User login
EHRs enhance clinical trial follow-up
Electronic health records (EHRs) can enhance results from randomized controlled trials (RCTs), according to research published in Scientific Reports.
Researchers found EHRs could be used to track trial participants, enabling long-term monitoring of medical interventions and health outcomes and providing new insights into population health.
“In this study, we reported on the feasibility and efficiency of electronic follow-up and compared it with traditional trial follow-up,” said study author Sue Jordan, PhD, MB BCh, of Swansea University in Swansea, UK.
“We gained new insights from outcomes electronically recorded 3 years after the end of the trial and could then identify the differences between trial data and electronic data.”
Dr Jordan and her colleagues followed up on RCT participants using EHRs in the Secure Anonymised Information Linkage (SAIL) databank at Swansea University Medical School.
In this RCT, investigators had assessed the impact of probiotics on asthma and eczema in children born from 2005 to 2007. The trial had 2 years of traditional fieldwork follow-up.
Dr Jordan and her colleagues compared field results to EHR results at 2 years in 93% of trial participants.
The researchers said EHRs improved retention of children from lower socio-economic groups, which helped reduce volunteer bias.
The team also performed electronic follow-up at 5 years, which provided the “first robust analysis of asthma endpoints.”
The researchers said the asthma endpoints are “generally more reliable” in the 5-year EHR data for 2 reasons. The first is that the children are older, and asthma typically appears after 2 years of age.
The second reason is that, with the fieldwork follow-up, parents or guardians may have mistakenly identified symptoms as asthma without a child actually having an asthma diagnosis.
“Trial data are vulnerable to misunderstandings of questionnaires or definitions of illness,” Dr Jordan noted.
She and her colleagues also pointed out that retention was still high (82%) and free of bias in socio-economic status with the 5-year EHR data.
“These results lead us to conclude that using electronic health records have benefits relating to the cost-effective, long-term monitoring of complex interventions, which could have a positive impact for future clinical trial design,” said study author Michael Gravenor, DPhil, of Swansea University.
Electronic health records (EHRs) can enhance results from randomized controlled trials (RCTs), according to research published in Scientific Reports.
Researchers found EHRs could be used to track trial participants, enabling long-term monitoring of medical interventions and health outcomes and providing new insights into population health.
“In this study, we reported on the feasibility and efficiency of electronic follow-up and compared it with traditional trial follow-up,” said study author Sue Jordan, PhD, MB BCh, of Swansea University in Swansea, UK.
“We gained new insights from outcomes electronically recorded 3 years after the end of the trial and could then identify the differences between trial data and electronic data.”
Dr Jordan and her colleagues followed up on RCT participants using EHRs in the Secure Anonymised Information Linkage (SAIL) databank at Swansea University Medical School.
In this RCT, investigators had assessed the impact of probiotics on asthma and eczema in children born from 2005 to 2007. The trial had 2 years of traditional fieldwork follow-up.
Dr Jordan and her colleagues compared field results to EHR results at 2 years in 93% of trial participants.
The researchers said EHRs improved retention of children from lower socio-economic groups, which helped reduce volunteer bias.
The team also performed electronic follow-up at 5 years, which provided the “first robust analysis of asthma endpoints.”
The researchers said the asthma endpoints are “generally more reliable” in the 5-year EHR data for 2 reasons. The first is that the children are older, and asthma typically appears after 2 years of age.
The second reason is that, with the fieldwork follow-up, parents or guardians may have mistakenly identified symptoms as asthma without a child actually having an asthma diagnosis.
“Trial data are vulnerable to misunderstandings of questionnaires or definitions of illness,” Dr Jordan noted.
She and her colleagues also pointed out that retention was still high (82%) and free of bias in socio-economic status with the 5-year EHR data.
“These results lead us to conclude that using electronic health records have benefits relating to the cost-effective, long-term monitoring of complex interventions, which could have a positive impact for future clinical trial design,” said study author Michael Gravenor, DPhil, of Swansea University.
Electronic health records (EHRs) can enhance results from randomized controlled trials (RCTs), according to research published in Scientific Reports.
Researchers found EHRs could be used to track trial participants, enabling long-term monitoring of medical interventions and health outcomes and providing new insights into population health.
“In this study, we reported on the feasibility and efficiency of electronic follow-up and compared it with traditional trial follow-up,” said study author Sue Jordan, PhD, MB BCh, of Swansea University in Swansea, UK.
“We gained new insights from outcomes electronically recorded 3 years after the end of the trial and could then identify the differences between trial data and electronic data.”
Dr Jordan and her colleagues followed up on RCT participants using EHRs in the Secure Anonymised Information Linkage (SAIL) databank at Swansea University Medical School.
In this RCT, investigators had assessed the impact of probiotics on asthma and eczema in children born from 2005 to 2007. The trial had 2 years of traditional fieldwork follow-up.
Dr Jordan and her colleagues compared field results to EHR results at 2 years in 93% of trial participants.
The researchers said EHRs improved retention of children from lower socio-economic groups, which helped reduce volunteer bias.
The team also performed electronic follow-up at 5 years, which provided the “first robust analysis of asthma endpoints.”
The researchers said the asthma endpoints are “generally more reliable” in the 5-year EHR data for 2 reasons. The first is that the children are older, and asthma typically appears after 2 years of age.
The second reason is that, with the fieldwork follow-up, parents or guardians may have mistakenly identified symptoms as asthma without a child actually having an asthma diagnosis.
“Trial data are vulnerable to misunderstandings of questionnaires or definitions of illness,” Dr Jordan noted.
She and her colleagues also pointed out that retention was still high (82%) and free of bias in socio-economic status with the 5-year EHR data.
“These results lead us to conclude that using electronic health records have benefits relating to the cost-effective, long-term monitoring of complex interventions, which could have a positive impact for future clinical trial design,” said study author Michael Gravenor, DPhil, of Swansea University.
Treating insomnia in cancer survivors
Treatment with acupuncture or cognitive behavioral therapy (CBT) can decrease the severity of insomnia among cancer survivors, according to new research.
Overall, improvements in insomnia were greatest in patients treated with CBT, and patients with mild insomnia at baseline had a significantly greater improvement with CBT than with acupuncture.
However, among patients who had moderate to severe insomnia at baseline, there was no significant difference in results with CBT and acupuncture.
Jun J. Mao, MD, of Memorial Sloan Kettering Cancer Center in New York, New York, presented these results in a press briefing in advance of the 2018 ASCO Annual Meeting.
Additional results are scheduled to be presented at the meeting as abstract 10001.
“Up to 60% of cancer survivors have some form of insomnia, but it is often underdiagnosed and undertreated,” Dr Mao said. “Our trial showed that both CBT-I [CBT for insomnia] and acupuncture were effective in treating moderate to severe insomnia, although CBT-I was more effective for those with mild symptoms of insomnia. Now, patients have more choices to manage their insomnia.”
Dr Mao and his colleagues studied 160 individuals who had completed cancer treatment. Their mean time since cancer diagnosis was about 6 years.
The subjects had received treatment for hematologic malignancies (8%) as well as breast (31%), prostate (23%), head and neck (7%), colorectal (6%), gynecological (4%), and other cancers (14%). Six percent of subjects had been treated for more than 1 type of cancer.
All subjects had been clinically diagnosed with insomnia. Seventy-nine percent had moderate (n=94) to severe (n=33) insomnia, and 21% had mild insomnia (n=33).
Interventions
Subjects were randomized to receive CBT or acupuncture for 8 weeks. Those who received CBT worked with a therapist to re-establish a restorative sleep schedule by:
- Reducing the amount of time spent in bed
- Limiting activities performed in bed to sleep and sexual activity
- Modifying unhelpful beliefs about sleep
- Promoting good sleep hygiene (setting a regular sleep schedule and avoiding activities that include light from tablets and cellphones, eating too late, and performing vigorous activities).
The study’s primary outcome was reduction in insomnia severity, as measured by the Insomnia Severity Index (ISI), from study entry to the end of treatment at week 8. Subjects were also reassessed at 20 weeks.
The ISI is a questionnaire that asks people to rate the severity of insomnia problems, such as difficulty falling asleep and staying asleep, and the impact of insomnia on their daily functioning and quality of life.
ISI scoring ranges from 0 to 28. Scores of 0 to 7 denote no clinically significant insomnia, 8 to 14 denote mild insomnia, 15 to 21 denote moderate insomnia, and 22 to 28 denote severe insomnia.
Results
At 8 weeks, the mean ISI score fell 10.9 points (from 18.5 to 7.5) for subjects who received CBT and 8.3 points (from 17.55 to 9.23) for those who received acupuncture (P=0.0007).
Among subjects with mild insomnia at baseline, far more responded to CBT than to acupuncture—85% and 18%, respectively (P<0.0001).
However, response rates were similar in subjects who had moderate to severe insomnia at baseline. Seventy-five percent of those who received CBT achieved a response, as did 66% of those who received acupuncture (P=0.26).
Both treatment groups had few mild adverse events, and all subjects maintained their improvements in insomnia at the 20-week assessment.
This study was funded by the Patient-Centered Outcomes Research Institute. The researchers’ disclosures are listed with the abstract.
Treatment with acupuncture or cognitive behavioral therapy (CBT) can decrease the severity of insomnia among cancer survivors, according to new research.
Overall, improvements in insomnia were greatest in patients treated with CBT, and patients with mild insomnia at baseline had a significantly greater improvement with CBT than with acupuncture.
However, among patients who had moderate to severe insomnia at baseline, there was no significant difference in results with CBT and acupuncture.
Jun J. Mao, MD, of Memorial Sloan Kettering Cancer Center in New York, New York, presented these results in a press briefing in advance of the 2018 ASCO Annual Meeting.
Additional results are scheduled to be presented at the meeting as abstract 10001.
“Up to 60% of cancer survivors have some form of insomnia, but it is often underdiagnosed and undertreated,” Dr Mao said. “Our trial showed that both CBT-I [CBT for insomnia] and acupuncture were effective in treating moderate to severe insomnia, although CBT-I was more effective for those with mild symptoms of insomnia. Now, patients have more choices to manage their insomnia.”
Dr Mao and his colleagues studied 160 individuals who had completed cancer treatment. Their mean time since cancer diagnosis was about 6 years.
The subjects had received treatment for hematologic malignancies (8%) as well as breast (31%), prostate (23%), head and neck (7%), colorectal (6%), gynecological (4%), and other cancers (14%). Six percent of subjects had been treated for more than 1 type of cancer.
All subjects had been clinically diagnosed with insomnia. Seventy-nine percent had moderate (n=94) to severe (n=33) insomnia, and 21% had mild insomnia (n=33).
Interventions
Subjects were randomized to receive CBT or acupuncture for 8 weeks. Those who received CBT worked with a therapist to re-establish a restorative sleep schedule by:
- Reducing the amount of time spent in bed
- Limiting activities performed in bed to sleep and sexual activity
- Modifying unhelpful beliefs about sleep
- Promoting good sleep hygiene (setting a regular sleep schedule and avoiding activities that include light from tablets and cellphones, eating too late, and performing vigorous activities).
The study’s primary outcome was reduction in insomnia severity, as measured by the Insomnia Severity Index (ISI), from study entry to the end of treatment at week 8. Subjects were also reassessed at 20 weeks.
The ISI is a questionnaire that asks people to rate the severity of insomnia problems, such as difficulty falling asleep and staying asleep, and the impact of insomnia on their daily functioning and quality of life.
ISI scoring ranges from 0 to 28. Scores of 0 to 7 denote no clinically significant insomnia, 8 to 14 denote mild insomnia, 15 to 21 denote moderate insomnia, and 22 to 28 denote severe insomnia.
Results
At 8 weeks, the mean ISI score fell 10.9 points (from 18.5 to 7.5) for subjects who received CBT and 8.3 points (from 17.55 to 9.23) for those who received acupuncture (P=0.0007).
Among subjects with mild insomnia at baseline, far more responded to CBT than to acupuncture—85% and 18%, respectively (P<0.0001).
However, response rates were similar in subjects who had moderate to severe insomnia at baseline. Seventy-five percent of those who received CBT achieved a response, as did 66% of those who received acupuncture (P=0.26).
Both treatment groups had few mild adverse events, and all subjects maintained their improvements in insomnia at the 20-week assessment.
This study was funded by the Patient-Centered Outcomes Research Institute. The researchers’ disclosures are listed with the abstract.
Treatment with acupuncture or cognitive behavioral therapy (CBT) can decrease the severity of insomnia among cancer survivors, according to new research.
Overall, improvements in insomnia were greatest in patients treated with CBT, and patients with mild insomnia at baseline had a significantly greater improvement with CBT than with acupuncture.
However, among patients who had moderate to severe insomnia at baseline, there was no significant difference in results with CBT and acupuncture.
Jun J. Mao, MD, of Memorial Sloan Kettering Cancer Center in New York, New York, presented these results in a press briefing in advance of the 2018 ASCO Annual Meeting.
Additional results are scheduled to be presented at the meeting as abstract 10001.
“Up to 60% of cancer survivors have some form of insomnia, but it is often underdiagnosed and undertreated,” Dr Mao said. “Our trial showed that both CBT-I [CBT for insomnia] and acupuncture were effective in treating moderate to severe insomnia, although CBT-I was more effective for those with mild symptoms of insomnia. Now, patients have more choices to manage their insomnia.”
Dr Mao and his colleagues studied 160 individuals who had completed cancer treatment. Their mean time since cancer diagnosis was about 6 years.
The subjects had received treatment for hematologic malignancies (8%) as well as breast (31%), prostate (23%), head and neck (7%), colorectal (6%), gynecological (4%), and other cancers (14%). Six percent of subjects had been treated for more than 1 type of cancer.
All subjects had been clinically diagnosed with insomnia. Seventy-nine percent had moderate (n=94) to severe (n=33) insomnia, and 21% had mild insomnia (n=33).
Interventions
Subjects were randomized to receive CBT or acupuncture for 8 weeks. Those who received CBT worked with a therapist to re-establish a restorative sleep schedule by:
- Reducing the amount of time spent in bed
- Limiting activities performed in bed to sleep and sexual activity
- Modifying unhelpful beliefs about sleep
- Promoting good sleep hygiene (setting a regular sleep schedule and avoiding activities that include light from tablets and cellphones, eating too late, and performing vigorous activities).
The study’s primary outcome was reduction in insomnia severity, as measured by the Insomnia Severity Index (ISI), from study entry to the end of treatment at week 8. Subjects were also reassessed at 20 weeks.
The ISI is a questionnaire that asks people to rate the severity of insomnia problems, such as difficulty falling asleep and staying asleep, and the impact of insomnia on their daily functioning and quality of life.
ISI scoring ranges from 0 to 28. Scores of 0 to 7 denote no clinically significant insomnia, 8 to 14 denote mild insomnia, 15 to 21 denote moderate insomnia, and 22 to 28 denote severe insomnia.
Results
At 8 weeks, the mean ISI score fell 10.9 points (from 18.5 to 7.5) for subjects who received CBT and 8.3 points (from 17.55 to 9.23) for those who received acupuncture (P=0.0007).
Among subjects with mild insomnia at baseline, far more responded to CBT than to acupuncture—85% and 18%, respectively (P<0.0001).
However, response rates were similar in subjects who had moderate to severe insomnia at baseline. Seventy-five percent of those who received CBT achieved a response, as did 66% of those who received acupuncture (P=0.26).
Both treatment groups had few mild adverse events, and all subjects maintained their improvements in insomnia at the 20-week assessment.
This study was funded by the Patient-Centered Outcomes Research Institute. The researchers’ disclosures are listed with the abstract.
Team analyzes skin odor to detect malaria
Changes in skin odor can reveal malaria infection in patients with no external symptoms, according to research published in PNAS.
Researchers examined chemical compounds released from the skin of Kenyan children and discovered characteristic patterns in these compounds that identified patients with acute and asymptomatic malaria infections.
“Our previous work in a mouse model found that malaria infection altered the odors of infected mice in ways that made them more attractive to mosquitoes, particularly at a stage of infection where the transmissible stage of the parasite was present at high levels,” said study author Consuelo De Moraes, PhD, of ETH Zurich in Switzerland.
“We also found long-term changes in the odor profiles of infected mice. [So] we had reason to hope that similar changes in human odors might provide biomarkers that could be used for diagnosis.”
To test this theory, Dr De Moraes and her colleagues studied more than 400 Kenyan school children. The researchers collected blood samples as well as samples of volatile substances released from the subjects’ skin.
The team used the blood samples to test for malaria, first via light microscopy and an SD Bioline Rapid Diagnostic Test, then using polymerase chain reaction (PCR) methods to confirm the initial results.
There were 330 subjects who were clearly positive or negative for malaria, and there were 66 subjects who were positive by PCR but negative by microscopy. The researchers compared these findings to results from the skin tests.
To assess the subjects’ skin, the researchers placed each child’s foot and arm into sealed Teflon bags and passed an air current over the skin for about 1 hour. The air was then channeled through special filters that collected the volatile compounds.
Using gas chromatography and mass spectrometry, the researchers then determined the identity and quantity of each compound to generate odor profiles for infected and uninfected children.
Further analysis of these profiles revealed volatile biomarkers that enabled the researchers to accurately identify whether a child was infected with the malaria parasite. Even for asymptomatic infections, the detection rate was close to 100%.
“This high detection rate was encouraging,” Dr De Moraes said. “Initially, we weren’t sure which chemical compounds we should be looking for.”
The researchers noted that malaria infection does not create new chemical compounds, but it alters the amounts of compounds that are already present in the odors of healthy people.
Odor profiles were different for malaria-infected and uninfected subjects, but profiles were also different for patients with acute and asymptomatic infections.
The researchers hope the biomarkers they identified could be used to develop a new tool for the early detection of malaria.
“These new volatile biomarkers are an important first step,” said Mark Mescher, of ETH Zurich. “Now, someone needs to develop an application that can be used cheaply and reliably in the field.”
“In the near-term, our goal is to refine the current findings to find the most reliable and effective biomarkers we can. There is still a lot more work to be done to develop a practical diagnostic assay.”
Changes in skin odor can reveal malaria infection in patients with no external symptoms, according to research published in PNAS.
Researchers examined chemical compounds released from the skin of Kenyan children and discovered characteristic patterns in these compounds that identified patients with acute and asymptomatic malaria infections.
“Our previous work in a mouse model found that malaria infection altered the odors of infected mice in ways that made them more attractive to mosquitoes, particularly at a stage of infection where the transmissible stage of the parasite was present at high levels,” said study author Consuelo De Moraes, PhD, of ETH Zurich in Switzerland.
“We also found long-term changes in the odor profiles of infected mice. [So] we had reason to hope that similar changes in human odors might provide biomarkers that could be used for diagnosis.”
To test this theory, Dr De Moraes and her colleagues studied more than 400 Kenyan school children. The researchers collected blood samples as well as samples of volatile substances released from the subjects’ skin.
The team used the blood samples to test for malaria, first via light microscopy and an SD Bioline Rapid Diagnostic Test, then using polymerase chain reaction (PCR) methods to confirm the initial results.
There were 330 subjects who were clearly positive or negative for malaria, and there were 66 subjects who were positive by PCR but negative by microscopy. The researchers compared these findings to results from the skin tests.
To assess the subjects’ skin, the researchers placed each child’s foot and arm into sealed Teflon bags and passed an air current over the skin for about 1 hour. The air was then channeled through special filters that collected the volatile compounds.
Using gas chromatography and mass spectrometry, the researchers then determined the identity and quantity of each compound to generate odor profiles for infected and uninfected children.
Further analysis of these profiles revealed volatile biomarkers that enabled the researchers to accurately identify whether a child was infected with the malaria parasite. Even for asymptomatic infections, the detection rate was close to 100%.
“This high detection rate was encouraging,” Dr De Moraes said. “Initially, we weren’t sure which chemical compounds we should be looking for.”
The researchers noted that malaria infection does not create new chemical compounds, but it alters the amounts of compounds that are already present in the odors of healthy people.
Odor profiles were different for malaria-infected and uninfected subjects, but profiles were also different for patients with acute and asymptomatic infections.
The researchers hope the biomarkers they identified could be used to develop a new tool for the early detection of malaria.
“These new volatile biomarkers are an important first step,” said Mark Mescher, of ETH Zurich. “Now, someone needs to develop an application that can be used cheaply and reliably in the field.”
“In the near-term, our goal is to refine the current findings to find the most reliable and effective biomarkers we can. There is still a lot more work to be done to develop a practical diagnostic assay.”
Changes in skin odor can reveal malaria infection in patients with no external symptoms, according to research published in PNAS.
Researchers examined chemical compounds released from the skin of Kenyan children and discovered characteristic patterns in these compounds that identified patients with acute and asymptomatic malaria infections.
“Our previous work in a mouse model found that malaria infection altered the odors of infected mice in ways that made them more attractive to mosquitoes, particularly at a stage of infection where the transmissible stage of the parasite was present at high levels,” said study author Consuelo De Moraes, PhD, of ETH Zurich in Switzerland.
“We also found long-term changes in the odor profiles of infected mice. [So] we had reason to hope that similar changes in human odors might provide biomarkers that could be used for diagnosis.”
To test this theory, Dr De Moraes and her colleagues studied more than 400 Kenyan school children. The researchers collected blood samples as well as samples of volatile substances released from the subjects’ skin.
The team used the blood samples to test for malaria, first via light microscopy and an SD Bioline Rapid Diagnostic Test, then using polymerase chain reaction (PCR) methods to confirm the initial results.
There were 330 subjects who were clearly positive or negative for malaria, and there were 66 subjects who were positive by PCR but negative by microscopy. The researchers compared these findings to results from the skin tests.
To assess the subjects’ skin, the researchers placed each child’s foot and arm into sealed Teflon bags and passed an air current over the skin for about 1 hour. The air was then channeled through special filters that collected the volatile compounds.
Using gas chromatography and mass spectrometry, the researchers then determined the identity and quantity of each compound to generate odor profiles for infected and uninfected children.
Further analysis of these profiles revealed volatile biomarkers that enabled the researchers to accurately identify whether a child was infected with the malaria parasite. Even for asymptomatic infections, the detection rate was close to 100%.
“This high detection rate was encouraging,” Dr De Moraes said. “Initially, we weren’t sure which chemical compounds we should be looking for.”
The researchers noted that malaria infection does not create new chemical compounds, but it alters the amounts of compounds that are already present in the odors of healthy people.
Odor profiles were different for malaria-infected and uninfected subjects, but profiles were also different for patients with acute and asymptomatic infections.
The researchers hope the biomarkers they identified could be used to develop a new tool for the early detection of malaria.
“These new volatile biomarkers are an important first step,” said Mark Mescher, of ETH Zurich. “Now, someone needs to develop an application that can be used cheaply and reliably in the field.”
“In the near-term, our goal is to refine the current findings to find the most reliable and effective biomarkers we can. There is still a lot more work to be done to develop a practical diagnostic assay.”
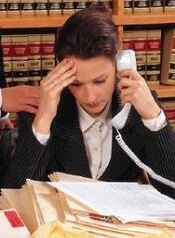
Study reveals gender imbalance in cancer research funding
A new study suggests male investigators in the UK receive more funding for cancer research than their female counterparts.
Researchers analyzed funding for more than 4000 studies and found that male primary investigators (PIs) were consistently awarded more funding.
The total investment value was 3.6 times greater for male PIs than for female PIs.
The mean award value was 1.6 times greater, and the median award value was 1.3 times greater for males.
Rifat Atun, MBBS, of Harvard T. H. Chan School of Public Health in Boston, Massachusetts, and his colleagues reported these findings in BMJ Open.
The researchers analyzed data on public and philanthropic cancer research funding awarded to UK institutions between 2000 and 2013.
From this data, the team identified 4186 eligible studies with a total investment value of £2.33 billion.
The researchers compared the total investment, number of awards, and mean and median award value between male and female PIs.
Male PIs were awarded 2890 (69%) grants with a total value of £1.8 billion (78%), while female PIs were awarded 1296 (31%) grants with a total value of £0.5 billion (22%).
The median award value was £252,647 (interquartile range, £127,343–£553,560) for men and £198,485 (interquartile range, £99,317–£382,650) for women.
The mean award value was £630,324 (standard deviation, £1,662,559) for men and £394,730 (standard deviation, £666,574) for women.
Dr Atun and his colleagues acknowledged that this study was dependent on the accuracy of original investment data from the funding bodies, and the team could not openly access data of private sector research funding nor obtain disaggregated data from Cancer Research UK, one of the largest funders of cancer research.
The researchers also noted that the gender discrepancies they observed “are likely multifactorial,” and the team was unable to “postulate the underlying mechanisms responsible.” Still, the data do suggest a “substantial” imbalance, which should be investigated.
A new study suggests male investigators in the UK receive more funding for cancer research than their female counterparts.
Researchers analyzed funding for more than 4000 studies and found that male primary investigators (PIs) were consistently awarded more funding.
The total investment value was 3.6 times greater for male PIs than for female PIs.
The mean award value was 1.6 times greater, and the median award value was 1.3 times greater for males.
Rifat Atun, MBBS, of Harvard T. H. Chan School of Public Health in Boston, Massachusetts, and his colleagues reported these findings in BMJ Open.
The researchers analyzed data on public and philanthropic cancer research funding awarded to UK institutions between 2000 and 2013.
From this data, the team identified 4186 eligible studies with a total investment value of £2.33 billion.
The researchers compared the total investment, number of awards, and mean and median award value between male and female PIs.
Male PIs were awarded 2890 (69%) grants with a total value of £1.8 billion (78%), while female PIs were awarded 1296 (31%) grants with a total value of £0.5 billion (22%).
The median award value was £252,647 (interquartile range, £127,343–£553,560) for men and £198,485 (interquartile range, £99,317–£382,650) for women.
The mean award value was £630,324 (standard deviation, £1,662,559) for men and £394,730 (standard deviation, £666,574) for women.
Dr Atun and his colleagues acknowledged that this study was dependent on the accuracy of original investment data from the funding bodies, and the team could not openly access data of private sector research funding nor obtain disaggregated data from Cancer Research UK, one of the largest funders of cancer research.
The researchers also noted that the gender discrepancies they observed “are likely multifactorial,” and the team was unable to “postulate the underlying mechanisms responsible.” Still, the data do suggest a “substantial” imbalance, which should be investigated.
A new study suggests male investigators in the UK receive more funding for cancer research than their female counterparts.
Researchers analyzed funding for more than 4000 studies and found that male primary investigators (PIs) were consistently awarded more funding.
The total investment value was 3.6 times greater for male PIs than for female PIs.
The mean award value was 1.6 times greater, and the median award value was 1.3 times greater for males.
Rifat Atun, MBBS, of Harvard T. H. Chan School of Public Health in Boston, Massachusetts, and his colleagues reported these findings in BMJ Open.
The researchers analyzed data on public and philanthropic cancer research funding awarded to UK institutions between 2000 and 2013.
From this data, the team identified 4186 eligible studies with a total investment value of £2.33 billion.
The researchers compared the total investment, number of awards, and mean and median award value between male and female PIs.
Male PIs were awarded 2890 (69%) grants with a total value of £1.8 billion (78%), while female PIs were awarded 1296 (31%) grants with a total value of £0.5 billion (22%).
The median award value was £252,647 (interquartile range, £127,343–£553,560) for men and £198,485 (interquartile range, £99,317–£382,650) for women.
The mean award value was £630,324 (standard deviation, £1,662,559) for men and £394,730 (standard deviation, £666,574) for women.
Dr Atun and his colleagues acknowledged that this study was dependent on the accuracy of original investment data from the funding bodies, and the team could not openly access data of private sector research funding nor obtain disaggregated data from Cancer Research UK, one of the largest funders of cancer research.
The researchers also noted that the gender discrepancies they observed “are likely multifactorial,” and the team was unable to “postulate the underlying mechanisms responsible.” Still, the data do suggest a “substantial” imbalance, which should be investigated.
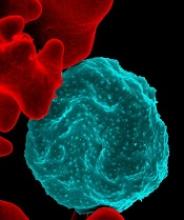
‘Essential’ genes could be targeted to treat malaria
More than 2000 genes are “essential” for the malaria parasite Plasmodium falciparum, according to research published in Science.
Researchers identified 2680 genes that appear necessary for growth and survival during P falciparum’s asexual blood stage.
The researchers therefore believe these genes could be viable therapeutic targets for P falciparum malaria.
“Malaria parasites are extremely technically difficult to manipulate and sequence, and, until this study, only a few of P falciparum’s essential genes had been determined,” said study author Iraad Bronner, of the Wellcome Sanger Institute in Hinxton, UK.
“Our technological advances enabled us to identify all the essential genes in P falciparum—the first time this has been possible for a human malaria parasite.”
To determine which genes P falciparum needs to survive and thrive, the researchers disrupted the parasite’s genes.
The team used piggyBac-transposon insertional mutagenesis to inactivate genes at random and then used DNA sequencing technology to identify which genes were affected.
The researchers made more than 38,000 mutations, then looked for genes that hadn’t been changed, implying they were essential for P falciparum to survive and grow.
This revealed 2680 non-mutable genes, about 1000 of which are conserved in all Plasmodium species and have unknown functions.
“What our team has done is develop a way to analyze every gene in this parasite’s genome,” said study author John H. Adams, PhD, of the University of South Florida in Tampa.
“Using our genetic analysis tools, we’re able to determine the relative importance of each gene for parasite survival. This understanding will help guide future drug development efforts targeting those essential genes.”
The researchers noted that the proteasome pathway had a “high ratio of essential to dispensable genes,” and recent research has linked this pathway to resistance to artemisinin combination therapy.
“We need new drug targets against malaria now more than ever, since our current antimalarial drugs are failing,” said study author Julian C. Rayner, PhD, of Wellcome Sanger Institute.
“This is the first large-scale genetic study in the major human malaria parasite P falciparum and gives a list of 2680 essential genes that researchers can prioritize as promising possible drug targets. We hope this functional genomics approach will help to speed up the pipeline to develop new treatments for this devastating disease.”
More than 2000 genes are “essential” for the malaria parasite Plasmodium falciparum, according to research published in Science.
Researchers identified 2680 genes that appear necessary for growth and survival during P falciparum’s asexual blood stage.
The researchers therefore believe these genes could be viable therapeutic targets for P falciparum malaria.
“Malaria parasites are extremely technically difficult to manipulate and sequence, and, until this study, only a few of P falciparum’s essential genes had been determined,” said study author Iraad Bronner, of the Wellcome Sanger Institute in Hinxton, UK.
“Our technological advances enabled us to identify all the essential genes in P falciparum—the first time this has been possible for a human malaria parasite.”
To determine which genes P falciparum needs to survive and thrive, the researchers disrupted the parasite’s genes.
The team used piggyBac-transposon insertional mutagenesis to inactivate genes at random and then used DNA sequencing technology to identify which genes were affected.
The researchers made more than 38,000 mutations, then looked for genes that hadn’t been changed, implying they were essential for P falciparum to survive and grow.
This revealed 2680 non-mutable genes, about 1000 of which are conserved in all Plasmodium species and have unknown functions.
“What our team has done is develop a way to analyze every gene in this parasite’s genome,” said study author John H. Adams, PhD, of the University of South Florida in Tampa.
“Using our genetic analysis tools, we’re able to determine the relative importance of each gene for parasite survival. This understanding will help guide future drug development efforts targeting those essential genes.”
The researchers noted that the proteasome pathway had a “high ratio of essential to dispensable genes,” and recent research has linked this pathway to resistance to artemisinin combination therapy.
“We need new drug targets against malaria now more than ever, since our current antimalarial drugs are failing,” said study author Julian C. Rayner, PhD, of Wellcome Sanger Institute.
“This is the first large-scale genetic study in the major human malaria parasite P falciparum and gives a list of 2680 essential genes that researchers can prioritize as promising possible drug targets. We hope this functional genomics approach will help to speed up the pipeline to develop new treatments for this devastating disease.”
More than 2000 genes are “essential” for the malaria parasite Plasmodium falciparum, according to research published in Science.
Researchers identified 2680 genes that appear necessary for growth and survival during P falciparum’s asexual blood stage.
The researchers therefore believe these genes could be viable therapeutic targets for P falciparum malaria.
“Malaria parasites are extremely technically difficult to manipulate and sequence, and, until this study, only a few of P falciparum’s essential genes had been determined,” said study author Iraad Bronner, of the Wellcome Sanger Institute in Hinxton, UK.
“Our technological advances enabled us to identify all the essential genes in P falciparum—the first time this has been possible for a human malaria parasite.”
To determine which genes P falciparum needs to survive and thrive, the researchers disrupted the parasite’s genes.
The team used piggyBac-transposon insertional mutagenesis to inactivate genes at random and then used DNA sequencing technology to identify which genes were affected.
The researchers made more than 38,000 mutations, then looked for genes that hadn’t been changed, implying they were essential for P falciparum to survive and grow.
This revealed 2680 non-mutable genes, about 1000 of which are conserved in all Plasmodium species and have unknown functions.
“What our team has done is develop a way to analyze every gene in this parasite’s genome,” said study author John H. Adams, PhD, of the University of South Florida in Tampa.
“Using our genetic analysis tools, we’re able to determine the relative importance of each gene for parasite survival. This understanding will help guide future drug development efforts targeting those essential genes.”
The researchers noted that the proteasome pathway had a “high ratio of essential to dispensable genes,” and recent research has linked this pathway to resistance to artemisinin combination therapy.
“We need new drug targets against malaria now more than ever, since our current antimalarial drugs are failing,” said study author Julian C. Rayner, PhD, of Wellcome Sanger Institute.
“This is the first large-scale genetic study in the major human malaria parasite P falciparum and gives a list of 2680 essential genes that researchers can prioritize as promising possible drug targets. We hope this functional genomics approach will help to speed up the pipeline to develop new treatments for this devastating disease.”
Many believe in unproven causes of cancer, survey shows
A new survey suggests many people believe certain environmental and lifestyle factors cause cancer even though there is insufficient evidence to support these beliefs.
In a survey of 1330 people in England, more than 40% of respondents said that stress and food additives can cause cancer.
More than a third of participants reported that cancer may result from exposure to electromagnetic frequencies and eating genetically modified foods.
“It’s worrying to see so many people endorse risk factors for which there is no convincing evidence,” said Samuel Smith, PhD, of the University of Leeds in the UK.
“Compared to past research, it appears the number of people believing in unproven causes of cancer has increased since the start of the century, which could be a result of changes to how we access news and information through the Internet and social media.”
Dr Smith and his colleagues reported results from the survey in European Journal of Cancer.
The researchers surveyed 1330 people with a mean age of 43.7. Slightly more than half (51.6%) were female, most (84.7%) were white, and most (67%) had post-16 qualifications (education beyond age 16).
The survey included questions about 11 known cancer risk factors, such as being overweight, alcohol consumption, having a relative with cancer, and infection with human papillomavirus (HPV).
The survey also included questions about 12 factors that are commonly believed to cause cancer but for which there is no scientific evidence to confirm the belief. Some of these include eating food containing artificial sweeteners and using mobile phones, cleaning products, and aerosol containers.
Respondents were asked how much they agree that each of the factors increase the risk of cancer. Response options were: strongly disagree, disagree, unsure, agree, and strongly agree.
Results
Participants provided a correct response to more of the questions about proven cancer risk factors than unproven factors—53% and 36%, respectively (P<0.01).
Most respondents knew that active smoking (88%) and exposure to smoking (80%) can cause cancer. However, only 30% of them knew that HPV or low fruit and vegetable consumption are proven cancer risk factors.
The most common unproven factors believed to cause cancer were stress (43%), food additives (42%), electromagnetic frequencies (35%), and genetically modified foods (34%).
In addition, 19% of respondents said using microwave ovens can cause cancer, and 15% said drinking from plastic bottles can cause cancer.
The researchers did note that belief in unproven causes of cancer did not mean a person was more likely to have risky lifestyle habits.
However, respondents who had better knowledge of proven causes were more likely to engage in habits that might reduce their risk of cancer.
“People’s beliefs are so important because they have an impact on the lifestyle choices they make,” said Lion Shahab, PhD, of University College London in the UK.
“Those with better awareness of proven causes of cancer were more likely not to smoke and to eat more fruit and vegetables.”
Dr Smith added, “It’s vital to improve public education about the causes of cancer if we want to help people make informed decisions about their lives and ensure they aren’t worrying unnecessarily.”
A new survey suggests many people believe certain environmental and lifestyle factors cause cancer even though there is insufficient evidence to support these beliefs.
In a survey of 1330 people in England, more than 40% of respondents said that stress and food additives can cause cancer.
More than a third of participants reported that cancer may result from exposure to electromagnetic frequencies and eating genetically modified foods.
“It’s worrying to see so many people endorse risk factors for which there is no convincing evidence,” said Samuel Smith, PhD, of the University of Leeds in the UK.
“Compared to past research, it appears the number of people believing in unproven causes of cancer has increased since the start of the century, which could be a result of changes to how we access news and information through the Internet and social media.”
Dr Smith and his colleagues reported results from the survey in European Journal of Cancer.
The researchers surveyed 1330 people with a mean age of 43.7. Slightly more than half (51.6%) were female, most (84.7%) were white, and most (67%) had post-16 qualifications (education beyond age 16).
The survey included questions about 11 known cancer risk factors, such as being overweight, alcohol consumption, having a relative with cancer, and infection with human papillomavirus (HPV).
The survey also included questions about 12 factors that are commonly believed to cause cancer but for which there is no scientific evidence to confirm the belief. Some of these include eating food containing artificial sweeteners and using mobile phones, cleaning products, and aerosol containers.
Respondents were asked how much they agree that each of the factors increase the risk of cancer. Response options were: strongly disagree, disagree, unsure, agree, and strongly agree.
Results
Participants provided a correct response to more of the questions about proven cancer risk factors than unproven factors—53% and 36%, respectively (P<0.01).
Most respondents knew that active smoking (88%) and exposure to smoking (80%) can cause cancer. However, only 30% of them knew that HPV or low fruit and vegetable consumption are proven cancer risk factors.
The most common unproven factors believed to cause cancer were stress (43%), food additives (42%), electromagnetic frequencies (35%), and genetically modified foods (34%).
In addition, 19% of respondents said using microwave ovens can cause cancer, and 15% said drinking from plastic bottles can cause cancer.
The researchers did note that belief in unproven causes of cancer did not mean a person was more likely to have risky lifestyle habits.
However, respondents who had better knowledge of proven causes were more likely to engage in habits that might reduce their risk of cancer.
“People’s beliefs are so important because they have an impact on the lifestyle choices they make,” said Lion Shahab, PhD, of University College London in the UK.
“Those with better awareness of proven causes of cancer were more likely not to smoke and to eat more fruit and vegetables.”
Dr Smith added, “It’s vital to improve public education about the causes of cancer if we want to help people make informed decisions about their lives and ensure they aren’t worrying unnecessarily.”
A new survey suggests many people believe certain environmental and lifestyle factors cause cancer even though there is insufficient evidence to support these beliefs.
In a survey of 1330 people in England, more than 40% of respondents said that stress and food additives can cause cancer.
More than a third of participants reported that cancer may result from exposure to electromagnetic frequencies and eating genetically modified foods.
“It’s worrying to see so many people endorse risk factors for which there is no convincing evidence,” said Samuel Smith, PhD, of the University of Leeds in the UK.
“Compared to past research, it appears the number of people believing in unproven causes of cancer has increased since the start of the century, which could be a result of changes to how we access news and information through the Internet and social media.”
Dr Smith and his colleagues reported results from the survey in European Journal of Cancer.
The researchers surveyed 1330 people with a mean age of 43.7. Slightly more than half (51.6%) were female, most (84.7%) were white, and most (67%) had post-16 qualifications (education beyond age 16).
The survey included questions about 11 known cancer risk factors, such as being overweight, alcohol consumption, having a relative with cancer, and infection with human papillomavirus (HPV).
The survey also included questions about 12 factors that are commonly believed to cause cancer but for which there is no scientific evidence to confirm the belief. Some of these include eating food containing artificial sweeteners and using mobile phones, cleaning products, and aerosol containers.
Respondents were asked how much they agree that each of the factors increase the risk of cancer. Response options were: strongly disagree, disagree, unsure, agree, and strongly agree.
Results
Participants provided a correct response to more of the questions about proven cancer risk factors than unproven factors—53% and 36%, respectively (P<0.01).
Most respondents knew that active smoking (88%) and exposure to smoking (80%) can cause cancer. However, only 30% of them knew that HPV or low fruit and vegetable consumption are proven cancer risk factors.
The most common unproven factors believed to cause cancer were stress (43%), food additives (42%), electromagnetic frequencies (35%), and genetically modified foods (34%).
In addition, 19% of respondents said using microwave ovens can cause cancer, and 15% said drinking from plastic bottles can cause cancer.
The researchers did note that belief in unproven causes of cancer did not mean a person was more likely to have risky lifestyle habits.
However, respondents who had better knowledge of proven causes were more likely to engage in habits that might reduce their risk of cancer.
“People’s beliefs are so important because they have an impact on the lifestyle choices they make,” said Lion Shahab, PhD, of University College London in the UK.
“Those with better awareness of proven causes of cancer were more likely not to smoke and to eat more fruit and vegetables.”
Dr Smith added, “It’s vital to improve public education about the causes of cancer if we want to help people make informed decisions about their lives and ensure they aren’t worrying unnecessarily.”
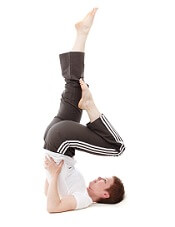
Exercise linked to risk of death in cancer patients
CHICAGO—Researchers have identified a link between habitual physical activity (PA) and mortality among cancer patients.
Engaging in regular PA, both pre- and post-diagnosis, was associated with a significantly lower risk of death for the entire population studied and for patients with 8 specific types of cancer.
However, the association was not significant for patients with other cancer types, including hematologic malignancies.
Rikki Cannioto, PhD, of Roswell Park Comprehensive Cancer Center in Buffalo, New York, and her colleagues presented these findings at the AACR Annual Meeting 2018 (abstract 5254*).
The researchers examined the association between habitual PA and outcomes in 5807 cancer patients enrolled in the Data Bank and BioRepository at Roswell Park between 2003 and 2016.
The population was 54.8% female and 93% white. The average age at diagnosis was 60.6 years.
The researchers looked at patterns of PA over time, from the decade before the cancer was diagnosed and continuing for up to 1 year after diagnosis.
Patients who engaged in regular, moderate- to vigorous-intensity PA (such as walking, running, aerobics, or other cardiovascular exercise) both before and after their diagnosis were considered habitually active, whereas those who did not exercise regularly were considered habitually inactive.
Overall, 52% of patients reported habitual activity, and 19% reported habitual inactivity. Twenty-three percent of patients said their activity level decreased after diagnosis, and 6% said their activity level increased.
Patients were followed through January 31, 2018. The median time to follow-up was 53 months, and 33.7% of patients (n=1956) died during the follow-up period.
Results
The researchers found that patients who were active before and after diagnosis were 40% more likely to survive than those who were habitually inactive (P<0.001). Habitually inactive patients had a 66% increased risk of mortality compared to active patients.
The habitually active patients had a 37-month mean survival advantage over the inactive patients.
In addition, patients whose activity level increased after diagnosis had a 25% lower risk of death than patients who remained inactive after diagnosis.
The researchers observed a significant (P<0.05) association between habitual PA and decreased mortality in patients with breast, colon, prostate, bladder, endometrial, ovarian, esophageal, and skin cancers.
However, the association between PA and mortality was not significant for patients with hematologic malignancies (P=0.59) or kidney, liver, lung, pancreas, stomach, or “other” cancers.
The researchers said the associations between habitual PA and decreased mortality remained consistent regardless of a patient’s sex, tumor stage, smoking status, or body mass index.
“[W]hen it comes to exercise, something is better than nothing, but regular, weekly exercise seems to really make a difference,” Dr Cannioto said.
“In fact, patients who were physically active 3 or 4 days a week experienced an even greater benefit than those who exercised daily, and patients who had only 1 or 2 days of regular activity per week did nearly as well. This is particularly encouraging, as cancer patients and survivors can be overwhelmed by current physical activity recommendations.”
*Information in the abstract differs from the presentation.
CHICAGO—Researchers have identified a link between habitual physical activity (PA) and mortality among cancer patients.
Engaging in regular PA, both pre- and post-diagnosis, was associated with a significantly lower risk of death for the entire population studied and for patients with 8 specific types of cancer.
However, the association was not significant for patients with other cancer types, including hematologic malignancies.
Rikki Cannioto, PhD, of Roswell Park Comprehensive Cancer Center in Buffalo, New York, and her colleagues presented these findings at the AACR Annual Meeting 2018 (abstract 5254*).
The researchers examined the association between habitual PA and outcomes in 5807 cancer patients enrolled in the Data Bank and BioRepository at Roswell Park between 2003 and 2016.
The population was 54.8% female and 93% white. The average age at diagnosis was 60.6 years.
The researchers looked at patterns of PA over time, from the decade before the cancer was diagnosed and continuing for up to 1 year after diagnosis.
Patients who engaged in regular, moderate- to vigorous-intensity PA (such as walking, running, aerobics, or other cardiovascular exercise) both before and after their diagnosis were considered habitually active, whereas those who did not exercise regularly were considered habitually inactive.
Overall, 52% of patients reported habitual activity, and 19% reported habitual inactivity. Twenty-three percent of patients said their activity level decreased after diagnosis, and 6% said their activity level increased.
Patients were followed through January 31, 2018. The median time to follow-up was 53 months, and 33.7% of patients (n=1956) died during the follow-up period.
Results
The researchers found that patients who were active before and after diagnosis were 40% more likely to survive than those who were habitually inactive (P<0.001). Habitually inactive patients had a 66% increased risk of mortality compared to active patients.
The habitually active patients had a 37-month mean survival advantage over the inactive patients.
In addition, patients whose activity level increased after diagnosis had a 25% lower risk of death than patients who remained inactive after diagnosis.
The researchers observed a significant (P<0.05) association between habitual PA and decreased mortality in patients with breast, colon, prostate, bladder, endometrial, ovarian, esophageal, and skin cancers.
However, the association between PA and mortality was not significant for patients with hematologic malignancies (P=0.59) or kidney, liver, lung, pancreas, stomach, or “other” cancers.
The researchers said the associations between habitual PA and decreased mortality remained consistent regardless of a patient’s sex, tumor stage, smoking status, or body mass index.
“[W]hen it comes to exercise, something is better than nothing, but regular, weekly exercise seems to really make a difference,” Dr Cannioto said.
“In fact, patients who were physically active 3 or 4 days a week experienced an even greater benefit than those who exercised daily, and patients who had only 1 or 2 days of regular activity per week did nearly as well. This is particularly encouraging, as cancer patients and survivors can be overwhelmed by current physical activity recommendations.”
*Information in the abstract differs from the presentation.
CHICAGO—Researchers have identified a link between habitual physical activity (PA) and mortality among cancer patients.
Engaging in regular PA, both pre- and post-diagnosis, was associated with a significantly lower risk of death for the entire population studied and for patients with 8 specific types of cancer.
However, the association was not significant for patients with other cancer types, including hematologic malignancies.
Rikki Cannioto, PhD, of Roswell Park Comprehensive Cancer Center in Buffalo, New York, and her colleagues presented these findings at the AACR Annual Meeting 2018 (abstract 5254*).
The researchers examined the association between habitual PA and outcomes in 5807 cancer patients enrolled in the Data Bank and BioRepository at Roswell Park between 2003 and 2016.
The population was 54.8% female and 93% white. The average age at diagnosis was 60.6 years.
The researchers looked at patterns of PA over time, from the decade before the cancer was diagnosed and continuing for up to 1 year after diagnosis.
Patients who engaged in regular, moderate- to vigorous-intensity PA (such as walking, running, aerobics, or other cardiovascular exercise) both before and after their diagnosis were considered habitually active, whereas those who did not exercise regularly were considered habitually inactive.
Overall, 52% of patients reported habitual activity, and 19% reported habitual inactivity. Twenty-three percent of patients said their activity level decreased after diagnosis, and 6% said their activity level increased.
Patients were followed through January 31, 2018. The median time to follow-up was 53 months, and 33.7% of patients (n=1956) died during the follow-up period.
Results
The researchers found that patients who were active before and after diagnosis were 40% more likely to survive than those who were habitually inactive (P<0.001). Habitually inactive patients had a 66% increased risk of mortality compared to active patients.
The habitually active patients had a 37-month mean survival advantage over the inactive patients.
In addition, patients whose activity level increased after diagnosis had a 25% lower risk of death than patients who remained inactive after diagnosis.
The researchers observed a significant (P<0.05) association between habitual PA and decreased mortality in patients with breast, colon, prostate, bladder, endometrial, ovarian, esophageal, and skin cancers.
However, the association between PA and mortality was not significant for patients with hematologic malignancies (P=0.59) or kidney, liver, lung, pancreas, stomach, or “other” cancers.
The researchers said the associations between habitual PA and decreased mortality remained consistent regardless of a patient’s sex, tumor stage, smoking status, or body mass index.
“[W]hen it comes to exercise, something is better than nothing, but regular, weekly exercise seems to really make a difference,” Dr Cannioto said.
“In fact, patients who were physically active 3 or 4 days a week experienced an even greater benefit than those who exercised daily, and patients who had only 1 or 2 days of regular activity per week did nearly as well. This is particularly encouraging, as cancer patients and survivors can be overwhelmed by current physical activity recommendations.”
*Information in the abstract differs from the presentation.
Groups launch open portal for cancer models
The European Bioinformatics Institute (EMBL-EBI) and The Jackson Laboratory (JAX) have developed an open cancer research portal for patient-derived xenograft (PDX) models.
The portal, known as PDX Finder, catalogues PDX models from numerous global repositories.
At present, PDX Finder contains more than 1900 models for a range of cancers, including hematologic malignancies.
Researchers can search for PDX models and submit their own on the PDX Finder website: http://www.pdxfinder.org.
“PDX models are increasingly recognized as clinically relevant because they retain the patient tumor characteristics and imitate a specific patient’s response to drugs more accurately than other models,” said Nathalie Conte, PDX Finder project lead at EMBL-EBI.
“However, until now, there was no open central catalogue for PDX models. PDX Finder enables cancer researchers to search through a wider variety of models more quickly, saving valuable time and enabling collaborations.”
PDX Finder builds on JAX’s PDX resource, which was developed in partnership with more than 20 medical centers in the US, and EMBL-EBI’s membership of EurOPDX. This ensures the scope and reach of PDX Finder is wider than any other individual resource available, according to JAX and EMBL-EBI.
“Both EMBL-EBI and JAX received independent funding from the National Cancer Institute [NCI] for projects that included implementation of online catalogues for PDX models,” noted Carol Bult, scientific director of the JAX PDX resource.
“Both groups had the goal to help basic and clinical cancer researchers find relevant models fast. With approval from the NCI, we instead collaborated to build a single, unified portal with international scope.”
The launch of PDX Finder comes just months after EMBL-EBI and JAX published the PDX minimal information standard, which sets standards for basic information needed to describe essential properties of a PDX model.
The standard ensures that every model in PDX Finder is carefully described to help researchers choose models that are most relevant to their work.
The European Bioinformatics Institute (EMBL-EBI) and The Jackson Laboratory (JAX) have developed an open cancer research portal for patient-derived xenograft (PDX) models.
The portal, known as PDX Finder, catalogues PDX models from numerous global repositories.
At present, PDX Finder contains more than 1900 models for a range of cancers, including hematologic malignancies.
Researchers can search for PDX models and submit their own on the PDX Finder website: http://www.pdxfinder.org.
“PDX models are increasingly recognized as clinically relevant because they retain the patient tumor characteristics and imitate a specific patient’s response to drugs more accurately than other models,” said Nathalie Conte, PDX Finder project lead at EMBL-EBI.
“However, until now, there was no open central catalogue for PDX models. PDX Finder enables cancer researchers to search through a wider variety of models more quickly, saving valuable time and enabling collaborations.”
PDX Finder builds on JAX’s PDX resource, which was developed in partnership with more than 20 medical centers in the US, and EMBL-EBI’s membership of EurOPDX. This ensures the scope and reach of PDX Finder is wider than any other individual resource available, according to JAX and EMBL-EBI.
“Both EMBL-EBI and JAX received independent funding from the National Cancer Institute [NCI] for projects that included implementation of online catalogues for PDX models,” noted Carol Bult, scientific director of the JAX PDX resource.
“Both groups had the goal to help basic and clinical cancer researchers find relevant models fast. With approval from the NCI, we instead collaborated to build a single, unified portal with international scope.”
The launch of PDX Finder comes just months after EMBL-EBI and JAX published the PDX minimal information standard, which sets standards for basic information needed to describe essential properties of a PDX model.
The standard ensures that every model in PDX Finder is carefully described to help researchers choose models that are most relevant to their work.
The European Bioinformatics Institute (EMBL-EBI) and The Jackson Laboratory (JAX) have developed an open cancer research portal for patient-derived xenograft (PDX) models.
The portal, known as PDX Finder, catalogues PDX models from numerous global repositories.
At present, PDX Finder contains more than 1900 models for a range of cancers, including hematologic malignancies.
Researchers can search for PDX models and submit their own on the PDX Finder website: http://www.pdxfinder.org.
“PDX models are increasingly recognized as clinically relevant because they retain the patient tumor characteristics and imitate a specific patient’s response to drugs more accurately than other models,” said Nathalie Conte, PDX Finder project lead at EMBL-EBI.
“However, until now, there was no open central catalogue for PDX models. PDX Finder enables cancer researchers to search through a wider variety of models more quickly, saving valuable time and enabling collaborations.”
PDX Finder builds on JAX’s PDX resource, which was developed in partnership with more than 20 medical centers in the US, and EMBL-EBI’s membership of EurOPDX. This ensures the scope and reach of PDX Finder is wider than any other individual resource available, according to JAX and EMBL-EBI.
“Both EMBL-EBI and JAX received independent funding from the National Cancer Institute [NCI] for projects that included implementation of online catalogues for PDX models,” noted Carol Bult, scientific director of the JAX PDX resource.
“Both groups had the goal to help basic and clinical cancer researchers find relevant models fast. With approval from the NCI, we instead collaborated to build a single, unified portal with international scope.”
The launch of PDX Finder comes just months after EMBL-EBI and JAX published the PDX minimal information standard, which sets standards for basic information needed to describe essential properties of a PDX model.
The standard ensures that every model in PDX Finder is carefully described to help researchers choose models that are most relevant to their work.
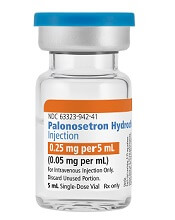
Generic antiemetic now available in US
Palonosetron Hydrochloride Injection, a generic alternative to Aloxi®, is now available in the US.
Fresenius Kabi’s Palonosetron Hydrochloride Injection is a 5-HT3 serotonin receptor that is approved for the prevention of nausea and vomiting in certain adults.
Palonosetron Hydrochloride Injection is available in a single-dose vial (0.25 mg per 5 mL).
In the US, Palonosetron Hydrochloride Injection is approved for the prevention of acute and delayed nausea and vomiting associated with initial and repeat courses of moderately emetogenic cancer chemotherapy.
The drug is also approved for the prevention of acute nausea and vomiting associated with initial and repeat courses of highly emetogenic cancer chemotherapy.
And Palonosetron Hydrochloride Injection is approved for the prevention of post-operative nausea and vomiting for up to 24 hours after surgery. Efficacy beyond 24 hours has not been demonstrated.
The full prescribing information for Palonosetron Hydrochloride Injection can be found on the Fresenius Kabi website.
Palonosetron Hydrochloride Injection, a generic alternative to Aloxi®, is now available in the US.
Fresenius Kabi’s Palonosetron Hydrochloride Injection is a 5-HT3 serotonin receptor that is approved for the prevention of nausea and vomiting in certain adults.
Palonosetron Hydrochloride Injection is available in a single-dose vial (0.25 mg per 5 mL).
In the US, Palonosetron Hydrochloride Injection is approved for the prevention of acute and delayed nausea and vomiting associated with initial and repeat courses of moderately emetogenic cancer chemotherapy.
The drug is also approved for the prevention of acute nausea and vomiting associated with initial and repeat courses of highly emetogenic cancer chemotherapy.
And Palonosetron Hydrochloride Injection is approved for the prevention of post-operative nausea and vomiting for up to 24 hours after surgery. Efficacy beyond 24 hours has not been demonstrated.
The full prescribing information for Palonosetron Hydrochloride Injection can be found on the Fresenius Kabi website.
Palonosetron Hydrochloride Injection, a generic alternative to Aloxi®, is now available in the US.
Fresenius Kabi’s Palonosetron Hydrochloride Injection is a 5-HT3 serotonin receptor that is approved for the prevention of nausea and vomiting in certain adults.
Palonosetron Hydrochloride Injection is available in a single-dose vial (0.25 mg per 5 mL).
In the US, Palonosetron Hydrochloride Injection is approved for the prevention of acute and delayed nausea and vomiting associated with initial and repeat courses of moderately emetogenic cancer chemotherapy.
The drug is also approved for the prevention of acute nausea and vomiting associated with initial and repeat courses of highly emetogenic cancer chemotherapy.
And Palonosetron Hydrochloride Injection is approved for the prevention of post-operative nausea and vomiting for up to 24 hours after surgery. Efficacy beyond 24 hours has not been demonstrated.
The full prescribing information for Palonosetron Hydrochloride Injection can be found on the Fresenius Kabi website.
Why iron can worsen malaria infection
Researchers believe they may have discovered why iron can sometimes worsen malaria infection.
By studying mice and samples from malaria patients, the researchers found that extra iron interferes with ferroportin, a protein that prevents a toxic buildup of iron in red blood cells and helps protect these cells against malaria infection.
The team also found a mutant form of ferroportin that occurs in African populations appears to protect against malaria.
These findings, published in Science, may help researchers and healthcare officials develop strategies to prevent and treat malaria.
“Our study helps solve a long-standing mystery,” said study author Tracey Rouault, MD, of the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Maryland.
“Iron supplements can sometimes worsen malaria infection and, conversely, iron deficiency can be protective in some cases. Our findings reveal that ferroportin—its function, as well as its regulation by iron levels—helps to explain these observations.”
The team found that red blood cells use ferroportin to remove excess iron, which malaria parasites consume as a food source.
In studies of mice, the researchers found the absence of ferroportin in erythroid cells caused iron to accumulate to toxic levels inside red blood cells. This, in turn, stressed the cells and shortened their life span.
In addition, the team found that mice lacking ferroportin had more parasites and worse outcomes when infected with malaria, compared to malaria-infected mice with intact ferroportin.
When they fed mice a high-iron diet, the researchers found that hepcidin regulated ferroportin in erythroid cells. The hormone, which is more abundant in high-iron environments, lowered ferroportin levels on erythroblasts and, subsequently, in red blood cells.
Additionally, hepcidin physically bound to ferroportin, preventing iron removal from the cells.
Next, the researchers sought to determine whether the ferroportin mutation Q248H, which is found in African populations, protects against malaria. This mutation shields ferroportin from hepcidin’s effects.
The team analyzed patient samples from 2 existing malaria studies. In one study, which enrolled children hospitalized for malaria in Zambia, 19.7% of the 66 patients had the Q248H mutation.
Children with the mutation tended to have fewer malarial parasites in their blood and tolerated their fevers for a longer period before coming to the hospital. While the trends were not statistically significant, they raise the possibility that Q248H reduces the iron available in the blood, therefore reducing the malaria parasite’s food source.
In the other study, which enrolled 290 pregnant women in Ghana, 8.6% had the Q248H mutation. Women with the mutation were significantly less likely to have pregnancy-associated malaria, in which parasites accumulate in the placenta and can cause adverse pregnancy and birth outcomes.
“Our findings suggest that Q248H does protect against malaria, possibly explaining why it occurs in people who live in malaria-endemic regions,” said study author De-Liang Zhang, PhD, of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
“Given the importance of iron metabolism overall, we will continue studying the ferroportin mutation and explore its other potential health effects.”
Researchers believe they may have discovered why iron can sometimes worsen malaria infection.
By studying mice and samples from malaria patients, the researchers found that extra iron interferes with ferroportin, a protein that prevents a toxic buildup of iron in red blood cells and helps protect these cells against malaria infection.
The team also found a mutant form of ferroportin that occurs in African populations appears to protect against malaria.
These findings, published in Science, may help researchers and healthcare officials develop strategies to prevent and treat malaria.
“Our study helps solve a long-standing mystery,” said study author Tracey Rouault, MD, of the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Maryland.
“Iron supplements can sometimes worsen malaria infection and, conversely, iron deficiency can be protective in some cases. Our findings reveal that ferroportin—its function, as well as its regulation by iron levels—helps to explain these observations.”
The team found that red blood cells use ferroportin to remove excess iron, which malaria parasites consume as a food source.
In studies of mice, the researchers found the absence of ferroportin in erythroid cells caused iron to accumulate to toxic levels inside red blood cells. This, in turn, stressed the cells and shortened their life span.
In addition, the team found that mice lacking ferroportin had more parasites and worse outcomes when infected with malaria, compared to malaria-infected mice with intact ferroportin.
When they fed mice a high-iron diet, the researchers found that hepcidin regulated ferroportin in erythroid cells. The hormone, which is more abundant in high-iron environments, lowered ferroportin levels on erythroblasts and, subsequently, in red blood cells.
Additionally, hepcidin physically bound to ferroportin, preventing iron removal from the cells.
Next, the researchers sought to determine whether the ferroportin mutation Q248H, which is found in African populations, protects against malaria. This mutation shields ferroportin from hepcidin’s effects.
The team analyzed patient samples from 2 existing malaria studies. In one study, which enrolled children hospitalized for malaria in Zambia, 19.7% of the 66 patients had the Q248H mutation.
Children with the mutation tended to have fewer malarial parasites in their blood and tolerated their fevers for a longer period before coming to the hospital. While the trends were not statistically significant, they raise the possibility that Q248H reduces the iron available in the blood, therefore reducing the malaria parasite’s food source.
In the other study, which enrolled 290 pregnant women in Ghana, 8.6% had the Q248H mutation. Women with the mutation were significantly less likely to have pregnancy-associated malaria, in which parasites accumulate in the placenta and can cause adverse pregnancy and birth outcomes.
“Our findings suggest that Q248H does protect against malaria, possibly explaining why it occurs in people who live in malaria-endemic regions,” said study author De-Liang Zhang, PhD, of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
“Given the importance of iron metabolism overall, we will continue studying the ferroportin mutation and explore its other potential health effects.”
Researchers believe they may have discovered why iron can sometimes worsen malaria infection.
By studying mice and samples from malaria patients, the researchers found that extra iron interferes with ferroportin, a protein that prevents a toxic buildup of iron in red blood cells and helps protect these cells against malaria infection.
The team also found a mutant form of ferroportin that occurs in African populations appears to protect against malaria.
These findings, published in Science, may help researchers and healthcare officials develop strategies to prevent and treat malaria.
“Our study helps solve a long-standing mystery,” said study author Tracey Rouault, MD, of the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Maryland.
“Iron supplements can sometimes worsen malaria infection and, conversely, iron deficiency can be protective in some cases. Our findings reveal that ferroportin—its function, as well as its regulation by iron levels—helps to explain these observations.”
The team found that red blood cells use ferroportin to remove excess iron, which malaria parasites consume as a food source.
In studies of mice, the researchers found the absence of ferroportin in erythroid cells caused iron to accumulate to toxic levels inside red blood cells. This, in turn, stressed the cells and shortened their life span.
In addition, the team found that mice lacking ferroportin had more parasites and worse outcomes when infected with malaria, compared to malaria-infected mice with intact ferroportin.
When they fed mice a high-iron diet, the researchers found that hepcidin regulated ferroportin in erythroid cells. The hormone, which is more abundant in high-iron environments, lowered ferroportin levels on erythroblasts and, subsequently, in red blood cells.
Additionally, hepcidin physically bound to ferroportin, preventing iron removal from the cells.
Next, the researchers sought to determine whether the ferroportin mutation Q248H, which is found in African populations, protects against malaria. This mutation shields ferroportin from hepcidin’s effects.
The team analyzed patient samples from 2 existing malaria studies. In one study, which enrolled children hospitalized for malaria in Zambia, 19.7% of the 66 patients had the Q248H mutation.
Children with the mutation tended to have fewer malarial parasites in their blood and tolerated their fevers for a longer period before coming to the hospital. While the trends were not statistically significant, they raise the possibility that Q248H reduces the iron available in the blood, therefore reducing the malaria parasite’s food source.
In the other study, which enrolled 290 pregnant women in Ghana, 8.6% had the Q248H mutation. Women with the mutation were significantly less likely to have pregnancy-associated malaria, in which parasites accumulate in the placenta and can cause adverse pregnancy and birth outcomes.
“Our findings suggest that Q248H does protect against malaria, possibly explaining why it occurs in people who live in malaria-endemic regions,” said study author De-Liang Zhang, PhD, of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
“Given the importance of iron metabolism overall, we will continue studying the ferroportin mutation and explore its other potential health effects.”