User login
Ixazomib improves PFS after ASCT in MM
SAN DIEGO—Ixazomib improved progression-free survival (PFS) following autologous stem cell transplant (ASCT) in patients with newly diagnosed multiple myeloma (MM) in the TOURMALINE-MM3 trial.
The oral proteasome inhibitor improved PFS by 39% compared to placebo.
In addition, treatment with ixazomib was well tolerated, and there was a low discontinuation rate.
TOURMALINE-MM3 is the first-ever randomized, double-blind, placebo-controlled study of a proteasome inhibitor used as maintenance after ASCT, according to Meletios A. Dimopoulos, MD, of the National and Kapodistrian University of Athens in Greece.
Dr. Dimopoulos presented results from the trial at the 2018 ASH Annual Meeting (abstract 301).
He said the results suggest ixazomib represents a new treatment option for maintenance after ASCT in MM.
“Proteasome inhibitors have a different mechanism of action and may provide an alternative to lenalidomide,” Dr. Dimopoulos said.
He noted that ixazomib has a manageable toxicity profile and “convenient” weekly oral dosing, making it “well suited” for maintenance.
The TOURMALINE-MM3 study (NCT02181413) included 656 MM patients randomized post-ASCT to receive weekly ixazomib or placebo for up to 2 years.
The median PFS was 26.5 months for ixazomib and 21.3 months for placebo (hazard ratio=0.720; 95% confidence interval, 0.582-0.890; P=0.002).
At a median follow-up of 31 months, the median overall survival has not been reached in either treatment arm.
The discontinuation rate due to adverse events was 7% for ixazomib and 5% for placebo.
Ixazomib was associated with “low toxicity,” Dr Dimopoulos said, and there was no difference in the rates of new primary malignancies, at 3% in both arms.
When asked by an attendee whether ixazomib would become the standard of care for younger MM patients in this setting, Dr. Dimopoulos said the results show that ixazomib “is an option for patients, especially for those where a physician may believe that a proteasome inhibitor may be indicated.”
However, when pressed to comment on how ixazomib compares with lenalidomide for maintenance, Dr. Dimopoulos remarked that current maintenance studies are moving in the direction of combining therapies.
“I think that instead of saying, ‘Is ixazomib better than lenalidomide or vice-versa,’ it is better to see how one may combine those drugs in subsets of patients or even combine these drugs with other agents,” he said.
A manuscript describing results of the TOURMALINE-MM3 study is in press at The Lancet, with an expected online publication date of December 10, Dr. Dimopoulos said.
TOURMALINE-MM3 is sponsored by Takeda (Millennium), the maker of ixazomib.
Dr. Dimopoulos reported honoraria and consultancy with Janssen, Takeda Pharmaceuticals, Amgen, Bristol-Myers Squibb, and Celgene.
SAN DIEGO—Ixazomib improved progression-free survival (PFS) following autologous stem cell transplant (ASCT) in patients with newly diagnosed multiple myeloma (MM) in the TOURMALINE-MM3 trial.
The oral proteasome inhibitor improved PFS by 39% compared to placebo.
In addition, treatment with ixazomib was well tolerated, and there was a low discontinuation rate.
TOURMALINE-MM3 is the first-ever randomized, double-blind, placebo-controlled study of a proteasome inhibitor used as maintenance after ASCT, according to Meletios A. Dimopoulos, MD, of the National and Kapodistrian University of Athens in Greece.
Dr. Dimopoulos presented results from the trial at the 2018 ASH Annual Meeting (abstract 301).
He said the results suggest ixazomib represents a new treatment option for maintenance after ASCT in MM.
“Proteasome inhibitors have a different mechanism of action and may provide an alternative to lenalidomide,” Dr. Dimopoulos said.
He noted that ixazomib has a manageable toxicity profile and “convenient” weekly oral dosing, making it “well suited” for maintenance.
The TOURMALINE-MM3 study (NCT02181413) included 656 MM patients randomized post-ASCT to receive weekly ixazomib or placebo for up to 2 years.
The median PFS was 26.5 months for ixazomib and 21.3 months for placebo (hazard ratio=0.720; 95% confidence interval, 0.582-0.890; P=0.002).
At a median follow-up of 31 months, the median overall survival has not been reached in either treatment arm.
The discontinuation rate due to adverse events was 7% for ixazomib and 5% for placebo.
Ixazomib was associated with “low toxicity,” Dr Dimopoulos said, and there was no difference in the rates of new primary malignancies, at 3% in both arms.
When asked by an attendee whether ixazomib would become the standard of care for younger MM patients in this setting, Dr. Dimopoulos said the results show that ixazomib “is an option for patients, especially for those where a physician may believe that a proteasome inhibitor may be indicated.”
However, when pressed to comment on how ixazomib compares with lenalidomide for maintenance, Dr. Dimopoulos remarked that current maintenance studies are moving in the direction of combining therapies.
“I think that instead of saying, ‘Is ixazomib better than lenalidomide or vice-versa,’ it is better to see how one may combine those drugs in subsets of patients or even combine these drugs with other agents,” he said.
A manuscript describing results of the TOURMALINE-MM3 study is in press at The Lancet, with an expected online publication date of December 10, Dr. Dimopoulos said.
TOURMALINE-MM3 is sponsored by Takeda (Millennium), the maker of ixazomib.
Dr. Dimopoulos reported honoraria and consultancy with Janssen, Takeda Pharmaceuticals, Amgen, Bristol-Myers Squibb, and Celgene.
SAN DIEGO—Ixazomib improved progression-free survival (PFS) following autologous stem cell transplant (ASCT) in patients with newly diagnosed multiple myeloma (MM) in the TOURMALINE-MM3 trial.
The oral proteasome inhibitor improved PFS by 39% compared to placebo.
In addition, treatment with ixazomib was well tolerated, and there was a low discontinuation rate.
TOURMALINE-MM3 is the first-ever randomized, double-blind, placebo-controlled study of a proteasome inhibitor used as maintenance after ASCT, according to Meletios A. Dimopoulos, MD, of the National and Kapodistrian University of Athens in Greece.
Dr. Dimopoulos presented results from the trial at the 2018 ASH Annual Meeting (abstract 301).
He said the results suggest ixazomib represents a new treatment option for maintenance after ASCT in MM.
“Proteasome inhibitors have a different mechanism of action and may provide an alternative to lenalidomide,” Dr. Dimopoulos said.
He noted that ixazomib has a manageable toxicity profile and “convenient” weekly oral dosing, making it “well suited” for maintenance.
The TOURMALINE-MM3 study (NCT02181413) included 656 MM patients randomized post-ASCT to receive weekly ixazomib or placebo for up to 2 years.
The median PFS was 26.5 months for ixazomib and 21.3 months for placebo (hazard ratio=0.720; 95% confidence interval, 0.582-0.890; P=0.002).
At a median follow-up of 31 months, the median overall survival has not been reached in either treatment arm.
The discontinuation rate due to adverse events was 7% for ixazomib and 5% for placebo.
Ixazomib was associated with “low toxicity,” Dr Dimopoulos said, and there was no difference in the rates of new primary malignancies, at 3% in both arms.
When asked by an attendee whether ixazomib would become the standard of care for younger MM patients in this setting, Dr. Dimopoulos said the results show that ixazomib “is an option for patients, especially for those where a physician may believe that a proteasome inhibitor may be indicated.”
However, when pressed to comment on how ixazomib compares with lenalidomide for maintenance, Dr. Dimopoulos remarked that current maintenance studies are moving in the direction of combining therapies.
“I think that instead of saying, ‘Is ixazomib better than lenalidomide or vice-versa,’ it is better to see how one may combine those drugs in subsets of patients or even combine these drugs with other agents,” he said.
A manuscript describing results of the TOURMALINE-MM3 study is in press at The Lancet, with an expected online publication date of December 10, Dr. Dimopoulos said.
TOURMALINE-MM3 is sponsored by Takeda (Millennium), the maker of ixazomib.
Dr. Dimopoulos reported honoraria and consultancy with Janssen, Takeda Pharmaceuticals, Amgen, Bristol-Myers Squibb, and Celgene.
Older people with CHIP are safe donor source for HSCT
New research suggests older individuals with clonal hematopoiesis of indeterminate potential (CHIP) are a safe donor source for allogeneic hematopoietic stem cell transplant (HSCT).
Researchers found that transplants from older donors with CHIP resulted in similar survival as transplants from older donors without CHIP.
HSCT recipients with CHIP donors had a lower risk of relapse or progression but a higher risk of chronic graft-versus-host disease (GHVD), and they were more likely to develop donor-cell malignancies.
Frederik Damm, MD, of Charité – University Medical Center Berlin in Germany, and his colleagues reported these findings in the Journal of Clinical Oncology.
Little is known about the influence of donor CHIP in allogeneic HSCT, according to the researchers.
However, an increasing number of older patients are receiving donations from older, mostly sibling, donors who may have CHIP. CHIP increases with age and is associated with a greater risk of hematologic cancers, cardiovascular disease, and death from coronary heart disease.
With this in mind, Dr. Damm and his colleagues set out to determine how donor CHIP affects the outcome of HSCT.
Between 1993 and 2017, the researchers collected blood samples from 500 healthy, related HSCT donors, age 55 or older, at 10 transplant centers in Germany and France. The researchers sequenced the samples with a 66-gene panel.
The team also assessed overall survival (OS), non-relapse mortality (NRM), cumulative incidence of relapse/progression (CIR/P), cytomegalovirus (CMV) reactivation, and acute and chronic GVHD in the HSCT recipients.
Mutation analysis
The researchers identified 92 clonal mutations in 80 (16.0%) of the 500 donors. The variant allele frequency was 5.9% (range, 2% to 43%). In 20 patients, 25 variant alleles were present at a frequency of 10% or greater.
The researchers detected a single gene mutation in 70 donors, nine donors had two mutations, and one donor had four mutations. The most frequently mutated genes were DNMT3A (40/500, 8%), TET2 (11/500, 2.2%), and ASXL1 (7/500, 1.4%).
Baseline characteristics such as age, sex, or stem cells harvested per kilogram of body weight were similar between donors with and without CHIP.
Recipient characteristics were also evenly distributed regarding donor CHIP status and baseline characteristics.
However, the researchers noted that donor CHIP was present significantly more often in donors for recipients with myeloid compared to lymphoid neoplasms—19.2% and 6.3%, respectively (P≤0.001).
The prevalence of donor CHIP increased with age, from 10.3% (ages 60 to 64) to 20.3% (ages 65 to 69), 22.5% (ages 70 to 74), and 28.6% (ages 75 to 79).
The researchers observed no statistically significant association between CHIP and age, most likely, they wrote, “because 82% of all donors in our cohort were age 60 to 69 years.”
Transplant outcome
Donor CHIP led to slightly faster leukocyte engraftment, although it did not impact thrombocyte engraftment time.
The cumulative incidence of leukocyte engraftment after 15 days was 64.1% for HSCT recipients with CHIP donors and 51.4% for those with non-CHIP donors (P=0.023).
Chronic GVHD after HSCT was more likely for recipients with CHIP donors, with a 5-year cumulative incidence of 52.9%, compared to 35.7% for patients with non-CHIP donors (P=0.008).
Multivariate analysis showed donor CHIP to be an independent risk factor for chronic GVHD when adjusted for antithymocyte globulin application and donor age.
The researchers identified donor DNMT3A mutation as the predominant CHIP factor for developing chronic GVHD. The incidence of chronic GVHD was 58.5% in patients with DNMT3A-mutated donors and 36.6% in patients with wild-type donors (P=0.006).
The researchers noted that no other CHIP mutations or characteristics affected the development of chronic GVHD.
Donor CHIP status did not impact the incidence of acute GVHD or CMV reactivation.
Transplant recipients with CHIP donors had a lower CIR/P (P=0.027) than recipients with non-CHIP donors. Patients whose donors had CHIP with a DNMT3A mutation also had a lower CIR/P (P=0.029).
Donor CHIP had no effect on NRM.
Neither donor CHIP nor donor DNMT3A mutational status impacted CIR/P or NRM in patients who underwent HSCT while they were in complete response (CR).
However, patients not in CR at the time of HSCT had a lower CIR/P when the donor was CHIP-positive (hazard ratio [HR]=0.49; 95% confidence interval [CI], 0.27 to 0.88; P=0.019) or had a DNMT3A mutation (HR=0.34; 95% CI, 0.15 to 0.81; P=0.015).
Two of 82 patients with CHIP donors developed donor-cell malignancies, but there were no donor-cell malignancies in recipients with non-CHIP donors (P=0.026).
Survival
“To our knowledge, we showed, for the first time, that donor CHIP did not affect the survival of 500 HSCT recipients,” the researchers wrote.
At a median follow-up of 3.3 years, the median OS was 2 years, and the 5-year OS was 37.6%.
The researchers observed no survival differences in patients with CHIP donors or non-CHIP donors (HR=0.88; 95% CI, 0.65 to 1.321; P=0.434). And the same was true for DNMT3A mutation (HR=0.89; 95% CI, 0.58 to 1.35; P=0.573).
The researchers pointed out that patients with myelodysplastic syndromes or acute myeloid leukemia who were not in CR when they underwent HSCT had a survival benefit with donor CHIP (HR=0.49; 95% CI, 0.28 to 0.86; P=0.011).
“This finding could implicate an important clinical potential in this difficult-to-treat subgroup,” the researchers noted.
However, this was not the case for patients with myeloproliferative neoplasia, for whom donor CHIP tended to reduce survival (P=0.077).
The research team recommended future studies be conducted in younger and unrelated donors to confirm the results of this study.
The research was funded by numerous grants and fellowships, and the researchers reported no relevant conflicts of interest.
New research suggests older individuals with clonal hematopoiesis of indeterminate potential (CHIP) are a safe donor source for allogeneic hematopoietic stem cell transplant (HSCT).
Researchers found that transplants from older donors with CHIP resulted in similar survival as transplants from older donors without CHIP.
HSCT recipients with CHIP donors had a lower risk of relapse or progression but a higher risk of chronic graft-versus-host disease (GHVD), and they were more likely to develop donor-cell malignancies.
Frederik Damm, MD, of Charité – University Medical Center Berlin in Germany, and his colleagues reported these findings in the Journal of Clinical Oncology.
Little is known about the influence of donor CHIP in allogeneic HSCT, according to the researchers.
However, an increasing number of older patients are receiving donations from older, mostly sibling, donors who may have CHIP. CHIP increases with age and is associated with a greater risk of hematologic cancers, cardiovascular disease, and death from coronary heart disease.
With this in mind, Dr. Damm and his colleagues set out to determine how donor CHIP affects the outcome of HSCT.
Between 1993 and 2017, the researchers collected blood samples from 500 healthy, related HSCT donors, age 55 or older, at 10 transplant centers in Germany and France. The researchers sequenced the samples with a 66-gene panel.
The team also assessed overall survival (OS), non-relapse mortality (NRM), cumulative incidence of relapse/progression (CIR/P), cytomegalovirus (CMV) reactivation, and acute and chronic GVHD in the HSCT recipients.
Mutation analysis
The researchers identified 92 clonal mutations in 80 (16.0%) of the 500 donors. The variant allele frequency was 5.9% (range, 2% to 43%). In 20 patients, 25 variant alleles were present at a frequency of 10% or greater.
The researchers detected a single gene mutation in 70 donors, nine donors had two mutations, and one donor had four mutations. The most frequently mutated genes were DNMT3A (40/500, 8%), TET2 (11/500, 2.2%), and ASXL1 (7/500, 1.4%).
Baseline characteristics such as age, sex, or stem cells harvested per kilogram of body weight were similar between donors with and without CHIP.
Recipient characteristics were also evenly distributed regarding donor CHIP status and baseline characteristics.
However, the researchers noted that donor CHIP was present significantly more often in donors for recipients with myeloid compared to lymphoid neoplasms—19.2% and 6.3%, respectively (P≤0.001).
The prevalence of donor CHIP increased with age, from 10.3% (ages 60 to 64) to 20.3% (ages 65 to 69), 22.5% (ages 70 to 74), and 28.6% (ages 75 to 79).
The researchers observed no statistically significant association between CHIP and age, most likely, they wrote, “because 82% of all donors in our cohort were age 60 to 69 years.”
Transplant outcome
Donor CHIP led to slightly faster leukocyte engraftment, although it did not impact thrombocyte engraftment time.
The cumulative incidence of leukocyte engraftment after 15 days was 64.1% for HSCT recipients with CHIP donors and 51.4% for those with non-CHIP donors (P=0.023).
Chronic GVHD after HSCT was more likely for recipients with CHIP donors, with a 5-year cumulative incidence of 52.9%, compared to 35.7% for patients with non-CHIP donors (P=0.008).
Multivariate analysis showed donor CHIP to be an independent risk factor for chronic GVHD when adjusted for antithymocyte globulin application and donor age.
The researchers identified donor DNMT3A mutation as the predominant CHIP factor for developing chronic GVHD. The incidence of chronic GVHD was 58.5% in patients with DNMT3A-mutated donors and 36.6% in patients with wild-type donors (P=0.006).
The researchers noted that no other CHIP mutations or characteristics affected the development of chronic GVHD.
Donor CHIP status did not impact the incidence of acute GVHD or CMV reactivation.
Transplant recipients with CHIP donors had a lower CIR/P (P=0.027) than recipients with non-CHIP donors. Patients whose donors had CHIP with a DNMT3A mutation also had a lower CIR/P (P=0.029).
Donor CHIP had no effect on NRM.
Neither donor CHIP nor donor DNMT3A mutational status impacted CIR/P or NRM in patients who underwent HSCT while they were in complete response (CR).
However, patients not in CR at the time of HSCT had a lower CIR/P when the donor was CHIP-positive (hazard ratio [HR]=0.49; 95% confidence interval [CI], 0.27 to 0.88; P=0.019) or had a DNMT3A mutation (HR=0.34; 95% CI, 0.15 to 0.81; P=0.015).
Two of 82 patients with CHIP donors developed donor-cell malignancies, but there were no donor-cell malignancies in recipients with non-CHIP donors (P=0.026).
Survival
“To our knowledge, we showed, for the first time, that donor CHIP did not affect the survival of 500 HSCT recipients,” the researchers wrote.
At a median follow-up of 3.3 years, the median OS was 2 years, and the 5-year OS was 37.6%.
The researchers observed no survival differences in patients with CHIP donors or non-CHIP donors (HR=0.88; 95% CI, 0.65 to 1.321; P=0.434). And the same was true for DNMT3A mutation (HR=0.89; 95% CI, 0.58 to 1.35; P=0.573).
The researchers pointed out that patients with myelodysplastic syndromes or acute myeloid leukemia who were not in CR when they underwent HSCT had a survival benefit with donor CHIP (HR=0.49; 95% CI, 0.28 to 0.86; P=0.011).
“This finding could implicate an important clinical potential in this difficult-to-treat subgroup,” the researchers noted.
However, this was not the case for patients with myeloproliferative neoplasia, for whom donor CHIP tended to reduce survival (P=0.077).
The research team recommended future studies be conducted in younger and unrelated donors to confirm the results of this study.
The research was funded by numerous grants and fellowships, and the researchers reported no relevant conflicts of interest.
New research suggests older individuals with clonal hematopoiesis of indeterminate potential (CHIP) are a safe donor source for allogeneic hematopoietic stem cell transplant (HSCT).
Researchers found that transplants from older donors with CHIP resulted in similar survival as transplants from older donors without CHIP.
HSCT recipients with CHIP donors had a lower risk of relapse or progression but a higher risk of chronic graft-versus-host disease (GHVD), and they were more likely to develop donor-cell malignancies.
Frederik Damm, MD, of Charité – University Medical Center Berlin in Germany, and his colleagues reported these findings in the Journal of Clinical Oncology.
Little is known about the influence of donor CHIP in allogeneic HSCT, according to the researchers.
However, an increasing number of older patients are receiving donations from older, mostly sibling, donors who may have CHIP. CHIP increases with age and is associated with a greater risk of hematologic cancers, cardiovascular disease, and death from coronary heart disease.
With this in mind, Dr. Damm and his colleagues set out to determine how donor CHIP affects the outcome of HSCT.
Between 1993 and 2017, the researchers collected blood samples from 500 healthy, related HSCT donors, age 55 or older, at 10 transplant centers in Germany and France. The researchers sequenced the samples with a 66-gene panel.
The team also assessed overall survival (OS), non-relapse mortality (NRM), cumulative incidence of relapse/progression (CIR/P), cytomegalovirus (CMV) reactivation, and acute and chronic GVHD in the HSCT recipients.
Mutation analysis
The researchers identified 92 clonal mutations in 80 (16.0%) of the 500 donors. The variant allele frequency was 5.9% (range, 2% to 43%). In 20 patients, 25 variant alleles were present at a frequency of 10% or greater.
The researchers detected a single gene mutation in 70 donors, nine donors had two mutations, and one donor had four mutations. The most frequently mutated genes were DNMT3A (40/500, 8%), TET2 (11/500, 2.2%), and ASXL1 (7/500, 1.4%).
Baseline characteristics such as age, sex, or stem cells harvested per kilogram of body weight were similar between donors with and without CHIP.
Recipient characteristics were also evenly distributed regarding donor CHIP status and baseline characteristics.
However, the researchers noted that donor CHIP was present significantly more often in donors for recipients with myeloid compared to lymphoid neoplasms—19.2% and 6.3%, respectively (P≤0.001).
The prevalence of donor CHIP increased with age, from 10.3% (ages 60 to 64) to 20.3% (ages 65 to 69), 22.5% (ages 70 to 74), and 28.6% (ages 75 to 79).
The researchers observed no statistically significant association between CHIP and age, most likely, they wrote, “because 82% of all donors in our cohort were age 60 to 69 years.”
Transplant outcome
Donor CHIP led to slightly faster leukocyte engraftment, although it did not impact thrombocyte engraftment time.
The cumulative incidence of leukocyte engraftment after 15 days was 64.1% for HSCT recipients with CHIP donors and 51.4% for those with non-CHIP donors (P=0.023).
Chronic GVHD after HSCT was more likely for recipients with CHIP donors, with a 5-year cumulative incidence of 52.9%, compared to 35.7% for patients with non-CHIP donors (P=0.008).
Multivariate analysis showed donor CHIP to be an independent risk factor for chronic GVHD when adjusted for antithymocyte globulin application and donor age.
The researchers identified donor DNMT3A mutation as the predominant CHIP factor for developing chronic GVHD. The incidence of chronic GVHD was 58.5% in patients with DNMT3A-mutated donors and 36.6% in patients with wild-type donors (P=0.006).
The researchers noted that no other CHIP mutations or characteristics affected the development of chronic GVHD.
Donor CHIP status did not impact the incidence of acute GVHD or CMV reactivation.
Transplant recipients with CHIP donors had a lower CIR/P (P=0.027) than recipients with non-CHIP donors. Patients whose donors had CHIP with a DNMT3A mutation also had a lower CIR/P (P=0.029).
Donor CHIP had no effect on NRM.
Neither donor CHIP nor donor DNMT3A mutational status impacted CIR/P or NRM in patients who underwent HSCT while they were in complete response (CR).
However, patients not in CR at the time of HSCT had a lower CIR/P when the donor was CHIP-positive (hazard ratio [HR]=0.49; 95% confidence interval [CI], 0.27 to 0.88; P=0.019) or had a DNMT3A mutation (HR=0.34; 95% CI, 0.15 to 0.81; P=0.015).
Two of 82 patients with CHIP donors developed donor-cell malignancies, but there were no donor-cell malignancies in recipients with non-CHIP donors (P=0.026).
Survival
“To our knowledge, we showed, for the first time, that donor CHIP did not affect the survival of 500 HSCT recipients,” the researchers wrote.
At a median follow-up of 3.3 years, the median OS was 2 years, and the 5-year OS was 37.6%.
The researchers observed no survival differences in patients with CHIP donors or non-CHIP donors (HR=0.88; 95% CI, 0.65 to 1.321; P=0.434). And the same was true for DNMT3A mutation (HR=0.89; 95% CI, 0.58 to 1.35; P=0.573).
The researchers pointed out that patients with myelodysplastic syndromes or acute myeloid leukemia who were not in CR when they underwent HSCT had a survival benefit with donor CHIP (HR=0.49; 95% CI, 0.28 to 0.86; P=0.011).
“This finding could implicate an important clinical potential in this difficult-to-treat subgroup,” the researchers noted.
However, this was not the case for patients with myeloproliferative neoplasia, for whom donor CHIP tended to reduce survival (P=0.077).
The research team recommended future studies be conducted in younger and unrelated donors to confirm the results of this study.
The research was funded by numerous grants and fellowships, and the researchers reported no relevant conflicts of interest.
Elderly NHL patients have higher NRM after HSCT
A retrospective study suggests elderly patients with non-Hodgkin lymphoma (NHL) are more likely to die, but not relapse, within a year of allogeneic hematopoietic stem cell transplant (allo-HSCT).
The rate of non-relapse mortality (NRM) at 1 year was significantly higher for elderly patients than for middle-aged or young patients.
However, the 3-year rate of relapse was similar across the age groups.
Charalampia Kyriakou, MD, PhD, of University College London in the U.K., and her colleagues reported these findings in Biology of Blood and Marrow Transplantation.
The investigators analyzed 3,919 patients with NHL who underwent allo-HSCT between 2003 and 2013.
The patients had follicular lymphoma (n=1,461), diffuse large B-cell lymphoma (n=1,192), mantle cell lymphoma (n=823), and peripheral T-cell lymphoma (n=443).
At the time of transplant, about 85% of patients were chemo-sensitive, with the remainder being chemo-refractory.
Results
The investigators compared outcomes in patients assigned to three age groups—young (18-50), middle-aged (51-65), and elderly (66-77).
NRM at 1 year was 13% for young patients, 20% for middle-aged patients, and 33% for elderly patients (P<0.001).
Overall survival at 3 years was 60% in young patients, 54% in middle-aged patients, and 38% in the elderly (P<0.001).
In contrast to these significant associations between age and survival, the rate of relapse at 3 years remained relatively consistent—30% in young patients, 31% in middle-aged patients, and 28% in elderly patients (P=0.355).
The increased risk of NRM in elderly patients could not be fully explained by comorbidities, although these were more common in the elderly.
After analyzing information from a subset of patients, the investigators concluded that “the presence of comorbidities is a significant risk factor for NRM and survival, but this does not fully explain the outcome disadvantages in our [elderly] group.”
Therefore, age remains an independent risk factor.
The investigators did not report conflicts of interest.
A retrospective study suggests elderly patients with non-Hodgkin lymphoma (NHL) are more likely to die, but not relapse, within a year of allogeneic hematopoietic stem cell transplant (allo-HSCT).
The rate of non-relapse mortality (NRM) at 1 year was significantly higher for elderly patients than for middle-aged or young patients.
However, the 3-year rate of relapse was similar across the age groups.
Charalampia Kyriakou, MD, PhD, of University College London in the U.K., and her colleagues reported these findings in Biology of Blood and Marrow Transplantation.
The investigators analyzed 3,919 patients with NHL who underwent allo-HSCT between 2003 and 2013.
The patients had follicular lymphoma (n=1,461), diffuse large B-cell lymphoma (n=1,192), mantle cell lymphoma (n=823), and peripheral T-cell lymphoma (n=443).
At the time of transplant, about 85% of patients were chemo-sensitive, with the remainder being chemo-refractory.
Results
The investigators compared outcomes in patients assigned to three age groups—young (18-50), middle-aged (51-65), and elderly (66-77).
NRM at 1 year was 13% for young patients, 20% for middle-aged patients, and 33% for elderly patients (P<0.001).
Overall survival at 3 years was 60% in young patients, 54% in middle-aged patients, and 38% in the elderly (P<0.001).
In contrast to these significant associations between age and survival, the rate of relapse at 3 years remained relatively consistent—30% in young patients, 31% in middle-aged patients, and 28% in elderly patients (P=0.355).
The increased risk of NRM in elderly patients could not be fully explained by comorbidities, although these were more common in the elderly.
After analyzing information from a subset of patients, the investigators concluded that “the presence of comorbidities is a significant risk factor for NRM and survival, but this does not fully explain the outcome disadvantages in our [elderly] group.”
Therefore, age remains an independent risk factor.
The investigators did not report conflicts of interest.
A retrospective study suggests elderly patients with non-Hodgkin lymphoma (NHL) are more likely to die, but not relapse, within a year of allogeneic hematopoietic stem cell transplant (allo-HSCT).
The rate of non-relapse mortality (NRM) at 1 year was significantly higher for elderly patients than for middle-aged or young patients.
However, the 3-year rate of relapse was similar across the age groups.
Charalampia Kyriakou, MD, PhD, of University College London in the U.K., and her colleagues reported these findings in Biology of Blood and Marrow Transplantation.
The investigators analyzed 3,919 patients with NHL who underwent allo-HSCT between 2003 and 2013.
The patients had follicular lymphoma (n=1,461), diffuse large B-cell lymphoma (n=1,192), mantle cell lymphoma (n=823), and peripheral T-cell lymphoma (n=443).
At the time of transplant, about 85% of patients were chemo-sensitive, with the remainder being chemo-refractory.
Results
The investigators compared outcomes in patients assigned to three age groups—young (18-50), middle-aged (51-65), and elderly (66-77).
NRM at 1 year was 13% for young patients, 20% for middle-aged patients, and 33% for elderly patients (P<0.001).
Overall survival at 3 years was 60% in young patients, 54% in middle-aged patients, and 38% in the elderly (P<0.001).
In contrast to these significant associations between age and survival, the rate of relapse at 3 years remained relatively consistent—30% in young patients, 31% in middle-aged patients, and 28% in elderly patients (P=0.355).
The increased risk of NRM in elderly patients could not be fully explained by comorbidities, although these were more common in the elderly.
After analyzing information from a subset of patients, the investigators concluded that “the presence of comorbidities is a significant risk factor for NRM and survival, but this does not fully explain the outcome disadvantages in our [elderly] group.”
Therefore, age remains an independent risk factor.
The investigators did not report conflicts of interest.
Study supports PBM program for HSCT recipients
BOSTON—A blood management program for patients undergoing hematopoietic stem cell transplant (HSCT) can reduce inappropriate transfusions and costs without compromising patient outcomes, a new study suggests.
Researchers retrospectively compared outcomes before and after implementation of a patient blood management (PBM) program at a single institution.
After the program was implemented, the number of transfusions and the units transfused declined without affecting patient mortality, intensive care unit (ICU) admission rates, or other transfusion-related complications.
In addition, the program saved the hospital more than $600,000 over a year.
Nilesh Jambhekar, MD, of the Mayo Clinic in Rochester, Minnesota, reported these results in a presentation at AABB 2018 (abstract PBM3-ST4-22*).
Study design
Dr. Jambhekar and his colleagues looked at blood product use both before and after the Mayo Clinic started a PBM program that included emphasis on AABB best practice guidelines and electronic clinical-decision support for transfusion orders.
The researchers evaluated the frequency and proportion of red blood cell (RBC) and platelet transfusions, total transfusion quantities, transfusions that occurred outside of the clinical guidelines, and the activity-based costs of transfusions.
Dr. Jambhekar acknowledged that the study relied on rigid hemoglobin and platelet thresholds when considering transfusions conducted outside of the guidelines, defined as RBCs administered for hemoglobin values greater than 7 g/dL and platelet transfusions for platelet counts greater than 10 x 109/L.
He noted, however, that the researchers conducted sensitivity analyses to account for exceptions such as patients with coronary disease or neutropenic fever.
The patient-centered outcomes the researchers evaluated included mortality, hospital and ICU admission rates, transfusion reactions, cerebrovascular and coronary ischemic events, and infections.
The study included data on 360 adults older than 18 who underwent HSCT in 2013, before the PBM program was implemented, and 368 transplanted in 2015, after implementation.
In each cohort, patients were followed out to 90 days after transplant.
Results
The total number of platelet units transfused dropped from 1,660 pre-PBM program to 1,417 post-PBM implementation. The total number of RBC units dropped from 1,158 to 826.
The researchers also saw changes in the proportions of inappropriate (outside guidelines) transfusions between the two time periods.
In 2013, 94.2% of RBC transfusions occurred outside the guidelines, compared with 35.4% in 2015 (P<0.0001). Similarly, the proportion of inappropriate platelet transfusions declined from 73.4% to 48.7% over the same time period (P<0.0001).
In addition, all-cause mortality at 3 months was significantly lower after the PBM program was introduced. The 3-month mortality rate was 30.7% for the 2013 cohort and 20.2% for the 2015 cohort (P=0.001).
Dr. Jambhekar noted that, in a multivariable analysis accounting for baseline differences between the groups, mortality for patients treated before the PBM program remained significantly higher, with an odds ratio of 1.85 (P=0.0008).
Neither hospital nor ICU admission within 30 days differed significantly between the groups, and there were no significant between-group differences in hospital or ICU lengths of stay.
Likewise, there were no significant between-group differences in myocardial infarctions, cerebrovascular events, sepsis, and febrile or allergic transfusion reactions.
Dr. Jambhekar noted that this study was retrospective in design and therefore could not fully account for potential confounders. It’s also unclear whether the results could be generalized for adoption by other institutions.
“In general, PBM implementation is probably helpful in reducing both platelet and PRBC [packed red blood cell] utilization, but it’s not an easy thing to do,” Dr. Jambhekar said.
“It requires institutional buy-in and key players to make it happen. Ongoing PBM-related activities like surveillance, education, and clinical decision feedback are critical to maintaining success that we’ve had.”
This study was internally funded. Dr. Jambhekar reported having nothing to disclose.
*Data presented differ from the abstract.
BOSTON—A blood management program for patients undergoing hematopoietic stem cell transplant (HSCT) can reduce inappropriate transfusions and costs without compromising patient outcomes, a new study suggests.
Researchers retrospectively compared outcomes before and after implementation of a patient blood management (PBM) program at a single institution.
After the program was implemented, the number of transfusions and the units transfused declined without affecting patient mortality, intensive care unit (ICU) admission rates, or other transfusion-related complications.
In addition, the program saved the hospital more than $600,000 over a year.
Nilesh Jambhekar, MD, of the Mayo Clinic in Rochester, Minnesota, reported these results in a presentation at AABB 2018 (abstract PBM3-ST4-22*).
Study design
Dr. Jambhekar and his colleagues looked at blood product use both before and after the Mayo Clinic started a PBM program that included emphasis on AABB best practice guidelines and electronic clinical-decision support for transfusion orders.
The researchers evaluated the frequency and proportion of red blood cell (RBC) and platelet transfusions, total transfusion quantities, transfusions that occurred outside of the clinical guidelines, and the activity-based costs of transfusions.
Dr. Jambhekar acknowledged that the study relied on rigid hemoglobin and platelet thresholds when considering transfusions conducted outside of the guidelines, defined as RBCs administered for hemoglobin values greater than 7 g/dL and platelet transfusions for platelet counts greater than 10 x 109/L.
He noted, however, that the researchers conducted sensitivity analyses to account for exceptions such as patients with coronary disease or neutropenic fever.
The patient-centered outcomes the researchers evaluated included mortality, hospital and ICU admission rates, transfusion reactions, cerebrovascular and coronary ischemic events, and infections.
The study included data on 360 adults older than 18 who underwent HSCT in 2013, before the PBM program was implemented, and 368 transplanted in 2015, after implementation.
In each cohort, patients were followed out to 90 days after transplant.
Results
The total number of platelet units transfused dropped from 1,660 pre-PBM program to 1,417 post-PBM implementation. The total number of RBC units dropped from 1,158 to 826.
The researchers also saw changes in the proportions of inappropriate (outside guidelines) transfusions between the two time periods.
In 2013, 94.2% of RBC transfusions occurred outside the guidelines, compared with 35.4% in 2015 (P<0.0001). Similarly, the proportion of inappropriate platelet transfusions declined from 73.4% to 48.7% over the same time period (P<0.0001).
In addition, all-cause mortality at 3 months was significantly lower after the PBM program was introduced. The 3-month mortality rate was 30.7% for the 2013 cohort and 20.2% for the 2015 cohort (P=0.001).
Dr. Jambhekar noted that, in a multivariable analysis accounting for baseline differences between the groups, mortality for patients treated before the PBM program remained significantly higher, with an odds ratio of 1.85 (P=0.0008).
Neither hospital nor ICU admission within 30 days differed significantly between the groups, and there were no significant between-group differences in hospital or ICU lengths of stay.
Likewise, there were no significant between-group differences in myocardial infarctions, cerebrovascular events, sepsis, and febrile or allergic transfusion reactions.
Dr. Jambhekar noted that this study was retrospective in design and therefore could not fully account for potential confounders. It’s also unclear whether the results could be generalized for adoption by other institutions.
“In general, PBM implementation is probably helpful in reducing both platelet and PRBC [packed red blood cell] utilization, but it’s not an easy thing to do,” Dr. Jambhekar said.
“It requires institutional buy-in and key players to make it happen. Ongoing PBM-related activities like surveillance, education, and clinical decision feedback are critical to maintaining success that we’ve had.”
This study was internally funded. Dr. Jambhekar reported having nothing to disclose.
*Data presented differ from the abstract.
BOSTON—A blood management program for patients undergoing hematopoietic stem cell transplant (HSCT) can reduce inappropriate transfusions and costs without compromising patient outcomes, a new study suggests.
Researchers retrospectively compared outcomes before and after implementation of a patient blood management (PBM) program at a single institution.
After the program was implemented, the number of transfusions and the units transfused declined without affecting patient mortality, intensive care unit (ICU) admission rates, or other transfusion-related complications.
In addition, the program saved the hospital more than $600,000 over a year.
Nilesh Jambhekar, MD, of the Mayo Clinic in Rochester, Minnesota, reported these results in a presentation at AABB 2018 (abstract PBM3-ST4-22*).
Study design
Dr. Jambhekar and his colleagues looked at blood product use both before and after the Mayo Clinic started a PBM program that included emphasis on AABB best practice guidelines and electronic clinical-decision support for transfusion orders.
The researchers evaluated the frequency and proportion of red blood cell (RBC) and platelet transfusions, total transfusion quantities, transfusions that occurred outside of the clinical guidelines, and the activity-based costs of transfusions.
Dr. Jambhekar acknowledged that the study relied on rigid hemoglobin and platelet thresholds when considering transfusions conducted outside of the guidelines, defined as RBCs administered for hemoglobin values greater than 7 g/dL and platelet transfusions for platelet counts greater than 10 x 109/L.
He noted, however, that the researchers conducted sensitivity analyses to account for exceptions such as patients with coronary disease or neutropenic fever.
The patient-centered outcomes the researchers evaluated included mortality, hospital and ICU admission rates, transfusion reactions, cerebrovascular and coronary ischemic events, and infections.
The study included data on 360 adults older than 18 who underwent HSCT in 2013, before the PBM program was implemented, and 368 transplanted in 2015, after implementation.
In each cohort, patients were followed out to 90 days after transplant.
Results
The total number of platelet units transfused dropped from 1,660 pre-PBM program to 1,417 post-PBM implementation. The total number of RBC units dropped from 1,158 to 826.
The researchers also saw changes in the proportions of inappropriate (outside guidelines) transfusions between the two time periods.
In 2013, 94.2% of RBC transfusions occurred outside the guidelines, compared with 35.4% in 2015 (P<0.0001). Similarly, the proportion of inappropriate platelet transfusions declined from 73.4% to 48.7% over the same time period (P<0.0001).
In addition, all-cause mortality at 3 months was significantly lower after the PBM program was introduced. The 3-month mortality rate was 30.7% for the 2013 cohort and 20.2% for the 2015 cohort (P=0.001).
Dr. Jambhekar noted that, in a multivariable analysis accounting for baseline differences between the groups, mortality for patients treated before the PBM program remained significantly higher, with an odds ratio of 1.85 (P=0.0008).
Neither hospital nor ICU admission within 30 days differed significantly between the groups, and there were no significant between-group differences in hospital or ICU lengths of stay.
Likewise, there were no significant between-group differences in myocardial infarctions, cerebrovascular events, sepsis, and febrile or allergic transfusion reactions.
Dr. Jambhekar noted that this study was retrospective in design and therefore could not fully account for potential confounders. It’s also unclear whether the results could be generalized for adoption by other institutions.
“In general, PBM implementation is probably helpful in reducing both platelet and PRBC [packed red blood cell] utilization, but it’s not an easy thing to do,” Dr. Jambhekar said.
“It requires institutional buy-in and key players to make it happen. Ongoing PBM-related activities like surveillance, education, and clinical decision feedback are critical to maintaining success that we’ve had.”
This study was internally funded. Dr. Jambhekar reported having nothing to disclose.
*Data presented differ from the abstract.
Changes related to AML relapse may be reversible
New research suggests relapse of acute myeloid leukemia (AML) after allogeneic hematopoietic stem cell transplant (HSCT) is related to changes in immune-related gene expression that may be reversible.
Researchers observed downregulation of major histocompatibility complex (MHC) class II genes in samples from patients who relapsed after HSCT.
However, interferon-gamma “rapidly reversed this phenotype” in vitro, according to the researchers.
Matthew J. Christopher, MD, PhD, of Washington University School of Medicine in St. Louis, Missouri, and his colleagues reported these findings in The New England Journal of Medicine.
The researchers set out to determine how genetic and epigenetic changes after HSCT may allow leukemic cells to avoid the graft-vs-leukemia effect and to see whether immune-related genes are affected by HSCT.
The team analyzed paired samples obtained at diagnosis and relapse from 15 AML patients who relapsed after HSCT and 20 AML patients who relapsed after chemotherapy. The team also analyzed additional samples from patients who relapsed after HSCT to validate initial findings.
Methods of analysis included enhanced exome sequencing, RNA sequencing, flow cytometry, and immunohistochemical analysis.
Findings
The researchers first looked for relapse-specific mutations but found no driver mutations associated with relapse after HSCT.
The mutations seen post-HSCT relapse were generally similar to those seen both before treatment and after relapse in patients who had undergone chemotherapy, and the researchers could not identify any patterns of mutations related to relapse.
They then looked for, but did not find, relapse-specific mutations in genes involved in modulation of immune checkpoints, antigen presentation, or cytokine signaling.
The researchers did, however, find evidence of epigenetic changes that were more common in the samples from patients with post-transplant relapses.
RNA sequencing showed that MHC class II genes (HLA-DPA1, HLA-DPB1, HLA-DQB1, and HLA-DRB1) were downregulated three- to 12-fold after transplant.
Flow cytometry and immunohistochemical analysis confirmed that MHC class II expression was decreased at relapse after HSCT in 17 of 34 samples evaluated.
The researchers said there was no association between the downregulation of MHC class II and donor type or use of immunosuppression.
To see whether the downregulation of MHC class II genes was reversible, the researchers treated three post-HSCT relapse samples with interferon-gamma, which is known to upregulate MHC class II on certain cells.
Culturing patient cells with interferon-gamma “rapidly induced MHC class II protein expression on leukemic blasts,” the researchers said. They observed “essentially full restoration of MHC class II protein expression in nearly all AML blasts after 72 hours.”
This study was supported by the National Institutes of Health, Leukemia and Lymphoma Society, and the Barnes-Jewish Hospital Foundation.
Several study authors reported personal fees and/or research support from industry outside the submitted work.
New research suggests relapse of acute myeloid leukemia (AML) after allogeneic hematopoietic stem cell transplant (HSCT) is related to changes in immune-related gene expression that may be reversible.
Researchers observed downregulation of major histocompatibility complex (MHC) class II genes in samples from patients who relapsed after HSCT.
However, interferon-gamma “rapidly reversed this phenotype” in vitro, according to the researchers.
Matthew J. Christopher, MD, PhD, of Washington University School of Medicine in St. Louis, Missouri, and his colleagues reported these findings in The New England Journal of Medicine.
The researchers set out to determine how genetic and epigenetic changes after HSCT may allow leukemic cells to avoid the graft-vs-leukemia effect and to see whether immune-related genes are affected by HSCT.
The team analyzed paired samples obtained at diagnosis and relapse from 15 AML patients who relapsed after HSCT and 20 AML patients who relapsed after chemotherapy. The team also analyzed additional samples from patients who relapsed after HSCT to validate initial findings.
Methods of analysis included enhanced exome sequencing, RNA sequencing, flow cytometry, and immunohistochemical analysis.
Findings
The researchers first looked for relapse-specific mutations but found no driver mutations associated with relapse after HSCT.
The mutations seen post-HSCT relapse were generally similar to those seen both before treatment and after relapse in patients who had undergone chemotherapy, and the researchers could not identify any patterns of mutations related to relapse.
They then looked for, but did not find, relapse-specific mutations in genes involved in modulation of immune checkpoints, antigen presentation, or cytokine signaling.
The researchers did, however, find evidence of epigenetic changes that were more common in the samples from patients with post-transplant relapses.
RNA sequencing showed that MHC class II genes (HLA-DPA1, HLA-DPB1, HLA-DQB1, and HLA-DRB1) were downregulated three- to 12-fold after transplant.
Flow cytometry and immunohistochemical analysis confirmed that MHC class II expression was decreased at relapse after HSCT in 17 of 34 samples evaluated.
The researchers said there was no association between the downregulation of MHC class II and donor type or use of immunosuppression.
To see whether the downregulation of MHC class II genes was reversible, the researchers treated three post-HSCT relapse samples with interferon-gamma, which is known to upregulate MHC class II on certain cells.
Culturing patient cells with interferon-gamma “rapidly induced MHC class II protein expression on leukemic blasts,” the researchers said. They observed “essentially full restoration of MHC class II protein expression in nearly all AML blasts after 72 hours.”
This study was supported by the National Institutes of Health, Leukemia and Lymphoma Society, and the Barnes-Jewish Hospital Foundation.
Several study authors reported personal fees and/or research support from industry outside the submitted work.
New research suggests relapse of acute myeloid leukemia (AML) after allogeneic hematopoietic stem cell transplant (HSCT) is related to changes in immune-related gene expression that may be reversible.
Researchers observed downregulation of major histocompatibility complex (MHC) class II genes in samples from patients who relapsed after HSCT.
However, interferon-gamma “rapidly reversed this phenotype” in vitro, according to the researchers.
Matthew J. Christopher, MD, PhD, of Washington University School of Medicine in St. Louis, Missouri, and his colleagues reported these findings in The New England Journal of Medicine.
The researchers set out to determine how genetic and epigenetic changes after HSCT may allow leukemic cells to avoid the graft-vs-leukemia effect and to see whether immune-related genes are affected by HSCT.
The team analyzed paired samples obtained at diagnosis and relapse from 15 AML patients who relapsed after HSCT and 20 AML patients who relapsed after chemotherapy. The team also analyzed additional samples from patients who relapsed after HSCT to validate initial findings.
Methods of analysis included enhanced exome sequencing, RNA sequencing, flow cytometry, and immunohistochemical analysis.
Findings
The researchers first looked for relapse-specific mutations but found no driver mutations associated with relapse after HSCT.
The mutations seen post-HSCT relapse were generally similar to those seen both before treatment and after relapse in patients who had undergone chemotherapy, and the researchers could not identify any patterns of mutations related to relapse.
They then looked for, but did not find, relapse-specific mutations in genes involved in modulation of immune checkpoints, antigen presentation, or cytokine signaling.
The researchers did, however, find evidence of epigenetic changes that were more common in the samples from patients with post-transplant relapses.
RNA sequencing showed that MHC class II genes (HLA-DPA1, HLA-DPB1, HLA-DQB1, and HLA-DRB1) were downregulated three- to 12-fold after transplant.
Flow cytometry and immunohistochemical analysis confirmed that MHC class II expression was decreased at relapse after HSCT in 17 of 34 samples evaluated.
The researchers said there was no association between the downregulation of MHC class II and donor type or use of immunosuppression.
To see whether the downregulation of MHC class II genes was reversible, the researchers treated three post-HSCT relapse samples with interferon-gamma, which is known to upregulate MHC class II on certain cells.
Culturing patient cells with interferon-gamma “rapidly induced MHC class II protein expression on leukemic blasts,” the researchers said. They observed “essentially full restoration of MHC class II protein expression in nearly all AML blasts after 72 hours.”
This study was supported by the National Institutes of Health, Leukemia and Lymphoma Society, and the Barnes-Jewish Hospital Foundation.
Several study authors reported personal fees and/or research support from industry outside the submitted work.
Ruxolitinib under priority review for acute GVHD
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for the JAK1/JAK2 inhibitor ruxolitinib (Jakafi®).
With this sNDA, Incyte Corporation is seeking approval for ruxolitinib as a treatment for patients with acute graft-versus-host-disease (GVHD) who have had an inadequate response to corticosteroids.
“If approved, ruxolitinib will be the first and only treatment available in the U.S. for patients with acute GVHD who have not responded adequately to corticosteroid therapy,” said Steven Stein, MD, chief medical officer at Incyte.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
In addition to priority review, ruxolitinib has received breakthrough therapy and orphan drug designations from the FDA as a treatment for acute GVHD.
The sNDA submission for ruxolitinib in acute GVHD is based on data from the phase 2 REACH1 trial (NCT02953678).
In this ongoing trial, researchers are evaluating ruxolitinib in combination with corticosteroids in patients who have steroid-refractory acute GVHD.
Incyte announced topline results from REACH1 in June, reporting on outcomes in 71 patients.
The study’s primary endpoint—overall response rate at day 28—was met. Ruxolitinib produced an overall response rate of 55% (39/71) at that time.
However, 73% of patients (52/71) responded to ruxolitinib at some point during the trial.
Incyte said the most common treatment-emergent adverse events were anemia (61%), thrombocytopenia (61%), and neutropenia (56%).
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for the JAK1/JAK2 inhibitor ruxolitinib (Jakafi®).
With this sNDA, Incyte Corporation is seeking approval for ruxolitinib as a treatment for patients with acute graft-versus-host-disease (GVHD) who have had an inadequate response to corticosteroids.
“If approved, ruxolitinib will be the first and only treatment available in the U.S. for patients with acute GVHD who have not responded adequately to corticosteroid therapy,” said Steven Stein, MD, chief medical officer at Incyte.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
In addition to priority review, ruxolitinib has received breakthrough therapy and orphan drug designations from the FDA as a treatment for acute GVHD.
The sNDA submission for ruxolitinib in acute GVHD is based on data from the phase 2 REACH1 trial (NCT02953678).
In this ongoing trial, researchers are evaluating ruxolitinib in combination with corticosteroids in patients who have steroid-refractory acute GVHD.
Incyte announced topline results from REACH1 in June, reporting on outcomes in 71 patients.
The study’s primary endpoint—overall response rate at day 28—was met. Ruxolitinib produced an overall response rate of 55% (39/71) at that time.
However, 73% of patients (52/71) responded to ruxolitinib at some point during the trial.
Incyte said the most common treatment-emergent adverse events were anemia (61%), thrombocytopenia (61%), and neutropenia (56%).
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for the JAK1/JAK2 inhibitor ruxolitinib (Jakafi®).
With this sNDA, Incyte Corporation is seeking approval for ruxolitinib as a treatment for patients with acute graft-versus-host-disease (GVHD) who have had an inadequate response to corticosteroids.
“If approved, ruxolitinib will be the first and only treatment available in the U.S. for patients with acute GVHD who have not responded adequately to corticosteroid therapy,” said Steven Stein, MD, chief medical officer at Incyte.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
In addition to priority review, ruxolitinib has received breakthrough therapy and orphan drug designations from the FDA as a treatment for acute GVHD.
The sNDA submission for ruxolitinib in acute GVHD is based on data from the phase 2 REACH1 trial (NCT02953678).
In this ongoing trial, researchers are evaluating ruxolitinib in combination with corticosteroids in patients who have steroid-refractory acute GVHD.
Incyte announced topline results from REACH1 in June, reporting on outcomes in 71 patients.
The study’s primary endpoint—overall response rate at day 28—was met. Ruxolitinib produced an overall response rate of 55% (39/71) at that time.
However, 73% of patients (52/71) responded to ruxolitinib at some point during the trial.
Incyte said the most common treatment-emergent adverse events were anemia (61%), thrombocytopenia (61%), and neutropenia (56%).
OMS721 receives orphan designation for HSCT-TMA
The U.S. Food and Drug Administration (FDA) has granted OMS721 orphan designation for the treatment of hematopoietic stem cell transplant-associated thrombotic microangiopathy (HSCT-TMA).
OMS721 is a monoclonal antibody targeting MASP-2, the effector enzyme of the lectin pathway of the complement system.
The FDA previously granted OMS721 breakthrough therapy designation for HSCT-TMA and orphan designation for the prevention of complement-mediated TMA, including HSCT-TMA.
Omeros Corporation, the company developing OMS721, has established a compassionate-use program for OMS721, which is active in the United States and Europe.
Clinical trials
Phase 3 clinical programs are in progress for OMS721 in atypical hemolytic uremic syndrome, immunoglobulin A nephropathy, and HSCT-TMA. Two phase 2 trials of OMS721—one in TMA and one in immunoglobulin A nephropathy—are ongoing.
Omeros released results from the phase 2 TMA trial (NCT02222545) in February.
The study includes adults with HSCT-TMA persisting for at least 2 weeks following immunosuppressive regimen modification or more than 30 days post-transplant. Patients receive weekly OMS721 treatments for 4 to 8 weeks at the discretion of the investigator.
At the time of Omeros’s announcement, 18 HSCT-TMA patients had been treated on this study.
These patients had a significantly longer median overall survival than historical controls—347 days and 21 days, respectively (P<0.0001).
Omeros also reported that markers of TMA activity significantly improved following OMS721 treatment.
The mean platelet count increased from 18,100 x 106/mL at baseline to 52,300 x 106/mL (P=0.017). The mean lactate dehydrogenase decreased from 591 U/L to 250 U/L (P<0.001). And the mean haptoglobin increased from 8 mg/dL to 141 mg/dL (P=0.003).
Mean creatinine remained stable—at approximately 120 μmol/L—but a majority of patients had co-existing conditions for which they were receiving nephrotoxic medications. These conditions included graft-versus-host disease, cytomegalovirus and human herpes virus 6 infections, prior sepsis, diffuse alveolar hemorrhage, and residual underlying malignancies.
The most commonly reported adverse events were diarrhea and neutropenia.
Four deaths occurred. One of these—due to acute renal and respiratory failure—was considered possibly related to OMS721. The other deaths were due to progression of acute myeloid leukemia (n=1) and neutropenic sepsis (n=2).
About orphan and breakthrough designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
The U.S. Food and Drug Administration (FDA) has granted OMS721 orphan designation for the treatment of hematopoietic stem cell transplant-associated thrombotic microangiopathy (HSCT-TMA).
OMS721 is a monoclonal antibody targeting MASP-2, the effector enzyme of the lectin pathway of the complement system.
The FDA previously granted OMS721 breakthrough therapy designation for HSCT-TMA and orphan designation for the prevention of complement-mediated TMA, including HSCT-TMA.
Omeros Corporation, the company developing OMS721, has established a compassionate-use program for OMS721, which is active in the United States and Europe.
Clinical trials
Phase 3 clinical programs are in progress for OMS721 in atypical hemolytic uremic syndrome, immunoglobulin A nephropathy, and HSCT-TMA. Two phase 2 trials of OMS721—one in TMA and one in immunoglobulin A nephropathy—are ongoing.
Omeros released results from the phase 2 TMA trial (NCT02222545) in February.
The study includes adults with HSCT-TMA persisting for at least 2 weeks following immunosuppressive regimen modification or more than 30 days post-transplant. Patients receive weekly OMS721 treatments for 4 to 8 weeks at the discretion of the investigator.
At the time of Omeros’s announcement, 18 HSCT-TMA patients had been treated on this study.
These patients had a significantly longer median overall survival than historical controls—347 days and 21 days, respectively (P<0.0001).
Omeros also reported that markers of TMA activity significantly improved following OMS721 treatment.
The mean platelet count increased from 18,100 x 106/mL at baseline to 52,300 x 106/mL (P=0.017). The mean lactate dehydrogenase decreased from 591 U/L to 250 U/L (P<0.001). And the mean haptoglobin increased from 8 mg/dL to 141 mg/dL (P=0.003).
Mean creatinine remained stable—at approximately 120 μmol/L—but a majority of patients had co-existing conditions for which they were receiving nephrotoxic medications. These conditions included graft-versus-host disease, cytomegalovirus and human herpes virus 6 infections, prior sepsis, diffuse alveolar hemorrhage, and residual underlying malignancies.
The most commonly reported adverse events were diarrhea and neutropenia.
Four deaths occurred. One of these—due to acute renal and respiratory failure—was considered possibly related to OMS721. The other deaths were due to progression of acute myeloid leukemia (n=1) and neutropenic sepsis (n=2).
About orphan and breakthrough designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
The U.S. Food and Drug Administration (FDA) has granted OMS721 orphan designation for the treatment of hematopoietic stem cell transplant-associated thrombotic microangiopathy (HSCT-TMA).
OMS721 is a monoclonal antibody targeting MASP-2, the effector enzyme of the lectin pathway of the complement system.
The FDA previously granted OMS721 breakthrough therapy designation for HSCT-TMA and orphan designation for the prevention of complement-mediated TMA, including HSCT-TMA.
Omeros Corporation, the company developing OMS721, has established a compassionate-use program for OMS721, which is active in the United States and Europe.
Clinical trials
Phase 3 clinical programs are in progress for OMS721 in atypical hemolytic uremic syndrome, immunoglobulin A nephropathy, and HSCT-TMA. Two phase 2 trials of OMS721—one in TMA and one in immunoglobulin A nephropathy—are ongoing.
Omeros released results from the phase 2 TMA trial (NCT02222545) in February.
The study includes adults with HSCT-TMA persisting for at least 2 weeks following immunosuppressive regimen modification or more than 30 days post-transplant. Patients receive weekly OMS721 treatments for 4 to 8 weeks at the discretion of the investigator.
At the time of Omeros’s announcement, 18 HSCT-TMA patients had been treated on this study.
These patients had a significantly longer median overall survival than historical controls—347 days and 21 days, respectively (P<0.0001).
Omeros also reported that markers of TMA activity significantly improved following OMS721 treatment.
The mean platelet count increased from 18,100 x 106/mL at baseline to 52,300 x 106/mL (P=0.017). The mean lactate dehydrogenase decreased from 591 U/L to 250 U/L (P<0.001). And the mean haptoglobin increased from 8 mg/dL to 141 mg/dL (P=0.003).
Mean creatinine remained stable—at approximately 120 μmol/L—but a majority of patients had co-existing conditions for which they were receiving nephrotoxic medications. These conditions included graft-versus-host disease, cytomegalovirus and human herpes virus 6 infections, prior sepsis, diffuse alveolar hemorrhage, and residual underlying malignancies.
The most commonly reported adverse events were diarrhea and neutropenia.
Four deaths occurred. One of these—due to acute renal and respiratory failure—was considered possibly related to OMS721. The other deaths were due to progression of acute myeloid leukemia (n=1) and neutropenic sepsis (n=2).
About orphan and breakthrough designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
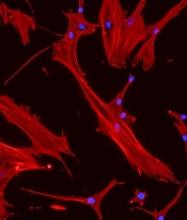
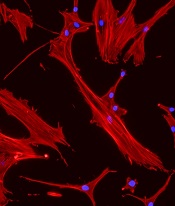
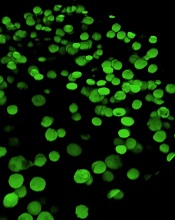
‘Mechanoprimed’ MSCs aid hematopoietic recovery
Specially grown mesenchymal stromal cells (MSCs) can improve hematopoietic recovery, according to preclinical research published in Stem Cell Research and Therapy.
Researchers grew MSCs on a surface with mechanical properties similar to those of bone marrow, which prompted the MSCs to secrete growth factors that aid hematopoietic recovery.
When implanted in irradiated mice, these “mechanoprimed” MSCs sped recovery of all hematopoietic lineages and improved the animals’ survival.
“[MSCs] act like drug factories,” explained study author Krystyn Van Vliet, PhD, of the Massachusetts Institute of Technology in Cambridge.
“They can become tissue lineage cells, but they also pump out a lot of factors that change the environment that the hematopoietic stem cells are operating in.”
Dr. Van Vliet and her colleagues noted that MSCs play an important role in supporting, maintaining, and expanding hematopoietic stem and progenitor cells (HSPCs). However, in a given population of MSCs, usually only about 20% of the cells produce the factors needed to stimulate hematopoietic recovery.
In an earlier study, Dr. Van Vliet and her colleagues showed they could sort MSCs with a microfluidic device that can identify the 20% of cells that promote hematopoietic recovery.
However, the researchers wanted to improve on that by finding a way to stimulate an entire population of MSCs to produce the necessary factors. To do that, they first had to discover which factors were the most important.
Analyses in mice suggested eight factors were associated with improved survival after irradiation—IL-6, IL-8, BMP2, EGF, FGF1, RANTES, VEGF-A, and ANG-1.
Mechanopriming
Having identified factors associated with hematopoietic recovery, Dr. Van Vliet and her colleagues explored the idea of mechanopriming MSCs so they would produce more of these factors.
Over the past decade, researchers have shown that varying the mechanical properties of surfaces on which stem cells are grown can affect their differentiation into mature cell types. However, in this study, the researchers showed that mechanical properties can also affect the factors stem cells secrete before committing to a specific lineage.
For the growth surface, Dr. Van Vliet and her colleagues tested a polymer called polydimethylsiloxane (PDMS). The team varied the mechanical stiffness of the PDMS surface to see how this would affect the MSCs.
MSCs grown on the least stiff PDMS surface produced the greatest number of factors necessary to induce differentiation in HSPCs. These MSCs were able to promote hematopoiesis in an in vitro co-culture model with HSPCs.
Testing in mice
The researchers then tested the mechanoprimed MSCs by implanting them into irradiated mice.
The mechanoprimed MSCs quickly repopulated the animals’ blood cells and helped them recover more quickly than mice treated with MSCs grown on traditional glass surfaces.
Mice that received mechanoprimed MSCs also recovered faster than mice treated with factor-producing MSCs selected by the microfluidic sorting device.
Dr. Van Vliet’s lab is now performing more animal studies in hopes of developing a combination treatment of MSCs and HSPCs that could be tested in humans.
The current research was funded by the National Institutes of Health and the BioSystems and Micromechanics Interdisciplinary Research Group of the Singapore-MIT Alliance for Research and Technology through the Singapore National Research Foundation.
The researchers said they had no competing interests.
Specially grown mesenchymal stromal cells (MSCs) can improve hematopoietic recovery, according to preclinical research published in Stem Cell Research and Therapy.
Researchers grew MSCs on a surface with mechanical properties similar to those of bone marrow, which prompted the MSCs to secrete growth factors that aid hematopoietic recovery.
When implanted in irradiated mice, these “mechanoprimed” MSCs sped recovery of all hematopoietic lineages and improved the animals’ survival.
“[MSCs] act like drug factories,” explained study author Krystyn Van Vliet, PhD, of the Massachusetts Institute of Technology in Cambridge.
“They can become tissue lineage cells, but they also pump out a lot of factors that change the environment that the hematopoietic stem cells are operating in.”
Dr. Van Vliet and her colleagues noted that MSCs play an important role in supporting, maintaining, and expanding hematopoietic stem and progenitor cells (HSPCs). However, in a given population of MSCs, usually only about 20% of the cells produce the factors needed to stimulate hematopoietic recovery.
In an earlier study, Dr. Van Vliet and her colleagues showed they could sort MSCs with a microfluidic device that can identify the 20% of cells that promote hematopoietic recovery.
However, the researchers wanted to improve on that by finding a way to stimulate an entire population of MSCs to produce the necessary factors. To do that, they first had to discover which factors were the most important.
Analyses in mice suggested eight factors were associated with improved survival after irradiation—IL-6, IL-8, BMP2, EGF, FGF1, RANTES, VEGF-A, and ANG-1.
Mechanopriming
Having identified factors associated with hematopoietic recovery, Dr. Van Vliet and her colleagues explored the idea of mechanopriming MSCs so they would produce more of these factors.
Over the past decade, researchers have shown that varying the mechanical properties of surfaces on which stem cells are grown can affect their differentiation into mature cell types. However, in this study, the researchers showed that mechanical properties can also affect the factors stem cells secrete before committing to a specific lineage.
For the growth surface, Dr. Van Vliet and her colleagues tested a polymer called polydimethylsiloxane (PDMS). The team varied the mechanical stiffness of the PDMS surface to see how this would affect the MSCs.
MSCs grown on the least stiff PDMS surface produced the greatest number of factors necessary to induce differentiation in HSPCs. These MSCs were able to promote hematopoiesis in an in vitro co-culture model with HSPCs.
Testing in mice
The researchers then tested the mechanoprimed MSCs by implanting them into irradiated mice.
The mechanoprimed MSCs quickly repopulated the animals’ blood cells and helped them recover more quickly than mice treated with MSCs grown on traditional glass surfaces.
Mice that received mechanoprimed MSCs also recovered faster than mice treated with factor-producing MSCs selected by the microfluidic sorting device.
Dr. Van Vliet’s lab is now performing more animal studies in hopes of developing a combination treatment of MSCs and HSPCs that could be tested in humans.
The current research was funded by the National Institutes of Health and the BioSystems and Micromechanics Interdisciplinary Research Group of the Singapore-MIT Alliance for Research and Technology through the Singapore National Research Foundation.
The researchers said they had no competing interests.
Specially grown mesenchymal stromal cells (MSCs) can improve hematopoietic recovery, according to preclinical research published in Stem Cell Research and Therapy.
Researchers grew MSCs on a surface with mechanical properties similar to those of bone marrow, which prompted the MSCs to secrete growth factors that aid hematopoietic recovery.
When implanted in irradiated mice, these “mechanoprimed” MSCs sped recovery of all hematopoietic lineages and improved the animals’ survival.
“[MSCs] act like drug factories,” explained study author Krystyn Van Vliet, PhD, of the Massachusetts Institute of Technology in Cambridge.
“They can become tissue lineage cells, but they also pump out a lot of factors that change the environment that the hematopoietic stem cells are operating in.”
Dr. Van Vliet and her colleagues noted that MSCs play an important role in supporting, maintaining, and expanding hematopoietic stem and progenitor cells (HSPCs). However, in a given population of MSCs, usually only about 20% of the cells produce the factors needed to stimulate hematopoietic recovery.
In an earlier study, Dr. Van Vliet and her colleagues showed they could sort MSCs with a microfluidic device that can identify the 20% of cells that promote hematopoietic recovery.
However, the researchers wanted to improve on that by finding a way to stimulate an entire population of MSCs to produce the necessary factors. To do that, they first had to discover which factors were the most important.
Analyses in mice suggested eight factors were associated with improved survival after irradiation—IL-6, IL-8, BMP2, EGF, FGF1, RANTES, VEGF-A, and ANG-1.
Mechanopriming
Having identified factors associated with hematopoietic recovery, Dr. Van Vliet and her colleagues explored the idea of mechanopriming MSCs so they would produce more of these factors.
Over the past decade, researchers have shown that varying the mechanical properties of surfaces on which stem cells are grown can affect their differentiation into mature cell types. However, in this study, the researchers showed that mechanical properties can also affect the factors stem cells secrete before committing to a specific lineage.
For the growth surface, Dr. Van Vliet and her colleagues tested a polymer called polydimethylsiloxane (PDMS). The team varied the mechanical stiffness of the PDMS surface to see how this would affect the MSCs.
MSCs grown on the least stiff PDMS surface produced the greatest number of factors necessary to induce differentiation in HSPCs. These MSCs were able to promote hematopoiesis in an in vitro co-culture model with HSPCs.
Testing in mice
The researchers then tested the mechanoprimed MSCs by implanting them into irradiated mice.
The mechanoprimed MSCs quickly repopulated the animals’ blood cells and helped them recover more quickly than mice treated with MSCs grown on traditional glass surfaces.
Mice that received mechanoprimed MSCs also recovered faster than mice treated with factor-producing MSCs selected by the microfluidic sorting device.
Dr. Van Vliet’s lab is now performing more animal studies in hopes of developing a combination treatment of MSCs and HSPCs that could be tested in humans.
The current research was funded by the National Institutes of Health and the BioSystems and Micromechanics Interdisciplinary Research Group of the Singapore-MIT Alliance for Research and Technology through the Singapore National Research Foundation.
The researchers said they had no competing interests.
Engineered MSCs could treat GVHD
LAUSANNE, SWITZERLAND—A mesenchymal stem cell (MSC) product could treat acute graft-versus-host disease (GVHD), according to preclinical research.
The product, apceth-201, improved symptoms of GVHD and prolonged survival in two mouse models.
Researchers described results with apceth-201 in a poster presentation at the Annual Congress of the European Society of Gene and Cell Therapy.
Most of the researchers involved in this study work for apceth Biopharma, the company developing apceth-201.
Apceth-201 consists of allogeneic human MSCs that have been genetically modified to express alpha-1 antitrypsin, a protease inhibitor exerting anti-inflammatory and tissue-protective functions.
In vitro assays showed that apceth-201 suppresses T-cell proliferation, polarizes macrophages to an anti-inflammatory M2 type, converts dendritic cells to a tolerogenic phenotype, and increases induction of regulatory T cells.
Apeceth-201 also demonstrated activity in vivo.
In a humanized GVHD model, treatment with apceth-201 improved bone marrow cellularity and reduced levels of inflammatory markers.
Additionally, mice treated with apceth-201 had double the median survival of mice treated with native MSCs.
Researchers also tested the effects of apceth-201 against GVHD in a model of haploidentical hematopoietic stem cell transplant.
All control mice succumbed to GVHD within 22 days, but more than half of mice treated with apceth-201 survived until the end of the experiment, which was 100 days.
All of the survivors had complete resolution of GVHD symptoms.
The researchers also said apceth-201 was safe. It did not impair T-cell-dependent antibody responses, and host resistance was similar in treated mice and controls.
“We are very excited with these results that clearly show the transformative therapeutic potential of apceth-201 in an immune-mediated disease with high unmet medical need and few treatment options,” said Christine Guenther, CEO of apceth Biopharma.
“Based on these promising and impressive data, we are currently preparing to initiate a phase 1/2 clinical study assessing the safety and efficacy of apceth-201 in adult steroid-refractory GVHD patients.”
LAUSANNE, SWITZERLAND—A mesenchymal stem cell (MSC) product could treat acute graft-versus-host disease (GVHD), according to preclinical research.
The product, apceth-201, improved symptoms of GVHD and prolonged survival in two mouse models.
Researchers described results with apceth-201 in a poster presentation at the Annual Congress of the European Society of Gene and Cell Therapy.
Most of the researchers involved in this study work for apceth Biopharma, the company developing apceth-201.
Apceth-201 consists of allogeneic human MSCs that have been genetically modified to express alpha-1 antitrypsin, a protease inhibitor exerting anti-inflammatory and tissue-protective functions.
In vitro assays showed that apceth-201 suppresses T-cell proliferation, polarizes macrophages to an anti-inflammatory M2 type, converts dendritic cells to a tolerogenic phenotype, and increases induction of regulatory T cells.
Apeceth-201 also demonstrated activity in vivo.
In a humanized GVHD model, treatment with apceth-201 improved bone marrow cellularity and reduced levels of inflammatory markers.
Additionally, mice treated with apceth-201 had double the median survival of mice treated with native MSCs.
Researchers also tested the effects of apceth-201 against GVHD in a model of haploidentical hematopoietic stem cell transplant.
All control mice succumbed to GVHD within 22 days, but more than half of mice treated with apceth-201 survived until the end of the experiment, which was 100 days.
All of the survivors had complete resolution of GVHD symptoms.
The researchers also said apceth-201 was safe. It did not impair T-cell-dependent antibody responses, and host resistance was similar in treated mice and controls.
“We are very excited with these results that clearly show the transformative therapeutic potential of apceth-201 in an immune-mediated disease with high unmet medical need and few treatment options,” said Christine Guenther, CEO of apceth Biopharma.
“Based on these promising and impressive data, we are currently preparing to initiate a phase 1/2 clinical study assessing the safety and efficacy of apceth-201 in adult steroid-refractory GVHD patients.”
LAUSANNE, SWITZERLAND—A mesenchymal stem cell (MSC) product could treat acute graft-versus-host disease (GVHD), according to preclinical research.
The product, apceth-201, improved symptoms of GVHD and prolonged survival in two mouse models.
Researchers described results with apceth-201 in a poster presentation at the Annual Congress of the European Society of Gene and Cell Therapy.
Most of the researchers involved in this study work for apceth Biopharma, the company developing apceth-201.
Apceth-201 consists of allogeneic human MSCs that have been genetically modified to express alpha-1 antitrypsin, a protease inhibitor exerting anti-inflammatory and tissue-protective functions.
In vitro assays showed that apceth-201 suppresses T-cell proliferation, polarizes macrophages to an anti-inflammatory M2 type, converts dendritic cells to a tolerogenic phenotype, and increases induction of regulatory T cells.
Apeceth-201 also demonstrated activity in vivo.
In a humanized GVHD model, treatment with apceth-201 improved bone marrow cellularity and reduced levels of inflammatory markers.
Additionally, mice treated with apceth-201 had double the median survival of mice treated with native MSCs.
Researchers also tested the effects of apceth-201 against GVHD in a model of haploidentical hematopoietic stem cell transplant.
All control mice succumbed to GVHD within 22 days, but more than half of mice treated with apceth-201 survived until the end of the experiment, which was 100 days.
All of the survivors had complete resolution of GVHD symptoms.
The researchers also said apceth-201 was safe. It did not impair T-cell-dependent antibody responses, and host resistance was similar in treated mice and controls.
“We are very excited with these results that clearly show the transformative therapeutic potential of apceth-201 in an immune-mediated disease with high unmet medical need and few treatment options,” said Christine Guenther, CEO of apceth Biopharma.
“Based on these promising and impressive data, we are currently preparing to initiate a phase 1/2 clinical study assessing the safety and efficacy of apceth-201 in adult steroid-refractory GVHD patients.”
Inhibitor could improve HSC donation and transplant
Preclinical research suggests a small-molecule inhibitor could potentially improve the donation and transplant of hematopoietic stem cells (HSCs).
One study showed that the inhibitor, CASIN, could improve HSC yields from murine transplant donors.
Another study showed that CASIN could be used as conditioning, with or without fludarabine, in murine transplant recipients.
Yi Zheng, PhD, of Cincinnati Children’s Cancer and Blood Diseases Institute in Ohio, and his colleagues conducted both studies and reported the results in Leukemia.
Previous research had shown that genetic ablation of CDC42 in HSCs mobilizes the cells without affecting their survival. CDC42 is a Rho family small GTPase that helps regulate HSC maintenance.
Dr. Zheng and his colleagues expanded upon this finding with two studies.
In the first study, the researchers identified CASIN, a small-molecule inhibitor of CDC42. The team tested CASIN in mice and found the inhibitor can effectively mobilize HSCs.
In fact, CASIN and plerixafor mobilized a similar number of phenotypic HSCs. However, HSCs harvested from CASIN-treated donor mice had better long-term reconstitution potential after transplant than HSCs harvested from plerixafor-treated mice.
In the second study, Dr. Zheng and his colleagues used CASIN to condition mice that were receiving HSC transplants.
The team found that CASIN reduced the number of phenotypic long-term HSCs in the bone marrow, starting 2 hours after CASIN administration and ending within 24 hours.
The researchers also found that CASIN synergized with fludarabine. Engraftment of transplanted HSCs was significantly higher in mice that received conditioning with CASIN and fludarabine than in mice that received either CASIN or fludarabine alone.
“Our data demonstrate that the new regimen of CASIN application has the potential to improve both sides of the transplant practice,” Dr. Zheng said. “It mobilizes higher quality donor HSCs during stem cell harvest, and it would condition transplant patients beforehand to increase engraftment efficiency.”
“This would be a major step forward, especially for the most vulnerable patients who cannot withstand the toxicity of chemotherapy conditioning regimens or are non-responsive to current [HSC] mobilization regimens.”
Both of these studies were funded, in part, by the National Institutes of Health. The authors declared no conflicts of interest.
Preclinical research suggests a small-molecule inhibitor could potentially improve the donation and transplant of hematopoietic stem cells (HSCs).
One study showed that the inhibitor, CASIN, could improve HSC yields from murine transplant donors.
Another study showed that CASIN could be used as conditioning, with or without fludarabine, in murine transplant recipients.
Yi Zheng, PhD, of Cincinnati Children’s Cancer and Blood Diseases Institute in Ohio, and his colleagues conducted both studies and reported the results in Leukemia.
Previous research had shown that genetic ablation of CDC42 in HSCs mobilizes the cells without affecting their survival. CDC42 is a Rho family small GTPase that helps regulate HSC maintenance.
Dr. Zheng and his colleagues expanded upon this finding with two studies.
In the first study, the researchers identified CASIN, a small-molecule inhibitor of CDC42. The team tested CASIN in mice and found the inhibitor can effectively mobilize HSCs.
In fact, CASIN and plerixafor mobilized a similar number of phenotypic HSCs. However, HSCs harvested from CASIN-treated donor mice had better long-term reconstitution potential after transplant than HSCs harvested from plerixafor-treated mice.
In the second study, Dr. Zheng and his colleagues used CASIN to condition mice that were receiving HSC transplants.
The team found that CASIN reduced the number of phenotypic long-term HSCs in the bone marrow, starting 2 hours after CASIN administration and ending within 24 hours.
The researchers also found that CASIN synergized with fludarabine. Engraftment of transplanted HSCs was significantly higher in mice that received conditioning with CASIN and fludarabine than in mice that received either CASIN or fludarabine alone.
“Our data demonstrate that the new regimen of CASIN application has the potential to improve both sides of the transplant practice,” Dr. Zheng said. “It mobilizes higher quality donor HSCs during stem cell harvest, and it would condition transplant patients beforehand to increase engraftment efficiency.”
“This would be a major step forward, especially for the most vulnerable patients who cannot withstand the toxicity of chemotherapy conditioning regimens or are non-responsive to current [HSC] mobilization regimens.”
Both of these studies were funded, in part, by the National Institutes of Health. The authors declared no conflicts of interest.
Preclinical research suggests a small-molecule inhibitor could potentially improve the donation and transplant of hematopoietic stem cells (HSCs).
One study showed that the inhibitor, CASIN, could improve HSC yields from murine transplant donors.
Another study showed that CASIN could be used as conditioning, with or without fludarabine, in murine transplant recipients.
Yi Zheng, PhD, of Cincinnati Children’s Cancer and Blood Diseases Institute in Ohio, and his colleagues conducted both studies and reported the results in Leukemia.
Previous research had shown that genetic ablation of CDC42 in HSCs mobilizes the cells without affecting their survival. CDC42 is a Rho family small GTPase that helps regulate HSC maintenance.
Dr. Zheng and his colleagues expanded upon this finding with two studies.
In the first study, the researchers identified CASIN, a small-molecule inhibitor of CDC42. The team tested CASIN in mice and found the inhibitor can effectively mobilize HSCs.
In fact, CASIN and plerixafor mobilized a similar number of phenotypic HSCs. However, HSCs harvested from CASIN-treated donor mice had better long-term reconstitution potential after transplant than HSCs harvested from plerixafor-treated mice.
In the second study, Dr. Zheng and his colleagues used CASIN to condition mice that were receiving HSC transplants.
The team found that CASIN reduced the number of phenotypic long-term HSCs in the bone marrow, starting 2 hours after CASIN administration and ending within 24 hours.
The researchers also found that CASIN synergized with fludarabine. Engraftment of transplanted HSCs was significantly higher in mice that received conditioning with CASIN and fludarabine than in mice that received either CASIN or fludarabine alone.
“Our data demonstrate that the new regimen of CASIN application has the potential to improve both sides of the transplant practice,” Dr. Zheng said. “It mobilizes higher quality donor HSCs during stem cell harvest, and it would condition transplant patients beforehand to increase engraftment efficiency.”
“This would be a major step forward, especially for the most vulnerable patients who cannot withstand the toxicity of chemotherapy conditioning regimens or are non-responsive to current [HSC] mobilization regimens.”
Both of these studies were funded, in part, by the National Institutes of Health. The authors declared no conflicts of interest.