User login
FDA expands approved indication for lenalidomide
The US Food and Drug Administration (FDA) has approved a new indication for lenalidomide (Revlimid).
The drug is now approved for use as maintenance therapy after autologous hematopoietic stem cell transplant (auto-HSCT) in patients with multiple myeloma (MM).
The expanded indication makes lenalidomide the first treatment to receive FDA approval for maintenance following auto-HSCT.
The drug was previously FDA-approved for use in combination with dexamethasone to treat patients with MM.
Lenalidomide is also FDA-approved to treat patients with transfusion-dependent anemia due to low-or intermediate-1-risk myelodysplastic syndromes associated with deletion 5q, with or without additional cytogenetic abnormalities.
And lenalidomide is FDA-approved to treat patients with mantle cell lymphoma who have relapsed or progressed after 2 prior therapies, one of which included bortezomib.
Lenalidomide is a product of Celgene.
Studies: Lenalidomide maintenance
The latest approval for lenalidomide was based on results of 2 cooperative group-led studies, CALGB 10010410 and IFM 2005-0211.
Results from both studies were published in NEJM in May 2012 (CALGB 100104, IFM 2005-02). The updated data reported here are included in the prescribing information for lenalidomide.
CALGB 100104 was a phase 3, double-blind study of 460 patients with newly diagnosed MM undergoing auto-HSCT. The patients received continuous daily treatment with lenalidomide or placebo until relapse.
IFM 2005-02 was a phase 3, double-blind study of 614 patients newly diagnosed with MM. The patients were randomized to receive a 2-month consolidation regimen after auto-HSCT, which consisted of lenalidomide monotherapy followed by continuous daily treatment with lenalidomide or placebo until relapse.
Survival
In both studies, the primary efficacy endpoint was progression-free survival (PFS). The PFS data for both studies were updated to reflect results as of March 2015.
In the CALGB study, the median PFS was 5.7 years in the lenalidomide arm and 1.9 years in the placebo arm (hazard ratio [HR]=0.38 [95% CI: 0.28-0.50]).
In the IFM study, the median PFS was 3.9 years in the lenalidomide arm and 2 years in the placebo arm (HR=0.53 [95% CI: 0.44-0.64]).
These studies were not powered for an overall survival (OS) endpoint. However, OS was recorded, and the OS data for both studies were updated to reflect results as of February 2016.
The median OS in the CALGB study was 9.3 years in the lenalidomide arm and 7 years in the placebo arm (HR=0.59 [95% CI: 0.44-0.78]).
In the IFM study, the median OS was 8.8 years in the lenalidomide arm and 7.3 years in the placebo arm (HR=0.90 [95% CI: 0.72-1.13]).
Adverse events
The most frequently reported adverse events in ≥20% of patients in the lenalidomide arm across both studies (CALGB and IFM, respectively) were neutropenia (79%, 61%), thrombocytopenia (72%, 24%), leukopenia (23%, 32%), anemia (21%, 9%), upper respiratory tract infection (27%, 11%), bronchitis (5%, 47%), nasopharyngitis (2%, 35%), cough (10%, 27%), gastroenteritis (0%, 23%), diarrhea (55%, 39%), rash (32%, 8%), fatigue (23%, 11%), asthenia (0%, 30%), muscle spasm (0%, 33%), and pyrexia (8%, 21%).
The most frequently reported grade 3/4 events (more than 20% in the lenalidomide arm) were neutropenia, thrombocytopenia, and leukopenia.
Hematologic second primary malignancies (SPM) occurred in 7.5% of patients receiving lenalidomide maintenance and 3.3% of controls.
The incidence of hematologic plus solid tumor SPM (excluding squamous cell carcinoma and basal cell carcinoma) was 14.9% in the lenalidomide group and 8.8% in the control group, with a median follow-up of 91.5 months.
Non-melanoma skin cancer SPM, including squamous cell carcinoma and basal cell carcinoma, occurred in 3.9% of patients receiving lenalidomide maintenance and 2.6% of controls. ![]()
The US Food and Drug Administration (FDA) has approved a new indication for lenalidomide (Revlimid).
The drug is now approved for use as maintenance therapy after autologous hematopoietic stem cell transplant (auto-HSCT) in patients with multiple myeloma (MM).
The expanded indication makes lenalidomide the first treatment to receive FDA approval for maintenance following auto-HSCT.
The drug was previously FDA-approved for use in combination with dexamethasone to treat patients with MM.
Lenalidomide is also FDA-approved to treat patients with transfusion-dependent anemia due to low-or intermediate-1-risk myelodysplastic syndromes associated with deletion 5q, with or without additional cytogenetic abnormalities.
And lenalidomide is FDA-approved to treat patients with mantle cell lymphoma who have relapsed or progressed after 2 prior therapies, one of which included bortezomib.
Lenalidomide is a product of Celgene.
Studies: Lenalidomide maintenance
The latest approval for lenalidomide was based on results of 2 cooperative group-led studies, CALGB 10010410 and IFM 2005-0211.
Results from both studies were published in NEJM in May 2012 (CALGB 100104, IFM 2005-02). The updated data reported here are included in the prescribing information for lenalidomide.
CALGB 100104 was a phase 3, double-blind study of 460 patients with newly diagnosed MM undergoing auto-HSCT. The patients received continuous daily treatment with lenalidomide or placebo until relapse.
IFM 2005-02 was a phase 3, double-blind study of 614 patients newly diagnosed with MM. The patients were randomized to receive a 2-month consolidation regimen after auto-HSCT, which consisted of lenalidomide monotherapy followed by continuous daily treatment with lenalidomide or placebo until relapse.
Survival
In both studies, the primary efficacy endpoint was progression-free survival (PFS). The PFS data for both studies were updated to reflect results as of March 2015.
In the CALGB study, the median PFS was 5.7 years in the lenalidomide arm and 1.9 years in the placebo arm (hazard ratio [HR]=0.38 [95% CI: 0.28-0.50]).
In the IFM study, the median PFS was 3.9 years in the lenalidomide arm and 2 years in the placebo arm (HR=0.53 [95% CI: 0.44-0.64]).
These studies were not powered for an overall survival (OS) endpoint. However, OS was recorded, and the OS data for both studies were updated to reflect results as of February 2016.
The median OS in the CALGB study was 9.3 years in the lenalidomide arm and 7 years in the placebo arm (HR=0.59 [95% CI: 0.44-0.78]).
In the IFM study, the median OS was 8.8 years in the lenalidomide arm and 7.3 years in the placebo arm (HR=0.90 [95% CI: 0.72-1.13]).
Adverse events
The most frequently reported adverse events in ≥20% of patients in the lenalidomide arm across both studies (CALGB and IFM, respectively) were neutropenia (79%, 61%), thrombocytopenia (72%, 24%), leukopenia (23%, 32%), anemia (21%, 9%), upper respiratory tract infection (27%, 11%), bronchitis (5%, 47%), nasopharyngitis (2%, 35%), cough (10%, 27%), gastroenteritis (0%, 23%), diarrhea (55%, 39%), rash (32%, 8%), fatigue (23%, 11%), asthenia (0%, 30%), muscle spasm (0%, 33%), and pyrexia (8%, 21%).
The most frequently reported grade 3/4 events (more than 20% in the lenalidomide arm) were neutropenia, thrombocytopenia, and leukopenia.
Hematologic second primary malignancies (SPM) occurred in 7.5% of patients receiving lenalidomide maintenance and 3.3% of controls.
The incidence of hematologic plus solid tumor SPM (excluding squamous cell carcinoma and basal cell carcinoma) was 14.9% in the lenalidomide group and 8.8% in the control group, with a median follow-up of 91.5 months.
Non-melanoma skin cancer SPM, including squamous cell carcinoma and basal cell carcinoma, occurred in 3.9% of patients receiving lenalidomide maintenance and 2.6% of controls. ![]()
The US Food and Drug Administration (FDA) has approved a new indication for lenalidomide (Revlimid).
The drug is now approved for use as maintenance therapy after autologous hematopoietic stem cell transplant (auto-HSCT) in patients with multiple myeloma (MM).
The expanded indication makes lenalidomide the first treatment to receive FDA approval for maintenance following auto-HSCT.
The drug was previously FDA-approved for use in combination with dexamethasone to treat patients with MM.
Lenalidomide is also FDA-approved to treat patients with transfusion-dependent anemia due to low-or intermediate-1-risk myelodysplastic syndromes associated with deletion 5q, with or without additional cytogenetic abnormalities.
And lenalidomide is FDA-approved to treat patients with mantle cell lymphoma who have relapsed or progressed after 2 prior therapies, one of which included bortezomib.
Lenalidomide is a product of Celgene.
Studies: Lenalidomide maintenance
The latest approval for lenalidomide was based on results of 2 cooperative group-led studies, CALGB 10010410 and IFM 2005-0211.
Results from both studies were published in NEJM in May 2012 (CALGB 100104, IFM 2005-02). The updated data reported here are included in the prescribing information for lenalidomide.
CALGB 100104 was a phase 3, double-blind study of 460 patients with newly diagnosed MM undergoing auto-HSCT. The patients received continuous daily treatment with lenalidomide or placebo until relapse.
IFM 2005-02 was a phase 3, double-blind study of 614 patients newly diagnosed with MM. The patients were randomized to receive a 2-month consolidation regimen after auto-HSCT, which consisted of lenalidomide monotherapy followed by continuous daily treatment with lenalidomide or placebo until relapse.
Survival
In both studies, the primary efficacy endpoint was progression-free survival (PFS). The PFS data for both studies were updated to reflect results as of March 2015.
In the CALGB study, the median PFS was 5.7 years in the lenalidomide arm and 1.9 years in the placebo arm (hazard ratio [HR]=0.38 [95% CI: 0.28-0.50]).
In the IFM study, the median PFS was 3.9 years in the lenalidomide arm and 2 years in the placebo arm (HR=0.53 [95% CI: 0.44-0.64]).
These studies were not powered for an overall survival (OS) endpoint. However, OS was recorded, and the OS data for both studies were updated to reflect results as of February 2016.
The median OS in the CALGB study was 9.3 years in the lenalidomide arm and 7 years in the placebo arm (HR=0.59 [95% CI: 0.44-0.78]).
In the IFM study, the median OS was 8.8 years in the lenalidomide arm and 7.3 years in the placebo arm (HR=0.90 [95% CI: 0.72-1.13]).
Adverse events
The most frequently reported adverse events in ≥20% of patients in the lenalidomide arm across both studies (CALGB and IFM, respectively) were neutropenia (79%, 61%), thrombocytopenia (72%, 24%), leukopenia (23%, 32%), anemia (21%, 9%), upper respiratory tract infection (27%, 11%), bronchitis (5%, 47%), nasopharyngitis (2%, 35%), cough (10%, 27%), gastroenteritis (0%, 23%), diarrhea (55%, 39%), rash (32%, 8%), fatigue (23%, 11%), asthenia (0%, 30%), muscle spasm (0%, 33%), and pyrexia (8%, 21%).
The most frequently reported grade 3/4 events (more than 20% in the lenalidomide arm) were neutropenia, thrombocytopenia, and leukopenia.
Hematologic second primary malignancies (SPM) occurred in 7.5% of patients receiving lenalidomide maintenance and 3.3% of controls.
The incidence of hematologic plus solid tumor SPM (excluding squamous cell carcinoma and basal cell carcinoma) was 14.9% in the lenalidomide group and 8.8% in the control group, with a median follow-up of 91.5 months.
Non-melanoma skin cancer SPM, including squamous cell carcinoma and basal cell carcinoma, occurred in 3.9% of patients receiving lenalidomide maintenance and 2.6% of controls. ![]()
CHMP recommends authorization of antiemetic agent
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for the antiemetic agent rolapitant (Varuby) as a treatment for adults with cancer.
The drug is intended to be used in combination with other antiemetic agents to prevent delayed nausea and vomiting associated with highly and moderately emetogenic chemotherapy.
The CHMP’s recommendation regarding rolapitant has been forwarded to the European Commission, which is expected to make a decision about the drug within 2 months.
If the commission authorizes marketing of rolapitant, the drug will be available as 90 mg film-coated tablets.
The applicant for rolapitant is Tesaro UK Limited.
Rolapitant clinical trials
Results from three phase 3 trials suggested that rolapitant (at 180 mg) in combination with a 5-HT3 receptor antagonist and dexamethasone was more effective than the 5-HT3 receptor antagonist and dexamethasone on their own (active control).
The 3-drug combination demonstrated a significant reduction in episodes of vomiting or use of rescue medication during the 25- to 120-hour period following administration of highly emetogenic and moderately emetogenic chemotherapy regimens.
In addition, patients who received rolapitant reported experiencing less nausea that interfered with normal daily life and fewer episodes of vomiting or retching over multiple cycles of chemotherapy.
Highly emetogenic chemotherapy
The clinical profile of rolapitant in cisplatin-based, highly emetogenic chemotherapy (HEC) was confirmed in two phase 3 studies: HEC1 and HEC2. Results from these trials were published in The Lancet Oncology in August 2015.
Both trials met their primary endpoint of complete response (CR) and demonstrated statistical superiority of the rolapitant combination compared to active control.
In HEC1, 264 patients received the rolapitant combination, and 262 received active control. The proportion of patients achieving a CR was 72.7% and 58.4%, respectively (P<0.001).
In HEC2, 271 patients received the rolapitant combination, and 273 received active control. The proportion of patients achieving a CR was 70.1% and 61.9%, respectively (P=0.043).
The most common adverse events (in the rolapitant and control groups, respectively) were neutropenia (9% and 8%), hiccups (5% and 4%), and abdominal pain (3% and 2%).
Moderately emetogenic chemotherapy
Researchers conducted another phase 3 trial to compare the rolapitant combination with active control in 1332 patients receiving moderately emetogenic chemotherapy. Results from this trial were also published in The Lancet Oncology in August 2015.
This trial met its primary endpoint of CR and demonstrated statistical superiority of the rolapitant combination compared to active control. The proportion of patients achieving a CR was 71.3% and 61.6%, respectively (P<0.001).
The most common adverse events (in the rolapitant and control groups, respectively) were decreased appetite (9% and 7%), neutropenia (7% and 6%), dizziness (6% and 4%), dyspepsia (4% and 2%), urinary tract infection (4% and 3%), stomatitis (4% and 2%), and anemia (3% and 2%). ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for the antiemetic agent rolapitant (Varuby) as a treatment for adults with cancer.
The drug is intended to be used in combination with other antiemetic agents to prevent delayed nausea and vomiting associated with highly and moderately emetogenic chemotherapy.
The CHMP’s recommendation regarding rolapitant has been forwarded to the European Commission, which is expected to make a decision about the drug within 2 months.
If the commission authorizes marketing of rolapitant, the drug will be available as 90 mg film-coated tablets.
The applicant for rolapitant is Tesaro UK Limited.
Rolapitant clinical trials
Results from three phase 3 trials suggested that rolapitant (at 180 mg) in combination with a 5-HT3 receptor antagonist and dexamethasone was more effective than the 5-HT3 receptor antagonist and dexamethasone on their own (active control).
The 3-drug combination demonstrated a significant reduction in episodes of vomiting or use of rescue medication during the 25- to 120-hour period following administration of highly emetogenic and moderately emetogenic chemotherapy regimens.
In addition, patients who received rolapitant reported experiencing less nausea that interfered with normal daily life and fewer episodes of vomiting or retching over multiple cycles of chemotherapy.
Highly emetogenic chemotherapy
The clinical profile of rolapitant in cisplatin-based, highly emetogenic chemotherapy (HEC) was confirmed in two phase 3 studies: HEC1 and HEC2. Results from these trials were published in The Lancet Oncology in August 2015.
Both trials met their primary endpoint of complete response (CR) and demonstrated statistical superiority of the rolapitant combination compared to active control.
In HEC1, 264 patients received the rolapitant combination, and 262 received active control. The proportion of patients achieving a CR was 72.7% and 58.4%, respectively (P<0.001).
In HEC2, 271 patients received the rolapitant combination, and 273 received active control. The proportion of patients achieving a CR was 70.1% and 61.9%, respectively (P=0.043).
The most common adverse events (in the rolapitant and control groups, respectively) were neutropenia (9% and 8%), hiccups (5% and 4%), and abdominal pain (3% and 2%).
Moderately emetogenic chemotherapy
Researchers conducted another phase 3 trial to compare the rolapitant combination with active control in 1332 patients receiving moderately emetogenic chemotherapy. Results from this trial were also published in The Lancet Oncology in August 2015.
This trial met its primary endpoint of CR and demonstrated statistical superiority of the rolapitant combination compared to active control. The proportion of patients achieving a CR was 71.3% and 61.6%, respectively (P<0.001).
The most common adverse events (in the rolapitant and control groups, respectively) were decreased appetite (9% and 7%), neutropenia (7% and 6%), dizziness (6% and 4%), dyspepsia (4% and 2%), urinary tract infection (4% and 3%), stomatitis (4% and 2%), and anemia (3% and 2%). ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for the antiemetic agent rolapitant (Varuby) as a treatment for adults with cancer.
The drug is intended to be used in combination with other antiemetic agents to prevent delayed nausea and vomiting associated with highly and moderately emetogenic chemotherapy.
The CHMP’s recommendation regarding rolapitant has been forwarded to the European Commission, which is expected to make a decision about the drug within 2 months.
If the commission authorizes marketing of rolapitant, the drug will be available as 90 mg film-coated tablets.
The applicant for rolapitant is Tesaro UK Limited.
Rolapitant clinical trials
Results from three phase 3 trials suggested that rolapitant (at 180 mg) in combination with a 5-HT3 receptor antagonist and dexamethasone was more effective than the 5-HT3 receptor antagonist and dexamethasone on their own (active control).
The 3-drug combination demonstrated a significant reduction in episodes of vomiting or use of rescue medication during the 25- to 120-hour period following administration of highly emetogenic and moderately emetogenic chemotherapy regimens.
In addition, patients who received rolapitant reported experiencing less nausea that interfered with normal daily life and fewer episodes of vomiting or retching over multiple cycles of chemotherapy.
Highly emetogenic chemotherapy
The clinical profile of rolapitant in cisplatin-based, highly emetogenic chemotherapy (HEC) was confirmed in two phase 3 studies: HEC1 and HEC2. Results from these trials were published in The Lancet Oncology in August 2015.
Both trials met their primary endpoint of complete response (CR) and demonstrated statistical superiority of the rolapitant combination compared to active control.
In HEC1, 264 patients received the rolapitant combination, and 262 received active control. The proportion of patients achieving a CR was 72.7% and 58.4%, respectively (P<0.001).
In HEC2, 271 patients received the rolapitant combination, and 273 received active control. The proportion of patients achieving a CR was 70.1% and 61.9%, respectively (P=0.043).
The most common adverse events (in the rolapitant and control groups, respectively) were neutropenia (9% and 8%), hiccups (5% and 4%), and abdominal pain (3% and 2%).
Moderately emetogenic chemotherapy
Researchers conducted another phase 3 trial to compare the rolapitant combination with active control in 1332 patients receiving moderately emetogenic chemotherapy. Results from this trial were also published in The Lancet Oncology in August 2015.
This trial met its primary endpoint of CR and demonstrated statistical superiority of the rolapitant combination compared to active control. The proportion of patients achieving a CR was 71.3% and 61.6%, respectively (P<0.001).
The most common adverse events (in the rolapitant and control groups, respectively) were decreased appetite (9% and 7%), neutropenia (7% and 6%), dizziness (6% and 4%), dyspepsia (4% and 2%), urinary tract infection (4% and 3%), stomatitis (4% and 2%), and anemia (3% and 2%). ![]()
CHMP advocates approval of edoxaban product
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that Roteas receive marketing authorization for the same indications as Lixiana.
Both Roteas and Lixiana are oral factor Xa inhibitors that contain the active ingredient edoxaban.
The CHMP has recommended approving Roteas for the treatment and prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE) in adults.
In addition, the CHMP has recommended approving Roteas for the prevention of stroke and systemic embolism in adults with nonvalvular atrial fibrillation (NVAF) who have 1 or more risk factors, such as congestive heart failure, hypertension, age of 75 or older, diabetes mellitus, prior stroke, or transient ischemic attack.
The European Commission approved Lixiana for these indications in June 2015.
If the European Commission decides to approve Roteas as well, the product will be available as film-coated tablets (15 mg, 30 mg, and 60 mg).
The European Commission is expected to make a decision about Roteas within 67 days from the CHMP’s adoption of its opinion (which occurred on February 23).
The application for Roteas was an informed consent application. In this type of application, reference is made to an authorized medicine if the marketing authorization holder of the reference medicine has given consent to the use of their dossier in the application procedure.
The applicant for Roteas is Daiichi Sankyo Europe GmbH, the company that also developed Lixiana.
Lixiana was approved based on data from a pair of phase 3 trials, ENGAGE AF-TIMI 48 and Hokusai-VTE.
Hokusai-VTE
In the Hokusai-VTE trial, researchers evaluated edoxaban in 4921 patients with DVT and 3319 with PE. Patients received initial treatment with low-molecular-weight heparin and were then randomized to receive edoxaban or warfarin daily for 3 to 12 months.
Overall, edoxaban proved as effective as warfarin. Recurrent, symptomatic DVT/PE occurred in 3.2% and 3.5% of patients, respectively (P<0.001 for non-inferiority).
In addition, the incidence of clinically relevant bleeding was significantly lower in the edoxaban arm than the warfarin arm—8.5% and 10.3%, respectively (P=0.004 for superiority).
ENGAGE-AF TIMI 48
In the ENGAGE AF-TIMI 48 trial, researchers compared edoxaban and warfarin as prophylaxis for stroke or systemic embolism in patients with NVAF.
The trial included 21,105 patients who were randomized to receive warfarin (n=7036), edoxaban at 60 mg (n=7035), or edoxaban at 30 mg (n=7034).
Edoxaban was at least non-inferior to warfarin with regard to efficacy. The annual incidence of stroke or systemic embolism was 1.50% with warfarin, 1.18% with edoxaban at 60 mg (P<0.001 for non-inferiority), and 1.61% with edoxaban at 30 mg (P=0.005 for non-inferiority).
In addition, edoxaban was associated with a significantly lower rate of major and fatal bleeding. The annual incidence of major bleeding was 3.43% with warfarin, 2.75% with edoxaban at 60 mg (P<0.001), and 1.61% with edoxaban at 30 mg (P<0.001).
Fatal bleeds occurred at an annual rate of 0.38% with warfarin, 0.21% with edoxaban at 60 mg (P=0.006), and 0.13% with edoxaban at 30 mg (P<0.001). ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that Roteas receive marketing authorization for the same indications as Lixiana.
Both Roteas and Lixiana are oral factor Xa inhibitors that contain the active ingredient edoxaban.
The CHMP has recommended approving Roteas for the treatment and prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE) in adults.
In addition, the CHMP has recommended approving Roteas for the prevention of stroke and systemic embolism in adults with nonvalvular atrial fibrillation (NVAF) who have 1 or more risk factors, such as congestive heart failure, hypertension, age of 75 or older, diabetes mellitus, prior stroke, or transient ischemic attack.
The European Commission approved Lixiana for these indications in June 2015.
If the European Commission decides to approve Roteas as well, the product will be available as film-coated tablets (15 mg, 30 mg, and 60 mg).
The European Commission is expected to make a decision about Roteas within 67 days from the CHMP’s adoption of its opinion (which occurred on February 23).
The application for Roteas was an informed consent application. In this type of application, reference is made to an authorized medicine if the marketing authorization holder of the reference medicine has given consent to the use of their dossier in the application procedure.
The applicant for Roteas is Daiichi Sankyo Europe GmbH, the company that also developed Lixiana.
Lixiana was approved based on data from a pair of phase 3 trials, ENGAGE AF-TIMI 48 and Hokusai-VTE.
Hokusai-VTE
In the Hokusai-VTE trial, researchers evaluated edoxaban in 4921 patients with DVT and 3319 with PE. Patients received initial treatment with low-molecular-weight heparin and were then randomized to receive edoxaban or warfarin daily for 3 to 12 months.
Overall, edoxaban proved as effective as warfarin. Recurrent, symptomatic DVT/PE occurred in 3.2% and 3.5% of patients, respectively (P<0.001 for non-inferiority).
In addition, the incidence of clinically relevant bleeding was significantly lower in the edoxaban arm than the warfarin arm—8.5% and 10.3%, respectively (P=0.004 for superiority).
ENGAGE-AF TIMI 48
In the ENGAGE AF-TIMI 48 trial, researchers compared edoxaban and warfarin as prophylaxis for stroke or systemic embolism in patients with NVAF.
The trial included 21,105 patients who were randomized to receive warfarin (n=7036), edoxaban at 60 mg (n=7035), or edoxaban at 30 mg (n=7034).
Edoxaban was at least non-inferior to warfarin with regard to efficacy. The annual incidence of stroke or systemic embolism was 1.50% with warfarin, 1.18% with edoxaban at 60 mg (P<0.001 for non-inferiority), and 1.61% with edoxaban at 30 mg (P=0.005 for non-inferiority).
In addition, edoxaban was associated with a significantly lower rate of major and fatal bleeding. The annual incidence of major bleeding was 3.43% with warfarin, 2.75% with edoxaban at 60 mg (P<0.001), and 1.61% with edoxaban at 30 mg (P<0.001).
Fatal bleeds occurred at an annual rate of 0.38% with warfarin, 0.21% with edoxaban at 60 mg (P=0.006), and 0.13% with edoxaban at 30 mg (P<0.001). ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that Roteas receive marketing authorization for the same indications as Lixiana.
Both Roteas and Lixiana are oral factor Xa inhibitors that contain the active ingredient edoxaban.
The CHMP has recommended approving Roteas for the treatment and prevention of deep vein thrombosis (DVT) and pulmonary embolism (PE) in adults.
In addition, the CHMP has recommended approving Roteas for the prevention of stroke and systemic embolism in adults with nonvalvular atrial fibrillation (NVAF) who have 1 or more risk factors, such as congestive heart failure, hypertension, age of 75 or older, diabetes mellitus, prior stroke, or transient ischemic attack.
The European Commission approved Lixiana for these indications in June 2015.
If the European Commission decides to approve Roteas as well, the product will be available as film-coated tablets (15 mg, 30 mg, and 60 mg).
The European Commission is expected to make a decision about Roteas within 67 days from the CHMP’s adoption of its opinion (which occurred on February 23).
The application for Roteas was an informed consent application. In this type of application, reference is made to an authorized medicine if the marketing authorization holder of the reference medicine has given consent to the use of their dossier in the application procedure.
The applicant for Roteas is Daiichi Sankyo Europe GmbH, the company that also developed Lixiana.
Lixiana was approved based on data from a pair of phase 3 trials, ENGAGE AF-TIMI 48 and Hokusai-VTE.
Hokusai-VTE
In the Hokusai-VTE trial, researchers evaluated edoxaban in 4921 patients with DVT and 3319 with PE. Patients received initial treatment with low-molecular-weight heparin and were then randomized to receive edoxaban or warfarin daily for 3 to 12 months.
Overall, edoxaban proved as effective as warfarin. Recurrent, symptomatic DVT/PE occurred in 3.2% and 3.5% of patients, respectively (P<0.001 for non-inferiority).
In addition, the incidence of clinically relevant bleeding was significantly lower in the edoxaban arm than the warfarin arm—8.5% and 10.3%, respectively (P=0.004 for superiority).
ENGAGE-AF TIMI 48
In the ENGAGE AF-TIMI 48 trial, researchers compared edoxaban and warfarin as prophylaxis for stroke or systemic embolism in patients with NVAF.
The trial included 21,105 patients who were randomized to receive warfarin (n=7036), edoxaban at 60 mg (n=7035), or edoxaban at 30 mg (n=7034).
Edoxaban was at least non-inferior to warfarin with regard to efficacy. The annual incidence of stroke or systemic embolism was 1.50% with warfarin, 1.18% with edoxaban at 60 mg (P<0.001 for non-inferiority), and 1.61% with edoxaban at 30 mg (P=0.005 for non-inferiority).
In addition, edoxaban was associated with a significantly lower rate of major and fatal bleeding. The annual incidence of major bleeding was 3.43% with warfarin, 2.75% with edoxaban at 60 mg (P<0.001), and 1.61% with edoxaban at 30 mg (P<0.001).
Fatal bleeds occurred at an annual rate of 0.38% with warfarin, 0.21% with edoxaban at 60 mg (P=0.006), and 0.13% with edoxaban at 30 mg (P<0.001). ![]()
CHMP recommends new indication for daratumumab
The CHMP recommended approving daratumumab in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone as treatment for adults with multiple myeloma (MM) who have received at least 1 prior therapy.
The CHMP’s recommendation has been forwarded to the European Commission, which is expected to make its decision on daratumumab within 2 months.
Daratumumab is a human IgG1k monoclonal antibody that binds to CD38, which is highly expressed on the surface of MM cells.
Daratumumab is being developed by Janssen Biotech, Inc. under an exclusive worldwide license from Genmab.
Phase 3 trials
The CHMP’s recommendation regarding daratumumab was based on data from the phase 3 POLLUX and CASTOR trials.
In the POLLUX trial, researchers compared treatment with lenalidomide and dexamethasone to treatment with daratumumab, lenalidomide, and dexamethasone in patients with relapsed or refractory MM.
Patients who received daratumumab in combination had a significantly higher response rate and longer progression-free survival than patients who received the 2-drug combination.
However, treatment with daratumumab was associated with infusion-related reactions and a higher incidence of neutropenia.
Results from this trial were published in NEJM in October 2016.
In the CASTOR trial, researchers compared treatment with bortezomib and dexamethasone to treatment with daratumumab, bortezomib, and dexamethasone in patients with previously treated MM.
Patients who received the 3-drug combination had a higher response rate, longer progression-free survival, and a higher incidence of grade 3/4 adverse events than those who received the 2-drug combination.
Results from this trial were published in NEJM in August 2016. ![]()
The CHMP recommended approving daratumumab in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone as treatment for adults with multiple myeloma (MM) who have received at least 1 prior therapy.
The CHMP’s recommendation has been forwarded to the European Commission, which is expected to make its decision on daratumumab within 2 months.
Daratumumab is a human IgG1k monoclonal antibody that binds to CD38, which is highly expressed on the surface of MM cells.
Daratumumab is being developed by Janssen Biotech, Inc. under an exclusive worldwide license from Genmab.
Phase 3 trials
The CHMP’s recommendation regarding daratumumab was based on data from the phase 3 POLLUX and CASTOR trials.
In the POLLUX trial, researchers compared treatment with lenalidomide and dexamethasone to treatment with daratumumab, lenalidomide, and dexamethasone in patients with relapsed or refractory MM.
Patients who received daratumumab in combination had a significantly higher response rate and longer progression-free survival than patients who received the 2-drug combination.
However, treatment with daratumumab was associated with infusion-related reactions and a higher incidence of neutropenia.
Results from this trial were published in NEJM in October 2016.
In the CASTOR trial, researchers compared treatment with bortezomib and dexamethasone to treatment with daratumumab, bortezomib, and dexamethasone in patients with previously treated MM.
Patients who received the 3-drug combination had a higher response rate, longer progression-free survival, and a higher incidence of grade 3/4 adverse events than those who received the 2-drug combination.
Results from this trial were published in NEJM in August 2016. ![]()
The CHMP recommended approving daratumumab in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone as treatment for adults with multiple myeloma (MM) who have received at least 1 prior therapy.
The CHMP’s recommendation has been forwarded to the European Commission, which is expected to make its decision on daratumumab within 2 months.
Daratumumab is a human IgG1k monoclonal antibody that binds to CD38, which is highly expressed on the surface of MM cells.
Daratumumab is being developed by Janssen Biotech, Inc. under an exclusive worldwide license from Genmab.
Phase 3 trials
The CHMP’s recommendation regarding daratumumab was based on data from the phase 3 POLLUX and CASTOR trials.
In the POLLUX trial, researchers compared treatment with lenalidomide and dexamethasone to treatment with daratumumab, lenalidomide, and dexamethasone in patients with relapsed or refractory MM.
Patients who received daratumumab in combination had a significantly higher response rate and longer progression-free survival than patients who received the 2-drug combination.
However, treatment with daratumumab was associated with infusion-related reactions and a higher incidence of neutropenia.
Results from this trial were published in NEJM in October 2016.
In the CASTOR trial, researchers compared treatment with bortezomib and dexamethasone to treatment with daratumumab, bortezomib, and dexamethasone in patients with previously treated MM.
Patients who received the 3-drug combination had a higher response rate, longer progression-free survival, and a higher incidence of grade 3/4 adverse events than those who received the 2-drug combination.
Results from this trial were published in NEJM in August 2016. ![]()
Drug granted orphan status for follicular lymphoma
The US Food and Drug Administration (FDA) has granted orphan designation to G100 for the treatment of follicular lymphoma.
G100 is a synthetic small-molecule toll-like receptor-4 agonist, glucopyranosyl lipid A, formulated in a stable emulsion.
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases. This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved.
G100 is being developed by Immune Design. The company says G100 works by leveraging the activation of innate and adaptive immunity in the tumor microenvironment to create an immune response against the tumor’s pre-existing antigens.
According to Immune Design, clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The ensuing induction of local and systemic immune responses has been shown to result in local and abscopal tumor control in preclinical studies.
In fact, G100, when combined with local radiation, demonstrated efficacy against A20 lymphoma in mice. This research was presented in a poster at the 2016 ASH Annual Meeting (abstract 4166).
In this study, investigators evaluated the immune response and therapeutic effects of intratumoral G100 alone, local radiation alone, and concomitant G100 and local radiation in mice with A20 lymphoma.
The investigators said the combination therapy demonstrated:
- Synergistic antitumor effects in both injected as well as uninjected tumors (abscopal effects)
- Synergistic induction of pro-inflammatory cytokine and chemokine environment, as well as induction of genes governing antigen processing and presentation
- Increased infiltration of T cells, including CD4 and CD8 T cells, in treated tumors.
In contrast, tumors that received only radiation had significantly lower T-cell levels than untreated tumors.
“These findings highlight the potential beneficial effect that immunotherapy with G100 could provide when given with radiation by modulating the tumor microenvironment to generate a systemic, durable, T-cell anti-tumor response,” said study investigator Ramesh Rengan, MD, of the University of Washington in Seattle.
“As shown in this model, G100 may hold potential as a treatment for lymphoma patients.”
To test that theory, Immune Design is conducting a phase 1/2 trial of G100 given with local radiation or the anti-PD-1 agent pembrolizumab to patients with follicular lymphoma. ![]()
The US Food and Drug Administration (FDA) has granted orphan designation to G100 for the treatment of follicular lymphoma.
G100 is a synthetic small-molecule toll-like receptor-4 agonist, glucopyranosyl lipid A, formulated in a stable emulsion.
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases. This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved.
G100 is being developed by Immune Design. The company says G100 works by leveraging the activation of innate and adaptive immunity in the tumor microenvironment to create an immune response against the tumor’s pre-existing antigens.
According to Immune Design, clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The ensuing induction of local and systemic immune responses has been shown to result in local and abscopal tumor control in preclinical studies.
In fact, G100, when combined with local radiation, demonstrated efficacy against A20 lymphoma in mice. This research was presented in a poster at the 2016 ASH Annual Meeting (abstract 4166).
In this study, investigators evaluated the immune response and therapeutic effects of intratumoral G100 alone, local radiation alone, and concomitant G100 and local radiation in mice with A20 lymphoma.
The investigators said the combination therapy demonstrated:
- Synergistic antitumor effects in both injected as well as uninjected tumors (abscopal effects)
- Synergistic induction of pro-inflammatory cytokine and chemokine environment, as well as induction of genes governing antigen processing and presentation
- Increased infiltration of T cells, including CD4 and CD8 T cells, in treated tumors.
In contrast, tumors that received only radiation had significantly lower T-cell levels than untreated tumors.
“These findings highlight the potential beneficial effect that immunotherapy with G100 could provide when given with radiation by modulating the tumor microenvironment to generate a systemic, durable, T-cell anti-tumor response,” said study investigator Ramesh Rengan, MD, of the University of Washington in Seattle.
“As shown in this model, G100 may hold potential as a treatment for lymphoma patients.”
To test that theory, Immune Design is conducting a phase 1/2 trial of G100 given with local radiation or the anti-PD-1 agent pembrolizumab to patients with follicular lymphoma. ![]()
The US Food and Drug Administration (FDA) has granted orphan designation to G100 for the treatment of follicular lymphoma.
G100 is a synthetic small-molecule toll-like receptor-4 agonist, glucopyranosyl lipid A, formulated in a stable emulsion.
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases. This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved.
G100 is being developed by Immune Design. The company says G100 works by leveraging the activation of innate and adaptive immunity in the tumor microenvironment to create an immune response against the tumor’s pre-existing antigens.
According to Immune Design, clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The ensuing induction of local and systemic immune responses has been shown to result in local and abscopal tumor control in preclinical studies.
In fact, G100, when combined with local radiation, demonstrated efficacy against A20 lymphoma in mice. This research was presented in a poster at the 2016 ASH Annual Meeting (abstract 4166).
In this study, investigators evaluated the immune response and therapeutic effects of intratumoral G100 alone, local radiation alone, and concomitant G100 and local radiation in mice with A20 lymphoma.
The investigators said the combination therapy demonstrated:
- Synergistic antitumor effects in both injected as well as uninjected tumors (abscopal effects)
- Synergistic induction of pro-inflammatory cytokine and chemokine environment, as well as induction of genes governing antigen processing and presentation
- Increased infiltration of T cells, including CD4 and CD8 T cells, in treated tumors.
In contrast, tumors that received only radiation had significantly lower T-cell levels than untreated tumors.
“These findings highlight the potential beneficial effect that immunotherapy with G100 could provide when given with radiation by modulating the tumor microenvironment to generate a systemic, durable, T-cell anti-tumor response,” said study investigator Ramesh Rengan, MD, of the University of Washington in Seattle.
“As shown in this model, G100 may hold potential as a treatment for lymphoma patients.”
To test that theory, Immune Design is conducting a phase 1/2 trial of G100 given with local radiation or the anti-PD-1 agent pembrolizumab to patients with follicular lymphoma. ![]()
European Commission approves rituximab biosimilar
The European Commission has approved a biosimilar rituximab product, Truxima™, for all the same indications as the reference product, MabThera.
This means Truxima (formerly called CT-P10) is approved for use in the European Union to treat patients with non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis (RA), granulomatosis with polyangiitis (GPA), and microscopic polyangiitis (MPA).
Truxima, a product of Celltrion Healthcare Hungary Kft, is the first biosimilar monoclonal antibody approved in an oncology indication worldwide.
The approval is based on data submitted to the European Medicines Agency.
The agency’s Committee for Medicinal Products for Human Use (CHMP) said the evidence suggests Truxima and MabThera are similar in terms of efficacy, safety, immunogenicity, pharmacodynamics, and pharmacokinetics in patients with RA and advanced follicular lymphoma (FL).
Therefore, the European Commission approved Truxima for the following indications.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV FL.
Truxima maintenance therapy is indicated for the treatment of FL patients responding to induction therapy.
Truxima monotherapy is indicated for the treatment of patients with stage III-IV FL who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that limited efficacy and safety data are available for patients previously treated with monoclonal antibodies, including rituximab, or patients who are refractory to previous rituximab plus chemotherapy.
RA, GPA, and MPA
Truxima in combination with methotrexate is indicated for the treatment of adults with severe, active RA who have had an inadequate response to or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active GPA or MPA.
Truxima studies
There are 3 ongoing, phase 3 trials of Truxima in patients with RA (NCT02149121), advanced FL (NCT02162771), and low-tumor-burden FL (NCT02260804).
Results from the phase 1/3 trial in patients with newly diagnosed, advanced FL suggest that Truxima and the reference rituximab are similar with regard to pharmacokinetics, immunogenicity, and safety (B Coiffier et al. ASH 2016, abstract 1807).
Results from the phase 3 study of RA patients indicate that Truxima is similar to reference products (EU and US-sourced rituximab) with regard to pharmacodynamics, safety, and efficacy for up to 24 weeks (DH Yoo et al. 2016 ACR/ARHP Annual Meeting, abstract 1635). ![]()
The European Commission has approved a biosimilar rituximab product, Truxima™, for all the same indications as the reference product, MabThera.
This means Truxima (formerly called CT-P10) is approved for use in the European Union to treat patients with non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis (RA), granulomatosis with polyangiitis (GPA), and microscopic polyangiitis (MPA).
Truxima, a product of Celltrion Healthcare Hungary Kft, is the first biosimilar monoclonal antibody approved in an oncology indication worldwide.
The approval is based on data submitted to the European Medicines Agency.
The agency’s Committee for Medicinal Products for Human Use (CHMP) said the evidence suggests Truxima and MabThera are similar in terms of efficacy, safety, immunogenicity, pharmacodynamics, and pharmacokinetics in patients with RA and advanced follicular lymphoma (FL).
Therefore, the European Commission approved Truxima for the following indications.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV FL.
Truxima maintenance therapy is indicated for the treatment of FL patients responding to induction therapy.
Truxima monotherapy is indicated for the treatment of patients with stage III-IV FL who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that limited efficacy and safety data are available for patients previously treated with monoclonal antibodies, including rituximab, or patients who are refractory to previous rituximab plus chemotherapy.
RA, GPA, and MPA
Truxima in combination with methotrexate is indicated for the treatment of adults with severe, active RA who have had an inadequate response to or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active GPA or MPA.
Truxima studies
There are 3 ongoing, phase 3 trials of Truxima in patients with RA (NCT02149121), advanced FL (NCT02162771), and low-tumor-burden FL (NCT02260804).
Results from the phase 1/3 trial in patients with newly diagnosed, advanced FL suggest that Truxima and the reference rituximab are similar with regard to pharmacokinetics, immunogenicity, and safety (B Coiffier et al. ASH 2016, abstract 1807).
Results from the phase 3 study of RA patients indicate that Truxima is similar to reference products (EU and US-sourced rituximab) with regard to pharmacodynamics, safety, and efficacy for up to 24 weeks (DH Yoo et al. 2016 ACR/ARHP Annual Meeting, abstract 1635). ![]()
The European Commission has approved a biosimilar rituximab product, Truxima™, for all the same indications as the reference product, MabThera.
This means Truxima (formerly called CT-P10) is approved for use in the European Union to treat patients with non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis (RA), granulomatosis with polyangiitis (GPA), and microscopic polyangiitis (MPA).
Truxima, a product of Celltrion Healthcare Hungary Kft, is the first biosimilar monoclonal antibody approved in an oncology indication worldwide.
The approval is based on data submitted to the European Medicines Agency.
The agency’s Committee for Medicinal Products for Human Use (CHMP) said the evidence suggests Truxima and MabThera are similar in terms of efficacy, safety, immunogenicity, pharmacodynamics, and pharmacokinetics in patients with RA and advanced follicular lymphoma (FL).
Therefore, the European Commission approved Truxima for the following indications.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV FL.
Truxima maintenance therapy is indicated for the treatment of FL patients responding to induction therapy.
Truxima monotherapy is indicated for the treatment of patients with stage III-IV FL who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that limited efficacy and safety data are available for patients previously treated with monoclonal antibodies, including rituximab, or patients who are refractory to previous rituximab plus chemotherapy.
RA, GPA, and MPA
Truxima in combination with methotrexate is indicated for the treatment of adults with severe, active RA who have had an inadequate response to or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active GPA or MPA.
Truxima studies
There are 3 ongoing, phase 3 trials of Truxima in patients with RA (NCT02149121), advanced FL (NCT02162771), and low-tumor-burden FL (NCT02260804).
Results from the phase 1/3 trial in patients with newly diagnosed, advanced FL suggest that Truxima and the reference rituximab are similar with regard to pharmacokinetics, immunogenicity, and safety (B Coiffier et al. ASH 2016, abstract 1807).
Results from the phase 3 study of RA patients indicate that Truxima is similar to reference products (EU and US-sourced rituximab) with regard to pharmacodynamics, safety, and efficacy for up to 24 weeks (DH Yoo et al. 2016 ACR/ARHP Annual Meeting, abstract 1635). ![]()
Group ranks TKIs according to cardiotoxicity
Researchers say they have devised a way to rank tyrosine kinase inhibitors (TKIs) based on their likelihood of causing lasting heart damage in patients.
The team found they could accurately identify those TKIs already known to be the most dangerous.
The researchers believe that, in the future, their system may prove useful in the early stages of drug development to screen new compounds for cardiotoxicity.
“This type of study represents a critical step forward from the usual process running from initial drug discovery and clinical trials in human patients,” said study author Joseph Wu, MD, PhD, of Stanford University School of Medicine in California.
“It will help pharmaceutical companies better focus their efforts on developing safer drugs, and it will provide patients more effective drugs with fewer side effects.”
Dr Wu and his colleagues described this research in Science Translational Medicine.
The researchers began with human induced pluripotent stem cell-derived cardiomyocytes generated from the cells of 11 healthy people and 2 patients with kidney cancer.
The team grew the cardiomyocytes in a dish and tested the effects of 21 commonly used TKIs on the cells.
Treatment with drug levels equivalent to those taken by patients often caused the cells to beat irregularly and begin to die. The cells also displayed differences in the electrophysiological signaling that controls their contraction.
The researchers used these and other measurements to develop a cardiac safety index for each drug. They found that TKIs known to be particularly dangerous to heart function had the lowest safety indices, and TKIs known to be better tolerated by patients ranked higher on the safety index.
High cardiotoxicity
Seven of the 21 TKIs tested were assigned cardiac safety indices at or below 0.1—the threshold limit at which the researchers designated a drug highly cardiotoxic.
These TKIs (from lowest to highest safety score) were vemurafenib, sorafenib, doxorubicin, regorafenib, vandetanib, crizotinib, and nilotinib.
Three of the most cardiotoxic TKIs (regorafenib, sorafenib, and vandetanib) are known to inhibit the same 2 signaling pathways: VEGFR2 and PDGFR.
The researchers noticed that cells treated with these 3 drugs ramped up the activity of a cellular signaling pathway that responds to insulin or IGF1, an insulin-like growth factor.
This discovery, coupled with the fact that treatment with insulin or IGF1 is known to enhance heart function during adverse cardiac events such as heart attacks, led the researchers to experiment further.
They found that exposing the cells to insulin or IGF1 made it less likely they would die due to TKIs blocking the VEGFR2 and PDGFR pathways. Although more research is needed, these findings suggest it may be possible to alleviate some of the heart damage in patients receiving these TKIs.
“There is a critical need for a way to ‘safety test’ all drugs earlier in development before they are administered to patients,” Dr Wu said. “Our drug safety index is a step in that direction.” ![]()
Researchers say they have devised a way to rank tyrosine kinase inhibitors (TKIs) based on their likelihood of causing lasting heart damage in patients.
The team found they could accurately identify those TKIs already known to be the most dangerous.
The researchers believe that, in the future, their system may prove useful in the early stages of drug development to screen new compounds for cardiotoxicity.
“This type of study represents a critical step forward from the usual process running from initial drug discovery and clinical trials in human patients,” said study author Joseph Wu, MD, PhD, of Stanford University School of Medicine in California.
“It will help pharmaceutical companies better focus their efforts on developing safer drugs, and it will provide patients more effective drugs with fewer side effects.”
Dr Wu and his colleagues described this research in Science Translational Medicine.
The researchers began with human induced pluripotent stem cell-derived cardiomyocytes generated from the cells of 11 healthy people and 2 patients with kidney cancer.
The team grew the cardiomyocytes in a dish and tested the effects of 21 commonly used TKIs on the cells.
Treatment with drug levels equivalent to those taken by patients often caused the cells to beat irregularly and begin to die. The cells also displayed differences in the electrophysiological signaling that controls their contraction.
The researchers used these and other measurements to develop a cardiac safety index for each drug. They found that TKIs known to be particularly dangerous to heart function had the lowest safety indices, and TKIs known to be better tolerated by patients ranked higher on the safety index.
High cardiotoxicity
Seven of the 21 TKIs tested were assigned cardiac safety indices at or below 0.1—the threshold limit at which the researchers designated a drug highly cardiotoxic.
These TKIs (from lowest to highest safety score) were vemurafenib, sorafenib, doxorubicin, regorafenib, vandetanib, crizotinib, and nilotinib.
Three of the most cardiotoxic TKIs (regorafenib, sorafenib, and vandetanib) are known to inhibit the same 2 signaling pathways: VEGFR2 and PDGFR.
The researchers noticed that cells treated with these 3 drugs ramped up the activity of a cellular signaling pathway that responds to insulin or IGF1, an insulin-like growth factor.
This discovery, coupled with the fact that treatment with insulin or IGF1 is known to enhance heart function during adverse cardiac events such as heart attacks, led the researchers to experiment further.
They found that exposing the cells to insulin or IGF1 made it less likely they would die due to TKIs blocking the VEGFR2 and PDGFR pathways. Although more research is needed, these findings suggest it may be possible to alleviate some of the heart damage in patients receiving these TKIs.
“There is a critical need for a way to ‘safety test’ all drugs earlier in development before they are administered to patients,” Dr Wu said. “Our drug safety index is a step in that direction.” ![]()
Researchers say they have devised a way to rank tyrosine kinase inhibitors (TKIs) based on their likelihood of causing lasting heart damage in patients.
The team found they could accurately identify those TKIs already known to be the most dangerous.
The researchers believe that, in the future, their system may prove useful in the early stages of drug development to screen new compounds for cardiotoxicity.
“This type of study represents a critical step forward from the usual process running from initial drug discovery and clinical trials in human patients,” said study author Joseph Wu, MD, PhD, of Stanford University School of Medicine in California.
“It will help pharmaceutical companies better focus their efforts on developing safer drugs, and it will provide patients more effective drugs with fewer side effects.”
Dr Wu and his colleagues described this research in Science Translational Medicine.
The researchers began with human induced pluripotent stem cell-derived cardiomyocytes generated from the cells of 11 healthy people and 2 patients with kidney cancer.
The team grew the cardiomyocytes in a dish and tested the effects of 21 commonly used TKIs on the cells.
Treatment with drug levels equivalent to those taken by patients often caused the cells to beat irregularly and begin to die. The cells also displayed differences in the electrophysiological signaling that controls their contraction.
The researchers used these and other measurements to develop a cardiac safety index for each drug. They found that TKIs known to be particularly dangerous to heart function had the lowest safety indices, and TKIs known to be better tolerated by patients ranked higher on the safety index.
High cardiotoxicity
Seven of the 21 TKIs tested were assigned cardiac safety indices at or below 0.1—the threshold limit at which the researchers designated a drug highly cardiotoxic.
These TKIs (from lowest to highest safety score) were vemurafenib, sorafenib, doxorubicin, regorafenib, vandetanib, crizotinib, and nilotinib.
Three of the most cardiotoxic TKIs (regorafenib, sorafenib, and vandetanib) are known to inhibit the same 2 signaling pathways: VEGFR2 and PDGFR.
The researchers noticed that cells treated with these 3 drugs ramped up the activity of a cellular signaling pathway that responds to insulin or IGF1, an insulin-like growth factor.
This discovery, coupled with the fact that treatment with insulin or IGF1 is known to enhance heart function during adverse cardiac events such as heart attacks, led the researchers to experiment further.
They found that exposing the cells to insulin or IGF1 made it less likely they would die due to TKIs blocking the VEGFR2 and PDGFR pathways. Although more research is needed, these findings suggest it may be possible to alleviate some of the heart damage in patients receiving these TKIs.
“There is a critical need for a way to ‘safety test’ all drugs earlier in development before they are administered to patients,” Dr Wu said. “Our drug safety index is a step in that direction.” ![]()
FDA approves IVIG product for PI and chronic ITP

Photo by Bill Branson
The US Food and Drug Administration (FDA) has approved an intravenous immunoglobulin (IVIG) product (Gammaplex® 10%) for the treatment of primary immunodeficiency (PI) and chronic immune thrombocytopenia (ITP) in adults.
PI includes, but is not limited to,
the humoral immune defect in common variable immunodeficiency, X-linked and congenital
agammaglobulinemia, Wiskott-Aldrich
syndrome, and severe combined immunodeficiencies.
Gammaplex 10% is manufactured by Bio Products Laboratory Limited (BPL).
Gammaplex 10% is made with the same process as BPL’s previously approved IVIG treatment, Gammaplex® 5% (immune globulin intravenous [human], 5% liquid).
Gammaplex 10% is more concentrated than Gammaplex 5%, with an immune globulin G (IgG) concentration of 100 g/L, and is stabilized with glycine.
The FDA’s approval of Gammaplex 10% was based on a 2-phase, crossover bioequivalence study comparing Gammaplex 10% and Gammaplex 5% in 33 adult patients with PI. This study is the first direct comparison of 10% and 5% IVIG products in the treatment of PI.
The primary endpoint of bioequivalence between the products was achieved, and trough levels of IgG were well maintained throughout the study.
Both Gammaplex 10% and Gammaplex 5% infusion rates were increased incrementally at 15-minute intervals if tolerated by the subject. The Gammaplex 10% infusion rate was increased to the maximum in 96% of infusions.
The mean infusion time for Gammaplex 10% was 1 hour and 51 minutes, which was 57 minutes faster than Gammaplex 5%.
There were no notable differences in the safety and tolerability of the 2 products.
The most common adverse events in patients receiving Gammaplex 10% were headache (12.5%), migraine (6.3%), and pyrexia (6.3%). There were no serious product-related adverse events.
The safety of Gammaplex 10% has not been established in adults with chronic ITP. The safety profile for Gammaplex 5% has been studied in a phase 3 trial of adults with chronic ITP, and it is anticipated that the safety profile for both formulations are comparable for ITP patients.
The most common adverse events in adults with chronic ITP receiving Gammaplex 5% were headache, vomiting, nausea, pyrexia, arthralgia, and dehydration. Serious adverse events were headache, vomiting, and dehydration.
The full prescribing information for Gammaplex 10%, which includes trial data, is available at http://www.gammaplex.com. ![]()

Photo by Bill Branson
The US Food and Drug Administration (FDA) has approved an intravenous immunoglobulin (IVIG) product (Gammaplex® 10%) for the treatment of primary immunodeficiency (PI) and chronic immune thrombocytopenia (ITP) in adults.
PI includes, but is not limited to,
the humoral immune defect in common variable immunodeficiency, X-linked and congenital
agammaglobulinemia, Wiskott-Aldrich
syndrome, and severe combined immunodeficiencies.
Gammaplex 10% is manufactured by Bio Products Laboratory Limited (BPL).
Gammaplex 10% is made with the same process as BPL’s previously approved IVIG treatment, Gammaplex® 5% (immune globulin intravenous [human], 5% liquid).
Gammaplex 10% is more concentrated than Gammaplex 5%, with an immune globulin G (IgG) concentration of 100 g/L, and is stabilized with glycine.
The FDA’s approval of Gammaplex 10% was based on a 2-phase, crossover bioequivalence study comparing Gammaplex 10% and Gammaplex 5% in 33 adult patients with PI. This study is the first direct comparison of 10% and 5% IVIG products in the treatment of PI.
The primary endpoint of bioequivalence between the products was achieved, and trough levels of IgG were well maintained throughout the study.
Both Gammaplex 10% and Gammaplex 5% infusion rates were increased incrementally at 15-minute intervals if tolerated by the subject. The Gammaplex 10% infusion rate was increased to the maximum in 96% of infusions.
The mean infusion time for Gammaplex 10% was 1 hour and 51 minutes, which was 57 minutes faster than Gammaplex 5%.
There were no notable differences in the safety and tolerability of the 2 products.
The most common adverse events in patients receiving Gammaplex 10% were headache (12.5%), migraine (6.3%), and pyrexia (6.3%). There were no serious product-related adverse events.
The safety of Gammaplex 10% has not been established in adults with chronic ITP. The safety profile for Gammaplex 5% has been studied in a phase 3 trial of adults with chronic ITP, and it is anticipated that the safety profile for both formulations are comparable for ITP patients.
The most common adverse events in adults with chronic ITP receiving Gammaplex 5% were headache, vomiting, nausea, pyrexia, arthralgia, and dehydration. Serious adverse events were headache, vomiting, and dehydration.
The full prescribing information for Gammaplex 10%, which includes trial data, is available at http://www.gammaplex.com. ![]()

Photo by Bill Branson
The US Food and Drug Administration (FDA) has approved an intravenous immunoglobulin (IVIG) product (Gammaplex® 10%) for the treatment of primary immunodeficiency (PI) and chronic immune thrombocytopenia (ITP) in adults.
PI includes, but is not limited to,
the humoral immune defect in common variable immunodeficiency, X-linked and congenital
agammaglobulinemia, Wiskott-Aldrich
syndrome, and severe combined immunodeficiencies.
Gammaplex 10% is manufactured by Bio Products Laboratory Limited (BPL).
Gammaplex 10% is made with the same process as BPL’s previously approved IVIG treatment, Gammaplex® 5% (immune globulin intravenous [human], 5% liquid).
Gammaplex 10% is more concentrated than Gammaplex 5%, with an immune globulin G (IgG) concentration of 100 g/L, and is stabilized with glycine.
The FDA’s approval of Gammaplex 10% was based on a 2-phase, crossover bioequivalence study comparing Gammaplex 10% and Gammaplex 5% in 33 adult patients with PI. This study is the first direct comparison of 10% and 5% IVIG products in the treatment of PI.
The primary endpoint of bioequivalence between the products was achieved, and trough levels of IgG were well maintained throughout the study.
Both Gammaplex 10% and Gammaplex 5% infusion rates were increased incrementally at 15-minute intervals if tolerated by the subject. The Gammaplex 10% infusion rate was increased to the maximum in 96% of infusions.
The mean infusion time for Gammaplex 10% was 1 hour and 51 minutes, which was 57 minutes faster than Gammaplex 5%.
There were no notable differences in the safety and tolerability of the 2 products.
The most common adverse events in patients receiving Gammaplex 10% were headache (12.5%), migraine (6.3%), and pyrexia (6.3%). There were no serious product-related adverse events.
The safety of Gammaplex 10% has not been established in adults with chronic ITP. The safety profile for Gammaplex 5% has been studied in a phase 3 trial of adults with chronic ITP, and it is anticipated that the safety profile for both formulations are comparable for ITP patients.
The most common adverse events in adults with chronic ITP receiving Gammaplex 5% were headache, vomiting, nausea, pyrexia, arthralgia, and dehydration. Serious adverse events were headache, vomiting, and dehydration.
The full prescribing information for Gammaplex 10%, which includes trial data, is available at http://www.gammaplex.com.
Therapy granted PIM designation for CTCL

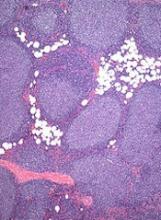
mycosis fungoides
The UK’s Medicines and Healthcare Products Regulatory Agency (MHRA) has granted SGX301 (synthetic hypericin) Promising Innovative Medicine (PIM) designation for the treatment of cutaneous T-cell lymphoma (CTCL).
The PIM designation is the first step toward inclusion in the Early Access to Medicines Scheme (EAMS).
EAMS provides early access to new medicines for patients with life-threatening and seriously debilitating conditions.
PIM status is awarded following an assessment of early nonclinical and clinical data by the MHRA.
PIM designation has been created as an early signal to companies that a product’s development plan is appropriate and indicates that a product could be a candidate for the second phase of the EAMS scheme once further development work has been conducted.
In the second phase, the product is made available to UK patients before a marketing authorization is approved.
The requirements for PIM designation are:
- The condition should be life-threatening or seriously debilitating with a high unmet medical need (ie, there is no method of treatment, diagnosis, or prevention available, or existing methods have serious limitations).
- The medicinal product is likely to offer a major advantage over methods currently used in the UK.
- The potential adverse effects of the medicinal product are likely to be outweighed by the benefits, allowing for the reasonable expectation of a positive benefit-risk balance. A positive benefit-risk balance should be based on preliminary scientific evidence, as justified by the applicant.
About SGX301
SGX301 is a photodynamic therapy utilizing safe, visible light for activation. The active ingredient in SGX301 is synthetic hypericin, a photosensitizer that is applied to skin lesions and then activated by fluorescent light 16 to 24 hours later.
Combined with photoactivation, hypericin has demonstrated significant antiproliferative effects on activated, normal human lymphoid cells and inhibited the growth of malignant T cells isolated from CTCL patients. Topical hypericin has also proven safe in a phase 1 study of healthy volunteers.
In a phase 2 trial of patients with CTCL (mycosis fungoides only) or psoriasis, topical hypericin conferred a significant improvement over placebo. Among CTCL patients, the treatment prompted a response rate of 58.3%, compared to an 8.3% response rate for placebo (P≤0.04).
Topical hypericin was also well tolerated in this trial. There were no deaths or serious adverse events related to the treatment. However, there were reports of mild to moderate burning, itching, erythema, and pruritus at the application site.
A phase 3 trial of SGX301 is currently recruiting patients. SGX301 is under development by Soligenix, Inc.

mycosis fungoides
The UK’s Medicines and Healthcare Products Regulatory Agency (MHRA) has granted SGX301 (synthetic hypericin) Promising Innovative Medicine (PIM) designation for the treatment of cutaneous T-cell lymphoma (CTCL).
The PIM designation is the first step toward inclusion in the Early Access to Medicines Scheme (EAMS).
EAMS provides early access to new medicines for patients with life-threatening and seriously debilitating conditions.
PIM status is awarded following an assessment of early nonclinical and clinical data by the MHRA.
PIM designation has been created as an early signal to companies that a product’s development plan is appropriate and indicates that a product could be a candidate for the second phase of the EAMS scheme once further development work has been conducted.
In the second phase, the product is made available to UK patients before a marketing authorization is approved.
The requirements for PIM designation are:
- The condition should be life-threatening or seriously debilitating with a high unmet medical need (ie, there is no method of treatment, diagnosis, or prevention available, or existing methods have serious limitations).
- The medicinal product is likely to offer a major advantage over methods currently used in the UK.
- The potential adverse effects of the medicinal product are likely to be outweighed by the benefits, allowing for the reasonable expectation of a positive benefit-risk balance. A positive benefit-risk balance should be based on preliminary scientific evidence, as justified by the applicant.
About SGX301
SGX301 is a photodynamic therapy utilizing safe, visible light for activation. The active ingredient in SGX301 is synthetic hypericin, a photosensitizer that is applied to skin lesions and then activated by fluorescent light 16 to 24 hours later.
Combined with photoactivation, hypericin has demonstrated significant antiproliferative effects on activated, normal human lymphoid cells and inhibited the growth of malignant T cells isolated from CTCL patients. Topical hypericin has also proven safe in a phase 1 study of healthy volunteers.
In a phase 2 trial of patients with CTCL (mycosis fungoides only) or psoriasis, topical hypericin conferred a significant improvement over placebo. Among CTCL patients, the treatment prompted a response rate of 58.3%, compared to an 8.3% response rate for placebo (P≤0.04).
Topical hypericin was also well tolerated in this trial. There were no deaths or serious adverse events related to the treatment. However, there were reports of mild to moderate burning, itching, erythema, and pruritus at the application site.
A phase 3 trial of SGX301 is currently recruiting patients. SGX301 is under development by Soligenix, Inc.

mycosis fungoides
The UK’s Medicines and Healthcare Products Regulatory Agency (MHRA) has granted SGX301 (synthetic hypericin) Promising Innovative Medicine (PIM) designation for the treatment of cutaneous T-cell lymphoma (CTCL).
The PIM designation is the first step toward inclusion in the Early Access to Medicines Scheme (EAMS).
EAMS provides early access to new medicines for patients with life-threatening and seriously debilitating conditions.
PIM status is awarded following an assessment of early nonclinical and clinical data by the MHRA.
PIM designation has been created as an early signal to companies that a product’s development plan is appropriate and indicates that a product could be a candidate for the second phase of the EAMS scheme once further development work has been conducted.
In the second phase, the product is made available to UK patients before a marketing authorization is approved.
The requirements for PIM designation are:
- The condition should be life-threatening or seriously debilitating with a high unmet medical need (ie, there is no method of treatment, diagnosis, or prevention available, or existing methods have serious limitations).
- The medicinal product is likely to offer a major advantage over methods currently used in the UK.
- The potential adverse effects of the medicinal product are likely to be outweighed by the benefits, allowing for the reasonable expectation of a positive benefit-risk balance. A positive benefit-risk balance should be based on preliminary scientific evidence, as justified by the applicant.
About SGX301
SGX301 is a photodynamic therapy utilizing safe, visible light for activation. The active ingredient in SGX301 is synthetic hypericin, a photosensitizer that is applied to skin lesions and then activated by fluorescent light 16 to 24 hours later.
Combined with photoactivation, hypericin has demonstrated significant antiproliferative effects on activated, normal human lymphoid cells and inhibited the growth of malignant T cells isolated from CTCL patients. Topical hypericin has also proven safe in a phase 1 study of healthy volunteers.
In a phase 2 trial of patients with CTCL (mycosis fungoides only) or psoriasis, topical hypericin conferred a significant improvement over placebo. Among CTCL patients, the treatment prompted a response rate of 58.3%, compared to an 8.3% response rate for placebo (P≤0.04).
Topical hypericin was also well tolerated in this trial. There were no deaths or serious adverse events related to the treatment. However, there were reports of mild to moderate burning, itching, erythema, and pruritus at the application site.
A phase 3 trial of SGX301 is currently recruiting patients. SGX301 is under development by Soligenix, Inc.
Cheap manufacture of generic cancer drugs is feasible, study shows

Photo courtesy of FDA
AMSTERDAM—New research suggests some generic cancer drugs could be manufactured for less than 1% of the prices currently charged in the US and UK.
For example, researchers calculated that manufacturing a 400 mg tablet of imatinib costs $0.92.
Charging $1.04 per tablet would cover costs and allow for a 10% profit margin.
However, the current price of imatinib is $84.36 per tablet in the UK and $247.74 per tablet in the US.
Melissa Barber, of the London School of Hygiene and Tropical Medicine in the UK, reported these findings at ECCO 2017: European Cancer Congress (abstract 1032).
Barber and her colleagues collected data on per-kilogram costs of exported active pharmaceutical ingredients (APIs) from an online database of Indian export logs.
The team then estimated generic prices for tablets through an established costing algorithm. They calculated per-dose API costs and added excipient costs of $2.63 per kg of finished pharmaceutical product and per-tablet costs of production of $0.01, plus a 10% profit margin accounting for a 26.6% average tax on profits (assuming manufacture in India.)
Finally, the researchers compared the calculated price to current unit prices in the US, UK, Spain, and India.
For imatinib, the team determined the cost of the API to be $2284 per kg and the API cost per tablet to be $0.91. They then added excipient cost ($0.002 per tablet), conversion cost ($0.01 per tablet), and a 10% profit margin accounting for a 26.6% tax on profits.
This resulted in the estimated generic price of $1.04 per tablet. The per-tablet price is below the estimated price in India ($0.22) but much higher than the estimated price in Spain ($57.53), the UK ($84.36), and the US ($247.74).
Barber noted that, according to her group’s calculations, imatinib could be produced for $54 a month.
Another drug that could be produced for a low cost is etoposide. Barber and her colleagues calculated a generic price for etoposide of $0.97 per 100 mg tablet.
However, the per-tablet price is $1.50 in India, $8.65 in Spain, $11.34 in the UK, and $87.14 in the US.
The researchers calculated a generic price for mercaptopurine of $0.03 per 50 mg tablet, which is the same as the per-tablet price in India. However, a 50 mg mercaptopurine tablet costs $3.14 in Spain, $2.56 in the UK, and $0.40 in the US.
“Showing that certain cancers could be treated for very low prices could transform the future of people with these cancers in very low-income countries where there are usually few or no treatment options,” Barber said.

Photo courtesy of FDA
AMSTERDAM—New research suggests some generic cancer drugs could be manufactured for less than 1% of the prices currently charged in the US and UK.
For example, researchers calculated that manufacturing a 400 mg tablet of imatinib costs $0.92.
Charging $1.04 per tablet would cover costs and allow for a 10% profit margin.
However, the current price of imatinib is $84.36 per tablet in the UK and $247.74 per tablet in the US.
Melissa Barber, of the London School of Hygiene and Tropical Medicine in the UK, reported these findings at ECCO 2017: European Cancer Congress (abstract 1032).
Barber and her colleagues collected data on per-kilogram costs of exported active pharmaceutical ingredients (APIs) from an online database of Indian export logs.
The team then estimated generic prices for tablets through an established costing algorithm. They calculated per-dose API costs and added excipient costs of $2.63 per kg of finished pharmaceutical product and per-tablet costs of production of $0.01, plus a 10% profit margin accounting for a 26.6% average tax on profits (assuming manufacture in India.)
Finally, the researchers compared the calculated price to current unit prices in the US, UK, Spain, and India.
For imatinib, the team determined the cost of the API to be $2284 per kg and the API cost per tablet to be $0.91. They then added excipient cost ($0.002 per tablet), conversion cost ($0.01 per tablet), and a 10% profit margin accounting for a 26.6% tax on profits.
This resulted in the estimated generic price of $1.04 per tablet. The per-tablet price is below the estimated price in India ($0.22) but much higher than the estimated price in Spain ($57.53), the UK ($84.36), and the US ($247.74).
Barber noted that, according to her group’s calculations, imatinib could be produced for $54 a month.
Another drug that could be produced for a low cost is etoposide. Barber and her colleagues calculated a generic price for etoposide of $0.97 per 100 mg tablet.
However, the per-tablet price is $1.50 in India, $8.65 in Spain, $11.34 in the UK, and $87.14 in the US.
The researchers calculated a generic price for mercaptopurine of $0.03 per 50 mg tablet, which is the same as the per-tablet price in India. However, a 50 mg mercaptopurine tablet costs $3.14 in Spain, $2.56 in the UK, and $0.40 in the US.
“Showing that certain cancers could be treated for very low prices could transform the future of people with these cancers in very low-income countries where there are usually few or no treatment options,” Barber said.

Photo courtesy of FDA
AMSTERDAM—New research suggests some generic cancer drugs could be manufactured for less than 1% of the prices currently charged in the US and UK.
For example, researchers calculated that manufacturing a 400 mg tablet of imatinib costs $0.92.
Charging $1.04 per tablet would cover costs and allow for a 10% profit margin.
However, the current price of imatinib is $84.36 per tablet in the UK and $247.74 per tablet in the US.
Melissa Barber, of the London School of Hygiene and Tropical Medicine in the UK, reported these findings at ECCO 2017: European Cancer Congress (abstract 1032).
Barber and her colleagues collected data on per-kilogram costs of exported active pharmaceutical ingredients (APIs) from an online database of Indian export logs.
The team then estimated generic prices for tablets through an established costing algorithm. They calculated per-dose API costs and added excipient costs of $2.63 per kg of finished pharmaceutical product and per-tablet costs of production of $0.01, plus a 10% profit margin accounting for a 26.6% average tax on profits (assuming manufacture in India.)
Finally, the researchers compared the calculated price to current unit prices in the US, UK, Spain, and India.
For imatinib, the team determined the cost of the API to be $2284 per kg and the API cost per tablet to be $0.91. They then added excipient cost ($0.002 per tablet), conversion cost ($0.01 per tablet), and a 10% profit margin accounting for a 26.6% tax on profits.
This resulted in the estimated generic price of $1.04 per tablet. The per-tablet price is below the estimated price in India ($0.22) but much higher than the estimated price in Spain ($57.53), the UK ($84.36), and the US ($247.74).
Barber noted that, according to her group’s calculations, imatinib could be produced for $54 a month.
Another drug that could be produced for a low cost is etoposide. Barber and her colleagues calculated a generic price for etoposide of $0.97 per 100 mg tablet.
However, the per-tablet price is $1.50 in India, $8.65 in Spain, $11.34 in the UK, and $87.14 in the US.
The researchers calculated a generic price for mercaptopurine of $0.03 per 50 mg tablet, which is the same as the per-tablet price in India. However, a 50 mg mercaptopurine tablet costs $3.14 in Spain, $2.56 in the UK, and $0.40 in the US.
“Showing that certain cancers could be treated for very low prices could transform the future of people with these cancers in very low-income countries where there are usually few or no treatment options,” Barber said.