User login
Canada expands approval for antihemophilic factor
Health Canada has extended the approved indication for Adynovate, a recombinant pegylated factor VIII (FVIII) product, in patients with hemophilia A.
The product is now approved for use in hemophilia A patients under the age of 12 for the control and prevention of bleeding episodes, as prophylaxis to prevent or reduce the frequency of bleeding, and for perioperative management of bleeding.
Adynovate (formerly BAX 855) was first approved in Canada in November 2016. At that time, it was authorized for use in hemophilia A patients age 12 and older as on-demand treatment, as prophylaxis, and for perioperative management.
Adynovate is built on the full-length Advate molecule, but Adynovate leverages pegylation technology designed to extend the amount of FVIII available for use in the body.
The technology was selected because it maintains the integrity of the parent molecule (Advate) while reducing the time at which the body clears Adynovate, resulting in an extended circulating half-life.
Health Canada’s decision to expand the indication for Adynovate is supported by results from a phase 3 trial of pediatric patients as well as a phase 3 trial of patients undergoing surgery.
Pediatric trial
The pediatric trial enrolled 73 patients, ages 1 to 11, with previously treated hemophilia A.
Sixty-six patients received twice-weekly prophylaxis with Adynovate (50 ± 10 IU/kg) for at least 6 months or 50 exposure days, whichever occurred last.
The median annualized bleeding rate was 2.0 for all bleeds and 0 for both joint and spontaneous bleeds.
Thirty-eight percent of patients did not have any bleeding episodes, 67% had no spontaneous bleeds, and 73% had no joint bleeds.
One patient developed inhibitors, but there were no other treatment-related adverse events.
Results from this trial were published in Haemophilia in November 2016 and are available in the Canadian product monograph for Adynovate.
Perioperative study
The perioperative study included 15 patients, ages 19 to 52, with severe hemophilia A who were undergoing surgical procedures (11 of them major and four minor).
The patients received Adynovate at varying doses and schedules, depending on each patient’s pharmacokinetic profile for major procedures or Adynovate incremental recovery for minor procedures.
Intraoperative and perioperative hemostatic efficacy of Adynovate was deemed “excellent” for all 15 patients. The “excellent” rating meant that blood loss was less than or equal to that expected for the type of procedure performed in a non-hemophilic population.
Postoperatively (day 1 after the procedure), hemostatic efficacy was rated “good” for one procedure and “excellent” for the rest. The “good” rating meant that postoperative blood loss was up to 50% more than expected for the type of procedure performed in a non-hemophilic population.
There were no treatment-related adverse events or signs of immunogenicity in this trial.
Results were published in Haemophilia in June 2016 and are available in the Canadian product monograph for Adynovate.
Health Canada has extended the approved indication for Adynovate, a recombinant pegylated factor VIII (FVIII) product, in patients with hemophilia A.
The product is now approved for use in hemophilia A patients under the age of 12 for the control and prevention of bleeding episodes, as prophylaxis to prevent or reduce the frequency of bleeding, and for perioperative management of bleeding.
Adynovate (formerly BAX 855) was first approved in Canada in November 2016. At that time, it was authorized for use in hemophilia A patients age 12 and older as on-demand treatment, as prophylaxis, and for perioperative management.
Adynovate is built on the full-length Advate molecule, but Adynovate leverages pegylation technology designed to extend the amount of FVIII available for use in the body.
The technology was selected because it maintains the integrity of the parent molecule (Advate) while reducing the time at which the body clears Adynovate, resulting in an extended circulating half-life.
Health Canada’s decision to expand the indication for Adynovate is supported by results from a phase 3 trial of pediatric patients as well as a phase 3 trial of patients undergoing surgery.
Pediatric trial
The pediatric trial enrolled 73 patients, ages 1 to 11, with previously treated hemophilia A.
Sixty-six patients received twice-weekly prophylaxis with Adynovate (50 ± 10 IU/kg) for at least 6 months or 50 exposure days, whichever occurred last.
The median annualized bleeding rate was 2.0 for all bleeds and 0 for both joint and spontaneous bleeds.
Thirty-eight percent of patients did not have any bleeding episodes, 67% had no spontaneous bleeds, and 73% had no joint bleeds.
One patient developed inhibitors, but there were no other treatment-related adverse events.
Results from this trial were published in Haemophilia in November 2016 and are available in the Canadian product monograph for Adynovate.
Perioperative study
The perioperative study included 15 patients, ages 19 to 52, with severe hemophilia A who were undergoing surgical procedures (11 of them major and four minor).
The patients received Adynovate at varying doses and schedules, depending on each patient’s pharmacokinetic profile for major procedures or Adynovate incremental recovery for minor procedures.
Intraoperative and perioperative hemostatic efficacy of Adynovate was deemed “excellent” for all 15 patients. The “excellent” rating meant that blood loss was less than or equal to that expected for the type of procedure performed in a non-hemophilic population.
Postoperatively (day 1 after the procedure), hemostatic efficacy was rated “good” for one procedure and “excellent” for the rest. The “good” rating meant that postoperative blood loss was up to 50% more than expected for the type of procedure performed in a non-hemophilic population.
There were no treatment-related adverse events or signs of immunogenicity in this trial.
Results were published in Haemophilia in June 2016 and are available in the Canadian product monograph for Adynovate.
Health Canada has extended the approved indication for Adynovate, a recombinant pegylated factor VIII (FVIII) product, in patients with hemophilia A.
The product is now approved for use in hemophilia A patients under the age of 12 for the control and prevention of bleeding episodes, as prophylaxis to prevent or reduce the frequency of bleeding, and for perioperative management of bleeding.
Adynovate (formerly BAX 855) was first approved in Canada in November 2016. At that time, it was authorized for use in hemophilia A patients age 12 and older as on-demand treatment, as prophylaxis, and for perioperative management.
Adynovate is built on the full-length Advate molecule, but Adynovate leverages pegylation technology designed to extend the amount of FVIII available for use in the body.
The technology was selected because it maintains the integrity of the parent molecule (Advate) while reducing the time at which the body clears Adynovate, resulting in an extended circulating half-life.
Health Canada’s decision to expand the indication for Adynovate is supported by results from a phase 3 trial of pediatric patients as well as a phase 3 trial of patients undergoing surgery.
Pediatric trial
The pediatric trial enrolled 73 patients, ages 1 to 11, with previously treated hemophilia A.
Sixty-six patients received twice-weekly prophylaxis with Adynovate (50 ± 10 IU/kg) for at least 6 months or 50 exposure days, whichever occurred last.
The median annualized bleeding rate was 2.0 for all bleeds and 0 for both joint and spontaneous bleeds.
Thirty-eight percent of patients did not have any bleeding episodes, 67% had no spontaneous bleeds, and 73% had no joint bleeds.
One patient developed inhibitors, but there were no other treatment-related adverse events.
Results from this trial were published in Haemophilia in November 2016 and are available in the Canadian product monograph for Adynovate.
Perioperative study
The perioperative study included 15 patients, ages 19 to 52, with severe hemophilia A who were undergoing surgical procedures (11 of them major and four minor).
The patients received Adynovate at varying doses and schedules, depending on each patient’s pharmacokinetic profile for major procedures or Adynovate incremental recovery for minor procedures.
Intraoperative and perioperative hemostatic efficacy of Adynovate was deemed “excellent” for all 15 patients. The “excellent” rating meant that blood loss was less than or equal to that expected for the type of procedure performed in a non-hemophilic population.
Postoperatively (day 1 after the procedure), hemostatic efficacy was rated “good” for one procedure and “excellent” for the rest. The “good” rating meant that postoperative blood loss was up to 50% more than expected for the type of procedure performed in a non-hemophilic population.
There were no treatment-related adverse events or signs of immunogenicity in this trial.
Results were published in Haemophilia in June 2016 and are available in the Canadian product monograph for Adynovate.
Pegfilgrastim biosimilar approved by EC
The European Commission (EC) has granted marketing authorization for Sandoz’s pegfilgrastim product Ziextenzo®, a biosimilar of Amgen’s Neulasta.
Ziextenzo is approved for the same use as the reference medicine—to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving cytotoxic chemotherapy for malignancies except chronic myeloid leukemia and myelodysplastic syndromes.
The approval is valid in all countries of the European Union as well as Norway, Iceland, and Liechtenstein.
The EC’s approval was based on research suggesting Ziextenzo is comparable to Neulasta in terms of safety, efficacy, pharmacokinetics, and pharmacodynamics.1,2,3,4
1. Blackwell K. et al. Pooled analysis of two randomized, double-blind trials comparing proposed biosimilar LA-EP2006 with reference pegfilgrastim in breast cancer. Ann Oncol 28, 2272-2277 (2017).
2. Nakov R. et al. Proposed biosimilar pegfilgrastim LA-EP2006 shows similarity in pharmacokinetics and pharmacodynamics to reference pegfilgrastim in healthy subjects. 2017 San Antonio Breast Cancer Symposium, abstract P3-14-10.
3. Blackwell K. et al. A Comparison of Proposed Biosimilar LA-EP2006 and Reference Pegfilgrastim for the Prevention of Neutropenia in Patients With Early-Stage Breast Cancer Receiving Myelosuppressive Adjuvant or Neoadjuvant Chemotherapy: Pegfilgrastim Randomized Oncology (Supportive Care) Trial to Evaluate Comparative Treatment (PROTECT-2), a Phase III, Randomized, Double-Blind Trial. Oncologist 21, 789-794 (2016).
4. Harbeck N. et al. Randomized, double-blind study comparing proposed biosimilar LA-EP2006 with reference pegfilgrastim in breast cancer. Future Oncol 12, 1359-1367 (2016).
The European Commission (EC) has granted marketing authorization for Sandoz’s pegfilgrastim product Ziextenzo®, a biosimilar of Amgen’s Neulasta.
Ziextenzo is approved for the same use as the reference medicine—to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving cytotoxic chemotherapy for malignancies except chronic myeloid leukemia and myelodysplastic syndromes.
The approval is valid in all countries of the European Union as well as Norway, Iceland, and Liechtenstein.
The EC’s approval was based on research suggesting Ziextenzo is comparable to Neulasta in terms of safety, efficacy, pharmacokinetics, and pharmacodynamics.1,2,3,4
1. Blackwell K. et al. Pooled analysis of two randomized, double-blind trials comparing proposed biosimilar LA-EP2006 with reference pegfilgrastim in breast cancer. Ann Oncol 28, 2272-2277 (2017).
2. Nakov R. et al. Proposed biosimilar pegfilgrastim LA-EP2006 shows similarity in pharmacokinetics and pharmacodynamics to reference pegfilgrastim in healthy subjects. 2017 San Antonio Breast Cancer Symposium, abstract P3-14-10.
3. Blackwell K. et al. A Comparison of Proposed Biosimilar LA-EP2006 and Reference Pegfilgrastim for the Prevention of Neutropenia in Patients With Early-Stage Breast Cancer Receiving Myelosuppressive Adjuvant or Neoadjuvant Chemotherapy: Pegfilgrastim Randomized Oncology (Supportive Care) Trial to Evaluate Comparative Treatment (PROTECT-2), a Phase III, Randomized, Double-Blind Trial. Oncologist 21, 789-794 (2016).
4. Harbeck N. et al. Randomized, double-blind study comparing proposed biosimilar LA-EP2006 with reference pegfilgrastim in breast cancer. Future Oncol 12, 1359-1367 (2016).
The European Commission (EC) has granted marketing authorization for Sandoz’s pegfilgrastim product Ziextenzo®, a biosimilar of Amgen’s Neulasta.
Ziextenzo is approved for the same use as the reference medicine—to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving cytotoxic chemotherapy for malignancies except chronic myeloid leukemia and myelodysplastic syndromes.
The approval is valid in all countries of the European Union as well as Norway, Iceland, and Liechtenstein.
The EC’s approval was based on research suggesting Ziextenzo is comparable to Neulasta in terms of safety, efficacy, pharmacokinetics, and pharmacodynamics.1,2,3,4
1. Blackwell K. et al. Pooled analysis of two randomized, double-blind trials comparing proposed biosimilar LA-EP2006 with reference pegfilgrastim in breast cancer. Ann Oncol 28, 2272-2277 (2017).
2. Nakov R. et al. Proposed biosimilar pegfilgrastim LA-EP2006 shows similarity in pharmacokinetics and pharmacodynamics to reference pegfilgrastim in healthy subjects. 2017 San Antonio Breast Cancer Symposium, abstract P3-14-10.
3. Blackwell K. et al. A Comparison of Proposed Biosimilar LA-EP2006 and Reference Pegfilgrastim for the Prevention of Neutropenia in Patients With Early-Stage Breast Cancer Receiving Myelosuppressive Adjuvant or Neoadjuvant Chemotherapy: Pegfilgrastim Randomized Oncology (Supportive Care) Trial to Evaluate Comparative Treatment (PROTECT-2), a Phase III, Randomized, Double-Blind Trial. Oncologist 21, 789-794 (2016).
4. Harbeck N. et al. Randomized, double-blind study comparing proposed biosimilar LA-EP2006 with reference pegfilgrastim in breast cancer. Future Oncol 12, 1359-1367 (2016).
EC approves pegfilgrastim biosimilar
The European Commission (EC) has approved Mundipharma’s pegfilgrastim product Pelmeg, a biosimilar of Amgen’s Neulasta.
Pelmeg is approved for use in reducing the duration of neutropenia and the incidence of febrile neutropenia in adults who receive cytotoxic chemotherapy for malignancies, with the exceptions of chronic myeloid leukemia and myelodysplastic syndromes.
The approval is valid in all countries of the European Union as well as Norway, Iceland, and Liechtenstein.
The EC’s approval of Pelmeg was supported by research showing pharmacokinetic comparability between Pelmeg and Neulasta at a dose of 6 mg, pharmacodynamic comparability at doses of 6 mg and 3 mg, and no clinically meaningful differences in the safety and immunogenicity profiles of Pelmeg and Neulasta.1,2,3
1. Roth K. et al. Demonstration of pharmacokinetic and pharmacodynamic comparability in healthy volunteers for B12019, a proposed pegfilgrastim biosimilar. ECCO 2017, abstract 241.
2. Roth K. et al. Comparability of pharmacodynamics and immunogenicity of B12019, a proposed pegfilgrastim biosimilar to Neulasta®. ASH 2017, abstract 1002.
3. Roth K. et al. Pharmacokinetic and pharmacodynamic comparability of B12019, a proposed pegfilgrastim biosimilar. ESMO 2017, poster 1573.
The European Commission (EC) has approved Mundipharma’s pegfilgrastim product Pelmeg, a biosimilar of Amgen’s Neulasta.
Pelmeg is approved for use in reducing the duration of neutropenia and the incidence of febrile neutropenia in adults who receive cytotoxic chemotherapy for malignancies, with the exceptions of chronic myeloid leukemia and myelodysplastic syndromes.
The approval is valid in all countries of the European Union as well as Norway, Iceland, and Liechtenstein.
The EC’s approval of Pelmeg was supported by research showing pharmacokinetic comparability between Pelmeg and Neulasta at a dose of 6 mg, pharmacodynamic comparability at doses of 6 mg and 3 mg, and no clinically meaningful differences in the safety and immunogenicity profiles of Pelmeg and Neulasta.1,2,3
1. Roth K. et al. Demonstration of pharmacokinetic and pharmacodynamic comparability in healthy volunteers for B12019, a proposed pegfilgrastim biosimilar. ECCO 2017, abstract 241.
2. Roth K. et al. Comparability of pharmacodynamics and immunogenicity of B12019, a proposed pegfilgrastim biosimilar to Neulasta®. ASH 2017, abstract 1002.
3. Roth K. et al. Pharmacokinetic and pharmacodynamic comparability of B12019, a proposed pegfilgrastim biosimilar. ESMO 2017, poster 1573.
The European Commission (EC) has approved Mundipharma’s pegfilgrastim product Pelmeg, a biosimilar of Amgen’s Neulasta.
Pelmeg is approved for use in reducing the duration of neutropenia and the incidence of febrile neutropenia in adults who receive cytotoxic chemotherapy for malignancies, with the exceptions of chronic myeloid leukemia and myelodysplastic syndromes.
The approval is valid in all countries of the European Union as well as Norway, Iceland, and Liechtenstein.
The EC’s approval of Pelmeg was supported by research showing pharmacokinetic comparability between Pelmeg and Neulasta at a dose of 6 mg, pharmacodynamic comparability at doses of 6 mg and 3 mg, and no clinically meaningful differences in the safety and immunogenicity profiles of Pelmeg and Neulasta.1,2,3
1. Roth K. et al. Demonstration of pharmacokinetic and pharmacodynamic comparability in healthy volunteers for B12019, a proposed pegfilgrastim biosimilar. ECCO 2017, abstract 241.
2. Roth K. et al. Comparability of pharmacodynamics and immunogenicity of B12019, a proposed pegfilgrastim biosimilar to Neulasta®. ASH 2017, abstract 1002.
3. Roth K. et al. Pharmacokinetic and pharmacodynamic comparability of B12019, a proposed pegfilgrastim biosimilar. ESMO 2017, poster 1573.
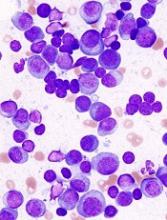
Haplo-HSCT feasible in multiple myeloma
A retrospective study suggests haploidentical hematopoietic stem cell transplant (haplo-HSCT) is feasible in patients with multiply relapsed or high-risk multiple myeloma (MM).
Investigators said haplo-HSCT produced an “acceptable” rate of non-relapse mortality (NRM)—21% at 1 year—in such patients.
“Our results demonstrate that [haplo-HSCT] can be safely performed in appropriate patients with MM who lack an HLA-matched sibling or unrelated donor,” the investigators wrote in Biology of Blood and Marrow Transplantation.
The research was conducted by Firoozeh Sahebi, MD, of City of Hope Medical Center in Duarte, California, and her colleagues.
The team analyzed data from 96 MM patients who had failed at least one previous autologous transplant and underwent haplo-HSCT between 2008 and 2016.
The patients had a median age of 54.9 (range, 36.6-73.3), and 65.6% were male. At baseline, 37.5% of patients were in very good partial response or better, 31.2% were in partial response, 13.5% had stable disease, and 17.7% had relapsed disease.
The median follow-up was 24 months. Almost all patients (97%) achieved neutrophil engraftment by day 28, and 75% had recovery of platelets by day 60.
Grade 2-4 acute graft-vs-host-disease occurred in 39% of patients by 100 days. Chronic graft-vs-host-disease was seen in 46% of patients at 2 years.
The rate of NRM was 21% at 1 year and 26% at 2 years. The cumulative risk of relapse and progression was 50% at 1 year and 56% at 2 years.
The 2-year progression-free survival (PFS) was 17%, and the 2-year overall survival (OS) was 48%.
In a univariate analysis, bone marrow transplant was associated with significantly better OS than peripheral blood transplant (P=0.001). However, there was no significant difference in PFS between the two.
NRM was lower with bone marrow transplant (P=0.016), and there was a trend toward a higher relapse rate with bone marrow (P=0.083).
The use of cyclophosphamide after transplant was associated with significantly better OS (P=0.009) but not PFS, NRM, or relapse.
Other factors—such as disease status and conditioning regimen—had no significant impact on survival, NRM, or relapse.
The investigators said they had no conflicts of interest related to this research.
A retrospective study suggests haploidentical hematopoietic stem cell transplant (haplo-HSCT) is feasible in patients with multiply relapsed or high-risk multiple myeloma (MM).
Investigators said haplo-HSCT produced an “acceptable” rate of non-relapse mortality (NRM)—21% at 1 year—in such patients.
“Our results demonstrate that [haplo-HSCT] can be safely performed in appropriate patients with MM who lack an HLA-matched sibling or unrelated donor,” the investigators wrote in Biology of Blood and Marrow Transplantation.
The research was conducted by Firoozeh Sahebi, MD, of City of Hope Medical Center in Duarte, California, and her colleagues.
The team analyzed data from 96 MM patients who had failed at least one previous autologous transplant and underwent haplo-HSCT between 2008 and 2016.
The patients had a median age of 54.9 (range, 36.6-73.3), and 65.6% were male. At baseline, 37.5% of patients were in very good partial response or better, 31.2% were in partial response, 13.5% had stable disease, and 17.7% had relapsed disease.
The median follow-up was 24 months. Almost all patients (97%) achieved neutrophil engraftment by day 28, and 75% had recovery of platelets by day 60.
Grade 2-4 acute graft-vs-host-disease occurred in 39% of patients by 100 days. Chronic graft-vs-host-disease was seen in 46% of patients at 2 years.
The rate of NRM was 21% at 1 year and 26% at 2 years. The cumulative risk of relapse and progression was 50% at 1 year and 56% at 2 years.
The 2-year progression-free survival (PFS) was 17%, and the 2-year overall survival (OS) was 48%.
In a univariate analysis, bone marrow transplant was associated with significantly better OS than peripheral blood transplant (P=0.001). However, there was no significant difference in PFS between the two.
NRM was lower with bone marrow transplant (P=0.016), and there was a trend toward a higher relapse rate with bone marrow (P=0.083).
The use of cyclophosphamide after transplant was associated with significantly better OS (P=0.009) but not PFS, NRM, or relapse.
Other factors—such as disease status and conditioning regimen—had no significant impact on survival, NRM, or relapse.
The investigators said they had no conflicts of interest related to this research.
A retrospective study suggests haploidentical hematopoietic stem cell transplant (haplo-HSCT) is feasible in patients with multiply relapsed or high-risk multiple myeloma (MM).
Investigators said haplo-HSCT produced an “acceptable” rate of non-relapse mortality (NRM)—21% at 1 year—in such patients.
“Our results demonstrate that [haplo-HSCT] can be safely performed in appropriate patients with MM who lack an HLA-matched sibling or unrelated donor,” the investigators wrote in Biology of Blood and Marrow Transplantation.
The research was conducted by Firoozeh Sahebi, MD, of City of Hope Medical Center in Duarte, California, and her colleagues.
The team analyzed data from 96 MM patients who had failed at least one previous autologous transplant and underwent haplo-HSCT between 2008 and 2016.
The patients had a median age of 54.9 (range, 36.6-73.3), and 65.6% were male. At baseline, 37.5% of patients were in very good partial response or better, 31.2% were in partial response, 13.5% had stable disease, and 17.7% had relapsed disease.
The median follow-up was 24 months. Almost all patients (97%) achieved neutrophil engraftment by day 28, and 75% had recovery of platelets by day 60.
Grade 2-4 acute graft-vs-host-disease occurred in 39% of patients by 100 days. Chronic graft-vs-host-disease was seen in 46% of patients at 2 years.
The rate of NRM was 21% at 1 year and 26% at 2 years. The cumulative risk of relapse and progression was 50% at 1 year and 56% at 2 years.
The 2-year progression-free survival (PFS) was 17%, and the 2-year overall survival (OS) was 48%.
In a univariate analysis, bone marrow transplant was associated with significantly better OS than peripheral blood transplant (P=0.001). However, there was no significant difference in PFS between the two.
NRM was lower with bone marrow transplant (P=0.016), and there was a trend toward a higher relapse rate with bone marrow (P=0.083).
The use of cyclophosphamide after transplant was associated with significantly better OS (P=0.009) but not PFS, NRM, or relapse.
Other factors—such as disease status and conditioning regimen—had no significant impact on survival, NRM, or relapse.
The investigators said they had no conflicts of interest related to this research.
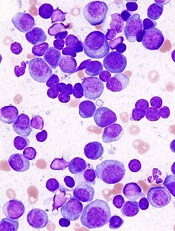
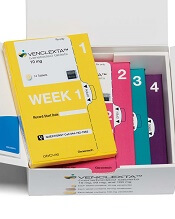
FDA approves venetoclax for AML
The U.S. Food and Drug Administration (FDA) has granted accelerated approval to venetoclax (Venclexta®) for use in acute myeloid leukemia (AML).
The BCL-2 inhibitor is now approved for use in combination with azacitidine, decitabine, or low-dose cytarabine to treat adults with newly diagnosed AML who are age 75 and older or who are ineligible for intensive chemotherapy.
The FDA grants accelerated approval based on a surrogate or intermediate endpoint that is reasonably likely to predict clinical benefit.
Therefore, continued approval of venetoclax in AML may be contingent upon verification of clinical benefit in confirmatory trials.
The approval is based on data from two studies—the phase 1 b M14-358 trial (NCT02203773) and the phase 1/2 M14-387 trial (NCT02287233).
M14-358 trial
In M14-358, newly diagnosed AML patients received venetoclax in combination with azacitidine (n=84) or decitabine (n=31). There were 67 patients in the azacitidine arm and 13 in the decitabine arm who were 75 or older or were ineligible for intensive induction chemotherapy.
Patients received venetoclax via a daily ramp-up to a final dose of 400 mg once daily. They received prophylaxis for tumor lysis syndrome and were hospitalized for monitoring during the ramp-up.
They received azacitidine at 75 mg/m2 on days 1-7 of each 28-day cycle or decitabine at 20 mg/m2 on days 1-5 of each cycle. Patients continued treatment until disease progression or unacceptable toxicity.
The median follow-up was 7.9 months for the azacitidine arm and 11 months for the decitabine arm.
The complete response (CR) rate was 37% (25/67) in the azacitidine arm and 54% (7/13) in the decitabine arm. The rates of CR with partial hematologic recovery were 24% (16/67) and 7.7% (1/13), respectively.
The most common adverse events (AEs)—occurring in at least 30% of patients in both arms—were nausea, diarrhea, constipation, neutropenia, thrombocytopenia, hemorrhage, peripheral edema, vomiting, fatigue, febrile neutropenia, rash, and anemia.
The incidence of serious AEs was 75% overall. The most frequent serious AEs (occurring in at least 5% of patients) were febrile neutropenia, pneumonia (excluding fungal), sepsis (excluding fungal), respiratory failure, and multiple organ dysfunction syndrome.
The incidence of fatal AEs was 1.5% within 30 days of treatment initiation.
M14-387 trial
The M14-387 trial included 82 AML patients who received venetoclax plus low-dose cytarabine. Patients were newly diagnosed with AML, but some had previous exposure to a hypomethylating agent for an antecedent hematologic disorder.
There were 61 patients who were 75 or older or were ineligible for intensive induction chemotherapy.
Patients received venetoclax via daily ramp-up to a final dose of 600 mg once daily. They received prophylaxis for tumor lysis syndrome and were hospitalized for monitoring during the ramp-up.
Cytarabine was given at 20 mg/m2 on days 1-10 of each 28-day cycle. Patients continued to receive treatment until disease progression or unacceptable toxicity.
At a median follow-up of 6.5 months, the CR rate was 21% (13/61), and the rate of CR with partial hematologic recovery was 21% (13/61).
The most common AEs (occurring in at least 30% of patients) were nausea, thrombocytopenia, hemorrhage, febrile neutropenia, neutropenia, diarrhea, fatigue, constipation, and dyspnea.
The incidence of serious AEs was 95%. The most frequent serious AEs (occurring in at least 5% of patients) were febrile neutropenia, sepsis (excluding fungal), hemorrhage, pneumonia (excluding fungal), and device-related infection.
The incidence of fatal AEs was 4.9% within 30 days of treatment initiation.
Additional details from the M14-358 and M14-387 trials are available in the prescribing information for venetoclax.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the United States and by AbbVie elsewhere.
The U.S. Food and Drug Administration (FDA) has granted accelerated approval to venetoclax (Venclexta®) for use in acute myeloid leukemia (AML).
The BCL-2 inhibitor is now approved for use in combination with azacitidine, decitabine, or low-dose cytarabine to treat adults with newly diagnosed AML who are age 75 and older or who are ineligible for intensive chemotherapy.
The FDA grants accelerated approval based on a surrogate or intermediate endpoint that is reasonably likely to predict clinical benefit.
Therefore, continued approval of venetoclax in AML may be contingent upon verification of clinical benefit in confirmatory trials.
The approval is based on data from two studies—the phase 1 b M14-358 trial (NCT02203773) and the phase 1/2 M14-387 trial (NCT02287233).
M14-358 trial
In M14-358, newly diagnosed AML patients received venetoclax in combination with azacitidine (n=84) or decitabine (n=31). There were 67 patients in the azacitidine arm and 13 in the decitabine arm who were 75 or older or were ineligible for intensive induction chemotherapy.
Patients received venetoclax via a daily ramp-up to a final dose of 400 mg once daily. They received prophylaxis for tumor lysis syndrome and were hospitalized for monitoring during the ramp-up.
They received azacitidine at 75 mg/m2 on days 1-7 of each 28-day cycle or decitabine at 20 mg/m2 on days 1-5 of each cycle. Patients continued treatment until disease progression or unacceptable toxicity.
The median follow-up was 7.9 months for the azacitidine arm and 11 months for the decitabine arm.
The complete response (CR) rate was 37% (25/67) in the azacitidine arm and 54% (7/13) in the decitabine arm. The rates of CR with partial hematologic recovery were 24% (16/67) and 7.7% (1/13), respectively.
The most common adverse events (AEs)—occurring in at least 30% of patients in both arms—were nausea, diarrhea, constipation, neutropenia, thrombocytopenia, hemorrhage, peripheral edema, vomiting, fatigue, febrile neutropenia, rash, and anemia.
The incidence of serious AEs was 75% overall. The most frequent serious AEs (occurring in at least 5% of patients) were febrile neutropenia, pneumonia (excluding fungal), sepsis (excluding fungal), respiratory failure, and multiple organ dysfunction syndrome.
The incidence of fatal AEs was 1.5% within 30 days of treatment initiation.
M14-387 trial
The M14-387 trial included 82 AML patients who received venetoclax plus low-dose cytarabine. Patients were newly diagnosed with AML, but some had previous exposure to a hypomethylating agent for an antecedent hematologic disorder.
There were 61 patients who were 75 or older or were ineligible for intensive induction chemotherapy.
Patients received venetoclax via daily ramp-up to a final dose of 600 mg once daily. They received prophylaxis for tumor lysis syndrome and were hospitalized for monitoring during the ramp-up.
Cytarabine was given at 20 mg/m2 on days 1-10 of each 28-day cycle. Patients continued to receive treatment until disease progression or unacceptable toxicity.
At a median follow-up of 6.5 months, the CR rate was 21% (13/61), and the rate of CR with partial hematologic recovery was 21% (13/61).
The most common AEs (occurring in at least 30% of patients) were nausea, thrombocytopenia, hemorrhage, febrile neutropenia, neutropenia, diarrhea, fatigue, constipation, and dyspnea.
The incidence of serious AEs was 95%. The most frequent serious AEs (occurring in at least 5% of patients) were febrile neutropenia, sepsis (excluding fungal), hemorrhage, pneumonia (excluding fungal), and device-related infection.
The incidence of fatal AEs was 4.9% within 30 days of treatment initiation.
Additional details from the M14-358 and M14-387 trials are available in the prescribing information for venetoclax.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the United States and by AbbVie elsewhere.
The U.S. Food and Drug Administration (FDA) has granted accelerated approval to venetoclax (Venclexta®) for use in acute myeloid leukemia (AML).
The BCL-2 inhibitor is now approved for use in combination with azacitidine, decitabine, or low-dose cytarabine to treat adults with newly diagnosed AML who are age 75 and older or who are ineligible for intensive chemotherapy.
The FDA grants accelerated approval based on a surrogate or intermediate endpoint that is reasonably likely to predict clinical benefit.
Therefore, continued approval of venetoclax in AML may be contingent upon verification of clinical benefit in confirmatory trials.
The approval is based on data from two studies—the phase 1 b M14-358 trial (NCT02203773) and the phase 1/2 M14-387 trial (NCT02287233).
M14-358 trial
In M14-358, newly diagnosed AML patients received venetoclax in combination with azacitidine (n=84) or decitabine (n=31). There were 67 patients in the azacitidine arm and 13 in the decitabine arm who were 75 or older or were ineligible for intensive induction chemotherapy.
Patients received venetoclax via a daily ramp-up to a final dose of 400 mg once daily. They received prophylaxis for tumor lysis syndrome and were hospitalized for monitoring during the ramp-up.
They received azacitidine at 75 mg/m2 on days 1-7 of each 28-day cycle or decitabine at 20 mg/m2 on days 1-5 of each cycle. Patients continued treatment until disease progression or unacceptable toxicity.
The median follow-up was 7.9 months for the azacitidine arm and 11 months for the decitabine arm.
The complete response (CR) rate was 37% (25/67) in the azacitidine arm and 54% (7/13) in the decitabine arm. The rates of CR with partial hematologic recovery were 24% (16/67) and 7.7% (1/13), respectively.
The most common adverse events (AEs)—occurring in at least 30% of patients in both arms—were nausea, diarrhea, constipation, neutropenia, thrombocytopenia, hemorrhage, peripheral edema, vomiting, fatigue, febrile neutropenia, rash, and anemia.
The incidence of serious AEs was 75% overall. The most frequent serious AEs (occurring in at least 5% of patients) were febrile neutropenia, pneumonia (excluding fungal), sepsis (excluding fungal), respiratory failure, and multiple organ dysfunction syndrome.
The incidence of fatal AEs was 1.5% within 30 days of treatment initiation.
M14-387 trial
The M14-387 trial included 82 AML patients who received venetoclax plus low-dose cytarabine. Patients were newly diagnosed with AML, but some had previous exposure to a hypomethylating agent for an antecedent hematologic disorder.
There were 61 patients who were 75 or older or were ineligible for intensive induction chemotherapy.
Patients received venetoclax via daily ramp-up to a final dose of 600 mg once daily. They received prophylaxis for tumor lysis syndrome and were hospitalized for monitoring during the ramp-up.
Cytarabine was given at 20 mg/m2 on days 1-10 of each 28-day cycle. Patients continued to receive treatment until disease progression or unacceptable toxicity.
At a median follow-up of 6.5 months, the CR rate was 21% (13/61), and the rate of CR with partial hematologic recovery was 21% (13/61).
The most common AEs (occurring in at least 30% of patients) were nausea, thrombocytopenia, hemorrhage, febrile neutropenia, neutropenia, diarrhea, fatigue, constipation, and dyspnea.
The incidence of serious AEs was 95%. The most frequent serious AEs (occurring in at least 5% of patients) were febrile neutropenia, sepsis (excluding fungal), hemorrhage, pneumonia (excluding fungal), and device-related infection.
The incidence of fatal AEs was 4.9% within 30 days of treatment initiation.
Additional details from the M14-358 and M14-387 trials are available in the prescribing information for venetoclax.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the United States and by AbbVie elsewhere.
FDA approves glasdegib for AML
The U.S. Food and Drug Administration (FDA) has approved the hedgehog pathway inhibitor glasdegib (Daurismo™) to treat certain patients with acute myeloid leukemia (AML).
Glasdegib is approved for use in combination with low-dose cytarabine (LDAC) to treat adults with newly diagnosed AML who are age 75 and older or who are ineligible for intensive chemotherapy.
Glasdegib was approved under priority review and also received orphan drug designation from the FDA.
The prescribing information for glasdegib includes a boxed warning detailing the risk of embryo-fetal death or severe birth defects associated with the drug.
The FDA’s approval of glasdegib is based on results from the phase 2 BRIGHT AML 1003 trial (NCT01546038).
This trial included 111 adults with newly diagnosed AML and 14 patients with other conditions.
The patients were randomized to receive glasdegib (at 100 mg daily) in combination with LDAC (n=84) or LDAC alone (n=41).
The complete response rate among the AML patients was 18.2% (14/77) in the glasdegib arm and 2.6% (1/38) in the LDAC arm.
The median overall survival was 8.3 months in the glasdegib arm and 4.3 months in the LDAC arm (hazard ratio=0.46; P=0.0002).
The most common adverse events (AEs) in the first 90 days of treatment—occurring in at least 30% of patients in either arm (glasdegib-LDAC and LDAC alone, respectively)—were:
- Anemia (43% and 42%)
- Fatigue (36% and 32%)
- Hemorrhage (36% and 42%)
- Febrile neutropenia (31% and 22%)
- Musculoskeletal pain (30% and 17%)
- Edema (30% and 20%)
- Thrombocytopenia (30% and 27%).
The incidence of serious AEs was 79% in the glasdegib arm. The most common serious AEs occurring in at least 5% of patients in this arm were febrile neutropenia (29%), pneumonia (23%), hemorrhage (12%), anemia (7%), and sepsis (7%).
Additional data from this trial are included in the prescribing information for glasdegib. Glasdegib is a product of Pfizer.
The U.S. Food and Drug Administration (FDA) has approved the hedgehog pathway inhibitor glasdegib (Daurismo™) to treat certain patients with acute myeloid leukemia (AML).
Glasdegib is approved for use in combination with low-dose cytarabine (LDAC) to treat adults with newly diagnosed AML who are age 75 and older or who are ineligible for intensive chemotherapy.
Glasdegib was approved under priority review and also received orphan drug designation from the FDA.
The prescribing information for glasdegib includes a boxed warning detailing the risk of embryo-fetal death or severe birth defects associated with the drug.
The FDA’s approval of glasdegib is based on results from the phase 2 BRIGHT AML 1003 trial (NCT01546038).
This trial included 111 adults with newly diagnosed AML and 14 patients with other conditions.
The patients were randomized to receive glasdegib (at 100 mg daily) in combination with LDAC (n=84) or LDAC alone (n=41).
The complete response rate among the AML patients was 18.2% (14/77) in the glasdegib arm and 2.6% (1/38) in the LDAC arm.
The median overall survival was 8.3 months in the glasdegib arm and 4.3 months in the LDAC arm (hazard ratio=0.46; P=0.0002).
The most common adverse events (AEs) in the first 90 days of treatment—occurring in at least 30% of patients in either arm (glasdegib-LDAC and LDAC alone, respectively)—were:
- Anemia (43% and 42%)
- Fatigue (36% and 32%)
- Hemorrhage (36% and 42%)
- Febrile neutropenia (31% and 22%)
- Musculoskeletal pain (30% and 17%)
- Edema (30% and 20%)
- Thrombocytopenia (30% and 27%).
The incidence of serious AEs was 79% in the glasdegib arm. The most common serious AEs occurring in at least 5% of patients in this arm were febrile neutropenia (29%), pneumonia (23%), hemorrhage (12%), anemia (7%), and sepsis (7%).
Additional data from this trial are included in the prescribing information for glasdegib. Glasdegib is a product of Pfizer.
The U.S. Food and Drug Administration (FDA) has approved the hedgehog pathway inhibitor glasdegib (Daurismo™) to treat certain patients with acute myeloid leukemia (AML).
Glasdegib is approved for use in combination with low-dose cytarabine (LDAC) to treat adults with newly diagnosed AML who are age 75 and older or who are ineligible for intensive chemotherapy.
Glasdegib was approved under priority review and also received orphan drug designation from the FDA.
The prescribing information for glasdegib includes a boxed warning detailing the risk of embryo-fetal death or severe birth defects associated with the drug.
The FDA’s approval of glasdegib is based on results from the phase 2 BRIGHT AML 1003 trial (NCT01546038).
This trial included 111 adults with newly diagnosed AML and 14 patients with other conditions.
The patients were randomized to receive glasdegib (at 100 mg daily) in combination with LDAC (n=84) or LDAC alone (n=41).
The complete response rate among the AML patients was 18.2% (14/77) in the glasdegib arm and 2.6% (1/38) in the LDAC arm.
The median overall survival was 8.3 months in the glasdegib arm and 4.3 months in the LDAC arm (hazard ratio=0.46; P=0.0002).
The most common adverse events (AEs) in the first 90 days of treatment—occurring in at least 30% of patients in either arm (glasdegib-LDAC and LDAC alone, respectively)—were:
- Anemia (43% and 42%)
- Fatigue (36% and 32%)
- Hemorrhage (36% and 42%)
- Febrile neutropenia (31% and 22%)
- Musculoskeletal pain (30% and 17%)
- Edema (30% and 20%)
- Thrombocytopenia (30% and 27%).
The incidence of serious AEs was 79% in the glasdegib arm. The most common serious AEs occurring in at least 5% of patients in this arm were febrile neutropenia (29%), pneumonia (23%), hemorrhage (12%), anemia (7%), and sepsis (7%).
Additional data from this trial are included in the prescribing information for glasdegib. Glasdegib is a product of Pfizer.
FDA approves first treatment for primary HLH
The U.S. Food and Drug Administration (FDA) has approved emapalumab-lzsg (Gamifant®) to treat primary hemophagocytic lymphohistiocytosis (HLH).
Emapalumab, an interferon gamma-blocking antibody, is approved to treat to treat patients of all ages (newborn and older) with primary HLH who have refractory, recurrent, or progressive disease or who cannot tolerate conventional HLH therapy.
Emapalumab is the first treatment to be FDA-approved for primary HLH, and it is expected to be available in the United States in the first quarter of 2019.
The FDA previously granted emapalumab priority review, breakthrough therapy designation, orphan drug designation, and rare pediatric disease designation.
The FDA’s approval of emapalumab is based on results from a phase 2/3 trial (NCT01818492).
The trial included 34 patients, 27 of whom had refractory, recurrent, or progressive disease or could not tolerate conventional HLH therapy.
Patients received emapalumab in combination with dexamethasone.
At the end of treatment, 63% (17/27) of patients had achieved a response, which was defined as complete response (n=7), partial response (n=8), or HLH improvement (n=2).
Seventy percent (n=19) of patients went on to hematopoietic stem cell transplant.
The most common adverse events were infections (56%), hypertension (41%), infusion-related reactions (27%), and pyrexia (24%).
Additional results from this study can be found in the prescribing information for emapalumab, which is available at www.gamifant.com.
Results are also scheduled to be presented at the 2018 ASH Annual Meeting (abstract LBA-6).
Emapalumab was developed by Novimmune SA. Sobi acquired global rights to the drug in August 2018.
The U.S. Food and Drug Administration (FDA) has approved emapalumab-lzsg (Gamifant®) to treat primary hemophagocytic lymphohistiocytosis (HLH).
Emapalumab, an interferon gamma-blocking antibody, is approved to treat to treat patients of all ages (newborn and older) with primary HLH who have refractory, recurrent, or progressive disease or who cannot tolerate conventional HLH therapy.
Emapalumab is the first treatment to be FDA-approved for primary HLH, and it is expected to be available in the United States in the first quarter of 2019.
The FDA previously granted emapalumab priority review, breakthrough therapy designation, orphan drug designation, and rare pediatric disease designation.
The FDA’s approval of emapalumab is based on results from a phase 2/3 trial (NCT01818492).
The trial included 34 patients, 27 of whom had refractory, recurrent, or progressive disease or could not tolerate conventional HLH therapy.
Patients received emapalumab in combination with dexamethasone.
At the end of treatment, 63% (17/27) of patients had achieved a response, which was defined as complete response (n=7), partial response (n=8), or HLH improvement (n=2).
Seventy percent (n=19) of patients went on to hematopoietic stem cell transplant.
The most common adverse events were infections (56%), hypertension (41%), infusion-related reactions (27%), and pyrexia (24%).
Additional results from this study can be found in the prescribing information for emapalumab, which is available at www.gamifant.com.
Results are also scheduled to be presented at the 2018 ASH Annual Meeting (abstract LBA-6).
Emapalumab was developed by Novimmune SA. Sobi acquired global rights to the drug in August 2018.
The U.S. Food and Drug Administration (FDA) has approved emapalumab-lzsg (Gamifant®) to treat primary hemophagocytic lymphohistiocytosis (HLH).
Emapalumab, an interferon gamma-blocking antibody, is approved to treat to treat patients of all ages (newborn and older) with primary HLH who have refractory, recurrent, or progressive disease or who cannot tolerate conventional HLH therapy.
Emapalumab is the first treatment to be FDA-approved for primary HLH, and it is expected to be available in the United States in the first quarter of 2019.
The FDA previously granted emapalumab priority review, breakthrough therapy designation, orphan drug designation, and rare pediatric disease designation.
The FDA’s approval of emapalumab is based on results from a phase 2/3 trial (NCT01818492).
The trial included 34 patients, 27 of whom had refractory, recurrent, or progressive disease or could not tolerate conventional HLH therapy.
Patients received emapalumab in combination with dexamethasone.
At the end of treatment, 63% (17/27) of patients had achieved a response, which was defined as complete response (n=7), partial response (n=8), or HLH improvement (n=2).
Seventy percent (n=19) of patients went on to hematopoietic stem cell transplant.
The most common adverse events were infections (56%), hypertension (41%), infusion-related reactions (27%), and pyrexia (24%).
Additional results from this study can be found in the prescribing information for emapalumab, which is available at www.gamifant.com.
Results are also scheduled to be presented at the 2018 ASH Annual Meeting (abstract LBA-6).
Emapalumab was developed by Novimmune SA. Sobi acquired global rights to the drug in August 2018.
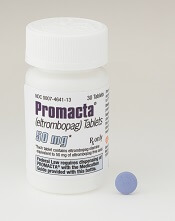
Eltrombopag approved as first-line SAA therapy
The U.S. Food and Drug Administration (FDA) has expanded the approved use of eltrombopag (Promacta®) in severe aplastic anemia (SAA).
Eltrombopag is now approved for use in combination with standard immunosuppressive therapy as first-line treatment for adults and pediatric patients age 2 and older with SAA.
Eltrombopag received breakthrough therapy designation and priority review for this indication.
Eltrombopag is also FDA-approved for SAA patients who have had an insufficient response to immunosuppressive therapy, for patients with chronic immune thrombocytopenia who have had an insufficient response to other treatments, and to treat thrombocytopenia in patients with chronic hepatitis C virus infection.
The FDA’s latest approval of eltrombopag is based on results from a phase 1/2 trial (NCT01623167), which were published in The New England Journal of Medicine in April 2017.
Updated results from the trial are available in the prescribing information for eltrombopag.
The trial included 153 previously untreated SAA patients age 2 and older. The patients received eltrombopag in combination with horse antithymocyte globulin and cyclosporine.
The starting dose of eltrombopag was:
- 150 mg once daily for patients age 12 and older (75 mg for East and Southeast Asians)
- 75 mg once daily for patients ages 6 to 11 (37.5 mg for East and Southeast Asians)
- 5 mg/kg once daily for patients ages 2 to 5 (1.25 mg/kg for East and Southeast Asians).
Patients were divided into three cohorts with different dosing schedules.
The recommended schedule, from the third cohort (n=92), was eltrombopag from day 1 to month 6, plus horse antithymocyte globulin and cyclosporine. All patients in this cohort were eligible to receive a low dose of cyclosporine for an additional 18 months if they achieved a hematologic response at 6 months.
Among the patients treated at the recommended dosing schedule, the 6-month overall response rate was 79%, and the complete response rate was 44%.
The median duration of both overall and complete response was 24.3 months.
The most common adverse events in these patients were ALT increase (29%), AST increase (17%), blood bilirubin increase (17%), rash (8%), and skin discoloration including hyperpigmentation (5%).
Eltrombopag is a product of Novartis.
The U.S. Food and Drug Administration (FDA) has expanded the approved use of eltrombopag (Promacta®) in severe aplastic anemia (SAA).
Eltrombopag is now approved for use in combination with standard immunosuppressive therapy as first-line treatment for adults and pediatric patients age 2 and older with SAA.
Eltrombopag received breakthrough therapy designation and priority review for this indication.
Eltrombopag is also FDA-approved for SAA patients who have had an insufficient response to immunosuppressive therapy, for patients with chronic immune thrombocytopenia who have had an insufficient response to other treatments, and to treat thrombocytopenia in patients with chronic hepatitis C virus infection.
The FDA’s latest approval of eltrombopag is based on results from a phase 1/2 trial (NCT01623167), which were published in The New England Journal of Medicine in April 2017.
Updated results from the trial are available in the prescribing information for eltrombopag.
The trial included 153 previously untreated SAA patients age 2 and older. The patients received eltrombopag in combination with horse antithymocyte globulin and cyclosporine.
The starting dose of eltrombopag was:
- 150 mg once daily for patients age 12 and older (75 mg for East and Southeast Asians)
- 75 mg once daily for patients ages 6 to 11 (37.5 mg for East and Southeast Asians)
- 5 mg/kg once daily for patients ages 2 to 5 (1.25 mg/kg for East and Southeast Asians).
Patients were divided into three cohorts with different dosing schedules.
The recommended schedule, from the third cohort (n=92), was eltrombopag from day 1 to month 6, plus horse antithymocyte globulin and cyclosporine. All patients in this cohort were eligible to receive a low dose of cyclosporine for an additional 18 months if they achieved a hematologic response at 6 months.
Among the patients treated at the recommended dosing schedule, the 6-month overall response rate was 79%, and the complete response rate was 44%.
The median duration of both overall and complete response was 24.3 months.
The most common adverse events in these patients were ALT increase (29%), AST increase (17%), blood bilirubin increase (17%), rash (8%), and skin discoloration including hyperpigmentation (5%).
Eltrombopag is a product of Novartis.
The U.S. Food and Drug Administration (FDA) has expanded the approved use of eltrombopag (Promacta®) in severe aplastic anemia (SAA).
Eltrombopag is now approved for use in combination with standard immunosuppressive therapy as first-line treatment for adults and pediatric patients age 2 and older with SAA.
Eltrombopag received breakthrough therapy designation and priority review for this indication.
Eltrombopag is also FDA-approved for SAA patients who have had an insufficient response to immunosuppressive therapy, for patients with chronic immune thrombocytopenia who have had an insufficient response to other treatments, and to treat thrombocytopenia in patients with chronic hepatitis C virus infection.
The FDA’s latest approval of eltrombopag is based on results from a phase 1/2 trial (NCT01623167), which were published in The New England Journal of Medicine in April 2017.
Updated results from the trial are available in the prescribing information for eltrombopag.
The trial included 153 previously untreated SAA patients age 2 and older. The patients received eltrombopag in combination with horse antithymocyte globulin and cyclosporine.
The starting dose of eltrombopag was:
- 150 mg once daily for patients age 12 and older (75 mg for East and Southeast Asians)
- 75 mg once daily for patients ages 6 to 11 (37.5 mg for East and Southeast Asians)
- 5 mg/kg once daily for patients ages 2 to 5 (1.25 mg/kg for East and Southeast Asians).
Patients were divided into three cohorts with different dosing schedules.
The recommended schedule, from the third cohort (n=92), was eltrombopag from day 1 to month 6, plus horse antithymocyte globulin and cyclosporine. All patients in this cohort were eligible to receive a low dose of cyclosporine for an additional 18 months if they achieved a hematologic response at 6 months.
Among the patients treated at the recommended dosing schedule, the 6-month overall response rate was 79%, and the complete response rate was 44%.
The median duration of both overall and complete response was 24.3 months.
The most common adverse events in these patients were ALT increase (29%), AST increase (17%), blood bilirubin increase (17%), rash (8%), and skin discoloration including hyperpigmentation (5%).
Eltrombopag is a product of Novartis.
Quick FDA approval for brentuximab vedotin in PTCL
The U.S. Food and Drug Administration (FDA) has approved a new indication for brentuximab vedotin (ADCETRIS®) less than 2 weeks after receiving the completed supplemental biologics license application (sBLA).
Brentuximab vedotin is now approved for use in combination with cyclophosphamide, doxorubicin, and prednisone (CHP) to treat adults with previously untreated systemic anaplastic large-cell lymphoma or other CD30-expressing peripheral T-cell lymphomas (PTCLs), including angioimmunoblastic T-cell lymphoma and PTCL not otherwise specified.
The FDA granted priority review and breakthrough therapy designation to the sBLA for brentuximab vedotin in this indication.
The FDA reviewed the sBLA under the Real-Time Oncology Review Pilot Program, which led to approval less than 2 weeks after the application was submitted in full.
“The Real-Time Oncology Review program allows the FDA to access key data prior to the official submission of the application, allowing the review team to begin their review earlier and communicate with the sponsor prior to the application’s actual submission,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products.
“When the sponsor submits the completed application, the review team will already be familiar with the data and be able to conduct a more efficient, timely, and thorough review.”
Trial data
The FDA’s approval is based on results from the phase 3 ECHELON-2 trial (NCT01777152).
Seattle Genetics, Inc. and Takeda Pharmaceutical Company Limited announced results from this trial last month. Additional results are scheduled to be presented at the 2018 ASH Annual Meeting (abstract 997).
The trial enrolled 452 patients with CD30-positive PTCL. The patients were randomized to receive brentuximab vedotin (BV) plus CHP or cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP).
The objective response rate was 83% in the BV-CHP arm and 72% in the CHOP arm (P=0.003). The complete response rate was 68% and 56%, respectively (P=0.007).
Progression-free survival was significantly better in the BV-CHP arm than in the CHOP arm (hazard ratio=0.71; P=0.011), as was overall survival (hazard ratio=0.66; P=0.024).
The most common adverse events of any grade that occurred in at least 20% of patients in the BV-CHP arm were peripheral neuropathy, nausea, diarrhea, neutropenia, lymphopenia, fatigue, mucositis, constipation, alopecia, pyrexia, vomiting, and anemia.
Serious adverse events occurring in at least 2% of patients in the BV-CHP arm included febrile neutropenia, pneumonia, pyrexia, and sepsis.
Results of this trial suggest prophylactic growth factors should be given to previously untreated PTCL patients receiving BV-CHP (starting at cycle 1).
The U.S. Food and Drug Administration (FDA) has approved a new indication for brentuximab vedotin (ADCETRIS®) less than 2 weeks after receiving the completed supplemental biologics license application (sBLA).
Brentuximab vedotin is now approved for use in combination with cyclophosphamide, doxorubicin, and prednisone (CHP) to treat adults with previously untreated systemic anaplastic large-cell lymphoma or other CD30-expressing peripheral T-cell lymphomas (PTCLs), including angioimmunoblastic T-cell lymphoma and PTCL not otherwise specified.
The FDA granted priority review and breakthrough therapy designation to the sBLA for brentuximab vedotin in this indication.
The FDA reviewed the sBLA under the Real-Time Oncology Review Pilot Program, which led to approval less than 2 weeks after the application was submitted in full.
“The Real-Time Oncology Review program allows the FDA to access key data prior to the official submission of the application, allowing the review team to begin their review earlier and communicate with the sponsor prior to the application’s actual submission,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products.
“When the sponsor submits the completed application, the review team will already be familiar with the data and be able to conduct a more efficient, timely, and thorough review.”
Trial data
The FDA’s approval is based on results from the phase 3 ECHELON-2 trial (NCT01777152).
Seattle Genetics, Inc. and Takeda Pharmaceutical Company Limited announced results from this trial last month. Additional results are scheduled to be presented at the 2018 ASH Annual Meeting (abstract 997).
The trial enrolled 452 patients with CD30-positive PTCL. The patients were randomized to receive brentuximab vedotin (BV) plus CHP or cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP).
The objective response rate was 83% in the BV-CHP arm and 72% in the CHOP arm (P=0.003). The complete response rate was 68% and 56%, respectively (P=0.007).
Progression-free survival was significantly better in the BV-CHP arm than in the CHOP arm (hazard ratio=0.71; P=0.011), as was overall survival (hazard ratio=0.66; P=0.024).
The most common adverse events of any grade that occurred in at least 20% of patients in the BV-CHP arm were peripheral neuropathy, nausea, diarrhea, neutropenia, lymphopenia, fatigue, mucositis, constipation, alopecia, pyrexia, vomiting, and anemia.
Serious adverse events occurring in at least 2% of patients in the BV-CHP arm included febrile neutropenia, pneumonia, pyrexia, and sepsis.
Results of this trial suggest prophylactic growth factors should be given to previously untreated PTCL patients receiving BV-CHP (starting at cycle 1).
The U.S. Food and Drug Administration (FDA) has approved a new indication for brentuximab vedotin (ADCETRIS®) less than 2 weeks after receiving the completed supplemental biologics license application (sBLA).
Brentuximab vedotin is now approved for use in combination with cyclophosphamide, doxorubicin, and prednisone (CHP) to treat adults with previously untreated systemic anaplastic large-cell lymphoma or other CD30-expressing peripheral T-cell lymphomas (PTCLs), including angioimmunoblastic T-cell lymphoma and PTCL not otherwise specified.
The FDA granted priority review and breakthrough therapy designation to the sBLA for brentuximab vedotin in this indication.
The FDA reviewed the sBLA under the Real-Time Oncology Review Pilot Program, which led to approval less than 2 weeks after the application was submitted in full.
“The Real-Time Oncology Review program allows the FDA to access key data prior to the official submission of the application, allowing the review team to begin their review earlier and communicate with the sponsor prior to the application’s actual submission,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products.
“When the sponsor submits the completed application, the review team will already be familiar with the data and be able to conduct a more efficient, timely, and thorough review.”
Trial data
The FDA’s approval is based on results from the phase 3 ECHELON-2 trial (NCT01777152).
Seattle Genetics, Inc. and Takeda Pharmaceutical Company Limited announced results from this trial last month. Additional results are scheduled to be presented at the 2018 ASH Annual Meeting (abstract 997).
The trial enrolled 452 patients with CD30-positive PTCL. The patients were randomized to receive brentuximab vedotin (BV) plus CHP or cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP).
The objective response rate was 83% in the BV-CHP arm and 72% in the CHOP arm (P=0.003). The complete response rate was 68% and 56%, respectively (P=0.007).
Progression-free survival was significantly better in the BV-CHP arm than in the CHOP arm (hazard ratio=0.71; P=0.011), as was overall survival (hazard ratio=0.66; P=0.024).
The most common adverse events of any grade that occurred in at least 20% of patients in the BV-CHP arm were peripheral neuropathy, nausea, diarrhea, neutropenia, lymphopenia, fatigue, mucositis, constipation, alopecia, pyrexia, vomiting, and anemia.
Serious adverse events occurring in at least 2% of patients in the BV-CHP arm included febrile neutropenia, pneumonia, pyrexia, and sepsis.
Results of this trial suggest prophylactic growth factors should be given to previously untreated PTCL patients receiving BV-CHP (starting at cycle 1).
FDA approves generic drugs for APL
The U.S. Food and Drug Administration (FDA) has now approved three generic arsenic trioxide products for use in patients with acute promyelocytic leukemia (APL).
Two of the products—from Zydus Cadila and Amring Pharmaceuticals—were approved on November 13.
The third—from Fresenius Kabi—was approved in August and launched in the United States last month.
All three injectable arsenic trioxide products (1 mg/mL) are generic versions of Teva’s Trisenox.
Since 2000, Trisenox has been FDA-approved to induce remission and as consolidation therapy for patients with APL who are refractory to, or have relapsed after, retinoid and anthracycline chemotherapy, and whose APL is characterized by presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
In January, the FDA approved Trisenox for use in combination with tretinoin to treat adults with newly diagnosed, low-risk APL with the t(15;17) translocation or PML/RAR-alpha gene expression.
The U.S. Food and Drug Administration (FDA) has now approved three generic arsenic trioxide products for use in patients with acute promyelocytic leukemia (APL).
Two of the products—from Zydus Cadila and Amring Pharmaceuticals—were approved on November 13.
The third—from Fresenius Kabi—was approved in August and launched in the United States last month.
All three injectable arsenic trioxide products (1 mg/mL) are generic versions of Teva’s Trisenox.
Since 2000, Trisenox has been FDA-approved to induce remission and as consolidation therapy for patients with APL who are refractory to, or have relapsed after, retinoid and anthracycline chemotherapy, and whose APL is characterized by presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
In January, the FDA approved Trisenox for use in combination with tretinoin to treat adults with newly diagnosed, low-risk APL with the t(15;17) translocation or PML/RAR-alpha gene expression.
The U.S. Food and Drug Administration (FDA) has now approved three generic arsenic trioxide products for use in patients with acute promyelocytic leukemia (APL).
Two of the products—from Zydus Cadila and Amring Pharmaceuticals—were approved on November 13.
The third—from Fresenius Kabi—was approved in August and launched in the United States last month.
All three injectable arsenic trioxide products (1 mg/mL) are generic versions of Teva’s Trisenox.
Since 2000, Trisenox has been FDA-approved to induce remission and as consolidation therapy for patients with APL who are refractory to, or have relapsed after, retinoid and anthracycline chemotherapy, and whose APL is characterized by presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
In January, the FDA approved Trisenox for use in combination with tretinoin to treat adults with newly diagnosed, low-risk APL with the t(15;17) translocation or PML/RAR-alpha gene expression.