User login
Project provides ‘unprecedented understanding’ of cancers
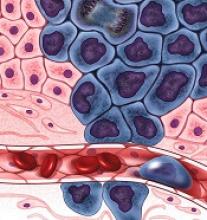
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
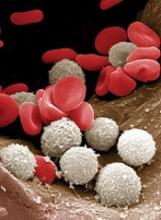
At-home measurement of WBCs
A portable device could be used to monitor patients’ white blood cell (WBC) levels at home, without the need for blood samples, according to researchers.
The team created a prototype that records video of blood cells flowing through capillaries just below the skin surface at the base of the fingernail.
The group is developing a computer algorithm that, in early testing, has been able to analyze the videos and determine if WBC levels are too low.
The researchers believe this type of device could be used to prevent infections among chemotherapy recipients.
“Our vision is that patients will have this portable device that they can take home, and they can monitor daily how they are reacting to the treatment,” said Carlos Castro-Gonzalez, PhD, of the Massachusetts Institute of Technology (MIT) in Cambridge, Massachusetts.
“If they go below the [safe WBC] threshold, then preventive treatment can be deployed.”
Dr Castro-Gonzalez and his colleagues described their prototype, and the testing of it, in Scientific Reports.
The device consists of a wide-field microscope that emits blue light, which penetrates about 50 to 150 microns below the skin and is reflected back to a video camera.
The researchers decided to image the skin at the base of the nail because the capillaries there are very close to the skin surface. These capillaries are so narrow that WBCs must squeeze through one at a time, making them easier to see.
The researchers tested the device in 11 patients at various points during their chemotherapy treatment.
The device does not provide precise WBC counts but allowed the team to differentiate cases of severe neutropenia (<500 neutrophils per μL) from non-neutropenic cases (>1500 neutrophils per μL).
To obtain enough data to make these classifications, the researchers recorded 1 minute of video per patient. Three blinded human assistants then watched the videos and noted whenever a WBC passed by.
However, since submitting their paper, the researchers have been developing a computer algorithm to perform the same task automatically.
“Based on the feature-set that our human raters identified, we are now developing an AI and machine-vision algorithm, with preliminary results that indicate the same accuracy as the raters,” said study author Aurélien Bourquard, PhD, of MIT.
The researchers have applied for patents on the technology and launched a company called Leuko, which is working on commercializing the technology with help from MIT.
To move the technology further toward commercialization, the researchers are building a new automated prototype.
“Automating the measurement process is key to making a viable home-use device,” said study author Ian Butterworth, of MIT. “The imaging needs to take place in the right spot on the patient’s finger, and the operation of the device must be straightforward.”
Using this new prototype, the researchers plan to test the device with additional cancer patients. And the team is investigating whether they can get accurate results with shorter lengths of video.
They also plan to adapt the technology so it can generate more precise WBC counts, which would make it useful for monitoring bone marrow transplant recipients or people with certain infectious diseases, Dr Castro-Gonzalez said.
This could also make it possible to determine whether chemotherapy patients can receive their next dose sooner than usual.
“There is a balancing act that oncologists must do,” said study author Alvaro Sanchez-Ferro, MD, of Centro Integral en Neurociencias A.C. HM CINAC in Madrid, Spain.
“Normally, doctors want to make chemotherapy as intensive as possible but without getting people too immunosuppressed. Current 21-day cycles are based on statistics of what most patients can take, but if you are ready early, then they can potentially bring you back early, and that can translate into better survival.”
A portable device could be used to monitor patients’ white blood cell (WBC) levels at home, without the need for blood samples, according to researchers.
The team created a prototype that records video of blood cells flowing through capillaries just below the skin surface at the base of the fingernail.
The group is developing a computer algorithm that, in early testing, has been able to analyze the videos and determine if WBC levels are too low.
The researchers believe this type of device could be used to prevent infections among chemotherapy recipients.
“Our vision is that patients will have this portable device that they can take home, and they can monitor daily how they are reacting to the treatment,” said Carlos Castro-Gonzalez, PhD, of the Massachusetts Institute of Technology (MIT) in Cambridge, Massachusetts.
“If they go below the [safe WBC] threshold, then preventive treatment can be deployed.”
Dr Castro-Gonzalez and his colleagues described their prototype, and the testing of it, in Scientific Reports.
The device consists of a wide-field microscope that emits blue light, which penetrates about 50 to 150 microns below the skin and is reflected back to a video camera.
The researchers decided to image the skin at the base of the nail because the capillaries there are very close to the skin surface. These capillaries are so narrow that WBCs must squeeze through one at a time, making them easier to see.
The researchers tested the device in 11 patients at various points during their chemotherapy treatment.
The device does not provide precise WBC counts but allowed the team to differentiate cases of severe neutropenia (<500 neutrophils per μL) from non-neutropenic cases (>1500 neutrophils per μL).
To obtain enough data to make these classifications, the researchers recorded 1 minute of video per patient. Three blinded human assistants then watched the videos and noted whenever a WBC passed by.
However, since submitting their paper, the researchers have been developing a computer algorithm to perform the same task automatically.
“Based on the feature-set that our human raters identified, we are now developing an AI and machine-vision algorithm, with preliminary results that indicate the same accuracy as the raters,” said study author Aurélien Bourquard, PhD, of MIT.
The researchers have applied for patents on the technology and launched a company called Leuko, which is working on commercializing the technology with help from MIT.
To move the technology further toward commercialization, the researchers are building a new automated prototype.
“Automating the measurement process is key to making a viable home-use device,” said study author Ian Butterworth, of MIT. “The imaging needs to take place in the right spot on the patient’s finger, and the operation of the device must be straightforward.”
Using this new prototype, the researchers plan to test the device with additional cancer patients. And the team is investigating whether they can get accurate results with shorter lengths of video.
They also plan to adapt the technology so it can generate more precise WBC counts, which would make it useful for monitoring bone marrow transplant recipients or people with certain infectious diseases, Dr Castro-Gonzalez said.
This could also make it possible to determine whether chemotherapy patients can receive their next dose sooner than usual.
“There is a balancing act that oncologists must do,” said study author Alvaro Sanchez-Ferro, MD, of Centro Integral en Neurociencias A.C. HM CINAC in Madrid, Spain.
“Normally, doctors want to make chemotherapy as intensive as possible but without getting people too immunosuppressed. Current 21-day cycles are based on statistics of what most patients can take, but if you are ready early, then they can potentially bring you back early, and that can translate into better survival.”
A portable device could be used to monitor patients’ white blood cell (WBC) levels at home, without the need for blood samples, according to researchers.
The team created a prototype that records video of blood cells flowing through capillaries just below the skin surface at the base of the fingernail.
The group is developing a computer algorithm that, in early testing, has been able to analyze the videos and determine if WBC levels are too low.
The researchers believe this type of device could be used to prevent infections among chemotherapy recipients.
“Our vision is that patients will have this portable device that they can take home, and they can monitor daily how they are reacting to the treatment,” said Carlos Castro-Gonzalez, PhD, of the Massachusetts Institute of Technology (MIT) in Cambridge, Massachusetts.
“If they go below the [safe WBC] threshold, then preventive treatment can be deployed.”
Dr Castro-Gonzalez and his colleagues described their prototype, and the testing of it, in Scientific Reports.
The device consists of a wide-field microscope that emits blue light, which penetrates about 50 to 150 microns below the skin and is reflected back to a video camera.
The researchers decided to image the skin at the base of the nail because the capillaries there are very close to the skin surface. These capillaries are so narrow that WBCs must squeeze through one at a time, making them easier to see.
The researchers tested the device in 11 patients at various points during their chemotherapy treatment.
The device does not provide precise WBC counts but allowed the team to differentiate cases of severe neutropenia (<500 neutrophils per μL) from non-neutropenic cases (>1500 neutrophils per μL).
To obtain enough data to make these classifications, the researchers recorded 1 minute of video per patient. Three blinded human assistants then watched the videos and noted whenever a WBC passed by.
However, since submitting their paper, the researchers have been developing a computer algorithm to perform the same task automatically.
“Based on the feature-set that our human raters identified, we are now developing an AI and machine-vision algorithm, with preliminary results that indicate the same accuracy as the raters,” said study author Aurélien Bourquard, PhD, of MIT.
The researchers have applied for patents on the technology and launched a company called Leuko, which is working on commercializing the technology with help from MIT.
To move the technology further toward commercialization, the researchers are building a new automated prototype.
“Automating the measurement process is key to making a viable home-use device,” said study author Ian Butterworth, of MIT. “The imaging needs to take place in the right spot on the patient’s finger, and the operation of the device must be straightforward.”
Using this new prototype, the researchers plan to test the device with additional cancer patients. And the team is investigating whether they can get accurate results with shorter lengths of video.
They also plan to adapt the technology so it can generate more precise WBC counts, which would make it useful for monitoring bone marrow transplant recipients or people with certain infectious diseases, Dr Castro-Gonzalez said.
This could also make it possible to determine whether chemotherapy patients can receive their next dose sooner than usual.
“There is a balancing act that oncologists must do,” said study author Alvaro Sanchez-Ferro, MD, of Centro Integral en Neurociencias A.C. HM CINAC in Madrid, Spain.
“Normally, doctors want to make chemotherapy as intensive as possible but without getting people too immunosuppressed. Current 21-day cycles are based on statistics of what most patients can take, but if you are ready early, then they can potentially bring you back early, and that can translate into better survival.”
How RBCs maintain their shape
New research indicates that non-muscle myosin II-A (NMIIA) plays a key role in maintaining red blood cell (RBC) shape and deformability.
Researchers found evidence to suggest that NMIIA forms filaments in RBCs, and specialized regions at both ends of the filaments can pull on actin to control the stiffness of the cell membrane.
“You need active contraction on the cell membrane, similar to how muscles contract,” explained study author Velia Fowler, PhD, of The Scripps Research Institute in La Jolla, California.
“The myosin pulls on the actin to provide tension in the membrane, and then that tension maintains the biconcave shape.”
Dr Fowler and her colleagues described these findings in PNAS.
The researchers noted that RBC shape and deformability depend upon the membrane skeleton—a network of actin filaments (F-actin) cross-linked by spectrin tetramers.
And although NMII motors are known to exert force on F-actin networks to control cell shapes, no one had investigated a function for NMII contractility in the spectrin–F-actin network of RBCs. So Dr Fowler and her colleagues did just that.
The researchers said their work suggests NMIIA is the predominant RBC NMII isoform, and NMIIA motor activity regulates interactions with the spectrin–F-actin network to control RBCs’ shape and deformability.
Specifically, NMIIA forms bipolar filaments in RBCs, and these filaments associate with F-actins via their motor domains. It is through these interactions that NMIIA contractile forces promote membrane tension to maintain RBC shape and deformability.
To test these findings, the researchers treated RBCs with a compound called blebbistatin, which inhibits NMII motor activity.
After treatment, the team observed a decrease in NMIIA filaments associated with the RBC membrane and evidence of decreased membrane tension. The treated RBCs became elongated and showed a reduction in biconcavity as well as an increase in deformability.
The researchers believe this work could have applications for diseases in which RBCs are deformed. In fact, the team thinks inhibiting NMIIA in RBCs might prove useful for treating patients with sickle cell disease, as it could restore some elasticity to the patients’ RBCs.
Going forward, the researchers hope to learn more about what regulates NMIIA’s activity in RBCs and other cells.
New research indicates that non-muscle myosin II-A (NMIIA) plays a key role in maintaining red blood cell (RBC) shape and deformability.
Researchers found evidence to suggest that NMIIA forms filaments in RBCs, and specialized regions at both ends of the filaments can pull on actin to control the stiffness of the cell membrane.
“You need active contraction on the cell membrane, similar to how muscles contract,” explained study author Velia Fowler, PhD, of The Scripps Research Institute in La Jolla, California.
“The myosin pulls on the actin to provide tension in the membrane, and then that tension maintains the biconcave shape.”
Dr Fowler and her colleagues described these findings in PNAS.
The researchers noted that RBC shape and deformability depend upon the membrane skeleton—a network of actin filaments (F-actin) cross-linked by spectrin tetramers.
And although NMII motors are known to exert force on F-actin networks to control cell shapes, no one had investigated a function for NMII contractility in the spectrin–F-actin network of RBCs. So Dr Fowler and her colleagues did just that.
The researchers said their work suggests NMIIA is the predominant RBC NMII isoform, and NMIIA motor activity regulates interactions with the spectrin–F-actin network to control RBCs’ shape and deformability.
Specifically, NMIIA forms bipolar filaments in RBCs, and these filaments associate with F-actins via their motor domains. It is through these interactions that NMIIA contractile forces promote membrane tension to maintain RBC shape and deformability.
To test these findings, the researchers treated RBCs with a compound called blebbistatin, which inhibits NMII motor activity.
After treatment, the team observed a decrease in NMIIA filaments associated with the RBC membrane and evidence of decreased membrane tension. The treated RBCs became elongated and showed a reduction in biconcavity as well as an increase in deformability.
The researchers believe this work could have applications for diseases in which RBCs are deformed. In fact, the team thinks inhibiting NMIIA in RBCs might prove useful for treating patients with sickle cell disease, as it could restore some elasticity to the patients’ RBCs.
Going forward, the researchers hope to learn more about what regulates NMIIA’s activity in RBCs and other cells.
New research indicates that non-muscle myosin II-A (NMIIA) plays a key role in maintaining red blood cell (RBC) shape and deformability.
Researchers found evidence to suggest that NMIIA forms filaments in RBCs, and specialized regions at both ends of the filaments can pull on actin to control the stiffness of the cell membrane.
“You need active contraction on the cell membrane, similar to how muscles contract,” explained study author Velia Fowler, PhD, of The Scripps Research Institute in La Jolla, California.
“The myosin pulls on the actin to provide tension in the membrane, and then that tension maintains the biconcave shape.”
Dr Fowler and her colleagues described these findings in PNAS.
The researchers noted that RBC shape and deformability depend upon the membrane skeleton—a network of actin filaments (F-actin) cross-linked by spectrin tetramers.
And although NMII motors are known to exert force on F-actin networks to control cell shapes, no one had investigated a function for NMII contractility in the spectrin–F-actin network of RBCs. So Dr Fowler and her colleagues did just that.
The researchers said their work suggests NMIIA is the predominant RBC NMII isoform, and NMIIA motor activity regulates interactions with the spectrin–F-actin network to control RBCs’ shape and deformability.
Specifically, NMIIA forms bipolar filaments in RBCs, and these filaments associate with F-actins via their motor domains. It is through these interactions that NMIIA contractile forces promote membrane tension to maintain RBC shape and deformability.
To test these findings, the researchers treated RBCs with a compound called blebbistatin, which inhibits NMII motor activity.
After treatment, the team observed a decrease in NMIIA filaments associated with the RBC membrane and evidence of decreased membrane tension. The treated RBCs became elongated and showed a reduction in biconcavity as well as an increase in deformability.
The researchers believe this work could have applications for diseases in which RBCs are deformed. In fact, the team thinks inhibiting NMIIA in RBCs might prove useful for treating patients with sickle cell disease, as it could restore some elasticity to the patients’ RBCs.
Going forward, the researchers hope to learn more about what regulates NMIIA’s activity in RBCs and other cells.
CHMP supports expanded approval for fosaprepitant
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended changing the terms of marketing authorization for fosaprepitant (Ivemend).
The product is already approved in the European Union (EU) for the prevention of acute and delayed nausea and vomiting associated with moderately or highly emetogenic cancer chemotherapy in adults.
Now, the CHMP is recommending that fosaprepitant be authorized for the same indication in pediatric patients age 6 months and older.
As it is in adults, fosaprepitant would be given to children as part of combination therapy.
The CHMP’s opinion on fosaprepitant will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the EU. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
Merck Sharp & Dohme Corp., the company developing fosaprepitant, has conducted a phase 2 trial assessing the pharmacokinetics, pharmacodynamics, safety, and tolerability of fosaprepitant for the prevention of chemotherapy-induced nausea and vomiting in children.
Patients ages 2 to 17 were randomized to receive 1 of 4 doses of fosaprepitant (0.4 mg/kg, 1.2 mg/kg, 3 mg/kg, and 5 mg/kg) or placebo in cycle 1. All patients also received ondansetron, with or without dexamethasone. Patients ages 0 to 11 were invited to participate in optional cycles 2 to 6, during which they received fosaprepitant at 3 mg/kg or 5 mg/kg.
Results from this trial have been posted on its clinicaltrials.gov page (NCT01697579).
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended changing the terms of marketing authorization for fosaprepitant (Ivemend).
The product is already approved in the European Union (EU) for the prevention of acute and delayed nausea and vomiting associated with moderately or highly emetogenic cancer chemotherapy in adults.
Now, the CHMP is recommending that fosaprepitant be authorized for the same indication in pediatric patients age 6 months and older.
As it is in adults, fosaprepitant would be given to children as part of combination therapy.
The CHMP’s opinion on fosaprepitant will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the EU. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
Merck Sharp & Dohme Corp., the company developing fosaprepitant, has conducted a phase 2 trial assessing the pharmacokinetics, pharmacodynamics, safety, and tolerability of fosaprepitant for the prevention of chemotherapy-induced nausea and vomiting in children.
Patients ages 2 to 17 were randomized to receive 1 of 4 doses of fosaprepitant (0.4 mg/kg, 1.2 mg/kg, 3 mg/kg, and 5 mg/kg) or placebo in cycle 1. All patients also received ondansetron, with or without dexamethasone. Patients ages 0 to 11 were invited to participate in optional cycles 2 to 6, during which they received fosaprepitant at 3 mg/kg or 5 mg/kg.
Results from this trial have been posted on its clinicaltrials.gov page (NCT01697579).
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended changing the terms of marketing authorization for fosaprepitant (Ivemend).
The product is already approved in the European Union (EU) for the prevention of acute and delayed nausea and vomiting associated with moderately or highly emetogenic cancer chemotherapy in adults.
Now, the CHMP is recommending that fosaprepitant be authorized for the same indication in pediatric patients age 6 months and older.
As it is in adults, fosaprepitant would be given to children as part of combination therapy.
The CHMP’s opinion on fosaprepitant will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the EU. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
Merck Sharp & Dohme Corp., the company developing fosaprepitant, has conducted a phase 2 trial assessing the pharmacokinetics, pharmacodynamics, safety, and tolerability of fosaprepitant for the prevention of chemotherapy-induced nausea and vomiting in children.
Patients ages 2 to 17 were randomized to receive 1 of 4 doses of fosaprepitant (0.4 mg/kg, 1.2 mg/kg, 3 mg/kg, and 5 mg/kg) or placebo in cycle 1. All patients also received ondansetron, with or without dexamethasone. Patients ages 0 to 11 were invited to participate in optional cycles 2 to 6, during which they received fosaprepitant at 3 mg/kg or 5 mg/kg.
Results from this trial have been posted on its clinicaltrials.gov page (NCT01697579).
Antibody protects mice from malaria infection
A human antibody can protect mice from infection with the malaria parasite Plasmodium falciparum, according to research published in Nature Medicine.
Researchers isolated the antibody, CIS43, from the blood of a volunteer who had received the PfSPZ Vaccine (Sanaria Inc.), an experimental vaccine made from whole, weakened malaria parasites.
The volunteer was later exposed to infectious malaria-carrying mosquitoes under carefully controlled conditions and did not become infected.
Researchers tested CIS43 in 2 different mouse models and found the antibody provided “high-level” protection from malaria infection.
In fact, CIS43 protects against malaria better than any antibody that has been described before, according to study author Marie Pancera, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington.
She and her colleagues found that CIS43 works by binding to an epitope located between the N terminus and central repeat domains of PfCP (P falciparum circumsporozoite protein).
This epitope is conserved across 99.8% of all known P falciparum strains, which, according to the researchers, makes it an attractive target for next-generation vaccines designed to elicit production of CIS43.
Researchers at the National Institute of Allergy and Infectious Diseases Vaccine Research Center are planning to conduct clinical trials of CIS43 next year.
A human antibody can protect mice from infection with the malaria parasite Plasmodium falciparum, according to research published in Nature Medicine.
Researchers isolated the antibody, CIS43, from the blood of a volunteer who had received the PfSPZ Vaccine (Sanaria Inc.), an experimental vaccine made from whole, weakened malaria parasites.
The volunteer was later exposed to infectious malaria-carrying mosquitoes under carefully controlled conditions and did not become infected.
Researchers tested CIS43 in 2 different mouse models and found the antibody provided “high-level” protection from malaria infection.
In fact, CIS43 protects against malaria better than any antibody that has been described before, according to study author Marie Pancera, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington.
She and her colleagues found that CIS43 works by binding to an epitope located between the N terminus and central repeat domains of PfCP (P falciparum circumsporozoite protein).
This epitope is conserved across 99.8% of all known P falciparum strains, which, according to the researchers, makes it an attractive target for next-generation vaccines designed to elicit production of CIS43.
Researchers at the National Institute of Allergy and Infectious Diseases Vaccine Research Center are planning to conduct clinical trials of CIS43 next year.
A human antibody can protect mice from infection with the malaria parasite Plasmodium falciparum, according to research published in Nature Medicine.
Researchers isolated the antibody, CIS43, from the blood of a volunteer who had received the PfSPZ Vaccine (Sanaria Inc.), an experimental vaccine made from whole, weakened malaria parasites.
The volunteer was later exposed to infectious malaria-carrying mosquitoes under carefully controlled conditions and did not become infected.
Researchers tested CIS43 in 2 different mouse models and found the antibody provided “high-level” protection from malaria infection.
In fact, CIS43 protects against malaria better than any antibody that has been described before, according to study author Marie Pancera, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington.
She and her colleagues found that CIS43 works by binding to an epitope located between the N terminus and central repeat domains of PfCP (P falciparum circumsporozoite protein).
This epitope is conserved across 99.8% of all known P falciparum strains, which, according to the researchers, makes it an attractive target for next-generation vaccines designed to elicit production of CIS43.
Researchers at the National Institute of Allergy and Infectious Diseases Vaccine Research Center are planning to conduct clinical trials of CIS43 next year.
How US healthcare compares to other countries
The US has similar healthcare utilization as other high-income countries but spends more and tends to have worse health outcomes, according to a new study.
In 2016, the US spent 17.8% of its gross domestic product on healthcare. For 10 other high-income countries, spending ranged from 9.6% to 12.4%.
However, sizes of physician and nursing workforces were comparable between the countries, numbers of hospital discharges were similar, and lengths of hospital stay were lower in the US than in most other countries.
Meanwhile, the US had the lowest life expectancy and the highest rate of infant mortality.
This research was published in JAMA.
“There’s been a lot of interest in international comparisons between America and other high-income countries, and there’s been a lot of vagueness about why exactly our [US] spending is so much higher and our health outcomes are not necessarily better and often worse,” said study author Ashish K. Jha, MD, of Harvard T. H. Chan School of Public Health in Boston, Massachusetts.
“This study really tries to fill in gaps, I think, across a wide range of issues, from structural capacity to utilization to prices to outcomes.”
For this study, Dr Jha and his colleagues analyzed recent healthcare data, primarily from 2013 to 2016. The team compared differences in healthcare spending, performance, and structural features between the US and 10 high-income countries—UK, Canada, Germany, Australia, Japan, Sweden, France, Netherlands, Switzerland, and Denmark.
Spending
In 2016, healthcare spending, as a percentage of gross domestic product, was as follows:
US—17.8%
Switzerland—12.4%
Sweden—11.9%
Germany—11.3%
France—11%
Japan—10.9%
Denmark—10.8%
Netherlands—10.5%
Canada—10.3%
UK—9.7%
Australia—9.6%.
“The big differences in spending really seem to be driven by prices,” Dr Jha said, noting that salaries for doctors and nurses, administrative expenditures, and pharmaceutical costs are “much higher” in the US.
The total spending on pharmaceuticals per capita was $1443 in the US but ranged from $466 (Netherlands) to $939 (Switzerland) in the other countries.
Administrative costs accounted for 8% of the total national health expenditure in the US but 1% (France, Japan) to 3% (Germany) in the other countries.
Outpatient care expenditures ranged from 22% (Netherlands) to 42% (US). Inpatient care expenditures ranged from 17% (Canada) to 32% (Netherlands), with 19% for the US. And expenditures for medical goods ranged from 10% (Denmark) to 20% (Germany), with the US at 14%.
Physicians’ and nurses’ salaries were higher in the US than other countries. For example, generalist physicians earned $218,173 in the US in 2016 but anywhere from $86,607 (Sweden) to $154,126 (Germany) in the other countries.
Utilization
Although US doctors and nurses earned more than their counterparts in comparator countries, there were no substantial between-country differences in the size of the physician and nursing workforces.
The number of working physicians for every 1000 people ranged from 2.1 (UK) to 4.3 (Switzerland), with the US at 2.6. The number of working nurses for every 1000 people ranged from 8.2 (UK) to 17.4 (Switzerland), with 11.1 for the US.
The US had comparable numbers of hospital beds as some of the other countries. The range was 2.5 (Sweden) to 13.2 (Japan) beds per 1000 people, with the US at 2.8.
The US ranked 6th when it came to hospital discharges for acute myocardial infarction (AMI, 192 per 100,000 people; range, 89 to 287), mental and behavioral issues (679 per 100,000 people; range, 119 to 1719), pneumonia (365 per 100,000 people; range, 187 to 567), and chronic obstructive pulmonary disease (230 per 100,000 people; range, 45 to 352).
The US had greater utilization of computed tomography than the other countries, with 245 examinations per 1000 people (range for other countries, 79 to 231). And US utilization of magnetic resonance imaging was higher than most countries, with 118 examinations per 1000 people (range, 41 to 131).
However, the US ranked on the lower end of the spectrum for length of hospital stay. The length of stay for a “normal delivery” childbirth ranged from a median of 1.5 days (UK) to 5.7 days (Japan), with the US clocking in at 2 days. The median length of stay for AMI ranged from a median of 3.9 days (Netherlands) to 10.3 days (Germany), with the US at 5.4 days.
“So much of the debate about healthcare these days is about over-utilization—that somehow our health system is uniquely bad at avoiding unnecessary services,” Dr Jha said. “I think these data really put that argument to rest. Except for a few pockets, utilization is not really different between us and these high-income Northern European countries, so maybe we need to spend a little less time focusing on that and a little bit more time focusing on prices of our healthcare system.”
Outcomes
The US ranked on the lower end of the spectrum for some mortality outcomes. Thirty-day stroke mortality per 1000 patients ranged from 4.2 in the US to 10 in Canada. Thirty-day AMI mortality per 1000 ranged from 4.1 (Australia) to 8.7 (Germany), with the US at 5.5.
However, infant mortality was highest in the US, at 5.8 deaths per 1000 live births (range for other countries, 2.1 to 5.1). And life expectancy was lowest in the US, at 78.8 years (range for other countries, 80.7 to 83.9).
The researchers noted that the US had the highest percentage of overweight or obese individuals age 15 and older, at 70.1% (range for other countries, 23.8% to 63.4%), but a low percentage of smokers (11.4%; range, 11.2% to 22.4%) and moderate alcohol consumption (8.8 L per capita; range, 7.2 to 11.9).
Limitations of this study include some differences in approaches to collecting and standardizing data across countries, as well as missing data for some countries.
The US has similar healthcare utilization as other high-income countries but spends more and tends to have worse health outcomes, according to a new study.
In 2016, the US spent 17.8% of its gross domestic product on healthcare. For 10 other high-income countries, spending ranged from 9.6% to 12.4%.
However, sizes of physician and nursing workforces were comparable between the countries, numbers of hospital discharges were similar, and lengths of hospital stay were lower in the US than in most other countries.
Meanwhile, the US had the lowest life expectancy and the highest rate of infant mortality.
This research was published in JAMA.
“There’s been a lot of interest in international comparisons between America and other high-income countries, and there’s been a lot of vagueness about why exactly our [US] spending is so much higher and our health outcomes are not necessarily better and often worse,” said study author Ashish K. Jha, MD, of Harvard T. H. Chan School of Public Health in Boston, Massachusetts.
“This study really tries to fill in gaps, I think, across a wide range of issues, from structural capacity to utilization to prices to outcomes.”
For this study, Dr Jha and his colleagues analyzed recent healthcare data, primarily from 2013 to 2016. The team compared differences in healthcare spending, performance, and structural features between the US and 10 high-income countries—UK, Canada, Germany, Australia, Japan, Sweden, France, Netherlands, Switzerland, and Denmark.
Spending
In 2016, healthcare spending, as a percentage of gross domestic product, was as follows:
US—17.8%
Switzerland—12.4%
Sweden—11.9%
Germany—11.3%
France—11%
Japan—10.9%
Denmark—10.8%
Netherlands—10.5%
Canada—10.3%
UK—9.7%
Australia—9.6%.
“The big differences in spending really seem to be driven by prices,” Dr Jha said, noting that salaries for doctors and nurses, administrative expenditures, and pharmaceutical costs are “much higher” in the US.
The total spending on pharmaceuticals per capita was $1443 in the US but ranged from $466 (Netherlands) to $939 (Switzerland) in the other countries.
Administrative costs accounted for 8% of the total national health expenditure in the US but 1% (France, Japan) to 3% (Germany) in the other countries.
Outpatient care expenditures ranged from 22% (Netherlands) to 42% (US). Inpatient care expenditures ranged from 17% (Canada) to 32% (Netherlands), with 19% for the US. And expenditures for medical goods ranged from 10% (Denmark) to 20% (Germany), with the US at 14%.
Physicians’ and nurses’ salaries were higher in the US than other countries. For example, generalist physicians earned $218,173 in the US in 2016 but anywhere from $86,607 (Sweden) to $154,126 (Germany) in the other countries.
Utilization
Although US doctors and nurses earned more than their counterparts in comparator countries, there were no substantial between-country differences in the size of the physician and nursing workforces.
The number of working physicians for every 1000 people ranged from 2.1 (UK) to 4.3 (Switzerland), with the US at 2.6. The number of working nurses for every 1000 people ranged from 8.2 (UK) to 17.4 (Switzerland), with 11.1 for the US.
The US had comparable numbers of hospital beds as some of the other countries. The range was 2.5 (Sweden) to 13.2 (Japan) beds per 1000 people, with the US at 2.8.
The US ranked 6th when it came to hospital discharges for acute myocardial infarction (AMI, 192 per 100,000 people; range, 89 to 287), mental and behavioral issues (679 per 100,000 people; range, 119 to 1719), pneumonia (365 per 100,000 people; range, 187 to 567), and chronic obstructive pulmonary disease (230 per 100,000 people; range, 45 to 352).
The US had greater utilization of computed tomography than the other countries, with 245 examinations per 1000 people (range for other countries, 79 to 231). And US utilization of magnetic resonance imaging was higher than most countries, with 118 examinations per 1000 people (range, 41 to 131).
However, the US ranked on the lower end of the spectrum for length of hospital stay. The length of stay for a “normal delivery” childbirth ranged from a median of 1.5 days (UK) to 5.7 days (Japan), with the US clocking in at 2 days. The median length of stay for AMI ranged from a median of 3.9 days (Netherlands) to 10.3 days (Germany), with the US at 5.4 days.
“So much of the debate about healthcare these days is about over-utilization—that somehow our health system is uniquely bad at avoiding unnecessary services,” Dr Jha said. “I think these data really put that argument to rest. Except for a few pockets, utilization is not really different between us and these high-income Northern European countries, so maybe we need to spend a little less time focusing on that and a little bit more time focusing on prices of our healthcare system.”
Outcomes
The US ranked on the lower end of the spectrum for some mortality outcomes. Thirty-day stroke mortality per 1000 patients ranged from 4.2 in the US to 10 in Canada. Thirty-day AMI mortality per 1000 ranged from 4.1 (Australia) to 8.7 (Germany), with the US at 5.5.
However, infant mortality was highest in the US, at 5.8 deaths per 1000 live births (range for other countries, 2.1 to 5.1). And life expectancy was lowest in the US, at 78.8 years (range for other countries, 80.7 to 83.9).
The researchers noted that the US had the highest percentage of overweight or obese individuals age 15 and older, at 70.1% (range for other countries, 23.8% to 63.4%), but a low percentage of smokers (11.4%; range, 11.2% to 22.4%) and moderate alcohol consumption (8.8 L per capita; range, 7.2 to 11.9).
Limitations of this study include some differences in approaches to collecting and standardizing data across countries, as well as missing data for some countries.
The US has similar healthcare utilization as other high-income countries but spends more and tends to have worse health outcomes, according to a new study.
In 2016, the US spent 17.8% of its gross domestic product on healthcare. For 10 other high-income countries, spending ranged from 9.6% to 12.4%.
However, sizes of physician and nursing workforces were comparable between the countries, numbers of hospital discharges were similar, and lengths of hospital stay were lower in the US than in most other countries.
Meanwhile, the US had the lowest life expectancy and the highest rate of infant mortality.
This research was published in JAMA.
“There’s been a lot of interest in international comparisons between America and other high-income countries, and there’s been a lot of vagueness about why exactly our [US] spending is so much higher and our health outcomes are not necessarily better and often worse,” said study author Ashish K. Jha, MD, of Harvard T. H. Chan School of Public Health in Boston, Massachusetts.
“This study really tries to fill in gaps, I think, across a wide range of issues, from structural capacity to utilization to prices to outcomes.”
For this study, Dr Jha and his colleagues analyzed recent healthcare data, primarily from 2013 to 2016. The team compared differences in healthcare spending, performance, and structural features between the US and 10 high-income countries—UK, Canada, Germany, Australia, Japan, Sweden, France, Netherlands, Switzerland, and Denmark.
Spending
In 2016, healthcare spending, as a percentage of gross domestic product, was as follows:
US—17.8%
Switzerland—12.4%
Sweden—11.9%
Germany—11.3%
France—11%
Japan—10.9%
Denmark—10.8%
Netherlands—10.5%
Canada—10.3%
UK—9.7%
Australia—9.6%.
“The big differences in spending really seem to be driven by prices,” Dr Jha said, noting that salaries for doctors and nurses, administrative expenditures, and pharmaceutical costs are “much higher” in the US.
The total spending on pharmaceuticals per capita was $1443 in the US but ranged from $466 (Netherlands) to $939 (Switzerland) in the other countries.
Administrative costs accounted for 8% of the total national health expenditure in the US but 1% (France, Japan) to 3% (Germany) in the other countries.
Outpatient care expenditures ranged from 22% (Netherlands) to 42% (US). Inpatient care expenditures ranged from 17% (Canada) to 32% (Netherlands), with 19% for the US. And expenditures for medical goods ranged from 10% (Denmark) to 20% (Germany), with the US at 14%.
Physicians’ and nurses’ salaries were higher in the US than other countries. For example, generalist physicians earned $218,173 in the US in 2016 but anywhere from $86,607 (Sweden) to $154,126 (Germany) in the other countries.
Utilization
Although US doctors and nurses earned more than their counterparts in comparator countries, there were no substantial between-country differences in the size of the physician and nursing workforces.
The number of working physicians for every 1000 people ranged from 2.1 (UK) to 4.3 (Switzerland), with the US at 2.6. The number of working nurses for every 1000 people ranged from 8.2 (UK) to 17.4 (Switzerland), with 11.1 for the US.
The US had comparable numbers of hospital beds as some of the other countries. The range was 2.5 (Sweden) to 13.2 (Japan) beds per 1000 people, with the US at 2.8.
The US ranked 6th when it came to hospital discharges for acute myocardial infarction (AMI, 192 per 100,000 people; range, 89 to 287), mental and behavioral issues (679 per 100,000 people; range, 119 to 1719), pneumonia (365 per 100,000 people; range, 187 to 567), and chronic obstructive pulmonary disease (230 per 100,000 people; range, 45 to 352).
The US had greater utilization of computed tomography than the other countries, with 245 examinations per 1000 people (range for other countries, 79 to 231). And US utilization of magnetic resonance imaging was higher than most countries, with 118 examinations per 1000 people (range, 41 to 131).
However, the US ranked on the lower end of the spectrum for length of hospital stay. The length of stay for a “normal delivery” childbirth ranged from a median of 1.5 days (UK) to 5.7 days (Japan), with the US clocking in at 2 days. The median length of stay for AMI ranged from a median of 3.9 days (Netherlands) to 10.3 days (Germany), with the US at 5.4 days.
“So much of the debate about healthcare these days is about over-utilization—that somehow our health system is uniquely bad at avoiding unnecessary services,” Dr Jha said. “I think these data really put that argument to rest. Except for a few pockets, utilization is not really different between us and these high-income Northern European countries, so maybe we need to spend a little less time focusing on that and a little bit more time focusing on prices of our healthcare system.”
Outcomes
The US ranked on the lower end of the spectrum for some mortality outcomes. Thirty-day stroke mortality per 1000 patients ranged from 4.2 in the US to 10 in Canada. Thirty-day AMI mortality per 1000 ranged from 4.1 (Australia) to 8.7 (Germany), with the US at 5.5.
However, infant mortality was highest in the US, at 5.8 deaths per 1000 live births (range for other countries, 2.1 to 5.1). And life expectancy was lowest in the US, at 78.8 years (range for other countries, 80.7 to 83.9).
The researchers noted that the US had the highest percentage of overweight or obese individuals age 15 and older, at 70.1% (range for other countries, 23.8% to 63.4%), but a low percentage of smokers (11.4%; range, 11.2% to 22.4%) and moderate alcohol consumption (8.8 L per capita; range, 7.2 to 11.9).
Limitations of this study include some differences in approaches to collecting and standardizing data across countries, as well as missing data for some countries.
Clinical trial registries don’t match up
A new study has revealed discrepancies in completion status for trials listed on ClinicalTrials.gov and the EU Clinical Trials Register (EUCTR).
Researchers evaluated nearly 10,500 trials listed on both registries and found that roughly 16% of them were marked as “completed” on one registry and “ongoing” on the other.
Most of these (91%) were listed as “ongoing” on EUCTR but “completed” on ClinicalTrials.gov.
“Trial registries are important public documents,” said Ben Goldacre, of the University of Oxford in the UK.
“Doctors, researchers, and patients rely on the information that trialists post about their clinical trial. Concerningly, we now show that this data is commonly inaccurate.”
Goldacre and his colleague, Jessica Fleminger, also from the University of Oxford, reported these findings in PLOS ONE.
The researchers looked at 10,492 clinical trials that were registered on both ClinicalTrials.gov and EUCTR.
For most of these trials (83.8%, n=8794), completion status was the same on both registries. But there were 1698 trials (16.2%) that were listed as “completed” on one registry and “ongoing” on another.
A majority of the discrepant trials (90.5%, n=1536) were “ongoing” on EUCTR and “complete” on ClinicalTrials.gov.
Overall, 43.1% (4530/10,492) of dual-registered trials were listed as “ongoing” on EUCTR, and 33.9% of these (1536/4530) were listed as “completed” on ClinicalTrials.gov.
Thirty percent (3156/10,492) of dual-registered trials were marked as “ongoing” on ClinicalTrials.gov, and 5.1% (162/3156) of these were marked as “completed” on EUCTR.
Goldacre and Fleminger said it is unclear whether researchers, registry owners, or both are responsible for these errors. Regardless, researchers identifying discrepancies should request clarifications from the trialists, and registry owners should undertake simple cross-checks of data to ensure that completion status is accurate.
A new study has revealed discrepancies in completion status for trials listed on ClinicalTrials.gov and the EU Clinical Trials Register (EUCTR).
Researchers evaluated nearly 10,500 trials listed on both registries and found that roughly 16% of them were marked as “completed” on one registry and “ongoing” on the other.
Most of these (91%) were listed as “ongoing” on EUCTR but “completed” on ClinicalTrials.gov.
“Trial registries are important public documents,” said Ben Goldacre, of the University of Oxford in the UK.
“Doctors, researchers, and patients rely on the information that trialists post about their clinical trial. Concerningly, we now show that this data is commonly inaccurate.”
Goldacre and his colleague, Jessica Fleminger, also from the University of Oxford, reported these findings in PLOS ONE.
The researchers looked at 10,492 clinical trials that were registered on both ClinicalTrials.gov and EUCTR.
For most of these trials (83.8%, n=8794), completion status was the same on both registries. But there were 1698 trials (16.2%) that were listed as “completed” on one registry and “ongoing” on another.
A majority of the discrepant trials (90.5%, n=1536) were “ongoing” on EUCTR and “complete” on ClinicalTrials.gov.
Overall, 43.1% (4530/10,492) of dual-registered trials were listed as “ongoing” on EUCTR, and 33.9% of these (1536/4530) were listed as “completed” on ClinicalTrials.gov.
Thirty percent (3156/10,492) of dual-registered trials were marked as “ongoing” on ClinicalTrials.gov, and 5.1% (162/3156) of these were marked as “completed” on EUCTR.
Goldacre and Fleminger said it is unclear whether researchers, registry owners, or both are responsible for these errors. Regardless, researchers identifying discrepancies should request clarifications from the trialists, and registry owners should undertake simple cross-checks of data to ensure that completion status is accurate.
A new study has revealed discrepancies in completion status for trials listed on ClinicalTrials.gov and the EU Clinical Trials Register (EUCTR).
Researchers evaluated nearly 10,500 trials listed on both registries and found that roughly 16% of them were marked as “completed” on one registry and “ongoing” on the other.
Most of these (91%) were listed as “ongoing” on EUCTR but “completed” on ClinicalTrials.gov.
“Trial registries are important public documents,” said Ben Goldacre, of the University of Oxford in the UK.
“Doctors, researchers, and patients rely on the information that trialists post about their clinical trial. Concerningly, we now show that this data is commonly inaccurate.”
Goldacre and his colleague, Jessica Fleminger, also from the University of Oxford, reported these findings in PLOS ONE.
The researchers looked at 10,492 clinical trials that were registered on both ClinicalTrials.gov and EUCTR.
For most of these trials (83.8%, n=8794), completion status was the same on both registries. But there were 1698 trials (16.2%) that were listed as “completed” on one registry and “ongoing” on another.
A majority of the discrepant trials (90.5%, n=1536) were “ongoing” on EUCTR and “complete” on ClinicalTrials.gov.
Overall, 43.1% (4530/10,492) of dual-registered trials were listed as “ongoing” on EUCTR, and 33.9% of these (1536/4530) were listed as “completed” on ClinicalTrials.gov.
Thirty percent (3156/10,492) of dual-registered trials were marked as “ongoing” on ClinicalTrials.gov, and 5.1% (162/3156) of these were marked as “completed” on EUCTR.
Goldacre and Fleminger said it is unclear whether researchers, registry owners, or both are responsible for these errors. Regardless, researchers identifying discrepancies should request clarifications from the trialists, and registry owners should undertake simple cross-checks of data to ensure that completion status is accurate.
Giving patients control of their healthcare data
The US Centers for Medicare & Medicaid Services (CMS) has announced new initiatives designed to give patients control of their healthcare data.
One initiative, MyHealthEData, is intended to “break down the barriers” that prevent patients from having electronic access to, and control of, their own health records, according to CMS Administrator Seema Verma.
The other initiative, Medicare’s Blue Button 2.0, is a new way for Medicare beneficiaries to access and share their personal health data in a universal digital format.
Verma discussed these programs and other changes CMS is making in a speech at the HIMSS18 Conference in Las Vegas.
MyHealthEData
The Trump Administration is launching MyHealthEData, a government-wide initiative intended to give patients electronic access to their healthcare data and allow patients to take that data with them from healthcare provider to healthcare provider.
The idea is that patients will be able to choose the provider that best meets their needs and give that provider secure access to their data.
“MyHealthEData makes it clear that patients should have access and control to share their data with whomever they want, making the patient the center of our healthcare system,” Verma said.
“Patients need to be able to control their information and know that it’s secure and private. Having access to their medical information will help them make decisions about their care and have a better understanding of their health.”
The MyHealthEData initiative is led by the White House Office of American Innovation, with participation from the Department of Health and Human Services and its CMS, Office of the National Coordinator for Health Information Technology, and National Institutes of Health, as well as the Department of Veterans Affairs.
Blue Button 2.0
Verma said Medicare’s Blue Button 2.0 will enable patients who participate in the traditional Medicare program to connect their claims data to the secure applications, providers, services, and research programs they trust.
“Beneficiaries will maintain complete control in how and when their data is used . . .,” Verma said.
In addition, Medicare’s Blue Button 2.0 is expected to foster increased competition among technology innovators to serve Medicare patients and their caregivers. More than 100 organizations have signed on to use Medicare’s Blue Button 2.0 to develop applications that will provide new tools to help patients manage their health.
“CMS serves more than 130 million beneficiaries through our programs, which means we are uniquely positioned to transform how important healthcare data is shared between patients and their doctors,” Verma said.
“Today, we are calling on private health plans to join us in sharing their data with patients because enabling patients to control their Medicare data so that they can quickly obtain and share it is critical to creating more patient empowerment.”
Additional changes
Verma announced that CMS intends to overhaul its Electronic Health Record (EHR) Incentive Programs to refocus them on interoperability and reduce the time and cost required of providers to comply with the programs’ requirements.
Verma also noted that CMS has implemented laws regarding information blocking, a practice in which providers prevent patients from accessing their data. Under some CMS programs, hospitals and clinicians must show they have not engaged in information-blocking activities.
Other ways in which CMS plans to empower patients with data include:
- Requiring providers to update their systems to ensure data sharing
- Requiring that patients’ data follow them after they are discharged from the hospital
- Working to streamline documentation and billing requirements for providers to allow doctors to spend more time with their patients
- Working to reduce the incidence of unnecessary and duplicative testing, which occurs as a result of providers not sharing data.
The US Centers for Medicare & Medicaid Services (CMS) has announced new initiatives designed to give patients control of their healthcare data.
One initiative, MyHealthEData, is intended to “break down the barriers” that prevent patients from having electronic access to, and control of, their own health records, according to CMS Administrator Seema Verma.
The other initiative, Medicare’s Blue Button 2.0, is a new way for Medicare beneficiaries to access and share their personal health data in a universal digital format.
Verma discussed these programs and other changes CMS is making in a speech at the HIMSS18 Conference in Las Vegas.
MyHealthEData
The Trump Administration is launching MyHealthEData, a government-wide initiative intended to give patients electronic access to their healthcare data and allow patients to take that data with them from healthcare provider to healthcare provider.
The idea is that patients will be able to choose the provider that best meets their needs and give that provider secure access to their data.
“MyHealthEData makes it clear that patients should have access and control to share their data with whomever they want, making the patient the center of our healthcare system,” Verma said.
“Patients need to be able to control their information and know that it’s secure and private. Having access to their medical information will help them make decisions about their care and have a better understanding of their health.”
The MyHealthEData initiative is led by the White House Office of American Innovation, with participation from the Department of Health and Human Services and its CMS, Office of the National Coordinator for Health Information Technology, and National Institutes of Health, as well as the Department of Veterans Affairs.
Blue Button 2.0
Verma said Medicare’s Blue Button 2.0 will enable patients who participate in the traditional Medicare program to connect their claims data to the secure applications, providers, services, and research programs they trust.
“Beneficiaries will maintain complete control in how and when their data is used . . .,” Verma said.
In addition, Medicare’s Blue Button 2.0 is expected to foster increased competition among technology innovators to serve Medicare patients and their caregivers. More than 100 organizations have signed on to use Medicare’s Blue Button 2.0 to develop applications that will provide new tools to help patients manage their health.
“CMS serves more than 130 million beneficiaries through our programs, which means we are uniquely positioned to transform how important healthcare data is shared between patients and their doctors,” Verma said.
“Today, we are calling on private health plans to join us in sharing their data with patients because enabling patients to control their Medicare data so that they can quickly obtain and share it is critical to creating more patient empowerment.”
Additional changes
Verma announced that CMS intends to overhaul its Electronic Health Record (EHR) Incentive Programs to refocus them on interoperability and reduce the time and cost required of providers to comply with the programs’ requirements.
Verma also noted that CMS has implemented laws regarding information blocking, a practice in which providers prevent patients from accessing their data. Under some CMS programs, hospitals and clinicians must show they have not engaged in information-blocking activities.
Other ways in which CMS plans to empower patients with data include:
- Requiring providers to update their systems to ensure data sharing
- Requiring that patients’ data follow them after they are discharged from the hospital
- Working to streamline documentation and billing requirements for providers to allow doctors to spend more time with their patients
- Working to reduce the incidence of unnecessary and duplicative testing, which occurs as a result of providers not sharing data.
The US Centers for Medicare & Medicaid Services (CMS) has announced new initiatives designed to give patients control of their healthcare data.
One initiative, MyHealthEData, is intended to “break down the barriers” that prevent patients from having electronic access to, and control of, their own health records, according to CMS Administrator Seema Verma.
The other initiative, Medicare’s Blue Button 2.0, is a new way for Medicare beneficiaries to access and share their personal health data in a universal digital format.
Verma discussed these programs and other changes CMS is making in a speech at the HIMSS18 Conference in Las Vegas.
MyHealthEData
The Trump Administration is launching MyHealthEData, a government-wide initiative intended to give patients electronic access to their healthcare data and allow patients to take that data with them from healthcare provider to healthcare provider.
The idea is that patients will be able to choose the provider that best meets their needs and give that provider secure access to their data.
“MyHealthEData makes it clear that patients should have access and control to share their data with whomever they want, making the patient the center of our healthcare system,” Verma said.
“Patients need to be able to control their information and know that it’s secure and private. Having access to their medical information will help them make decisions about their care and have a better understanding of their health.”
The MyHealthEData initiative is led by the White House Office of American Innovation, with participation from the Department of Health and Human Services and its CMS, Office of the National Coordinator for Health Information Technology, and National Institutes of Health, as well as the Department of Veterans Affairs.
Blue Button 2.0
Verma said Medicare’s Blue Button 2.0 will enable patients who participate in the traditional Medicare program to connect their claims data to the secure applications, providers, services, and research programs they trust.
“Beneficiaries will maintain complete control in how and when their data is used . . .,” Verma said.
In addition, Medicare’s Blue Button 2.0 is expected to foster increased competition among technology innovators to serve Medicare patients and their caregivers. More than 100 organizations have signed on to use Medicare’s Blue Button 2.0 to develop applications that will provide new tools to help patients manage their health.
“CMS serves more than 130 million beneficiaries through our programs, which means we are uniquely positioned to transform how important healthcare data is shared between patients and their doctors,” Verma said.
“Today, we are calling on private health plans to join us in sharing their data with patients because enabling patients to control their Medicare data so that they can quickly obtain and share it is critical to creating more patient empowerment.”
Additional changes
Verma announced that CMS intends to overhaul its Electronic Health Record (EHR) Incentive Programs to refocus them on interoperability and reduce the time and cost required of providers to comply with the programs’ requirements.
Verma also noted that CMS has implemented laws regarding information blocking, a practice in which providers prevent patients from accessing their data. Under some CMS programs, hospitals and clinicians must show they have not engaged in information-blocking activities.
Other ways in which CMS plans to empower patients with data include:
- Requiring providers to update their systems to ensure data sharing
- Requiring that patients’ data follow them after they are discharged from the hospital
- Working to streamline documentation and billing requirements for providers to allow doctors to spend more time with their patients
- Working to reduce the incidence of unnecessary and duplicative testing, which occurs as a result of providers not sharing data.
CHMP endorses drug delivery system
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended a label variation for Neulasta® (pegfilgrastim) to include the Neulasta® Onpro® Kit.
The Neulasta Onpro Kit is an on-body injector (OBI) delivery system for Neulasta, which is approved in the European Union to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults treated with cytotoxic chemotherapy for malignancy (with the exception of chronic myeloid leukemia and myelodysplastic syndromes).
The Neulasta Onpro Kit includes a specifically designed Neulasta pre-filled syringe along with a single-use OBI. The small, lightweight OBI is applied to a patient’s skin on the same day of chemotherapy.
The OBI is intended to facilitate timed delivery of the correct dose of Neulasta and eliminate the need for patients to return to a healthcare setting the day after they receive chemotherapy.
The CHMP’s opinion on the Neulasta Onpro Kit will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the centralized marketing authorization of Neulasta will be updated to include information on the Neulasta Onpro Kit in the drug’s label.
This change will be valid throughout the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions about Neulasta’s label on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended a label variation for Neulasta® (pegfilgrastim) to include the Neulasta® Onpro® Kit.
The Neulasta Onpro Kit is an on-body injector (OBI) delivery system for Neulasta, which is approved in the European Union to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults treated with cytotoxic chemotherapy for malignancy (with the exception of chronic myeloid leukemia and myelodysplastic syndromes).
The Neulasta Onpro Kit includes a specifically designed Neulasta pre-filled syringe along with a single-use OBI. The small, lightweight OBI is applied to a patient’s skin on the same day of chemotherapy.
The OBI is intended to facilitate timed delivery of the correct dose of Neulasta and eliminate the need for patients to return to a healthcare setting the day after they receive chemotherapy.
The CHMP’s opinion on the Neulasta Onpro Kit will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the centralized marketing authorization of Neulasta will be updated to include information on the Neulasta Onpro Kit in the drug’s label.
This change will be valid throughout the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions about Neulasta’s label on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended a label variation for Neulasta® (pegfilgrastim) to include the Neulasta® Onpro® Kit.
The Neulasta Onpro Kit is an on-body injector (OBI) delivery system for Neulasta, which is approved in the European Union to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults treated with cytotoxic chemotherapy for malignancy (with the exception of chronic myeloid leukemia and myelodysplastic syndromes).
The Neulasta Onpro Kit includes a specifically designed Neulasta pre-filled syringe along with a single-use OBI. The small, lightweight OBI is applied to a patient’s skin on the same day of chemotherapy.
The OBI is intended to facilitate timed delivery of the correct dose of Neulasta and eliminate the need for patients to return to a healthcare setting the day after they receive chemotherapy.
The CHMP’s opinion on the Neulasta Onpro Kit will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the centralized marketing authorization of Neulasta will be updated to include information on the Neulasta Onpro Kit in the drug’s label.
This change will be valid throughout the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions about Neulasta’s label on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
AYA cancer patients lost to follow-up
ORLANDO—Many adolescent and young adult (AYA) cancer survivors don’t continue with follow-up care, according to a new study.
Researchers analyzed nearly 2400 AYAs diagnosed with cancer between 2000 and 2015 and found that 37% of these patients had no follow-up visits since 2015.
The proportion of patients with follow-up visits in 2016 did not vary according to cancer type or insurance status, but it did vary according to patients’ time since last cancer treatment.
These findings were presented at the 2018 Cancer Survivorship Symposium (abstract 29).
“Many adolescents and young adults are unaware of what their long-term risks are after they have finished their cancer treatment,” said study investigator Lynda M. Beaupin, MD, of the Roswell Park Cancer Institute in Buffalo, New York.
“Doctors and other healthcare providers need to be more diligent in letting these patients know about future potential side effects and health risks that could occur based on certain aspects of their cancer treatment.”
In a previous study, Dr Beaupin and her colleagues conducted a focus group discussion with 27 AYAs, ages 18 to 39, to query them about the major barriers that prevented them from seeking follow-up care.
Among the factors mentioned were poor communication with their oncologists, ongoing problems in adjusting to life as a cancer survivor, and loss of health insurance.
As a follow-up to that focus group session, the investigators looked at a larger group of AYAs who were treated at Roswell Park Comprehensive Cancer Center.
The team analyzed data from the cancer center’s tumor registry, which included information on a patient’s current age, age at cancer diagnosis, gender, date of diagnosis, date of most recent doctor visit, and type of cancer.
The investigators also looked at patient-provided information on follow-up doctor appointments and insurance status for 2 cohorts of AYA cancer survivors. Patients in cohort A were diagnosed with cancer between 2010 and 2014, and patients in cohort B were diagnosed between 2005 and 2009.
The most common types of cancer were leukemia/lymphoma, melanoma, germ cell tumors, and thyroid and breast cancers.
Findings
There were 2367 patients, ages 18 to 39, who were diagnosed with cancer between 2000 and 2015.
Thirty-seven percent of these patients did not have a follow-up visit since 2015.
There was no difference in follow-up contact according to cancer type or insurance status. However, length of time since patients’ final cancer treatment was a factor in not scheduling a follow-up appointment.
Regardless of insurance status, 33% of cohort A (diagnosed 2010-2014) and 48% of cohort B (diagnosed 2005-2009) did not have a follow-up visit in 2016.
Among insured patients, 33% of those in cohort A and 47% of those in cohort B did not have a visit in 2016. Among uninsured patients, the percentages were 39% and 46%, respectively.
Next steps
The investigators hope to conduct future studies looking at other factors that may affect AYAs’ willingness to seek follow-up care, such as employment status, distance to a cancer center, whether they are getting tested or treated at a facility other than a cancer center, and how AYAs perceive their current quality of life.
“These patients have the potential to live a normal lifespan, and we need to educate them to become their own advocates so they may receive follow-up care on a regular basis,” Dr Beaupin said.
“We hope they continue to receive that follow-up at an established cancer center that has the facilities to assess cardiac health and provide rehabilitation if needed. There are now established survivorship programs nationwide that can provide follow-up care for those who have completed treatment.”
This study was supported by the National Cancer Institute.
ORLANDO—Many adolescent and young adult (AYA) cancer survivors don’t continue with follow-up care, according to a new study.
Researchers analyzed nearly 2400 AYAs diagnosed with cancer between 2000 and 2015 and found that 37% of these patients had no follow-up visits since 2015.
The proportion of patients with follow-up visits in 2016 did not vary according to cancer type or insurance status, but it did vary according to patients’ time since last cancer treatment.
These findings were presented at the 2018 Cancer Survivorship Symposium (abstract 29).
“Many adolescents and young adults are unaware of what their long-term risks are after they have finished their cancer treatment,” said study investigator Lynda M. Beaupin, MD, of the Roswell Park Cancer Institute in Buffalo, New York.
“Doctors and other healthcare providers need to be more diligent in letting these patients know about future potential side effects and health risks that could occur based on certain aspects of their cancer treatment.”
In a previous study, Dr Beaupin and her colleagues conducted a focus group discussion with 27 AYAs, ages 18 to 39, to query them about the major barriers that prevented them from seeking follow-up care.
Among the factors mentioned were poor communication with their oncologists, ongoing problems in adjusting to life as a cancer survivor, and loss of health insurance.
As a follow-up to that focus group session, the investigators looked at a larger group of AYAs who were treated at Roswell Park Comprehensive Cancer Center.
The team analyzed data from the cancer center’s tumor registry, which included information on a patient’s current age, age at cancer diagnosis, gender, date of diagnosis, date of most recent doctor visit, and type of cancer.
The investigators also looked at patient-provided information on follow-up doctor appointments and insurance status for 2 cohorts of AYA cancer survivors. Patients in cohort A were diagnosed with cancer between 2010 and 2014, and patients in cohort B were diagnosed between 2005 and 2009.
The most common types of cancer were leukemia/lymphoma, melanoma, germ cell tumors, and thyroid and breast cancers.
Findings
There were 2367 patients, ages 18 to 39, who were diagnosed with cancer between 2000 and 2015.
Thirty-seven percent of these patients did not have a follow-up visit since 2015.
There was no difference in follow-up contact according to cancer type or insurance status. However, length of time since patients’ final cancer treatment was a factor in not scheduling a follow-up appointment.
Regardless of insurance status, 33% of cohort A (diagnosed 2010-2014) and 48% of cohort B (diagnosed 2005-2009) did not have a follow-up visit in 2016.
Among insured patients, 33% of those in cohort A and 47% of those in cohort B did not have a visit in 2016. Among uninsured patients, the percentages were 39% and 46%, respectively.
Next steps
The investigators hope to conduct future studies looking at other factors that may affect AYAs’ willingness to seek follow-up care, such as employment status, distance to a cancer center, whether they are getting tested or treated at a facility other than a cancer center, and how AYAs perceive their current quality of life.
“These patients have the potential to live a normal lifespan, and we need to educate them to become their own advocates so they may receive follow-up care on a regular basis,” Dr Beaupin said.
“We hope they continue to receive that follow-up at an established cancer center that has the facilities to assess cardiac health and provide rehabilitation if needed. There are now established survivorship programs nationwide that can provide follow-up care for those who have completed treatment.”
This study was supported by the National Cancer Institute.
ORLANDO—Many adolescent and young adult (AYA) cancer survivors don’t continue with follow-up care, according to a new study.
Researchers analyzed nearly 2400 AYAs diagnosed with cancer between 2000 and 2015 and found that 37% of these patients had no follow-up visits since 2015.
The proportion of patients with follow-up visits in 2016 did not vary according to cancer type or insurance status, but it did vary according to patients’ time since last cancer treatment.
These findings were presented at the 2018 Cancer Survivorship Symposium (abstract 29).
“Many adolescents and young adults are unaware of what their long-term risks are after they have finished their cancer treatment,” said study investigator Lynda M. Beaupin, MD, of the Roswell Park Cancer Institute in Buffalo, New York.
“Doctors and other healthcare providers need to be more diligent in letting these patients know about future potential side effects and health risks that could occur based on certain aspects of their cancer treatment.”
In a previous study, Dr Beaupin and her colleagues conducted a focus group discussion with 27 AYAs, ages 18 to 39, to query them about the major barriers that prevented them from seeking follow-up care.
Among the factors mentioned were poor communication with their oncologists, ongoing problems in adjusting to life as a cancer survivor, and loss of health insurance.
As a follow-up to that focus group session, the investigators looked at a larger group of AYAs who were treated at Roswell Park Comprehensive Cancer Center.
The team analyzed data from the cancer center’s tumor registry, which included information on a patient’s current age, age at cancer diagnosis, gender, date of diagnosis, date of most recent doctor visit, and type of cancer.
The investigators also looked at patient-provided information on follow-up doctor appointments and insurance status for 2 cohorts of AYA cancer survivors. Patients in cohort A were diagnosed with cancer between 2010 and 2014, and patients in cohort B were diagnosed between 2005 and 2009.
The most common types of cancer were leukemia/lymphoma, melanoma, germ cell tumors, and thyroid and breast cancers.
Findings
There were 2367 patients, ages 18 to 39, who were diagnosed with cancer between 2000 and 2015.
Thirty-seven percent of these patients did not have a follow-up visit since 2015.
There was no difference in follow-up contact according to cancer type or insurance status. However, length of time since patients’ final cancer treatment was a factor in not scheduling a follow-up appointment.
Regardless of insurance status, 33% of cohort A (diagnosed 2010-2014) and 48% of cohort B (diagnosed 2005-2009) did not have a follow-up visit in 2016.
Among insured patients, 33% of those in cohort A and 47% of those in cohort B did not have a visit in 2016. Among uninsured patients, the percentages were 39% and 46%, respectively.
Next steps
The investigators hope to conduct future studies looking at other factors that may affect AYAs’ willingness to seek follow-up care, such as employment status, distance to a cancer center, whether they are getting tested or treated at a facility other than a cancer center, and how AYAs perceive their current quality of life.
“These patients have the potential to live a normal lifespan, and we need to educate them to become their own advocates so they may receive follow-up care on a regular basis,” Dr Beaupin said.
“We hope they continue to receive that follow-up at an established cancer center that has the facilities to assess cardiac health and provide rehabilitation if needed. There are now established survivorship programs nationwide that can provide follow-up care for those who have completed treatment.”
This study was supported by the National Cancer Institute.