User login
FDA approves elotuzumab for MM

Photo courtesy of
Bristol-Myers Squibb
The US Food and Drug Administration (FDA) has approved elotuzumab (Empliciti) for use in combination with lenalidomide and dexamethasone to treat multiple myeloma (MM) patients who have received 1 to 3 prior therapies.
Elotuzumab is an immunostimulatory antibody that specifically targets signaling lymphocyte activation molecule family member 7 (SLAMF7), a cell-surface glycoprotein that is expressed on myeloma cells independent of cytogenetic abnormalities.
Elotuzumab is the first immunostimulatory antibody approved for MM.
Bristol-Myers Squibb said it expects to begin shipping elotuzumab this week. The drug will be available for injection for intravenous use in 300 mg and 400 mg vials.
Elotuzumab is currently under review by the European Medicines Agency and has been granted accelerated assessment.
The FDA previously granted elotuzumab breakthrough therapy designation, orphan drug designation, and priority review.
Bristol-Myers Squibb and AbbVie are co-developing elotuzumab, with Bristol-Myers Squibb solely responsible for commercial activities. For more details on the drug, see the full prescribing information.
ELOQUENT-2 trial
The FDA’s approval of elotuzumab is primarily based on data from the phase 3 ELOQUENT-2 trial, which were presented at ASCO 2015 and published in NEJM.
The trial included 646 MM patients who had received 1 to 3 prior therapies. Baseline patient demographics and disease characteristics were well balanced between treatment arms.
Patients were randomized 1:1 to receive either elotuzumab at 10 mg/kg in combination with lenalidomide and dexamethasone (len-dex) or len-dex alone in 4-week cycles until disease progression or unacceptable toxicity.
The minimum follow-up for all study subjects was 24 months. The co-primary endpoints were progression-free survival (PFS) and overall response rate.
The overall response rate was 78.5% in the elotuzumab arm and 65.5% in the len-dex arm (P=0.0002).
The median PFS was 19.4 months in the elotuzumab arm and 14.9 months in the len-dex arm (P=0.0004). At 1 year, the PFS was 68% in the elotuzumab arm and 57% in the len-dex arm. At 2 years, the PFS was 41% and 27%, respectively.
Serious adverse events occurred in 65.4% of patients in the elotuzumab arm and 56.5% in the len-dex arm. The most frequent serious adverse events in each arm, respectively, were pneumonia (15.4% vs 11%), pyrexia (6.9% vs 4.7%), respiratory tract infection (3.1% vs 1.3%), anemia (2.8% vs 1.9%), pulmonary embolism (3.1% vs 2.5%), and acute renal failure (2.5% vs 1.9%).
The most common adverse events in the elotuzumab arm and len-dex arm, respectively, were fatigue (61.6% vs 51.7%), diarrhea (46.9% vs 36.0%), pyrexia (37.4% vs 24.6%), constipation (35.5% vs 27.1%), cough (34.3% vs 18.9%), peripheral neuropathy (26.7% vs 20.8%), nasopharyngitis (24.5% vs 19.2%), upper respiratory tract infection (22.6% vs 17.4%), decreased appetite (20.8% vs 12.6%), and pneumonia (20.1% vs 14.2%). ![]()

Photo courtesy of
Bristol-Myers Squibb
The US Food and Drug Administration (FDA) has approved elotuzumab (Empliciti) for use in combination with lenalidomide and dexamethasone to treat multiple myeloma (MM) patients who have received 1 to 3 prior therapies.
Elotuzumab is an immunostimulatory antibody that specifically targets signaling lymphocyte activation molecule family member 7 (SLAMF7), a cell-surface glycoprotein that is expressed on myeloma cells independent of cytogenetic abnormalities.
Elotuzumab is the first immunostimulatory antibody approved for MM.
Bristol-Myers Squibb said it expects to begin shipping elotuzumab this week. The drug will be available for injection for intravenous use in 300 mg and 400 mg vials.
Elotuzumab is currently under review by the European Medicines Agency and has been granted accelerated assessment.
The FDA previously granted elotuzumab breakthrough therapy designation, orphan drug designation, and priority review.
Bristol-Myers Squibb and AbbVie are co-developing elotuzumab, with Bristol-Myers Squibb solely responsible for commercial activities. For more details on the drug, see the full prescribing information.
ELOQUENT-2 trial
The FDA’s approval of elotuzumab is primarily based on data from the phase 3 ELOQUENT-2 trial, which were presented at ASCO 2015 and published in NEJM.
The trial included 646 MM patients who had received 1 to 3 prior therapies. Baseline patient demographics and disease characteristics were well balanced between treatment arms.
Patients were randomized 1:1 to receive either elotuzumab at 10 mg/kg in combination with lenalidomide and dexamethasone (len-dex) or len-dex alone in 4-week cycles until disease progression or unacceptable toxicity.
The minimum follow-up for all study subjects was 24 months. The co-primary endpoints were progression-free survival (PFS) and overall response rate.
The overall response rate was 78.5% in the elotuzumab arm and 65.5% in the len-dex arm (P=0.0002).
The median PFS was 19.4 months in the elotuzumab arm and 14.9 months in the len-dex arm (P=0.0004). At 1 year, the PFS was 68% in the elotuzumab arm and 57% in the len-dex arm. At 2 years, the PFS was 41% and 27%, respectively.
Serious adverse events occurred in 65.4% of patients in the elotuzumab arm and 56.5% in the len-dex arm. The most frequent serious adverse events in each arm, respectively, were pneumonia (15.4% vs 11%), pyrexia (6.9% vs 4.7%), respiratory tract infection (3.1% vs 1.3%), anemia (2.8% vs 1.9%), pulmonary embolism (3.1% vs 2.5%), and acute renal failure (2.5% vs 1.9%).
The most common adverse events in the elotuzumab arm and len-dex arm, respectively, were fatigue (61.6% vs 51.7%), diarrhea (46.9% vs 36.0%), pyrexia (37.4% vs 24.6%), constipation (35.5% vs 27.1%), cough (34.3% vs 18.9%), peripheral neuropathy (26.7% vs 20.8%), nasopharyngitis (24.5% vs 19.2%), upper respiratory tract infection (22.6% vs 17.4%), decreased appetite (20.8% vs 12.6%), and pneumonia (20.1% vs 14.2%). ![]()

Photo courtesy of
Bristol-Myers Squibb
The US Food and Drug Administration (FDA) has approved elotuzumab (Empliciti) for use in combination with lenalidomide and dexamethasone to treat multiple myeloma (MM) patients who have received 1 to 3 prior therapies.
Elotuzumab is an immunostimulatory antibody that specifically targets signaling lymphocyte activation molecule family member 7 (SLAMF7), a cell-surface glycoprotein that is expressed on myeloma cells independent of cytogenetic abnormalities.
Elotuzumab is the first immunostimulatory antibody approved for MM.
Bristol-Myers Squibb said it expects to begin shipping elotuzumab this week. The drug will be available for injection for intravenous use in 300 mg and 400 mg vials.
Elotuzumab is currently under review by the European Medicines Agency and has been granted accelerated assessment.
The FDA previously granted elotuzumab breakthrough therapy designation, orphan drug designation, and priority review.
Bristol-Myers Squibb and AbbVie are co-developing elotuzumab, with Bristol-Myers Squibb solely responsible for commercial activities. For more details on the drug, see the full prescribing information.
ELOQUENT-2 trial
The FDA’s approval of elotuzumab is primarily based on data from the phase 3 ELOQUENT-2 trial, which were presented at ASCO 2015 and published in NEJM.
The trial included 646 MM patients who had received 1 to 3 prior therapies. Baseline patient demographics and disease characteristics were well balanced between treatment arms.
Patients were randomized 1:1 to receive either elotuzumab at 10 mg/kg in combination with lenalidomide and dexamethasone (len-dex) or len-dex alone in 4-week cycles until disease progression or unacceptable toxicity.
The minimum follow-up for all study subjects was 24 months. The co-primary endpoints were progression-free survival (PFS) and overall response rate.
The overall response rate was 78.5% in the elotuzumab arm and 65.5% in the len-dex arm (P=0.0002).
The median PFS was 19.4 months in the elotuzumab arm and 14.9 months in the len-dex arm (P=0.0004). At 1 year, the PFS was 68% in the elotuzumab arm and 57% in the len-dex arm. At 2 years, the PFS was 41% and 27%, respectively.
Serious adverse events occurred in 65.4% of patients in the elotuzumab arm and 56.5% in the len-dex arm. The most frequent serious adverse events in each arm, respectively, were pneumonia (15.4% vs 11%), pyrexia (6.9% vs 4.7%), respiratory tract infection (3.1% vs 1.3%), anemia (2.8% vs 1.9%), pulmonary embolism (3.1% vs 2.5%), and acute renal failure (2.5% vs 1.9%).
The most common adverse events in the elotuzumab arm and len-dex arm, respectively, were fatigue (61.6% vs 51.7%), diarrhea (46.9% vs 36.0%), pyrexia (37.4% vs 24.6%), constipation (35.5% vs 27.1%), cough (34.3% vs 18.9%), peripheral neuropathy (26.7% vs 20.8%), nasopharyngitis (24.5% vs 19.2%), upper respiratory tract infection (22.6% vs 17.4%), decreased appetite (20.8% vs 12.6%), and pneumonia (20.1% vs 14.2%). ![]()
Elotuzumab approved for multiple myeloma
Elotuzumab (Empliciti) has been approved as combination therapy for individuals with relapsed or refractory multiple myeloma, the Food and Drug Administration announced Nov. 30.
Elotuzumab’s approval was based on a randomized, open-label clinical trial of 646 individuals with relapsed or refractory multiple myeloma. The multicenter trial compared progression-free survival (PFS) and overall response rate (ORR) for 321 individuals receiving lenalidomide (Revlimid) and dexamethasone to the PFS and ORR for 325 individuals receiving elotuzumab, lenalidomide, and dexamethasone.
For individuals receiving elotuzumab together with lenalidomide and dexamethasone, the median PFS of 19.4 months was significantly longer than the median 14.9 months of PFS seen in those receiving just lenalidomide and dexamethasone. For the elotuzumab-containing arm, the ORR was also significantly greater at 78.5%, compared with an ORR of 65.5% for the arm not receiving elotuzumab.
Slightly more patients in the elotuzumab-containing arm experienced serious adverse events, at 65.4% vs. 56.5% for those not receiving elotuzumab. Of the adverse reactions seen in more than 20% of patients, those that occurred more frequently in patients receiving elotuzumab included fatigue, diarrhea, fever, constipation, cough, peripheral neuropathy, upper respiratory tract infection, decreased appetite, and pneumonia.
Elotuzumab is a monoclonal antibody given intravenously; it can interfere with determination of complete response, and infusion reactions, infections, second primary malignancies, and hepatotoxicity may also occur.
Elotuzumab’s target is the surface antigen signaling lymphocyte activation molecule family 7 (SLAMF7). This protein is present on malignant cells in multiple myeloma and is also present on human immune cells such as natural killer cells and monocytes. The recommended dosing is 10 mg/kg intravenously weekly for 2 weeks, then every 2 weeks until disease progression or unacceptable toxicity occurs. Acetaminophen and histamine1 (H1) and H2 blockade should be given preadministration.
“The approval of elotuzumab marks another important milestone in the treatment of multiple myeloma in a short period of time,” Walter M. Capone, president and CEO of the Multiple Myeloma Research Foundation, said in a statement.
Today’s approval is the third in November for multiple myeloma therapies, following the Nov. 16 approval of the monoclonal antibody daratumumab (Darzalex) and the Nov. 20 approval of the oral proteasome inhibitor ixazomib (Ninlaro).
Elotuzumab received priority review by the FDA as a breakthrough drug and also has orphan drug designation. Elotuzumab will be marketed as Empliciti by Bristol-Myers Squibb.
On Twitter @karioakes
Elotuzumab (Empliciti) has been approved as combination therapy for individuals with relapsed or refractory multiple myeloma, the Food and Drug Administration announced Nov. 30.
Elotuzumab’s approval was based on a randomized, open-label clinical trial of 646 individuals with relapsed or refractory multiple myeloma. The multicenter trial compared progression-free survival (PFS) and overall response rate (ORR) for 321 individuals receiving lenalidomide (Revlimid) and dexamethasone to the PFS and ORR for 325 individuals receiving elotuzumab, lenalidomide, and dexamethasone.
For individuals receiving elotuzumab together with lenalidomide and dexamethasone, the median PFS of 19.4 months was significantly longer than the median 14.9 months of PFS seen in those receiving just lenalidomide and dexamethasone. For the elotuzumab-containing arm, the ORR was also significantly greater at 78.5%, compared with an ORR of 65.5% for the arm not receiving elotuzumab.
Slightly more patients in the elotuzumab-containing arm experienced serious adverse events, at 65.4% vs. 56.5% for those not receiving elotuzumab. Of the adverse reactions seen in more than 20% of patients, those that occurred more frequently in patients receiving elotuzumab included fatigue, diarrhea, fever, constipation, cough, peripheral neuropathy, upper respiratory tract infection, decreased appetite, and pneumonia.
Elotuzumab is a monoclonal antibody given intravenously; it can interfere with determination of complete response, and infusion reactions, infections, second primary malignancies, and hepatotoxicity may also occur.
Elotuzumab’s target is the surface antigen signaling lymphocyte activation molecule family 7 (SLAMF7). This protein is present on malignant cells in multiple myeloma and is also present on human immune cells such as natural killer cells and monocytes. The recommended dosing is 10 mg/kg intravenously weekly for 2 weeks, then every 2 weeks until disease progression or unacceptable toxicity occurs. Acetaminophen and histamine1 (H1) and H2 blockade should be given preadministration.
“The approval of elotuzumab marks another important milestone in the treatment of multiple myeloma in a short period of time,” Walter M. Capone, president and CEO of the Multiple Myeloma Research Foundation, said in a statement.
Today’s approval is the third in November for multiple myeloma therapies, following the Nov. 16 approval of the monoclonal antibody daratumumab (Darzalex) and the Nov. 20 approval of the oral proteasome inhibitor ixazomib (Ninlaro).
Elotuzumab received priority review by the FDA as a breakthrough drug and also has orphan drug designation. Elotuzumab will be marketed as Empliciti by Bristol-Myers Squibb.
On Twitter @karioakes
Elotuzumab (Empliciti) has been approved as combination therapy for individuals with relapsed or refractory multiple myeloma, the Food and Drug Administration announced Nov. 30.
Elotuzumab’s approval was based on a randomized, open-label clinical trial of 646 individuals with relapsed or refractory multiple myeloma. The multicenter trial compared progression-free survival (PFS) and overall response rate (ORR) for 321 individuals receiving lenalidomide (Revlimid) and dexamethasone to the PFS and ORR for 325 individuals receiving elotuzumab, lenalidomide, and dexamethasone.
For individuals receiving elotuzumab together with lenalidomide and dexamethasone, the median PFS of 19.4 months was significantly longer than the median 14.9 months of PFS seen in those receiving just lenalidomide and dexamethasone. For the elotuzumab-containing arm, the ORR was also significantly greater at 78.5%, compared with an ORR of 65.5% for the arm not receiving elotuzumab.
Slightly more patients in the elotuzumab-containing arm experienced serious adverse events, at 65.4% vs. 56.5% for those not receiving elotuzumab. Of the adverse reactions seen in more than 20% of patients, those that occurred more frequently in patients receiving elotuzumab included fatigue, diarrhea, fever, constipation, cough, peripheral neuropathy, upper respiratory tract infection, decreased appetite, and pneumonia.
Elotuzumab is a monoclonal antibody given intravenously; it can interfere with determination of complete response, and infusion reactions, infections, second primary malignancies, and hepatotoxicity may also occur.
Elotuzumab’s target is the surface antigen signaling lymphocyte activation molecule family 7 (SLAMF7). This protein is present on malignant cells in multiple myeloma and is also present on human immune cells such as natural killer cells and monocytes. The recommended dosing is 10 mg/kg intravenously weekly for 2 weeks, then every 2 weeks until disease progression or unacceptable toxicity occurs. Acetaminophen and histamine1 (H1) and H2 blockade should be given preadministration.
“The approval of elotuzumab marks another important milestone in the treatment of multiple myeloma in a short period of time,” Walter M. Capone, president and CEO of the Multiple Myeloma Research Foundation, said in a statement.
Today’s approval is the third in November for multiple myeloma therapies, following the Nov. 16 approval of the monoclonal antibody daratumumab (Darzalex) and the Nov. 20 approval of the oral proteasome inhibitor ixazomib (Ninlaro).
Elotuzumab received priority review by the FDA as a breakthrough drug and also has orphan drug designation. Elotuzumab will be marketed as Empliciti by Bristol-Myers Squibb.
On Twitter @karioakes
Prognostic test for MM granted CE-IVD mark

Photo courtesy of SkylineDx
The MMprofiler™, a test used to risk-stratify patients with multiple myeloma (MM), has received the CE-IVD mark.
The CE-IVD mark indicates that an in vitro device complies with the European In Vitro Diagnostics Directive and may be legally commercialized and distributed in the European Union.
The MMprofiler classifies patients into high- or standard-risk groups based on the activity of 92 genes considered to be related to MM.
In a 2012 Leukemia paper, researchers described a gene-expression signature, now known as SKY92, that maps the activity of the 92 genes. MM patients who were defined as high-risk by the SKY92 gene signature (called “the EMC92 gene signature” in the paper) had inferior overall survival.
Subsequent studies, including one recently published in Blood, have shown that patients whose plasma cells are SKY92-positive have, on average, 4-times shorter survival and relapse more quickly after treatment than patients whose cells are SKY92-negative.
The intention of the MMprofiler is to classify MM patients according to the SKY92 gene signature and help healthcare professionals select appropriate treatment on the basis of existing guidelines. Healthcare professionals may also decide to monitor patients differently according to their risk group.
The MMprofiler is a product of SkylineDx. The test is run on the company’s proprietary Profiler™ platform, which makes centralized data analysis possible for labs that have the necessary equipment.
To run the MMprofiler test, labs must install a software module on their Affymetrix DX2 Gene scanning equipment and establish a secured gateway connection with the Profiler platform. Then, the lab can process a patient sample and generate the raw genetic data.
The patient’s bone marrow sample is purified, processed, applied to a biochip, and analyzed in the scanner. This is how the MMprofiler determines the active properties of the various genes in the plasma cells of each patient.
The data is then processed via the software system, which reveals the genetic subtype of the plasma cells. Knowing the SKY92 genetic subtype can help healthcare professionals distinguish between high-risk and standard-risk patients.
For more information on the test, visit www.mmprofiler.com. ![]()

Photo courtesy of SkylineDx
The MMprofiler™, a test used to risk-stratify patients with multiple myeloma (MM), has received the CE-IVD mark.
The CE-IVD mark indicates that an in vitro device complies with the European In Vitro Diagnostics Directive and may be legally commercialized and distributed in the European Union.
The MMprofiler classifies patients into high- or standard-risk groups based on the activity of 92 genes considered to be related to MM.
In a 2012 Leukemia paper, researchers described a gene-expression signature, now known as SKY92, that maps the activity of the 92 genes. MM patients who were defined as high-risk by the SKY92 gene signature (called “the EMC92 gene signature” in the paper) had inferior overall survival.
Subsequent studies, including one recently published in Blood, have shown that patients whose plasma cells are SKY92-positive have, on average, 4-times shorter survival and relapse more quickly after treatment than patients whose cells are SKY92-negative.
The intention of the MMprofiler is to classify MM patients according to the SKY92 gene signature and help healthcare professionals select appropriate treatment on the basis of existing guidelines. Healthcare professionals may also decide to monitor patients differently according to their risk group.
The MMprofiler is a product of SkylineDx. The test is run on the company’s proprietary Profiler™ platform, which makes centralized data analysis possible for labs that have the necessary equipment.
To run the MMprofiler test, labs must install a software module on their Affymetrix DX2 Gene scanning equipment and establish a secured gateway connection with the Profiler platform. Then, the lab can process a patient sample and generate the raw genetic data.
The patient’s bone marrow sample is purified, processed, applied to a biochip, and analyzed in the scanner. This is how the MMprofiler determines the active properties of the various genes in the plasma cells of each patient.
The data is then processed via the software system, which reveals the genetic subtype of the plasma cells. Knowing the SKY92 genetic subtype can help healthcare professionals distinguish between high-risk and standard-risk patients.
For more information on the test, visit www.mmprofiler.com. ![]()

Photo courtesy of SkylineDx
The MMprofiler™, a test used to risk-stratify patients with multiple myeloma (MM), has received the CE-IVD mark.
The CE-IVD mark indicates that an in vitro device complies with the European In Vitro Diagnostics Directive and may be legally commercialized and distributed in the European Union.
The MMprofiler classifies patients into high- or standard-risk groups based on the activity of 92 genes considered to be related to MM.
In a 2012 Leukemia paper, researchers described a gene-expression signature, now known as SKY92, that maps the activity of the 92 genes. MM patients who were defined as high-risk by the SKY92 gene signature (called “the EMC92 gene signature” in the paper) had inferior overall survival.
Subsequent studies, including one recently published in Blood, have shown that patients whose plasma cells are SKY92-positive have, on average, 4-times shorter survival and relapse more quickly after treatment than patients whose cells are SKY92-negative.
The intention of the MMprofiler is to classify MM patients according to the SKY92 gene signature and help healthcare professionals select appropriate treatment on the basis of existing guidelines. Healthcare professionals may also decide to monitor patients differently according to their risk group.
The MMprofiler is a product of SkylineDx. The test is run on the company’s proprietary Profiler™ platform, which makes centralized data analysis possible for labs that have the necessary equipment.
To run the MMprofiler test, labs must install a software module on their Affymetrix DX2 Gene scanning equipment and establish a secured gateway connection with the Profiler platform. Then, the lab can process a patient sample and generate the raw genetic data.
The patient’s bone marrow sample is purified, processed, applied to a biochip, and analyzed in the scanner. This is how the MMprofiler determines the active properties of the various genes in the plasma cells of each patient.
The data is then processed via the software system, which reveals the genetic subtype of the plasma cells. Knowing the SKY92 genetic subtype can help healthcare professionals distinguish between high-risk and standard-risk patients.
For more information on the test, visit www.mmprofiler.com. ![]()
Template can help guide care for cancer survivors

for radiation therapy
Photo by Rhoda Baer
A new template can help standardize plans for long-term care of cancer survivors who have undergone radiation therapy (RT), according to the American Society for Radiation Oncology (ASTRO).
An ASTRO advisory committee created the template to coordinate post-treatment care for cancer survivors among primary care providers (PCPs) and oncology
specialists (radiation, medical, and surgical), as well as patients themselves.
Details on the template appear in Practical Radiation Oncology.
“Factors such as earlier detection of cancer, increasingly effective treatment options, and an aging population lead to a growing number of cancer survivors and, ultimately, a need to educate and empower these individuals for their ongoing care,” said ASTRO chair Bruce D. Minsky, MD.
“The ASTRO template is designed to foster better coordination of post-treatment care for cancer survivors, including greater clarity in the dialogue between radiation oncologists and PCPs for issues such as less common side effects that may appear well after treatment is complete.”
Many radiation oncologists may already provide their patients with post-treatment materials such as diagnosis and treatment summaries, contacts for ancillary services such as financial or nutritional counselling, and information on potential late treatment effects.
But the ASTRO template coordinates these components in a central, plain-language document.
It also enables practices to meet new accreditation requirements set by the American College of Surgeons Commission on Cancer (CoC).
In response to a 2006 recommendation from the Institutes of Medicine that cancer patients be provided with a survivorship care plan (SCP) following treatment, CoC issued a mandate that cancer programs provide SCPs for all curative cancer patients by 2019 to maintain accreditation.
ASTRO’s template includes both elements required by the CoC in SCPs—namely, a summary of past treatment and directions for future care.
The treatment summary outlines the survivor’s diagnosis and stage information; treatment details such as the site, dosage, and schedule of RT; and contact information for providers who delivered the treatment.
The plan for follow-up care covers anticipated toxicities from RT, expected course of recovery from treatment-related toxicities, possible functional and/or social limitations, recommendations for preventative measures and behaviors, cancer information resources, and referrals to supportive care providers.
“This 2-page template facilitates consistency in SCPs across the discipline and also reduces the time and effort required by providers to complete each individual plan,” said Ronald Chen, MD, of the University of North Carolina at Chapel Hill.
“The field of radiation oncology has a long tradition of creating treatment summaries for each patient, even before the Institute of Medicine recommended survivorship care plans in 2006. This radiation-oncology-specific template will serve a dual purpose as both a traditional radiation oncology treatment summary and a plan for survivorship care that meets CoC requirements, thus reducing the burden on radiation oncologists from having to create 2 documents for each patient.” ![]()

for radiation therapy
Photo by Rhoda Baer
A new template can help standardize plans for long-term care of cancer survivors who have undergone radiation therapy (RT), according to the American Society for Radiation Oncology (ASTRO).
An ASTRO advisory committee created the template to coordinate post-treatment care for cancer survivors among primary care providers (PCPs) and oncology
specialists (radiation, medical, and surgical), as well as patients themselves.
Details on the template appear in Practical Radiation Oncology.
“Factors such as earlier detection of cancer, increasingly effective treatment options, and an aging population lead to a growing number of cancer survivors and, ultimately, a need to educate and empower these individuals for their ongoing care,” said ASTRO chair Bruce D. Minsky, MD.
“The ASTRO template is designed to foster better coordination of post-treatment care for cancer survivors, including greater clarity in the dialogue between radiation oncologists and PCPs for issues such as less common side effects that may appear well after treatment is complete.”
Many radiation oncologists may already provide their patients with post-treatment materials such as diagnosis and treatment summaries, contacts for ancillary services such as financial or nutritional counselling, and information on potential late treatment effects.
But the ASTRO template coordinates these components in a central, plain-language document.
It also enables practices to meet new accreditation requirements set by the American College of Surgeons Commission on Cancer (CoC).
In response to a 2006 recommendation from the Institutes of Medicine that cancer patients be provided with a survivorship care plan (SCP) following treatment, CoC issued a mandate that cancer programs provide SCPs for all curative cancer patients by 2019 to maintain accreditation.
ASTRO’s template includes both elements required by the CoC in SCPs—namely, a summary of past treatment and directions for future care.
The treatment summary outlines the survivor’s diagnosis and stage information; treatment details such as the site, dosage, and schedule of RT; and contact information for providers who delivered the treatment.
The plan for follow-up care covers anticipated toxicities from RT, expected course of recovery from treatment-related toxicities, possible functional and/or social limitations, recommendations for preventative measures and behaviors, cancer information resources, and referrals to supportive care providers.
“This 2-page template facilitates consistency in SCPs across the discipline and also reduces the time and effort required by providers to complete each individual plan,” said Ronald Chen, MD, of the University of North Carolina at Chapel Hill.
“The field of radiation oncology has a long tradition of creating treatment summaries for each patient, even before the Institute of Medicine recommended survivorship care plans in 2006. This radiation-oncology-specific template will serve a dual purpose as both a traditional radiation oncology treatment summary and a plan for survivorship care that meets CoC requirements, thus reducing the burden on radiation oncologists from having to create 2 documents for each patient.” ![]()

for radiation therapy
Photo by Rhoda Baer
A new template can help standardize plans for long-term care of cancer survivors who have undergone radiation therapy (RT), according to the American Society for Radiation Oncology (ASTRO).
An ASTRO advisory committee created the template to coordinate post-treatment care for cancer survivors among primary care providers (PCPs) and oncology
specialists (radiation, medical, and surgical), as well as patients themselves.
Details on the template appear in Practical Radiation Oncology.
“Factors such as earlier detection of cancer, increasingly effective treatment options, and an aging population lead to a growing number of cancer survivors and, ultimately, a need to educate and empower these individuals for their ongoing care,” said ASTRO chair Bruce D. Minsky, MD.
“The ASTRO template is designed to foster better coordination of post-treatment care for cancer survivors, including greater clarity in the dialogue between radiation oncologists and PCPs for issues such as less common side effects that may appear well after treatment is complete.”
Many radiation oncologists may already provide their patients with post-treatment materials such as diagnosis and treatment summaries, contacts for ancillary services such as financial or nutritional counselling, and information on potential late treatment effects.
But the ASTRO template coordinates these components in a central, plain-language document.
It also enables practices to meet new accreditation requirements set by the American College of Surgeons Commission on Cancer (CoC).
In response to a 2006 recommendation from the Institutes of Medicine that cancer patients be provided with a survivorship care plan (SCP) following treatment, CoC issued a mandate that cancer programs provide SCPs for all curative cancer patients by 2019 to maintain accreditation.
ASTRO’s template includes both elements required by the CoC in SCPs—namely, a summary of past treatment and directions for future care.
The treatment summary outlines the survivor’s diagnosis and stage information; treatment details such as the site, dosage, and schedule of RT; and contact information for providers who delivered the treatment.
The plan for follow-up care covers anticipated toxicities from RT, expected course of recovery from treatment-related toxicities, possible functional and/or social limitations, recommendations for preventative measures and behaviors, cancer information resources, and referrals to supportive care providers.
“This 2-page template facilitates consistency in SCPs across the discipline and also reduces the time and effort required by providers to complete each individual plan,” said Ronald Chen, MD, of the University of North Carolina at Chapel Hill.
“The field of radiation oncology has a long tradition of creating treatment summaries for each patient, even before the Institute of Medicine recommended survivorship care plans in 2006. This radiation-oncology-specific template will serve a dual purpose as both a traditional radiation oncology treatment summary and a plan for survivorship care that meets CoC requirements, thus reducing the burden on radiation oncologists from having to create 2 documents for each patient.” ![]()
FDA approves ixazomib for MM

The US Food and Drug Administration (FDA) has approved ixazomib (Ninlaro), the first oral proteasome inhibitor, for use in combination with lenalidomide and dexamethasone to treat multiple myeloma (MM) patients who have received at least 1 prior therapy.
The FDA previously granted ixazomib priority review and orphan designation.
The regulatory submission for ixazomib was primarily based on results from the first interim analysis of the phase 3 TOURMALINE-MM1 trial.
In this trial, patients with relapsed and/or refractory MM who received ixazomib plus lenalidomide and dexamethasone had superior progression-free survival when compared to patients who received placebo plus lenalidomide and dexamethasone.
Results from TOURMALINE-MM1 are scheduled to be presented at the 2015 ASH Annual Meeting (abstract 727) in December.
Ixazomib is currently under investigation in 3 other phase 3 trials of MM patients:
- TOURMALINE-MM2, investigating ixazomib vs placebo, both in combination with lenalidomide and dexamethasone in patients with newly diagnosed MM
- TOURMALINE-MM3, investigating ixazomib vs placebo as maintenance therapy in patients with newly diagnosed MM following induction therapy and autologous stem cell transplant
- TOURMALINE-MM4, investigating ixazomib vs placebo as maintenance therapy in patients with newly diagnosed MM who have not undergone autologous stem cell transplant.
Ixazomib is marketed by Takeda Pharmaceuticals. ![]()

The US Food and Drug Administration (FDA) has approved ixazomib (Ninlaro), the first oral proteasome inhibitor, for use in combination with lenalidomide and dexamethasone to treat multiple myeloma (MM) patients who have received at least 1 prior therapy.
The FDA previously granted ixazomib priority review and orphan designation.
The regulatory submission for ixazomib was primarily based on results from the first interim analysis of the phase 3 TOURMALINE-MM1 trial.
In this trial, patients with relapsed and/or refractory MM who received ixazomib plus lenalidomide and dexamethasone had superior progression-free survival when compared to patients who received placebo plus lenalidomide and dexamethasone.
Results from TOURMALINE-MM1 are scheduled to be presented at the 2015 ASH Annual Meeting (abstract 727) in December.
Ixazomib is currently under investigation in 3 other phase 3 trials of MM patients:
- TOURMALINE-MM2, investigating ixazomib vs placebo, both in combination with lenalidomide and dexamethasone in patients with newly diagnosed MM
- TOURMALINE-MM3, investigating ixazomib vs placebo as maintenance therapy in patients with newly diagnosed MM following induction therapy and autologous stem cell transplant
- TOURMALINE-MM4, investigating ixazomib vs placebo as maintenance therapy in patients with newly diagnosed MM who have not undergone autologous stem cell transplant.
Ixazomib is marketed by Takeda Pharmaceuticals. ![]()

The US Food and Drug Administration (FDA) has approved ixazomib (Ninlaro), the first oral proteasome inhibitor, for use in combination with lenalidomide and dexamethasone to treat multiple myeloma (MM) patients who have received at least 1 prior therapy.
The FDA previously granted ixazomib priority review and orphan designation.
The regulatory submission for ixazomib was primarily based on results from the first interim analysis of the phase 3 TOURMALINE-MM1 trial.
In this trial, patients with relapsed and/or refractory MM who received ixazomib plus lenalidomide and dexamethasone had superior progression-free survival when compared to patients who received placebo plus lenalidomide and dexamethasone.
Results from TOURMALINE-MM1 are scheduled to be presented at the 2015 ASH Annual Meeting (abstract 727) in December.
Ixazomib is currently under investigation in 3 other phase 3 trials of MM patients:
- TOURMALINE-MM2, investigating ixazomib vs placebo, both in combination with lenalidomide and dexamethasone in patients with newly diagnosed MM
- TOURMALINE-MM3, investigating ixazomib vs placebo as maintenance therapy in patients with newly diagnosed MM following induction therapy and autologous stem cell transplant
- TOURMALINE-MM4, investigating ixazomib vs placebo as maintenance therapy in patients with newly diagnosed MM who have not undergone autologous stem cell transplant.
Ixazomib is marketed by Takeda Pharmaceuticals. ![]()
EC approves carfilzomib for relapsed MM

Photo courtesy of Amgen
The European Commission (EC) has granted marketing authorization for carfilzomib (Kyprolis) to be used in combination with lenalidomide and dexamethasone to treat adults with multiple myeloma (MM) who have received at least 1 prior therapy.
Carfilzomib is the first irreversible proteasome inhibitor approved in the European Union (EU) as part of combination treatment for patients with relapsed MM.
Carfilzomib was granted orphan designation in the EU in 2008. The drug also received accelerated assessment, which shortened the review period from 210 days to 150 days.
Carfilzomib is a product of Onyx Pharmaceuticals, Inc., a subsidiary of Amgen that holds development and commercialization rights to the drug globally, excluding Japan.
ASPIRE trial
The EC approved carfilzomib based on data from the phase 3 ASPIRE trial, which were presented at ASH 2014 and published in NEJM.
The trial enrolled 792 patients with relapsed or refractory MM who had received 1 to 3 prior lines of therapy. The patients were randomized (1:1) to receive carfilzomib plus lenalidomide and dexamethasone (KRd) or just lenalidomide and dexamethasone (Rd) for 18 cycles.
Lenalidomide and dexamethasone were continued thereafter until disease progression. There was no planned cross-over from the control arm to treatment with carfilzomib.
The study’s primary endpoint was progression-free survival. The median progression-free survival was significantly longer in the KRd arm than the Rd arm—26.3 months and 17.6 months, respectively (hazard ratio=0.69, P=0.0001).
At the time of analysis, the difference in overall survival did not reach the prespecified boundary for statistical significance.
The overall response rate was 87% in the KRd arm and 67% in the Rd arm. The median duration of response was 28.6 months and 21.2 months, respectively.
The rates of death due to adverse events (AEs) within 30 days of the last dose were similar between the treatment arms.
The most common causes of death not due to progressive disease occurring in patients in the KRd arm and the Rd arm, respectively, were cardiac disorders (3% vs 2%), infection (2% vs 3%), renal events (0% vs less than 1%), and other AEs (2% vs 3%).
Serious AEs were reported in 60% of patients in the KRd arm and 54% in the Rd arm. The most common serious AEs reported in the KRd arm and the Rd arm, respectively, were pneumonia (14% vs 11%), respiratory tract infection (4% vs 2%), pyrexia (4% vs 2%), and pulmonary embolism (3% vs 2%).
Global development
In the US, carfilzomib is approved for use in combination with lenalidomide and dexamethasone to treat MM patients who have received 1 to 3 prior lines of therapy.
Carfilzomib also has accelerated approval in the US as a single agent to treat MM patients who have received at least 2 prior therapies, including bortezomib and an immunomodulatory agent, and have demonstrated disease progression on or within 60 days of the completion of last therapy.
Amgen plans to submit data from the phase 3 ENDEAVOR trial for potential authorization of carfilzomib in combination with dexamethasone in the EU.
This data serves as the basis of the supplemental new drug application of carfilzomib in combination with dexamethasone for patients with relapsed MM, which has been accepted for priority review in the US.
In addition to the US and EU, carfilzomib is approved for use in Argentina, Israel, Kuwait, Mexico, Thailand, and Colombia. Additional regulatory applications for the drug have been submitted to health authorities worldwide. ![]()

Photo courtesy of Amgen
The European Commission (EC) has granted marketing authorization for carfilzomib (Kyprolis) to be used in combination with lenalidomide and dexamethasone to treat adults with multiple myeloma (MM) who have received at least 1 prior therapy.
Carfilzomib is the first irreversible proteasome inhibitor approved in the European Union (EU) as part of combination treatment for patients with relapsed MM.
Carfilzomib was granted orphan designation in the EU in 2008. The drug also received accelerated assessment, which shortened the review period from 210 days to 150 days.
Carfilzomib is a product of Onyx Pharmaceuticals, Inc., a subsidiary of Amgen that holds development and commercialization rights to the drug globally, excluding Japan.
ASPIRE trial
The EC approved carfilzomib based on data from the phase 3 ASPIRE trial, which were presented at ASH 2014 and published in NEJM.
The trial enrolled 792 patients with relapsed or refractory MM who had received 1 to 3 prior lines of therapy. The patients were randomized (1:1) to receive carfilzomib plus lenalidomide and dexamethasone (KRd) or just lenalidomide and dexamethasone (Rd) for 18 cycles.
Lenalidomide and dexamethasone were continued thereafter until disease progression. There was no planned cross-over from the control arm to treatment with carfilzomib.
The study’s primary endpoint was progression-free survival. The median progression-free survival was significantly longer in the KRd arm than the Rd arm—26.3 months and 17.6 months, respectively (hazard ratio=0.69, P=0.0001).
At the time of analysis, the difference in overall survival did not reach the prespecified boundary for statistical significance.
The overall response rate was 87% in the KRd arm and 67% in the Rd arm. The median duration of response was 28.6 months and 21.2 months, respectively.
The rates of death due to adverse events (AEs) within 30 days of the last dose were similar between the treatment arms.
The most common causes of death not due to progressive disease occurring in patients in the KRd arm and the Rd arm, respectively, were cardiac disorders (3% vs 2%), infection (2% vs 3%), renal events (0% vs less than 1%), and other AEs (2% vs 3%).
Serious AEs were reported in 60% of patients in the KRd arm and 54% in the Rd arm. The most common serious AEs reported in the KRd arm and the Rd arm, respectively, were pneumonia (14% vs 11%), respiratory tract infection (4% vs 2%), pyrexia (4% vs 2%), and pulmonary embolism (3% vs 2%).
Global development
In the US, carfilzomib is approved for use in combination with lenalidomide and dexamethasone to treat MM patients who have received 1 to 3 prior lines of therapy.
Carfilzomib also has accelerated approval in the US as a single agent to treat MM patients who have received at least 2 prior therapies, including bortezomib and an immunomodulatory agent, and have demonstrated disease progression on or within 60 days of the completion of last therapy.
Amgen plans to submit data from the phase 3 ENDEAVOR trial for potential authorization of carfilzomib in combination with dexamethasone in the EU.
This data serves as the basis of the supplemental new drug application of carfilzomib in combination with dexamethasone for patients with relapsed MM, which has been accepted for priority review in the US.
In addition to the US and EU, carfilzomib is approved for use in Argentina, Israel, Kuwait, Mexico, Thailand, and Colombia. Additional regulatory applications for the drug have been submitted to health authorities worldwide. ![]()

Photo courtesy of Amgen
The European Commission (EC) has granted marketing authorization for carfilzomib (Kyprolis) to be used in combination with lenalidomide and dexamethasone to treat adults with multiple myeloma (MM) who have received at least 1 prior therapy.
Carfilzomib is the first irreversible proteasome inhibitor approved in the European Union (EU) as part of combination treatment for patients with relapsed MM.
Carfilzomib was granted orphan designation in the EU in 2008. The drug also received accelerated assessment, which shortened the review period from 210 days to 150 days.
Carfilzomib is a product of Onyx Pharmaceuticals, Inc., a subsidiary of Amgen that holds development and commercialization rights to the drug globally, excluding Japan.
ASPIRE trial
The EC approved carfilzomib based on data from the phase 3 ASPIRE trial, which were presented at ASH 2014 and published in NEJM.
The trial enrolled 792 patients with relapsed or refractory MM who had received 1 to 3 prior lines of therapy. The patients were randomized (1:1) to receive carfilzomib plus lenalidomide and dexamethasone (KRd) or just lenalidomide and dexamethasone (Rd) for 18 cycles.
Lenalidomide and dexamethasone were continued thereafter until disease progression. There was no planned cross-over from the control arm to treatment with carfilzomib.
The study’s primary endpoint was progression-free survival. The median progression-free survival was significantly longer in the KRd arm than the Rd arm—26.3 months and 17.6 months, respectively (hazard ratio=0.69, P=0.0001).
At the time of analysis, the difference in overall survival did not reach the prespecified boundary for statistical significance.
The overall response rate was 87% in the KRd arm and 67% in the Rd arm. The median duration of response was 28.6 months and 21.2 months, respectively.
The rates of death due to adverse events (AEs) within 30 days of the last dose were similar between the treatment arms.
The most common causes of death not due to progressive disease occurring in patients in the KRd arm and the Rd arm, respectively, were cardiac disorders (3% vs 2%), infection (2% vs 3%), renal events (0% vs less than 1%), and other AEs (2% vs 3%).
Serious AEs were reported in 60% of patients in the KRd arm and 54% in the Rd arm. The most common serious AEs reported in the KRd arm and the Rd arm, respectively, were pneumonia (14% vs 11%), respiratory tract infection (4% vs 2%), pyrexia (4% vs 2%), and pulmonary embolism (3% vs 2%).
Global development
In the US, carfilzomib is approved for use in combination with lenalidomide and dexamethasone to treat MM patients who have received 1 to 3 prior lines of therapy.
Carfilzomib also has accelerated approval in the US as a single agent to treat MM patients who have received at least 2 prior therapies, including bortezomib and an immunomodulatory agent, and have demonstrated disease progression on or within 60 days of the completion of last therapy.
Amgen plans to submit data from the phase 3 ENDEAVOR trial for potential authorization of carfilzomib in combination with dexamethasone in the EU.
This data serves as the basis of the supplemental new drug application of carfilzomib in combination with dexamethasone for patients with relapsed MM, which has been accepted for priority review in the US.
In addition to the US and EU, carfilzomib is approved for use in Argentina, Israel, Kuwait, Mexico, Thailand, and Colombia. Additional regulatory applications for the drug have been submitted to health authorities worldwide. ![]()
Ixazomib approved for multiple myeloma combo treatment
Ixazomib has been approved by the Food and Drug Administration to be used in a combination treatment for patients with multiple myeloma who have received at least one other treatment for their disease, the agency announced on Nov. 20.
Approval was based on a randomized, double-blind clinical trial of 722 patients with multiple myeloma who had received at least one prior treatment. Compared with patients receiving lenalidomide, dexamethasone, and placebo, those receiving lenalidomide, dexamethasone, and ixazomib had a statistically significant improvement in progression-free survival (PFS). The median PFS for the ixazomib arm was 20.6 months, compared with 14.7 months for the placebo, lenalidomide, and dexamethasone arm.
Common adverse reactions occurring more often in ixazomib-treated patients included diarrhea, constipation, thrombocytopenia, peripheral neuropathy, nausea, peripheral edema, vomiting, and back pain.
Secondary outcome measures are still being evaluated for ixazomib in this ongoing trial. Efficacy measures include overall survival, overall response rate, duration of response and time to progression. Secondary safety and quality of life–related measures include tracking adverse events, lab value abnormalities, as well as performance status and global health status.
Ixazomib, marketed as Ninlaro by Takeda Pharmaceuticals, is the first FDA-approved oral proteasome inhibitor. Proteasome inhibitors as a class take advantage of tumor cells’ reliance on proteasomal clearance of unwanted proteins; ixazomib and other proteasome inhibitors have an antiproliferative effect and promote tumor cell apoptosis. The drug was approved early under the FDA’s priority review program.
“The field of cancer treatment, and multiple myeloma in particular, has never seen a watershed moment like this,” Walter M. Capone, president and CEO of the Multiple Myeloma Research Foundation, said in a statement. He noted that on Nov. 16, the FDA approved daratumumab, the first monoclonal antibody approved to treat multiple myeloma.
Clinical trials are currently underway to investigate the use of ixazomib in patients with residual multiple myeloma, as maintenance therapy following autologous and stem cell transplant procedures for multiple myeloma, and in other cancer types.
On Twitter @karioakes
Ixazomib has been approved by the Food and Drug Administration to be used in a combination treatment for patients with multiple myeloma who have received at least one other treatment for their disease, the agency announced on Nov. 20.
Approval was based on a randomized, double-blind clinical trial of 722 patients with multiple myeloma who had received at least one prior treatment. Compared with patients receiving lenalidomide, dexamethasone, and placebo, those receiving lenalidomide, dexamethasone, and ixazomib had a statistically significant improvement in progression-free survival (PFS). The median PFS for the ixazomib arm was 20.6 months, compared with 14.7 months for the placebo, lenalidomide, and dexamethasone arm.
Common adverse reactions occurring more often in ixazomib-treated patients included diarrhea, constipation, thrombocytopenia, peripheral neuropathy, nausea, peripheral edema, vomiting, and back pain.
Secondary outcome measures are still being evaluated for ixazomib in this ongoing trial. Efficacy measures include overall survival, overall response rate, duration of response and time to progression. Secondary safety and quality of life–related measures include tracking adverse events, lab value abnormalities, as well as performance status and global health status.
Ixazomib, marketed as Ninlaro by Takeda Pharmaceuticals, is the first FDA-approved oral proteasome inhibitor. Proteasome inhibitors as a class take advantage of tumor cells’ reliance on proteasomal clearance of unwanted proteins; ixazomib and other proteasome inhibitors have an antiproliferative effect and promote tumor cell apoptosis. The drug was approved early under the FDA’s priority review program.
“The field of cancer treatment, and multiple myeloma in particular, has never seen a watershed moment like this,” Walter M. Capone, president and CEO of the Multiple Myeloma Research Foundation, said in a statement. He noted that on Nov. 16, the FDA approved daratumumab, the first monoclonal antibody approved to treat multiple myeloma.
Clinical trials are currently underway to investigate the use of ixazomib in patients with residual multiple myeloma, as maintenance therapy following autologous and stem cell transplant procedures for multiple myeloma, and in other cancer types.
On Twitter @karioakes
Ixazomib has been approved by the Food and Drug Administration to be used in a combination treatment for patients with multiple myeloma who have received at least one other treatment for their disease, the agency announced on Nov. 20.
Approval was based on a randomized, double-blind clinical trial of 722 patients with multiple myeloma who had received at least one prior treatment. Compared with patients receiving lenalidomide, dexamethasone, and placebo, those receiving lenalidomide, dexamethasone, and ixazomib had a statistically significant improvement in progression-free survival (PFS). The median PFS for the ixazomib arm was 20.6 months, compared with 14.7 months for the placebo, lenalidomide, and dexamethasone arm.
Common adverse reactions occurring more often in ixazomib-treated patients included diarrhea, constipation, thrombocytopenia, peripheral neuropathy, nausea, peripheral edema, vomiting, and back pain.
Secondary outcome measures are still being evaluated for ixazomib in this ongoing trial. Efficacy measures include overall survival, overall response rate, duration of response and time to progression. Secondary safety and quality of life–related measures include tracking adverse events, lab value abnormalities, as well as performance status and global health status.
Ixazomib, marketed as Ninlaro by Takeda Pharmaceuticals, is the first FDA-approved oral proteasome inhibitor. Proteasome inhibitors as a class take advantage of tumor cells’ reliance on proteasomal clearance of unwanted proteins; ixazomib and other proteasome inhibitors have an antiproliferative effect and promote tumor cell apoptosis. The drug was approved early under the FDA’s priority review program.
“The field of cancer treatment, and multiple myeloma in particular, has never seen a watershed moment like this,” Walter M. Capone, president and CEO of the Multiple Myeloma Research Foundation, said in a statement. He noted that on Nov. 16, the FDA approved daratumumab, the first monoclonal antibody approved to treat multiple myeloma.
Clinical trials are currently underway to investigate the use of ixazomib in patients with residual multiple myeloma, as maintenance therapy following autologous and stem cell transplant procedures for multiple myeloma, and in other cancer types.
On Twitter @karioakes
Model enables screening of MM drugs

showing multiple myeloma
Researchers have created a 3-dimensional model that can be used to screen drugs designed to treat multiple myeloma (MM).
The team developed 3D tissue-engineered bone marrow (3DTEBM) cultures that could, ideally, help physicians determine which drug or combination therapy might be most effective for a particular MM patient.
The cultures also provide guidance regarding dosage.
The researchers described this work in Biomaterials.
“Even before the patient completes all of the MRIs, CT scans, and other imaging procedures following diagnosis, we can have a recommendation for which drug and dosage to prescribe,” said study author Kareem Azab, PhD, of Washington University School of Medicine in St Louis, Missouri. “The test results come in 3 to 4 days.”
Dr Azab and his colleagues developed their 3DTEBM cultures using bone marrow samples from MM patients. The team took small samples of a patient’s cells and remodeled them in the lab.
This tumor microenvironment includes the cancer cells and neighboring blood vessels, immune cells, and other components whose interaction can help or inhibit the tumor cells’ growth. Drugs are tested on the remodeled patient cells to determine which treatment is likely to be most effective.
Dr Azab’s method gauges the sensitivity of a patient’s cells to different drugs at any time in the course of the disease.
Therefore, as a patient’s disease becomes more resistant to particular drugs, continued drug screening could suggest when to change therapies. This could save valuable time, Dr Azab said.
“Now, we have a drug test that closely replicates what’s going on with a patient at any given moment,” he noted. “We think this method has a better chance of working than existing options.”
The 3DTEBM cultures are currently being tested in a clinical trial of MM patients.
To further the technology, Dr Azab and his colleagues have launched a company, Cellatrix, in coordination with Washington University’s Office of Technology Management and BioGenerator, a nonprofit organization that helps launch bioscience companies.
Cellatrix is scheduled to begin testing potential therapies on behalf of pharmaceutical companies soon. Dr Azab’s team is also studying how well the screening method works for patients with leukemia or lymphoma. ![]()

showing multiple myeloma
Researchers have created a 3-dimensional model that can be used to screen drugs designed to treat multiple myeloma (MM).
The team developed 3D tissue-engineered bone marrow (3DTEBM) cultures that could, ideally, help physicians determine which drug or combination therapy might be most effective for a particular MM patient.
The cultures also provide guidance regarding dosage.
The researchers described this work in Biomaterials.
“Even before the patient completes all of the MRIs, CT scans, and other imaging procedures following diagnosis, we can have a recommendation for which drug and dosage to prescribe,” said study author Kareem Azab, PhD, of Washington University School of Medicine in St Louis, Missouri. “The test results come in 3 to 4 days.”
Dr Azab and his colleagues developed their 3DTEBM cultures using bone marrow samples from MM patients. The team took small samples of a patient’s cells and remodeled them in the lab.
This tumor microenvironment includes the cancer cells and neighboring blood vessels, immune cells, and other components whose interaction can help or inhibit the tumor cells’ growth. Drugs are tested on the remodeled patient cells to determine which treatment is likely to be most effective.
Dr Azab’s method gauges the sensitivity of a patient’s cells to different drugs at any time in the course of the disease.
Therefore, as a patient’s disease becomes more resistant to particular drugs, continued drug screening could suggest when to change therapies. This could save valuable time, Dr Azab said.
“Now, we have a drug test that closely replicates what’s going on with a patient at any given moment,” he noted. “We think this method has a better chance of working than existing options.”
The 3DTEBM cultures are currently being tested in a clinical trial of MM patients.
To further the technology, Dr Azab and his colleagues have launched a company, Cellatrix, in coordination with Washington University’s Office of Technology Management and BioGenerator, a nonprofit organization that helps launch bioscience companies.
Cellatrix is scheduled to begin testing potential therapies on behalf of pharmaceutical companies soon. Dr Azab’s team is also studying how well the screening method works for patients with leukemia or lymphoma. ![]()

showing multiple myeloma
Researchers have created a 3-dimensional model that can be used to screen drugs designed to treat multiple myeloma (MM).
The team developed 3D tissue-engineered bone marrow (3DTEBM) cultures that could, ideally, help physicians determine which drug or combination therapy might be most effective for a particular MM patient.
The cultures also provide guidance regarding dosage.
The researchers described this work in Biomaterials.
“Even before the patient completes all of the MRIs, CT scans, and other imaging procedures following diagnosis, we can have a recommendation for which drug and dosage to prescribe,” said study author Kareem Azab, PhD, of Washington University School of Medicine in St Louis, Missouri. “The test results come in 3 to 4 days.”
Dr Azab and his colleagues developed their 3DTEBM cultures using bone marrow samples from MM patients. The team took small samples of a patient’s cells and remodeled them in the lab.
This tumor microenvironment includes the cancer cells and neighboring blood vessels, immune cells, and other components whose interaction can help or inhibit the tumor cells’ growth. Drugs are tested on the remodeled patient cells to determine which treatment is likely to be most effective.
Dr Azab’s method gauges the sensitivity of a patient’s cells to different drugs at any time in the course of the disease.
Therefore, as a patient’s disease becomes more resistant to particular drugs, continued drug screening could suggest when to change therapies. This could save valuable time, Dr Azab said.
“Now, we have a drug test that closely replicates what’s going on with a patient at any given moment,” he noted. “We think this method has a better chance of working than existing options.”
The 3DTEBM cultures are currently being tested in a clinical trial of MM patients.
To further the technology, Dr Azab and his colleagues have launched a company, Cellatrix, in coordination with Washington University’s Office of Technology Management and BioGenerator, a nonprofit organization that helps launch bioscience companies.
Cellatrix is scheduled to begin testing potential therapies on behalf of pharmaceutical companies soon. Dr Azab’s team is also studying how well the screening method works for patients with leukemia or lymphoma. ![]()
Team characterizes EMH niche
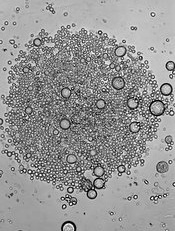
Image by John Perry
Previous studies have shown that hematopoietic stresses—such as myelofibrosis, anemia, and myeloablation—can induce extramedullary hematopoiesis (EMH), in which hematopoietic stem cells (HSCs) are mobilized to sites outside the bone marrow.
The splenic red pulp is known to be a prominent site of EMH in both mice and humans, but not much is known about the EMH niche.
Now, investigators say they have characterized this niche.
They detailed their findings in Nature.
The team used mouse models to examine the expression patterns of 2 known niche cell factors, SCF and CXCL12.
They discovered that the hematopoietic microenvironment in the spleen is found near sinusoidal blood vessels and is created by endothelial cells and perivascular stromal cells, just like the microenvironment in the bone marrow.
“Under emergency conditions, the endothelial cells and perivascular stromal cells that reside in the spleen are induced to proliferate so they can sustain all the new blood-forming stem cells that migrate into the spleen,” explained study author Sean Morrison, PhD, of the University of Texas Southwestern Medical Center, Dallas.
“We determined that this process in the spleen is physiologically important for responding to hematopoietic stress. Without it, the mice we studied could not maintain normal blood cell counts during pregnancy or quickly regenerate blood cell counts after bleeding or chemotherapy.”
The investigators believe these findings could aid the development of therapeutic interventions to enhance blood formation following chemotherapy or HSC transplant and thus accelerate the recovery of blood cell counts. ![]()
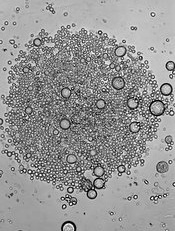
Image by John Perry
Previous studies have shown that hematopoietic stresses—such as myelofibrosis, anemia, and myeloablation—can induce extramedullary hematopoiesis (EMH), in which hematopoietic stem cells (HSCs) are mobilized to sites outside the bone marrow.
The splenic red pulp is known to be a prominent site of EMH in both mice and humans, but not much is known about the EMH niche.
Now, investigators say they have characterized this niche.
They detailed their findings in Nature.
The team used mouse models to examine the expression patterns of 2 known niche cell factors, SCF and CXCL12.
They discovered that the hematopoietic microenvironment in the spleen is found near sinusoidal blood vessels and is created by endothelial cells and perivascular stromal cells, just like the microenvironment in the bone marrow.
“Under emergency conditions, the endothelial cells and perivascular stromal cells that reside in the spleen are induced to proliferate so they can sustain all the new blood-forming stem cells that migrate into the spleen,” explained study author Sean Morrison, PhD, of the University of Texas Southwestern Medical Center, Dallas.
“We determined that this process in the spleen is physiologically important for responding to hematopoietic stress. Without it, the mice we studied could not maintain normal blood cell counts during pregnancy or quickly regenerate blood cell counts after bleeding or chemotherapy.”
The investigators believe these findings could aid the development of therapeutic interventions to enhance blood formation following chemotherapy or HSC transplant and thus accelerate the recovery of blood cell counts. ![]()
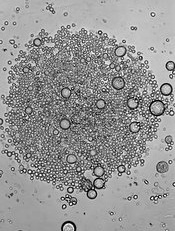
Image by John Perry
Previous studies have shown that hematopoietic stresses—such as myelofibrosis, anemia, and myeloablation—can induce extramedullary hematopoiesis (EMH), in which hematopoietic stem cells (HSCs) are mobilized to sites outside the bone marrow.
The splenic red pulp is known to be a prominent site of EMH in both mice and humans, but not much is known about the EMH niche.
Now, investigators say they have characterized this niche.
They detailed their findings in Nature.
The team used mouse models to examine the expression patterns of 2 known niche cell factors, SCF and CXCL12.
They discovered that the hematopoietic microenvironment in the spleen is found near sinusoidal blood vessels and is created by endothelial cells and perivascular stromal cells, just like the microenvironment in the bone marrow.
“Under emergency conditions, the endothelial cells and perivascular stromal cells that reside in the spleen are induced to proliferate so they can sustain all the new blood-forming stem cells that migrate into the spleen,” explained study author Sean Morrison, PhD, of the University of Texas Southwestern Medical Center, Dallas.
“We determined that this process in the spleen is physiologically important for responding to hematopoietic stress. Without it, the mice we studied could not maintain normal blood cell counts during pregnancy or quickly regenerate blood cell counts after bleeding or chemotherapy.”
The investigators believe these findings could aid the development of therapeutic interventions to enhance blood formation following chemotherapy or HSC transplant and thus accelerate the recovery of blood cell counts.
FDA approves daratumumab for multiple myeloma
The Food and Drug Administration has granted accelerated approval to daratumumab for the treatment of patients with multiple myeloma who have received at least three prior lines of therapy, the agency announced Nov. 16. Daratumumab is the first monoclonal antibody approved for the treatment of multiple myeloma.
Approval was based on an objective response rate of 29% (95% confidence interval, 21%-39%) with a median response duration of 7.4 months in 106 patients with relapsed or refractory multiple myeloma treated with daratumumab monotherapy in a multicenter, open-label study.
Safety was evaluated in 156 patients in two open-label studies. The most frequently reported adverse reactions were infusion reactions, fatigue, nausea, back pain, pyrexia, cough, and upper respiratory tract infection. The most common laboratory abnormalities were lymphopenia, neutropenia, anemia, and thrombocytopenia, the FDA said.
Daratumumab, marketed as Darzalex, interferes with blood bank cross-matching, specifically with Indirect Antiglobulin Tests, and the FDA recommends that, if a transfusion is necessary, to inform the blood bank that a patient has received daratumumab.
As a condition of accelerated approval, the FDA is requiring manufacturer Janssen Biotech to follow-up with a randomized trial establishing the superiority of daratumumab over standard therapy. The company has several ongoing multicenter, randomized trials in patients with multiple myeloma with a primary endpoint of progression-free survival.
The recommended dose and schedule for daratumumab is 16 mg/kg once every week for 8 weeks, then once every 2 weeks for 16 weeks, then once every 4 weeks until disease progression.
The Food and Drug Administration has granted accelerated approval to daratumumab for the treatment of patients with multiple myeloma who have received at least three prior lines of therapy, the agency announced Nov. 16. Daratumumab is the first monoclonal antibody approved for the treatment of multiple myeloma.
Approval was based on an objective response rate of 29% (95% confidence interval, 21%-39%) with a median response duration of 7.4 months in 106 patients with relapsed or refractory multiple myeloma treated with daratumumab monotherapy in a multicenter, open-label study.
Safety was evaluated in 156 patients in two open-label studies. The most frequently reported adverse reactions were infusion reactions, fatigue, nausea, back pain, pyrexia, cough, and upper respiratory tract infection. The most common laboratory abnormalities were lymphopenia, neutropenia, anemia, and thrombocytopenia, the FDA said.
Daratumumab, marketed as Darzalex, interferes with blood bank cross-matching, specifically with Indirect Antiglobulin Tests, and the FDA recommends that, if a transfusion is necessary, to inform the blood bank that a patient has received daratumumab.
As a condition of accelerated approval, the FDA is requiring manufacturer Janssen Biotech to follow-up with a randomized trial establishing the superiority of daratumumab over standard therapy. The company has several ongoing multicenter, randomized trials in patients with multiple myeloma with a primary endpoint of progression-free survival.
The recommended dose and schedule for daratumumab is 16 mg/kg once every week for 8 weeks, then once every 2 weeks for 16 weeks, then once every 4 weeks until disease progression.
The Food and Drug Administration has granted accelerated approval to daratumumab for the treatment of patients with multiple myeloma who have received at least three prior lines of therapy, the agency announced Nov. 16. Daratumumab is the first monoclonal antibody approved for the treatment of multiple myeloma.
Approval was based on an objective response rate of 29% (95% confidence interval, 21%-39%) with a median response duration of 7.4 months in 106 patients with relapsed or refractory multiple myeloma treated with daratumumab monotherapy in a multicenter, open-label study.
Safety was evaluated in 156 patients in two open-label studies. The most frequently reported adverse reactions were infusion reactions, fatigue, nausea, back pain, pyrexia, cough, and upper respiratory tract infection. The most common laboratory abnormalities were lymphopenia, neutropenia, anemia, and thrombocytopenia, the FDA said.
Daratumumab, marketed as Darzalex, interferes with blood bank cross-matching, specifically with Indirect Antiglobulin Tests, and the FDA recommends that, if a transfusion is necessary, to inform the blood bank that a patient has received daratumumab.
As a condition of accelerated approval, the FDA is requiring manufacturer Janssen Biotech to follow-up with a randomized trial establishing the superiority of daratumumab over standard therapy. The company has several ongoing multicenter, randomized trials in patients with multiple myeloma with a primary endpoint of progression-free survival.
The recommended dose and schedule for daratumumab is 16 mg/kg once every week for 8 weeks, then once every 2 weeks for 16 weeks, then once every 4 weeks until disease progression.