User login
Medicare Penalties Make Hospital-Acquired-Infection Solutions a Priority
A shift in governmental regulations regarding reimbursement for hospital-acquired infections (HAIs) is forcing hospitals to take a closer look at how to reduce them. A recent study in Infection Control and Hospital Epidemiology shows that copper-alloy surfaces may be one such solution.3 According to the study, although only 9% of the touch surfaces in each ICU were replaced with copper components, there were 58% fewer HAI cases.1
“Before these regulations, hospitals didn’t necessarily want technology to decrease HAI rates, because the more infections and complications, the longer the length of patient stay, the greater the reimbursement, and the better the bottom line,” says Archelle Georgiou, MD, president of Georgiou Consulting LLC in Minneapolis and an advisor to the Copper Development Association.
Three regulations that have resulted in reimbursements to hospitals getting cut include:
- The Deficit Reduction Act of 2005, which was implemented on Oct. 1, 2008, which states that Medicare will not reimburse for certain types of HAIs;
- Section 3025 of the Affordable Care Act (signed into law in 2010), which incentivizes hospitals to decrease their readmission rates, which frequently are caused by HAIs. Beginning this fall, hospitals are getting reduced reimbursement when their readmission rates exceed a certain threshold. The maximum penalty in 2013 is 1% and will increase to 3% by 2015; and
- Section 1886 of the Affordable Care Act, which describes value-based purchasing and makes hospitals eligible to receive incentive payments for achieving better care on certain quality metrics. Funding for the program comes from withholding payment from poor-performing hospitals. The financial impact to hospitals started this year. In 2014, urinary tract infections and vascular-catheter-associated infections will be among the targeted conditions measured by CMS to calculate incentives and penalties.
“Hospitals are now feeling a direct impact from all of this,” Dr. Georgiou says. “Back in 2008, hospitals were noticing, but it was hard to get their attention since only one program was impacting their bottom line. But, pretty soon, hospitals risk losing upwards of 5% of their Medicare reimbursement for decreased quality.
“Reducing HAIs is clearly on the priority list of chief operating officers. They are very aware of the impact to their bottom line. They are looking to their vendors and suppliers to develop strategies to work with their hospitals to improve performance around these metrics.”
Karen Appold is a freelance writer in Pennsylvania.
A shift in governmental regulations regarding reimbursement for hospital-acquired infections (HAIs) is forcing hospitals to take a closer look at how to reduce them. A recent study in Infection Control and Hospital Epidemiology shows that copper-alloy surfaces may be one such solution.3 According to the study, although only 9% of the touch surfaces in each ICU were replaced with copper components, there were 58% fewer HAI cases.1
“Before these regulations, hospitals didn’t necessarily want technology to decrease HAI rates, because the more infections and complications, the longer the length of patient stay, the greater the reimbursement, and the better the bottom line,” says Archelle Georgiou, MD, president of Georgiou Consulting LLC in Minneapolis and an advisor to the Copper Development Association.
Three regulations that have resulted in reimbursements to hospitals getting cut include:
- The Deficit Reduction Act of 2005, which was implemented on Oct. 1, 2008, which states that Medicare will not reimburse for certain types of HAIs;
- Section 3025 of the Affordable Care Act (signed into law in 2010), which incentivizes hospitals to decrease their readmission rates, which frequently are caused by HAIs. Beginning this fall, hospitals are getting reduced reimbursement when their readmission rates exceed a certain threshold. The maximum penalty in 2013 is 1% and will increase to 3% by 2015; and
- Section 1886 of the Affordable Care Act, which describes value-based purchasing and makes hospitals eligible to receive incentive payments for achieving better care on certain quality metrics. Funding for the program comes from withholding payment from poor-performing hospitals. The financial impact to hospitals started this year. In 2014, urinary tract infections and vascular-catheter-associated infections will be among the targeted conditions measured by CMS to calculate incentives and penalties.
“Hospitals are now feeling a direct impact from all of this,” Dr. Georgiou says. “Back in 2008, hospitals were noticing, but it was hard to get their attention since only one program was impacting their bottom line. But, pretty soon, hospitals risk losing upwards of 5% of their Medicare reimbursement for decreased quality.
“Reducing HAIs is clearly on the priority list of chief operating officers. They are very aware of the impact to their bottom line. They are looking to their vendors and suppliers to develop strategies to work with their hospitals to improve performance around these metrics.”
Karen Appold is a freelance writer in Pennsylvania.
A shift in governmental regulations regarding reimbursement for hospital-acquired infections (HAIs) is forcing hospitals to take a closer look at how to reduce them. A recent study in Infection Control and Hospital Epidemiology shows that copper-alloy surfaces may be one such solution.3 According to the study, although only 9% of the touch surfaces in each ICU were replaced with copper components, there were 58% fewer HAI cases.1
“Before these regulations, hospitals didn’t necessarily want technology to decrease HAI rates, because the more infections and complications, the longer the length of patient stay, the greater the reimbursement, and the better the bottom line,” says Archelle Georgiou, MD, president of Georgiou Consulting LLC in Minneapolis and an advisor to the Copper Development Association.
Three regulations that have resulted in reimbursements to hospitals getting cut include:
- The Deficit Reduction Act of 2005, which was implemented on Oct. 1, 2008, which states that Medicare will not reimburse for certain types of HAIs;
- Section 3025 of the Affordable Care Act (signed into law in 2010), which incentivizes hospitals to decrease their readmission rates, which frequently are caused by HAIs. Beginning this fall, hospitals are getting reduced reimbursement when their readmission rates exceed a certain threshold. The maximum penalty in 2013 is 1% and will increase to 3% by 2015; and
- Section 1886 of the Affordable Care Act, which describes value-based purchasing and makes hospitals eligible to receive incentive payments for achieving better care on certain quality metrics. Funding for the program comes from withholding payment from poor-performing hospitals. The financial impact to hospitals started this year. In 2014, urinary tract infections and vascular-catheter-associated infections will be among the targeted conditions measured by CMS to calculate incentives and penalties.
“Hospitals are now feeling a direct impact from all of this,” Dr. Georgiou says. “Back in 2008, hospitals were noticing, but it was hard to get their attention since only one program was impacting their bottom line. But, pretty soon, hospitals risk losing upwards of 5% of their Medicare reimbursement for decreased quality.
“Reducing HAIs is clearly on the priority list of chief operating officers. They are very aware of the impact to their bottom line. They are looking to their vendors and suppliers to develop strategies to work with their hospitals to improve performance around these metrics.”
Karen Appold is a freelance writer in Pennsylvania.
How Copper Could Solve Problem of Hospital-Acquired Infections

—James Pile, MD, FACP, SFHM, vice chair, department of hospital medicine, Cleveland Clinic
Hospital-acquired infections (HAIs) are on the rise despite efforts to decrease them. HAIs cause an estimated 100,000 deaths annually and account for up to $45 billion in health-care costs. Adding fuel to the fire, bacteria increasingly are becoming resistant to last-resort drugs. Despite this gloomy outlook, a recent study in Infection Control and Hospital Epidemiology shows that a material known for its antimicrobial properties for more than 4,000 years—copper—might be a light at the end of this darkening tunnel.1
Ancient Indians stored water in copper pots to prevent illness, says lead study author Cassandra D. Salgado, MD, associate professor of medicine, hospital epidemiologist, and medical director for infection prevention at the Medical University of South Carolina (MUSC) in Charleston. But copper rarely is used in that manner today because molded plastics and stainless steel are less expensive and easier to mass-produce.
Dr. Salgado explains that the antimicrobial effect of copper-alloy surfaces is a result of the metal stealing electrons from the bacteria when they come into contact with each other. “Once the bacteria donate the electrons to the copper metal, this places the organism into a state of electrical-charge deficit,” she says. “As a consequence, free radicals are generated inside the cell, which ultimately leads to the cell’s death.”
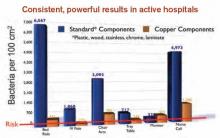
Copper-alloy surfaces kill 99.9% of bacteria in less than two hours, says Harold T. Michels, PhD, PE, senior vice president of technology and technical services for Copper Development Association Inc. in New York, who was a study author. On other surfaces, bacteria may live for multiple days or even months.
Unlike current methods used to decrease HAIs (i.e. hand-washing and sanitizing surfaces), copper components don’t require human intervention or compliance to be effective.
“It supplements what these other things can do; it’s in the background and it’s always working,” Michels says.

—Cassandra D. Salgado, MD, associate professor of medicine, hospital epidemiologist, medical director for infection prevention, Medical University of South Carolina, Charleston
Study Specifics
To conduct the study, copper prototypes of items touched most frequently by patients, health-care providers, and visitors were made and placed in patient rooms located within ICUs. “We placed the copper around the patient [much like a defensive perimeter] to reduce the likelihood that the health-care worker or visitor would introduce the infectious agent to the patient,” says the study’s lead investigator, Michael Schmidt, PhD, a professor and vice chair of MUSC’s department of microbiology and immunology.
Then, bacterial loads were measured on each object. For every study room, there was a control room without copper objects. Researchers were most interested in methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus (VRE). For a period of time, bacterial burdens were measured in both copper rooms and control rooms.
Results exceeded the researchers’ expectations. Although only 7% of the touch surfaces in each ICU were replaced with copper components, there were 58% fewer HAI cases. The rate of HAI and/or MRSA or VRE colonization in ICU rooms with copper-alloy surfaces was significantly lower than that in standard ICU rooms (0.071 versus 0.123). For HAIs only, the rate was reduced to 0.034 from 0.081.3
“We were pleasantly surprised with the reductions,” Dr. Salgado says. “We consistently saw a more than 50% reduction in HAIs in all study sites.”
Archelle Georgiou, MD, president of Georgiou Consulting LLC in Minneapolis and an advisor to the Copper Development Association, is an advocate for making the health-care system simpler and safer for consumers. She says copper is a “game-changer.”
“It’s a brand-new way of thinking about decreasing the number of HAIs,” she says.
Green Light?
In light of the study’s encouraging findings, hospitalist and infectious-disease specialist James Pile, MD, FACP, SFHM, vice chair of the Department of Hospital Medicine at Cleveland Clinic, says that although study results appear valid, “it didn’t provide any final answers.”
“It would be premature for a hospital to install copper based on this study,” he says, adding he didn’t find the study results surprising, because copper is known to have antimicrobial properties.
But, Dr. Pile says, the study did provide proof of concept and opens the door for larger, more definitive studies that will show if installing copper in hospital rooms is worthwhile.
“If future studies confirm earlier results, then hospitals should seriously consider copper installations,” he says.
Barriers to Implementation
Despite the promising outlook for copper in dramatically reducing HAIs, implantation of copper components is off to a slow start.
Negotiations with the Environmental Protection Agency, the federal agency with jurisdiction over public-health claims for antimicrobial surfaces, started in 2004. Testing started in 2005. Although federal registration was completed in February 2008, it wasn’t until late 2011 that all regulatory issues were resolved for manufacturers.
“The regulatory process created delays in educating hospitals and the public about copper’s effectiveness in killing certain bacteria,” Dr. Georgiou explains. “As a result, American manufacturers with the ability to make copper components weren’t developing products because they couldn’t sell them.”
Now that the regulatory issues have been resolved, U.S. manufacturers are beginning to make copper components. The first wave of commercial products came on the market in late 2011. Meanwhile, European countries have not been delayed and are well ahead of U.S. hospitals in implementing copper components.
Presently, nine U.S. hospitals have installed some form of copper components, including door hardware, cabinet pulls, sinks, stretchers, and IV poles, Michels reports.
Despite these advances, hospitals may be slow to incorporate copper components due to a variety of reasons:
Cost. Dr. Pile believes that cost will be the major barrier. “Installing copper surfaces won’t be cheap,” he says. “But, then again, HAIs are very costly. I think it will be more difficult to justify their existence if they can be prevented. If copper is effective in preventing HAIs, it would prove to be cost-effective over time.”
Dr. Salgado concurs. “A study needs to be done on the cost-effectiveness of copper surfaces,” she says. “Health economists estimate that if copper surfaces were incorporated into ICUs, after three to six months, those surfaces would pay for themselves. That is not a long time period. Hospitals need to understand that there will be upfront costs but that they will realize benefits downstream.”
The Center for Medicare & Medicaid Services (CMS) has reported that one infection adds $43,000 in patient costs.4 A typical U.S. hospital room contains $100,000 worth of goods and equipment.
“When you do the math using the amount of copper in our study, the cost would be between $1 and $10 per patient,” Dr. Schmidt says. “It’s also important to note that an infection adds 19 days to a patient’s hospital stay.”
Aesthetics. For some, appearance may be a concern. “Copper is actually an appealing material that is offered in an array of colors and surface finishes,” Dr. Michels says. Because a copper-and-brass combination is more prone to tarnishing, a copper-nickel alloy may be more desirable.
Availability. Copper components are not produced and marketed to U.S. hospitals; however, they are available. “We are hoping with our study and future studies that some medical-device companies, as well as hospital-furniture manufacturers, will jump on board to look at ways to mass-produce items,” Dr. Salgado says.
Acceptance. The study published in Infection Control and Hospital Epidemiology validated the effectiveness of copper in decreasing HAIs. This pilot study, however, was not blinded.3
“It was pretty apparent to providers where copper surfaces were located, which tends to result in some bias. Future studies will, hopefully, try to answer questions regarding healthcare providers’ behaviors with different surfaces,” says Dr. Salgado, noting researchers in California and Chile also are studying the effects of copper surfaces in hospitals.
Possible loss of efficacy. Even if a surface is effective initially, Dr. Pile points out that it’s possible for that to change. “I have a theoretical concern that, over time, bacterial pathogens may develop a tolerance to copper,” he says. “Bacterial adversaries have been able to overcome any type of treatment that we have devised for them thus far. But this remains to be seen.”
This has been an issue with other surfaces; once microbes establish a foothold, it is hard to eliminate them. But Dr. Schmidt says because bacteria are killed so quickly on copper surfaces and cleaning is only required once daily, the ability to establish a foothold is greatly reduced, if not completely eliminated.

—Harold T. Michels, PhD, PE, senior vice president of technology and technical services, Copper Development Association Inc.
Champion Proven Strategies
Dr. Pile sees antimicrobial stewardship as a great opportunity for hospitalists as a specialty. In fact, the Centers for Disease Control and Prevention is partnering with HM groups on piloting multiple antimicrobial stewardship initiatives at several sites.
Dr. Pile suggests that leaders spearhead formal quality-improvement efforts, be involved with patient-safety efforts, and serve as physician champions.
“No one is better positioned to do this than hospitalists, because we own the hospital environment,” he says. “We have an incredible stake in making sure that our inpatient environment provides safe and high-value care.”
As a result of the published study, Dr. Salgado says discussions are underway with hospital leaders at MUSC to determine if copper surfaces will be used in its ICUs and, if so, how changes will be implemented.
Karen Appold is a freelance writer in Pennsylvania.
References
- Klevens RM, Edwards JR, Richards CL, et al. Estimating healthcare-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007;122:160-166.
- Scott RD. The Direct Medical Costs of Healthcare-Associated Infections in U.S. Hospitals and the Benefits of Prevention. Atlanta: Centers for Disease Control and Prevention, 2009.
- Salgado CD, Sepkowitz KA, John JF, et al. Copper Surfaces Reduce the Rate of Healthcare-Acquired Infections in the Intensive Care Unit. Infect Control Hosp Epidemiol. 2013;34(5):479-486.
- Healthcare Cost and Utilization Project. Statistical Brief No. 94. Agency for Healthcare Research and Quality. Aug. 2010. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb94.pdf. Accessed Aug. 6, 2013.

—James Pile, MD, FACP, SFHM, vice chair, department of hospital medicine, Cleveland Clinic
Hospital-acquired infections (HAIs) are on the rise despite efforts to decrease them. HAIs cause an estimated 100,000 deaths annually and account for up to $45 billion in health-care costs. Adding fuel to the fire, bacteria increasingly are becoming resistant to last-resort drugs. Despite this gloomy outlook, a recent study in Infection Control and Hospital Epidemiology shows that a material known for its antimicrobial properties for more than 4,000 years—copper—might be a light at the end of this darkening tunnel.1
Ancient Indians stored water in copper pots to prevent illness, says lead study author Cassandra D. Salgado, MD, associate professor of medicine, hospital epidemiologist, and medical director for infection prevention at the Medical University of South Carolina (MUSC) in Charleston. But copper rarely is used in that manner today because molded plastics and stainless steel are less expensive and easier to mass-produce.
Dr. Salgado explains that the antimicrobial effect of copper-alloy surfaces is a result of the metal stealing electrons from the bacteria when they come into contact with each other. “Once the bacteria donate the electrons to the copper metal, this places the organism into a state of electrical-charge deficit,” she says. “As a consequence, free radicals are generated inside the cell, which ultimately leads to the cell’s death.”
Copper-alloy surfaces kill 99.9% of bacteria in less than two hours, says Harold T. Michels, PhD, PE, senior vice president of technology and technical services for Copper Development Association Inc. in New York, who was a study author. On other surfaces, bacteria may live for multiple days or even months.
Unlike current methods used to decrease HAIs (i.e. hand-washing and sanitizing surfaces), copper components don’t require human intervention or compliance to be effective.
“It supplements what these other things can do; it’s in the background and it’s always working,” Michels says.

—Cassandra D. Salgado, MD, associate professor of medicine, hospital epidemiologist, medical director for infection prevention, Medical University of South Carolina, Charleston
Study Specifics
To conduct the study, copper prototypes of items touched most frequently by patients, health-care providers, and visitors were made and placed in patient rooms located within ICUs. “We placed the copper around the patient [much like a defensive perimeter] to reduce the likelihood that the health-care worker or visitor would introduce the infectious agent to the patient,” says the study’s lead investigator, Michael Schmidt, PhD, a professor and vice chair of MUSC’s department of microbiology and immunology.
Then, bacterial loads were measured on each object. For every study room, there was a control room without copper objects. Researchers were most interested in methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus (VRE). For a period of time, bacterial burdens were measured in both copper rooms and control rooms.
Results exceeded the researchers’ expectations. Although only 7% of the touch surfaces in each ICU were replaced with copper components, there were 58% fewer HAI cases. The rate of HAI and/or MRSA or VRE colonization in ICU rooms with copper-alloy surfaces was significantly lower than that in standard ICU rooms (0.071 versus 0.123). For HAIs only, the rate was reduced to 0.034 from 0.081.3
“We were pleasantly surprised with the reductions,” Dr. Salgado says. “We consistently saw a more than 50% reduction in HAIs in all study sites.”
Archelle Georgiou, MD, president of Georgiou Consulting LLC in Minneapolis and an advisor to the Copper Development Association, is an advocate for making the health-care system simpler and safer for consumers. She says copper is a “game-changer.”
“It’s a brand-new way of thinking about decreasing the number of HAIs,” she says.
Green Light?
In light of the study’s encouraging findings, hospitalist and infectious-disease specialist James Pile, MD, FACP, SFHM, vice chair of the Department of Hospital Medicine at Cleveland Clinic, says that although study results appear valid, “it didn’t provide any final answers.”
“It would be premature for a hospital to install copper based on this study,” he says, adding he didn’t find the study results surprising, because copper is known to have antimicrobial properties.
But, Dr. Pile says, the study did provide proof of concept and opens the door for larger, more definitive studies that will show if installing copper in hospital rooms is worthwhile.
“If future studies confirm earlier results, then hospitals should seriously consider copper installations,” he says.
Barriers to Implementation
Despite the promising outlook for copper in dramatically reducing HAIs, implantation of copper components is off to a slow start.
Negotiations with the Environmental Protection Agency, the federal agency with jurisdiction over public-health claims for antimicrobial surfaces, started in 2004. Testing started in 2005. Although federal registration was completed in February 2008, it wasn’t until late 2011 that all regulatory issues were resolved for manufacturers.
“The regulatory process created delays in educating hospitals and the public about copper’s effectiveness in killing certain bacteria,” Dr. Georgiou explains. “As a result, American manufacturers with the ability to make copper components weren’t developing products because they couldn’t sell them.”
Now that the regulatory issues have been resolved, U.S. manufacturers are beginning to make copper components. The first wave of commercial products came on the market in late 2011. Meanwhile, European countries have not been delayed and are well ahead of U.S. hospitals in implementing copper components.
Presently, nine U.S. hospitals have installed some form of copper components, including door hardware, cabinet pulls, sinks, stretchers, and IV poles, Michels reports.
Despite these advances, hospitals may be slow to incorporate copper components due to a variety of reasons:
Cost. Dr. Pile believes that cost will be the major barrier. “Installing copper surfaces won’t be cheap,” he says. “But, then again, HAIs are very costly. I think it will be more difficult to justify their existence if they can be prevented. If copper is effective in preventing HAIs, it would prove to be cost-effective over time.”
Dr. Salgado concurs. “A study needs to be done on the cost-effectiveness of copper surfaces,” she says. “Health economists estimate that if copper surfaces were incorporated into ICUs, after three to six months, those surfaces would pay for themselves. That is not a long time period. Hospitals need to understand that there will be upfront costs but that they will realize benefits downstream.”
The Center for Medicare & Medicaid Services (CMS) has reported that one infection adds $43,000 in patient costs.4 A typical U.S. hospital room contains $100,000 worth of goods and equipment.
“When you do the math using the amount of copper in our study, the cost would be between $1 and $10 per patient,” Dr. Schmidt says. “It’s also important to note that an infection adds 19 days to a patient’s hospital stay.”
Aesthetics. For some, appearance may be a concern. “Copper is actually an appealing material that is offered in an array of colors and surface finishes,” Dr. Michels says. Because a copper-and-brass combination is more prone to tarnishing, a copper-nickel alloy may be more desirable.
Availability. Copper components are not produced and marketed to U.S. hospitals; however, they are available. “We are hoping with our study and future studies that some medical-device companies, as well as hospital-furniture manufacturers, will jump on board to look at ways to mass-produce items,” Dr. Salgado says.
Acceptance. The study published in Infection Control and Hospital Epidemiology validated the effectiveness of copper in decreasing HAIs. This pilot study, however, was not blinded.3
“It was pretty apparent to providers where copper surfaces were located, which tends to result in some bias. Future studies will, hopefully, try to answer questions regarding healthcare providers’ behaviors with different surfaces,” says Dr. Salgado, noting researchers in California and Chile also are studying the effects of copper surfaces in hospitals.
Possible loss of efficacy. Even if a surface is effective initially, Dr. Pile points out that it’s possible for that to change. “I have a theoretical concern that, over time, bacterial pathogens may develop a tolerance to copper,” he says. “Bacterial adversaries have been able to overcome any type of treatment that we have devised for them thus far. But this remains to be seen.”
This has been an issue with other surfaces; once microbes establish a foothold, it is hard to eliminate them. But Dr. Schmidt says because bacteria are killed so quickly on copper surfaces and cleaning is only required once daily, the ability to establish a foothold is greatly reduced, if not completely eliminated.

—Harold T. Michels, PhD, PE, senior vice president of technology and technical services, Copper Development Association Inc.
Champion Proven Strategies
Dr. Pile sees antimicrobial stewardship as a great opportunity for hospitalists as a specialty. In fact, the Centers for Disease Control and Prevention is partnering with HM groups on piloting multiple antimicrobial stewardship initiatives at several sites.
Dr. Pile suggests that leaders spearhead formal quality-improvement efforts, be involved with patient-safety efforts, and serve as physician champions.
“No one is better positioned to do this than hospitalists, because we own the hospital environment,” he says. “We have an incredible stake in making sure that our inpatient environment provides safe and high-value care.”
As a result of the published study, Dr. Salgado says discussions are underway with hospital leaders at MUSC to determine if copper surfaces will be used in its ICUs and, if so, how changes will be implemented.
Karen Appold is a freelance writer in Pennsylvania.
References
- Klevens RM, Edwards JR, Richards CL, et al. Estimating healthcare-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007;122:160-166.
- Scott RD. The Direct Medical Costs of Healthcare-Associated Infections in U.S. Hospitals and the Benefits of Prevention. Atlanta: Centers for Disease Control and Prevention, 2009.
- Salgado CD, Sepkowitz KA, John JF, et al. Copper Surfaces Reduce the Rate of Healthcare-Acquired Infections in the Intensive Care Unit. Infect Control Hosp Epidemiol. 2013;34(5):479-486.
- Healthcare Cost and Utilization Project. Statistical Brief No. 94. Agency for Healthcare Research and Quality. Aug. 2010. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb94.pdf. Accessed Aug. 6, 2013.

—James Pile, MD, FACP, SFHM, vice chair, department of hospital medicine, Cleveland Clinic
Hospital-acquired infections (HAIs) are on the rise despite efforts to decrease them. HAIs cause an estimated 100,000 deaths annually and account for up to $45 billion in health-care costs. Adding fuel to the fire, bacteria increasingly are becoming resistant to last-resort drugs. Despite this gloomy outlook, a recent study in Infection Control and Hospital Epidemiology shows that a material known for its antimicrobial properties for more than 4,000 years—copper—might be a light at the end of this darkening tunnel.1
Ancient Indians stored water in copper pots to prevent illness, says lead study author Cassandra D. Salgado, MD, associate professor of medicine, hospital epidemiologist, and medical director for infection prevention at the Medical University of South Carolina (MUSC) in Charleston. But copper rarely is used in that manner today because molded plastics and stainless steel are less expensive and easier to mass-produce.
Dr. Salgado explains that the antimicrobial effect of copper-alloy surfaces is a result of the metal stealing electrons from the bacteria when they come into contact with each other. “Once the bacteria donate the electrons to the copper metal, this places the organism into a state of electrical-charge deficit,” she says. “As a consequence, free radicals are generated inside the cell, which ultimately leads to the cell’s death.”
Copper-alloy surfaces kill 99.9% of bacteria in less than two hours, says Harold T. Michels, PhD, PE, senior vice president of technology and technical services for Copper Development Association Inc. in New York, who was a study author. On other surfaces, bacteria may live for multiple days or even months.
Unlike current methods used to decrease HAIs (i.e. hand-washing and sanitizing surfaces), copper components don’t require human intervention or compliance to be effective.
“It supplements what these other things can do; it’s in the background and it’s always working,” Michels says.

—Cassandra D. Salgado, MD, associate professor of medicine, hospital epidemiologist, medical director for infection prevention, Medical University of South Carolina, Charleston
Study Specifics
To conduct the study, copper prototypes of items touched most frequently by patients, health-care providers, and visitors were made and placed in patient rooms located within ICUs. “We placed the copper around the patient [much like a defensive perimeter] to reduce the likelihood that the health-care worker or visitor would introduce the infectious agent to the patient,” says the study’s lead investigator, Michael Schmidt, PhD, a professor and vice chair of MUSC’s department of microbiology and immunology.
Then, bacterial loads were measured on each object. For every study room, there was a control room without copper objects. Researchers were most interested in methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus (VRE). For a period of time, bacterial burdens were measured in both copper rooms and control rooms.
Results exceeded the researchers’ expectations. Although only 7% of the touch surfaces in each ICU were replaced with copper components, there were 58% fewer HAI cases. The rate of HAI and/or MRSA or VRE colonization in ICU rooms with copper-alloy surfaces was significantly lower than that in standard ICU rooms (0.071 versus 0.123). For HAIs only, the rate was reduced to 0.034 from 0.081.3
“We were pleasantly surprised with the reductions,” Dr. Salgado says. “We consistently saw a more than 50% reduction in HAIs in all study sites.”
Archelle Georgiou, MD, president of Georgiou Consulting LLC in Minneapolis and an advisor to the Copper Development Association, is an advocate for making the health-care system simpler and safer for consumers. She says copper is a “game-changer.”
“It’s a brand-new way of thinking about decreasing the number of HAIs,” she says.
Green Light?
In light of the study’s encouraging findings, hospitalist and infectious-disease specialist James Pile, MD, FACP, SFHM, vice chair of the Department of Hospital Medicine at Cleveland Clinic, says that although study results appear valid, “it didn’t provide any final answers.”
“It would be premature for a hospital to install copper based on this study,” he says, adding he didn’t find the study results surprising, because copper is known to have antimicrobial properties.
But, Dr. Pile says, the study did provide proof of concept and opens the door for larger, more definitive studies that will show if installing copper in hospital rooms is worthwhile.
“If future studies confirm earlier results, then hospitals should seriously consider copper installations,” he says.
Barriers to Implementation
Despite the promising outlook for copper in dramatically reducing HAIs, implantation of copper components is off to a slow start.
Negotiations with the Environmental Protection Agency, the federal agency with jurisdiction over public-health claims for antimicrobial surfaces, started in 2004. Testing started in 2005. Although federal registration was completed in February 2008, it wasn’t until late 2011 that all regulatory issues were resolved for manufacturers.
“The regulatory process created delays in educating hospitals and the public about copper’s effectiveness in killing certain bacteria,” Dr. Georgiou explains. “As a result, American manufacturers with the ability to make copper components weren’t developing products because they couldn’t sell them.”
Now that the regulatory issues have been resolved, U.S. manufacturers are beginning to make copper components. The first wave of commercial products came on the market in late 2011. Meanwhile, European countries have not been delayed and are well ahead of U.S. hospitals in implementing copper components.
Presently, nine U.S. hospitals have installed some form of copper components, including door hardware, cabinet pulls, sinks, stretchers, and IV poles, Michels reports.
Despite these advances, hospitals may be slow to incorporate copper components due to a variety of reasons:
Cost. Dr. Pile believes that cost will be the major barrier. “Installing copper surfaces won’t be cheap,” he says. “But, then again, HAIs are very costly. I think it will be more difficult to justify their existence if they can be prevented. If copper is effective in preventing HAIs, it would prove to be cost-effective over time.”
Dr. Salgado concurs. “A study needs to be done on the cost-effectiveness of copper surfaces,” she says. “Health economists estimate that if copper surfaces were incorporated into ICUs, after three to six months, those surfaces would pay for themselves. That is not a long time period. Hospitals need to understand that there will be upfront costs but that they will realize benefits downstream.”
The Center for Medicare & Medicaid Services (CMS) has reported that one infection adds $43,000 in patient costs.4 A typical U.S. hospital room contains $100,000 worth of goods and equipment.
“When you do the math using the amount of copper in our study, the cost would be between $1 and $10 per patient,” Dr. Schmidt says. “It’s also important to note that an infection adds 19 days to a patient’s hospital stay.”
Aesthetics. For some, appearance may be a concern. “Copper is actually an appealing material that is offered in an array of colors and surface finishes,” Dr. Michels says. Because a copper-and-brass combination is more prone to tarnishing, a copper-nickel alloy may be more desirable.
Availability. Copper components are not produced and marketed to U.S. hospitals; however, they are available. “We are hoping with our study and future studies that some medical-device companies, as well as hospital-furniture manufacturers, will jump on board to look at ways to mass-produce items,” Dr. Salgado says.
Acceptance. The study published in Infection Control and Hospital Epidemiology validated the effectiveness of copper in decreasing HAIs. This pilot study, however, was not blinded.3
“It was pretty apparent to providers where copper surfaces were located, which tends to result in some bias. Future studies will, hopefully, try to answer questions regarding healthcare providers’ behaviors with different surfaces,” says Dr. Salgado, noting researchers in California and Chile also are studying the effects of copper surfaces in hospitals.
Possible loss of efficacy. Even if a surface is effective initially, Dr. Pile points out that it’s possible for that to change. “I have a theoretical concern that, over time, bacterial pathogens may develop a tolerance to copper,” he says. “Bacterial adversaries have been able to overcome any type of treatment that we have devised for them thus far. But this remains to be seen.”
This has been an issue with other surfaces; once microbes establish a foothold, it is hard to eliminate them. But Dr. Schmidt says because bacteria are killed so quickly on copper surfaces and cleaning is only required once daily, the ability to establish a foothold is greatly reduced, if not completely eliminated.

—Harold T. Michels, PhD, PE, senior vice president of technology and technical services, Copper Development Association Inc.
Champion Proven Strategies
Dr. Pile sees antimicrobial stewardship as a great opportunity for hospitalists as a specialty. In fact, the Centers for Disease Control and Prevention is partnering with HM groups on piloting multiple antimicrobial stewardship initiatives at several sites.
Dr. Pile suggests that leaders spearhead formal quality-improvement efforts, be involved with patient-safety efforts, and serve as physician champions.
“No one is better positioned to do this than hospitalists, because we own the hospital environment,” he says. “We have an incredible stake in making sure that our inpatient environment provides safe and high-value care.”
As a result of the published study, Dr. Salgado says discussions are underway with hospital leaders at MUSC to determine if copper surfaces will be used in its ICUs and, if so, how changes will be implemented.
Karen Appold is a freelance writer in Pennsylvania.
References
- Klevens RM, Edwards JR, Richards CL, et al. Estimating healthcare-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007;122:160-166.
- Scott RD. The Direct Medical Costs of Healthcare-Associated Infections in U.S. Hospitals and the Benefits of Prevention. Atlanta: Centers for Disease Control and Prevention, 2009.
- Salgado CD, Sepkowitz KA, John JF, et al. Copper Surfaces Reduce the Rate of Healthcare-Acquired Infections in the Intensive Care Unit. Infect Control Hosp Epidemiol. 2013;34(5):479-486.
- Healthcare Cost and Utilization Project. Statistical Brief No. 94. Agency for Healthcare Research and Quality. Aug. 2010. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb94.pdf. Accessed Aug. 6, 2013.
Prediction Model Identifies Potentially Avoidable 30-Day Readmissions
Clinical question: Can a prediction model based on administrative and clinical data identify potentially avoidable 30-day readmissions in medical patients prior to discharge?
Background: An estimated 18% of Medicare beneficiaries are readmitted to the hospital within 30 days of discharge, costing nearly $17 billion per year. Interventions to reduce readmission rates are costly and should be focused on high-risk patients. To date, using models to predict 30-day readmission has been problematic and unreliable.
Study design: Retrospective cohort.
Setting: Academic medical center in Boston.
Synopsis: Using consecutive discharges from all medical services of Brigham and Women’s Hospital occurring over one year, this study derived and internally validated a prediction model for potentially avoidable 30-day readmissions. Of 10,731 discharges, there were 2,399 (22%) 30-day readmissions, and 879 (8.5%) were deemed potentially avoidable. Seven independent predictors for readmission were identified and used to create a predictor score referred to as the HOSPITAL score. Predictors included hemoglobin and sodium levels at discharge, number of hospitalizations in the past year, and four features of the index hospitalization, including type, discharge from an oncology service, presence of procedures, and length of stay. The score was internally validated and found to predict potentially avoidable 30-day readmission in medical patients with fair discriminatory power and good calibration.
This study is unique in that none of the classic comorbidities (e.g. congestive heart failure) were associated with a higher risk of 30-day readmission. Previously unrecognized predictors, including hemoglobin, sodium, and number of procedures performed, were incorporated. This suggests that comorbidities are not as important as illness severity or clinical instability. Hospitalists should await studies that externally validate the HOSPITAL score before incorporating it into practice.
Bottom line: A unique and simple seven-item prediction model identifies potentially avoidable 30-day readmissions but needs to be externally validated before being widely utilized.
Citation: Donze J, Drahomir A, Williams D, Schnipper JL. Potentially avoidable 30-day hospital readmissions in medical patients. JAMA Intern Med. 2013;137(8):632-638.
Clinical question: Can a prediction model based on administrative and clinical data identify potentially avoidable 30-day readmissions in medical patients prior to discharge?
Background: An estimated 18% of Medicare beneficiaries are readmitted to the hospital within 30 days of discharge, costing nearly $17 billion per year. Interventions to reduce readmission rates are costly and should be focused on high-risk patients. To date, using models to predict 30-day readmission has been problematic and unreliable.
Study design: Retrospective cohort.
Setting: Academic medical center in Boston.
Synopsis: Using consecutive discharges from all medical services of Brigham and Women’s Hospital occurring over one year, this study derived and internally validated a prediction model for potentially avoidable 30-day readmissions. Of 10,731 discharges, there were 2,399 (22%) 30-day readmissions, and 879 (8.5%) were deemed potentially avoidable. Seven independent predictors for readmission were identified and used to create a predictor score referred to as the HOSPITAL score. Predictors included hemoglobin and sodium levels at discharge, number of hospitalizations in the past year, and four features of the index hospitalization, including type, discharge from an oncology service, presence of procedures, and length of stay. The score was internally validated and found to predict potentially avoidable 30-day readmission in medical patients with fair discriminatory power and good calibration.
This study is unique in that none of the classic comorbidities (e.g. congestive heart failure) were associated with a higher risk of 30-day readmission. Previously unrecognized predictors, including hemoglobin, sodium, and number of procedures performed, were incorporated. This suggests that comorbidities are not as important as illness severity or clinical instability. Hospitalists should await studies that externally validate the HOSPITAL score before incorporating it into practice.
Bottom line: A unique and simple seven-item prediction model identifies potentially avoidable 30-day readmissions but needs to be externally validated before being widely utilized.
Citation: Donze J, Drahomir A, Williams D, Schnipper JL. Potentially avoidable 30-day hospital readmissions in medical patients. JAMA Intern Med. 2013;137(8):632-638.
Clinical question: Can a prediction model based on administrative and clinical data identify potentially avoidable 30-day readmissions in medical patients prior to discharge?
Background: An estimated 18% of Medicare beneficiaries are readmitted to the hospital within 30 days of discharge, costing nearly $17 billion per year. Interventions to reduce readmission rates are costly and should be focused on high-risk patients. To date, using models to predict 30-day readmission has been problematic and unreliable.
Study design: Retrospective cohort.
Setting: Academic medical center in Boston.
Synopsis: Using consecutive discharges from all medical services of Brigham and Women’s Hospital occurring over one year, this study derived and internally validated a prediction model for potentially avoidable 30-day readmissions. Of 10,731 discharges, there were 2,399 (22%) 30-day readmissions, and 879 (8.5%) were deemed potentially avoidable. Seven independent predictors for readmission were identified and used to create a predictor score referred to as the HOSPITAL score. Predictors included hemoglobin and sodium levels at discharge, number of hospitalizations in the past year, and four features of the index hospitalization, including type, discharge from an oncology service, presence of procedures, and length of stay. The score was internally validated and found to predict potentially avoidable 30-day readmission in medical patients with fair discriminatory power and good calibration.
This study is unique in that none of the classic comorbidities (e.g. congestive heart failure) were associated with a higher risk of 30-day readmission. Previously unrecognized predictors, including hemoglobin, sodium, and number of procedures performed, were incorporated. This suggests that comorbidities are not as important as illness severity or clinical instability. Hospitalists should await studies that externally validate the HOSPITAL score before incorporating it into practice.
Bottom line: A unique and simple seven-item prediction model identifies potentially avoidable 30-day readmissions but needs to be externally validated before being widely utilized.
Citation: Donze J, Drahomir A, Williams D, Schnipper JL. Potentially avoidable 30-day hospital readmissions in medical patients. JAMA Intern Med. 2013;137(8):632-638.
IPC-UCSF Fellowship for Hospitalist Group Leaders Demands a Stretch
The yearlong IPC-UCSF Fellowship for Hospitalist Leaders brings about 40 IPC: The Hospitalist Company group leaders together for a series of three-day training sessions and ongoing distance learning, executive coaching, and project mentoring.
The program emphasizes role plays and simulations, and even involves an acting coach to help participants learn to make more effective presentations, such as harnessing the power of storytelling, says Niraj L. Sehgal, MD, MPH, a hospitalist at the University of California at San Francisco (UCSF) who directs the fellowship through UCSF’s Center for Health Professions.
The first class graduated in November 2011, and the third is in session. Participants implement a mentored project in their home facility, with measurable results, as a vehicle for leadership development in such areas as quality improvement (QI), patient safety, or readmissions prevention. But the specific project is not as important as whether or not that project is well-designed to stretch the individual in areas where they weren’t comfortable before, Dr. Sehgal says.
Through her QI project, Jasmin Baleva, MD, of Memorial Hermann Memorial City Medical Center in Houston, a 2012 participant, found an alternate to the costly nocturnist model while maintaining the time it takes for the first hospitalist encounter with newly admitted patients. “I think the IPC-UCSF project gave my proposal a little more legitimacy,” she tells TH. “They also taught me how to present it in an effective package and to approach the C-suite feeling less intimidated.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
The yearlong IPC-UCSF Fellowship for Hospitalist Leaders brings about 40 IPC: The Hospitalist Company group leaders together for a series of three-day training sessions and ongoing distance learning, executive coaching, and project mentoring.
The program emphasizes role plays and simulations, and even involves an acting coach to help participants learn to make more effective presentations, such as harnessing the power of storytelling, says Niraj L. Sehgal, MD, MPH, a hospitalist at the University of California at San Francisco (UCSF) who directs the fellowship through UCSF’s Center for Health Professions.
The first class graduated in November 2011, and the third is in session. Participants implement a mentored project in their home facility, with measurable results, as a vehicle for leadership development in such areas as quality improvement (QI), patient safety, or readmissions prevention. But the specific project is not as important as whether or not that project is well-designed to stretch the individual in areas where they weren’t comfortable before, Dr. Sehgal says.
Through her QI project, Jasmin Baleva, MD, of Memorial Hermann Memorial City Medical Center in Houston, a 2012 participant, found an alternate to the costly nocturnist model while maintaining the time it takes for the first hospitalist encounter with newly admitted patients. “I think the IPC-UCSF project gave my proposal a little more legitimacy,” she tells TH. “They also taught me how to present it in an effective package and to approach the C-suite feeling less intimidated.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
The yearlong IPC-UCSF Fellowship for Hospitalist Leaders brings about 40 IPC: The Hospitalist Company group leaders together for a series of three-day training sessions and ongoing distance learning, executive coaching, and project mentoring.
The program emphasizes role plays and simulations, and even involves an acting coach to help participants learn to make more effective presentations, such as harnessing the power of storytelling, says Niraj L. Sehgal, MD, MPH, a hospitalist at the University of California at San Francisco (UCSF) who directs the fellowship through UCSF’s Center for Health Professions.
The first class graduated in November 2011, and the third is in session. Participants implement a mentored project in their home facility, with measurable results, as a vehicle for leadership development in such areas as quality improvement (QI), patient safety, or readmissions prevention. But the specific project is not as important as whether or not that project is well-designed to stretch the individual in areas where they weren’t comfortable before, Dr. Sehgal says.
Through her QI project, Jasmin Baleva, MD, of Memorial Hermann Memorial City Medical Center in Houston, a 2012 participant, found an alternate to the costly nocturnist model while maintaining the time it takes for the first hospitalist encounter with newly admitted patients. “I think the IPC-UCSF project gave my proposal a little more legitimacy,” she tells TH. “They also taught me how to present it in an effective package and to approach the C-suite feeling less intimidated.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
Hospitals' Battle Against Superbugs Goes Robotic
One in 20 hospitalized patients picks up an infection in the hospital, and a recent article by the Associated Press describes the emergence of new technologies to fight antibiotic-resistant superbugs: “They sweep. They swab. They sterilize. And still the germs persist.”1
Hospitals across the country are testing new approaches to stop the spread of superbugs, which are tied to an estimated 100,000 deaths per year, according to the CDC. New approaches include robotlike machines that emit ultraviolet light or hydrogen-peroxide vapors, germ-resistant copper bed rails and call buttons, antimicrobial linens and wall paint, and hydrogel post-surgical dressings infused with silver ions that have antimicrobial properties.
Research firm Frost & Sullivan estimates that the market for bug-killing products and technologies will grow to $80 million from $30 million in the next three years. And yet evidence of positive outcomes from them continues to be debated.
“In short, escalating antimicrobial-resistance issues have us facing the prospect of untreatable bacterial pathogens, particularly involving gram-negative organisms,” James Pile, MD, FACP, SFHM, a hospital medicine and infectious diseases physician at Cleveland Clinic, wrote in an email. “In fact, many of our hospitals already deal with a limited number of infections caused by bacteria we have no clearly effective antibiotics against; the issue is only going to get worse.”
As an example, the CDC recently issued a warning about carbapenum-resistant Enterobacteriaceae (CRE), which has a 40% mortality rate and last year was reported in 4.6% of U.S. hospitals.2 CDC recommends that hospitals use more of the existing prevention measures against CRE, including active-case detection and segregation of patients and the staff who care for them. Dr. Pile says health facilities need to do a better job of preventing infections involving multi-drug-resistant pathogens, but in the meantime, “proven technologies such as proper hand hygiene and antimicrobial stewardship are more important than ever.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
One in 20 hospitalized patients picks up an infection in the hospital, and a recent article by the Associated Press describes the emergence of new technologies to fight antibiotic-resistant superbugs: “They sweep. They swab. They sterilize. And still the germs persist.”1
Hospitals across the country are testing new approaches to stop the spread of superbugs, which are tied to an estimated 100,000 deaths per year, according to the CDC. New approaches include robotlike machines that emit ultraviolet light or hydrogen-peroxide vapors, germ-resistant copper bed rails and call buttons, antimicrobial linens and wall paint, and hydrogel post-surgical dressings infused with silver ions that have antimicrobial properties.
Research firm Frost & Sullivan estimates that the market for bug-killing products and technologies will grow to $80 million from $30 million in the next three years. And yet evidence of positive outcomes from them continues to be debated.
“In short, escalating antimicrobial-resistance issues have us facing the prospect of untreatable bacterial pathogens, particularly involving gram-negative organisms,” James Pile, MD, FACP, SFHM, a hospital medicine and infectious diseases physician at Cleveland Clinic, wrote in an email. “In fact, many of our hospitals already deal with a limited number of infections caused by bacteria we have no clearly effective antibiotics against; the issue is only going to get worse.”
As an example, the CDC recently issued a warning about carbapenum-resistant Enterobacteriaceae (CRE), which has a 40% mortality rate and last year was reported in 4.6% of U.S. hospitals.2 CDC recommends that hospitals use more of the existing prevention measures against CRE, including active-case detection and segregation of patients and the staff who care for them. Dr. Pile says health facilities need to do a better job of preventing infections involving multi-drug-resistant pathogens, but in the meantime, “proven technologies such as proper hand hygiene and antimicrobial stewardship are more important than ever.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
One in 20 hospitalized patients picks up an infection in the hospital, and a recent article by the Associated Press describes the emergence of new technologies to fight antibiotic-resistant superbugs: “They sweep. They swab. They sterilize. And still the germs persist.”1
Hospitals across the country are testing new approaches to stop the spread of superbugs, which are tied to an estimated 100,000 deaths per year, according to the CDC. New approaches include robotlike machines that emit ultraviolet light or hydrogen-peroxide vapors, germ-resistant copper bed rails and call buttons, antimicrobial linens and wall paint, and hydrogel post-surgical dressings infused with silver ions that have antimicrobial properties.
Research firm Frost & Sullivan estimates that the market for bug-killing products and technologies will grow to $80 million from $30 million in the next three years. And yet evidence of positive outcomes from them continues to be debated.
“In short, escalating antimicrobial-resistance issues have us facing the prospect of untreatable bacterial pathogens, particularly involving gram-negative organisms,” James Pile, MD, FACP, SFHM, a hospital medicine and infectious diseases physician at Cleveland Clinic, wrote in an email. “In fact, many of our hospitals already deal with a limited number of infections caused by bacteria we have no clearly effective antibiotics against; the issue is only going to get worse.”
As an example, the CDC recently issued a warning about carbapenum-resistant Enterobacteriaceae (CRE), which has a 40% mortality rate and last year was reported in 4.6% of U.S. hospitals.2 CDC recommends that hospitals use more of the existing prevention measures against CRE, including active-case detection and segregation of patients and the staff who care for them. Dr. Pile says health facilities need to do a better job of preventing infections involving multi-drug-resistant pathogens, but in the meantime, “proven technologies such as proper hand hygiene and antimicrobial stewardship are more important than ever.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
Hospitalists Share Information, Insights Through RIV Posters at HM13
One of the busiest times of HM13—and, come to think of it, every recent annual meeting—is the poster session for the Research, Innovations, and Clinical Vignettes (RIV) competition. This year, more than 800 abstracts were submitted and reviewed, with nearly 600 being accepted for presentation at HM13. That meant thousands of hospitalists thumbtacking posters to rows and rows of portable bulletin boards in the Gaylord National Resort & Convention Center’s massive exhibit hall.
With all those posters and accompanying oral presentations, it’s impossible for RIV judges to chat with everybody, so they choose finalists based on the abstracts, then listen to quick-hit summaries before choosing a winner on site. And meeting attendees are just as strapped for time, so they do the best they can to see as many posters as they can, taking time to network with old connections and make new ones.
So with all the limitations on how many people will interact with your poster, the small chance of winning Best in Show, and the hundreds of work hours that go into a poster presentation, why do it?
“To share is what I think is really important,” says Todd Hecht, MD, FACP, SFHM, associate professor of clinical medicine at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia. “If you don’t let other people know what you’re doing, they can’t bring it to their institutions, nor can you learn from others and bring their innovations to your own hospital.”
Dr. Hecht, director of the Anticoagulation Management Center and Anticoagulation Management Program at the Hospital of the University of Pennsylvania, takes the poster sessions very seriously. This year, he entered a poster in both the Innovations and Vignette categories. His Innovations poster, “Impact of a Multidisciplinary Safety Checklist on the Rate of Preventable Hospital Complications and Standardization of Care,” was a finalist.
That meant that, at the very least, he’d be able to explain to at least two judges what motivated his research team’s project. And what was the inspiration? A 90-year-old male patient with metastatic melanoma who, in the fall of 2011, refused to take medication for VTE prophylaxis, as lesions on his skin made the process rather painful. After refusing the doses for a bit, though, the high-risk patient unsurprisingly developed a pulmonary embolism (PE).
The man survived the PE, but Dr. Hecht and his colleagues began to wonder how many patients refuse VTE prophylaxis. So they investigated, and it turned out that from December 2010 to February 2011, 26.4% of the prescribed doses of prophylaxis on the medicine floors they studied were missed. Moreover, nearly 80% of all missed doses on the medicine floors were due to patient refusal.
“It was astonishing to me that it was that high,” Dr. Hecht says. “If there were 1,000 doses in a month, 260 of them were not being given—and 205 of them were not given because they were refused.”
Checklist Integration
So Dr. Hecht and colleagues set out to create a checklist that could be used daily on multidisciplinary rounds to help reduce the risk of VTE. First question on the list: Has prophylaxis been ordered, and if so, is the patient refusing it? Knowing that patients are “refusing” medication can lead to discussions about why that is happening, which in turn can lead to ways to convince the patient that the preventative measure is a good idea.
Dr. Hecht says the team also realized a checklist creates the opportunity to improve other quality metrics, such as hospital-associated infections (HAIs). Two questions on the checklist ask whether indwelling urinary catheters (IUCs) and central venous catheters (CVCs) can be removed. Two questions ask if telemetry can be stopped and whether there are any pain-management concerns. A final query asks whether there are any nursing, social work, or discharge-related questions—a step that, according to Dr. Hecht, loops the entire multidisciplinary team into the care-plan discussion.
“An ongoing challenge is making sure it’s not just questions being asked and being answered by rote,” Dr. Hecht says. “Just pause and think for just a second for each question. You can get through the checklist in 10 seconds, but you can’t go through the checklist in two seconds.”
The project’s results are what made it a finalist. After the checklist intervention, the number of missed doses of VTE prophylaxis plummeted 59% to just 10.9% (P<0.001) from September to November 2012; the number of “patient refused” doses dropped to 6.3% (P<0.001).
Not only was Dr. Hecht caught off guard by his findings, but so were the judges who visited his poster—Mangla Gulati, MD, FHM, of the University of Maryland School of Medicine and Rachel George, MD, MBA, FHM, of Cogent HMG.
“I wonder if it’s like that in every hospital,” Dr. George says. “I’d like to know.”
The positive reaction and feedback to Dr. Hecht’s poster, however, was not enough to win the Innovations category. That honor went to “SEPTRIS: Improving Sepsis Recognition and Management Through a Mobile Educational Game,” which was developed by a team of researchers at Stanford University in Palo Alto, Calif. The video game
(http://med.stanford.edu/septris/)—a mashup of sepsis and the once-popular Tetris puzzle game—already has been played 17,000 times and is on its way to being shared in other languages.
“Win or lose, it doesn’t matter,” Dr. Hecht says. “The goal is to share your information with other people and learn from them.”
Peter Watson, MD, FACP, FHM, sees it the same way. That’s why this year he was both judge and judged. The division head of hospital medicine for Henry Ford Medical Group in Detroit was part of a group presenting “Feasibility and Efficacy of a Specialized Pilot Training Program to Enhance Inpatient Communication Skills of Hospitalists.” He was a judge for the Research portion of the contest. He says he’s hard-pressed to say which process he enjoyed more, but one trick of the poster trade he passes along is that “judging actually makes you a better presenter on the back end,” especially when it comes to describing in less than five minutes a poster whose work may date back 12 to 18 months.
“In your brain,” he says, “you have a Tolstoy novel of information, but you have to break that down into a paragraph of CliffsNotes, and actually convince the people that are judging you that you have a really cool project that either is going to have a big impact in the field or may lead to other big studies or is going to impress somebody so much that they’re going to go back to their institution and say, ‘Hey, I’m going to do that.’”
Dr. Watson also urges people not to be discouraged by not winning the poster contest. First, all of the accepted abstracts get published online (www.shmabstracts.com) by the Journal of Hospital Medicine, a high point for medical students, residents, and early-career physicians looking to make a mark. Second, presenting information of value to one’s peers is the definition of a specialty that prides itself on collaboration.
“To see a second-year medical student presenting all the way up to a very senior division chief and everything in between is a really good example for our profession,” he says. “That’s really the magic of this meeting.”
Richard Quinn is a freelance writer in New Jersey.
One of the busiest times of HM13—and, come to think of it, every recent annual meeting—is the poster session for the Research, Innovations, and Clinical Vignettes (RIV) competition. This year, more than 800 abstracts were submitted and reviewed, with nearly 600 being accepted for presentation at HM13. That meant thousands of hospitalists thumbtacking posters to rows and rows of portable bulletin boards in the Gaylord National Resort & Convention Center’s massive exhibit hall.
With all those posters and accompanying oral presentations, it’s impossible for RIV judges to chat with everybody, so they choose finalists based on the abstracts, then listen to quick-hit summaries before choosing a winner on site. And meeting attendees are just as strapped for time, so they do the best they can to see as many posters as they can, taking time to network with old connections and make new ones.
So with all the limitations on how many people will interact with your poster, the small chance of winning Best in Show, and the hundreds of work hours that go into a poster presentation, why do it?
“To share is what I think is really important,” says Todd Hecht, MD, FACP, SFHM, associate professor of clinical medicine at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia. “If you don’t let other people know what you’re doing, they can’t bring it to their institutions, nor can you learn from others and bring their innovations to your own hospital.”
Dr. Hecht, director of the Anticoagulation Management Center and Anticoagulation Management Program at the Hospital of the University of Pennsylvania, takes the poster sessions very seriously. This year, he entered a poster in both the Innovations and Vignette categories. His Innovations poster, “Impact of a Multidisciplinary Safety Checklist on the Rate of Preventable Hospital Complications and Standardization of Care,” was a finalist.
That meant that, at the very least, he’d be able to explain to at least two judges what motivated his research team’s project. And what was the inspiration? A 90-year-old male patient with metastatic melanoma who, in the fall of 2011, refused to take medication for VTE prophylaxis, as lesions on his skin made the process rather painful. After refusing the doses for a bit, though, the high-risk patient unsurprisingly developed a pulmonary embolism (PE).
The man survived the PE, but Dr. Hecht and his colleagues began to wonder how many patients refuse VTE prophylaxis. So they investigated, and it turned out that from December 2010 to February 2011, 26.4% of the prescribed doses of prophylaxis on the medicine floors they studied were missed. Moreover, nearly 80% of all missed doses on the medicine floors were due to patient refusal.
“It was astonishing to me that it was that high,” Dr. Hecht says. “If there were 1,000 doses in a month, 260 of them were not being given—and 205 of them were not given because they were refused.”
Checklist Integration
So Dr. Hecht and colleagues set out to create a checklist that could be used daily on multidisciplinary rounds to help reduce the risk of VTE. First question on the list: Has prophylaxis been ordered, and if so, is the patient refusing it? Knowing that patients are “refusing” medication can lead to discussions about why that is happening, which in turn can lead to ways to convince the patient that the preventative measure is a good idea.
Dr. Hecht says the team also realized a checklist creates the opportunity to improve other quality metrics, such as hospital-associated infections (HAIs). Two questions on the checklist ask whether indwelling urinary catheters (IUCs) and central venous catheters (CVCs) can be removed. Two questions ask if telemetry can be stopped and whether there are any pain-management concerns. A final query asks whether there are any nursing, social work, or discharge-related questions—a step that, according to Dr. Hecht, loops the entire multidisciplinary team into the care-plan discussion.
“An ongoing challenge is making sure it’s not just questions being asked and being answered by rote,” Dr. Hecht says. “Just pause and think for just a second for each question. You can get through the checklist in 10 seconds, but you can’t go through the checklist in two seconds.”
The project’s results are what made it a finalist. After the checklist intervention, the number of missed doses of VTE prophylaxis plummeted 59% to just 10.9% (P<0.001) from September to November 2012; the number of “patient refused” doses dropped to 6.3% (P<0.001).
Not only was Dr. Hecht caught off guard by his findings, but so were the judges who visited his poster—Mangla Gulati, MD, FHM, of the University of Maryland School of Medicine and Rachel George, MD, MBA, FHM, of Cogent HMG.
“I wonder if it’s like that in every hospital,” Dr. George says. “I’d like to know.”
The positive reaction and feedback to Dr. Hecht’s poster, however, was not enough to win the Innovations category. That honor went to “SEPTRIS: Improving Sepsis Recognition and Management Through a Mobile Educational Game,” which was developed by a team of researchers at Stanford University in Palo Alto, Calif. The video game
(http://med.stanford.edu/septris/)—a mashup of sepsis and the once-popular Tetris puzzle game—already has been played 17,000 times and is on its way to being shared in other languages.
“Win or lose, it doesn’t matter,” Dr. Hecht says. “The goal is to share your information with other people and learn from them.”
Peter Watson, MD, FACP, FHM, sees it the same way. That’s why this year he was both judge and judged. The division head of hospital medicine for Henry Ford Medical Group in Detroit was part of a group presenting “Feasibility and Efficacy of a Specialized Pilot Training Program to Enhance Inpatient Communication Skills of Hospitalists.” He was a judge for the Research portion of the contest. He says he’s hard-pressed to say which process he enjoyed more, but one trick of the poster trade he passes along is that “judging actually makes you a better presenter on the back end,” especially when it comes to describing in less than five minutes a poster whose work may date back 12 to 18 months.
“In your brain,” he says, “you have a Tolstoy novel of information, but you have to break that down into a paragraph of CliffsNotes, and actually convince the people that are judging you that you have a really cool project that either is going to have a big impact in the field or may lead to other big studies or is going to impress somebody so much that they’re going to go back to their institution and say, ‘Hey, I’m going to do that.’”
Dr. Watson also urges people not to be discouraged by not winning the poster contest. First, all of the accepted abstracts get published online (www.shmabstracts.com) by the Journal of Hospital Medicine, a high point for medical students, residents, and early-career physicians looking to make a mark. Second, presenting information of value to one’s peers is the definition of a specialty that prides itself on collaboration.
“To see a second-year medical student presenting all the way up to a very senior division chief and everything in between is a really good example for our profession,” he says. “That’s really the magic of this meeting.”
Richard Quinn is a freelance writer in New Jersey.
One of the busiest times of HM13—and, come to think of it, every recent annual meeting—is the poster session for the Research, Innovations, and Clinical Vignettes (RIV) competition. This year, more than 800 abstracts were submitted and reviewed, with nearly 600 being accepted for presentation at HM13. That meant thousands of hospitalists thumbtacking posters to rows and rows of portable bulletin boards in the Gaylord National Resort & Convention Center’s massive exhibit hall.
With all those posters and accompanying oral presentations, it’s impossible for RIV judges to chat with everybody, so they choose finalists based on the abstracts, then listen to quick-hit summaries before choosing a winner on site. And meeting attendees are just as strapped for time, so they do the best they can to see as many posters as they can, taking time to network with old connections and make new ones.
So with all the limitations on how many people will interact with your poster, the small chance of winning Best in Show, and the hundreds of work hours that go into a poster presentation, why do it?
“To share is what I think is really important,” says Todd Hecht, MD, FACP, SFHM, associate professor of clinical medicine at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia. “If you don’t let other people know what you’re doing, they can’t bring it to their institutions, nor can you learn from others and bring their innovations to your own hospital.”
Dr. Hecht, director of the Anticoagulation Management Center and Anticoagulation Management Program at the Hospital of the University of Pennsylvania, takes the poster sessions very seriously. This year, he entered a poster in both the Innovations and Vignette categories. His Innovations poster, “Impact of a Multidisciplinary Safety Checklist on the Rate of Preventable Hospital Complications and Standardization of Care,” was a finalist.
That meant that, at the very least, he’d be able to explain to at least two judges what motivated his research team’s project. And what was the inspiration? A 90-year-old male patient with metastatic melanoma who, in the fall of 2011, refused to take medication for VTE prophylaxis, as lesions on his skin made the process rather painful. After refusing the doses for a bit, though, the high-risk patient unsurprisingly developed a pulmonary embolism (PE).
The man survived the PE, but Dr. Hecht and his colleagues began to wonder how many patients refuse VTE prophylaxis. So they investigated, and it turned out that from December 2010 to February 2011, 26.4% of the prescribed doses of prophylaxis on the medicine floors they studied were missed. Moreover, nearly 80% of all missed doses on the medicine floors were due to patient refusal.
“It was astonishing to me that it was that high,” Dr. Hecht says. “If there were 1,000 doses in a month, 260 of them were not being given—and 205 of them were not given because they were refused.”
Checklist Integration
So Dr. Hecht and colleagues set out to create a checklist that could be used daily on multidisciplinary rounds to help reduce the risk of VTE. First question on the list: Has prophylaxis been ordered, and if so, is the patient refusing it? Knowing that patients are “refusing” medication can lead to discussions about why that is happening, which in turn can lead to ways to convince the patient that the preventative measure is a good idea.
Dr. Hecht says the team also realized a checklist creates the opportunity to improve other quality metrics, such as hospital-associated infections (HAIs). Two questions on the checklist ask whether indwelling urinary catheters (IUCs) and central venous catheters (CVCs) can be removed. Two questions ask if telemetry can be stopped and whether there are any pain-management concerns. A final query asks whether there are any nursing, social work, or discharge-related questions—a step that, according to Dr. Hecht, loops the entire multidisciplinary team into the care-plan discussion.
“An ongoing challenge is making sure it’s not just questions being asked and being answered by rote,” Dr. Hecht says. “Just pause and think for just a second for each question. You can get through the checklist in 10 seconds, but you can’t go through the checklist in two seconds.”
The project’s results are what made it a finalist. After the checklist intervention, the number of missed doses of VTE prophylaxis plummeted 59% to just 10.9% (P<0.001) from September to November 2012; the number of “patient refused” doses dropped to 6.3% (P<0.001).
Not only was Dr. Hecht caught off guard by his findings, but so were the judges who visited his poster—Mangla Gulati, MD, FHM, of the University of Maryland School of Medicine and Rachel George, MD, MBA, FHM, of Cogent HMG.
“I wonder if it’s like that in every hospital,” Dr. George says. “I’d like to know.”
The positive reaction and feedback to Dr. Hecht’s poster, however, was not enough to win the Innovations category. That honor went to “SEPTRIS: Improving Sepsis Recognition and Management Through a Mobile Educational Game,” which was developed by a team of researchers at Stanford University in Palo Alto, Calif. The video game
(http://med.stanford.edu/septris/)—a mashup of sepsis and the once-popular Tetris puzzle game—already has been played 17,000 times and is on its way to being shared in other languages.
“Win or lose, it doesn’t matter,” Dr. Hecht says. “The goal is to share your information with other people and learn from them.”
Peter Watson, MD, FACP, FHM, sees it the same way. That’s why this year he was both judge and judged. The division head of hospital medicine for Henry Ford Medical Group in Detroit was part of a group presenting “Feasibility and Efficacy of a Specialized Pilot Training Program to Enhance Inpatient Communication Skills of Hospitalists.” He was a judge for the Research portion of the contest. He says he’s hard-pressed to say which process he enjoyed more, but one trick of the poster trade he passes along is that “judging actually makes you a better presenter on the back end,” especially when it comes to describing in less than five minutes a poster whose work may date back 12 to 18 months.
“In your brain,” he says, “you have a Tolstoy novel of information, but you have to break that down into a paragraph of CliffsNotes, and actually convince the people that are judging you that you have a really cool project that either is going to have a big impact in the field or may lead to other big studies or is going to impress somebody so much that they’re going to go back to their institution and say, ‘Hey, I’m going to do that.’”
Dr. Watson also urges people not to be discouraged by not winning the poster contest. First, all of the accepted abstracts get published online (www.shmabstracts.com) by the Journal of Hospital Medicine, a high point for medical students, residents, and early-career physicians looking to make a mark. Second, presenting information of value to one’s peers is the definition of a specialty that prides itself on collaboration.
“To see a second-year medical student presenting all the way up to a very senior division chief and everything in between is a really good example for our profession,” he says. “That’s really the magic of this meeting.”
Richard Quinn is a freelance writer in New Jersey.
Speakers at HM13 Stress Overarching Reform, Day-to-Day Implementation
To some HM13 attendees, the keynote speakers might have seemed to be talking about different things.
Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer and director of the Center for Clinical Standards and Quality at the Centers for Medicare & Medicaid Services (CMS), hinted at promising results from the first accountable-care organizations (ACOs) and noted a meaningful reduction in 30-day readmission rates for the first time in years.
David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles, told hospitalists that unless they’re getting patient care right every time, they’re not getting it right enough. And nothing would make him happier than seeing fewer hospitalists at SHM’s annual meeting—because that would mean fewer hospitalized patients.
HM pioneer Bob Wachter, MD, MHM, said it’s time for hospitalists to link their quality-improvement (QI) efforts and safety acumen to projects focused on cutting costs and reducing waste in the health-care system.
So while each made their points in a different way, each plenary speaker left many meeting-goers with a similar thought: Hospitalists are positioned at the nexus of big-picture reform and day-to-day implementation. So if hospitalists as a specialty continue to embrace teamwork, evidence-based practice, quality, safety, and a sense that the patient comes first, they will cement themselves as leaders in the next iteration of health-care delivery.
“There is enormous change going on in the healthcare system,” says SHM CEO Larry Wellikson. “And we are right in the middle of this. We are essential. If we are bad, we are going to sink it. And if we’re great, we are going to take it to another level.”
Needle Movement
Dr. Conway said some of that progress already is evident. He disclosed that initial findings from the first data sets coming from the first ACOs are showing promising results, though he can’t go into detail until the information is publicly released. However, he did boast that after decades of Medicare readmission rates hovering around 19%, data from late 2012 and early 2013 show that figure has dropped to below 18%.
“That is a 1.5% to 2% shift in readmissions nationally,” he said. “It is a credit to the work you and others are doing in the field. That’s hundreds of thousands of Medicare beneficiaries that are not readmitted every year, that stay home healthy. … It’s a tremendous example of moving a national needle.”
He dismissed those who attribute the initial readmission progress solely to penalties instituted on readmissions, though he acknowledged that CMS is using both carrots and sticks to push change.
“It’s a combination of interventions,” he said.
And all of those initiatives must be aimed jointly at improving the patient experience, said Dr. Feinberg, a child psychiatrist by training whose mantra is “patient-centeredness.” Dr. Feinberg’s reputation is that of a physician-administrator who puts patients first. For example, even though his health system (www.uclahealth.org) is in the 99th percentile for patient satisfaction, he is unhappy. That’s because the top ranking means roughly 85 out of every 100 patients served are pretty happy with their experience.
“It means that we’re the cream of the crap,” he said. “Of the last 100 people we took care of, 15 of them—and, by definition, those 15 people are someone’s mom, someone’s brother, someone’s coworker—would not refer us to a friend, or rate us a 9 or 10. So, I think, while we’ve really moved the needle, we’re really not done until we get it right with every patient, every time.”
He added that those who argue against difficult or time-consuming innovations and improvements that better patient care are arguing against the moral high ground of how they would want a family member to be treated in the hospital.
“The pushback I hear is, ‘Some of this stuff is unpreventable,’” Dr. Feinberg said. “Well, maybe it’s unpreventable the way we’re doing it now. But maybe we need to think differently. Maybe it is unpreventable, but if this decreases the prevalence, or makes it better, then to me, it’s important to do.”
Dr. Feinberg, who took over as UCLA Health System’s president in 2011, says he still spends several hours every day talking to patients. For those who say there’s not enough time to stay connected to patients and that all the time spent making sure patients are happy takes away from other activities, he says they’re forgetting what brought them into medicine in the first place: healing. He blames the delivery system for stifling what he believes is a provider’s desire to help people.
“We haven’t allowed the culture to come out,” he said. “I think it’s there.”
Dr. Wachter has a similar faith in the hospitalist culture—although his is based in the pluripotent nature of the specialty. Hospitalists have worked hard to be viewed as “generalists, able to solve all kinds of problems,” and that means the specialty is poised to adapt and thrive.
“We will morph into what is needed,” said Dr. Wachter, a past president of SHM whose titles include chief of the division of hospital medicine at the University of California at San Francisco and chair of the American Board of Internal Medicine. “That will be all sorts of things: comanagement, dealing with the residency limits in teaching hospitals, systems improvement, cost reductions, transitions, working in skilled nursing facilities, all the specialty hospitalists.
“We will fill new niches,” he said.
What Dr. Wachter does not want to see is that the field grows “fat and happy,” as it is now firmly entrenched in the U.S. health-care delivery system. In fact, he urged hospitalists to welcome change, particularly initiatives that improve quality and safety, reduce costs and waste, and, ultimately, improve the patient experience.
But he cautioned against conceptually separating QI and cost reduction. Instead, they should be viewed as equally meaningful parts of his oft-quoted value equation, which, viewed from the health-care consumer’s point of view, is quality divided by cost.
“You can’t survive and thrive in a world with the kinds of pressures that we have to improve performance if you do business the same old way,” he added. “It’s no longer possible to achieve the things you need to achieve handling these as single projects. You need to transform the way you think about care.”
Richard Quinn is a freelance writer in New Jersey.
To some HM13 attendees, the keynote speakers might have seemed to be talking about different things.
Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer and director of the Center for Clinical Standards and Quality at the Centers for Medicare & Medicaid Services (CMS), hinted at promising results from the first accountable-care organizations (ACOs) and noted a meaningful reduction in 30-day readmission rates for the first time in years.
David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles, told hospitalists that unless they’re getting patient care right every time, they’re not getting it right enough. And nothing would make him happier than seeing fewer hospitalists at SHM’s annual meeting—because that would mean fewer hospitalized patients.
HM pioneer Bob Wachter, MD, MHM, said it’s time for hospitalists to link their quality-improvement (QI) efforts and safety acumen to projects focused on cutting costs and reducing waste in the health-care system.
So while each made their points in a different way, each plenary speaker left many meeting-goers with a similar thought: Hospitalists are positioned at the nexus of big-picture reform and day-to-day implementation. So if hospitalists as a specialty continue to embrace teamwork, evidence-based practice, quality, safety, and a sense that the patient comes first, they will cement themselves as leaders in the next iteration of health-care delivery.
“There is enormous change going on in the healthcare system,” says SHM CEO Larry Wellikson. “And we are right in the middle of this. We are essential. If we are bad, we are going to sink it. And if we’re great, we are going to take it to another level.”
Needle Movement
Dr. Conway said some of that progress already is evident. He disclosed that initial findings from the first data sets coming from the first ACOs are showing promising results, though he can’t go into detail until the information is publicly released. However, he did boast that after decades of Medicare readmission rates hovering around 19%, data from late 2012 and early 2013 show that figure has dropped to below 18%.
“That is a 1.5% to 2% shift in readmissions nationally,” he said. “It is a credit to the work you and others are doing in the field. That’s hundreds of thousands of Medicare beneficiaries that are not readmitted every year, that stay home healthy. … It’s a tremendous example of moving a national needle.”
He dismissed those who attribute the initial readmission progress solely to penalties instituted on readmissions, though he acknowledged that CMS is using both carrots and sticks to push change.
“It’s a combination of interventions,” he said.
And all of those initiatives must be aimed jointly at improving the patient experience, said Dr. Feinberg, a child psychiatrist by training whose mantra is “patient-centeredness.” Dr. Feinberg’s reputation is that of a physician-administrator who puts patients first. For example, even though his health system (www.uclahealth.org) is in the 99th percentile for patient satisfaction, he is unhappy. That’s because the top ranking means roughly 85 out of every 100 patients served are pretty happy with their experience.
“It means that we’re the cream of the crap,” he said. “Of the last 100 people we took care of, 15 of them—and, by definition, those 15 people are someone’s mom, someone’s brother, someone’s coworker—would not refer us to a friend, or rate us a 9 or 10. So, I think, while we’ve really moved the needle, we’re really not done until we get it right with every patient, every time.”
He added that those who argue against difficult or time-consuming innovations and improvements that better patient care are arguing against the moral high ground of how they would want a family member to be treated in the hospital.
“The pushback I hear is, ‘Some of this stuff is unpreventable,’” Dr. Feinberg said. “Well, maybe it’s unpreventable the way we’re doing it now. But maybe we need to think differently. Maybe it is unpreventable, but if this decreases the prevalence, or makes it better, then to me, it’s important to do.”
Dr. Feinberg, who took over as UCLA Health System’s president in 2011, says he still spends several hours every day talking to patients. For those who say there’s not enough time to stay connected to patients and that all the time spent making sure patients are happy takes away from other activities, he says they’re forgetting what brought them into medicine in the first place: healing. He blames the delivery system for stifling what he believes is a provider’s desire to help people.
“We haven’t allowed the culture to come out,” he said. “I think it’s there.”
Dr. Wachter has a similar faith in the hospitalist culture—although his is based in the pluripotent nature of the specialty. Hospitalists have worked hard to be viewed as “generalists, able to solve all kinds of problems,” and that means the specialty is poised to adapt and thrive.
“We will morph into what is needed,” said Dr. Wachter, a past president of SHM whose titles include chief of the division of hospital medicine at the University of California at San Francisco and chair of the American Board of Internal Medicine. “That will be all sorts of things: comanagement, dealing with the residency limits in teaching hospitals, systems improvement, cost reductions, transitions, working in skilled nursing facilities, all the specialty hospitalists.
“We will fill new niches,” he said.
What Dr. Wachter does not want to see is that the field grows “fat and happy,” as it is now firmly entrenched in the U.S. health-care delivery system. In fact, he urged hospitalists to welcome change, particularly initiatives that improve quality and safety, reduce costs and waste, and, ultimately, improve the patient experience.
But he cautioned against conceptually separating QI and cost reduction. Instead, they should be viewed as equally meaningful parts of his oft-quoted value equation, which, viewed from the health-care consumer’s point of view, is quality divided by cost.
“You can’t survive and thrive in a world with the kinds of pressures that we have to improve performance if you do business the same old way,” he added. “It’s no longer possible to achieve the things you need to achieve handling these as single projects. You need to transform the way you think about care.”
Richard Quinn is a freelance writer in New Jersey.
To some HM13 attendees, the keynote speakers might have seemed to be talking about different things.
Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer and director of the Center for Clinical Standards and Quality at the Centers for Medicare & Medicaid Services (CMS), hinted at promising results from the first accountable-care organizations (ACOs) and noted a meaningful reduction in 30-day readmission rates for the first time in years.
David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles, told hospitalists that unless they’re getting patient care right every time, they’re not getting it right enough. And nothing would make him happier than seeing fewer hospitalists at SHM’s annual meeting—because that would mean fewer hospitalized patients.
HM pioneer Bob Wachter, MD, MHM, said it’s time for hospitalists to link their quality-improvement (QI) efforts and safety acumen to projects focused on cutting costs and reducing waste in the health-care system.
So while each made their points in a different way, each plenary speaker left many meeting-goers with a similar thought: Hospitalists are positioned at the nexus of big-picture reform and day-to-day implementation. So if hospitalists as a specialty continue to embrace teamwork, evidence-based practice, quality, safety, and a sense that the patient comes first, they will cement themselves as leaders in the next iteration of health-care delivery.
“There is enormous change going on in the healthcare system,” says SHM CEO Larry Wellikson. “And we are right in the middle of this. We are essential. If we are bad, we are going to sink it. And if we’re great, we are going to take it to another level.”
Needle Movement
Dr. Conway said some of that progress already is evident. He disclosed that initial findings from the first data sets coming from the first ACOs are showing promising results, though he can’t go into detail until the information is publicly released. However, he did boast that after decades of Medicare readmission rates hovering around 19%, data from late 2012 and early 2013 show that figure has dropped to below 18%.
“That is a 1.5% to 2% shift in readmissions nationally,” he said. “It is a credit to the work you and others are doing in the field. That’s hundreds of thousands of Medicare beneficiaries that are not readmitted every year, that stay home healthy. … It’s a tremendous example of moving a national needle.”
He dismissed those who attribute the initial readmission progress solely to penalties instituted on readmissions, though he acknowledged that CMS is using both carrots and sticks to push change.
“It’s a combination of interventions,” he said.
And all of those initiatives must be aimed jointly at improving the patient experience, said Dr. Feinberg, a child psychiatrist by training whose mantra is “patient-centeredness.” Dr. Feinberg’s reputation is that of a physician-administrator who puts patients first. For example, even though his health system (www.uclahealth.org) is in the 99th percentile for patient satisfaction, he is unhappy. That’s because the top ranking means roughly 85 out of every 100 patients served are pretty happy with their experience.
“It means that we’re the cream of the crap,” he said. “Of the last 100 people we took care of, 15 of them—and, by definition, those 15 people are someone’s mom, someone’s brother, someone’s coworker—would not refer us to a friend, or rate us a 9 or 10. So, I think, while we’ve really moved the needle, we’re really not done until we get it right with every patient, every time.”
He added that those who argue against difficult or time-consuming innovations and improvements that better patient care are arguing against the moral high ground of how they would want a family member to be treated in the hospital.
“The pushback I hear is, ‘Some of this stuff is unpreventable,’” Dr. Feinberg said. “Well, maybe it’s unpreventable the way we’re doing it now. But maybe we need to think differently. Maybe it is unpreventable, but if this decreases the prevalence, or makes it better, then to me, it’s important to do.”
Dr. Feinberg, who took over as UCLA Health System’s president in 2011, says he still spends several hours every day talking to patients. For those who say there’s not enough time to stay connected to patients and that all the time spent making sure patients are happy takes away from other activities, he says they’re forgetting what brought them into medicine in the first place: healing. He blames the delivery system for stifling what he believes is a provider’s desire to help people.
“We haven’t allowed the culture to come out,” he said. “I think it’s there.”
Dr. Wachter has a similar faith in the hospitalist culture—although his is based in the pluripotent nature of the specialty. Hospitalists have worked hard to be viewed as “generalists, able to solve all kinds of problems,” and that means the specialty is poised to adapt and thrive.
“We will morph into what is needed,” said Dr. Wachter, a past president of SHM whose titles include chief of the division of hospital medicine at the University of California at San Francisco and chair of the American Board of Internal Medicine. “That will be all sorts of things: comanagement, dealing with the residency limits in teaching hospitals, systems improvement, cost reductions, transitions, working in skilled nursing facilities, all the specialty hospitalists.
“We will fill new niches,” he said.
What Dr. Wachter does not want to see is that the field grows “fat and happy,” as it is now firmly entrenched in the U.S. health-care delivery system. In fact, he urged hospitalists to welcome change, particularly initiatives that improve quality and safety, reduce costs and waste, and, ultimately, improve the patient experience.
But he cautioned against conceptually separating QI and cost reduction. Instead, they should be viewed as equally meaningful parts of his oft-quoted value equation, which, viewed from the health-care consumer’s point of view, is quality divided by cost.
“You can’t survive and thrive in a world with the kinds of pressures that we have to improve performance if you do business the same old way,” he added. “It’s no longer possible to achieve the things you need to achieve handling these as single projects. You need to transform the way you think about care.”
Richard Quinn is a freelance writer in New Jersey.
Health-Care Journalists Tackle Barriers to Hospital Safety Records
The Association of Health Care Journalists, a professional association that includes 1,400 journalists, is tackling some of the barriers consumers and advocates face when trying to access such information as hospital safety records. AHCJ’s www.HospitalInfections.org is a free, searchable news application that went live in March with detailed reports of deficiencies cited in federal inspection visits for acute- and critical-access hospitals nationwide.
Through years of advocacy, AHCJ has filed Freedom of Information Act requests and negotiated with the Centers for Medicare & Medicaid Services (CMS) to get access to hospital safety information in electronic form.
CMS’ Hospital Compare website (www.medicare.gov/hospitalcompare) and the Joint Commission’s Quality Check (www.qualitycheck.org) program both publicly report hospital quality data, but they have significant time lags and data that are difficult for the average consumer to understand, according to AHCJ. The association touts its new site as an “early attempt by an advocacy group to make hospital safety information easier to access and more consumer-driven.”
“Being able to easily review the performance of your local hospital is vital for health-care journalists and for the public,” AHCJ president Charles Ornstein, a senior reporter at ProPublica in New York, said in a statement.
Larry Beresford is a freelance writer in San Francisco
References
- Weigel C, Suen W, Gupta G. Using Lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013 Feb 4 [Epub ahead of print].
- Morganti KG, Lovejoy S, Beckjord EB, Haviland AM, Haas AC, Farley DO. A retrospective evaluation of the Perfecting Patient Care University training program for health care organizations. Am J Med Qual. 2013 Apr 9 [Epub ahead of print].
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators’ Academy: fulfilling an unmet need for faculty development. Am J Med Qual. 2013 Apr 11 [Epub ahead of print].
- Dong XQ, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 Apr 8:1-7. doi: 10.1001/jamainternmed.2013.238 [Epub ahead of print].
- Cisco mConcierge. 90% American workers use their own smartphones for work. Cisco mConcierge website. Available at: http://www.ciscomcon.com/sw/swchannel/registration/internet/registrationcfm?SWAPPID=91&RegPageID=350200&SWTHEMEID=12949. Accessed
The Association of Health Care Journalists, a professional association that includes 1,400 journalists, is tackling some of the barriers consumers and advocates face when trying to access such information as hospital safety records. AHCJ’s www.HospitalInfections.org is a free, searchable news application that went live in March with detailed reports of deficiencies cited in federal inspection visits for acute- and critical-access hospitals nationwide.
Through years of advocacy, AHCJ has filed Freedom of Information Act requests and negotiated with the Centers for Medicare & Medicaid Services (CMS) to get access to hospital safety information in electronic form.
CMS’ Hospital Compare website (www.medicare.gov/hospitalcompare) and the Joint Commission’s Quality Check (www.qualitycheck.org) program both publicly report hospital quality data, but they have significant time lags and data that are difficult for the average consumer to understand, according to AHCJ. The association touts its new site as an “early attempt by an advocacy group to make hospital safety information easier to access and more consumer-driven.”
“Being able to easily review the performance of your local hospital is vital for health-care journalists and for the public,” AHCJ president Charles Ornstein, a senior reporter at ProPublica in New York, said in a statement.
Larry Beresford is a freelance writer in San Francisco
References
- Weigel C, Suen W, Gupta G. Using Lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013 Feb 4 [Epub ahead of print].
- Morganti KG, Lovejoy S, Beckjord EB, Haviland AM, Haas AC, Farley DO. A retrospective evaluation of the Perfecting Patient Care University training program for health care organizations. Am J Med Qual. 2013 Apr 9 [Epub ahead of print].
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators’ Academy: fulfilling an unmet need for faculty development. Am J Med Qual. 2013 Apr 11 [Epub ahead of print].
- Dong XQ, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 Apr 8:1-7. doi: 10.1001/jamainternmed.2013.238 [Epub ahead of print].
- Cisco mConcierge. 90% American workers use their own smartphones for work. Cisco mConcierge website. Available at: http://www.ciscomcon.com/sw/swchannel/registration/internet/registrationcfm?SWAPPID=91&RegPageID=350200&SWTHEMEID=12949. Accessed
The Association of Health Care Journalists, a professional association that includes 1,400 journalists, is tackling some of the barriers consumers and advocates face when trying to access such information as hospital safety records. AHCJ’s www.HospitalInfections.org is a free, searchable news application that went live in March with detailed reports of deficiencies cited in federal inspection visits for acute- and critical-access hospitals nationwide.
Through years of advocacy, AHCJ has filed Freedom of Information Act requests and negotiated with the Centers for Medicare & Medicaid Services (CMS) to get access to hospital safety information in electronic form.
CMS’ Hospital Compare website (www.medicare.gov/hospitalcompare) and the Joint Commission’s Quality Check (www.qualitycheck.org) program both publicly report hospital quality data, but they have significant time lags and data that are difficult for the average consumer to understand, according to AHCJ. The association touts its new site as an “early attempt by an advocacy group to make hospital safety information easier to access and more consumer-driven.”
“Being able to easily review the performance of your local hospital is vital for health-care journalists and for the public,” AHCJ president Charles Ornstein, a senior reporter at ProPublica in New York, said in a statement.
Larry Beresford is a freelance writer in San Francisco
References
- Weigel C, Suen W, Gupta G. Using Lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013 Feb 4 [Epub ahead of print].
- Morganti KG, Lovejoy S, Beckjord EB, Haviland AM, Haas AC, Farley DO. A retrospective evaluation of the Perfecting Patient Care University training program for health care organizations. Am J Med Qual. 2013 Apr 9 [Epub ahead of print].
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators’ Academy: fulfilling an unmet need for faculty development. Am J Med Qual. 2013 Apr 11 [Epub ahead of print].
- Dong XQ, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 Apr 8:1-7. doi: 10.1001/jamainternmed.2013.238 [Epub ahead of print].
- Cisco mConcierge. 90% American workers use their own smartphones for work. Cisco mConcierge website. Available at: http://www.ciscomcon.com/sw/swchannel/registration/internet/registrationcfm?SWAPPID=91&RegPageID=350200&SWTHEMEID=12949. Accessed
Medical Centers Take Tips from Other Industries
Curriculums using Lean quality-improvement (QI) principles and techniques are becoming entrenched in medical teaching programs across the country.
A curriculum based on Lean QI is teaching medical residents at Boston Medical Center techniques based on successes in manufacturing and service industries, according to Charlene Weigel, MD, who now works as a hospitalist at Mount Auburn Hospital in Cambridge, Mass. Residents also are learning about implementation of Lean principles at the medical center, Dr. Weigel and co-authors report in a study published in the American Journal of Medical Quality.1
“In Week One, we gave an introduction to QI and explained what Lean means,” Dr. Weigel says. Three other interactive sessions explored such techniques as how to create process maps and root-cause analysis, and identifying steps that aren’t helpful. The 90 residents and eight Boston University School of Public Health students also created 17 group QI project plans. “The goal was for the QI classwork and ideas to become implemented in hospital QI projects, but logistically, we had to scale back expectations for that initial go-round,” Dr. Weigel says.
The medical center recently started a second cycle of the QI course, with students from the first cycle encouraged to continue their QI projects on their own. One group submitted its project as an Institute for Healthcare Improvement storyboard at a national meeting.
“The experience also exposed the residents to our interprofessional team structure, which reflects their future working relationships and professional roles in QI,” Dr. Weigel says.
Lean concepts also are the basis for the Perfecting Patient Care University (PPCU, www.prhi.org/perfecting-patient-care/what-is-ppc), a QI training program for health-care leaders and clinicians offered in a variety of formats by the Pittsburgh Regional Health Initiative, a regional health collaborative. An evaluation of outcomes at PPCU was published online in the American Journal of Medical Quality in April.2 The same journal also describes the curriculum, program evaluation, and lessons learned by SHM’s Quality and Safety Educators Academy (http://sites.hospitalmedicine.org/qsea), which provides training in QI and patient safety for teaching faculty.3 The academy, a 2.5-day course, is co-sponsored by the Alliance for Academic Internal Medicine.
Larry Beresford is a freelance writer in San Francisco
References
- Weigel C, Suen W, Gupta G. Using Lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013 Feb 4 [Epub ahead of print].
- Morganti KG, Lovejoy S, Beckjord EB, Haviland AM, Haas AC, Farley DO. A retrospective evaluation of the Perfecting Patient Care University training program for health care organizations. Am J Med Qual. 2013 Apr 9 [Epub ahead of print].
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators’ Academy: fulfilling an unmet need for faculty development. Am J Med Qual. 2013 Apr 11 [Epub ahead of print].
- Dong XQ, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 Apr 8:1-7. doi: 10.1001/jamainternmed.2013.238 [Epub ahead of print].
- Cisco mConcierge. 90% American workers use their own smartphones for work. Cisco mConcierge website. Available at: http://www.ciscomcon.com/sw/swchannel/registration/internet/registrationcfm?SWAPPID=91&RegPageID=350200&SWTHEMEID=12949. Accessed
Curriculums using Lean quality-improvement (QI) principles and techniques are becoming entrenched in medical teaching programs across the country.
A curriculum based on Lean QI is teaching medical residents at Boston Medical Center techniques based on successes in manufacturing and service industries, according to Charlene Weigel, MD, who now works as a hospitalist at Mount Auburn Hospital in Cambridge, Mass. Residents also are learning about implementation of Lean principles at the medical center, Dr. Weigel and co-authors report in a study published in the American Journal of Medical Quality.1
“In Week One, we gave an introduction to QI and explained what Lean means,” Dr. Weigel says. Three other interactive sessions explored such techniques as how to create process maps and root-cause analysis, and identifying steps that aren’t helpful. The 90 residents and eight Boston University School of Public Health students also created 17 group QI project plans. “The goal was for the QI classwork and ideas to become implemented in hospital QI projects, but logistically, we had to scale back expectations for that initial go-round,” Dr. Weigel says.
The medical center recently started a second cycle of the QI course, with students from the first cycle encouraged to continue their QI projects on their own. One group submitted its project as an Institute for Healthcare Improvement storyboard at a national meeting.
“The experience also exposed the residents to our interprofessional team structure, which reflects their future working relationships and professional roles in QI,” Dr. Weigel says.
Lean concepts also are the basis for the Perfecting Patient Care University (PPCU, www.prhi.org/perfecting-patient-care/what-is-ppc), a QI training program for health-care leaders and clinicians offered in a variety of formats by the Pittsburgh Regional Health Initiative, a regional health collaborative. An evaluation of outcomes at PPCU was published online in the American Journal of Medical Quality in April.2 The same journal also describes the curriculum, program evaluation, and lessons learned by SHM’s Quality and Safety Educators Academy (http://sites.hospitalmedicine.org/qsea), which provides training in QI and patient safety for teaching faculty.3 The academy, a 2.5-day course, is co-sponsored by the Alliance for Academic Internal Medicine.
Larry Beresford is a freelance writer in San Francisco
References
- Weigel C, Suen W, Gupta G. Using Lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013 Feb 4 [Epub ahead of print].
- Morganti KG, Lovejoy S, Beckjord EB, Haviland AM, Haas AC, Farley DO. A retrospective evaluation of the Perfecting Patient Care University training program for health care organizations. Am J Med Qual. 2013 Apr 9 [Epub ahead of print].
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators’ Academy: fulfilling an unmet need for faculty development. Am J Med Qual. 2013 Apr 11 [Epub ahead of print].
- Dong XQ, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 Apr 8:1-7. doi: 10.1001/jamainternmed.2013.238 [Epub ahead of print].
- Cisco mConcierge. 90% American workers use their own smartphones for work. Cisco mConcierge website. Available at: http://www.ciscomcon.com/sw/swchannel/registration/internet/registrationcfm?SWAPPID=91&RegPageID=350200&SWTHEMEID=12949. Accessed
Curriculums using Lean quality-improvement (QI) principles and techniques are becoming entrenched in medical teaching programs across the country.
A curriculum based on Lean QI is teaching medical residents at Boston Medical Center techniques based on successes in manufacturing and service industries, according to Charlene Weigel, MD, who now works as a hospitalist at Mount Auburn Hospital in Cambridge, Mass. Residents also are learning about implementation of Lean principles at the medical center, Dr. Weigel and co-authors report in a study published in the American Journal of Medical Quality.1
“In Week One, we gave an introduction to QI and explained what Lean means,” Dr. Weigel says. Three other interactive sessions explored such techniques as how to create process maps and root-cause analysis, and identifying steps that aren’t helpful. The 90 residents and eight Boston University School of Public Health students also created 17 group QI project plans. “The goal was for the QI classwork and ideas to become implemented in hospital QI projects, but logistically, we had to scale back expectations for that initial go-round,” Dr. Weigel says.
The medical center recently started a second cycle of the QI course, with students from the first cycle encouraged to continue their QI projects on their own. One group submitted its project as an Institute for Healthcare Improvement storyboard at a national meeting.
“The experience also exposed the residents to our interprofessional team structure, which reflects their future working relationships and professional roles in QI,” Dr. Weigel says.
Lean concepts also are the basis for the Perfecting Patient Care University (PPCU, www.prhi.org/perfecting-patient-care/what-is-ppc), a QI training program for health-care leaders and clinicians offered in a variety of formats by the Pittsburgh Regional Health Initiative, a regional health collaborative. An evaluation of outcomes at PPCU was published online in the American Journal of Medical Quality in April.2 The same journal also describes the curriculum, program evaluation, and lessons learned by SHM’s Quality and Safety Educators Academy (http://sites.hospitalmedicine.org/qsea), which provides training in QI and patient safety for teaching faculty.3 The academy, a 2.5-day course, is co-sponsored by the Alliance for Academic Internal Medicine.
Larry Beresford is a freelance writer in San Francisco
References
- Weigel C, Suen W, Gupta G. Using Lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013 Feb 4 [Epub ahead of print].
- Morganti KG, Lovejoy S, Beckjord EB, Haviland AM, Haas AC, Farley DO. A retrospective evaluation of the Perfecting Patient Care University training program for health care organizations. Am J Med Qual. 2013 Apr 9 [Epub ahead of print].
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators’ Academy: fulfilling an unmet need for faculty development. Am J Med Qual. 2013 Apr 11 [Epub ahead of print].
- Dong XQ, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 Apr 8:1-7. doi: 10.1001/jamainternmed.2013.238 [Epub ahead of print].
- Cisco mConcierge. 90% American workers use their own smartphones for work. Cisco mConcierge website. Available at: http://www.ciscomcon.com/sw/swchannel/registration/internet/registrationcfm?SWAPPID=91&RegPageID=350200&SWTHEMEID=12949. Accessed
Hospitalists Can Get Ahead Through Quality and Patient Safety Initiatives
Are you a hospitalist who, on daily rounds, often thinks, “There’s got to be a better way to do this”? You might be just the type of person who can carve a niche for yourself in hospital quality and patient safety—and advance your career in the process.
Successful navigation of the quality-improvement (QI) and patient-safety domains, according to three veteran hospitalists, requires an initial passion and an incremental approach. Now is an especially good time, they agree, for young hospitalists to engage in these types of initiatives.
Why Do It?
In her capacity as president of the Mid-Atlantic Business Unit for Brentwood, Tenn.-based CogentHMG, Julia Wright, MD, SFHM, FACP, often encourages young recruits to consider participation in QI and patient-safety initiatives. She admits that the transition from residency to a busy HM practice, with its higher patient volumes and a faster pace, can be daunting at first. Still, she tries to cultivate interest in initiatives and establish a realistic timeframe for involvement.
There are many reasons to consider this as a career step. Dr. Wright says that quality and patient safety dovetail with hospitalists’ initial reasons for choosing medicine: to improve patients’ lives.
Janet Nagamine, RN, MD, SFHM, former patient safety officer and assistant chief of quality at Kaiser Permanente in Santa Clara, Calif., describes the fit this way: “I might be a good doctor, but as a hospitalist, I rely on many others within the system to deliver, so my patients can’t get good care until the entire system is running well,” she says. “There are all kinds of opportunities to fix our [hospital] system, and I really believe that hospitalists cannot separate themselves from that engagement.”
Elizabeth Gundersen, MD, FHM, of Fort Lauderdale, Fla., agrees that it’s a natural step to think about the ways to make a difference on a larger level. At her former institution, the University of Massachusetts (UMass) Medical School in Worcester, she parlayed her interest in QI to work her way up from ground-level hospitalist to associate chief of her division and quality officer for the hospital. “Physicians get a lot of satisfaction from helping individual patients,” she says. “One thing I really liked about getting involved with quality improvement was being able to make a difference for patients on a systems level.”
An Incremental Path
The path to her current position began with a very specific issue for Dr. Nagamine, an SHM board member who also serves as a Project BOOST co-investigator. “Although I have been doing patient safety since before they had a name for it, I didn’t start out saying that I wanted a career in quality and safety,” she says. “I was trying to take better care of my patients with diabetes, but controlling their glucose was extremely challenging because all the related variables—timing and amount of their insulin dosage, when and how much they had eaten—were charted in different places. This made it hard to adjust their insulin appropriately.”
It quickly became clear to Dr. Nagamine that the solution had to be systemic. She realized that something as basic as taking care of her patients with diabetes required multiple departments (i.e. dietary, nursing, and pharmacy) to furnish information in an integrated manner. So she joined the diabetes committee and went to work on the issue. She helped devise a flow chart that could be used by all relevant departments. A further evolution on the path emanated from one of her patients receiving the wrong medication. She joined the medication safety committee, became chair, “and the next thing you know, I’m in charge of patient safety, and an assistant chief of quality.”
Training Is Necessary
QI and patient-safety methodologies have become sophisticated disciplines in the past two decades, Dr. Wright says. Access to training in QI basics now is readily available to early-career hospitalists. For example, CogentHMG offers program support for QI so that anyone interested “doesn’t have to start from scratch anymore; we can help show them the way and support them in doing it.”
This month, HM13 (www.hospital medicine2013.org)—just outside Washington, D.C.—will offer multiple sessions on quality, as well as the “Initiating Quality Improvement Projects with Built-In Sustainment” workshop, led by Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) core investigator Peter Kaboli, MD, MS, who will address sustainability.
Beyond methodological tools, success in quality and patient safety requires the ability to motivate people, often across multiple disciplines, Dr. Nagamine says. “If you want things to work better, you must invite the right people to the table. For example, we often forget to include key nonclinical stakeholders,” she adds.
When working with hospitals across the country to implement rapid-response tTeams, Dr. Nagamine often reminds them to invite the operators, or “key people,” in the process.
“If you put patient safety at the core of your initiative and create the context for that, most people will agree that it’s the right thing to do and will get on board, even if it’s an extra step for them,” she says. “Know your audience, listen to their perspective, and learn what matters to them. And to most people, it matters that they give good patient care.”
Gretchen Henkel is a freelance writer in California.
Are you a hospitalist who, on daily rounds, often thinks, “There’s got to be a better way to do this”? You might be just the type of person who can carve a niche for yourself in hospital quality and patient safety—and advance your career in the process.
Successful navigation of the quality-improvement (QI) and patient-safety domains, according to three veteran hospitalists, requires an initial passion and an incremental approach. Now is an especially good time, they agree, for young hospitalists to engage in these types of initiatives.
Why Do It?
In her capacity as president of the Mid-Atlantic Business Unit for Brentwood, Tenn.-based CogentHMG, Julia Wright, MD, SFHM, FACP, often encourages young recruits to consider participation in QI and patient-safety initiatives. She admits that the transition from residency to a busy HM practice, with its higher patient volumes and a faster pace, can be daunting at first. Still, she tries to cultivate interest in initiatives and establish a realistic timeframe for involvement.
There are many reasons to consider this as a career step. Dr. Wright says that quality and patient safety dovetail with hospitalists’ initial reasons for choosing medicine: to improve patients’ lives.
Janet Nagamine, RN, MD, SFHM, former patient safety officer and assistant chief of quality at Kaiser Permanente in Santa Clara, Calif., describes the fit this way: “I might be a good doctor, but as a hospitalist, I rely on many others within the system to deliver, so my patients can’t get good care until the entire system is running well,” she says. “There are all kinds of opportunities to fix our [hospital] system, and I really believe that hospitalists cannot separate themselves from that engagement.”
Elizabeth Gundersen, MD, FHM, of Fort Lauderdale, Fla., agrees that it’s a natural step to think about the ways to make a difference on a larger level. At her former institution, the University of Massachusetts (UMass) Medical School in Worcester, she parlayed her interest in QI to work her way up from ground-level hospitalist to associate chief of her division and quality officer for the hospital. “Physicians get a lot of satisfaction from helping individual patients,” she says. “One thing I really liked about getting involved with quality improvement was being able to make a difference for patients on a systems level.”
An Incremental Path
The path to her current position began with a very specific issue for Dr. Nagamine, an SHM board member who also serves as a Project BOOST co-investigator. “Although I have been doing patient safety since before they had a name for it, I didn’t start out saying that I wanted a career in quality and safety,” she says. “I was trying to take better care of my patients with diabetes, but controlling their glucose was extremely challenging because all the related variables—timing and amount of their insulin dosage, when and how much they had eaten—were charted in different places. This made it hard to adjust their insulin appropriately.”
It quickly became clear to Dr. Nagamine that the solution had to be systemic. She realized that something as basic as taking care of her patients with diabetes required multiple departments (i.e. dietary, nursing, and pharmacy) to furnish information in an integrated manner. So she joined the diabetes committee and went to work on the issue. She helped devise a flow chart that could be used by all relevant departments. A further evolution on the path emanated from one of her patients receiving the wrong medication. She joined the medication safety committee, became chair, “and the next thing you know, I’m in charge of patient safety, and an assistant chief of quality.”
Training Is Necessary
QI and patient-safety methodologies have become sophisticated disciplines in the past two decades, Dr. Wright says. Access to training in QI basics now is readily available to early-career hospitalists. For example, CogentHMG offers program support for QI so that anyone interested “doesn’t have to start from scratch anymore; we can help show them the way and support them in doing it.”
This month, HM13 (www.hospital medicine2013.org)—just outside Washington, D.C.—will offer multiple sessions on quality, as well as the “Initiating Quality Improvement Projects with Built-In Sustainment” workshop, led by Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) core investigator Peter Kaboli, MD, MS, who will address sustainability.
Beyond methodological tools, success in quality and patient safety requires the ability to motivate people, often across multiple disciplines, Dr. Nagamine says. “If you want things to work better, you must invite the right people to the table. For example, we often forget to include key nonclinical stakeholders,” she adds.
When working with hospitals across the country to implement rapid-response tTeams, Dr. Nagamine often reminds them to invite the operators, or “key people,” in the process.
“If you put patient safety at the core of your initiative and create the context for that, most people will agree that it’s the right thing to do and will get on board, even if it’s an extra step for them,” she says. “Know your audience, listen to their perspective, and learn what matters to them. And to most people, it matters that they give good patient care.”
Gretchen Henkel is a freelance writer in California.
Are you a hospitalist who, on daily rounds, often thinks, “There’s got to be a better way to do this”? You might be just the type of person who can carve a niche for yourself in hospital quality and patient safety—and advance your career in the process.
Successful navigation of the quality-improvement (QI) and patient-safety domains, according to three veteran hospitalists, requires an initial passion and an incremental approach. Now is an especially good time, they agree, for young hospitalists to engage in these types of initiatives.
Why Do It?
In her capacity as president of the Mid-Atlantic Business Unit for Brentwood, Tenn.-based CogentHMG, Julia Wright, MD, SFHM, FACP, often encourages young recruits to consider participation in QI and patient-safety initiatives. She admits that the transition from residency to a busy HM practice, with its higher patient volumes and a faster pace, can be daunting at first. Still, she tries to cultivate interest in initiatives and establish a realistic timeframe for involvement.
There are many reasons to consider this as a career step. Dr. Wright says that quality and patient safety dovetail with hospitalists’ initial reasons for choosing medicine: to improve patients’ lives.
Janet Nagamine, RN, MD, SFHM, former patient safety officer and assistant chief of quality at Kaiser Permanente in Santa Clara, Calif., describes the fit this way: “I might be a good doctor, but as a hospitalist, I rely on many others within the system to deliver, so my patients can’t get good care until the entire system is running well,” she says. “There are all kinds of opportunities to fix our [hospital] system, and I really believe that hospitalists cannot separate themselves from that engagement.”
Elizabeth Gundersen, MD, FHM, of Fort Lauderdale, Fla., agrees that it’s a natural step to think about the ways to make a difference on a larger level. At her former institution, the University of Massachusetts (UMass) Medical School in Worcester, she parlayed her interest in QI to work her way up from ground-level hospitalist to associate chief of her division and quality officer for the hospital. “Physicians get a lot of satisfaction from helping individual patients,” she says. “One thing I really liked about getting involved with quality improvement was being able to make a difference for patients on a systems level.”
An Incremental Path
The path to her current position began with a very specific issue for Dr. Nagamine, an SHM board member who also serves as a Project BOOST co-investigator. “Although I have been doing patient safety since before they had a name for it, I didn’t start out saying that I wanted a career in quality and safety,” she says. “I was trying to take better care of my patients with diabetes, but controlling their glucose was extremely challenging because all the related variables—timing and amount of their insulin dosage, when and how much they had eaten—were charted in different places. This made it hard to adjust their insulin appropriately.”
It quickly became clear to Dr. Nagamine that the solution had to be systemic. She realized that something as basic as taking care of her patients with diabetes required multiple departments (i.e. dietary, nursing, and pharmacy) to furnish information in an integrated manner. So she joined the diabetes committee and went to work on the issue. She helped devise a flow chart that could be used by all relevant departments. A further evolution on the path emanated from one of her patients receiving the wrong medication. She joined the medication safety committee, became chair, “and the next thing you know, I’m in charge of patient safety, and an assistant chief of quality.”
Training Is Necessary
QI and patient-safety methodologies have become sophisticated disciplines in the past two decades, Dr. Wright says. Access to training in QI basics now is readily available to early-career hospitalists. For example, CogentHMG offers program support for QI so that anyone interested “doesn’t have to start from scratch anymore; we can help show them the way and support them in doing it.”
This month, HM13 (www.hospital medicine2013.org)—just outside Washington, D.C.—will offer multiple sessions on quality, as well as the “Initiating Quality Improvement Projects with Built-In Sustainment” workshop, led by Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) core investigator Peter Kaboli, MD, MS, who will address sustainability.
Beyond methodological tools, success in quality and patient safety requires the ability to motivate people, often across multiple disciplines, Dr. Nagamine says. “If you want things to work better, you must invite the right people to the table. For example, we often forget to include key nonclinical stakeholders,” she adds.
When working with hospitals across the country to implement rapid-response tTeams, Dr. Nagamine often reminds them to invite the operators, or “key people,” in the process.
“If you put patient safety at the core of your initiative and create the context for that, most people will agree that it’s the right thing to do and will get on board, even if it’s an extra step for them,” she says. “Know your audience, listen to their perspective, and learn what matters to them. And to most people, it matters that they give good patient care.”
Gretchen Henkel is a freelance writer in California.