User login
Anti-GM-CSF antibody reduced CAR T-cell toxicity
HOUSTON – Neutralizing granulocyte-macrophage colony-stimulating factor (GM-CSF) may be an effective strategy not only to manage toxicities associated with chimeric antigen receptor (CAR) T-cell therapy, but also to enhance CAR-T cell function, an investigator reported at the Transplantation & Cellular Therapy Meetings.
The GM-CSF targeted monoclonal antibody lenzilumab reduced neurotoxicity and cytokine release syndrome (CRS) related to CD19-targeted CAR T-cell therapy in a patient-derived xenograft model, said investigator Rosalie M. Sterner, an MD-PhD student in the department of immunology at Mayo Clinic, Rochester, Minn.
Other investigations showed that neutralizing or knocking out GM-CSF enhanced the antitumor functions of the CAR T cells, Ms. Sterner said in a podium presentation at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
“GM-CSF blockade does not impair CAR T-cell effector function, and in fact, enhances CAR T-cell effector functions in certain models, and actually can help to ameliorate CAR T-cell associated toxicities,” Ms. Sterner said.
Based on these early findings, the investigators have designed a phase 2 clinical trial to see if lenzilumab can prevent CAR T cell-related toxicities in patients with diffuse large B-cell lymphoma.
GM-CSF, a cytokine produced by T cells and myeloid cells, is the most statistically significantly elevated serum marker in patients with severe neurotoxicity related to CAR T-cell therapy, Ms. Sterner told attendees.
Investigations have shown that the combination of lenzilumab plus CD19-targeted T-cell therapy did not impair CAR T-cell function in vivo or in vitro, she said.
In other studies, they investigated the impact of GM-CSF neutralization in mice engrafted with primary acute lymphocytic leukemia (ALL) blasts and treated with high doses of CD19 CAR T-cells, lenzilumab, and a murine GM-CSF blocking antibody to neutralize the mouse GM-CSF. That strategy prevented weight loss, decreased myeloid cytokines, reduced cerebral edema, and enhanced disease control, Ms. Sterner said.
Investigators also reported on CD19 CAR T-cells with reduced GM-CSF secretion due to CRISPR/Cas9 gene editing of the GM-CSF gene during the CAR T-cell manufacturing process. Xenograft model results showed a slight enhancement of disease control for those GM-CSF knockout CAR T cells versus standard CAR T cells.
More details of the investigations were recently published in Blood (2019;133:697-709).
Taken together, the investigations highlight GM-CSF inhibition as a novel approach to reducing neurotoxicity and CRS that may also enhance CAR T-cell effector functions, Ms. Sterner said.
Ms. Sterner reported having no financial disclosures related to her presentation.
SOURCE: Sterner R et al. TCT 2019, Abstract 5.
HOUSTON – Neutralizing granulocyte-macrophage colony-stimulating factor (GM-CSF) may be an effective strategy not only to manage toxicities associated with chimeric antigen receptor (CAR) T-cell therapy, but also to enhance CAR-T cell function, an investigator reported at the Transplantation & Cellular Therapy Meetings.
The GM-CSF targeted monoclonal antibody lenzilumab reduced neurotoxicity and cytokine release syndrome (CRS) related to CD19-targeted CAR T-cell therapy in a patient-derived xenograft model, said investigator Rosalie M. Sterner, an MD-PhD student in the department of immunology at Mayo Clinic, Rochester, Minn.
Other investigations showed that neutralizing or knocking out GM-CSF enhanced the antitumor functions of the CAR T cells, Ms. Sterner said in a podium presentation at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
“GM-CSF blockade does not impair CAR T-cell effector function, and in fact, enhances CAR T-cell effector functions in certain models, and actually can help to ameliorate CAR T-cell associated toxicities,” Ms. Sterner said.
Based on these early findings, the investigators have designed a phase 2 clinical trial to see if lenzilumab can prevent CAR T cell-related toxicities in patients with diffuse large B-cell lymphoma.
GM-CSF, a cytokine produced by T cells and myeloid cells, is the most statistically significantly elevated serum marker in patients with severe neurotoxicity related to CAR T-cell therapy, Ms. Sterner told attendees.
Investigations have shown that the combination of lenzilumab plus CD19-targeted T-cell therapy did not impair CAR T-cell function in vivo or in vitro, she said.
In other studies, they investigated the impact of GM-CSF neutralization in mice engrafted with primary acute lymphocytic leukemia (ALL) blasts and treated with high doses of CD19 CAR T-cells, lenzilumab, and a murine GM-CSF blocking antibody to neutralize the mouse GM-CSF. That strategy prevented weight loss, decreased myeloid cytokines, reduced cerebral edema, and enhanced disease control, Ms. Sterner said.
Investigators also reported on CD19 CAR T-cells with reduced GM-CSF secretion due to CRISPR/Cas9 gene editing of the GM-CSF gene during the CAR T-cell manufacturing process. Xenograft model results showed a slight enhancement of disease control for those GM-CSF knockout CAR T cells versus standard CAR T cells.
More details of the investigations were recently published in Blood (2019;133:697-709).
Taken together, the investigations highlight GM-CSF inhibition as a novel approach to reducing neurotoxicity and CRS that may also enhance CAR T-cell effector functions, Ms. Sterner said.
Ms. Sterner reported having no financial disclosures related to her presentation.
SOURCE: Sterner R et al. TCT 2019, Abstract 5.
HOUSTON – Neutralizing granulocyte-macrophage colony-stimulating factor (GM-CSF) may be an effective strategy not only to manage toxicities associated with chimeric antigen receptor (CAR) T-cell therapy, but also to enhance CAR-T cell function, an investigator reported at the Transplantation & Cellular Therapy Meetings.
The GM-CSF targeted monoclonal antibody lenzilumab reduced neurotoxicity and cytokine release syndrome (CRS) related to CD19-targeted CAR T-cell therapy in a patient-derived xenograft model, said investigator Rosalie M. Sterner, an MD-PhD student in the department of immunology at Mayo Clinic, Rochester, Minn.
Other investigations showed that neutralizing or knocking out GM-CSF enhanced the antitumor functions of the CAR T cells, Ms. Sterner said in a podium presentation at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
“GM-CSF blockade does not impair CAR T-cell effector function, and in fact, enhances CAR T-cell effector functions in certain models, and actually can help to ameliorate CAR T-cell associated toxicities,” Ms. Sterner said.
Based on these early findings, the investigators have designed a phase 2 clinical trial to see if lenzilumab can prevent CAR T cell-related toxicities in patients with diffuse large B-cell lymphoma.
GM-CSF, a cytokine produced by T cells and myeloid cells, is the most statistically significantly elevated serum marker in patients with severe neurotoxicity related to CAR T-cell therapy, Ms. Sterner told attendees.
Investigations have shown that the combination of lenzilumab plus CD19-targeted T-cell therapy did not impair CAR T-cell function in vivo or in vitro, she said.
In other studies, they investigated the impact of GM-CSF neutralization in mice engrafted with primary acute lymphocytic leukemia (ALL) blasts and treated with high doses of CD19 CAR T-cells, lenzilumab, and a murine GM-CSF blocking antibody to neutralize the mouse GM-CSF. That strategy prevented weight loss, decreased myeloid cytokines, reduced cerebral edema, and enhanced disease control, Ms. Sterner said.
Investigators also reported on CD19 CAR T-cells with reduced GM-CSF secretion due to CRISPR/Cas9 gene editing of the GM-CSF gene during the CAR T-cell manufacturing process. Xenograft model results showed a slight enhancement of disease control for those GM-CSF knockout CAR T cells versus standard CAR T cells.
More details of the investigations were recently published in Blood (2019;133:697-709).
Taken together, the investigations highlight GM-CSF inhibition as a novel approach to reducing neurotoxicity and CRS that may also enhance CAR T-cell effector functions, Ms. Sterner said.
Ms. Sterner reported having no financial disclosures related to her presentation.
SOURCE: Sterner R et al. TCT 2019, Abstract 5.
REPORTING FROM TCT 2019
Treosulfan may become standard in allo-HCT for AML/MDS
HOUSTON – A treosulfan-based conditioning regimen could become standard prior to allogeneic transplant in elderly or comorbid patients with acute myeloid leukemia or myelodysplastic syndromes, according to the lead investigator in a phase 3 trial.
The treosulfan/fludarabine myeloablative conditioning regimen had noninferior event-free survival, compared with a reduced-intensity busulfan-based regimen in the large, randomized trial that included elderly patients and those with multiple comorbidities, said researcher Dietrich Wilhelm Beelen, MD, PhD.
The experimental regimen was superior to busulfan in overall survival, nonrelapse mortality, and complete donor chimerism in the trial, added Dr. Beelen, who is with the department of bone marrow transplantation at the West German Cancer Center, University Hospital of Essen, Germany.
“The study results point to a potential benefit of the treosulfan/fludarabine regimen, while the early safety profile, engraftment kinetics, acute or chronic graft-versus-host-disease (GvHD), and the relapse risk of both regimens appear comparable,” Dr. Beelen said at the Transplantation & Cellular Therapy Meetings.
Allogeneic hematopoietic cell transplantation (HCT) is challenging in elderly and comorbid patients, who have an increased risk of nonrelapse mortality with standard myeloablative regimens, according to Dr. Beelen, who presented results on behalf of investigators from the international MC-FludT.14/L Study Group.
Their phase 3 randomized trial included patients who were 50-70 years of age, or who had a Hematopoietic Cell Transplantation Comorbidity Index of 2 or greater. The final analysis included 551 patients (352 with AML and 199 with MDS).
The primary endpoint of the study was event-free survival at 2 years. That endpoint comprised relapse/progression of disease, graft failure, or death.
Patient enrollment was terminated early the MC-FludT.14/L study following an interim analysis that investigators said “clearly demonstrated” the noninferiority of the treosulfan/fludarabine regimen versus the reduced intensity busulfan/fludarabine regimen.
In the final analysis, event-free survival at 2 years was about 14.5 percentage points higher in the treosulfan group, at 65.7% versus 51.2% (P = .0000001), Dr. Beelen reported at the meeting.
A number of other secondary endpoints also favored treosulfan/fludarabine over busulfan, including overall survival (P = .0037), nonrelapse mortality (P = .0343), and survival free of chronic GvHD or relapse (P = .0030).
These results help establish the new treosulfan/fludarabine regimen as a “relatively well-tolerable and effective preparative regimen” in elderly or comorbid AML/MDS patients, Dr. Beelen said.
However, treosulfan has not been authorized for use in allogeneic HCT conditioning regimens, and so should be considered experimental in this setting, he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Beelen reported honoraria, travel support, and trial documentation support provided by medac GmbH, which sponsored the trial.
SOURCE: Beelen DW et al. TCT 2019, Abstract 4.
HOUSTON – A treosulfan-based conditioning regimen could become standard prior to allogeneic transplant in elderly or comorbid patients with acute myeloid leukemia or myelodysplastic syndromes, according to the lead investigator in a phase 3 trial.
The treosulfan/fludarabine myeloablative conditioning regimen had noninferior event-free survival, compared with a reduced-intensity busulfan-based regimen in the large, randomized trial that included elderly patients and those with multiple comorbidities, said researcher Dietrich Wilhelm Beelen, MD, PhD.
The experimental regimen was superior to busulfan in overall survival, nonrelapse mortality, and complete donor chimerism in the trial, added Dr. Beelen, who is with the department of bone marrow transplantation at the West German Cancer Center, University Hospital of Essen, Germany.
“The study results point to a potential benefit of the treosulfan/fludarabine regimen, while the early safety profile, engraftment kinetics, acute or chronic graft-versus-host-disease (GvHD), and the relapse risk of both regimens appear comparable,” Dr. Beelen said at the Transplantation & Cellular Therapy Meetings.
Allogeneic hematopoietic cell transplantation (HCT) is challenging in elderly and comorbid patients, who have an increased risk of nonrelapse mortality with standard myeloablative regimens, according to Dr. Beelen, who presented results on behalf of investigators from the international MC-FludT.14/L Study Group.
Their phase 3 randomized trial included patients who were 50-70 years of age, or who had a Hematopoietic Cell Transplantation Comorbidity Index of 2 or greater. The final analysis included 551 patients (352 with AML and 199 with MDS).
The primary endpoint of the study was event-free survival at 2 years. That endpoint comprised relapse/progression of disease, graft failure, or death.
Patient enrollment was terminated early the MC-FludT.14/L study following an interim analysis that investigators said “clearly demonstrated” the noninferiority of the treosulfan/fludarabine regimen versus the reduced intensity busulfan/fludarabine regimen.
In the final analysis, event-free survival at 2 years was about 14.5 percentage points higher in the treosulfan group, at 65.7% versus 51.2% (P = .0000001), Dr. Beelen reported at the meeting.
A number of other secondary endpoints also favored treosulfan/fludarabine over busulfan, including overall survival (P = .0037), nonrelapse mortality (P = .0343), and survival free of chronic GvHD or relapse (P = .0030).
These results help establish the new treosulfan/fludarabine regimen as a “relatively well-tolerable and effective preparative regimen” in elderly or comorbid AML/MDS patients, Dr. Beelen said.
However, treosulfan has not been authorized for use in allogeneic HCT conditioning regimens, and so should be considered experimental in this setting, he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Beelen reported honoraria, travel support, and trial documentation support provided by medac GmbH, which sponsored the trial.
SOURCE: Beelen DW et al. TCT 2019, Abstract 4.
HOUSTON – A treosulfan-based conditioning regimen could become standard prior to allogeneic transplant in elderly or comorbid patients with acute myeloid leukemia or myelodysplastic syndromes, according to the lead investigator in a phase 3 trial.
The treosulfan/fludarabine myeloablative conditioning regimen had noninferior event-free survival, compared with a reduced-intensity busulfan-based regimen in the large, randomized trial that included elderly patients and those with multiple comorbidities, said researcher Dietrich Wilhelm Beelen, MD, PhD.
The experimental regimen was superior to busulfan in overall survival, nonrelapse mortality, and complete donor chimerism in the trial, added Dr. Beelen, who is with the department of bone marrow transplantation at the West German Cancer Center, University Hospital of Essen, Germany.
“The study results point to a potential benefit of the treosulfan/fludarabine regimen, while the early safety profile, engraftment kinetics, acute or chronic graft-versus-host-disease (GvHD), and the relapse risk of both regimens appear comparable,” Dr. Beelen said at the Transplantation & Cellular Therapy Meetings.
Allogeneic hematopoietic cell transplantation (HCT) is challenging in elderly and comorbid patients, who have an increased risk of nonrelapse mortality with standard myeloablative regimens, according to Dr. Beelen, who presented results on behalf of investigators from the international MC-FludT.14/L Study Group.
Their phase 3 randomized trial included patients who were 50-70 years of age, or who had a Hematopoietic Cell Transplantation Comorbidity Index of 2 or greater. The final analysis included 551 patients (352 with AML and 199 with MDS).
The primary endpoint of the study was event-free survival at 2 years. That endpoint comprised relapse/progression of disease, graft failure, or death.
Patient enrollment was terminated early the MC-FludT.14/L study following an interim analysis that investigators said “clearly demonstrated” the noninferiority of the treosulfan/fludarabine regimen versus the reduced intensity busulfan/fludarabine regimen.
In the final analysis, event-free survival at 2 years was about 14.5 percentage points higher in the treosulfan group, at 65.7% versus 51.2% (P = .0000001), Dr. Beelen reported at the meeting.
A number of other secondary endpoints also favored treosulfan/fludarabine over busulfan, including overall survival (P = .0037), nonrelapse mortality (P = .0343), and survival free of chronic GvHD or relapse (P = .0030).
These results help establish the new treosulfan/fludarabine regimen as a “relatively well-tolerable and effective preparative regimen” in elderly or comorbid AML/MDS patients, Dr. Beelen said.
However, treosulfan has not been authorized for use in allogeneic HCT conditioning regimens, and so should be considered experimental in this setting, he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Beelen reported honoraria, travel support, and trial documentation support provided by medac GmbH, which sponsored the trial.
SOURCE: Beelen DW et al. TCT 2019, Abstract 4.
REPORTING FROM TCT 2019
Ultrasound method predicts liver complications in pediatric transplant
HOUSTON – An ultrasound method for assessing liver stiffness might be useful for predicting which pediatric patients will develop a life-threatening complication of hematopoietic stem cell transplantation.
Shear wave elastography values predicted severe hepatic sinusoidal obstruction syndrome/veno-occlusive disease (SOS/VOD) at least 4 days before standard diagnostic criteria in most patients treated in a small, prospective, two-center study, Sherwin S. Chan, MD, PhD, said at the Transplantation & Cellular Therapy Meetings.
Early identification of SOS/VOD using elastography could be beneficial in light of data showing that timing is critical in the administration of defibrotide, a treatment recommended for severe and very severe patients, according to Dr. Chan, vice chair of radiology for the University of Missouri at Kansas City.
“If you’re able to initiate it early, you can really increase day 100 survival,” Dr. Chan said in an oral presentation.
The data presented included 54 pediatric patients undergoing transplantation at one of two institutions.
At one site, the patients underwent shear wave elastography evaluation 10 days before the conditioning regimen began, and again at 5 and 14 days after the transplant. At the other site, patients with suspected SOS/VOD were enrolled and underwent elastography every other day for up to 10 exams.
Those are very different imaging protocols, Dr. Chan acknowledged in his presentation, noting that the studies started independently and data were pooled as investigators at the two institutions became aware of one another’s work.
A total of 16 patients, or 30%, developed SOS/VOD, Dr. Chan reported. Of those 16 cases, 12 (75%) were severe or very severe by the recent European Society for Blood and Marrow Transplantation (EBMT) criteria.
Increased shear wave elastography velocity was the best predictor of severe SOS/VOD, according to Dr. Chan, with a cutoff value of 1.65 m/s being 92% sensitive and 67% specific for severe SOS/VOD.
That threshold was passed at least 4 days before severe grading or death in 9 out of the 12 severe cases, he added.
Accordingly, a prospective, multicenter trial has been initiated at a number of U.S. centers to investigate whether the findings of this study are generalizable to other patient populations, Dr. Chan said at the meeting held by the American Society of Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At this meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy.
That prospective, multicenter trial is supported by Jazz Pharmaceuticals, according to Dr. Chan, who reported consulting with Jazz Pharmaceuticals in his disclosure statement.
SOURCE: Chan SS et al. TCT 2019, Abstract 55.
HOUSTON – An ultrasound method for assessing liver stiffness might be useful for predicting which pediatric patients will develop a life-threatening complication of hematopoietic stem cell transplantation.
Shear wave elastography values predicted severe hepatic sinusoidal obstruction syndrome/veno-occlusive disease (SOS/VOD) at least 4 days before standard diagnostic criteria in most patients treated in a small, prospective, two-center study, Sherwin S. Chan, MD, PhD, said at the Transplantation & Cellular Therapy Meetings.
Early identification of SOS/VOD using elastography could be beneficial in light of data showing that timing is critical in the administration of defibrotide, a treatment recommended for severe and very severe patients, according to Dr. Chan, vice chair of radiology for the University of Missouri at Kansas City.
“If you’re able to initiate it early, you can really increase day 100 survival,” Dr. Chan said in an oral presentation.
The data presented included 54 pediatric patients undergoing transplantation at one of two institutions.
At one site, the patients underwent shear wave elastography evaluation 10 days before the conditioning regimen began, and again at 5 and 14 days after the transplant. At the other site, patients with suspected SOS/VOD were enrolled and underwent elastography every other day for up to 10 exams.
Those are very different imaging protocols, Dr. Chan acknowledged in his presentation, noting that the studies started independently and data were pooled as investigators at the two institutions became aware of one another’s work.
A total of 16 patients, or 30%, developed SOS/VOD, Dr. Chan reported. Of those 16 cases, 12 (75%) were severe or very severe by the recent European Society for Blood and Marrow Transplantation (EBMT) criteria.
Increased shear wave elastography velocity was the best predictor of severe SOS/VOD, according to Dr. Chan, with a cutoff value of 1.65 m/s being 92% sensitive and 67% specific for severe SOS/VOD.
That threshold was passed at least 4 days before severe grading or death in 9 out of the 12 severe cases, he added.
Accordingly, a prospective, multicenter trial has been initiated at a number of U.S. centers to investigate whether the findings of this study are generalizable to other patient populations, Dr. Chan said at the meeting held by the American Society of Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At this meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy.
That prospective, multicenter trial is supported by Jazz Pharmaceuticals, according to Dr. Chan, who reported consulting with Jazz Pharmaceuticals in his disclosure statement.
SOURCE: Chan SS et al. TCT 2019, Abstract 55.
HOUSTON – An ultrasound method for assessing liver stiffness might be useful for predicting which pediatric patients will develop a life-threatening complication of hematopoietic stem cell transplantation.
Shear wave elastography values predicted severe hepatic sinusoidal obstruction syndrome/veno-occlusive disease (SOS/VOD) at least 4 days before standard diagnostic criteria in most patients treated in a small, prospective, two-center study, Sherwin S. Chan, MD, PhD, said at the Transplantation & Cellular Therapy Meetings.
Early identification of SOS/VOD using elastography could be beneficial in light of data showing that timing is critical in the administration of defibrotide, a treatment recommended for severe and very severe patients, according to Dr. Chan, vice chair of radiology for the University of Missouri at Kansas City.
“If you’re able to initiate it early, you can really increase day 100 survival,” Dr. Chan said in an oral presentation.
The data presented included 54 pediatric patients undergoing transplantation at one of two institutions.
At one site, the patients underwent shear wave elastography evaluation 10 days before the conditioning regimen began, and again at 5 and 14 days after the transplant. At the other site, patients with suspected SOS/VOD were enrolled and underwent elastography every other day for up to 10 exams.
Those are very different imaging protocols, Dr. Chan acknowledged in his presentation, noting that the studies started independently and data were pooled as investigators at the two institutions became aware of one another’s work.
A total of 16 patients, or 30%, developed SOS/VOD, Dr. Chan reported. Of those 16 cases, 12 (75%) were severe or very severe by the recent European Society for Blood and Marrow Transplantation (EBMT) criteria.
Increased shear wave elastography velocity was the best predictor of severe SOS/VOD, according to Dr. Chan, with a cutoff value of 1.65 m/s being 92% sensitive and 67% specific for severe SOS/VOD.
That threshold was passed at least 4 days before severe grading or death in 9 out of the 12 severe cases, he added.
Accordingly, a prospective, multicenter trial has been initiated at a number of U.S. centers to investigate whether the findings of this study are generalizable to other patient populations, Dr. Chan said at the meeting held by the American Society of Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At this meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy.
That prospective, multicenter trial is supported by Jazz Pharmaceuticals, according to Dr. Chan, who reported consulting with Jazz Pharmaceuticals in his disclosure statement.
SOURCE: Chan SS et al. TCT 2019, Abstract 55.
REPORTING FROM TCT 2019
Haplo-HCT shows viability in DLBCL
For patients with diffuse large B-cell lymphoma (DLBCL) who need allogeneic hematopoietic cell transplantation (allo-HCT), a haploidentical family member could be a viable donor, according to a retrospective study of 1,438 patients.
When combined with nonmyeloablative/reduced intensity conditioning (NMC/RIC) and posttransplant cyclophosphamide (PTCy), patients treated with haploidentical HCT (haplo-HCT) had outcomes similar to those seen in patients with matched donors, reported Peter Dreger, MD, of the University of Heidelberg (Germany) and his colleagues.
“Using well-matched sibling donors (MSDs) or unrelated donors (MUDs), allo-HCT can result in sustained disease control in 30% to 45% of patients with DLBCL who have early disease recurrence after standard chemoimmunotherapy or have failed auto-HCT [autologous HCT],” the investigators wrote in Blood Advances. “However, the search for a well-matched unrelated donor could be time-consuming and unsuccessful in up to 50% of the patients in need.”
But the present findings suggest that haplo-HCT may one day improve these odds by providing a larger pool of potential donors.
The patients in the study were divided into four treatment groups: haplo-HCT (n = 132), MSD (n = 525), MUD with T-cell depletion (n = 403), and MUD without T-cell depletion (n = 378). For graft-versus-host disease (GVHD) prophylaxis, patients in the haplo-HCT group received PTCy, with or without a calcineurin inhibitor and mycophenolate mofetil, whereas all patients with matched donors received a calcineurin inhibitor. T-cell depletion was accomplished by in vivo antithymocyte globulin and alemtuzumab.
The primary end point was overall survival (OS). Secondary end points were progression-free survival (PFS), progression/relapse, and nonrelapse mortality (NRM).
After a median follow-up of 4.1 years, all groups had similar outcomes, without statistical differences in multivariable analysis.
In the haplo-HCT group, the 3-year OS rate was 46%, the NRM rate was 22%, the PFS rate was 38%, and the relapse/progression rate was 41%.
Of note, patients receiving haplo-HCT did have a lower cumulative incidence of chronic GVHD, at 15% after 1 year and 18% after 2 years. These rates were significantly lower than the other groups’ 1- and 2-year GVHD rates, which were as follows: MSD, 41% and 48%; MUD with T-cell depletion, 23% and 27%; and MUD without T-cell depletion, 48% and 57%.
The investigators noted that these disparities may actually be caused by the use of bone marrow grafts in the haplo-HCT group instead of peripheral blood grafts, which were used in most of the patients in the other groups.
Overall, the findings were encouraging, but the investigators cautioned that “additional studies are needed before haploidentical donors can be considered as equivalent to well-matched related or unrelated donors in patients with DLBCL.”
The study was funded by the Center for International Blood & Marrow Transplant Research (CIBMTR) and the European Society for Blood and Marrow Transplantation. CIBMTR is supported by grants from the U.S. government and the pharmaceutical industry. The authors reported having no competing financial interests.
SOURCE: Dreger P et al. Blood Adv. 2019 Feb 12;3(3):360-9.
For patients with diffuse large B-cell lymphoma (DLBCL) who need allogeneic hematopoietic cell transplantation (allo-HCT), a haploidentical family member could be a viable donor, according to a retrospective study of 1,438 patients.
When combined with nonmyeloablative/reduced intensity conditioning (NMC/RIC) and posttransplant cyclophosphamide (PTCy), patients treated with haploidentical HCT (haplo-HCT) had outcomes similar to those seen in patients with matched donors, reported Peter Dreger, MD, of the University of Heidelberg (Germany) and his colleagues.
“Using well-matched sibling donors (MSDs) or unrelated donors (MUDs), allo-HCT can result in sustained disease control in 30% to 45% of patients with DLBCL who have early disease recurrence after standard chemoimmunotherapy or have failed auto-HCT [autologous HCT],” the investigators wrote in Blood Advances. “However, the search for a well-matched unrelated donor could be time-consuming and unsuccessful in up to 50% of the patients in need.”
But the present findings suggest that haplo-HCT may one day improve these odds by providing a larger pool of potential donors.
The patients in the study were divided into four treatment groups: haplo-HCT (n = 132), MSD (n = 525), MUD with T-cell depletion (n = 403), and MUD without T-cell depletion (n = 378). For graft-versus-host disease (GVHD) prophylaxis, patients in the haplo-HCT group received PTCy, with or without a calcineurin inhibitor and mycophenolate mofetil, whereas all patients with matched donors received a calcineurin inhibitor. T-cell depletion was accomplished by in vivo antithymocyte globulin and alemtuzumab.
The primary end point was overall survival (OS). Secondary end points were progression-free survival (PFS), progression/relapse, and nonrelapse mortality (NRM).
After a median follow-up of 4.1 years, all groups had similar outcomes, without statistical differences in multivariable analysis.
In the haplo-HCT group, the 3-year OS rate was 46%, the NRM rate was 22%, the PFS rate was 38%, and the relapse/progression rate was 41%.
Of note, patients receiving haplo-HCT did have a lower cumulative incidence of chronic GVHD, at 15% after 1 year and 18% after 2 years. These rates were significantly lower than the other groups’ 1- and 2-year GVHD rates, which were as follows: MSD, 41% and 48%; MUD with T-cell depletion, 23% and 27%; and MUD without T-cell depletion, 48% and 57%.
The investigators noted that these disparities may actually be caused by the use of bone marrow grafts in the haplo-HCT group instead of peripheral blood grafts, which were used in most of the patients in the other groups.
Overall, the findings were encouraging, but the investigators cautioned that “additional studies are needed before haploidentical donors can be considered as equivalent to well-matched related or unrelated donors in patients with DLBCL.”
The study was funded by the Center for International Blood & Marrow Transplant Research (CIBMTR) and the European Society for Blood and Marrow Transplantation. CIBMTR is supported by grants from the U.S. government and the pharmaceutical industry. The authors reported having no competing financial interests.
SOURCE: Dreger P et al. Blood Adv. 2019 Feb 12;3(3):360-9.
For patients with diffuse large B-cell lymphoma (DLBCL) who need allogeneic hematopoietic cell transplantation (allo-HCT), a haploidentical family member could be a viable donor, according to a retrospective study of 1,438 patients.
When combined with nonmyeloablative/reduced intensity conditioning (NMC/RIC) and posttransplant cyclophosphamide (PTCy), patients treated with haploidentical HCT (haplo-HCT) had outcomes similar to those seen in patients with matched donors, reported Peter Dreger, MD, of the University of Heidelberg (Germany) and his colleagues.
“Using well-matched sibling donors (MSDs) or unrelated donors (MUDs), allo-HCT can result in sustained disease control in 30% to 45% of patients with DLBCL who have early disease recurrence after standard chemoimmunotherapy or have failed auto-HCT [autologous HCT],” the investigators wrote in Blood Advances. “However, the search for a well-matched unrelated donor could be time-consuming and unsuccessful in up to 50% of the patients in need.”
But the present findings suggest that haplo-HCT may one day improve these odds by providing a larger pool of potential donors.
The patients in the study were divided into four treatment groups: haplo-HCT (n = 132), MSD (n = 525), MUD with T-cell depletion (n = 403), and MUD without T-cell depletion (n = 378). For graft-versus-host disease (GVHD) prophylaxis, patients in the haplo-HCT group received PTCy, with or without a calcineurin inhibitor and mycophenolate mofetil, whereas all patients with matched donors received a calcineurin inhibitor. T-cell depletion was accomplished by in vivo antithymocyte globulin and alemtuzumab.
The primary end point was overall survival (OS). Secondary end points were progression-free survival (PFS), progression/relapse, and nonrelapse mortality (NRM).
After a median follow-up of 4.1 years, all groups had similar outcomes, without statistical differences in multivariable analysis.
In the haplo-HCT group, the 3-year OS rate was 46%, the NRM rate was 22%, the PFS rate was 38%, and the relapse/progression rate was 41%.
Of note, patients receiving haplo-HCT did have a lower cumulative incidence of chronic GVHD, at 15% after 1 year and 18% after 2 years. These rates were significantly lower than the other groups’ 1- and 2-year GVHD rates, which were as follows: MSD, 41% and 48%; MUD with T-cell depletion, 23% and 27%; and MUD without T-cell depletion, 48% and 57%.
The investigators noted that these disparities may actually be caused by the use of bone marrow grafts in the haplo-HCT group instead of peripheral blood grafts, which were used in most of the patients in the other groups.
Overall, the findings were encouraging, but the investigators cautioned that “additional studies are needed before haploidentical donors can be considered as equivalent to well-matched related or unrelated donors in patients with DLBCL.”
The study was funded by the Center for International Blood & Marrow Transplant Research (CIBMTR) and the European Society for Blood and Marrow Transplantation. CIBMTR is supported by grants from the U.S. government and the pharmaceutical industry. The authors reported having no competing financial interests.
SOURCE: Dreger P et al. Blood Adv. 2019 Feb 12;3(3):360-9.
FROM BLOOD ADVANCES
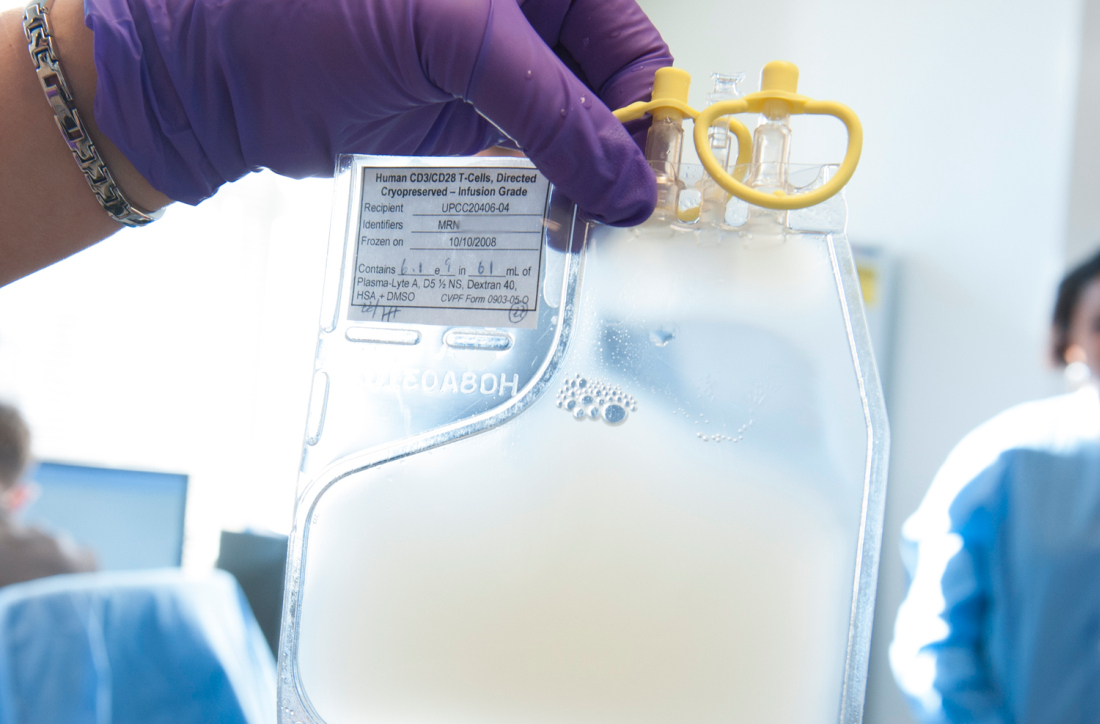
CMS proposes coverage of CAR T-cell therapy in trials
The Centers for Medicare & Medicaid Services has proposed to cover chimeric antigen receptor (CAR) T-cell therapy for cancer patients participating in clinical trials that study the treatment’s effectiveness, according to a Feb. 15 announcement.
The proposed national coverage determination would require CMS to cover CAR T-cell therapies nationwide when the treatment is offered in CMS-approved registries or clinical studies in which patients are monitored for 2 or more years following treatment.
Results from the studies would help CMS identify which patients benefit most from CAR T-cell therapies and inform future coverage decisions, CMS Administrator Seema Verma said.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” Ms. Verma said in a statement. “Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
As part of the proposal, CMS would cover autologous treatment with T cells expressing at least one chimeric antigen receptor (CAR) through coverage with evidence development when prescribed by a treating oncologist and performed in a hospital, according to a summary of the proposal.
The patient and hospital must meet specific criteria to be eligible for coverage, including that patients have relapsed or refractory cancer and do not have a comorbidity that would otherwise preclude patient benefit.
Hospitals, meanwhile, must have a cellular therapy program consisting of an integrated medical team that includes a clinical program director, a quality manager, and at least one physician experienced in cellular therapy, among other requirements.
CMS also would require that treatment is an FDA-approved biologic, providing targeted therapy for a known antigen expressed in the patient’s cancer according to an FDA indication. Repeat treatment would be covered only when a new primary cancer diagnosis is made by the treating oncologist and certain patient conditions are met.
Both inpatient and outpatient settings for the CAR T-cell therapy treatment are acceptable under the proposal. In either case, the patient and the hospital must be participating in a prospective, national, audited registry that consecutively enrolls patients, accepts all manufactured products, follows the patient for at least 2 years, and addresses a set of approved evidence-development questions. Additionally, all registries must be reviewed and approved by CMS.
The proposed national coverage determination was the result of an Aug. 22, 2018 meeting of the Medicare Evidence Development & Coverage Advisory Committee. The committee provides CMS with an external assessment of the appropriateness of therapies under review.
Public comments about the CAR T-cell therapy proposal will be accepted online here until March 15. A final decision on the proposal is expected by May 2019.
The agency’s proposal follows an Aug. 17 final rule by CMS that sets a new payment scheme for inpatient administration of two CAR T-cell therapies. The rule categorizes CAR T-cell therapies under the umbrella of the renamed Medicare Severity–Diagnosis Related Groups 016 – Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy – and assigns ICD-10 PCS procedure codes XW033C3 and XW043C3 to the use of axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) in the inpatient setting for fiscal year 2019, which began in October 2018. CMS also approved a temporary New Technology Add-On Payment for use of the therapies with a maximum threshold of $186,500.
In April 2018, CMS announced payment rates for outpatient administration of the two drugs, settling on $395,380 for axicabtagene ciloleucel and $500,839 for tisagenlecleucel. The two medications have list prices of $373,000 and $475,000, respectively.
The Centers for Medicare & Medicaid Services has proposed to cover chimeric antigen receptor (CAR) T-cell therapy for cancer patients participating in clinical trials that study the treatment’s effectiveness, according to a Feb. 15 announcement.
The proposed national coverage determination would require CMS to cover CAR T-cell therapies nationwide when the treatment is offered in CMS-approved registries or clinical studies in which patients are monitored for 2 or more years following treatment.
Results from the studies would help CMS identify which patients benefit most from CAR T-cell therapies and inform future coverage decisions, CMS Administrator Seema Verma said.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” Ms. Verma said in a statement. “Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
As part of the proposal, CMS would cover autologous treatment with T cells expressing at least one chimeric antigen receptor (CAR) through coverage with evidence development when prescribed by a treating oncologist and performed in a hospital, according to a summary of the proposal.
The patient and hospital must meet specific criteria to be eligible for coverage, including that patients have relapsed or refractory cancer and do not have a comorbidity that would otherwise preclude patient benefit.
Hospitals, meanwhile, must have a cellular therapy program consisting of an integrated medical team that includes a clinical program director, a quality manager, and at least one physician experienced in cellular therapy, among other requirements.
CMS also would require that treatment is an FDA-approved biologic, providing targeted therapy for a known antigen expressed in the patient’s cancer according to an FDA indication. Repeat treatment would be covered only when a new primary cancer diagnosis is made by the treating oncologist and certain patient conditions are met.
Both inpatient and outpatient settings for the CAR T-cell therapy treatment are acceptable under the proposal. In either case, the patient and the hospital must be participating in a prospective, national, audited registry that consecutively enrolls patients, accepts all manufactured products, follows the patient for at least 2 years, and addresses a set of approved evidence-development questions. Additionally, all registries must be reviewed and approved by CMS.
The proposed national coverage determination was the result of an Aug. 22, 2018 meeting of the Medicare Evidence Development & Coverage Advisory Committee. The committee provides CMS with an external assessment of the appropriateness of therapies under review.
Public comments about the CAR T-cell therapy proposal will be accepted online here until March 15. A final decision on the proposal is expected by May 2019.
The agency’s proposal follows an Aug. 17 final rule by CMS that sets a new payment scheme for inpatient administration of two CAR T-cell therapies. The rule categorizes CAR T-cell therapies under the umbrella of the renamed Medicare Severity–Diagnosis Related Groups 016 – Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy – and assigns ICD-10 PCS procedure codes XW033C3 and XW043C3 to the use of axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) in the inpatient setting for fiscal year 2019, which began in October 2018. CMS also approved a temporary New Technology Add-On Payment for use of the therapies with a maximum threshold of $186,500.
In April 2018, CMS announced payment rates for outpatient administration of the two drugs, settling on $395,380 for axicabtagene ciloleucel and $500,839 for tisagenlecleucel. The two medications have list prices of $373,000 and $475,000, respectively.
The Centers for Medicare & Medicaid Services has proposed to cover chimeric antigen receptor (CAR) T-cell therapy for cancer patients participating in clinical trials that study the treatment’s effectiveness, according to a Feb. 15 announcement.
The proposed national coverage determination would require CMS to cover CAR T-cell therapies nationwide when the treatment is offered in CMS-approved registries or clinical studies in which patients are monitored for 2 or more years following treatment.
Results from the studies would help CMS identify which patients benefit most from CAR T-cell therapies and inform future coverage decisions, CMS Administrator Seema Verma said.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” Ms. Verma said in a statement. “Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
As part of the proposal, CMS would cover autologous treatment with T cells expressing at least one chimeric antigen receptor (CAR) through coverage with evidence development when prescribed by a treating oncologist and performed in a hospital, according to a summary of the proposal.
The patient and hospital must meet specific criteria to be eligible for coverage, including that patients have relapsed or refractory cancer and do not have a comorbidity that would otherwise preclude patient benefit.
Hospitals, meanwhile, must have a cellular therapy program consisting of an integrated medical team that includes a clinical program director, a quality manager, and at least one physician experienced in cellular therapy, among other requirements.
CMS also would require that treatment is an FDA-approved biologic, providing targeted therapy for a known antigen expressed in the patient’s cancer according to an FDA indication. Repeat treatment would be covered only when a new primary cancer diagnosis is made by the treating oncologist and certain patient conditions are met.
Both inpatient and outpatient settings for the CAR T-cell therapy treatment are acceptable under the proposal. In either case, the patient and the hospital must be participating in a prospective, national, audited registry that consecutively enrolls patients, accepts all manufactured products, follows the patient for at least 2 years, and addresses a set of approved evidence-development questions. Additionally, all registries must be reviewed and approved by CMS.
The proposed national coverage determination was the result of an Aug. 22, 2018 meeting of the Medicare Evidence Development & Coverage Advisory Committee. The committee provides CMS with an external assessment of the appropriateness of therapies under review.
Public comments about the CAR T-cell therapy proposal will be accepted online here until March 15. A final decision on the proposal is expected by May 2019.
The agency’s proposal follows an Aug. 17 final rule by CMS that sets a new payment scheme for inpatient administration of two CAR T-cell therapies. The rule categorizes CAR T-cell therapies under the umbrella of the renamed Medicare Severity–Diagnosis Related Groups 016 – Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy – and assigns ICD-10 PCS procedure codes XW033C3 and XW043C3 to the use of axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) in the inpatient setting for fiscal year 2019, which began in October 2018. CMS also approved a temporary New Technology Add-On Payment for use of the therapies with a maximum threshold of $186,500.
In April 2018, CMS announced payment rates for outpatient administration of the two drugs, settling on $395,380 for axicabtagene ciloleucel and $500,839 for tisagenlecleucel. The two medications have list prices of $373,000 and $475,000, respectively.
PD-1 blockade plus CD19 CAR T boosts CAR T-cell persistence
SAN DIEGO – Checkpoint inhibition can be used safely and effectively with CD19-directed chimeric antigen receptor (CAR) T-cell therapy in children with relapsed B-cell acute lymphoblastic leukemia (ALL), and it may bolster CAR T-cell effects and persistence, suggest the findings in a series of 14 patients at the Children’s Hospital of Philadelphia.
Combined programmed death-1 (PD-1) blockade and CAR T-cell therapy appeared to have particular benefit in patients with early B-cell recovery and in those with bulky extramedullary disease, Shannon Maude, MD, PhD, reported during a press conference at the annual meeting of the American Society of Hematology.
The patients, aged 4-17 years with heavily pretreated relapsed B-ALL (13 patients) or B lymphoblastic lymphoma (1 patient), were treated with CD19-directed CAR T-cell therapy, including CTL019 in 4 patients and CTL119 in 10 patients, followed by pembrolizumab (in 13 patients) or nivolumab (in 1 patient).
Six patients received the combination therapy because of early B-cell recovery after initial CAR T-cell infusion, four patients had relapsed or refractory (R/R) bulky extramedullary disease, and four patients had failed to respond or relapsed after initial CAR T-cell therapy.
Three of the six with poor persistence of response reestablished B-cell aplasia (a reflection of CAR T-cell function) after reinfusion of the CAR T-cell product followed by infusion with PD-1 blockade, and they have “sustained CR [complete response] with B-cell aplasia, showing continued persistence of their CAR T cells,” said Dr. Maude, an attending physician in the Cancer Center at Children’s Hospital of Philadelphia.
Of the four patients with R/R bulky extramedullary disease, two patients had a partial response and two patients had CR, she said, explaining that it was hypothesized that the “PD-1 checkpoint pathway may be activated through the microenvironment in that extramedullary situation.”
However, all four patients who had partial or no response to initial CAR T-cell therapy progressed after PD-1 administration, she said, noting that “in one patient, this progression was marked by reduced CD19 expression, which was probably the mode of escape from CD19 CAR T cells.”
Prior studies have shown that patients who respond to CAR T-cell therapy have persistence of CD19 CAR T cells, whereas those with loss of CD19 CAR T cells within 6 months of infusion have a higher rate of relapse, Dr. Maude explained.
“Our hypothesis was that T cells, upon activation, may become exhausted through activation of immune checkpoint pathways, that one such pathway – PD-1 – may be involved in early loss of CD19 CAR T cells and therefore that the combination [of CD19 CAR T-cell therapy] with PD-1 checkpoint blockade may improve the function of the CAR T cells and their persistence,” she said.
The combined approach was well tolerated in this study, she said, noting that mild cytokine release syndrome symptoms and fever typical of CAR T-cell proliferative responses were observed in three patients within 2 days of starting pembrolizumab.
Other adverse effects associated with PD-1 inhibition, including acute pancreatitis, hypothyroidism, arthralgias, and urticaria, occurred in one patient each. There were four cases of grade 3-4 cytopenias that were deemed tolerable or reversible upon discontinuation.
“We show that PD-1 checkpoint inhibitors can be safely combined with CD19 CAR T-cell therapy and that this mechanism may be useful to improve CAR T-cell persistence,” Dr. Maude said.
These findings, which showed particular benefit in patients with poor persistence marked by early B-cell recovery and in those with R/R bulky extramedullary disease, should help inform future use of checkpoint inhibitors after CAR T-cell therapy, she added.
Dr. Maude reported financial ties to Novartis.
SOURCE: Li AM et al. ASH 2018, Abstract 556.
SAN DIEGO – Checkpoint inhibition can be used safely and effectively with CD19-directed chimeric antigen receptor (CAR) T-cell therapy in children with relapsed B-cell acute lymphoblastic leukemia (ALL), and it may bolster CAR T-cell effects and persistence, suggest the findings in a series of 14 patients at the Children’s Hospital of Philadelphia.
Combined programmed death-1 (PD-1) blockade and CAR T-cell therapy appeared to have particular benefit in patients with early B-cell recovery and in those with bulky extramedullary disease, Shannon Maude, MD, PhD, reported during a press conference at the annual meeting of the American Society of Hematology.
The patients, aged 4-17 years with heavily pretreated relapsed B-ALL (13 patients) or B lymphoblastic lymphoma (1 patient), were treated with CD19-directed CAR T-cell therapy, including CTL019 in 4 patients and CTL119 in 10 patients, followed by pembrolizumab (in 13 patients) or nivolumab (in 1 patient).
Six patients received the combination therapy because of early B-cell recovery after initial CAR T-cell infusion, four patients had relapsed or refractory (R/R) bulky extramedullary disease, and four patients had failed to respond or relapsed after initial CAR T-cell therapy.
Three of the six with poor persistence of response reestablished B-cell aplasia (a reflection of CAR T-cell function) after reinfusion of the CAR T-cell product followed by infusion with PD-1 blockade, and they have “sustained CR [complete response] with B-cell aplasia, showing continued persistence of their CAR T cells,” said Dr. Maude, an attending physician in the Cancer Center at Children’s Hospital of Philadelphia.
Of the four patients with R/R bulky extramedullary disease, two patients had a partial response and two patients had CR, she said, explaining that it was hypothesized that the “PD-1 checkpoint pathway may be activated through the microenvironment in that extramedullary situation.”
However, all four patients who had partial or no response to initial CAR T-cell therapy progressed after PD-1 administration, she said, noting that “in one patient, this progression was marked by reduced CD19 expression, which was probably the mode of escape from CD19 CAR T cells.”
Prior studies have shown that patients who respond to CAR T-cell therapy have persistence of CD19 CAR T cells, whereas those with loss of CD19 CAR T cells within 6 months of infusion have a higher rate of relapse, Dr. Maude explained.
“Our hypothesis was that T cells, upon activation, may become exhausted through activation of immune checkpoint pathways, that one such pathway – PD-1 – may be involved in early loss of CD19 CAR T cells and therefore that the combination [of CD19 CAR T-cell therapy] with PD-1 checkpoint blockade may improve the function of the CAR T cells and their persistence,” she said.
The combined approach was well tolerated in this study, she said, noting that mild cytokine release syndrome symptoms and fever typical of CAR T-cell proliferative responses were observed in three patients within 2 days of starting pembrolizumab.
Other adverse effects associated with PD-1 inhibition, including acute pancreatitis, hypothyroidism, arthralgias, and urticaria, occurred in one patient each. There were four cases of grade 3-4 cytopenias that were deemed tolerable or reversible upon discontinuation.
“We show that PD-1 checkpoint inhibitors can be safely combined with CD19 CAR T-cell therapy and that this mechanism may be useful to improve CAR T-cell persistence,” Dr. Maude said.
These findings, which showed particular benefit in patients with poor persistence marked by early B-cell recovery and in those with R/R bulky extramedullary disease, should help inform future use of checkpoint inhibitors after CAR T-cell therapy, she added.
Dr. Maude reported financial ties to Novartis.
SOURCE: Li AM et al. ASH 2018, Abstract 556.
SAN DIEGO – Checkpoint inhibition can be used safely and effectively with CD19-directed chimeric antigen receptor (CAR) T-cell therapy in children with relapsed B-cell acute lymphoblastic leukemia (ALL), and it may bolster CAR T-cell effects and persistence, suggest the findings in a series of 14 patients at the Children’s Hospital of Philadelphia.
Combined programmed death-1 (PD-1) blockade and CAR T-cell therapy appeared to have particular benefit in patients with early B-cell recovery and in those with bulky extramedullary disease, Shannon Maude, MD, PhD, reported during a press conference at the annual meeting of the American Society of Hematology.
The patients, aged 4-17 years with heavily pretreated relapsed B-ALL (13 patients) or B lymphoblastic lymphoma (1 patient), were treated with CD19-directed CAR T-cell therapy, including CTL019 in 4 patients and CTL119 in 10 patients, followed by pembrolizumab (in 13 patients) or nivolumab (in 1 patient).
Six patients received the combination therapy because of early B-cell recovery after initial CAR T-cell infusion, four patients had relapsed or refractory (R/R) bulky extramedullary disease, and four patients had failed to respond or relapsed after initial CAR T-cell therapy.
Three of the six with poor persistence of response reestablished B-cell aplasia (a reflection of CAR T-cell function) after reinfusion of the CAR T-cell product followed by infusion with PD-1 blockade, and they have “sustained CR [complete response] with B-cell aplasia, showing continued persistence of their CAR T cells,” said Dr. Maude, an attending physician in the Cancer Center at Children’s Hospital of Philadelphia.
Of the four patients with R/R bulky extramedullary disease, two patients had a partial response and two patients had CR, she said, explaining that it was hypothesized that the “PD-1 checkpoint pathway may be activated through the microenvironment in that extramedullary situation.”
However, all four patients who had partial or no response to initial CAR T-cell therapy progressed after PD-1 administration, she said, noting that “in one patient, this progression was marked by reduced CD19 expression, which was probably the mode of escape from CD19 CAR T cells.”
Prior studies have shown that patients who respond to CAR T-cell therapy have persistence of CD19 CAR T cells, whereas those with loss of CD19 CAR T cells within 6 months of infusion have a higher rate of relapse, Dr. Maude explained.
“Our hypothesis was that T cells, upon activation, may become exhausted through activation of immune checkpoint pathways, that one such pathway – PD-1 – may be involved in early loss of CD19 CAR T cells and therefore that the combination [of CD19 CAR T-cell therapy] with PD-1 checkpoint blockade may improve the function of the CAR T cells and their persistence,” she said.
The combined approach was well tolerated in this study, she said, noting that mild cytokine release syndrome symptoms and fever typical of CAR T-cell proliferative responses were observed in three patients within 2 days of starting pembrolizumab.
Other adverse effects associated with PD-1 inhibition, including acute pancreatitis, hypothyroidism, arthralgias, and urticaria, occurred in one patient each. There were four cases of grade 3-4 cytopenias that were deemed tolerable or reversible upon discontinuation.
“We show that PD-1 checkpoint inhibitors can be safely combined with CD19 CAR T-cell therapy and that this mechanism may be useful to improve CAR T-cell persistence,” Dr. Maude said.
These findings, which showed particular benefit in patients with poor persistence marked by early B-cell recovery and in those with R/R bulky extramedullary disease, should help inform future use of checkpoint inhibitors after CAR T-cell therapy, she added.
Dr. Maude reported financial ties to Novartis.
SOURCE: Li AM et al. ASH 2018, Abstract 556.
REPORTING FROM ASH 2018
Key clinical point: Major finding: Three of six patients with poor CAR T-cell persistence had a complete response after treatment with the combination therapy. Study details: A clinical study of 14 patients with relapsed B-ALL.
Disclosures: Dr. Maude reported financial relationships with Novartis.
Source: Li AM et al. ASH 2018, Abstract 556.
Novel bispecific CAR shows promise in B-cell malignancies
SAN DIEGO – A chimeric antigen receptor (CAR) targeting both CD19 and CD22 shows promising safety and efficacy for the treatment of relapsed or refractory B-cell malignancies in adults, according to early findings from a phase 1 trial of the novel bispecific CAR.
Of six patients with diffuse large B-cell lymphoma (DLBCL) and two patients with B-cell acute lymphoblastic leukemia (B-ALL) enrolled in the single-institution dose escalation study and available for safety analysis after the bispecific CAR T-cell infusion, five developed reversible grade 1 cytokine release syndrome (CRS) and one developed grade 2 CRS requiring treatment with tocilizumab, Nasheed Hossain, MD, reported at the annual meeting of the American Society of Hematology.
Additionally, two patients developed grade 1 neurotoxicity, and one developed grade 2 neurotoxicity requiring treatment with dexamethasone.
“But no dose-limiting toxicities have been encountered thus far,” said Dr. Hossain of Loyola University Medical Center, Chicago. “With regard to efficacy, the DLBCL overall response rate is 60%, with 1 [complete response] and 2 [partial responses] at day 28 and day 90, and the ALL overall response rate is 100%, with 1 CR and 1 PR at day 28.
“With longer follow-up, five patients have relapsed and biopsies at the time of progression all showed ongoing CD19 expression,” he said, adding that all enrolled patients are alive, except for one patient who died from disease progression.
Study participants were adults aged 35-75 years with DLBCL or B-ALL that was refractory to standard therapies.
“Our primary objectives are twofold: One is to determine the feasibility of making our CAR ... and [the other] is to assess the safety using an escalating CAR dose following standard cyclophosphamide/fludarabine conditioning,” Dr. Hossain said.
The dose assessed in the current analysis was 1 x 106 CAR T cells/kg; other planned doses include 3 x 106 CAR T cells/kg and 1 x 107 CAR T cells/kg, he said.
All patients underwent lymphodepletion with cyclophosphamide (500 mg/m2 daily x 3 doses) and fludarabine (30 mg/m2 daily x 3 doses) followed by CAR T-cell infusion 2 days later.
The findings of this ongoing study – the first in-human study of a bispecific loop CAR in the United States – suggest that the novel CAR has low toxicity and promising efficacy, Dr. Hossain said.
Currently approved therapies target CD19 alone, he said, noting that they all use the same anti-CD19 domain, but different costimulatory domains, and have good clinical efficacy of greater than 70% CRs in ALL and up to 52% CRs in DLBCL.
“But questions remain about determining the durability of response and the causes of therapy failure,” he said.
One common cause of treatment failure is CD19 antigen loss, and efforts to reduce such antigen loss using bispecific loop CARs targeting both CD19 and CD22 have shown promise. The CAR construct evaluated in this study was developed to target CD19 and CD22 with intracellular signaling domains incorporating 4-1BB and CD3-zeta to overcome CD19 immune escape.
“We have now escalated the dose to 3 x 106 CAR T cells/kg ... and an expansion study of 60 patients will follow,” Dr. Hossain said.
A companion phase 1 pediatric trial using the same CAR construct is also underway, with preliminary data presented at the ASH meeting demonstrating safety and tolerability in children with relapsed or refractory B-cell ALL.
Dr. Hossain reported having no financial disclosures.
SOURCE: Hossain N et al. ASH 2018, Abstract 490.
SAN DIEGO – A chimeric antigen receptor (CAR) targeting both CD19 and CD22 shows promising safety and efficacy for the treatment of relapsed or refractory B-cell malignancies in adults, according to early findings from a phase 1 trial of the novel bispecific CAR.
Of six patients with diffuse large B-cell lymphoma (DLBCL) and two patients with B-cell acute lymphoblastic leukemia (B-ALL) enrolled in the single-institution dose escalation study and available for safety analysis after the bispecific CAR T-cell infusion, five developed reversible grade 1 cytokine release syndrome (CRS) and one developed grade 2 CRS requiring treatment with tocilizumab, Nasheed Hossain, MD, reported at the annual meeting of the American Society of Hematology.
Additionally, two patients developed grade 1 neurotoxicity, and one developed grade 2 neurotoxicity requiring treatment with dexamethasone.
“But no dose-limiting toxicities have been encountered thus far,” said Dr. Hossain of Loyola University Medical Center, Chicago. “With regard to efficacy, the DLBCL overall response rate is 60%, with 1 [complete response] and 2 [partial responses] at day 28 and day 90, and the ALL overall response rate is 100%, with 1 CR and 1 PR at day 28.
“With longer follow-up, five patients have relapsed and biopsies at the time of progression all showed ongoing CD19 expression,” he said, adding that all enrolled patients are alive, except for one patient who died from disease progression.
Study participants were adults aged 35-75 years with DLBCL or B-ALL that was refractory to standard therapies.
“Our primary objectives are twofold: One is to determine the feasibility of making our CAR ... and [the other] is to assess the safety using an escalating CAR dose following standard cyclophosphamide/fludarabine conditioning,” Dr. Hossain said.
The dose assessed in the current analysis was 1 x 106 CAR T cells/kg; other planned doses include 3 x 106 CAR T cells/kg and 1 x 107 CAR T cells/kg, he said.
All patients underwent lymphodepletion with cyclophosphamide (500 mg/m2 daily x 3 doses) and fludarabine (30 mg/m2 daily x 3 doses) followed by CAR T-cell infusion 2 days later.
The findings of this ongoing study – the first in-human study of a bispecific loop CAR in the United States – suggest that the novel CAR has low toxicity and promising efficacy, Dr. Hossain said.
Currently approved therapies target CD19 alone, he said, noting that they all use the same anti-CD19 domain, but different costimulatory domains, and have good clinical efficacy of greater than 70% CRs in ALL and up to 52% CRs in DLBCL.
“But questions remain about determining the durability of response and the causes of therapy failure,” he said.
One common cause of treatment failure is CD19 antigen loss, and efforts to reduce such antigen loss using bispecific loop CARs targeting both CD19 and CD22 have shown promise. The CAR construct evaluated in this study was developed to target CD19 and CD22 with intracellular signaling domains incorporating 4-1BB and CD3-zeta to overcome CD19 immune escape.
“We have now escalated the dose to 3 x 106 CAR T cells/kg ... and an expansion study of 60 patients will follow,” Dr. Hossain said.
A companion phase 1 pediatric trial using the same CAR construct is also underway, with preliminary data presented at the ASH meeting demonstrating safety and tolerability in children with relapsed or refractory B-cell ALL.
Dr. Hossain reported having no financial disclosures.
SOURCE: Hossain N et al. ASH 2018, Abstract 490.
SAN DIEGO – A chimeric antigen receptor (CAR) targeting both CD19 and CD22 shows promising safety and efficacy for the treatment of relapsed or refractory B-cell malignancies in adults, according to early findings from a phase 1 trial of the novel bispecific CAR.
Of six patients with diffuse large B-cell lymphoma (DLBCL) and two patients with B-cell acute lymphoblastic leukemia (B-ALL) enrolled in the single-institution dose escalation study and available for safety analysis after the bispecific CAR T-cell infusion, five developed reversible grade 1 cytokine release syndrome (CRS) and one developed grade 2 CRS requiring treatment with tocilizumab, Nasheed Hossain, MD, reported at the annual meeting of the American Society of Hematology.
Additionally, two patients developed grade 1 neurotoxicity, and one developed grade 2 neurotoxicity requiring treatment with dexamethasone.
“But no dose-limiting toxicities have been encountered thus far,” said Dr. Hossain of Loyola University Medical Center, Chicago. “With regard to efficacy, the DLBCL overall response rate is 60%, with 1 [complete response] and 2 [partial responses] at day 28 and day 90, and the ALL overall response rate is 100%, with 1 CR and 1 PR at day 28.
“With longer follow-up, five patients have relapsed and biopsies at the time of progression all showed ongoing CD19 expression,” he said, adding that all enrolled patients are alive, except for one patient who died from disease progression.
Study participants were adults aged 35-75 years with DLBCL or B-ALL that was refractory to standard therapies.
“Our primary objectives are twofold: One is to determine the feasibility of making our CAR ... and [the other] is to assess the safety using an escalating CAR dose following standard cyclophosphamide/fludarabine conditioning,” Dr. Hossain said.
The dose assessed in the current analysis was 1 x 106 CAR T cells/kg; other planned doses include 3 x 106 CAR T cells/kg and 1 x 107 CAR T cells/kg, he said.
All patients underwent lymphodepletion with cyclophosphamide (500 mg/m2 daily x 3 doses) and fludarabine (30 mg/m2 daily x 3 doses) followed by CAR T-cell infusion 2 days later.
The findings of this ongoing study – the first in-human study of a bispecific loop CAR in the United States – suggest that the novel CAR has low toxicity and promising efficacy, Dr. Hossain said.
Currently approved therapies target CD19 alone, he said, noting that they all use the same anti-CD19 domain, but different costimulatory domains, and have good clinical efficacy of greater than 70% CRs in ALL and up to 52% CRs in DLBCL.
“But questions remain about determining the durability of response and the causes of therapy failure,” he said.
One common cause of treatment failure is CD19 antigen loss, and efforts to reduce such antigen loss using bispecific loop CARs targeting both CD19 and CD22 have shown promise. The CAR construct evaluated in this study was developed to target CD19 and CD22 with intracellular signaling domains incorporating 4-1BB and CD3-zeta to overcome CD19 immune escape.
“We have now escalated the dose to 3 x 106 CAR T cells/kg ... and an expansion study of 60 patients will follow,” Dr. Hossain said.
A companion phase 1 pediatric trial using the same CAR construct is also underway, with preliminary data presented at the ASH meeting demonstrating safety and tolerability in children with relapsed or refractory B-cell ALL.
Dr. Hossain reported having no financial disclosures.
SOURCE: Hossain N et al. ASH 2018, Abstract 490.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: Grade 1 cytokine release syndrome occurred in five patients, and grade 2 CRS occurred in one patient; there were no dose-limiting toxicities.
Study details: A phase 1 dose escalation study of nine patients.
Disclosures: Dr. Hossain reported having no financial disclosures.
Source: Hossain N et al. ASH 2018, Abstract 490.
Group proposes new grading systems for CRS, neurotoxicity
A group of experts has proposed new consensus definitions and grading systems for cytokine release syndrome (CRS) and neurotoxicity related to immune effector cell therapies.
The group hopes their recommendations will be widely accepted and used in both trials and the clinical setting.
The recommendations were devised by 49 experts at a meeting supported by the American Society for Blood and Marrow Transplantation (ASBMT), compiled by a writing group, and reviewed by stakeholders.
Daniel W. Lee, MD, of the University of Virginia School of Medicine in Charlottesville, and his colleagues described the ASBMT consensus definitions and grading systems in Biology of Blood and Marrow Transplantation.
CRS
The ASBMT consensus definition for CRS is “a supraphysiologic response following any immune therapy that results in the activation or engagement of endogenous or infused T cells and/or other immune effector cells.”
To be diagnosed with CRS, a patient must have a fever and may have the following symptoms:
- Hypotension
- Capillary leak (hypoxia)
- End organ dysfunction.
The ASBMT consensus for grading CRS is as follows:
- Grade 1—Patient has a fever, defined as a temperature of 38.0°C or higher
- Grade 2—Patient has a fever, hypotension that doesn’t require vasopressors, and/or hypoxia that requires oxygen delivered by low-flow nasal cannula (≤6 L/min) or blow-by
- Grade 3—Patient has a fever, hypotension requiring one vasopressor (with or without vasopressin), and/or hypoxia (not attributable to any other cause) that requires high-flow nasal cannula (>6 L/min), facemask, non-rebreather mask, or venturi mask
- Grade 4—Patient has a fever, hypotension requiring multiple vasopressors (excluding vasopressin), and/or hypoxia (not attributable to any other cause) requiring positive-pressure ventilation
- Grade 5—Death due to CRS when there is no other “principle factor” leading to death.
Typically, severe CRS can be considered resolved if “fever, oxygen, and pressor requirements have resolved,” Dr. Lee and his coauthors said.
The authors also stressed that neurotoxicity that occurs with or after CRS “does not inform the grade of CRS but is instead captured separately in the neurotoxicity scale.”
Neurotoxicity
Dr. Lee and his coauthors said neurotoxicity in this setting is called “immune effector cell-associated neurotoxicity syndrome (ICANS).”
The ASBMT consensus definition for ICANs is “a disorder characterized by a pathologic process involving the central nervous system following any immune therapy that results in the activation or engagement of endogenous or infused T cells and/or other immune effector cells.”
Symptoms of ICANS may include:
- Aphasia
- Altered level of consciousness
- Impairment of cognitive skills
- Motor weakness
- Seizures
- Cerebral edema.
The ASBMT consensus for grading ICANS in adults and children age 12 and older is as follows:
- Grade 1—Patient has a score of 7-9 on the 10-point immune effector cell-associated encephalopathy (ICE) assessment and awakens spontaneously
- Grade 2—Patient has a score of 3-6 on the ICE assessment and will awaken to the sound of a voice
- Grade 3—Patient has a score of 0-2 on the ICE assessment, awakens only to tactile stimulus, has any clinical seizure that resolves rapidly or non-convulsive seizures that resolve with intervention, has focal/local edema on neuroimaging
- Grade 4—Patient is unable to perform the ICE assessment, is unarousable or requires “vigorous stimuli” to be aroused, has life-threatening seizure (lasting more than 5 minutes) or repetitive clinical or electrical seizures without return to baseline in between, has deep focal motor weakness, and/or has decerebrate or decorticate posturing, cranial nerve VI palsy, papilledema, Cushing’s triad, or signs of diffuse cerebral edema on neuroimaging
- Grade 5—Death due to ICANS when there is no other “principle factor” leading to death.
Dr. Lee and his coauthors noted that the ICE assessment is not suitable for children younger than 12. For these patients (and older patients with baseline developmental delays), ICANS can be assessed using the Cornell Assessment of Pediatric Delirium (CAPD).
The ASBMT consensus for grading ICANS in children younger than 12 (or older patients with developmental delays) is as follows:
- Grade 1—Patient has a CAPD score lower than 9 and awakens spontaneously
- Grade 2—Patient has a CAPD score lower than 9 and will awaken to the sound of a voice
- Grade 3—Patient has a CAPD score of 9 or higher, awakens only to tactile stimulus, has any clinical seizure that resolves rapidly or non-convulsive seizures that resolve with intervention, and/or has focal/local edema on neuroimaging
- Grade 4—Patient is unable to perform CAPD, is unarousable or requires “vigorous stimuli” to be aroused, has life-threatening seizure (lasting more than 5 minutes) or repetitive clinical or electrical seizures without return to baseline in between, has deep focal motor weakness, and/or has decerebrate or decorticate posturing, cranial nerve VI palsy, papilledema, Cushing’s triad, or signs of diffuse cerebral edema on neuroimaging
- Grade 5—Death due to ICANS when there is no other “principle factor” leading to death.
Dr. Lee and his coauthors reported relationships with a range of companies.
A group of experts has proposed new consensus definitions and grading systems for cytokine release syndrome (CRS) and neurotoxicity related to immune effector cell therapies.
The group hopes their recommendations will be widely accepted and used in both trials and the clinical setting.
The recommendations were devised by 49 experts at a meeting supported by the American Society for Blood and Marrow Transplantation (ASBMT), compiled by a writing group, and reviewed by stakeholders.
Daniel W. Lee, MD, of the University of Virginia School of Medicine in Charlottesville, and his colleagues described the ASBMT consensus definitions and grading systems in Biology of Blood and Marrow Transplantation.
CRS
The ASBMT consensus definition for CRS is “a supraphysiologic response following any immune therapy that results in the activation or engagement of endogenous or infused T cells and/or other immune effector cells.”
To be diagnosed with CRS, a patient must have a fever and may have the following symptoms:
- Hypotension
- Capillary leak (hypoxia)
- End organ dysfunction.
The ASBMT consensus for grading CRS is as follows:
- Grade 1—Patient has a fever, defined as a temperature of 38.0°C or higher
- Grade 2—Patient has a fever, hypotension that doesn’t require vasopressors, and/or hypoxia that requires oxygen delivered by low-flow nasal cannula (≤6 L/min) or blow-by
- Grade 3—Patient has a fever, hypotension requiring one vasopressor (with or without vasopressin), and/or hypoxia (not attributable to any other cause) that requires high-flow nasal cannula (>6 L/min), facemask, non-rebreather mask, or venturi mask
- Grade 4—Patient has a fever, hypotension requiring multiple vasopressors (excluding vasopressin), and/or hypoxia (not attributable to any other cause) requiring positive-pressure ventilation
- Grade 5—Death due to CRS when there is no other “principle factor” leading to death.
Typically, severe CRS can be considered resolved if “fever, oxygen, and pressor requirements have resolved,” Dr. Lee and his coauthors said.
The authors also stressed that neurotoxicity that occurs with or after CRS “does not inform the grade of CRS but is instead captured separately in the neurotoxicity scale.”
Neurotoxicity
Dr. Lee and his coauthors said neurotoxicity in this setting is called “immune effector cell-associated neurotoxicity syndrome (ICANS).”
The ASBMT consensus definition for ICANs is “a disorder characterized by a pathologic process involving the central nervous system following any immune therapy that results in the activation or engagement of endogenous or infused T cells and/or other immune effector cells.”
Symptoms of ICANS may include:
- Aphasia
- Altered level of consciousness
- Impairment of cognitive skills
- Motor weakness
- Seizures
- Cerebral edema.
The ASBMT consensus for grading ICANS in adults and children age 12 and older is as follows:
- Grade 1—Patient has a score of 7-9 on the 10-point immune effector cell-associated encephalopathy (ICE) assessment and awakens spontaneously
- Grade 2—Patient has a score of 3-6 on the ICE assessment and will awaken to the sound of a voice
- Grade 3—Patient has a score of 0-2 on the ICE assessment, awakens only to tactile stimulus, has any clinical seizure that resolves rapidly or non-convulsive seizures that resolve with intervention, has focal/local edema on neuroimaging
- Grade 4—Patient is unable to perform the ICE assessment, is unarousable or requires “vigorous stimuli” to be aroused, has life-threatening seizure (lasting more than 5 minutes) or repetitive clinical or electrical seizures without return to baseline in between, has deep focal motor weakness, and/or has decerebrate or decorticate posturing, cranial nerve VI palsy, papilledema, Cushing’s triad, or signs of diffuse cerebral edema on neuroimaging
- Grade 5—Death due to ICANS when there is no other “principle factor” leading to death.
Dr. Lee and his coauthors noted that the ICE assessment is not suitable for children younger than 12. For these patients (and older patients with baseline developmental delays), ICANS can be assessed using the Cornell Assessment of Pediatric Delirium (CAPD).
The ASBMT consensus for grading ICANS in children younger than 12 (or older patients with developmental delays) is as follows:
- Grade 1—Patient has a CAPD score lower than 9 and awakens spontaneously
- Grade 2—Patient has a CAPD score lower than 9 and will awaken to the sound of a voice
- Grade 3—Patient has a CAPD score of 9 or higher, awakens only to tactile stimulus, has any clinical seizure that resolves rapidly or non-convulsive seizures that resolve with intervention, and/or has focal/local edema on neuroimaging
- Grade 4—Patient is unable to perform CAPD, is unarousable or requires “vigorous stimuli” to be aroused, has life-threatening seizure (lasting more than 5 minutes) or repetitive clinical or electrical seizures without return to baseline in between, has deep focal motor weakness, and/or has decerebrate or decorticate posturing, cranial nerve VI palsy, papilledema, Cushing’s triad, or signs of diffuse cerebral edema on neuroimaging
- Grade 5—Death due to ICANS when there is no other “principle factor” leading to death.
Dr. Lee and his coauthors reported relationships with a range of companies.
A group of experts has proposed new consensus definitions and grading systems for cytokine release syndrome (CRS) and neurotoxicity related to immune effector cell therapies.
The group hopes their recommendations will be widely accepted and used in both trials and the clinical setting.
The recommendations were devised by 49 experts at a meeting supported by the American Society for Blood and Marrow Transplantation (ASBMT), compiled by a writing group, and reviewed by stakeholders.
Daniel W. Lee, MD, of the University of Virginia School of Medicine in Charlottesville, and his colleagues described the ASBMT consensus definitions and grading systems in Biology of Blood and Marrow Transplantation.
CRS
The ASBMT consensus definition for CRS is “a supraphysiologic response following any immune therapy that results in the activation or engagement of endogenous or infused T cells and/or other immune effector cells.”
To be diagnosed with CRS, a patient must have a fever and may have the following symptoms:
- Hypotension
- Capillary leak (hypoxia)
- End organ dysfunction.
The ASBMT consensus for grading CRS is as follows:
- Grade 1—Patient has a fever, defined as a temperature of 38.0°C or higher
- Grade 2—Patient has a fever, hypotension that doesn’t require vasopressors, and/or hypoxia that requires oxygen delivered by low-flow nasal cannula (≤6 L/min) or blow-by
- Grade 3—Patient has a fever, hypotension requiring one vasopressor (with or without vasopressin), and/or hypoxia (not attributable to any other cause) that requires high-flow nasal cannula (>6 L/min), facemask, non-rebreather mask, or venturi mask
- Grade 4—Patient has a fever, hypotension requiring multiple vasopressors (excluding vasopressin), and/or hypoxia (not attributable to any other cause) requiring positive-pressure ventilation
- Grade 5—Death due to CRS when there is no other “principle factor” leading to death.
Typically, severe CRS can be considered resolved if “fever, oxygen, and pressor requirements have resolved,” Dr. Lee and his coauthors said.
The authors also stressed that neurotoxicity that occurs with or after CRS “does not inform the grade of CRS but is instead captured separately in the neurotoxicity scale.”
Neurotoxicity
Dr. Lee and his coauthors said neurotoxicity in this setting is called “immune effector cell-associated neurotoxicity syndrome (ICANS).”
The ASBMT consensus definition for ICANs is “a disorder characterized by a pathologic process involving the central nervous system following any immune therapy that results in the activation or engagement of endogenous or infused T cells and/or other immune effector cells.”
Symptoms of ICANS may include:
- Aphasia
- Altered level of consciousness
- Impairment of cognitive skills
- Motor weakness
- Seizures
- Cerebral edema.
The ASBMT consensus for grading ICANS in adults and children age 12 and older is as follows:
- Grade 1—Patient has a score of 7-9 on the 10-point immune effector cell-associated encephalopathy (ICE) assessment and awakens spontaneously
- Grade 2—Patient has a score of 3-6 on the ICE assessment and will awaken to the sound of a voice
- Grade 3—Patient has a score of 0-2 on the ICE assessment, awakens only to tactile stimulus, has any clinical seizure that resolves rapidly or non-convulsive seizures that resolve with intervention, has focal/local edema on neuroimaging
- Grade 4—Patient is unable to perform the ICE assessment, is unarousable or requires “vigorous stimuli” to be aroused, has life-threatening seizure (lasting more than 5 minutes) or repetitive clinical or electrical seizures without return to baseline in between, has deep focal motor weakness, and/or has decerebrate or decorticate posturing, cranial nerve VI palsy, papilledema, Cushing’s triad, or signs of diffuse cerebral edema on neuroimaging
- Grade 5—Death due to ICANS when there is no other “principle factor” leading to death.
Dr. Lee and his coauthors noted that the ICE assessment is not suitable for children younger than 12. For these patients (and older patients with baseline developmental delays), ICANS can be assessed using the Cornell Assessment of Pediatric Delirium (CAPD).
The ASBMT consensus for grading ICANS in children younger than 12 (or older patients with developmental delays) is as follows:
- Grade 1—Patient has a CAPD score lower than 9 and awakens spontaneously
- Grade 2—Patient has a CAPD score lower than 9 and will awaken to the sound of a voice
- Grade 3—Patient has a CAPD score of 9 or higher, awakens only to tactile stimulus, has any clinical seizure that resolves rapidly or non-convulsive seizures that resolve with intervention, and/or has focal/local edema on neuroimaging
- Grade 4—Patient is unable to perform CAPD, is unarousable or requires “vigorous stimuli” to be aroused, has life-threatening seizure (lasting more than 5 minutes) or repetitive clinical or electrical seizures without return to baseline in between, has deep focal motor weakness, and/or has decerebrate or decorticate posturing, cranial nerve VI palsy, papilledema, Cushing’s triad, or signs of diffuse cerebral edema on neuroimaging
- Grade 5—Death due to ICANS when there is no other “principle factor” leading to death.
Dr. Lee and his coauthors reported relationships with a range of companies.
CHMP recommends treosulfan for allo-HSCT conditioning
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for treosulfan (Trecondi) as part of conditioning prior to allogeneic hematopoietic stem cell transplant (allo-HSCT).
The full indication is for treosulfan to be used in combination with fludarabine for conditioning prior to allo-HSCT in adults with malignant and non-malignant diseases and in pediatric patients older than 1 month who have malignant diseases.
The CHMP’s recommendation for treosulfan will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of a CHMP recommendation.
The CHMP’s opinion of treosulfan is supported by results from a phase 3 trial (NCT00822393), which were presented at the 2017 ASH Annual Meeting.
In this trial, investigators compared two conditioning regimens, treosulfan-fludarabine and busulfan-fludarabine, in elderly or comorbid patients with acute myeloid leukemia or myelodysplastic syndromes who were undergoing allo-HSCT.
The ASH data included 476 patients from the final analysis.
Investigators said safety results between day -6 and day +28 were similar with the two regimens.
The same was true for trilineage engraftment and the cumulative incidence of relapse/progression at 24 months after allo-HSCT.
However, survival rates were higher in the treosulfan arm.
The event-free survival at 24 months was 64.0% in the treosulfan arm and 50.4% in the busulfan arm (P=0.0000164). The overall survival at 24 months was 72.5% and 56.4%, respectively (P=0.0082).
Transplant-related mortality at 24 months was 11.3% in the treosulfan arm and 28.2% in the busulfan arm (P=0.0201).
This trial was sponsored by medac GmbH.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for treosulfan (Trecondi) as part of conditioning prior to allogeneic hematopoietic stem cell transplant (allo-HSCT).
The full indication is for treosulfan to be used in combination with fludarabine for conditioning prior to allo-HSCT in adults with malignant and non-malignant diseases and in pediatric patients older than 1 month who have malignant diseases.
The CHMP’s recommendation for treosulfan will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of a CHMP recommendation.
The CHMP’s opinion of treosulfan is supported by results from a phase 3 trial (NCT00822393), which were presented at the 2017 ASH Annual Meeting.
In this trial, investigators compared two conditioning regimens, treosulfan-fludarabine and busulfan-fludarabine, in elderly or comorbid patients with acute myeloid leukemia or myelodysplastic syndromes who were undergoing allo-HSCT.
The ASH data included 476 patients from the final analysis.
Investigators said safety results between day -6 and day +28 were similar with the two regimens.
The same was true for trilineage engraftment and the cumulative incidence of relapse/progression at 24 months after allo-HSCT.
However, survival rates were higher in the treosulfan arm.
The event-free survival at 24 months was 64.0% in the treosulfan arm and 50.4% in the busulfan arm (P=0.0000164). The overall survival at 24 months was 72.5% and 56.4%, respectively (P=0.0082).
Transplant-related mortality at 24 months was 11.3% in the treosulfan arm and 28.2% in the busulfan arm (P=0.0201).
This trial was sponsored by medac GmbH.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for treosulfan (Trecondi) as part of conditioning prior to allogeneic hematopoietic stem cell transplant (allo-HSCT).
The full indication is for treosulfan to be used in combination with fludarabine for conditioning prior to allo-HSCT in adults with malignant and non-malignant diseases and in pediatric patients older than 1 month who have malignant diseases.
The CHMP’s recommendation for treosulfan will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of a CHMP recommendation.
The CHMP’s opinion of treosulfan is supported by results from a phase 3 trial (NCT00822393), which were presented at the 2017 ASH Annual Meeting.
In this trial, investigators compared two conditioning regimens, treosulfan-fludarabine and busulfan-fludarabine, in elderly or comorbid patients with acute myeloid leukemia or myelodysplastic syndromes who were undergoing allo-HSCT.
The ASH data included 476 patients from the final analysis.
Investigators said safety results between day -6 and day +28 were similar with the two regimens.
The same was true for trilineage engraftment and the cumulative incidence of relapse/progression at 24 months after allo-HSCT.
However, survival rates were higher in the treosulfan arm.
The event-free survival at 24 months was 64.0% in the treosulfan arm and 50.4% in the busulfan arm (P=0.0000164). The overall survival at 24 months was 72.5% and 56.4%, respectively (P=0.0082).
Transplant-related mortality at 24 months was 11.3% in the treosulfan arm and 28.2% in the busulfan arm (P=0.0201).
This trial was sponsored by medac GmbH.
MetS after HSCT linked to CV events, second cancers
SAN DIEGO—Patients who develop metabolic syndrome (MetS) after hematopoietic stem cell transplant (HSCT) have an increased risk of cardiovascular (CV) events and second malignancies, according to research presented at the 2018 ASH Annual Meeting.
Researchers found that HSCT recipients had a higher prevalence of MetS than the general population, and the incidence of MetS increased with age.
In addition, MetS was a predictor of CV events, and these events were associated with second malignancy.
“Our data support metabolic syndrome being an age-related late effect of transplant that is strongly associated with not only cardiovascular events but also the occurrence of second cancers, and this is a novel finding,” said Diana M. Greenfield, RN, PhD, of Sheffield Teaching Hospitals NHS Foundation Trust in Sheffield, United Kingdom.
Dr. Greenfield presented the data at ASH as abstract 251.
She noted that previous studies have reported rates of MetS after HSCT ranging from 31% to 49%. Intensive chemotherapy and radiation have been associated with MetS, and proposed mechanisms of MetS after HSCT include:
- Conditioning regimen-mediated damage to the neuro-hormonal system and vascular endothelium
- Immunological and inflammatory effects of allo-grafting, including graft-vs-host disease (GVHD) and treatment.
“Those with metabolic syndrome in the general population are already known to be twice as likely to develop cardiovascular disease as those without metabolic syndrome,” Dr. Greenfield noted. “The risk of cardiovascular hospitalizations and mortality is 3.6-fold higher in transplant patients vs the general population.”
With all this in mind, she and her colleagues set out to determine the prevalence of MetS and associated complications among HSCT recipients treated at 9 European centers in Belgium, France, Germany, Turkey, and the United Kingdom.
The researchers analyzed 462 patients—375 who had received an allogeneic HSCT and 87 who had undergone autologous HSCT. All patients were at least 18 years of age and at least 2 years post-HSCT.
The median age at transplant was 43 (interquartile range, 32-53), and 57.4% of patients were male.
Patients’ diagnoses included acute leukemia (37.9%), lymphoma (27.3%), myelodysplastic syndromes/myeloproliferative neoplasms (13%), chronic leukemia (12.3%), plasma cell disorders (5%), bone marrow failure (4.1%), solid tumors (0.2%), and inherited disorders (0.2%).
Results
The prevalence of MetS in this population was 30.4%. This is higher than the prevalence in the general population in Europe, which is 25%, according to the World Health Organization.
There was no significant difference in MetS prevalence between allogeneic and autologous HSCT recipients—29% and 35.6%, respectively.
However, there was a significant difference in MetS prevalence by age (P<0.001 with increasing age).
Among allogeneic HSCT recipients, there was no relationship between MetS prevalence and the presence or degree of acute or chronic GVHD, current use of immunosuppressive therapy, or conditioning intensity.
There was a significantly higher prevalence of CV events in patients with MetS than in patients without the syndrome—22.6% and 10.7%, respectively (P=0.006).
And logistic regression analysis confirmed that MetS is a predictor of CV events (odds ratio [OR]=4.72; 95% confidence interval [CI], 2.11-10.57).
The researchers also found that increasing age influenced the prevalence of MetS (OR=7.3; 95% CI, 3.2-16.8) and CV events (OR=3; 95% CI, 0.8-11.32) for patients older than 50, compared to patients in the 18-29 age group.
And CV events were associated with second malignancy (OR=7.93; 95% CI, 2.91-21.61).
“Early intervention of reversible features of metabolic syndrome with lifestyle and medical management may reduce the risk of cardiovascular events,” Dr. Greenfield said. “Meanwhile, screening and management should be robustly integrated within routine transplant long-term follow-up care.”
She added that the CIBMTR and EBMT guidelines on MetS and CV disease after HSCT should help in that regard.
Dr. Greenfield reported no conflicts of interest. However, her fellow researchers reported relationships with a range of pharmaceutical companies.
SAN DIEGO—Patients who develop metabolic syndrome (MetS) after hematopoietic stem cell transplant (HSCT) have an increased risk of cardiovascular (CV) events and second malignancies, according to research presented at the 2018 ASH Annual Meeting.
Researchers found that HSCT recipients had a higher prevalence of MetS than the general population, and the incidence of MetS increased with age.
In addition, MetS was a predictor of CV events, and these events were associated with second malignancy.
“Our data support metabolic syndrome being an age-related late effect of transplant that is strongly associated with not only cardiovascular events but also the occurrence of second cancers, and this is a novel finding,” said Diana M. Greenfield, RN, PhD, of Sheffield Teaching Hospitals NHS Foundation Trust in Sheffield, United Kingdom.
Dr. Greenfield presented the data at ASH as abstract 251.
She noted that previous studies have reported rates of MetS after HSCT ranging from 31% to 49%. Intensive chemotherapy and radiation have been associated with MetS, and proposed mechanisms of MetS after HSCT include:
- Conditioning regimen-mediated damage to the neuro-hormonal system and vascular endothelium
- Immunological and inflammatory effects of allo-grafting, including graft-vs-host disease (GVHD) and treatment.
“Those with metabolic syndrome in the general population are already known to be twice as likely to develop cardiovascular disease as those without metabolic syndrome,” Dr. Greenfield noted. “The risk of cardiovascular hospitalizations and mortality is 3.6-fold higher in transplant patients vs the general population.”
With all this in mind, she and her colleagues set out to determine the prevalence of MetS and associated complications among HSCT recipients treated at 9 European centers in Belgium, France, Germany, Turkey, and the United Kingdom.
The researchers analyzed 462 patients—375 who had received an allogeneic HSCT and 87 who had undergone autologous HSCT. All patients were at least 18 years of age and at least 2 years post-HSCT.
The median age at transplant was 43 (interquartile range, 32-53), and 57.4% of patients were male.
Patients’ diagnoses included acute leukemia (37.9%), lymphoma (27.3%), myelodysplastic syndromes/myeloproliferative neoplasms (13%), chronic leukemia (12.3%), plasma cell disorders (5%), bone marrow failure (4.1%), solid tumors (0.2%), and inherited disorders (0.2%).
Results
The prevalence of MetS in this population was 30.4%. This is higher than the prevalence in the general population in Europe, which is 25%, according to the World Health Organization.
There was no significant difference in MetS prevalence between allogeneic and autologous HSCT recipients—29% and 35.6%, respectively.
However, there was a significant difference in MetS prevalence by age (P<0.001 with increasing age).
Among allogeneic HSCT recipients, there was no relationship between MetS prevalence and the presence or degree of acute or chronic GVHD, current use of immunosuppressive therapy, or conditioning intensity.
There was a significantly higher prevalence of CV events in patients with MetS than in patients without the syndrome—22.6% and 10.7%, respectively (P=0.006).
And logistic regression analysis confirmed that MetS is a predictor of CV events (odds ratio [OR]=4.72; 95% confidence interval [CI], 2.11-10.57).
The researchers also found that increasing age influenced the prevalence of MetS (OR=7.3; 95% CI, 3.2-16.8) and CV events (OR=3; 95% CI, 0.8-11.32) for patients older than 50, compared to patients in the 18-29 age group.
And CV events were associated with second malignancy (OR=7.93; 95% CI, 2.91-21.61).
“Early intervention of reversible features of metabolic syndrome with lifestyle and medical management may reduce the risk of cardiovascular events,” Dr. Greenfield said. “Meanwhile, screening and management should be robustly integrated within routine transplant long-term follow-up care.”
She added that the CIBMTR and EBMT guidelines on MetS and CV disease after HSCT should help in that regard.
Dr. Greenfield reported no conflicts of interest. However, her fellow researchers reported relationships with a range of pharmaceutical companies.
SAN DIEGO—Patients who develop metabolic syndrome (MetS) after hematopoietic stem cell transplant (HSCT) have an increased risk of cardiovascular (CV) events and second malignancies, according to research presented at the 2018 ASH Annual Meeting.
Researchers found that HSCT recipients had a higher prevalence of MetS than the general population, and the incidence of MetS increased with age.
In addition, MetS was a predictor of CV events, and these events were associated with second malignancy.
“Our data support metabolic syndrome being an age-related late effect of transplant that is strongly associated with not only cardiovascular events but also the occurrence of second cancers, and this is a novel finding,” said Diana M. Greenfield, RN, PhD, of Sheffield Teaching Hospitals NHS Foundation Trust in Sheffield, United Kingdom.
Dr. Greenfield presented the data at ASH as abstract 251.
She noted that previous studies have reported rates of MetS after HSCT ranging from 31% to 49%. Intensive chemotherapy and radiation have been associated with MetS, and proposed mechanisms of MetS after HSCT include:
- Conditioning regimen-mediated damage to the neuro-hormonal system and vascular endothelium
- Immunological and inflammatory effects of allo-grafting, including graft-vs-host disease (GVHD) and treatment.
“Those with metabolic syndrome in the general population are already known to be twice as likely to develop cardiovascular disease as those without metabolic syndrome,” Dr. Greenfield noted. “The risk of cardiovascular hospitalizations and mortality is 3.6-fold higher in transplant patients vs the general population.”
With all this in mind, she and her colleagues set out to determine the prevalence of MetS and associated complications among HSCT recipients treated at 9 European centers in Belgium, France, Germany, Turkey, and the United Kingdom.
The researchers analyzed 462 patients—375 who had received an allogeneic HSCT and 87 who had undergone autologous HSCT. All patients were at least 18 years of age and at least 2 years post-HSCT.
The median age at transplant was 43 (interquartile range, 32-53), and 57.4% of patients were male.
Patients’ diagnoses included acute leukemia (37.9%), lymphoma (27.3%), myelodysplastic syndromes/myeloproliferative neoplasms (13%), chronic leukemia (12.3%), plasma cell disorders (5%), bone marrow failure (4.1%), solid tumors (0.2%), and inherited disorders (0.2%).
Results
The prevalence of MetS in this population was 30.4%. This is higher than the prevalence in the general population in Europe, which is 25%, according to the World Health Organization.
There was no significant difference in MetS prevalence between allogeneic and autologous HSCT recipients—29% and 35.6%, respectively.
However, there was a significant difference in MetS prevalence by age (P<0.001 with increasing age).
Among allogeneic HSCT recipients, there was no relationship between MetS prevalence and the presence or degree of acute or chronic GVHD, current use of immunosuppressive therapy, or conditioning intensity.
There was a significantly higher prevalence of CV events in patients with MetS than in patients without the syndrome—22.6% and 10.7%, respectively (P=0.006).
And logistic regression analysis confirmed that MetS is a predictor of CV events (odds ratio [OR]=4.72; 95% confidence interval [CI], 2.11-10.57).
The researchers also found that increasing age influenced the prevalence of MetS (OR=7.3; 95% CI, 3.2-16.8) and CV events (OR=3; 95% CI, 0.8-11.32) for patients older than 50, compared to patients in the 18-29 age group.
And CV events were associated with second malignancy (OR=7.93; 95% CI, 2.91-21.61).
“Early intervention of reversible features of metabolic syndrome with lifestyle and medical management may reduce the risk of cardiovascular events,” Dr. Greenfield said. “Meanwhile, screening and management should be robustly integrated within routine transplant long-term follow-up care.”
She added that the CIBMTR and EBMT guidelines on MetS and CV disease after HSCT should help in that regard.
Dr. Greenfield reported no conflicts of interest. However, her fellow researchers reported relationships with a range of pharmaceutical companies.