User login
House Dems endorse ACA special enrollment period for pregnancy
A group of 55 House Democrats is endorsing an effort to add pregnancy to the list of qualifying life events that allow individuals to select or change their health coverage outside of the annual open enrollment period.
In a March 12 letter to Health and Human Services Secretary Sylvia Burwell, the lawmakers called on the agency to “exercise its authority” and, through subregulatory guidance, create a special enrollment period triggered by pregnancy for health plans that participate in the Affordable Care Act’s insurance marketplaces.
“This is a critical protection – good maternity care is essential for the well-being of women and children,” the lawmakers wrote, noting that women who do not receive prenatal are more likely to have an infant die in the first month, and that maternal mortality rates are up to four times higher for women who do not receive prenatal care.
Although the Affordable Care Act requires coverage of maternity care as an essential health benefit, women are not eligible for this coverage if they are uninsured and become pregnant outside of the open enrollment period, or if they are enrolled in an older health plan that is exempt from offering the ACA’s essential health benefits.
Special enrollment periods already exist under the ACA for the birth of a child but not for pregnancy.
A separate letter sent the same day and signed by 32 organizations, including the American Congress of Obstetricians and Gynecologists and the Association of Reproductive Health Professionals, also calls on HHS to make the regulatory change.
A group of 55 House Democrats is endorsing an effort to add pregnancy to the list of qualifying life events that allow individuals to select or change their health coverage outside of the annual open enrollment period.
In a March 12 letter to Health and Human Services Secretary Sylvia Burwell, the lawmakers called on the agency to “exercise its authority” and, through subregulatory guidance, create a special enrollment period triggered by pregnancy for health plans that participate in the Affordable Care Act’s insurance marketplaces.
“This is a critical protection – good maternity care is essential for the well-being of women and children,” the lawmakers wrote, noting that women who do not receive prenatal are more likely to have an infant die in the first month, and that maternal mortality rates are up to four times higher for women who do not receive prenatal care.
Although the Affordable Care Act requires coverage of maternity care as an essential health benefit, women are not eligible for this coverage if they are uninsured and become pregnant outside of the open enrollment period, or if they are enrolled in an older health plan that is exempt from offering the ACA’s essential health benefits.
Special enrollment periods already exist under the ACA for the birth of a child but not for pregnancy.
A separate letter sent the same day and signed by 32 organizations, including the American Congress of Obstetricians and Gynecologists and the Association of Reproductive Health Professionals, also calls on HHS to make the regulatory change.
A group of 55 House Democrats is endorsing an effort to add pregnancy to the list of qualifying life events that allow individuals to select or change their health coverage outside of the annual open enrollment period.
In a March 12 letter to Health and Human Services Secretary Sylvia Burwell, the lawmakers called on the agency to “exercise its authority” and, through subregulatory guidance, create a special enrollment period triggered by pregnancy for health plans that participate in the Affordable Care Act’s insurance marketplaces.
“This is a critical protection – good maternity care is essential for the well-being of women and children,” the lawmakers wrote, noting that women who do not receive prenatal are more likely to have an infant die in the first month, and that maternal mortality rates are up to four times higher for women who do not receive prenatal care.
Although the Affordable Care Act requires coverage of maternity care as an essential health benefit, women are not eligible for this coverage if they are uninsured and become pregnant outside of the open enrollment period, or if they are enrolled in an older health plan that is exempt from offering the ACA’s essential health benefits.
Special enrollment periods already exist under the ACA for the birth of a child but not for pregnancy.
A separate letter sent the same day and signed by 32 organizations, including the American Congress of Obstetricians and Gynecologists and the Association of Reproductive Health Professionals, also calls on HHS to make the regulatory change.
Fewer women report stressful events in the year before giving birth
The prevalence of stressful life events decreased slightly for women in the year preceding their infant’s birth during 2000 to 2010, according to a report from the Centers for Disease Control and Prevention.
In 2010, slightly more than 70% of women reported at least one stressful life event (SLE) in the year before giving birth. The self-reported prevalence of SLEs, however, had a statistically significant decrease over the decade, the CDC investigators wrote, with the prevalence of at least one SLE falling 0.54 percentage points per year from 2000 to 2010.
In 2010, the biggest cause of stress was financial, with 51% of women reporting at least one financial SLE. Just under 30% reported at least one emotional SLE, 28.5% reported at least one partner-related SLE (such as divorce or separation), and just under 18% reported at least one traumatic SLE. The average number of SLEs was 1.81 in 2010.
“Current research suggests that increased prenatal stress is associated with adverse pregnancy outcomes, including low birth weight, preterm birth, and peripartum depression,” the investigators wrote. “However, there is evidence that social support has a mitigating effect on the relationship between stress and adverse pregnancy outcomes.”
Find the full report in the CDC’s Morbidity and Mortality Weekly Report (2015 March 13;64:247-51).
The prevalence of stressful life events decreased slightly for women in the year preceding their infant’s birth during 2000 to 2010, according to a report from the Centers for Disease Control and Prevention.
In 2010, slightly more than 70% of women reported at least one stressful life event (SLE) in the year before giving birth. The self-reported prevalence of SLEs, however, had a statistically significant decrease over the decade, the CDC investigators wrote, with the prevalence of at least one SLE falling 0.54 percentage points per year from 2000 to 2010.
In 2010, the biggest cause of stress was financial, with 51% of women reporting at least one financial SLE. Just under 30% reported at least one emotional SLE, 28.5% reported at least one partner-related SLE (such as divorce or separation), and just under 18% reported at least one traumatic SLE. The average number of SLEs was 1.81 in 2010.
“Current research suggests that increased prenatal stress is associated with adverse pregnancy outcomes, including low birth weight, preterm birth, and peripartum depression,” the investigators wrote. “However, there is evidence that social support has a mitigating effect on the relationship between stress and adverse pregnancy outcomes.”
Find the full report in the CDC’s Morbidity and Mortality Weekly Report (2015 March 13;64:247-51).
The prevalence of stressful life events decreased slightly for women in the year preceding their infant’s birth during 2000 to 2010, according to a report from the Centers for Disease Control and Prevention.
In 2010, slightly more than 70% of women reported at least one stressful life event (SLE) in the year before giving birth. The self-reported prevalence of SLEs, however, had a statistically significant decrease over the decade, the CDC investigators wrote, with the prevalence of at least one SLE falling 0.54 percentage points per year from 2000 to 2010.
In 2010, the biggest cause of stress was financial, with 51% of women reporting at least one financial SLE. Just under 30% reported at least one emotional SLE, 28.5% reported at least one partner-related SLE (such as divorce or separation), and just under 18% reported at least one traumatic SLE. The average number of SLEs was 1.81 in 2010.
“Current research suggests that increased prenatal stress is associated with adverse pregnancy outcomes, including low birth weight, preterm birth, and peripartum depression,” the investigators wrote. “However, there is evidence that social support has a mitigating effect on the relationship between stress and adverse pregnancy outcomes.”
Find the full report in the CDC’s Morbidity and Mortality Weekly Report (2015 March 13;64:247-51).
Racial differences in birth outcomes noted in women using ART
AT ENDO 2015
SAN DIEGO – Compared to white women undergoing assisted reproductive technology, black women were more likely to have preterm births and deliver small-for-gestational-age infants, a large prospective cohort study demonstrated.
“What this means in the long-term outcomes and what this means as far as counseling [ART patients] is a tricky subject, but I think it does warrant more study,” Dr. Snigdha Alur, the study’s lead author, said in an interview at the meeting of the Endocrine Society.
Assisted reproductive technology “is an increasingly employed form of treatment, prompting interest in which factors could predict or influence its success. Despite black women having the highest prevalence of infertility and ample investigation on racial disparities influencing pregnancy outcomes, few have evaluated whether race also affects ART outcomes,” Dr. Alur of the department of obstetrics and gynecology at the University of Rochester (N.Y.) Medical Center, and her associates wrote in a late-breaking abstract.
In an effort to explore whether adverse pregnancy outcomes differ between white and black women using ART, the researchers evaluated data from 1,871 singleton births to women resulting from ART delivered in the Central and Finger Lakes regions of New York state between 2005 and 2013.
The women completed the state’s perinatal data system questionnaire pertaining to their and their partners’ background and their prenatal care, labor course, and birth outcome. These data were combined with obstetric records including birth size and gestational age. A preterm birth was defined as one delivered at less than 37 weeks’ gestational age, while a very preterm birth was defined as one delivered at less than 34 weeks’ gestational age. A small-for-gestational-age (SGA) infant and a very SGA infant were defined as gender-adjusted weight less than 10% and less than 5%, respectively.
Of the 1,871 singleton births studied, 47 were to black women and 1,824 were to white women. After the researchers adjusted for maternal age, smoking status, highest level of education, and other covariates, black women were significantly more likely to have preterm births (odds ratio, 2.63) but not very preterm births (OR, 2.17), compared with their white counterparts. They also had significantly increased odds of having a SGA (OR, 2.71) or a very SGA infant (OR, 3.01), compared with white women.
“It could be that we have to alter some of our counseling and education based on some of these findings,” Dr. Alur said. “Maybe it’s not just the ART, but there could be other factors playing a role [in poorer outcomes for black ART pregnancies] that need further research.”
Dr. Alur reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT ENDO 2015
SAN DIEGO – Compared to white women undergoing assisted reproductive technology, black women were more likely to have preterm births and deliver small-for-gestational-age infants, a large prospective cohort study demonstrated.
“What this means in the long-term outcomes and what this means as far as counseling [ART patients] is a tricky subject, but I think it does warrant more study,” Dr. Snigdha Alur, the study’s lead author, said in an interview at the meeting of the Endocrine Society.
Assisted reproductive technology “is an increasingly employed form of treatment, prompting interest in which factors could predict or influence its success. Despite black women having the highest prevalence of infertility and ample investigation on racial disparities influencing pregnancy outcomes, few have evaluated whether race also affects ART outcomes,” Dr. Alur of the department of obstetrics and gynecology at the University of Rochester (N.Y.) Medical Center, and her associates wrote in a late-breaking abstract.
In an effort to explore whether adverse pregnancy outcomes differ between white and black women using ART, the researchers evaluated data from 1,871 singleton births to women resulting from ART delivered in the Central and Finger Lakes regions of New York state between 2005 and 2013.
The women completed the state’s perinatal data system questionnaire pertaining to their and their partners’ background and their prenatal care, labor course, and birth outcome. These data were combined with obstetric records including birth size and gestational age. A preterm birth was defined as one delivered at less than 37 weeks’ gestational age, while a very preterm birth was defined as one delivered at less than 34 weeks’ gestational age. A small-for-gestational-age (SGA) infant and a very SGA infant were defined as gender-adjusted weight less than 10% and less than 5%, respectively.
Of the 1,871 singleton births studied, 47 were to black women and 1,824 were to white women. After the researchers adjusted for maternal age, smoking status, highest level of education, and other covariates, black women were significantly more likely to have preterm births (odds ratio, 2.63) but not very preterm births (OR, 2.17), compared with their white counterparts. They also had significantly increased odds of having a SGA (OR, 2.71) or a very SGA infant (OR, 3.01), compared with white women.
“It could be that we have to alter some of our counseling and education based on some of these findings,” Dr. Alur said. “Maybe it’s not just the ART, but there could be other factors playing a role [in poorer outcomes for black ART pregnancies] that need further research.”
Dr. Alur reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT ENDO 2015
SAN DIEGO – Compared to white women undergoing assisted reproductive technology, black women were more likely to have preterm births and deliver small-for-gestational-age infants, a large prospective cohort study demonstrated.
“What this means in the long-term outcomes and what this means as far as counseling [ART patients] is a tricky subject, but I think it does warrant more study,” Dr. Snigdha Alur, the study’s lead author, said in an interview at the meeting of the Endocrine Society.
Assisted reproductive technology “is an increasingly employed form of treatment, prompting interest in which factors could predict or influence its success. Despite black women having the highest prevalence of infertility and ample investigation on racial disparities influencing pregnancy outcomes, few have evaluated whether race also affects ART outcomes,” Dr. Alur of the department of obstetrics and gynecology at the University of Rochester (N.Y.) Medical Center, and her associates wrote in a late-breaking abstract.
In an effort to explore whether adverse pregnancy outcomes differ between white and black women using ART, the researchers evaluated data from 1,871 singleton births to women resulting from ART delivered in the Central and Finger Lakes regions of New York state between 2005 and 2013.
The women completed the state’s perinatal data system questionnaire pertaining to their and their partners’ background and their prenatal care, labor course, and birth outcome. These data were combined with obstetric records including birth size and gestational age. A preterm birth was defined as one delivered at less than 37 weeks’ gestational age, while a very preterm birth was defined as one delivered at less than 34 weeks’ gestational age. A small-for-gestational-age (SGA) infant and a very SGA infant were defined as gender-adjusted weight less than 10% and less than 5%, respectively.
Of the 1,871 singleton births studied, 47 were to black women and 1,824 were to white women. After the researchers adjusted for maternal age, smoking status, highest level of education, and other covariates, black women were significantly more likely to have preterm births (odds ratio, 2.63) but not very preterm births (OR, 2.17), compared with their white counterparts. They also had significantly increased odds of having a SGA (OR, 2.71) or a very SGA infant (OR, 3.01), compared with white women.
“It could be that we have to alter some of our counseling and education based on some of these findings,” Dr. Alur said. “Maybe it’s not just the ART, but there could be other factors playing a role [in poorer outcomes for black ART pregnancies] that need further research.”
Dr. Alur reported having no relevant financial conflicts.
On Twitter @dougbrunk
Key clinical point: Black women with singleton births from assisted reproductive technology were more likely to have preterm births and deliver SGA infants when compared with white women who also used ART.
Major finding: Black women were significantly more likely to have preterm births (OR 2.63) but not very preterm births (OR 2.17), when compared with their white counterparts. They also had significantly increased odds of having a SGA (OR 2.71) or a very SGA infant (OR 3.01).
Data source: A prospective analysis of 1,871 births to women resulting from ART delivered in the Central and Finger Lakes regions of New York State between 2005 and 2013.
Disclosures: Dr. Alur reported having no relevant financial conflicts.
ACOG President John Jennings comments on the risks of home birth
Responses from both sides of the home-birth controversy are parried in an Opinion Page debate titled “Is Home Birth Ever a Safe Choice?” published on February 24, 2015, in the New York Times.
Debaters include John Jennings, MD, President of the American Congress of Obstetricians and Gynecologists (ACOG); Tekoa King, a certified nurse midwife (CNM) and Deputy Editor of the Journal of Midwifery & Women’s Health; Amos Grunebaum, MD, Director of Obstetrics, and Frank Chervenak, MD, Obstetrician and Gynecologist-in-chief at New York-Presbyterian Hospital, Weill Medical College of Cornell University; Marinah Valenzuela Farrell, a certified professional midwife (CPM) and president of the Midwives Alliance of North America; Aaron Caughey, MD, Chair of the Department of Obstetrics and Gynecology and Associate Dean for Women’s Health Research and Policy at Oregon Health and Science University’s School of Medicine; and Aja Graydon, a musician who experienced home birth.
To read the New York Times article, click here.
Responses from both sides of the home-birth controversy are parried in an Opinion Page debate titled “Is Home Birth Ever a Safe Choice?” published on February 24, 2015, in the New York Times.
Debaters include John Jennings, MD, President of the American Congress of Obstetricians and Gynecologists (ACOG); Tekoa King, a certified nurse midwife (CNM) and Deputy Editor of the Journal of Midwifery & Women’s Health; Amos Grunebaum, MD, Director of Obstetrics, and Frank Chervenak, MD, Obstetrician and Gynecologist-in-chief at New York-Presbyterian Hospital, Weill Medical College of Cornell University; Marinah Valenzuela Farrell, a certified professional midwife (CPM) and president of the Midwives Alliance of North America; Aaron Caughey, MD, Chair of the Department of Obstetrics and Gynecology and Associate Dean for Women’s Health Research and Policy at Oregon Health and Science University’s School of Medicine; and Aja Graydon, a musician who experienced home birth.
To read the New York Times article, click here.
Responses from both sides of the home-birth controversy are parried in an Opinion Page debate titled “Is Home Birth Ever a Safe Choice?” published on February 24, 2015, in the New York Times.
Debaters include John Jennings, MD, President of the American Congress of Obstetricians and Gynecologists (ACOG); Tekoa King, a certified nurse midwife (CNM) and Deputy Editor of the Journal of Midwifery & Women’s Health; Amos Grunebaum, MD, Director of Obstetrics, and Frank Chervenak, MD, Obstetrician and Gynecologist-in-chief at New York-Presbyterian Hospital, Weill Medical College of Cornell University; Marinah Valenzuela Farrell, a certified professional midwife (CPM) and president of the Midwives Alliance of North America; Aaron Caughey, MD, Chair of the Department of Obstetrics and Gynecology and Associate Dean for Women’s Health Research and Policy at Oregon Health and Science University’s School of Medicine; and Aja Graydon, a musician who experienced home birth.
To read the New York Times article, click here.
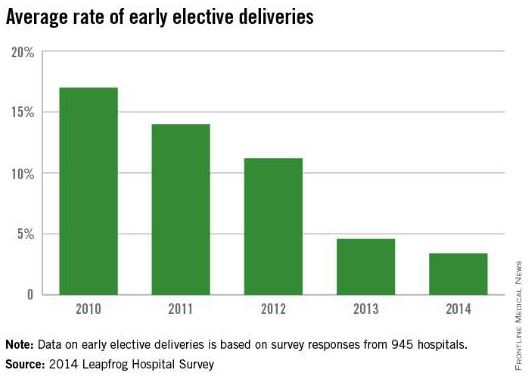
Leapfrog: Early elective deliveries down nationally, but rates vary
The practice of early elective deliveries is down across the country, but there is still wide variation in meeting maternal quality indicators at U.S. hospitals, according to a new report from the Leapfrog Group.
Among 945 hospitals that voluntarily reported quality data to the Leapfrog Group, 78% performed early elective deliveries less than 5% of the time in 2014. The current data shows a steady decline in the early elective deliveries – scheduled cesarean deliveries or elective inductions that occur prior to 39 weeks’ gestation without a medical indication. Between 2010 and 2014, the national average rate of early elective deliveries dropped from 17% to 3.4%.
But variation remains. Among 82 hospitals that reported data in 2014, the rate of early elective deliveries was more than 10%. The rate was higher in rural areas than at hospitals in urban areas, the report found.
The Leapfrog Group report also shows some small gains in decreasing the use of episiotomy at U.S. hospitals. The national average rate of episiotomies decreased from 13% in 2012 to 11.3% in 2014.
However, there was also wide variation in this measure. Of the 990 hospitals that reported episiotomy data, 65% met the Leapfrog goal of performing the procedure 12% of the time or less. In 25 hospitals, the rate was 1% or less, while it was 40% or more in 12 hospitals.
U.S. hospitals have made virtually no progress in ensuring that high-risk deliveries are performed at hospitals with experienced, on-site neonatal intensive care units, according to the report.
Hospitals met the Leapfrog standard for high-risk deliveries if they delivered at least 50 very-low-birth-weight babies per year and ensured that at least 80% of mothers received antenatal steroids prior to delivery, or if they maintained a lower-than-average morbidity/mortality rate for very-low-birth-weight babies and provided antenatal steroids prior to delivery for at least 80% of mothers.
In 2014, the number of high-risk deliveries that occurred in hospitals meeting the Leapfrog standard was 24.4% of 435 hospitals, compared with 24% of 451 hospitals during the previous year.
The Leapfrog Group report relies on voluntary reporting from adult general acute care and freestanding pediatric hospitals across the United States. The report was prepared by Castlight Health.
On Twitter @maryellenny
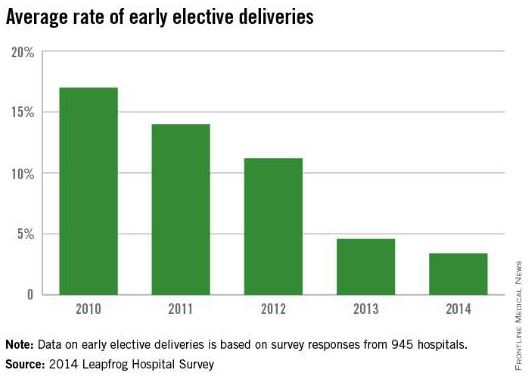
The practice of early elective deliveries is down across the country, but there is still wide variation in meeting maternal quality indicators at U.S. hospitals, according to a new report from the Leapfrog Group.
Among 945 hospitals that voluntarily reported quality data to the Leapfrog Group, 78% performed early elective deliveries less than 5% of the time in 2014. The current data shows a steady decline in the early elective deliveries – scheduled cesarean deliveries or elective inductions that occur prior to 39 weeks’ gestation without a medical indication. Between 2010 and 2014, the national average rate of early elective deliveries dropped from 17% to 3.4%.
But variation remains. Among 82 hospitals that reported data in 2014, the rate of early elective deliveries was more than 10%. The rate was higher in rural areas than at hospitals in urban areas, the report found.
The Leapfrog Group report also shows some small gains in decreasing the use of episiotomy at U.S. hospitals. The national average rate of episiotomies decreased from 13% in 2012 to 11.3% in 2014.
However, there was also wide variation in this measure. Of the 990 hospitals that reported episiotomy data, 65% met the Leapfrog goal of performing the procedure 12% of the time or less. In 25 hospitals, the rate was 1% or less, while it was 40% or more in 12 hospitals.
U.S. hospitals have made virtually no progress in ensuring that high-risk deliveries are performed at hospitals with experienced, on-site neonatal intensive care units, according to the report.
Hospitals met the Leapfrog standard for high-risk deliveries if they delivered at least 50 very-low-birth-weight babies per year and ensured that at least 80% of mothers received antenatal steroids prior to delivery, or if they maintained a lower-than-average morbidity/mortality rate for very-low-birth-weight babies and provided antenatal steroids prior to delivery for at least 80% of mothers.
In 2014, the number of high-risk deliveries that occurred in hospitals meeting the Leapfrog standard was 24.4% of 435 hospitals, compared with 24% of 451 hospitals during the previous year.
The Leapfrog Group report relies on voluntary reporting from adult general acute care and freestanding pediatric hospitals across the United States. The report was prepared by Castlight Health.
On Twitter @maryellenny
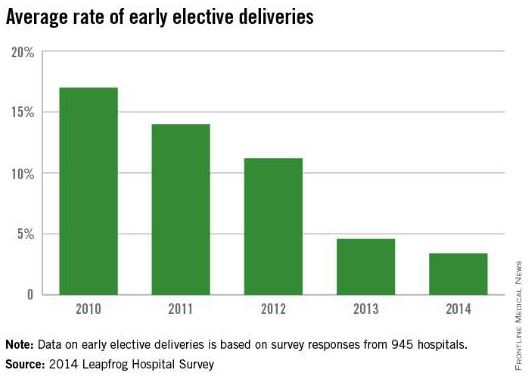
The practice of early elective deliveries is down across the country, but there is still wide variation in meeting maternal quality indicators at U.S. hospitals, according to a new report from the Leapfrog Group.
Among 945 hospitals that voluntarily reported quality data to the Leapfrog Group, 78% performed early elective deliveries less than 5% of the time in 2014. The current data shows a steady decline in the early elective deliveries – scheduled cesarean deliveries or elective inductions that occur prior to 39 weeks’ gestation without a medical indication. Between 2010 and 2014, the national average rate of early elective deliveries dropped from 17% to 3.4%.
But variation remains. Among 82 hospitals that reported data in 2014, the rate of early elective deliveries was more than 10%. The rate was higher in rural areas than at hospitals in urban areas, the report found.
The Leapfrog Group report also shows some small gains in decreasing the use of episiotomy at U.S. hospitals. The national average rate of episiotomies decreased from 13% in 2012 to 11.3% in 2014.
However, there was also wide variation in this measure. Of the 990 hospitals that reported episiotomy data, 65% met the Leapfrog goal of performing the procedure 12% of the time or less. In 25 hospitals, the rate was 1% or less, while it was 40% or more in 12 hospitals.
U.S. hospitals have made virtually no progress in ensuring that high-risk deliveries are performed at hospitals with experienced, on-site neonatal intensive care units, according to the report.
Hospitals met the Leapfrog standard for high-risk deliveries if they delivered at least 50 very-low-birth-weight babies per year and ensured that at least 80% of mothers received antenatal steroids prior to delivery, or if they maintained a lower-than-average morbidity/mortality rate for very-low-birth-weight babies and provided antenatal steroids prior to delivery for at least 80% of mothers.
In 2014, the number of high-risk deliveries that occurred in hospitals meeting the Leapfrog standard was 24.4% of 435 hospitals, compared with 24% of 451 hospitals during the previous year.
The Leapfrog Group report relies on voluntary reporting from adult general acute care and freestanding pediatric hospitals across the United States. The report was prepared by Castlight Health.
On Twitter @maryellenny
Extending second stage of labor raised maternal and neonatal morbidity
SAN DIEGO – The crossing times for the rate of spontaneous vaginal delivery versus a composite maternal or neonatal morbidity/mortality occurred slightly earlier than current recommended guidelines for women with an epidural (2.6 hours versus 3 hours), regardless of parity, results from a large federally funded retrospective study showed.
After this time, the risk of morbidity was higher than the chance of vaginal delivery.
But for women without an epidural, the crossing times for spontaneous vaginal delivery (SVD) and any morbidity occurred slightly later than current guidelines suggest (2.4 hours versus 2 hours in nulliparous women, and 2.3 hours versus 1 hour in multiparous women). Only in multiparous women without an epidural did the lines cross at least 1 hour later, Dr. Katherine Laughon Grantz said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We provide data that can be used to balance chances of SVD versus morbidity with increasing duration of second stage,” said Dr. Grantz, an investigator at the National Institute of Child Health and Human Development.
A June 2000 clinical management guideline from the American College of Obstetricians and Gynecologists states that operative vaginal delivery is indicated for nulliparous women who lack progress after 3 hours with an epidural, or 2 hours without an epidural. For multiparous women, the guideline is 2 hours with an epidural and 1 hour without. Dr. Grantz said that historical guidance for the 2-hour rule was first described in the 1850s by expert opinion and case series.
“Recently, however, it’s been recommended that it is safe to extend the current ACOG guidelines by 1 hour,” she said.
In 2014, Dr. Grantz and her colleagues published a study showing that prolonged second stage is associated with increased risk of maternal and neonatal morbidity (Obstet. Gynecol. 2014;124:57-67).
“Therefore, our group wanted to take this a step further, to determine the second-stage duration wherein the chance of vaginal delivery became so low it was outweighed by the increased risk of morbidity,” she said.
The researchers used data from the Consortium on Safe Labor, a study of 19 hospitals within 12 medical institutions in the United States. Medical records from 228,438 deliveries between 2002 and 2008 were evaluated, including patient demographics, prenatal complications, labor and delivery information, and maternal and neonatal outcomes.
They limited the analysis to singleton gestations delivered greater than or equal to 36 weeks’ gestation and excluded nonvertex presentation, antepartum stillbirth prior to onset of labor, women with a prior uterine scar, congenital anomalies, and cervical exams prior to vaginal delivery that were less than 10 cm or missing. This resulted in a total of 103,415 deliveries studied.
The researchers analyzed the groups in four strata: by parity (nulliparous or multiparous), and by epidural status (yes or no). Four outcomes were studied: spontaneous vaginal delivery; a composite of maternal morbidity (which included postpartum hemorrhage, blood transfusion, cesarean hysterectomy, endometritis, or ICU admission); composite neonatal morbidity/mortality (including shoulder dystocia, 5-minute Apgar score of less than 4, need for continuous positive airway pressure resuscitation or higher, NICU admission, sepsis, pneumonia, hypoxic-ischemic encephalopathy/periventricular leukomalacia, seizure, intracranial hemorrhage/periventricular hemorrhage, asphyxia, or neonatal death); and any maternal or neonatal morbidity.
They calculated the hazard rates of each outcome and created joint models for hazard rates that model rate of spontaneous vaginal delivery versus the risk of each of the three morbidity categories.
Dr. Grantz reported that for nulliparous women with an epidural, extending the second stage from 3 to 4 hours resulted in 16% of maternal and 15% of neonatal morbidities, with approximately 5.5% additional SVD during that hour.
“Our data are limited because these are retrospective data,” Dr. Grantz noted. “Women who were allowed to continue with a prolonged second stage might have been different than women who did not continue with a prolonged second stage. We also did not have information on delayed versus active pushing, and we lacked long-term maternal and child outcomes.”
But the major strength of the study is the large number of deliveries, she said, which allowed the researchers to investigate rare neonatal outcomes at term.
The study was supported by the NICHD. Dr. Grantz reported having no relevant financial conflicts.
On Twitter @dougbrunk
SAN DIEGO – The crossing times for the rate of spontaneous vaginal delivery versus a composite maternal or neonatal morbidity/mortality occurred slightly earlier than current recommended guidelines for women with an epidural (2.6 hours versus 3 hours), regardless of parity, results from a large federally funded retrospective study showed.
After this time, the risk of morbidity was higher than the chance of vaginal delivery.
But for women without an epidural, the crossing times for spontaneous vaginal delivery (SVD) and any morbidity occurred slightly later than current guidelines suggest (2.4 hours versus 2 hours in nulliparous women, and 2.3 hours versus 1 hour in multiparous women). Only in multiparous women without an epidural did the lines cross at least 1 hour later, Dr. Katherine Laughon Grantz said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We provide data that can be used to balance chances of SVD versus morbidity with increasing duration of second stage,” said Dr. Grantz, an investigator at the National Institute of Child Health and Human Development.
A June 2000 clinical management guideline from the American College of Obstetricians and Gynecologists states that operative vaginal delivery is indicated for nulliparous women who lack progress after 3 hours with an epidural, or 2 hours without an epidural. For multiparous women, the guideline is 2 hours with an epidural and 1 hour without. Dr. Grantz said that historical guidance for the 2-hour rule was first described in the 1850s by expert opinion and case series.
“Recently, however, it’s been recommended that it is safe to extend the current ACOG guidelines by 1 hour,” she said.
In 2014, Dr. Grantz and her colleagues published a study showing that prolonged second stage is associated with increased risk of maternal and neonatal morbidity (Obstet. Gynecol. 2014;124:57-67).
“Therefore, our group wanted to take this a step further, to determine the second-stage duration wherein the chance of vaginal delivery became so low it was outweighed by the increased risk of morbidity,” she said.
The researchers used data from the Consortium on Safe Labor, a study of 19 hospitals within 12 medical institutions in the United States. Medical records from 228,438 deliveries between 2002 and 2008 were evaluated, including patient demographics, prenatal complications, labor and delivery information, and maternal and neonatal outcomes.
They limited the analysis to singleton gestations delivered greater than or equal to 36 weeks’ gestation and excluded nonvertex presentation, antepartum stillbirth prior to onset of labor, women with a prior uterine scar, congenital anomalies, and cervical exams prior to vaginal delivery that were less than 10 cm or missing. This resulted in a total of 103,415 deliveries studied.
The researchers analyzed the groups in four strata: by parity (nulliparous or multiparous), and by epidural status (yes or no). Four outcomes were studied: spontaneous vaginal delivery; a composite of maternal morbidity (which included postpartum hemorrhage, blood transfusion, cesarean hysterectomy, endometritis, or ICU admission); composite neonatal morbidity/mortality (including shoulder dystocia, 5-minute Apgar score of less than 4, need for continuous positive airway pressure resuscitation or higher, NICU admission, sepsis, pneumonia, hypoxic-ischemic encephalopathy/periventricular leukomalacia, seizure, intracranial hemorrhage/periventricular hemorrhage, asphyxia, or neonatal death); and any maternal or neonatal morbidity.
They calculated the hazard rates of each outcome and created joint models for hazard rates that model rate of spontaneous vaginal delivery versus the risk of each of the three morbidity categories.
Dr. Grantz reported that for nulliparous women with an epidural, extending the second stage from 3 to 4 hours resulted in 16% of maternal and 15% of neonatal morbidities, with approximately 5.5% additional SVD during that hour.
“Our data are limited because these are retrospective data,” Dr. Grantz noted. “Women who were allowed to continue with a prolonged second stage might have been different than women who did not continue with a prolonged second stage. We also did not have information on delayed versus active pushing, and we lacked long-term maternal and child outcomes.”
But the major strength of the study is the large number of deliveries, she said, which allowed the researchers to investigate rare neonatal outcomes at term.
The study was supported by the NICHD. Dr. Grantz reported having no relevant financial conflicts.
On Twitter @dougbrunk
SAN DIEGO – The crossing times for the rate of spontaneous vaginal delivery versus a composite maternal or neonatal morbidity/mortality occurred slightly earlier than current recommended guidelines for women with an epidural (2.6 hours versus 3 hours), regardless of parity, results from a large federally funded retrospective study showed.
After this time, the risk of morbidity was higher than the chance of vaginal delivery.
But for women without an epidural, the crossing times for spontaneous vaginal delivery (SVD) and any morbidity occurred slightly later than current guidelines suggest (2.4 hours versus 2 hours in nulliparous women, and 2.3 hours versus 1 hour in multiparous women). Only in multiparous women without an epidural did the lines cross at least 1 hour later, Dr. Katherine Laughon Grantz said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We provide data that can be used to balance chances of SVD versus morbidity with increasing duration of second stage,” said Dr. Grantz, an investigator at the National Institute of Child Health and Human Development.
A June 2000 clinical management guideline from the American College of Obstetricians and Gynecologists states that operative vaginal delivery is indicated for nulliparous women who lack progress after 3 hours with an epidural, or 2 hours without an epidural. For multiparous women, the guideline is 2 hours with an epidural and 1 hour without. Dr. Grantz said that historical guidance for the 2-hour rule was first described in the 1850s by expert opinion and case series.
“Recently, however, it’s been recommended that it is safe to extend the current ACOG guidelines by 1 hour,” she said.
In 2014, Dr. Grantz and her colleagues published a study showing that prolonged second stage is associated with increased risk of maternal and neonatal morbidity (Obstet. Gynecol. 2014;124:57-67).
“Therefore, our group wanted to take this a step further, to determine the second-stage duration wherein the chance of vaginal delivery became so low it was outweighed by the increased risk of morbidity,” she said.
The researchers used data from the Consortium on Safe Labor, a study of 19 hospitals within 12 medical institutions in the United States. Medical records from 228,438 deliveries between 2002 and 2008 were evaluated, including patient demographics, prenatal complications, labor and delivery information, and maternal and neonatal outcomes.
They limited the analysis to singleton gestations delivered greater than or equal to 36 weeks’ gestation and excluded nonvertex presentation, antepartum stillbirth prior to onset of labor, women with a prior uterine scar, congenital anomalies, and cervical exams prior to vaginal delivery that were less than 10 cm or missing. This resulted in a total of 103,415 deliveries studied.
The researchers analyzed the groups in four strata: by parity (nulliparous or multiparous), and by epidural status (yes or no). Four outcomes were studied: spontaneous vaginal delivery; a composite of maternal morbidity (which included postpartum hemorrhage, blood transfusion, cesarean hysterectomy, endometritis, or ICU admission); composite neonatal morbidity/mortality (including shoulder dystocia, 5-minute Apgar score of less than 4, need for continuous positive airway pressure resuscitation or higher, NICU admission, sepsis, pneumonia, hypoxic-ischemic encephalopathy/periventricular leukomalacia, seizure, intracranial hemorrhage/periventricular hemorrhage, asphyxia, or neonatal death); and any maternal or neonatal morbidity.
They calculated the hazard rates of each outcome and created joint models for hazard rates that model rate of spontaneous vaginal delivery versus the risk of each of the three morbidity categories.
Dr. Grantz reported that for nulliparous women with an epidural, extending the second stage from 3 to 4 hours resulted in 16% of maternal and 15% of neonatal morbidities, with approximately 5.5% additional SVD during that hour.
“Our data are limited because these are retrospective data,” Dr. Grantz noted. “Women who were allowed to continue with a prolonged second stage might have been different than women who did not continue with a prolonged second stage. We also did not have information on delayed versus active pushing, and we lacked long-term maternal and child outcomes.”
But the major strength of the study is the large number of deliveries, she said, which allowed the researchers to investigate rare neonatal outcomes at term.
The study was supported by the NICHD. Dr. Grantz reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT THE PREGNANCY MEETING
Key clinical point: Extending the second stage in nulliparous women from 3 hours to 4 hours was associated with an increased rate of maternal and neonatal morbidity.
Major finding: Among nulliparous women with an epidural, extending the second stage of labor from 3 hours to 4 hours resulted in 16% of maternal and 15% of neonatal morbidities, with approximately 5.5% additional spontaneous vaginal deliveries during that hour.
Data source: A retrospective study of medical records from 103,415 deliveries between 2002 and 2008.
Disclosures: The study was supported by the National Institute of Child Health and Human Development. Dr. Grantz reported having no relevant financial conflicts.
TOLAC: Induction poses no maternal risk vs. expectant management
SAN DIEGO – Maternal morbidity was not consistently increased in a study of women with one prior cesarean delivery who were attempting a trial of labor and who were induced between 37 and 40 weeks, according to a secondary analysis of data from the National Institutes of Health Consortium on Safe Labor.
But the risk of admission to the neonatal intensive care unit did increase among women induced at 37 weeks, Dr. Justin Lappen reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Further, induction at 37, 38, and 39 weeks of gestation increased the risk of a failed trial of labor after cesarean section (TOLAC) in the 1,626 women in the retrospective multicenter study who were induced, compared with 4,407 who were managed expectantly (odds ratios, 1.53, 1.74, and 2.16, respectively).
The induction group was compared at gestational weeks 37-40 with all undelivered women in the expectant management group. After adjustment for prior spontaneous vaginal delivery, body mass index, hypertensive disorders, maternal age, week of gestation, birth weight, and neonatal gender, induction was not associated with any consistent increase in the risk of maternal morbidity (odds ratios at weeks 37-40 were 0.49, 0.64, 1.87, and 1.06, respectively).
The researchers defined maternal morbidity based on a composite of outcomes including hysterectomy, transfusion, intensive care unit transfer, venous thromboembolism, and death.
The increased risk of the composite maternal morbidity at 39 weeks was primarily the result of a significantly increased risk of transfusion among women with failed TOLAC, said Dr. Lappen of Case Western Reserve University, Cleveland.
However, among those who were induced at 37 weeks, the risk of neonatal ICU admission was increased, compared with women being expectantly managed who delivered at or beyond 37 weeks (OR, 2.51).
No increased risk was seen in those induced beyond 37 weeks, and no increased risk in neonatal morbidity – defined as a composite of 5-minute Apgar scores of less than 5, arterial cord pH less than 7.0, asphyxia, hypoxic ischemic encephalopathy, and death – was seen with induction at any week of gestation analyzed, Dr. Lappen said.
“Our findings should not change the current obstetric practice, which supports an individualized approach to the use of induction in appropriate candidates attempting TOLAC, Dr. Lappen said.
The researchers also performed a subset analysis in a low-risk cohort derived by excluding all women with chronic conditions who were ineligible for expectant management and by limiting the induction group to include only nonmedically indicated inductions of labor.
The association between induction and composite maternal morbidity was unchanged in this subset analysis, with greater risk seen at 39 weeks – again in association with increased risk of transfusion among those with a failed TOLAC attempt.
However, the association between induction and NICU admission at 37 weeks was no longer present in the low-risk cohort, and the risk was cut in half at 39 weeks in this cohort (OR, 0.52). As in the entire cohort, no association between induction and neonatal morbidity was present.
“Consistent with the primary cohort, nonmedically indicated induction was associated with an increased risk of failed TOLAC,” Dr. Lappen said. This finding was statistically significant at 38 and 39 weeks (ORs, 2.67 and 2.34, respectively), he said.
No association was seen between induction and uterine rupture in either the entire cohort or the low-risk cohort, he said.
Study subjects were women with a live, singleton gestation of at least 37 weeks identified from the Consortium on Safe Labor, a cohort of more than 228,600 deliveries at 12 centers between 2002 and 2008, which was designed to characterize current obstetric practice and outcomes.
Dr. Lappen reported having no financial disclosures.
SAN DIEGO – Maternal morbidity was not consistently increased in a study of women with one prior cesarean delivery who were attempting a trial of labor and who were induced between 37 and 40 weeks, according to a secondary analysis of data from the National Institutes of Health Consortium on Safe Labor.
But the risk of admission to the neonatal intensive care unit did increase among women induced at 37 weeks, Dr. Justin Lappen reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Further, induction at 37, 38, and 39 weeks of gestation increased the risk of a failed trial of labor after cesarean section (TOLAC) in the 1,626 women in the retrospective multicenter study who were induced, compared with 4,407 who were managed expectantly (odds ratios, 1.53, 1.74, and 2.16, respectively).
The induction group was compared at gestational weeks 37-40 with all undelivered women in the expectant management group. After adjustment for prior spontaneous vaginal delivery, body mass index, hypertensive disorders, maternal age, week of gestation, birth weight, and neonatal gender, induction was not associated with any consistent increase in the risk of maternal morbidity (odds ratios at weeks 37-40 were 0.49, 0.64, 1.87, and 1.06, respectively).
The researchers defined maternal morbidity based on a composite of outcomes including hysterectomy, transfusion, intensive care unit transfer, venous thromboembolism, and death.
The increased risk of the composite maternal morbidity at 39 weeks was primarily the result of a significantly increased risk of transfusion among women with failed TOLAC, said Dr. Lappen of Case Western Reserve University, Cleveland.
However, among those who were induced at 37 weeks, the risk of neonatal ICU admission was increased, compared with women being expectantly managed who delivered at or beyond 37 weeks (OR, 2.51).
No increased risk was seen in those induced beyond 37 weeks, and no increased risk in neonatal morbidity – defined as a composite of 5-minute Apgar scores of less than 5, arterial cord pH less than 7.0, asphyxia, hypoxic ischemic encephalopathy, and death – was seen with induction at any week of gestation analyzed, Dr. Lappen said.
“Our findings should not change the current obstetric practice, which supports an individualized approach to the use of induction in appropriate candidates attempting TOLAC, Dr. Lappen said.
The researchers also performed a subset analysis in a low-risk cohort derived by excluding all women with chronic conditions who were ineligible for expectant management and by limiting the induction group to include only nonmedically indicated inductions of labor.
The association between induction and composite maternal morbidity was unchanged in this subset analysis, with greater risk seen at 39 weeks – again in association with increased risk of transfusion among those with a failed TOLAC attempt.
However, the association between induction and NICU admission at 37 weeks was no longer present in the low-risk cohort, and the risk was cut in half at 39 weeks in this cohort (OR, 0.52). As in the entire cohort, no association between induction and neonatal morbidity was present.
“Consistent with the primary cohort, nonmedically indicated induction was associated with an increased risk of failed TOLAC,” Dr. Lappen said. This finding was statistically significant at 38 and 39 weeks (ORs, 2.67 and 2.34, respectively), he said.
No association was seen between induction and uterine rupture in either the entire cohort or the low-risk cohort, he said.
Study subjects were women with a live, singleton gestation of at least 37 weeks identified from the Consortium on Safe Labor, a cohort of more than 228,600 deliveries at 12 centers between 2002 and 2008, which was designed to characterize current obstetric practice and outcomes.
Dr. Lappen reported having no financial disclosures.
SAN DIEGO – Maternal morbidity was not consistently increased in a study of women with one prior cesarean delivery who were attempting a trial of labor and who were induced between 37 and 40 weeks, according to a secondary analysis of data from the National Institutes of Health Consortium on Safe Labor.
But the risk of admission to the neonatal intensive care unit did increase among women induced at 37 weeks, Dr. Justin Lappen reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Further, induction at 37, 38, and 39 weeks of gestation increased the risk of a failed trial of labor after cesarean section (TOLAC) in the 1,626 women in the retrospective multicenter study who were induced, compared with 4,407 who were managed expectantly (odds ratios, 1.53, 1.74, and 2.16, respectively).
The induction group was compared at gestational weeks 37-40 with all undelivered women in the expectant management group. After adjustment for prior spontaneous vaginal delivery, body mass index, hypertensive disorders, maternal age, week of gestation, birth weight, and neonatal gender, induction was not associated with any consistent increase in the risk of maternal morbidity (odds ratios at weeks 37-40 were 0.49, 0.64, 1.87, and 1.06, respectively).
The researchers defined maternal morbidity based on a composite of outcomes including hysterectomy, transfusion, intensive care unit transfer, venous thromboembolism, and death.
The increased risk of the composite maternal morbidity at 39 weeks was primarily the result of a significantly increased risk of transfusion among women with failed TOLAC, said Dr. Lappen of Case Western Reserve University, Cleveland.
However, among those who were induced at 37 weeks, the risk of neonatal ICU admission was increased, compared with women being expectantly managed who delivered at or beyond 37 weeks (OR, 2.51).
No increased risk was seen in those induced beyond 37 weeks, and no increased risk in neonatal morbidity – defined as a composite of 5-minute Apgar scores of less than 5, arterial cord pH less than 7.0, asphyxia, hypoxic ischemic encephalopathy, and death – was seen with induction at any week of gestation analyzed, Dr. Lappen said.
“Our findings should not change the current obstetric practice, which supports an individualized approach to the use of induction in appropriate candidates attempting TOLAC, Dr. Lappen said.
The researchers also performed a subset analysis in a low-risk cohort derived by excluding all women with chronic conditions who were ineligible for expectant management and by limiting the induction group to include only nonmedically indicated inductions of labor.
The association between induction and composite maternal morbidity was unchanged in this subset analysis, with greater risk seen at 39 weeks – again in association with increased risk of transfusion among those with a failed TOLAC attempt.
However, the association between induction and NICU admission at 37 weeks was no longer present in the low-risk cohort, and the risk was cut in half at 39 weeks in this cohort (OR, 0.52). As in the entire cohort, no association between induction and neonatal morbidity was present.
“Consistent with the primary cohort, nonmedically indicated induction was associated with an increased risk of failed TOLAC,” Dr. Lappen said. This finding was statistically significant at 38 and 39 weeks (ORs, 2.67 and 2.34, respectively), he said.
No association was seen between induction and uterine rupture in either the entire cohort or the low-risk cohort, he said.
Study subjects were women with a live, singleton gestation of at least 37 weeks identified from the Consortium on Safe Labor, a cohort of more than 228,600 deliveries at 12 centers between 2002 and 2008, which was designed to characterize current obstetric practice and outcomes.
Dr. Lappen reported having no financial disclosures.
AT THE PREGNANCY MEETING
Key clinical point: An individualized approach is warranted for induction in appropriate candidates attempting TOLAC.
Major finding: Induction was not consistently associated with composite maternal morbidity (odds ratios at weeks 37-40 were 0.49, 0.64, 1.87, and 1.06, respectively).
Data source: A secondary analysis of data from a retrospective multicenter study of 6,033 women.
Disclosures: Dr. Lappen reported having no financial disclosures.
NIH to invest $41.5 million for human placenta research
The National Institutes of Health is pledging nearly $42 million to understand and monitor the development of the human placenta.
Previously, studies of the placenta have been limited to ultrasounds, blood tests, and the examination of postdelivery placental tissue. With the infusion of funding, the NIH seeks to develop new technology or new ways to use the existing technology that would allow physicians to safely track how the placenta functions during pregnancy. For instance, these technologies might gauge how blood and oxygen flow through the placenta or how the placenta transmits nutrients to the fetus.
The new funding is the agency’s latest contribution to the Human Placenta Project, which is also delving into the environmental factors that impact the placenta.
“The placenta is a fascinating organ, but it’s one of the least understood. For researchers who want to apply their skills in an area of medicine that isn’t being looked at as much as both scientific opportunity and human health warrant, this is a wonderful chance,” Dr. Alan E. Guttmacher, director of NIH’s National Institute of Child Health and Human Development, said in the statement.The full announcement is available on the NIH website.
The National Institutes of Health is pledging nearly $42 million to understand and monitor the development of the human placenta.
Previously, studies of the placenta have been limited to ultrasounds, blood tests, and the examination of postdelivery placental tissue. With the infusion of funding, the NIH seeks to develop new technology or new ways to use the existing technology that would allow physicians to safely track how the placenta functions during pregnancy. For instance, these technologies might gauge how blood and oxygen flow through the placenta or how the placenta transmits nutrients to the fetus.
The new funding is the agency’s latest contribution to the Human Placenta Project, which is also delving into the environmental factors that impact the placenta.
“The placenta is a fascinating organ, but it’s one of the least understood. For researchers who want to apply their skills in an area of medicine that isn’t being looked at as much as both scientific opportunity and human health warrant, this is a wonderful chance,” Dr. Alan E. Guttmacher, director of NIH’s National Institute of Child Health and Human Development, said in the statement.The full announcement is available on the NIH website.
The National Institutes of Health is pledging nearly $42 million to understand and monitor the development of the human placenta.
Previously, studies of the placenta have been limited to ultrasounds, blood tests, and the examination of postdelivery placental tissue. With the infusion of funding, the NIH seeks to develop new technology or new ways to use the existing technology that would allow physicians to safely track how the placenta functions during pregnancy. For instance, these technologies might gauge how blood and oxygen flow through the placenta or how the placenta transmits nutrients to the fetus.
The new funding is the agency’s latest contribution to the Human Placenta Project, which is also delving into the environmental factors that impact the placenta.
“The placenta is a fascinating organ, but it’s one of the least understood. For researchers who want to apply their skills in an area of medicine that isn’t being looked at as much as both scientific opportunity and human health warrant, this is a wonderful chance,” Dr. Alan E. Guttmacher, director of NIH’s National Institute of Child Health and Human Development, said in the statement.The full announcement is available on the NIH website.
Groups spotlight birth defect prevention in first-ever world awareness day
On March 3, organizations around the world will mark the first-ever World Birth Defects Day by sharing stories and educating the public using the social media hashtag #WorldBDay.
The Centers for Disease Control and Prevention, the March of Dimes, and 10 other organizations have partnered for the awareness-raising event.
The goal is raise awareness not just about the incidence of serious birth defects, but also to increase understanding of the available treatments, expand services for those with birth defects, and improve implementation of primary prevention programs.
Almost 8 million infants each year are born with a serious birth defect of genetic or partially genetic origin, according to the March of Dimes Global Report on Birth Defects. Hundreds of thousands more are born with serious birth defects caused by postconception maternal exposure to environmental agents, including alcohol, medications, rubella, syphilis, and iodine deficiency.
On March 3, organizations around the world will mark the first-ever World Birth Defects Day by sharing stories and educating the public using the social media hashtag #WorldBDay.
The Centers for Disease Control and Prevention, the March of Dimes, and 10 other organizations have partnered for the awareness-raising event.
The goal is raise awareness not just about the incidence of serious birth defects, but also to increase understanding of the available treatments, expand services for those with birth defects, and improve implementation of primary prevention programs.
Almost 8 million infants each year are born with a serious birth defect of genetic or partially genetic origin, according to the March of Dimes Global Report on Birth Defects. Hundreds of thousands more are born with serious birth defects caused by postconception maternal exposure to environmental agents, including alcohol, medications, rubella, syphilis, and iodine deficiency.
On March 3, organizations around the world will mark the first-ever World Birth Defects Day by sharing stories and educating the public using the social media hashtag #WorldBDay.
The Centers for Disease Control and Prevention, the March of Dimes, and 10 other organizations have partnered for the awareness-raising event.
The goal is raise awareness not just about the incidence of serious birth defects, but also to increase understanding of the available treatments, expand services for those with birth defects, and improve implementation of primary prevention programs.
Almost 8 million infants each year are born with a serious birth defect of genetic or partially genetic origin, according to the March of Dimes Global Report on Birth Defects. Hundreds of thousands more are born with serious birth defects caused by postconception maternal exposure to environmental agents, including alcohol, medications, rubella, syphilis, and iodine deficiency.
Does tight control of hypertension in pregnancy produce better perinatal outcomes?
The question of degree of control of hypertension during pregnancy has been debated for many years. The primary concern, which is mainly theoretical, is that tight control of hypertension may lead to underperfusion of the uterus, ultimately resulting in fetal growth restriction. This study adds to the available body of literature on this subject.
Details of the trial
In this pragmatic randomized clinical trial, 987 women with office diastolic BP of 90 to 105 mm Hg (or 85 to 105 mm Hg if they were taking a hypertensive medication) between 14 weeks, zero days of gestation and 33 weeks, 6 days of gestation were randomized to tight (n = 488) versus less-tight control of hypertension (n = 493).
Practitioners were encouraged to use labetalol for treatment. The primary outcome was pregnancy loss (miscarriage, ectopic pregnancy, pregnancy termination, stillbirth, or neonatal death) or the need for high-level neonatal care (defined as greater than normal newborn care for more than 48 hours until 28 days of life or discharge home). Secondary outcomes included serious maternal morbidity as late as 6 weeks postpartum. Statistical analysis was based on the intent-to-treat principle.
Adherence to assigned treatment was good, at approximately 75% in each arm. As stated above, the study found no differences in the combined primary endpoint between the two groups. It also found no differences in other perinatal outcomes, including small size for gestational age or other adverse neonatal outcomes. Maternal complications generally were similar as well, with the exception of severe hypertension, which was more common in the less-tight control group.
Strengths and weaknesses of the study
This trial has several important strengths, including its pragmatic design, making it more applicable to everyday practice. Other strengths include rigorous methods and a large sample size.
Two main weaknesses hamper the study, however:
- the inclusion of both chronic hypertension and gestational hypertension. In my opinion, the much more clinically relevant question concerns women with chronic hypertension, who have a long duration of treatment.
- the choice of high-level neonatal care as part of the composite endpoint. This aspect of the composite outcome drove the endpoint in terms of numbers, but it is unclear to me what its clinical relevance is. In my opinion, it is a poor surrogate for the neonatal outcomes we really care about.
What this evidence means for practice
This study does not establish a foundation for a change in clinical practice. At best, it supports the maternal safety of less-tight control of hypertension in pregnancy. That aspect of the trial may find its way into counseling of the patient.
–George Macones, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The question of degree of control of hypertension during pregnancy has been debated for many years. The primary concern, which is mainly theoretical, is that tight control of hypertension may lead to underperfusion of the uterus, ultimately resulting in fetal growth restriction. This study adds to the available body of literature on this subject.
Details of the trial
In this pragmatic randomized clinical trial, 987 women with office diastolic BP of 90 to 105 mm Hg (or 85 to 105 mm Hg if they were taking a hypertensive medication) between 14 weeks, zero days of gestation and 33 weeks, 6 days of gestation were randomized to tight (n = 488) versus less-tight control of hypertension (n = 493).
Practitioners were encouraged to use labetalol for treatment. The primary outcome was pregnancy loss (miscarriage, ectopic pregnancy, pregnancy termination, stillbirth, or neonatal death) or the need for high-level neonatal care (defined as greater than normal newborn care for more than 48 hours until 28 days of life or discharge home). Secondary outcomes included serious maternal morbidity as late as 6 weeks postpartum. Statistical analysis was based on the intent-to-treat principle.
Adherence to assigned treatment was good, at approximately 75% in each arm. As stated above, the study found no differences in the combined primary endpoint between the two groups. It also found no differences in other perinatal outcomes, including small size for gestational age or other adverse neonatal outcomes. Maternal complications generally were similar as well, with the exception of severe hypertension, which was more common in the less-tight control group.
Strengths and weaknesses of the study
This trial has several important strengths, including its pragmatic design, making it more applicable to everyday practice. Other strengths include rigorous methods and a large sample size.
Two main weaknesses hamper the study, however:
- the inclusion of both chronic hypertension and gestational hypertension. In my opinion, the much more clinically relevant question concerns women with chronic hypertension, who have a long duration of treatment.
- the choice of high-level neonatal care as part of the composite endpoint. This aspect of the composite outcome drove the endpoint in terms of numbers, but it is unclear to me what its clinical relevance is. In my opinion, it is a poor surrogate for the neonatal outcomes we really care about.
What this evidence means for practice
This study does not establish a foundation for a change in clinical practice. At best, it supports the maternal safety of less-tight control of hypertension in pregnancy. That aspect of the trial may find its way into counseling of the patient.
–George Macones, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The question of degree of control of hypertension during pregnancy has been debated for many years. The primary concern, which is mainly theoretical, is that tight control of hypertension may lead to underperfusion of the uterus, ultimately resulting in fetal growth restriction. This study adds to the available body of literature on this subject.
Details of the trial
In this pragmatic randomized clinical trial, 987 women with office diastolic BP of 90 to 105 mm Hg (or 85 to 105 mm Hg if they were taking a hypertensive medication) between 14 weeks, zero days of gestation and 33 weeks, 6 days of gestation were randomized to tight (n = 488) versus less-tight control of hypertension (n = 493).
Practitioners were encouraged to use labetalol for treatment. The primary outcome was pregnancy loss (miscarriage, ectopic pregnancy, pregnancy termination, stillbirth, or neonatal death) or the need for high-level neonatal care (defined as greater than normal newborn care for more than 48 hours until 28 days of life or discharge home). Secondary outcomes included serious maternal morbidity as late as 6 weeks postpartum. Statistical analysis was based on the intent-to-treat principle.
Adherence to assigned treatment was good, at approximately 75% in each arm. As stated above, the study found no differences in the combined primary endpoint between the two groups. It also found no differences in other perinatal outcomes, including small size for gestational age or other adverse neonatal outcomes. Maternal complications generally were similar as well, with the exception of severe hypertension, which was more common in the less-tight control group.
Strengths and weaknesses of the study
This trial has several important strengths, including its pragmatic design, making it more applicable to everyday practice. Other strengths include rigorous methods and a large sample size.
Two main weaknesses hamper the study, however:
- the inclusion of both chronic hypertension and gestational hypertension. In my opinion, the much more clinically relevant question concerns women with chronic hypertension, who have a long duration of treatment.
- the choice of high-level neonatal care as part of the composite endpoint. This aspect of the composite outcome drove the endpoint in terms of numbers, but it is unclear to me what its clinical relevance is. In my opinion, it is a poor surrogate for the neonatal outcomes we really care about.
What this evidence means for practice
This study does not establish a foundation for a change in clinical practice. At best, it supports the maternal safety of less-tight control of hypertension in pregnancy. That aspect of the trial may find its way into counseling of the patient.
–George Macones, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.









