User login
DSCs ‘promising’ for severe acute GVHD
Placenta-derived decidua stromal cells (DSCs) can treat severe acute graft-versus-host disease (GVHD), according to a small study.
When given in the optimal way, DSCs produced GVHD responses in all patients, and the 1-year survival rate was 76%.
Steroid-refractory (SR) patients who received DSCs had superior 1-year survival rates compared to SR historical controls and SR patients who received mesenchymal stem cells (MSCs).
Olle Ringdén, MD, PhD, of Karolinska Institutet in Huddinge, Sweden, and his colleagues reported these findings in STEM CELLS Translational Medicine.
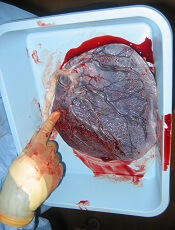
“There were a couple of things that led us to be curious about [DSCs as a treatment for GVHD],” Dr Ringdén said. “First, placenta plays an important role in helping the mother’s body tolerate the developing fetus.”
“[S]econd, placenta has been used in Africa for 100 years to successfully treat burn injuries. This speaks somewhat to its effectiveness and safety. We also found that placenta-derived DSCs are immunosuppressive in vitro and in vivo, which led us to wonder if they might cure severe acute GVHD.”
To test their theory, the team conducted a study of 38 patients with severe acute GVHD, including 25 SR patients.
The patients received DSCs in 1 of 2 groups. In group 1 (n=17), DSCs were infused in buffer supplemented with 10% AB plasma. In group 2 (n=21), the buffer was supplemented with 5% albumin.
Group 1 received significantly fewer infusions than group 2—1 (range, 1-5) and 2 (range, 1-6), respectively (P=0.002). But group 1 had a significantly higher median cell dose—2.0 x 106 DSCs/kg (range, 0.9-2.8) vs 1.2 x 106 DSCs/kg (range, 0.9-2.9; P<0.001).
Cell passage was significantly lower in group 1 than group 2—2 (range, 2-4) and 4 (range, 2-4), respectively (P<0.001). And cell viability was significantly lower in group 1 than 2—90% (range, 70-97) and 95% (range, 69-100), respectively (P<0.001).
Patients
There were no significant differences in baseline characteristics between groups 1 and 2. The median ages were 54.5 (range, 0.9-65.6) and 48.9 (range, 1.6-72.4), respectively.
Most patients were male (9 in group 1 and 16 in group 2), and most had malignant disease (14 and 17, respectively).
The most common graft source was peripheral blood stem cells (14 in group 1 and 16 in group 2), and most patients had a matched, unrelated donor (10 and 14, respectively).
Most patients received reduced-intensity conditioning (9 in group 1 and 17 in group 2) and GVHD prophylaxis with cyclosporine/methotrexate (13 in both groups).
All cases of GVHD were localized to the gut. Fifteen patients in each group had grade 3 GVHD. Two patients in group 1 and 6 in group 2 had grade 2 GVHD.
Results
Responses and survival rates were superior in group 2, but there was no significant difference in relapse or chronic GVHD between the groups.
In group 1, 7 patients did not respond, 5 had a partial response, and 5 had a complete response. In group 2, all patients responded, 10 with a partial response and 11 with a complete response (between-group difference, P=0.01).
The 1-year survival rate was 47% in group 1 and 76% in group 2 (P=0.016). The rate of GVHD-related mortality was 41% and 5%, respectively (P=0.003).
The cumulative incidence of chronic GVHD at 1.5 years was 36% in group 1 and 31% in group 2. The relapse rate was 29% and 18%, respectively.
The researchers compared SR patients in groups 1 (n=13) and 2 (n=11) to SR patients treated with bone marrow-derived MSCs (n=15) and SR historical controls (n=32).
The 1-year survival rate was 73% in SR group 2, which was significantly higher than the 31% survival rate in SR group 1 (P=0.02), the 20% rate in SR MSC recipients (P=0.0015), and the 3% rate in SR historical controls (P<0.001).
Severe adverse events in the DSC recipients included relapse (n=8), pneumonia (n=5), proven or probable invasive fungal infection (n=6), bacterial infection (n=2), graft failure (n=3), multiple organ failure (n=1), viral infection (n=2), central nervous system complications (n=2), septicemia (n=2), skin squamous cell carcinoma (n=2), and acute pancreatitis (n=1).
Causes of death in DSC recipients included acute GVHD (n=9), relapse (n=2), bacterial infection (n=2), invasive fungal infection (n=1), liver failure (n=1), hemorrhage (n=1), and secondary malignancy (n=1).
“Collectively, we think these data demonstrate that DSCs are a promising treatment for severe acute GVHD,” Dr Ringdén said. “But it was a small patient group, so, to further assess safety and efficacy, a larger, prospective trial will be necessary.”
“If an effective therapy for severe acute GVHD is indeed found and validated, it will increase the usefulness of stem cell transplantation with a possible broadening of indications.”
Placenta-derived decidua stromal cells (DSCs) can treat severe acute graft-versus-host disease (GVHD), according to a small study.
When given in the optimal way, DSCs produced GVHD responses in all patients, and the 1-year survival rate was 76%.
Steroid-refractory (SR) patients who received DSCs had superior 1-year survival rates compared to SR historical controls and SR patients who received mesenchymal stem cells (MSCs).
Olle Ringdén, MD, PhD, of Karolinska Institutet in Huddinge, Sweden, and his colleagues reported these findings in STEM CELLS Translational Medicine.
“There were a couple of things that led us to be curious about [DSCs as a treatment for GVHD],” Dr Ringdén said. “First, placenta plays an important role in helping the mother’s body tolerate the developing fetus.”
“[S]econd, placenta has been used in Africa for 100 years to successfully treat burn injuries. This speaks somewhat to its effectiveness and safety. We also found that placenta-derived DSCs are immunosuppressive in vitro and in vivo, which led us to wonder if they might cure severe acute GVHD.”
To test their theory, the team conducted a study of 38 patients with severe acute GVHD, including 25 SR patients.
The patients received DSCs in 1 of 2 groups. In group 1 (n=17), DSCs were infused in buffer supplemented with 10% AB plasma. In group 2 (n=21), the buffer was supplemented with 5% albumin.
Group 1 received significantly fewer infusions than group 2—1 (range, 1-5) and 2 (range, 1-6), respectively (P=0.002). But group 1 had a significantly higher median cell dose—2.0 x 106 DSCs/kg (range, 0.9-2.8) vs 1.2 x 106 DSCs/kg (range, 0.9-2.9; P<0.001).
Cell passage was significantly lower in group 1 than group 2—2 (range, 2-4) and 4 (range, 2-4), respectively (P<0.001). And cell viability was significantly lower in group 1 than 2—90% (range, 70-97) and 95% (range, 69-100), respectively (P<0.001).
Patients
There were no significant differences in baseline characteristics between groups 1 and 2. The median ages were 54.5 (range, 0.9-65.6) and 48.9 (range, 1.6-72.4), respectively.
Most patients were male (9 in group 1 and 16 in group 2), and most had malignant disease (14 and 17, respectively).
The most common graft source was peripheral blood stem cells (14 in group 1 and 16 in group 2), and most patients had a matched, unrelated donor (10 and 14, respectively).
Most patients received reduced-intensity conditioning (9 in group 1 and 17 in group 2) and GVHD prophylaxis with cyclosporine/methotrexate (13 in both groups).
All cases of GVHD were localized to the gut. Fifteen patients in each group had grade 3 GVHD. Two patients in group 1 and 6 in group 2 had grade 2 GVHD.
Results
Responses and survival rates were superior in group 2, but there was no significant difference in relapse or chronic GVHD between the groups.
In group 1, 7 patients did not respond, 5 had a partial response, and 5 had a complete response. In group 2, all patients responded, 10 with a partial response and 11 with a complete response (between-group difference, P=0.01).
The 1-year survival rate was 47% in group 1 and 76% in group 2 (P=0.016). The rate of GVHD-related mortality was 41% and 5%, respectively (P=0.003).
The cumulative incidence of chronic GVHD at 1.5 years was 36% in group 1 and 31% in group 2. The relapse rate was 29% and 18%, respectively.
The researchers compared SR patients in groups 1 (n=13) and 2 (n=11) to SR patients treated with bone marrow-derived MSCs (n=15) and SR historical controls (n=32).
The 1-year survival rate was 73% in SR group 2, which was significantly higher than the 31% survival rate in SR group 1 (P=0.02), the 20% rate in SR MSC recipients (P=0.0015), and the 3% rate in SR historical controls (P<0.001).
Severe adverse events in the DSC recipients included relapse (n=8), pneumonia (n=5), proven or probable invasive fungal infection (n=6), bacterial infection (n=2), graft failure (n=3), multiple organ failure (n=1), viral infection (n=2), central nervous system complications (n=2), septicemia (n=2), skin squamous cell carcinoma (n=2), and acute pancreatitis (n=1).
Causes of death in DSC recipients included acute GVHD (n=9), relapse (n=2), bacterial infection (n=2), invasive fungal infection (n=1), liver failure (n=1), hemorrhage (n=1), and secondary malignancy (n=1).
“Collectively, we think these data demonstrate that DSCs are a promising treatment for severe acute GVHD,” Dr Ringdén said. “But it was a small patient group, so, to further assess safety and efficacy, a larger, prospective trial will be necessary.”
“If an effective therapy for severe acute GVHD is indeed found and validated, it will increase the usefulness of stem cell transplantation with a possible broadening of indications.”
Placenta-derived decidua stromal cells (DSCs) can treat severe acute graft-versus-host disease (GVHD), according to a small study.
When given in the optimal way, DSCs produced GVHD responses in all patients, and the 1-year survival rate was 76%.
Steroid-refractory (SR) patients who received DSCs had superior 1-year survival rates compared to SR historical controls and SR patients who received mesenchymal stem cells (MSCs).
Olle Ringdén, MD, PhD, of Karolinska Institutet in Huddinge, Sweden, and his colleagues reported these findings in STEM CELLS Translational Medicine.
“There were a couple of things that led us to be curious about [DSCs as a treatment for GVHD],” Dr Ringdén said. “First, placenta plays an important role in helping the mother’s body tolerate the developing fetus.”
“[S]econd, placenta has been used in Africa for 100 years to successfully treat burn injuries. This speaks somewhat to its effectiveness and safety. We also found that placenta-derived DSCs are immunosuppressive in vitro and in vivo, which led us to wonder if they might cure severe acute GVHD.”
To test their theory, the team conducted a study of 38 patients with severe acute GVHD, including 25 SR patients.
The patients received DSCs in 1 of 2 groups. In group 1 (n=17), DSCs were infused in buffer supplemented with 10% AB plasma. In group 2 (n=21), the buffer was supplemented with 5% albumin.
Group 1 received significantly fewer infusions than group 2—1 (range, 1-5) and 2 (range, 1-6), respectively (P=0.002). But group 1 had a significantly higher median cell dose—2.0 x 106 DSCs/kg (range, 0.9-2.8) vs 1.2 x 106 DSCs/kg (range, 0.9-2.9; P<0.001).
Cell passage was significantly lower in group 1 than group 2—2 (range, 2-4) and 4 (range, 2-4), respectively (P<0.001). And cell viability was significantly lower in group 1 than 2—90% (range, 70-97) and 95% (range, 69-100), respectively (P<0.001).
Patients
There were no significant differences in baseline characteristics between groups 1 and 2. The median ages were 54.5 (range, 0.9-65.6) and 48.9 (range, 1.6-72.4), respectively.
Most patients were male (9 in group 1 and 16 in group 2), and most had malignant disease (14 and 17, respectively).
The most common graft source was peripheral blood stem cells (14 in group 1 and 16 in group 2), and most patients had a matched, unrelated donor (10 and 14, respectively).
Most patients received reduced-intensity conditioning (9 in group 1 and 17 in group 2) and GVHD prophylaxis with cyclosporine/methotrexate (13 in both groups).
All cases of GVHD were localized to the gut. Fifteen patients in each group had grade 3 GVHD. Two patients in group 1 and 6 in group 2 had grade 2 GVHD.
Results
Responses and survival rates were superior in group 2, but there was no significant difference in relapse or chronic GVHD between the groups.
In group 1, 7 patients did not respond, 5 had a partial response, and 5 had a complete response. In group 2, all patients responded, 10 with a partial response and 11 with a complete response (between-group difference, P=0.01).
The 1-year survival rate was 47% in group 1 and 76% in group 2 (P=0.016). The rate of GVHD-related mortality was 41% and 5%, respectively (P=0.003).
The cumulative incidence of chronic GVHD at 1.5 years was 36% in group 1 and 31% in group 2. The relapse rate was 29% and 18%, respectively.
The researchers compared SR patients in groups 1 (n=13) and 2 (n=11) to SR patients treated with bone marrow-derived MSCs (n=15) and SR historical controls (n=32).
The 1-year survival rate was 73% in SR group 2, which was significantly higher than the 31% survival rate in SR group 1 (P=0.02), the 20% rate in SR MSC recipients (P=0.0015), and the 3% rate in SR historical controls (P<0.001).
Severe adverse events in the DSC recipients included relapse (n=8), pneumonia (n=5), proven or probable invasive fungal infection (n=6), bacterial infection (n=2), graft failure (n=3), multiple organ failure (n=1), viral infection (n=2), central nervous system complications (n=2), septicemia (n=2), skin squamous cell carcinoma (n=2), and acute pancreatitis (n=1).
Causes of death in DSC recipients included acute GVHD (n=9), relapse (n=2), bacterial infection (n=2), invasive fungal infection (n=1), liver failure (n=1), hemorrhage (n=1), and secondary malignancy (n=1).
“Collectively, we think these data demonstrate that DSCs are a promising treatment for severe acute GVHD,” Dr Ringdén said. “But it was a small patient group, so, to further assess safety and efficacy, a larger, prospective trial will be necessary.”
“If an effective therapy for severe acute GVHD is indeed found and validated, it will increase the usefulness of stem cell transplantation with a possible broadening of indications.”
Promising results with expanded UCB product
SALT LAKE CITY—An expanded umbilical cord blood (UCB) product can produce favorable outcomes as a stand-alone graft, according to a presentation at the 2018 BMT Tandem Meetings.
The product, MGTA-456, provided “rapid and durable” engraftment in patients with hematologic malignancies, according to John E. Wagner, MD, of the University of Minnesota in Minneapolis.
He also said MGTA-456 “preserved the clinical benefits” of UCB transplant, including low rates of graft-vs-host disease (GVHD) and high overall survival (OS).
Dr Wagner presented these results as one of the “Best Abstracts” at this year’s BMT Tandem Meetings (abstract 4). The research was supported by Novartis and Magenta Therapeutics.
MGTA-456 is developed by dividing a UCB unit into a CD34- portion and a CD34+ portion, then expanding the CD34+ portion for 15 days via culture with an aryl hydrocarbon receptor antagonist (SR-1), stem cell factor, FLT3 ligand, interleukin-6, and thrombopoietin.
In a previous study,* MGTA-456 enhanced hematopoietic recovery when given as half of a double UCB transplant.
With the current research, Dr Wagner and his colleagues evaluated MGTA-456 as a stand-alone graft. The team conducted two phase 2 trials of MGTA-456, one in which patients received myeloablative conditioning (MAC) and one in which patients received non-myeloablative conditioning (NMAC).
Treatment
Each trial included 10 patients with a high-risk hematologic malignancy and a partially HLA-matched UCB unit. In each trial, 1 patient could not receive MGTA-456 due to low expansion.
So 9 patients received MAC—cyclophosphamide (CY) at 60 mg/kg/day on days -6 and -5, fludarabine (FLU) at 25 mg/m2/day on days -7 to -5, and total body irradiation (TBI) at 1320 cGy on days -4 to -1.
And 9 patients received NMAC—CY at 50 mg/kg on day -6, FLU at 40 mg/m2/day on days -6 to -2, and TBI at 200 cGy on day -1. Some patients who had not received recent chemotherapy also received antithymocyte globulin as part of their conditioning regimen.
For MAC recipients, the median expansion of CD34+ cells was 406-fold (range, 162-1643). The median CD34 cell dose they received was 16.2 x 106/kg.
For NMAC recipients, the median expansion of CD34+ cells was 274-fold (range, 42-527). The median CD34 cell dose they received was 13.4 x 106/kg.
All patients received cyclosporine and mycophenolate mofetil as GVHD prophylaxis.
Dr Wagner and his colleagues compared outcomes in these MGTA-456 recipients to outcomes in historical control subjects—151 patients who received MAC and 132 who received NMAC.
MAC recipients
The 9 MAC/MGTA-456 recipients had a median age of 25 (range, 15-53). Seven of the patients had acute leukemia, 1 had myelodysplastic syndrome (MDS), and 1 had lymphoma.
Eleven percent of patients had high-risk disease, 89% were cytomegalovirus seropositive, and 89% had a Karnofsky performance score of 90 to 100.
The only significant difference between the MGTA-456 recipients and historical controls was weight. The median weight was 93.8 kg (range, 41-107) for MGTA-456 recipients and 66.7 kg (range, 11-136) for controls (P=0.04).
The MGTA-456 recipients had superior hematopoietic recovery compared to historical controls.
The rate of neutrophil engraftment was 100% for MGTA-456 recipients and 89% for controls. The median time to neutrophil engraftment was 14 days and 23 days, respectively (P<0.01).
The rate of platelet engraftment was 89% for MGTA-456 recipients and 71% for controls. The median time to platelet engraftment was 46 days and 64 days, respectively (P=0.01).
There was no significant difference between MGTA-456 recipients and historical controls when it came to GVHD or OS.
The incidence of grade 3-4 acute GVHD at 100 days was 22% for MGTA-456 recipients and 24% for controls (P=0.78). The incidence of chronic GVHD at 1 year was 11% and 21%, respectively (P=0.48).
The 2-year OS rate was 67% in MGTA-456 recipients and 55% in controls (P=0.59).
NMAC recipients
There were significant differences between the 9 NMAC/MGTA-456 recipients and the 132 NMAC historical controls when it came to age (P=0.03), disease type (P<0.01), and disease status (P=0.03).
The median age was 65 (range, 29-70) for MGTA-456 recipients and 53 (range, 6-72) for historical controls. The median weights were 93.4 kg (range, 55-111) and 81.4 kg (range, 22-145), respectively.
Diagnoses among MGTA-456 recipients included acute leukemia (n=1), MDS (n=4), chronic leukemia (n=1), lymphoma (n=1), and “other” (n=2). Diagnoses among historical controls included acute leukemia (n=61), MDS (n=25), chronic leukemia (n=9), lymphoma (n=35), and “other” (n=2).
Eighty-nine percent of MGTA-456 recipients and 49% of historical controls had high-risk disease. Sixty-seven percent and 64%, respectively, were cytomegalovirus seropositive. Sixty-seven percent and 85%, respectively, had a Karnofsky performance score of 90 to 100.
NMAC recipients who received MGTA-456 had superior neutrophil recovery but platelet recovery that was comparable to that of historical controls.
The rate of neutrophil engraftment was 100% in MGTA-456 recipients and 95% in historical controls. The median time to neutrophil engraftment was 7 days and 15 days, respectively (P<0.01).
The rate of platelet engraftment was 56% for MGTA-456 recipients and 77% for historical controls. The median time to platelet engraftment was 107 days and 47 days, respectively (P=0.19).
There was no significant difference between MGTA-456 recipients and historical controls when it came to GVHD or OS.
The incidence of grade 3-4 acute GVHD at 100 days was 43% for MGTA-456 recipients and 15% for controls (P=0.11). The incidence of chronic GVHD at 1 year was 0% and 19%, respectively (P=0.17).
The 2-year OS rate was 44% in MGTA-456 recipients and 49% in controls (P=0.80).
*Wagner JE Jr et al; Phase I/II Trial of StemRegenin-1 Expanded Umbilical Cord Blood Hematopoietic Stem Cells Supports Testing as a Stand-Alone Graft. Cell Stem Cell 2016; 18(1):144-155.
SALT LAKE CITY—An expanded umbilical cord blood (UCB) product can produce favorable outcomes as a stand-alone graft, according to a presentation at the 2018 BMT Tandem Meetings.
The product, MGTA-456, provided “rapid and durable” engraftment in patients with hematologic malignancies, according to John E. Wagner, MD, of the University of Minnesota in Minneapolis.
He also said MGTA-456 “preserved the clinical benefits” of UCB transplant, including low rates of graft-vs-host disease (GVHD) and high overall survival (OS).
Dr Wagner presented these results as one of the “Best Abstracts” at this year’s BMT Tandem Meetings (abstract 4). The research was supported by Novartis and Magenta Therapeutics.
MGTA-456 is developed by dividing a UCB unit into a CD34- portion and a CD34+ portion, then expanding the CD34+ portion for 15 days via culture with an aryl hydrocarbon receptor antagonist (SR-1), stem cell factor, FLT3 ligand, interleukin-6, and thrombopoietin.
In a previous study,* MGTA-456 enhanced hematopoietic recovery when given as half of a double UCB transplant.
With the current research, Dr Wagner and his colleagues evaluated MGTA-456 as a stand-alone graft. The team conducted two phase 2 trials of MGTA-456, one in which patients received myeloablative conditioning (MAC) and one in which patients received non-myeloablative conditioning (NMAC).
Treatment
Each trial included 10 patients with a high-risk hematologic malignancy and a partially HLA-matched UCB unit. In each trial, 1 patient could not receive MGTA-456 due to low expansion.
So 9 patients received MAC—cyclophosphamide (CY) at 60 mg/kg/day on days -6 and -5, fludarabine (FLU) at 25 mg/m2/day on days -7 to -5, and total body irradiation (TBI) at 1320 cGy on days -4 to -1.
And 9 patients received NMAC—CY at 50 mg/kg on day -6, FLU at 40 mg/m2/day on days -6 to -2, and TBI at 200 cGy on day -1. Some patients who had not received recent chemotherapy also received antithymocyte globulin as part of their conditioning regimen.
For MAC recipients, the median expansion of CD34+ cells was 406-fold (range, 162-1643). The median CD34 cell dose they received was 16.2 x 106/kg.
For NMAC recipients, the median expansion of CD34+ cells was 274-fold (range, 42-527). The median CD34 cell dose they received was 13.4 x 106/kg.
All patients received cyclosporine and mycophenolate mofetil as GVHD prophylaxis.
Dr Wagner and his colleagues compared outcomes in these MGTA-456 recipients to outcomes in historical control subjects—151 patients who received MAC and 132 who received NMAC.
MAC recipients
The 9 MAC/MGTA-456 recipients had a median age of 25 (range, 15-53). Seven of the patients had acute leukemia, 1 had myelodysplastic syndrome (MDS), and 1 had lymphoma.
Eleven percent of patients had high-risk disease, 89% were cytomegalovirus seropositive, and 89% had a Karnofsky performance score of 90 to 100.
The only significant difference between the MGTA-456 recipients and historical controls was weight. The median weight was 93.8 kg (range, 41-107) for MGTA-456 recipients and 66.7 kg (range, 11-136) for controls (P=0.04).
The MGTA-456 recipients had superior hematopoietic recovery compared to historical controls.
The rate of neutrophil engraftment was 100% for MGTA-456 recipients and 89% for controls. The median time to neutrophil engraftment was 14 days and 23 days, respectively (P<0.01).
The rate of platelet engraftment was 89% for MGTA-456 recipients and 71% for controls. The median time to platelet engraftment was 46 days and 64 days, respectively (P=0.01).
There was no significant difference between MGTA-456 recipients and historical controls when it came to GVHD or OS.
The incidence of grade 3-4 acute GVHD at 100 days was 22% for MGTA-456 recipients and 24% for controls (P=0.78). The incidence of chronic GVHD at 1 year was 11% and 21%, respectively (P=0.48).
The 2-year OS rate was 67% in MGTA-456 recipients and 55% in controls (P=0.59).
NMAC recipients
There were significant differences between the 9 NMAC/MGTA-456 recipients and the 132 NMAC historical controls when it came to age (P=0.03), disease type (P<0.01), and disease status (P=0.03).
The median age was 65 (range, 29-70) for MGTA-456 recipients and 53 (range, 6-72) for historical controls. The median weights were 93.4 kg (range, 55-111) and 81.4 kg (range, 22-145), respectively.
Diagnoses among MGTA-456 recipients included acute leukemia (n=1), MDS (n=4), chronic leukemia (n=1), lymphoma (n=1), and “other” (n=2). Diagnoses among historical controls included acute leukemia (n=61), MDS (n=25), chronic leukemia (n=9), lymphoma (n=35), and “other” (n=2).
Eighty-nine percent of MGTA-456 recipients and 49% of historical controls had high-risk disease. Sixty-seven percent and 64%, respectively, were cytomegalovirus seropositive. Sixty-seven percent and 85%, respectively, had a Karnofsky performance score of 90 to 100.
NMAC recipients who received MGTA-456 had superior neutrophil recovery but platelet recovery that was comparable to that of historical controls.
The rate of neutrophil engraftment was 100% in MGTA-456 recipients and 95% in historical controls. The median time to neutrophil engraftment was 7 days and 15 days, respectively (P<0.01).
The rate of platelet engraftment was 56% for MGTA-456 recipients and 77% for historical controls. The median time to platelet engraftment was 107 days and 47 days, respectively (P=0.19).
There was no significant difference between MGTA-456 recipients and historical controls when it came to GVHD or OS.
The incidence of grade 3-4 acute GVHD at 100 days was 43% for MGTA-456 recipients and 15% for controls (P=0.11). The incidence of chronic GVHD at 1 year was 0% and 19%, respectively (P=0.17).
The 2-year OS rate was 44% in MGTA-456 recipients and 49% in controls (P=0.80).
*Wagner JE Jr et al; Phase I/II Trial of StemRegenin-1 Expanded Umbilical Cord Blood Hematopoietic Stem Cells Supports Testing as a Stand-Alone Graft. Cell Stem Cell 2016; 18(1):144-155.
SALT LAKE CITY—An expanded umbilical cord blood (UCB) product can produce favorable outcomes as a stand-alone graft, according to a presentation at the 2018 BMT Tandem Meetings.
The product, MGTA-456, provided “rapid and durable” engraftment in patients with hematologic malignancies, according to John E. Wagner, MD, of the University of Minnesota in Minneapolis.
He also said MGTA-456 “preserved the clinical benefits” of UCB transplant, including low rates of graft-vs-host disease (GVHD) and high overall survival (OS).
Dr Wagner presented these results as one of the “Best Abstracts” at this year’s BMT Tandem Meetings (abstract 4). The research was supported by Novartis and Magenta Therapeutics.
MGTA-456 is developed by dividing a UCB unit into a CD34- portion and a CD34+ portion, then expanding the CD34+ portion for 15 days via culture with an aryl hydrocarbon receptor antagonist (SR-1), stem cell factor, FLT3 ligand, interleukin-6, and thrombopoietin.
In a previous study,* MGTA-456 enhanced hematopoietic recovery when given as half of a double UCB transplant.
With the current research, Dr Wagner and his colleagues evaluated MGTA-456 as a stand-alone graft. The team conducted two phase 2 trials of MGTA-456, one in which patients received myeloablative conditioning (MAC) and one in which patients received non-myeloablative conditioning (NMAC).
Treatment
Each trial included 10 patients with a high-risk hematologic malignancy and a partially HLA-matched UCB unit. In each trial, 1 patient could not receive MGTA-456 due to low expansion.
So 9 patients received MAC—cyclophosphamide (CY) at 60 mg/kg/day on days -6 and -5, fludarabine (FLU) at 25 mg/m2/day on days -7 to -5, and total body irradiation (TBI) at 1320 cGy on days -4 to -1.
And 9 patients received NMAC—CY at 50 mg/kg on day -6, FLU at 40 mg/m2/day on days -6 to -2, and TBI at 200 cGy on day -1. Some patients who had not received recent chemotherapy also received antithymocyte globulin as part of their conditioning regimen.
For MAC recipients, the median expansion of CD34+ cells was 406-fold (range, 162-1643). The median CD34 cell dose they received was 16.2 x 106/kg.
For NMAC recipients, the median expansion of CD34+ cells was 274-fold (range, 42-527). The median CD34 cell dose they received was 13.4 x 106/kg.
All patients received cyclosporine and mycophenolate mofetil as GVHD prophylaxis.
Dr Wagner and his colleagues compared outcomes in these MGTA-456 recipients to outcomes in historical control subjects—151 patients who received MAC and 132 who received NMAC.
MAC recipients
The 9 MAC/MGTA-456 recipients had a median age of 25 (range, 15-53). Seven of the patients had acute leukemia, 1 had myelodysplastic syndrome (MDS), and 1 had lymphoma.
Eleven percent of patients had high-risk disease, 89% were cytomegalovirus seropositive, and 89% had a Karnofsky performance score of 90 to 100.
The only significant difference between the MGTA-456 recipients and historical controls was weight. The median weight was 93.8 kg (range, 41-107) for MGTA-456 recipients and 66.7 kg (range, 11-136) for controls (P=0.04).
The MGTA-456 recipients had superior hematopoietic recovery compared to historical controls.
The rate of neutrophil engraftment was 100% for MGTA-456 recipients and 89% for controls. The median time to neutrophil engraftment was 14 days and 23 days, respectively (P<0.01).
The rate of platelet engraftment was 89% for MGTA-456 recipients and 71% for controls. The median time to platelet engraftment was 46 days and 64 days, respectively (P=0.01).
There was no significant difference between MGTA-456 recipients and historical controls when it came to GVHD or OS.
The incidence of grade 3-4 acute GVHD at 100 days was 22% for MGTA-456 recipients and 24% for controls (P=0.78). The incidence of chronic GVHD at 1 year was 11% and 21%, respectively (P=0.48).
The 2-year OS rate was 67% in MGTA-456 recipients and 55% in controls (P=0.59).
NMAC recipients
There were significant differences between the 9 NMAC/MGTA-456 recipients and the 132 NMAC historical controls when it came to age (P=0.03), disease type (P<0.01), and disease status (P=0.03).
The median age was 65 (range, 29-70) for MGTA-456 recipients and 53 (range, 6-72) for historical controls. The median weights were 93.4 kg (range, 55-111) and 81.4 kg (range, 22-145), respectively.
Diagnoses among MGTA-456 recipients included acute leukemia (n=1), MDS (n=4), chronic leukemia (n=1), lymphoma (n=1), and “other” (n=2). Diagnoses among historical controls included acute leukemia (n=61), MDS (n=25), chronic leukemia (n=9), lymphoma (n=35), and “other” (n=2).
Eighty-nine percent of MGTA-456 recipients and 49% of historical controls had high-risk disease. Sixty-seven percent and 64%, respectively, were cytomegalovirus seropositive. Sixty-seven percent and 85%, respectively, had a Karnofsky performance score of 90 to 100.
NMAC recipients who received MGTA-456 had superior neutrophil recovery but platelet recovery that was comparable to that of historical controls.
The rate of neutrophil engraftment was 100% in MGTA-456 recipients and 95% in historical controls. The median time to neutrophil engraftment was 7 days and 15 days, respectively (P<0.01).
The rate of platelet engraftment was 56% for MGTA-456 recipients and 77% for historical controls. The median time to platelet engraftment was 107 days and 47 days, respectively (P=0.19).
There was no significant difference between MGTA-456 recipients and historical controls when it came to GVHD or OS.
The incidence of grade 3-4 acute GVHD at 100 days was 43% for MGTA-456 recipients and 15% for controls (P=0.11). The incidence of chronic GVHD at 1 year was 0% and 19%, respectively (P=0.17).
The 2-year OS rate was 44% in MGTA-456 recipients and 49% in controls (P=0.80).
*Wagner JE Jr et al; Phase I/II Trial of StemRegenin-1 Expanded Umbilical Cord Blood Hematopoietic Stem Cells Supports Testing as a Stand-Alone Graft. Cell Stem Cell 2016; 18(1):144-155.
Outcomes appear similar with MAC and RIC
SALT LAKE CITY—New research suggests outcomes may be similar whether patients receive myeloablative conditioning (MAC) or reduced-intensity conditioning (RIC) prior to haploidentical peripheral blood stem cell transplant (haploPBSCT) with post-transplant cyclophosphamide (PTCy).
Results from 2 parallel, phase 2 trials showed that MAC-PTCy-haploPBSCT and RIC-PTCy-haploPBSCT produced comparable rates of engraftment, acute and chronic graft-versus host disease (GVHD), relapse, and non-relapse mortality (NRM).
Rates of overall survival (OS) and event-free survival (EFS) were significantly higher in the MAC group. However, the fact that some RIC recipients had received prior allogeneic transplants—and none of the MAC recipients had—appeared to play a role in survival outcomes.
Junichi Sugita, MD, PhD, of Hokkaido University in Sapporo, Japan, presented these results at the 2018 BMT Tandem Meetings (abstract 50*).
To compare MAC and RIC in the context of PTCy-haploPBSCT, Dr Sugita and his colleagues conducted 2 parallel studies—JSCT Haplo 14 MAC and JSCT Haplo 14 RIC.
Patients
There were 50 patients in the MAC trial and 77 in the RIC trial. They had median ages of 36 (range, 17 to 60) and 58 (range, 22 to 65), respectively (P<0.01). There was a greater percentage of male patients among MAC recipients (82% vs 62%, P=0.028).
Diagnoses were similar between the groups and included:
- Acute myeloid leukemia—23 MAC, 34 RIC
- Acute lymphoblastic leukemia—11 MAC, 14 RIC
- Myelodysplastic syndromes/myeloproliferative neoplasms—6 MAC, 12 RIC
- Lymphoma—6 MAC, 14 RIC
- “Other”—4 MAC, 3 RIC.
Forty-eight percent (n=24) of MAC recipients and 58% (n=45) of RIC recipients were not in remission at transplant (P=0.48). There were no significant differences in disease risk index (P=0.34).
Thirty-nine percent of RIC recipients (n=30) had a history of allogeneic transplant, but none of the MAC recipients did (P<0.01).
Conditioning and prophylaxis
There were 2 MAC regimens. One consisted of fludarabine (Flu, 30 mg/m2/day on days -6 to -4) plus total body irradiation (TBI, 12 Gy on days -3 to -1). The other consisted of Flu (30 mg/m2/day on days -6 to -2), busulfan (BU, 3.2 mg/kg/day on days -6 to -3), and TBI (4 Gy on day -1).
The RIC regimen consisted of Flu (30 mg/m2/day on days -6 to -2), BU (3.2 mg/kg/day on days -4 to -3), and TBI (4 Gy on day -1).
All patients received GVHD prophylaxis consisting of cyclophosphamide (50 mg/kg/day on days 3 and 4), tacrolimus (days 5 to 180), and mycophenolate mofetil (days 5 to 60).
Graft
Siblings were the most common donors for MAC recipients (50%, n=25), followed by parents (28%, n=14), children (16%, n=8), and “other” donors (6%, n=3).
Children were the most common donors for RIC recipients (60%, n=46), followed by siblings (33%, n=25), and parents (8%, n=6).
There was no significant difference between MAC and RIC recipients when it came to human leukocyte antigen matching, cytomegalovirus serostatus, or CD34 cell dose.
However, there was a significant difference in donor-recipient gender matching (P=0.033).
Fifty-two percent (n=26) of MAC recipients and 62% (n=48) of RIC recipients had a donor-recipient gender match. Forty-two percent (n=21) and 22% (n=17), respectively, had female donor to male recipient.
Engraftment and GVHD
“Hematopoietic recovery was similar between MAC and RIC,” Dr Sugita said.
The cumulative incidence of neutrophil engraftment was 98% in MAC recipients and 94% in RIC recipients. The median time to neutrophil engraftment was 17 days and 18 days, respectively (P=0.10).
The cumulative incidence of platelet engraftment was 84% in the MAC recipients and 74% in the RIC recipients. The median time to platelet engraftment was 31 days and 37 days, respectively (P=0.32).
“Complete chimerism was achieved in all engrafted patients,” Dr Sugita noted.
There was no significant difference between MAC and RIC recipients when it came to acute or chronic GVHD.
At day 100, the cumulative incidence of grade 2-4 acute GVHD was 18% in the MAC group and 14% in the RIC group (P=0.52). Grade 3-4 acute GVHD was 8% and 5%, respectively (P=0.52).
At 2 years, the cumulative incidence of all-grade chronic GVHD was 36% in the MAC group and 27% in the RIC group (P=0.24). Moderate to severe chronic GVHD was 20% in both groups (P=1.0).
Relapse and survival
There was no significant between-group difference in NRM or relapse.
The cumulative incidence of NRM at 2 years was 20% in the RIC group and 10% in the MAC group (P=0.15). The cumulative incidence of relapse at 2 years was 45% and 36%, respectively (P=0.32).
Survival was superior in the MAC recipients. The 2-year OS was 68% in the MAC group and 44% in the RIC group (P=0.02). The 2-year EFS was 54% and 35%, respectively (P=0.04).
However, survival appeared to be affected by history of allogeneic transplant.
“Patients with a history of prior allogenic SCT have significantly worse overall survival and event-free survival,” Dr Sugita said.
Two-year OS was 31% in RIC recipients with a history of transplant and 52% in RIC recipients without a history of transplant (P=0.04). The OS was 68% in MAC recipients, all of whom had no history of transplant.
Two-year EFS was 21%, 44%, and 54%, respectively (P=0.02 for difference between 2 RIC groups).
In a multivariate analysis, conditioning regimen was not a significant predictor of NRM. The hazard ratio (HR) for RIC was 1.13 (P=0.85).
Likewise, conditioning regimen was not a significant predictor of relapse (HR=0.81, P=0.53), OS (HR=0.85, P=0.66), or EFS (HR=0.73, P=0.34).
“Our results indicate that both MAC and RIC are valid options for PTCy-haplo,” Dr Sugita said in closing.
“Ideally, a more precise comparison of MAC and RIC should be studied further in the setting of, if possible, a randomized trial.”
*Data in the abstract differs from the presentation.
SALT LAKE CITY—New research suggests outcomes may be similar whether patients receive myeloablative conditioning (MAC) or reduced-intensity conditioning (RIC) prior to haploidentical peripheral blood stem cell transplant (haploPBSCT) with post-transplant cyclophosphamide (PTCy).
Results from 2 parallel, phase 2 trials showed that MAC-PTCy-haploPBSCT and RIC-PTCy-haploPBSCT produced comparable rates of engraftment, acute and chronic graft-versus host disease (GVHD), relapse, and non-relapse mortality (NRM).
Rates of overall survival (OS) and event-free survival (EFS) were significantly higher in the MAC group. However, the fact that some RIC recipients had received prior allogeneic transplants—and none of the MAC recipients had—appeared to play a role in survival outcomes.
Junichi Sugita, MD, PhD, of Hokkaido University in Sapporo, Japan, presented these results at the 2018 BMT Tandem Meetings (abstract 50*).
To compare MAC and RIC in the context of PTCy-haploPBSCT, Dr Sugita and his colleagues conducted 2 parallel studies—JSCT Haplo 14 MAC and JSCT Haplo 14 RIC.
Patients
There were 50 patients in the MAC trial and 77 in the RIC trial. They had median ages of 36 (range, 17 to 60) and 58 (range, 22 to 65), respectively (P<0.01). There was a greater percentage of male patients among MAC recipients (82% vs 62%, P=0.028).
Diagnoses were similar between the groups and included:
- Acute myeloid leukemia—23 MAC, 34 RIC
- Acute lymphoblastic leukemia—11 MAC, 14 RIC
- Myelodysplastic syndromes/myeloproliferative neoplasms—6 MAC, 12 RIC
- Lymphoma—6 MAC, 14 RIC
- “Other”—4 MAC, 3 RIC.
Forty-eight percent (n=24) of MAC recipients and 58% (n=45) of RIC recipients were not in remission at transplant (P=0.48). There were no significant differences in disease risk index (P=0.34).
Thirty-nine percent of RIC recipients (n=30) had a history of allogeneic transplant, but none of the MAC recipients did (P<0.01).
Conditioning and prophylaxis
There were 2 MAC regimens. One consisted of fludarabine (Flu, 30 mg/m2/day on days -6 to -4) plus total body irradiation (TBI, 12 Gy on days -3 to -1). The other consisted of Flu (30 mg/m2/day on days -6 to -2), busulfan (BU, 3.2 mg/kg/day on days -6 to -3), and TBI (4 Gy on day -1).
The RIC regimen consisted of Flu (30 mg/m2/day on days -6 to -2), BU (3.2 mg/kg/day on days -4 to -3), and TBI (4 Gy on day -1).
All patients received GVHD prophylaxis consisting of cyclophosphamide (50 mg/kg/day on days 3 and 4), tacrolimus (days 5 to 180), and mycophenolate mofetil (days 5 to 60).
Graft
Siblings were the most common donors for MAC recipients (50%, n=25), followed by parents (28%, n=14), children (16%, n=8), and “other” donors (6%, n=3).
Children were the most common donors for RIC recipients (60%, n=46), followed by siblings (33%, n=25), and parents (8%, n=6).
There was no significant difference between MAC and RIC recipients when it came to human leukocyte antigen matching, cytomegalovirus serostatus, or CD34 cell dose.
However, there was a significant difference in donor-recipient gender matching (P=0.033).
Fifty-two percent (n=26) of MAC recipients and 62% (n=48) of RIC recipients had a donor-recipient gender match. Forty-two percent (n=21) and 22% (n=17), respectively, had female donor to male recipient.
Engraftment and GVHD
“Hematopoietic recovery was similar between MAC and RIC,” Dr Sugita said.
The cumulative incidence of neutrophil engraftment was 98% in MAC recipients and 94% in RIC recipients. The median time to neutrophil engraftment was 17 days and 18 days, respectively (P=0.10).
The cumulative incidence of platelet engraftment was 84% in the MAC recipients and 74% in the RIC recipients. The median time to platelet engraftment was 31 days and 37 days, respectively (P=0.32).
“Complete chimerism was achieved in all engrafted patients,” Dr Sugita noted.
There was no significant difference between MAC and RIC recipients when it came to acute or chronic GVHD.
At day 100, the cumulative incidence of grade 2-4 acute GVHD was 18% in the MAC group and 14% in the RIC group (P=0.52). Grade 3-4 acute GVHD was 8% and 5%, respectively (P=0.52).
At 2 years, the cumulative incidence of all-grade chronic GVHD was 36% in the MAC group and 27% in the RIC group (P=0.24). Moderate to severe chronic GVHD was 20% in both groups (P=1.0).
Relapse and survival
There was no significant between-group difference in NRM or relapse.
The cumulative incidence of NRM at 2 years was 20% in the RIC group and 10% in the MAC group (P=0.15). The cumulative incidence of relapse at 2 years was 45% and 36%, respectively (P=0.32).
Survival was superior in the MAC recipients. The 2-year OS was 68% in the MAC group and 44% in the RIC group (P=0.02). The 2-year EFS was 54% and 35%, respectively (P=0.04).
However, survival appeared to be affected by history of allogeneic transplant.
“Patients with a history of prior allogenic SCT have significantly worse overall survival and event-free survival,” Dr Sugita said.
Two-year OS was 31% in RIC recipients with a history of transplant and 52% in RIC recipients without a history of transplant (P=0.04). The OS was 68% in MAC recipients, all of whom had no history of transplant.
Two-year EFS was 21%, 44%, and 54%, respectively (P=0.02 for difference between 2 RIC groups).
In a multivariate analysis, conditioning regimen was not a significant predictor of NRM. The hazard ratio (HR) for RIC was 1.13 (P=0.85).
Likewise, conditioning regimen was not a significant predictor of relapse (HR=0.81, P=0.53), OS (HR=0.85, P=0.66), or EFS (HR=0.73, P=0.34).
“Our results indicate that both MAC and RIC are valid options for PTCy-haplo,” Dr Sugita said in closing.
“Ideally, a more precise comparison of MAC and RIC should be studied further in the setting of, if possible, a randomized trial.”
*Data in the abstract differs from the presentation.
SALT LAKE CITY—New research suggests outcomes may be similar whether patients receive myeloablative conditioning (MAC) or reduced-intensity conditioning (RIC) prior to haploidentical peripheral blood stem cell transplant (haploPBSCT) with post-transplant cyclophosphamide (PTCy).
Results from 2 parallel, phase 2 trials showed that MAC-PTCy-haploPBSCT and RIC-PTCy-haploPBSCT produced comparable rates of engraftment, acute and chronic graft-versus host disease (GVHD), relapse, and non-relapse mortality (NRM).
Rates of overall survival (OS) and event-free survival (EFS) were significantly higher in the MAC group. However, the fact that some RIC recipients had received prior allogeneic transplants—and none of the MAC recipients had—appeared to play a role in survival outcomes.
Junichi Sugita, MD, PhD, of Hokkaido University in Sapporo, Japan, presented these results at the 2018 BMT Tandem Meetings (abstract 50*).
To compare MAC and RIC in the context of PTCy-haploPBSCT, Dr Sugita and his colleagues conducted 2 parallel studies—JSCT Haplo 14 MAC and JSCT Haplo 14 RIC.
Patients
There were 50 patients in the MAC trial and 77 in the RIC trial. They had median ages of 36 (range, 17 to 60) and 58 (range, 22 to 65), respectively (P<0.01). There was a greater percentage of male patients among MAC recipients (82% vs 62%, P=0.028).
Diagnoses were similar between the groups and included:
- Acute myeloid leukemia—23 MAC, 34 RIC
- Acute lymphoblastic leukemia—11 MAC, 14 RIC
- Myelodysplastic syndromes/myeloproliferative neoplasms—6 MAC, 12 RIC
- Lymphoma—6 MAC, 14 RIC
- “Other”—4 MAC, 3 RIC.
Forty-eight percent (n=24) of MAC recipients and 58% (n=45) of RIC recipients were not in remission at transplant (P=0.48). There were no significant differences in disease risk index (P=0.34).
Thirty-nine percent of RIC recipients (n=30) had a history of allogeneic transplant, but none of the MAC recipients did (P<0.01).
Conditioning and prophylaxis
There were 2 MAC regimens. One consisted of fludarabine (Flu, 30 mg/m2/day on days -6 to -4) plus total body irradiation (TBI, 12 Gy on days -3 to -1). The other consisted of Flu (30 mg/m2/day on days -6 to -2), busulfan (BU, 3.2 mg/kg/day on days -6 to -3), and TBI (4 Gy on day -1).
The RIC regimen consisted of Flu (30 mg/m2/day on days -6 to -2), BU (3.2 mg/kg/day on days -4 to -3), and TBI (4 Gy on day -1).
All patients received GVHD prophylaxis consisting of cyclophosphamide (50 mg/kg/day on days 3 and 4), tacrolimus (days 5 to 180), and mycophenolate mofetil (days 5 to 60).
Graft
Siblings were the most common donors for MAC recipients (50%, n=25), followed by parents (28%, n=14), children (16%, n=8), and “other” donors (6%, n=3).
Children were the most common donors for RIC recipients (60%, n=46), followed by siblings (33%, n=25), and parents (8%, n=6).
There was no significant difference between MAC and RIC recipients when it came to human leukocyte antigen matching, cytomegalovirus serostatus, or CD34 cell dose.
However, there was a significant difference in donor-recipient gender matching (P=0.033).
Fifty-two percent (n=26) of MAC recipients and 62% (n=48) of RIC recipients had a donor-recipient gender match. Forty-two percent (n=21) and 22% (n=17), respectively, had female donor to male recipient.
Engraftment and GVHD
“Hematopoietic recovery was similar between MAC and RIC,” Dr Sugita said.
The cumulative incidence of neutrophil engraftment was 98% in MAC recipients and 94% in RIC recipients. The median time to neutrophil engraftment was 17 days and 18 days, respectively (P=0.10).
The cumulative incidence of platelet engraftment was 84% in the MAC recipients and 74% in the RIC recipients. The median time to platelet engraftment was 31 days and 37 days, respectively (P=0.32).
“Complete chimerism was achieved in all engrafted patients,” Dr Sugita noted.
There was no significant difference between MAC and RIC recipients when it came to acute or chronic GVHD.
At day 100, the cumulative incidence of grade 2-4 acute GVHD was 18% in the MAC group and 14% in the RIC group (P=0.52). Grade 3-4 acute GVHD was 8% and 5%, respectively (P=0.52).
At 2 years, the cumulative incidence of all-grade chronic GVHD was 36% in the MAC group and 27% in the RIC group (P=0.24). Moderate to severe chronic GVHD was 20% in both groups (P=1.0).
Relapse and survival
There was no significant between-group difference in NRM or relapse.
The cumulative incidence of NRM at 2 years was 20% in the RIC group and 10% in the MAC group (P=0.15). The cumulative incidence of relapse at 2 years was 45% and 36%, respectively (P=0.32).
Survival was superior in the MAC recipients. The 2-year OS was 68% in the MAC group and 44% in the RIC group (P=0.02). The 2-year EFS was 54% and 35%, respectively (P=0.04).
However, survival appeared to be affected by history of allogeneic transplant.
“Patients with a history of prior allogenic SCT have significantly worse overall survival and event-free survival,” Dr Sugita said.
Two-year OS was 31% in RIC recipients with a history of transplant and 52% in RIC recipients without a history of transplant (P=0.04). The OS was 68% in MAC recipients, all of whom had no history of transplant.
Two-year EFS was 21%, 44%, and 54%, respectively (P=0.02 for difference between 2 RIC groups).
In a multivariate analysis, conditioning regimen was not a significant predictor of NRM. The hazard ratio (HR) for RIC was 1.13 (P=0.85).
Likewise, conditioning regimen was not a significant predictor of relapse (HR=0.81, P=0.53), OS (HR=0.85, P=0.66), or EFS (HR=0.73, P=0.34).
“Our results indicate that both MAC and RIC are valid options for PTCy-haplo,” Dr Sugita said in closing.
“Ideally, a more precise comparison of MAC and RIC should be studied further in the setting of, if possible, a randomized trial.”
*Data in the abstract differs from the presentation.
Agent can reveal HSC engraftment faster
An imaging agent can safely show engraftment of hematopoietic stem cells (HSCs) just days after transplant, according to research published in The Lancet Haematology.
The agent is 18F-fluorothymidine (18F-FLT), a radio-labeled analogue of thymidine.
Past studies have shown that 18F-FLT is incorporated into HSCs.
With the current study, researchers wanted to determine if 18F-FLT could allow them to safely visualize transplanted HSCs.
Kirsten M. Williams, MD, of Children’s National Health System in Washington, DC, and her colleagues tested 18F-FLT in 23 patients undergoing HSC transplant to treat high-risk hematologic malignancies.
The patients first underwent total body irradiation to destroy their own HSCs and then received donor HSCs.
The patients underwent PET/CT scans 1 day before they were infused with HSCs as well as post-transplant at 5 or 9 days, 28 days, and 1 year.
Results
All patients engrafted, a finding that was reflected in blood tests conducted 2 to 4 weeks after transplant. However, imaging results revealed more details.
“Through the images we took, these patients could see the new cells growing in their bodies,” Dr Williams said. “They loved that.”
The researchers and the patients saw the HSCs take a complex journey as they engrafted.
First, HSCs migrated to the patients’ livers and spleens. Next, the cells went to the thoracic spine, the axial spine, the sternum, and the arms and legs.
By 1 year, most of the HSCs were concentrated in the bones that make up the trunk of the body, including the hip, where most biopsies to assess marrow function take place.
This pathway is the same one HSCs take in the fetus when they first form.
The researchers also found the radiation in 18F-FLT did not adversely affect engraftment.
And imaging could reveal successful engraftment at 5 days post-transplant, “which was up to 20 days before engraftment became clinically evident,” according to the researchers.
Dr Williams and her colleagues believe use of 18F-FLT could potentially help patients avoid bone marrow biopsies or, at the very least, help target those biopsies.
And the agent might be helpful for taking stock of HSCs in conditions such as aplastic anemia.
“What happens with HSCs always has been a mystery,” Dr Williams said. “Now, we can start to open that black box.”
An imaging agent can safely show engraftment of hematopoietic stem cells (HSCs) just days after transplant, according to research published in The Lancet Haematology.
The agent is 18F-fluorothymidine (18F-FLT), a radio-labeled analogue of thymidine.
Past studies have shown that 18F-FLT is incorporated into HSCs.
With the current study, researchers wanted to determine if 18F-FLT could allow them to safely visualize transplanted HSCs.
Kirsten M. Williams, MD, of Children’s National Health System in Washington, DC, and her colleagues tested 18F-FLT in 23 patients undergoing HSC transplant to treat high-risk hematologic malignancies.
The patients first underwent total body irradiation to destroy their own HSCs and then received donor HSCs.
The patients underwent PET/CT scans 1 day before they were infused with HSCs as well as post-transplant at 5 or 9 days, 28 days, and 1 year.
Results
All patients engrafted, a finding that was reflected in blood tests conducted 2 to 4 weeks after transplant. However, imaging results revealed more details.
“Through the images we took, these patients could see the new cells growing in their bodies,” Dr Williams said. “They loved that.”
The researchers and the patients saw the HSCs take a complex journey as they engrafted.
First, HSCs migrated to the patients’ livers and spleens. Next, the cells went to the thoracic spine, the axial spine, the sternum, and the arms and legs.
By 1 year, most of the HSCs were concentrated in the bones that make up the trunk of the body, including the hip, where most biopsies to assess marrow function take place.
This pathway is the same one HSCs take in the fetus when they first form.
The researchers also found the radiation in 18F-FLT did not adversely affect engraftment.
And imaging could reveal successful engraftment at 5 days post-transplant, “which was up to 20 days before engraftment became clinically evident,” according to the researchers.
Dr Williams and her colleagues believe use of 18F-FLT could potentially help patients avoid bone marrow biopsies or, at the very least, help target those biopsies.
And the agent might be helpful for taking stock of HSCs in conditions such as aplastic anemia.
“What happens with HSCs always has been a mystery,” Dr Williams said. “Now, we can start to open that black box.”
An imaging agent can safely show engraftment of hematopoietic stem cells (HSCs) just days after transplant, according to research published in The Lancet Haematology.
The agent is 18F-fluorothymidine (18F-FLT), a radio-labeled analogue of thymidine.
Past studies have shown that 18F-FLT is incorporated into HSCs.
With the current study, researchers wanted to determine if 18F-FLT could allow them to safely visualize transplanted HSCs.
Kirsten M. Williams, MD, of Children’s National Health System in Washington, DC, and her colleagues tested 18F-FLT in 23 patients undergoing HSC transplant to treat high-risk hematologic malignancies.
The patients first underwent total body irradiation to destroy their own HSCs and then received donor HSCs.
The patients underwent PET/CT scans 1 day before they were infused with HSCs as well as post-transplant at 5 or 9 days, 28 days, and 1 year.
Results
All patients engrafted, a finding that was reflected in blood tests conducted 2 to 4 weeks after transplant. However, imaging results revealed more details.
“Through the images we took, these patients could see the new cells growing in their bodies,” Dr Williams said. “They loved that.”
The researchers and the patients saw the HSCs take a complex journey as they engrafted.
First, HSCs migrated to the patients’ livers and spleens. Next, the cells went to the thoracic spine, the axial spine, the sternum, and the arms and legs.
By 1 year, most of the HSCs were concentrated in the bones that make up the trunk of the body, including the hip, where most biopsies to assess marrow function take place.
This pathway is the same one HSCs take in the fetus when they first form.
The researchers also found the radiation in 18F-FLT did not adversely affect engraftment.
And imaging could reveal successful engraftment at 5 days post-transplant, “which was up to 20 days before engraftment became clinically evident,” according to the researchers.
Dr Williams and her colleagues believe use of 18F-FLT could potentially help patients avoid bone marrow biopsies or, at the very least, help target those biopsies.
And the agent might be helpful for taking stock of HSCs in conditions such as aplastic anemia.
“What happens with HSCs always has been a mystery,” Dr Williams said. “Now, we can start to open that black box.”
HSCT approach provides ‘excellent’ survival in FA
SALT LAKE CITY—A “risk-adjusted” approach leads to “excellent” survival in patients with Fanconi anemia (FA) undergoing alternative donor hematopoietic stem cell transplant (HSCT), according to a speaker at the 2018 BMT Tandem Meetings.
All FA patients who received personalized doses of busulfan in place of total body irradiation (TBI) were alive and disease-free after undergoing HSCT for bone marrow failure or myelodysplastic syndrome (MDS).
None of the patients developed graft-vs-host disease (GVHD), and the most common toxicity was viral infection.
Parinda A. Mehta, MD, of Cincinnati Children’s Hospital Medical Center in Ohio, presented these results at this year’s BMT Tandem Meetings as abstract 109.*
“We all know that inherent chemotherapy and radiation sensitivity makes transplant for patients with Fanconi anemia quite challenging,” Dr Mehta began. “In our recently published, prospective, multi-institutional study, we showed excellent outcomes of alternative donor transplant in patients with Fanconi anemia without using radiation.”
“In that study,** TBI was replaced by pharmacokinetically adjusted busulfan. It proved that, yes, we can do alternative donor transplant successfully without radiation by showing an overall survival of 80% for a total of 45 patients. We were quite ecstatic to see these numbers.”
The study also showed that younger patients fared better with this regimen, and younger patients did best with the lowest dose of busulfan tested (0.6 mg/kg vs 0.8 to 1.0 mg/kg). In addition, patients who underwent HSCT for bone marrow failure had better outcomes than patients who had MDS.
This led Dr Mehta and her colleagues to hypothesize that adjusting busulfan dosing based on a patient’s age and disease status at HSCT could minimize toxicity and improve outcomes.
Patients
The researchers tested their theory in 22 FA patients. They had a median age of 7 (range, 4-27), and most (n=13) were female.
Twelve patients had pancytopenia, 6 had severe single-lineage cytopenia, 3 had low-grade MDS, and 1 patient had acute myeloid leukemia (AML).
Eighteen patients had a history of transfusions, and 3 had a history of androgen use.
Treatment
The preparative regimen consisted of 4 doses of busulfan (every 12 hours on day -7 to -6), followed by cyclophosphamide at 10 mg/kg/day (on day -5 to -2), fludarabine at 35 mg/m2/day (on day -5 to -2), and rabbit antithymocyte globulin at 2.5 mg/kg/day (on day -5 to -2).
Busulfan doses were adjusted according to age and disease status.
Children (age 18 and younger) with bone marrow failure received busulfan at 0.6 to 0.8 mg/kg. Children with MDS/AML received busulfan at 0.8 to 1.0 mg/kg. Adults (19 and older) received the lowest dose of busulfan—0.4 mg/kg—regardless of disease status.
“At the first sight, this will look counterintuitive . . . ,” Dr Mehta said. “However, based on our previous experience, in general and also from results of our previous study, this was specifically designed to avoid upfront TRM [transplant-related mortality] for these adult patients.”
All 22 patients received CD34-selected, T-cell-depleted peripheral blood stem cells from unrelated donors. Eleven patients received a fully matched graft (10/10), 8 patients had a 9/10 match, and 3 had an 8/10 match.
The median number of CD34+ cells/kg was 23.9 x 106 (range, 4.9-76.6), and the median number of CD3 cells/kg was 1 x 104 (range, 0.003-3.1).
T-cell depletion was the only GVHD prophylaxis used.
Patients with MDS/AML could receive azacitidine at day 42 after HSCT, an option intended to prevent relapse in these patients.
Toxicity
There were no cases of acute or chronic GVHD.
Toxicities included infections (n=24), oral mucositis (n=14), hyperbilirubinemia (n=2), pulmonary hemorrhage (n=1), and sinusoidal obstruction syndrome (n=1).
There were 20 viral infections, 4 bacterial infections, and no fungal infections. Viral infections included BK virus (n=7), cytomegalovirus (n=6), Epstein-Barr virus (n=6), and adenovirus (n=1).
Dr Mehta noted that viral infections are “not unexpected in a T-cell-depleted graft setting.”
“Because we know this complication [can occur], and we worry about our patients, one of the things that, in recent years, we have done is, we manufacture viral-specific CTLs [cytotoxic T lymphocytes] for all of these patients ahead of time whenever possible,” she said.
“To give you an example, 19 out of these 20 patients’ viral infections—or rather, viremias—are completely under control with the use of either antivirals or donor-specific CTLs, including a third-party CTL in one of the patients.”
Response and survival
All 22 patients engrafted. The median time to neutrophil engraftment was 9 days (range, 8-10), and the median time to platelet engraftment was 16 days (range, 11-40).
Twenty-one of the 22 patients (95%) were alive and disease-free at last follow-up. The median follow-up was 21 months (range, 6-44).
The single AML patient achieved remission but died of post-transplant lymphoproliferative disorder (PTLD) on day 202 after HSCT. Dr Mehta said this was due to partial loss of follow-up and noncompliance with medical recommendations during PTLD treatment.
The AML patient also had “significant upfront toxicity” but “recovered very nicely,” according to Dr Mehta. He had severe mucositis, herpetic stomatitis, and sinusoidal obstruction syndrome that responded to defibrotide.
“Overall, we are quite excited to see 95% overall survival for this cohort and conclude that the current risk-adjusted approach leads to excellent overall survival and disease-free survival in patients undergoing alternative donor transplant either for marrow failure or MDS/AML,” Dr Mehta said.
“Enrollment is ongoing, and we hope to see continued success in patients with MDS/AML as well as in adult patients.”
*Data in the abstract differ from the presentation.
**Mehta PA et al. Radiation-free, alternative donor HCT for Fanconi anemia patients: results from a prospective multi-institutional study. Blood 2017; doi: https://doi.org/10.1182/blood-2016-09-743112.
SALT LAKE CITY—A “risk-adjusted” approach leads to “excellent” survival in patients with Fanconi anemia (FA) undergoing alternative donor hematopoietic stem cell transplant (HSCT), according to a speaker at the 2018 BMT Tandem Meetings.
All FA patients who received personalized doses of busulfan in place of total body irradiation (TBI) were alive and disease-free after undergoing HSCT for bone marrow failure or myelodysplastic syndrome (MDS).
None of the patients developed graft-vs-host disease (GVHD), and the most common toxicity was viral infection.
Parinda A. Mehta, MD, of Cincinnati Children’s Hospital Medical Center in Ohio, presented these results at this year’s BMT Tandem Meetings as abstract 109.*
“We all know that inherent chemotherapy and radiation sensitivity makes transplant for patients with Fanconi anemia quite challenging,” Dr Mehta began. “In our recently published, prospective, multi-institutional study, we showed excellent outcomes of alternative donor transplant in patients with Fanconi anemia without using radiation.”
“In that study,** TBI was replaced by pharmacokinetically adjusted busulfan. It proved that, yes, we can do alternative donor transplant successfully without radiation by showing an overall survival of 80% for a total of 45 patients. We were quite ecstatic to see these numbers.”
The study also showed that younger patients fared better with this regimen, and younger patients did best with the lowest dose of busulfan tested (0.6 mg/kg vs 0.8 to 1.0 mg/kg). In addition, patients who underwent HSCT for bone marrow failure had better outcomes than patients who had MDS.
This led Dr Mehta and her colleagues to hypothesize that adjusting busulfan dosing based on a patient’s age and disease status at HSCT could minimize toxicity and improve outcomes.
Patients
The researchers tested their theory in 22 FA patients. They had a median age of 7 (range, 4-27), and most (n=13) were female.
Twelve patients had pancytopenia, 6 had severe single-lineage cytopenia, 3 had low-grade MDS, and 1 patient had acute myeloid leukemia (AML).
Eighteen patients had a history of transfusions, and 3 had a history of androgen use.
Treatment
The preparative regimen consisted of 4 doses of busulfan (every 12 hours on day -7 to -6), followed by cyclophosphamide at 10 mg/kg/day (on day -5 to -2), fludarabine at 35 mg/m2/day (on day -5 to -2), and rabbit antithymocyte globulin at 2.5 mg/kg/day (on day -5 to -2).
Busulfan doses were adjusted according to age and disease status.
Children (age 18 and younger) with bone marrow failure received busulfan at 0.6 to 0.8 mg/kg. Children with MDS/AML received busulfan at 0.8 to 1.0 mg/kg. Adults (19 and older) received the lowest dose of busulfan—0.4 mg/kg—regardless of disease status.
“At the first sight, this will look counterintuitive . . . ,” Dr Mehta said. “However, based on our previous experience, in general and also from results of our previous study, this was specifically designed to avoid upfront TRM [transplant-related mortality] for these adult patients.”
All 22 patients received CD34-selected, T-cell-depleted peripheral blood stem cells from unrelated donors. Eleven patients received a fully matched graft (10/10), 8 patients had a 9/10 match, and 3 had an 8/10 match.
The median number of CD34+ cells/kg was 23.9 x 106 (range, 4.9-76.6), and the median number of CD3 cells/kg was 1 x 104 (range, 0.003-3.1).
T-cell depletion was the only GVHD prophylaxis used.
Patients with MDS/AML could receive azacitidine at day 42 after HSCT, an option intended to prevent relapse in these patients.
Toxicity
There were no cases of acute or chronic GVHD.
Toxicities included infections (n=24), oral mucositis (n=14), hyperbilirubinemia (n=2), pulmonary hemorrhage (n=1), and sinusoidal obstruction syndrome (n=1).
There were 20 viral infections, 4 bacterial infections, and no fungal infections. Viral infections included BK virus (n=7), cytomegalovirus (n=6), Epstein-Barr virus (n=6), and adenovirus (n=1).
Dr Mehta noted that viral infections are “not unexpected in a T-cell-depleted graft setting.”
“Because we know this complication [can occur], and we worry about our patients, one of the things that, in recent years, we have done is, we manufacture viral-specific CTLs [cytotoxic T lymphocytes] for all of these patients ahead of time whenever possible,” she said.
“To give you an example, 19 out of these 20 patients’ viral infections—or rather, viremias—are completely under control with the use of either antivirals or donor-specific CTLs, including a third-party CTL in one of the patients.”
Response and survival
All 22 patients engrafted. The median time to neutrophil engraftment was 9 days (range, 8-10), and the median time to platelet engraftment was 16 days (range, 11-40).
Twenty-one of the 22 patients (95%) were alive and disease-free at last follow-up. The median follow-up was 21 months (range, 6-44).
The single AML patient achieved remission but died of post-transplant lymphoproliferative disorder (PTLD) on day 202 after HSCT. Dr Mehta said this was due to partial loss of follow-up and noncompliance with medical recommendations during PTLD treatment.
The AML patient also had “significant upfront toxicity” but “recovered very nicely,” according to Dr Mehta. He had severe mucositis, herpetic stomatitis, and sinusoidal obstruction syndrome that responded to defibrotide.
“Overall, we are quite excited to see 95% overall survival for this cohort and conclude that the current risk-adjusted approach leads to excellent overall survival and disease-free survival in patients undergoing alternative donor transplant either for marrow failure or MDS/AML,” Dr Mehta said.
“Enrollment is ongoing, and we hope to see continued success in patients with MDS/AML as well as in adult patients.”
*Data in the abstract differ from the presentation.
**Mehta PA et al. Radiation-free, alternative donor HCT for Fanconi anemia patients: results from a prospective multi-institutional study. Blood 2017; doi: https://doi.org/10.1182/blood-2016-09-743112.
SALT LAKE CITY—A “risk-adjusted” approach leads to “excellent” survival in patients with Fanconi anemia (FA) undergoing alternative donor hematopoietic stem cell transplant (HSCT), according to a speaker at the 2018 BMT Tandem Meetings.
All FA patients who received personalized doses of busulfan in place of total body irradiation (TBI) were alive and disease-free after undergoing HSCT for bone marrow failure or myelodysplastic syndrome (MDS).
None of the patients developed graft-vs-host disease (GVHD), and the most common toxicity was viral infection.
Parinda A. Mehta, MD, of Cincinnati Children’s Hospital Medical Center in Ohio, presented these results at this year’s BMT Tandem Meetings as abstract 109.*
“We all know that inherent chemotherapy and radiation sensitivity makes transplant for patients with Fanconi anemia quite challenging,” Dr Mehta began. “In our recently published, prospective, multi-institutional study, we showed excellent outcomes of alternative donor transplant in patients with Fanconi anemia without using radiation.”
“In that study,** TBI was replaced by pharmacokinetically adjusted busulfan. It proved that, yes, we can do alternative donor transplant successfully without radiation by showing an overall survival of 80% for a total of 45 patients. We were quite ecstatic to see these numbers.”
The study also showed that younger patients fared better with this regimen, and younger patients did best with the lowest dose of busulfan tested (0.6 mg/kg vs 0.8 to 1.0 mg/kg). In addition, patients who underwent HSCT for bone marrow failure had better outcomes than patients who had MDS.
This led Dr Mehta and her colleagues to hypothesize that adjusting busulfan dosing based on a patient’s age and disease status at HSCT could minimize toxicity and improve outcomes.
Patients
The researchers tested their theory in 22 FA patients. They had a median age of 7 (range, 4-27), and most (n=13) were female.
Twelve patients had pancytopenia, 6 had severe single-lineage cytopenia, 3 had low-grade MDS, and 1 patient had acute myeloid leukemia (AML).
Eighteen patients had a history of transfusions, and 3 had a history of androgen use.
Treatment
The preparative regimen consisted of 4 doses of busulfan (every 12 hours on day -7 to -6), followed by cyclophosphamide at 10 mg/kg/day (on day -5 to -2), fludarabine at 35 mg/m2/day (on day -5 to -2), and rabbit antithymocyte globulin at 2.5 mg/kg/day (on day -5 to -2).
Busulfan doses were adjusted according to age and disease status.
Children (age 18 and younger) with bone marrow failure received busulfan at 0.6 to 0.8 mg/kg. Children with MDS/AML received busulfan at 0.8 to 1.0 mg/kg. Adults (19 and older) received the lowest dose of busulfan—0.4 mg/kg—regardless of disease status.
“At the first sight, this will look counterintuitive . . . ,” Dr Mehta said. “However, based on our previous experience, in general and also from results of our previous study, this was specifically designed to avoid upfront TRM [transplant-related mortality] for these adult patients.”
All 22 patients received CD34-selected, T-cell-depleted peripheral blood stem cells from unrelated donors. Eleven patients received a fully matched graft (10/10), 8 patients had a 9/10 match, and 3 had an 8/10 match.
The median number of CD34+ cells/kg was 23.9 x 106 (range, 4.9-76.6), and the median number of CD3 cells/kg was 1 x 104 (range, 0.003-3.1).
T-cell depletion was the only GVHD prophylaxis used.
Patients with MDS/AML could receive azacitidine at day 42 after HSCT, an option intended to prevent relapse in these patients.
Toxicity
There were no cases of acute or chronic GVHD.
Toxicities included infections (n=24), oral mucositis (n=14), hyperbilirubinemia (n=2), pulmonary hemorrhage (n=1), and sinusoidal obstruction syndrome (n=1).
There were 20 viral infections, 4 bacterial infections, and no fungal infections. Viral infections included BK virus (n=7), cytomegalovirus (n=6), Epstein-Barr virus (n=6), and adenovirus (n=1).
Dr Mehta noted that viral infections are “not unexpected in a T-cell-depleted graft setting.”
“Because we know this complication [can occur], and we worry about our patients, one of the things that, in recent years, we have done is, we manufacture viral-specific CTLs [cytotoxic T lymphocytes] for all of these patients ahead of time whenever possible,” she said.
“To give you an example, 19 out of these 20 patients’ viral infections—or rather, viremias—are completely under control with the use of either antivirals or donor-specific CTLs, including a third-party CTL in one of the patients.”
Response and survival
All 22 patients engrafted. The median time to neutrophil engraftment was 9 days (range, 8-10), and the median time to platelet engraftment was 16 days (range, 11-40).
Twenty-one of the 22 patients (95%) were alive and disease-free at last follow-up. The median follow-up was 21 months (range, 6-44).
The single AML patient achieved remission but died of post-transplant lymphoproliferative disorder (PTLD) on day 202 after HSCT. Dr Mehta said this was due to partial loss of follow-up and noncompliance with medical recommendations during PTLD treatment.
The AML patient also had “significant upfront toxicity” but “recovered very nicely,” according to Dr Mehta. He had severe mucositis, herpetic stomatitis, and sinusoidal obstruction syndrome that responded to defibrotide.
“Overall, we are quite excited to see 95% overall survival for this cohort and conclude that the current risk-adjusted approach leads to excellent overall survival and disease-free survival in patients undergoing alternative donor transplant either for marrow failure or MDS/AML,” Dr Mehta said.
“Enrollment is ongoing, and we hope to see continued success in patients with MDS/AML as well as in adult patients.”
*Data in the abstract differ from the presentation.
**Mehta PA et al. Radiation-free, alternative donor HCT for Fanconi anemia patients: results from a prospective multi-institutional study. Blood 2017; doi: https://doi.org/10.1182/blood-2016-09-743112.
Study confirms higher risk of infection with CB transplant
SALT LAKE CITY—Results of a large, retrospective analysis support the notion that patients who receive cord blood (CB) transplants have a higher risk of infection than other hematopoietic stem cell transplant (HSCT) recipients.
Investigators found that CB recipients had a significantly higher risk of bacterial, viral, and fungal infections in the early post-transplant period than patients who received peripheral blood (PB) or bone marrow (BM) transplants.
In addition, CB recipients had longer hospital stays, higher inpatient costs, and greater inpatient mortality than PB and BM recipients.
Amandeep Godara, MD, of Tufts Medical Center in Boston, Massachusetts, presented these results at the 2018 BMT Tandem Meetings (abstract 30*).
“Infections are considered more common in cord blood transplant recipients based on some prior retrospective analyses,” Dr Godara noted. “But there is limited data comparing these infectious complications between cord blood transplant and peripheral blood/bone marrow stem cell transplants during the inpatient stay for the stem cell transplant.”
With this in mind, Dr Godara and his colleagues analyzed data from the Healthcare Cost and Utilization Project National Inpatient Sample. This database covers 46 US states and contains data from more than 7 million hospital stays each year.
The investigators searched the database for hospital admissions for HSCT from 2002 to 2014. They identified 2979 CB transplants and 56,845 PB or BM transplants.
The CB recipients had a median age of 48, and 55% were male. Fifty-nine percent were white, 18% Hispanic, 13% black, 5% Asian, and 5% “other.” Sixty-six percent of patients had acute leukemia, 18% non-Hodgkin lymphoma, 5% Hodgkin lymphoma, and 11% “other” diseases.
The PB/BM recipients had a median age of 45, and 58% were male. Seventy-nine percent were white, 8% Hispanic, 6% black, 3% Asian, and 4% “other.” Sixty-one percent of patients had acute leukemia, 16% non-Hodgkin lymphoma, 4% Hodgkin lymphoma, and 19% “other” diseases.
Results
Dr Godara and his colleagues compared the rates and types of infection from the time of HSCT to hospital discharge in CB and PB/BM recipients. The team also compared early inpatient mortality, the cost of hospitalization, and the length of hospital stay.
“[W]e observed a higher risk for infections in cord blood transplant patients compared to peripheral blood and bone marrow stem cell transplant patients, and this risk for infection extended through a wide spectrum of pathogens,” Dr Godara said.
“We also observed a higher all-cause inpatient mortality in cord blood transplant compared to peripheral blood and bone marrow transplant, especially in patients who had bacterial sepsis or invasive fungal infection.”
The rate of bacterial sepsis was 34.87% in CB recipients and 20.20% in PB/BM recipients (P<0.0001). Rates of viral infection were 20.05% and 8.19%, respectively (P<0.0001). And rates of invasive fungal infection were 12.87% and 7.89% (P<0.0001).
There was a similar distribution of bacterial infections in CB and PB/BM recipients. The most common was pneumonia (47% and 41%, respectively), followed by abdominal infections (29% and 31%, respectively), urinary tract infections (17% and 21%, respectively), central line-associated bloodstream infections (4% and 6%, respectively), and acute sinusitis (3% and 1%, respectively).
The rate of Clostridium difficile infection was significantly higher in CB recipients than PB/BM recipients—11.75% and 8.90%, respectively (P=0.02). However, there was no significant difference in mortality related to C. difficile—14% and 10%, respectively (P=0.3).
On the other hand, all-cause inpatient mortality was significantly higher in CB recipients than PB/BM recipients—16% and 7%, respectively (P<0.0001).
Inpatient mortality rates were significantly higher for CB recipients with bacterial sepsis (33% vs 23%, P=0.001) and invasive fungal infections (29% vs 16%, P=0.0045) but not viral infections (19% vs 17%, P=0.5).
The median length of hospital stay was 36 days for CB recipients and 25 days for PB/BM recipients. The mean inpatient charges were $448,892 and $250,437 respectively.
*Data in the abstract differ from the presentation.
SALT LAKE CITY—Results of a large, retrospective analysis support the notion that patients who receive cord blood (CB) transplants have a higher risk of infection than other hematopoietic stem cell transplant (HSCT) recipients.
Investigators found that CB recipients had a significantly higher risk of bacterial, viral, and fungal infections in the early post-transplant period than patients who received peripheral blood (PB) or bone marrow (BM) transplants.
In addition, CB recipients had longer hospital stays, higher inpatient costs, and greater inpatient mortality than PB and BM recipients.
Amandeep Godara, MD, of Tufts Medical Center in Boston, Massachusetts, presented these results at the 2018 BMT Tandem Meetings (abstract 30*).
“Infections are considered more common in cord blood transplant recipients based on some prior retrospective analyses,” Dr Godara noted. “But there is limited data comparing these infectious complications between cord blood transplant and peripheral blood/bone marrow stem cell transplants during the inpatient stay for the stem cell transplant.”
With this in mind, Dr Godara and his colleagues analyzed data from the Healthcare Cost and Utilization Project National Inpatient Sample. This database covers 46 US states and contains data from more than 7 million hospital stays each year.
The investigators searched the database for hospital admissions for HSCT from 2002 to 2014. They identified 2979 CB transplants and 56,845 PB or BM transplants.
The CB recipients had a median age of 48, and 55% were male. Fifty-nine percent were white, 18% Hispanic, 13% black, 5% Asian, and 5% “other.” Sixty-six percent of patients had acute leukemia, 18% non-Hodgkin lymphoma, 5% Hodgkin lymphoma, and 11% “other” diseases.
The PB/BM recipients had a median age of 45, and 58% were male. Seventy-nine percent were white, 8% Hispanic, 6% black, 3% Asian, and 4% “other.” Sixty-one percent of patients had acute leukemia, 16% non-Hodgkin lymphoma, 4% Hodgkin lymphoma, and 19% “other” diseases.
Results
Dr Godara and his colleagues compared the rates and types of infection from the time of HSCT to hospital discharge in CB and PB/BM recipients. The team also compared early inpatient mortality, the cost of hospitalization, and the length of hospital stay.
“[W]e observed a higher risk for infections in cord blood transplant patients compared to peripheral blood and bone marrow stem cell transplant patients, and this risk for infection extended through a wide spectrum of pathogens,” Dr Godara said.
“We also observed a higher all-cause inpatient mortality in cord blood transplant compared to peripheral blood and bone marrow transplant, especially in patients who had bacterial sepsis or invasive fungal infection.”
The rate of bacterial sepsis was 34.87% in CB recipients and 20.20% in PB/BM recipients (P<0.0001). Rates of viral infection were 20.05% and 8.19%, respectively (P<0.0001). And rates of invasive fungal infection were 12.87% and 7.89% (P<0.0001).
There was a similar distribution of bacterial infections in CB and PB/BM recipients. The most common was pneumonia (47% and 41%, respectively), followed by abdominal infections (29% and 31%, respectively), urinary tract infections (17% and 21%, respectively), central line-associated bloodstream infections (4% and 6%, respectively), and acute sinusitis (3% and 1%, respectively).
The rate of Clostridium difficile infection was significantly higher in CB recipients than PB/BM recipients—11.75% and 8.90%, respectively (P=0.02). However, there was no significant difference in mortality related to C. difficile—14% and 10%, respectively (P=0.3).
On the other hand, all-cause inpatient mortality was significantly higher in CB recipients than PB/BM recipients—16% and 7%, respectively (P<0.0001).
Inpatient mortality rates were significantly higher for CB recipients with bacterial sepsis (33% vs 23%, P=0.001) and invasive fungal infections (29% vs 16%, P=0.0045) but not viral infections (19% vs 17%, P=0.5).
The median length of hospital stay was 36 days for CB recipients and 25 days for PB/BM recipients. The mean inpatient charges were $448,892 and $250,437 respectively.
*Data in the abstract differ from the presentation.
SALT LAKE CITY—Results of a large, retrospective analysis support the notion that patients who receive cord blood (CB) transplants have a higher risk of infection than other hematopoietic stem cell transplant (HSCT) recipients.
Investigators found that CB recipients had a significantly higher risk of bacterial, viral, and fungal infections in the early post-transplant period than patients who received peripheral blood (PB) or bone marrow (BM) transplants.
In addition, CB recipients had longer hospital stays, higher inpatient costs, and greater inpatient mortality than PB and BM recipients.
Amandeep Godara, MD, of Tufts Medical Center in Boston, Massachusetts, presented these results at the 2018 BMT Tandem Meetings (abstract 30*).
“Infections are considered more common in cord blood transplant recipients based on some prior retrospective analyses,” Dr Godara noted. “But there is limited data comparing these infectious complications between cord blood transplant and peripheral blood/bone marrow stem cell transplants during the inpatient stay for the stem cell transplant.”
With this in mind, Dr Godara and his colleagues analyzed data from the Healthcare Cost and Utilization Project National Inpatient Sample. This database covers 46 US states and contains data from more than 7 million hospital stays each year.
The investigators searched the database for hospital admissions for HSCT from 2002 to 2014. They identified 2979 CB transplants and 56,845 PB or BM transplants.
The CB recipients had a median age of 48, and 55% were male. Fifty-nine percent were white, 18% Hispanic, 13% black, 5% Asian, and 5% “other.” Sixty-six percent of patients had acute leukemia, 18% non-Hodgkin lymphoma, 5% Hodgkin lymphoma, and 11% “other” diseases.
The PB/BM recipients had a median age of 45, and 58% were male. Seventy-nine percent were white, 8% Hispanic, 6% black, 3% Asian, and 4% “other.” Sixty-one percent of patients had acute leukemia, 16% non-Hodgkin lymphoma, 4% Hodgkin lymphoma, and 19% “other” diseases.
Results
Dr Godara and his colleagues compared the rates and types of infection from the time of HSCT to hospital discharge in CB and PB/BM recipients. The team also compared early inpatient mortality, the cost of hospitalization, and the length of hospital stay.
“[W]e observed a higher risk for infections in cord blood transplant patients compared to peripheral blood and bone marrow stem cell transplant patients, and this risk for infection extended through a wide spectrum of pathogens,” Dr Godara said.
“We also observed a higher all-cause inpatient mortality in cord blood transplant compared to peripheral blood and bone marrow transplant, especially in patients who had bacterial sepsis or invasive fungal infection.”
The rate of bacterial sepsis was 34.87% in CB recipients and 20.20% in PB/BM recipients (P<0.0001). Rates of viral infection were 20.05% and 8.19%, respectively (P<0.0001). And rates of invasive fungal infection were 12.87% and 7.89% (P<0.0001).
There was a similar distribution of bacterial infections in CB and PB/BM recipients. The most common was pneumonia (47% and 41%, respectively), followed by abdominal infections (29% and 31%, respectively), urinary tract infections (17% and 21%, respectively), central line-associated bloodstream infections (4% and 6%, respectively), and acute sinusitis (3% and 1%, respectively).
The rate of Clostridium difficile infection was significantly higher in CB recipients than PB/BM recipients—11.75% and 8.90%, respectively (P=0.02). However, there was no significant difference in mortality related to C. difficile—14% and 10%, respectively (P=0.3).
On the other hand, all-cause inpatient mortality was significantly higher in CB recipients than PB/BM recipients—16% and 7%, respectively (P<0.0001).
Inpatient mortality rates were significantly higher for CB recipients with bacterial sepsis (33% vs 23%, P=0.001) and invasive fungal infections (29% vs 16%, P=0.0045) but not viral infections (19% vs 17%, P=0.5).
The median length of hospital stay was 36 days for CB recipients and 25 days for PB/BM recipients. The mean inpatient charges were $448,892 and $250,437 respectively.
*Data in the abstract differ from the presentation.
Team identifies biomarkers for cGVHD in kids
SALT LAKE CITY—Researchers say they have identified prognostic biomarkers for chronic graft-vs-host disease (cGVHD) in children.
The group found that recent thymic emigrants (RTEs) and regulatory T cells expressing CD31 and CD45RA (Treg RTEs) were significantly lower at day 100 after transplant in patients who developed cGVHD.
Because prior research indicated that RTEs are higher in adults with cGVHD, the researchers concluded that thymic function may play a bigger role in cGVHD development for children than for adults.
Geoff D.E. Cuvelier, MD, of CancerCare Manitoba in Winnipeg, Canada, presented these findings at the 2018 BMT Tandem Meetings (abstract 104).
“Our group became interested in these populations of recent thymic emigrants when 2 adult studies1,2 . . . showed that higher proportions of recent thymic emigrants at day 100 were prognostic for the development of chronic graft-vs-host disease,” Dr Cuvelier said.
This led his group to evaluate whether RTEs (CD4+CD45RA+CD31+ T cells), as well as Treg RTEs—Tregs (CD4+CD25+CD127Low) that co-express naïve and recently emigrated markers (CD45RA+CD31+)—are prognostic for pediatric cGVHD at day 100 after allogeneic hematopoietic stem cell transplant (allo-HSCT).
The researchers’ study enrolled patients younger than 18 years of age who underwent allo-HSCT to treat malignant and non-malignant diseases. There were 144 patients who had 1 year of follow-up after allo-HSCT.
Thirty-seven of the patients (25.7%) had cGVHD, and 34 (23.6%) had late acute GVHD (post-day 100). The remaining 73 patients (50.7%) had neither cGVHD nor late acute GVHD, so they served as controls.
Twenty cases of cGVHD were severe, 12 were moderate, and 5 were mild. cGVHD was initially diagnosed at a mean of 192 days post-transplant. The median number of organ systems involved was 3 (range, 1-6). Seventeen patients (46%) had overlap syndrome.
The researchers found that RTEs as a percentage of CD4 T cells were significantly lower at day 100 in patients with cGVHD than in controls—7.8% and 13.5%, respectively (P=0.007). The difference between controls and patients with late acute GVHD was not significant—13.5% and 9.4%, respectively (P=0.08).
Treg RTEs as a percentage of all Tregs were also significantly lower at day 100 in patients with cGVHD than in controls—6.4% and 13.2%, respectively (P=0.002). Again, the difference between controls and patients with late acute GVHD was not significant—13.2% and 9.1%, respectively (P=0.06).
However, further analysis revealed that percentages of RTEs and Treg RTEs were significantly lower at day 100 in patients who developed any type of GVHD after day 100.
The percentage of RTEs was 13.5% in controls and 8.5% in patients with any GVHD after day 100 (P=0.009). The percentage of Treg RTEs was 13.2% and 7.6%, respectively (P=0.004).
“Both recent thymic emigrants and Treg RTEs at day 100 are prognostic biomarkers for chronic graft-vs-host disease in children in this large, multi-institutional, prospective trial,” Dr Cuvelier said in closing.
“Unlike adults, in children, RTEs are proportionally lower, not higher, in patients that later develop chronic GVHD compared to no chronic GVHD. This may suggest that thymic dysfunction and thymic output may play a greater role in chronic GVHD development in children compared to adults.”
To expand upon this research, Dr Cuvelier and his colleagues are planning to begin model building using prognostic cellular and plasma biomarkers at day 100 to determine high-risk profiles for cGVHD.
1. Greinix HT et al; CD19+CD21low B Cells and CD4+CD45RA+CD31+ T Cells Correlate with First Diagnosis of Chronic Graft-versus-Host Disease. BBMT 2015; 21(2):250-258.
2. Li AM et al. An Early Naïve T Cell Population Lacking PD1 Expression at Day 100 As A Prognostic Biomarker of Chronic GVHD. TSS 2017; 210.6.
SALT LAKE CITY—Researchers say they have identified prognostic biomarkers for chronic graft-vs-host disease (cGVHD) in children.
The group found that recent thymic emigrants (RTEs) and regulatory T cells expressing CD31 and CD45RA (Treg RTEs) were significantly lower at day 100 after transplant in patients who developed cGVHD.
Because prior research indicated that RTEs are higher in adults with cGVHD, the researchers concluded that thymic function may play a bigger role in cGVHD development for children than for adults.
Geoff D.E. Cuvelier, MD, of CancerCare Manitoba in Winnipeg, Canada, presented these findings at the 2018 BMT Tandem Meetings (abstract 104).
“Our group became interested in these populations of recent thymic emigrants when 2 adult studies1,2 . . . showed that higher proportions of recent thymic emigrants at day 100 were prognostic for the development of chronic graft-vs-host disease,” Dr Cuvelier said.
This led his group to evaluate whether RTEs (CD4+CD45RA+CD31+ T cells), as well as Treg RTEs—Tregs (CD4+CD25+CD127Low) that co-express naïve and recently emigrated markers (CD45RA+CD31+)—are prognostic for pediatric cGVHD at day 100 after allogeneic hematopoietic stem cell transplant (allo-HSCT).
The researchers’ study enrolled patients younger than 18 years of age who underwent allo-HSCT to treat malignant and non-malignant diseases. There were 144 patients who had 1 year of follow-up after allo-HSCT.
Thirty-seven of the patients (25.7%) had cGVHD, and 34 (23.6%) had late acute GVHD (post-day 100). The remaining 73 patients (50.7%) had neither cGVHD nor late acute GVHD, so they served as controls.
Twenty cases of cGVHD were severe, 12 were moderate, and 5 were mild. cGVHD was initially diagnosed at a mean of 192 days post-transplant. The median number of organ systems involved was 3 (range, 1-6). Seventeen patients (46%) had overlap syndrome.
The researchers found that RTEs as a percentage of CD4 T cells were significantly lower at day 100 in patients with cGVHD than in controls—7.8% and 13.5%, respectively (P=0.007). The difference between controls and patients with late acute GVHD was not significant—13.5% and 9.4%, respectively (P=0.08).
Treg RTEs as a percentage of all Tregs were also significantly lower at day 100 in patients with cGVHD than in controls—6.4% and 13.2%, respectively (P=0.002). Again, the difference between controls and patients with late acute GVHD was not significant—13.2% and 9.1%, respectively (P=0.06).
However, further analysis revealed that percentages of RTEs and Treg RTEs were significantly lower at day 100 in patients who developed any type of GVHD after day 100.
The percentage of RTEs was 13.5% in controls and 8.5% in patients with any GVHD after day 100 (P=0.009). The percentage of Treg RTEs was 13.2% and 7.6%, respectively (P=0.004).
“Both recent thymic emigrants and Treg RTEs at day 100 are prognostic biomarkers for chronic graft-vs-host disease in children in this large, multi-institutional, prospective trial,” Dr Cuvelier said in closing.
“Unlike adults, in children, RTEs are proportionally lower, not higher, in patients that later develop chronic GVHD compared to no chronic GVHD. This may suggest that thymic dysfunction and thymic output may play a greater role in chronic GVHD development in children compared to adults.”
To expand upon this research, Dr Cuvelier and his colleagues are planning to begin model building using prognostic cellular and plasma biomarkers at day 100 to determine high-risk profiles for cGVHD.
1. Greinix HT et al; CD19+CD21low B Cells and CD4+CD45RA+CD31+ T Cells Correlate with First Diagnosis of Chronic Graft-versus-Host Disease. BBMT 2015; 21(2):250-258.
2. Li AM et al. An Early Naïve T Cell Population Lacking PD1 Expression at Day 100 As A Prognostic Biomarker of Chronic GVHD. TSS 2017; 210.6.
SALT LAKE CITY—Researchers say they have identified prognostic biomarkers for chronic graft-vs-host disease (cGVHD) in children.
The group found that recent thymic emigrants (RTEs) and regulatory T cells expressing CD31 and CD45RA (Treg RTEs) were significantly lower at day 100 after transplant in patients who developed cGVHD.
Because prior research indicated that RTEs are higher in adults with cGVHD, the researchers concluded that thymic function may play a bigger role in cGVHD development for children than for adults.
Geoff D.E. Cuvelier, MD, of CancerCare Manitoba in Winnipeg, Canada, presented these findings at the 2018 BMT Tandem Meetings (abstract 104).
“Our group became interested in these populations of recent thymic emigrants when 2 adult studies1,2 . . . showed that higher proportions of recent thymic emigrants at day 100 were prognostic for the development of chronic graft-vs-host disease,” Dr Cuvelier said.
This led his group to evaluate whether RTEs (CD4+CD45RA+CD31+ T cells), as well as Treg RTEs—Tregs (CD4+CD25+CD127Low) that co-express naïve and recently emigrated markers (CD45RA+CD31+)—are prognostic for pediatric cGVHD at day 100 after allogeneic hematopoietic stem cell transplant (allo-HSCT).
The researchers’ study enrolled patients younger than 18 years of age who underwent allo-HSCT to treat malignant and non-malignant diseases. There were 144 patients who had 1 year of follow-up after allo-HSCT.
Thirty-seven of the patients (25.7%) had cGVHD, and 34 (23.6%) had late acute GVHD (post-day 100). The remaining 73 patients (50.7%) had neither cGVHD nor late acute GVHD, so they served as controls.
Twenty cases of cGVHD were severe, 12 were moderate, and 5 were mild. cGVHD was initially diagnosed at a mean of 192 days post-transplant. The median number of organ systems involved was 3 (range, 1-6). Seventeen patients (46%) had overlap syndrome.
The researchers found that RTEs as a percentage of CD4 T cells were significantly lower at day 100 in patients with cGVHD than in controls—7.8% and 13.5%, respectively (P=0.007). The difference between controls and patients with late acute GVHD was not significant—13.5% and 9.4%, respectively (P=0.08).
Treg RTEs as a percentage of all Tregs were also significantly lower at day 100 in patients with cGVHD than in controls—6.4% and 13.2%, respectively (P=0.002). Again, the difference between controls and patients with late acute GVHD was not significant—13.2% and 9.1%, respectively (P=0.06).
However, further analysis revealed that percentages of RTEs and Treg RTEs were significantly lower at day 100 in patients who developed any type of GVHD after day 100.
The percentage of RTEs was 13.5% in controls and 8.5% in patients with any GVHD after day 100 (P=0.009). The percentage of Treg RTEs was 13.2% and 7.6%, respectively (P=0.004).
“Both recent thymic emigrants and Treg RTEs at day 100 are prognostic biomarkers for chronic graft-vs-host disease in children in this large, multi-institutional, prospective trial,” Dr Cuvelier said in closing.
“Unlike adults, in children, RTEs are proportionally lower, not higher, in patients that later develop chronic GVHD compared to no chronic GVHD. This may suggest that thymic dysfunction and thymic output may play a greater role in chronic GVHD development in children compared to adults.”
To expand upon this research, Dr Cuvelier and his colleagues are planning to begin model building using prognostic cellular and plasma biomarkers at day 100 to determine high-risk profiles for cGVHD.
1. Greinix HT et al; CD19+CD21low B Cells and CD4+CD45RA+CD31+ T Cells Correlate with First Diagnosis of Chronic Graft-versus-Host Disease. BBMT 2015; 21(2):250-258.
2. Li AM et al. An Early Naïve T Cell Population Lacking PD1 Expression at Day 100 As A Prognostic Biomarker of Chronic GVHD. TSS 2017; 210.6.
Expanded UCB product can stand alone
SALT LAKE CITY—The expanded umbilical cord blood (UCB) product NiCord can be used as a stand-alone graft, according to research presented at the 2018 BMT Tandem Meetings.
Researchers found that a single NiCord unit provided “robust” engraftment in a phase 1/2 study of patients with high-risk hematologic malignancies.
NiCord recipients had quicker neutrophil and platelet engraftment than matched control subjects who received standard myeloablative UCB transplant (single or double).
Mitchell Horwitz, MD, of the Duke University Medical Center in Durham, North Carolina, presented these results at the meeting as abstract 49.* The research was sponsored by Gamida Cell, the company developing NiCord.
“[NiCord] is an ex vivo expanded cell product that’s derived from an entire unit of umbilical cord blood,” Dr Horwitz explained. “It’s manufactured starting with a CD133-positive selection, which is the progenitor cell population that’s cultured, and a T-cell containing CD133-negative fraction that is provided also at the time of transplant.”
“The culture system contains nicotinamide—that’s the active ingredient in the culture. And that’s supplemented with cytokines—thrombopoietin, IL-6, FLT-3 ligand, and stem cell factor. The culture is 21 days.”
Previous research showed that double UCB transplant including a NiCord unit could provide benefits over standard double UCB transplant. This led Dr Horwitz and his colleagues to wonder if NiCord could be used as a stand-alone graft.
So the team evaluated the safety and efficacy of NiCord alone in 36 adolescents/adults with high-risk hematologic malignancies.
Patients had acute myelogenous leukemia (n=17), acute lymphoblastic leukemia (n=9), myelodysplastic syndrome (n=7), chronic myelogenous leukemia (n=2), and Hodgkin lymphoma (n=1).
Most patients had intermediate (n=15) or high-risk (n=13) disease. They had a median age of 44 (range, 13-63) and a median weight of 75 kg (range, 41-125).
Treatment
For conditioning, 19 patients received thiotepa, busulfan, and fludarabine. Fifteen patients received total body irradiation and fludarabine with or without cyclophosphamide or thiotepa. And 2 patients received clofarabine, fludarabine, and busulfan.
Most patients had a 4/6 human leukocyte antigen (HLA) match (n=26), 8 had a 5/6 HLA match, and 2 had a 6/6 HLA match.
The median total nucleated cell dose was 2.4 x 107/kg prior to expansion of the UCB unit and 3.7 x 107/kg after expansion. The median CD34+ cell dose was 0.2 x 106/kg and 6.3 x 106/kg, respectively.
“CD34 cells were expanded 33-fold in the 3-week culture system,” Dr Horwitz noted. “That translated to a median CD34 dose of 6.3 x 106/kg, a dose comparable to what would be obtained from an adult donor graft.”
Engraftment
There was 1 case of primary graft failure and 2 cases of secondary graft failure. One case of secondary graft failure was associated with an HHV-6 infection, and the other was due to a lethal adenovirus infection.
Of those patients who engrafted, 97% achieved full donor chimerism, and 3% had mixed chimerism.
Dr Horwitz and his colleagues compared engraftment results in the NiCord recipients to results in a cohort of patients from the CIBMTR registry who underwent UCB transplants from 2010 to 2013. They had similar characteristics as the NiCord patients—age, conditioning regimen, disease status, etc.
In total, there were 148 CIBMTR registry patients, 20% of whom received a single UCB unit.
The median time to neutrophil engraftment was 11.5 days (range, 6-26) with NiCord and 21 days in the CIBMTR matched control cohort (P<0.001). The cumulative incidence of neutrophil engraftment was 94.4% and 89.7%, respectively.
The median time to platelet engraftment was 34 days (range, 25-96) with NiCord and 46 days in the CIBMTR controls (P<0.001). The cumulative incidence of platelet engraftment was 80.6% and 67.1%, respectively.
“There’s a median 10-day reduction in neutrophil recovery [and] 12-day reduction in time to platelet recovery [with NiCord],” Dr Horwitz noted. “There is evidence of robust and durable engraftment with a NiCord unit, with one patient now over 7 years from his first transplant on the pilot trial.”
Relapse, survival, and GVHD
Dr Horwitz reported other outcomes in the NiCord recipients without making comparisons to the CIBMTR matched controls.
The estimated 2-year rate of non-relapse mortality in NiCord recipients was 23.8%, and the estimated 2-year incidence of relapse was 33.2%.
The estimated disease-free survival was 49.1% at 1 year and 43.0% at 2 years. The estimated overall survival was 51.2% at 1 year and 2 years.
At 100 days, the rate of grade 2-4 acute GVHD was 44.0%, and the rate of grade 3-4 acute GVHD was 11.1%.
The estimated 1-year rate of mild to severe chronic GVHD was 40.5%, and the estimated 2-year rate of moderate to severe chronic GVHD was 9.8%.
Dr Horwitz said these “promising results” have led to the launch of a phase 3 registration trial in which researchers are comparing NiCord to standard single or double UCB transplant. The trial is open for accrual.
*Information in the abstract differs from the presentation.
SALT LAKE CITY—The expanded umbilical cord blood (UCB) product NiCord can be used as a stand-alone graft, according to research presented at the 2018 BMT Tandem Meetings.
Researchers found that a single NiCord unit provided “robust” engraftment in a phase 1/2 study of patients with high-risk hematologic malignancies.
NiCord recipients had quicker neutrophil and platelet engraftment than matched control subjects who received standard myeloablative UCB transplant (single or double).
Mitchell Horwitz, MD, of the Duke University Medical Center in Durham, North Carolina, presented these results at the meeting as abstract 49.* The research was sponsored by Gamida Cell, the company developing NiCord.
“[NiCord] is an ex vivo expanded cell product that’s derived from an entire unit of umbilical cord blood,” Dr Horwitz explained. “It’s manufactured starting with a CD133-positive selection, which is the progenitor cell population that’s cultured, and a T-cell containing CD133-negative fraction that is provided also at the time of transplant.”
“The culture system contains nicotinamide—that’s the active ingredient in the culture. And that’s supplemented with cytokines—thrombopoietin, IL-6, FLT-3 ligand, and stem cell factor. The culture is 21 days.”
Previous research showed that double UCB transplant including a NiCord unit could provide benefits over standard double UCB transplant. This led Dr Horwitz and his colleagues to wonder if NiCord could be used as a stand-alone graft.
So the team evaluated the safety and efficacy of NiCord alone in 36 adolescents/adults with high-risk hematologic malignancies.
Patients had acute myelogenous leukemia (n=17), acute lymphoblastic leukemia (n=9), myelodysplastic syndrome (n=7), chronic myelogenous leukemia (n=2), and Hodgkin lymphoma (n=1).
Most patients had intermediate (n=15) or high-risk (n=13) disease. They had a median age of 44 (range, 13-63) and a median weight of 75 kg (range, 41-125).
Treatment
For conditioning, 19 patients received thiotepa, busulfan, and fludarabine. Fifteen patients received total body irradiation and fludarabine with or without cyclophosphamide or thiotepa. And 2 patients received clofarabine, fludarabine, and busulfan.
Most patients had a 4/6 human leukocyte antigen (HLA) match (n=26), 8 had a 5/6 HLA match, and 2 had a 6/6 HLA match.
The median total nucleated cell dose was 2.4 x 107/kg prior to expansion of the UCB unit and 3.7 x 107/kg after expansion. The median CD34+ cell dose was 0.2 x 106/kg and 6.3 x 106/kg, respectively.
“CD34 cells were expanded 33-fold in the 3-week culture system,” Dr Horwitz noted. “That translated to a median CD34 dose of 6.3 x 106/kg, a dose comparable to what would be obtained from an adult donor graft.”
Engraftment
There was 1 case of primary graft failure and 2 cases of secondary graft failure. One case of secondary graft failure was associated with an HHV-6 infection, and the other was due to a lethal adenovirus infection.
Of those patients who engrafted, 97% achieved full donor chimerism, and 3% had mixed chimerism.
Dr Horwitz and his colleagues compared engraftment results in the NiCord recipients to results in a cohort of patients from the CIBMTR registry who underwent UCB transplants from 2010 to 2013. They had similar characteristics as the NiCord patients—age, conditioning regimen, disease status, etc.
In total, there were 148 CIBMTR registry patients, 20% of whom received a single UCB unit.
The median time to neutrophil engraftment was 11.5 days (range, 6-26) with NiCord and 21 days in the CIBMTR matched control cohort (P<0.001). The cumulative incidence of neutrophil engraftment was 94.4% and 89.7%, respectively.
The median time to platelet engraftment was 34 days (range, 25-96) with NiCord and 46 days in the CIBMTR controls (P<0.001). The cumulative incidence of platelet engraftment was 80.6% and 67.1%, respectively.
“There’s a median 10-day reduction in neutrophil recovery [and] 12-day reduction in time to platelet recovery [with NiCord],” Dr Horwitz noted. “There is evidence of robust and durable engraftment with a NiCord unit, with one patient now over 7 years from his first transplant on the pilot trial.”
Relapse, survival, and GVHD
Dr Horwitz reported other outcomes in the NiCord recipients without making comparisons to the CIBMTR matched controls.
The estimated 2-year rate of non-relapse mortality in NiCord recipients was 23.8%, and the estimated 2-year incidence of relapse was 33.2%.
The estimated disease-free survival was 49.1% at 1 year and 43.0% at 2 years. The estimated overall survival was 51.2% at 1 year and 2 years.
At 100 days, the rate of grade 2-4 acute GVHD was 44.0%, and the rate of grade 3-4 acute GVHD was 11.1%.
The estimated 1-year rate of mild to severe chronic GVHD was 40.5%, and the estimated 2-year rate of moderate to severe chronic GVHD was 9.8%.
Dr Horwitz said these “promising results” have led to the launch of a phase 3 registration trial in which researchers are comparing NiCord to standard single or double UCB transplant. The trial is open for accrual.
*Information in the abstract differs from the presentation.
SALT LAKE CITY—The expanded umbilical cord blood (UCB) product NiCord can be used as a stand-alone graft, according to research presented at the 2018 BMT Tandem Meetings.
Researchers found that a single NiCord unit provided “robust” engraftment in a phase 1/2 study of patients with high-risk hematologic malignancies.
NiCord recipients had quicker neutrophil and platelet engraftment than matched control subjects who received standard myeloablative UCB transplant (single or double).
Mitchell Horwitz, MD, of the Duke University Medical Center in Durham, North Carolina, presented these results at the meeting as abstract 49.* The research was sponsored by Gamida Cell, the company developing NiCord.
“[NiCord] is an ex vivo expanded cell product that’s derived from an entire unit of umbilical cord blood,” Dr Horwitz explained. “It’s manufactured starting with a CD133-positive selection, which is the progenitor cell population that’s cultured, and a T-cell containing CD133-negative fraction that is provided also at the time of transplant.”
“The culture system contains nicotinamide—that’s the active ingredient in the culture. And that’s supplemented with cytokines—thrombopoietin, IL-6, FLT-3 ligand, and stem cell factor. The culture is 21 days.”
Previous research showed that double UCB transplant including a NiCord unit could provide benefits over standard double UCB transplant. This led Dr Horwitz and his colleagues to wonder if NiCord could be used as a stand-alone graft.
So the team evaluated the safety and efficacy of NiCord alone in 36 adolescents/adults with high-risk hematologic malignancies.
Patients had acute myelogenous leukemia (n=17), acute lymphoblastic leukemia (n=9), myelodysplastic syndrome (n=7), chronic myelogenous leukemia (n=2), and Hodgkin lymphoma (n=1).
Most patients had intermediate (n=15) or high-risk (n=13) disease. They had a median age of 44 (range, 13-63) and a median weight of 75 kg (range, 41-125).
Treatment
For conditioning, 19 patients received thiotepa, busulfan, and fludarabine. Fifteen patients received total body irradiation and fludarabine with or without cyclophosphamide or thiotepa. And 2 patients received clofarabine, fludarabine, and busulfan.
Most patients had a 4/6 human leukocyte antigen (HLA) match (n=26), 8 had a 5/6 HLA match, and 2 had a 6/6 HLA match.
The median total nucleated cell dose was 2.4 x 107/kg prior to expansion of the UCB unit and 3.7 x 107/kg after expansion. The median CD34+ cell dose was 0.2 x 106/kg and 6.3 x 106/kg, respectively.
“CD34 cells were expanded 33-fold in the 3-week culture system,” Dr Horwitz noted. “That translated to a median CD34 dose of 6.3 x 106/kg, a dose comparable to what would be obtained from an adult donor graft.”
Engraftment
There was 1 case of primary graft failure and 2 cases of secondary graft failure. One case of secondary graft failure was associated with an HHV-6 infection, and the other was due to a lethal adenovirus infection.
Of those patients who engrafted, 97% achieved full donor chimerism, and 3% had mixed chimerism.
Dr Horwitz and his colleagues compared engraftment results in the NiCord recipients to results in a cohort of patients from the CIBMTR registry who underwent UCB transplants from 2010 to 2013. They had similar characteristics as the NiCord patients—age, conditioning regimen, disease status, etc.
In total, there were 148 CIBMTR registry patients, 20% of whom received a single UCB unit.
The median time to neutrophil engraftment was 11.5 days (range, 6-26) with NiCord and 21 days in the CIBMTR matched control cohort (P<0.001). The cumulative incidence of neutrophil engraftment was 94.4% and 89.7%, respectively.
The median time to platelet engraftment was 34 days (range, 25-96) with NiCord and 46 days in the CIBMTR controls (P<0.001). The cumulative incidence of platelet engraftment was 80.6% and 67.1%, respectively.
“There’s a median 10-day reduction in neutrophil recovery [and] 12-day reduction in time to platelet recovery [with NiCord],” Dr Horwitz noted. “There is evidence of robust and durable engraftment with a NiCord unit, with one patient now over 7 years from his first transplant on the pilot trial.”
Relapse, survival, and GVHD
Dr Horwitz reported other outcomes in the NiCord recipients without making comparisons to the CIBMTR matched controls.
The estimated 2-year rate of non-relapse mortality in NiCord recipients was 23.8%, and the estimated 2-year incidence of relapse was 33.2%.
The estimated disease-free survival was 49.1% at 1 year and 43.0% at 2 years. The estimated overall survival was 51.2% at 1 year and 2 years.
At 100 days, the rate of grade 2-4 acute GVHD was 44.0%, and the rate of grade 3-4 acute GVHD was 11.1%.
The estimated 1-year rate of mild to severe chronic GVHD was 40.5%, and the estimated 2-year rate of moderate to severe chronic GVHD was 9.8%.
Dr Horwitz said these “promising results” have led to the launch of a phase 3 registration trial in which researchers are comparing NiCord to standard single or double UCB transplant. The trial is open for accrual.
*Information in the abstract differs from the presentation.
Minihaplo-BMT can cure severe hemoglobinopathies
SALT LAKE CITY—Cure of severe hemoglobinopathies is now possible for most patients, according to a speaker at the 2018 BMT Tandem Meetings.
Results of a small study suggest that nonmyeloablative haploidentical bone marrow transplant (minihaplo-BMT), when used with 400 cGy total body irradiation and post-transplant cyclophosphamide, can cure sickle cell disease (SCD) and beta-thalassemia while conferring limited toxicity.
“This is our second study showing that you can certainly get rid of these conditions using haploidentical donors and, also, that you can cure these conditions with a nonmyeloablative regimen,” said Javier Bolaños-Meade, MD, of Johns Hopkins University in Baltimore, Maryland.
“What we saw [in the current study] is that increasing the total body irradiation from 200 cGy to 400 cGy can overcome the very high rate of graft failure we observed in our prior study.”
However, the results also suggest that major ABO incompatible donors should be avoided.
Dr Bolaños-Meade presented these findings as a late-breaking abstract (LBA3) at this year’s BMT Tandem Meetings.
He began the presentation by pointing out that allogeneic BMT is the only potential cure for SCD and beta-thalassemia. Unfortunately, most of these patients have been excluded from transplant due to a lack of matched donors, concerns over graft-vs-host disease (GVHD), and/or compromised end organ function precluding them from myeloablative conditioning.
With a prior study, Dr Bolaños-Meade and his colleagues found that minihaplo-BMT with post-transplant cyclophosphamide expanded the donor pool and was well tolerated in patients with SCD. However, the rate of secondary graft failure was high, at 43%.
“We hypothesized that increasing the amount of radiation that was given to these patients, making the regimen absolutely more intensive, will help us to overcome this rate of graft failure and retain the tolerability of the regimen,” Dr Bolaños-Meade said.
He and his colleagues tested this theory in 12 patients with SCD and 5 with beta-thalassemia.
The SCD patients had a median age of 26 (range, 6-31), and most (n=8) were female. Ten were African-American, and 2 were of Arab descent.
All SCD patients had at least 2 hospital admissions in the last 2 years, 5 had osteonecrosis, 3 were transfusion-dependent, 2 had a history of acute chest syndrome, and 1 patient had changes in brain magnetic resonance imaging.
The thalassemia patients had a median age of 7 (range, 6-16). Four were female, and all 5 were of Arab descent. All patients were transfusion-dependent from infancy.
Treatment
All patients received antithymocyte globulin (rabbit) at 0.5 mg/kg on day -9 and 2 mg/kg on days -8 and -7, fludarabine at 30 mg/m2 on days -6 to -2, cyclophosphamide at 14.5 mg/kg on days -6 and -5, and total body irradiation at 400 cGy on day -1.
Patients received unmanipulated bone marrow that was collected and infused on day 0. Donors included 1 aunt, 4 brothers, 3 sisters, 5 mothers, and 4 fathers. There were 2 major ABO incompatible pairs, 5 minor ABO incompatible pairs, and 10 ABO compatible pairs.
For GVHD prophylaxis, patients received 50 mg/kg/day of cyclophosphamide on days 3 and 4, sirolimus (levels of 5-10 ng/dl) from days 5 to 365, and mycophenolate mofetil at 1 g every 8 hours from days 5 to 35.
Efficacy
All 17 patients are still alive at a median follow-up of 15 months (range, 3-34).
“Of all the patients transplanted, we only observed 1 graft failure,” Dr Bolaños-Meade said. “This is in sharp contrast to the 40% graft failure in our prior study.”
Thirteen patients achieved full donor chimerism, and 3 had mixed chimerism.
Four of the 5 beta-thalassemia patients achieved full donor chimerism, and 1 had mixed chimerism. All 5 patients became transfusion-independent.
Eleven of the 12 SCD patients engrafted, and 9 achieved full donor chimerism.
All but one of the engrafted SCD patients became transfusion-independent. The exception was a mixed chimeric patient who had a major ABO mismatched donor. The patient remains transfusion-dependent more than 30 months after BMT.
“This is the main problem we have seen in all our sickle cell and hemoglobinopathy experiences,” Dr Bolaños-Meade said. “If you have a major ABO incompatibility, and there’s mixed chimerism, you’re asking for trouble.”
Toxicity
All SCD patients had sickle cell crises after antithymocyte globulin. Other toxicities included sirolimus-induced diabetes in 1 patient, worsening of Meniere’s disease in 1 patient, and BK cystitis in 1 patient.
Two patients developed grade 2 acute GVHD, and 1 developed grade 3 acute GVHD. Three patients had chronic GVHD, 2 mild and 1 moderate.
However, all cases of GVHD resolved. And, of the 8 engrafted patients with more than 1 year of follow-up, 6 are off systemic immunosuppression.
SALT LAKE CITY—Cure of severe hemoglobinopathies is now possible for most patients, according to a speaker at the 2018 BMT Tandem Meetings.
Results of a small study suggest that nonmyeloablative haploidentical bone marrow transplant (minihaplo-BMT), when used with 400 cGy total body irradiation and post-transplant cyclophosphamide, can cure sickle cell disease (SCD) and beta-thalassemia while conferring limited toxicity.
“This is our second study showing that you can certainly get rid of these conditions using haploidentical donors and, also, that you can cure these conditions with a nonmyeloablative regimen,” said Javier Bolaños-Meade, MD, of Johns Hopkins University in Baltimore, Maryland.
“What we saw [in the current study] is that increasing the total body irradiation from 200 cGy to 400 cGy can overcome the very high rate of graft failure we observed in our prior study.”
However, the results also suggest that major ABO incompatible donors should be avoided.
Dr Bolaños-Meade presented these findings as a late-breaking abstract (LBA3) at this year’s BMT Tandem Meetings.
He began the presentation by pointing out that allogeneic BMT is the only potential cure for SCD and beta-thalassemia. Unfortunately, most of these patients have been excluded from transplant due to a lack of matched donors, concerns over graft-vs-host disease (GVHD), and/or compromised end organ function precluding them from myeloablative conditioning.
With a prior study, Dr Bolaños-Meade and his colleagues found that minihaplo-BMT with post-transplant cyclophosphamide expanded the donor pool and was well tolerated in patients with SCD. However, the rate of secondary graft failure was high, at 43%.
“We hypothesized that increasing the amount of radiation that was given to these patients, making the regimen absolutely more intensive, will help us to overcome this rate of graft failure and retain the tolerability of the regimen,” Dr Bolaños-Meade said.
He and his colleagues tested this theory in 12 patients with SCD and 5 with beta-thalassemia.
The SCD patients had a median age of 26 (range, 6-31), and most (n=8) were female. Ten were African-American, and 2 were of Arab descent.
All SCD patients had at least 2 hospital admissions in the last 2 years, 5 had osteonecrosis, 3 were transfusion-dependent, 2 had a history of acute chest syndrome, and 1 patient had changes in brain magnetic resonance imaging.
The thalassemia patients had a median age of 7 (range, 6-16). Four were female, and all 5 were of Arab descent. All patients were transfusion-dependent from infancy.
Treatment
All patients received antithymocyte globulin (rabbit) at 0.5 mg/kg on day -9 and 2 mg/kg on days -8 and -7, fludarabine at 30 mg/m2 on days -6 to -2, cyclophosphamide at 14.5 mg/kg on days -6 and -5, and total body irradiation at 400 cGy on day -1.
Patients received unmanipulated bone marrow that was collected and infused on day 0. Donors included 1 aunt, 4 brothers, 3 sisters, 5 mothers, and 4 fathers. There were 2 major ABO incompatible pairs, 5 minor ABO incompatible pairs, and 10 ABO compatible pairs.
For GVHD prophylaxis, patients received 50 mg/kg/day of cyclophosphamide on days 3 and 4, sirolimus (levels of 5-10 ng/dl) from days 5 to 365, and mycophenolate mofetil at 1 g every 8 hours from days 5 to 35.
Efficacy
All 17 patients are still alive at a median follow-up of 15 months (range, 3-34).
“Of all the patients transplanted, we only observed 1 graft failure,” Dr Bolaños-Meade said. “This is in sharp contrast to the 40% graft failure in our prior study.”
Thirteen patients achieved full donor chimerism, and 3 had mixed chimerism.
Four of the 5 beta-thalassemia patients achieved full donor chimerism, and 1 had mixed chimerism. All 5 patients became transfusion-independent.
Eleven of the 12 SCD patients engrafted, and 9 achieved full donor chimerism.
All but one of the engrafted SCD patients became transfusion-independent. The exception was a mixed chimeric patient who had a major ABO mismatched donor. The patient remains transfusion-dependent more than 30 months after BMT.
“This is the main problem we have seen in all our sickle cell and hemoglobinopathy experiences,” Dr Bolaños-Meade said. “If you have a major ABO incompatibility, and there’s mixed chimerism, you’re asking for trouble.”
Toxicity
All SCD patients had sickle cell crises after antithymocyte globulin. Other toxicities included sirolimus-induced diabetes in 1 patient, worsening of Meniere’s disease in 1 patient, and BK cystitis in 1 patient.
Two patients developed grade 2 acute GVHD, and 1 developed grade 3 acute GVHD. Three patients had chronic GVHD, 2 mild and 1 moderate.
However, all cases of GVHD resolved. And, of the 8 engrafted patients with more than 1 year of follow-up, 6 are off systemic immunosuppression.
SALT LAKE CITY—Cure of severe hemoglobinopathies is now possible for most patients, according to a speaker at the 2018 BMT Tandem Meetings.
Results of a small study suggest that nonmyeloablative haploidentical bone marrow transplant (minihaplo-BMT), when used with 400 cGy total body irradiation and post-transplant cyclophosphamide, can cure sickle cell disease (SCD) and beta-thalassemia while conferring limited toxicity.
“This is our second study showing that you can certainly get rid of these conditions using haploidentical donors and, also, that you can cure these conditions with a nonmyeloablative regimen,” said Javier Bolaños-Meade, MD, of Johns Hopkins University in Baltimore, Maryland.
“What we saw [in the current study] is that increasing the total body irradiation from 200 cGy to 400 cGy can overcome the very high rate of graft failure we observed in our prior study.”
However, the results also suggest that major ABO incompatible donors should be avoided.
Dr Bolaños-Meade presented these findings as a late-breaking abstract (LBA3) at this year’s BMT Tandem Meetings.
He began the presentation by pointing out that allogeneic BMT is the only potential cure for SCD and beta-thalassemia. Unfortunately, most of these patients have been excluded from transplant due to a lack of matched donors, concerns over graft-vs-host disease (GVHD), and/or compromised end organ function precluding them from myeloablative conditioning.
With a prior study, Dr Bolaños-Meade and his colleagues found that minihaplo-BMT with post-transplant cyclophosphamide expanded the donor pool and was well tolerated in patients with SCD. However, the rate of secondary graft failure was high, at 43%.
“We hypothesized that increasing the amount of radiation that was given to these patients, making the regimen absolutely more intensive, will help us to overcome this rate of graft failure and retain the tolerability of the regimen,” Dr Bolaños-Meade said.
He and his colleagues tested this theory in 12 patients with SCD and 5 with beta-thalassemia.
The SCD patients had a median age of 26 (range, 6-31), and most (n=8) were female. Ten were African-American, and 2 were of Arab descent.
All SCD patients had at least 2 hospital admissions in the last 2 years, 5 had osteonecrosis, 3 were transfusion-dependent, 2 had a history of acute chest syndrome, and 1 patient had changes in brain magnetic resonance imaging.
The thalassemia patients had a median age of 7 (range, 6-16). Four were female, and all 5 were of Arab descent. All patients were transfusion-dependent from infancy.
Treatment
All patients received antithymocyte globulin (rabbit) at 0.5 mg/kg on day -9 and 2 mg/kg on days -8 and -7, fludarabine at 30 mg/m2 on days -6 to -2, cyclophosphamide at 14.5 mg/kg on days -6 and -5, and total body irradiation at 400 cGy on day -1.
Patients received unmanipulated bone marrow that was collected and infused on day 0. Donors included 1 aunt, 4 brothers, 3 sisters, 5 mothers, and 4 fathers. There were 2 major ABO incompatible pairs, 5 minor ABO incompatible pairs, and 10 ABO compatible pairs.
For GVHD prophylaxis, patients received 50 mg/kg/day of cyclophosphamide on days 3 and 4, sirolimus (levels of 5-10 ng/dl) from days 5 to 365, and mycophenolate mofetil at 1 g every 8 hours from days 5 to 35.
Efficacy
All 17 patients are still alive at a median follow-up of 15 months (range, 3-34).
“Of all the patients transplanted, we only observed 1 graft failure,” Dr Bolaños-Meade said. “This is in sharp contrast to the 40% graft failure in our prior study.”
Thirteen patients achieved full donor chimerism, and 3 had mixed chimerism.
Four of the 5 beta-thalassemia patients achieved full donor chimerism, and 1 had mixed chimerism. All 5 patients became transfusion-independent.
Eleven of the 12 SCD patients engrafted, and 9 achieved full donor chimerism.
All but one of the engrafted SCD patients became transfusion-independent. The exception was a mixed chimeric patient who had a major ABO mismatched donor. The patient remains transfusion-dependent more than 30 months after BMT.
“This is the main problem we have seen in all our sickle cell and hemoglobinopathy experiences,” Dr Bolaños-Meade said. “If you have a major ABO incompatibility, and there’s mixed chimerism, you’re asking for trouble.”
Toxicity
All SCD patients had sickle cell crises after antithymocyte globulin. Other toxicities included sirolimus-induced diabetes in 1 patient, worsening of Meniere’s disease in 1 patient, and BK cystitis in 1 patient.
Two patients developed grade 2 acute GVHD, and 1 developed grade 3 acute GVHD. Three patients had chronic GVHD, 2 mild and 1 moderate.
However, all cases of GVHD resolved. And, of the 8 engrafted patients with more than 1 year of follow-up, 6 are off systemic immunosuppression.
Regimen deemed ‘safe and feasible’ in MM
SALT LAKE CITY—A novel transplant regimen is “safe and feasible” for patients with multiple myeloma (MM), according to a presentation at the 2018 BMT Tandem Meetings.
Researchers conducted a phase 1 trial investigating the addition of elotuzumab and autologous peripheral blood mononuclear cell (PBMC) reconstitution to standard autologous hematopoietic stem cell transplant (ASCT) and lenalidomide maintenance in MM patients.
The regimen was considered well tolerated, as most adverse events (AEs) were grade 1 or 2.
The complete response (CR) rate was 40% at both 90 days and 1 year after ASCT.
Keren Osman, MD, of Mount Sinai Health System in New York, New York, reported these results as abstract 26.* This is an investigator-sponsored study, conducted in collaboration with Bristol Myers Squibb, the company marketing elotuzumab.
Dr Osman noted that elotuzumab is a humanized IgG1 monoclonal antibody targeting SLAMF7. The drug directly activates natural killer (NK) cells through the SLAMF7 pathway and Fc receptors. Elotuzumab also targets SLAMF7 on MM cells and facilitates interaction with NK cells to mediate the killing of MM cells through antibody-dependent cellular cytotoxicity.
“The hypothesis behind this phase 1 study was that . . ., in the peri-transplant period, if we add elotuzumab, we will succeed in promoting NK-mediated elimination of residual multiple myeloma cells as well as promote transition from innate to adaptive immune responses against multiple myeloma-associated antigens,” Dr Osman said.
She and her colleagues tested this hypothesis in 15 MM patients. They had a median age of 59 (range, 49-70), and 60% of them were male.
Forty percent of patients had stage I disease, 27% had stage II, and 20% had stage III. All patients had an ECOG status of 0 (47%) or 1 (53%).
The patients had a median of 174 days since diagnosis (range, 98-393).
All patients had received 1 to 2 prior lines of therapy. They all had bortezomib as part of their induction therapy, and 67% of them had received lenalidomide.
Seventy-three percent of patients had any cytogenetic abnormality, and 47% had high-risk cytogenetics.
Treatment
Patients underwent leukopheresis for PBMC collection, followed by standard peripheral blood stem cell mobilization and harvest.
They received standard melphalan conditioning on day -1 and autologous stem cell rescue on day 0. Autologous PBMCs were reinfused on day 3 after stem cell infusion.
Elotuzumab was given at 20 mg/kg intravenously on day 4. The drug was given every 28 days up to cycle 12.
Lenalidomide maintenance was given at 10 mg orally on days 1 to 21 of every 28-day cycle, starting with cycle 4 of elotuzumab (90 days post-ASCT). Maintenance could continue beyond cycle 12 at the investigators’ discretion.
Thirteen patients completed a year of treatment. One patient withdrew from the study due to early progression. The other patient withdrew due to personal choice and had a very good partial response (VGPR) at withdrawal.
Safety
“The majority of the adverse events, including infusion reactions attributable to elotuzumab, were grade 2 or lower,” Dr Osman noted. “And there were no AEs related to PBMC administration.”
One patient had a delay in hematopoietic reconstitution, which resulted in hospitalization exceeding 21 days.
One patient had grade 3 hypertension, which was attributed to elotuzumab and resolved with supportive care.
Eight patients had grade 3 lymphopenia, which was associated with elotuzumab, during the maintenance phase. Patients received prophylactic antibiotics, and there were no opportunistic infections.
Efficacy
At screening (after induction but before ASCT), 13 patients (87%) had a VGPR, and 2 (13%) had a partial response (PR).
At 90 days post-ASCT, 2 patients (13%) had a stringent CR, and 4 (27%) had a CR. Six patients (40%) had a VGPR, and 2 (13%) had a PR. One patient (7%) had progressed.
“In this very high-risk PR/VGPR population, stem cell transplant with elotuzumab and PBMC infusion resulted in a CR rate of 40%—with 13% of patients achieving stringent CR—by day 90,” Dr Osman noted. “And maintenance elotuzumab plus lenalidomide promoted further conversion to 33% stringent CR by 1 year.”
At 1 year, 5 patients (33%) had a stringent CR, and 1 (7%) had a CR. Six patients (40%) had a VGPR, and 1 (7%) had a PR. Two patients (13%) had progressed.
So the 1-year progression-free survival rate was 86% (13/15).
“In conclusion, we see that elotuzumab and PBMC administration with standard autologous stem cell transplant and lenalidomide maintenance for consolidation therapy in multiple myeloma is certainly both safe and feasible,” Dr Osman said. “We’re planning a phase 2 study.”
*Information in the abstract differs from the presentation.
SALT LAKE CITY—A novel transplant regimen is “safe and feasible” for patients with multiple myeloma (MM), according to a presentation at the 2018 BMT Tandem Meetings.
Researchers conducted a phase 1 trial investigating the addition of elotuzumab and autologous peripheral blood mononuclear cell (PBMC) reconstitution to standard autologous hematopoietic stem cell transplant (ASCT) and lenalidomide maintenance in MM patients.
The regimen was considered well tolerated, as most adverse events (AEs) were grade 1 or 2.
The complete response (CR) rate was 40% at both 90 days and 1 year after ASCT.
Keren Osman, MD, of Mount Sinai Health System in New York, New York, reported these results as abstract 26.* This is an investigator-sponsored study, conducted in collaboration with Bristol Myers Squibb, the company marketing elotuzumab.
Dr Osman noted that elotuzumab is a humanized IgG1 monoclonal antibody targeting SLAMF7. The drug directly activates natural killer (NK) cells through the SLAMF7 pathway and Fc receptors. Elotuzumab also targets SLAMF7 on MM cells and facilitates interaction with NK cells to mediate the killing of MM cells through antibody-dependent cellular cytotoxicity.
“The hypothesis behind this phase 1 study was that . . ., in the peri-transplant period, if we add elotuzumab, we will succeed in promoting NK-mediated elimination of residual multiple myeloma cells as well as promote transition from innate to adaptive immune responses against multiple myeloma-associated antigens,” Dr Osman said.
She and her colleagues tested this hypothesis in 15 MM patients. They had a median age of 59 (range, 49-70), and 60% of them were male.
Forty percent of patients had stage I disease, 27% had stage II, and 20% had stage III. All patients had an ECOG status of 0 (47%) or 1 (53%).
The patients had a median of 174 days since diagnosis (range, 98-393).
All patients had received 1 to 2 prior lines of therapy. They all had bortezomib as part of their induction therapy, and 67% of them had received lenalidomide.
Seventy-three percent of patients had any cytogenetic abnormality, and 47% had high-risk cytogenetics.
Treatment
Patients underwent leukopheresis for PBMC collection, followed by standard peripheral blood stem cell mobilization and harvest.
They received standard melphalan conditioning on day -1 and autologous stem cell rescue on day 0. Autologous PBMCs were reinfused on day 3 after stem cell infusion.
Elotuzumab was given at 20 mg/kg intravenously on day 4. The drug was given every 28 days up to cycle 12.
Lenalidomide maintenance was given at 10 mg orally on days 1 to 21 of every 28-day cycle, starting with cycle 4 of elotuzumab (90 days post-ASCT). Maintenance could continue beyond cycle 12 at the investigators’ discretion.
Thirteen patients completed a year of treatment. One patient withdrew from the study due to early progression. The other patient withdrew due to personal choice and had a very good partial response (VGPR) at withdrawal.
Safety
“The majority of the adverse events, including infusion reactions attributable to elotuzumab, were grade 2 or lower,” Dr Osman noted. “And there were no AEs related to PBMC administration.”
One patient had a delay in hematopoietic reconstitution, which resulted in hospitalization exceeding 21 days.
One patient had grade 3 hypertension, which was attributed to elotuzumab and resolved with supportive care.
Eight patients had grade 3 lymphopenia, which was associated with elotuzumab, during the maintenance phase. Patients received prophylactic antibiotics, and there were no opportunistic infections.
Efficacy
At screening (after induction but before ASCT), 13 patients (87%) had a VGPR, and 2 (13%) had a partial response (PR).
At 90 days post-ASCT, 2 patients (13%) had a stringent CR, and 4 (27%) had a CR. Six patients (40%) had a VGPR, and 2 (13%) had a PR. One patient (7%) had progressed.
“In this very high-risk PR/VGPR population, stem cell transplant with elotuzumab and PBMC infusion resulted in a CR rate of 40%—with 13% of patients achieving stringent CR—by day 90,” Dr Osman noted. “And maintenance elotuzumab plus lenalidomide promoted further conversion to 33% stringent CR by 1 year.”
At 1 year, 5 patients (33%) had a stringent CR, and 1 (7%) had a CR. Six patients (40%) had a VGPR, and 1 (7%) had a PR. Two patients (13%) had progressed.
So the 1-year progression-free survival rate was 86% (13/15).
“In conclusion, we see that elotuzumab and PBMC administration with standard autologous stem cell transplant and lenalidomide maintenance for consolidation therapy in multiple myeloma is certainly both safe and feasible,” Dr Osman said. “We’re planning a phase 2 study.”
*Information in the abstract differs from the presentation.
SALT LAKE CITY—A novel transplant regimen is “safe and feasible” for patients with multiple myeloma (MM), according to a presentation at the 2018 BMT Tandem Meetings.
Researchers conducted a phase 1 trial investigating the addition of elotuzumab and autologous peripheral blood mononuclear cell (PBMC) reconstitution to standard autologous hematopoietic stem cell transplant (ASCT) and lenalidomide maintenance in MM patients.
The regimen was considered well tolerated, as most adverse events (AEs) were grade 1 or 2.
The complete response (CR) rate was 40% at both 90 days and 1 year after ASCT.
Keren Osman, MD, of Mount Sinai Health System in New York, New York, reported these results as abstract 26.* This is an investigator-sponsored study, conducted in collaboration with Bristol Myers Squibb, the company marketing elotuzumab.
Dr Osman noted that elotuzumab is a humanized IgG1 monoclonal antibody targeting SLAMF7. The drug directly activates natural killer (NK) cells through the SLAMF7 pathway and Fc receptors. Elotuzumab also targets SLAMF7 on MM cells and facilitates interaction with NK cells to mediate the killing of MM cells through antibody-dependent cellular cytotoxicity.
“The hypothesis behind this phase 1 study was that . . ., in the peri-transplant period, if we add elotuzumab, we will succeed in promoting NK-mediated elimination of residual multiple myeloma cells as well as promote transition from innate to adaptive immune responses against multiple myeloma-associated antigens,” Dr Osman said.
She and her colleagues tested this hypothesis in 15 MM patients. They had a median age of 59 (range, 49-70), and 60% of them were male.
Forty percent of patients had stage I disease, 27% had stage II, and 20% had stage III. All patients had an ECOG status of 0 (47%) or 1 (53%).
The patients had a median of 174 days since diagnosis (range, 98-393).
All patients had received 1 to 2 prior lines of therapy. They all had bortezomib as part of their induction therapy, and 67% of them had received lenalidomide.
Seventy-three percent of patients had any cytogenetic abnormality, and 47% had high-risk cytogenetics.
Treatment
Patients underwent leukopheresis for PBMC collection, followed by standard peripheral blood stem cell mobilization and harvest.
They received standard melphalan conditioning on day -1 and autologous stem cell rescue on day 0. Autologous PBMCs were reinfused on day 3 after stem cell infusion.
Elotuzumab was given at 20 mg/kg intravenously on day 4. The drug was given every 28 days up to cycle 12.
Lenalidomide maintenance was given at 10 mg orally on days 1 to 21 of every 28-day cycle, starting with cycle 4 of elotuzumab (90 days post-ASCT). Maintenance could continue beyond cycle 12 at the investigators’ discretion.
Thirteen patients completed a year of treatment. One patient withdrew from the study due to early progression. The other patient withdrew due to personal choice and had a very good partial response (VGPR) at withdrawal.
Safety
“The majority of the adverse events, including infusion reactions attributable to elotuzumab, were grade 2 or lower,” Dr Osman noted. “And there were no AEs related to PBMC administration.”
One patient had a delay in hematopoietic reconstitution, which resulted in hospitalization exceeding 21 days.
One patient had grade 3 hypertension, which was attributed to elotuzumab and resolved with supportive care.
Eight patients had grade 3 lymphopenia, which was associated with elotuzumab, during the maintenance phase. Patients received prophylactic antibiotics, and there were no opportunistic infections.
Efficacy
At screening (after induction but before ASCT), 13 patients (87%) had a VGPR, and 2 (13%) had a partial response (PR).
At 90 days post-ASCT, 2 patients (13%) had a stringent CR, and 4 (27%) had a CR. Six patients (40%) had a VGPR, and 2 (13%) had a PR. One patient (7%) had progressed.
“In this very high-risk PR/VGPR population, stem cell transplant with elotuzumab and PBMC infusion resulted in a CR rate of 40%—with 13% of patients achieving stringent CR—by day 90,” Dr Osman noted. “And maintenance elotuzumab plus lenalidomide promoted further conversion to 33% stringent CR by 1 year.”
At 1 year, 5 patients (33%) had a stringent CR, and 1 (7%) had a CR. Six patients (40%) had a VGPR, and 1 (7%) had a PR. Two patients (13%) had progressed.
So the 1-year progression-free survival rate was 86% (13/15).
“In conclusion, we see that elotuzumab and PBMC administration with standard autologous stem cell transplant and lenalidomide maintenance for consolidation therapy in multiple myeloma is certainly both safe and feasible,” Dr Osman said. “We’re planning a phase 2 study.”
*Information in the abstract differs from the presentation.