User login
Gene variants linked to survival after HSCT
New research has revealed a link between rare gene variants and survival after hematopoietic stem cell transplant (HSCT).
Researchers performed exome sequencing in nearly 2500 HSCT recipients and their matched, unrelated donors.
The sequencing revealed several gene variants—in both donors and recipients—that were significantly associated with overall survival (OS), transplant-related mortality (TRM), and disease-related mortality (DRM) after HSCT.
Qianqian Zhu, PhD, of Roswell Park Comprehensive Cancer Center in Buffalo, New York, and her colleagues described these findings in Blood.
The team performed exome sequencing—using the Illumina HumanExome BeadChip—in patients who participated in the DISCOVeRY-BMT study.
This included 2473 HSCT recipients who had acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic syndromes. It also included 2221 donors who were a 10/10 human leukocyte antigen match for each recipient.
The researchers looked at genetic variants in donors and recipients and assessed the variants’ associations with OS, TRM, and DRM.
Variants in recipients
Analyses revealed an increased risk of TRM when there was a mismatch between donors and recipients for a variant in TEX38—rs200092801. The increased risk was even more pronounced when either the recipient or the donor was female.
Among the recipients mismatched with their donors at rs200092801, every female recipient and every recipient with a female donor died from TRM. In comparison, 44% of the male recipients with male donors died from TRM.
The researchers said the rs200092801 variant may prompt the production of a mutant peptide that can be presented by MHC-I molecules to immune cells to trigger downstream immune response and TRM.
Dr Zhu and her colleagues also identified variants that appeared to have a positive impact on TRM and OS.
Recipients who had any of 6 variants in the gene OR51D1 had a decreased risk of TRM and improved OS.
The variants (rs138224979, rs148606808, rs141786655, rs61745314, rs200394876, and rs149135276) were not associated with DRM, so the researchers concluded that the improvement in OS was driven by protection against TRM.
Donor variants linked to OS
Donors had variants in 4 genes—ALPP, EMID1, SLC44A5, and LRP1—that were associated with OS but not TRM or DRM.
The 3 variants identified in ALPP (rs144454460, rs140078460, and rs142493383) were associated with improved OS.
And the 2 variants in SLC44A5 (rs143004355 and rs149696907) were associated with worse OS.
There were 2 variants in EMID1. One was associated with improved OS (rs34772704), and the other was associated with decreased OS (rs139996840).
And there were 27 variants in LRP1. Some had a positive association with OS, and others had a negative association.
Donor variants linked to TRM and DRM
Six variants in the HHAT gene were associated with TRM. Five of the variants appeared to have a protective effect against TRM (rs145455128, rs146916002, rs61744143, rs149597734, and rs145943928). For the other variant (rs141591165), the apparent effect was inconsistent between patient cohorts.
There were 3 variants in LYZL4 associated with DRM. Two were associated with an increased risk of DRM (rs147770623 and rs76947105), and 1 appeared to have a protective effect (rs181886204).
Six variants in NT5E appeared to have a protective effect against DRM (rs200250022, rs200369370, rs41271617, rs200648774, rs144719925, and rs145505137).
The researchers said the variants in NT5E probably reduce the enzyme activity of the gene. This supports preclinical findings showing that targeted blockade of NT5E can slow tumor growth.
“We have just started to uncover the biological relevance of these new and unexpected genes to a patient’s survival after [HSCT],” Dr Zhu said.
“Our findings shed light on new areas that were not considered before, but we need to further replicate and test our findings. We’re hoping that additional studies of this type will continue to discover novel genes leading to improved outcomes for patients.”
New research has revealed a link between rare gene variants and survival after hematopoietic stem cell transplant (HSCT).
Researchers performed exome sequencing in nearly 2500 HSCT recipients and their matched, unrelated donors.
The sequencing revealed several gene variants—in both donors and recipients—that were significantly associated with overall survival (OS), transplant-related mortality (TRM), and disease-related mortality (DRM) after HSCT.
Qianqian Zhu, PhD, of Roswell Park Comprehensive Cancer Center in Buffalo, New York, and her colleagues described these findings in Blood.
The team performed exome sequencing—using the Illumina HumanExome BeadChip—in patients who participated in the DISCOVeRY-BMT study.
This included 2473 HSCT recipients who had acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic syndromes. It also included 2221 donors who were a 10/10 human leukocyte antigen match for each recipient.
The researchers looked at genetic variants in donors and recipients and assessed the variants’ associations with OS, TRM, and DRM.
Variants in recipients
Analyses revealed an increased risk of TRM when there was a mismatch between donors and recipients for a variant in TEX38—rs200092801. The increased risk was even more pronounced when either the recipient or the donor was female.
Among the recipients mismatched with their donors at rs200092801, every female recipient and every recipient with a female donor died from TRM. In comparison, 44% of the male recipients with male donors died from TRM.
The researchers said the rs200092801 variant may prompt the production of a mutant peptide that can be presented by MHC-I molecules to immune cells to trigger downstream immune response and TRM.
Dr Zhu and her colleagues also identified variants that appeared to have a positive impact on TRM and OS.
Recipients who had any of 6 variants in the gene OR51D1 had a decreased risk of TRM and improved OS.
The variants (rs138224979, rs148606808, rs141786655, rs61745314, rs200394876, and rs149135276) were not associated with DRM, so the researchers concluded that the improvement in OS was driven by protection against TRM.
Donor variants linked to OS
Donors had variants in 4 genes—ALPP, EMID1, SLC44A5, and LRP1—that were associated with OS but not TRM or DRM.
The 3 variants identified in ALPP (rs144454460, rs140078460, and rs142493383) were associated with improved OS.
And the 2 variants in SLC44A5 (rs143004355 and rs149696907) were associated with worse OS.
There were 2 variants in EMID1. One was associated with improved OS (rs34772704), and the other was associated with decreased OS (rs139996840).
And there were 27 variants in LRP1. Some had a positive association with OS, and others had a negative association.
Donor variants linked to TRM and DRM
Six variants in the HHAT gene were associated with TRM. Five of the variants appeared to have a protective effect against TRM (rs145455128, rs146916002, rs61744143, rs149597734, and rs145943928). For the other variant (rs141591165), the apparent effect was inconsistent between patient cohorts.
There were 3 variants in LYZL4 associated with DRM. Two were associated with an increased risk of DRM (rs147770623 and rs76947105), and 1 appeared to have a protective effect (rs181886204).
Six variants in NT5E appeared to have a protective effect against DRM (rs200250022, rs200369370, rs41271617, rs200648774, rs144719925, and rs145505137).
The researchers said the variants in NT5E probably reduce the enzyme activity of the gene. This supports preclinical findings showing that targeted blockade of NT5E can slow tumor growth.
“We have just started to uncover the biological relevance of these new and unexpected genes to a patient’s survival after [HSCT],” Dr Zhu said.
“Our findings shed light on new areas that were not considered before, but we need to further replicate and test our findings. We’re hoping that additional studies of this type will continue to discover novel genes leading to improved outcomes for patients.”
New research has revealed a link between rare gene variants and survival after hematopoietic stem cell transplant (HSCT).
Researchers performed exome sequencing in nearly 2500 HSCT recipients and their matched, unrelated donors.
The sequencing revealed several gene variants—in both donors and recipients—that were significantly associated with overall survival (OS), transplant-related mortality (TRM), and disease-related mortality (DRM) after HSCT.
Qianqian Zhu, PhD, of Roswell Park Comprehensive Cancer Center in Buffalo, New York, and her colleagues described these findings in Blood.
The team performed exome sequencing—using the Illumina HumanExome BeadChip—in patients who participated in the DISCOVeRY-BMT study.
This included 2473 HSCT recipients who had acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic syndromes. It also included 2221 donors who were a 10/10 human leukocyte antigen match for each recipient.
The researchers looked at genetic variants in donors and recipients and assessed the variants’ associations with OS, TRM, and DRM.
Variants in recipients
Analyses revealed an increased risk of TRM when there was a mismatch between donors and recipients for a variant in TEX38—rs200092801. The increased risk was even more pronounced when either the recipient or the donor was female.
Among the recipients mismatched with their donors at rs200092801, every female recipient and every recipient with a female donor died from TRM. In comparison, 44% of the male recipients with male donors died from TRM.
The researchers said the rs200092801 variant may prompt the production of a mutant peptide that can be presented by MHC-I molecules to immune cells to trigger downstream immune response and TRM.
Dr Zhu and her colleagues also identified variants that appeared to have a positive impact on TRM and OS.
Recipients who had any of 6 variants in the gene OR51D1 had a decreased risk of TRM and improved OS.
The variants (rs138224979, rs148606808, rs141786655, rs61745314, rs200394876, and rs149135276) were not associated with DRM, so the researchers concluded that the improvement in OS was driven by protection against TRM.
Donor variants linked to OS
Donors had variants in 4 genes—ALPP, EMID1, SLC44A5, and LRP1—that were associated with OS but not TRM or DRM.
The 3 variants identified in ALPP (rs144454460, rs140078460, and rs142493383) were associated with improved OS.
And the 2 variants in SLC44A5 (rs143004355 and rs149696907) were associated with worse OS.
There were 2 variants in EMID1. One was associated with improved OS (rs34772704), and the other was associated with decreased OS (rs139996840).
And there were 27 variants in LRP1. Some had a positive association with OS, and others had a negative association.
Donor variants linked to TRM and DRM
Six variants in the HHAT gene were associated with TRM. Five of the variants appeared to have a protective effect against TRM (rs145455128, rs146916002, rs61744143, rs149597734, and rs145943928). For the other variant (rs141591165), the apparent effect was inconsistent between patient cohorts.
There were 3 variants in LYZL4 associated with DRM. Two were associated with an increased risk of DRM (rs147770623 and rs76947105), and 1 appeared to have a protective effect (rs181886204).
Six variants in NT5E appeared to have a protective effect against DRM (rs200250022, rs200369370, rs41271617, rs200648774, rs144719925, and rs145505137).
The researchers said the variants in NT5E probably reduce the enzyme activity of the gene. This supports preclinical findings showing that targeted blockade of NT5E can slow tumor growth.
“We have just started to uncover the biological relevance of these new and unexpected genes to a patient’s survival after [HSCT],” Dr Zhu said.
“Our findings shed light on new areas that were not considered before, but we need to further replicate and test our findings. We’re hoping that additional studies of this type will continue to discover novel genes leading to improved outcomes for patients.”
MicroRNAs required for cGVHD development
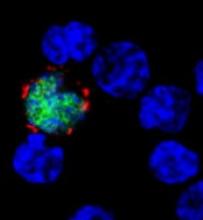
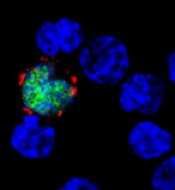
New research suggests a family of microRNAs, miR-17-92, plays a key role in chronic graft-versus-host disease (cGVHD).
Researchers found miR-17-92 is responsible for the T- and B-cell pathogenicity that causes cGVHD.
The team also discovered that pharmacological inhibition of miR-17 alleviated the symptoms of cGVHD in mice.
Yongxia Wu, PhD, of the Medical University of South Carolina in Charleston, and her colleagues reported these findings in Blood.
The researchers previously found that miR-17-92 regulates CD4 T-cell proliferation and Th1 and Treg differentiation in acute (a) GVHD.
So the team set out to investigate whether miR-17-92 regulates T- and B-cell differentiation and function in the development of cGVHD.
“Chronic GVHD has a different pathophysiology and different target organs than aGVHD,” Dr Wu noted. “It’s been a big challenge to try to find a target for cGVHD therapies because of the more complex immune reaction in cGVHD and the fact that its cellular and molecular mechanisms are not as well understood.”
“We decided to extend our aGVHD study to cGVHD, but there’s no single, well-defined murine model that can reflect all of the clinical manifestations seen in cGVHD patients. So we decided to study 4 different cGVHD models to best understand how miR-17-92 contributes overall, across many clinical presentations.”
The team performed a series of experiments in murine models of cGVHD after allogeneic bone marrow transplant (BMT). This included models of scleroderma that had transitioned from aGVHD to cGVHD, classic cGVHD scleroderma, lung inflammation, and a lupus-like condition.
The experiments revealed shared mechanisms by which miR-17-92 mediates cGVHD progression—namely, by regulating T helper-cell differentiation, B-cell activation, germinal center responses, and autoantibody production.
“The mechanism for how miR-17-92 regulates T and B cells was very consistent,” Dr Wu said. “In other words, we did not find any big differences among the models.”
The researchers also assessed whether pharmacological inhibition of miR-17 or miR-19—“key members in the miR-17-92 cluster”—might be effective in the treatment of cGVHD.
The team tested antagomirs specific for miR-17 or miR-19 in the scleroderma cGVHD model and the lupus-like condition.
Anti-miR-17, but not anti-miR-19, reduced skin damage in the scleroderma model and alleviated proteinuria in the lupus-like condition.
“So we not only found a new mechanism for cGVHD development by demonstrating that miR-17-92 is heavily involved in the T- and B-cell responses that lead to cGVHD, but we also found that blocking miR-17 substantially reduced cGVHD symptoms in mice,” Dr Wu said.
“That’s exciting because it provides strong evidence that this miR may be a good target for controlling cGVHD after allogeneic BMT.”
Now, Dr Wu and her colleagues are investigating how other microRNAs may be involved in regulating T- and B-cell function during allogeneic BMT.
New research suggests a family of microRNAs, miR-17-92, plays a key role in chronic graft-versus-host disease (cGVHD).
Researchers found miR-17-92 is responsible for the T- and B-cell pathogenicity that causes cGVHD.
The team also discovered that pharmacological inhibition of miR-17 alleviated the symptoms of cGVHD in mice.
Yongxia Wu, PhD, of the Medical University of South Carolina in Charleston, and her colleagues reported these findings in Blood.
The researchers previously found that miR-17-92 regulates CD4 T-cell proliferation and Th1 and Treg differentiation in acute (a) GVHD.
So the team set out to investigate whether miR-17-92 regulates T- and B-cell differentiation and function in the development of cGVHD.
“Chronic GVHD has a different pathophysiology and different target organs than aGVHD,” Dr Wu noted. “It’s been a big challenge to try to find a target for cGVHD therapies because of the more complex immune reaction in cGVHD and the fact that its cellular and molecular mechanisms are not as well understood.”
“We decided to extend our aGVHD study to cGVHD, but there’s no single, well-defined murine model that can reflect all of the clinical manifestations seen in cGVHD patients. So we decided to study 4 different cGVHD models to best understand how miR-17-92 contributes overall, across many clinical presentations.”
The team performed a series of experiments in murine models of cGVHD after allogeneic bone marrow transplant (BMT). This included models of scleroderma that had transitioned from aGVHD to cGVHD, classic cGVHD scleroderma, lung inflammation, and a lupus-like condition.
The experiments revealed shared mechanisms by which miR-17-92 mediates cGVHD progression—namely, by regulating T helper-cell differentiation, B-cell activation, germinal center responses, and autoantibody production.
“The mechanism for how miR-17-92 regulates T and B cells was very consistent,” Dr Wu said. “In other words, we did not find any big differences among the models.”
The researchers also assessed whether pharmacological inhibition of miR-17 or miR-19—“key members in the miR-17-92 cluster”—might be effective in the treatment of cGVHD.
The team tested antagomirs specific for miR-17 or miR-19 in the scleroderma cGVHD model and the lupus-like condition.
Anti-miR-17, but not anti-miR-19, reduced skin damage in the scleroderma model and alleviated proteinuria in the lupus-like condition.
“So we not only found a new mechanism for cGVHD development by demonstrating that miR-17-92 is heavily involved in the T- and B-cell responses that lead to cGVHD, but we also found that blocking miR-17 substantially reduced cGVHD symptoms in mice,” Dr Wu said.
“That’s exciting because it provides strong evidence that this miR may be a good target for controlling cGVHD after allogeneic BMT.”
Now, Dr Wu and her colleagues are investigating how other microRNAs may be involved in regulating T- and B-cell function during allogeneic BMT.
New research suggests a family of microRNAs, miR-17-92, plays a key role in chronic graft-versus-host disease (cGVHD).
Researchers found miR-17-92 is responsible for the T- and B-cell pathogenicity that causes cGVHD.
The team also discovered that pharmacological inhibition of miR-17 alleviated the symptoms of cGVHD in mice.
Yongxia Wu, PhD, of the Medical University of South Carolina in Charleston, and her colleagues reported these findings in Blood.
The researchers previously found that miR-17-92 regulates CD4 T-cell proliferation and Th1 and Treg differentiation in acute (a) GVHD.
So the team set out to investigate whether miR-17-92 regulates T- and B-cell differentiation and function in the development of cGVHD.
“Chronic GVHD has a different pathophysiology and different target organs than aGVHD,” Dr Wu noted. “It’s been a big challenge to try to find a target for cGVHD therapies because of the more complex immune reaction in cGVHD and the fact that its cellular and molecular mechanisms are not as well understood.”
“We decided to extend our aGVHD study to cGVHD, but there’s no single, well-defined murine model that can reflect all of the clinical manifestations seen in cGVHD patients. So we decided to study 4 different cGVHD models to best understand how miR-17-92 contributes overall, across many clinical presentations.”
The team performed a series of experiments in murine models of cGVHD after allogeneic bone marrow transplant (BMT). This included models of scleroderma that had transitioned from aGVHD to cGVHD, classic cGVHD scleroderma, lung inflammation, and a lupus-like condition.
The experiments revealed shared mechanisms by which miR-17-92 mediates cGVHD progression—namely, by regulating T helper-cell differentiation, B-cell activation, germinal center responses, and autoantibody production.
“The mechanism for how miR-17-92 regulates T and B cells was very consistent,” Dr Wu said. “In other words, we did not find any big differences among the models.”
The researchers also assessed whether pharmacological inhibition of miR-17 or miR-19—“key members in the miR-17-92 cluster”—might be effective in the treatment of cGVHD.
The team tested antagomirs specific for miR-17 or miR-19 in the scleroderma cGVHD model and the lupus-like condition.
Anti-miR-17, but not anti-miR-19, reduced skin damage in the scleroderma model and alleviated proteinuria in the lupus-like condition.
“So we not only found a new mechanism for cGVHD development by demonstrating that miR-17-92 is heavily involved in the T- and B-cell responses that lead to cGVHD, but we also found that blocking miR-17 substantially reduced cGVHD symptoms in mice,” Dr Wu said.
“That’s exciting because it provides strong evidence that this miR may be a good target for controlling cGVHD after allogeneic BMT.”
Now, Dr Wu and her colleagues are investigating how other microRNAs may be involved in regulating T- and B-cell function during allogeneic BMT.
MSC product receives orphan designation
The US Food and Drug Administration (FDA) has granted orphan drug designation to CYP-001 for the treatment of acute graft-versus-host disease (GVHD).
CYP-001 is a mesenchymal stem cell (MSC) product manufactured using Cynata Therapeutics Limited’s proprietary Cymerus™ technology.
According to Cynata, this technology enables economic manufacture of MSCs at commercial scale through the production of an MSC precursor called a mesenchymoangioblast (MCA).
The Cymerus MCA platform provides a source of MSCs that is independent of donor limitations and provides a potential “off-the-shelf” stem cell platform for therapeutic use, Cynata says.
The company recently released results from the first cohort of patients in its ongoing phase 1 trial of CYP-001 for the treatment of steroid-resistant acute GVHD.
The trial includes adults who received an allogeneic hematopoietic stem cell transplant to treat a hematologic disorder and were then diagnosed with steroid-resistant, grade 2-4 GVHD.
The first 8 patients were enrolled in cohort A, where they received 2 infusions of CYP-001 at a dose of 1 million cells/kg, up to a maximum dose of 100 million cells. There was 1 week between the 2 CYP-001 infusions in each patient.
For these 8 patients, overall survival at day 100 was 87.5%.
The overall response rate by day 100 was 100%, with all 8 patients showing an improvement in the severity of GVHD by at least 1 grade compared to baseline.
The complete response rate by day 100 was 50%, meaning GVHD signs/symptoms completely resolved in 4 of the 8 patients.
No treatment-related serious adverse events or safety concerns have been identified to date.
The next 8 patients will be enrolled in cohort B and receive 2 infusions of CYP-001 at a dose of 2 million cells/kg, up to a maximum dose of 200 million cells. Recruitment of these patients is progressing.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to CYP-001 for the treatment of acute graft-versus-host disease (GVHD).
CYP-001 is a mesenchymal stem cell (MSC) product manufactured using Cynata Therapeutics Limited’s proprietary Cymerus™ technology.
According to Cynata, this technology enables economic manufacture of MSCs at commercial scale through the production of an MSC precursor called a mesenchymoangioblast (MCA).
The Cymerus MCA platform provides a source of MSCs that is independent of donor limitations and provides a potential “off-the-shelf” stem cell platform for therapeutic use, Cynata says.
The company recently released results from the first cohort of patients in its ongoing phase 1 trial of CYP-001 for the treatment of steroid-resistant acute GVHD.
The trial includes adults who received an allogeneic hematopoietic stem cell transplant to treat a hematologic disorder and were then diagnosed with steroid-resistant, grade 2-4 GVHD.
The first 8 patients were enrolled in cohort A, where they received 2 infusions of CYP-001 at a dose of 1 million cells/kg, up to a maximum dose of 100 million cells. There was 1 week between the 2 CYP-001 infusions in each patient.
For these 8 patients, overall survival at day 100 was 87.5%.
The overall response rate by day 100 was 100%, with all 8 patients showing an improvement in the severity of GVHD by at least 1 grade compared to baseline.
The complete response rate by day 100 was 50%, meaning GVHD signs/symptoms completely resolved in 4 of the 8 patients.
No treatment-related serious adverse events or safety concerns have been identified to date.
The next 8 patients will be enrolled in cohort B and receive 2 infusions of CYP-001 at a dose of 2 million cells/kg, up to a maximum dose of 200 million cells. Recruitment of these patients is progressing.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to CYP-001 for the treatment of acute graft-versus-host disease (GVHD).
CYP-001 is a mesenchymal stem cell (MSC) product manufactured using Cynata Therapeutics Limited’s proprietary Cymerus™ technology.
According to Cynata, this technology enables economic manufacture of MSCs at commercial scale through the production of an MSC precursor called a mesenchymoangioblast (MCA).
The Cymerus MCA platform provides a source of MSCs that is independent of donor limitations and provides a potential “off-the-shelf” stem cell platform for therapeutic use, Cynata says.
The company recently released results from the first cohort of patients in its ongoing phase 1 trial of CYP-001 for the treatment of steroid-resistant acute GVHD.
The trial includes adults who received an allogeneic hematopoietic stem cell transplant to treat a hematologic disorder and were then diagnosed with steroid-resistant, grade 2-4 GVHD.
The first 8 patients were enrolled in cohort A, where they received 2 infusions of CYP-001 at a dose of 1 million cells/kg, up to a maximum dose of 100 million cells. There was 1 week between the 2 CYP-001 infusions in each patient.
For these 8 patients, overall survival at day 100 was 87.5%.
The overall response rate by day 100 was 100%, with all 8 patients showing an improvement in the severity of GVHD by at least 1 grade compared to baseline.
The complete response rate by day 100 was 50%, meaning GVHD signs/symptoms completely resolved in 4 of the 8 patients.
No treatment-related serious adverse events or safety concerns have been identified to date.
The next 8 patients will be enrolled in cohort B and receive 2 infusions of CYP-001 at a dose of 2 million cells/kg, up to a maximum dose of 200 million cells. Recruitment of these patients is progressing.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
UCART19 can bridge to transplant in adults
LISBON—Preliminary data from a phase 1 trial suggest UCART19 can serve as a bridge to transplant in adults with relapsed/refractory (R/R) B-cell acute lymphoblastic leukemia (B-ALL).
This “universal,” donor-derived, chimeric antigen receptor (CAR) T-cell therapy produced complete responses (CRs) in 6 of 9 patients treated.
Five of the patients who were negative for minimal residual disease (MRD) proceeded to allogeneic hematopoietic stem cell transplant (allo-HSCT).
Two of the 5 patients were still alive and in MRD-negative remission at last follow-up, but 1 had relapsed and 2 died.
A total of 4 patients died in this trial—1 from a dose-limiting toxicity (DLT), 1 from progressive disease, 1 from infection, and 1 from pulmonary hemorrhage.
“These early results for UCART19 are very encouraging, both in terms of manageable safety and the impressive complete molecular remission rate in these hard-to-treat adult patients with R/R B-ALL,” said principal investigator Reuben Benjamin, MBBS, PhD, a consultant hematologist at King’s College London in the UK.
Dr Benjamin presented these results, from the CALM trial, at the 44th Annual Meeting of the EBMT (abstract OS10-4*).
The CALM trial is sponsored by Servier. In 2015, Servier acquired exclusive rights from Cellectis for UCART19, which is being co-developed by Servier and Pfizer.
Patients and treatment
Dr Benjamin presented results in 9 patients with R/R B-ALL who had a median age of 23 (range, 18-49).
All patients had morphological disease or an MRD level of at least 1 x 10-3 (via flow cytometry and/or qPCR) at baseline. The median disease burden was 8% (range, 0-95).
Four patients had received 1 to 3 prior therapies, and 5 had received 4 or more prior treatments. Six patients had prior inotuzumab ozogamicin, 2 had prior blinatumomab, and 7 had prior allo-HSCT. The median time to relapse after allo-HSCT was 5.9 months (range, 4.1-11).
Patients underwent lymphodepletion with fludarabine, cyclophosphamide, and alemtuzumab (n=8) or fludarabine and cyclophosphamide (n=1).
They received UCART19 at 2 dose levels—6 x 106 total cells (n=6) or 6 to 8 x 107 total cells (n=3).
Toxicity
There were 2 DLTs, 1 at each dose level. At the lower dose, the DLT was grade 4 cytokine release syndrome (CRS) associated with grade 5 neutropenic sepsis. The patient with this DLT died at day 15 post-infusion.
At the higher dose level, the DLT was grade 4 prolonged cytopenia associated with infection and pulmonary hemorrhage. This patient died at day 82 post-infusion, 19 days after undergoing allo-HSCT.
In all, 8 patients had CRS. One patient had grade 1, 6 had grade 2, and 1 had grade 4 CRS. Seven patients had complete resolution of CRS.
Two patients had neurotoxic events, both grade 1.
Three patients had prolonged cytopenia, all grade 4. This was defined as persistent neutropenia and/or thrombocytopenia beyond day 42 after UCART19 infusion, except if the patient had >5% bone marrow blasts.
Two patients had neutropenic sepsis, grade 4 and grade 5.
Three patients had cytomegalovirus infection, all grade 2. Two patients had adenovirus infection, grade 1 and grade 3.
One patient had grade 1 acute cutaneous graft-versus-host disease.
Efficacy
Six of 9 patients achieved a CR, and 5 were MRD-negative by flow cytometry or qPCR. All 5 patients proceeded to allo-HSCT.
After transplant, 2 patients were still MRD-negative at 8 months, 1 patient relapsed after 6 months, and 2 patients died while MRD-negative. The deaths were due to infection and pulmonary hemorrhage.
Two other deaths were due to a DLT (neutropenic sepsis associated with CRS) and progressive disease.
Of the 5 patients who are alive, 2 are still MRD-negative after allo-HSCT. One of these patients relapsed after the first UCART19 infusion, received a second infusion, and achieved an MRD-negative CR that enabled transplant.
The remaining 3 patients who are still alive did not undergo transplant. One of these patients relapsed after achieving MRD-positive remission, and 1 relapsed after MRD-negative remission. The third patient relapsed and received a second UCART19 infusion. This patient has yet to respond to the second infusion but has minimal follow-up.
Recruitment in this study is ongoing at the higher dose level—6 to 8 x 107 total cells.
*Data in the abstract were updated in the presentation.
LISBON—Preliminary data from a phase 1 trial suggest UCART19 can serve as a bridge to transplant in adults with relapsed/refractory (R/R) B-cell acute lymphoblastic leukemia (B-ALL).
This “universal,” donor-derived, chimeric antigen receptor (CAR) T-cell therapy produced complete responses (CRs) in 6 of 9 patients treated.
Five of the patients who were negative for minimal residual disease (MRD) proceeded to allogeneic hematopoietic stem cell transplant (allo-HSCT).
Two of the 5 patients were still alive and in MRD-negative remission at last follow-up, but 1 had relapsed and 2 died.
A total of 4 patients died in this trial—1 from a dose-limiting toxicity (DLT), 1 from progressive disease, 1 from infection, and 1 from pulmonary hemorrhage.
“These early results for UCART19 are very encouraging, both in terms of manageable safety and the impressive complete molecular remission rate in these hard-to-treat adult patients with R/R B-ALL,” said principal investigator Reuben Benjamin, MBBS, PhD, a consultant hematologist at King’s College London in the UK.
Dr Benjamin presented these results, from the CALM trial, at the 44th Annual Meeting of the EBMT (abstract OS10-4*).
The CALM trial is sponsored by Servier. In 2015, Servier acquired exclusive rights from Cellectis for UCART19, which is being co-developed by Servier and Pfizer.
Patients and treatment
Dr Benjamin presented results in 9 patients with R/R B-ALL who had a median age of 23 (range, 18-49).
All patients had morphological disease or an MRD level of at least 1 x 10-3 (via flow cytometry and/or qPCR) at baseline. The median disease burden was 8% (range, 0-95).
Four patients had received 1 to 3 prior therapies, and 5 had received 4 or more prior treatments. Six patients had prior inotuzumab ozogamicin, 2 had prior blinatumomab, and 7 had prior allo-HSCT. The median time to relapse after allo-HSCT was 5.9 months (range, 4.1-11).
Patients underwent lymphodepletion with fludarabine, cyclophosphamide, and alemtuzumab (n=8) or fludarabine and cyclophosphamide (n=1).
They received UCART19 at 2 dose levels—6 x 106 total cells (n=6) or 6 to 8 x 107 total cells (n=3).
Toxicity
There were 2 DLTs, 1 at each dose level. At the lower dose, the DLT was grade 4 cytokine release syndrome (CRS) associated with grade 5 neutropenic sepsis. The patient with this DLT died at day 15 post-infusion.
At the higher dose level, the DLT was grade 4 prolonged cytopenia associated with infection and pulmonary hemorrhage. This patient died at day 82 post-infusion, 19 days after undergoing allo-HSCT.
In all, 8 patients had CRS. One patient had grade 1, 6 had grade 2, and 1 had grade 4 CRS. Seven patients had complete resolution of CRS.
Two patients had neurotoxic events, both grade 1.
Three patients had prolonged cytopenia, all grade 4. This was defined as persistent neutropenia and/or thrombocytopenia beyond day 42 after UCART19 infusion, except if the patient had >5% bone marrow blasts.
Two patients had neutropenic sepsis, grade 4 and grade 5.
Three patients had cytomegalovirus infection, all grade 2. Two patients had adenovirus infection, grade 1 and grade 3.
One patient had grade 1 acute cutaneous graft-versus-host disease.
Efficacy
Six of 9 patients achieved a CR, and 5 were MRD-negative by flow cytometry or qPCR. All 5 patients proceeded to allo-HSCT.
After transplant, 2 patients were still MRD-negative at 8 months, 1 patient relapsed after 6 months, and 2 patients died while MRD-negative. The deaths were due to infection and pulmonary hemorrhage.
Two other deaths were due to a DLT (neutropenic sepsis associated with CRS) and progressive disease.
Of the 5 patients who are alive, 2 are still MRD-negative after allo-HSCT. One of these patients relapsed after the first UCART19 infusion, received a second infusion, and achieved an MRD-negative CR that enabled transplant.
The remaining 3 patients who are still alive did not undergo transplant. One of these patients relapsed after achieving MRD-positive remission, and 1 relapsed after MRD-negative remission. The third patient relapsed and received a second UCART19 infusion. This patient has yet to respond to the second infusion but has minimal follow-up.
Recruitment in this study is ongoing at the higher dose level—6 to 8 x 107 total cells.
*Data in the abstract were updated in the presentation.
LISBON—Preliminary data from a phase 1 trial suggest UCART19 can serve as a bridge to transplant in adults with relapsed/refractory (R/R) B-cell acute lymphoblastic leukemia (B-ALL).
This “universal,” donor-derived, chimeric antigen receptor (CAR) T-cell therapy produced complete responses (CRs) in 6 of 9 patients treated.
Five of the patients who were negative for minimal residual disease (MRD) proceeded to allogeneic hematopoietic stem cell transplant (allo-HSCT).
Two of the 5 patients were still alive and in MRD-negative remission at last follow-up, but 1 had relapsed and 2 died.
A total of 4 patients died in this trial—1 from a dose-limiting toxicity (DLT), 1 from progressive disease, 1 from infection, and 1 from pulmonary hemorrhage.
“These early results for UCART19 are very encouraging, both in terms of manageable safety and the impressive complete molecular remission rate in these hard-to-treat adult patients with R/R B-ALL,” said principal investigator Reuben Benjamin, MBBS, PhD, a consultant hematologist at King’s College London in the UK.
Dr Benjamin presented these results, from the CALM trial, at the 44th Annual Meeting of the EBMT (abstract OS10-4*).
The CALM trial is sponsored by Servier. In 2015, Servier acquired exclusive rights from Cellectis for UCART19, which is being co-developed by Servier and Pfizer.
Patients and treatment
Dr Benjamin presented results in 9 patients with R/R B-ALL who had a median age of 23 (range, 18-49).
All patients had morphological disease or an MRD level of at least 1 x 10-3 (via flow cytometry and/or qPCR) at baseline. The median disease burden was 8% (range, 0-95).
Four patients had received 1 to 3 prior therapies, and 5 had received 4 or more prior treatments. Six patients had prior inotuzumab ozogamicin, 2 had prior blinatumomab, and 7 had prior allo-HSCT. The median time to relapse after allo-HSCT was 5.9 months (range, 4.1-11).
Patients underwent lymphodepletion with fludarabine, cyclophosphamide, and alemtuzumab (n=8) or fludarabine and cyclophosphamide (n=1).
They received UCART19 at 2 dose levels—6 x 106 total cells (n=6) or 6 to 8 x 107 total cells (n=3).
Toxicity
There were 2 DLTs, 1 at each dose level. At the lower dose, the DLT was grade 4 cytokine release syndrome (CRS) associated with grade 5 neutropenic sepsis. The patient with this DLT died at day 15 post-infusion.
At the higher dose level, the DLT was grade 4 prolonged cytopenia associated with infection and pulmonary hemorrhage. This patient died at day 82 post-infusion, 19 days after undergoing allo-HSCT.
In all, 8 patients had CRS. One patient had grade 1, 6 had grade 2, and 1 had grade 4 CRS. Seven patients had complete resolution of CRS.
Two patients had neurotoxic events, both grade 1.
Three patients had prolonged cytopenia, all grade 4. This was defined as persistent neutropenia and/or thrombocytopenia beyond day 42 after UCART19 infusion, except if the patient had >5% bone marrow blasts.
Two patients had neutropenic sepsis, grade 4 and grade 5.
Three patients had cytomegalovirus infection, all grade 2. Two patients had adenovirus infection, grade 1 and grade 3.
One patient had grade 1 acute cutaneous graft-versus-host disease.
Efficacy
Six of 9 patients achieved a CR, and 5 were MRD-negative by flow cytometry or qPCR. All 5 patients proceeded to allo-HSCT.
After transplant, 2 patients were still MRD-negative at 8 months, 1 patient relapsed after 6 months, and 2 patients died while MRD-negative. The deaths were due to infection and pulmonary hemorrhage.
Two other deaths were due to a DLT (neutropenic sepsis associated with CRS) and progressive disease.
Of the 5 patients who are alive, 2 are still MRD-negative after allo-HSCT. One of these patients relapsed after the first UCART19 infusion, received a second infusion, and achieved an MRD-negative CR that enabled transplant.
The remaining 3 patients who are still alive did not undergo transplant. One of these patients relapsed after achieving MRD-positive remission, and 1 relapsed after MRD-negative remission. The third patient relapsed and received a second UCART19 infusion. This patient has yet to respond to the second infusion but has minimal follow-up.
Recruitment in this study is ongoing at the higher dose level—6 to 8 x 107 total cells.
*Data in the abstract were updated in the presentation.
Phase 1 results with UCART19 in kids
LISBON—Early results from a phase 1, pediatric trial of UCART19 expand upon results observed in children who received the therapy via a compassionate use program.
Two patients with relapsed/refractory B-cell acute lymphoblastic leukemia (B-ALL) received UCART19, a “universal,” donor-derived chimeric antigen receptor (CAR) T-cell therapy, via the program.
Both achieved remission and were still alive at last follow-up, more than 2 years after proceeding to transplant.
In the phase 1 trial, 5 of 6 B-ALL patients have achieved remission and gone on to transplant.
Three of the patients are still alive, and 2 are still negative for minimal residual disease (MRD) at 10 months and 11 months after UCART19 infusion.
However, 2 patients died of progression, and 1 died of transplant-related complications.
Paul Veys, MBBS, of Great Ormond Street Hospital (GOSH) in London, UK, presented these results, from the PALL trial, at the 44th Annual Meeting of the EBMT (abstract OS18-5*).
The trial is sponsored by Servier. In 2015, Servier acquired exclusive rights from Cellectis for UCART19, which is being co-developed by Servier and Pfizer.
Prior experience
Researchers previously reported results with UCART19 in 2 infants with relapsed/refractory B-ALL who had exhausted all other treatment options and received UCART19 via a compassionate use program.
Both patients achieved remission after UCART19 and proceeded to allogeneic hematopoietic stem cell transplant (allo-HSCT).
When these results were published, in January 2017, both patients were still alive and leukemia-free at last follow-up—12 months and 18 months after UCART19 infusion.
Dr Veys provided an update, noting that these patients were still alive and in remission at 24 months and 30 months after allo-HSCT.
Phase 1 patients and treatment
Thus far, the phase 1 trial has enrolled and treated 6 patients with relapsed B-ALL. They had a median age of 3.75 (range, 0.8-16.4).
All patients had morphological disease or an MRD level of at least 1 x 10-3 (via flow cytometry and/or qPCR) at baseline.
One patient had received 1 prior therapy, 2 had 3 prior therapies, and 3 had 4 or more prior therapies. Two patients had prior inotuzumab ozogamicin, and 2 had prior allo-HSCT. Both had relapsed within 6 months of allo-HSCT.
Five patients had less than 10% bone marrow blasts prior to lymphodepletion, and 1 had greater than 50% blasts.
Patients underwent lymphodepletion with fludarabine, cyclophosphamide, and alemtuzumab (n=5) or fludarabine and cyclophosphamide (n=1).
The patients received UCART19 at doses of 2 x 107 total cells or 1.1 to 2.3 x 106 cells/kg.
Toxicity
All 6 patients developed cytokine release syndrome (CRS), including grade 1 (n=1), grade 2 (n=4), and grade 3 (n-1) CRS. However, all 6 cases resolved completely.
Three patients had neurotoxic events, 2 grade 1 and 1 grade 2. One patient had grade 3 febrile neutropenia.
Three patients had grade 4 prolonged cytopenia. This was defined as persistent neutropenia and/or thrombocytopenia beyond day 42 after UCART19 infusion, except if the patient had >5% bone marrow blasts.
One patient had grade 1 adenovirus infection, 1 had grade 3 cytomegalovirus infection, 2 had grade 3 BK virus hemorrhagic cystitis, and 1 had grade 4 metapneumovirus infection.
One patient had grade 1 acute cutaneous graft-versus-host disease.
Efficacy
All 6 patients achieved a complete response at day 28 to 42 after UCART19 infusion. Five patients achieved MRD negativity according to flow cytometry, and 3 were MRD-negative according to PCR.
The 5 flow-MRD-negative patients went on to receive an allo-HSCT between 49 days and 62 days after UCART19 infusion. Conditioning consisted of total body irradiation and fludarabine, with or without cyclophosphamide and antithymocyte globulin. All of these patients received a dose of rituximab as well, which was intended to target any remaining UCART19 cells.
Two patients relapsed 3 months after transplant and died at 7 months and 8 months after UCART19 infusion. One of these patients was CD19-, and 1 was CD19+, but both were MRD-positive by PCR prior to receiving their transplant.
A third patient died 2.5 months after allo-HSCT from transplant-related complications, including thrombotic microangiopathy, BK hemorrhagic cystitis, and nephritis.
The remaining 3 patients are still alive at 1.5 months, 10 months, and 11 months after UCART19 infusion. Two are still MRD-negative, and 1 is MRD-positive. The MRD-positive patient has not undergone allo-HSCT.
*Data in the abstract were updated in the presentation.
LISBON—Early results from a phase 1, pediatric trial of UCART19 expand upon results observed in children who received the therapy via a compassionate use program.
Two patients with relapsed/refractory B-cell acute lymphoblastic leukemia (B-ALL) received UCART19, a “universal,” donor-derived chimeric antigen receptor (CAR) T-cell therapy, via the program.
Both achieved remission and were still alive at last follow-up, more than 2 years after proceeding to transplant.
In the phase 1 trial, 5 of 6 B-ALL patients have achieved remission and gone on to transplant.
Three of the patients are still alive, and 2 are still negative for minimal residual disease (MRD) at 10 months and 11 months after UCART19 infusion.
However, 2 patients died of progression, and 1 died of transplant-related complications.
Paul Veys, MBBS, of Great Ormond Street Hospital (GOSH) in London, UK, presented these results, from the PALL trial, at the 44th Annual Meeting of the EBMT (abstract OS18-5*).
The trial is sponsored by Servier. In 2015, Servier acquired exclusive rights from Cellectis for UCART19, which is being co-developed by Servier and Pfizer.
Prior experience
Researchers previously reported results with UCART19 in 2 infants with relapsed/refractory B-ALL who had exhausted all other treatment options and received UCART19 via a compassionate use program.
Both patients achieved remission after UCART19 and proceeded to allogeneic hematopoietic stem cell transplant (allo-HSCT).
When these results were published, in January 2017, both patients were still alive and leukemia-free at last follow-up—12 months and 18 months after UCART19 infusion.
Dr Veys provided an update, noting that these patients were still alive and in remission at 24 months and 30 months after allo-HSCT.
Phase 1 patients and treatment
Thus far, the phase 1 trial has enrolled and treated 6 patients with relapsed B-ALL. They had a median age of 3.75 (range, 0.8-16.4).
All patients had morphological disease or an MRD level of at least 1 x 10-3 (via flow cytometry and/or qPCR) at baseline.
One patient had received 1 prior therapy, 2 had 3 prior therapies, and 3 had 4 or more prior therapies. Two patients had prior inotuzumab ozogamicin, and 2 had prior allo-HSCT. Both had relapsed within 6 months of allo-HSCT.
Five patients had less than 10% bone marrow blasts prior to lymphodepletion, and 1 had greater than 50% blasts.
Patients underwent lymphodepletion with fludarabine, cyclophosphamide, and alemtuzumab (n=5) or fludarabine and cyclophosphamide (n=1).
The patients received UCART19 at doses of 2 x 107 total cells or 1.1 to 2.3 x 106 cells/kg.
Toxicity
All 6 patients developed cytokine release syndrome (CRS), including grade 1 (n=1), grade 2 (n=4), and grade 3 (n-1) CRS. However, all 6 cases resolved completely.
Three patients had neurotoxic events, 2 grade 1 and 1 grade 2. One patient had grade 3 febrile neutropenia.
Three patients had grade 4 prolonged cytopenia. This was defined as persistent neutropenia and/or thrombocytopenia beyond day 42 after UCART19 infusion, except if the patient had >5% bone marrow blasts.
One patient had grade 1 adenovirus infection, 1 had grade 3 cytomegalovirus infection, 2 had grade 3 BK virus hemorrhagic cystitis, and 1 had grade 4 metapneumovirus infection.
One patient had grade 1 acute cutaneous graft-versus-host disease.
Efficacy
All 6 patients achieved a complete response at day 28 to 42 after UCART19 infusion. Five patients achieved MRD negativity according to flow cytometry, and 3 were MRD-negative according to PCR.
The 5 flow-MRD-negative patients went on to receive an allo-HSCT between 49 days and 62 days after UCART19 infusion. Conditioning consisted of total body irradiation and fludarabine, with or without cyclophosphamide and antithymocyte globulin. All of these patients received a dose of rituximab as well, which was intended to target any remaining UCART19 cells.
Two patients relapsed 3 months after transplant and died at 7 months and 8 months after UCART19 infusion. One of these patients was CD19-, and 1 was CD19+, but both were MRD-positive by PCR prior to receiving their transplant.
A third patient died 2.5 months after allo-HSCT from transplant-related complications, including thrombotic microangiopathy, BK hemorrhagic cystitis, and nephritis.
The remaining 3 patients are still alive at 1.5 months, 10 months, and 11 months after UCART19 infusion. Two are still MRD-negative, and 1 is MRD-positive. The MRD-positive patient has not undergone allo-HSCT.
*Data in the abstract were updated in the presentation.
LISBON—Early results from a phase 1, pediatric trial of UCART19 expand upon results observed in children who received the therapy via a compassionate use program.
Two patients with relapsed/refractory B-cell acute lymphoblastic leukemia (B-ALL) received UCART19, a “universal,” donor-derived chimeric antigen receptor (CAR) T-cell therapy, via the program.
Both achieved remission and were still alive at last follow-up, more than 2 years after proceeding to transplant.
In the phase 1 trial, 5 of 6 B-ALL patients have achieved remission and gone on to transplant.
Three of the patients are still alive, and 2 are still negative for minimal residual disease (MRD) at 10 months and 11 months after UCART19 infusion.
However, 2 patients died of progression, and 1 died of transplant-related complications.
Paul Veys, MBBS, of Great Ormond Street Hospital (GOSH) in London, UK, presented these results, from the PALL trial, at the 44th Annual Meeting of the EBMT (abstract OS18-5*).
The trial is sponsored by Servier. In 2015, Servier acquired exclusive rights from Cellectis for UCART19, which is being co-developed by Servier and Pfizer.
Prior experience
Researchers previously reported results with UCART19 in 2 infants with relapsed/refractory B-ALL who had exhausted all other treatment options and received UCART19 via a compassionate use program.
Both patients achieved remission after UCART19 and proceeded to allogeneic hematopoietic stem cell transplant (allo-HSCT).
When these results were published, in January 2017, both patients were still alive and leukemia-free at last follow-up—12 months and 18 months after UCART19 infusion.
Dr Veys provided an update, noting that these patients were still alive and in remission at 24 months and 30 months after allo-HSCT.
Phase 1 patients and treatment
Thus far, the phase 1 trial has enrolled and treated 6 patients with relapsed B-ALL. They had a median age of 3.75 (range, 0.8-16.4).
All patients had morphological disease or an MRD level of at least 1 x 10-3 (via flow cytometry and/or qPCR) at baseline.
One patient had received 1 prior therapy, 2 had 3 prior therapies, and 3 had 4 or more prior therapies. Two patients had prior inotuzumab ozogamicin, and 2 had prior allo-HSCT. Both had relapsed within 6 months of allo-HSCT.
Five patients had less than 10% bone marrow blasts prior to lymphodepletion, and 1 had greater than 50% blasts.
Patients underwent lymphodepletion with fludarabine, cyclophosphamide, and alemtuzumab (n=5) or fludarabine and cyclophosphamide (n=1).
The patients received UCART19 at doses of 2 x 107 total cells or 1.1 to 2.3 x 106 cells/kg.
Toxicity
All 6 patients developed cytokine release syndrome (CRS), including grade 1 (n=1), grade 2 (n=4), and grade 3 (n-1) CRS. However, all 6 cases resolved completely.
Three patients had neurotoxic events, 2 grade 1 and 1 grade 2. One patient had grade 3 febrile neutropenia.
Three patients had grade 4 prolonged cytopenia. This was defined as persistent neutropenia and/or thrombocytopenia beyond day 42 after UCART19 infusion, except if the patient had >5% bone marrow blasts.
One patient had grade 1 adenovirus infection, 1 had grade 3 cytomegalovirus infection, 2 had grade 3 BK virus hemorrhagic cystitis, and 1 had grade 4 metapneumovirus infection.
One patient had grade 1 acute cutaneous graft-versus-host disease.
Efficacy
All 6 patients achieved a complete response at day 28 to 42 after UCART19 infusion. Five patients achieved MRD negativity according to flow cytometry, and 3 were MRD-negative according to PCR.
The 5 flow-MRD-negative patients went on to receive an allo-HSCT between 49 days and 62 days after UCART19 infusion. Conditioning consisted of total body irradiation and fludarabine, with or without cyclophosphamide and antithymocyte globulin. All of these patients received a dose of rituximab as well, which was intended to target any remaining UCART19 cells.
Two patients relapsed 3 months after transplant and died at 7 months and 8 months after UCART19 infusion. One of these patients was CD19-, and 1 was CD19+, but both were MRD-positive by PCR prior to receiving their transplant.
A third patient died 2.5 months after allo-HSCT from transplant-related complications, including thrombotic microangiopathy, BK hemorrhagic cystitis, and nephritis.
The remaining 3 patients are still alive at 1.5 months, 10 months, and 11 months after UCART19 infusion. Two are still MRD-negative, and 1 is MRD-positive. The MRD-positive patient has not undergone allo-HSCT.
*Data in the abstract were updated in the presentation.
Mortality in patients with PTLD
LISBON—A review of recent studies has revealed a “significant burden” of mortality related to post-transplant lymphoproliferative disorder (PTLD), according to researchers.
Of the 120 PTLD patients studied, 64% died and 42.5% died with PTLD.
The median time from hematopoietic stem cell transplant (HSCT) to the development of PTLD was about 9 weeks in children and 11 weeks in adults.
The median time from PTLD diagnosis to death was about 6 weeks in adults and 8 weeks in children.
These findings were presented at 44th Annual Meeting of the EBMT (abstract A219).
The research was funded by Atara Biotherapeutics, Inc., which is developing tabelecleucel (formerly ATA129), a T-cell immunotherapy intended to treat patients with Epstein-Barr virus-associated PTLD who have failed treatment with rituximab.
The review included 9 articles, published in 2005 and later, detailing studies of patients who developed PTLD after HSCT.
There were 120 patients. They had a mean age of 28.97, 67% were male, and 79% had received rituximab.
The 31 pediatric patients had a mean age of 9.84, 81% were male, and 74% had received rituximab. The 89 adult patients had a mean age of 35.63, 62% were male, and 81% had received rituximab.
Among the 16 pediatric patients with available data, the median time from HSCT to PTLD diagnosis was 65 days, and the mean was 138 days.
For the 59 adults with available data, the median time from HSCT to PTLD was 76 days, and the mean was 132 days.
The all-cause mortality rate was 64% in the entire population (77/120), 71% in children (22/31), and 62% in adults (55/89).
Overall, 42.5% of patients (51/120) died with PTLD—35.5% of children (11/31) and 44.9% of adults (40/89).
Among the patients who died with PTLD, the median time from PTLD diagnosis to death was 55 days for children and 40 days for adults. The mean time from PTLD to death was 71 days and 51 days, respectively.
There were 110 patients with available overall survival data. The median survival time from PTLD diagnosis was 116 days in the entire cohort, 153 days in children, and 92 days in adults.
“Patients with PTLD following [HSCT] experience high mortality rates under the current standard of care due to aggressive disease that often rapidly progresses to death after diagnosis,” said Chris Haqq, MD, PhD, of Atara Biotherapeutics.
“Children and relatively young adults in their prime working years are disproportionately affected. Atara is dedicated to progressing tab‑cel™ development in the ongoing phase 3 clinical studies to potentially address the compelling medical need for patients with this life-threatening condition.”
LISBON—A review of recent studies has revealed a “significant burden” of mortality related to post-transplant lymphoproliferative disorder (PTLD), according to researchers.
Of the 120 PTLD patients studied, 64% died and 42.5% died with PTLD.
The median time from hematopoietic stem cell transplant (HSCT) to the development of PTLD was about 9 weeks in children and 11 weeks in adults.
The median time from PTLD diagnosis to death was about 6 weeks in adults and 8 weeks in children.
These findings were presented at 44th Annual Meeting of the EBMT (abstract A219).
The research was funded by Atara Biotherapeutics, Inc., which is developing tabelecleucel (formerly ATA129), a T-cell immunotherapy intended to treat patients with Epstein-Barr virus-associated PTLD who have failed treatment with rituximab.
The review included 9 articles, published in 2005 and later, detailing studies of patients who developed PTLD after HSCT.
There were 120 patients. They had a mean age of 28.97, 67% were male, and 79% had received rituximab.
The 31 pediatric patients had a mean age of 9.84, 81% were male, and 74% had received rituximab. The 89 adult patients had a mean age of 35.63, 62% were male, and 81% had received rituximab.
Among the 16 pediatric patients with available data, the median time from HSCT to PTLD diagnosis was 65 days, and the mean was 138 days.
For the 59 adults with available data, the median time from HSCT to PTLD was 76 days, and the mean was 132 days.
The all-cause mortality rate was 64% in the entire population (77/120), 71% in children (22/31), and 62% in adults (55/89).
Overall, 42.5% of patients (51/120) died with PTLD—35.5% of children (11/31) and 44.9% of adults (40/89).
Among the patients who died with PTLD, the median time from PTLD diagnosis to death was 55 days for children and 40 days for adults. The mean time from PTLD to death was 71 days and 51 days, respectively.
There were 110 patients with available overall survival data. The median survival time from PTLD diagnosis was 116 days in the entire cohort, 153 days in children, and 92 days in adults.
“Patients with PTLD following [HSCT] experience high mortality rates under the current standard of care due to aggressive disease that often rapidly progresses to death after diagnosis,” said Chris Haqq, MD, PhD, of Atara Biotherapeutics.
“Children and relatively young adults in their prime working years are disproportionately affected. Atara is dedicated to progressing tab‑cel™ development in the ongoing phase 3 clinical studies to potentially address the compelling medical need for patients with this life-threatening condition.”
LISBON—A review of recent studies has revealed a “significant burden” of mortality related to post-transplant lymphoproliferative disorder (PTLD), according to researchers.
Of the 120 PTLD patients studied, 64% died and 42.5% died with PTLD.
The median time from hematopoietic stem cell transplant (HSCT) to the development of PTLD was about 9 weeks in children and 11 weeks in adults.
The median time from PTLD diagnosis to death was about 6 weeks in adults and 8 weeks in children.
These findings were presented at 44th Annual Meeting of the EBMT (abstract A219).
The research was funded by Atara Biotherapeutics, Inc., which is developing tabelecleucel (formerly ATA129), a T-cell immunotherapy intended to treat patients with Epstein-Barr virus-associated PTLD who have failed treatment with rituximab.
The review included 9 articles, published in 2005 and later, detailing studies of patients who developed PTLD after HSCT.
There were 120 patients. They had a mean age of 28.97, 67% were male, and 79% had received rituximab.
The 31 pediatric patients had a mean age of 9.84, 81% were male, and 74% had received rituximab. The 89 adult patients had a mean age of 35.63, 62% were male, and 81% had received rituximab.
Among the 16 pediatric patients with available data, the median time from HSCT to PTLD diagnosis was 65 days, and the mean was 138 days.
For the 59 adults with available data, the median time from HSCT to PTLD was 76 days, and the mean was 132 days.
The all-cause mortality rate was 64% in the entire population (77/120), 71% in children (22/31), and 62% in adults (55/89).
Overall, 42.5% of patients (51/120) died with PTLD—35.5% of children (11/31) and 44.9% of adults (40/89).
Among the patients who died with PTLD, the median time from PTLD diagnosis to death was 55 days for children and 40 days for adults. The mean time from PTLD to death was 71 days and 51 days, respectively.
There were 110 patients with available overall survival data. The median survival time from PTLD diagnosis was 116 days in the entire cohort, 153 days in children, and 92 days in adults.
“Patients with PTLD following [HSCT] experience high mortality rates under the current standard of care due to aggressive disease that often rapidly progresses to death after diagnosis,” said Chris Haqq, MD, PhD, of Atara Biotherapeutics.
“Children and relatively young adults in their prime working years are disproportionately affected. Atara is dedicated to progressing tab‑cel™ development in the ongoing phase 3 clinical studies to potentially address the compelling medical need for patients with this life-threatening condition.”
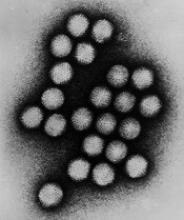
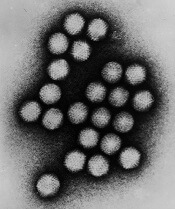
Kids may have higher rate of AdV infection after HSCT
LISBON—Results of a large study revealed a higher incidence of adenovirus (AdV) infection after allogeneic hematopoietic stem cell transplant (allo-HSCT) in children than adults.
The rate of AdV infection in the 6 months after allo-HSCT was 32% in children and 6% in adults.
However, researchers believe this data may be influenced by a lack of routine AdV screening in adults.
These findings—from the AdVance study—were reported at the 44th Annual Meeting of the EBMT as abstracts OS9-7 and B043.*
Other results from AdVance were also presented at the meeting, with mortality data reported as abstract OS9-8 and hospitalization data reported as abstract B073. The AdVance study was sponsored by Chimerix, Inc.
“The robust findings of the AdVance study are extremely important for transplant clinicians, as we seek to better understand the rates and clinical outcomes of adenovirus infection and assess ways to evaluate antiviral therapies,” said study investigator Marco Zecca, MD, of Fondazione IRCCS Policlinico San Matteo in Pavia, Italy.
AdVance is a multi-center, retrospective study of 4276 allo-HSCT recipients—1738 pediatric patients and 2538 adults. The patients underwent transplants at 50 centers in Europe from January 2013 to September 2015.
Abstract OS9-7: Incidence
Thirty-two percent (n=558) of pediatric patients developed an AdV infection in the first 6 months after allo-HSCT, and 23% (n=395) developed detectable AdV viremia. Fourteen percent (n=241) had AdV viremia ≥ 1000 copies/mL, a level previously associated with negative clinical outcomes.
Meanwhile, 6% (n=141) of adults had an AdV infection in the 6 months after transplant, 3% (n=77) developed AdV viremia, and 2% (n=39) had ≥ 1000 copies /mL.
Further analysis revealed that age, donor type, and use of T-cell depletion were independent predictors of AdV viremia ≥ 1000 copies/mL.
Older age was associated with a lower risk of AdV viremia ≥ 1000 copies/mL. There was a stepwise reduction in risk with increasing age (compared to ages 0-2, P=0.104 for ages 2-12, P=0.001 for ages 13-17, and P<0.0001 for ages 18-65+).
T-cell depletion was associated with an increased risk of AdV viremia ≥ 1000 copies/mL. Compared to no T-cell depletion, there was an increased risk for depletion with antithymocyte globulin (P=0.036) or alemtuzumab (P<0.0001) and for ex vivo depletion (P=0.002).
Compared to patients who received a matched related transplant, recipients of other transplants had an increased risk of AdV viremia ≥ 1000 copies/mL. This includes matched unrelated (P=0.016), cord blood (P=0.011), haploidentical (P=0.007), and mismatched (P<0.001) transplants.
Abstract B043: Screening
Dr Zecca and his colleagues believe the difference in AdV incidence between children and adults may have been affected by a lack of routine screening in adults.
To assess the use of screening, the investigators analyzed practice surveys from physicians at centers included in the AdVance study. There were 28 survey respondents who treat pediatric patients and 14 who treat adults.
All 28 physicians treating pediatric patients said there is routine AdV screening at their center. Ninety-three percent of these doctors said they routinely screen all pediatric allo-HSCT recipients for AdV infection. The remaining 7% said they screen patients considered to be at high-risk of AdV infection.
Thirty-six percent of the physicians treating adults (5/14) said they routinely screen for AdV, and 21% (3/14) said they routinely screen all of their adult allo-HSCT recipients for AdV infection.
Of the 11 doctors who said they did not routinely screen adult allo-HSCT recipients, some said they would screen recipients with a high-risk of AdV infection, such as those with graft-versus-host disease (4/11) or those who received haploidentical, mismatched, or cord blood transplants (3/11).
*Data in the abstracts differ from the presentations.
LISBON—Results of a large study revealed a higher incidence of adenovirus (AdV) infection after allogeneic hematopoietic stem cell transplant (allo-HSCT) in children than adults.
The rate of AdV infection in the 6 months after allo-HSCT was 32% in children and 6% in adults.
However, researchers believe this data may be influenced by a lack of routine AdV screening in adults.
These findings—from the AdVance study—were reported at the 44th Annual Meeting of the EBMT as abstracts OS9-7 and B043.*
Other results from AdVance were also presented at the meeting, with mortality data reported as abstract OS9-8 and hospitalization data reported as abstract B073. The AdVance study was sponsored by Chimerix, Inc.
“The robust findings of the AdVance study are extremely important for transplant clinicians, as we seek to better understand the rates and clinical outcomes of adenovirus infection and assess ways to evaluate antiviral therapies,” said study investigator Marco Zecca, MD, of Fondazione IRCCS Policlinico San Matteo in Pavia, Italy.
AdVance is a multi-center, retrospective study of 4276 allo-HSCT recipients—1738 pediatric patients and 2538 adults. The patients underwent transplants at 50 centers in Europe from January 2013 to September 2015.
Abstract OS9-7: Incidence
Thirty-two percent (n=558) of pediatric patients developed an AdV infection in the first 6 months after allo-HSCT, and 23% (n=395) developed detectable AdV viremia. Fourteen percent (n=241) had AdV viremia ≥ 1000 copies/mL, a level previously associated with negative clinical outcomes.
Meanwhile, 6% (n=141) of adults had an AdV infection in the 6 months after transplant, 3% (n=77) developed AdV viremia, and 2% (n=39) had ≥ 1000 copies /mL.
Further analysis revealed that age, donor type, and use of T-cell depletion were independent predictors of AdV viremia ≥ 1000 copies/mL.
Older age was associated with a lower risk of AdV viremia ≥ 1000 copies/mL. There was a stepwise reduction in risk with increasing age (compared to ages 0-2, P=0.104 for ages 2-12, P=0.001 for ages 13-17, and P<0.0001 for ages 18-65+).
T-cell depletion was associated with an increased risk of AdV viremia ≥ 1000 copies/mL. Compared to no T-cell depletion, there was an increased risk for depletion with antithymocyte globulin (P=0.036) or alemtuzumab (P<0.0001) and for ex vivo depletion (P=0.002).
Compared to patients who received a matched related transplant, recipients of other transplants had an increased risk of AdV viremia ≥ 1000 copies/mL. This includes matched unrelated (P=0.016), cord blood (P=0.011), haploidentical (P=0.007), and mismatched (P<0.001) transplants.
Abstract B043: Screening
Dr Zecca and his colleagues believe the difference in AdV incidence between children and adults may have been affected by a lack of routine screening in adults.
To assess the use of screening, the investigators analyzed practice surveys from physicians at centers included in the AdVance study. There were 28 survey respondents who treat pediatric patients and 14 who treat adults.
All 28 physicians treating pediatric patients said there is routine AdV screening at their center. Ninety-three percent of these doctors said they routinely screen all pediatric allo-HSCT recipients for AdV infection. The remaining 7% said they screen patients considered to be at high-risk of AdV infection.
Thirty-six percent of the physicians treating adults (5/14) said they routinely screen for AdV, and 21% (3/14) said they routinely screen all of their adult allo-HSCT recipients for AdV infection.
Of the 11 doctors who said they did not routinely screen adult allo-HSCT recipients, some said they would screen recipients with a high-risk of AdV infection, such as those with graft-versus-host disease (4/11) or those who received haploidentical, mismatched, or cord blood transplants (3/11).
*Data in the abstracts differ from the presentations.
LISBON—Results of a large study revealed a higher incidence of adenovirus (AdV) infection after allogeneic hematopoietic stem cell transplant (allo-HSCT) in children than adults.
The rate of AdV infection in the 6 months after allo-HSCT was 32% in children and 6% in adults.
However, researchers believe this data may be influenced by a lack of routine AdV screening in adults.
These findings—from the AdVance study—were reported at the 44th Annual Meeting of the EBMT as abstracts OS9-7 and B043.*
Other results from AdVance were also presented at the meeting, with mortality data reported as abstract OS9-8 and hospitalization data reported as abstract B073. The AdVance study was sponsored by Chimerix, Inc.
“The robust findings of the AdVance study are extremely important for transplant clinicians, as we seek to better understand the rates and clinical outcomes of adenovirus infection and assess ways to evaluate antiviral therapies,” said study investigator Marco Zecca, MD, of Fondazione IRCCS Policlinico San Matteo in Pavia, Italy.
AdVance is a multi-center, retrospective study of 4276 allo-HSCT recipients—1738 pediatric patients and 2538 adults. The patients underwent transplants at 50 centers in Europe from January 2013 to September 2015.
Abstract OS9-7: Incidence
Thirty-two percent (n=558) of pediatric patients developed an AdV infection in the first 6 months after allo-HSCT, and 23% (n=395) developed detectable AdV viremia. Fourteen percent (n=241) had AdV viremia ≥ 1000 copies/mL, a level previously associated with negative clinical outcomes.
Meanwhile, 6% (n=141) of adults had an AdV infection in the 6 months after transplant, 3% (n=77) developed AdV viremia, and 2% (n=39) had ≥ 1000 copies /mL.
Further analysis revealed that age, donor type, and use of T-cell depletion were independent predictors of AdV viremia ≥ 1000 copies/mL.
Older age was associated with a lower risk of AdV viremia ≥ 1000 copies/mL. There was a stepwise reduction in risk with increasing age (compared to ages 0-2, P=0.104 for ages 2-12, P=0.001 for ages 13-17, and P<0.0001 for ages 18-65+).
T-cell depletion was associated with an increased risk of AdV viremia ≥ 1000 copies/mL. Compared to no T-cell depletion, there was an increased risk for depletion with antithymocyte globulin (P=0.036) or alemtuzumab (P<0.0001) and for ex vivo depletion (P=0.002).
Compared to patients who received a matched related transplant, recipients of other transplants had an increased risk of AdV viremia ≥ 1000 copies/mL. This includes matched unrelated (P=0.016), cord blood (P=0.011), haploidentical (P=0.007), and mismatched (P<0.001) transplants.
Abstract B043: Screening
Dr Zecca and his colleagues believe the difference in AdV incidence between children and adults may have been affected by a lack of routine screening in adults.
To assess the use of screening, the investigators analyzed practice surveys from physicians at centers included in the AdVance study. There were 28 survey respondents who treat pediatric patients and 14 who treat adults.
All 28 physicians treating pediatric patients said there is routine AdV screening at their center. Ninety-three percent of these doctors said they routinely screen all pediatric allo-HSCT recipients for AdV infection. The remaining 7% said they screen patients considered to be at high-risk of AdV infection.
Thirty-six percent of the physicians treating adults (5/14) said they routinely screen for AdV, and 21% (3/14) said they routinely screen all of their adult allo-HSCT recipients for AdV infection.
Of the 11 doctors who said they did not routinely screen adult allo-HSCT recipients, some said they would screen recipients with a high-risk of AdV infection, such as those with graft-versus-host disease (4/11) or those who received haploidentical, mismatched, or cord blood transplants (3/11).
*Data in the abstracts differ from the presentations.
AdV viral burden linked to mortality in kids
LISBON—Data from the AdVance study revealed a “strong correlation” between adenovirus (AdV) viral load and mortality in pediatric recipients of allogeneic hematopoietic stem cell transplant (allo-HSCT), according to researchers.
The team found that patients with the highest AdV viral burden had roughly 12 times the risk of all-cause mortality as patients with the lowest viral burden.
These findings were presented at the 44th Annual Meeting of the EBMT (abstract OS9-8).*
Other findings from AdVance were also reported at the meeting (abstracts OS9-7 and B043 as well as B073). The study was sponsored by Chimerix, Inc.
AdVance is a multi-center, retrospective study of 4276 allo-HSCT recipients, including 1738 pediatric patients. The patients underwent transplants at 50 centers in Europe from January 2013 to September 2015.
Thirty-two percent (n=558) of pediatric patients developed an AdV infection in the first 6 months after allo-HSCT. Twenty-three percent (n=395) developed detectable AdV viremia, and 14% (n=241) had AdV viremia ≥ 1000 copies/mL.
The researchers assessed AdV plasma viral burden, measured by time-averaged area under the curve (AAUC) over 16 weeks from the time of viremia ≥ 1000 copies/mL, and its correlation with all-cause mortality.
“[T]he highest mortality was observed in those with the greatest adenovirus burden,” said AdVance investigator Marco Zecca, MD, of Fondazione IRCCS Policlinico San Matteo in Pavia, Italy.
He and his colleagues divided patients into 4 quartiles according to AdV AAUC, with the third and fourth quartiles reflecting higher, more prolonged AdV viremia.
Rates of all-cause mortality at 6 months (from the first viremia ≥ 1000 copies/mL) were 52% in the fourth quartile, 10% in the third, 7% in the second, and 3% in the first quartile.
Forty percent of patients in the fourth quartile died within 2 months of transplant.
The hazard ratio for mortality was 11.7 in the fourth quartile, 2.7 in the third, and 1.5 in the second, with the first quartile as the reference.
“These data suggest that AdV AAUC is an appropriate endpoint to assess the potential benefits of antiviral therapies for the treatment of adenovirus,” Dr Zecca concluded.
*Data in the abstract differ from the presentation.
LISBON—Data from the AdVance study revealed a “strong correlation” between adenovirus (AdV) viral load and mortality in pediatric recipients of allogeneic hematopoietic stem cell transplant (allo-HSCT), according to researchers.
The team found that patients with the highest AdV viral burden had roughly 12 times the risk of all-cause mortality as patients with the lowest viral burden.
These findings were presented at the 44th Annual Meeting of the EBMT (abstract OS9-8).*
Other findings from AdVance were also reported at the meeting (abstracts OS9-7 and B043 as well as B073). The study was sponsored by Chimerix, Inc.
AdVance is a multi-center, retrospective study of 4276 allo-HSCT recipients, including 1738 pediatric patients. The patients underwent transplants at 50 centers in Europe from January 2013 to September 2015.
Thirty-two percent (n=558) of pediatric patients developed an AdV infection in the first 6 months after allo-HSCT. Twenty-three percent (n=395) developed detectable AdV viremia, and 14% (n=241) had AdV viremia ≥ 1000 copies/mL.
The researchers assessed AdV plasma viral burden, measured by time-averaged area under the curve (AAUC) over 16 weeks from the time of viremia ≥ 1000 copies/mL, and its correlation with all-cause mortality.
“[T]he highest mortality was observed in those with the greatest adenovirus burden,” said AdVance investigator Marco Zecca, MD, of Fondazione IRCCS Policlinico San Matteo in Pavia, Italy.
He and his colleagues divided patients into 4 quartiles according to AdV AAUC, with the third and fourth quartiles reflecting higher, more prolonged AdV viremia.
Rates of all-cause mortality at 6 months (from the first viremia ≥ 1000 copies/mL) were 52% in the fourth quartile, 10% in the third, 7% in the second, and 3% in the first quartile.
Forty percent of patients in the fourth quartile died within 2 months of transplant.
The hazard ratio for mortality was 11.7 in the fourth quartile, 2.7 in the third, and 1.5 in the second, with the first quartile as the reference.
“These data suggest that AdV AAUC is an appropriate endpoint to assess the potential benefits of antiviral therapies for the treatment of adenovirus,” Dr Zecca concluded.
*Data in the abstract differ from the presentation.
LISBON—Data from the AdVance study revealed a “strong correlation” between adenovirus (AdV) viral load and mortality in pediatric recipients of allogeneic hematopoietic stem cell transplant (allo-HSCT), according to researchers.
The team found that patients with the highest AdV viral burden had roughly 12 times the risk of all-cause mortality as patients with the lowest viral burden.
These findings were presented at the 44th Annual Meeting of the EBMT (abstract OS9-8).*
Other findings from AdVance were also reported at the meeting (abstracts OS9-7 and B043 as well as B073). The study was sponsored by Chimerix, Inc.
AdVance is a multi-center, retrospective study of 4276 allo-HSCT recipients, including 1738 pediatric patients. The patients underwent transplants at 50 centers in Europe from January 2013 to September 2015.
Thirty-two percent (n=558) of pediatric patients developed an AdV infection in the first 6 months after allo-HSCT. Twenty-three percent (n=395) developed detectable AdV viremia, and 14% (n=241) had AdV viremia ≥ 1000 copies/mL.
The researchers assessed AdV plasma viral burden, measured by time-averaged area under the curve (AAUC) over 16 weeks from the time of viremia ≥ 1000 copies/mL, and its correlation with all-cause mortality.
“[T]he highest mortality was observed in those with the greatest adenovirus burden,” said AdVance investigator Marco Zecca, MD, of Fondazione IRCCS Policlinico San Matteo in Pavia, Italy.
He and his colleagues divided patients into 4 quartiles according to AdV AAUC, with the third and fourth quartiles reflecting higher, more prolonged AdV viremia.
Rates of all-cause mortality at 6 months (from the first viremia ≥ 1000 copies/mL) were 52% in the fourth quartile, 10% in the third, 7% in the second, and 3% in the first quartile.
Forty percent of patients in the fourth quartile died within 2 months of transplant.
The hazard ratio for mortality was 11.7 in the fourth quartile, 2.7 in the third, and 1.5 in the second, with the first quartile as the reference.
“These data suggest that AdV AAUC is an appropriate endpoint to assess the potential benefits of antiviral therapies for the treatment of adenovirus,” Dr Zecca concluded.
*Data in the abstract differ from the presentation.
Manufactured graft deemed safe in blood cancer patients
LISBON—Phase 1 results suggest a programmed cellular therapy is safe for use in patients with hematologic malignancies.
The therapy, ProTmune, is being developed as a next-generation allogeneic graft intended to reduce the incidence and severity of acute graft-versus-host disease (GVHD) after hematopoietic stem cell transplant (HSCT).
Three of 7 patients who received ProTmune in this trial did develop acute GVHD, and 2 patients died.
However, the remaining 5 patients were still alive and disease-free at last follow-up.
There were no serious adverse events (AEs) attributed to ProTmune. The most common AEs were nausea, vomiting, and chest pain.
These results were presented at the 44th Annual Meeting of the EBMT (abstract A401*).
The trial, known as PROTECT, is sponsored by Fate Therapeutics, the company developing ProTmune.
The phase 1 portion of PROTECT enrolled 7 adults with hematologic malignancies—1 with myelodysplastic syndrome, 3 with acute lymphoblastic leukemia, and 3 with acute myeloid leukemia.
Patients were set to undergo matched, unrelated donor HSCT and received ProTmune as the graft. ProTmune is manufactured by modulating a mobilized peripheral blood graft with 2 small molecules, FT1050 and FT4145.
The patients ranged in age from 34 to 69, and most (n=5) were female. For conditioning, patients received fludarabine/busulfan (n=1), busulfan/cyclophosphamide (n=1), fludarabine/melphalan (n=3), or cyclophosphamide/total body irradiation (n=2).
Results
The data cut-off was February 26, 2018. The median time on study was 228 days (range, 151 to 353).
None of the patients had graft failure. The median time to neutrophil engraftment was 18 days (range, 14 to 22).
Three patients had acute GVHD at day 100 after HSCT. Two patients had grade 2 skin GVHD, and 1 had grade 3 GVHD in the skin and gut.
All 3 patients responded to steroid treatment. GVHD resolved in 5 days for the patient with grade 3 GVHD. For the grade 2 patients, GVHD resolved in 7 days and 8 days, respectively.
None of the patients relapsed, but 2 died—1 of pulmonary edema and 1 of atrial fibrillation.
AEs related to ProTmune included grade 1 vomiting (n=2), grade 2 nausea (n=2), and grade 2 chest pain (n=1).
Phase 2
The phase 2 portion of PROTECT is ongoing. This is a randomized, controlled, double-blinded trial designed to assess the safety and efficacy of ProTmune in up to 60 adults with hematologic malignancies undergoing matched, unrelated donor HSCT following myeloablative conditioning.
Patients are being randomized, in a 1:1 ratio, to receive either ProTmune or a conventional, mobilized peripheral blood cell graft from a matched, unrelated donor.
The primary efficacy endpoint is the cumulative incidence of grade 2-4 acute GVHD by day 100 post-HSCT. Rates of chronic GVHD, cancer relapse, disease-free survival, and overall survival are also being assessed.
*Some data in the abstract differ from the presentation.
LISBON—Phase 1 results suggest a programmed cellular therapy is safe for use in patients with hematologic malignancies.
The therapy, ProTmune, is being developed as a next-generation allogeneic graft intended to reduce the incidence and severity of acute graft-versus-host disease (GVHD) after hematopoietic stem cell transplant (HSCT).
Three of 7 patients who received ProTmune in this trial did develop acute GVHD, and 2 patients died.
However, the remaining 5 patients were still alive and disease-free at last follow-up.
There were no serious adverse events (AEs) attributed to ProTmune. The most common AEs were nausea, vomiting, and chest pain.
These results were presented at the 44th Annual Meeting of the EBMT (abstract A401*).
The trial, known as PROTECT, is sponsored by Fate Therapeutics, the company developing ProTmune.
The phase 1 portion of PROTECT enrolled 7 adults with hematologic malignancies—1 with myelodysplastic syndrome, 3 with acute lymphoblastic leukemia, and 3 with acute myeloid leukemia.
Patients were set to undergo matched, unrelated donor HSCT and received ProTmune as the graft. ProTmune is manufactured by modulating a mobilized peripheral blood graft with 2 small molecules, FT1050 and FT4145.
The patients ranged in age from 34 to 69, and most (n=5) were female. For conditioning, patients received fludarabine/busulfan (n=1), busulfan/cyclophosphamide (n=1), fludarabine/melphalan (n=3), or cyclophosphamide/total body irradiation (n=2).
Results
The data cut-off was February 26, 2018. The median time on study was 228 days (range, 151 to 353).
None of the patients had graft failure. The median time to neutrophil engraftment was 18 days (range, 14 to 22).
Three patients had acute GVHD at day 100 after HSCT. Two patients had grade 2 skin GVHD, and 1 had grade 3 GVHD in the skin and gut.
All 3 patients responded to steroid treatment. GVHD resolved in 5 days for the patient with grade 3 GVHD. For the grade 2 patients, GVHD resolved in 7 days and 8 days, respectively.
None of the patients relapsed, but 2 died—1 of pulmonary edema and 1 of atrial fibrillation.
AEs related to ProTmune included grade 1 vomiting (n=2), grade 2 nausea (n=2), and grade 2 chest pain (n=1).
Phase 2
The phase 2 portion of PROTECT is ongoing. This is a randomized, controlled, double-blinded trial designed to assess the safety and efficacy of ProTmune in up to 60 adults with hematologic malignancies undergoing matched, unrelated donor HSCT following myeloablative conditioning.
Patients are being randomized, in a 1:1 ratio, to receive either ProTmune or a conventional, mobilized peripheral blood cell graft from a matched, unrelated donor.
The primary efficacy endpoint is the cumulative incidence of grade 2-4 acute GVHD by day 100 post-HSCT. Rates of chronic GVHD, cancer relapse, disease-free survival, and overall survival are also being assessed.
*Some data in the abstract differ from the presentation.
LISBON—Phase 1 results suggest a programmed cellular therapy is safe for use in patients with hematologic malignancies.
The therapy, ProTmune, is being developed as a next-generation allogeneic graft intended to reduce the incidence and severity of acute graft-versus-host disease (GVHD) after hematopoietic stem cell transplant (HSCT).
Three of 7 patients who received ProTmune in this trial did develop acute GVHD, and 2 patients died.
However, the remaining 5 patients were still alive and disease-free at last follow-up.
There were no serious adverse events (AEs) attributed to ProTmune. The most common AEs were nausea, vomiting, and chest pain.
These results were presented at the 44th Annual Meeting of the EBMT (abstract A401*).
The trial, known as PROTECT, is sponsored by Fate Therapeutics, the company developing ProTmune.
The phase 1 portion of PROTECT enrolled 7 adults with hematologic malignancies—1 with myelodysplastic syndrome, 3 with acute lymphoblastic leukemia, and 3 with acute myeloid leukemia.
Patients were set to undergo matched, unrelated donor HSCT and received ProTmune as the graft. ProTmune is manufactured by modulating a mobilized peripheral blood graft with 2 small molecules, FT1050 and FT4145.
The patients ranged in age from 34 to 69, and most (n=5) were female. For conditioning, patients received fludarabine/busulfan (n=1), busulfan/cyclophosphamide (n=1), fludarabine/melphalan (n=3), or cyclophosphamide/total body irradiation (n=2).
Results
The data cut-off was February 26, 2018. The median time on study was 228 days (range, 151 to 353).
None of the patients had graft failure. The median time to neutrophil engraftment was 18 days (range, 14 to 22).
Three patients had acute GVHD at day 100 after HSCT. Two patients had grade 2 skin GVHD, and 1 had grade 3 GVHD in the skin and gut.
All 3 patients responded to steroid treatment. GVHD resolved in 5 days for the patient with grade 3 GVHD. For the grade 2 patients, GVHD resolved in 7 days and 8 days, respectively.
None of the patients relapsed, but 2 died—1 of pulmonary edema and 1 of atrial fibrillation.
AEs related to ProTmune included grade 1 vomiting (n=2), grade 2 nausea (n=2), and grade 2 chest pain (n=1).
Phase 2
The phase 2 portion of PROTECT is ongoing. This is a randomized, controlled, double-blinded trial designed to assess the safety and efficacy of ProTmune in up to 60 adults with hematologic malignancies undergoing matched, unrelated donor HSCT following myeloablative conditioning.
Patients are being randomized, in a 1:1 ratio, to receive either ProTmune or a conventional, mobilized peripheral blood cell graft from a matched, unrelated donor.
The primary efficacy endpoint is the cumulative incidence of grade 2-4 acute GVHD by day 100 post-HSCT. Rates of chronic GVHD, cancer relapse, disease-free survival, and overall survival are also being assessed.
*Some data in the abstract differ from the presentation.
GPS consolidation may prolong PFS after ASCT
LISBON—Post-transplant therapy including galinpepimut-S (GPS) may prolong progression-free survival (PFS) in patients with high-risk multiple myeloma (MM), according to new research.
In a phase 2 trial, MM patients who received GPS and lenalidomide or bortezomib after autologous stem cell transplant (ASCT) had a median PFS of 23.6 months.
“Currently, post-transplant maintenance therapies for these difficult-to-treat patients are seemingly limited, with PFS rarely exceeding 12 to 14 months,” said Guenther Koehne, MD, PhD, from Miami Cancer Institute of Baptist Health South Florida.
Dr Koehne presented results observed with lenalidomide/bortezomib maintenance plus GPS consolidation at the 44th Annual Meeting of the EBMT (abstract OS4-6).
The trial was supported by the Leo A. Guthart and Kathryn Medina Research Fund and SELLAS Life Sciences Group, the company developing GPS.
The study enrolled 19 MM patients. Fifteen of them had high-risk cytogenetics at diagnosis, and 18 were at least minimal residual disease-positive after ASCT.
The goal of GPS therapy was to stimulate an immune response to prevent or delay MM progression. GPS is a cancer immunotherapeutic consisting of 4 modified peptide chains that induce an innate immune response against the WT1 antigen.
Patients began receiving GPS within 22 days of ASCT. They received 6 doses, administered subcutaneously with the oil emulsifier montanide every 2 weeks. Injection sites were pre-stimulated with granulocyte-macrophage colony-stimulating factor (70 μg) on days -2 (± 1 day) and 0 of each GPS vaccination.
The patients underwent clinical, immune response, and correlative assessment 2 to 4 weeks after the 6th GPS dose. Then, they received 6 additional monthly doses of GPS as well as lenalidomide (n=18) or bortezomib (n=1) maintenance, starting on day 100 post-ASCT. They underwent clinical, immune response, and correlative assessment again, 2 to 4 weeks after the 12th GPS dose.
Results
Dr Koehne said GPS stimulated time-dependent CD4+ or CD8+ T-cell immune responses specific for all 4 WT1 peptides within GPS, 2 of which are heteroclitic.
Immune responses were confirmed in up to 91% of patients, with multivalent immune responses in up to 64% of patients. And 75% of patients had multifunctional cross-epitope T-cell reactivity to antigenic epitopes against which the hosts were not specifically immunized, in a pattern akin to epitope spreading.
Dr Koehne also said immune responses were linked to clinical activity. In patients who received all 12 doses of GPS (n=12), there was a “strong and bidirectional association” between clinical benefit—defined as complete response (CR) or very good partial response (VGPR)—and frequency of CD4/CD8 immune responses.
Of those patients who had achieved CR/VGPR upon completion of GPS treatment, 100% (n=11) had CD4 immune responses and 81.8% (n=9) had CD8 immune responses.
Among patients who maintained immune response positivity, the CR/VGPR rate was 54.6% if CD4 immune response positivity to any of the 4 native GPS peptides was maintained and 44.0% if CD8 immune response positivity to any of the 4 native GPS peptides was maintained.
The PFS was 81% at 12 months and 62% at 18 months. The median PFS was 23.6 months (range, 15.2 to not reached).
The overall survival was 88% at 18 months, and the median overall survival was not reached.
LISBON—Post-transplant therapy including galinpepimut-S (GPS) may prolong progression-free survival (PFS) in patients with high-risk multiple myeloma (MM), according to new research.
In a phase 2 trial, MM patients who received GPS and lenalidomide or bortezomib after autologous stem cell transplant (ASCT) had a median PFS of 23.6 months.
“Currently, post-transplant maintenance therapies for these difficult-to-treat patients are seemingly limited, with PFS rarely exceeding 12 to 14 months,” said Guenther Koehne, MD, PhD, from Miami Cancer Institute of Baptist Health South Florida.
Dr Koehne presented results observed with lenalidomide/bortezomib maintenance plus GPS consolidation at the 44th Annual Meeting of the EBMT (abstract OS4-6).
The trial was supported by the Leo A. Guthart and Kathryn Medina Research Fund and SELLAS Life Sciences Group, the company developing GPS.
The study enrolled 19 MM patients. Fifteen of them had high-risk cytogenetics at diagnosis, and 18 were at least minimal residual disease-positive after ASCT.
The goal of GPS therapy was to stimulate an immune response to prevent or delay MM progression. GPS is a cancer immunotherapeutic consisting of 4 modified peptide chains that induce an innate immune response against the WT1 antigen.
Patients began receiving GPS within 22 days of ASCT. They received 6 doses, administered subcutaneously with the oil emulsifier montanide every 2 weeks. Injection sites were pre-stimulated with granulocyte-macrophage colony-stimulating factor (70 μg) on days -2 (± 1 day) and 0 of each GPS vaccination.
The patients underwent clinical, immune response, and correlative assessment 2 to 4 weeks after the 6th GPS dose. Then, they received 6 additional monthly doses of GPS as well as lenalidomide (n=18) or bortezomib (n=1) maintenance, starting on day 100 post-ASCT. They underwent clinical, immune response, and correlative assessment again, 2 to 4 weeks after the 12th GPS dose.
Results
Dr Koehne said GPS stimulated time-dependent CD4+ or CD8+ T-cell immune responses specific for all 4 WT1 peptides within GPS, 2 of which are heteroclitic.
Immune responses were confirmed in up to 91% of patients, with multivalent immune responses in up to 64% of patients. And 75% of patients had multifunctional cross-epitope T-cell reactivity to antigenic epitopes against which the hosts were not specifically immunized, in a pattern akin to epitope spreading.
Dr Koehne also said immune responses were linked to clinical activity. In patients who received all 12 doses of GPS (n=12), there was a “strong and bidirectional association” between clinical benefit—defined as complete response (CR) or very good partial response (VGPR)—and frequency of CD4/CD8 immune responses.
Of those patients who had achieved CR/VGPR upon completion of GPS treatment, 100% (n=11) had CD4 immune responses and 81.8% (n=9) had CD8 immune responses.
Among patients who maintained immune response positivity, the CR/VGPR rate was 54.6% if CD4 immune response positivity to any of the 4 native GPS peptides was maintained and 44.0% if CD8 immune response positivity to any of the 4 native GPS peptides was maintained.
The PFS was 81% at 12 months and 62% at 18 months. The median PFS was 23.6 months (range, 15.2 to not reached).
The overall survival was 88% at 18 months, and the median overall survival was not reached.
LISBON—Post-transplant therapy including galinpepimut-S (GPS) may prolong progression-free survival (PFS) in patients with high-risk multiple myeloma (MM), according to new research.
In a phase 2 trial, MM patients who received GPS and lenalidomide or bortezomib after autologous stem cell transplant (ASCT) had a median PFS of 23.6 months.
“Currently, post-transplant maintenance therapies for these difficult-to-treat patients are seemingly limited, with PFS rarely exceeding 12 to 14 months,” said Guenther Koehne, MD, PhD, from Miami Cancer Institute of Baptist Health South Florida.
Dr Koehne presented results observed with lenalidomide/bortezomib maintenance plus GPS consolidation at the 44th Annual Meeting of the EBMT (abstract OS4-6).
The trial was supported by the Leo A. Guthart and Kathryn Medina Research Fund and SELLAS Life Sciences Group, the company developing GPS.
The study enrolled 19 MM patients. Fifteen of them had high-risk cytogenetics at diagnosis, and 18 were at least minimal residual disease-positive after ASCT.
The goal of GPS therapy was to stimulate an immune response to prevent or delay MM progression. GPS is a cancer immunotherapeutic consisting of 4 modified peptide chains that induce an innate immune response against the WT1 antigen.
Patients began receiving GPS within 22 days of ASCT. They received 6 doses, administered subcutaneously with the oil emulsifier montanide every 2 weeks. Injection sites were pre-stimulated with granulocyte-macrophage colony-stimulating factor (70 μg) on days -2 (± 1 day) and 0 of each GPS vaccination.
The patients underwent clinical, immune response, and correlative assessment 2 to 4 weeks after the 6th GPS dose. Then, they received 6 additional monthly doses of GPS as well as lenalidomide (n=18) or bortezomib (n=1) maintenance, starting on day 100 post-ASCT. They underwent clinical, immune response, and correlative assessment again, 2 to 4 weeks after the 12th GPS dose.
Results
Dr Koehne said GPS stimulated time-dependent CD4+ or CD8+ T-cell immune responses specific for all 4 WT1 peptides within GPS, 2 of which are heteroclitic.
Immune responses were confirmed in up to 91% of patients, with multivalent immune responses in up to 64% of patients. And 75% of patients had multifunctional cross-epitope T-cell reactivity to antigenic epitopes against which the hosts were not specifically immunized, in a pattern akin to epitope spreading.
Dr Koehne also said immune responses were linked to clinical activity. In patients who received all 12 doses of GPS (n=12), there was a “strong and bidirectional association” between clinical benefit—defined as complete response (CR) or very good partial response (VGPR)—and frequency of CD4/CD8 immune responses.
Of those patients who had achieved CR/VGPR upon completion of GPS treatment, 100% (n=11) had CD4 immune responses and 81.8% (n=9) had CD8 immune responses.
Among patients who maintained immune response positivity, the CR/VGPR rate was 54.6% if CD4 immune response positivity to any of the 4 native GPS peptides was maintained and 44.0% if CD8 immune response positivity to any of the 4 native GPS peptides was maintained.
The PFS was 81% at 12 months and 62% at 18 months. The median PFS was 23.6 months (range, 15.2 to not reached).
The overall survival was 88% at 18 months, and the median overall survival was not reached.