User login
Group finds inconsistencies in genome sequencing procedures

Photo courtesy of NIGMS
Researchers say they have identified substantial differences in the procedures and quality of cancer genome sequencing between sequencing centers.
And this led to dramatic discrepancies in the number and types of somatic mutations detected when using the same cancer genome sequences for analysis.
The group’s study involved 83 researchers from 78 institutions participating in the International Cancer Genomics Consortium (ICGC).
The ICGC is an international effort to establish a comprehensive description of genomic, transcriptomic, and epigenomic changes in 50 different tumor types and/or subtypes that are thought to be of clinical and societal importance across the globe.
The consortium is characterizing more than 25,000 cancer genomes and carrying out 78 projects supported by different national and international funding agencies.
For the current project, which was published in Nature Communications, researchers studied a patient with chronic lymphocytic leukemia and a patient with medulloblastoma.
The team analyzed the entire tumor genome of each patient and compared it to the normal genome of the same patient to decipher the molecular causes for these cancers.
The researchers said they saw “widely varying mutation call rates and low concordance among analysis pipelines.”
So they established a reference mutation dataset to assess analytical procedures. They said this “gold-set” reference database has helped the ICGC community improve procedures for identifying more true somatic mutations in cancer genomes and making fewer false-positive calls.
“The findings of our study have far-reaching implications for cancer genome analysis,” said Ivo Gut, of Centro Nacional de Analisis Genómico in Barcelona, Spain.
“We have found many inconsistencies in both the sequencing of cancer genomes and the data analysis at different sites. We are making our findings available to the scientific and diagnostic community so that they can improve their systems and generate more standardized and consistent results.” ![]()

Photo courtesy of NIGMS
Researchers say they have identified substantial differences in the procedures and quality of cancer genome sequencing between sequencing centers.
And this led to dramatic discrepancies in the number and types of somatic mutations detected when using the same cancer genome sequences for analysis.
The group’s study involved 83 researchers from 78 institutions participating in the International Cancer Genomics Consortium (ICGC).
The ICGC is an international effort to establish a comprehensive description of genomic, transcriptomic, and epigenomic changes in 50 different tumor types and/or subtypes that are thought to be of clinical and societal importance across the globe.
The consortium is characterizing more than 25,000 cancer genomes and carrying out 78 projects supported by different national and international funding agencies.
For the current project, which was published in Nature Communications, researchers studied a patient with chronic lymphocytic leukemia and a patient with medulloblastoma.
The team analyzed the entire tumor genome of each patient and compared it to the normal genome of the same patient to decipher the molecular causes for these cancers.
The researchers said they saw “widely varying mutation call rates and low concordance among analysis pipelines.”
So they established a reference mutation dataset to assess analytical procedures. They said this “gold-set” reference database has helped the ICGC community improve procedures for identifying more true somatic mutations in cancer genomes and making fewer false-positive calls.
“The findings of our study have far-reaching implications for cancer genome analysis,” said Ivo Gut, of Centro Nacional de Analisis Genómico in Barcelona, Spain.
“We have found many inconsistencies in both the sequencing of cancer genomes and the data analysis at different sites. We are making our findings available to the scientific and diagnostic community so that they can improve their systems and generate more standardized and consistent results.” ![]()

Photo courtesy of NIGMS
Researchers say they have identified substantial differences in the procedures and quality of cancer genome sequencing between sequencing centers.
And this led to dramatic discrepancies in the number and types of somatic mutations detected when using the same cancer genome sequences for analysis.
The group’s study involved 83 researchers from 78 institutions participating in the International Cancer Genomics Consortium (ICGC).
The ICGC is an international effort to establish a comprehensive description of genomic, transcriptomic, and epigenomic changes in 50 different tumor types and/or subtypes that are thought to be of clinical and societal importance across the globe.
The consortium is characterizing more than 25,000 cancer genomes and carrying out 78 projects supported by different national and international funding agencies.
For the current project, which was published in Nature Communications, researchers studied a patient with chronic lymphocytic leukemia and a patient with medulloblastoma.
The team analyzed the entire tumor genome of each patient and compared it to the normal genome of the same patient to decipher the molecular causes for these cancers.
The researchers said they saw “widely varying mutation call rates and low concordance among analysis pipelines.”
So they established a reference mutation dataset to assess analytical procedures. They said this “gold-set” reference database has helped the ICGC community improve procedures for identifying more true somatic mutations in cancer genomes and making fewer false-positive calls.
“The findings of our study have far-reaching implications for cancer genome analysis,” said Ivo Gut, of Centro Nacional de Analisis Genómico in Barcelona, Spain.
“We have found many inconsistencies in both the sequencing of cancer genomes and the data analysis at different sites. We are making our findings available to the scientific and diagnostic community so that they can improve their systems and generate more standardized and consistent results.” ![]()
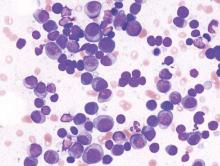
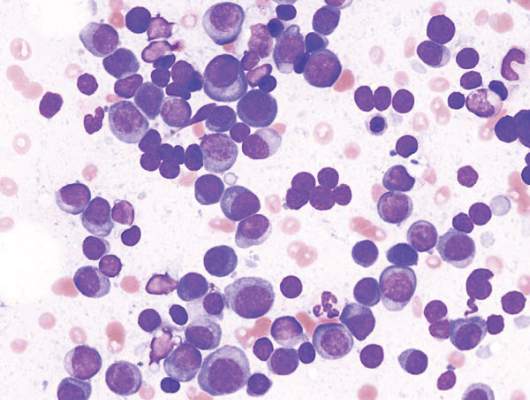
Anti-PD-1, IMiD combo immunotherapy active in heavily pretreated myeloma
ORLANDO – Partnering the PD-1 antibody pembrolizumab with pomalidomide and dexamethasone induced responses in 60% of 27 patients with heavily pretreated relapsed and/or refractory multiple myeloma in a phase II trial.
This included 1 stringent complete response, 4 very good partial responses (VGPR), and 11 partial responses (PR). Eight patients had stable disease and 3 progressed.
Further, the overall response rate was 55% (2 VGPR, 9 PR) in patients double-refractory to immunomodulatory drugs (IMiDs) and proteasome inhibitors (PIs) and 50% (1 VGPR and 5 PR) in those with high-risk cytogenetics.
“The regimen shows promising anti-myeloma activity in heavily pretreated patients” and had a “predictable and manageable side-effect profile,” Dr. Asraf Badros of University of Maryland Marlene and Stewart Greenebaum Cancer Center, Baltimore, said at the annual meeting of the American Society of Hematology.
The investigators hypothesized that blocking signaling of the programmed cell death protein 1 (PD-1) and its ligand PD-L1 with pembrolizumab (Keytruda) would activate multiple myeloma-specific cytotoxic T cells that could be further enhanced by the immunomodulator pomalidomide (Pomalyst).
The primary goal of the ongoing study is to establish the safety of the combination therapy.
In all, 33 patients received 28-day cycles of pembrolizumab 200 mg intravenous every 2 weeks plus pomalidomide 4 mg daily for 21 days and dexamethasone 40 mg weekly (20 mg for patients older than 70 years). After 24 months, responders will continue pomalidomide and dexamethasone alone until progression.
At enrollment, patients had to have relapsed and/or refractory disease after at least two lines of prior therapy including an IMiD and a PI, an ECOG performance status of less than 2, and adequate organ function.
Key exclusion criteria are an active autoimmune disease requiring systemic treatment or a history of severe autoimmune disease such as interstitial lung disease or active, non-infectious pneumonitis.
Patients received a median of three prior lines of therapy, 67% had prior autologous transplant, 89% were refractory to lenalidomide, and 70% were double-refractory to both IMiDs and PIs. The median age was 65 years (range 42-81 years), 73% were male, and 42% had high-risk deletion 17p and/or a translocation of chromosomes 14 and 16 [t(14;16)].
The median number of cycles was six and median follow-up short at 7.4 months.
The most common adverse events reported in 10% of all grades were fatigue and hypoglycemia, mostly grades 1 and 2.
The most serious adverse events in the study were pneumonia and infection, including one death due to sepsis, Dr. Badros said. Two other patients died as a result of disease progression and one because of a cardiac event.
“We reported a lot, actually, of immune-related adverse events,” he said.
In 10% of patients, the investigators noted pneumonitis, one of which was grade 3, as well as hyperthyroidism and autoimmune hepatitis. Pembrolizumab was not stopped and the pneumonitis was treated with steroids until symptoms resolved. Patients resumed the assigned doses, though one patient withdrew consent.
The pneumonitis did not appear to be associated with prior therapy and it “responded extremely quickly and well to the steroids, indicating it might be a cytokine release issue,” Dr. Badros said.
Five patients required pomalidomide dose reductions due to neutropenia in two, and one case each of rash, palpitations, and fatigue. After the septic death, antibiotic prophylaxis was started in all patients, he said.
A total of 22 patients remain on study, with 7 patients discontinuing because of disease progression.
Given the short follow-up, it is “too early to talk about progression-free and overall-survival, but the signal we are getting is quite impressive,” Dr. Badros said.
The investigators also tried to look at PD-L1 expression in bone marrow samples collected at screening and on day 1 of cycle 3. No PD-L1 expression was found on plasma cells in the first patient, about 40% expression in the second, and 100% expression in the third, which is consistent with the heterogeneity of PD-L1 expression reported previously in the literature, Dr. Badros said. PD-L1 expression on bone marrow biopsies was very hard to standardize and they are exploring various methods to assess the impact of fixation and decalcification on level of expression, he added.
Dr. Badros disclosed off-label use of pembrolizumab and no relevant conflicts of interest.
ORLANDO – Partnering the PD-1 antibody pembrolizumab with pomalidomide and dexamethasone induced responses in 60% of 27 patients with heavily pretreated relapsed and/or refractory multiple myeloma in a phase II trial.
This included 1 stringent complete response, 4 very good partial responses (VGPR), and 11 partial responses (PR). Eight patients had stable disease and 3 progressed.
Further, the overall response rate was 55% (2 VGPR, 9 PR) in patients double-refractory to immunomodulatory drugs (IMiDs) and proteasome inhibitors (PIs) and 50% (1 VGPR and 5 PR) in those with high-risk cytogenetics.
“The regimen shows promising anti-myeloma activity in heavily pretreated patients” and had a “predictable and manageable side-effect profile,” Dr. Asraf Badros of University of Maryland Marlene and Stewart Greenebaum Cancer Center, Baltimore, said at the annual meeting of the American Society of Hematology.
The investigators hypothesized that blocking signaling of the programmed cell death protein 1 (PD-1) and its ligand PD-L1 with pembrolizumab (Keytruda) would activate multiple myeloma-specific cytotoxic T cells that could be further enhanced by the immunomodulator pomalidomide (Pomalyst).
The primary goal of the ongoing study is to establish the safety of the combination therapy.
In all, 33 patients received 28-day cycles of pembrolizumab 200 mg intravenous every 2 weeks plus pomalidomide 4 mg daily for 21 days and dexamethasone 40 mg weekly (20 mg for patients older than 70 years). After 24 months, responders will continue pomalidomide and dexamethasone alone until progression.
At enrollment, patients had to have relapsed and/or refractory disease after at least two lines of prior therapy including an IMiD and a PI, an ECOG performance status of less than 2, and adequate organ function.
Key exclusion criteria are an active autoimmune disease requiring systemic treatment or a history of severe autoimmune disease such as interstitial lung disease or active, non-infectious pneumonitis.
Patients received a median of three prior lines of therapy, 67% had prior autologous transplant, 89% were refractory to lenalidomide, and 70% were double-refractory to both IMiDs and PIs. The median age was 65 years (range 42-81 years), 73% were male, and 42% had high-risk deletion 17p and/or a translocation of chromosomes 14 and 16 [t(14;16)].
The median number of cycles was six and median follow-up short at 7.4 months.
The most common adverse events reported in 10% of all grades were fatigue and hypoglycemia, mostly grades 1 and 2.
The most serious adverse events in the study were pneumonia and infection, including one death due to sepsis, Dr. Badros said. Two other patients died as a result of disease progression and one because of a cardiac event.
“We reported a lot, actually, of immune-related adverse events,” he said.
In 10% of patients, the investigators noted pneumonitis, one of which was grade 3, as well as hyperthyroidism and autoimmune hepatitis. Pembrolizumab was not stopped and the pneumonitis was treated with steroids until symptoms resolved. Patients resumed the assigned doses, though one patient withdrew consent.
The pneumonitis did not appear to be associated with prior therapy and it “responded extremely quickly and well to the steroids, indicating it might be a cytokine release issue,” Dr. Badros said.
Five patients required pomalidomide dose reductions due to neutropenia in two, and one case each of rash, palpitations, and fatigue. After the septic death, antibiotic prophylaxis was started in all patients, he said.
A total of 22 patients remain on study, with 7 patients discontinuing because of disease progression.
Given the short follow-up, it is “too early to talk about progression-free and overall-survival, but the signal we are getting is quite impressive,” Dr. Badros said.
The investigators also tried to look at PD-L1 expression in bone marrow samples collected at screening and on day 1 of cycle 3. No PD-L1 expression was found on plasma cells in the first patient, about 40% expression in the second, and 100% expression in the third, which is consistent with the heterogeneity of PD-L1 expression reported previously in the literature, Dr. Badros said. PD-L1 expression on bone marrow biopsies was very hard to standardize and they are exploring various methods to assess the impact of fixation and decalcification on level of expression, he added.
Dr. Badros disclosed off-label use of pembrolizumab and no relevant conflicts of interest.
ORLANDO – Partnering the PD-1 antibody pembrolizumab with pomalidomide and dexamethasone induced responses in 60% of 27 patients with heavily pretreated relapsed and/or refractory multiple myeloma in a phase II trial.
This included 1 stringent complete response, 4 very good partial responses (VGPR), and 11 partial responses (PR). Eight patients had stable disease and 3 progressed.
Further, the overall response rate was 55% (2 VGPR, 9 PR) in patients double-refractory to immunomodulatory drugs (IMiDs) and proteasome inhibitors (PIs) and 50% (1 VGPR and 5 PR) in those with high-risk cytogenetics.
“The regimen shows promising anti-myeloma activity in heavily pretreated patients” and had a “predictable and manageable side-effect profile,” Dr. Asraf Badros of University of Maryland Marlene and Stewart Greenebaum Cancer Center, Baltimore, said at the annual meeting of the American Society of Hematology.
The investigators hypothesized that blocking signaling of the programmed cell death protein 1 (PD-1) and its ligand PD-L1 with pembrolizumab (Keytruda) would activate multiple myeloma-specific cytotoxic T cells that could be further enhanced by the immunomodulator pomalidomide (Pomalyst).
The primary goal of the ongoing study is to establish the safety of the combination therapy.
In all, 33 patients received 28-day cycles of pembrolizumab 200 mg intravenous every 2 weeks plus pomalidomide 4 mg daily for 21 days and dexamethasone 40 mg weekly (20 mg for patients older than 70 years). After 24 months, responders will continue pomalidomide and dexamethasone alone until progression.
At enrollment, patients had to have relapsed and/or refractory disease after at least two lines of prior therapy including an IMiD and a PI, an ECOG performance status of less than 2, and adequate organ function.
Key exclusion criteria are an active autoimmune disease requiring systemic treatment or a history of severe autoimmune disease such as interstitial lung disease or active, non-infectious pneumonitis.
Patients received a median of three prior lines of therapy, 67% had prior autologous transplant, 89% were refractory to lenalidomide, and 70% were double-refractory to both IMiDs and PIs. The median age was 65 years (range 42-81 years), 73% were male, and 42% had high-risk deletion 17p and/or a translocation of chromosomes 14 and 16 [t(14;16)].
The median number of cycles was six and median follow-up short at 7.4 months.
The most common adverse events reported in 10% of all grades were fatigue and hypoglycemia, mostly grades 1 and 2.
The most serious adverse events in the study were pneumonia and infection, including one death due to sepsis, Dr. Badros said. Two other patients died as a result of disease progression and one because of a cardiac event.
“We reported a lot, actually, of immune-related adverse events,” he said.
In 10% of patients, the investigators noted pneumonitis, one of which was grade 3, as well as hyperthyroidism and autoimmune hepatitis. Pembrolizumab was not stopped and the pneumonitis was treated with steroids until symptoms resolved. Patients resumed the assigned doses, though one patient withdrew consent.
The pneumonitis did not appear to be associated with prior therapy and it “responded extremely quickly and well to the steroids, indicating it might be a cytokine release issue,” Dr. Badros said.
Five patients required pomalidomide dose reductions due to neutropenia in two, and one case each of rash, palpitations, and fatigue. After the septic death, antibiotic prophylaxis was started in all patients, he said.
A total of 22 patients remain on study, with 7 patients discontinuing because of disease progression.
Given the short follow-up, it is “too early to talk about progression-free and overall-survival, but the signal we are getting is quite impressive,” Dr. Badros said.
The investigators also tried to look at PD-L1 expression in bone marrow samples collected at screening and on day 1 of cycle 3. No PD-L1 expression was found on plasma cells in the first patient, about 40% expression in the second, and 100% expression in the third, which is consistent with the heterogeneity of PD-L1 expression reported previously in the literature, Dr. Badros said. PD-L1 expression on bone marrow biopsies was very hard to standardize and they are exploring various methods to assess the impact of fixation and decalcification on level of expression, he added.
Dr. Badros disclosed off-label use of pembrolizumab and no relevant conflicts of interest.
AT ASH 2015
Key clinical point: Pembrolizumab in combination with pomalidomide and dexamethasone has shown strong clinical activity in heavily pretreated relapsed or refractory multiple myeloma.
Major finding: The overall response rate was 60% in 27 evaluable patients.
Data source: Ongoing phase II study of 33 patients with relapsed/refractory multiple myeloma.
Disclosures: Dr. Badros disclosed off-label use of pembrolizumab and no relevant conflicts of interest.
VIDEO: Top-line results from Tourmaline in multiple myeloma, plus ongoing trials and treatment selection
ORLANDO – The combination of the oral proteasome inhibitor ixazomib (Ninlaro, recently approved by the Food and Drug Administration) with lenalidomide and dexamethasone was associated with a 35% improvement in progression free survival in the Tourmaline trial.
In a video interview, Tourmaline investigator Dr. Shaji Kumar, professor of medicine at the Mayo Clinic, Rochester, Minn., discussed the top-line study results, the status of ongoing trials with ixazomib in other combination regimens, and the decision rationales that will need to be considered in selecting one of the newly approved multiple myeloma therapies.
Dr. Kumar has received funding from Takeda, the makers of ixazomib; he has also received funding from Celgene, Onyx, Janssen, and Sanofi.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – The combination of the oral proteasome inhibitor ixazomib (Ninlaro, recently approved by the Food and Drug Administration) with lenalidomide and dexamethasone was associated with a 35% improvement in progression free survival in the Tourmaline trial.
In a video interview, Tourmaline investigator Dr. Shaji Kumar, professor of medicine at the Mayo Clinic, Rochester, Minn., discussed the top-line study results, the status of ongoing trials with ixazomib in other combination regimens, and the decision rationales that will need to be considered in selecting one of the newly approved multiple myeloma therapies.
Dr. Kumar has received funding from Takeda, the makers of ixazomib; he has also received funding from Celgene, Onyx, Janssen, and Sanofi.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – The combination of the oral proteasome inhibitor ixazomib (Ninlaro, recently approved by the Food and Drug Administration) with lenalidomide and dexamethasone was associated with a 35% improvement in progression free survival in the Tourmaline trial.
In a video interview, Tourmaline investigator Dr. Shaji Kumar, professor of medicine at the Mayo Clinic, Rochester, Minn., discussed the top-line study results, the status of ongoing trials with ixazomib in other combination regimens, and the decision rationales that will need to be considered in selecting one of the newly approved multiple myeloma therapies.
Dr. Kumar has received funding from Takeda, the makers of ixazomib; he has also received funding from Celgene, Onyx, Janssen, and Sanofi.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASH 2015
ASH: Daratumumab and len/dex produce high response rates in refractory myeloma
ORLANDO – A combination of two standard therapies and the newly approved targeted agent daratumumab was associated with a high overall response rate and induced rapid, deep, and durable responses in patients with relapsed or refractory multiple myeloma, according to results of a phase I/II study presented at the annual meeting of the American Society of Hematology.
The median time to first response was 1 month; median time to best response was 5.1 months; and the median duration of response had not been reached at the most recent analysis. At 1 year, 91% of 26 patients with a partial response or better had not experienced disease progression. The 18-month progression-free survival rate was 72%, and the 18-month overall survival rate was 90%.
“I have been looking forward to this day since I dosed the first patient with daratumumab in 2007. We have come a long way,” Dr. Torben Plesner said at a briefing at the meeting.
The study is one of several trials examining the use of daratumumab (Darzalex) in various combination regimens. Daratumumab (Darzalex) was recently approved by the Food and Drug Administration as monotherapy for use in patients with relapsed or refractory multiple myeloma for whom three or more prior lines of therapy, including proteasome inhibitors or immunomodulators, have failed.
Updated data on an expansion cohort from the study show that the combination of lenalidomide and dexamethasone (len/dex) with daratumumab was associated with an 81% (26 patients) overall response rate (ORR). This included stringent complete responses (sCR) in 25% (8 patients), complete responses in 9% (3 patients), and very good partial responses in 28% (9 patients), and 6 partial responses
“The responses were durable and they occurred rapidly,” said Dr. Plesner of Vejle Hospital and the University of Southern Denmark in Vejle.
Dr. Plesner presented updated results from the expansion cohort of the GEN503 study looking at the combination of daratumumab and len/dex.
In the open-label, single-arm study, patients received 16 mg/kg intravenous infusions of daratumumab once weekly for the first 2 months, twice weekly for months 3 through 6, and once every 4 weeks thereafter, plus oral lenalidomide 25 mg on days 1 through 21 of every 28-day cycle, and oral dexamethasone 40 mg once weekly.
In the dose-escalation phase, patients with relapsed multiple myeloma following two to four prior lines of therapy were enrolled. In the expansion cohort phase, patients with relapsed disease after at least one line of therapy could be enrolled, with no upper limit on the number of prior regimens.
The primary endpoint was adverse events; the most common were neutropenia in 84% of patients, cough in 50%, diarrhea, and muscle spasms (44% each).
Half of all patients had a serious adverse event, but the only events that occurred in more than one patient were neutropenia (three), gastroenteritis (two), and pyrexia (two). Infusion-related reactions, primarily during the first infusion, occurred in 56%, and the severity was grade 2 or less. Reactions were managed either with premedication or by slowing the infusion rate.
Two randomized phase III studies of the combination of daratumumab and len/dex are ongoing: the POLLUX trial, looking at the drugs in patients with relapsed/refractory disease, and the MAIA trial, using the combination as first-line therapy for newly diagnosed patients.
Speaking about the wealth of new therapies for multiple myeloma and other hematologic malignancies discussed at the briefing, Dr. Robert Hromas, professor of medicine at the University of Florida in Gainesville, commented that “I’ve been in the field for years and I can’t explain the excitement among blood doctors. It’s extraordinary, but we see plateaus lasting years now.”
“It’s so much fun to be a blood doctor,” he added.
The GEN503 trial is sponsored by Janssen. Dr. Plesner disclosed serving on an advisory board for, and receiving research funding from, Janssen. Dr. Hromas had no relevant disclosures.
ORLANDO – A combination of two standard therapies and the newly approved targeted agent daratumumab was associated with a high overall response rate and induced rapid, deep, and durable responses in patients with relapsed or refractory multiple myeloma, according to results of a phase I/II study presented at the annual meeting of the American Society of Hematology.
The median time to first response was 1 month; median time to best response was 5.1 months; and the median duration of response had not been reached at the most recent analysis. At 1 year, 91% of 26 patients with a partial response or better had not experienced disease progression. The 18-month progression-free survival rate was 72%, and the 18-month overall survival rate was 90%.
“I have been looking forward to this day since I dosed the first patient with daratumumab in 2007. We have come a long way,” Dr. Torben Plesner said at a briefing at the meeting.
The study is one of several trials examining the use of daratumumab (Darzalex) in various combination regimens. Daratumumab (Darzalex) was recently approved by the Food and Drug Administration as monotherapy for use in patients with relapsed or refractory multiple myeloma for whom three or more prior lines of therapy, including proteasome inhibitors or immunomodulators, have failed.
Updated data on an expansion cohort from the study show that the combination of lenalidomide and dexamethasone (len/dex) with daratumumab was associated with an 81% (26 patients) overall response rate (ORR). This included stringent complete responses (sCR) in 25% (8 patients), complete responses in 9% (3 patients), and very good partial responses in 28% (9 patients), and 6 partial responses
“The responses were durable and they occurred rapidly,” said Dr. Plesner of Vejle Hospital and the University of Southern Denmark in Vejle.
Dr. Plesner presented updated results from the expansion cohort of the GEN503 study looking at the combination of daratumumab and len/dex.
In the open-label, single-arm study, patients received 16 mg/kg intravenous infusions of daratumumab once weekly for the first 2 months, twice weekly for months 3 through 6, and once every 4 weeks thereafter, plus oral lenalidomide 25 mg on days 1 through 21 of every 28-day cycle, and oral dexamethasone 40 mg once weekly.
In the dose-escalation phase, patients with relapsed multiple myeloma following two to four prior lines of therapy were enrolled. In the expansion cohort phase, patients with relapsed disease after at least one line of therapy could be enrolled, with no upper limit on the number of prior regimens.
The primary endpoint was adverse events; the most common were neutropenia in 84% of patients, cough in 50%, diarrhea, and muscle spasms (44% each).
Half of all patients had a serious adverse event, but the only events that occurred in more than one patient were neutropenia (three), gastroenteritis (two), and pyrexia (two). Infusion-related reactions, primarily during the first infusion, occurred in 56%, and the severity was grade 2 or less. Reactions were managed either with premedication or by slowing the infusion rate.
Two randomized phase III studies of the combination of daratumumab and len/dex are ongoing: the POLLUX trial, looking at the drugs in patients with relapsed/refractory disease, and the MAIA trial, using the combination as first-line therapy for newly diagnosed patients.
Speaking about the wealth of new therapies for multiple myeloma and other hematologic malignancies discussed at the briefing, Dr. Robert Hromas, professor of medicine at the University of Florida in Gainesville, commented that “I’ve been in the field for years and I can’t explain the excitement among blood doctors. It’s extraordinary, but we see plateaus lasting years now.”
“It’s so much fun to be a blood doctor,” he added.
The GEN503 trial is sponsored by Janssen. Dr. Plesner disclosed serving on an advisory board for, and receiving research funding from, Janssen. Dr. Hromas had no relevant disclosures.
ORLANDO – A combination of two standard therapies and the newly approved targeted agent daratumumab was associated with a high overall response rate and induced rapid, deep, and durable responses in patients with relapsed or refractory multiple myeloma, according to results of a phase I/II study presented at the annual meeting of the American Society of Hematology.
The median time to first response was 1 month; median time to best response was 5.1 months; and the median duration of response had not been reached at the most recent analysis. At 1 year, 91% of 26 patients with a partial response or better had not experienced disease progression. The 18-month progression-free survival rate was 72%, and the 18-month overall survival rate was 90%.
“I have been looking forward to this day since I dosed the first patient with daratumumab in 2007. We have come a long way,” Dr. Torben Plesner said at a briefing at the meeting.
The study is one of several trials examining the use of daratumumab (Darzalex) in various combination regimens. Daratumumab (Darzalex) was recently approved by the Food and Drug Administration as monotherapy for use in patients with relapsed or refractory multiple myeloma for whom three or more prior lines of therapy, including proteasome inhibitors or immunomodulators, have failed.
Updated data on an expansion cohort from the study show that the combination of lenalidomide and dexamethasone (len/dex) with daratumumab was associated with an 81% (26 patients) overall response rate (ORR). This included stringent complete responses (sCR) in 25% (8 patients), complete responses in 9% (3 patients), and very good partial responses in 28% (9 patients), and 6 partial responses
“The responses were durable and they occurred rapidly,” said Dr. Plesner of Vejle Hospital and the University of Southern Denmark in Vejle.
Dr. Plesner presented updated results from the expansion cohort of the GEN503 study looking at the combination of daratumumab and len/dex.
In the open-label, single-arm study, patients received 16 mg/kg intravenous infusions of daratumumab once weekly for the first 2 months, twice weekly for months 3 through 6, and once every 4 weeks thereafter, plus oral lenalidomide 25 mg on days 1 through 21 of every 28-day cycle, and oral dexamethasone 40 mg once weekly.
In the dose-escalation phase, patients with relapsed multiple myeloma following two to four prior lines of therapy were enrolled. In the expansion cohort phase, patients with relapsed disease after at least one line of therapy could be enrolled, with no upper limit on the number of prior regimens.
The primary endpoint was adverse events; the most common were neutropenia in 84% of patients, cough in 50%, diarrhea, and muscle spasms (44% each).
Half of all patients had a serious adverse event, but the only events that occurred in more than one patient were neutropenia (three), gastroenteritis (two), and pyrexia (two). Infusion-related reactions, primarily during the first infusion, occurred in 56%, and the severity was grade 2 or less. Reactions were managed either with premedication or by slowing the infusion rate.
Two randomized phase III studies of the combination of daratumumab and len/dex are ongoing: the POLLUX trial, looking at the drugs in patients with relapsed/refractory disease, and the MAIA trial, using the combination as first-line therapy for newly diagnosed patients.
Speaking about the wealth of new therapies for multiple myeloma and other hematologic malignancies discussed at the briefing, Dr. Robert Hromas, professor of medicine at the University of Florida in Gainesville, commented that “I’ve been in the field for years and I can’t explain the excitement among blood doctors. It’s extraordinary, but we see plateaus lasting years now.”
“It’s so much fun to be a blood doctor,” he added.
The GEN503 trial is sponsored by Janssen. Dr. Plesner disclosed serving on an advisory board for, and receiving research funding from, Janssen. Dr. Hromas had no relevant disclosures.
AT ASH 2015
Key clinical point: The combination of the targeted agent daratumumab (Darzalex) with len/dex was highly effective in heavily pretreated patients with multiple myeloma.
Major finding: The overall response rate was 81% (26 of 32 patients).
Data source: Open-label, single-arm expansion cohort from a phase I/II trial in 32 patients.
Disclosures: The GEN503 trial is sponsored by Janssen. Dr. Plesner disclosed serving on an advisory board for, and receiving research funding from, Janssen.
ASH: All-oral regimen extends multiple myeloma PFS
ORLANDO – The first all-oral drug combination for treatment of relapsed/refractory multiple myeloma significantly extended progression-free survival (PFS), based on the first of three planned interim analyses from a phase 3 trial.
The combination of the oral proteasome inhibitor ixazomib (Ninlaro, recently approved by the U.S. Food and Drug Administration) with lenalidomide and dexamethasone (len/dex) was associated with a 35% improvement in PFS, compared with len/dex and placebo, reported Dr. Philippe Moreau from Université Hospital of Nantes (France), Hôtel-Dieu.
The ixazomib combination also was associated with a significantly better median time to progression, at 21.4 vs. 15.7 months (P = .007). The time to response and duration of response were not significantly different, however, for the two groups in the placebo-controlled, randomized study of 722 patients.
“Ixazomib, when combined with len/dex for patients with relapsed and/or refractory multiple myeloma, was associated a significant and meaningful improvement in progression-free survival, significantly improved time to progression, and confirmed response rates,” Dr. Moreau said at a briefing at the American Society of Hematology annual meeting.
Dr. Moreau presented results of the phase III Tourmaline study, which compared len/dex plus weekly ixazomib or len/dex with weekly placebo in adults who have relapsed/refractory multiple myeloma following one to three prior lines of therapy and were not refractory to either prior lenalidomide or proteasome inhibitor–based therapy.
The study met its primary endpoint of a PFS advantage for the addition of ixazomib. The median PFS for ixazomib plus len/dex was 20.6 months, compared with 14.7 months for len/dex plus placebo. The hazard ratio for PFS with ixazomib-containing combination was 0.742 (P = .012).
The confirmed overall response rate (partial response or greater) was 78% with ixazomib vs. 71% with placebo (P = .035). The respective very good partial response or better rates were 48% vs. 39% (P = .014).
A total of 722 patients were randomized to either ixazomib 4 mg or placebo weekly on days 1, 8, 15 and 22 of each 28-day cycle, with oral lenalidomide 25 mg on days 1 through 21 (with dose reductions in patients with renal impairment at the investigator’s discretion) and oral dexamethasone 40 mg on days 1, 8, 15, and 22.
Patients were stratified at randomization by the number of prior therapies (one vs. two or three), previous proteasome-inhibitor exposure, and by International Staging System for multiple myeloma stage I or II vs. III. Cycles were repeated until disease progression or until patients experienced unacceptable toxicity.
The overall median age of patients was 66 (range, 30-91) years. In all, 70% had received a prior proteasome inhibitor, 88% had International Staging System stage I or II disease, and 59% had received just one prior line of therapy.
Dr. Moreau noted that the responses were rapid and durable with a median time to response of 1.1 months for ixazomib and 1.9 months for placebo, and a median duration of response of 20.5 months and 15 months, respectively. Neither difference was significant.
The incidence of grade 3 or greater adverse events was 68% for patients on ixazomib vs. 61% with placebo. A higher incidence of thrombocytopenia with ixazomib (19% vs. 9%) primarily accounted for the difference.
Dr. Moreau noted that peripheral neuropathy, a common problem with intravenous proteasome inhibitors, was low with ixazomib, and patients did not report significant changes in their quality of life.
The study was sponsored by Millennium Pharmaceuticals. Dr. Moreau disclosed receiving honoraria from the company.
ORLANDO – The first all-oral drug combination for treatment of relapsed/refractory multiple myeloma significantly extended progression-free survival (PFS), based on the first of three planned interim analyses from a phase 3 trial.
The combination of the oral proteasome inhibitor ixazomib (Ninlaro, recently approved by the U.S. Food and Drug Administration) with lenalidomide and dexamethasone (len/dex) was associated with a 35% improvement in PFS, compared with len/dex and placebo, reported Dr. Philippe Moreau from Université Hospital of Nantes (France), Hôtel-Dieu.
The ixazomib combination also was associated with a significantly better median time to progression, at 21.4 vs. 15.7 months (P = .007). The time to response and duration of response were not significantly different, however, for the two groups in the placebo-controlled, randomized study of 722 patients.
“Ixazomib, when combined with len/dex for patients with relapsed and/or refractory multiple myeloma, was associated a significant and meaningful improvement in progression-free survival, significantly improved time to progression, and confirmed response rates,” Dr. Moreau said at a briefing at the American Society of Hematology annual meeting.
Dr. Moreau presented results of the phase III Tourmaline study, which compared len/dex plus weekly ixazomib or len/dex with weekly placebo in adults who have relapsed/refractory multiple myeloma following one to three prior lines of therapy and were not refractory to either prior lenalidomide or proteasome inhibitor–based therapy.
The study met its primary endpoint of a PFS advantage for the addition of ixazomib. The median PFS for ixazomib plus len/dex was 20.6 months, compared with 14.7 months for len/dex plus placebo. The hazard ratio for PFS with ixazomib-containing combination was 0.742 (P = .012).
The confirmed overall response rate (partial response or greater) was 78% with ixazomib vs. 71% with placebo (P = .035). The respective very good partial response or better rates were 48% vs. 39% (P = .014).
A total of 722 patients were randomized to either ixazomib 4 mg or placebo weekly on days 1, 8, 15 and 22 of each 28-day cycle, with oral lenalidomide 25 mg on days 1 through 21 (with dose reductions in patients with renal impairment at the investigator’s discretion) and oral dexamethasone 40 mg on days 1, 8, 15, and 22.
Patients were stratified at randomization by the number of prior therapies (one vs. two or three), previous proteasome-inhibitor exposure, and by International Staging System for multiple myeloma stage I or II vs. III. Cycles were repeated until disease progression or until patients experienced unacceptable toxicity.
The overall median age of patients was 66 (range, 30-91) years. In all, 70% had received a prior proteasome inhibitor, 88% had International Staging System stage I or II disease, and 59% had received just one prior line of therapy.
Dr. Moreau noted that the responses were rapid and durable with a median time to response of 1.1 months for ixazomib and 1.9 months for placebo, and a median duration of response of 20.5 months and 15 months, respectively. Neither difference was significant.
The incidence of grade 3 or greater adverse events was 68% for patients on ixazomib vs. 61% with placebo. A higher incidence of thrombocytopenia with ixazomib (19% vs. 9%) primarily accounted for the difference.
Dr. Moreau noted that peripheral neuropathy, a common problem with intravenous proteasome inhibitors, was low with ixazomib, and patients did not report significant changes in their quality of life.
The study was sponsored by Millennium Pharmaceuticals. Dr. Moreau disclosed receiving honoraria from the company.
ORLANDO – The first all-oral drug combination for treatment of relapsed/refractory multiple myeloma significantly extended progression-free survival (PFS), based on the first of three planned interim analyses from a phase 3 trial.
The combination of the oral proteasome inhibitor ixazomib (Ninlaro, recently approved by the U.S. Food and Drug Administration) with lenalidomide and dexamethasone (len/dex) was associated with a 35% improvement in PFS, compared with len/dex and placebo, reported Dr. Philippe Moreau from Université Hospital of Nantes (France), Hôtel-Dieu.
The ixazomib combination also was associated with a significantly better median time to progression, at 21.4 vs. 15.7 months (P = .007). The time to response and duration of response were not significantly different, however, for the two groups in the placebo-controlled, randomized study of 722 patients.
“Ixazomib, when combined with len/dex for patients with relapsed and/or refractory multiple myeloma, was associated a significant and meaningful improvement in progression-free survival, significantly improved time to progression, and confirmed response rates,” Dr. Moreau said at a briefing at the American Society of Hematology annual meeting.
Dr. Moreau presented results of the phase III Tourmaline study, which compared len/dex plus weekly ixazomib or len/dex with weekly placebo in adults who have relapsed/refractory multiple myeloma following one to three prior lines of therapy and were not refractory to either prior lenalidomide or proteasome inhibitor–based therapy.
The study met its primary endpoint of a PFS advantage for the addition of ixazomib. The median PFS for ixazomib plus len/dex was 20.6 months, compared with 14.7 months for len/dex plus placebo. The hazard ratio for PFS with ixazomib-containing combination was 0.742 (P = .012).
The confirmed overall response rate (partial response or greater) was 78% with ixazomib vs. 71% with placebo (P = .035). The respective very good partial response or better rates were 48% vs. 39% (P = .014).
A total of 722 patients were randomized to either ixazomib 4 mg or placebo weekly on days 1, 8, 15 and 22 of each 28-day cycle, with oral lenalidomide 25 mg on days 1 through 21 (with dose reductions in patients with renal impairment at the investigator’s discretion) and oral dexamethasone 40 mg on days 1, 8, 15, and 22.
Patients were stratified at randomization by the number of prior therapies (one vs. two or three), previous proteasome-inhibitor exposure, and by International Staging System for multiple myeloma stage I or II vs. III. Cycles were repeated until disease progression or until patients experienced unacceptable toxicity.
The overall median age of patients was 66 (range, 30-91) years. In all, 70% had received a prior proteasome inhibitor, 88% had International Staging System stage I or II disease, and 59% had received just one prior line of therapy.
Dr. Moreau noted that the responses were rapid and durable with a median time to response of 1.1 months for ixazomib and 1.9 months for placebo, and a median duration of response of 20.5 months and 15 months, respectively. Neither difference was significant.
The incidence of grade 3 or greater adverse events was 68% for patients on ixazomib vs. 61% with placebo. A higher incidence of thrombocytopenia with ixazomib (19% vs. 9%) primarily accounted for the difference.
Dr. Moreau noted that peripheral neuropathy, a common problem with intravenous proteasome inhibitors, was low with ixazomib, and patients did not report significant changes in their quality of life.
The study was sponsored by Millennium Pharmaceuticals. Dr. Moreau disclosed receiving honoraria from the company.
AT ASH 2015
Key clinical point: Ixazomib added to lenalidomide and dexamethasone is an effective all-oral drug regimen in relapsed/refractory multiple myeloma.
Major finding: The combination was associated with a 35% improvement in progression-free survival, compared with len/dex and placebo.
Data source: Randomized placebo-controlled trial in 722 patients with relapsed/refractory multiple myeloma treated with one to three prior lines of therapy.
Disclosures: The study was sponsored by Millennium Pharmaceuticals. Dr. Moreau disclosed receiving honoraria from the company.
VIDEO: Targeted agent, len/dex combo perform ‘impressively’ in advanced multiple myeloma
ORLANDO – A combination of daratumumab (Darzalex) with lenalidomide and dexamethasone (len/dex) was associated with a high overall response rate, including stringent complete responses, in patients with heavily pretreated relapsed/refractory multiple myeloma.
Daratumumab was recently approved by the Food and Drug Administration as monotherapy in patients with relapsed/refractory multiple myeloma.
Dr. Torben Plesner of Vejle Hospital and the University of Southern Denmark in Vejle, who dosed the first patient with daratumumab in 2007, discusses updated findings from a phase I/II trial of the daratumumab and len/dex combination.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – A combination of daratumumab (Darzalex) with lenalidomide and dexamethasone (len/dex) was associated with a high overall response rate, including stringent complete responses, in patients with heavily pretreated relapsed/refractory multiple myeloma.
Daratumumab was recently approved by the Food and Drug Administration as monotherapy in patients with relapsed/refractory multiple myeloma.
Dr. Torben Plesner of Vejle Hospital and the University of Southern Denmark in Vejle, who dosed the first patient with daratumumab in 2007, discusses updated findings from a phase I/II trial of the daratumumab and len/dex combination.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – A combination of daratumumab (Darzalex) with lenalidomide and dexamethasone (len/dex) was associated with a high overall response rate, including stringent complete responses, in patients with heavily pretreated relapsed/refractory multiple myeloma.
Daratumumab was recently approved by the Food and Drug Administration as monotherapy in patients with relapsed/refractory multiple myeloma.
Dr. Torben Plesner of Vejle Hospital and the University of Southern Denmark in Vejle, who dosed the first patient with daratumumab in 2007, discusses updated findings from a phase I/II trial of the daratumumab and len/dex combination.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASH 2015
Cancer drug prices vary widely from country to country

Photo by Bill Branson
The price of cancer drugs varies widely between European countries, Australia, and New Zealand, according to a study published in The Lancet Oncology.
The study indicates that, overall, the UK and Mediterranean countries such as Greece, Spain, and Portugal pay the lowest average unit manufacturer prices for a group of 31 originator cancer drugs (new drugs under patent).
And Sweden, Switzerland, and Germany pay the highest prices.
The greatest differences in price were noted for gemcitabine, which costs €209 per vial in New Zealand and €43 in Australia, and zoledronic acid, which costs €330 per vial in New Zealand but €128 in Greece.*
“Public payers in Germany are paying 223% more in terms of official prices for interferon alfa 2b for melanoma and leukemia treatment than those in Greece,” noted study author Sabine Vogler, PhD, of the WHO Collaborating Centre for Pharmaceutical Pricing and Reimbursement Policies in Vienna, Austria.
“For gefitinib to treat non-small-lung cancer, the price in Germany is 172% higher than in New Zealand.”
To uncover these price differences, Dr Vogler and her colleagues reviewed official drug price data from the Pharma Price Information (PPI) service of the Austrian Public Health Institute for 16 European countries**, and from the pharmaceutical schedules in Australia and New Zealand.
The researchers compared what manufacturers charged for a unit (ie, price per tablet or vial) of 31 originator cancer drugs in June 2013.
None of these drugs had a unit price lower than €10. Four drugs (13%) had an average unit manufacturer price between €250 and €500, and 2 drugs (6%) had an average unit price between €500 and €1000.
Seven drugs (23%) had an average unit price higher than €1000. For example, plerixafor cost over €5000 per injection.
The price differences between the highest- and lowest-priced countries ranged from 28% to 50% for a third of the drugs sampled, between 50% and 100% for half of the drugs, and between 100% and 200% for 3 drugs (10%).
The researchers noted that information on real drug prices is scarce. The cancer drug prices they surveyed did not include confidential discounts such as those agreed upon in managed-entry arrangements that are increasingly used in countries such as Australia, Italy, the UK, and the Netherlands.
“Some high-income countries have managed to barter the manufacturers down to lower prices, but these agreements, including the agreed prices, are confidential,” Dr Vogler explained.
“Although these agreements ensure patient access to new drugs, other countries risk overpaying when setting drug prices through the common practice of external price referencing, or international price comparison, because they can only use the official undiscounted prices as a benchmark. There needs to be far more transparency.”
“We hope that our findings will provide concrete evidence for policymakers to take action to address high prices and ensure more transparency in cancer drug pricing so that costs and access to new drugs does not depend on where a patient lives.” ![]()
*Gemcitabine and zoledronic acid have generic versions in several countries, and originator prices were decreased in some countries following patent expiry but not in others.
**Austria, Belgium, Denmark, Germany, Greece, Finland, France, Italy, Ireland, the Netherlands, Norway, Portugal, Spain, Sweden, Switzerland, and the UK.

Photo by Bill Branson
The price of cancer drugs varies widely between European countries, Australia, and New Zealand, according to a study published in The Lancet Oncology.
The study indicates that, overall, the UK and Mediterranean countries such as Greece, Spain, and Portugal pay the lowest average unit manufacturer prices for a group of 31 originator cancer drugs (new drugs under patent).
And Sweden, Switzerland, and Germany pay the highest prices.
The greatest differences in price were noted for gemcitabine, which costs €209 per vial in New Zealand and €43 in Australia, and zoledronic acid, which costs €330 per vial in New Zealand but €128 in Greece.*
“Public payers in Germany are paying 223% more in terms of official prices for interferon alfa 2b for melanoma and leukemia treatment than those in Greece,” noted study author Sabine Vogler, PhD, of the WHO Collaborating Centre for Pharmaceutical Pricing and Reimbursement Policies in Vienna, Austria.
“For gefitinib to treat non-small-lung cancer, the price in Germany is 172% higher than in New Zealand.”
To uncover these price differences, Dr Vogler and her colleagues reviewed official drug price data from the Pharma Price Information (PPI) service of the Austrian Public Health Institute for 16 European countries**, and from the pharmaceutical schedules in Australia and New Zealand.
The researchers compared what manufacturers charged for a unit (ie, price per tablet or vial) of 31 originator cancer drugs in June 2013.
None of these drugs had a unit price lower than €10. Four drugs (13%) had an average unit manufacturer price between €250 and €500, and 2 drugs (6%) had an average unit price between €500 and €1000.
Seven drugs (23%) had an average unit price higher than €1000. For example, plerixafor cost over €5000 per injection.
The price differences between the highest- and lowest-priced countries ranged from 28% to 50% for a third of the drugs sampled, between 50% and 100% for half of the drugs, and between 100% and 200% for 3 drugs (10%).
The researchers noted that information on real drug prices is scarce. The cancer drug prices they surveyed did not include confidential discounts such as those agreed upon in managed-entry arrangements that are increasingly used in countries such as Australia, Italy, the UK, and the Netherlands.
“Some high-income countries have managed to barter the manufacturers down to lower prices, but these agreements, including the agreed prices, are confidential,” Dr Vogler explained.
“Although these agreements ensure patient access to new drugs, other countries risk overpaying when setting drug prices through the common practice of external price referencing, or international price comparison, because they can only use the official undiscounted prices as a benchmark. There needs to be far more transparency.”
“We hope that our findings will provide concrete evidence for policymakers to take action to address high prices and ensure more transparency in cancer drug pricing so that costs and access to new drugs does not depend on where a patient lives.” ![]()
*Gemcitabine and zoledronic acid have generic versions in several countries, and originator prices were decreased in some countries following patent expiry but not in others.
**Austria, Belgium, Denmark, Germany, Greece, Finland, France, Italy, Ireland, the Netherlands, Norway, Portugal, Spain, Sweden, Switzerland, and the UK.

Photo by Bill Branson
The price of cancer drugs varies widely between European countries, Australia, and New Zealand, according to a study published in The Lancet Oncology.
The study indicates that, overall, the UK and Mediterranean countries such as Greece, Spain, and Portugal pay the lowest average unit manufacturer prices for a group of 31 originator cancer drugs (new drugs under patent).
And Sweden, Switzerland, and Germany pay the highest prices.
The greatest differences in price were noted for gemcitabine, which costs €209 per vial in New Zealand and €43 in Australia, and zoledronic acid, which costs €330 per vial in New Zealand but €128 in Greece.*
“Public payers in Germany are paying 223% more in terms of official prices for interferon alfa 2b for melanoma and leukemia treatment than those in Greece,” noted study author Sabine Vogler, PhD, of the WHO Collaborating Centre for Pharmaceutical Pricing and Reimbursement Policies in Vienna, Austria.
“For gefitinib to treat non-small-lung cancer, the price in Germany is 172% higher than in New Zealand.”
To uncover these price differences, Dr Vogler and her colleagues reviewed official drug price data from the Pharma Price Information (PPI) service of the Austrian Public Health Institute for 16 European countries**, and from the pharmaceutical schedules in Australia and New Zealand.
The researchers compared what manufacturers charged for a unit (ie, price per tablet or vial) of 31 originator cancer drugs in June 2013.
None of these drugs had a unit price lower than €10. Four drugs (13%) had an average unit manufacturer price between €250 and €500, and 2 drugs (6%) had an average unit price between €500 and €1000.
Seven drugs (23%) had an average unit price higher than €1000. For example, plerixafor cost over €5000 per injection.
The price differences between the highest- and lowest-priced countries ranged from 28% to 50% for a third of the drugs sampled, between 50% and 100% for half of the drugs, and between 100% and 200% for 3 drugs (10%).
The researchers noted that information on real drug prices is scarce. The cancer drug prices they surveyed did not include confidential discounts such as those agreed upon in managed-entry arrangements that are increasingly used in countries such as Australia, Italy, the UK, and the Netherlands.
“Some high-income countries have managed to barter the manufacturers down to lower prices, but these agreements, including the agreed prices, are confidential,” Dr Vogler explained.
“Although these agreements ensure patient access to new drugs, other countries risk overpaying when setting drug prices through the common practice of external price referencing, or international price comparison, because they can only use the official undiscounted prices as a benchmark. There needs to be far more transparency.”
“We hope that our findings will provide concrete evidence for policymakers to take action to address high prices and ensure more transparency in cancer drug pricing so that costs and access to new drugs does not depend on where a patient lives.” ![]()
*Gemcitabine and zoledronic acid have generic versions in several countries, and originator prices were decreased in some countries following patent expiry but not in others.
**Austria, Belgium, Denmark, Germany, Greece, Finland, France, Italy, Ireland, the Netherlands, Norway, Portugal, Spain, Sweden, Switzerland, and the UK.
ASH: Carfilzomib doubles progression free survival in head-to-head trial with bortezomib
In a head-to-head clinical trial, carfilzomib (Kyprolis) plus dexamethasone doubled the length of progression-free survival (PFS) when compared with bortezomib (Velcade) plus dexamethasone for individuals with relapsed or refractory multiple myeloma. Response rates were also significantly higher for those receiving carfilzomib, though neither medication could overcome high-risk cytogenetic factors.
The international multi-center phase 3 open-label ENDEAVOR study (clinicaltrials.gov ID: NCT01568866) compared outcomes for a total of 929 patients who were randomized 1:1 to receive one of the treatments. Randomization was stratified to account for prior treatments, including prior proteasome treatment, as well as disease severity by International Staging System stage.
Reporting for the ENDEAVOR investigators, Dr. Meletios Dimopoulos and his co-authors published their results in The Lancet simultaneously with a presentation at the annual meeting of the American Society of Hematology [Lancet Oncol, http://dx.doi.org/10.1016/S1470-2045(15)00464-7] . Dr. Dimopoulos is a professor in the department of clinical therapeutics at the school of medicine of the National and Kapodistrian University of Athens.
The primary endpoint, PFS in the intention-to-treat population, differed significantly between the study arms when the data were analyzed at a pre-planned interim analysis. For those receiving carfilzomib, PFS was 18.7 months, compared with 9.4 months in the bortezomib group, for a hazard ratio of 0.53 (P less than 0.0001). Data were drawn from a pre-specified interim analysis, and study participation is ongoing, with 28-day dosing cycles repeated until disease progression occurrs or the patients experience unacceptable toxicity or withdraw consent.
Investigators had pre-specified subgroup analyses to examine what populations fared better and worse in each arm. Prior bortezomib exposure did not significantly affect PFS for those receiving carfilzomib. Not enough patients had received carfilzomib prior to the study to permit analysis of this effect. Though carfilzomib arm patients with high-risk factors on cytogenetic analysis fared slightly better than those on bortezomib, “neither proteasome inhibitor appears to significantly overcome the adverse prognostic effect of high-risk cytogenetics,” wrote Dr. Dimopoulos and his co-authors.
Secondary outcome measures included the numbers of patients in each arm achieving complete response or better (with this group broken into “stringent complete response” as well as complete response). Significantly more carfilzomib than bortezomib patients reached this mark (58 patients [13%] vs 29 patients [6%], P equal to 0.001). A larger group of patients in each arm met the secondary outcome measure of experiencing very good partial response or better, with those on the carfelzomib arm faring significantly better than those receiving bortezomib (252 [54%] vs 133 [29%], P less than 0.0001).
Dr. Dimopoulos and his co-authors remarked on the importance of these findings, noting that “The finding that the proportion of patients with a complete response or better and very good partial response or better was higher in the carfilzomib group than in the bortezomib group is encouraging because studies have shown an association between depth of response and improved survival in patients with multiple myeloma.”
ENDEAVOR’s safety analyses included all patients who received at least one dose of study drug. Overall, the carfilzomib patients had a 48% rate of serious adverse events (224 of 463 patients for this analysis), compared to 36% of the bortezomib group (162 of 456 patients).
On-study death rates were similar between the two groups, with 18 of 464 patients (4%) in the carfilzomib group and 16 of 465 patients (3%) in the bortezomib group dying during the study period. Four deaths in each arm were judged related to disease progression.
A pre-planned substudy examined cardiac function for patients in both study arms, and did not find increased risk of left or right ventricular dysfunction or cumulative cardiac injury for carfilzomib when compared with bortezomib.
The open label nature of the study, an acknowledged limitation, was necessitated by the different dosing regimens of the two drugs, but the treatment allocation was hidden from the independent review committee that assessed participant disease status. The funder was also masked to per-group treatment results.
Carfilzomib’s irreversable proteosome inhibition may lead to more sustained proteasomal inhibition, Dr. Dimopoulous and his co-authors posited. Also, carfilzomib can overcome bortezomib resistance and is more potent against cell lines naive to this class of drugs in preclinical studies, they said.
“Taken together, the results from the ENDEAVOR study suggest an important role for carfilzomib-based regimens for patients with relapsed or refractory jultiple myeloma,” wrote Dr. Dimopoulos and his collaborators.
The study was supported by Onyx Pharmaceuticals, Inc, a subsidiary of Amgen. Dr. Dimopoulos reported non-financial support from Onyx Pharmaceuticals, Celgene Corporation, and Ortho-Biotech. Several co-authors reported multiple financial associations with pharmaceutical companies.
On Twitter @karioakes
In a head-to-head clinical trial, carfilzomib (Kyprolis) plus dexamethasone doubled the length of progression-free survival (PFS) when compared with bortezomib (Velcade) plus dexamethasone for individuals with relapsed or refractory multiple myeloma. Response rates were also significantly higher for those receiving carfilzomib, though neither medication could overcome high-risk cytogenetic factors.
The international multi-center phase 3 open-label ENDEAVOR study (clinicaltrials.gov ID: NCT01568866) compared outcomes for a total of 929 patients who were randomized 1:1 to receive one of the treatments. Randomization was stratified to account for prior treatments, including prior proteasome treatment, as well as disease severity by International Staging System stage.
Reporting for the ENDEAVOR investigators, Dr. Meletios Dimopoulos and his co-authors published their results in The Lancet simultaneously with a presentation at the annual meeting of the American Society of Hematology [Lancet Oncol, http://dx.doi.org/10.1016/S1470-2045(15)00464-7] . Dr. Dimopoulos is a professor in the department of clinical therapeutics at the school of medicine of the National and Kapodistrian University of Athens.
The primary endpoint, PFS in the intention-to-treat population, differed significantly between the study arms when the data were analyzed at a pre-planned interim analysis. For those receiving carfilzomib, PFS was 18.7 months, compared with 9.4 months in the bortezomib group, for a hazard ratio of 0.53 (P less than 0.0001). Data were drawn from a pre-specified interim analysis, and study participation is ongoing, with 28-day dosing cycles repeated until disease progression occurrs or the patients experience unacceptable toxicity or withdraw consent.
Investigators had pre-specified subgroup analyses to examine what populations fared better and worse in each arm. Prior bortezomib exposure did not significantly affect PFS for those receiving carfilzomib. Not enough patients had received carfilzomib prior to the study to permit analysis of this effect. Though carfilzomib arm patients with high-risk factors on cytogenetic analysis fared slightly better than those on bortezomib, “neither proteasome inhibitor appears to significantly overcome the adverse prognostic effect of high-risk cytogenetics,” wrote Dr. Dimopoulos and his co-authors.
Secondary outcome measures included the numbers of patients in each arm achieving complete response or better (with this group broken into “stringent complete response” as well as complete response). Significantly more carfilzomib than bortezomib patients reached this mark (58 patients [13%] vs 29 patients [6%], P equal to 0.001). A larger group of patients in each arm met the secondary outcome measure of experiencing very good partial response or better, with those on the carfelzomib arm faring significantly better than those receiving bortezomib (252 [54%] vs 133 [29%], P less than 0.0001).
Dr. Dimopoulos and his co-authors remarked on the importance of these findings, noting that “The finding that the proportion of patients with a complete response or better and very good partial response or better was higher in the carfilzomib group than in the bortezomib group is encouraging because studies have shown an association between depth of response and improved survival in patients with multiple myeloma.”
ENDEAVOR’s safety analyses included all patients who received at least one dose of study drug. Overall, the carfilzomib patients had a 48% rate of serious adverse events (224 of 463 patients for this analysis), compared to 36% of the bortezomib group (162 of 456 patients).
On-study death rates were similar between the two groups, with 18 of 464 patients (4%) in the carfilzomib group and 16 of 465 patients (3%) in the bortezomib group dying during the study period. Four deaths in each arm were judged related to disease progression.
A pre-planned substudy examined cardiac function for patients in both study arms, and did not find increased risk of left or right ventricular dysfunction or cumulative cardiac injury for carfilzomib when compared with bortezomib.
The open label nature of the study, an acknowledged limitation, was necessitated by the different dosing regimens of the two drugs, but the treatment allocation was hidden from the independent review committee that assessed participant disease status. The funder was also masked to per-group treatment results.
Carfilzomib’s irreversable proteosome inhibition may lead to more sustained proteasomal inhibition, Dr. Dimopoulous and his co-authors posited. Also, carfilzomib can overcome bortezomib resistance and is more potent against cell lines naive to this class of drugs in preclinical studies, they said.
“Taken together, the results from the ENDEAVOR study suggest an important role for carfilzomib-based regimens for patients with relapsed or refractory jultiple myeloma,” wrote Dr. Dimopoulos and his collaborators.
The study was supported by Onyx Pharmaceuticals, Inc, a subsidiary of Amgen. Dr. Dimopoulos reported non-financial support from Onyx Pharmaceuticals, Celgene Corporation, and Ortho-Biotech. Several co-authors reported multiple financial associations with pharmaceutical companies.
On Twitter @karioakes
In a head-to-head clinical trial, carfilzomib (Kyprolis) plus dexamethasone doubled the length of progression-free survival (PFS) when compared with bortezomib (Velcade) plus dexamethasone for individuals with relapsed or refractory multiple myeloma. Response rates were also significantly higher for those receiving carfilzomib, though neither medication could overcome high-risk cytogenetic factors.
The international multi-center phase 3 open-label ENDEAVOR study (clinicaltrials.gov ID: NCT01568866) compared outcomes for a total of 929 patients who were randomized 1:1 to receive one of the treatments. Randomization was stratified to account for prior treatments, including prior proteasome treatment, as well as disease severity by International Staging System stage.
Reporting for the ENDEAVOR investigators, Dr. Meletios Dimopoulos and his co-authors published their results in The Lancet simultaneously with a presentation at the annual meeting of the American Society of Hematology [Lancet Oncol, http://dx.doi.org/10.1016/S1470-2045(15)00464-7] . Dr. Dimopoulos is a professor in the department of clinical therapeutics at the school of medicine of the National and Kapodistrian University of Athens.
The primary endpoint, PFS in the intention-to-treat population, differed significantly between the study arms when the data were analyzed at a pre-planned interim analysis. For those receiving carfilzomib, PFS was 18.7 months, compared with 9.4 months in the bortezomib group, for a hazard ratio of 0.53 (P less than 0.0001). Data were drawn from a pre-specified interim analysis, and study participation is ongoing, with 28-day dosing cycles repeated until disease progression occurrs or the patients experience unacceptable toxicity or withdraw consent.
Investigators had pre-specified subgroup analyses to examine what populations fared better and worse in each arm. Prior bortezomib exposure did not significantly affect PFS for those receiving carfilzomib. Not enough patients had received carfilzomib prior to the study to permit analysis of this effect. Though carfilzomib arm patients with high-risk factors on cytogenetic analysis fared slightly better than those on bortezomib, “neither proteasome inhibitor appears to significantly overcome the adverse prognostic effect of high-risk cytogenetics,” wrote Dr. Dimopoulos and his co-authors.
Secondary outcome measures included the numbers of patients in each arm achieving complete response or better (with this group broken into “stringent complete response” as well as complete response). Significantly more carfilzomib than bortezomib patients reached this mark (58 patients [13%] vs 29 patients [6%], P equal to 0.001). A larger group of patients in each arm met the secondary outcome measure of experiencing very good partial response or better, with those on the carfelzomib arm faring significantly better than those receiving bortezomib (252 [54%] vs 133 [29%], P less than 0.0001).
Dr. Dimopoulos and his co-authors remarked on the importance of these findings, noting that “The finding that the proportion of patients with a complete response or better and very good partial response or better was higher in the carfilzomib group than in the bortezomib group is encouraging because studies have shown an association between depth of response and improved survival in patients with multiple myeloma.”
ENDEAVOR’s safety analyses included all patients who received at least one dose of study drug. Overall, the carfilzomib patients had a 48% rate of serious adverse events (224 of 463 patients for this analysis), compared to 36% of the bortezomib group (162 of 456 patients).
On-study death rates were similar between the two groups, with 18 of 464 patients (4%) in the carfilzomib group and 16 of 465 patients (3%) in the bortezomib group dying during the study period. Four deaths in each arm were judged related to disease progression.
A pre-planned substudy examined cardiac function for patients in both study arms, and did not find increased risk of left or right ventricular dysfunction or cumulative cardiac injury for carfilzomib when compared with bortezomib.
The open label nature of the study, an acknowledged limitation, was necessitated by the different dosing regimens of the two drugs, but the treatment allocation was hidden from the independent review committee that assessed participant disease status. The funder was also masked to per-group treatment results.
Carfilzomib’s irreversable proteosome inhibition may lead to more sustained proteasomal inhibition, Dr. Dimopoulous and his co-authors posited. Also, carfilzomib can overcome bortezomib resistance and is more potent against cell lines naive to this class of drugs in preclinical studies, they said.
“Taken together, the results from the ENDEAVOR study suggest an important role for carfilzomib-based regimens for patients with relapsed or refractory jultiple myeloma,” wrote Dr. Dimopoulos and his collaborators.
The study was supported by Onyx Pharmaceuticals, Inc, a subsidiary of Amgen. Dr. Dimopoulos reported non-financial support from Onyx Pharmaceuticals, Celgene Corporation, and Ortho-Biotech. Several co-authors reported multiple financial associations with pharmaceutical companies.
On Twitter @karioakes
FROM ASH 2015
Key clinical point: Carfilzomib nearly doubled progression-free survival (PFS) compared with bortezomib for relapsed and refractory multiple myeloma
Major finding: For those receiving carfilzomib, PFS was 18.7 months, compared with 9.4 months in the bortezomib group, for a hazard ratio of 0.53 (P less than .0001).
Data source: International randomized open-label clinical trial of 979 patients with refractory or relapsed multiple myeloma.
Disclosures: The study was supported by Onyx Pharmaceuticals, Inc, a subsidiary of Amgen. Dr. Dimopoulos reported non-financial support from Onyx Pharmaceuticals, Celgene Corporation, and Ortho-Biotech. Several co-authors reported multiple financial associations with pharmaceutical companies.
Bone can reactivate dormant MM cells, study suggests

to the tibia of a mouse
Image courtesy of the Garvan
Institute of Medical Research
Cancer cells that lie dormant in the bone can be “woken up” by changes in their surroundings, according to researchers.
The group used microscopy techniques to study multiple myeloma (MM) cells that lay “sleeping” in mouse bones.
The experiment revealed that dormant cells can be reactivated when bone tissue is broken down around them, suggesting new possibilities for
treating metastatic cancers in bone.
“Once a cancer spreads to bone, it becomes notoriously difficult to treat,” said study author Peter Croucher, PhD, of the Garvan Institute of Medical Research in Sydney, New South Wales, Australia.
“So it’s important to establish exactly what wakes those cells in bone. Is it some signal within the cells themselves, or is it a change in their environment?”
The researchers set out to discover which scenario is correct and reported their findings in Nature Communications.
Using a technique called intravital 2-photon microscopy, the team tracked the fate of dormant MM cells in the tibia of living mice.
They introduced MM cells into the mice and watched as a small number of the cells lodged in the tibia and “went to sleep.” These cells could be detected because they contained a fluorescent dye that was quickly lost from dividing cells.
“Because we were looking at a long bone like a tibia, we could watch the same sleeping cancer cells, in the same bone, in the same mouse, over a long period of time, and this is something that hasn’t been done before,” said Tri Giang Phan, PhD, of the Garvan Institute of Medical Research.
Dr Croucher said that studying the same set of cells over a period of months revealed vital clues about what caused them to reactivate.
“Because we’ve done it this way, we can show that there are a great many dormant cells, yet only some of them get woken up, and those that do wake, wake at different times,” he noted.
“We even saw some cells that woke then went back to sleep again. The fact that these myeloma cells behave so differently, despite coming from the same cancer cell line, gave us our first clue that it is a signal from outside the cells that is controlling when they wake.”
Explaining the phenomenon
The researchers’ next challenge was to determine the precise nature of the “wake-up call” from bone.
“[W]e’ve shown that bone’s dynamic process of building up and breaking down can send signals to cancer cells to stay sleeping or to wake,” said Michelle McDonald, PhD, of the Garvan Institute of Medical Research.
“We were able to show that myeloma cells are usually kept asleep by close association with a layer of osteoblast-like cells, called bone-lining cells, in the endosteum. The bone-lining cells are essentially inactive, so we can think of them as providing a quiet environment in which myeloma cells sleep undisturbed.”
“Crucially, we can wake those myeloma cells by activating osteoclasts, which break down bone tissue. We think the osteoclasts are physically changing the local environment of the cancer cells and waking them up in the process, as if they were literally throwing them out of bed.”
“We know that bone remodeling is going on in all of us. So a myeloma cell could be woken in an essentially random fashion, by having its local environment remodeled by osteoclasts. Essentially, a cancer cell could be woken by being in the wrong place at the wrong time.”
Implications for treatment
So what do these findings mean for treating secondary cancers in bone?
“Now we can see that the cancer cells are woken by changes in the surrounding bone, we can think in a whole new way about treating bone metastasis,” Dr Croucher said. “And there are 2 treatment approaches in particular that have promise.”
“The first is that we could inhibit the breakdown of bone by osteoclasts so as to keep cancer cells in long-term hibernation. In fact, there are already drugs that can do this, such as bisphosphonates, and there’s already evidence that these drugs do improve survival in breast cancer patients.”
“The other, more radical, option is to do the opposite—to wake the sleeping cells by activating osteoclasts and driving the breakdown of bone. Most cancer treatments target active, dividing cells. So waking the sleeping cells should make them susceptible to those therapies and, ultimately, could eradicate any residual disease.” ![]()

to the tibia of a mouse
Image courtesy of the Garvan
Institute of Medical Research
Cancer cells that lie dormant in the bone can be “woken up” by changes in their surroundings, according to researchers.
The group used microscopy techniques to study multiple myeloma (MM) cells that lay “sleeping” in mouse bones.
The experiment revealed that dormant cells can be reactivated when bone tissue is broken down around them, suggesting new possibilities for
treating metastatic cancers in bone.
“Once a cancer spreads to bone, it becomes notoriously difficult to treat,” said study author Peter Croucher, PhD, of the Garvan Institute of Medical Research in Sydney, New South Wales, Australia.
“So it’s important to establish exactly what wakes those cells in bone. Is it some signal within the cells themselves, or is it a change in their environment?”
The researchers set out to discover which scenario is correct and reported their findings in Nature Communications.
Using a technique called intravital 2-photon microscopy, the team tracked the fate of dormant MM cells in the tibia of living mice.
They introduced MM cells into the mice and watched as a small number of the cells lodged in the tibia and “went to sleep.” These cells could be detected because they contained a fluorescent dye that was quickly lost from dividing cells.
“Because we were looking at a long bone like a tibia, we could watch the same sleeping cancer cells, in the same bone, in the same mouse, over a long period of time, and this is something that hasn’t been done before,” said Tri Giang Phan, PhD, of the Garvan Institute of Medical Research.
Dr Croucher said that studying the same set of cells over a period of months revealed vital clues about what caused them to reactivate.
“Because we’ve done it this way, we can show that there are a great many dormant cells, yet only some of them get woken up, and those that do wake, wake at different times,” he noted.
“We even saw some cells that woke then went back to sleep again. The fact that these myeloma cells behave so differently, despite coming from the same cancer cell line, gave us our first clue that it is a signal from outside the cells that is controlling when they wake.”
Explaining the phenomenon
The researchers’ next challenge was to determine the precise nature of the “wake-up call” from bone.
“[W]e’ve shown that bone’s dynamic process of building up and breaking down can send signals to cancer cells to stay sleeping or to wake,” said Michelle McDonald, PhD, of the Garvan Institute of Medical Research.
“We were able to show that myeloma cells are usually kept asleep by close association with a layer of osteoblast-like cells, called bone-lining cells, in the endosteum. The bone-lining cells are essentially inactive, so we can think of them as providing a quiet environment in which myeloma cells sleep undisturbed.”
“Crucially, we can wake those myeloma cells by activating osteoclasts, which break down bone tissue. We think the osteoclasts are physically changing the local environment of the cancer cells and waking them up in the process, as if they were literally throwing them out of bed.”
“We know that bone remodeling is going on in all of us. So a myeloma cell could be woken in an essentially random fashion, by having its local environment remodeled by osteoclasts. Essentially, a cancer cell could be woken by being in the wrong place at the wrong time.”
Implications for treatment
So what do these findings mean for treating secondary cancers in bone?
“Now we can see that the cancer cells are woken by changes in the surrounding bone, we can think in a whole new way about treating bone metastasis,” Dr Croucher said. “And there are 2 treatment approaches in particular that have promise.”
“The first is that we could inhibit the breakdown of bone by osteoclasts so as to keep cancer cells in long-term hibernation. In fact, there are already drugs that can do this, such as bisphosphonates, and there’s already evidence that these drugs do improve survival in breast cancer patients.”
“The other, more radical, option is to do the opposite—to wake the sleeping cells by activating osteoclasts and driving the breakdown of bone. Most cancer treatments target active, dividing cells. So waking the sleeping cells should make them susceptible to those therapies and, ultimately, could eradicate any residual disease.” ![]()

to the tibia of a mouse
Image courtesy of the Garvan
Institute of Medical Research
Cancer cells that lie dormant in the bone can be “woken up” by changes in their surroundings, according to researchers.
The group used microscopy techniques to study multiple myeloma (MM) cells that lay “sleeping” in mouse bones.
The experiment revealed that dormant cells can be reactivated when bone tissue is broken down around them, suggesting new possibilities for
treating metastatic cancers in bone.
“Once a cancer spreads to bone, it becomes notoriously difficult to treat,” said study author Peter Croucher, PhD, of the Garvan Institute of Medical Research in Sydney, New South Wales, Australia.
“So it’s important to establish exactly what wakes those cells in bone. Is it some signal within the cells themselves, or is it a change in their environment?”
The researchers set out to discover which scenario is correct and reported their findings in Nature Communications.
Using a technique called intravital 2-photon microscopy, the team tracked the fate of dormant MM cells in the tibia of living mice.
They introduced MM cells into the mice and watched as a small number of the cells lodged in the tibia and “went to sleep.” These cells could be detected because they contained a fluorescent dye that was quickly lost from dividing cells.
“Because we were looking at a long bone like a tibia, we could watch the same sleeping cancer cells, in the same bone, in the same mouse, over a long period of time, and this is something that hasn’t been done before,” said Tri Giang Phan, PhD, of the Garvan Institute of Medical Research.
Dr Croucher said that studying the same set of cells over a period of months revealed vital clues about what caused them to reactivate.
“Because we’ve done it this way, we can show that there are a great many dormant cells, yet only some of them get woken up, and those that do wake, wake at different times,” he noted.
“We even saw some cells that woke then went back to sleep again. The fact that these myeloma cells behave so differently, despite coming from the same cancer cell line, gave us our first clue that it is a signal from outside the cells that is controlling when they wake.”
Explaining the phenomenon
The researchers’ next challenge was to determine the precise nature of the “wake-up call” from bone.
“[W]e’ve shown that bone’s dynamic process of building up and breaking down can send signals to cancer cells to stay sleeping or to wake,” said Michelle McDonald, PhD, of the Garvan Institute of Medical Research.
“We were able to show that myeloma cells are usually kept asleep by close association with a layer of osteoblast-like cells, called bone-lining cells, in the endosteum. The bone-lining cells are essentially inactive, so we can think of them as providing a quiet environment in which myeloma cells sleep undisturbed.”
“Crucially, we can wake those myeloma cells by activating osteoclasts, which break down bone tissue. We think the osteoclasts are physically changing the local environment of the cancer cells and waking them up in the process, as if they were literally throwing them out of bed.”
“We know that bone remodeling is going on in all of us. So a myeloma cell could be woken in an essentially random fashion, by having its local environment remodeled by osteoclasts. Essentially, a cancer cell could be woken by being in the wrong place at the wrong time.”
Implications for treatment
So what do these findings mean for treating secondary cancers in bone?
“Now we can see that the cancer cells are woken by changes in the surrounding bone, we can think in a whole new way about treating bone metastasis,” Dr Croucher said. “And there are 2 treatment approaches in particular that have promise.”
“The first is that we could inhibit the breakdown of bone by osteoclasts so as to keep cancer cells in long-term hibernation. In fact, there are already drugs that can do this, such as bisphosphonates, and there’s already evidence that these drugs do improve survival in breast cancer patients.”
“The other, more radical, option is to do the opposite—to wake the sleeping cells by activating osteoclasts and driving the breakdown of bone. Most cancer treatments target active, dividing cells. So waking the sleeping cells should make them susceptible to those therapies and, ultimately, could eradicate any residual disease.” ![]()
Multiple myeloma advances will be a hot topic at ASH
With the approvals of three new therapies for multiple myeloma in just the last month – elotuzumab, ixazomib, and daratumumab – sessions at ASH 2015 will be buzzing with discussions of how the availability of these new therapies is likely to influence disease management. Other leading abstracts, highlighted at a press conference prior to the annual meeting of the American Society of Hematology, address gene therapy, precision medicine, and stem cell transplant for sickle cell disease. We’re providing the links to these top abstracts here, and invite you to look for our upcoming daily newsletters and next-best-thing-to-being-there coverage of ASH.
Experimental, targeted treatments for blood cancer
• 507: Daratumumab in Combination with Lenalidomide and Dexamethasone in Patients with Relapsed or Relapsed and Refractory Multiple Myeloma: Updated Results of a Phase I/II Study (GEN503).
• 727: Ixazomib, an Investigational Oral Proteasome Inhibitor (PI), in Combination with Lenalidomide and Dexamethasone (IRd), Significantly Extends Progression-Free Survival (PFS) for Patients (Pts) with Relapsed and/or Refractory Multiple Myeloma (RRMM): The Phase III Tourmaline-MM1 Study (NCT01564537).
• 391: Autologous Transplantation for Multiple Myeloma in the Era of New Drugs: A Phase III Study of the Intergroupe Francophone Du Myelome (IFM/DFCI 2009 Trial).
• 495: Results from the International, Randomized Phase III Study of Ibrutinib Versus Chlorambucil in Patients 65 Years and Older with Treatment-Naïve CLL/SLL (RESONATE-2TM).
Experimental gene therapy
• 201: Update of Results from the Northstar Study (HGB-204): A Phase I/II Study of Gene Therapy for Beta-Thalassemia Major Via Transplantation of Autologous Hematopoietic Stem Cells Transduced Ex-Vivo with a Lentiviral Beta AT87Q-Globin Vector (LentiGlobin BB305 Drug Product).
• 261: Lentiviral Hematopoietic Stem Cell Gene Therapy for Older Patients with X-Linked Severe Combined Immunodeficiency.
Precision medicine
• 250: Genetic Risk Factors for the Development of Osteonecrosis in Children Under Age 10 Treated for Acute Lymphoblastic Leukemia.
• Special Scientific Symposium: Precision Medicine in Cancer Therapy.
Coagulation
• 5: Source of Factor VIII Replacement (PLASMATIC OR RECOMBINANT) and Incidence of Inhibitory Alloantibodies in Previously Untreated Patients with Severe Hemophilia a: The Multicenter Randomized Sippet Study.
New sickle cell disease research
•541: Hematopoietic Stem Cell Transplantation from HLA Identical Sibling For Sickle Cell Disease an International Survey on Behalf of Eurocord-Monacord, EBMT Paediatric Disease Working Party and CIBMTR.
With the approvals of three new therapies for multiple myeloma in just the last month – elotuzumab, ixazomib, and daratumumab – sessions at ASH 2015 will be buzzing with discussions of how the availability of these new therapies is likely to influence disease management. Other leading abstracts, highlighted at a press conference prior to the annual meeting of the American Society of Hematology, address gene therapy, precision medicine, and stem cell transplant for sickle cell disease. We’re providing the links to these top abstracts here, and invite you to look for our upcoming daily newsletters and next-best-thing-to-being-there coverage of ASH.
Experimental, targeted treatments for blood cancer
• 507: Daratumumab in Combination with Lenalidomide and Dexamethasone in Patients with Relapsed or Relapsed and Refractory Multiple Myeloma: Updated Results of a Phase I/II Study (GEN503).
• 727: Ixazomib, an Investigational Oral Proteasome Inhibitor (PI), in Combination with Lenalidomide and Dexamethasone (IRd), Significantly Extends Progression-Free Survival (PFS) for Patients (Pts) with Relapsed and/or Refractory Multiple Myeloma (RRMM): The Phase III Tourmaline-MM1 Study (NCT01564537).
• 391: Autologous Transplantation for Multiple Myeloma in the Era of New Drugs: A Phase III Study of the Intergroupe Francophone Du Myelome (IFM/DFCI 2009 Trial).
• 495: Results from the International, Randomized Phase III Study of Ibrutinib Versus Chlorambucil in Patients 65 Years and Older with Treatment-Naïve CLL/SLL (RESONATE-2TM).
Experimental gene therapy
• 201: Update of Results from the Northstar Study (HGB-204): A Phase I/II Study of Gene Therapy for Beta-Thalassemia Major Via Transplantation of Autologous Hematopoietic Stem Cells Transduced Ex-Vivo with a Lentiviral Beta AT87Q-Globin Vector (LentiGlobin BB305 Drug Product).
• 261: Lentiviral Hematopoietic Stem Cell Gene Therapy for Older Patients with X-Linked Severe Combined Immunodeficiency.
Precision medicine
• 250: Genetic Risk Factors for the Development of Osteonecrosis in Children Under Age 10 Treated for Acute Lymphoblastic Leukemia.
• Special Scientific Symposium: Precision Medicine in Cancer Therapy.
Coagulation
• 5: Source of Factor VIII Replacement (PLASMATIC OR RECOMBINANT) and Incidence of Inhibitory Alloantibodies in Previously Untreated Patients with Severe Hemophilia a: The Multicenter Randomized Sippet Study.
New sickle cell disease research
•541: Hematopoietic Stem Cell Transplantation from HLA Identical Sibling For Sickle Cell Disease an International Survey on Behalf of Eurocord-Monacord, EBMT Paediatric Disease Working Party and CIBMTR.
With the approvals of three new therapies for multiple myeloma in just the last month – elotuzumab, ixazomib, and daratumumab – sessions at ASH 2015 will be buzzing with discussions of how the availability of these new therapies is likely to influence disease management. Other leading abstracts, highlighted at a press conference prior to the annual meeting of the American Society of Hematology, address gene therapy, precision medicine, and stem cell transplant for sickle cell disease. We’re providing the links to these top abstracts here, and invite you to look for our upcoming daily newsletters and next-best-thing-to-being-there coverage of ASH.
Experimental, targeted treatments for blood cancer
• 507: Daratumumab in Combination with Lenalidomide and Dexamethasone in Patients with Relapsed or Relapsed and Refractory Multiple Myeloma: Updated Results of a Phase I/II Study (GEN503).
• 727: Ixazomib, an Investigational Oral Proteasome Inhibitor (PI), in Combination with Lenalidomide and Dexamethasone (IRd), Significantly Extends Progression-Free Survival (PFS) for Patients (Pts) with Relapsed and/or Refractory Multiple Myeloma (RRMM): The Phase III Tourmaline-MM1 Study (NCT01564537).
• 391: Autologous Transplantation for Multiple Myeloma in the Era of New Drugs: A Phase III Study of the Intergroupe Francophone Du Myelome (IFM/DFCI 2009 Trial).
• 495: Results from the International, Randomized Phase III Study of Ibrutinib Versus Chlorambucil in Patients 65 Years and Older with Treatment-Naïve CLL/SLL (RESONATE-2TM).
Experimental gene therapy
• 201: Update of Results from the Northstar Study (HGB-204): A Phase I/II Study of Gene Therapy for Beta-Thalassemia Major Via Transplantation of Autologous Hematopoietic Stem Cells Transduced Ex-Vivo with a Lentiviral Beta AT87Q-Globin Vector (LentiGlobin BB305 Drug Product).
• 261: Lentiviral Hematopoietic Stem Cell Gene Therapy for Older Patients with X-Linked Severe Combined Immunodeficiency.
Precision medicine
• 250: Genetic Risk Factors for the Development of Osteonecrosis in Children Under Age 10 Treated for Acute Lymphoblastic Leukemia.
• Special Scientific Symposium: Precision Medicine in Cancer Therapy.
Coagulation
• 5: Source of Factor VIII Replacement (PLASMATIC OR RECOMBINANT) and Incidence of Inhibitory Alloantibodies in Previously Untreated Patients with Severe Hemophilia a: The Multicenter Randomized Sippet Study.
New sickle cell disease research
•541: Hematopoietic Stem Cell Transplantation from HLA Identical Sibling For Sickle Cell Disease an International Survey on Behalf of Eurocord-Monacord, EBMT Paediatric Disease Working Party and CIBMTR.
FROM ASH 2015