User login
Top reads from the CHEST journal portfolio
Studying endotypes in sleep apnea, diagnostic testing in ILD, and inhaled corticosteroid use in children
Journal CHEST®
By Xiaoting Wang, MM, and colleagues
This study from the Shanghai Sleep Health Study cohort enhances our understanding of physiologic endotypes in sleep apnea—nonpositional OSA (NPOSA) and positional OSA (POSA). The study found that nonanatomic traits play a more significant role in POSA severity. Patients with POSA exhibited lower arousal thresholds and greater ventilatory compensation, while anatomical abnormalities were more prominent in NPOSA. This research underscores the need for personalized treatment strategies based on specific endotypes, especially with the increasing emergence of alternatives to CPAP therapy, such as mandibular advancement therapy and hypoglossal nerve stimulation. Patients with obesity with NPOSA were found to have elevated loop gain, which is known to be impacted by weight loss. This is particularly relevant in light of recent studies showing that new GLP-1 agonists can dramatically reduce sleep apnea severity. Future research should focus on refining these personalized approaches and integrating alternative treatments to provide a more individualized approach to managing sleep apnea.
– Commentary by Shyam Subramanian, MD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Pulmonary
By Fayez Kheir, MD, and colleagues
The novel mRNA genomic array, Envisia Genomic Classifier (EGC), used in this study has been shown to be highly specific for a histopathologic diagnosis of usual interstitial pneumonia (UIP). A diagnosis of UIP carries significant prognostic import as patients exhibit a higher risk for progressive fibrosis and death compared with other interstitial lung diseases (ILDs). In this retrospective study, the combination of bronchoscopic lung cryobiopsy and EGC testing was associated with a significant change in clinical management of those living with an indeterminate ILD. Participants were more likely to be started on antifibrotic therapy following this intervention. This study emphasizes the need for prospective trials on the diagnostic yield of molecular phenotyping with bronchoscopic lung biopsy compared with the traditional surgical approach for the undifferentiated ILD.
– Commentary by Michael Marll, MD, Member of the CHEST Physician Editorial Board
CHEST® Critical Care
By Elizabeth Landzberg, MD, and colleagues
Respiratory illness is the most common reason for both hospitalization and ICU admission in children. Studies suggest inhaled corticosteroids (ICSs) may protect adults with direct lung injury (DLI) from developing respiratory failure. However, there is a paucity of literature on this therapeutic intervention within the pediatric population. This retrospective, large, single-center study identified children seeking treatment at the emergency department (ED) with DLI before hospitalization. ICS use before hospitalization was associated with one-half the odds of escalation to intubation and noninvasive respiratory support (NRS) in pediatric patients seeking treatment in the ED with DLI. The protective effect was greatest in patients with a history of asthma. According to the authors, this is the first study to assess ICS exposure before hospitalization and progression to respiratory failure in all-cause pediatric DLI. It highlights the need for future studies to evaluate whether a role exists for early prophylactic ICS use in pediatric DLI without status asthmaticus, stratified by history of asthma.
– Commentary by Anne C. Coates, MD, FCCP, Member of the CHEST Physician Editorial Board
Studying endotypes in sleep apnea, diagnostic testing in ILD, and inhaled corticosteroid use in children
Studying endotypes in sleep apnea, diagnostic testing in ILD, and inhaled corticosteroid use in children
Journal CHEST®
By Xiaoting Wang, MM, and colleagues
This study from the Shanghai Sleep Health Study cohort enhances our understanding of physiologic endotypes in sleep apnea—nonpositional OSA (NPOSA) and positional OSA (POSA). The study found that nonanatomic traits play a more significant role in POSA severity. Patients with POSA exhibited lower arousal thresholds and greater ventilatory compensation, while anatomical abnormalities were more prominent in NPOSA. This research underscores the need for personalized treatment strategies based on specific endotypes, especially with the increasing emergence of alternatives to CPAP therapy, such as mandibular advancement therapy and hypoglossal nerve stimulation. Patients with obesity with NPOSA were found to have elevated loop gain, which is known to be impacted by weight loss. This is particularly relevant in light of recent studies showing that new GLP-1 agonists can dramatically reduce sleep apnea severity. Future research should focus on refining these personalized approaches and integrating alternative treatments to provide a more individualized approach to managing sleep apnea.
– Commentary by Shyam Subramanian, MD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Pulmonary
By Fayez Kheir, MD, and colleagues
The novel mRNA genomic array, Envisia Genomic Classifier (EGC), used in this study has been shown to be highly specific for a histopathologic diagnosis of usual interstitial pneumonia (UIP). A diagnosis of UIP carries significant prognostic import as patients exhibit a higher risk for progressive fibrosis and death compared with other interstitial lung diseases (ILDs). In this retrospective study, the combination of bronchoscopic lung cryobiopsy and EGC testing was associated with a significant change in clinical management of those living with an indeterminate ILD. Participants were more likely to be started on antifibrotic therapy following this intervention. This study emphasizes the need for prospective trials on the diagnostic yield of molecular phenotyping with bronchoscopic lung biopsy compared with the traditional surgical approach for the undifferentiated ILD.
– Commentary by Michael Marll, MD, Member of the CHEST Physician Editorial Board
CHEST® Critical Care
By Elizabeth Landzberg, MD, and colleagues
Respiratory illness is the most common reason for both hospitalization and ICU admission in children. Studies suggest inhaled corticosteroids (ICSs) may protect adults with direct lung injury (DLI) from developing respiratory failure. However, there is a paucity of literature on this therapeutic intervention within the pediatric population. This retrospective, large, single-center study identified children seeking treatment at the emergency department (ED) with DLI before hospitalization. ICS use before hospitalization was associated with one-half the odds of escalation to intubation and noninvasive respiratory support (NRS) in pediatric patients seeking treatment in the ED with DLI. The protective effect was greatest in patients with a history of asthma. According to the authors, this is the first study to assess ICS exposure before hospitalization and progression to respiratory failure in all-cause pediatric DLI. It highlights the need for future studies to evaluate whether a role exists for early prophylactic ICS use in pediatric DLI without status asthmaticus, stratified by history of asthma.
– Commentary by Anne C. Coates, MD, FCCP, Member of the CHEST Physician Editorial Board
Journal CHEST®
By Xiaoting Wang, MM, and colleagues
This study from the Shanghai Sleep Health Study cohort enhances our understanding of physiologic endotypes in sleep apnea—nonpositional OSA (NPOSA) and positional OSA (POSA). The study found that nonanatomic traits play a more significant role in POSA severity. Patients with POSA exhibited lower arousal thresholds and greater ventilatory compensation, while anatomical abnormalities were more prominent in NPOSA. This research underscores the need for personalized treatment strategies based on specific endotypes, especially with the increasing emergence of alternatives to CPAP therapy, such as mandibular advancement therapy and hypoglossal nerve stimulation. Patients with obesity with NPOSA were found to have elevated loop gain, which is known to be impacted by weight loss. This is particularly relevant in light of recent studies showing that new GLP-1 agonists can dramatically reduce sleep apnea severity. Future research should focus on refining these personalized approaches and integrating alternative treatments to provide a more individualized approach to managing sleep apnea.
– Commentary by Shyam Subramanian, MD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Pulmonary
By Fayez Kheir, MD, and colleagues
The novel mRNA genomic array, Envisia Genomic Classifier (EGC), used in this study has been shown to be highly specific for a histopathologic diagnosis of usual interstitial pneumonia (UIP). A diagnosis of UIP carries significant prognostic import as patients exhibit a higher risk for progressive fibrosis and death compared with other interstitial lung diseases (ILDs). In this retrospective study, the combination of bronchoscopic lung cryobiopsy and EGC testing was associated with a significant change in clinical management of those living with an indeterminate ILD. Participants were more likely to be started on antifibrotic therapy following this intervention. This study emphasizes the need for prospective trials on the diagnostic yield of molecular phenotyping with bronchoscopic lung biopsy compared with the traditional surgical approach for the undifferentiated ILD.
– Commentary by Michael Marll, MD, Member of the CHEST Physician Editorial Board
CHEST® Critical Care
By Elizabeth Landzberg, MD, and colleagues
Respiratory illness is the most common reason for both hospitalization and ICU admission in children. Studies suggest inhaled corticosteroids (ICSs) may protect adults with direct lung injury (DLI) from developing respiratory failure. However, there is a paucity of literature on this therapeutic intervention within the pediatric population. This retrospective, large, single-center study identified children seeking treatment at the emergency department (ED) with DLI before hospitalization. ICS use before hospitalization was associated with one-half the odds of escalation to intubation and noninvasive respiratory support (NRS) in pediatric patients seeking treatment in the ED with DLI. The protective effect was greatest in patients with a history of asthma. According to the authors, this is the first study to assess ICS exposure before hospitalization and progression to respiratory failure in all-cause pediatric DLI. It highlights the need for future studies to evaluate whether a role exists for early prophylactic ICS use in pediatric DLI without status asthmaticus, stratified by history of asthma.
– Commentary by Anne C. Coates, MD, FCCP, Member of the CHEST Physician Editorial Board
APPs and POCUS: Overcoming credentialing challenges
APP INTERSECTION
Advanced practice providers (APPs) play an integral role in the care and management of patients both in the ICU and across the spectrum of health care. Due to reduced residency hours and the coming physician shortage, APPs are playing, and will continue to play, a greater role in the care and management of critically ill patients.
Point of care ultrasound (POCUS) is a key diagnostic modality that promotes rapid diagnosis, shortens time to key interventions, and allows for interval reassessment. However, the benefit relies heavily on operator skill to obtain good quality images, interpret this within the context of the patient, and know what interventions, if any, to make. It is imperative that APPs, given their role within critical care, become not only familiar with POCUS but demonstrate proficiency in practice.
Before this can become standard, there are a number of challenges to overcome. Educational institutions are behind on integrating POCUS into the APP curriculum.1 Additionally, APPs have few opportunities to develop these skills as residencies and fellowships are not required prior to entering the workforce. Instead, for a majority of APPs, POCUS training relies on nonstandardized on-the-job training or an (typically expensive) off-site training, for which they may not receive reimbursement. Other barriers include cultural practices that limit POCUS use by APPs; inability to upload and document images obtained; lack of willing, skilled mentors with time to provide feedback and assess for clinical competence; and even accessibility of ultrasound machines.2
Despite these challenges, the clinical benefits of utilizing ultrasound in practice necessitates overcoming these barriers. Institutionally, when APPs perform POCUS, it can lead to more rapid diagnosis and triage of patients, provide billing opportunities, and may reduce overall costs of care. From an APP perspective, having formalized training and credentialing can lead to more consistent POCUS assessment between providers, comprehensive patient care, security in one’s skills and knowledge base, and a tangible way of communicating one’s credibility between institutions.
While some institutions have overcome these barriers and APPs are trained and credentialed in POCUS, this is not always the norm. For this to come to fruition, we need educators to incorporate this into curriculum, colleagues who are willing to mentor learners, cultural changes to allow APPs to develop and utilize necessary skills for practice, clear structure for obtaining and maintaining competency, physicians to champion these efforts, and institutions to credential skilled APPs. Until then, it is important that we as APPs seek to facilitate these institutional changes and continue to set and maintain high quality standards for ourselves.
CHEST 2024 is for APPs too
With more than 300 educational sessions on the CHEST 2024 program, it can be overwhelming to figure out which ones you should put on your schedule. That’s why CHEST asked Danielle McCamey, DNP, CRNP, ACNP-BC, FCCP, and LaDonna Brown, DNP, CRNA, of DNPs of Color (DOC), as well as Corinne Young, MSN, FNP-C, FCCP, of the Association of Pulmonary Advanced Practice Providers (APAPP), for their recommendations on sessions that advanced practice providers shouldn’t miss. Visit chestnet.org/annual-meeting-apps for all of their recommendations.
References
1. Rudy S, Widmar B, Wilbeck J. Ultrasound education for nurse practitioner students: strategies for curricular integration. J Nurse Pract. 2024;20(6):104986.
2. Resnyk J, Weichold A. Barriers to learning and performing point-of-care ultrasound (POCUS): An integrative review. J Prof Nursing. 2024;54:54-62.
APP INTERSECTION
Advanced practice providers (APPs) play an integral role in the care and management of patients both in the ICU and across the spectrum of health care. Due to reduced residency hours and the coming physician shortage, APPs are playing, and will continue to play, a greater role in the care and management of critically ill patients.
Point of care ultrasound (POCUS) is a key diagnostic modality that promotes rapid diagnosis, shortens time to key interventions, and allows for interval reassessment. However, the benefit relies heavily on operator skill to obtain good quality images, interpret this within the context of the patient, and know what interventions, if any, to make. It is imperative that APPs, given their role within critical care, become not only familiar with POCUS but demonstrate proficiency in practice.
Before this can become standard, there are a number of challenges to overcome. Educational institutions are behind on integrating POCUS into the APP curriculum.1 Additionally, APPs have few opportunities to develop these skills as residencies and fellowships are not required prior to entering the workforce. Instead, for a majority of APPs, POCUS training relies on nonstandardized on-the-job training or an (typically expensive) off-site training, for which they may not receive reimbursement. Other barriers include cultural practices that limit POCUS use by APPs; inability to upload and document images obtained; lack of willing, skilled mentors with time to provide feedback and assess for clinical competence; and even accessibility of ultrasound machines.2
Despite these challenges, the clinical benefits of utilizing ultrasound in practice necessitates overcoming these barriers. Institutionally, when APPs perform POCUS, it can lead to more rapid diagnosis and triage of patients, provide billing opportunities, and may reduce overall costs of care. From an APP perspective, having formalized training and credentialing can lead to more consistent POCUS assessment between providers, comprehensive patient care, security in one’s skills and knowledge base, and a tangible way of communicating one’s credibility between institutions.
While some institutions have overcome these barriers and APPs are trained and credentialed in POCUS, this is not always the norm. For this to come to fruition, we need educators to incorporate this into curriculum, colleagues who are willing to mentor learners, cultural changes to allow APPs to develop and utilize necessary skills for practice, clear structure for obtaining and maintaining competency, physicians to champion these efforts, and institutions to credential skilled APPs. Until then, it is important that we as APPs seek to facilitate these institutional changes and continue to set and maintain high quality standards for ourselves.
CHEST 2024 is for APPs too
With more than 300 educational sessions on the CHEST 2024 program, it can be overwhelming to figure out which ones you should put on your schedule. That’s why CHEST asked Danielle McCamey, DNP, CRNP, ACNP-BC, FCCP, and LaDonna Brown, DNP, CRNA, of DNPs of Color (DOC), as well as Corinne Young, MSN, FNP-C, FCCP, of the Association of Pulmonary Advanced Practice Providers (APAPP), for their recommendations on sessions that advanced practice providers shouldn’t miss. Visit chestnet.org/annual-meeting-apps for all of their recommendations.
References
1. Rudy S, Widmar B, Wilbeck J. Ultrasound education for nurse practitioner students: strategies for curricular integration. J Nurse Pract. 2024;20(6):104986.
2. Resnyk J, Weichold A. Barriers to learning and performing point-of-care ultrasound (POCUS): An integrative review. J Prof Nursing. 2024;54:54-62.
APP INTERSECTION
Advanced practice providers (APPs) play an integral role in the care and management of patients both in the ICU and across the spectrum of health care. Due to reduced residency hours and the coming physician shortage, APPs are playing, and will continue to play, a greater role in the care and management of critically ill patients.
Point of care ultrasound (POCUS) is a key diagnostic modality that promotes rapid diagnosis, shortens time to key interventions, and allows for interval reassessment. However, the benefit relies heavily on operator skill to obtain good quality images, interpret this within the context of the patient, and know what interventions, if any, to make. It is imperative that APPs, given their role within critical care, become not only familiar with POCUS but demonstrate proficiency in practice.
Before this can become standard, there are a number of challenges to overcome. Educational institutions are behind on integrating POCUS into the APP curriculum.1 Additionally, APPs have few opportunities to develop these skills as residencies and fellowships are not required prior to entering the workforce. Instead, for a majority of APPs, POCUS training relies on nonstandardized on-the-job training or an (typically expensive) off-site training, for which they may not receive reimbursement. Other barriers include cultural practices that limit POCUS use by APPs; inability to upload and document images obtained; lack of willing, skilled mentors with time to provide feedback and assess for clinical competence; and even accessibility of ultrasound machines.2
Despite these challenges, the clinical benefits of utilizing ultrasound in practice necessitates overcoming these barriers. Institutionally, when APPs perform POCUS, it can lead to more rapid diagnosis and triage of patients, provide billing opportunities, and may reduce overall costs of care. From an APP perspective, having formalized training and credentialing can lead to more consistent POCUS assessment between providers, comprehensive patient care, security in one’s skills and knowledge base, and a tangible way of communicating one’s credibility between institutions.
While some institutions have overcome these barriers and APPs are trained and credentialed in POCUS, this is not always the norm. For this to come to fruition, we need educators to incorporate this into curriculum, colleagues who are willing to mentor learners, cultural changes to allow APPs to develop and utilize necessary skills for practice, clear structure for obtaining and maintaining competency, physicians to champion these efforts, and institutions to credential skilled APPs. Until then, it is important that we as APPs seek to facilitate these institutional changes and continue to set and maintain high quality standards for ourselves.
CHEST 2024 is for APPs too
With more than 300 educational sessions on the CHEST 2024 program, it can be overwhelming to figure out which ones you should put on your schedule. That’s why CHEST asked Danielle McCamey, DNP, CRNP, ACNP-BC, FCCP, and LaDonna Brown, DNP, CRNA, of DNPs of Color (DOC), as well as Corinne Young, MSN, FNP-C, FCCP, of the Association of Pulmonary Advanced Practice Providers (APAPP), for their recommendations on sessions that advanced practice providers shouldn’t miss. Visit chestnet.org/annual-meeting-apps for all of their recommendations.
References
1. Rudy S, Widmar B, Wilbeck J. Ultrasound education for nurse practitioner students: strategies for curricular integration. J Nurse Pract. 2024;20(6):104986.
2. Resnyk J, Weichold A. Barriers to learning and performing point-of-care ultrasound (POCUS): An integrative review. J Prof Nursing. 2024;54:54-62.
In memoriam: Dr. James E. Dalen
CHEST was recently informed of the death of former CHEST President, James E. Dalen, MD, MPH, Master FCCP. He served as CHEST President from 1985 to 1986.
Dr. Dalen was a graduate of Washington State University. (His undergraduate education was temporarily interrupted when he served as a Corpsman in the Navy and Marines.) He held a master’s degree from the University of Michigan, an MD from the University of Washington, an MPH from Harvard University, and an honorary Doctor of Science degree from the University of Massachusetts. He was internationally recognized as a medical visionary and esteemed cardiologist.
Dr. Dalen’s academic career spanned 3 medical schools. During the time he spent at each, he achieved great things and nurtured great ideas that helped transform medicine. From 1967 to 1975, he was on the faculty of Harvard Medical School (and the Peter Bent Brigham Hospital). From 1975 to 1988, he was a faculty member at the University of Massachusetts Medical School where he served as Chairman of Cardiovascular Medicine from 1975 to 1977 and as Chairman of Medicine from 1977 to 1988. From 1986 to 1987, he served as Interim Chancellor of the University of Massachusetts at the Worcester Campus. Dr. Dalen left Massachusetts in 1988 to become the Dean of the University of Arizona College of Medicine.
During his tenure as Dean and Vice-President at the University of Arizona, Dr. Dalen oversaw the establishment of the Zuckerman College of Public Health, the Arizona Center for Integrative Medicine, and the Arizona Telemedicine Program. Successful fundraising under his leadership led to the establishment of new research facilities, including the Children’s Research Center, the Sarver Heart Center, the Arizona Arthritis Center, and a major expansion of the Arizona Cancer Center. While at the University of Arizona College of Medicine, Dr. Dalen recognized the importance of integrative medicine and the need to promote integrative medicine in the academic environment. With the active participation of Dr. Andrew Weil, this led to the creation of the Academic Consortium for Integrative Medicine and Health and the Arizona Center for Integrative Medicine.
Dr. Dalen received many teaching awards. In 1987, he received the Distinguished Public Service Award from the University of Massachusetts. In 1988, he was named the University of Washington Distinguished Medical Alumnus of the Year and received the Alumni Achievement Award from Washington State University. In 2000, he received the College Medal from CHEST and was named a Master Fellow. In 2010, he was awarded the Harvard School of Public Health’s highest honor for its alumni: the 2010 Alumni Award of Merit. In 2012, he was named a Master Fellow of the American College of Physicians and was awarded an honorary Doctor of Science degree by the University of Massachusetts in 2013. In 2015, he received the Bravewell Distinguished Service Award from the Academic Consortium for Integrative Medicine and Health for his role as one of the founders of the consortium and as one of the founders of the Arizona Center for Integrative Medicine at the University of Arizona.
In his spare time, he enjoyed reading, gardening, sailing, art, and music and was a lifelong student with a passion for the pursuit of knowledge. Dr. Dalen enjoyed watching basketball, particularly the Arizona Wildcats. His favorite place to spend time was by the ocean in Coronado, California. Dr. Dalen was an advocate for public health, social justice, and health care reform throughout his life and career. He mentored thousands of medical students and championed access to health care for populations who were underserved. He touched many lives as a leading physician and caring friend.
Dr. Dalen is survived by his devoted wife, Priscilla M. Dalen (Dunton); loving children, James E. Dalen, Jr, and Angela M. Snodgrass (Dalen); daughter-in-law, Suzan M. Dalen; son-in-law, Daniel N. Snodgrass; and many step-grandchildren. We remember our colleague and extend our sincere condolences.
CHEST was recently informed of the death of former CHEST President, James E. Dalen, MD, MPH, Master FCCP. He served as CHEST President from 1985 to 1986.
Dr. Dalen was a graduate of Washington State University. (His undergraduate education was temporarily interrupted when he served as a Corpsman in the Navy and Marines.) He held a master’s degree from the University of Michigan, an MD from the University of Washington, an MPH from Harvard University, and an honorary Doctor of Science degree from the University of Massachusetts. He was internationally recognized as a medical visionary and esteemed cardiologist.
Dr. Dalen’s academic career spanned 3 medical schools. During the time he spent at each, he achieved great things and nurtured great ideas that helped transform medicine. From 1967 to 1975, he was on the faculty of Harvard Medical School (and the Peter Bent Brigham Hospital). From 1975 to 1988, he was a faculty member at the University of Massachusetts Medical School where he served as Chairman of Cardiovascular Medicine from 1975 to 1977 and as Chairman of Medicine from 1977 to 1988. From 1986 to 1987, he served as Interim Chancellor of the University of Massachusetts at the Worcester Campus. Dr. Dalen left Massachusetts in 1988 to become the Dean of the University of Arizona College of Medicine.
During his tenure as Dean and Vice-President at the University of Arizona, Dr. Dalen oversaw the establishment of the Zuckerman College of Public Health, the Arizona Center for Integrative Medicine, and the Arizona Telemedicine Program. Successful fundraising under his leadership led to the establishment of new research facilities, including the Children’s Research Center, the Sarver Heart Center, the Arizona Arthritis Center, and a major expansion of the Arizona Cancer Center. While at the University of Arizona College of Medicine, Dr. Dalen recognized the importance of integrative medicine and the need to promote integrative medicine in the academic environment. With the active participation of Dr. Andrew Weil, this led to the creation of the Academic Consortium for Integrative Medicine and Health and the Arizona Center for Integrative Medicine.
Dr. Dalen received many teaching awards. In 1987, he received the Distinguished Public Service Award from the University of Massachusetts. In 1988, he was named the University of Washington Distinguished Medical Alumnus of the Year and received the Alumni Achievement Award from Washington State University. In 2000, he received the College Medal from CHEST and was named a Master Fellow. In 2010, he was awarded the Harvard School of Public Health’s highest honor for its alumni: the 2010 Alumni Award of Merit. In 2012, he was named a Master Fellow of the American College of Physicians and was awarded an honorary Doctor of Science degree by the University of Massachusetts in 2013. In 2015, he received the Bravewell Distinguished Service Award from the Academic Consortium for Integrative Medicine and Health for his role as one of the founders of the consortium and as one of the founders of the Arizona Center for Integrative Medicine at the University of Arizona.
In his spare time, he enjoyed reading, gardening, sailing, art, and music and was a lifelong student with a passion for the pursuit of knowledge. Dr. Dalen enjoyed watching basketball, particularly the Arizona Wildcats. His favorite place to spend time was by the ocean in Coronado, California. Dr. Dalen was an advocate for public health, social justice, and health care reform throughout his life and career. He mentored thousands of medical students and championed access to health care for populations who were underserved. He touched many lives as a leading physician and caring friend.
Dr. Dalen is survived by his devoted wife, Priscilla M. Dalen (Dunton); loving children, James E. Dalen, Jr, and Angela M. Snodgrass (Dalen); daughter-in-law, Suzan M. Dalen; son-in-law, Daniel N. Snodgrass; and many step-grandchildren. We remember our colleague and extend our sincere condolences.
CHEST was recently informed of the death of former CHEST President, James E. Dalen, MD, MPH, Master FCCP. He served as CHEST President from 1985 to 1986.
Dr. Dalen was a graduate of Washington State University. (His undergraduate education was temporarily interrupted when he served as a Corpsman in the Navy and Marines.) He held a master’s degree from the University of Michigan, an MD from the University of Washington, an MPH from Harvard University, and an honorary Doctor of Science degree from the University of Massachusetts. He was internationally recognized as a medical visionary and esteemed cardiologist.
Dr. Dalen’s academic career spanned 3 medical schools. During the time he spent at each, he achieved great things and nurtured great ideas that helped transform medicine. From 1967 to 1975, he was on the faculty of Harvard Medical School (and the Peter Bent Brigham Hospital). From 1975 to 1988, he was a faculty member at the University of Massachusetts Medical School where he served as Chairman of Cardiovascular Medicine from 1975 to 1977 and as Chairman of Medicine from 1977 to 1988. From 1986 to 1987, he served as Interim Chancellor of the University of Massachusetts at the Worcester Campus. Dr. Dalen left Massachusetts in 1988 to become the Dean of the University of Arizona College of Medicine.
During his tenure as Dean and Vice-President at the University of Arizona, Dr. Dalen oversaw the establishment of the Zuckerman College of Public Health, the Arizona Center for Integrative Medicine, and the Arizona Telemedicine Program. Successful fundraising under his leadership led to the establishment of new research facilities, including the Children’s Research Center, the Sarver Heart Center, the Arizona Arthritis Center, and a major expansion of the Arizona Cancer Center. While at the University of Arizona College of Medicine, Dr. Dalen recognized the importance of integrative medicine and the need to promote integrative medicine in the academic environment. With the active participation of Dr. Andrew Weil, this led to the creation of the Academic Consortium for Integrative Medicine and Health and the Arizona Center for Integrative Medicine.
Dr. Dalen received many teaching awards. In 1987, he received the Distinguished Public Service Award from the University of Massachusetts. In 1988, he was named the University of Washington Distinguished Medical Alumnus of the Year and received the Alumni Achievement Award from Washington State University. In 2000, he received the College Medal from CHEST and was named a Master Fellow. In 2010, he was awarded the Harvard School of Public Health’s highest honor for its alumni: the 2010 Alumni Award of Merit. In 2012, he was named a Master Fellow of the American College of Physicians and was awarded an honorary Doctor of Science degree by the University of Massachusetts in 2013. In 2015, he received the Bravewell Distinguished Service Award from the Academic Consortium for Integrative Medicine and Health for his role as one of the founders of the consortium and as one of the founders of the Arizona Center for Integrative Medicine at the University of Arizona.
In his spare time, he enjoyed reading, gardening, sailing, art, and music and was a lifelong student with a passion for the pursuit of knowledge. Dr. Dalen enjoyed watching basketball, particularly the Arizona Wildcats. His favorite place to spend time was by the ocean in Coronado, California. Dr. Dalen was an advocate for public health, social justice, and health care reform throughout his life and career. He mentored thousands of medical students and championed access to health care for populations who were underserved. He touched many lives as a leading physician and caring friend.
Dr. Dalen is survived by his devoted wife, Priscilla M. Dalen (Dunton); loving children, James E. Dalen, Jr, and Angela M. Snodgrass (Dalen); daughter-in-law, Suzan M. Dalen; son-in-law, Daniel N. Snodgrass; and many step-grandchildren. We remember our colleague and extend our sincere condolences.
Physician-Scientist Taps into Microbiome to Fight Cancer
The lowest point in the nascent career of Neelendu Dey, MD, helped seal his fate as a physician-scientist.
He had just started his first year as a resident at University of California, San Francisco. One of his patients was a 30-year-old woman who was dying of metastatic colorectal cancer. “I was in my mid-20s interacting with an individual just a few years older than I am, going through one of the most terrible health outcomes one could imagine,” Dr. Dey said.
He remembers asking the patient what he could do for her, how he could make her feel more comfortable. “That feeling of helplessness, particularly as we think about young people developing cancer, it really stuck with me through the years,” he said.
In an interview, he talked about his dual role as a physician and scientist, and how those two interests are guiding his research in precancerous conditions of the colon.
Cases like that of the young woman with colon cancer “really help drive the urgency of the work we do, and the research questions we ask, as we try to move the ball forward and help folks at earlier stages,” he said.
Q: Why did you choose GI?
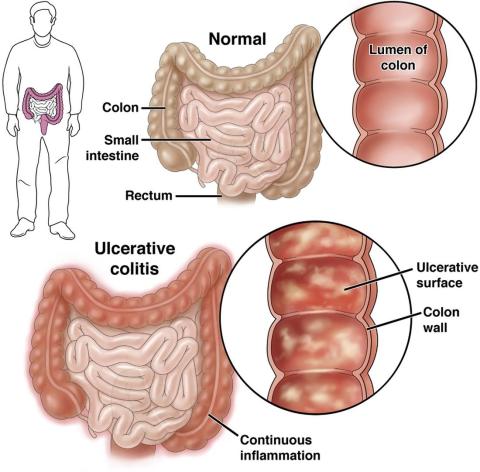
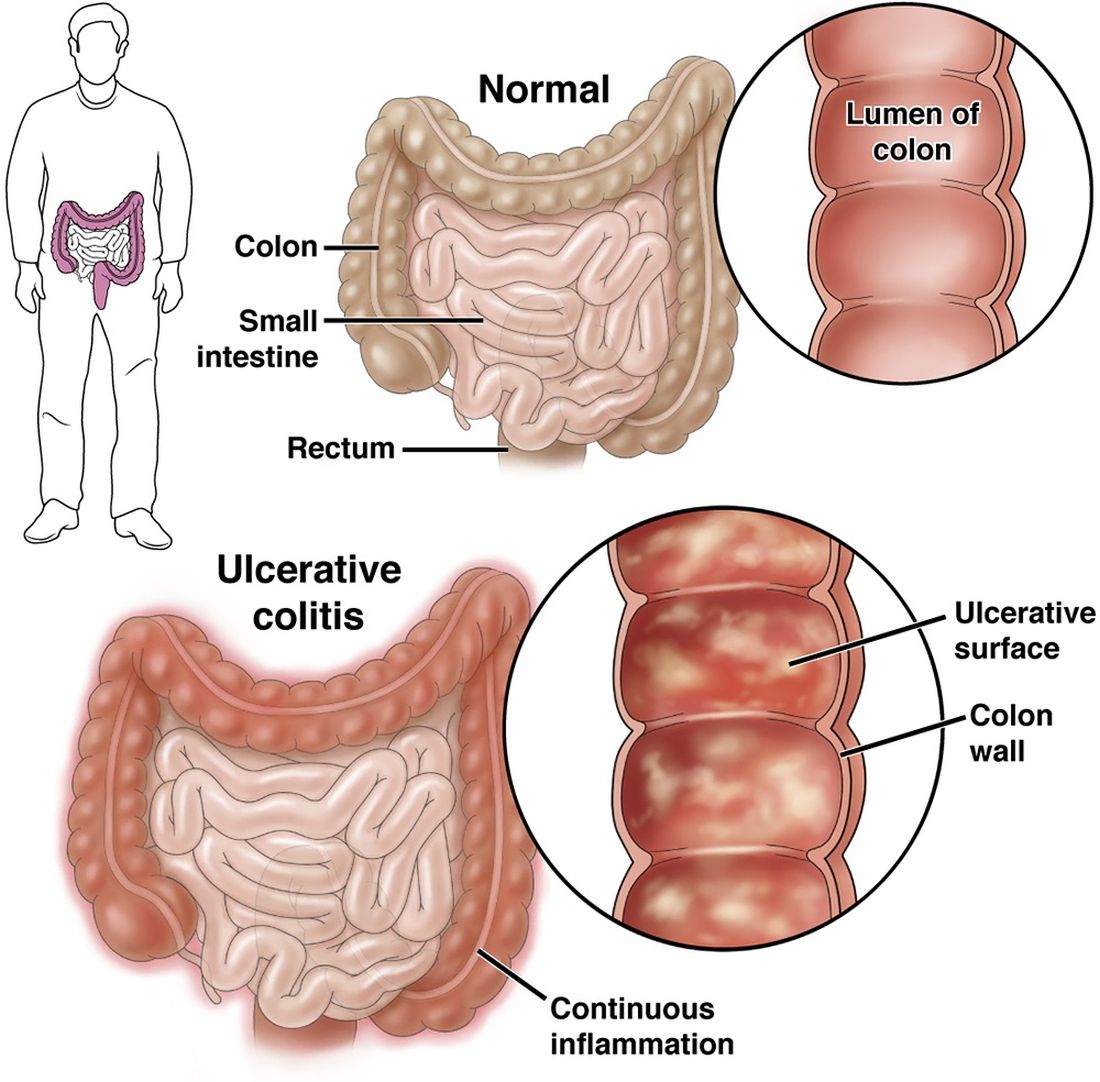
When you think about what sorts of chronic diseases really impact your quality of life, gut health is one of the chief contributors among various aspects of health. And that really appealed to me — the ability to take someone who is essentially handicapped by a series of illnesses and symptoms that derive from the GI tract and enable them to return to the person they want to be, to be productive in the way that they want to be, and have a rewarding life.
As I thought about how I wanted to contribute to the future of medicine, one of the ways in which I’ve always thought that I would do that is through research. When I considered the fields that really appealed to me, both from that clinical standpoint and research standpoint, GI was one that really stood out. There has been a lot of exciting research going on in GI. My lab currently studies the microbiome, and I feel like this is an area in which we can contribute.
Q: What role does digestive health play in overall health?
Obviously, the direct answer is gut health is so critical in something like nutritional intake. Some GI symptoms, if your gut health has gone awry, can really be detrimental in terms of quality of life. But one less obvious role that digestive health plays is its long-term effects. We’re starting to appreciate that gut health, the gut microbiome, and gut immune education are probably long-term players. Some experiences in early life might shape our immunity in ways that have consequences for us much later in life. Whether we get early life antibiotics, for example, may potentially contribute to colorectal cancer down the line. Thinking about the long-term players is more challenging, but it’s also an appealing opportunity as we think about how we can shape medicine moving forward.
Q: What practice challenges have you faced in your career?
First, being a physician-scientist. It’s challenging to be either a physician alone or to be a researcher alone. And trying to do both includes the challenges of both individual worlds. It just takes more time to get all the prerequisite training. And second, there are just challenges with getting the opportunities to contribute in the ways that you want — to get the research funding, to get the papers out, things like that.
Q: Tell me about the work you’ve been doing in your lab to develop microbiome-based strategies for preventing and treating cancer.
The microbiome presents several opportunities when it comes to cancer prevention. One is identifying markers of cancer risk, or of general good health down the line. Some of those biomarkers could — potentially — feed directly into personalized risk assessment and maybe even inform a future screening strategy. The second opportunity the microbiome presents is if we identify a microbe that influences your cancer risk, can we then understand and exploit, or utilize, that mechanism to mitigate cancer risk in the future? Our lab has done work looking at subspecies levels of microbes that track with health or cancer. We’ve done some work to identify what these subspecies groupings are and have identified some links to certain precancerous changes in the colon. We think that there’s an opportunity here for future interventions.
Q: Have you published other papers?
We recently published another paper describing how some microbes can interact with a tumor suppressor gene and are influenced in a sex-biased manner to drive tumorigenesis in a mouse model. We think, based on what we’re seeing in human data, that there may be some relationships and we’re exploring that now as well.
Q: What is your vision for the future in GI, and in your career?
The vision that I have is to create clinical tools that can expand our reach and our effectiveness and cancer prevention. I think that there are opportunities for leveraging microbiome research to accomplish this. And one outcome I could imagine is leveraging some of these insights to expand noninvasive screening at even earlier ages than we do now. I mean, we just dialed back the recommended age for colonoscopy for average risk individuals to 45. But I could envision a future in which noninvasive screening starts earlier, in which the first stool-based tests that we deploy to assess personalized risk are used in the pediatric clinic.
Lightning Round
Texting or talking?
Talking
Favorite city in the United States besides the one you live in?
St. Louis
Cat or dog person?
Both
If you weren’t a GI, what would you be?
Musician
Best place you went on vacation?
Borneo
Favorite sport?
Soccer
Favorite ice cream?
Cashew-based salted caramel
What song do you have to sing along with when you hear it?
Sweet Child of Mine
Favorite movie or TV show?
25th Hour or Shawshank Redemption
Optimist or Pessimist?
Optimist
The lowest point in the nascent career of Neelendu Dey, MD, helped seal his fate as a physician-scientist.
He had just started his first year as a resident at University of California, San Francisco. One of his patients was a 30-year-old woman who was dying of metastatic colorectal cancer. “I was in my mid-20s interacting with an individual just a few years older than I am, going through one of the most terrible health outcomes one could imagine,” Dr. Dey said.
He remembers asking the patient what he could do for her, how he could make her feel more comfortable. “That feeling of helplessness, particularly as we think about young people developing cancer, it really stuck with me through the years,” he said.
In an interview, he talked about his dual role as a physician and scientist, and how those two interests are guiding his research in precancerous conditions of the colon.
Cases like that of the young woman with colon cancer “really help drive the urgency of the work we do, and the research questions we ask, as we try to move the ball forward and help folks at earlier stages,” he said.
Q: Why did you choose GI?
When you think about what sorts of chronic diseases really impact your quality of life, gut health is one of the chief contributors among various aspects of health. And that really appealed to me — the ability to take someone who is essentially handicapped by a series of illnesses and symptoms that derive from the GI tract and enable them to return to the person they want to be, to be productive in the way that they want to be, and have a rewarding life.
As I thought about how I wanted to contribute to the future of medicine, one of the ways in which I’ve always thought that I would do that is through research. When I considered the fields that really appealed to me, both from that clinical standpoint and research standpoint, GI was one that really stood out. There has been a lot of exciting research going on in GI. My lab currently studies the microbiome, and I feel like this is an area in which we can contribute.
Q: What role does digestive health play in overall health?
Obviously, the direct answer is gut health is so critical in something like nutritional intake. Some GI symptoms, if your gut health has gone awry, can really be detrimental in terms of quality of life. But one less obvious role that digestive health plays is its long-term effects. We’re starting to appreciate that gut health, the gut microbiome, and gut immune education are probably long-term players. Some experiences in early life might shape our immunity in ways that have consequences for us much later in life. Whether we get early life antibiotics, for example, may potentially contribute to colorectal cancer down the line. Thinking about the long-term players is more challenging, but it’s also an appealing opportunity as we think about how we can shape medicine moving forward.
Q: What practice challenges have you faced in your career?
First, being a physician-scientist. It’s challenging to be either a physician alone or to be a researcher alone. And trying to do both includes the challenges of both individual worlds. It just takes more time to get all the prerequisite training. And second, there are just challenges with getting the opportunities to contribute in the ways that you want — to get the research funding, to get the papers out, things like that.
Q: Tell me about the work you’ve been doing in your lab to develop microbiome-based strategies for preventing and treating cancer.
The microbiome presents several opportunities when it comes to cancer prevention. One is identifying markers of cancer risk, or of general good health down the line. Some of those biomarkers could — potentially — feed directly into personalized risk assessment and maybe even inform a future screening strategy. The second opportunity the microbiome presents is if we identify a microbe that influences your cancer risk, can we then understand and exploit, or utilize, that mechanism to mitigate cancer risk in the future? Our lab has done work looking at subspecies levels of microbes that track with health or cancer. We’ve done some work to identify what these subspecies groupings are and have identified some links to certain precancerous changes in the colon. We think that there’s an opportunity here for future interventions.
Q: Have you published other papers?
We recently published another paper describing how some microbes can interact with a tumor suppressor gene and are influenced in a sex-biased manner to drive tumorigenesis in a mouse model. We think, based on what we’re seeing in human data, that there may be some relationships and we’re exploring that now as well.
Q: What is your vision for the future in GI, and in your career?
The vision that I have is to create clinical tools that can expand our reach and our effectiveness and cancer prevention. I think that there are opportunities for leveraging microbiome research to accomplish this. And one outcome I could imagine is leveraging some of these insights to expand noninvasive screening at even earlier ages than we do now. I mean, we just dialed back the recommended age for colonoscopy for average risk individuals to 45. But I could envision a future in which noninvasive screening starts earlier, in which the first stool-based tests that we deploy to assess personalized risk are used in the pediatric clinic.
Lightning Round
Texting or talking?
Talking
Favorite city in the United States besides the one you live in?
St. Louis
Cat or dog person?
Both
If you weren’t a GI, what would you be?
Musician
Best place you went on vacation?
Borneo
Favorite sport?
Soccer
Favorite ice cream?
Cashew-based salted caramel
What song do you have to sing along with when you hear it?
Sweet Child of Mine
Favorite movie or TV show?
25th Hour or Shawshank Redemption
Optimist or Pessimist?
Optimist
The lowest point in the nascent career of Neelendu Dey, MD, helped seal his fate as a physician-scientist.
He had just started his first year as a resident at University of California, San Francisco. One of his patients was a 30-year-old woman who was dying of metastatic colorectal cancer. “I was in my mid-20s interacting with an individual just a few years older than I am, going through one of the most terrible health outcomes one could imagine,” Dr. Dey said.
He remembers asking the patient what he could do for her, how he could make her feel more comfortable. “That feeling of helplessness, particularly as we think about young people developing cancer, it really stuck with me through the years,” he said.
In an interview, he talked about his dual role as a physician and scientist, and how those two interests are guiding his research in precancerous conditions of the colon.
Cases like that of the young woman with colon cancer “really help drive the urgency of the work we do, and the research questions we ask, as we try to move the ball forward and help folks at earlier stages,” he said.
Q: Why did you choose GI?
When you think about what sorts of chronic diseases really impact your quality of life, gut health is one of the chief contributors among various aspects of health. And that really appealed to me — the ability to take someone who is essentially handicapped by a series of illnesses and symptoms that derive from the GI tract and enable them to return to the person they want to be, to be productive in the way that they want to be, and have a rewarding life.
As I thought about how I wanted to contribute to the future of medicine, one of the ways in which I’ve always thought that I would do that is through research. When I considered the fields that really appealed to me, both from that clinical standpoint and research standpoint, GI was one that really stood out. There has been a lot of exciting research going on in GI. My lab currently studies the microbiome, and I feel like this is an area in which we can contribute.
Q: What role does digestive health play in overall health?
Obviously, the direct answer is gut health is so critical in something like nutritional intake. Some GI symptoms, if your gut health has gone awry, can really be detrimental in terms of quality of life. But one less obvious role that digestive health plays is its long-term effects. We’re starting to appreciate that gut health, the gut microbiome, and gut immune education are probably long-term players. Some experiences in early life might shape our immunity in ways that have consequences for us much later in life. Whether we get early life antibiotics, for example, may potentially contribute to colorectal cancer down the line. Thinking about the long-term players is more challenging, but it’s also an appealing opportunity as we think about how we can shape medicine moving forward.
Q: What practice challenges have you faced in your career?
First, being a physician-scientist. It’s challenging to be either a physician alone or to be a researcher alone. And trying to do both includes the challenges of both individual worlds. It just takes more time to get all the prerequisite training. And second, there are just challenges with getting the opportunities to contribute in the ways that you want — to get the research funding, to get the papers out, things like that.
Q: Tell me about the work you’ve been doing in your lab to develop microbiome-based strategies for preventing and treating cancer.
The microbiome presents several opportunities when it comes to cancer prevention. One is identifying markers of cancer risk, or of general good health down the line. Some of those biomarkers could — potentially — feed directly into personalized risk assessment and maybe even inform a future screening strategy. The second opportunity the microbiome presents is if we identify a microbe that influences your cancer risk, can we then understand and exploit, or utilize, that mechanism to mitigate cancer risk in the future? Our lab has done work looking at subspecies levels of microbes that track with health or cancer. We’ve done some work to identify what these subspecies groupings are and have identified some links to certain precancerous changes in the colon. We think that there’s an opportunity here for future interventions.
Q: Have you published other papers?
We recently published another paper describing how some microbes can interact with a tumor suppressor gene and are influenced in a sex-biased manner to drive tumorigenesis in a mouse model. We think, based on what we’re seeing in human data, that there may be some relationships and we’re exploring that now as well.
Q: What is your vision for the future in GI, and in your career?
The vision that I have is to create clinical tools that can expand our reach and our effectiveness and cancer prevention. I think that there are opportunities for leveraging microbiome research to accomplish this. And one outcome I could imagine is leveraging some of these insights to expand noninvasive screening at even earlier ages than we do now. I mean, we just dialed back the recommended age for colonoscopy for average risk individuals to 45. But I could envision a future in which noninvasive screening starts earlier, in which the first stool-based tests that we deploy to assess personalized risk are used in the pediatric clinic.
Lightning Round
Texting or talking?
Talking
Favorite city in the United States besides the one you live in?
St. Louis
Cat or dog person?
Both
If you weren’t a GI, what would you be?
Musician
Best place you went on vacation?
Borneo
Favorite sport?
Soccer
Favorite ice cream?
Cashew-based salted caramel
What song do you have to sing along with when you hear it?
Sweet Child of Mine
Favorite movie or TV show?
25th Hour or Shawshank Redemption
Optimist or Pessimist?
Optimist
Elevate Your Career: AGA Women in GI Regional Workshops Await
As a woman in a dynamic and ever-changing profession, balancing life as a powerhouse physician or scientist is no easy feat. AGA recognizes the challenges you face and is committed to addressing them directly at the AGA Women in GI Regional Workshops. The program has been expanded to six workshops in 2024.
. Participate in candid discussions regarding the challenges you face as a woman navigating the 21st century healthcare environment. Derive inspiration from your community and cultivate meaningful connections that will carry you beyond the workshop.
You may choose to join us in person or virtually, whatever fits into your busy schedule. We are also pleased to offer grants of $300 to support travel and registration fees for trainee and early career women. Additional details for the Maria Leo-Lieber Travel Award may be found in your confirmation email.
Register today for the final three workshops.
Rocky Mountain West
Saturday, Sept. 8
Colorado Springs, Colorado
Deadline to apply for a travel grant: Aug. 23
Deadline to register: Aug. 30
Southwest
Saturday, Sept. 14
Houston, Texas
Deadline to apply for a travel grant: Aug. 30
Deadline to register: Sept. 6
Southeast
Saturday, Nov. 2
Coral Gables, Florida
Deadline to apply for a travel grant: Oct. 8
Deadline to register: Oct. 25
This program is supported by Janssen.
As a woman in a dynamic and ever-changing profession, balancing life as a powerhouse physician or scientist is no easy feat. AGA recognizes the challenges you face and is committed to addressing them directly at the AGA Women in GI Regional Workshops. The program has been expanded to six workshops in 2024.
. Participate in candid discussions regarding the challenges you face as a woman navigating the 21st century healthcare environment. Derive inspiration from your community and cultivate meaningful connections that will carry you beyond the workshop.
You may choose to join us in person or virtually, whatever fits into your busy schedule. We are also pleased to offer grants of $300 to support travel and registration fees for trainee and early career women. Additional details for the Maria Leo-Lieber Travel Award may be found in your confirmation email.
Register today for the final three workshops.
Rocky Mountain West
Saturday, Sept. 8
Colorado Springs, Colorado
Deadline to apply for a travel grant: Aug. 23
Deadline to register: Aug. 30
Southwest
Saturday, Sept. 14
Houston, Texas
Deadline to apply for a travel grant: Aug. 30
Deadline to register: Sept. 6
Southeast
Saturday, Nov. 2
Coral Gables, Florida
Deadline to apply for a travel grant: Oct. 8
Deadline to register: Oct. 25
This program is supported by Janssen.
As a woman in a dynamic and ever-changing profession, balancing life as a powerhouse physician or scientist is no easy feat. AGA recognizes the challenges you face and is committed to addressing them directly at the AGA Women in GI Regional Workshops. The program has been expanded to six workshops in 2024.
. Participate in candid discussions regarding the challenges you face as a woman navigating the 21st century healthcare environment. Derive inspiration from your community and cultivate meaningful connections that will carry you beyond the workshop.
You may choose to join us in person or virtually, whatever fits into your busy schedule. We are also pleased to offer grants of $300 to support travel and registration fees for trainee and early career women. Additional details for the Maria Leo-Lieber Travel Award may be found in your confirmation email.
Register today for the final three workshops.
Rocky Mountain West
Saturday, Sept. 8
Colorado Springs, Colorado
Deadline to apply for a travel grant: Aug. 23
Deadline to register: Aug. 30
Southwest
Saturday, Sept. 14
Houston, Texas
Deadline to apply for a travel grant: Aug. 30
Deadline to register: Sept. 6
Southeast
Saturday, Nov. 2
Coral Gables, Florida
Deadline to apply for a travel grant: Oct. 8
Deadline to register: Oct. 25
This program is supported by Janssen.
How To Navigate Your First Job
In a special episode live from Digestive Disease Week® (DDW) 2024, host Dr. Matthew Whitson talks with returning guest Dr. Janice Jou. Dr. Jou is a transplant hematologist at the Portland VA and currently serves as professor of medicine and fellowship program director at Oregon Health & Science University. Don’t miss her insight as she shares advice all about what she wishes she knew when going into her first job in gastroenterology. Dr. Jou also answers questions from the audience on topics including “when to say no” and the importance of encouraging emotional transparency with fellows and faculty.
Catch up with past episodes and subscribe wherever you listen to podcasts. You can also listen by clicking on the episode name below.
- Episode 5: Janice Jou: Live from #DDW2024 with tips for your first job
- Episode 4: Loren Rabinowitz and Rachel Issaka: Building research collaborations
- Episode 3: Andy Tau: How to treat GI emergencies
- Episode 2: Laurel Fisher and Asma Khapra: Advancing and advocating for women in GI
- Episode 1: Barbara Jung: Unpacking mentorship with AGA’s president
In a special episode live from Digestive Disease Week® (DDW) 2024, host Dr. Matthew Whitson talks with returning guest Dr. Janice Jou. Dr. Jou is a transplant hematologist at the Portland VA and currently serves as professor of medicine and fellowship program director at Oregon Health & Science University. Don’t miss her insight as she shares advice all about what she wishes she knew when going into her first job in gastroenterology. Dr. Jou also answers questions from the audience on topics including “when to say no” and the importance of encouraging emotional transparency with fellows and faculty.
Catch up with past episodes and subscribe wherever you listen to podcasts. You can also listen by clicking on the episode name below.
- Episode 5: Janice Jou: Live from #DDW2024 with tips for your first job
- Episode 4: Loren Rabinowitz and Rachel Issaka: Building research collaborations
- Episode 3: Andy Tau: How to treat GI emergencies
- Episode 2: Laurel Fisher and Asma Khapra: Advancing and advocating for women in GI
- Episode 1: Barbara Jung: Unpacking mentorship with AGA’s president
In a special episode live from Digestive Disease Week® (DDW) 2024, host Dr. Matthew Whitson talks with returning guest Dr. Janice Jou. Dr. Jou is a transplant hematologist at the Portland VA and currently serves as professor of medicine and fellowship program director at Oregon Health & Science University. Don’t miss her insight as she shares advice all about what she wishes she knew when going into her first job in gastroenterology. Dr. Jou also answers questions from the audience on topics including “when to say no” and the importance of encouraging emotional transparency with fellows and faculty.
Catch up with past episodes and subscribe wherever you listen to podcasts. You can also listen by clicking on the episode name below.
- Episode 5: Janice Jou: Live from #DDW2024 with tips for your first job
- Episode 4: Loren Rabinowitz and Rachel Issaka: Building research collaborations
- Episode 3: Andy Tau: How to treat GI emergencies
- Episode 2: Laurel Fisher and Asma Khapra: Advancing and advocating for women in GI
- Episode 1: Barbara Jung: Unpacking mentorship with AGA’s president
AGA Issues Guidance on Identifying, Treating Cyclic Vomiting Syndrome
, according to a new clinical practice update from the American Gastroenterological Association.
CVS affects up to 2% of U.S. adults and is more common in women, young adults, and those with a personal or family history of migraine headaches. However, most patients don’t receive a diagnosis or often experience years of delay in receiving effective treatment.
“A diagnosis is a powerful tool. Not only does it help patients make sense of debilitating symptoms, but it allows healthcare providers to create an effective treatment plan,” said author David J. Levinthal, MD, AGAF, director of the Neurogastroenterology and Motility Center at the University of Pittsburgh Medical Center.
The update was published online in Gastroenterology.
Understanding Cyclic Vomiting Syndrome
CVS is a chronic disorder of gut-brain interaction (DGBI), which is characterized by acute episodes of nausea and vomiting, separated by time without symptoms. Patients can usually identify a pattern of symptoms that show up during and between episodes.
CVS can vary, ranging from mild — with less than four episodes per year and lasting less than 2 days — to moderate-severe — with more than four episodes per year, lasting more than 2 days, and requiring at least one emergency department visit or hospitalization.
The disorder has four distinct phases — inter-episodic, prodromal, emetic, and recovery — that align with distinct treatment and management strategies. Between episodes, patients typically don’t experience repetitive vomiting but may experience symptoms such as mild nausea, indigestion, and occasional vomiting. Although CVS episodes can happen at any time, most tend to occur in the early morning.
For diagnosis, clinicians should consider CVS in adults presenting with episodic bouts of repetitive vomiting, following criteria established by the Rome Foundation. Rome IV criteria include acute-onset vomiting lasting less than 7 days, at least three discrete episodes in a year with two in the previous 6 months, and an absence of vomiting between episodes separated by at least 1 week of baseline health.

About 65% of patients with CVS experience prodromal symptoms, which last for about an hour before the onset of vomiting and may include panic, a sense of doom, and an inability to communicate effectively. During prodromal or emetic phases, patients have also reported fatigue, brain fog, restlessness, anxiety, headache, bowel urgency, abdominal pain, flushing, or shakiness.
As with migraines, CVS episodes may often be triggered by psychological and physiological factors, particularly stress. Episodes can stem from both negative stress, such as a death or relationship conflicts, as well as positive stress, such as birthdays and vacations. Other triggers include sleep deprivation, hormonal fluctuations linked to the menstrual cycle, travel, motion sickness, or acute infections.
Adult CVS is associated with several conditions, particularly mood disorders, including anxiety, depression, and panic disorder. Patients may also experience migraines, seizure disorders, or autonomic imbalances, such as postural orthostatic tachycardia syndrome, which may indicate pathophysiological mechanisms and routes for management.
The American Neurogastroenterology and Motility Society recommends testing to rule out similar or overlapping conditions, such as Addison’s disease, hypothyroidism, and hepatic porphyria. Diagnostic workup should include blood work, urinalysis, and one-time esophagogastroduodenoscopy or upper gastrointestinal imaging. Repeated imaging and gastric emptying scans should be avoided.
Providing Treatment and Prevention
For treatment, knowing the CVS phase is “essential,” the authors wrote. For instance, during the prodromal phase, abortive therapies can halt the transition to the emetic phase, and earlier intervention is associated with a higher probability of stopping an episode. The authors recommend intranasal sumatriptan, ondansetron, antihistamines, and sedatives.
During the emetic phase, supportive therapy can help terminate the episode. This may include continuing the abortive regimen and going to the emergency department for hydration and antiemetic medications. Patients may also find relief in a quiet, darker room in the emergency department, along with IV benzodiazepines, with the goal of inducing sedation.
During the recovery phase, patients should rest and focus on rehydration and nutrition to return to the well phase.
During the well or inter-episodic phase, patients can follow lifestyle measures to identify and avoid triggers, such as taking prophylactic medication (tricyclic antidepressants, anticonvulsants, and neurokinin-1 receptor antagonists such as aprepitant), reducing stress, and implementing a good sleep routine.
As part of patient education, clinicians can discuss the four phases and rehearse the actions to take to prevent or stop an episode.
“CVS has a significant impact on patients, families, and the healthcare system. The unpredictable and disruptive nature of episodes can result in reduced health-related quality of life, job loss precipitated by work absenteeism, and even divorce,” said Rosita Frazier, MD, a gastroenterologist at Mayo Clinic Arizona in Scottsdale who specializes in DGBI and CVS. Dr. Frazier, who wasn’t involved with the clinical practice update, has previously written about CVS diagnosis and management.
“Providing an individualized care plan for all patients could potentially address this problem and improve the physician-patient interaction,” she said. “Educational efforts to raise awareness among the medical community and increase both patient and provider engagement can optimize outcomes and are needed to address this critical problem.”
The authors received no specific funding for this update. Dr. Levinthal is a consultant for Takeda Pharmaceuticals and Mahana. Dr. Frazier reported no relevant financial disclosures.
, according to a new clinical practice update from the American Gastroenterological Association.
CVS affects up to 2% of U.S. adults and is more common in women, young adults, and those with a personal or family history of migraine headaches. However, most patients don’t receive a diagnosis or often experience years of delay in receiving effective treatment.
“A diagnosis is a powerful tool. Not only does it help patients make sense of debilitating symptoms, but it allows healthcare providers to create an effective treatment plan,” said author David J. Levinthal, MD, AGAF, director of the Neurogastroenterology and Motility Center at the University of Pittsburgh Medical Center.
The update was published online in Gastroenterology.
Understanding Cyclic Vomiting Syndrome
CVS is a chronic disorder of gut-brain interaction (DGBI), which is characterized by acute episodes of nausea and vomiting, separated by time without symptoms. Patients can usually identify a pattern of symptoms that show up during and between episodes.
CVS can vary, ranging from mild — with less than four episodes per year and lasting less than 2 days — to moderate-severe — with more than four episodes per year, lasting more than 2 days, and requiring at least one emergency department visit or hospitalization.
The disorder has four distinct phases — inter-episodic, prodromal, emetic, and recovery — that align with distinct treatment and management strategies. Between episodes, patients typically don’t experience repetitive vomiting but may experience symptoms such as mild nausea, indigestion, and occasional vomiting. Although CVS episodes can happen at any time, most tend to occur in the early morning.
For diagnosis, clinicians should consider CVS in adults presenting with episodic bouts of repetitive vomiting, following criteria established by the Rome Foundation. Rome IV criteria include acute-onset vomiting lasting less than 7 days, at least three discrete episodes in a year with two in the previous 6 months, and an absence of vomiting between episodes separated by at least 1 week of baseline health.

About 65% of patients with CVS experience prodromal symptoms, which last for about an hour before the onset of vomiting and may include panic, a sense of doom, and an inability to communicate effectively. During prodromal or emetic phases, patients have also reported fatigue, brain fog, restlessness, anxiety, headache, bowel urgency, abdominal pain, flushing, or shakiness.
As with migraines, CVS episodes may often be triggered by psychological and physiological factors, particularly stress. Episodes can stem from both negative stress, such as a death or relationship conflicts, as well as positive stress, such as birthdays and vacations. Other triggers include sleep deprivation, hormonal fluctuations linked to the menstrual cycle, travel, motion sickness, or acute infections.
Adult CVS is associated with several conditions, particularly mood disorders, including anxiety, depression, and panic disorder. Patients may also experience migraines, seizure disorders, or autonomic imbalances, such as postural orthostatic tachycardia syndrome, which may indicate pathophysiological mechanisms and routes for management.
The American Neurogastroenterology and Motility Society recommends testing to rule out similar or overlapping conditions, such as Addison’s disease, hypothyroidism, and hepatic porphyria. Diagnostic workup should include blood work, urinalysis, and one-time esophagogastroduodenoscopy or upper gastrointestinal imaging. Repeated imaging and gastric emptying scans should be avoided.
Providing Treatment and Prevention
For treatment, knowing the CVS phase is “essential,” the authors wrote. For instance, during the prodromal phase, abortive therapies can halt the transition to the emetic phase, and earlier intervention is associated with a higher probability of stopping an episode. The authors recommend intranasal sumatriptan, ondansetron, antihistamines, and sedatives.
During the emetic phase, supportive therapy can help terminate the episode. This may include continuing the abortive regimen and going to the emergency department for hydration and antiemetic medications. Patients may also find relief in a quiet, darker room in the emergency department, along with IV benzodiazepines, with the goal of inducing sedation.
During the recovery phase, patients should rest and focus on rehydration and nutrition to return to the well phase.
During the well or inter-episodic phase, patients can follow lifestyle measures to identify and avoid triggers, such as taking prophylactic medication (tricyclic antidepressants, anticonvulsants, and neurokinin-1 receptor antagonists such as aprepitant), reducing stress, and implementing a good sleep routine.
As part of patient education, clinicians can discuss the four phases and rehearse the actions to take to prevent or stop an episode.
“CVS has a significant impact on patients, families, and the healthcare system. The unpredictable and disruptive nature of episodes can result in reduced health-related quality of life, job loss precipitated by work absenteeism, and even divorce,” said Rosita Frazier, MD, a gastroenterologist at Mayo Clinic Arizona in Scottsdale who specializes in DGBI and CVS. Dr. Frazier, who wasn’t involved with the clinical practice update, has previously written about CVS diagnosis and management.
“Providing an individualized care plan for all patients could potentially address this problem and improve the physician-patient interaction,” she said. “Educational efforts to raise awareness among the medical community and increase both patient and provider engagement can optimize outcomes and are needed to address this critical problem.”
The authors received no specific funding for this update. Dr. Levinthal is a consultant for Takeda Pharmaceuticals and Mahana. Dr. Frazier reported no relevant financial disclosures.
, according to a new clinical practice update from the American Gastroenterological Association.
CVS affects up to 2% of U.S. adults and is more common in women, young adults, and those with a personal or family history of migraine headaches. However, most patients don’t receive a diagnosis or often experience years of delay in receiving effective treatment.
“A diagnosis is a powerful tool. Not only does it help patients make sense of debilitating symptoms, but it allows healthcare providers to create an effective treatment plan,” said author David J. Levinthal, MD, AGAF, director of the Neurogastroenterology and Motility Center at the University of Pittsburgh Medical Center.
The update was published online in Gastroenterology.
Understanding Cyclic Vomiting Syndrome
CVS is a chronic disorder of gut-brain interaction (DGBI), which is characterized by acute episodes of nausea and vomiting, separated by time without symptoms. Patients can usually identify a pattern of symptoms that show up during and between episodes.
CVS can vary, ranging from mild — with less than four episodes per year and lasting less than 2 days — to moderate-severe — with more than four episodes per year, lasting more than 2 days, and requiring at least one emergency department visit or hospitalization.
The disorder has four distinct phases — inter-episodic, prodromal, emetic, and recovery — that align with distinct treatment and management strategies. Between episodes, patients typically don’t experience repetitive vomiting but may experience symptoms such as mild nausea, indigestion, and occasional vomiting. Although CVS episodes can happen at any time, most tend to occur in the early morning.
For diagnosis, clinicians should consider CVS in adults presenting with episodic bouts of repetitive vomiting, following criteria established by the Rome Foundation. Rome IV criteria include acute-onset vomiting lasting less than 7 days, at least three discrete episodes in a year with two in the previous 6 months, and an absence of vomiting between episodes separated by at least 1 week of baseline health.

About 65% of patients with CVS experience prodromal symptoms, which last for about an hour before the onset of vomiting and may include panic, a sense of doom, and an inability to communicate effectively. During prodromal or emetic phases, patients have also reported fatigue, brain fog, restlessness, anxiety, headache, bowel urgency, abdominal pain, flushing, or shakiness.
As with migraines, CVS episodes may often be triggered by psychological and physiological factors, particularly stress. Episodes can stem from both negative stress, such as a death or relationship conflicts, as well as positive stress, such as birthdays and vacations. Other triggers include sleep deprivation, hormonal fluctuations linked to the menstrual cycle, travel, motion sickness, or acute infections.
Adult CVS is associated with several conditions, particularly mood disorders, including anxiety, depression, and panic disorder. Patients may also experience migraines, seizure disorders, or autonomic imbalances, such as postural orthostatic tachycardia syndrome, which may indicate pathophysiological mechanisms and routes for management.
The American Neurogastroenterology and Motility Society recommends testing to rule out similar or overlapping conditions, such as Addison’s disease, hypothyroidism, and hepatic porphyria. Diagnostic workup should include blood work, urinalysis, and one-time esophagogastroduodenoscopy or upper gastrointestinal imaging. Repeated imaging and gastric emptying scans should be avoided.
Providing Treatment and Prevention
For treatment, knowing the CVS phase is “essential,” the authors wrote. For instance, during the prodromal phase, abortive therapies can halt the transition to the emetic phase, and earlier intervention is associated with a higher probability of stopping an episode. The authors recommend intranasal sumatriptan, ondansetron, antihistamines, and sedatives.
During the emetic phase, supportive therapy can help terminate the episode. This may include continuing the abortive regimen and going to the emergency department for hydration and antiemetic medications. Patients may also find relief in a quiet, darker room in the emergency department, along with IV benzodiazepines, with the goal of inducing sedation.
During the recovery phase, patients should rest and focus on rehydration and nutrition to return to the well phase.
During the well or inter-episodic phase, patients can follow lifestyle measures to identify and avoid triggers, such as taking prophylactic medication (tricyclic antidepressants, anticonvulsants, and neurokinin-1 receptor antagonists such as aprepitant), reducing stress, and implementing a good sleep routine.
As part of patient education, clinicians can discuss the four phases and rehearse the actions to take to prevent or stop an episode.
“CVS has a significant impact on patients, families, and the healthcare system. The unpredictable and disruptive nature of episodes can result in reduced health-related quality of life, job loss precipitated by work absenteeism, and even divorce,” said Rosita Frazier, MD, a gastroenterologist at Mayo Clinic Arizona in Scottsdale who specializes in DGBI and CVS. Dr. Frazier, who wasn’t involved with the clinical practice update, has previously written about CVS diagnosis and management.
“Providing an individualized care plan for all patients could potentially address this problem and improve the physician-patient interaction,” she said. “Educational efforts to raise awareness among the medical community and increase both patient and provider engagement can optimize outcomes and are needed to address this critical problem.”
The authors received no specific funding for this update. Dr. Levinthal is a consultant for Takeda Pharmaceuticals and Mahana. Dr. Frazier reported no relevant financial disclosures.
FROM GASTROENTEROLOGY
We’re Making Progress in the Fight Against GI Cancers
The House Appropriations Committee has included AGA-provided language on gastric and esophageal cancers in the FY25 Labor, Health, and Human Services report.
Gastric and esophageal cancers rates are rising and have a low 5-year survival rate and are highly fatal due to the lack of screening — despite both cancers typically being associated with reduced mortality. Delays in diagnosis lead to poor prognoses when the cancer is already at an advanced stage.
These cancers receive disproportionately low funding and have the lowest ratio of funding to lethality to any other cancer.
That’s why it’s crucial to close the gap and increase screening for GI cancers that are less commonly screened for.
AGA’s provided language encourages NIH to develop, test and implement screening strategies for gastric and esophageal cancers using non-endoscopic screening modalities, personalized clinical risk stratification for screenings and biomarker-based risk-stratification.
Why is this important?
This submission is the first time AGA language on gastric and esophageal cancer has been requested and included in the committee’s report. This illustrates the Committee’s recognition of the importance of GI cancer detection and the work being done by NIH.
What does this mean for GI?
This is an important first step to increasing access to cancer screenings! We look forward to working with our champions on Capitol Hill to increase patient access GI cancer screenings.
The House Appropriations Committee has included AGA-provided language on gastric and esophageal cancers in the FY25 Labor, Health, and Human Services report.
Gastric and esophageal cancers rates are rising and have a low 5-year survival rate and are highly fatal due to the lack of screening — despite both cancers typically being associated with reduced mortality. Delays in diagnosis lead to poor prognoses when the cancer is already at an advanced stage.
These cancers receive disproportionately low funding and have the lowest ratio of funding to lethality to any other cancer.
That’s why it’s crucial to close the gap and increase screening for GI cancers that are less commonly screened for.
AGA’s provided language encourages NIH to develop, test and implement screening strategies for gastric and esophageal cancers using non-endoscopic screening modalities, personalized clinical risk stratification for screenings and biomarker-based risk-stratification.
Why is this important?
This submission is the first time AGA language on gastric and esophageal cancer has been requested and included in the committee’s report. This illustrates the Committee’s recognition of the importance of GI cancer detection and the work being done by NIH.
What does this mean for GI?
This is an important first step to increasing access to cancer screenings! We look forward to working with our champions on Capitol Hill to increase patient access GI cancer screenings.
The House Appropriations Committee has included AGA-provided language on gastric and esophageal cancers in the FY25 Labor, Health, and Human Services report.
Gastric and esophageal cancers rates are rising and have a low 5-year survival rate and are highly fatal due to the lack of screening — despite both cancers typically being associated with reduced mortality. Delays in diagnosis lead to poor prognoses when the cancer is already at an advanced stage.
These cancers receive disproportionately low funding and have the lowest ratio of funding to lethality to any other cancer.
That’s why it’s crucial to close the gap and increase screening for GI cancers that are less commonly screened for.
AGA’s provided language encourages NIH to develop, test and implement screening strategies for gastric and esophageal cancers using non-endoscopic screening modalities, personalized clinical risk stratification for screenings and biomarker-based risk-stratification.
Why is this important?
This submission is the first time AGA language on gastric and esophageal cancer has been requested and included in the committee’s report. This illustrates the Committee’s recognition of the importance of GI cancer detection and the work being done by NIH.
What does this mean for GI?
This is an important first step to increasing access to cancer screenings! We look forward to working with our champions on Capitol Hill to increase patient access GI cancer screenings.
Check Out Our New Ulcerative Colitis Clinician Toolkit
Check out and bookmark AGA’s new ulcerative colitis toolkit, which compiles all our ulcerative colitis clinical guidance, continuing education resources, patient education, and FAQs into one convenient toolkit.
Curious about our other toolkits? Check out our toolkit on Crohn’s disease.
The new UC toolkit includes clinical guidance on:
- Role of biomarkers for the management of ulcerative colitis
- Medical management of moderate to severe ulcerative colitis
- Management of pouchitis and inflammatory pouch disorders
For more resources for ulcerative colitis patients, visit the Patient Center on the AGA website.
The AGA Patient Center has a variety of information that can be shared with your patients, including tips on diet, vaccine recommendations, and information on biosimilars.
Check out and bookmark AGA’s new ulcerative colitis toolkit, which compiles all our ulcerative colitis clinical guidance, continuing education resources, patient education, and FAQs into one convenient toolkit.
Curious about our other toolkits? Check out our toolkit on Crohn’s disease.
The new UC toolkit includes clinical guidance on:
- Role of biomarkers for the management of ulcerative colitis
- Medical management of moderate to severe ulcerative colitis
- Management of pouchitis and inflammatory pouch disorders
For more resources for ulcerative colitis patients, visit the Patient Center on the AGA website.
The AGA Patient Center has a variety of information that can be shared with your patients, including tips on diet, vaccine recommendations, and information on biosimilars.
Check out and bookmark AGA’s new ulcerative colitis toolkit, which compiles all our ulcerative colitis clinical guidance, continuing education resources, patient education, and FAQs into one convenient toolkit.
Curious about our other toolkits? Check out our toolkit on Crohn’s disease.
The new UC toolkit includes clinical guidance on:
- Role of biomarkers for the management of ulcerative colitis
- Medical management of moderate to severe ulcerative colitis
- Management of pouchitis and inflammatory pouch disorders
For more resources for ulcerative colitis patients, visit the Patient Center on the AGA website.
The AGA Patient Center has a variety of information that can be shared with your patients, including tips on diet, vaccine recommendations, and information on biosimilars.
Announcing Our 2024 AGA Council Chair and Section Leaders
Meet Our New Chair
Douglas J. Robertson, MD, MPH, AGAFAGA Institute Council Chair
VA Medical Center, White River Junction, Vermont
Geisel School of Medicine at Dartmouth, Hanover, New Hampshire
Dr. Robertson will serve as council chair for 3 years (May 2024-May 2027; DDW 2025, 2026 and 2027).
Section Leadership
, the driving force behind AGA’s programming at Digestive Disease Week (DDW). We welcome 8 members into their new roles as section vice chairs, joining the existing 17 Council members. Each new vice chair will serve a 2-year term that began immediately following this year’s DDW meeting and extends through DDW 2026. Following their term as vice chair, they will move into the role of section chair for an additional 2 years through DDW 2028.

We are also pleased to announce the members joining nominating committees during the 2026 nomination/election cycle. The chairs of the nominating committee will be the immediate past section chairs, whom we also recognize and thank for their service and dedication to the section and the council.
Basic & Clinical Intestinal Disorders (BCID)
Uma Sundaram, MDVice chair
Marshall University School of Medicine, Huntington, West Virginia
Nominating committee members
- Colleen Renee Kelly, MD, AGAF, Chair
- Amy C. Engevik, PhD, Medical University of South Carolina
- Ravinder Gill, PhD, University of Illinois at Chicago
- Madhusudan Grover, MD, Mayo Clinic, Rochester, Minnesota
- Lisa L. Strate, MD, Harborview Medical Center, Seattle
Clinical Practice (CP)
Linda Anh Nguyen, MDVice Chair
Stanford (Calif.) University School of Medicine
Nominating committee members
- Gary W. Falk, MD, MS, AGAF, Chair
- Megan Adams, MD, JD, MSc, VA Ann Arbor Healthcare System Endoscopy Unit
- Mohammad Bilal, MD, Minneapolis VA Health Care System
- Carolyn Newberry, MD, Weill Cornell Medical Center, New York
- Adam Weizman, MD, MSc, Mount Sinai Hospital, Toronto
Endoscopy, Technology & Imaging (ETI)
Vivek Kaul, MD, AGAFVice Chair
University of Rochester (N.Y.) Medical Center
Nominating committee members
- Irving Waxman, MD, Chair
- Sushovan Guha, MD, PhD, University of Texas at Houston
- Pichamol Jirapinyo, MD, MPH, Brigham and Women’s Hospital, Boston
- Vladimir Kushnir, MD, Washington University St. Louis Barnes–Jewish West County Hospital
- Andrew C. Storm, MD, Mayo Clinic, Rochester, Minnesota
Immunology, Microbiology & Inflammatory Bowel Diseases (IMIBD)
Florian Rieder, MDVice Chair
Cleveland Clinic Foundation
Nominating committee members
- Fernando S. Velayos, MD, AGAF, Chair
- Brigid S. Boland, MD, University of California, San Diego
- Karen L. Edelblum, PhD, Icahn School of Medicine at Mount Sinai, New York
- Michael Kattah, MD, PhD, UCSF Gastroenterology
- Andres J. Yarur, MD, Cedars Sinai Medical Center. Los Angeles
Liver & Biliary (LB)
Don Rockey, MDVice Chair
Medical University of South Carolina, Charleston
Nominating committee members
- Gyongyi Szabo, MD, PhD, AGAF, Chair
- Brett Fortune, MD, MSc, Montefiore Medical Center
- Ruben Hernaez, MD, MPH, PhD, Baylor College of Medicine, Houston
- Cynthia Ann Moylan, MD, MHS, MS, Duke University, Durham, North Carolina
- Douglas A. Simonetto, MD, Mayo Clinic, Rochester, Minnesota
Microbiome & Microbial Therapy (MMT)
Jessica Allegretti, MD, MPHVice Chair
Brigham and Women’s Hospital, Boston
Nominating committee members
- Purna C. Kashyap, MBBS, AGAF, Chair
- Melinda Engevik, PhD, Medical University of South Carolina
- Christian Jobin, PhD, University of Florida
- Vanessa Leone, PhD, The University of Wisconsin–Madison
- Jun Yu, MD, PhD, The Chinese University of Hong Kong
Obesity, Metabolism & Nutrition (OMN)
Berkeley M. Limketkai, MD, PhDVice Chair
University of California Los Angeles
Nominating committee members
- Andres Jose Acosta, MD, PhD, Chair
- Barham K. Abu Dayyeh, MD, MPH, Mayo Clinic, Rochester, Minnesota
- Alan L. Buchman, MD, MSPH, University of Illinois at Chicago
- Octavia Pickett-Blakely, MD, MHS, Hospital of the University of Pennsylvania
- Robert Shulman, MD, Texas Children’s Hospital, Baylor College of Medicine
Pediatric Gastroenterology & Developmental Biology (PGDB)
Kelli L. VanDussen, PhDVice Chair
Cincinnati Children’s Hospital Medical Center
Meet Our New Chair
Douglas J. Robertson, MD, MPH, AGAFAGA Institute Council Chair
VA Medical Center, White River Junction, Vermont
Geisel School of Medicine at Dartmouth, Hanover, New Hampshire
Dr. Robertson will serve as council chair for 3 years (May 2024-May 2027; DDW 2025, 2026 and 2027).
Section Leadership
, the driving force behind AGA’s programming at Digestive Disease Week (DDW). We welcome 8 members into their new roles as section vice chairs, joining the existing 17 Council members. Each new vice chair will serve a 2-year term that began immediately following this year’s DDW meeting and extends through DDW 2026. Following their term as vice chair, they will move into the role of section chair for an additional 2 years through DDW 2028.

We are also pleased to announce the members joining nominating committees during the 2026 nomination/election cycle. The chairs of the nominating committee will be the immediate past section chairs, whom we also recognize and thank for their service and dedication to the section and the council.
Basic & Clinical Intestinal Disorders (BCID)
Uma Sundaram, MDVice chair
Marshall University School of Medicine, Huntington, West Virginia
Nominating committee members
- Colleen Renee Kelly, MD, AGAF, Chair
- Amy C. Engevik, PhD, Medical University of South Carolina
- Ravinder Gill, PhD, University of Illinois at Chicago
- Madhusudan Grover, MD, Mayo Clinic, Rochester, Minnesota
- Lisa L. Strate, MD, Harborview Medical Center, Seattle
Clinical Practice (CP)
Linda Anh Nguyen, MDVice Chair
Stanford (Calif.) University School of Medicine
Nominating committee members
- Gary W. Falk, MD, MS, AGAF, Chair
- Megan Adams, MD, JD, MSc, VA Ann Arbor Healthcare System Endoscopy Unit
- Mohammad Bilal, MD, Minneapolis VA Health Care System
- Carolyn Newberry, MD, Weill Cornell Medical Center, New York
- Adam Weizman, MD, MSc, Mount Sinai Hospital, Toronto
Endoscopy, Technology & Imaging (ETI)
Vivek Kaul, MD, AGAFVice Chair
University of Rochester (N.Y.) Medical Center
Nominating committee members
- Irving Waxman, MD, Chair
- Sushovan Guha, MD, PhD, University of Texas at Houston
- Pichamol Jirapinyo, MD, MPH, Brigham and Women’s Hospital, Boston
- Vladimir Kushnir, MD, Washington University St. Louis Barnes–Jewish West County Hospital
- Andrew C. Storm, MD, Mayo Clinic, Rochester, Minnesota
Immunology, Microbiology & Inflammatory Bowel Diseases (IMIBD)
Florian Rieder, MDVice Chair
Cleveland Clinic Foundation
Nominating committee members
- Fernando S. Velayos, MD, AGAF, Chair
- Brigid S. Boland, MD, University of California, San Diego
- Karen L. Edelblum, PhD, Icahn School of Medicine at Mount Sinai, New York
- Michael Kattah, MD, PhD, UCSF Gastroenterology
- Andres J. Yarur, MD, Cedars Sinai Medical Center. Los Angeles
Liver & Biliary (LB)
Don Rockey, MDVice Chair
Medical University of South Carolina, Charleston
Nominating committee members
- Gyongyi Szabo, MD, PhD, AGAF, Chair
- Brett Fortune, MD, MSc, Montefiore Medical Center
- Ruben Hernaez, MD, MPH, PhD, Baylor College of Medicine, Houston
- Cynthia Ann Moylan, MD, MHS, MS, Duke University, Durham, North Carolina
- Douglas A. Simonetto, MD, Mayo Clinic, Rochester, Minnesota
Microbiome & Microbial Therapy (MMT)
Jessica Allegretti, MD, MPHVice Chair
Brigham and Women’s Hospital, Boston
Nominating committee members
- Purna C. Kashyap, MBBS, AGAF, Chair
- Melinda Engevik, PhD, Medical University of South Carolina
- Christian Jobin, PhD, University of Florida
- Vanessa Leone, PhD, The University of Wisconsin–Madison
- Jun Yu, MD, PhD, The Chinese University of Hong Kong
Obesity, Metabolism & Nutrition (OMN)
Berkeley M. Limketkai, MD, PhDVice Chair
University of California Los Angeles
Nominating committee members
- Andres Jose Acosta, MD, PhD, Chair
- Barham K. Abu Dayyeh, MD, MPH, Mayo Clinic, Rochester, Minnesota
- Alan L. Buchman, MD, MSPH, University of Illinois at Chicago
- Octavia Pickett-Blakely, MD, MHS, Hospital of the University of Pennsylvania
- Robert Shulman, MD, Texas Children’s Hospital, Baylor College of Medicine
Pediatric Gastroenterology & Developmental Biology (PGDB)
Kelli L. VanDussen, PhDVice Chair
Cincinnati Children’s Hospital Medical Center
Meet Our New Chair
Douglas J. Robertson, MD, MPH, AGAFAGA Institute Council Chair
VA Medical Center, White River Junction, Vermont
Geisel School of Medicine at Dartmouth, Hanover, New Hampshire
Dr. Robertson will serve as council chair for 3 years (May 2024-May 2027; DDW 2025, 2026 and 2027).
Section Leadership
, the driving force behind AGA’s programming at Digestive Disease Week (DDW). We welcome 8 members into their new roles as section vice chairs, joining the existing 17 Council members. Each new vice chair will serve a 2-year term that began immediately following this year’s DDW meeting and extends through DDW 2026. Following their term as vice chair, they will move into the role of section chair for an additional 2 years through DDW 2028.

We are also pleased to announce the members joining nominating committees during the 2026 nomination/election cycle. The chairs of the nominating committee will be the immediate past section chairs, whom we also recognize and thank for their service and dedication to the section and the council.
Basic & Clinical Intestinal Disorders (BCID)
Uma Sundaram, MDVice chair
Marshall University School of Medicine, Huntington, West Virginia
Nominating committee members
- Colleen Renee Kelly, MD, AGAF, Chair
- Amy C. Engevik, PhD, Medical University of South Carolina
- Ravinder Gill, PhD, University of Illinois at Chicago
- Madhusudan Grover, MD, Mayo Clinic, Rochester, Minnesota
- Lisa L. Strate, MD, Harborview Medical Center, Seattle
Clinical Practice (CP)
Linda Anh Nguyen, MDVice Chair
Stanford (Calif.) University School of Medicine
Nominating committee members
- Gary W. Falk, MD, MS, AGAF, Chair
- Megan Adams, MD, JD, MSc, VA Ann Arbor Healthcare System Endoscopy Unit
- Mohammad Bilal, MD, Minneapolis VA Health Care System
- Carolyn Newberry, MD, Weill Cornell Medical Center, New York
- Adam Weizman, MD, MSc, Mount Sinai Hospital, Toronto
Endoscopy, Technology & Imaging (ETI)
Vivek Kaul, MD, AGAFVice Chair
University of Rochester (N.Y.) Medical Center
Nominating committee members
- Irving Waxman, MD, Chair
- Sushovan Guha, MD, PhD, University of Texas at Houston
- Pichamol Jirapinyo, MD, MPH, Brigham and Women’s Hospital, Boston
- Vladimir Kushnir, MD, Washington University St. Louis Barnes–Jewish West County Hospital
- Andrew C. Storm, MD, Mayo Clinic, Rochester, Minnesota
Immunology, Microbiology & Inflammatory Bowel Diseases (IMIBD)
Florian Rieder, MDVice Chair
Cleveland Clinic Foundation
Nominating committee members
- Fernando S. Velayos, MD, AGAF, Chair
- Brigid S. Boland, MD, University of California, San Diego
- Karen L. Edelblum, PhD, Icahn School of Medicine at Mount Sinai, New York
- Michael Kattah, MD, PhD, UCSF Gastroenterology
- Andres J. Yarur, MD, Cedars Sinai Medical Center. Los Angeles
Liver & Biliary (LB)
Don Rockey, MDVice Chair
Medical University of South Carolina, Charleston
Nominating committee members
- Gyongyi Szabo, MD, PhD, AGAF, Chair
- Brett Fortune, MD, MSc, Montefiore Medical Center
- Ruben Hernaez, MD, MPH, PhD, Baylor College of Medicine, Houston
- Cynthia Ann Moylan, MD, MHS, MS, Duke University, Durham, North Carolina
- Douglas A. Simonetto, MD, Mayo Clinic, Rochester, Minnesota
Microbiome & Microbial Therapy (MMT)
Jessica Allegretti, MD, MPHVice Chair
Brigham and Women’s Hospital, Boston
Nominating committee members
- Purna C. Kashyap, MBBS, AGAF, Chair
- Melinda Engevik, PhD, Medical University of South Carolina
- Christian Jobin, PhD, University of Florida
- Vanessa Leone, PhD, The University of Wisconsin–Madison
- Jun Yu, MD, PhD, The Chinese University of Hong Kong
Obesity, Metabolism & Nutrition (OMN)
Berkeley M. Limketkai, MD, PhDVice Chair
University of California Los Angeles
Nominating committee members
- Andres Jose Acosta, MD, PhD, Chair
- Barham K. Abu Dayyeh, MD, MPH, Mayo Clinic, Rochester, Minnesota
- Alan L. Buchman, MD, MSPH, University of Illinois at Chicago
- Octavia Pickett-Blakely, MD, MHS, Hospital of the University of Pennsylvania
- Robert Shulman, MD, Texas Children’s Hospital, Baylor College of Medicine
Pediatric Gastroenterology & Developmental Biology (PGDB)
Kelli L. VanDussen, PhDVice Chair
Cincinnati Children’s Hospital Medical Center