User login
EASL publishes new PBC guidelines
The European Association for the Study of the Liver has published a new guideline for the diagnosis, treatment, and management of primary biliary cholangitis.
PBC is likely in patients with persistent cholestatic symptoms or who have pruritis and fatigue. A diagnosis of PBC can be made if a patient has elevated alkaline phosphatase and antimitochondrial antibody, although elevated antimitochondrial antibody alone is not enough to diagnose PBC. Liver biopsy is not recommended, and liver imaging is not necessary to prove PBC but can be used to eliminate extrahepatic causes of cholestasis.
Pruritis, fatigue, and sicca complex are the most common symptoms of PBC and can significantly effect quality of life. Pruritis can be treated with cholestyramine or rifampicin. Clinicians should seek out and treat associated and alternate causes of fatigue and advise patients on strategies to avoid compounding fatigue problems. Sicca complex should be treated appropriately and, if patients develop refractory symptoms, referred to a specialist.
Complications of liver disease caused by PBC include osteoporosis, fat-soluble vitamin substitution, hyperlipidemia, varices, hepatocellular carcinoma, and need for liver transplant, though the need for liver transplant in PBC patient has decreased over time.
“Treatment guidelines facilitate a holistic life-long approach to the management of patients with PBC, and care pathways should be developed locally to capture the needs of patients. These can be subject to independent quality evaluation,” EASL concluded.
Find the full clinical guideline in the Journal of Hepatology (2017. doi: 10.1016/j.jhep.2017.03.022).
The European Association for the Study of the Liver has published a new guideline for the diagnosis, treatment, and management of primary biliary cholangitis.
PBC is likely in patients with persistent cholestatic symptoms or who have pruritis and fatigue. A diagnosis of PBC can be made if a patient has elevated alkaline phosphatase and antimitochondrial antibody, although elevated antimitochondrial antibody alone is not enough to diagnose PBC. Liver biopsy is not recommended, and liver imaging is not necessary to prove PBC but can be used to eliminate extrahepatic causes of cholestasis.
Pruritis, fatigue, and sicca complex are the most common symptoms of PBC and can significantly effect quality of life. Pruritis can be treated with cholestyramine or rifampicin. Clinicians should seek out and treat associated and alternate causes of fatigue and advise patients on strategies to avoid compounding fatigue problems. Sicca complex should be treated appropriately and, if patients develop refractory symptoms, referred to a specialist.
Complications of liver disease caused by PBC include osteoporosis, fat-soluble vitamin substitution, hyperlipidemia, varices, hepatocellular carcinoma, and need for liver transplant, though the need for liver transplant in PBC patient has decreased over time.
“Treatment guidelines facilitate a holistic life-long approach to the management of patients with PBC, and care pathways should be developed locally to capture the needs of patients. These can be subject to independent quality evaluation,” EASL concluded.
Find the full clinical guideline in the Journal of Hepatology (2017. doi: 10.1016/j.jhep.2017.03.022).
The European Association for the Study of the Liver has published a new guideline for the diagnosis, treatment, and management of primary biliary cholangitis.
PBC is likely in patients with persistent cholestatic symptoms or who have pruritis and fatigue. A diagnosis of PBC can be made if a patient has elevated alkaline phosphatase and antimitochondrial antibody, although elevated antimitochondrial antibody alone is not enough to diagnose PBC. Liver biopsy is not recommended, and liver imaging is not necessary to prove PBC but can be used to eliminate extrahepatic causes of cholestasis.
Pruritis, fatigue, and sicca complex are the most common symptoms of PBC and can significantly effect quality of life. Pruritis can be treated with cholestyramine or rifampicin. Clinicians should seek out and treat associated and alternate causes of fatigue and advise patients on strategies to avoid compounding fatigue problems. Sicca complex should be treated appropriately and, if patients develop refractory symptoms, referred to a specialist.
Complications of liver disease caused by PBC include osteoporosis, fat-soluble vitamin substitution, hyperlipidemia, varices, hepatocellular carcinoma, and need for liver transplant, though the need for liver transplant in PBC patient has decreased over time.
“Treatment guidelines facilitate a holistic life-long approach to the management of patients with PBC, and care pathways should be developed locally to capture the needs of patients. These can be subject to independent quality evaluation,” EASL concluded.
Find the full clinical guideline in the Journal of Hepatology (2017. doi: 10.1016/j.jhep.2017.03.022).
FROM THE JOURNAL OF HEPATOLOGY
For chronic abdominal pain, THC resembled placebo
Seven weeks of treatment with delta-9-atetrahydrocannabinol (THC) did not improve chronic abdominal pain in a placebo-controlled trial of 65 adults.
Treatment “was safe and well tolerated,” but did not significantly reduce pain scores or secondary efficacy outcomes, Marjan de Vries, MSc, and her associates wrote in the July issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2016.09.147). Studies have not clearly shown that THC improves central pain sensitization, a key mechanism in chronic abdominal pain, they noted. Future studies of THC and central sensitization include quantitative sensory testing or electroencephalography, they added.
Source: American Gastroenterological Association
Treatment-refractory chronic abdominal pain is common after abdominal surgery or in chronic pancreatitis, wrote Ms. de Vries of Radboud University Medical Center, Nijmegen, the Netherlands. Affected patients tend to develop central sensitization, or hyper-responsive nociceptive central nervous system pathways. When this happens, pain no longer couples reliably with peripheral stimuli, and therapy targeting central nociceptive pathways is indicated. The main psychoactive compound of Cannabis sativa is THC, which interacts with CB1 receptors in the central nervous system, including in areas of the brain that help regulate emotions, such as the amygdala. Emotion-processing circuits are often overactive in chronic pain, and disrupting them might help modify pain perception, the investigators hypothesized. Therefore, they randomly assigned 65 adults with at least 3 months of abdominal pain related to chronic pancreatitis or abdominal surgery to receive oral placebo or THC tablets three times daily for 50-52 days. The 31 patients in the THC group received step-up dosing (3 mg per dose for 5 days, followed by 5 mg per dose for 5 days) followed by stable dosing at 8 mg. Both groups continued other prescribed analgesics as usual, including oxycontin, fentanyl, morphine, codeine, tramadol, paracetamol, anti-epileptics, and nonsteroidal anti-inflammatories. All but two study participants were white, 25 were male, and 24 were female.
At baseline, all patients reported pain of at least 3 on an 11-point visual analogue scale (VAS). By days 50-52, average VAS scores decreased by 1.6 points (40%) in the THC group and by 1.9 points (37%) in the placebo group (P = .9). Although a strong placebo effect is common in studies of visceral pain, that did not prevent pregabalin from significantly outperforming placebo in another similarly designed randomized clinical trial of patients from this study group with chronic pancreatitis, the investigators noted.
The THC and placebo groups also resembled each other on various secondary outcome measures, including patient global impression of change, pain catastrophizing, pain-related anxiety, measures of depression and generalized anxiety, and subjective impressions of alertness, mood, feeling “high,” drowsiness, and difficulties in controlling thoughts. The only exception was that the THC group showed a trend toward improvement on the Short Form 36, compared with the placebo group (P = .051).
Pharmacokinetic analysis showed good oral absorption of THC. Dizziness, somnolence, and headache were common in both groups, but were more frequent with THC than placebo, as was nausea, dry mouth, and visual impairment. There were no serious treatment-related adverse events, although seven patients stopped THC because they could not tolerate the maximum dose.
Some evidence suggests that the shift from acute to chronic pain entails a transition from nociceptive to cognitive, affective, and autonomic sensitization, the researchers noted. “Therefore, an agent targeting particular brain areas related to the cognitive emotional feature of chronic pain, such as THC, might be efficacious in our chronic pain population, but might be better measured by using affective outcomes of pain,” they concluded.
The trial was supported by a grant from the European Union, the European Fund for Regional Development, and the Province of Gelderland. The THC was provided by Echo Pharmaceuticals, Nijmegen, the Netherlands. The investigators reported having no conflicts of interest.
Seven weeks of treatment with delta-9-atetrahydrocannabinol (THC) did not improve chronic abdominal pain in a placebo-controlled trial of 65 adults.
Treatment “was safe and well tolerated,” but did not significantly reduce pain scores or secondary efficacy outcomes, Marjan de Vries, MSc, and her associates wrote in the July issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2016.09.147). Studies have not clearly shown that THC improves central pain sensitization, a key mechanism in chronic abdominal pain, they noted. Future studies of THC and central sensitization include quantitative sensory testing or electroencephalography, they added.
Source: American Gastroenterological Association
Treatment-refractory chronic abdominal pain is common after abdominal surgery or in chronic pancreatitis, wrote Ms. de Vries of Radboud University Medical Center, Nijmegen, the Netherlands. Affected patients tend to develop central sensitization, or hyper-responsive nociceptive central nervous system pathways. When this happens, pain no longer couples reliably with peripheral stimuli, and therapy targeting central nociceptive pathways is indicated. The main psychoactive compound of Cannabis sativa is THC, which interacts with CB1 receptors in the central nervous system, including in areas of the brain that help regulate emotions, such as the amygdala. Emotion-processing circuits are often overactive in chronic pain, and disrupting them might help modify pain perception, the investigators hypothesized. Therefore, they randomly assigned 65 adults with at least 3 months of abdominal pain related to chronic pancreatitis or abdominal surgery to receive oral placebo or THC tablets three times daily for 50-52 days. The 31 patients in the THC group received step-up dosing (3 mg per dose for 5 days, followed by 5 mg per dose for 5 days) followed by stable dosing at 8 mg. Both groups continued other prescribed analgesics as usual, including oxycontin, fentanyl, morphine, codeine, tramadol, paracetamol, anti-epileptics, and nonsteroidal anti-inflammatories. All but two study participants were white, 25 were male, and 24 were female.
At baseline, all patients reported pain of at least 3 on an 11-point visual analogue scale (VAS). By days 50-52, average VAS scores decreased by 1.6 points (40%) in the THC group and by 1.9 points (37%) in the placebo group (P = .9). Although a strong placebo effect is common in studies of visceral pain, that did not prevent pregabalin from significantly outperforming placebo in another similarly designed randomized clinical trial of patients from this study group with chronic pancreatitis, the investigators noted.
The THC and placebo groups also resembled each other on various secondary outcome measures, including patient global impression of change, pain catastrophizing, pain-related anxiety, measures of depression and generalized anxiety, and subjective impressions of alertness, mood, feeling “high,” drowsiness, and difficulties in controlling thoughts. The only exception was that the THC group showed a trend toward improvement on the Short Form 36, compared with the placebo group (P = .051).
Pharmacokinetic analysis showed good oral absorption of THC. Dizziness, somnolence, and headache were common in both groups, but were more frequent with THC than placebo, as was nausea, dry mouth, and visual impairment. There were no serious treatment-related adverse events, although seven patients stopped THC because they could not tolerate the maximum dose.
Some evidence suggests that the shift from acute to chronic pain entails a transition from nociceptive to cognitive, affective, and autonomic sensitization, the researchers noted. “Therefore, an agent targeting particular brain areas related to the cognitive emotional feature of chronic pain, such as THC, might be efficacious in our chronic pain population, but might be better measured by using affective outcomes of pain,” they concluded.
The trial was supported by a grant from the European Union, the European Fund for Regional Development, and the Province of Gelderland. The THC was provided by Echo Pharmaceuticals, Nijmegen, the Netherlands. The investigators reported having no conflicts of interest.
Seven weeks of treatment with delta-9-atetrahydrocannabinol (THC) did not improve chronic abdominal pain in a placebo-controlled trial of 65 adults.
Treatment “was safe and well tolerated,” but did not significantly reduce pain scores or secondary efficacy outcomes, Marjan de Vries, MSc, and her associates wrote in the July issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2016.09.147). Studies have not clearly shown that THC improves central pain sensitization, a key mechanism in chronic abdominal pain, they noted. Future studies of THC and central sensitization include quantitative sensory testing or electroencephalography, they added.
Source: American Gastroenterological Association
Treatment-refractory chronic abdominal pain is common after abdominal surgery or in chronic pancreatitis, wrote Ms. de Vries of Radboud University Medical Center, Nijmegen, the Netherlands. Affected patients tend to develop central sensitization, or hyper-responsive nociceptive central nervous system pathways. When this happens, pain no longer couples reliably with peripheral stimuli, and therapy targeting central nociceptive pathways is indicated. The main psychoactive compound of Cannabis sativa is THC, which interacts with CB1 receptors in the central nervous system, including in areas of the brain that help regulate emotions, such as the amygdala. Emotion-processing circuits are often overactive in chronic pain, and disrupting them might help modify pain perception, the investigators hypothesized. Therefore, they randomly assigned 65 adults with at least 3 months of abdominal pain related to chronic pancreatitis or abdominal surgery to receive oral placebo or THC tablets three times daily for 50-52 days. The 31 patients in the THC group received step-up dosing (3 mg per dose for 5 days, followed by 5 mg per dose for 5 days) followed by stable dosing at 8 mg. Both groups continued other prescribed analgesics as usual, including oxycontin, fentanyl, morphine, codeine, tramadol, paracetamol, anti-epileptics, and nonsteroidal anti-inflammatories. All but two study participants were white, 25 were male, and 24 were female.
At baseline, all patients reported pain of at least 3 on an 11-point visual analogue scale (VAS). By days 50-52, average VAS scores decreased by 1.6 points (40%) in the THC group and by 1.9 points (37%) in the placebo group (P = .9). Although a strong placebo effect is common in studies of visceral pain, that did not prevent pregabalin from significantly outperforming placebo in another similarly designed randomized clinical trial of patients from this study group with chronic pancreatitis, the investigators noted.
The THC and placebo groups also resembled each other on various secondary outcome measures, including patient global impression of change, pain catastrophizing, pain-related anxiety, measures of depression and generalized anxiety, and subjective impressions of alertness, mood, feeling “high,” drowsiness, and difficulties in controlling thoughts. The only exception was that the THC group showed a trend toward improvement on the Short Form 36, compared with the placebo group (P = .051).
Pharmacokinetic analysis showed good oral absorption of THC. Dizziness, somnolence, and headache were common in both groups, but were more frequent with THC than placebo, as was nausea, dry mouth, and visual impairment. There were no serious treatment-related adverse events, although seven patients stopped THC because they could not tolerate the maximum dose.
Some evidence suggests that the shift from acute to chronic pain entails a transition from nociceptive to cognitive, affective, and autonomic sensitization, the researchers noted. “Therefore, an agent targeting particular brain areas related to the cognitive emotional feature of chronic pain, such as THC, might be efficacious in our chronic pain population, but might be better measured by using affective outcomes of pain,” they concluded.
The trial was supported by a grant from the European Union, the European Fund for Regional Development, and the Province of Gelderland. The THC was provided by Echo Pharmaceuticals, Nijmegen, the Netherlands. The investigators reported having no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Tetrahydrocannabinol did not improve chronic abdominal pain more than did placebo.
Major finding: By days 50-52, average VAS scores decreased by 1.6 points (40%) in the THC group and by 1.9 points (37%) in the placebo group (P = .9).
Data source: A phase II, placebo-controlled study of 65 patients with chronic abdominal pain for at least 3 months who received either placebo or delta-9-atetrahydrocannabinol (THC), 8 mg three times daily.
Disclosures: The trial was supported by a grant from the European Union, the European Fund for Regional Development, and the Province of Gelderland. The THC was provided by Echo Pharmaceuticals, Nijmegen, the Netherlands. The investigators reported having no conflicts of interest.
Sjögren’s syndrome most common extrahepatic PBC manifestation
Extrahepatic manifestations of primary biliary cholangitis (PBC) occur in 73% of patients, with Sjögren’s syndrome, thyroid dysfunction, and systemic sclerosis being the most common, according to a literature review from Sara Chalifoux, MD, and her associates.
Sjögren’s syndrome occurs in 3.5%-73% of PBC patients, usually presenting with dry eyes and oral complications. Sjögren’s treatment in PBC patients involves symptom management associated with exocrine gland infiltration.
Thyroid diseases are present in 5.6%-23.6% of PBC patients. Hashimoto’s thyroiditis is the most common hypothyroidism in PBC patients, presenting with symptoms such as constipation, bradycardia, oligomenorrhea, and inability to concentrate. Grave’s disease is the most common hyperthyroidism, presenting with symptoms such as palpitations, tremulousness, heat intolerance, and weight loss.
Systemic sclerosis occurs in 1.4%-12.3% of PBC patients. Multiple studies found that limited cutaneous systemic sclerosis was more common in PBC patients than was the diffuse form of the disease.
Other diseases that may have a connection to PBC but lack solid, compelling evidence to make a firm association include rheumatoid arthritis, systemic lupus erythematosus, and celiac disease. While many PBC patients have irritable bowel disorder, there is no significant association between the two conditions.
“The patient care team should include practitioners in rheumatology, endocrinology, pulmonology, and cardiology when indicated. Patients should follow up regularly with their primary care physicians. As some of these extrahepatic manifestations can lead to diseases with a poor prognosis, vigilant screening and close follow-up will lead to prompt identification and treatment,” the investigators noted.
The investigators reported no financial conflicts of interest.
Find the full study in Gut and Liver (doi: 10.5009/gnl16365).
Extrahepatic manifestations of primary biliary cholangitis (PBC) occur in 73% of patients, with Sjögren’s syndrome, thyroid dysfunction, and systemic sclerosis being the most common, according to a literature review from Sara Chalifoux, MD, and her associates.
Sjögren’s syndrome occurs in 3.5%-73% of PBC patients, usually presenting with dry eyes and oral complications. Sjögren’s treatment in PBC patients involves symptom management associated with exocrine gland infiltration.
Thyroid diseases are present in 5.6%-23.6% of PBC patients. Hashimoto’s thyroiditis is the most common hypothyroidism in PBC patients, presenting with symptoms such as constipation, bradycardia, oligomenorrhea, and inability to concentrate. Grave’s disease is the most common hyperthyroidism, presenting with symptoms such as palpitations, tremulousness, heat intolerance, and weight loss.
Systemic sclerosis occurs in 1.4%-12.3% of PBC patients. Multiple studies found that limited cutaneous systemic sclerosis was more common in PBC patients than was the diffuse form of the disease.
Other diseases that may have a connection to PBC but lack solid, compelling evidence to make a firm association include rheumatoid arthritis, systemic lupus erythematosus, and celiac disease. While many PBC patients have irritable bowel disorder, there is no significant association between the two conditions.
“The patient care team should include practitioners in rheumatology, endocrinology, pulmonology, and cardiology when indicated. Patients should follow up regularly with their primary care physicians. As some of these extrahepatic manifestations can lead to diseases with a poor prognosis, vigilant screening and close follow-up will lead to prompt identification and treatment,” the investigators noted.
The investigators reported no financial conflicts of interest.
Find the full study in Gut and Liver (doi: 10.5009/gnl16365).
Extrahepatic manifestations of primary biliary cholangitis (PBC) occur in 73% of patients, with Sjögren’s syndrome, thyroid dysfunction, and systemic sclerosis being the most common, according to a literature review from Sara Chalifoux, MD, and her associates.
Sjögren’s syndrome occurs in 3.5%-73% of PBC patients, usually presenting with dry eyes and oral complications. Sjögren’s treatment in PBC patients involves symptom management associated with exocrine gland infiltration.
Thyroid diseases are present in 5.6%-23.6% of PBC patients. Hashimoto’s thyroiditis is the most common hypothyroidism in PBC patients, presenting with symptoms such as constipation, bradycardia, oligomenorrhea, and inability to concentrate. Grave’s disease is the most common hyperthyroidism, presenting with symptoms such as palpitations, tremulousness, heat intolerance, and weight loss.
Systemic sclerosis occurs in 1.4%-12.3% of PBC patients. Multiple studies found that limited cutaneous systemic sclerosis was more common in PBC patients than was the diffuse form of the disease.
Other diseases that may have a connection to PBC but lack solid, compelling evidence to make a firm association include rheumatoid arthritis, systemic lupus erythematosus, and celiac disease. While many PBC patients have irritable bowel disorder, there is no significant association between the two conditions.
“The patient care team should include practitioners in rheumatology, endocrinology, pulmonology, and cardiology when indicated. Patients should follow up regularly with their primary care physicians. As some of these extrahepatic manifestations can lead to diseases with a poor prognosis, vigilant screening and close follow-up will lead to prompt identification and treatment,” the investigators noted.
The investigators reported no financial conflicts of interest.
Find the full study in Gut and Liver (doi: 10.5009/gnl16365).
FROM GUT AND LIVER
AKI doubles risk of death for those with acute pancreatitis
CHICAGO – Acute kidney injury (AKI) doubles the risk of death among patients hospitalized for acute pancreatitis, Kalpit Devani, MD, reported at the annual Digestive Disease Week®.
This severe complication of acute pancreatitis also significantly increases the length of stay and drives up hospital costs, said Dr. Devani of East Tennessee State University, Johnson City. Fortunately, although the risks associated with it remain high, death from AKI in the setting of acute pancreatitis has decreased significantly, from a high of 17% in 2002 to 6.4% in 2012, Dr. Devani determined in his database review.
“Increasing awareness and prompt diagnosis of AKI could be the reason for the increasing trend of prevalence of AKI in acute pancreatitis patients,” he said in an interview. “Decreasing mortality can be related to adherence to recent advances in the management approach of acute pancreatitis, such as early (within 24 hours) and aggressive intravenous hydration and early enteral feeding.”
Dr. Devani examined these trends in data extracted from the National Inpatient Sample, 2002-2012. During that 10-year period, almost 3.5 million adults were hospitalized for acute pancreatitis. These patients were a mean of 53 years old, and half were women. Their mean length of stay was just over 5 days, at a mean cost of about $12,000. Of these, 273,687 (7.9%) also developed AKI.
There were some significant differences between those who did and did not develop AKI. AKI patients were significantly older (61 vs. 53 years), and less likely to be women (43% vs. 51%). They had a higher Charlson Comorbidity Index score (1.49 vs. 0.84). They were also significantly more likely to develop a number of complications, including systemic inflammatory response syndrome (2% vs. 0.4%), septic shock (6% vs. 0.3%), sepsis (8.7% vs. 1.4%), acute respiratory failure (18% vs. 2%), and electrolyte disorder (72% vs. 30%).
Not surprisingly, their length of stay was significantly longer (10 vs. 5 days), as was hospitalization cost ($25,923 vs. $10,889). Mortality was much higher, at almost 9% vs. 0.7%.
In a propensity matching analysis, Dr. Devani matched 53,000 pairs of acute pancreatitis patients with and without AKI. This determined that those with AKI faced a doubling in the risk of in-hospital mortality.
He also examined temporal trends with regard to the complication. The rate of diagnosed AKI in hospitalized acute pancreatitis cases rose dramatically, from 4% in 2002 to 11.6% in 2012. However, mortality in acute pancreatitis patients decreased among both those with AKI (17%-6%) and those without (1%-0.4%).
The mean length of stay in patients with AKI and pancreatitis likewise fell, from 14.8 to 8.6 days. Not surprisingly, total hospitalization cost for these patients fell as well ($42,975-$20,716).
Among pancreatitis patients without AKI, length of stay and costs declined, although not as dramatically as they did among AKI patients (6-5 days; $13,654-$10,895).
Dr. Devani had no financial disclosures.
[email protected]
On Twitter @alz_gal
CHICAGO – Acute kidney injury (AKI) doubles the risk of death among patients hospitalized for acute pancreatitis, Kalpit Devani, MD, reported at the annual Digestive Disease Week®.
This severe complication of acute pancreatitis also significantly increases the length of stay and drives up hospital costs, said Dr. Devani of East Tennessee State University, Johnson City. Fortunately, although the risks associated with it remain high, death from AKI in the setting of acute pancreatitis has decreased significantly, from a high of 17% in 2002 to 6.4% in 2012, Dr. Devani determined in his database review.
“Increasing awareness and prompt diagnosis of AKI could be the reason for the increasing trend of prevalence of AKI in acute pancreatitis patients,” he said in an interview. “Decreasing mortality can be related to adherence to recent advances in the management approach of acute pancreatitis, such as early (within 24 hours) and aggressive intravenous hydration and early enteral feeding.”
Dr. Devani examined these trends in data extracted from the National Inpatient Sample, 2002-2012. During that 10-year period, almost 3.5 million adults were hospitalized for acute pancreatitis. These patients were a mean of 53 years old, and half were women. Their mean length of stay was just over 5 days, at a mean cost of about $12,000. Of these, 273,687 (7.9%) also developed AKI.
There were some significant differences between those who did and did not develop AKI. AKI patients were significantly older (61 vs. 53 years), and less likely to be women (43% vs. 51%). They had a higher Charlson Comorbidity Index score (1.49 vs. 0.84). They were also significantly more likely to develop a number of complications, including systemic inflammatory response syndrome (2% vs. 0.4%), septic shock (6% vs. 0.3%), sepsis (8.7% vs. 1.4%), acute respiratory failure (18% vs. 2%), and electrolyte disorder (72% vs. 30%).
Not surprisingly, their length of stay was significantly longer (10 vs. 5 days), as was hospitalization cost ($25,923 vs. $10,889). Mortality was much higher, at almost 9% vs. 0.7%.
In a propensity matching analysis, Dr. Devani matched 53,000 pairs of acute pancreatitis patients with and without AKI. This determined that those with AKI faced a doubling in the risk of in-hospital mortality.
He also examined temporal trends with regard to the complication. The rate of diagnosed AKI in hospitalized acute pancreatitis cases rose dramatically, from 4% in 2002 to 11.6% in 2012. However, mortality in acute pancreatitis patients decreased among both those with AKI (17%-6%) and those without (1%-0.4%).
The mean length of stay in patients with AKI and pancreatitis likewise fell, from 14.8 to 8.6 days. Not surprisingly, total hospitalization cost for these patients fell as well ($42,975-$20,716).
Among pancreatitis patients without AKI, length of stay and costs declined, although not as dramatically as they did among AKI patients (6-5 days; $13,654-$10,895).
Dr. Devani had no financial disclosures.
[email protected]
On Twitter @alz_gal
CHICAGO – Acute kidney injury (AKI) doubles the risk of death among patients hospitalized for acute pancreatitis, Kalpit Devani, MD, reported at the annual Digestive Disease Week®.
This severe complication of acute pancreatitis also significantly increases the length of stay and drives up hospital costs, said Dr. Devani of East Tennessee State University, Johnson City. Fortunately, although the risks associated with it remain high, death from AKI in the setting of acute pancreatitis has decreased significantly, from a high of 17% in 2002 to 6.4% in 2012, Dr. Devani determined in his database review.
“Increasing awareness and prompt diagnosis of AKI could be the reason for the increasing trend of prevalence of AKI in acute pancreatitis patients,” he said in an interview. “Decreasing mortality can be related to adherence to recent advances in the management approach of acute pancreatitis, such as early (within 24 hours) and aggressive intravenous hydration and early enteral feeding.”
Dr. Devani examined these trends in data extracted from the National Inpatient Sample, 2002-2012. During that 10-year period, almost 3.5 million adults were hospitalized for acute pancreatitis. These patients were a mean of 53 years old, and half were women. Their mean length of stay was just over 5 days, at a mean cost of about $12,000. Of these, 273,687 (7.9%) also developed AKI.
There were some significant differences between those who did and did not develop AKI. AKI patients were significantly older (61 vs. 53 years), and less likely to be women (43% vs. 51%). They had a higher Charlson Comorbidity Index score (1.49 vs. 0.84). They were also significantly more likely to develop a number of complications, including systemic inflammatory response syndrome (2% vs. 0.4%), septic shock (6% vs. 0.3%), sepsis (8.7% vs. 1.4%), acute respiratory failure (18% vs. 2%), and electrolyte disorder (72% vs. 30%).
Not surprisingly, their length of stay was significantly longer (10 vs. 5 days), as was hospitalization cost ($25,923 vs. $10,889). Mortality was much higher, at almost 9% vs. 0.7%.
In a propensity matching analysis, Dr. Devani matched 53,000 pairs of acute pancreatitis patients with and without AKI. This determined that those with AKI faced a doubling in the risk of in-hospital mortality.
He also examined temporal trends with regard to the complication. The rate of diagnosed AKI in hospitalized acute pancreatitis cases rose dramatically, from 4% in 2002 to 11.6% in 2012. However, mortality in acute pancreatitis patients decreased among both those with AKI (17%-6%) and those without (1%-0.4%).
The mean length of stay in patients with AKI and pancreatitis likewise fell, from 14.8 to 8.6 days. Not surprisingly, total hospitalization cost for these patients fell as well ($42,975-$20,716).
Among pancreatitis patients without AKI, length of stay and costs declined, although not as dramatically as they did among AKI patients (6-5 days; $13,654-$10,895).
Dr. Devani had no financial disclosures.
[email protected]
On Twitter @alz_gal
AT DDW
Key clinical point:
Major finding: Mortality among those with AKI was 9% vs. 0.7% among those without. After controlling for confounders, the risk of death was doubled.
Data source: A 10-year National Inpatient Sample database review comprising 3.5 million patients with pancreatitis.
Disclosures: Dr. Devani had no financial disclosures.
Recurrent acute pancreatitis significantly impairs both mental and physical quality of life
CHICAGO – Despite its intermittent and unpredictable nature, recurrent acute pancreatitis exacts a significant toll on patients’ physical and mental quality of life.
It is well-known that patients with chronic pancreatitis suffer physically and emotionally. However, the same understanding has not been engendered for those who experience recurrent acute pancreatitis (RAP), Gregory A. Cote, MD, said at the annual Digestive Disease Week®. Sporadic episodes of acute pancreatitis may cause persistent declines in quality of life.
“RAP clearly leads to a significant reduction in physical and mental quality of life, despite its erratic and sporadic nature,” Dr. Cote said. “Smoking and self-reported disability are very important drivers of these reductions, and a concomitant diagnosis of diabetes exacerbates that even further.”
To explore RAP’s impact on mental and physical quality of life, Dr. Cote examined data from three related cross-sectional North American Pancreatitis Studies (NAPS): the NAPS2, NAPS2-CV (Continuation and Validation), and NAPS2-AS (Ancillary Study).
These studies comprised 2,619 subjects who were enrolled at 27 U.S. sites from 2000 to 2014. Both patients and their physicians completed detailed baseline questionnaires that included personal and family history, risk factors, symptoms, and the 12-Item Short Form Health Survey (SF-12), a detailed quality of life measure.
A score of 50 is the mean for the U.S. general population, and a difference of 3 points or more is considered clinically relevant, Dr. Cote noted.
He parsed the cohort into three groups: those with RAP (508), those with chronic pancreatitis (1,086), and a reference group of healthy controls who were also in the database (1,025).
Some significant between-group differences were immediately obvious, Dr. Cote said. Patients with RAP were significantly younger than both chronic pancreatitis patients (CP) and controls (45 vs. 51 and 49 years, respectively). They also experienced their first bout of acute pancreatitis sooner than CP patients became symptomatic (40 vs. 44 years). Gender was a factor as well: CP patients were more often men (55% vs. 46%).
The pattern of alcohol use between the groups was difficult to interpret, he said. About one-quarter of RAP patients abstained, another fourth were light drinkers, and another fourth moderate drinkers – 12% drank heavily and 7% very heavily. In contrast, frequent drinking was more common among CP patients, with 12% reporting that they drank heavily and 33% very heavily.
CP patients were significantly more likely to be smokers, with 75% reporting current or past tobacco use, compared with 55% of RAP patients. More RAP patients reported never smoking (44% vs. 25%).
RAP patients fell between CP patients and controls in terms of medical comorbidities, including diabetes, renal disease or kidney failure, heart disease, and liver disease.
On the SF-12 physical component section, RAP patients scored a mean of 41 points – significantly worse than controls (51) but significantly better than CP patients (37). The findings were similar for the mental component score: RAP patients scored a mean of 45, compared with 52 in controls and 43 in CP patients.
Dr. Cote performed a multivariate analysis that controlled for age, sex, tobacco and alcohol use, and diabetes. Again, he found that, compared with controls, RAP was associated with significantly reduced scores on both the physical and mental components (mean 8.5 and 6.5 points, respectively).
“The magnitude of reduction was even greater for chronic pancreatitis, with an 11-point reduction on the physical component score and a 7.6-point reduction on the mental component score.
He then sought to identify which clinical characteristics most contributed to this impact on quality of life.
On the physical component score, several were significant, including female sex, which was associated with a 4.4-point decrease; prior pancreatic surgery (–3.3); endocrine insufficiency (–4.6); past smoking (–2.5); current smoking (–3.6); and self-reported physical disability (–9.5).
The mental component score breakdown echoed some of these. Self-reported disability exerted the largest impact, bringing the mental score down by a mean of 5.4 points. Other significant factors were smoking less than a pack a day (–2.5) and smoking more than a pack a day (–4.6). Any suspicion of chronic pancreatitis by the treating physician was associated with a 2.9-point decrease on the score.
“Our findings stress that this is not a disease that can be followed conservatively. We have to investigate interventions that will attenuate it, not only because these patients may go on to develop chronic pancreatitis but because, in their current state, most are experiencing significant reductions in their quality of life.”
Dr Cote had no financial disclosures.
[email protected]
On Twitter @alz_gal
CHICAGO – Despite its intermittent and unpredictable nature, recurrent acute pancreatitis exacts a significant toll on patients’ physical and mental quality of life.
It is well-known that patients with chronic pancreatitis suffer physically and emotionally. However, the same understanding has not been engendered for those who experience recurrent acute pancreatitis (RAP), Gregory A. Cote, MD, said at the annual Digestive Disease Week®. Sporadic episodes of acute pancreatitis may cause persistent declines in quality of life.
“RAP clearly leads to a significant reduction in physical and mental quality of life, despite its erratic and sporadic nature,” Dr. Cote said. “Smoking and self-reported disability are very important drivers of these reductions, and a concomitant diagnosis of diabetes exacerbates that even further.”
To explore RAP’s impact on mental and physical quality of life, Dr. Cote examined data from three related cross-sectional North American Pancreatitis Studies (NAPS): the NAPS2, NAPS2-CV (Continuation and Validation), and NAPS2-AS (Ancillary Study).
These studies comprised 2,619 subjects who were enrolled at 27 U.S. sites from 2000 to 2014. Both patients and their physicians completed detailed baseline questionnaires that included personal and family history, risk factors, symptoms, and the 12-Item Short Form Health Survey (SF-12), a detailed quality of life measure.
A score of 50 is the mean for the U.S. general population, and a difference of 3 points or more is considered clinically relevant, Dr. Cote noted.
He parsed the cohort into three groups: those with RAP (508), those with chronic pancreatitis (1,086), and a reference group of healthy controls who were also in the database (1,025).
Some significant between-group differences were immediately obvious, Dr. Cote said. Patients with RAP were significantly younger than both chronic pancreatitis patients (CP) and controls (45 vs. 51 and 49 years, respectively). They also experienced their first bout of acute pancreatitis sooner than CP patients became symptomatic (40 vs. 44 years). Gender was a factor as well: CP patients were more often men (55% vs. 46%).
The pattern of alcohol use between the groups was difficult to interpret, he said. About one-quarter of RAP patients abstained, another fourth were light drinkers, and another fourth moderate drinkers – 12% drank heavily and 7% very heavily. In contrast, frequent drinking was more common among CP patients, with 12% reporting that they drank heavily and 33% very heavily.
CP patients were significantly more likely to be smokers, with 75% reporting current or past tobacco use, compared with 55% of RAP patients. More RAP patients reported never smoking (44% vs. 25%).
RAP patients fell between CP patients and controls in terms of medical comorbidities, including diabetes, renal disease or kidney failure, heart disease, and liver disease.
On the SF-12 physical component section, RAP patients scored a mean of 41 points – significantly worse than controls (51) but significantly better than CP patients (37). The findings were similar for the mental component score: RAP patients scored a mean of 45, compared with 52 in controls and 43 in CP patients.
Dr. Cote performed a multivariate analysis that controlled for age, sex, tobacco and alcohol use, and diabetes. Again, he found that, compared with controls, RAP was associated with significantly reduced scores on both the physical and mental components (mean 8.5 and 6.5 points, respectively).
“The magnitude of reduction was even greater for chronic pancreatitis, with an 11-point reduction on the physical component score and a 7.6-point reduction on the mental component score.
He then sought to identify which clinical characteristics most contributed to this impact on quality of life.
On the physical component score, several were significant, including female sex, which was associated with a 4.4-point decrease; prior pancreatic surgery (–3.3); endocrine insufficiency (–4.6); past smoking (–2.5); current smoking (–3.6); and self-reported physical disability (–9.5).
The mental component score breakdown echoed some of these. Self-reported disability exerted the largest impact, bringing the mental score down by a mean of 5.4 points. Other significant factors were smoking less than a pack a day (–2.5) and smoking more than a pack a day (–4.6). Any suspicion of chronic pancreatitis by the treating physician was associated with a 2.9-point decrease on the score.
“Our findings stress that this is not a disease that can be followed conservatively. We have to investigate interventions that will attenuate it, not only because these patients may go on to develop chronic pancreatitis but because, in their current state, most are experiencing significant reductions in their quality of life.”
Dr Cote had no financial disclosures.
[email protected]
On Twitter @alz_gal
CHICAGO – Despite its intermittent and unpredictable nature, recurrent acute pancreatitis exacts a significant toll on patients’ physical and mental quality of life.
It is well-known that patients with chronic pancreatitis suffer physically and emotionally. However, the same understanding has not been engendered for those who experience recurrent acute pancreatitis (RAP), Gregory A. Cote, MD, said at the annual Digestive Disease Week®. Sporadic episodes of acute pancreatitis may cause persistent declines in quality of life.
“RAP clearly leads to a significant reduction in physical and mental quality of life, despite its erratic and sporadic nature,” Dr. Cote said. “Smoking and self-reported disability are very important drivers of these reductions, and a concomitant diagnosis of diabetes exacerbates that even further.”
To explore RAP’s impact on mental and physical quality of life, Dr. Cote examined data from three related cross-sectional North American Pancreatitis Studies (NAPS): the NAPS2, NAPS2-CV (Continuation and Validation), and NAPS2-AS (Ancillary Study).
These studies comprised 2,619 subjects who were enrolled at 27 U.S. sites from 2000 to 2014. Both patients and their physicians completed detailed baseline questionnaires that included personal and family history, risk factors, symptoms, and the 12-Item Short Form Health Survey (SF-12), a detailed quality of life measure.
A score of 50 is the mean for the U.S. general population, and a difference of 3 points or more is considered clinically relevant, Dr. Cote noted.
He parsed the cohort into three groups: those with RAP (508), those with chronic pancreatitis (1,086), and a reference group of healthy controls who were also in the database (1,025).
Some significant between-group differences were immediately obvious, Dr. Cote said. Patients with RAP were significantly younger than both chronic pancreatitis patients (CP) and controls (45 vs. 51 and 49 years, respectively). They also experienced their first bout of acute pancreatitis sooner than CP patients became symptomatic (40 vs. 44 years). Gender was a factor as well: CP patients were more often men (55% vs. 46%).
The pattern of alcohol use between the groups was difficult to interpret, he said. About one-quarter of RAP patients abstained, another fourth were light drinkers, and another fourth moderate drinkers – 12% drank heavily and 7% very heavily. In contrast, frequent drinking was more common among CP patients, with 12% reporting that they drank heavily and 33% very heavily.
CP patients were significantly more likely to be smokers, with 75% reporting current or past tobacco use, compared with 55% of RAP patients. More RAP patients reported never smoking (44% vs. 25%).
RAP patients fell between CP patients and controls in terms of medical comorbidities, including diabetes, renal disease or kidney failure, heart disease, and liver disease.
On the SF-12 physical component section, RAP patients scored a mean of 41 points – significantly worse than controls (51) but significantly better than CP patients (37). The findings were similar for the mental component score: RAP patients scored a mean of 45, compared with 52 in controls and 43 in CP patients.
Dr. Cote performed a multivariate analysis that controlled for age, sex, tobacco and alcohol use, and diabetes. Again, he found that, compared with controls, RAP was associated with significantly reduced scores on both the physical and mental components (mean 8.5 and 6.5 points, respectively).
“The magnitude of reduction was even greater for chronic pancreatitis, with an 11-point reduction on the physical component score and a 7.6-point reduction on the mental component score.
He then sought to identify which clinical characteristics most contributed to this impact on quality of life.
On the physical component score, several were significant, including female sex, which was associated with a 4.4-point decrease; prior pancreatic surgery (–3.3); endocrine insufficiency (–4.6); past smoking (–2.5); current smoking (–3.6); and self-reported physical disability (–9.5).
The mental component score breakdown echoed some of these. Self-reported disability exerted the largest impact, bringing the mental score down by a mean of 5.4 points. Other significant factors were smoking less than a pack a day (–2.5) and smoking more than a pack a day (–4.6). Any suspicion of chronic pancreatitis by the treating physician was associated with a 2.9-point decrease on the score.
“Our findings stress that this is not a disease that can be followed conservatively. We have to investigate interventions that will attenuate it, not only because these patients may go on to develop chronic pancreatitis but because, in their current state, most are experiencing significant reductions in their quality of life.”
Dr Cote had no financial disclosures.
[email protected]
On Twitter @alz_gal
AT DDW
Key clinical point:
Major finding: On a physical QOL scale, patients scored a mean of 41 points – 10 points lower than controls. The mental QOL score was 7 points lower.
Data source: The database review comprised 2,619 subjects.
Disclosures: Dr. Cote had no financial disclosures.
Half of newly detected antimicrobial antibodies do not lead to PBC
Nearly half of newly detected antimitochondrial antibodies (AMAs) in clinical practice do not lead to a diagnosis of primary biliary cholangitis (PBC), according to a prospective study.
Geraldine Dahlqvist, MD, and her associates examined 720 patients whose AMA tests were registered during a 1-year census period. They were divided into groups according to whether they were newly diagnosed (275), were previously diagnosed (216), or had a nonestablished diagnosis (229) of PBC. Results showed the prevalence of AMA-positive patients without evidence of PBC was 16.1 per 100,000 inhabitants. It was four (all AMA-positive patients) to six (PBC patients) times higher in women than in men. The median age was 58 years, with the median AMA titer at 1:16. Normal serum alkaline phosphatases (ALP) were 74%, and were 1.5 times above the upper limit of normal in 13% of patients, while cirrhosis was found in 6%. Among the patients with normal ALP and no evidence of cirrhosis, the 5-year incidence rate of PBC was 16%.
It was noted that no patients died officially from PBC in this study. The 1-, 3-, and 5-year rates of survival were 95%, 90%, and 75% (95% CI, 63-87), respectively, compared with 90% in the control group.
“The younger age and lower autoantibody titer of these patients, together with the frequent mild abnormalities of their biochemical liver tests, supports a very early, presymptomatic precholestatic stage of the disease,” Dr. Dahlqvist, of Catholic University of Louvain (Belgium), and her colleagues noted. “The incidence of clinical manifestations of PBC seems, however, much lower than previously reported.”
Find the full story in Hepatology (doi: 10.1002/hep.28559).
Nearly half of newly detected antimitochondrial antibodies (AMAs) in clinical practice do not lead to a diagnosis of primary biliary cholangitis (PBC), according to a prospective study.
Geraldine Dahlqvist, MD, and her associates examined 720 patients whose AMA tests were registered during a 1-year census period. They were divided into groups according to whether they were newly diagnosed (275), were previously diagnosed (216), or had a nonestablished diagnosis (229) of PBC. Results showed the prevalence of AMA-positive patients without evidence of PBC was 16.1 per 100,000 inhabitants. It was four (all AMA-positive patients) to six (PBC patients) times higher in women than in men. The median age was 58 years, with the median AMA titer at 1:16. Normal serum alkaline phosphatases (ALP) were 74%, and were 1.5 times above the upper limit of normal in 13% of patients, while cirrhosis was found in 6%. Among the patients with normal ALP and no evidence of cirrhosis, the 5-year incidence rate of PBC was 16%.
It was noted that no patients died officially from PBC in this study. The 1-, 3-, and 5-year rates of survival were 95%, 90%, and 75% (95% CI, 63-87), respectively, compared with 90% in the control group.
“The younger age and lower autoantibody titer of these patients, together with the frequent mild abnormalities of their biochemical liver tests, supports a very early, presymptomatic precholestatic stage of the disease,” Dr. Dahlqvist, of Catholic University of Louvain (Belgium), and her colleagues noted. “The incidence of clinical manifestations of PBC seems, however, much lower than previously reported.”
Find the full story in Hepatology (doi: 10.1002/hep.28559).
Nearly half of newly detected antimitochondrial antibodies (AMAs) in clinical practice do not lead to a diagnosis of primary biliary cholangitis (PBC), according to a prospective study.
Geraldine Dahlqvist, MD, and her associates examined 720 patients whose AMA tests were registered during a 1-year census period. They were divided into groups according to whether they were newly diagnosed (275), were previously diagnosed (216), or had a nonestablished diagnosis (229) of PBC. Results showed the prevalence of AMA-positive patients without evidence of PBC was 16.1 per 100,000 inhabitants. It was four (all AMA-positive patients) to six (PBC patients) times higher in women than in men. The median age was 58 years, with the median AMA titer at 1:16. Normal serum alkaline phosphatases (ALP) were 74%, and were 1.5 times above the upper limit of normal in 13% of patients, while cirrhosis was found in 6%. Among the patients with normal ALP and no evidence of cirrhosis, the 5-year incidence rate of PBC was 16%.
It was noted that no patients died officially from PBC in this study. The 1-, 3-, and 5-year rates of survival were 95%, 90%, and 75% (95% CI, 63-87), respectively, compared with 90% in the control group.
“The younger age and lower autoantibody titer of these patients, together with the frequent mild abnormalities of their biochemical liver tests, supports a very early, presymptomatic precholestatic stage of the disease,” Dr. Dahlqvist, of Catholic University of Louvain (Belgium), and her colleagues noted. “The incidence of clinical manifestations of PBC seems, however, much lower than previously reported.”
Find the full story in Hepatology (doi: 10.1002/hep.28559).
FROM HEPATOLOGY
Mild, moderate hypertriglyceridemia raises pancreatitis risk
Mild to moderate hypertriglyceridemia, not just severe hypertriglyceridemia, is associated with increased risk of acute pancreatitis, according to a report published in JAMA Internal Medicine.
Severe hypertriglyceridemia is a recognized risk factor for acute pancreatitis, but “there is no consensus on a clear threshold above which triglycerides” raise that risk. The American College of Gastroenterology and The Endocrine Society state that levels over 1,000 mg/dL should be considered a risk factor, while the European Society of Cardiology and the European Atherosclerosis Society set the cutoff at 885 mg/dL, said Simon B. Pedersen, MD, of the department of clinical biochemistry, Herlev and Gentofte Hospital, Copenhagen University, Denmark, and his associates.
To examine whether lower triglyceride levels also put patients at risk for acute pancreatitis, the investigators analyzed data from two large prospective longitudinal studies of the general Danish population. They included 116,550 consecutive men and women who provided nonfasting triglyceride measurements and were followed for a median of 6.7 years. During that time, 434 of these participants developed acute pancreatitis.
The risk of developing acute pancreatitis increased with increasing triglyceride levels starting at the mildly elevated level of only 177 mg/dL. Compared with normal triglyceride levels of less than 89 mg/dL, the risk increased with a hazard ratio (HR) of 1.6 at 89-176 mg/dL, an HR of 2.3 at 177-265 mg/dL, an HR of 2.9 at 266-353 mg/dL, an HR of 3.9 at 354-442 mg/dL, and an HR of 8.7 at 443 mg/dL or above, Dr. Pedersen and his associates said (JAMA Intern. Med. 2016;176:1834-42).
This linear association persisted after the data were adjusted to account for potential confounders such as patient age, sex, body mass index, smoking status, alcohol intake, and education level, as well as the presence or absence of hypertension, diabetes, alcohol use, gallstone disease, and statin therapy.
This study was supported by the Herlev and Gentofte Hospital and Copenhagen University Hospital. Dr. Pedersen reported having no relevant financial disclosures; one of his associates reported ties to AstraZeneca, Merck, Omthera, Ionis, and Kowa.
Mild to moderate hypertriglyceridemia, not just severe hypertriglyceridemia, is associated with increased risk of acute pancreatitis, according to a report published in JAMA Internal Medicine.
Severe hypertriglyceridemia is a recognized risk factor for acute pancreatitis, but “there is no consensus on a clear threshold above which triglycerides” raise that risk. The American College of Gastroenterology and The Endocrine Society state that levels over 1,000 mg/dL should be considered a risk factor, while the European Society of Cardiology and the European Atherosclerosis Society set the cutoff at 885 mg/dL, said Simon B. Pedersen, MD, of the department of clinical biochemistry, Herlev and Gentofte Hospital, Copenhagen University, Denmark, and his associates.
To examine whether lower triglyceride levels also put patients at risk for acute pancreatitis, the investigators analyzed data from two large prospective longitudinal studies of the general Danish population. They included 116,550 consecutive men and women who provided nonfasting triglyceride measurements and were followed for a median of 6.7 years. During that time, 434 of these participants developed acute pancreatitis.
The risk of developing acute pancreatitis increased with increasing triglyceride levels starting at the mildly elevated level of only 177 mg/dL. Compared with normal triglyceride levels of less than 89 mg/dL, the risk increased with a hazard ratio (HR) of 1.6 at 89-176 mg/dL, an HR of 2.3 at 177-265 mg/dL, an HR of 2.9 at 266-353 mg/dL, an HR of 3.9 at 354-442 mg/dL, and an HR of 8.7 at 443 mg/dL or above, Dr. Pedersen and his associates said (JAMA Intern. Med. 2016;176:1834-42).
This linear association persisted after the data were adjusted to account for potential confounders such as patient age, sex, body mass index, smoking status, alcohol intake, and education level, as well as the presence or absence of hypertension, diabetes, alcohol use, gallstone disease, and statin therapy.
This study was supported by the Herlev and Gentofte Hospital and Copenhagen University Hospital. Dr. Pedersen reported having no relevant financial disclosures; one of his associates reported ties to AstraZeneca, Merck, Omthera, Ionis, and Kowa.
Mild to moderate hypertriglyceridemia, not just severe hypertriglyceridemia, is associated with increased risk of acute pancreatitis, according to a report published in JAMA Internal Medicine.
Severe hypertriglyceridemia is a recognized risk factor for acute pancreatitis, but “there is no consensus on a clear threshold above which triglycerides” raise that risk. The American College of Gastroenterology and The Endocrine Society state that levels over 1,000 mg/dL should be considered a risk factor, while the European Society of Cardiology and the European Atherosclerosis Society set the cutoff at 885 mg/dL, said Simon B. Pedersen, MD, of the department of clinical biochemistry, Herlev and Gentofte Hospital, Copenhagen University, Denmark, and his associates.
To examine whether lower triglyceride levels also put patients at risk for acute pancreatitis, the investigators analyzed data from two large prospective longitudinal studies of the general Danish population. They included 116,550 consecutive men and women who provided nonfasting triglyceride measurements and were followed for a median of 6.7 years. During that time, 434 of these participants developed acute pancreatitis.
The risk of developing acute pancreatitis increased with increasing triglyceride levels starting at the mildly elevated level of only 177 mg/dL. Compared with normal triglyceride levels of less than 89 mg/dL, the risk increased with a hazard ratio (HR) of 1.6 at 89-176 mg/dL, an HR of 2.3 at 177-265 mg/dL, an HR of 2.9 at 266-353 mg/dL, an HR of 3.9 at 354-442 mg/dL, and an HR of 8.7 at 443 mg/dL or above, Dr. Pedersen and his associates said (JAMA Intern. Med. 2016;176:1834-42).
This linear association persisted after the data were adjusted to account for potential confounders such as patient age, sex, body mass index, smoking status, alcohol intake, and education level, as well as the presence or absence of hypertension, diabetes, alcohol use, gallstone disease, and statin therapy.
This study was supported by the Herlev and Gentofte Hospital and Copenhagen University Hospital. Dr. Pedersen reported having no relevant financial disclosures; one of his associates reported ties to AstraZeneca, Merck, Omthera, Ionis, and Kowa.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Mild to moderate hypertriglyceridemia is associated with increased risk of acute pancreatitis.
Major finding: Compared with normal triglyceride levels of less than 89 mg/dL, the risk for acute pancreatitis increased with a hazard ratio (HR) of 1.6 at 89-176 mg/dL, an HR of 2.3 at 177-265 mg/dL, an HR of 2.9 at 266-353 mg/dL, an HR of 3.9 at 354-442 mg/dL, and an HR of 8.7 at 443 mg/dL or above.
Data source: A prospective, longitudinal cohort study involving 116,550 adults followed for 6.7 years.
Disclosures: This study was supported by the Herlev and Gentofte Hospital and Copenhagen University Hospital. Dr. Pedersen reported having no relevant financial disclosures; one of his associates reported ties to AstraZeneca, Merck, Omthera, Ionis, and Kowa.
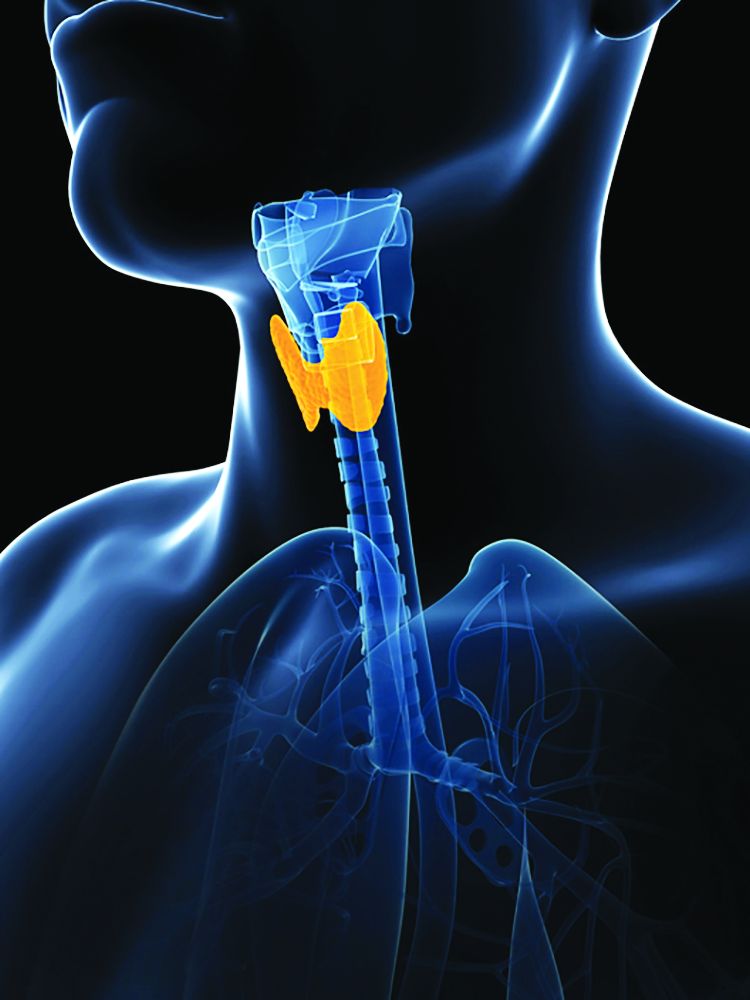
Thyroid disease does not affect primary biliary cholangitis complications
While associations are known to exist between primary biliary cholangitis (PBC) and many different types of thyroid disease (TD), a new study shows that the mere presence of thyroid disease does not have any bearing on the hepatic complications or progression of PBC.
“The prevalence of TD in PBC reportedly ranges between 7.24% and 14.4%, the most often encountered thyroid dysfunction being Hashimoto’s thyroiditis,” wrote the study’s authors, led by Annarosa Floreani, MD, of the University of Padua (Italy).
Of the 921 total patients enrolled, 150 (16.3%) had TD. The most common TD patients had were Hashimoto’s thyroiditis, which 94 (10.2%) individuals had; Graves’ disease, found in 15 (1.6%) patients; multinodular goiter, which 22 (2.4%) patients had; thyroid cancer, which was found in 7 (0.8%); and “other thyroid conditions,” which affected 12 (1.3%) patients. Patients from Padua had significantly more Graves’ disease and thyroid cancer than those from Barcelona: 11 (15.7%) versus 4 (5.0%) for Graves’ (P = .03), and 6 (8.6%) versus 1 (1.3%) for thyroid cancer (P = .03), respectively. However, no significant differences were found in PBC patients who had TD and those who did not, when it came to comparing the histologic stages at which they were diagnosed with PBC, hepatic decompensation events, occurrence of hepatocellular carcinoma, or liver transplantation rate. Furthermore, TD was not found to affect PBC survival rates, either positively or negatively.
“The results of our study confirm that TDs are often associated with PBC, especially Hashimoto’s thyroiditis, which shares an autoimmune etiology with PBC,” the authors concluded, adding that “More importantly … the clinical characteristics and natural history of PBC were much the same in the two cohorts, as demonstrated by the absence of significant differences regarding histological stage at diagnosis (the only exception being more patients in stage III in the Italian cohort); biochemical data; response to UDCA [ursodeoxycholic acid]; the association with other extrahepatic autoimmune disorders; the occurrence of clinical events; and survival.”
No funding source was reported for this study. Dr. Floreani and her coauthors did not report any financial disclosures relevant to this study.
While associations are known to exist between primary biliary cholangitis (PBC) and many different types of thyroid disease (TD), a new study shows that the mere presence of thyroid disease does not have any bearing on the hepatic complications or progression of PBC.
“The prevalence of TD in PBC reportedly ranges between 7.24% and 14.4%, the most often encountered thyroid dysfunction being Hashimoto’s thyroiditis,” wrote the study’s authors, led by Annarosa Floreani, MD, of the University of Padua (Italy).
Of the 921 total patients enrolled, 150 (16.3%) had TD. The most common TD patients had were Hashimoto’s thyroiditis, which 94 (10.2%) individuals had; Graves’ disease, found in 15 (1.6%) patients; multinodular goiter, which 22 (2.4%) patients had; thyroid cancer, which was found in 7 (0.8%); and “other thyroid conditions,” which affected 12 (1.3%) patients. Patients from Padua had significantly more Graves’ disease and thyroid cancer than those from Barcelona: 11 (15.7%) versus 4 (5.0%) for Graves’ (P = .03), and 6 (8.6%) versus 1 (1.3%) for thyroid cancer (P = .03), respectively. However, no significant differences were found in PBC patients who had TD and those who did not, when it came to comparing the histologic stages at which they were diagnosed with PBC, hepatic decompensation events, occurrence of hepatocellular carcinoma, or liver transplantation rate. Furthermore, TD was not found to affect PBC survival rates, either positively or negatively.
“The results of our study confirm that TDs are often associated with PBC, especially Hashimoto’s thyroiditis, which shares an autoimmune etiology with PBC,” the authors concluded, adding that “More importantly … the clinical characteristics and natural history of PBC were much the same in the two cohorts, as demonstrated by the absence of significant differences regarding histological stage at diagnosis (the only exception being more patients in stage III in the Italian cohort); biochemical data; response to UDCA [ursodeoxycholic acid]; the association with other extrahepatic autoimmune disorders; the occurrence of clinical events; and survival.”
No funding source was reported for this study. Dr. Floreani and her coauthors did not report any financial disclosures relevant to this study.
While associations are known to exist between primary biliary cholangitis (PBC) and many different types of thyroid disease (TD), a new study shows that the mere presence of thyroid disease does not have any bearing on the hepatic complications or progression of PBC.
“The prevalence of TD in PBC reportedly ranges between 7.24% and 14.4%, the most often encountered thyroid dysfunction being Hashimoto’s thyroiditis,” wrote the study’s authors, led by Annarosa Floreani, MD, of the University of Padua (Italy).
Of the 921 total patients enrolled, 150 (16.3%) had TD. The most common TD patients had were Hashimoto’s thyroiditis, which 94 (10.2%) individuals had; Graves’ disease, found in 15 (1.6%) patients; multinodular goiter, which 22 (2.4%) patients had; thyroid cancer, which was found in 7 (0.8%); and “other thyroid conditions,” which affected 12 (1.3%) patients. Patients from Padua had significantly more Graves’ disease and thyroid cancer than those from Barcelona: 11 (15.7%) versus 4 (5.0%) for Graves’ (P = .03), and 6 (8.6%) versus 1 (1.3%) for thyroid cancer (P = .03), respectively. However, no significant differences were found in PBC patients who had TD and those who did not, when it came to comparing the histologic stages at which they were diagnosed with PBC, hepatic decompensation events, occurrence of hepatocellular carcinoma, or liver transplantation rate. Furthermore, TD was not found to affect PBC survival rates, either positively or negatively.
“The results of our study confirm that TDs are often associated with PBC, especially Hashimoto’s thyroiditis, which shares an autoimmune etiology with PBC,” the authors concluded, adding that “More importantly … the clinical characteristics and natural history of PBC were much the same in the two cohorts, as demonstrated by the absence of significant differences regarding histological stage at diagnosis (the only exception being more patients in stage III in the Italian cohort); biochemical data; response to UDCA [ursodeoxycholic acid]; the association with other extrahepatic autoimmune disorders; the occurrence of clinical events; and survival.”
No funding source was reported for this study. Dr. Floreani and her coauthors did not report any financial disclosures relevant to this study.
Key clinical point:
Major finding: 150 of 921 PBC patients had TD (16.3%), but there was no correlation between PBC patients who had TD and their histologic stage either at diagnosis, hepatic decompensation events, occurrence of hepatocelluler carcinoma, or liver transplantation rates.
Data source: Prospective study of 921 PBC patients in Padua and Barcelona from 1975 to 2015.
Disclosures: No funding source was disclosed; authors reported no relevant financial disclosures.
PBC patients show brain abnormalities before cirrhosis occurs
Brain abnormalities associated with primary biliary cholangitis (PBC) can be observed via magnetic resonance imaging before significant liver damage occurs, according to V.B.P. Grover, MD, and associates at the Liver Unit and Robert Steiner MRI Unit, MRC Clinical Sciences Centre, Imperial College London.
In a study of 13 newly diagnosed precirrhotic PBC patients and 17 healthy volunteers, mean magnetization transfer ratios (MTR) were lower in the thalamus, putamen, and head of caudate in PBC patients, compared with the control group, with the greatest difference seen in the thalamus. Severity of PBC symptoms did not have any significant effect on MTR.
An increase in the apparent diffusion coefficient was seen in the thalamus of PBC patients; however, no significant difference in cerebral metabolite ratios or pallidal index was observed. No correlation between neuroimaging data, lab data, symptom severity scores, or age was observed.
“Larger scale, and in particular linear studies, will be needed to explore the relationship of this change to symptoms and its response to therapies such as UDCA [ursodeoxycholic acid] and OCA [obeticholic acid]. The presence of brain change so early in the disease process would, however, suggest that the current step-up approach to therapy in which treatment change follows failure of a therapy type may allow the progressive accumulation of brain injury whilst waiting for adequate therapeutic response,” the investigators concluded.
Find the full study in Alimentary Pharmacology & Therapeutics (doi: 10.1111/apt.13797).
Brain abnormalities associated with primary biliary cholangitis (PBC) can be observed via magnetic resonance imaging before significant liver damage occurs, according to V.B.P. Grover, MD, and associates at the Liver Unit and Robert Steiner MRI Unit, MRC Clinical Sciences Centre, Imperial College London.
In a study of 13 newly diagnosed precirrhotic PBC patients and 17 healthy volunteers, mean magnetization transfer ratios (MTR) were lower in the thalamus, putamen, and head of caudate in PBC patients, compared with the control group, with the greatest difference seen in the thalamus. Severity of PBC symptoms did not have any significant effect on MTR.
An increase in the apparent diffusion coefficient was seen in the thalamus of PBC patients; however, no significant difference in cerebral metabolite ratios or pallidal index was observed. No correlation between neuroimaging data, lab data, symptom severity scores, or age was observed.
“Larger scale, and in particular linear studies, will be needed to explore the relationship of this change to symptoms and its response to therapies such as UDCA [ursodeoxycholic acid] and OCA [obeticholic acid]. The presence of brain change so early in the disease process would, however, suggest that the current step-up approach to therapy in which treatment change follows failure of a therapy type may allow the progressive accumulation of brain injury whilst waiting for adequate therapeutic response,” the investigators concluded.
Find the full study in Alimentary Pharmacology & Therapeutics (doi: 10.1111/apt.13797).
Brain abnormalities associated with primary biliary cholangitis (PBC) can be observed via magnetic resonance imaging before significant liver damage occurs, according to V.B.P. Grover, MD, and associates at the Liver Unit and Robert Steiner MRI Unit, MRC Clinical Sciences Centre, Imperial College London.
In a study of 13 newly diagnosed precirrhotic PBC patients and 17 healthy volunteers, mean magnetization transfer ratios (MTR) were lower in the thalamus, putamen, and head of caudate in PBC patients, compared with the control group, with the greatest difference seen in the thalamus. Severity of PBC symptoms did not have any significant effect on MTR.
An increase in the apparent diffusion coefficient was seen in the thalamus of PBC patients; however, no significant difference in cerebral metabolite ratios or pallidal index was observed. No correlation between neuroimaging data, lab data, symptom severity scores, or age was observed.
“Larger scale, and in particular linear studies, will be needed to explore the relationship of this change to symptoms and its response to therapies such as UDCA [ursodeoxycholic acid] and OCA [obeticholic acid]. The presence of brain change so early in the disease process would, however, suggest that the current step-up approach to therapy in which treatment change follows failure of a therapy type may allow the progressive accumulation of brain injury whilst waiting for adequate therapeutic response,” the investigators concluded.
Find the full study in Alimentary Pharmacology & Therapeutics (doi: 10.1111/apt.13797).
FROM ALIMENTARY PHARMACOLOGY & THERAPEUTICS
Causes of recurrent pediatric pancreatitis start to emerge
MONTREAL – Once children have a first bout of acute pancreatitis, a second, separate episode of acute pancreatitis most often occurs in patients with genetically triggered pancreatitis, those who are taller or weigh more than average, and patients with pancreatic necrosis, based on multicenter, prospective data collected from 83 patients.
This is the first reported study to prospectively follow pediatric cases of acute pancreatitis, and additional studies with more patients are needed to better identify the factors predisposing patients to recurrent episodes of acute pancreatitis and to quantify the amount of risk these factors pose, Katherine F. Sweeny, MD, said at the annual meeting of the Federation of the International Societies of Pediatric Gastroenterology, Hepatology, and Nutrition.
The analysis focused on the 83 patients with at least 3 months of follow-up. During observation, 17 (20%) of the patients developed a second episode of acute pancreatitis that was distinguished from the initial episode by either at least 1 pain-free month or by complete normalization of amylase and lipase levels between the two episodes. Thirteen of the 17 recurrences occurred within 5 months of the first episode, with 11 of these occurring within the first 3 months after the first attack, a subgroup Dr. Sweeny called the “rapid progressors.”
Comparison of the 11 rapid progressors with the other 72 patients showed that the rapid progressors were significantly taller and weighed more. In addition, two of the 11 rapid progressors had pancreatic necrosis while none of the other patients had this complication.
The pancreatitis etiologies of the 11 rapid progressors also highlighted the potent influence a mutation can have on producing recurrent acute pancreatitis. Four of the 11 rapid progressors had a genetic mutation linked to pancreatitis susceptibility, and five of the six patients with a genetic cause for their index episode of pancreatitis developed a second acute episode during follow-up, said Dr. Sweeny, a pediatrician at Cincinnati Children’s Hospital Medical Center. In contrast, the next most effective cause of recurrent pancreatitis was a toxin or drug, which resulted in about a 25% incidence rate of a second episode. All of the other pancreatitis etiologies had recurrence rates of 10% or less.
Collecting better information on the causes of recurrent pancreatitis and chronic pancreatitis is especially important because of the rising incidence of acute pediatric pancreatitis, currently about one case in every 10,000 children and adolescents. Prior to formation of the INSPPIRE consortium, studies of pediatric pancreatitis had largely been limited to single-center retrospective reviews. The limitations of these data have made it hard to predict which patients with a first episode of acute pancreatitis will progress to a second episode or beyond, Dr. Sweeny said.
Dr. Sweeny had no disclosures.
[email protected]
On Twitter @mitchelzoler
MONTREAL – Once children have a first bout of acute pancreatitis, a second, separate episode of acute pancreatitis most often occurs in patients with genetically triggered pancreatitis, those who are taller or weigh more than average, and patients with pancreatic necrosis, based on multicenter, prospective data collected from 83 patients.
This is the first reported study to prospectively follow pediatric cases of acute pancreatitis, and additional studies with more patients are needed to better identify the factors predisposing patients to recurrent episodes of acute pancreatitis and to quantify the amount of risk these factors pose, Katherine F. Sweeny, MD, said at the annual meeting of the Federation of the International Societies of Pediatric Gastroenterology, Hepatology, and Nutrition.
The analysis focused on the 83 patients with at least 3 months of follow-up. During observation, 17 (20%) of the patients developed a second episode of acute pancreatitis that was distinguished from the initial episode by either at least 1 pain-free month or by complete normalization of amylase and lipase levels between the two episodes. Thirteen of the 17 recurrences occurred within 5 months of the first episode, with 11 of these occurring within the first 3 months after the first attack, a subgroup Dr. Sweeny called the “rapid progressors.”
Comparison of the 11 rapid progressors with the other 72 patients showed that the rapid progressors were significantly taller and weighed more. In addition, two of the 11 rapid progressors had pancreatic necrosis while none of the other patients had this complication.
The pancreatitis etiologies of the 11 rapid progressors also highlighted the potent influence a mutation can have on producing recurrent acute pancreatitis. Four of the 11 rapid progressors had a genetic mutation linked to pancreatitis susceptibility, and five of the six patients with a genetic cause for their index episode of pancreatitis developed a second acute episode during follow-up, said Dr. Sweeny, a pediatrician at Cincinnati Children’s Hospital Medical Center. In contrast, the next most effective cause of recurrent pancreatitis was a toxin or drug, which resulted in about a 25% incidence rate of a second episode. All of the other pancreatitis etiologies had recurrence rates of 10% or less.
Collecting better information on the causes of recurrent pancreatitis and chronic pancreatitis is especially important because of the rising incidence of acute pediatric pancreatitis, currently about one case in every 10,000 children and adolescents. Prior to formation of the INSPPIRE consortium, studies of pediatric pancreatitis had largely been limited to single-center retrospective reviews. The limitations of these data have made it hard to predict which patients with a first episode of acute pancreatitis will progress to a second episode or beyond, Dr. Sweeny said.
Dr. Sweeny had no disclosures.
[email protected]
On Twitter @mitchelzoler
MONTREAL – Once children have a first bout of acute pancreatitis, a second, separate episode of acute pancreatitis most often occurs in patients with genetically triggered pancreatitis, those who are taller or weigh more than average, and patients with pancreatic necrosis, based on multicenter, prospective data collected from 83 patients.
This is the first reported study to prospectively follow pediatric cases of acute pancreatitis, and additional studies with more patients are needed to better identify the factors predisposing patients to recurrent episodes of acute pancreatitis and to quantify the amount of risk these factors pose, Katherine F. Sweeny, MD, said at the annual meeting of the Federation of the International Societies of Pediatric Gastroenterology, Hepatology, and Nutrition.
The analysis focused on the 83 patients with at least 3 months of follow-up. During observation, 17 (20%) of the patients developed a second episode of acute pancreatitis that was distinguished from the initial episode by either at least 1 pain-free month or by complete normalization of amylase and lipase levels between the two episodes. Thirteen of the 17 recurrences occurred within 5 months of the first episode, with 11 of these occurring within the first 3 months after the first attack, a subgroup Dr. Sweeny called the “rapid progressors.”
Comparison of the 11 rapid progressors with the other 72 patients showed that the rapid progressors were significantly taller and weighed more. In addition, two of the 11 rapid progressors had pancreatic necrosis while none of the other patients had this complication.
The pancreatitis etiologies of the 11 rapid progressors also highlighted the potent influence a mutation can have on producing recurrent acute pancreatitis. Four of the 11 rapid progressors had a genetic mutation linked to pancreatitis susceptibility, and five of the six patients with a genetic cause for their index episode of pancreatitis developed a second acute episode during follow-up, said Dr. Sweeny, a pediatrician at Cincinnati Children’s Hospital Medical Center. In contrast, the next most effective cause of recurrent pancreatitis was a toxin or drug, which resulted in about a 25% incidence rate of a second episode. All of the other pancreatitis etiologies had recurrence rates of 10% or less.
Collecting better information on the causes of recurrent pancreatitis and chronic pancreatitis is especially important because of the rising incidence of acute pediatric pancreatitis, currently about one case in every 10,000 children and adolescents. Prior to formation of the INSPPIRE consortium, studies of pediatric pancreatitis had largely been limited to single-center retrospective reviews. The limitations of these data have made it hard to predict which patients with a first episode of acute pancreatitis will progress to a second episode or beyond, Dr. Sweeny said.
Dr. Sweeny had no disclosures.
[email protected]
On Twitter @mitchelzoler
AT WCPGHAN 2016
Key clinical point:
Major finding: Overall, 17 of 83 patients (20%) had recurrent acute pancreatitis, but among six patients with a genetic cause, five had recurrences.
Data source: Eighty-three patients enrolled in INSPPIRE, an international consortium formed to prospectively study pediatric pancreatitis.
Disclosures: Dr. Sweeny had no disclosures.