User login
FDA approves antidote for factor Xa inhibitors
The US Food and Drug Administration (FDA) has granted accelerated approval for andexanet alfa (Andexxa®), the first antidote for the reversal of factor Xa inhibitors.
Andexanet alfa is approved for use in patients treated with rivaroxaban or apixaban when reversal of anticoagulation is needed due to life-threatening or uncontrolled bleeding.
Andexanet alfa was granted accelerated approval for this indication based on the drug’s anti-factor Xa activity in healthy volunteers.
Continued FDA approval of andexanet alfa may be contingent upon post-marketing study results to demonstrate an improvement in hemostasis in patients taking rivaroxaban or apixaban who require reversal of anticoagulation.
The post-marketing requirement is a trial in which patients will be randomized to receive either andexanet alfa or usual care. This study is scheduled to start in 2019, with results expected to be available in 2023.
Portola Pharmaceuticals, Inc., said it expects to launch andexanet alfa in early June. This drug will be produced using the generation 1 manufacturing process.
A broader commercial launch of andexanet alfa is anticipated in early 2019, dependent upon FDA approval of the generation 2 manufacturing process.
Supporting trials
The FDA’s approval of andexanet alfa is supported by data from a pair of phase 3 studies—ANNEXA-R and ANNEXA-A.
These trials were designed to evaluate the safety and efficacy of andexanet alfa in reversing the anticoagulant activity of rivaroxaban and apixaban in healthy volunteers.
Results from both studies were published in NEJM in 2015.
The FDA also assessed interim data from the ongoing ANNEXA-4 study as part of the review and approval of andexanet alfa.
In ANNEXA-4, researchers are evaluating andexanet alfa in patients experiencing major bleeding while taking factor Xa inhibitors.
Interim results from this trial were presented at the American College of Cardiology’s 67th Annual Scientific Session & Expo in March.
About andexanet alfa
Andexanet alfa is a modified human factor Xa molecule that acts as a decoy to target and sequester both oral and injectable factor Xa inhibitors in the blood. Once bound, the factor Xa inhibitors are unable to bind to and inhibit native factor Xa, thus potentially allowing for the restoration of normal hemostatic processes.
Portola Pharmaceuticals first submitted the biologics license application (BLA) for andexanet alfa in December 2015. The FDA had already granted andexanet alfa orphan drug designation earlier in 2015 and breakthrough therapy designation in 2013.
With its first BLA submission, Portola was seeking approval for andexanet alfa as a reversal agent for patients anticoagulated with an oral or injectable factor Xa inhibitor—apixaban, rivaroxaban, edoxaban, or enoxaparin—who experience serious uncontrolled or life-threatening bleeding or who require urgent or emergency surgery.
In August 2016, the FDA issued a complete response letter explaining why the agency could not approve andexanet alfa for this indication.
The FDA requested additional information related to manufacturing of the drug and asked Portola for additional data to support the inclusion of edoxaban and enoxaparin on andexanet alfa’s label. This was because the ANNEXA-A and ANNEXA-R trials only included subjects who received apixaban or rivaroxaban.
In August 2017, Portola resubmitted the BLA for andexanet alfa. This time, the company sought approval of the drug only for patients on apixaban or rivaroxaban who are experiencing uncontrolled or life-threatening bleeding.
For additional information on andexanet alfa, visit https://www.andexxa.com/.
The US Food and Drug Administration (FDA) has granted accelerated approval for andexanet alfa (Andexxa®), the first antidote for the reversal of factor Xa inhibitors.
Andexanet alfa is approved for use in patients treated with rivaroxaban or apixaban when reversal of anticoagulation is needed due to life-threatening or uncontrolled bleeding.
Andexanet alfa was granted accelerated approval for this indication based on the drug’s anti-factor Xa activity in healthy volunteers.
Continued FDA approval of andexanet alfa may be contingent upon post-marketing study results to demonstrate an improvement in hemostasis in patients taking rivaroxaban or apixaban who require reversal of anticoagulation.
The post-marketing requirement is a trial in which patients will be randomized to receive either andexanet alfa or usual care. This study is scheduled to start in 2019, with results expected to be available in 2023.
Portola Pharmaceuticals, Inc., said it expects to launch andexanet alfa in early June. This drug will be produced using the generation 1 manufacturing process.
A broader commercial launch of andexanet alfa is anticipated in early 2019, dependent upon FDA approval of the generation 2 manufacturing process.
Supporting trials
The FDA’s approval of andexanet alfa is supported by data from a pair of phase 3 studies—ANNEXA-R and ANNEXA-A.
These trials were designed to evaluate the safety and efficacy of andexanet alfa in reversing the anticoagulant activity of rivaroxaban and apixaban in healthy volunteers.
Results from both studies were published in NEJM in 2015.
The FDA also assessed interim data from the ongoing ANNEXA-4 study as part of the review and approval of andexanet alfa.
In ANNEXA-4, researchers are evaluating andexanet alfa in patients experiencing major bleeding while taking factor Xa inhibitors.
Interim results from this trial were presented at the American College of Cardiology’s 67th Annual Scientific Session & Expo in March.
About andexanet alfa
Andexanet alfa is a modified human factor Xa molecule that acts as a decoy to target and sequester both oral and injectable factor Xa inhibitors in the blood. Once bound, the factor Xa inhibitors are unable to bind to and inhibit native factor Xa, thus potentially allowing for the restoration of normal hemostatic processes.
Portola Pharmaceuticals first submitted the biologics license application (BLA) for andexanet alfa in December 2015. The FDA had already granted andexanet alfa orphan drug designation earlier in 2015 and breakthrough therapy designation in 2013.
With its first BLA submission, Portola was seeking approval for andexanet alfa as a reversal agent for patients anticoagulated with an oral or injectable factor Xa inhibitor—apixaban, rivaroxaban, edoxaban, or enoxaparin—who experience serious uncontrolled or life-threatening bleeding or who require urgent or emergency surgery.
In August 2016, the FDA issued a complete response letter explaining why the agency could not approve andexanet alfa for this indication.
The FDA requested additional information related to manufacturing of the drug and asked Portola for additional data to support the inclusion of edoxaban and enoxaparin on andexanet alfa’s label. This was because the ANNEXA-A and ANNEXA-R trials only included subjects who received apixaban or rivaroxaban.
In August 2017, Portola resubmitted the BLA for andexanet alfa. This time, the company sought approval of the drug only for patients on apixaban or rivaroxaban who are experiencing uncontrolled or life-threatening bleeding.
For additional information on andexanet alfa, visit https://www.andexxa.com/.
The US Food and Drug Administration (FDA) has granted accelerated approval for andexanet alfa (Andexxa®), the first antidote for the reversal of factor Xa inhibitors.
Andexanet alfa is approved for use in patients treated with rivaroxaban or apixaban when reversal of anticoagulation is needed due to life-threatening or uncontrolled bleeding.
Andexanet alfa was granted accelerated approval for this indication based on the drug’s anti-factor Xa activity in healthy volunteers.
Continued FDA approval of andexanet alfa may be contingent upon post-marketing study results to demonstrate an improvement in hemostasis in patients taking rivaroxaban or apixaban who require reversal of anticoagulation.
The post-marketing requirement is a trial in which patients will be randomized to receive either andexanet alfa or usual care. This study is scheduled to start in 2019, with results expected to be available in 2023.
Portola Pharmaceuticals, Inc., said it expects to launch andexanet alfa in early June. This drug will be produced using the generation 1 manufacturing process.
A broader commercial launch of andexanet alfa is anticipated in early 2019, dependent upon FDA approval of the generation 2 manufacturing process.
Supporting trials
The FDA’s approval of andexanet alfa is supported by data from a pair of phase 3 studies—ANNEXA-R and ANNEXA-A.
These trials were designed to evaluate the safety and efficacy of andexanet alfa in reversing the anticoagulant activity of rivaroxaban and apixaban in healthy volunteers.
Results from both studies were published in NEJM in 2015.
The FDA also assessed interim data from the ongoing ANNEXA-4 study as part of the review and approval of andexanet alfa.
In ANNEXA-4, researchers are evaluating andexanet alfa in patients experiencing major bleeding while taking factor Xa inhibitors.
Interim results from this trial were presented at the American College of Cardiology’s 67th Annual Scientific Session & Expo in March.
About andexanet alfa
Andexanet alfa is a modified human factor Xa molecule that acts as a decoy to target and sequester both oral and injectable factor Xa inhibitors in the blood. Once bound, the factor Xa inhibitors are unable to bind to and inhibit native factor Xa, thus potentially allowing for the restoration of normal hemostatic processes.
Portola Pharmaceuticals first submitted the biologics license application (BLA) for andexanet alfa in December 2015. The FDA had already granted andexanet alfa orphan drug designation earlier in 2015 and breakthrough therapy designation in 2013.
With its first BLA submission, Portola was seeking approval for andexanet alfa as a reversal agent for patients anticoagulated with an oral or injectable factor Xa inhibitor—apixaban, rivaroxaban, edoxaban, or enoxaparin—who experience serious uncontrolled or life-threatening bleeding or who require urgent or emergency surgery.
In August 2016, the FDA issued a complete response letter explaining why the agency could not approve andexanet alfa for this indication.
The FDA requested additional information related to manufacturing of the drug and asked Portola for additional data to support the inclusion of edoxaban and enoxaparin on andexanet alfa’s label. This was because the ANNEXA-A and ANNEXA-R trials only included subjects who received apixaban or rivaroxaban.
In August 2017, Portola resubmitted the BLA for andexanet alfa. This time, the company sought approval of the drug only for patients on apixaban or rivaroxaban who are experiencing uncontrolled or life-threatening bleeding.
For additional information on andexanet alfa, visit https://www.andexxa.com/.
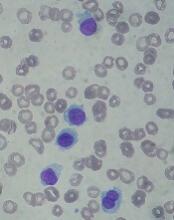
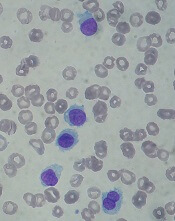
CHMP backs approval of dasatinib for kids
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended changes to the marketing authorization for dasatinib (Sprycel).
The CHMP is recommending approval for dasatinib as a treatment for pediatric patients with newly diagnosed, Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase (CP) or Ph+ CML-CP that is resistant or intolerant to prior therapy, including imatinib.
The CHMP has also recommended approval of a new formulation of dasatinib—a powder for oral suspension (PFOS)—for use in pediatric patients.
Dasatinib is already approved in the European Union to treat adults with:
- Newly diagnosed Ph+ CML-CP
- Chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy, including imatinib
- Ph+ acute lymphoblastic leukemia and lymphoid blast CML with resistance or intolerance to prior therapy.
The CHMP’s opinion on dasatinib for pediatric patients will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
The CHMP’s opinion on dasatinib for pediatric patients is supported by 2 studies. Results from the phase 1 study (NCT00306202) were published in the Journal of Clinical Oncology in 2013. Phase 2 (NCT00777036) results were published in the same journal this year.
Phase 1
The phase 1 trial included 17 patients with CML-CP, all of whom had received prior imatinib.
Eleven patients received dasatinib at a starting dose of 60 mg/m2 once daily, and 6 received the drug at a starting dose of 80 mg/m2 once daily. Dose escalation was allowed based on tolerance and response. The median duration of treatment was 24.1 months (range, 2.3 to 50.6 months).
The 60 mg/m2 starting dose appeared more tolerable than 80 mg/m2 dose.
Drug-related adverse events (AEs) occurring in at least 20% of patients included neutropenia (82.4%), anemia (70.6%), thrombocytopenia (64.7%), nausea (29.4%), headache (35.3%), diarrhea (23.5%), and pain in extremity (23.5%). Grade 3-4 AEs included neutropenia (23.5%), thrombocytopenia (11.8%), and headache (5.9%). There were no drug-related deaths.
Ninety-four percent of patients achieved a complete hematologic response (CHR), 88% had a major cytogenetic response (MCyR), 82% had a complete cytogenetic response (CCyR), 47% had a major molecular response (MMR), and 24% had a complete molecular response (CMR).
Patients who received the lower starting dose of dasatinib had lower rates of cumulative CCyR (72.7% vs 100%) and CHR (90.9% vs 100%) but higher rates of cumulative MMR (54.5% vs 33.3%) and CMR (27.3% vs 16.7).
The median progression-free survival (PFS) and overall survival (OS) had not been reached at last follow-up. At 24 months, the estimated PFS was 61%, and the estimated OS was 88%.
Phase 2
The phase 2 trial included 29 patients with imatinib-resistant/intolerant CML-CP and 84 with newly diagnosed CML-CP.
The previously treated patients received dasatinib tablets. Newly diagnosed patients were treated with dasatinib tablets (n=51) or PFOS (n=33). Patients who started on PFOS could switch to tablets after receiving PFOS for at least 1 year. Sixty-seven percent of patients on PFOS switched to tablets due to patient preference.
The average daily dose of dasatinib was 58.18 mg/m2 in the previously treated patients and 59.84 mg/m2 in the newly diagnosed patients (for both tablets and PFOS). The median duration of treatment was 49.91 months (range, 1.9 to 90.2) and 42.30 months (range, 0.1 to 75.2), respectively.
Rates of confirmed CHR (at any time) were 93% in the previously treated patients and 96% in the newly diagnosed patients.
At 12 months, previously treated patients had an MMR rate of 41% and a CMR rate of 7%. In newly diagnosed patients, MMR was 52%, and CMR was 8%.
At 24 months, previously treated patients had an MMR rate of 55% and a CMR rate of 17%. In the newly diagnosed patients, MMR was 70%, and CMR was 21%.
The rate of MCyR at any time was 89.7% in all previously treated patients and 90% when the researchers excluded patients with MCyR or unknown cytogenetic status at baseline.
The rate of CCyR at any time was 94% in all newly diagnosed patients and 93.9% when the researchers excluded patients with CCyR or unknown cytogenetic status at baseline.
The median PFS and OS had not been reached at last follow-up. The estimated 48-month PFS was 78% in the previously treated patients and 93% in the newly diagnosed patients. The estimated 48-month OS was 96% and 100%, respectively.
Dasatinib-related AEs occurring in at least 10% of the previously treated patients included nausea/vomiting (31%), myalgia/arthralgia (17%), fatigue (14%), rash (14%), diarrhea (14%), hemorrhage (10%), bone growth and development events (10%), and shortness of breath (10%).
Dasatinib-related AEs occurring in at least 10% of the newly diagnosed patients included nausea/vomiting (20%), myalgia/arthralgia (10%), fatigue (11%), rash (19%), diarrhea (18%), and hemorrhage (10%).
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended changes to the marketing authorization for dasatinib (Sprycel).
The CHMP is recommending approval for dasatinib as a treatment for pediatric patients with newly diagnosed, Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase (CP) or Ph+ CML-CP that is resistant or intolerant to prior therapy, including imatinib.
The CHMP has also recommended approval of a new formulation of dasatinib—a powder for oral suspension (PFOS)—for use in pediatric patients.
Dasatinib is already approved in the European Union to treat adults with:
- Newly diagnosed Ph+ CML-CP
- Chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy, including imatinib
- Ph+ acute lymphoblastic leukemia and lymphoid blast CML with resistance or intolerance to prior therapy.
The CHMP’s opinion on dasatinib for pediatric patients will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
The CHMP’s opinion on dasatinib for pediatric patients is supported by 2 studies. Results from the phase 1 study (NCT00306202) were published in the Journal of Clinical Oncology in 2013. Phase 2 (NCT00777036) results were published in the same journal this year.
Phase 1
The phase 1 trial included 17 patients with CML-CP, all of whom had received prior imatinib.
Eleven patients received dasatinib at a starting dose of 60 mg/m2 once daily, and 6 received the drug at a starting dose of 80 mg/m2 once daily. Dose escalation was allowed based on tolerance and response. The median duration of treatment was 24.1 months (range, 2.3 to 50.6 months).
The 60 mg/m2 starting dose appeared more tolerable than 80 mg/m2 dose.
Drug-related adverse events (AEs) occurring in at least 20% of patients included neutropenia (82.4%), anemia (70.6%), thrombocytopenia (64.7%), nausea (29.4%), headache (35.3%), diarrhea (23.5%), and pain in extremity (23.5%). Grade 3-4 AEs included neutropenia (23.5%), thrombocytopenia (11.8%), and headache (5.9%). There were no drug-related deaths.
Ninety-four percent of patients achieved a complete hematologic response (CHR), 88% had a major cytogenetic response (MCyR), 82% had a complete cytogenetic response (CCyR), 47% had a major molecular response (MMR), and 24% had a complete molecular response (CMR).
Patients who received the lower starting dose of dasatinib had lower rates of cumulative CCyR (72.7% vs 100%) and CHR (90.9% vs 100%) but higher rates of cumulative MMR (54.5% vs 33.3%) and CMR (27.3% vs 16.7).
The median progression-free survival (PFS) and overall survival (OS) had not been reached at last follow-up. At 24 months, the estimated PFS was 61%, and the estimated OS was 88%.
Phase 2
The phase 2 trial included 29 patients with imatinib-resistant/intolerant CML-CP and 84 with newly diagnosed CML-CP.
The previously treated patients received dasatinib tablets. Newly diagnosed patients were treated with dasatinib tablets (n=51) or PFOS (n=33). Patients who started on PFOS could switch to tablets after receiving PFOS for at least 1 year. Sixty-seven percent of patients on PFOS switched to tablets due to patient preference.
The average daily dose of dasatinib was 58.18 mg/m2 in the previously treated patients and 59.84 mg/m2 in the newly diagnosed patients (for both tablets and PFOS). The median duration of treatment was 49.91 months (range, 1.9 to 90.2) and 42.30 months (range, 0.1 to 75.2), respectively.
Rates of confirmed CHR (at any time) were 93% in the previously treated patients and 96% in the newly diagnosed patients.
At 12 months, previously treated patients had an MMR rate of 41% and a CMR rate of 7%. In newly diagnosed patients, MMR was 52%, and CMR was 8%.
At 24 months, previously treated patients had an MMR rate of 55% and a CMR rate of 17%. In the newly diagnosed patients, MMR was 70%, and CMR was 21%.
The rate of MCyR at any time was 89.7% in all previously treated patients and 90% when the researchers excluded patients with MCyR or unknown cytogenetic status at baseline.
The rate of CCyR at any time was 94% in all newly diagnosed patients and 93.9% when the researchers excluded patients with CCyR or unknown cytogenetic status at baseline.
The median PFS and OS had not been reached at last follow-up. The estimated 48-month PFS was 78% in the previously treated patients and 93% in the newly diagnosed patients. The estimated 48-month OS was 96% and 100%, respectively.
Dasatinib-related AEs occurring in at least 10% of the previously treated patients included nausea/vomiting (31%), myalgia/arthralgia (17%), fatigue (14%), rash (14%), diarrhea (14%), hemorrhage (10%), bone growth and development events (10%), and shortness of breath (10%).
Dasatinib-related AEs occurring in at least 10% of the newly diagnosed patients included nausea/vomiting (20%), myalgia/arthralgia (10%), fatigue (11%), rash (19%), diarrhea (18%), and hemorrhage (10%).
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended changes to the marketing authorization for dasatinib (Sprycel).
The CHMP is recommending approval for dasatinib as a treatment for pediatric patients with newly diagnosed, Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase (CP) or Ph+ CML-CP that is resistant or intolerant to prior therapy, including imatinib.
The CHMP has also recommended approval of a new formulation of dasatinib—a powder for oral suspension (PFOS)—for use in pediatric patients.
Dasatinib is already approved in the European Union to treat adults with:
- Newly diagnosed Ph+ CML-CP
- Chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy, including imatinib
- Ph+ acute lymphoblastic leukemia and lymphoid blast CML with resistance or intolerance to prior therapy.
The CHMP’s opinion on dasatinib for pediatric patients will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
The CHMP’s opinion on dasatinib for pediatric patients is supported by 2 studies. Results from the phase 1 study (NCT00306202) were published in the Journal of Clinical Oncology in 2013. Phase 2 (NCT00777036) results were published in the same journal this year.
Phase 1
The phase 1 trial included 17 patients with CML-CP, all of whom had received prior imatinib.
Eleven patients received dasatinib at a starting dose of 60 mg/m2 once daily, and 6 received the drug at a starting dose of 80 mg/m2 once daily. Dose escalation was allowed based on tolerance and response. The median duration of treatment was 24.1 months (range, 2.3 to 50.6 months).
The 60 mg/m2 starting dose appeared more tolerable than 80 mg/m2 dose.
Drug-related adverse events (AEs) occurring in at least 20% of patients included neutropenia (82.4%), anemia (70.6%), thrombocytopenia (64.7%), nausea (29.4%), headache (35.3%), diarrhea (23.5%), and pain in extremity (23.5%). Grade 3-4 AEs included neutropenia (23.5%), thrombocytopenia (11.8%), and headache (5.9%). There were no drug-related deaths.
Ninety-four percent of patients achieved a complete hematologic response (CHR), 88% had a major cytogenetic response (MCyR), 82% had a complete cytogenetic response (CCyR), 47% had a major molecular response (MMR), and 24% had a complete molecular response (CMR).
Patients who received the lower starting dose of dasatinib had lower rates of cumulative CCyR (72.7% vs 100%) and CHR (90.9% vs 100%) but higher rates of cumulative MMR (54.5% vs 33.3%) and CMR (27.3% vs 16.7).
The median progression-free survival (PFS) and overall survival (OS) had not been reached at last follow-up. At 24 months, the estimated PFS was 61%, and the estimated OS was 88%.
Phase 2
The phase 2 trial included 29 patients with imatinib-resistant/intolerant CML-CP and 84 with newly diagnosed CML-CP.
The previously treated patients received dasatinib tablets. Newly diagnosed patients were treated with dasatinib tablets (n=51) or PFOS (n=33). Patients who started on PFOS could switch to tablets after receiving PFOS for at least 1 year. Sixty-seven percent of patients on PFOS switched to tablets due to patient preference.
The average daily dose of dasatinib was 58.18 mg/m2 in the previously treated patients and 59.84 mg/m2 in the newly diagnosed patients (for both tablets and PFOS). The median duration of treatment was 49.91 months (range, 1.9 to 90.2) and 42.30 months (range, 0.1 to 75.2), respectively.
Rates of confirmed CHR (at any time) were 93% in the previously treated patients and 96% in the newly diagnosed patients.
At 12 months, previously treated patients had an MMR rate of 41% and a CMR rate of 7%. In newly diagnosed patients, MMR was 52%, and CMR was 8%.
At 24 months, previously treated patients had an MMR rate of 55% and a CMR rate of 17%. In the newly diagnosed patients, MMR was 70%, and CMR was 21%.
The rate of MCyR at any time was 89.7% in all previously treated patients and 90% when the researchers excluded patients with MCyR or unknown cytogenetic status at baseline.
The rate of CCyR at any time was 94% in all newly diagnosed patients and 93.9% when the researchers excluded patients with CCyR or unknown cytogenetic status at baseline.
The median PFS and OS had not been reached at last follow-up. The estimated 48-month PFS was 78% in the previously treated patients and 93% in the newly diagnosed patients. The estimated 48-month OS was 96% and 100%, respectively.
Dasatinib-related AEs occurring in at least 10% of the previously treated patients included nausea/vomiting (31%), myalgia/arthralgia (17%), fatigue (14%), rash (14%), diarrhea (14%), hemorrhage (10%), bone growth and development events (10%), and shortness of breath (10%).
Dasatinib-related AEs occurring in at least 10% of the newly diagnosed patients included nausea/vomiting (20%), myalgia/arthralgia (10%), fatigue (11%), rash (19%), diarrhea (18%), and hemorrhage (10%).
CHMP recommends approval for generic carmustine
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion of Carmustine Obvius, a generic version of Carmubris.
The CHMP is recommending marketing authorization for Carmustine Obvius as second-line treatment for Hodgkin and non-Hodgkin lymphoma as well as to treat new or recurrent brain tumors, including glioblastoma, medulloblastoma, astrocytoma, and metastatic brain tumors.
The CHMP’s opinion on Carmustine Obvius will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP’s recommendation, the commission will grant a centralized marketing authorization that will be valid in the European Union.
The EC typically makes a decision on a product within 67 days of the CHMP’s recommendation.
If approved, Carmustine Obvius will be available as a 100 mg powder and solvent for solution for infusion.
The active substance of Carmustine Obvius is carmustine, an alkylating antineoplastic agent of the nitrosourea type, which prevents DNA replication and transcription by alkylating reactive sites on nucleoproteins.
Carmustine Obvius is a generic of Carmubris, which has been authorized in the European Union since July 31, 1996.
Since Carmustine Obvius is administered intravenously and is 100% bioavailable, a bioequivalence study of the drug versus Carmubris was not required.
Carmustine Obvius is a product of Obvius Investment B.V.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion of Carmustine Obvius, a generic version of Carmubris.
The CHMP is recommending marketing authorization for Carmustine Obvius as second-line treatment for Hodgkin and non-Hodgkin lymphoma as well as to treat new or recurrent brain tumors, including glioblastoma, medulloblastoma, astrocytoma, and metastatic brain tumors.
The CHMP’s opinion on Carmustine Obvius will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP’s recommendation, the commission will grant a centralized marketing authorization that will be valid in the European Union.
The EC typically makes a decision on a product within 67 days of the CHMP’s recommendation.
If approved, Carmustine Obvius will be available as a 100 mg powder and solvent for solution for infusion.
The active substance of Carmustine Obvius is carmustine, an alkylating antineoplastic agent of the nitrosourea type, which prevents DNA replication and transcription by alkylating reactive sites on nucleoproteins.
Carmustine Obvius is a generic of Carmubris, which has been authorized in the European Union since July 31, 1996.
Since Carmustine Obvius is administered intravenously and is 100% bioavailable, a bioequivalence study of the drug versus Carmubris was not required.
Carmustine Obvius is a product of Obvius Investment B.V.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion of Carmustine Obvius, a generic version of Carmubris.
The CHMP is recommending marketing authorization for Carmustine Obvius as second-line treatment for Hodgkin and non-Hodgkin lymphoma as well as to treat new or recurrent brain tumors, including glioblastoma, medulloblastoma, astrocytoma, and metastatic brain tumors.
The CHMP’s opinion on Carmustine Obvius will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP’s recommendation, the commission will grant a centralized marketing authorization that will be valid in the European Union.
The EC typically makes a decision on a product within 67 days of the CHMP’s recommendation.
If approved, Carmustine Obvius will be available as a 100 mg powder and solvent for solution for infusion.
The active substance of Carmustine Obvius is carmustine, an alkylating antineoplastic agent of the nitrosourea type, which prevents DNA replication and transcription by alkylating reactive sites on nucleoproteins.
Carmustine Obvius is a generic of Carmubris, which has been authorized in the European Union since July 31, 1996.
Since Carmustine Obvius is administered intravenously and is 100% bioavailable, a bioequivalence study of the drug versus Carmubris was not required.
Carmustine Obvius is a product of Obvius Investment B.V.
GO approved to treat AML in Europe
The European Commission has authorized use of gemtuzumab ozogamicin (GO, Mylotarg™) as a treatment for patients with acute myeloid leukemia (AML).
GO is now approved for use in combination with daunorubicin and cytarabine to treat patients age 15 and older who have previously untreated, de novo, CD33-positive AML, not including acute promyelocytic leukemia.
GO is an antibody-drug conjugate composed of the cytotoxic agent calicheamicin attached to a monoclonal antibody targeting CD33, an antigen expressed on the surface of myeloblasts in up to 90% of AML patients.
When GO binds to the CD33 antigen on the cell surface, it is absorbed into the cell, and calicheamicin is released, causing cell death.
Previous rejection
The European Commission’s approval of GO follows a positive opinion from the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP). In February, the CHMP recommended that GO receive marketing authorization for the aforementioned indication.
However, the CHMP previously issued a negative opinion of GO (first in 2007, confirmed in 2008), saying the drug should not receive marketing authorization.
The proposed indication for GO at that time was as re-induction treatment in adults with CD33-positive AML in first relapse who were not candidates for other intensive re-induction chemotherapy regimens and were either older than 60 or had a duration of first remission lasting less than 12 months.
The CHMP said there was insufficient evidence to establish the effectiveness of GO in AML, and the drug’s benefits did not outweigh its risks.
Phase 3 trial
The current marketing authorization application for GO is supported by data from an investigator-led, phase 3, randomized trial known as ALFA-0701. Updated results from this trial are available in the US prescribing information for GO.
ALFA-0701 included 271 patients with newly diagnosed, de novo AML who were 50 to 70 years of age.
Patients were randomized (1:1) to receive induction consisting of daunorubicin (60 mg/m2 on days 1 to 3) and cytarabine (200 mg/m2 on days 1 to 7) with (n=135) or without (n=136) GO at 3 mg/m2 (up to a maximum of 1 vial) on days 1, 4, and 7. Patients who did not achieve a response after first induction could receive a second induction with daunorubicin and cytarabine alone.
Patients with a response received consolidation therapy with 2 courses of treatment including daunorubicin (60 mg/m2 on day 1 of first consolidation course; 60 mg/m2 on days 1 and 2 of second consolidation course) and cytarabine (1 g/m2 every 12 hours on days 1 to 4) with or without GO at 3 mg/m2 (up to a maximum of 1 vial) on day 1 according to their initial randomization.
Patients who achieved remission were also eligible for allogeneic transplant. An interval of at least 2 months between the last dose of GO and transplant was recommended.
Baseline characteristics were largely well balanced between the treatment arms, but there was a higher percentage of males in the GO arm than the control arm—55% and 44%, respectively.
The study’s primary endpoint was event-free survival. The median event-free survival was 17.3 months in the GO arm and 9.5 months in the control arm (hazard ratio=0.56; 95% CI: 0.42-0.76; P<0.001).
There was no significant difference in overall survival between the treatment arms. (Updated overall survival data have not been released).
All patients in this trial developed severe neutropenia, thrombocytopenia, and anemia. However, the incidence of prolonged, grade 3–4 thrombocytopenia in the absence of active leukemia was higher in the GO arm.
Treatment-emergent adverse events (AEs) considered most important for understanding the safety profile of GO were hemorrhage, veno-occlusive liver disease (VOD), and severe infections.
Treatment discontinuation due to any AE occurred in 31% of patients in the GO arm and 7% of those in the control arm. The most frequent AEs leading to discontinuation for patients on GO were thrombocytopenia (15%), VOD (3%), and septic shock (2%).
Fatal AEs occurred in 8 patients (6%) in the GO arm and 3 (2%) in the control arm. In the GO arm, 3 patients died of VOD, 4 died of hemorrhage-related events, and 1 died of a suspected cardiac cause. All 3 fatal AEs in the control arm were sepsis.
The European Commission has authorized use of gemtuzumab ozogamicin (GO, Mylotarg™) as a treatment for patients with acute myeloid leukemia (AML).
GO is now approved for use in combination with daunorubicin and cytarabine to treat patients age 15 and older who have previously untreated, de novo, CD33-positive AML, not including acute promyelocytic leukemia.
GO is an antibody-drug conjugate composed of the cytotoxic agent calicheamicin attached to a monoclonal antibody targeting CD33, an antigen expressed on the surface of myeloblasts in up to 90% of AML patients.
When GO binds to the CD33 antigen on the cell surface, it is absorbed into the cell, and calicheamicin is released, causing cell death.
Previous rejection
The European Commission’s approval of GO follows a positive opinion from the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP). In February, the CHMP recommended that GO receive marketing authorization for the aforementioned indication.
However, the CHMP previously issued a negative opinion of GO (first in 2007, confirmed in 2008), saying the drug should not receive marketing authorization.
The proposed indication for GO at that time was as re-induction treatment in adults with CD33-positive AML in first relapse who were not candidates for other intensive re-induction chemotherapy regimens and were either older than 60 or had a duration of first remission lasting less than 12 months.
The CHMP said there was insufficient evidence to establish the effectiveness of GO in AML, and the drug’s benefits did not outweigh its risks.
Phase 3 trial
The current marketing authorization application for GO is supported by data from an investigator-led, phase 3, randomized trial known as ALFA-0701. Updated results from this trial are available in the US prescribing information for GO.
ALFA-0701 included 271 patients with newly diagnosed, de novo AML who were 50 to 70 years of age.
Patients were randomized (1:1) to receive induction consisting of daunorubicin (60 mg/m2 on days 1 to 3) and cytarabine (200 mg/m2 on days 1 to 7) with (n=135) or without (n=136) GO at 3 mg/m2 (up to a maximum of 1 vial) on days 1, 4, and 7. Patients who did not achieve a response after first induction could receive a second induction with daunorubicin and cytarabine alone.
Patients with a response received consolidation therapy with 2 courses of treatment including daunorubicin (60 mg/m2 on day 1 of first consolidation course; 60 mg/m2 on days 1 and 2 of second consolidation course) and cytarabine (1 g/m2 every 12 hours on days 1 to 4) with or without GO at 3 mg/m2 (up to a maximum of 1 vial) on day 1 according to their initial randomization.
Patients who achieved remission were also eligible for allogeneic transplant. An interval of at least 2 months between the last dose of GO and transplant was recommended.
Baseline characteristics were largely well balanced between the treatment arms, but there was a higher percentage of males in the GO arm than the control arm—55% and 44%, respectively.
The study’s primary endpoint was event-free survival. The median event-free survival was 17.3 months in the GO arm and 9.5 months in the control arm (hazard ratio=0.56; 95% CI: 0.42-0.76; P<0.001).
There was no significant difference in overall survival between the treatment arms. (Updated overall survival data have not been released).
All patients in this trial developed severe neutropenia, thrombocytopenia, and anemia. However, the incidence of prolonged, grade 3–4 thrombocytopenia in the absence of active leukemia was higher in the GO arm.
Treatment-emergent adverse events (AEs) considered most important for understanding the safety profile of GO were hemorrhage, veno-occlusive liver disease (VOD), and severe infections.
Treatment discontinuation due to any AE occurred in 31% of patients in the GO arm and 7% of those in the control arm. The most frequent AEs leading to discontinuation for patients on GO were thrombocytopenia (15%), VOD (3%), and septic shock (2%).
Fatal AEs occurred in 8 patients (6%) in the GO arm and 3 (2%) in the control arm. In the GO arm, 3 patients died of VOD, 4 died of hemorrhage-related events, and 1 died of a suspected cardiac cause. All 3 fatal AEs in the control arm were sepsis.
The European Commission has authorized use of gemtuzumab ozogamicin (GO, Mylotarg™) as a treatment for patients with acute myeloid leukemia (AML).
GO is now approved for use in combination with daunorubicin and cytarabine to treat patients age 15 and older who have previously untreated, de novo, CD33-positive AML, not including acute promyelocytic leukemia.
GO is an antibody-drug conjugate composed of the cytotoxic agent calicheamicin attached to a monoclonal antibody targeting CD33, an antigen expressed on the surface of myeloblasts in up to 90% of AML patients.
When GO binds to the CD33 antigen on the cell surface, it is absorbed into the cell, and calicheamicin is released, causing cell death.
Previous rejection
The European Commission’s approval of GO follows a positive opinion from the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP). In February, the CHMP recommended that GO receive marketing authorization for the aforementioned indication.
However, the CHMP previously issued a negative opinion of GO (first in 2007, confirmed in 2008), saying the drug should not receive marketing authorization.
The proposed indication for GO at that time was as re-induction treatment in adults with CD33-positive AML in first relapse who were not candidates for other intensive re-induction chemotherapy regimens and were either older than 60 or had a duration of first remission lasting less than 12 months.
The CHMP said there was insufficient evidence to establish the effectiveness of GO in AML, and the drug’s benefits did not outweigh its risks.
Phase 3 trial
The current marketing authorization application for GO is supported by data from an investigator-led, phase 3, randomized trial known as ALFA-0701. Updated results from this trial are available in the US prescribing information for GO.
ALFA-0701 included 271 patients with newly diagnosed, de novo AML who were 50 to 70 years of age.
Patients were randomized (1:1) to receive induction consisting of daunorubicin (60 mg/m2 on days 1 to 3) and cytarabine (200 mg/m2 on days 1 to 7) with (n=135) or without (n=136) GO at 3 mg/m2 (up to a maximum of 1 vial) on days 1, 4, and 7. Patients who did not achieve a response after first induction could receive a second induction with daunorubicin and cytarabine alone.
Patients with a response received consolidation therapy with 2 courses of treatment including daunorubicin (60 mg/m2 on day 1 of first consolidation course; 60 mg/m2 on days 1 and 2 of second consolidation course) and cytarabine (1 g/m2 every 12 hours on days 1 to 4) with or without GO at 3 mg/m2 (up to a maximum of 1 vial) on day 1 according to their initial randomization.
Patients who achieved remission were also eligible for allogeneic transplant. An interval of at least 2 months between the last dose of GO and transplant was recommended.
Baseline characteristics were largely well balanced between the treatment arms, but there was a higher percentage of males in the GO arm than the control arm—55% and 44%, respectively.
The study’s primary endpoint was event-free survival. The median event-free survival was 17.3 months in the GO arm and 9.5 months in the control arm (hazard ratio=0.56; 95% CI: 0.42-0.76; P<0.001).
There was no significant difference in overall survival between the treatment arms. (Updated overall survival data have not been released).
All patients in this trial developed severe neutropenia, thrombocytopenia, and anemia. However, the incidence of prolonged, grade 3–4 thrombocytopenia in the absence of active leukemia was higher in the GO arm.
Treatment-emergent adverse events (AEs) considered most important for understanding the safety profile of GO were hemorrhage, veno-occlusive liver disease (VOD), and severe infections.
Treatment discontinuation due to any AE occurred in 31% of patients in the GO arm and 7% of those in the control arm. The most frequent AEs leading to discontinuation for patients on GO were thrombocytopenia (15%), VOD (3%), and septic shock (2%).
Fatal AEs occurred in 8 patients (6%) in the GO arm and 3 (2%) in the control arm. In the GO arm, 3 patients died of VOD, 4 died of hemorrhage-related events, and 1 died of a suspected cardiac cause. All 3 fatal AEs in the control arm were sepsis.
Idarucizumab receives full FDA approval
The US Food and Drug Administration (FDA) has granted full approval to idarucizumab (Praxbind®), the specific reversal agent for dabigatran etexilate mesylate (Pradaxa®).
Idarucizumab received accelerated approval from the FDA in October 2015.
Now, the drug has full approval for use in reversing dabigatran’s anticoagulant effects in patients who require emergency surgery/urgent procedures and those who experience life-threatening or uncontrolled bleeding.
When the FDA granted idarucizumab accelerated approval, continued approval of the drug was contingent upon results from the phase 3 RE-VERSE AD™ trial.
Final results from RE-VERSE AD were published in NEJM in July 2017.
The trial enrolled 503 patients who required dabigatran reversal. They were divided into 2 groups:
- Group A included 301 patients with uncontrolled or life-threatening bleeding complications (eg, intracranial hemorrhage or severe trauma after a car accident)
- Group B included 202 patients requiring an invasive procedure or an emergency surgery or intervention (eg, surgery for an open fracture after a fall).
The study’s primary endpoint was the degree of reversal of the anticoagulant effect of dabigatran achieved by idarucizumab within 4 hours. The median maximum percentage reversal was 100%, as assessed on the basis of either the diluted thrombin time or the ecarin clotting time.
In group A, 68% of evaluable patients (134/203) had confirmed bleeding cessation within 24 hours of idarucizumab administration. Their median time to hemostasis after idarucizumab administration was 2.5 hours. (The time to the cessation of bleeding could not be assessed in 98 patients with intracranial bleeding.)
For patients in group B, their required procedures began a median of 1.6 hours from idarucizumab administration. Hemostasis during the procedure was described as normal for 93.4% of the patients, mildly abnormal in 5.1%, and moderately abnormal in 1.5%.
At 90 days, thrombotic events had occurred in 6.3% of patients in group A and 7.4% of those in group B. The 90-day mortality rates were 18.8% and 18.9%, respectively.
The US Food and Drug Administration (FDA) has granted full approval to idarucizumab (Praxbind®), the specific reversal agent for dabigatran etexilate mesylate (Pradaxa®).
Idarucizumab received accelerated approval from the FDA in October 2015.
Now, the drug has full approval for use in reversing dabigatran’s anticoagulant effects in patients who require emergency surgery/urgent procedures and those who experience life-threatening or uncontrolled bleeding.
When the FDA granted idarucizumab accelerated approval, continued approval of the drug was contingent upon results from the phase 3 RE-VERSE AD™ trial.
Final results from RE-VERSE AD were published in NEJM in July 2017.
The trial enrolled 503 patients who required dabigatran reversal. They were divided into 2 groups:
- Group A included 301 patients with uncontrolled or life-threatening bleeding complications (eg, intracranial hemorrhage or severe trauma after a car accident)
- Group B included 202 patients requiring an invasive procedure or an emergency surgery or intervention (eg, surgery for an open fracture after a fall).
The study’s primary endpoint was the degree of reversal of the anticoagulant effect of dabigatran achieved by idarucizumab within 4 hours. The median maximum percentage reversal was 100%, as assessed on the basis of either the diluted thrombin time or the ecarin clotting time.
In group A, 68% of evaluable patients (134/203) had confirmed bleeding cessation within 24 hours of idarucizumab administration. Their median time to hemostasis after idarucizumab administration was 2.5 hours. (The time to the cessation of bleeding could not be assessed in 98 patients with intracranial bleeding.)
For patients in group B, their required procedures began a median of 1.6 hours from idarucizumab administration. Hemostasis during the procedure was described as normal for 93.4% of the patients, mildly abnormal in 5.1%, and moderately abnormal in 1.5%.
At 90 days, thrombotic events had occurred in 6.3% of patients in group A and 7.4% of those in group B. The 90-day mortality rates were 18.8% and 18.9%, respectively.
The US Food and Drug Administration (FDA) has granted full approval to idarucizumab (Praxbind®), the specific reversal agent for dabigatran etexilate mesylate (Pradaxa®).
Idarucizumab received accelerated approval from the FDA in October 2015.
Now, the drug has full approval for use in reversing dabigatran’s anticoagulant effects in patients who require emergency surgery/urgent procedures and those who experience life-threatening or uncontrolled bleeding.
When the FDA granted idarucizumab accelerated approval, continued approval of the drug was contingent upon results from the phase 3 RE-VERSE AD™ trial.
Final results from RE-VERSE AD were published in NEJM in July 2017.
The trial enrolled 503 patients who required dabigatran reversal. They were divided into 2 groups:
- Group A included 301 patients with uncontrolled or life-threatening bleeding complications (eg, intracranial hemorrhage or severe trauma after a car accident)
- Group B included 202 patients requiring an invasive procedure or an emergency surgery or intervention (eg, surgery for an open fracture after a fall).
The study’s primary endpoint was the degree of reversal of the anticoagulant effect of dabigatran achieved by idarucizumab within 4 hours. The median maximum percentage reversal was 100%, as assessed on the basis of either the diluted thrombin time or the ecarin clotting time.
In group A, 68% of evaluable patients (134/203) had confirmed bleeding cessation within 24 hours of idarucizumab administration. Their median time to hemostasis after idarucizumab administration was 2.5 hours. (The time to the cessation of bleeding could not be assessed in 98 patients with intracranial bleeding.)
For patients in group B, their required procedures began a median of 1.6 hours from idarucizumab administration. Hemostasis during the procedure was described as normal for 93.4% of the patients, mildly abnormal in 5.1%, and moderately abnormal in 1.5%.
At 90 days, thrombotic events had occurred in 6.3% of patients in group A and 7.4% of those in group B. The 90-day mortality rates were 18.8% and 18.9%, respectively.
Fostamatinib approved to treat adults with chronic ITP
The US Food and Drug Administration (FDA) has granted approval for the oral SYK inhibitor fostamatinib disodium hexahydrate (Tavalisse™).
Fostamatinib is now approved for the treatment of thrombocytopenia in adults with chronic immune thrombocytopenia (ITP) who have had an insufficient response to a previous treatment.
Rigel Pharmaceuticals, Inc., plans to launch fostamatinib in the US in late May 2018.
The FDA’s approval of fostamatinib was supported by data from the FIT clinical program, which included 2 randomized, placebo-controlled, phase 3 trials—FIT-1 (NCT02076399) and FIT-2 (NCT02076412)—and an open-label extension study—FIT-3 (NCT02077192)—as well as an initial proof-of-concept study.
FIT-1 and FIT-2
FIT-1 and FIT-2 included 150 patients with persistent or chronic ITP who had an insufficient response to previous treatment. The patients had a median age of 54 (range, 20 to 88), 61% were female, and 93% were white.
Prior ITP treatments included corticosteroids (94%), immunoglobulins (53%), and thrombopoietin receptor agonists (48%). Thirty-five percent of patients had undergone splenectomy.
The patients’ median platelet count at baseline was 16 x 109/L, and 47% were on stable ITP therapy.
In each study, patients were randomized 2:1 to receive fostamatinib or placebo for 24 weeks. In FIT-1, 76 patients were randomized—51 to fostamatinib and 25 to placebo. In FIT-2, 74 patients were randomized—50 to fostamatinib and 24 to placebo.
All patients initially received fostamatinib at 100 mg twice daily. Most (88%) were escalated to 150 mg twice daily at week 4 or later. Patients could also receive stable concurrent ITP therapy—glucocorticoids (< 20 mg prednisone equivalent per day), azathioprine, or danazol—and rescue therapy if needed.
The efficacy of fostamatinib was based on stable platelet response, defined as a platelet count of at least 50 x 109/L on at least 4 of the 6 visits between weeks 14 to 24.
In FIT-1, 18% of patients in the fostamatinib arm and 0% of those in the placebo arm achieved a stable platelet response (P=0.03).
In FIT-2, 16% of patients in the fostamatinib arm and 4% in the placebo arm achieved a stable platelet response. In this trial, the between-arm difference was not statistically significant.
For both studies, the incidence of bleeding was 29% in the fostamatinib arm and 37% in the placebo arm. The rate of severe bleeding-related events was 1% and 6%, respectively, and the rate of serious bleeding-related events was 4% and 10%, respectively.
FIT-3
Patients from FIT-1 and FIT-2 could enroll in FIT-3 if they completed 24 weeks of treatment or did not respond to treatment any time after 12 weeks.
Patients who were in response at the time of roll over (those who had achieved a platelet count of at least 50 x 109/L) continued in FIT-3 at their current dose and regimen.
Non-responders received fostamatinib at 100 mg twice daily regardless of their dose and regimen in the prior study.
In all, 123 patients were enrolled—44 previously randomized to placebo and 79 previously randomized to fostamatinib. Half of patients (n=61) discontinued the study early.
Of the 44 patients with prior placebo, 10 (23%) had a stable platelet response to fostamatinib. This included a patient who was a responder to placebo in the prior study.
In FIT-3, stable platelet response was defined as having no 2 visits, at least 4 weeks apart, with a platelet count less than 50 x 109/L without an intervening visit with a platelet count of at least 50 x 109/L (unrelated to rescue therapy) within a period of 12 weeks after the patient’s initial achievement of the target platelet count.
Of all the responders in the FIT trials, there were 18 who maintained a platelet count of at least 50 x 109/L for 12 months or longer.
For more details on these trials and fostamatinib, see the full prescribing information, which is available at www.TAVALISSE.com.
The US Food and Drug Administration (FDA) has granted approval for the oral SYK inhibitor fostamatinib disodium hexahydrate (Tavalisse™).
Fostamatinib is now approved for the treatment of thrombocytopenia in adults with chronic immune thrombocytopenia (ITP) who have had an insufficient response to a previous treatment.
Rigel Pharmaceuticals, Inc., plans to launch fostamatinib in the US in late May 2018.
The FDA’s approval of fostamatinib was supported by data from the FIT clinical program, which included 2 randomized, placebo-controlled, phase 3 trials—FIT-1 (NCT02076399) and FIT-2 (NCT02076412)—and an open-label extension study—FIT-3 (NCT02077192)—as well as an initial proof-of-concept study.
FIT-1 and FIT-2
FIT-1 and FIT-2 included 150 patients with persistent or chronic ITP who had an insufficient response to previous treatment. The patients had a median age of 54 (range, 20 to 88), 61% were female, and 93% were white.
Prior ITP treatments included corticosteroids (94%), immunoglobulins (53%), and thrombopoietin receptor agonists (48%). Thirty-five percent of patients had undergone splenectomy.
The patients’ median platelet count at baseline was 16 x 109/L, and 47% were on stable ITP therapy.
In each study, patients were randomized 2:1 to receive fostamatinib or placebo for 24 weeks. In FIT-1, 76 patients were randomized—51 to fostamatinib and 25 to placebo. In FIT-2, 74 patients were randomized—50 to fostamatinib and 24 to placebo.
All patients initially received fostamatinib at 100 mg twice daily. Most (88%) were escalated to 150 mg twice daily at week 4 or later. Patients could also receive stable concurrent ITP therapy—glucocorticoids (< 20 mg prednisone equivalent per day), azathioprine, or danazol—and rescue therapy if needed.
The efficacy of fostamatinib was based on stable platelet response, defined as a platelet count of at least 50 x 109/L on at least 4 of the 6 visits between weeks 14 to 24.
In FIT-1, 18% of patients in the fostamatinib arm and 0% of those in the placebo arm achieved a stable platelet response (P=0.03).
In FIT-2, 16% of patients in the fostamatinib arm and 4% in the placebo arm achieved a stable platelet response. In this trial, the between-arm difference was not statistically significant.
For both studies, the incidence of bleeding was 29% in the fostamatinib arm and 37% in the placebo arm. The rate of severe bleeding-related events was 1% and 6%, respectively, and the rate of serious bleeding-related events was 4% and 10%, respectively.
FIT-3
Patients from FIT-1 and FIT-2 could enroll in FIT-3 if they completed 24 weeks of treatment or did not respond to treatment any time after 12 weeks.
Patients who were in response at the time of roll over (those who had achieved a platelet count of at least 50 x 109/L) continued in FIT-3 at their current dose and regimen.
Non-responders received fostamatinib at 100 mg twice daily regardless of their dose and regimen in the prior study.
In all, 123 patients were enrolled—44 previously randomized to placebo and 79 previously randomized to fostamatinib. Half of patients (n=61) discontinued the study early.
Of the 44 patients with prior placebo, 10 (23%) had a stable platelet response to fostamatinib. This included a patient who was a responder to placebo in the prior study.
In FIT-3, stable platelet response was defined as having no 2 visits, at least 4 weeks apart, with a platelet count less than 50 x 109/L without an intervening visit with a platelet count of at least 50 x 109/L (unrelated to rescue therapy) within a period of 12 weeks after the patient’s initial achievement of the target platelet count.
Of all the responders in the FIT trials, there were 18 who maintained a platelet count of at least 50 x 109/L for 12 months or longer.
For more details on these trials and fostamatinib, see the full prescribing information, which is available at www.TAVALISSE.com.
The US Food and Drug Administration (FDA) has granted approval for the oral SYK inhibitor fostamatinib disodium hexahydrate (Tavalisse™).
Fostamatinib is now approved for the treatment of thrombocytopenia in adults with chronic immune thrombocytopenia (ITP) who have had an insufficient response to a previous treatment.
Rigel Pharmaceuticals, Inc., plans to launch fostamatinib in the US in late May 2018.
The FDA’s approval of fostamatinib was supported by data from the FIT clinical program, which included 2 randomized, placebo-controlled, phase 3 trials—FIT-1 (NCT02076399) and FIT-2 (NCT02076412)—and an open-label extension study—FIT-3 (NCT02077192)—as well as an initial proof-of-concept study.
FIT-1 and FIT-2
FIT-1 and FIT-2 included 150 patients with persistent or chronic ITP who had an insufficient response to previous treatment. The patients had a median age of 54 (range, 20 to 88), 61% were female, and 93% were white.
Prior ITP treatments included corticosteroids (94%), immunoglobulins (53%), and thrombopoietin receptor agonists (48%). Thirty-five percent of patients had undergone splenectomy.
The patients’ median platelet count at baseline was 16 x 109/L, and 47% were on stable ITP therapy.
In each study, patients were randomized 2:1 to receive fostamatinib or placebo for 24 weeks. In FIT-1, 76 patients were randomized—51 to fostamatinib and 25 to placebo. In FIT-2, 74 patients were randomized—50 to fostamatinib and 24 to placebo.
All patients initially received fostamatinib at 100 mg twice daily. Most (88%) were escalated to 150 mg twice daily at week 4 or later. Patients could also receive stable concurrent ITP therapy—glucocorticoids (< 20 mg prednisone equivalent per day), azathioprine, or danazol—and rescue therapy if needed.
The efficacy of fostamatinib was based on stable platelet response, defined as a platelet count of at least 50 x 109/L on at least 4 of the 6 visits between weeks 14 to 24.
In FIT-1, 18% of patients in the fostamatinib arm and 0% of those in the placebo arm achieved a stable platelet response (P=0.03).
In FIT-2, 16% of patients in the fostamatinib arm and 4% in the placebo arm achieved a stable platelet response. In this trial, the between-arm difference was not statistically significant.
For both studies, the incidence of bleeding was 29% in the fostamatinib arm and 37% in the placebo arm. The rate of severe bleeding-related events was 1% and 6%, respectively, and the rate of serious bleeding-related events was 4% and 10%, respectively.
FIT-3
Patients from FIT-1 and FIT-2 could enroll in FIT-3 if they completed 24 weeks of treatment or did not respond to treatment any time after 12 weeks.
Patients who were in response at the time of roll over (those who had achieved a platelet count of at least 50 x 109/L) continued in FIT-3 at their current dose and regimen.
Non-responders received fostamatinib at 100 mg twice daily regardless of their dose and regimen in the prior study.
In all, 123 patients were enrolled—44 previously randomized to placebo and 79 previously randomized to fostamatinib. Half of patients (n=61) discontinued the study early.
Of the 44 patients with prior placebo, 10 (23%) had a stable platelet response to fostamatinib. This included a patient who was a responder to placebo in the prior study.
In FIT-3, stable platelet response was defined as having no 2 visits, at least 4 weeks apart, with a platelet count less than 50 x 109/L without an intervening visit with a platelet count of at least 50 x 109/L (unrelated to rescue therapy) within a period of 12 weeks after the patient’s initial achievement of the target platelet count.
Of all the responders in the FIT trials, there were 18 who maintained a platelet count of at least 50 x 109/L for 12 months or longer.
For more details on these trials and fostamatinib, see the full prescribing information, which is available at www.TAVALISSE.com.
FDA expands approved use of product for VWD
The US Food and Drug Administration (FDA) has expanded the approved use of Vonvendi, a recombinant von Willebrand factor product.
Vonvendi is now approved for perioperative management of bleeding in adults (age 18 and older) with von Willebrand disease (VWD).
Vonvendi was previously FDA-approved for on-demand treatment and control of bleeding episodes in adults with VWD.
“Persons with von Willebrand disease face a heightened risk of bleeding during surgery and may require factor treatment before, during, or after surgery,” said Michael Tarantino, MD, of the Bleeding & Clotting Disorders Institute in Peoria, Illinois.
“For surgeries requiring repeated, frequent infusions with combined von Willebrand factor and factor VIII concentrates, an excessive rise in factor VIII levels may increase the risk of thromboembolic complications, such as blood clots. The expanded use for Vonvendi in surgical settings gives healthcare professionals flexibility in treating von Willebrand disease with an appropriate dose of von Willebrand factor, with or without recombinant factor VIII, based on each patient’s unique needs.”
The FDA’s approval of Vonvendi in surgical settings was based on results from a phase 3 trial. The study enrolled 15 adults with severe VWD who were undergoing elective surgical procedures (10 of them major procedures).
Patients received Vonvendi at 40 to 60 IU per kg of body weight 12 to 24 hours before surgery. Within 3 hours of surgery, each patient’s factor VIII level (FVIII:C) was assessed, with a target of 30 IU/dL for minor surgeries and 60 IU/dL for major surgeries.
Within an hour of surgery, patients received a dose of Vonvendi, with or without recombinant factor VIII, depending on the target FVIII:C levels at the 3-hour assessment.
The study’s primary endpoint was met. Vonvendi demonstrated overall hemostatic efficacy, as assessed 24 hours after the last perioperative infusion or the completion of the study visit, whichever occurred earlier.
Intra- and post-operative hemostasis was rated as “excellent” (as good as or better than expected) in 60% of patients and “good” (probably as good as expected) in 40% of patients.
One patient developed deep vein thrombosis 3 days after undergoing hip replacement surgery.
One patient tested positive for binding antibodies to von Willebrand factor. None of the patients developed binding antibodies against potential impurities such as rFurin, CHO-protein, or mouse IgG.
More details on this study are available in the full prescribing information for Vonvendi.
The US Food and Drug Administration (FDA) has expanded the approved use of Vonvendi, a recombinant von Willebrand factor product.
Vonvendi is now approved for perioperative management of bleeding in adults (age 18 and older) with von Willebrand disease (VWD).
Vonvendi was previously FDA-approved for on-demand treatment and control of bleeding episodes in adults with VWD.
“Persons with von Willebrand disease face a heightened risk of bleeding during surgery and may require factor treatment before, during, or after surgery,” said Michael Tarantino, MD, of the Bleeding & Clotting Disorders Institute in Peoria, Illinois.
“For surgeries requiring repeated, frequent infusions with combined von Willebrand factor and factor VIII concentrates, an excessive rise in factor VIII levels may increase the risk of thromboembolic complications, such as blood clots. The expanded use for Vonvendi in surgical settings gives healthcare professionals flexibility in treating von Willebrand disease with an appropriate dose of von Willebrand factor, with or without recombinant factor VIII, based on each patient’s unique needs.”
The FDA’s approval of Vonvendi in surgical settings was based on results from a phase 3 trial. The study enrolled 15 adults with severe VWD who were undergoing elective surgical procedures (10 of them major procedures).
Patients received Vonvendi at 40 to 60 IU per kg of body weight 12 to 24 hours before surgery. Within 3 hours of surgery, each patient’s factor VIII level (FVIII:C) was assessed, with a target of 30 IU/dL for minor surgeries and 60 IU/dL for major surgeries.
Within an hour of surgery, patients received a dose of Vonvendi, with or without recombinant factor VIII, depending on the target FVIII:C levels at the 3-hour assessment.
The study’s primary endpoint was met. Vonvendi demonstrated overall hemostatic efficacy, as assessed 24 hours after the last perioperative infusion or the completion of the study visit, whichever occurred earlier.
Intra- and post-operative hemostasis was rated as “excellent” (as good as or better than expected) in 60% of patients and “good” (probably as good as expected) in 40% of patients.
One patient developed deep vein thrombosis 3 days after undergoing hip replacement surgery.
One patient tested positive for binding antibodies to von Willebrand factor. None of the patients developed binding antibodies against potential impurities such as rFurin, CHO-protein, or mouse IgG.
More details on this study are available in the full prescribing information for Vonvendi.
The US Food and Drug Administration (FDA) has expanded the approved use of Vonvendi, a recombinant von Willebrand factor product.
Vonvendi is now approved for perioperative management of bleeding in adults (age 18 and older) with von Willebrand disease (VWD).
Vonvendi was previously FDA-approved for on-demand treatment and control of bleeding episodes in adults with VWD.
“Persons with von Willebrand disease face a heightened risk of bleeding during surgery and may require factor treatment before, during, or after surgery,” said Michael Tarantino, MD, of the Bleeding & Clotting Disorders Institute in Peoria, Illinois.
“For surgeries requiring repeated, frequent infusions with combined von Willebrand factor and factor VIII concentrates, an excessive rise in factor VIII levels may increase the risk of thromboembolic complications, such as blood clots. The expanded use for Vonvendi in surgical settings gives healthcare professionals flexibility in treating von Willebrand disease with an appropriate dose of von Willebrand factor, with or without recombinant factor VIII, based on each patient’s unique needs.”
The FDA’s approval of Vonvendi in surgical settings was based on results from a phase 3 trial. The study enrolled 15 adults with severe VWD who were undergoing elective surgical procedures (10 of them major procedures).
Patients received Vonvendi at 40 to 60 IU per kg of body weight 12 to 24 hours before surgery. Within 3 hours of surgery, each patient’s factor VIII level (FVIII:C) was assessed, with a target of 30 IU/dL for minor surgeries and 60 IU/dL for major surgeries.
Within an hour of surgery, patients received a dose of Vonvendi, with or without recombinant factor VIII, depending on the target FVIII:C levels at the 3-hour assessment.
The study’s primary endpoint was met. Vonvendi demonstrated overall hemostatic efficacy, as assessed 24 hours after the last perioperative infusion or the completion of the study visit, whichever occurred earlier.
Intra- and post-operative hemostasis was rated as “excellent” (as good as or better than expected) in 60% of patients and “good” (probably as good as expected) in 40% of patients.
One patient developed deep vein thrombosis 3 days after undergoing hip replacement surgery.
One patient tested positive for binding antibodies to von Willebrand factor. None of the patients developed binding antibodies against potential impurities such as rFurin, CHO-protein, or mouse IgG.
More details on this study are available in the full prescribing information for Vonvendi.
Generic melphalan available in US
Fresenius Kabi’s Melphalan Hydrochloride for Injection, a generic version of Alkeran®, is now available in the US.
Melphalan Hydrochloride for Injection is available as a 2-vial kit containing 1 single-dose vial of melphalan hydrochloride equivalent to 50 mg of melphalan and 1 vial of sterile diluent.
Melphalan Hydrochloride for Injection is indicated for the palliative treatment of patients with multiple myeloma for whom oral therapy is not appropriate.
For more details on Melphalan Hydrochloride for Injection, see the full prescribing information.
Fresenius Kabi’s Melphalan Hydrochloride for Injection, a generic version of Alkeran®, is now available in the US.
Melphalan Hydrochloride for Injection is available as a 2-vial kit containing 1 single-dose vial of melphalan hydrochloride equivalent to 50 mg of melphalan and 1 vial of sterile diluent.
Melphalan Hydrochloride for Injection is indicated for the palliative treatment of patients with multiple myeloma for whom oral therapy is not appropriate.
For more details on Melphalan Hydrochloride for Injection, see the full prescribing information.
Fresenius Kabi’s Melphalan Hydrochloride for Injection, a generic version of Alkeran®, is now available in the US.
Melphalan Hydrochloride for Injection is available as a 2-vial kit containing 1 single-dose vial of melphalan hydrochloride equivalent to 50 mg of melphalan and 1 vial of sterile diluent.
Melphalan Hydrochloride for Injection is indicated for the palliative treatment of patients with multiple myeloma for whom oral therapy is not appropriate.
For more details on Melphalan Hydrochloride for Injection, see the full prescribing information.
Health Canada approves product for adult ALL
Health Canada has approved inotuzumab ozogamicin (Besponsa™) as monotherapy for adults with relapsed or refractory, CD22-positive, B-cell precursor acute lymphoblastic leukemia (ALL).
Inotuzumab ozogamicin is the first and only CD22-directed antibody-drug conjugate approved for this indication.
The product consists of a monoclonal antibody targeting CD22 and a cytotoxic agent known as calicheamicin.
Health Canada’s approval of inotuzumab ozogamicin is based on results from the phase 3 INO-VATE trial, which were published in NEJM in June 2016.
The trial enrolled 326 adults with relapsed or refractory B-cell precursor ALL.
Patients received inotuzumab ozogamicin or 1 of 3 chemotherapy regimens—high-dose cytarabine; cytarabine plus mitoxantrone; or fludarabine, cytarabine, and granulocyte colony-stimulating factor.
The rate of complete remission, including incomplete hematologic recovery, was 80.7% in the inotuzumab arm and 29.4% in the chemotherapy arm (P<0.001). The median duration of remission was 4.6 months and 3.1 months, respectively (P=0.03).
Forty-one percent of patients treated with inotuzumab and 11% of those who received chemotherapy proceeded to stem cell transplant directly after treatment (P<0.001).
The median progression-free survival was 5.0 months in the inotuzumab arm and 1.8 months in the chemotherapy arm (P<0.001).
The median overall survival was 7.7 months and 6.7 months, respectively (P=0.04). This did not meet the prespecified boundary of significance (P=0.0208).
Liver-related adverse events were more common in the inotuzumab arm than the chemotherapy arm. The most frequent of these were increased aspartate aminotransferase level (20% vs 10%), hyperbilirubinemia (15% vs 10%), and increased alanine aminotransferase level (14% vs 11%).
Veno-occlusive liver disease occurred in 11% of patients in the inotuzumab arm and 1% in the chemotherapy arm.
There were 17 deaths during treatment in the inotuzumab arm and 11 in the chemotherapy arm. Four deaths were considered related to inotuzumab, and 2 were deemed related to chemotherapy.
Health Canada has approved inotuzumab ozogamicin (Besponsa™) as monotherapy for adults with relapsed or refractory, CD22-positive, B-cell precursor acute lymphoblastic leukemia (ALL).
Inotuzumab ozogamicin is the first and only CD22-directed antibody-drug conjugate approved for this indication.
The product consists of a monoclonal antibody targeting CD22 and a cytotoxic agent known as calicheamicin.
Health Canada’s approval of inotuzumab ozogamicin is based on results from the phase 3 INO-VATE trial, which were published in NEJM in June 2016.
The trial enrolled 326 adults with relapsed or refractory B-cell precursor ALL.
Patients received inotuzumab ozogamicin or 1 of 3 chemotherapy regimens—high-dose cytarabine; cytarabine plus mitoxantrone; or fludarabine, cytarabine, and granulocyte colony-stimulating factor.
The rate of complete remission, including incomplete hematologic recovery, was 80.7% in the inotuzumab arm and 29.4% in the chemotherapy arm (P<0.001). The median duration of remission was 4.6 months and 3.1 months, respectively (P=0.03).
Forty-one percent of patients treated with inotuzumab and 11% of those who received chemotherapy proceeded to stem cell transplant directly after treatment (P<0.001).
The median progression-free survival was 5.0 months in the inotuzumab arm and 1.8 months in the chemotherapy arm (P<0.001).
The median overall survival was 7.7 months and 6.7 months, respectively (P=0.04). This did not meet the prespecified boundary of significance (P=0.0208).
Liver-related adverse events were more common in the inotuzumab arm than the chemotherapy arm. The most frequent of these were increased aspartate aminotransferase level (20% vs 10%), hyperbilirubinemia (15% vs 10%), and increased alanine aminotransferase level (14% vs 11%).
Veno-occlusive liver disease occurred in 11% of patients in the inotuzumab arm and 1% in the chemotherapy arm.
There were 17 deaths during treatment in the inotuzumab arm and 11 in the chemotherapy arm. Four deaths were considered related to inotuzumab, and 2 were deemed related to chemotherapy.
Health Canada has approved inotuzumab ozogamicin (Besponsa™) as monotherapy for adults with relapsed or refractory, CD22-positive, B-cell precursor acute lymphoblastic leukemia (ALL).
Inotuzumab ozogamicin is the first and only CD22-directed antibody-drug conjugate approved for this indication.
The product consists of a monoclonal antibody targeting CD22 and a cytotoxic agent known as calicheamicin.
Health Canada’s approval of inotuzumab ozogamicin is based on results from the phase 3 INO-VATE trial, which were published in NEJM in June 2016.
The trial enrolled 326 adults with relapsed or refractory B-cell precursor ALL.
Patients received inotuzumab ozogamicin or 1 of 3 chemotherapy regimens—high-dose cytarabine; cytarabine plus mitoxantrone; or fludarabine, cytarabine, and granulocyte colony-stimulating factor.
The rate of complete remission, including incomplete hematologic recovery, was 80.7% in the inotuzumab arm and 29.4% in the chemotherapy arm (P<0.001). The median duration of remission was 4.6 months and 3.1 months, respectively (P=0.03).
Forty-one percent of patients treated with inotuzumab and 11% of those who received chemotherapy proceeded to stem cell transplant directly after treatment (P<0.001).
The median progression-free survival was 5.0 months in the inotuzumab arm and 1.8 months in the chemotherapy arm (P<0.001).
The median overall survival was 7.7 months and 6.7 months, respectively (P=0.04). This did not meet the prespecified boundary of significance (P=0.0208).
Liver-related adverse events were more common in the inotuzumab arm than the chemotherapy arm. The most frequent of these were increased aspartate aminotransferase level (20% vs 10%), hyperbilirubinemia (15% vs 10%), and increased alanine aminotransferase level (14% vs 11%).
Veno-occlusive liver disease occurred in 11% of patients in the inotuzumab arm and 1% in the chemotherapy arm.
There were 17 deaths during treatment in the inotuzumab arm and 11 in the chemotherapy arm. Four deaths were considered related to inotuzumab, and 2 were deemed related to chemotherapy.
Drug receives priority review for HCL
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for moxetumomab pasudotox, an investigational anti-CD22 recombinant immunotoxin.
With this BLA, AstraZeneca is seeking approval for moxetumomab pasudotox for the treatment of adults with hairy cell leukemia (HCL) who have received at least 2 prior lines of therapy.
The FDA expects to make a decision on the BLA in the third quarter of this year.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
About moxetumomab pasudotox
Moxetumomab pasudotox (formerly CAT-8015 or HA22) is composed of a binding portion of an anti-CD22 antibody fused to a toxin. After binding to CD22, the molecule is internalized, processed, and releases its modified protein toxin, which inhibits protein translation and leads to apoptosis.
In addition to priority review, moxetumomab pasudotox has received orphan drug designation from the FDA.
Moxetumomab pasudotox has been tested in a phase 1 trial. Initial results from this trial were published in the Journal of Clinical Oncology in 2012. Long-term follow-up was presented at the 2017 ASH Annual Meeting.
The ASH data included 49 patients with relapsed/refractory HCL. Their median age was 57 (range, 40-77), most (n=41) were male, and they had a median of 35 (range, 1-60,444) circulating HCL cells/mm3 at baseline (in 48 evaluable patients).
Twenty-eight patients received moxetumomab pasudotox in the dose-escalation portion of the study—at 5, 10, 20, 30, 40, or 50 µg/kg—and 21 received the drug at 50 µg/kg for the extension portion of the study.
Among the 33 patients who received moxetumomab pasudotox at 50 µg/kg, the overall response rate was 88%, and the complete response (CR) rate was 64% (n=21). The median time to CR was 3.6 months, and the median duration of CR was 70.3 months.
The median follow-up was 75 months for the entire study population. At 72 months, the progression-free survival (PFS) rate was 77%.
The researchers found that minimal residual disease (MRD) negativity (via immunohistochemistry) was associated with extended response duration and prolonged PFS.
The MRD evaluation included 19 MRD+ patients and 18 MRD- patients. Forty-seven percent of the MRD+ patients (n=9) and 94% of the MRD- patients (n=17) had a CR as their best response.
The median duration of CR was 13.1 months among the MRD+ patients and was not reached among the MRD- patients (P=0.0002). The median PFS was 82.1 months among the MRD+ patients and not reached among the MRD- patients (P=0.0031).
Moxetumomab pasudotox did not undergo phase 2 testing but proceeded to a phase 3 trial. In this single-arm study, researchers evaluated the drug in HCL patients who had received at least 2 prior therapies.
According to AstraZeneca, the study’s primary endpoint—durable CR—was met. The company said the phase 3 results will be presented at an upcoming medical meeting.
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for moxetumomab pasudotox, an investigational anti-CD22 recombinant immunotoxin.
With this BLA, AstraZeneca is seeking approval for moxetumomab pasudotox for the treatment of adults with hairy cell leukemia (HCL) who have received at least 2 prior lines of therapy.
The FDA expects to make a decision on the BLA in the third quarter of this year.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
About moxetumomab pasudotox
Moxetumomab pasudotox (formerly CAT-8015 or HA22) is composed of a binding portion of an anti-CD22 antibody fused to a toxin. After binding to CD22, the molecule is internalized, processed, and releases its modified protein toxin, which inhibits protein translation and leads to apoptosis.
In addition to priority review, moxetumomab pasudotox has received orphan drug designation from the FDA.
Moxetumomab pasudotox has been tested in a phase 1 trial. Initial results from this trial were published in the Journal of Clinical Oncology in 2012. Long-term follow-up was presented at the 2017 ASH Annual Meeting.
The ASH data included 49 patients with relapsed/refractory HCL. Their median age was 57 (range, 40-77), most (n=41) were male, and they had a median of 35 (range, 1-60,444) circulating HCL cells/mm3 at baseline (in 48 evaluable patients).
Twenty-eight patients received moxetumomab pasudotox in the dose-escalation portion of the study—at 5, 10, 20, 30, 40, or 50 µg/kg—and 21 received the drug at 50 µg/kg for the extension portion of the study.
Among the 33 patients who received moxetumomab pasudotox at 50 µg/kg, the overall response rate was 88%, and the complete response (CR) rate was 64% (n=21). The median time to CR was 3.6 months, and the median duration of CR was 70.3 months.
The median follow-up was 75 months for the entire study population. At 72 months, the progression-free survival (PFS) rate was 77%.
The researchers found that minimal residual disease (MRD) negativity (via immunohistochemistry) was associated with extended response duration and prolonged PFS.
The MRD evaluation included 19 MRD+ patients and 18 MRD- patients. Forty-seven percent of the MRD+ patients (n=9) and 94% of the MRD- patients (n=17) had a CR as their best response.
The median duration of CR was 13.1 months among the MRD+ patients and was not reached among the MRD- patients (P=0.0002). The median PFS was 82.1 months among the MRD+ patients and not reached among the MRD- patients (P=0.0031).
Moxetumomab pasudotox did not undergo phase 2 testing but proceeded to a phase 3 trial. In this single-arm study, researchers evaluated the drug in HCL patients who had received at least 2 prior therapies.
According to AstraZeneca, the study’s primary endpoint—durable CR—was met. The company said the phase 3 results will be presented at an upcoming medical meeting.
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for moxetumomab pasudotox, an investigational anti-CD22 recombinant immunotoxin.
With this BLA, AstraZeneca is seeking approval for moxetumomab pasudotox for the treatment of adults with hairy cell leukemia (HCL) who have received at least 2 prior lines of therapy.
The FDA expects to make a decision on the BLA in the third quarter of this year.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
About moxetumomab pasudotox
Moxetumomab pasudotox (formerly CAT-8015 or HA22) is composed of a binding portion of an anti-CD22 antibody fused to a toxin. After binding to CD22, the molecule is internalized, processed, and releases its modified protein toxin, which inhibits protein translation and leads to apoptosis.
In addition to priority review, moxetumomab pasudotox has received orphan drug designation from the FDA.
Moxetumomab pasudotox has been tested in a phase 1 trial. Initial results from this trial were published in the Journal of Clinical Oncology in 2012. Long-term follow-up was presented at the 2017 ASH Annual Meeting.
The ASH data included 49 patients with relapsed/refractory HCL. Their median age was 57 (range, 40-77), most (n=41) were male, and they had a median of 35 (range, 1-60,444) circulating HCL cells/mm3 at baseline (in 48 evaluable patients).
Twenty-eight patients received moxetumomab pasudotox in the dose-escalation portion of the study—at 5, 10, 20, 30, 40, or 50 µg/kg—and 21 received the drug at 50 µg/kg for the extension portion of the study.
Among the 33 patients who received moxetumomab pasudotox at 50 µg/kg, the overall response rate was 88%, and the complete response (CR) rate was 64% (n=21). The median time to CR was 3.6 months, and the median duration of CR was 70.3 months.
The median follow-up was 75 months for the entire study population. At 72 months, the progression-free survival (PFS) rate was 77%.
The researchers found that minimal residual disease (MRD) negativity (via immunohistochemistry) was associated with extended response duration and prolonged PFS.
The MRD evaluation included 19 MRD+ patients and 18 MRD- patients. Forty-seven percent of the MRD+ patients (n=9) and 94% of the MRD- patients (n=17) had a CR as their best response.
The median duration of CR was 13.1 months among the MRD+ patients and was not reached among the MRD- patients (P=0.0002). The median PFS was 82.1 months among the MRD+ patients and not reached among the MRD- patients (P=0.0031).
Moxetumomab pasudotox did not undergo phase 2 testing but proceeded to a phase 3 trial. In this single-arm study, researchers evaluated the drug in HCL patients who had received at least 2 prior therapies.
According to AstraZeneca, the study’s primary endpoint—durable CR—was met. The company said the phase 3 results will be presented at an upcoming medical meeting.