were excluded from the study.
Although statins stood out as another possible risk reducer, the investigators noted that “randomized clinical trials are required to confirm the chemopreventive effect of statins.”
Similarly, the investigators suggested that a prospective trial is needed before aspirin can be adopted as an HCC preventive.
The study was funded by the Ministry of Science and Technology, National Health Research Institutes, and Taichung (Taiwan) Veterans General Hospital, Taiwan. One author reported financial compensation from Gilead and Bristol-Myers Squibb.
SOURCE: Lee T-Y et al. JAMA Intern Med. 2019 Mar 18. doi:10.1001/jamainternmed.2018.8342.
Sixteen years of data showed that daily aspirin therapy reduced the risk of HBV-related HCC by 29%, reported lead author Teng-Yu Lee, MD, PhD, of Taichung (Taiwan) Veterans General Hospital and his colleagues. Analysis also showed that antiviral nucleos(t)ide analogue therapy and statin use were independently associated with reduced risk of HCC, whereas older age, cirrhosis, and male sex increased risk.
“Therapy with [nucleos(t)ide analogues] is associated with reductions in HCC risk, but the risk is not erased,” the investigators wrote in JAMA Internal Medicine. “Therefore, using only [nucleos(t)ide analogue] therapy may not be enough for HCC prevention. Antiviral therapy is not indicated in most HBV carriers, so another effective way of reducing HCC risk needs to be developed.”
Previous studies have shown that aspirin can reduce the risk of colorectal cancer; however, data supporting aspirin for HCC prevention are limited to a few animal models and human studies, the latter of which are statistically unreliable.
“Therefore, we conducted a nationwide cohort study to evaluate the association of daily aspirin therapy with HBV-related HCC,” the investigators wrote.
They screened 204,507 patients with HBV included in the Taiwanese National Health Insurance Research Database (NHIRD) between 1997 and 2012, first excluding any with confounding conditions, such as hepatitis C infection or alcoholic liver disease. Next, 2,123 patients were identified who had taken aspirin for 90 days or longer. Finally, these cases were randomly matched with 8,492 control patients with HBV who had never received antiplatelet therapy. The main measured outcome was diagnosis with HCC. Patients were followed until this diagnosis was made, death occurred, or the end of the study period.
Analysis showed that most patients were male (72.4%) and took aspirin for about 4 years, usually prescribed for cardiovascular disease risk factors. Almost all patients in the treatment group (98%) received an aspirin dose of 100 mg or less.
After 5 years, the cumulative incidence of HCC in the aspirin group was 5.20% versus 7.87% in the control group (P less than .001). Multivariable analysis revealed that daily aspirin was associated with a significant risk reduction of 29% (HR 0.71; P less than .001), as were nucleos(t)ide analogues and statins, which lowered risk by 46% and 38%, respectively. In contrast, risk increased with older age at the rate of 1% per year, male sex carried an additional risk of 75%, and liver cirrhosis was associated with a 2.89-fold risk increase.
“In the present study, we report that daily aspirin therapy was associated with a reduced incidence of HCC in patients with [chronic hepatitis B],” the investigators wrote. “Our findings may be of help in future efforts to further improve the chemoprevention of HBV-related HCC, and a proof-of-concept study is thus warranted.”
The investigators described several mechanisms that may have contribute to the possible risk reduction provided by aspirin. For one, aspirin inhibits platelet activation, which is associated with development of HBV-related liver disease. Additional benefit may come from induction of HCC cell apoptosis, control of tumor growth, reduced liver fibrosis, and increased liver regeneration, all of which have been associated with aspirin in rodent models.
“Hepatitis B virus–related HCC is generally a consequence of chronic inflammation due to hepatitis, fibrosis, dysplasia, and tumor growth,” the investigators wrote, suggesting that aspirin-related reductions in inflammation could also explain reduced neoplastic activity.
To assess for increased risk of peptic ulcers secondary to aspirin, the investigators performed a subanalysis of peptic ulcer bleeding. These results showed that rates of peptic ulcer bleeding, at around 5%-6%, were similar between the aspirin group and the control group. Among other variables, cirrhosis didn’t significantly affect rates of peptic ulcer bleeding, and aspirin users had similar rates of peptic ulcer bleeding regardless of HBV status. Because of the study design, however, the investigators cautioned that these analyses could underestimate ulcer risk because patients who could not tolerate aspirin for at least 90 days were excluded from the study.
Although statins stood out as another possible risk reducer, the investigators noted that “randomized clinical trials are required to confirm the chemopreventive effect of statins.”
Similarly, the investigators suggested that a prospective trial is needed before aspirin can be adopted as an HCC preventive.
The study was funded by the Ministry of Science and Technology, National Health Research Institutes, and Taichung (Taiwan) Veterans General Hospital, Taiwan. One author reported financial compensation from Gilead and Bristol-Myers Squibb.
SOURCE: Lee T-Y et al. JAMA Intern Med. 2019 Mar 18. doi:10.1001/jamainternmed.2018.8342.
Sixteen years of data showed that daily aspirin therapy reduced the risk of HBV-related HCC by 29%, reported lead author Teng-Yu Lee, MD, PhD, of Taichung (Taiwan) Veterans General Hospital and his colleagues. Analysis also showed that antiviral nucleos(t)ide analogue therapy and statin use were independently associated with reduced risk of HCC, whereas older age, cirrhosis, and male sex increased risk.
“Therapy with [nucleos(t)ide analogues] is associated with reductions in HCC risk, but the risk is not erased,” the investigators wrote in JAMA Internal Medicine. “Therefore, using only [nucleos(t)ide analogue] therapy may not be enough for HCC prevention. Antiviral therapy is not indicated in most HBV carriers, so another effective way of reducing HCC risk needs to be developed.”
Previous studies have shown that aspirin can reduce the risk of colorectal cancer; however, data supporting aspirin for HCC prevention are limited to a few animal models and human studies, the latter of which are statistically unreliable.
“Therefore, we conducted a nationwide cohort study to evaluate the association of daily aspirin therapy with HBV-related HCC,” the investigators wrote.
They screened 204,507 patients with HBV included in the Taiwanese National Health Insurance Research Database (NHIRD) between 1997 and 2012, first excluding any with confounding conditions, such as hepatitis C infection or alcoholic liver disease. Next, 2,123 patients were identified who had taken aspirin for 90 days or longer. Finally, these cases were randomly matched with 8,492 control patients with HBV who had never received antiplatelet therapy. The main measured outcome was diagnosis with HCC. Patients were followed until this diagnosis was made, death occurred, or the end of the study period.
Analysis showed that most patients were male (72.4%) and took aspirin for about 4 years, usually prescribed for cardiovascular disease risk factors. Almost all patients in the treatment group (98%) received an aspirin dose of 100 mg or less.
After 5 years, the cumulative incidence of HCC in the aspirin group was 5.20% versus 7.87% in the control group (P less than .001). Multivariable analysis revealed that daily aspirin was associated with a significant risk reduction of 29% (HR 0.71; P less than .001), as were nucleos(t)ide analogues and statins, which lowered risk by 46% and 38%, respectively. In contrast, risk increased with older age at the rate of 1% per year, male sex carried an additional risk of 75%, and liver cirrhosis was associated with a 2.89-fold risk increase.
“In the present study, we report that daily aspirin therapy was associated with a reduced incidence of HCC in patients with [chronic hepatitis B],” the investigators wrote. “Our findings may be of help in future efforts to further improve the chemoprevention of HBV-related HCC, and a proof-of-concept study is thus warranted.”
The investigators described several mechanisms that may have contribute to the possible risk reduction provided by aspirin. For one, aspirin inhibits platelet activation, which is associated with development of HBV-related liver disease. Additional benefit may come from induction of HCC cell apoptosis, control of tumor growth, reduced liver fibrosis, and increased liver regeneration, all of which have been associated with aspirin in rodent models.
“Hepatitis B virus–related HCC is generally a consequence of chronic inflammation due to hepatitis, fibrosis, dysplasia, and tumor growth,” the investigators wrote, suggesting that aspirin-related reductions in inflammation could also explain reduced neoplastic activity.
To assess for increased risk of peptic ulcers secondary to aspirin, the investigators performed a subanalysis of peptic ulcer bleeding. These results showed that rates of peptic ulcer bleeding, at around 5%-6%, were similar between the aspirin group and the control group. Among other variables, cirrhosis didn’t significantly affect rates of peptic ulcer bleeding, and aspirin users had similar rates of peptic ulcer bleeding regardless of HBV status. Because of the study design, however, the investigators cautioned that these analyses could underestimate ulcer risk because patients who could not tolerate aspirin for at least 90 days were excluded from the study.
Although statins stood out as another possible risk reducer, the investigators noted that “randomized clinical trials are required to confirm the chemopreventive effect of statins.”
Similarly, the investigators suggested that a prospective trial is needed before aspirin can be adopted as an HCC preventive.
The study was funded by the Ministry of Science and Technology, National Health Research Institutes, and Taichung (Taiwan) Veterans General Hospital, Taiwan. One author reported financial compensation from Gilead and Bristol-Myers Squibb.
SOURCE: Lee T-Y et al. JAMA Intern Med. 2019 Mar 18. doi:10.1001/jamainternmed.2018.8342.
FROM JAMA INTERNAL MEDICINE
For patients with end-stage liver disease, acute care incurs steep costs
End-of-life care for patients with end-stage liver disease cost more than four of the five most expensive chronic medical conditions, according to the findings of a population-based study in Canada.
During their final year of life, patients with end-stage liver disease incurred a median of $51,191 Canadian dollars in health care costs (interquartile range, $28,510-$86,659) – approximately $2,360 more than ischemic heart disease, $1,830 more than diabetes, $1,600 more than mental health disorders, and $600 more than congestive heart failure, Erin M. Kelly, MD, of the University of Ottawa, and her associates wrote in Clinical Gastroenterology and Hepatology. Only chronic renal disease cost more (median, $55,453). Most health care costs of end-stage liver disease covered the final 90 days of life and were tied to high use of hospital resources, the researchers said.
In the United States, more than 150,000 patients are hospitalized for end-stage liver disease every year at a price tag of $4 billion, Dr. Kelly and her associates noted. This price tag is expected to rise further because of epidemic levels of obesity and related nonalcoholic fatty liver disease. The shortage of livers for transplantation and the fact that many patients with cirrhosis are not transplantation candidates leave many in end-of-life care. Given the lack of population-level data on costs of this care, the researchers studied data for all individuals who died in Ontario – Canada’s largest province – between April 2010 and March 2013. The data source was the Institute for Clinical Evaluative Sciences, a nonprofit group that tracks diagnoses, health care, outcomes, and costs.
Among 264,723 decedents, 5,087 (1.9%) had a diagnosis of end-stage liver disease. These patients died a median of 15 years earlier than other patients (median age of death, 65 vs. 80 years old). During the last year of life, 99% visited the emergency department or were hospitalized, compared with 86% of other patients. Importantly, health care costs for the two groups were similar up until the final 90 days of life, when there was “a clear divergence,” the researchers said. A total of 51% of the costs of the final 12 months of care related to acute care during the final 90 days of life. Consequently, during their last 3 months, patients with end-stage liver disease cost the health care system 46% more than other individuals, the difference remained statistically significant after accounting for demographics and comorbidities, and the picture changed little after excluding transplantation patients and those with hepatocellular carcinoma.
Medical care for patients with end-stage liver disease is complex – often involving serious infections, gastrointestinal bleeding, renal dysfunction, electrolyte disturbances, and worsening encephalopathy – and often involves frequent hospital readmissions, the researchers noted. Nonetheless, the findings highlight the need to consider steps such as advanced care planning and palliative care to help keep patients with end-stage liver disease from dying in acute care settings, they concluded. Such steps “may direct services toward more appropriate sectors, while reducing costs.”
The Ontario Ministry of Health and Long-Term Care supported the work. The researchers reported having no competing interests.
SOURCE: Kelly EM et al. Clin Gastroenterol Hepatol. 2019 Jan 28. doi: 10.1016/j.cgh.2019.01.046.
End-of-life care for patients with end-stage liver disease cost more than four of the five most expensive chronic medical conditions, according to the findings of a population-based study in Canada.
During their final year of life, patients with end-stage liver disease incurred a median of $51,191 Canadian dollars in health care costs (interquartile range, $28,510-$86,659) – approximately $2,360 more than ischemic heart disease, $1,830 more than diabetes, $1,600 more than mental health disorders, and $600 more than congestive heart failure, Erin M. Kelly, MD, of the University of Ottawa, and her associates wrote in Clinical Gastroenterology and Hepatology. Only chronic renal disease cost more (median, $55,453). Most health care costs of end-stage liver disease covered the final 90 days of life and were tied to high use of hospital resources, the researchers said.
In the United States, more than 150,000 patients are hospitalized for end-stage liver disease every year at a price tag of $4 billion, Dr. Kelly and her associates noted. This price tag is expected to rise further because of epidemic levels of obesity and related nonalcoholic fatty liver disease. The shortage of livers for transplantation and the fact that many patients with cirrhosis are not transplantation candidates leave many in end-of-life care. Given the lack of population-level data on costs of this care, the researchers studied data for all individuals who died in Ontario – Canada’s largest province – between April 2010 and March 2013. The data source was the Institute for Clinical Evaluative Sciences, a nonprofit group that tracks diagnoses, health care, outcomes, and costs.
Among 264,723 decedents, 5,087 (1.9%) had a diagnosis of end-stage liver disease. These patients died a median of 15 years earlier than other patients (median age of death, 65 vs. 80 years old). During the last year of life, 99% visited the emergency department or were hospitalized, compared with 86% of other patients. Importantly, health care costs for the two groups were similar up until the final 90 days of life, when there was “a clear divergence,” the researchers said. A total of 51% of the costs of the final 12 months of care related to acute care during the final 90 days of life. Consequently, during their last 3 months, patients with end-stage liver disease cost the health care system 46% more than other individuals, the difference remained statistically significant after accounting for demographics and comorbidities, and the picture changed little after excluding transplantation patients and those with hepatocellular carcinoma.
Medical care for patients with end-stage liver disease is complex – often involving serious infections, gastrointestinal bleeding, renal dysfunction, electrolyte disturbances, and worsening encephalopathy – and often involves frequent hospital readmissions, the researchers noted. Nonetheless, the findings highlight the need to consider steps such as advanced care planning and palliative care to help keep patients with end-stage liver disease from dying in acute care settings, they concluded. Such steps “may direct services toward more appropriate sectors, while reducing costs.”
The Ontario Ministry of Health and Long-Term Care supported the work. The researchers reported having no competing interests.
SOURCE: Kelly EM et al. Clin Gastroenterol Hepatol. 2019 Jan 28. doi: 10.1016/j.cgh.2019.01.046.
End-of-life care for patients with end-stage liver disease cost more than four of the five most expensive chronic medical conditions, according to the findings of a population-based study in Canada.
During their final year of life, patients with end-stage liver disease incurred a median of $51,191 Canadian dollars in health care costs (interquartile range, $28,510-$86,659) – approximately $2,360 more than ischemic heart disease, $1,830 more than diabetes, $1,600 more than mental health disorders, and $600 more than congestive heart failure, Erin M. Kelly, MD, of the University of Ottawa, and her associates wrote in Clinical Gastroenterology and Hepatology. Only chronic renal disease cost more (median, $55,453). Most health care costs of end-stage liver disease covered the final 90 days of life and were tied to high use of hospital resources, the researchers said.
In the United States, more than 150,000 patients are hospitalized for end-stage liver disease every year at a price tag of $4 billion, Dr. Kelly and her associates noted. This price tag is expected to rise further because of epidemic levels of obesity and related nonalcoholic fatty liver disease. The shortage of livers for transplantation and the fact that many patients with cirrhosis are not transplantation candidates leave many in end-of-life care. Given the lack of population-level data on costs of this care, the researchers studied data for all individuals who died in Ontario – Canada’s largest province – between April 2010 and March 2013. The data source was the Institute for Clinical Evaluative Sciences, a nonprofit group that tracks diagnoses, health care, outcomes, and costs.
Among 264,723 decedents, 5,087 (1.9%) had a diagnosis of end-stage liver disease. These patients died a median of 15 years earlier than other patients (median age of death, 65 vs. 80 years old). During the last year of life, 99% visited the emergency department or were hospitalized, compared with 86% of other patients. Importantly, health care costs for the two groups were similar up until the final 90 days of life, when there was “a clear divergence,” the researchers said. A total of 51% of the costs of the final 12 months of care related to acute care during the final 90 days of life. Consequently, during their last 3 months, patients with end-stage liver disease cost the health care system 46% more than other individuals, the difference remained statistically significant after accounting for demographics and comorbidities, and the picture changed little after excluding transplantation patients and those with hepatocellular carcinoma.
Medical care for patients with end-stage liver disease is complex – often involving serious infections, gastrointestinal bleeding, renal dysfunction, electrolyte disturbances, and worsening encephalopathy – and often involves frequent hospital readmissions, the researchers noted. Nonetheless, the findings highlight the need to consider steps such as advanced care planning and palliative care to help keep patients with end-stage liver disease from dying in acute care settings, they concluded. Such steps “may direct services toward more appropriate sectors, while reducing costs.”
The Ontario Ministry of Health and Long-Term Care supported the work. The researchers reported having no competing interests.
SOURCE: Kelly EM et al. Clin Gastroenterol Hepatol. 2019 Jan 28. doi: 10.1016/j.cgh.2019.01.046.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Cirrhosis model predicts decompensation across diverse populations
A prognostic model that uses serum albumin-bilirubin (ALBI) and Fibrosis-4 (FIB-4) scores can identify patients with cirrhosis who are at high risk of liver decompensation, according to investigators.
During validation testing, the scoring system performed well among European and Middle Eastern patients, which supports prognostic value across diverse populations, reported lead author Neil Guha, MRCP, PhD, of the University of Nottingham (U.K.) and his colleagues, who suggested that the scoring system could fix an important practice gap.
“Identification of patients [with chronic liver disease] that need intensive monitoring and timely intervention is challenging,” the investigators wrote in Clinical Gastroenterology and Hepatology. “Robust prognostic tools using simple laboratory variables, with potential for implementation in nonspecialist settings and across different health care systems, have significant appeal.”
Although existing scoring systems have been used for decades, they have clear limitations, the investigators noted, referring to predictive ability that may be too little, too late.
“[T]hese scoring systems provide value after synthetic liver function has become significantly deranged and provide only short-term prognostic value,” the investigators wrote. “Presently, there are no scores, performed in routine clinical practice, that provide robust prognostic stratification within early, compensated cirrhosis over the medium/long term.”
To fulfill this need, the investigators developed and validated a prognostic model that incorporates data from the ALBI and FIB-4 scoring systems because these tests measure both fibrosis and function. The development phase involved 145 patients with compensated cirrhosis from Nottingham. Almost half of the cohort had liver disease because of alcohol (44.8%), while about one out of three patients had nonalcoholic fatty liver disease (29.7%). After investigators collected baseline clinical features and scores, patients were followed for a median of 4.59 years, during which time decompensation events were recorded (ascites, variceal bleeding, and encephalopathy). Decompensation occurred in about one out of five patients (19.3%) in the U.K. group, with ascites being the most common (71.4%). Using these findings, the investigators created the prognostic model, which classified patients as having either low or high risk of decompensation. In the development cohort, patients with high risk scores had a hazard ratio for decompensation of 7.10.
In the second part of the study, the investigators validated their model with two clinically distinct groups in Dublin, Ireland (prospective; n = 141), and Menoufia, Egypt (retrospective; n = 93).
In the Dublin cohort, the most common etiologies were alcohol (39.7%) and hepatitis C (29.8%). Over a maximum observational period of 6.4 years, the decompensation rate was lower than the development group, at 12.1%. Types of decompensation also differed, with variceal bleeding being the most common (47.1%). Patients with high risk scores had a higher HR for decompensation than the U.K. cohort, at 12.54.
In the Egypt group, the most common causes of liver disease were nonalcoholic fatty liver disease (47.3%) and hepatitis C (34.4%). The maximum follow-up period was 10.6 years, during which time 38.7% of patients experienced decompensation, with ascites being the most common form (57.1%). The HR of 5.10 was the lowest of all cohorts.
The investigators noted that the cohorts represented unique patient populations with different etiological patterns. “This provides reassurance that the model has generalizability for stratifying liver disease at an international level,” the investigators wrote, suggesting that ALBI and FIB-4 can be used in low-resource and community settings.
“A frequently leveled criticism of algorithms such as ALBI-FIB-4 is that they are too complicated to be applied routinely in the clinical setting,” the investigators wrote. “To overcome this problem we developed a simple online calculator which can be accessed using the following link: https://jscalc.io/calc/gdEJj89Wz5PirkSL.”
“We have shown that routinely available laboratory variables, combined in a novel algorithm, ALBI-FIB-4, can stratify patients with cirrhosis for future risk of liver decompensation,” the investigators concluded. “The ability to do this in the context of early, compensated cirrhosis with preserved liver synthetic function whilst also predicting long-term clinical outcomes has clinical utility for international health care systems.”
The study was funded by National Institute for Health Research (NIHR) Nottingham Digestive Diseases Biomedical Research Centre based at Nottingham University Hospitals NHS Trust and the University of Nottingham. The investigators declared no conflicts of interest.
SOURCE: Guha N et al. CGH. 2019 Feb 1. doi: 10.1016/j.cgh.2019.01.042.
A prognostic model that uses serum albumin-bilirubin (ALBI) and Fibrosis-4 (FIB-4) scores can identify patients with cirrhosis who are at high risk of liver decompensation, according to investigators.
During validation testing, the scoring system performed well among European and Middle Eastern patients, which supports prognostic value across diverse populations, reported lead author Neil Guha, MRCP, PhD, of the University of Nottingham (U.K.) and his colleagues, who suggested that the scoring system could fix an important practice gap.
“Identification of patients [with chronic liver disease] that need intensive monitoring and timely intervention is challenging,” the investigators wrote in Clinical Gastroenterology and Hepatology. “Robust prognostic tools using simple laboratory variables, with potential for implementation in nonspecialist settings and across different health care systems, have significant appeal.”
Although existing scoring systems have been used for decades, they have clear limitations, the investigators noted, referring to predictive ability that may be too little, too late.
“[T]hese scoring systems provide value after synthetic liver function has become significantly deranged and provide only short-term prognostic value,” the investigators wrote. “Presently, there are no scores, performed in routine clinical practice, that provide robust prognostic stratification within early, compensated cirrhosis over the medium/long term.”
To fulfill this need, the investigators developed and validated a prognostic model that incorporates data from the ALBI and FIB-4 scoring systems because these tests measure both fibrosis and function. The development phase involved 145 patients with compensated cirrhosis from Nottingham. Almost half of the cohort had liver disease because of alcohol (44.8%), while about one out of three patients had nonalcoholic fatty liver disease (29.7%). After investigators collected baseline clinical features and scores, patients were followed for a median of 4.59 years, during which time decompensation events were recorded (ascites, variceal bleeding, and encephalopathy). Decompensation occurred in about one out of five patients (19.3%) in the U.K. group, with ascites being the most common (71.4%). Using these findings, the investigators created the prognostic model, which classified patients as having either low or high risk of decompensation. In the development cohort, patients with high risk scores had a hazard ratio for decompensation of 7.10.
In the second part of the study, the investigators validated their model with two clinically distinct groups in Dublin, Ireland (prospective; n = 141), and Menoufia, Egypt (retrospective; n = 93).
In the Dublin cohort, the most common etiologies were alcohol (39.7%) and hepatitis C (29.8%). Over a maximum observational period of 6.4 years, the decompensation rate was lower than the development group, at 12.1%. Types of decompensation also differed, with variceal bleeding being the most common (47.1%). Patients with high risk scores had a higher HR for decompensation than the U.K. cohort, at 12.54.
In the Egypt group, the most common causes of liver disease were nonalcoholic fatty liver disease (47.3%) and hepatitis C (34.4%). The maximum follow-up period was 10.6 years, during which time 38.7% of patients experienced decompensation, with ascites being the most common form (57.1%). The HR of 5.10 was the lowest of all cohorts.
The investigators noted that the cohorts represented unique patient populations with different etiological patterns. “This provides reassurance that the model has generalizability for stratifying liver disease at an international level,” the investigators wrote, suggesting that ALBI and FIB-4 can be used in low-resource and community settings.
“A frequently leveled criticism of algorithms such as ALBI-FIB-4 is that they are too complicated to be applied routinely in the clinical setting,” the investigators wrote. “To overcome this problem we developed a simple online calculator which can be accessed using the following link: https://jscalc.io/calc/gdEJj89Wz5PirkSL.”
“We have shown that routinely available laboratory variables, combined in a novel algorithm, ALBI-FIB-4, can stratify patients with cirrhosis for future risk of liver decompensation,” the investigators concluded. “The ability to do this in the context of early, compensated cirrhosis with preserved liver synthetic function whilst also predicting long-term clinical outcomes has clinical utility for international health care systems.”
The study was funded by National Institute for Health Research (NIHR) Nottingham Digestive Diseases Biomedical Research Centre based at Nottingham University Hospitals NHS Trust and the University of Nottingham. The investigators declared no conflicts of interest.
SOURCE: Guha N et al. CGH. 2019 Feb 1. doi: 10.1016/j.cgh.2019.01.042.
A prognostic model that uses serum albumin-bilirubin (ALBI) and Fibrosis-4 (FIB-4) scores can identify patients with cirrhosis who are at high risk of liver decompensation, according to investigators.
During validation testing, the scoring system performed well among European and Middle Eastern patients, which supports prognostic value across diverse populations, reported lead author Neil Guha, MRCP, PhD, of the University of Nottingham (U.K.) and his colleagues, who suggested that the scoring system could fix an important practice gap.
“Identification of patients [with chronic liver disease] that need intensive monitoring and timely intervention is challenging,” the investigators wrote in Clinical Gastroenterology and Hepatology. “Robust prognostic tools using simple laboratory variables, with potential for implementation in nonspecialist settings and across different health care systems, have significant appeal.”
Although existing scoring systems have been used for decades, they have clear limitations, the investigators noted, referring to predictive ability that may be too little, too late.
“[T]hese scoring systems provide value after synthetic liver function has become significantly deranged and provide only short-term prognostic value,” the investigators wrote. “Presently, there are no scores, performed in routine clinical practice, that provide robust prognostic stratification within early, compensated cirrhosis over the medium/long term.”
To fulfill this need, the investigators developed and validated a prognostic model that incorporates data from the ALBI and FIB-4 scoring systems because these tests measure both fibrosis and function. The development phase involved 145 patients with compensated cirrhosis from Nottingham. Almost half of the cohort had liver disease because of alcohol (44.8%), while about one out of three patients had nonalcoholic fatty liver disease (29.7%). After investigators collected baseline clinical features and scores, patients were followed for a median of 4.59 years, during which time decompensation events were recorded (ascites, variceal bleeding, and encephalopathy). Decompensation occurred in about one out of five patients (19.3%) in the U.K. group, with ascites being the most common (71.4%). Using these findings, the investigators created the prognostic model, which classified patients as having either low or high risk of decompensation. In the development cohort, patients with high risk scores had a hazard ratio for decompensation of 7.10.
In the second part of the study, the investigators validated their model with two clinically distinct groups in Dublin, Ireland (prospective; n = 141), and Menoufia, Egypt (retrospective; n = 93).
In the Dublin cohort, the most common etiologies were alcohol (39.7%) and hepatitis C (29.8%). Over a maximum observational period of 6.4 years, the decompensation rate was lower than the development group, at 12.1%. Types of decompensation also differed, with variceal bleeding being the most common (47.1%). Patients with high risk scores had a higher HR for decompensation than the U.K. cohort, at 12.54.
In the Egypt group, the most common causes of liver disease were nonalcoholic fatty liver disease (47.3%) and hepatitis C (34.4%). The maximum follow-up period was 10.6 years, during which time 38.7% of patients experienced decompensation, with ascites being the most common form (57.1%). The HR of 5.10 was the lowest of all cohorts.
The investigators noted that the cohorts represented unique patient populations with different etiological patterns. “This provides reassurance that the model has generalizability for stratifying liver disease at an international level,” the investigators wrote, suggesting that ALBI and FIB-4 can be used in low-resource and community settings.
“A frequently leveled criticism of algorithms such as ALBI-FIB-4 is that they are too complicated to be applied routinely in the clinical setting,” the investigators wrote. “To overcome this problem we developed a simple online calculator which can be accessed using the following link: https://jscalc.io/calc/gdEJj89Wz5PirkSL.”
“We have shown that routinely available laboratory variables, combined in a novel algorithm, ALBI-FIB-4, can stratify patients with cirrhosis for future risk of liver decompensation,” the investigators concluded. “The ability to do this in the context of early, compensated cirrhosis with preserved liver synthetic function whilst also predicting long-term clinical outcomes has clinical utility for international health care systems.”
The study was funded by National Institute for Health Research (NIHR) Nottingham Digestive Diseases Biomedical Research Centre based at Nottingham University Hospitals NHS Trust and the University of Nottingham. The investigators declared no conflicts of interest.
SOURCE: Guha N et al. CGH. 2019 Feb 1. doi: 10.1016/j.cgh.2019.01.042.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Will inpatient albumin help in decompensated cirrhosis?
PHILADELPHIA – , according to Vijay Shah, MD, chair of the division of gastroenterology and hepatology at Mayo Clinic, Rochester, Minn.
“These are interesting studies, but I don’t think we’re ready yet to use this broadly,” Dr. Shah said at the meeting jointly provided by Rutgers and Global Academy for Medical Education.
Current guidelines do describe the use of albumin for large-volume paracentesis and other specific inpatient situations; however, extrapolating its long-term use has been explored in two major studies that recently came out with contradictory findings.
In the ANSWER trial, as reported in the Lancet, investigators at 33 centers randomized patients with cirrhosis and uncomplicated ascites to either standard medical treatment with or without human albumin, at 40 g twice weekly for 2 weeks, followed by 40 g weekly for up to 18 months.
Those investigators found that long-term albumin prolonged overall survival, with a 38% reduction in the mortality hazard ratio, with similar rates of serious, nonliver adverse events, leading them to conclude that this intervention may act as a disease-modifying treatment in decompensated cirrhosis patients.
By contrast, however, a recent randomized, placebo-controlled trial reported in the Journal of Hepatology showed that albumin plus midodrine, an alpha-adrenergic vasoconstrictor, did not improve survival among patients with decompensated cirrhosis on the liver transplant waiting list, at least at the doses administered (midodrine 15-30 mg/day and albumin 40 g every 15 days for a year).
While this particular combination of albumin plus midodrine did decrease renin and aldosterone levels, the intervention did not prevent complications or improve survival, investigators said at the time. Complication rates were 37% and 43% for treatment and placebo, respectively (P = .402), with low rates of death in both groups and no significant difference in mortality at 1 year (P = .527).
Dr. Shah said the discrepant results may be attributable to specific differences in study design or enrollment.
“It’s just hand waving, but it may be related to the dose of albumin, or may be related to the types of patients – the second study was in patients who are waiting for liver transplantation,” he told attendees. “But I don’t think that there’s currently enough evidence to use albumin in your patients in the outpatient setting.”
There is a third study, recently published in the American Journal of Gastroenterology, looking at data for a large end-stage liver disease cohort with hyponatremia. Investigators observed a higher rate of hyponatremia resolution and improved 30-day survival in those who had received albumin (total mean amount, 225 g) versus those who had not.
Considering all of this evidence taken together, Dr. Shah said he would not favor using outpatient albumin at this point – though he advised attendees to watch for a currently recruiting phase 3 randomized study, known as PRECIOSA, which is evaluating long-term administration of human albumin 20% injectable solution, dosed by body weight, in patients with decompensated cirrhosis and ascites.
Dr. Shah indicated that he is a consultant for Afimmune, Durect Corporation, Enterome, GRI Bio, Merck Research Laboratories, Novartis Pharma, and Vital Therapeutics. Global Academy and this news organization are owned by the same company.
PHILADELPHIA – , according to Vijay Shah, MD, chair of the division of gastroenterology and hepatology at Mayo Clinic, Rochester, Minn.
“These are interesting studies, but I don’t think we’re ready yet to use this broadly,” Dr. Shah said at the meeting jointly provided by Rutgers and Global Academy for Medical Education.
Current guidelines do describe the use of albumin for large-volume paracentesis and other specific inpatient situations; however, extrapolating its long-term use has been explored in two major studies that recently came out with contradictory findings.
In the ANSWER trial, as reported in the Lancet, investigators at 33 centers randomized patients with cirrhosis and uncomplicated ascites to either standard medical treatment with or without human albumin, at 40 g twice weekly for 2 weeks, followed by 40 g weekly for up to 18 months.
Those investigators found that long-term albumin prolonged overall survival, with a 38% reduction in the mortality hazard ratio, with similar rates of serious, nonliver adverse events, leading them to conclude that this intervention may act as a disease-modifying treatment in decompensated cirrhosis patients.
By contrast, however, a recent randomized, placebo-controlled trial reported in the Journal of Hepatology showed that albumin plus midodrine, an alpha-adrenergic vasoconstrictor, did not improve survival among patients with decompensated cirrhosis on the liver transplant waiting list, at least at the doses administered (midodrine 15-30 mg/day and albumin 40 g every 15 days for a year).
While this particular combination of albumin plus midodrine did decrease renin and aldosterone levels, the intervention did not prevent complications or improve survival, investigators said at the time. Complication rates were 37% and 43% for treatment and placebo, respectively (P = .402), with low rates of death in both groups and no significant difference in mortality at 1 year (P = .527).
Dr. Shah said the discrepant results may be attributable to specific differences in study design or enrollment.
“It’s just hand waving, but it may be related to the dose of albumin, or may be related to the types of patients – the second study was in patients who are waiting for liver transplantation,” he told attendees. “But I don’t think that there’s currently enough evidence to use albumin in your patients in the outpatient setting.”
There is a third study, recently published in the American Journal of Gastroenterology, looking at data for a large end-stage liver disease cohort with hyponatremia. Investigators observed a higher rate of hyponatremia resolution and improved 30-day survival in those who had received albumin (total mean amount, 225 g) versus those who had not.
Considering all of this evidence taken together, Dr. Shah said he would not favor using outpatient albumin at this point – though he advised attendees to watch for a currently recruiting phase 3 randomized study, known as PRECIOSA, which is evaluating long-term administration of human albumin 20% injectable solution, dosed by body weight, in patients with decompensated cirrhosis and ascites.
Dr. Shah indicated that he is a consultant for Afimmune, Durect Corporation, Enterome, GRI Bio, Merck Research Laboratories, Novartis Pharma, and Vital Therapeutics. Global Academy and this news organization are owned by the same company.
PHILADELPHIA – , according to Vijay Shah, MD, chair of the division of gastroenterology and hepatology at Mayo Clinic, Rochester, Minn.
“These are interesting studies, but I don’t think we’re ready yet to use this broadly,” Dr. Shah said at the meeting jointly provided by Rutgers and Global Academy for Medical Education.
Current guidelines do describe the use of albumin for large-volume paracentesis and other specific inpatient situations; however, extrapolating its long-term use has been explored in two major studies that recently came out with contradictory findings.
In the ANSWER trial, as reported in the Lancet, investigators at 33 centers randomized patients with cirrhosis and uncomplicated ascites to either standard medical treatment with or without human albumin, at 40 g twice weekly for 2 weeks, followed by 40 g weekly for up to 18 months.
Those investigators found that long-term albumin prolonged overall survival, with a 38% reduction in the mortality hazard ratio, with similar rates of serious, nonliver adverse events, leading them to conclude that this intervention may act as a disease-modifying treatment in decompensated cirrhosis patients.
By contrast, however, a recent randomized, placebo-controlled trial reported in the Journal of Hepatology showed that albumin plus midodrine, an alpha-adrenergic vasoconstrictor, did not improve survival among patients with decompensated cirrhosis on the liver transplant waiting list, at least at the doses administered (midodrine 15-30 mg/day and albumin 40 g every 15 days for a year).
While this particular combination of albumin plus midodrine did decrease renin and aldosterone levels, the intervention did not prevent complications or improve survival, investigators said at the time. Complication rates were 37% and 43% for treatment and placebo, respectively (P = .402), with low rates of death in both groups and no significant difference in mortality at 1 year (P = .527).
Dr. Shah said the discrepant results may be attributable to specific differences in study design or enrollment.
“It’s just hand waving, but it may be related to the dose of albumin, or may be related to the types of patients – the second study was in patients who are waiting for liver transplantation,” he told attendees. “But I don’t think that there’s currently enough evidence to use albumin in your patients in the outpatient setting.”
There is a third study, recently published in the American Journal of Gastroenterology, looking at data for a large end-stage liver disease cohort with hyponatremia. Investigators observed a higher rate of hyponatremia resolution and improved 30-day survival in those who had received albumin (total mean amount, 225 g) versus those who had not.
Considering all of this evidence taken together, Dr. Shah said he would not favor using outpatient albumin at this point – though he advised attendees to watch for a currently recruiting phase 3 randomized study, known as PRECIOSA, which is evaluating long-term administration of human albumin 20% injectable solution, dosed by body weight, in patients with decompensated cirrhosis and ascites.
Dr. Shah indicated that he is a consultant for Afimmune, Durect Corporation, Enterome, GRI Bio, Merck Research Laboratories, Novartis Pharma, and Vital Therapeutics. Global Academy and this news organization are owned by the same company.
REPORTING FROM DIGESTIVE DISEASES: NEW ADVANCES