User login
Vaccine candidate fails to prevent malaria in humans
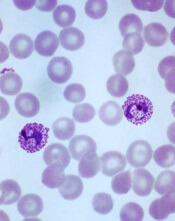
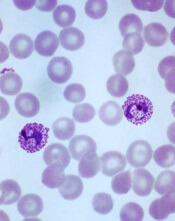
Plasmodium vivax
Image by Mae Melvin
Results of a phase 1 trial suggest a vaccine candidate does not prevent Plasmodium vivax malaria.
The vaccine, VMP001/AS01B, did not prevent malaria in any of the 30 subjects tested, although it did significantly delay parasitemia in 59% of subjects.
Lieutenant Colonel Jason W. Bennett, of the Walter Reed Army Institute
of Research (WRAIR) in Silver Spring, Maryland, and his colleagues reported these results in PLOS Neglected Tropical Diseases.
The vaccine antigen VMP001 is an Escherichia coli-produced, synthetic, chimeric, recombinant protein that incorporates the 3 major domains of circumsporozoite protein but is distinct from the native molecule. The VMP001 antigen was adjuvanted with AS01B, a proprietary liposome-based adjuvant system from GlaxoSmithKline.
For this phase 1 study, the investigators tested VMP001/AS01B in 30 healthy volunteers. The subjects received 3 intramuscular injections of VMP001 at 15 μg (n=10), 30 μg (n=10), or 60 μg (n=10), respectively, all formulated in 500 μL of AS01B at each immunization.
Fourteen days after the third immunization, the subjects were exposed to mosquitoes carrying P vivax. Six non-vaccinated control subjects were exposed to the mosquitoes as well.
The investigators said VMP001/AS01B was well tolerated and generated robust immune responses. However, it did not protect the subjects from malaria infection.
Still, the vaccine induced a “small but significant” delay in time to parasitemia in 59% of vaccinated subjects, when compared to controls.
Colonel Robert Paris, director of the US Military Malaria Research Program at WRAIR, believes the investigators can use the results of this study to design a better vaccine for P vivax malaria.
“Findings from the analysis of the immune response of vaccinated subjects have given us clues to improve vaccine candidates,” he said. “[S]tudies are now underway at WRAIR to develop next-generation vivax vaccines.” ![]()
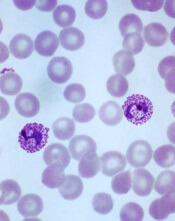
Plasmodium vivax
Image by Mae Melvin
Results of a phase 1 trial suggest a vaccine candidate does not prevent Plasmodium vivax malaria.
The vaccine, VMP001/AS01B, did not prevent malaria in any of the 30 subjects tested, although it did significantly delay parasitemia in 59% of subjects.
Lieutenant Colonel Jason W. Bennett, of the Walter Reed Army Institute
of Research (WRAIR) in Silver Spring, Maryland, and his colleagues reported these results in PLOS Neglected Tropical Diseases.
The vaccine antigen VMP001 is an Escherichia coli-produced, synthetic, chimeric, recombinant protein that incorporates the 3 major domains of circumsporozoite protein but is distinct from the native molecule. The VMP001 antigen was adjuvanted with AS01B, a proprietary liposome-based adjuvant system from GlaxoSmithKline.
For this phase 1 study, the investigators tested VMP001/AS01B in 30 healthy volunteers. The subjects received 3 intramuscular injections of VMP001 at 15 μg (n=10), 30 μg (n=10), or 60 μg (n=10), respectively, all formulated in 500 μL of AS01B at each immunization.
Fourteen days after the third immunization, the subjects were exposed to mosquitoes carrying P vivax. Six non-vaccinated control subjects were exposed to the mosquitoes as well.
The investigators said VMP001/AS01B was well tolerated and generated robust immune responses. However, it did not protect the subjects from malaria infection.
Still, the vaccine induced a “small but significant” delay in time to parasitemia in 59% of vaccinated subjects, when compared to controls.
Colonel Robert Paris, director of the US Military Malaria Research Program at WRAIR, believes the investigators can use the results of this study to design a better vaccine for P vivax malaria.
“Findings from the analysis of the immune response of vaccinated subjects have given us clues to improve vaccine candidates,” he said. “[S]tudies are now underway at WRAIR to develop next-generation vivax vaccines.” ![]()
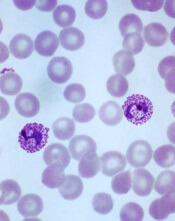
Plasmodium vivax
Image by Mae Melvin
Results of a phase 1 trial suggest a vaccine candidate does not prevent Plasmodium vivax malaria.
The vaccine, VMP001/AS01B, did not prevent malaria in any of the 30 subjects tested, although it did significantly delay parasitemia in 59% of subjects.
Lieutenant Colonel Jason W. Bennett, of the Walter Reed Army Institute
of Research (WRAIR) in Silver Spring, Maryland, and his colleagues reported these results in PLOS Neglected Tropical Diseases.
The vaccine antigen VMP001 is an Escherichia coli-produced, synthetic, chimeric, recombinant protein that incorporates the 3 major domains of circumsporozoite protein but is distinct from the native molecule. The VMP001 antigen was adjuvanted with AS01B, a proprietary liposome-based adjuvant system from GlaxoSmithKline.
For this phase 1 study, the investigators tested VMP001/AS01B in 30 healthy volunteers. The subjects received 3 intramuscular injections of VMP001 at 15 μg (n=10), 30 μg (n=10), or 60 μg (n=10), respectively, all formulated in 500 μL of AS01B at each immunization.
Fourteen days after the third immunization, the subjects were exposed to mosquitoes carrying P vivax. Six non-vaccinated control subjects were exposed to the mosquitoes as well.
The investigators said VMP001/AS01B was well tolerated and generated robust immune responses. However, it did not protect the subjects from malaria infection.
Still, the vaccine induced a “small but significant” delay in time to parasitemia in 59% of vaccinated subjects, when compared to controls.
Colonel Robert Paris, director of the US Military Malaria Research Program at WRAIR, believes the investigators can use the results of this study to design a better vaccine for P vivax malaria.
“Findings from the analysis of the immune response of vaccinated subjects have given us clues to improve vaccine candidates,” he said. “[S]tudies are now underway at WRAIR to develop next-generation vivax vaccines.” ![]()
FDA authorizes CDC’s test for Zika virus

Photo by Jeremy L. Grisham
The US Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) for a laboratory test used to detect the Zika virus.
The test, which was developed by the Centers for Disease Control and Prevention (CDC), is called the Zika IgM Antibody Capture Enzyme-Linked Immunosorbent Assay (Zika MAC-ELISA).
It will be distributed to certain laboratories in the US and abroad over the next 2 weeks.
The test will not be available in US hospitals or other primary care settings.
The Zika MAC-ELISA test can detect human immunoglobulin M (IgM) antibodies to the Zika virus. These antibodies appear in the blood of an infected person 4 to 5 days after the start of the illness, and they remain in the blood for about 12 weeks.
The Zika MAC-ELISA test is intended for use in sera or cerebrospinal fluid when submitted with a patient-matched serum sample from individuals meeting CDC Zika clinical and epidemiological criteria for testing. This includes people with a history of symptoms associated with Zika and/or people who have recently traveled to an area that has active Zika transmission.
Results of Zika MAC-ELISA tests require careful interpretation. The test can give false-positive results when someone has been infected with a virus closely related to Zika (such as dengue virus).
When positive or inconclusive results occur, additional testing (plaque reduction neutralization test) to confirm the presence of antibodies to Zika virus will be performed by the CDC or a CDC-authorized laboratory.
Moreover, a negative test result does not necessarily mean a person has not been infected with Zika virus. If a sample is collected just after a person becomes ill, there may not be enough IgM antibodies for the test to measure, resulting in a false-negative.
Similarly, if the sample was collected more than 12 weeks after illness, it is possible that the body has successfully fought the virus and IgM antibody levels have dropped below the detectable limit.
The CDC will begin distributing the Zika MAC-ELISA test over the next 2 weeks to qualified laboratories in the Laboratory Response Network, an integrated network of domestic and international laboratories that can respond to public health emergencies.
About the EUA
An EUA allows the use of unapproved medical products or unapproved uses of approved medical products in an emergency. The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
As there are no commercially available diagnostic tests approved by the FDA for the detection of Zika virus infection, the agency decided an EUA was crucial to ensure timely access to a diagnostic tool.
The FDA issued the EUA for the Zika MAC-ELISA test based on data submitted by the CDC and on the US Secretary of Health and Human Services’ declaration that circumstances exist to justify the emergency use of in vitro diagnostic tests for the detection of Zika virus and Zika virus infection. This EUA will end when the Secretary’s declaration ends, unless the FDA revokes it sooner. ![]()

Photo by Jeremy L. Grisham
The US Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) for a laboratory test used to detect the Zika virus.
The test, which was developed by the Centers for Disease Control and Prevention (CDC), is called the Zika IgM Antibody Capture Enzyme-Linked Immunosorbent Assay (Zika MAC-ELISA).
It will be distributed to certain laboratories in the US and abroad over the next 2 weeks.
The test will not be available in US hospitals or other primary care settings.
The Zika MAC-ELISA test can detect human immunoglobulin M (IgM) antibodies to the Zika virus. These antibodies appear in the blood of an infected person 4 to 5 days after the start of the illness, and they remain in the blood for about 12 weeks.
The Zika MAC-ELISA test is intended for use in sera or cerebrospinal fluid when submitted with a patient-matched serum sample from individuals meeting CDC Zika clinical and epidemiological criteria for testing. This includes people with a history of symptoms associated with Zika and/or people who have recently traveled to an area that has active Zika transmission.
Results of Zika MAC-ELISA tests require careful interpretation. The test can give false-positive results when someone has been infected with a virus closely related to Zika (such as dengue virus).
When positive or inconclusive results occur, additional testing (plaque reduction neutralization test) to confirm the presence of antibodies to Zika virus will be performed by the CDC or a CDC-authorized laboratory.
Moreover, a negative test result does not necessarily mean a person has not been infected with Zika virus. If a sample is collected just after a person becomes ill, there may not be enough IgM antibodies for the test to measure, resulting in a false-negative.
Similarly, if the sample was collected more than 12 weeks after illness, it is possible that the body has successfully fought the virus and IgM antibody levels have dropped below the detectable limit.
The CDC will begin distributing the Zika MAC-ELISA test over the next 2 weeks to qualified laboratories in the Laboratory Response Network, an integrated network of domestic and international laboratories that can respond to public health emergencies.
About the EUA
An EUA allows the use of unapproved medical products or unapproved uses of approved medical products in an emergency. The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
As there are no commercially available diagnostic tests approved by the FDA for the detection of Zika virus infection, the agency decided an EUA was crucial to ensure timely access to a diagnostic tool.
The FDA issued the EUA for the Zika MAC-ELISA test based on data submitted by the CDC and on the US Secretary of Health and Human Services’ declaration that circumstances exist to justify the emergency use of in vitro diagnostic tests for the detection of Zika virus and Zika virus infection. This EUA will end when the Secretary’s declaration ends, unless the FDA revokes it sooner. ![]()

Photo by Jeremy L. Grisham
The US Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) for a laboratory test used to detect the Zika virus.
The test, which was developed by the Centers for Disease Control and Prevention (CDC), is called the Zika IgM Antibody Capture Enzyme-Linked Immunosorbent Assay (Zika MAC-ELISA).
It will be distributed to certain laboratories in the US and abroad over the next 2 weeks.
The test will not be available in US hospitals or other primary care settings.
The Zika MAC-ELISA test can detect human immunoglobulin M (IgM) antibodies to the Zika virus. These antibodies appear in the blood of an infected person 4 to 5 days after the start of the illness, and they remain in the blood for about 12 weeks.
The Zika MAC-ELISA test is intended for use in sera or cerebrospinal fluid when submitted with a patient-matched serum sample from individuals meeting CDC Zika clinical and epidemiological criteria for testing. This includes people with a history of symptoms associated with Zika and/or people who have recently traveled to an area that has active Zika transmission.
Results of Zika MAC-ELISA tests require careful interpretation. The test can give false-positive results when someone has been infected with a virus closely related to Zika (such as dengue virus).
When positive or inconclusive results occur, additional testing (plaque reduction neutralization test) to confirm the presence of antibodies to Zika virus will be performed by the CDC or a CDC-authorized laboratory.
Moreover, a negative test result does not necessarily mean a person has not been infected with Zika virus. If a sample is collected just after a person becomes ill, there may not be enough IgM antibodies for the test to measure, resulting in a false-negative.
Similarly, if the sample was collected more than 12 weeks after illness, it is possible that the body has successfully fought the virus and IgM antibody levels have dropped below the detectable limit.
The CDC will begin distributing the Zika MAC-ELISA test over the next 2 weeks to qualified laboratories in the Laboratory Response Network, an integrated network of domestic and international laboratories that can respond to public health emergencies.
About the EUA
An EUA allows the use of unapproved medical products or unapproved uses of approved medical products in an emergency. The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
As there are no commercially available diagnostic tests approved by the FDA for the detection of Zika virus infection, the agency decided an EUA was crucial to ensure timely access to a diagnostic tool.
The FDA issued the EUA for the Zika MAC-ELISA test based on data submitted by the CDC and on the US Secretary of Health and Human Services’ declaration that circumstances exist to justify the emergency use of in vitro diagnostic tests for the detection of Zika virus and Zika virus infection. This EUA will end when the Secretary’s declaration ends, unless the FDA revokes it sooner. ![]()
Team develops hospital-based Zika test

Photo by Juan D. Alfonso
Two institutions in Houston, Texas, have developed the US’s first hospital-based, rapid diagnostic test for the Zika virus.
Pathologists and clinical laboratory scientists at Texas Children’s Hospital and Houston Methodist Hospital developed the test, which is customized to each hospital’s diagnostic laboratory and can provide results within several hours.
The test can be performed on blood, amniotic fluid, urine, or spinal fluid.
The test identifies virus-specific RNA sequences to detect Zika virus. It can distinguish Zika infection from dengue, West Nile, or chikungunya infections.
Right now, only registered patients at Texas Children’s or Houston Methodist Hospital can receive the test, but the labs will consider referral testing from other hospitals and clinics in the future.
Initially, the test will be offered to patients with a positive travel history and symptoms consistent with acute Zika virus infection (eg, rash, arthralgia, or fever) or asymptomatic pregnant women with a positive travel history to any of the Zika-affected countries.
The goal of hospital-based testing for Zika virus is to prevent the delays that may occur with testing conducted in local and state public health laboratories and the Centers for Disease Control and Prevention.
“Hospital-based testing that is state-of-the-art enables our physicians and patients to get very rapid diagnostic answers,” said James M. Musser, MD, PhD, of Houston Methodist Hospital.
“If tests need to be repeated or if our treating doctors need to talk with our pathologists, we have the resources near patient care settings.”
The collaboration between Texas Children’s and Houston Methodist Hospital was sponsored by the L.E. and Virginia Simmons Collaborative in Virus Detection and Surveillance. This program was designed to facilitate rapid development of tests for virus detection in a large metropolitan area. ![]()

Photo by Juan D. Alfonso
Two institutions in Houston, Texas, have developed the US’s first hospital-based, rapid diagnostic test for the Zika virus.
Pathologists and clinical laboratory scientists at Texas Children’s Hospital and Houston Methodist Hospital developed the test, which is customized to each hospital’s diagnostic laboratory and can provide results within several hours.
The test can be performed on blood, amniotic fluid, urine, or spinal fluid.
The test identifies virus-specific RNA sequences to detect Zika virus. It can distinguish Zika infection from dengue, West Nile, or chikungunya infections.
Right now, only registered patients at Texas Children’s or Houston Methodist Hospital can receive the test, but the labs will consider referral testing from other hospitals and clinics in the future.
Initially, the test will be offered to patients with a positive travel history and symptoms consistent with acute Zika virus infection (eg, rash, arthralgia, or fever) or asymptomatic pregnant women with a positive travel history to any of the Zika-affected countries.
The goal of hospital-based testing for Zika virus is to prevent the delays that may occur with testing conducted in local and state public health laboratories and the Centers for Disease Control and Prevention.
“Hospital-based testing that is state-of-the-art enables our physicians and patients to get very rapid diagnostic answers,” said James M. Musser, MD, PhD, of Houston Methodist Hospital.
“If tests need to be repeated or if our treating doctors need to talk with our pathologists, we have the resources near patient care settings.”
The collaboration between Texas Children’s and Houston Methodist Hospital was sponsored by the L.E. and Virginia Simmons Collaborative in Virus Detection and Surveillance. This program was designed to facilitate rapid development of tests for virus detection in a large metropolitan area. ![]()

Photo by Juan D. Alfonso
Two institutions in Houston, Texas, have developed the US’s first hospital-based, rapid diagnostic test for the Zika virus.
Pathologists and clinical laboratory scientists at Texas Children’s Hospital and Houston Methodist Hospital developed the test, which is customized to each hospital’s diagnostic laboratory and can provide results within several hours.
The test can be performed on blood, amniotic fluid, urine, or spinal fluid.
The test identifies virus-specific RNA sequences to detect Zika virus. It can distinguish Zika infection from dengue, West Nile, or chikungunya infections.
Right now, only registered patients at Texas Children’s or Houston Methodist Hospital can receive the test, but the labs will consider referral testing from other hospitals and clinics in the future.
Initially, the test will be offered to patients with a positive travel history and symptoms consistent with acute Zika virus infection (eg, rash, arthralgia, or fever) or asymptomatic pregnant women with a positive travel history to any of the Zika-affected countries.
The goal of hospital-based testing for Zika virus is to prevent the delays that may occur with testing conducted in local and state public health laboratories and the Centers for Disease Control and Prevention.
“Hospital-based testing that is state-of-the-art enables our physicians and patients to get very rapid diagnostic answers,” said James M. Musser, MD, PhD, of Houston Methodist Hospital.
“If tests need to be repeated or if our treating doctors need to talk with our pathologists, we have the resources near patient care settings.”
The collaboration between Texas Children’s and Houston Methodist Hospital was sponsored by the L.E. and Virginia Simmons Collaborative in Virus Detection and Surveillance. This program was designed to facilitate rapid development of tests for virus detection in a large metropolitan area. ![]()
Protein ‘map’ could aid development of malaria vaccine
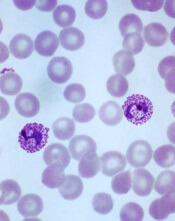
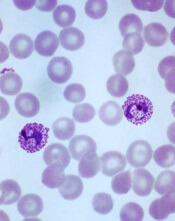
Plasmodium vivax
Image by Mae Melvin
Researchers say they have determined the structure of the protein PvRBP2a, which is used by the malaria parasite Plasmodium vivax to infect human red blood cells.
This revealed that PvRBP2a is structurally similar to PfRh5, the essential erythrocyte-binding protein in the parasite P falciparum.
The researchers believe these findings could help scientists generate new tools to prevent infection with malaria parasites.
Wai-Hong Tham, PhD, of The Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia, and her colleagues conducted this research and reported the results in PNAS.
“We have produced the first 3-dimensional, atomic resolution structure of the protein [PvRBP2a] using the Australian Synchrotron in Melbourne,” Dr Tham said.
She and her colleagues found that PvRBP2a consists of 10 α-helices and 1 short β-hairpin. And although PvRBP2a is structurally similar to PfRh5, the 2 proteins have different surface properties.
“The 3-dimensional map showed us that the proteins are folded in the same way—like having similar origami instructions,” Dr Tham said. “The difference is actually in the electrical charge on the surface of the molecules.”
“Now that we have an atomic-resolution map, we hope to identify a common part of the protein that could be used to design a vaccine not only for Plasmodium vivax but potentially for both vivax and falciparum.”
“These two species of malaria are responsible for the majority of malaria infections worldwide, so a vaccine that targets both would be a critical addition to our arsenal.”
Dr Tham said there is growing evidence that developing better treatments or preventive strategies for P vivax malaria is imperative for malaria eradication.
“Not only is P vivax the most widespread species of malaria, it is also more difficult to treat because it can hide in the liver for long periods of time without symptoms,” she said. “In addition, studies show that effective treatment of falciparum malaria tends to be accompanied by a resurgence of P vivax, so it is critical to continue looking for better ways to manage this species.” ![]()
Plasmodium vivax
Image by Mae Melvin
Researchers say they have determined the structure of the protein PvRBP2a, which is used by the malaria parasite Plasmodium vivax to infect human red blood cells.
This revealed that PvRBP2a is structurally similar to PfRh5, the essential erythrocyte-binding protein in the parasite P falciparum.
The researchers believe these findings could help scientists generate new tools to prevent infection with malaria parasites.
Wai-Hong Tham, PhD, of The Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia, and her colleagues conducted this research and reported the results in PNAS.
“We have produced the first 3-dimensional, atomic resolution structure of the protein [PvRBP2a] using the Australian Synchrotron in Melbourne,” Dr Tham said.
She and her colleagues found that PvRBP2a consists of 10 α-helices and 1 short β-hairpin. And although PvRBP2a is structurally similar to PfRh5, the 2 proteins have different surface properties.
“The 3-dimensional map showed us that the proteins are folded in the same way—like having similar origami instructions,” Dr Tham said. “The difference is actually in the electrical charge on the surface of the molecules.”
“Now that we have an atomic-resolution map, we hope to identify a common part of the protein that could be used to design a vaccine not only for Plasmodium vivax but potentially for both vivax and falciparum.”
“These two species of malaria are responsible for the majority of malaria infections worldwide, so a vaccine that targets both would be a critical addition to our arsenal.”
Dr Tham said there is growing evidence that developing better treatments or preventive strategies for P vivax malaria is imperative for malaria eradication.
“Not only is P vivax the most widespread species of malaria, it is also more difficult to treat because it can hide in the liver for long periods of time without symptoms,” she said. “In addition, studies show that effective treatment of falciparum malaria tends to be accompanied by a resurgence of P vivax, so it is critical to continue looking for better ways to manage this species.” ![]()
Plasmodium vivax
Image by Mae Melvin
Researchers say they have determined the structure of the protein PvRBP2a, which is used by the malaria parasite Plasmodium vivax to infect human red blood cells.
This revealed that PvRBP2a is structurally similar to PfRh5, the essential erythrocyte-binding protein in the parasite P falciparum.
The researchers believe these findings could help scientists generate new tools to prevent infection with malaria parasites.
Wai-Hong Tham, PhD, of The Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia, and her colleagues conducted this research and reported the results in PNAS.
“We have produced the first 3-dimensional, atomic resolution structure of the protein [PvRBP2a] using the Australian Synchrotron in Melbourne,” Dr Tham said.
She and her colleagues found that PvRBP2a consists of 10 α-helices and 1 short β-hairpin. And although PvRBP2a is structurally similar to PfRh5, the 2 proteins have different surface properties.
“The 3-dimensional map showed us that the proteins are folded in the same way—like having similar origami instructions,” Dr Tham said. “The difference is actually in the electrical charge on the surface of the molecules.”
“Now that we have an atomic-resolution map, we hope to identify a common part of the protein that could be used to design a vaccine not only for Plasmodium vivax but potentially for both vivax and falciparum.”
“These two species of malaria are responsible for the majority of malaria infections worldwide, so a vaccine that targets both would be a critical addition to our arsenal.”
Dr Tham said there is growing evidence that developing better treatments or preventive strategies for P vivax malaria is imperative for malaria eradication.
“Not only is P vivax the most widespread species of malaria, it is also more difficult to treat because it can hide in the liver for long periods of time without symptoms,” she said. “In addition, studies show that effective treatment of falciparum malaria tends to be accompanied by a resurgence of P vivax, so it is critical to continue looking for better ways to manage this species.” ![]()
Blood collection set gets FDA clearance, CE mark

Photo by Graham Colm
A new blood collection set has received 510(k) clearance from the US Food and Drug Administration as well as the CE mark, which means it can be marketed within the European Economic Area.
The BD Vacutainer® UltraTouch™ Push Button Blood Collection Set is engineered to minimize patient discomfort during blood collection.
The set uses proprietary needle technology—Pentapoint™ Comfort and RightGauge™ Ultra-Thin Wall technology.
According to the manufacturer, BD, this technology can reduce penetration forces without compromising tube fill times or sample quality.
Research has shown that PentaPoint™ Comfort 5-bevel needle technology helps reduce the chance of a painful injection by creating a flatter, thinner surface to help penetrate the skin with significantly greater ease.1
When combined with RightGauge™ technology, which increases the needle’s inner diameter and enables clinicians to select a smaller gauge needle without sacrificing sample quality and blood flow, the BD Vacutainer® UltraTouch™ Push Button Blood Collection Set has been shown to reduce penetration forces by up to 32% when compared to another blood collection set.2
“The ability to use smaller gauge needles should also help clinicians access veins more successfully,” said Ana K. Stankovic, MD, PhD, worldwide vice president of Medical Affairs for BD Life Sciences – Preanalytical Systems and Global Health.
“This could prove especially valuable in patient populations—such as oncology, geriatric, and pediatric—that often have difficult or fragile veins.”
Dr Stankovic also noted that clinicians may be reluctant to use smaller gauge needles for fear of increasing hemolysis as the blood passes slowly through the narrow cannula.
“With BD Vacutainer® UltraTouch™ Push Button Blood Collection Sets, clinicians can select the gauge that is most appropriate for their patients, without compromising sample quality, testing accuracy, and their own efficiency,” she said. ![]()
1. Hirsch LJ, et al. Journal of Diabetes Science and Technology. 2012, 6(2):328-35.
2. 2015 BD bench testing versus BD Vacutainer® Push Button Blood Collection Sets.

Photo by Graham Colm
A new blood collection set has received 510(k) clearance from the US Food and Drug Administration as well as the CE mark, which means it can be marketed within the European Economic Area.
The BD Vacutainer® UltraTouch™ Push Button Blood Collection Set is engineered to minimize patient discomfort during blood collection.
The set uses proprietary needle technology—Pentapoint™ Comfort and RightGauge™ Ultra-Thin Wall technology.
According to the manufacturer, BD, this technology can reduce penetration forces without compromising tube fill times or sample quality.
Research has shown that PentaPoint™ Comfort 5-bevel needle technology helps reduce the chance of a painful injection by creating a flatter, thinner surface to help penetrate the skin with significantly greater ease.1
When combined with RightGauge™ technology, which increases the needle’s inner diameter and enables clinicians to select a smaller gauge needle without sacrificing sample quality and blood flow, the BD Vacutainer® UltraTouch™ Push Button Blood Collection Set has been shown to reduce penetration forces by up to 32% when compared to another blood collection set.2
“The ability to use smaller gauge needles should also help clinicians access veins more successfully,” said Ana K. Stankovic, MD, PhD, worldwide vice president of Medical Affairs for BD Life Sciences – Preanalytical Systems and Global Health.
“This could prove especially valuable in patient populations—such as oncology, geriatric, and pediatric—that often have difficult or fragile veins.”
Dr Stankovic also noted that clinicians may be reluctant to use smaller gauge needles for fear of increasing hemolysis as the blood passes slowly through the narrow cannula.
“With BD Vacutainer® UltraTouch™ Push Button Blood Collection Sets, clinicians can select the gauge that is most appropriate for their patients, without compromising sample quality, testing accuracy, and their own efficiency,” she said. ![]()
1. Hirsch LJ, et al. Journal of Diabetes Science and Technology. 2012, 6(2):328-35.
2. 2015 BD bench testing versus BD Vacutainer® Push Button Blood Collection Sets.

Photo by Graham Colm
A new blood collection set has received 510(k) clearance from the US Food and Drug Administration as well as the CE mark, which means it can be marketed within the European Economic Area.
The BD Vacutainer® UltraTouch™ Push Button Blood Collection Set is engineered to minimize patient discomfort during blood collection.
The set uses proprietary needle technology—Pentapoint™ Comfort and RightGauge™ Ultra-Thin Wall technology.
According to the manufacturer, BD, this technology can reduce penetration forces without compromising tube fill times or sample quality.
Research has shown that PentaPoint™ Comfort 5-bevel needle technology helps reduce the chance of a painful injection by creating a flatter, thinner surface to help penetrate the skin with significantly greater ease.1
When combined with RightGauge™ technology, which increases the needle’s inner diameter and enables clinicians to select a smaller gauge needle without sacrificing sample quality and blood flow, the BD Vacutainer® UltraTouch™ Push Button Blood Collection Set has been shown to reduce penetration forces by up to 32% when compared to another blood collection set.2
“The ability to use smaller gauge needles should also help clinicians access veins more successfully,” said Ana K. Stankovic, MD, PhD, worldwide vice president of Medical Affairs for BD Life Sciences – Preanalytical Systems and Global Health.
“This could prove especially valuable in patient populations—such as oncology, geriatric, and pediatric—that often have difficult or fragile veins.”
Dr Stankovic also noted that clinicians may be reluctant to use smaller gauge needles for fear of increasing hemolysis as the blood passes slowly through the narrow cannula.
“With BD Vacutainer® UltraTouch™ Push Button Blood Collection Sets, clinicians can select the gauge that is most appropriate for their patients, without compromising sample quality, testing accuracy, and their own efficiency,” she said. ![]()
1. Hirsch LJ, et al. Journal of Diabetes Science and Technology. 2012, 6(2):328-35.
2. 2015 BD bench testing versus BD Vacutainer® Push Button Blood Collection Sets.
Risk of reproductive problems in male cancer survivors

A study of Norwegian men has revealed several factors that may help predict reproductive problems among males diagnosed with cancer before age 25.
Cancer type, age at diagnosis, and time period of diagnosis were all associated with the likelihood of paternity.
And although cancer survivors were less likely to reproduce and more likely to use assisted reproductive technology, their first offspring were no less healthy than the offspring of control subjects.
This research was published in the British Journal of Cancer.
The study began with all Norwegian men born between 1965 and 1985 (n=626,495). The researchers excluded men who emigrated or died before reaching fertile age, which left 2687 men who were diagnosed with cancer before age 25 and 607,668 cancer-free controls.
The most common cancers were testicular cancer (27%), CNS tumors (18%), lymphoma (15%), and leukemia (13%). Thirty percent of the cancer cases were diagnosed in childhood (0–14 years of age), 26% in adolescence (15–19 years), and 43% in young adulthood (20–24 years).
Nine percent (n=247) of cancer cases were diagnosed from 1965 through 1979, 50% (n=1346) from 1980 through 1994, and 41% (n=1094) from 1995 through 2007.
The cancer survivors were less likely to have children than controls, with a hazard ratio (HR) of 0.72.
The reduction in paternity was significant for survivors of leukemia (HR=0.78), lymphoma (HR=0.78), testicular cancer (HR=0.77), CNS tumors (HR=0.45), bone tumors (HR=0.69), sympathetic nervous system tumors (HR=0.50), and retinoblastoma (HR=0.52).
The reduction in paternity was also more pronounced for cancer patients diagnosed before 1995. The HR was 0.61 for those diagnosed from 1965 through 1979 and 0.66 for those diagnosed from 1980 through 1994.
Patients who were diagnosed before age 15 were less likely to reproduce as well, with an HR of 0.59.
“These finds are important for male cancer survivors, seeing as we can identify groups at risk of having reproduction problems,” said study author Maria Winther Gunnes, a PhD candidate at the University of Bergen in Norway.
Another finding was that male cancer survivors were more likely than controls to have pregnancies resulting from assisted reproductive technology. The relative risk was 3.32.
When assessed by cancer type, the relative risk was 2.29 for leukemia, 3.79 for lymphoma, 2.41 for CNS tumors, 5.71 for sympathetic nervous system tumors, 2.20 for renal tumors, 4.77 for bone tumors, 1.32 for soft tissue sarcomas, 3.70 for testicular cancer, 4.36 for thyroid carcinoma, and 0.45 for malignant melanoma.
There was no increased risk among the first offspring of cancer survivors for perinatal death, congenital malformations, being small for gestational age, low birth weight, or preterm birth.
“It is important to be able to assure young male cancer survivors that their illness and treatment will not have a negative impact on their own children,” Gunnes said. ![]()

A study of Norwegian men has revealed several factors that may help predict reproductive problems among males diagnosed with cancer before age 25.
Cancer type, age at diagnosis, and time period of diagnosis were all associated with the likelihood of paternity.
And although cancer survivors were less likely to reproduce and more likely to use assisted reproductive technology, their first offspring were no less healthy than the offspring of control subjects.
This research was published in the British Journal of Cancer.
The study began with all Norwegian men born between 1965 and 1985 (n=626,495). The researchers excluded men who emigrated or died before reaching fertile age, which left 2687 men who were diagnosed with cancer before age 25 and 607,668 cancer-free controls.
The most common cancers were testicular cancer (27%), CNS tumors (18%), lymphoma (15%), and leukemia (13%). Thirty percent of the cancer cases were diagnosed in childhood (0–14 years of age), 26% in adolescence (15–19 years), and 43% in young adulthood (20–24 years).
Nine percent (n=247) of cancer cases were diagnosed from 1965 through 1979, 50% (n=1346) from 1980 through 1994, and 41% (n=1094) from 1995 through 2007.
The cancer survivors were less likely to have children than controls, with a hazard ratio (HR) of 0.72.
The reduction in paternity was significant for survivors of leukemia (HR=0.78), lymphoma (HR=0.78), testicular cancer (HR=0.77), CNS tumors (HR=0.45), bone tumors (HR=0.69), sympathetic nervous system tumors (HR=0.50), and retinoblastoma (HR=0.52).
The reduction in paternity was also more pronounced for cancer patients diagnosed before 1995. The HR was 0.61 for those diagnosed from 1965 through 1979 and 0.66 for those diagnosed from 1980 through 1994.
Patients who were diagnosed before age 15 were less likely to reproduce as well, with an HR of 0.59.
“These finds are important for male cancer survivors, seeing as we can identify groups at risk of having reproduction problems,” said study author Maria Winther Gunnes, a PhD candidate at the University of Bergen in Norway.
Another finding was that male cancer survivors were more likely than controls to have pregnancies resulting from assisted reproductive technology. The relative risk was 3.32.
When assessed by cancer type, the relative risk was 2.29 for leukemia, 3.79 for lymphoma, 2.41 for CNS tumors, 5.71 for sympathetic nervous system tumors, 2.20 for renal tumors, 4.77 for bone tumors, 1.32 for soft tissue sarcomas, 3.70 for testicular cancer, 4.36 for thyroid carcinoma, and 0.45 for malignant melanoma.
There was no increased risk among the first offspring of cancer survivors for perinatal death, congenital malformations, being small for gestational age, low birth weight, or preterm birth.
“It is important to be able to assure young male cancer survivors that their illness and treatment will not have a negative impact on their own children,” Gunnes said. ![]()

A study of Norwegian men has revealed several factors that may help predict reproductive problems among males diagnosed with cancer before age 25.
Cancer type, age at diagnosis, and time period of diagnosis were all associated with the likelihood of paternity.
And although cancer survivors were less likely to reproduce and more likely to use assisted reproductive technology, their first offspring were no less healthy than the offspring of control subjects.
This research was published in the British Journal of Cancer.
The study began with all Norwegian men born between 1965 and 1985 (n=626,495). The researchers excluded men who emigrated or died before reaching fertile age, which left 2687 men who were diagnosed with cancer before age 25 and 607,668 cancer-free controls.
The most common cancers were testicular cancer (27%), CNS tumors (18%), lymphoma (15%), and leukemia (13%). Thirty percent of the cancer cases were diagnosed in childhood (0–14 years of age), 26% in adolescence (15–19 years), and 43% in young adulthood (20–24 years).
Nine percent (n=247) of cancer cases were diagnosed from 1965 through 1979, 50% (n=1346) from 1980 through 1994, and 41% (n=1094) from 1995 through 2007.
The cancer survivors were less likely to have children than controls, with a hazard ratio (HR) of 0.72.
The reduction in paternity was significant for survivors of leukemia (HR=0.78), lymphoma (HR=0.78), testicular cancer (HR=0.77), CNS tumors (HR=0.45), bone tumors (HR=0.69), sympathetic nervous system tumors (HR=0.50), and retinoblastoma (HR=0.52).
The reduction in paternity was also more pronounced for cancer patients diagnosed before 1995. The HR was 0.61 for those diagnosed from 1965 through 1979 and 0.66 for those diagnosed from 1980 through 1994.
Patients who were diagnosed before age 15 were less likely to reproduce as well, with an HR of 0.59.
“These finds are important for male cancer survivors, seeing as we can identify groups at risk of having reproduction problems,” said study author Maria Winther Gunnes, a PhD candidate at the University of Bergen in Norway.
Another finding was that male cancer survivors were more likely than controls to have pregnancies resulting from assisted reproductive technology. The relative risk was 3.32.
When assessed by cancer type, the relative risk was 2.29 for leukemia, 3.79 for lymphoma, 2.41 for CNS tumors, 5.71 for sympathetic nervous system tumors, 2.20 for renal tumors, 4.77 for bone tumors, 1.32 for soft tissue sarcomas, 3.70 for testicular cancer, 4.36 for thyroid carcinoma, and 0.45 for malignant melanoma.
There was no increased risk among the first offspring of cancer survivors for perinatal death, congenital malformations, being small for gestational age, low birth weight, or preterm birth.
“It is important to be able to assure young male cancer survivors that their illness and treatment will not have a negative impact on their own children,” Gunnes said. ![]()
Study: Academic centers fail to report trial results

Photo by Daniel Sone
A study published in The BMJ indicates that leading US academic medical centers often fail to report clinical trial results in a timely manner, despite ethical obligations and even statutory requirements to do so.
Of the more than 4000 clinical trials studied, 67% had results disseminated at some point after trial completion, 29% were published within 2 years of completion, and 13% had results posted on ClinicalTrials.gov within 2 years of completion.
Harlan Krumholz, MD, of Yale School of Medicine in New Haven, Connecticut, and his colleagues conducted this study.
They evaluated 4347 registered trials conducted at 51 leading US academic institutions and completed between October 2007 and September 2010.
Overall, 67% of the trials (2892/4347) had been published or had results reported as of July 2014. Thirty-six percent (n=1560) had results disseminated within 2 years of trial completion.
Fifty-seven percent of trials (n=2458) had been published as of July 2014, and 29% (n=1245) were published within 2 years of completion.
Twenty-seven percent of trials (n=1166) had results reported on ClinicalTrials.gov as of July 2014, and 13% (n=547) had results reported within 2 years of completion.
There was marked variation in the dissemination of trial results across institutions. There was a more than 2-fold variation in the average time from study completion to dissemination of results and a more than 3-fold variation in the rate of dissemination across institutions.
Dr Krumholz and his colleagues noted that there are no repercussions to academic institutions or individual investigators for failing to report trial results, and there is no effective enforcement mechanism. ![]()

Photo by Daniel Sone
A study published in The BMJ indicates that leading US academic medical centers often fail to report clinical trial results in a timely manner, despite ethical obligations and even statutory requirements to do so.
Of the more than 4000 clinical trials studied, 67% had results disseminated at some point after trial completion, 29% were published within 2 years of completion, and 13% had results posted on ClinicalTrials.gov within 2 years of completion.
Harlan Krumholz, MD, of Yale School of Medicine in New Haven, Connecticut, and his colleagues conducted this study.
They evaluated 4347 registered trials conducted at 51 leading US academic institutions and completed between October 2007 and September 2010.
Overall, 67% of the trials (2892/4347) had been published or had results reported as of July 2014. Thirty-six percent (n=1560) had results disseminated within 2 years of trial completion.
Fifty-seven percent of trials (n=2458) had been published as of July 2014, and 29% (n=1245) were published within 2 years of completion.
Twenty-seven percent of trials (n=1166) had results reported on ClinicalTrials.gov as of July 2014, and 13% (n=547) had results reported within 2 years of completion.
There was marked variation in the dissemination of trial results across institutions. There was a more than 2-fold variation in the average time from study completion to dissemination of results and a more than 3-fold variation in the rate of dissemination across institutions.
Dr Krumholz and his colleagues noted that there are no repercussions to academic institutions or individual investigators for failing to report trial results, and there is no effective enforcement mechanism. ![]()

Photo by Daniel Sone
A study published in The BMJ indicates that leading US academic medical centers often fail to report clinical trial results in a timely manner, despite ethical obligations and even statutory requirements to do so.
Of the more than 4000 clinical trials studied, 67% had results disseminated at some point after trial completion, 29% were published within 2 years of completion, and 13% had results posted on ClinicalTrials.gov within 2 years of completion.
Harlan Krumholz, MD, of Yale School of Medicine in New Haven, Connecticut, and his colleagues conducted this study.
They evaluated 4347 registered trials conducted at 51 leading US academic institutions and completed between October 2007 and September 2010.
Overall, 67% of the trials (2892/4347) had been published or had results reported as of July 2014. Thirty-six percent (n=1560) had results disseminated within 2 years of trial completion.
Fifty-seven percent of trials (n=2458) had been published as of July 2014, and 29% (n=1245) were published within 2 years of completion.
Twenty-seven percent of trials (n=1166) had results reported on ClinicalTrials.gov as of July 2014, and 13% (n=547) had results reported within 2 years of completion.
There was marked variation in the dissemination of trial results across institutions. There was a more than 2-fold variation in the average time from study completion to dissemination of results and a more than 3-fold variation in the rate of dissemination across institutions.
Dr Krumholz and his colleagues noted that there are no repercussions to academic institutions or individual investigators for failing to report trial results, and there is no effective enforcement mechanism.
NIH’s peer-review process is flawed, team says

Photo by Rhoda Baer
The peer-review process the National Institutes of Health (NIH) use to allocate government research funds to US scientists may work no better than distributing those dollars at random, according to a group of researchers.
The group said their findings, published in eLife, suggest that peer review is not necessarily funding the best science, and awarding grants by lottery might actually produce equally good, if not better, results.
“The NIH claims that they are funding the best grants by the best scientists,” said study author Arturo Casadevall, MD, PhD, of the Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland.
“While [our] data would argue that the NIH is funding a lot of very good science, they are also leaving a lot of very good science on the table. The government can’t afford to fund every good grant proposal, but the problems with the current system make it worse than awarding grants through a lottery.”
The researchers noted that the NIH rejects the majority of research grant proposals it receives. To decide which proposals to fund, the organization relies on expert panels whose members score each application. Funding decisions are made on the basis of these scores and the amount of available funds.
In recent years, the NIH has only funded those proposals ranked around the top 10%. The 2015 annual research budget for the NIH was $30.1 billion.
For their study, Dr Casadevall and his colleagues reanalyzed data on the 102,740 research project grants funded by the NIH from 1980 through 2008.
Another group of researchers previously collected the data. Their research, published in Science in 2015, suggested that peer review works, as the highest ranked research projects funded by the NIH earned the most citations.
For the current study, Dr Casadevall and his colleagues decided to look only at the top 20% of grants awarded. They found very little difference between the top-ranked projects and those projects ranked in the 20th percentile when it came to citations.
What the peer-review process can do, they determined, is discriminate between very good science and very bad science—that is, those in the top 20% versus those below the 50th percentile.
“We are not criticizing the peer reviewers,” said study author Ferric Fang, MD, of the University of Washington in Seattle.
“We are simply showing that there are limits to the ability of peer review to predict future productivity based on grant applications. This suggests that some of the resources and effort spent on ranking applications might be better spent elsewhere. While the average productivity of grants with better scores was somewhat higher, the differences were extremely small, raising questions as to whether the effort is worthwhile.”
The researchers noted that peer review isn’t cheap. The annual budget of the NIH Center for Scientific Review is $110 million. Individual NIH institutes and centers also spend money on peer review. The team said that money could be used toward more grants.
They also noted that peer review allows for substantial subjectivity. The objection of a single member of the committee can effectively kill a grant proposal, whether that objection is legitimate or not.
“When people’s opinions count a lot, we may be doing worse than choosing at random,” Dr Casadevall said. “A negative word at the table can often swing the debate. And this is how we allocate research funding in this country.”
However, Dr Casadevall and his colleagues do not recommend abandoning the peer-review process completely. They believe a way to improve the system might be to continue using peer review to identify the top proposals but then place those proposals into a lottery, with grants awarded at random.

Photo by Rhoda Baer
The peer-review process the National Institutes of Health (NIH) use to allocate government research funds to US scientists may work no better than distributing those dollars at random, according to a group of researchers.
The group said their findings, published in eLife, suggest that peer review is not necessarily funding the best science, and awarding grants by lottery might actually produce equally good, if not better, results.
“The NIH claims that they are funding the best grants by the best scientists,” said study author Arturo Casadevall, MD, PhD, of the Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland.
“While [our] data would argue that the NIH is funding a lot of very good science, they are also leaving a lot of very good science on the table. The government can’t afford to fund every good grant proposal, but the problems with the current system make it worse than awarding grants through a lottery.”
The researchers noted that the NIH rejects the majority of research grant proposals it receives. To decide which proposals to fund, the organization relies on expert panels whose members score each application. Funding decisions are made on the basis of these scores and the amount of available funds.
In recent years, the NIH has only funded those proposals ranked around the top 10%. The 2015 annual research budget for the NIH was $30.1 billion.
For their study, Dr Casadevall and his colleagues reanalyzed data on the 102,740 research project grants funded by the NIH from 1980 through 2008.
Another group of researchers previously collected the data. Their research, published in Science in 2015, suggested that peer review works, as the highest ranked research projects funded by the NIH earned the most citations.
For the current study, Dr Casadevall and his colleagues decided to look only at the top 20% of grants awarded. They found very little difference between the top-ranked projects and those projects ranked in the 20th percentile when it came to citations.
What the peer-review process can do, they determined, is discriminate between very good science and very bad science—that is, those in the top 20% versus those below the 50th percentile.
“We are not criticizing the peer reviewers,” said study author Ferric Fang, MD, of the University of Washington in Seattle.
“We are simply showing that there are limits to the ability of peer review to predict future productivity based on grant applications. This suggests that some of the resources and effort spent on ranking applications might be better spent elsewhere. While the average productivity of grants with better scores was somewhat higher, the differences were extremely small, raising questions as to whether the effort is worthwhile.”
The researchers noted that peer review isn’t cheap. The annual budget of the NIH Center for Scientific Review is $110 million. Individual NIH institutes and centers also spend money on peer review. The team said that money could be used toward more grants.
They also noted that peer review allows for substantial subjectivity. The objection of a single member of the committee can effectively kill a grant proposal, whether that objection is legitimate or not.
“When people’s opinions count a lot, we may be doing worse than choosing at random,” Dr Casadevall said. “A negative word at the table can often swing the debate. And this is how we allocate research funding in this country.”
However, Dr Casadevall and his colleagues do not recommend abandoning the peer-review process completely. They believe a way to improve the system might be to continue using peer review to identify the top proposals but then place those proposals into a lottery, with grants awarded at random.

Photo by Rhoda Baer
The peer-review process the National Institutes of Health (NIH) use to allocate government research funds to US scientists may work no better than distributing those dollars at random, according to a group of researchers.
The group said their findings, published in eLife, suggest that peer review is not necessarily funding the best science, and awarding grants by lottery might actually produce equally good, if not better, results.
“The NIH claims that they are funding the best grants by the best scientists,” said study author Arturo Casadevall, MD, PhD, of the Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland.
“While [our] data would argue that the NIH is funding a lot of very good science, they are also leaving a lot of very good science on the table. The government can’t afford to fund every good grant proposal, but the problems with the current system make it worse than awarding grants through a lottery.”
The researchers noted that the NIH rejects the majority of research grant proposals it receives. To decide which proposals to fund, the organization relies on expert panels whose members score each application. Funding decisions are made on the basis of these scores and the amount of available funds.
In recent years, the NIH has only funded those proposals ranked around the top 10%. The 2015 annual research budget for the NIH was $30.1 billion.
For their study, Dr Casadevall and his colleagues reanalyzed data on the 102,740 research project grants funded by the NIH from 1980 through 2008.
Another group of researchers previously collected the data. Their research, published in Science in 2015, suggested that peer review works, as the highest ranked research projects funded by the NIH earned the most citations.
For the current study, Dr Casadevall and his colleagues decided to look only at the top 20% of grants awarded. They found very little difference between the top-ranked projects and those projects ranked in the 20th percentile when it came to citations.
What the peer-review process can do, they determined, is discriminate between very good science and very bad science—that is, those in the top 20% versus those below the 50th percentile.
“We are not criticizing the peer reviewers,” said study author Ferric Fang, MD, of the University of Washington in Seattle.
“We are simply showing that there are limits to the ability of peer review to predict future productivity based on grant applications. This suggests that some of the resources and effort spent on ranking applications might be better spent elsewhere. While the average productivity of grants with better scores was somewhat higher, the differences were extremely small, raising questions as to whether the effort is worthwhile.”
The researchers noted that peer review isn’t cheap. The annual budget of the NIH Center for Scientific Review is $110 million. Individual NIH institutes and centers also spend money on peer review. The team said that money could be used toward more grants.
They also noted that peer review allows for substantial subjectivity. The objection of a single member of the committee can effectively kill a grant proposal, whether that objection is legitimate or not.
“When people’s opinions count a lot, we may be doing worse than choosing at random,” Dr Casadevall said. “A negative word at the table can often swing the debate. And this is how we allocate research funding in this country.”
However, Dr Casadevall and his colleagues do not recommend abandoning the peer-review process completely. They believe a way to improve the system might be to continue using peer review to identify the top proposals but then place those proposals into a lottery, with grants awarded at random.
NICE says it can’t recommend sepsis tests

Photo by Juan D. Alfonso
The National Institute for Health and Care Excellence (NICE) has said there is not enough evidence to recommend the routine use of 3 new tests to help identify the cause of sepsis.
The agency issued a final diagnostics guidance recommending further research on the tests—the LightCycler SeptiFast Test MGRADE (Roche Diagnostics), SepsiTest (Molzym Molecular Diagnostics), and IRIDICA BAC BSI assay (Abbott Laboratories).
All 3 tests analyze whole blood samples to identify bacterial and fungal DNA. The tests aim to identify the causes of infection much quicker than traditional microbiology techniques, which require blood samples to be incubated and cultured before pathogens can be identified.
“Rapid molecular tests that can identify the cause of an infection in hours rather than the days typically needed for traditional microbiology tests could ensure the most appropriate antibiotics are used much earlier,” said Carole Longson, NICE Health Technology Evaluation Centre Director.
“This, in turn, could improve outcomes for patients with suspected bloodstream infections, as well as help to reduce the spread of resistant microbes. The independent diagnostics advisory committee [advising NICE on the tests] concluded that, although the tests show promise, there is currently not enough evidence to recommend their routine adoption in the NHS [National Health Service].”
“They felt the tests may offer clinical benefit by providing results more quickly, but there was currently too much uncertainty in their accuracy for clinicians to be able to use them as the basis for clinical decision-making in people with suspected bloodstream infections, who can be acutely unwell.”
“The committee therefore decided that further research should be encouraged to provide robust evidence, particularly around demonstrating the value of using the test results in clinical decision-making.”
The diagnostics guidance on the tests is available on the NICE website.

Photo by Juan D. Alfonso
The National Institute for Health and Care Excellence (NICE) has said there is not enough evidence to recommend the routine use of 3 new tests to help identify the cause of sepsis.
The agency issued a final diagnostics guidance recommending further research on the tests—the LightCycler SeptiFast Test MGRADE (Roche Diagnostics), SepsiTest (Molzym Molecular Diagnostics), and IRIDICA BAC BSI assay (Abbott Laboratories).
All 3 tests analyze whole blood samples to identify bacterial and fungal DNA. The tests aim to identify the causes of infection much quicker than traditional microbiology techniques, which require blood samples to be incubated and cultured before pathogens can be identified.
“Rapid molecular tests that can identify the cause of an infection in hours rather than the days typically needed for traditional microbiology tests could ensure the most appropriate antibiotics are used much earlier,” said Carole Longson, NICE Health Technology Evaluation Centre Director.
“This, in turn, could improve outcomes for patients with suspected bloodstream infections, as well as help to reduce the spread of resistant microbes. The independent diagnostics advisory committee [advising NICE on the tests] concluded that, although the tests show promise, there is currently not enough evidence to recommend their routine adoption in the NHS [National Health Service].”
“They felt the tests may offer clinical benefit by providing results more quickly, but there was currently too much uncertainty in their accuracy for clinicians to be able to use them as the basis for clinical decision-making in people with suspected bloodstream infections, who can be acutely unwell.”
“The committee therefore decided that further research should be encouraged to provide robust evidence, particularly around demonstrating the value of using the test results in clinical decision-making.”
The diagnostics guidance on the tests is available on the NICE website.

Photo by Juan D. Alfonso
The National Institute for Health and Care Excellence (NICE) has said there is not enough evidence to recommend the routine use of 3 new tests to help identify the cause of sepsis.
The agency issued a final diagnostics guidance recommending further research on the tests—the LightCycler SeptiFast Test MGRADE (Roche Diagnostics), SepsiTest (Molzym Molecular Diagnostics), and IRIDICA BAC BSI assay (Abbott Laboratories).
All 3 tests analyze whole blood samples to identify bacterial and fungal DNA. The tests aim to identify the causes of infection much quicker than traditional microbiology techniques, which require blood samples to be incubated and cultured before pathogens can be identified.
“Rapid molecular tests that can identify the cause of an infection in hours rather than the days typically needed for traditional microbiology tests could ensure the most appropriate antibiotics are used much earlier,” said Carole Longson, NICE Health Technology Evaluation Centre Director.
“This, in turn, could improve outcomes for patients with suspected bloodstream infections, as well as help to reduce the spread of resistant microbes. The independent diagnostics advisory committee [advising NICE on the tests] concluded that, although the tests show promise, there is currently not enough evidence to recommend their routine adoption in the NHS [National Health Service].”
“They felt the tests may offer clinical benefit by providing results more quickly, but there was currently too much uncertainty in their accuracy for clinicians to be able to use them as the basis for clinical decision-making in people with suspected bloodstream infections, who can be acutely unwell.”
“The committee therefore decided that further research should be encouraged to provide robust evidence, particularly around demonstrating the value of using the test results in clinical decision-making.”
The diagnostics guidance on the tests is available on the NICE website.
Team finds potential marker of long-term HSCs

in the bone marrow
Nearly 30 years after the discovery of the hematopoietic stem cell (HSC), researchers believe they have found a marker specific to long-term HSCs—the gene Hoxb5.
If confirmed, this finding would help settle long-standing debates about the identity of long-term HSCs and their support cells.
It may also pave the way for understanding how long-term HSCs maintain themselves and provide scientists with the necessary information to grow HSCs in the lab.
Irving Weissman, MD, of Stanford University School of Medicine in California, and his colleagues described this work in a letter to Nature.
In 1988, Dr Weissman and his colleagues isolated the HSC. Since that time, researchers have had mixed success in their attempts to get a detailed picture of how HSCs maintain themselves and grow in the body.
Over the years, it became clear why. HSCs come in 2 forms—short-term HSCs that lose their powers of replication over time and long-term HSCs that can replicate indefinitely.
With the new study, Dr Weissman and his colleagues believe they have found a reliable way to tell the difference between long-term and short-term HSCs. Namely, the presence of Hoxb5.
“In this paper, we have found a single marker that, in the entire bone marrow, is only found in these long-term stem cells,” Dr Weissman said.
The researchers hope this finding will enable them to look at how nearby cells create a niche where the long-term HSCs are supported and maintained.
“For nearly 30 years, people have been trying to grow HSCs outside the body and have not been able to do it; it’s arguably the ‘holy grail’ in this field,” said James Y. Chen, an MD/PhD candidate at Stanford University School of Medicine.
“Now that we have an anchor, a way to look at long-term HSCs, we can look at the cells around them to understand and, ideally, recreate the niche.”
An extensive search
Over the years, scientists have proposed various markers that they felt were unique to long-term HSCs, but the reliability of each proposed marker has been heatedly debated by other research groups, said Masanori Miyanishi, MD, PhD, also of Stanford University School of Medicine.
In an attempt to settle the issue, Chen and Dr Miyanishi examined a list of more than 100 genes that are expressed in the bone marrow and seemed like good candidates to be unique markers of long-term HSCs.
The researchers eliminated genes that are turned on in areas of the bone that don’t involve the creation of new blood and immune cells. That narrowed the field to 45 genes.
The team then performed an analysis to determine how much protein these genes were making in various cells. They found that only 3 proteins were produced at a high enough level to mark HSCs.
Finally, the researchers needed to find if 1 of these 3 was turned on in long-term HSCs and turned off in short-term HSCs.
Although they couldn’t yet identify which cells were long-term HSCs, the team knew that any collection of HSCs should have both long-term and short-term HSCs, so they expected to find the candidate gene turned off in some cells and on in others. Only 1 gene fit that bill—Hoxb5.
The researchers pointed out that there may be other unique markers of long-term HSCs, such as genes that weren’t among the initial group of genes screened. But among the screened genes, only Hoxb5 was a unique identifier of the long-term HSC.
Finding the niche
The researchers were also able to solve another mystery by showing where in the bone marrow long-term HSCs reside.
Satoshi Yamazaki, PhD, and Hiromitsu Nakauchi, MD, PhD, both from the University of Tokyo in Japan, used new technology to prepare bone marrow tissue and do computational analyses that validated the location and architecture of the HSC niche.
“More than 90% of these cells reside on a particular type of blood vessel called venous sinusoids,” Dr Nakauchi said.
The researchers believe the ability to identify long-term HSCs will give scientists a powerful tool for further study.
“This opens the way to observe long-term HSCs and other cells in the niche as they exist in the body, without transplanting them,” Dr Weissman said. “This is how science works, by getting down to the purest irreducible element—in this case, blood stem cells—in order to develop new tools and understandings.”

in the bone marrow
Nearly 30 years after the discovery of the hematopoietic stem cell (HSC), researchers believe they have found a marker specific to long-term HSCs—the gene Hoxb5.
If confirmed, this finding would help settle long-standing debates about the identity of long-term HSCs and their support cells.
It may also pave the way for understanding how long-term HSCs maintain themselves and provide scientists with the necessary information to grow HSCs in the lab.
Irving Weissman, MD, of Stanford University School of Medicine in California, and his colleagues described this work in a letter to Nature.
In 1988, Dr Weissman and his colleagues isolated the HSC. Since that time, researchers have had mixed success in their attempts to get a detailed picture of how HSCs maintain themselves and grow in the body.
Over the years, it became clear why. HSCs come in 2 forms—short-term HSCs that lose their powers of replication over time and long-term HSCs that can replicate indefinitely.
With the new study, Dr Weissman and his colleagues believe they have found a reliable way to tell the difference between long-term and short-term HSCs. Namely, the presence of Hoxb5.
“In this paper, we have found a single marker that, in the entire bone marrow, is only found in these long-term stem cells,” Dr Weissman said.
The researchers hope this finding will enable them to look at how nearby cells create a niche where the long-term HSCs are supported and maintained.
“For nearly 30 years, people have been trying to grow HSCs outside the body and have not been able to do it; it’s arguably the ‘holy grail’ in this field,” said James Y. Chen, an MD/PhD candidate at Stanford University School of Medicine.
“Now that we have an anchor, a way to look at long-term HSCs, we can look at the cells around them to understand and, ideally, recreate the niche.”
An extensive search
Over the years, scientists have proposed various markers that they felt were unique to long-term HSCs, but the reliability of each proposed marker has been heatedly debated by other research groups, said Masanori Miyanishi, MD, PhD, also of Stanford University School of Medicine.
In an attempt to settle the issue, Chen and Dr Miyanishi examined a list of more than 100 genes that are expressed in the bone marrow and seemed like good candidates to be unique markers of long-term HSCs.
The researchers eliminated genes that are turned on in areas of the bone that don’t involve the creation of new blood and immune cells. That narrowed the field to 45 genes.
The team then performed an analysis to determine how much protein these genes were making in various cells. They found that only 3 proteins were produced at a high enough level to mark HSCs.
Finally, the researchers needed to find if 1 of these 3 was turned on in long-term HSCs and turned off in short-term HSCs.
Although they couldn’t yet identify which cells were long-term HSCs, the team knew that any collection of HSCs should have both long-term and short-term HSCs, so they expected to find the candidate gene turned off in some cells and on in others. Only 1 gene fit that bill—Hoxb5.
The researchers pointed out that there may be other unique markers of long-term HSCs, such as genes that weren’t among the initial group of genes screened. But among the screened genes, only Hoxb5 was a unique identifier of the long-term HSC.
Finding the niche
The researchers were also able to solve another mystery by showing where in the bone marrow long-term HSCs reside.
Satoshi Yamazaki, PhD, and Hiromitsu Nakauchi, MD, PhD, both from the University of Tokyo in Japan, used new technology to prepare bone marrow tissue and do computational analyses that validated the location and architecture of the HSC niche.
“More than 90% of these cells reside on a particular type of blood vessel called venous sinusoids,” Dr Nakauchi said.
The researchers believe the ability to identify long-term HSCs will give scientists a powerful tool for further study.
“This opens the way to observe long-term HSCs and other cells in the niche as they exist in the body, without transplanting them,” Dr Weissman said. “This is how science works, by getting down to the purest irreducible element—in this case, blood stem cells—in order to develop new tools and understandings.”

in the bone marrow
Nearly 30 years after the discovery of the hematopoietic stem cell (HSC), researchers believe they have found a marker specific to long-term HSCs—the gene Hoxb5.
If confirmed, this finding would help settle long-standing debates about the identity of long-term HSCs and their support cells.
It may also pave the way for understanding how long-term HSCs maintain themselves and provide scientists with the necessary information to grow HSCs in the lab.
Irving Weissman, MD, of Stanford University School of Medicine in California, and his colleagues described this work in a letter to Nature.
In 1988, Dr Weissman and his colleagues isolated the HSC. Since that time, researchers have had mixed success in their attempts to get a detailed picture of how HSCs maintain themselves and grow in the body.
Over the years, it became clear why. HSCs come in 2 forms—short-term HSCs that lose their powers of replication over time and long-term HSCs that can replicate indefinitely.
With the new study, Dr Weissman and his colleagues believe they have found a reliable way to tell the difference between long-term and short-term HSCs. Namely, the presence of Hoxb5.
“In this paper, we have found a single marker that, in the entire bone marrow, is only found in these long-term stem cells,” Dr Weissman said.
The researchers hope this finding will enable them to look at how nearby cells create a niche where the long-term HSCs are supported and maintained.
“For nearly 30 years, people have been trying to grow HSCs outside the body and have not been able to do it; it’s arguably the ‘holy grail’ in this field,” said James Y. Chen, an MD/PhD candidate at Stanford University School of Medicine.
“Now that we have an anchor, a way to look at long-term HSCs, we can look at the cells around them to understand and, ideally, recreate the niche.”
An extensive search
Over the years, scientists have proposed various markers that they felt were unique to long-term HSCs, but the reliability of each proposed marker has been heatedly debated by other research groups, said Masanori Miyanishi, MD, PhD, also of Stanford University School of Medicine.
In an attempt to settle the issue, Chen and Dr Miyanishi examined a list of more than 100 genes that are expressed in the bone marrow and seemed like good candidates to be unique markers of long-term HSCs.
The researchers eliminated genes that are turned on in areas of the bone that don’t involve the creation of new blood and immune cells. That narrowed the field to 45 genes.
The team then performed an analysis to determine how much protein these genes were making in various cells. They found that only 3 proteins were produced at a high enough level to mark HSCs.
Finally, the researchers needed to find if 1 of these 3 was turned on in long-term HSCs and turned off in short-term HSCs.
Although they couldn’t yet identify which cells were long-term HSCs, the team knew that any collection of HSCs should have both long-term and short-term HSCs, so they expected to find the candidate gene turned off in some cells and on in others. Only 1 gene fit that bill—Hoxb5.
The researchers pointed out that there may be other unique markers of long-term HSCs, such as genes that weren’t among the initial group of genes screened. But among the screened genes, only Hoxb5 was a unique identifier of the long-term HSC.
Finding the niche
The researchers were also able to solve another mystery by showing where in the bone marrow long-term HSCs reside.
Satoshi Yamazaki, PhD, and Hiromitsu Nakauchi, MD, PhD, both from the University of Tokyo in Japan, used new technology to prepare bone marrow tissue and do computational analyses that validated the location and architecture of the HSC niche.
“More than 90% of these cells reside on a particular type of blood vessel called venous sinusoids,” Dr Nakauchi said.
The researchers believe the ability to identify long-term HSCs will give scientists a powerful tool for further study.
“This opens the way to observe long-term HSCs and other cells in the niche as they exist in the body, without transplanting them,” Dr Weissman said. “This is how science works, by getting down to the purest irreducible element—in this case, blood stem cells—in order to develop new tools and understandings.”