User login
Stigma is a family affair
Each year, 60 million Americans experience mental illness. Across the United States, each year, regardless of race, age, religion, or economic status, mental illness affects the lives of one in four adults and one in 10 children. This means that someone in every family has mental illness.
Most of our patients probably don’t tell anyone that they or one of their family members has mental illness They probably are doing what most of us do: Pretend it’s not there. Why? Because the stigma of mental illness is pervasive and destructive. What can we do to decrease the stigma?
The word stigma is derived from Greek and means "to mark the body." The bearer of the mark, or the stigma, is avoided and shunned. This practice has continued through the ages. In medieval times, if a person had a mental illness, he or she was thought to be possessed by demons and viewed as weak. Today, people with mental illness are viewed as menacing, deviant, unpredictable, incompetent, or even dangerous. It is entirely reasonable then, that we would want to avoid the stigma of mental illness. However, this prejudice against mental illness must be challenged.
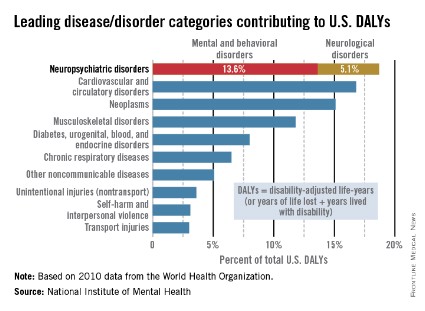
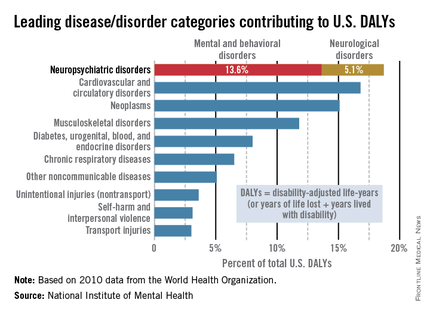
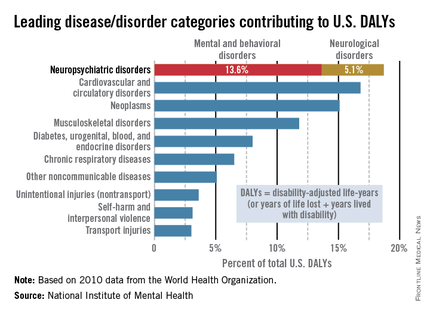
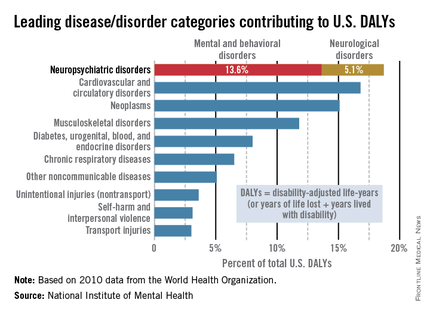
Mental illness accounts for increased morbidity and mortality as well as lifetime disability. The World Health Organization (WHO) estimates that neuropsychiatric disorders are the leading cause of disability in the United States, followed by cardiovascular and circulatory diseases, and neoplasms. The neuropsychiatric disorders category, which includes mental and behavioral disorders, accounts for 13.6% of total U.S. disability-adjusted life years (DALYs). Neurological disorders account for 5.1% of total U.S. DALYs.
Impact on the family
Not only does stigma affect individuals, it affects family members as well. Family members suffer from SBA, or stigma by association (Brit. J. Psych. 2002;181:494-8), also known as courtesy stigma (Social. Psychiatry Psychiatr. Epidemiol. 2003;38:593-602). Families share stigma because families share a genetic heritage. Families share stigma by assuming responsibility for their family members’ behaviors. Families share stigma because they are seen as having common motivations (J. Pers. Soc. Psychol. 2012;102:224-41).
SBA causes psychological distress in family members (Rehabil. Psychol. 2013;58:73-80; J. Nerv. Ment. Dis. 1987;175:4-11; Br. J. Psychiatry 2002;181:494-8; and Schizophr. Bull. 1998;24:115-126).
Psychological complaints, such as brooding, inner unrest, and irritability, and physical complaints, such as insomnia, fatigue, and neck and shoulder pain, have been attributed to the psychological distress of SBA. Family members may avoid social interactions and conceal their relationship to the family member who is mentally ill (Acad. Psychiatry 2008;32:87-91). They might psychologically distance themselves from a relative with mental illness.
SBA varies by disease type, family role, and age. The greatest SBA is associated with drug dependence. These family members are blamed for the illness, held responsible for relapse, and viewed as incompetent. In the study of Patrick W. Corrigan, Psy.D., (J. Fam. Psychol. 2006;20:239-46), family members report feelings of "contamination" and shame. Severe depression or panic and phobias engender less stigma. More educated people are less likely to report feelings of stigma.
According to Dr. Corrigan, SBA varies by family role: Parents are blamed for causing the child’s mental illness, siblings are blamed for not ensuring that relatives with mental illness adhere to treatment plans, and children are fearful of being "contaminated" with the mental illness of their parent. The closer the relationship, the less the stigma is perceived as defining the person. Family closeness can reduce stigma (The Gerontologist 2012;52:89-97). Regarding age, a British study showed that the highest stigma is reported in the 16- to 19-year-old age group (Br. J. Psychiatry 2000;177:4-7).
Psychiatry as a profession has not helped diminish stigma. It is not uncommon to hear psychiatrists assign blame to parents or spouses. Psychiatrists often believe that the family has a role in the patient’s illness. How many spouses have been told they are "codependent" with the implication that they have somehow "caused the illness"? What can we do diminish stigma?
Fighting stigma
Fighting stigma means confronting stigma (Advances in Psychiatric Treatment 2000;6:65-72). Most efforts worldwide have begun with the idea of educating people about mental illness. These efforts, focused on promoting mental illness as a biological illness, have had limited success and in some situations actually increased stigma (Acta Psychiatr. Scand. 2012; 125:440-52). The answer may lie in targeted education: specific facts for specific groups.
For example, young couples with children become less fearful after education targeted specifically for them (Br. J. Psychiatry 1996;168:191-8). Antistigma campaigns are common throughout the world. The websites of most professional psychiatric organizations, such as the American Psychiatric Association, the Royal College of Psychiatrists, and the College of Psychiatrists of Ireland, provide information about antistigma campaigns. Organizations often partner with mental health charities. Antistigma efforts also focus on publishing articles about stigma as the Lancet did in a series a few years ago (1998;352:1048). It is unclear whether these efforts reduce stigma. Dr. Corrigan suggests that meeting people who have mental illness weakens the tendency to link mental illness and violence (Psychiatric Rehabilitation Skills 2002;6: 312-34).
The current consensus is that antistigma campaigns should focus on the competence of people with mental illness. In this vein, the Scottish Mental Health Arts & Film Festival highlights the contributions that people with mental illness make to society. The festival, which began in 2007, also sponsors a contest for films that depict people with mental illness in realistic, holistic ways. In 2013, the festival drew 12,000 attendees and sparked 120 newspaper articles that emphasized the fact that people with mental illness are generally active, useful members of society.
Meanwhile, a Canadian antistigma campaign tells the stories of people with mental illness and provides evidence of the competence of these people. The APA’s public service video series, "A Healthy Minds Minute," features celebrities and prominent figures calling for equal access to quality care, and insurance coverage for people with mental illness and substance use disorders.
What do we do to reduce stigma? Psychiatrists such as William Beardslee have written about their personal experience of a family member with mental illness. A member of the Association of Family Psychiatrists, Julie Totten, lost her brother to suicide and in response, she developed an organization called Families for Depression Awareness, which is devoted to reducing the stigma of mental illness. For me, it is my personal campaign to say: "One in four means that someone in everyone’s family has mental illness."
What more can we do?
• Speak up when you hear or see stigma.
• Stress the normalcy of people who have mental illness.
• Come out of the closet on behalf of yourself or a family member.
• Include people who acknowledge they suffer from mental illness in antistigma campaigns.
• Discuss the role of stigma with patients and their families. Ask "How has stigma affected you as a family? In what ways has your family helped reduce the stigma of your mental illness?"
• Encourage attendance at support groups, such as NAMI (the National Alliance on Mental Illness).
• Embrace your family member or yourself: Look for personal qualities that wipe out stigma.
• Don’t allow people to stigmatize patients: It might be your family member they are talking about.
• Talk positively about respecting our patients.
• Start a conversation to reduce stigma.
• Remember that fighting stigma means confronting stigma.
Dr. Heru is an associate professor of psychiatry at the University of Colorado at Denver, Aurora. She has been a member of the Association of Family Psychiatrists since 2002 and currently serves as the organization’s treasurer. She is the author of a new book, "Working With Families in Medical Settings" (New York: Routledge, 2013).
Each year, 60 million Americans experience mental illness. Across the United States, each year, regardless of race, age, religion, or economic status, mental illness affects the lives of one in four adults and one in 10 children. This means that someone in every family has mental illness.
Most of our patients probably don’t tell anyone that they or one of their family members has mental illness They probably are doing what most of us do: Pretend it’s not there. Why? Because the stigma of mental illness is pervasive and destructive. What can we do to decrease the stigma?
The word stigma is derived from Greek and means "to mark the body." The bearer of the mark, or the stigma, is avoided and shunned. This practice has continued through the ages. In medieval times, if a person had a mental illness, he or she was thought to be possessed by demons and viewed as weak. Today, people with mental illness are viewed as menacing, deviant, unpredictable, incompetent, or even dangerous. It is entirely reasonable then, that we would want to avoid the stigma of mental illness. However, this prejudice against mental illness must be challenged.
Mental illness accounts for increased morbidity and mortality as well as lifetime disability. The World Health Organization (WHO) estimates that neuropsychiatric disorders are the leading cause of disability in the United States, followed by cardiovascular and circulatory diseases, and neoplasms. The neuropsychiatric disorders category, which includes mental and behavioral disorders, accounts for 13.6% of total U.S. disability-adjusted life years (DALYs). Neurological disorders account for 5.1% of total U.S. DALYs.
Impact on the family
Not only does stigma affect individuals, it affects family members as well. Family members suffer from SBA, or stigma by association (Brit. J. Psych. 2002;181:494-8), also known as courtesy stigma (Social. Psychiatry Psychiatr. Epidemiol. 2003;38:593-602). Families share stigma because families share a genetic heritage. Families share stigma by assuming responsibility for their family members’ behaviors. Families share stigma because they are seen as having common motivations (J. Pers. Soc. Psychol. 2012;102:224-41).
SBA causes psychological distress in family members (Rehabil. Psychol. 2013;58:73-80; J. Nerv. Ment. Dis. 1987;175:4-11; Br. J. Psychiatry 2002;181:494-8; and Schizophr. Bull. 1998;24:115-126).
Psychological complaints, such as brooding, inner unrest, and irritability, and physical complaints, such as insomnia, fatigue, and neck and shoulder pain, have been attributed to the psychological distress of SBA. Family members may avoid social interactions and conceal their relationship to the family member who is mentally ill (Acad. Psychiatry 2008;32:87-91). They might psychologically distance themselves from a relative with mental illness.
SBA varies by disease type, family role, and age. The greatest SBA is associated with drug dependence. These family members are blamed for the illness, held responsible for relapse, and viewed as incompetent. In the study of Patrick W. Corrigan, Psy.D., (J. Fam. Psychol. 2006;20:239-46), family members report feelings of "contamination" and shame. Severe depression or panic and phobias engender less stigma. More educated people are less likely to report feelings of stigma.
According to Dr. Corrigan, SBA varies by family role: Parents are blamed for causing the child’s mental illness, siblings are blamed for not ensuring that relatives with mental illness adhere to treatment plans, and children are fearful of being "contaminated" with the mental illness of their parent. The closer the relationship, the less the stigma is perceived as defining the person. Family closeness can reduce stigma (The Gerontologist 2012;52:89-97). Regarding age, a British study showed that the highest stigma is reported in the 16- to 19-year-old age group (Br. J. Psychiatry 2000;177:4-7).
Psychiatry as a profession has not helped diminish stigma. It is not uncommon to hear psychiatrists assign blame to parents or spouses. Psychiatrists often believe that the family has a role in the patient’s illness. How many spouses have been told they are "codependent" with the implication that they have somehow "caused the illness"? What can we do diminish stigma?
Fighting stigma
Fighting stigma means confronting stigma (Advances in Psychiatric Treatment 2000;6:65-72). Most efforts worldwide have begun with the idea of educating people about mental illness. These efforts, focused on promoting mental illness as a biological illness, have had limited success and in some situations actually increased stigma (Acta Psychiatr. Scand. 2012; 125:440-52). The answer may lie in targeted education: specific facts for specific groups.
For example, young couples with children become less fearful after education targeted specifically for them (Br. J. Psychiatry 1996;168:191-8). Antistigma campaigns are common throughout the world. The websites of most professional psychiatric organizations, such as the American Psychiatric Association, the Royal College of Psychiatrists, and the College of Psychiatrists of Ireland, provide information about antistigma campaigns. Organizations often partner with mental health charities. Antistigma efforts also focus on publishing articles about stigma as the Lancet did in a series a few years ago (1998;352:1048). It is unclear whether these efforts reduce stigma. Dr. Corrigan suggests that meeting people who have mental illness weakens the tendency to link mental illness and violence (Psychiatric Rehabilitation Skills 2002;6: 312-34).
The current consensus is that antistigma campaigns should focus on the competence of people with mental illness. In this vein, the Scottish Mental Health Arts & Film Festival highlights the contributions that people with mental illness make to society. The festival, which began in 2007, also sponsors a contest for films that depict people with mental illness in realistic, holistic ways. In 2013, the festival drew 12,000 attendees and sparked 120 newspaper articles that emphasized the fact that people with mental illness are generally active, useful members of society.
Meanwhile, a Canadian antistigma campaign tells the stories of people with mental illness and provides evidence of the competence of these people. The APA’s public service video series, "A Healthy Minds Minute," features celebrities and prominent figures calling for equal access to quality care, and insurance coverage for people with mental illness and substance use disorders.
What do we do to reduce stigma? Psychiatrists such as William Beardslee have written about their personal experience of a family member with mental illness. A member of the Association of Family Psychiatrists, Julie Totten, lost her brother to suicide and in response, she developed an organization called Families for Depression Awareness, which is devoted to reducing the stigma of mental illness. For me, it is my personal campaign to say: "One in four means that someone in everyone’s family has mental illness."
What more can we do?
• Speak up when you hear or see stigma.
• Stress the normalcy of people who have mental illness.
• Come out of the closet on behalf of yourself or a family member.
• Include people who acknowledge they suffer from mental illness in antistigma campaigns.
• Discuss the role of stigma with patients and their families. Ask "How has stigma affected you as a family? In what ways has your family helped reduce the stigma of your mental illness?"
• Encourage attendance at support groups, such as NAMI (the National Alliance on Mental Illness).
• Embrace your family member or yourself: Look for personal qualities that wipe out stigma.
• Don’t allow people to stigmatize patients: It might be your family member they are talking about.
• Talk positively about respecting our patients.
• Start a conversation to reduce stigma.
• Remember that fighting stigma means confronting stigma.
Dr. Heru is an associate professor of psychiatry at the University of Colorado at Denver, Aurora. She has been a member of the Association of Family Psychiatrists since 2002 and currently serves as the organization’s treasurer. She is the author of a new book, "Working With Families in Medical Settings" (New York: Routledge, 2013).
Each year, 60 million Americans experience mental illness. Across the United States, each year, regardless of race, age, religion, or economic status, mental illness affects the lives of one in four adults and one in 10 children. This means that someone in every family has mental illness.
Most of our patients probably don’t tell anyone that they or one of their family members has mental illness They probably are doing what most of us do: Pretend it’s not there. Why? Because the stigma of mental illness is pervasive and destructive. What can we do to decrease the stigma?
The word stigma is derived from Greek and means "to mark the body." The bearer of the mark, or the stigma, is avoided and shunned. This practice has continued through the ages. In medieval times, if a person had a mental illness, he or she was thought to be possessed by demons and viewed as weak. Today, people with mental illness are viewed as menacing, deviant, unpredictable, incompetent, or even dangerous. It is entirely reasonable then, that we would want to avoid the stigma of mental illness. However, this prejudice against mental illness must be challenged.
Mental illness accounts for increased morbidity and mortality as well as lifetime disability. The World Health Organization (WHO) estimates that neuropsychiatric disorders are the leading cause of disability in the United States, followed by cardiovascular and circulatory diseases, and neoplasms. The neuropsychiatric disorders category, which includes mental and behavioral disorders, accounts for 13.6% of total U.S. disability-adjusted life years (DALYs). Neurological disorders account for 5.1% of total U.S. DALYs.
Impact on the family
Not only does stigma affect individuals, it affects family members as well. Family members suffer from SBA, or stigma by association (Brit. J. Psych. 2002;181:494-8), also known as courtesy stigma (Social. Psychiatry Psychiatr. Epidemiol. 2003;38:593-602). Families share stigma because families share a genetic heritage. Families share stigma by assuming responsibility for their family members’ behaviors. Families share stigma because they are seen as having common motivations (J. Pers. Soc. Psychol. 2012;102:224-41).
SBA causes psychological distress in family members (Rehabil. Psychol. 2013;58:73-80; J. Nerv. Ment. Dis. 1987;175:4-11; Br. J. Psychiatry 2002;181:494-8; and Schizophr. Bull. 1998;24:115-126).
Psychological complaints, such as brooding, inner unrest, and irritability, and physical complaints, such as insomnia, fatigue, and neck and shoulder pain, have been attributed to the psychological distress of SBA. Family members may avoid social interactions and conceal their relationship to the family member who is mentally ill (Acad. Psychiatry 2008;32:87-91). They might psychologically distance themselves from a relative with mental illness.
SBA varies by disease type, family role, and age. The greatest SBA is associated with drug dependence. These family members are blamed for the illness, held responsible for relapse, and viewed as incompetent. In the study of Patrick W. Corrigan, Psy.D., (J. Fam. Psychol. 2006;20:239-46), family members report feelings of "contamination" and shame. Severe depression or panic and phobias engender less stigma. More educated people are less likely to report feelings of stigma.
According to Dr. Corrigan, SBA varies by family role: Parents are blamed for causing the child’s mental illness, siblings are blamed for not ensuring that relatives with mental illness adhere to treatment plans, and children are fearful of being "contaminated" with the mental illness of their parent. The closer the relationship, the less the stigma is perceived as defining the person. Family closeness can reduce stigma (The Gerontologist 2012;52:89-97). Regarding age, a British study showed that the highest stigma is reported in the 16- to 19-year-old age group (Br. J. Psychiatry 2000;177:4-7).
Psychiatry as a profession has not helped diminish stigma. It is not uncommon to hear psychiatrists assign blame to parents or spouses. Psychiatrists often believe that the family has a role in the patient’s illness. How many spouses have been told they are "codependent" with the implication that they have somehow "caused the illness"? What can we do diminish stigma?
Fighting stigma
Fighting stigma means confronting stigma (Advances in Psychiatric Treatment 2000;6:65-72). Most efforts worldwide have begun with the idea of educating people about mental illness. These efforts, focused on promoting mental illness as a biological illness, have had limited success and in some situations actually increased stigma (Acta Psychiatr. Scand. 2012; 125:440-52). The answer may lie in targeted education: specific facts for specific groups.
For example, young couples with children become less fearful after education targeted specifically for them (Br. J. Psychiatry 1996;168:191-8). Antistigma campaigns are common throughout the world. The websites of most professional psychiatric organizations, such as the American Psychiatric Association, the Royal College of Psychiatrists, and the College of Psychiatrists of Ireland, provide information about antistigma campaigns. Organizations often partner with mental health charities. Antistigma efforts also focus on publishing articles about stigma as the Lancet did in a series a few years ago (1998;352:1048). It is unclear whether these efforts reduce stigma. Dr. Corrigan suggests that meeting people who have mental illness weakens the tendency to link mental illness and violence (Psychiatric Rehabilitation Skills 2002;6: 312-34).
The current consensus is that antistigma campaigns should focus on the competence of people with mental illness. In this vein, the Scottish Mental Health Arts & Film Festival highlights the contributions that people with mental illness make to society. The festival, which began in 2007, also sponsors a contest for films that depict people with mental illness in realistic, holistic ways. In 2013, the festival drew 12,000 attendees and sparked 120 newspaper articles that emphasized the fact that people with mental illness are generally active, useful members of society.
Meanwhile, a Canadian antistigma campaign tells the stories of people with mental illness and provides evidence of the competence of these people. The APA’s public service video series, "A Healthy Minds Minute," features celebrities and prominent figures calling for equal access to quality care, and insurance coverage for people with mental illness and substance use disorders.
What do we do to reduce stigma? Psychiatrists such as William Beardslee have written about their personal experience of a family member with mental illness. A member of the Association of Family Psychiatrists, Julie Totten, lost her brother to suicide and in response, she developed an organization called Families for Depression Awareness, which is devoted to reducing the stigma of mental illness. For me, it is my personal campaign to say: "One in four means that someone in everyone’s family has mental illness."
What more can we do?
• Speak up when you hear or see stigma.
• Stress the normalcy of people who have mental illness.
• Come out of the closet on behalf of yourself or a family member.
• Include people who acknowledge they suffer from mental illness in antistigma campaigns.
• Discuss the role of stigma with patients and their families. Ask "How has stigma affected you as a family? In what ways has your family helped reduce the stigma of your mental illness?"
• Encourage attendance at support groups, such as NAMI (the National Alliance on Mental Illness).
• Embrace your family member or yourself: Look for personal qualities that wipe out stigma.
• Don’t allow people to stigmatize patients: It might be your family member they are talking about.
• Talk positively about respecting our patients.
• Start a conversation to reduce stigma.
• Remember that fighting stigma means confronting stigma.
Dr. Heru is an associate professor of psychiatry at the University of Colorado at Denver, Aurora. She has been a member of the Association of Family Psychiatrists since 2002 and currently serves as the organization’s treasurer. She is the author of a new book, "Working With Families in Medical Settings" (New York: Routledge, 2013).
Thinking about the institution of marriage – Part II
An earlier column reviewed the institution of marriage up to the middle of the last century. Since the 1950s, postmodernism has been gathering momentum, beginning as a critique of art, architecture, philosophy, and how we think about society and culture. Views on many aspects of our lives, as we live it, began to change.
Postmodernism stands in contrast to the "modern’ " or scientific view that touts a singularity of truth and a singular view of the world. Social construction is a type of postmodern theory that states that truth, reality, and knowledge are based in the social context of that particular person. This aspect of postmodernism is most applicable to mental health professionals assessing and treating patients, and to families in specific social and cultural contexts.
A postmodern view of the family considers the traditional view of the family, the "nuclear family," as only one view. Other forms of family and other views of marriage that had been marginalized, considered deviant and nonconforming, are now brought forward and considered as viable alternatives. Postmodernism discards many assumptions that we have been taught. One assumption that is being reexamined, for example, is that sexual nonexclusivity or extra-relationship sex, or romantic involvements are symptoms of troubled relationships or forms of sexual acting out.
Another assumption that needs to be reexamined is the notion that family structures found in other cultures are "abnormal" or dysfunctional. These assumptions are not necessarily true or false but require assessment in context of the relationship at hand. Postmodernism challenges us to assess each family variation on its own merit.
Beginnings
In the 20th century, Monica McGoldrick, Ph.D., one of the strong voices in family therapy, advocated for increased sensitivity to cultural variation. Her book, "Ethnicity and Family Therapy" (New York: The Guilford Press, 2005), describes characteristics of common ethnicities in American society.
Family therapists have attempted to address "nontraditional" families with articles, for example, about raising a biracial child, what to do if your child identifies as gay, etc. Most older articles focused on helping families "cope" with the nontraditional. Family therapists are now more willing to acknowledge "difference" as a normal rather than a pathological variant, and to recognize strengths inherent in diversity.
Acknowledging diversity
Marlene F. Watson, Ph.D., brings a nuanced understanding of the African American family, detailing the effect of slavery on the individuals in the family, and how internalized racism can be recognized and managed in family therapy (e-book, "Facing the Black Shadow," 2013). This is an important book for therapists, especially those who come from traditional families, as it articulates the reality of African American lives in a way that therapists can apply to clinical practice.
Dr. Watson illustrates through case examples how internalized racism affects marriages, and offers effective ways to help couples negotiate and overcome the negative aspects of their heritage. A postmodern stance also will help the couple recognize the resilience and strengths that are inherent in overcoming adversity.
Linda M. Burton, Ph.D., and Cecily R. Hardaway, Ph.D., highlight the role of "othermothers" in raising children in low-income families, be they white, Latino, or African American. They define "othermothering" as a form of coparenting, distinct from stepparenting. Women othermother children who are their romantic partners’ children from previous and concurrent relationships. Compared to stepfamilies, these multiple partner fertility relationships are more prevalent among young couples with limited financial resources, contentious relationships, and serial childbearing through serial repartnering.
In general, low-income women and women of color take on this style of coparenting to help the biological parents of relatives and friends who have limited social and psychological capital to protect and raise "good children"(Fam. Process. 2012;51:343-59). Family therapists will become much more effective if they understand and recognize that the motivation behind this form of mothering fosters resilience in the mothers. The more we know and understand alternate family structures, the more we can work toward building and sustaining resilience.
Assimilation has for many decades been the main focus of political and therapeutic endeavors. In postmodern times, transnationalism described a new way of thinking about relationships that extend across national boundaries and cultures (Fam. Process. 2007;46:157-71).
Immigrants maintain connections with their countries of origin with children who are parented by grandparents, or other relatives, perhaps in several countries at the same time. Family members use Skype, often daily, to connect with the matriarch or patriarch "back home."
Postmodern theories of social justice and cultural diversity work well with immigrants, bringing multiple perspectives into the treatment room. Immigrants bring many complex and diverse values in relation to marriage, gender, parenting, and religious practices. A social justice approach focuses on the racism and discrimination that is common in the lives of immigrants. Marriage might take place across nations, be arranged, or might be mixed race or mixed nationalities. Therapy that acknowledges these complexities will be most helpful. We still need to think further about global family life, how relationships evolve over long distances, and how to develop systemic and transnational interventions for separations and reunifications.
Sex and marriage
Nelson Mandela’s father had four wives, and he reported in an interview that he considered all of them his mothers and gained support from them all.
Polygamy has flourished in Africa and Asia for centuries, and more than 40 countries recognize polygamous marriages. In the former Soviet republic of Kazakhstan, rich Kazakhs used to buy second wives from parents, often in exchange for livestock. Since Kazakhstan’s independence in 1991, polygamy, although illegal, has again become common practice and is a status symbol for rich Kazakhs. Polygamy reportedly also is a way out of poverty for young women who save money and support their relatives back home
In the United Kingdom, polygamy has become more common in Muslim communities. Successful British Muslim women, who have delayed marriage to build careers, may choose to become a co-wife. They choose to share a husband in a relationship that they see as sanctioned by Islam. These women retain an independent lifestyle. "I didn’t want a full-time husband," one Muslim woman noted in an interview.
In the United States, the practice of polygamy was officially ended in the Mormon church in 1890. Nevertheless, several small "fundamentalist" groups continue the practice. One family of 14 wives and 17 children, the Browns of Nevada, are stars of a reality show that they reportedly hope educates the public about the choice.
Polyandry, a woman with multiple husbands, is described in many cultures. This practice frequently involves the marriage of all brothers in a family to the same wife, which allows family-owned land to remain undivided. In some cultures, such as the Inuit, a man might arrange a second husband (frequently his brother) for his wife because he knows that, when he is absent, the second husband will protect his wife. Should she become pregnant while he is gone, it would be by someone he had approved in advance.
Penn State’s Stephen Beckerman, Ph.D., and his colleagues, in their study of the Bari people of Venezuela, found that children understood to have two fathers are significantly more likely to survive to age 15 than are children with only one. This is called "informal polyandry," because while the two fathers might not be formally married to and living with the mother in all cases, the society around them officially recognizes both men as legitimate mates to the mother, and father to her child.
Polyamory, the practice of open, multiple-partner relationships, is a structure that is increasingly common in Western countries, according to sociologist Elisabeth Sheff, Ph.D. Dr. Sheff’s 15 years of research leads her to believe that polyamory is a "legitimate relationship style that can be tremendously rewarding for adults and provide excellent nurturing for children."
She said she has found that children aged 5-8 do not seem to care about how the adults relate to one another, as long as they are taken care of. Overall, such children seem to fare well as long as they live in stable, loving homes.
Making this practice work, she acknowledges, is "time consuming and potentially fraught with emotional booby traps." People in polyamorous relationships emphasize that their relationships are about emotional connections with others, as opposed to primarily physical relationships.
The term polyfidelity, a subset of polyamory, was coined in the 1970s by members of the Kerista commune, which started in New York City in 1956. Polyfidelity is a concept in which clusters of friends form nonmonogamous sexual relationships. Under this family structure, group members do not relate sexually to anyone outside of the family group.
Although mainstream Judaism does not accept polyamory, some people do consider themselves Jewish and polyamorous. Sharon Kleinbaum, the senior rabbi at Congregation Beit Simchat Torah in New York, has said that polyamory is a choice that does not preclude a Jewishly observant, socially conscious life. Some polyamorous Jews also point to biblical patriarchs having multiple wives and concubines as evidence that polyamorous relationships can be sacred in Judaism.
Jim Fleckenstein, director of the Institute for 21st-Century Relationships, has said that the polyamory movement has been driven by science fiction and feminism. He states that disillusionment with monogamy occurs "because of widespread cheating and divorce."
One fact going for the polys (as they are often known), is the belief that polyamory is more honest and less hypocritical than monogamy with secret affairs. A manual, "What Psychology Professionals Should Know About Polyamory," for psychotherapists who deal with polyamorous clients, was published in September 2009 by the National Coalition for Sexual Freedom.
The late Michael Shernoff, who was an openly gay psychotherapist, wrote that nonmonogamy is "a well-accepted part of gay subculture," and that somewhere between 30% and 67% of men in male couples reported being in a sexually nonmonogamous relationship. A majority of male couples are not sexually exclusive, but describe themselves as emotionally monogamous.
Mr. Shernoff stated: One of the biggest differences between male couples and mixed-sex couples is that many, but by no means all, within the gay community have an easier acceptance of sexual nonexclusivity than does heterosexual society in general. Research confirms that nonmonogamy in and of itself does not create a problem for male couples when it has been openly negotiated (Fam. Process. 2006;45:407-18).
The role of affairs in marriage can now be subjected to a more nuanced discussion, after digesting the above views and practice of marriage. What is the meaning of an affair? What is an open relationship? What are the models of intimacy? Is an affair a breach in the couple’s definition of intimacy? What are the rules? How does a couple define an affair within the context of their own relationship?
Conclusion
Postmodernism provides family therapists a new set of theories and a new language for describing the variety of families. As Jacqueline Hudak, Ph.D., and Shawn V. Giammattei, Ph.D., have written: "As family therapists, we are uniquely poised to transform the meanings attached to ‘marriage’ and ‘family,’ to focus on the quality of relationships rather than on the gender of a partner or the assumption of particular roles" ("Expanding Our Social Justice Practices: Advances in Theory and Practice," Washington: American Family Therapy Academy, Winter 2010).
The traditional view of marriage is referred to as "heteronormativity" and is defined by the belief that a viable family consists of "a heterosexual mother and a father raising heterosexual children together" ("Handbook of Qualitative Research," Thousand Oaks, Calif.:Sage, 2000). Despite the above expansion of views on marriage and families, heteronormativity remains the current organizing principle of family theory, practice, research, and training. It will take many decades to shift the dominant paradigm. Developing awareness, and listening to families and couples is the first step.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
An earlier column reviewed the institution of marriage up to the middle of the last century. Since the 1950s, postmodernism has been gathering momentum, beginning as a critique of art, architecture, philosophy, and how we think about society and culture. Views on many aspects of our lives, as we live it, began to change.
Postmodernism stands in contrast to the "modern’ " or scientific view that touts a singularity of truth and a singular view of the world. Social construction is a type of postmodern theory that states that truth, reality, and knowledge are based in the social context of that particular person. This aspect of postmodernism is most applicable to mental health professionals assessing and treating patients, and to families in specific social and cultural contexts.
A postmodern view of the family considers the traditional view of the family, the "nuclear family," as only one view. Other forms of family and other views of marriage that had been marginalized, considered deviant and nonconforming, are now brought forward and considered as viable alternatives. Postmodernism discards many assumptions that we have been taught. One assumption that is being reexamined, for example, is that sexual nonexclusivity or extra-relationship sex, or romantic involvements are symptoms of troubled relationships or forms of sexual acting out.
Another assumption that needs to be reexamined is the notion that family structures found in other cultures are "abnormal" or dysfunctional. These assumptions are not necessarily true or false but require assessment in context of the relationship at hand. Postmodernism challenges us to assess each family variation on its own merit.
Beginnings
In the 20th century, Monica McGoldrick, Ph.D., one of the strong voices in family therapy, advocated for increased sensitivity to cultural variation. Her book, "Ethnicity and Family Therapy" (New York: The Guilford Press, 2005), describes characteristics of common ethnicities in American society.
Family therapists have attempted to address "nontraditional" families with articles, for example, about raising a biracial child, what to do if your child identifies as gay, etc. Most older articles focused on helping families "cope" with the nontraditional. Family therapists are now more willing to acknowledge "difference" as a normal rather than a pathological variant, and to recognize strengths inherent in diversity.
Acknowledging diversity
Marlene F. Watson, Ph.D., brings a nuanced understanding of the African American family, detailing the effect of slavery on the individuals in the family, and how internalized racism can be recognized and managed in family therapy (e-book, "Facing the Black Shadow," 2013). This is an important book for therapists, especially those who come from traditional families, as it articulates the reality of African American lives in a way that therapists can apply to clinical practice.
Dr. Watson illustrates through case examples how internalized racism affects marriages, and offers effective ways to help couples negotiate and overcome the negative aspects of their heritage. A postmodern stance also will help the couple recognize the resilience and strengths that are inherent in overcoming adversity.
Linda M. Burton, Ph.D., and Cecily R. Hardaway, Ph.D., highlight the role of "othermothers" in raising children in low-income families, be they white, Latino, or African American. They define "othermothering" as a form of coparenting, distinct from stepparenting. Women othermother children who are their romantic partners’ children from previous and concurrent relationships. Compared to stepfamilies, these multiple partner fertility relationships are more prevalent among young couples with limited financial resources, contentious relationships, and serial childbearing through serial repartnering.
In general, low-income women and women of color take on this style of coparenting to help the biological parents of relatives and friends who have limited social and psychological capital to protect and raise "good children"(Fam. Process. 2012;51:343-59). Family therapists will become much more effective if they understand and recognize that the motivation behind this form of mothering fosters resilience in the mothers. The more we know and understand alternate family structures, the more we can work toward building and sustaining resilience.
Assimilation has for many decades been the main focus of political and therapeutic endeavors. In postmodern times, transnationalism described a new way of thinking about relationships that extend across national boundaries and cultures (Fam. Process. 2007;46:157-71).
Immigrants maintain connections with their countries of origin with children who are parented by grandparents, or other relatives, perhaps in several countries at the same time. Family members use Skype, often daily, to connect with the matriarch or patriarch "back home."
Postmodern theories of social justice and cultural diversity work well with immigrants, bringing multiple perspectives into the treatment room. Immigrants bring many complex and diverse values in relation to marriage, gender, parenting, and religious practices. A social justice approach focuses on the racism and discrimination that is common in the lives of immigrants. Marriage might take place across nations, be arranged, or might be mixed race or mixed nationalities. Therapy that acknowledges these complexities will be most helpful. We still need to think further about global family life, how relationships evolve over long distances, and how to develop systemic and transnational interventions for separations and reunifications.
Sex and marriage
Nelson Mandela’s father had four wives, and he reported in an interview that he considered all of them his mothers and gained support from them all.
Polygamy has flourished in Africa and Asia for centuries, and more than 40 countries recognize polygamous marriages. In the former Soviet republic of Kazakhstan, rich Kazakhs used to buy second wives from parents, often in exchange for livestock. Since Kazakhstan’s independence in 1991, polygamy, although illegal, has again become common practice and is a status symbol for rich Kazakhs. Polygamy reportedly also is a way out of poverty for young women who save money and support their relatives back home
In the United Kingdom, polygamy has become more common in Muslim communities. Successful British Muslim women, who have delayed marriage to build careers, may choose to become a co-wife. They choose to share a husband in a relationship that they see as sanctioned by Islam. These women retain an independent lifestyle. "I didn’t want a full-time husband," one Muslim woman noted in an interview.
In the United States, the practice of polygamy was officially ended in the Mormon church in 1890. Nevertheless, several small "fundamentalist" groups continue the practice. One family of 14 wives and 17 children, the Browns of Nevada, are stars of a reality show that they reportedly hope educates the public about the choice.
Polyandry, a woman with multiple husbands, is described in many cultures. This practice frequently involves the marriage of all brothers in a family to the same wife, which allows family-owned land to remain undivided. In some cultures, such as the Inuit, a man might arrange a second husband (frequently his brother) for his wife because he knows that, when he is absent, the second husband will protect his wife. Should she become pregnant while he is gone, it would be by someone he had approved in advance.
Penn State’s Stephen Beckerman, Ph.D., and his colleagues, in their study of the Bari people of Venezuela, found that children understood to have two fathers are significantly more likely to survive to age 15 than are children with only one. This is called "informal polyandry," because while the two fathers might not be formally married to and living with the mother in all cases, the society around them officially recognizes both men as legitimate mates to the mother, and father to her child.
Polyamory, the practice of open, multiple-partner relationships, is a structure that is increasingly common in Western countries, according to sociologist Elisabeth Sheff, Ph.D. Dr. Sheff’s 15 years of research leads her to believe that polyamory is a "legitimate relationship style that can be tremendously rewarding for adults and provide excellent nurturing for children."
She said she has found that children aged 5-8 do not seem to care about how the adults relate to one another, as long as they are taken care of. Overall, such children seem to fare well as long as they live in stable, loving homes.
Making this practice work, she acknowledges, is "time consuming and potentially fraught with emotional booby traps." People in polyamorous relationships emphasize that their relationships are about emotional connections with others, as opposed to primarily physical relationships.
The term polyfidelity, a subset of polyamory, was coined in the 1970s by members of the Kerista commune, which started in New York City in 1956. Polyfidelity is a concept in which clusters of friends form nonmonogamous sexual relationships. Under this family structure, group members do not relate sexually to anyone outside of the family group.
Although mainstream Judaism does not accept polyamory, some people do consider themselves Jewish and polyamorous. Sharon Kleinbaum, the senior rabbi at Congregation Beit Simchat Torah in New York, has said that polyamory is a choice that does not preclude a Jewishly observant, socially conscious life. Some polyamorous Jews also point to biblical patriarchs having multiple wives and concubines as evidence that polyamorous relationships can be sacred in Judaism.
Jim Fleckenstein, director of the Institute for 21st-Century Relationships, has said that the polyamory movement has been driven by science fiction and feminism. He states that disillusionment with monogamy occurs "because of widespread cheating and divorce."
One fact going for the polys (as they are often known), is the belief that polyamory is more honest and less hypocritical than monogamy with secret affairs. A manual, "What Psychology Professionals Should Know About Polyamory," for psychotherapists who deal with polyamorous clients, was published in September 2009 by the National Coalition for Sexual Freedom.
The late Michael Shernoff, who was an openly gay psychotherapist, wrote that nonmonogamy is "a well-accepted part of gay subculture," and that somewhere between 30% and 67% of men in male couples reported being in a sexually nonmonogamous relationship. A majority of male couples are not sexually exclusive, but describe themselves as emotionally monogamous.
Mr. Shernoff stated: One of the biggest differences between male couples and mixed-sex couples is that many, but by no means all, within the gay community have an easier acceptance of sexual nonexclusivity than does heterosexual society in general. Research confirms that nonmonogamy in and of itself does not create a problem for male couples when it has been openly negotiated (Fam. Process. 2006;45:407-18).
The role of affairs in marriage can now be subjected to a more nuanced discussion, after digesting the above views and practice of marriage. What is the meaning of an affair? What is an open relationship? What are the models of intimacy? Is an affair a breach in the couple’s definition of intimacy? What are the rules? How does a couple define an affair within the context of their own relationship?
Conclusion
Postmodernism provides family therapists a new set of theories and a new language for describing the variety of families. As Jacqueline Hudak, Ph.D., and Shawn V. Giammattei, Ph.D., have written: "As family therapists, we are uniquely poised to transform the meanings attached to ‘marriage’ and ‘family,’ to focus on the quality of relationships rather than on the gender of a partner or the assumption of particular roles" ("Expanding Our Social Justice Practices: Advances in Theory and Practice," Washington: American Family Therapy Academy, Winter 2010).
The traditional view of marriage is referred to as "heteronormativity" and is defined by the belief that a viable family consists of "a heterosexual mother and a father raising heterosexual children together" ("Handbook of Qualitative Research," Thousand Oaks, Calif.:Sage, 2000). Despite the above expansion of views on marriage and families, heteronormativity remains the current organizing principle of family theory, practice, research, and training. It will take many decades to shift the dominant paradigm. Developing awareness, and listening to families and couples is the first step.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
An earlier column reviewed the institution of marriage up to the middle of the last century. Since the 1950s, postmodernism has been gathering momentum, beginning as a critique of art, architecture, philosophy, and how we think about society and culture. Views on many aspects of our lives, as we live it, began to change.
Postmodernism stands in contrast to the "modern’ " or scientific view that touts a singularity of truth and a singular view of the world. Social construction is a type of postmodern theory that states that truth, reality, and knowledge are based in the social context of that particular person. This aspect of postmodernism is most applicable to mental health professionals assessing and treating patients, and to families in specific social and cultural contexts.
A postmodern view of the family considers the traditional view of the family, the "nuclear family," as only one view. Other forms of family and other views of marriage that had been marginalized, considered deviant and nonconforming, are now brought forward and considered as viable alternatives. Postmodernism discards many assumptions that we have been taught. One assumption that is being reexamined, for example, is that sexual nonexclusivity or extra-relationship sex, or romantic involvements are symptoms of troubled relationships or forms of sexual acting out.
Another assumption that needs to be reexamined is the notion that family structures found in other cultures are "abnormal" or dysfunctional. These assumptions are not necessarily true or false but require assessment in context of the relationship at hand. Postmodernism challenges us to assess each family variation on its own merit.
Beginnings
In the 20th century, Monica McGoldrick, Ph.D., one of the strong voices in family therapy, advocated for increased sensitivity to cultural variation. Her book, "Ethnicity and Family Therapy" (New York: The Guilford Press, 2005), describes characteristics of common ethnicities in American society.
Family therapists have attempted to address "nontraditional" families with articles, for example, about raising a biracial child, what to do if your child identifies as gay, etc. Most older articles focused on helping families "cope" with the nontraditional. Family therapists are now more willing to acknowledge "difference" as a normal rather than a pathological variant, and to recognize strengths inherent in diversity.
Acknowledging diversity
Marlene F. Watson, Ph.D., brings a nuanced understanding of the African American family, detailing the effect of slavery on the individuals in the family, and how internalized racism can be recognized and managed in family therapy (e-book, "Facing the Black Shadow," 2013). This is an important book for therapists, especially those who come from traditional families, as it articulates the reality of African American lives in a way that therapists can apply to clinical practice.
Dr. Watson illustrates through case examples how internalized racism affects marriages, and offers effective ways to help couples negotiate and overcome the negative aspects of their heritage. A postmodern stance also will help the couple recognize the resilience and strengths that are inherent in overcoming adversity.
Linda M. Burton, Ph.D., and Cecily R. Hardaway, Ph.D., highlight the role of "othermothers" in raising children in low-income families, be they white, Latino, or African American. They define "othermothering" as a form of coparenting, distinct from stepparenting. Women othermother children who are their romantic partners’ children from previous and concurrent relationships. Compared to stepfamilies, these multiple partner fertility relationships are more prevalent among young couples with limited financial resources, contentious relationships, and serial childbearing through serial repartnering.
In general, low-income women and women of color take on this style of coparenting to help the biological parents of relatives and friends who have limited social and psychological capital to protect and raise "good children"(Fam. Process. 2012;51:343-59). Family therapists will become much more effective if they understand and recognize that the motivation behind this form of mothering fosters resilience in the mothers. The more we know and understand alternate family structures, the more we can work toward building and sustaining resilience.
Assimilation has for many decades been the main focus of political and therapeutic endeavors. In postmodern times, transnationalism described a new way of thinking about relationships that extend across national boundaries and cultures (Fam. Process. 2007;46:157-71).
Immigrants maintain connections with their countries of origin with children who are parented by grandparents, or other relatives, perhaps in several countries at the same time. Family members use Skype, often daily, to connect with the matriarch or patriarch "back home."
Postmodern theories of social justice and cultural diversity work well with immigrants, bringing multiple perspectives into the treatment room. Immigrants bring many complex and diverse values in relation to marriage, gender, parenting, and religious practices. A social justice approach focuses on the racism and discrimination that is common in the lives of immigrants. Marriage might take place across nations, be arranged, or might be mixed race or mixed nationalities. Therapy that acknowledges these complexities will be most helpful. We still need to think further about global family life, how relationships evolve over long distances, and how to develop systemic and transnational interventions for separations and reunifications.
Sex and marriage
Nelson Mandela’s father had four wives, and he reported in an interview that he considered all of them his mothers and gained support from them all.
Polygamy has flourished in Africa and Asia for centuries, and more than 40 countries recognize polygamous marriages. In the former Soviet republic of Kazakhstan, rich Kazakhs used to buy second wives from parents, often in exchange for livestock. Since Kazakhstan’s independence in 1991, polygamy, although illegal, has again become common practice and is a status symbol for rich Kazakhs. Polygamy reportedly also is a way out of poverty for young women who save money and support their relatives back home
In the United Kingdom, polygamy has become more common in Muslim communities. Successful British Muslim women, who have delayed marriage to build careers, may choose to become a co-wife. They choose to share a husband in a relationship that they see as sanctioned by Islam. These women retain an independent lifestyle. "I didn’t want a full-time husband," one Muslim woman noted in an interview.
In the United States, the practice of polygamy was officially ended in the Mormon church in 1890. Nevertheless, several small "fundamentalist" groups continue the practice. One family of 14 wives and 17 children, the Browns of Nevada, are stars of a reality show that they reportedly hope educates the public about the choice.
Polyandry, a woman with multiple husbands, is described in many cultures. This practice frequently involves the marriage of all brothers in a family to the same wife, which allows family-owned land to remain undivided. In some cultures, such as the Inuit, a man might arrange a second husband (frequently his brother) for his wife because he knows that, when he is absent, the second husband will protect his wife. Should she become pregnant while he is gone, it would be by someone he had approved in advance.
Penn State’s Stephen Beckerman, Ph.D., and his colleagues, in their study of the Bari people of Venezuela, found that children understood to have two fathers are significantly more likely to survive to age 15 than are children with only one. This is called "informal polyandry," because while the two fathers might not be formally married to and living with the mother in all cases, the society around them officially recognizes both men as legitimate mates to the mother, and father to her child.
Polyamory, the practice of open, multiple-partner relationships, is a structure that is increasingly common in Western countries, according to sociologist Elisabeth Sheff, Ph.D. Dr. Sheff’s 15 years of research leads her to believe that polyamory is a "legitimate relationship style that can be tremendously rewarding for adults and provide excellent nurturing for children."
She said she has found that children aged 5-8 do not seem to care about how the adults relate to one another, as long as they are taken care of. Overall, such children seem to fare well as long as they live in stable, loving homes.
Making this practice work, she acknowledges, is "time consuming and potentially fraught with emotional booby traps." People in polyamorous relationships emphasize that their relationships are about emotional connections with others, as opposed to primarily physical relationships.
The term polyfidelity, a subset of polyamory, was coined in the 1970s by members of the Kerista commune, which started in New York City in 1956. Polyfidelity is a concept in which clusters of friends form nonmonogamous sexual relationships. Under this family structure, group members do not relate sexually to anyone outside of the family group.
Although mainstream Judaism does not accept polyamory, some people do consider themselves Jewish and polyamorous. Sharon Kleinbaum, the senior rabbi at Congregation Beit Simchat Torah in New York, has said that polyamory is a choice that does not preclude a Jewishly observant, socially conscious life. Some polyamorous Jews also point to biblical patriarchs having multiple wives and concubines as evidence that polyamorous relationships can be sacred in Judaism.
Jim Fleckenstein, director of the Institute for 21st-Century Relationships, has said that the polyamory movement has been driven by science fiction and feminism. He states that disillusionment with monogamy occurs "because of widespread cheating and divorce."
One fact going for the polys (as they are often known), is the belief that polyamory is more honest and less hypocritical than monogamy with secret affairs. A manual, "What Psychology Professionals Should Know About Polyamory," for psychotherapists who deal with polyamorous clients, was published in September 2009 by the National Coalition for Sexual Freedom.
The late Michael Shernoff, who was an openly gay psychotherapist, wrote that nonmonogamy is "a well-accepted part of gay subculture," and that somewhere between 30% and 67% of men in male couples reported being in a sexually nonmonogamous relationship. A majority of male couples are not sexually exclusive, but describe themselves as emotionally monogamous.
Mr. Shernoff stated: One of the biggest differences between male couples and mixed-sex couples is that many, but by no means all, within the gay community have an easier acceptance of sexual nonexclusivity than does heterosexual society in general. Research confirms that nonmonogamy in and of itself does not create a problem for male couples when it has been openly negotiated (Fam. Process. 2006;45:407-18).
The role of affairs in marriage can now be subjected to a more nuanced discussion, after digesting the above views and practice of marriage. What is the meaning of an affair? What is an open relationship? What are the models of intimacy? Is an affair a breach in the couple’s definition of intimacy? What are the rules? How does a couple define an affair within the context of their own relationship?
Conclusion
Postmodernism provides family therapists a new set of theories and a new language for describing the variety of families. As Jacqueline Hudak, Ph.D., and Shawn V. Giammattei, Ph.D., have written: "As family therapists, we are uniquely poised to transform the meanings attached to ‘marriage’ and ‘family,’ to focus on the quality of relationships rather than on the gender of a partner or the assumption of particular roles" ("Expanding Our Social Justice Practices: Advances in Theory and Practice," Washington: American Family Therapy Academy, Winter 2010).
The traditional view of marriage is referred to as "heteronormativity" and is defined by the belief that a viable family consists of "a heterosexual mother and a father raising heterosexual children together" ("Handbook of Qualitative Research," Thousand Oaks, Calif.:Sage, 2000). Despite the above expansion of views on marriage and families, heteronormativity remains the current organizing principle of family theory, practice, research, and training. It will take many decades to shift the dominant paradigm. Developing awareness, and listening to families and couples is the first step.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Thinking about the institution of marriage – Part I
Throughout history, views of marriage have evolved as societies change. Since the 6th century, the Roman Catholic Church has played a prominent role in thinking and developing our ideas about marriage and family. In October, the church sent out a document that included a questionnaire to its bishops around the world to find out what Catholics think about the "modern family." The Vatican sent out the document in preparation for the Synod of Bishops on the Family, which is slated for October 2014. Before we get the results, let’s review how society has reflected on marriage and family.
Historically, marriages often were strategic alliances between families. It was common for marriage to be between first and second cousins in order to strengthen family ties. Polygamy has been common throughout history and continues in many communities to this day.
Monogamy is also found throughout history, but in 1215, the Catholic Church decreed that partners had to publicly post notices of an impending marriage in a local parish to cut down on the number of invalid marriages. Until the 1500s, the Catholic Church accepted a couple’s word that they had exchanged marriage vows, with no witnesses or corroborating evidence needed. In the 1500s, with the rise in Protestantism, marriage became a civil matter rather than a sacrament. By 1639, states such as Massachusetts began requiring marriage licenses, and by the 19th century, marriage licenses were common in the United States.
Marriage through the ages
Here is a listing of the way in which marriage has been conceptualized over the years:
Arranged alliances: A strategic alliance between families.
Family ties: Keeping alliances within the family; the majority of all marriages throughout history were between first and second cousins.
Polygamy: A phenomenon that has been common throughout history.
Babies optional: In many early cultures, men could dissolve a marriage or take another wife if a woman was infertile. However, the early Christian church was a trailblazer in arguing that marriage was not contingent upon producing offspring.
Monogamy: This practice became the guiding principle for Western marriages between the 6th and 9th centuries because of the church.
Sacred vs. secular: In 1215, the Roman Catholic Church decreed that partners had to publicly post notices, or banns, of an impending marriage in a local parish in order to cut down on the number of invalid marriages. Until the 1500s, the church accepted a couple’s word that they had exchanged marriage vows, with no witnesses or corroborating evidence needed.
Civil marriage: By 1639, states such as Massachusetts began requiring marriage licenses and, by the 19th century, marriage licenses were common in the United States.
Romance: By the 1900s, mutual attraction became important.
Market economics: Families historically controlled access to inheritance of agricultural land, but with the spread of a market economy, it becomes possible for people to marry outside of this inheritance.
Women’s equality: About 50 years ago, in Western countries, women and men began to have equal rights and responsibilities. Instead of being about unique, gender-based roles, most partners conceived of their unions in terms of flexible divisions of labor, companionship, and mutual sexual attraction.
Same-sex marriages: One of the reasons for the stunningly rapid increase in acceptance of same-sex marriage is because heterosexuals have completely changed their notion that all marriages are between a man and a woman, notes Stephanie Coontz, Ph.D. "We now believe marriage is based on love, mutual sexual attraction, equality, and a flexible division of labor."
Source: Adapted from "Marriage, a History: From Obedience to Intimacy, or How Love Conquered Marriage," (New York: Viking, 2005), by Dr. Coontz.
A sacred view of marriage
The Catholic position throughout history has been that marriage is one of the seven sacraments bestowed by Christ. This questionnaire is an attempt by the Vatican to understand more about "mixed or interreligious marriages; the single-parent family; polygamy; marriages with the consequent problem of a dowry, sometimes understood as the purchase price of the woman; the caste system; a culture of noncommitment and a presumption that the marriage bond can be temporary; forms of feminism hostile to the Church; migration and the reformulation of the very concept of the family; relativist pluralism in the conception of marriage; the influence of the media on popular culture in its understanding of marriage and family life; underlying trends of thought in legislative proposals which devalue the idea of permanence and faithfulness in the marriage covenant; an increase in the practice of surrogate motherhood (wombs for hire); and new interpretations of what is considered a human right."
Thirty-nine questions are on the questionnaire. Questions 4, 5, and 6 are of most interest to family psychiatrists. Deserving of admiration is its concern for families in migration and for the mistreatment of women.
The terms "regular" and "irregular," used in the questionnaire, are canonical terms unrelated to what actually happens in any given society. It should also be explained that Catholics who married always had to declare that they would welcome such children as God happened to send along, recognizing that he might choose not to send any. A decision to refuse to accept the possibility of children invalidated the marriage vows and constitutes grounds for annulment.
Excerpts from the Vatican document
Questions 4, 5, and 6 of the Vatican’s questionnaire seem aimed at gathering data on different kinds of families. Here are those three questions:
Pastoral Care in Certain Difficult Marital Situations
a) Is cohabitation ad experimentum a pastoral reality in your particular Church? Can you approximate a percentage?
b) Do unions which are not recognized either religiously or civilly exist? Are reliable statistics available?
c) Are separated couples and those divorced and remarried a pastoral reality in your particular Church? Can you approximate a percentage? How do you deal with this situation in appropriate pastoral programmes? (sic)
d) In all the above cases, how do the baptized live in this irregular situation? Are they aware of it? Are they simply indifferent? Do they feel marginalized or suffer from the impossibility of receiving the sacraments?
f) Could a simplification of canonical practice in recognizing a declaration of nullity of the marriage bond provide a positive contribution to solving the problems of the persons involved? If yes, what form would it take?
Does a ministry exist to attend to these cases? Describe this pastoral ministry? Do such programmes exist on the national and diocesan levels? How is God’s mercy proclaimed to separated couples and those divorced and remarried, and how does the Church put into practice her support for them in their journey of faith?
On Unions of Persons of the Same Sex
a) Is there a law in your country recognizing civil unions for people of the same-sex and equating it in some way to marriage?
b) What is the attitude of the local and particular Churches towards both the State as the promoter of civil unions between persons of the same sex and the people involved in this type of union?
c) What pastoral attention can be given to people who have chosen to live in these types of union?
In the case of unions of persons of the same sex who have adopted children, what can be done pastorally in light of transmitting the faith?
The Education of Children in Irregular Marriages
a) What is the estimated proportion of children and adolescents in these cases, as regards children who are born and raised in regularly constituted families?
b) How do parents in these situations approach the Church? What do they ask? Do they request the sacraments only or do they also want catechesis and the general teaching of religion?
c) How do the particular Churches attempt to meet the needs of the parents of these children to provide them with a Christian education?
Source: Pastoral Challenges to the Family in the Context of Evangelization
A secular view of marriage
A secular view of marriage has been advanced by economists Betsey Stevenson, Ph.D., and Justin Wolfers, Ph.D., who describe the extent to which marriage is shaped by economic forces. "Productive marriage" is based on a division of labor. In the earlier part of the 20th century in Western countries, school, education, and the emerging TV and magazine markets illustrated how women could be good homemakers and men could be good providers. The liberation of women through education and access to birth control changed the playing field. Prior to this, college-educated women were the least likely to marry. Since the 1960s and 1970s, educated women could prevent pregnancy and support themselves, and found little use for the previous productive model of marriage.
Men, also, did not see educated, financially independent women as suitable marriage partners. The high divorce rate among those who married in the1970s reflected discontent with this model of the productive marriage.
In contrast, Dr. Stevenson and Dr. Wolfers write, "hedonic marriage" occurs when people who marry are of similar age, educational background, and perhaps occupation. The hedonic marriage better suits educated women who seek a companion, and it thrives when time and resources are available to enjoy companionable life. Same-sex marriages make sense when considered in this broad frame. Supporting this concept is the fact that couples who have married in recent years are more likely to stay together than were their parents’ generation. Of course, this discourse is only relevant in parts of the world in which women have access to birth control and opportunities for education, work, and social standing.
Romance and marriage
The question of romance in marriage is the hardest for psychiatrists, as scientists, to address. Romance has always been around, sometimes present in marriages and sometimes not. Romance is thought to be both essential and nonessential to marriage, depending on the purpose of the marriage. A good discussion by Dr. Henry Grunebaum can be found an article titled "Thinking about romantic/erotic love" in the Journal of Marital and Family Therapy(1997;23:295-307). His main points are that we do not have control over our feelings of romantic/erotic love, that these feelings occur relatively infrequently during most people’s lives, that being with a partner whom one loves, is valued and regarded as a good, that it sometimes conflicts with other values and goods, and lastly that although love is regarded as one essential basis for marriage, other qualities and capacities are important in sustaining a long-term relationship such as a marriage. He concludes with, "What makes matters even more challenging is the fact that we ask a great deal of marriage, of any serious intimate relationship. Perhaps the greatest demand we make is that it should combine passion and stability, romance and monogamy, transports of tenderness and excitement from the person who will also perform the many mundane tasks of daily living. In other words, meld everyday love with romantic/erotic love." He offers suggestions for discussion and guidelines for therapists.
Applying all of this in our work
As family psychiatrists, we can allow couples and families a therapeutic space to discuss the meaning and assumptions in their marriage. We can discuss the frame of the marriage: Is it sacred, secular, or postmodern? In this way, we can provide a context to the current struggles that couples and families might have.
To begin, we can ask about the past. We can say, "People get married for different reasons. What were your reasons? Do you consider your marriage to be a sacred or a secular? What does this mean to you?"
Delving deeper and focusing more on the present, "What is your current experience of your marriage? How do your expectations differ now than from your expectations in the past? What is the role of romance in your marriage?
What type of marriage did you want when you began this marriage? Is there romance in your marriage? What kind of marriage do you want now?
Focusing on going forward we can ask: "What works well in your marriage/family? What are your strengths? What needs to change in your marriage?"
In the late 1970s, postmodernism emerged in the world. Postmodernism stands in contrast to the "modern" or scientific view that touts a singularity of truth and a singular view of the world. Social construction is a type of postmodern theory that states that truth, reality, and knowledge are based in the social context of that particular person. Inevitably, postmodernism affects how we think about and conceptualize marriage. Postmodernism and marriage will be the subject of the next column.
I would like to thank Peter Chaloner, M.A., LL.B, B.A. (Honors), and Dip. Theo., for his comments and corrections.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Throughout history, views of marriage have evolved as societies change. Since the 6th century, the Roman Catholic Church has played a prominent role in thinking and developing our ideas about marriage and family. In October, the church sent out a document that included a questionnaire to its bishops around the world to find out what Catholics think about the "modern family." The Vatican sent out the document in preparation for the Synod of Bishops on the Family, which is slated for October 2014. Before we get the results, let’s review how society has reflected on marriage and family.
Historically, marriages often were strategic alliances between families. It was common for marriage to be between first and second cousins in order to strengthen family ties. Polygamy has been common throughout history and continues in many communities to this day.
Monogamy is also found throughout history, but in 1215, the Catholic Church decreed that partners had to publicly post notices of an impending marriage in a local parish to cut down on the number of invalid marriages. Until the 1500s, the Catholic Church accepted a couple’s word that they had exchanged marriage vows, with no witnesses or corroborating evidence needed. In the 1500s, with the rise in Protestantism, marriage became a civil matter rather than a sacrament. By 1639, states such as Massachusetts began requiring marriage licenses, and by the 19th century, marriage licenses were common in the United States.
Marriage through the ages
Here is a listing of the way in which marriage has been conceptualized over the years:
Arranged alliances: A strategic alliance between families.
Family ties: Keeping alliances within the family; the majority of all marriages throughout history were between first and second cousins.
Polygamy: A phenomenon that has been common throughout history.
Babies optional: In many early cultures, men could dissolve a marriage or take another wife if a woman was infertile. However, the early Christian church was a trailblazer in arguing that marriage was not contingent upon producing offspring.
Monogamy: This practice became the guiding principle for Western marriages between the 6th and 9th centuries because of the church.
Sacred vs. secular: In 1215, the Roman Catholic Church decreed that partners had to publicly post notices, or banns, of an impending marriage in a local parish in order to cut down on the number of invalid marriages. Until the 1500s, the church accepted a couple’s word that they had exchanged marriage vows, with no witnesses or corroborating evidence needed.
Civil marriage: By 1639, states such as Massachusetts began requiring marriage licenses and, by the 19th century, marriage licenses were common in the United States.
Romance: By the 1900s, mutual attraction became important.
Market economics: Families historically controlled access to inheritance of agricultural land, but with the spread of a market economy, it becomes possible for people to marry outside of this inheritance.
Women’s equality: About 50 years ago, in Western countries, women and men began to have equal rights and responsibilities. Instead of being about unique, gender-based roles, most partners conceived of their unions in terms of flexible divisions of labor, companionship, and mutual sexual attraction.
Same-sex marriages: One of the reasons for the stunningly rapid increase in acceptance of same-sex marriage is because heterosexuals have completely changed their notion that all marriages are between a man and a woman, notes Stephanie Coontz, Ph.D. "We now believe marriage is based on love, mutual sexual attraction, equality, and a flexible division of labor."
Source: Adapted from "Marriage, a History: From Obedience to Intimacy, or How Love Conquered Marriage," (New York: Viking, 2005), by Dr. Coontz.
A sacred view of marriage
The Catholic position throughout history has been that marriage is one of the seven sacraments bestowed by Christ. This questionnaire is an attempt by the Vatican to understand more about "mixed or interreligious marriages; the single-parent family; polygamy; marriages with the consequent problem of a dowry, sometimes understood as the purchase price of the woman; the caste system; a culture of noncommitment and a presumption that the marriage bond can be temporary; forms of feminism hostile to the Church; migration and the reformulation of the very concept of the family; relativist pluralism in the conception of marriage; the influence of the media on popular culture in its understanding of marriage and family life; underlying trends of thought in legislative proposals which devalue the idea of permanence and faithfulness in the marriage covenant; an increase in the practice of surrogate motherhood (wombs for hire); and new interpretations of what is considered a human right."
Thirty-nine questions are on the questionnaire. Questions 4, 5, and 6 are of most interest to family psychiatrists. Deserving of admiration is its concern for families in migration and for the mistreatment of women.
The terms "regular" and "irregular," used in the questionnaire, are canonical terms unrelated to what actually happens in any given society. It should also be explained that Catholics who married always had to declare that they would welcome such children as God happened to send along, recognizing that he might choose not to send any. A decision to refuse to accept the possibility of children invalidated the marriage vows and constitutes grounds for annulment.
Excerpts from the Vatican document
Questions 4, 5, and 6 of the Vatican’s questionnaire seem aimed at gathering data on different kinds of families. Here are those three questions:
Pastoral Care in Certain Difficult Marital Situations
a) Is cohabitation ad experimentum a pastoral reality in your particular Church? Can you approximate a percentage?
b) Do unions which are not recognized either religiously or civilly exist? Are reliable statistics available?
c) Are separated couples and those divorced and remarried a pastoral reality in your particular Church? Can you approximate a percentage? How do you deal with this situation in appropriate pastoral programmes? (sic)
d) In all the above cases, how do the baptized live in this irregular situation? Are they aware of it? Are they simply indifferent? Do they feel marginalized or suffer from the impossibility of receiving the sacraments?
f) Could a simplification of canonical practice in recognizing a declaration of nullity of the marriage bond provide a positive contribution to solving the problems of the persons involved? If yes, what form would it take?
Does a ministry exist to attend to these cases? Describe this pastoral ministry? Do such programmes exist on the national and diocesan levels? How is God’s mercy proclaimed to separated couples and those divorced and remarried, and how does the Church put into practice her support for them in their journey of faith?
On Unions of Persons of the Same Sex
a) Is there a law in your country recognizing civil unions for people of the same-sex and equating it in some way to marriage?
b) What is the attitude of the local and particular Churches towards both the State as the promoter of civil unions between persons of the same sex and the people involved in this type of union?
c) What pastoral attention can be given to people who have chosen to live in these types of union?
In the case of unions of persons of the same sex who have adopted children, what can be done pastorally in light of transmitting the faith?
The Education of Children in Irregular Marriages
a) What is the estimated proportion of children and adolescents in these cases, as regards children who are born and raised in regularly constituted families?
b) How do parents in these situations approach the Church? What do they ask? Do they request the sacraments only or do they also want catechesis and the general teaching of religion?
c) How do the particular Churches attempt to meet the needs of the parents of these children to provide them with a Christian education?
Source: Pastoral Challenges to the Family in the Context of Evangelization
A secular view of marriage
A secular view of marriage has been advanced by economists Betsey Stevenson, Ph.D., and Justin Wolfers, Ph.D., who describe the extent to which marriage is shaped by economic forces. "Productive marriage" is based on a division of labor. In the earlier part of the 20th century in Western countries, school, education, and the emerging TV and magazine markets illustrated how women could be good homemakers and men could be good providers. The liberation of women through education and access to birth control changed the playing field. Prior to this, college-educated women were the least likely to marry. Since the 1960s and 1970s, educated women could prevent pregnancy and support themselves, and found little use for the previous productive model of marriage.
Men, also, did not see educated, financially independent women as suitable marriage partners. The high divorce rate among those who married in the1970s reflected discontent with this model of the productive marriage.
In contrast, Dr. Stevenson and Dr. Wolfers write, "hedonic marriage" occurs when people who marry are of similar age, educational background, and perhaps occupation. The hedonic marriage better suits educated women who seek a companion, and it thrives when time and resources are available to enjoy companionable life. Same-sex marriages make sense when considered in this broad frame. Supporting this concept is the fact that couples who have married in recent years are more likely to stay together than were their parents’ generation. Of course, this discourse is only relevant in parts of the world in which women have access to birth control and opportunities for education, work, and social standing.
Romance and marriage
The question of romance in marriage is the hardest for psychiatrists, as scientists, to address. Romance has always been around, sometimes present in marriages and sometimes not. Romance is thought to be both essential and nonessential to marriage, depending on the purpose of the marriage. A good discussion by Dr. Henry Grunebaum can be found an article titled "Thinking about romantic/erotic love" in the Journal of Marital and Family Therapy(1997;23:295-307). His main points are that we do not have control over our feelings of romantic/erotic love, that these feelings occur relatively infrequently during most people’s lives, that being with a partner whom one loves, is valued and regarded as a good, that it sometimes conflicts with other values and goods, and lastly that although love is regarded as one essential basis for marriage, other qualities and capacities are important in sustaining a long-term relationship such as a marriage. He concludes with, "What makes matters even more challenging is the fact that we ask a great deal of marriage, of any serious intimate relationship. Perhaps the greatest demand we make is that it should combine passion and stability, romance and monogamy, transports of tenderness and excitement from the person who will also perform the many mundane tasks of daily living. In other words, meld everyday love with romantic/erotic love." He offers suggestions for discussion and guidelines for therapists.
Applying all of this in our work
As family psychiatrists, we can allow couples and families a therapeutic space to discuss the meaning and assumptions in their marriage. We can discuss the frame of the marriage: Is it sacred, secular, or postmodern? In this way, we can provide a context to the current struggles that couples and families might have.
To begin, we can ask about the past. We can say, "People get married for different reasons. What were your reasons? Do you consider your marriage to be a sacred or a secular? What does this mean to you?"
Delving deeper and focusing more on the present, "What is your current experience of your marriage? How do your expectations differ now than from your expectations in the past? What is the role of romance in your marriage?
What type of marriage did you want when you began this marriage? Is there romance in your marriage? What kind of marriage do you want now?
Focusing on going forward we can ask: "What works well in your marriage/family? What are your strengths? What needs to change in your marriage?"
In the late 1970s, postmodernism emerged in the world. Postmodernism stands in contrast to the "modern" or scientific view that touts a singularity of truth and a singular view of the world. Social construction is a type of postmodern theory that states that truth, reality, and knowledge are based in the social context of that particular person. Inevitably, postmodernism affects how we think about and conceptualize marriage. Postmodernism and marriage will be the subject of the next column.
I would like to thank Peter Chaloner, M.A., LL.B, B.A. (Honors), and Dip. Theo., for his comments and corrections.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Throughout history, views of marriage have evolved as societies change. Since the 6th century, the Roman Catholic Church has played a prominent role in thinking and developing our ideas about marriage and family. In October, the church sent out a document that included a questionnaire to its bishops around the world to find out what Catholics think about the "modern family." The Vatican sent out the document in preparation for the Synod of Bishops on the Family, which is slated for October 2014. Before we get the results, let’s review how society has reflected on marriage and family.
Historically, marriages often were strategic alliances between families. It was common for marriage to be between first and second cousins in order to strengthen family ties. Polygamy has been common throughout history and continues in many communities to this day.
Monogamy is also found throughout history, but in 1215, the Catholic Church decreed that partners had to publicly post notices of an impending marriage in a local parish to cut down on the number of invalid marriages. Until the 1500s, the Catholic Church accepted a couple’s word that they had exchanged marriage vows, with no witnesses or corroborating evidence needed. In the 1500s, with the rise in Protestantism, marriage became a civil matter rather than a sacrament. By 1639, states such as Massachusetts began requiring marriage licenses, and by the 19th century, marriage licenses were common in the United States.
Marriage through the ages
Here is a listing of the way in which marriage has been conceptualized over the years:
Arranged alliances: A strategic alliance between families.
Family ties: Keeping alliances within the family; the majority of all marriages throughout history were between first and second cousins.
Polygamy: A phenomenon that has been common throughout history.
Babies optional: In many early cultures, men could dissolve a marriage or take another wife if a woman was infertile. However, the early Christian church was a trailblazer in arguing that marriage was not contingent upon producing offspring.
Monogamy: This practice became the guiding principle for Western marriages between the 6th and 9th centuries because of the church.
Sacred vs. secular: In 1215, the Roman Catholic Church decreed that partners had to publicly post notices, or banns, of an impending marriage in a local parish in order to cut down on the number of invalid marriages. Until the 1500s, the church accepted a couple’s word that they had exchanged marriage vows, with no witnesses or corroborating evidence needed.
Civil marriage: By 1639, states such as Massachusetts began requiring marriage licenses and, by the 19th century, marriage licenses were common in the United States.
Romance: By the 1900s, mutual attraction became important.
Market economics: Families historically controlled access to inheritance of agricultural land, but with the spread of a market economy, it becomes possible for people to marry outside of this inheritance.
Women’s equality: About 50 years ago, in Western countries, women and men began to have equal rights and responsibilities. Instead of being about unique, gender-based roles, most partners conceived of their unions in terms of flexible divisions of labor, companionship, and mutual sexual attraction.
Same-sex marriages: One of the reasons for the stunningly rapid increase in acceptance of same-sex marriage is because heterosexuals have completely changed their notion that all marriages are between a man and a woman, notes Stephanie Coontz, Ph.D. "We now believe marriage is based on love, mutual sexual attraction, equality, and a flexible division of labor."
Source: Adapted from "Marriage, a History: From Obedience to Intimacy, or How Love Conquered Marriage," (New York: Viking, 2005), by Dr. Coontz.
A sacred view of marriage
The Catholic position throughout history has been that marriage is one of the seven sacraments bestowed by Christ. This questionnaire is an attempt by the Vatican to understand more about "mixed or interreligious marriages; the single-parent family; polygamy; marriages with the consequent problem of a dowry, sometimes understood as the purchase price of the woman; the caste system; a culture of noncommitment and a presumption that the marriage bond can be temporary; forms of feminism hostile to the Church; migration and the reformulation of the very concept of the family; relativist pluralism in the conception of marriage; the influence of the media on popular culture in its understanding of marriage and family life; underlying trends of thought in legislative proposals which devalue the idea of permanence and faithfulness in the marriage covenant; an increase in the practice of surrogate motherhood (wombs for hire); and new interpretations of what is considered a human right."
Thirty-nine questions are on the questionnaire. Questions 4, 5, and 6 are of most interest to family psychiatrists. Deserving of admiration is its concern for families in migration and for the mistreatment of women.
The terms "regular" and "irregular," used in the questionnaire, are canonical terms unrelated to what actually happens in any given society. It should also be explained that Catholics who married always had to declare that they would welcome such children as God happened to send along, recognizing that he might choose not to send any. A decision to refuse to accept the possibility of children invalidated the marriage vows and constitutes grounds for annulment.
Excerpts from the Vatican document
Questions 4, 5, and 6 of the Vatican’s questionnaire seem aimed at gathering data on different kinds of families. Here are those three questions:
Pastoral Care in Certain Difficult Marital Situations
a) Is cohabitation ad experimentum a pastoral reality in your particular Church? Can you approximate a percentage?
b) Do unions which are not recognized either religiously or civilly exist? Are reliable statistics available?
c) Are separated couples and those divorced and remarried a pastoral reality in your particular Church? Can you approximate a percentage? How do you deal with this situation in appropriate pastoral programmes? (sic)
d) In all the above cases, how do the baptized live in this irregular situation? Are they aware of it? Are they simply indifferent? Do they feel marginalized or suffer from the impossibility of receiving the sacraments?
f) Could a simplification of canonical practice in recognizing a declaration of nullity of the marriage bond provide a positive contribution to solving the problems of the persons involved? If yes, what form would it take?
Does a ministry exist to attend to these cases? Describe this pastoral ministry? Do such programmes exist on the national and diocesan levels? How is God’s mercy proclaimed to separated couples and those divorced and remarried, and how does the Church put into practice her support for them in their journey of faith?
On Unions of Persons of the Same Sex
a) Is there a law in your country recognizing civil unions for people of the same-sex and equating it in some way to marriage?
b) What is the attitude of the local and particular Churches towards both the State as the promoter of civil unions between persons of the same sex and the people involved in this type of union?
c) What pastoral attention can be given to people who have chosen to live in these types of union?
In the case of unions of persons of the same sex who have adopted children, what can be done pastorally in light of transmitting the faith?
The Education of Children in Irregular Marriages
a) What is the estimated proportion of children and adolescents in these cases, as regards children who are born and raised in regularly constituted families?
b) How do parents in these situations approach the Church? What do they ask? Do they request the sacraments only or do they also want catechesis and the general teaching of religion?
c) How do the particular Churches attempt to meet the needs of the parents of these children to provide them with a Christian education?
Source: Pastoral Challenges to the Family in the Context of Evangelization
A secular view of marriage
A secular view of marriage has been advanced by economists Betsey Stevenson, Ph.D., and Justin Wolfers, Ph.D., who describe the extent to which marriage is shaped by economic forces. "Productive marriage" is based on a division of labor. In the earlier part of the 20th century in Western countries, school, education, and the emerging TV and magazine markets illustrated how women could be good homemakers and men could be good providers. The liberation of women through education and access to birth control changed the playing field. Prior to this, college-educated women were the least likely to marry. Since the 1960s and 1970s, educated women could prevent pregnancy and support themselves, and found little use for the previous productive model of marriage.
Men, also, did not see educated, financially independent women as suitable marriage partners. The high divorce rate among those who married in the1970s reflected discontent with this model of the productive marriage.
In contrast, Dr. Stevenson and Dr. Wolfers write, "hedonic marriage" occurs when people who marry are of similar age, educational background, and perhaps occupation. The hedonic marriage better suits educated women who seek a companion, and it thrives when time and resources are available to enjoy companionable life. Same-sex marriages make sense when considered in this broad frame. Supporting this concept is the fact that couples who have married in recent years are more likely to stay together than were their parents’ generation. Of course, this discourse is only relevant in parts of the world in which women have access to birth control and opportunities for education, work, and social standing.
Romance and marriage
The question of romance in marriage is the hardest for psychiatrists, as scientists, to address. Romance has always been around, sometimes present in marriages and sometimes not. Romance is thought to be both essential and nonessential to marriage, depending on the purpose of the marriage. A good discussion by Dr. Henry Grunebaum can be found an article titled "Thinking about romantic/erotic love" in the Journal of Marital and Family Therapy(1997;23:295-307). His main points are that we do not have control over our feelings of romantic/erotic love, that these feelings occur relatively infrequently during most people’s lives, that being with a partner whom one loves, is valued and regarded as a good, that it sometimes conflicts with other values and goods, and lastly that although love is regarded as one essential basis for marriage, other qualities and capacities are important in sustaining a long-term relationship such as a marriage. He concludes with, "What makes matters even more challenging is the fact that we ask a great deal of marriage, of any serious intimate relationship. Perhaps the greatest demand we make is that it should combine passion and stability, romance and monogamy, transports of tenderness and excitement from the person who will also perform the many mundane tasks of daily living. In other words, meld everyday love with romantic/erotic love." He offers suggestions for discussion and guidelines for therapists.
Applying all of this in our work
As family psychiatrists, we can allow couples and families a therapeutic space to discuss the meaning and assumptions in their marriage. We can discuss the frame of the marriage: Is it sacred, secular, or postmodern? In this way, we can provide a context to the current struggles that couples and families might have.
To begin, we can ask about the past. We can say, "People get married for different reasons. What were your reasons? Do you consider your marriage to be a sacred or a secular? What does this mean to you?"
Delving deeper and focusing more on the present, "What is your current experience of your marriage? How do your expectations differ now than from your expectations in the past? What is the role of romance in your marriage?
What type of marriage did you want when you began this marriage? Is there romance in your marriage? What kind of marriage do you want now?
Focusing on going forward we can ask: "What works well in your marriage/family? What are your strengths? What needs to change in your marriage?"
In the late 1970s, postmodernism emerged in the world. Postmodernism stands in contrast to the "modern" or scientific view that touts a singularity of truth and a singular view of the world. Social construction is a type of postmodern theory that states that truth, reality, and knowledge are based in the social context of that particular person. Inevitably, postmodernism affects how we think about and conceptualize marriage. Postmodernism and marriage will be the subject of the next column.
I would like to thank Peter Chaloner, M.A., LL.B, B.A. (Honors), and Dip. Theo., for his comments and corrections.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
The essential role of family in treating bipolar disorder
Kevin was doing very well in law school, until he showed up at his professor’s house in the middle of the night. Normally a thoughtful, quiet, introverted young man, Kevin was hardly recognizable to his professor, who found him outside yelling loudly and demanding to speak about an underground conspiracy he believed he had uncovered. He had always been a good student, and his family was very proud of his accomplishments up until now. At the age of 24, Kevin’s first manic episode was triggered by late nights studying for his law school exams and marijuana use to cope with stress.
Police responded to noise complaints, and Kevin was hospitalized. The manic episode resolved surprisingly quickly in the absence of marijuana use and with the help of an atypical antipsychotic. The patient’s intelligence and articulate lawyer-in-training charm made his inpatient doctors hard pressed to justify an extended hospital stay, and he was discharged 3 days later with a prescription and instructions for follow-up. He promptly discarded both.
When his next manic episode arose, Kevin disappeared for 2 weeks, and after fearing the worst, Kevin’s family was relieved to receive a call from Kevin’s aunt, who lived across the country and had just found him at her doorstep. This time, without the involvement of law enforcement, there seemed to be no way for Kevin’s mother, father, older sister, and aunt to persuade Kevin to enter the hospital or to take medications. Kevin’s aunt accompanied him on a plane home, and in the face of Kevin’s unwillingness to enter treatment alone, they decided to enter treatment as a family.
Predictors of episodes
The strongest predictors of future episodes and poor outcome in patients with bipolar disorder are a greater number of previous episodes, shorter intervals between episodes, a history of psychosis, a history of anxiety, persistence of affective symptoms and episodes, and stressful life events. Some evidence has suggested that poor job functioning, lack of social support, increased expressed emotion in the family, and introverted or obsessional personality traits all might predict poor outcome in bipolar disorder (J. Psychiatr. Pract. 2006;12:269-82).
An overwhelmingly emotional home environment can make a large contribution to relapse. Multiple studies have shown that a high level of "expressed emotion" (characterized by overinvolvement and excessive criticism) predicts patient relapse independent of medication compliance, baseline symptoms, and demographics (Arch. Gen. Psychiatry 1988;45:225-31)
Because bipolar disorder is an unpredictable, potentially destructive illness, it is important to grab any factors that we and our patients might have control over and do our best to modify them positively. With this in mind, the Family Focused Treatment (FFT) model was developed, with the philosophy that by keeping patients well informed about the facts and realities of the disorder and working on the communication and coping mechanisms operating within the family, relapse prevention and emotional stability will be better maintained. In this way, the predictive factors of stressful life events, poor social support, and family-expressed emotion can be modified. FFT is a time limited (usually 12 sessions), highly effective treatment modality.
The principles of FFT were adapted into an ongoing-treatment model that can be implemented in a community setting, termed Family Inclusive Treatment (FIT) and used by the Family Center for Bipolar in New York City, for example. FIT consists of an engagement period at the initiation of treatment, focused on psychoeducation and relapse prevention planning. FIT is unique in that every patient is required to sign a release of information giving permission for full, open communication at all times between the patient’s clinician and a treatment partner of their choosing.
After the initial engagement period, there are quarterly family visits to supplement regular individual treatment. Other modalities such as individual therapy, pharmacotherapy, and group therapy are used according to the clinician’s judgment.
This form of treatment is innovative in that it treats bipolar illness just like any other chronic illness. It promotes open communication between families of patients with bipolar disorder and the patients themselves with regard to symptoms and medications. In this way patients are not isolated from their families; they can talk openly with one another and their clinician as they would do if somebody in the family had Alzheimer’s disease or diabetes.
It has been reported that up to 46% of the caregivers of patients with bipolar disorder report depression, and up to 32.4% report use of mental health services. These symptoms tend to be dependent on the nature of the caregiving relationship, suggesting that specialized interventions addressing the psychiatric needs of bipolar families might result in improved outcomes for both patients and their family members, in addition to decreases in health care costs (J. Affect. Disord. 2010;121:10-21).
Together with therapy and medication management, clinicians working in the FIT model strive to create an environment that minimizes, as much as possible, the impact of bipolar disorder on the affected individuals and their close loved ones.
Many studies have confirmed the efficacy of various psychosocial treatments for bipolar disorder (J. Consult. Clin. Psychol. 2003;7:482-92; J. Clin. Psychiatry 2006;67 [suppl. 11]:28-33; J. Affect. Disord. 2007;98:11-27), and there has been a push for the integration of psychosocial treatment with pharmacotherapy, as the latter is less often sufficient on its own in preventing relapse.
Patient, family begin journey
Kevin and his family entered into family treatment. They started off with the psychoeducation portion of the treatment, and many of the myths and misinformation that they had held about bipolar disorder were dispelled. Even Kevin was able to engage in the information exchange, which he initially approached from an academic, impersonal vantage point. The communication skills phase proved more problematic as it became more personal, but still, the focus was on the family’s communication and not on Kevin as a psychiatric patient, so he responded well.
It was uncovered that Kevin’s father has always been highly critical, and Kevin’s mother tends to overprotect her children to compensate. They were taught new skills to express their feelings toward one another, and especially toward Kevin, in more productive and positive ways. In addition, they got a chance to practice those skills in subsequent sessions.
The modules continued in this vein until the family portion of treatment had completed. By this time, Kevin had developed a good rapport with his clinician, and he continued treatment despite his persistent reservations about accepting his illness. The family environment improved, and though Kevin was only sporadically compliant with his medication, the reduced stress at home and improved coping skills drove him less often to use marijuana for "self-medication," which decreased his manic episodes.
Kevin’s family periodically rejoined him in treatment sessions at predefined intervals, to check in and assess his and their progress. They were comfortable speaking with Kevin’s doctor and would call when they noticed any of the warning signs that they had collaboratively determined as markers of upcoming mania. In this way, they were all effective at keeping Kevin’s moods stable and keeping him out of the hospital.
The psychiatrist in routine practice might neither follow a manualized algorithm for family treatment nor have the time or resources at her disposal to provide a full "curriculum." Still, she can have the same success in engaging a family in understanding their loved one’s illness and contributing to the family member’s stability.
Objectives for family-focused treatment
The following objectives are adapted from "Bipolar Disorder: A Family-Focused Treatment Approach," 2nd ed. (New York: The Guilford Press, 2010):
• Encourage the patient and the family to admit that there is a vulnerability to future episodes by educating them about the natural course, progression, and chronic nature of bipolar disorder.
• Enable the patient and the family to recognize that medications are important for controlling symptoms. Provide concrete evidence for the importance and efficacy of medications and the risks of discontinuation. Explore reasons for resisting medications, including fears about becoming dependent.
• Help the patient and the family see the differences between the patient’s personality and his/her illness. Make a list of the patient’s positive attributes and a separate list of warning signs of mania. Frequently reinforce the distinction between the two.
• Assist the patient and the family in dealing with stressors that might cause a recurrence and help them rebuild family relationship ruptures after an episode. Suggest methods for positive, constructive communication such as active listening (nodding, making eye contact, paraphrasing, asking relevant questions) and expressing positive feelings toward a family member related to a specific example of a behavior.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013). Dr. Mednick is an attending psychiatrist at the Family Center for Bipolar at Beth Israel Medical Center in New York City.
Kevin was doing very well in law school, until he showed up at his professor’s house in the middle of the night. Normally a thoughtful, quiet, introverted young man, Kevin was hardly recognizable to his professor, who found him outside yelling loudly and demanding to speak about an underground conspiracy he believed he had uncovered. He had always been a good student, and his family was very proud of his accomplishments up until now. At the age of 24, Kevin’s first manic episode was triggered by late nights studying for his law school exams and marijuana use to cope with stress.
Police responded to noise complaints, and Kevin was hospitalized. The manic episode resolved surprisingly quickly in the absence of marijuana use and with the help of an atypical antipsychotic. The patient’s intelligence and articulate lawyer-in-training charm made his inpatient doctors hard pressed to justify an extended hospital stay, and he was discharged 3 days later with a prescription and instructions for follow-up. He promptly discarded both.
When his next manic episode arose, Kevin disappeared for 2 weeks, and after fearing the worst, Kevin’s family was relieved to receive a call from Kevin’s aunt, who lived across the country and had just found him at her doorstep. This time, without the involvement of law enforcement, there seemed to be no way for Kevin’s mother, father, older sister, and aunt to persuade Kevin to enter the hospital or to take medications. Kevin’s aunt accompanied him on a plane home, and in the face of Kevin’s unwillingness to enter treatment alone, they decided to enter treatment as a family.
Predictors of episodes
The strongest predictors of future episodes and poor outcome in patients with bipolar disorder are a greater number of previous episodes, shorter intervals between episodes, a history of psychosis, a history of anxiety, persistence of affective symptoms and episodes, and stressful life events. Some evidence has suggested that poor job functioning, lack of social support, increased expressed emotion in the family, and introverted or obsessional personality traits all might predict poor outcome in bipolar disorder (J. Psychiatr. Pract. 2006;12:269-82).
An overwhelmingly emotional home environment can make a large contribution to relapse. Multiple studies have shown that a high level of "expressed emotion" (characterized by overinvolvement and excessive criticism) predicts patient relapse independent of medication compliance, baseline symptoms, and demographics (Arch. Gen. Psychiatry 1988;45:225-31)
Because bipolar disorder is an unpredictable, potentially destructive illness, it is important to grab any factors that we and our patients might have control over and do our best to modify them positively. With this in mind, the Family Focused Treatment (FFT) model was developed, with the philosophy that by keeping patients well informed about the facts and realities of the disorder and working on the communication and coping mechanisms operating within the family, relapse prevention and emotional stability will be better maintained. In this way, the predictive factors of stressful life events, poor social support, and family-expressed emotion can be modified. FFT is a time limited (usually 12 sessions), highly effective treatment modality.
The principles of FFT were adapted into an ongoing-treatment model that can be implemented in a community setting, termed Family Inclusive Treatment (FIT) and used by the Family Center for Bipolar in New York City, for example. FIT consists of an engagement period at the initiation of treatment, focused on psychoeducation and relapse prevention planning. FIT is unique in that every patient is required to sign a release of information giving permission for full, open communication at all times between the patient’s clinician and a treatment partner of their choosing.
After the initial engagement period, there are quarterly family visits to supplement regular individual treatment. Other modalities such as individual therapy, pharmacotherapy, and group therapy are used according to the clinician’s judgment.
This form of treatment is innovative in that it treats bipolar illness just like any other chronic illness. It promotes open communication between families of patients with bipolar disorder and the patients themselves with regard to symptoms and medications. In this way patients are not isolated from their families; they can talk openly with one another and their clinician as they would do if somebody in the family had Alzheimer’s disease or diabetes.
It has been reported that up to 46% of the caregivers of patients with bipolar disorder report depression, and up to 32.4% report use of mental health services. These symptoms tend to be dependent on the nature of the caregiving relationship, suggesting that specialized interventions addressing the psychiatric needs of bipolar families might result in improved outcomes for both patients and their family members, in addition to decreases in health care costs (J. Affect. Disord. 2010;121:10-21).
Together with therapy and medication management, clinicians working in the FIT model strive to create an environment that minimizes, as much as possible, the impact of bipolar disorder on the affected individuals and their close loved ones.
Many studies have confirmed the efficacy of various psychosocial treatments for bipolar disorder (J. Consult. Clin. Psychol. 2003;7:482-92; J. Clin. Psychiatry 2006;67 [suppl. 11]:28-33; J. Affect. Disord. 2007;98:11-27), and there has been a push for the integration of psychosocial treatment with pharmacotherapy, as the latter is less often sufficient on its own in preventing relapse.
Patient, family begin journey
Kevin and his family entered into family treatment. They started off with the psychoeducation portion of the treatment, and many of the myths and misinformation that they had held about bipolar disorder were dispelled. Even Kevin was able to engage in the information exchange, which he initially approached from an academic, impersonal vantage point. The communication skills phase proved more problematic as it became more personal, but still, the focus was on the family’s communication and not on Kevin as a psychiatric patient, so he responded well.
It was uncovered that Kevin’s father has always been highly critical, and Kevin’s mother tends to overprotect her children to compensate. They were taught new skills to express their feelings toward one another, and especially toward Kevin, in more productive and positive ways. In addition, they got a chance to practice those skills in subsequent sessions.
The modules continued in this vein until the family portion of treatment had completed. By this time, Kevin had developed a good rapport with his clinician, and he continued treatment despite his persistent reservations about accepting his illness. The family environment improved, and though Kevin was only sporadically compliant with his medication, the reduced stress at home and improved coping skills drove him less often to use marijuana for "self-medication," which decreased his manic episodes.
Kevin’s family periodically rejoined him in treatment sessions at predefined intervals, to check in and assess his and their progress. They were comfortable speaking with Kevin’s doctor and would call when they noticed any of the warning signs that they had collaboratively determined as markers of upcoming mania. In this way, they were all effective at keeping Kevin’s moods stable and keeping him out of the hospital.
The psychiatrist in routine practice might neither follow a manualized algorithm for family treatment nor have the time or resources at her disposal to provide a full "curriculum." Still, she can have the same success in engaging a family in understanding their loved one’s illness and contributing to the family member’s stability.
Objectives for family-focused treatment
The following objectives are adapted from "Bipolar Disorder: A Family-Focused Treatment Approach," 2nd ed. (New York: The Guilford Press, 2010):
• Encourage the patient and the family to admit that there is a vulnerability to future episodes by educating them about the natural course, progression, and chronic nature of bipolar disorder.
• Enable the patient and the family to recognize that medications are important for controlling symptoms. Provide concrete evidence for the importance and efficacy of medications and the risks of discontinuation. Explore reasons for resisting medications, including fears about becoming dependent.
• Help the patient and the family see the differences between the patient’s personality and his/her illness. Make a list of the patient’s positive attributes and a separate list of warning signs of mania. Frequently reinforce the distinction between the two.
• Assist the patient and the family in dealing with stressors that might cause a recurrence and help them rebuild family relationship ruptures after an episode. Suggest methods for positive, constructive communication such as active listening (nodding, making eye contact, paraphrasing, asking relevant questions) and expressing positive feelings toward a family member related to a specific example of a behavior.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013). Dr. Mednick is an attending psychiatrist at the Family Center for Bipolar at Beth Israel Medical Center in New York City.
Kevin was doing very well in law school, until he showed up at his professor’s house in the middle of the night. Normally a thoughtful, quiet, introverted young man, Kevin was hardly recognizable to his professor, who found him outside yelling loudly and demanding to speak about an underground conspiracy he believed he had uncovered. He had always been a good student, and his family was very proud of his accomplishments up until now. At the age of 24, Kevin’s first manic episode was triggered by late nights studying for his law school exams and marijuana use to cope with stress.
Police responded to noise complaints, and Kevin was hospitalized. The manic episode resolved surprisingly quickly in the absence of marijuana use and with the help of an atypical antipsychotic. The patient’s intelligence and articulate lawyer-in-training charm made his inpatient doctors hard pressed to justify an extended hospital stay, and he was discharged 3 days later with a prescription and instructions for follow-up. He promptly discarded both.
When his next manic episode arose, Kevin disappeared for 2 weeks, and after fearing the worst, Kevin’s family was relieved to receive a call from Kevin’s aunt, who lived across the country and had just found him at her doorstep. This time, without the involvement of law enforcement, there seemed to be no way for Kevin’s mother, father, older sister, and aunt to persuade Kevin to enter the hospital or to take medications. Kevin’s aunt accompanied him on a plane home, and in the face of Kevin’s unwillingness to enter treatment alone, they decided to enter treatment as a family.
Predictors of episodes
The strongest predictors of future episodes and poor outcome in patients with bipolar disorder are a greater number of previous episodes, shorter intervals between episodes, a history of psychosis, a history of anxiety, persistence of affective symptoms and episodes, and stressful life events. Some evidence has suggested that poor job functioning, lack of social support, increased expressed emotion in the family, and introverted or obsessional personality traits all might predict poor outcome in bipolar disorder (J. Psychiatr. Pract. 2006;12:269-82).
An overwhelmingly emotional home environment can make a large contribution to relapse. Multiple studies have shown that a high level of "expressed emotion" (characterized by overinvolvement and excessive criticism) predicts patient relapse independent of medication compliance, baseline symptoms, and demographics (Arch. Gen. Psychiatry 1988;45:225-31)
Because bipolar disorder is an unpredictable, potentially destructive illness, it is important to grab any factors that we and our patients might have control over and do our best to modify them positively. With this in mind, the Family Focused Treatment (FFT) model was developed, with the philosophy that by keeping patients well informed about the facts and realities of the disorder and working on the communication and coping mechanisms operating within the family, relapse prevention and emotional stability will be better maintained. In this way, the predictive factors of stressful life events, poor social support, and family-expressed emotion can be modified. FFT is a time limited (usually 12 sessions), highly effective treatment modality.
The principles of FFT were adapted into an ongoing-treatment model that can be implemented in a community setting, termed Family Inclusive Treatment (FIT) and used by the Family Center for Bipolar in New York City, for example. FIT consists of an engagement period at the initiation of treatment, focused on psychoeducation and relapse prevention planning. FIT is unique in that every patient is required to sign a release of information giving permission for full, open communication at all times between the patient’s clinician and a treatment partner of their choosing.
After the initial engagement period, there are quarterly family visits to supplement regular individual treatment. Other modalities such as individual therapy, pharmacotherapy, and group therapy are used according to the clinician’s judgment.
This form of treatment is innovative in that it treats bipolar illness just like any other chronic illness. It promotes open communication between families of patients with bipolar disorder and the patients themselves with regard to symptoms and medications. In this way patients are not isolated from their families; they can talk openly with one another and their clinician as they would do if somebody in the family had Alzheimer’s disease or diabetes.
It has been reported that up to 46% of the caregivers of patients with bipolar disorder report depression, and up to 32.4% report use of mental health services. These symptoms tend to be dependent on the nature of the caregiving relationship, suggesting that specialized interventions addressing the psychiatric needs of bipolar families might result in improved outcomes for both patients and their family members, in addition to decreases in health care costs (J. Affect. Disord. 2010;121:10-21).
Together with therapy and medication management, clinicians working in the FIT model strive to create an environment that minimizes, as much as possible, the impact of bipolar disorder on the affected individuals and their close loved ones.
Many studies have confirmed the efficacy of various psychosocial treatments for bipolar disorder (J. Consult. Clin. Psychol. 2003;7:482-92; J. Clin. Psychiatry 2006;67 [suppl. 11]:28-33; J. Affect. Disord. 2007;98:11-27), and there has been a push for the integration of psychosocial treatment with pharmacotherapy, as the latter is less often sufficient on its own in preventing relapse.
Patient, family begin journey
Kevin and his family entered into family treatment. They started off with the psychoeducation portion of the treatment, and many of the myths and misinformation that they had held about bipolar disorder were dispelled. Even Kevin was able to engage in the information exchange, which he initially approached from an academic, impersonal vantage point. The communication skills phase proved more problematic as it became more personal, but still, the focus was on the family’s communication and not on Kevin as a psychiatric patient, so he responded well.
It was uncovered that Kevin’s father has always been highly critical, and Kevin’s mother tends to overprotect her children to compensate. They were taught new skills to express their feelings toward one another, and especially toward Kevin, in more productive and positive ways. In addition, they got a chance to practice those skills in subsequent sessions.
The modules continued in this vein until the family portion of treatment had completed. By this time, Kevin had developed a good rapport with his clinician, and he continued treatment despite his persistent reservations about accepting his illness. The family environment improved, and though Kevin was only sporadically compliant with his medication, the reduced stress at home and improved coping skills drove him less often to use marijuana for "self-medication," which decreased his manic episodes.
Kevin’s family periodically rejoined him in treatment sessions at predefined intervals, to check in and assess his and their progress. They were comfortable speaking with Kevin’s doctor and would call when they noticed any of the warning signs that they had collaboratively determined as markers of upcoming mania. In this way, they were all effective at keeping Kevin’s moods stable and keeping him out of the hospital.
The psychiatrist in routine practice might neither follow a manualized algorithm for family treatment nor have the time or resources at her disposal to provide a full "curriculum." Still, she can have the same success in engaging a family in understanding their loved one’s illness and contributing to the family member’s stability.
Objectives for family-focused treatment
The following objectives are adapted from "Bipolar Disorder: A Family-Focused Treatment Approach," 2nd ed. (New York: The Guilford Press, 2010):
• Encourage the patient and the family to admit that there is a vulnerability to future episodes by educating them about the natural course, progression, and chronic nature of bipolar disorder.
• Enable the patient and the family to recognize that medications are important for controlling symptoms. Provide concrete evidence for the importance and efficacy of medications and the risks of discontinuation. Explore reasons for resisting medications, including fears about becoming dependent.
• Help the patient and the family see the differences between the patient’s personality and his/her illness. Make a list of the patient’s positive attributes and a separate list of warning signs of mania. Frequently reinforce the distinction between the two.
• Assist the patient and the family in dealing with stressors that might cause a recurrence and help them rebuild family relationship ruptures after an episode. Suggest methods for positive, constructive communication such as active listening (nodding, making eye contact, paraphrasing, asking relevant questions) and expressing positive feelings toward a family member related to a specific example of a behavior.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013). Dr. Mednick is an attending psychiatrist at the Family Center for Bipolar at Beth Israel Medical Center in New York City.
Tailored therapy needed to conquer IPV
Conducting effective family therapy is never a one-size-fits-all proposition. In our work with families, we must keep in mind that, just as the dynamics in each family are different, so, too, must be our approaches. This is particularly the case for people who are experiencing intimate partner violence, or IPV.
The cases of three patients described below illustrate that point well; I’ve changed the patients’ names to protect their anonymity.
Belkis
She is a hardworking immigrant making minimum wage as a housekeeper. She presents to her psychiatric outpatient appointment with complaints of being sad and anxious. When asked about her husband and their relationship, she says tentatively that they disagree about things. She doesn’t acknowledge any abuse until she is asked directly, then she hangs her head down and looks ashamed. "He tells me I am not a good wife." With encouragement, she admits that she would like to leave him but has nowhere to go and is afraid that he will really hurt her if she tries to leave. "I tried before, and he threatened to kill me if I tried again."
Melanie
She is a well-educated women working as a writer and has a good income. She presents to her psychiatric outpatient appointment with complaints of being sad and anxious. When asked about her husband and their relationship, she says that he is abusive to her. She states that she would like to come into therapy to figure out why she has not been able to leave him. "What ties me to him?" She says her friends tell her she should leave. "There must be a reason I stay; can you help me figure it out? I cannot move to another relationship without understanding what is going on in this one."
Zelda
She is a successful saleswoman and comes into the office with the complaint that she and her husband are having problems. On direct questioning, she affirms that that two do engage in direct fighting that gets physical at times. She says she often initiates the violence. She wants to stay with her husband and says they both want to make a go of things. They want to come into couples therapy and work on improving their relationship. But they fear that if they do go to a therapist together, as soon as she says there is violence in their relationship, she will be refused treatment.
Different cases, different approaches
Belkis benefits from treatment that focuses on support, education about domestic violence, and help with developing a safety plan. She wants to leave but needs the help and structure to do so.
Melanie enters individual therapy, and comes to understand that in her relationship with her husband, she is reenacting the relationship she had as a child with her parents. As a child, she felt like she was there only to help her mother clean and care for her sibling and that her needs and desires did not matter.
She felt that her elder brother was the favorite and that she had to support him as he pursued his studies. In her current relationship, she strives to "matter as a person" and not be seen as someone to do the cooking and the chores. She speaks back to her husband and challenges him when he demeans her. When she understands that the dynamic that binds her to her husband is the same dynamic that she experienced growing up, she feels relieved. "Now I can begin to think about taking care of myself and setting my own goals for my life. Now I can leave my past behind," she said.
Zelda and her husband want couples therapy. Both are committed to the relationship and stopping the violence as well as learning how to solve problems, communicate better, and meet each other’s needs by asking and negotiating. Before entering couples therapy, they agree to stop any violence while in treatment. The therapist teaches them skills to "take a time out" when conflict arises. As I’ve written previously, if patients are unable to discuss the issue calmly, they bring it to therapy (Adv. Psychiatric Treat. 2007;13:376-83).
How common is IPV?
Violence against women was not viewed as a serious issue until the second wave of feminism increased awareness, pushed for legislation, and increased resources.
How should we understand IPV? This phenomenon is often bidirectional, where each partner is both an aggressor and a victim, although women remain much more likely to be injured by partner violence than are men (Am. J. Public Health 2007;97:941-7).
In an outpatient sample of couples seeking marital therapy, 64% of wives and 61% of husbands were classified as aggressive (Violence Vict. 1994;9:107-24). In 272 engaged couples, 44% of women and 31% of men reported physical violence toward their partners (J. Consult. Clin. Psychol. 1989;57:263-8). As illustrated by the three cases above, IPV occurs across a range, from the classic male perpetrator and female victim, to the couple that engages in mutual violence.
Why do women stay?
Researchers such as Virginia Goldner, Ph.D., of the Ackerman Institute for the Family in New York, have contributed significantly to the understanding of why women stay in violent relationships. Dr. Goldner describes a generational imperative that is passed from mothers to daughters (Fam. Process 1990;29:343-64). This often includes the view that the role of women is to preserve the family, regardless of either the personal cost or the presence of abuse or violence.
Daughters raised in a highly patriarchal family might suffer existential neglect and be undervalued except in their capacity as caregiver to others in the family. Therefore, staying in a relationship protects the woman against guilt that she might feel if she gives up her caretaking role. These daughters may grow up with the belief that "being loved" is contingent upon denial of their self, being selfless. They may see the opposite as "being selfish" and not compatible with their self-image. Melanie certainly identified this guilt and had difficulty thinking about meeting her own needs.
Asking women about their mothers and the internalized view of themselves as independent agents can expose this dilemma. These daughters may see their mothers as powerless, devalued, and depressed. Being loyal to their mothers means accepting a subjugated role, while allying with their fathers means betraying their mothers and their own sense of themselves, as a woman.
If you decide to take a couple into therapy, it is important to interview each member of the couple individually before starting couples therapy. The information you glean from these interviews also will help determine when to offer and when not to offer couples therapy.
Factors that should encourage you not to proceed with couples therapy include the uncontrolled, continuous use of alcohol or drugs; fear of serious injury from the patient’s partner; severe violence that has resulted in the victim requiring medical attention; conviction for a violent crime or violation of a restraining order; prior use of a weapon against the partner; prior threat to kill the partner; stalking or other partner-focused obsessional behavior; and bizarre forms of violence, such as sadistic violence.
Here are a few guidelines for assessing intimate partner violence:
• Ask about relationship violence. Consider use of a questionnaire.
• If present, determine severity and ask about fear of partner.
• Identify risk factors for the potentially lethal relationship.
• If substance misuse is present, recommend abstinence and refer for treatment.
• If the couple wishes to stay together and to resolve the intimate partner violence, refer for conjoint treatment with a specialized family therapist.
• Assess and treat common comorbidities such as major depressive disorder and post-traumatic stress disorder.
Belkis, Melanie, and Zelda are three different women in abusive relationships who require three different solutions. Each patient requires a treatment based on their unique history and goals. Make sure that you are a family psychiatrist who understands the differences between your patients – and that you are able to provide a solution tailored to teach patient’s needs.
Elements of a safety plan
Encourage patients who in the midst of intimate partner violence to take the following steps to keep them and their families safe:
• Memorize phone numbers of people to call in emergency.
• Teach older children important phone numbers and when to dial 911.
• Keep information about domestic violence shelters in a safe place where you can get it quickly when you need it.
• Buy a cell phone that the abuser does not know about.
• Try to open your own bank account.
• Stay in touch with friends and neighbors. Do not cut yourself off from people.
• Rehearse your escape plan until you know it by heart.
• Leave a set of car keys, extra money, a change of clothes, and copies of important documents with a trusted friend or relative.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Conducting effective family therapy is never a one-size-fits-all proposition. In our work with families, we must keep in mind that, just as the dynamics in each family are different, so, too, must be our approaches. This is particularly the case for people who are experiencing intimate partner violence, or IPV.
The cases of three patients described below illustrate that point well; I’ve changed the patients’ names to protect their anonymity.
Belkis
She is a hardworking immigrant making minimum wage as a housekeeper. She presents to her psychiatric outpatient appointment with complaints of being sad and anxious. When asked about her husband and their relationship, she says tentatively that they disagree about things. She doesn’t acknowledge any abuse until she is asked directly, then she hangs her head down and looks ashamed. "He tells me I am not a good wife." With encouragement, she admits that she would like to leave him but has nowhere to go and is afraid that he will really hurt her if she tries to leave. "I tried before, and he threatened to kill me if I tried again."
Melanie
She is a well-educated women working as a writer and has a good income. She presents to her psychiatric outpatient appointment with complaints of being sad and anxious. When asked about her husband and their relationship, she says that he is abusive to her. She states that she would like to come into therapy to figure out why she has not been able to leave him. "What ties me to him?" She says her friends tell her she should leave. "There must be a reason I stay; can you help me figure it out? I cannot move to another relationship without understanding what is going on in this one."
Zelda
She is a successful saleswoman and comes into the office with the complaint that she and her husband are having problems. On direct questioning, she affirms that that two do engage in direct fighting that gets physical at times. She says she often initiates the violence. She wants to stay with her husband and says they both want to make a go of things. They want to come into couples therapy and work on improving their relationship. But they fear that if they do go to a therapist together, as soon as she says there is violence in their relationship, she will be refused treatment.
Different cases, different approaches
Belkis benefits from treatment that focuses on support, education about domestic violence, and help with developing a safety plan. She wants to leave but needs the help and structure to do so.
Melanie enters individual therapy, and comes to understand that in her relationship with her husband, she is reenacting the relationship she had as a child with her parents. As a child, she felt like she was there only to help her mother clean and care for her sibling and that her needs and desires did not matter.
She felt that her elder brother was the favorite and that she had to support him as he pursued his studies. In her current relationship, she strives to "matter as a person" and not be seen as someone to do the cooking and the chores. She speaks back to her husband and challenges him when he demeans her. When she understands that the dynamic that binds her to her husband is the same dynamic that she experienced growing up, she feels relieved. "Now I can begin to think about taking care of myself and setting my own goals for my life. Now I can leave my past behind," she said.
Zelda and her husband want couples therapy. Both are committed to the relationship and stopping the violence as well as learning how to solve problems, communicate better, and meet each other’s needs by asking and negotiating. Before entering couples therapy, they agree to stop any violence while in treatment. The therapist teaches them skills to "take a time out" when conflict arises. As I’ve written previously, if patients are unable to discuss the issue calmly, they bring it to therapy (Adv. Psychiatric Treat. 2007;13:376-83).
How common is IPV?
Violence against women was not viewed as a serious issue until the second wave of feminism increased awareness, pushed for legislation, and increased resources.
How should we understand IPV? This phenomenon is often bidirectional, where each partner is both an aggressor and a victim, although women remain much more likely to be injured by partner violence than are men (Am. J. Public Health 2007;97:941-7).
In an outpatient sample of couples seeking marital therapy, 64% of wives and 61% of husbands were classified as aggressive (Violence Vict. 1994;9:107-24). In 272 engaged couples, 44% of women and 31% of men reported physical violence toward their partners (J. Consult. Clin. Psychol. 1989;57:263-8). As illustrated by the three cases above, IPV occurs across a range, from the classic male perpetrator and female victim, to the couple that engages in mutual violence.
Why do women stay?
Researchers such as Virginia Goldner, Ph.D., of the Ackerman Institute for the Family in New York, have contributed significantly to the understanding of why women stay in violent relationships. Dr. Goldner describes a generational imperative that is passed from mothers to daughters (Fam. Process 1990;29:343-64). This often includes the view that the role of women is to preserve the family, regardless of either the personal cost or the presence of abuse or violence.
Daughters raised in a highly patriarchal family might suffer existential neglect and be undervalued except in their capacity as caregiver to others in the family. Therefore, staying in a relationship protects the woman against guilt that she might feel if she gives up her caretaking role. These daughters may grow up with the belief that "being loved" is contingent upon denial of their self, being selfless. They may see the opposite as "being selfish" and not compatible with their self-image. Melanie certainly identified this guilt and had difficulty thinking about meeting her own needs.
Asking women about their mothers and the internalized view of themselves as independent agents can expose this dilemma. These daughters may see their mothers as powerless, devalued, and depressed. Being loyal to their mothers means accepting a subjugated role, while allying with their fathers means betraying their mothers and their own sense of themselves, as a woman.
If you decide to take a couple into therapy, it is important to interview each member of the couple individually before starting couples therapy. The information you glean from these interviews also will help determine when to offer and when not to offer couples therapy.
Factors that should encourage you not to proceed with couples therapy include the uncontrolled, continuous use of alcohol or drugs; fear of serious injury from the patient’s partner; severe violence that has resulted in the victim requiring medical attention; conviction for a violent crime or violation of a restraining order; prior use of a weapon against the partner; prior threat to kill the partner; stalking or other partner-focused obsessional behavior; and bizarre forms of violence, such as sadistic violence.
Here are a few guidelines for assessing intimate partner violence:
• Ask about relationship violence. Consider use of a questionnaire.
• If present, determine severity and ask about fear of partner.
• Identify risk factors for the potentially lethal relationship.
• If substance misuse is present, recommend abstinence and refer for treatment.
• If the couple wishes to stay together and to resolve the intimate partner violence, refer for conjoint treatment with a specialized family therapist.
• Assess and treat common comorbidities such as major depressive disorder and post-traumatic stress disorder.
Belkis, Melanie, and Zelda are three different women in abusive relationships who require three different solutions. Each patient requires a treatment based on their unique history and goals. Make sure that you are a family psychiatrist who understands the differences between your patients – and that you are able to provide a solution tailored to teach patient’s needs.
Elements of a safety plan
Encourage patients who in the midst of intimate partner violence to take the following steps to keep them and their families safe:
• Memorize phone numbers of people to call in emergency.
• Teach older children important phone numbers and when to dial 911.
• Keep information about domestic violence shelters in a safe place where you can get it quickly when you need it.
• Buy a cell phone that the abuser does not know about.
• Try to open your own bank account.
• Stay in touch with friends and neighbors. Do not cut yourself off from people.
• Rehearse your escape plan until you know it by heart.
• Leave a set of car keys, extra money, a change of clothes, and copies of important documents with a trusted friend or relative.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Conducting effective family therapy is never a one-size-fits-all proposition. In our work with families, we must keep in mind that, just as the dynamics in each family are different, so, too, must be our approaches. This is particularly the case for people who are experiencing intimate partner violence, or IPV.
The cases of three patients described below illustrate that point well; I’ve changed the patients’ names to protect their anonymity.
Belkis
She is a hardworking immigrant making minimum wage as a housekeeper. She presents to her psychiatric outpatient appointment with complaints of being sad and anxious. When asked about her husband and their relationship, she says tentatively that they disagree about things. She doesn’t acknowledge any abuse until she is asked directly, then she hangs her head down and looks ashamed. "He tells me I am not a good wife." With encouragement, she admits that she would like to leave him but has nowhere to go and is afraid that he will really hurt her if she tries to leave. "I tried before, and he threatened to kill me if I tried again."
Melanie
She is a well-educated women working as a writer and has a good income. She presents to her psychiatric outpatient appointment with complaints of being sad and anxious. When asked about her husband and their relationship, she says that he is abusive to her. She states that she would like to come into therapy to figure out why she has not been able to leave him. "What ties me to him?" She says her friends tell her she should leave. "There must be a reason I stay; can you help me figure it out? I cannot move to another relationship without understanding what is going on in this one."
Zelda
She is a successful saleswoman and comes into the office with the complaint that she and her husband are having problems. On direct questioning, she affirms that that two do engage in direct fighting that gets physical at times. She says she often initiates the violence. She wants to stay with her husband and says they both want to make a go of things. They want to come into couples therapy and work on improving their relationship. But they fear that if they do go to a therapist together, as soon as she says there is violence in their relationship, she will be refused treatment.
Different cases, different approaches
Belkis benefits from treatment that focuses on support, education about domestic violence, and help with developing a safety plan. She wants to leave but needs the help and structure to do so.
Melanie enters individual therapy, and comes to understand that in her relationship with her husband, she is reenacting the relationship she had as a child with her parents. As a child, she felt like she was there only to help her mother clean and care for her sibling and that her needs and desires did not matter.
She felt that her elder brother was the favorite and that she had to support him as he pursued his studies. In her current relationship, she strives to "matter as a person" and not be seen as someone to do the cooking and the chores. She speaks back to her husband and challenges him when he demeans her. When she understands that the dynamic that binds her to her husband is the same dynamic that she experienced growing up, she feels relieved. "Now I can begin to think about taking care of myself and setting my own goals for my life. Now I can leave my past behind," she said.
Zelda and her husband want couples therapy. Both are committed to the relationship and stopping the violence as well as learning how to solve problems, communicate better, and meet each other’s needs by asking and negotiating. Before entering couples therapy, they agree to stop any violence while in treatment. The therapist teaches them skills to "take a time out" when conflict arises. As I’ve written previously, if patients are unable to discuss the issue calmly, they bring it to therapy (Adv. Psychiatric Treat. 2007;13:376-83).
How common is IPV?
Violence against women was not viewed as a serious issue until the second wave of feminism increased awareness, pushed for legislation, and increased resources.
How should we understand IPV? This phenomenon is often bidirectional, where each partner is both an aggressor and a victim, although women remain much more likely to be injured by partner violence than are men (Am. J. Public Health 2007;97:941-7).
In an outpatient sample of couples seeking marital therapy, 64% of wives and 61% of husbands were classified as aggressive (Violence Vict. 1994;9:107-24). In 272 engaged couples, 44% of women and 31% of men reported physical violence toward their partners (J. Consult. Clin. Psychol. 1989;57:263-8). As illustrated by the three cases above, IPV occurs across a range, from the classic male perpetrator and female victim, to the couple that engages in mutual violence.
Why do women stay?
Researchers such as Virginia Goldner, Ph.D., of the Ackerman Institute for the Family in New York, have contributed significantly to the understanding of why women stay in violent relationships. Dr. Goldner describes a generational imperative that is passed from mothers to daughters (Fam. Process 1990;29:343-64). This often includes the view that the role of women is to preserve the family, regardless of either the personal cost or the presence of abuse or violence.
Daughters raised in a highly patriarchal family might suffer existential neglect and be undervalued except in their capacity as caregiver to others in the family. Therefore, staying in a relationship protects the woman against guilt that she might feel if she gives up her caretaking role. These daughters may grow up with the belief that "being loved" is contingent upon denial of their self, being selfless. They may see the opposite as "being selfish" and not compatible with their self-image. Melanie certainly identified this guilt and had difficulty thinking about meeting her own needs.
Asking women about their mothers and the internalized view of themselves as independent agents can expose this dilemma. These daughters may see their mothers as powerless, devalued, and depressed. Being loyal to their mothers means accepting a subjugated role, while allying with their fathers means betraying their mothers and their own sense of themselves, as a woman.
If you decide to take a couple into therapy, it is important to interview each member of the couple individually before starting couples therapy. The information you glean from these interviews also will help determine when to offer and when not to offer couples therapy.
Factors that should encourage you not to proceed with couples therapy include the uncontrolled, continuous use of alcohol or drugs; fear of serious injury from the patient’s partner; severe violence that has resulted in the victim requiring medical attention; conviction for a violent crime or violation of a restraining order; prior use of a weapon against the partner; prior threat to kill the partner; stalking or other partner-focused obsessional behavior; and bizarre forms of violence, such as sadistic violence.
Here are a few guidelines for assessing intimate partner violence:
• Ask about relationship violence. Consider use of a questionnaire.
• If present, determine severity and ask about fear of partner.
• Identify risk factors for the potentially lethal relationship.
• If substance misuse is present, recommend abstinence and refer for treatment.
• If the couple wishes to stay together and to resolve the intimate partner violence, refer for conjoint treatment with a specialized family therapist.
• Assess and treat common comorbidities such as major depressive disorder and post-traumatic stress disorder.
Belkis, Melanie, and Zelda are three different women in abusive relationships who require three different solutions. Each patient requires a treatment based on their unique history and goals. Make sure that you are a family psychiatrist who understands the differences between your patients – and that you are able to provide a solution tailored to teach patient’s needs.
Elements of a safety plan
Encourage patients who in the midst of intimate partner violence to take the following steps to keep them and their families safe:
• Memorize phone numbers of people to call in emergency.
• Teach older children important phone numbers and when to dial 911.
• Keep information about domestic violence shelters in a safe place where you can get it quickly when you need it.
• Buy a cell phone that the abuser does not know about.
• Try to open your own bank account.
• Stay in touch with friends and neighbors. Do not cut yourself off from people.
• Rehearse your escape plan until you know it by heart.
• Leave a set of car keys, extra money, a change of clothes, and copies of important documents with a trusted friend or relative.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Family narratives and the intergenerational transmission of resilience
Carmen Bugan read her poems to her family. Her father had been imprisoned by Securitate, the Romanian secret police, for anticommunist rhetoric that he distributed on leaflets to people’s mailboxes. Securitate tracked him down by examining the leaflets for identifying typescript that they linked to one of his typewriters. He buried his other typewriter in the garden to escape detection. He would dig it up when he wanted to write serious anticommunist literature, then rebury it again in the garden.
"It is not important that the poem stays or goes," Carmen writes. "I discover a way to relieve our family’s suffering even though when I read the poems to Mom and my sister it seems that I create more pain at first.
"Mom loves the words, loves explanations of feelings to negotiate pain, and I can provide this for her. My sister says her feelings are exteriorized, articulated by the emotions in the poem and I can help bring things out" ("Burying the Typewriter," Minneapolis: Graywolf Press, 2012, p. 124).
Carmen created a poetic narrative to help her family manage their suffering. In this way, she helped her family become close and share a sense of belonging together. Carmen was able to transmute the family’s experience of trauma into a story that articulated their survival. Her poems became a written narrative of her family’s history. Resilience was created and passed along through the generations. This is the intergenerational transmission of resilience.
Intergenerational transmission has been shown in trauma; antisocial behavior; violence; religion; politics; substance abuse (J. Res. Adolesc. 1995;5:225-52); depression (J. Fam. Psychol. 2003;17:545-56); attachment (Psychol. Bull. 1995;117:387-403); perfectionism (J. Fam. Psychol. 2005;19:358-66); poverty; being on welfare; teenage pregnancy; education; and family life trajectories ("Intergenerational Transmission of Behavioral Patterns: Similarity of Parents’ and Children’s Family-Life Trajectories," Netherlands Interdisciplinary Demographical Institute, The Hague, 2006).
In short, there is evidence for the intergenerational transmission of everything bad. It is time to create evidence of the intergenerational transmission of resilience.
Researchers who study intergenerational legacies have discovered that children who know the most about their families have a strong sense of control over their lives, higher self-esteem, and the strongest "intergenerational self," compared with children who know less about their families. Marshall P. Duke, Ph.D., and his colleagues developed a measure called "Do You Know?" that asks children questions about their family. Examples of questions are "Do you know where your grandparents grew up? Do you know where your mom and dad went to high school?" (Psychotherapy 2008;45,268-72).
Dr. Duke identifies three common family narratives:
• The ascending family narrative: "Son, when we came to this country, we had nothing. Our family worked. We opened a store. Your grandfather went to high school. Your father went to college. And now you ... "
• The descending narrative: "Sweetheart, we used to have it all. Then we lost everything."
• The oscillating family narrative: "Dear, let me tell you, we’ve had ups and downs in our family. We built a family business. Your grandfather was a pillar of the community. Your mother was on the board of the hospital. But we also had setbacks. You had an uncle who was once arrested. We had a house burn down. Your father lost a job. But no matter what happened, we always stuck together as a family."
Healing narratives are prominent in American Indian and folk medicine traditions but also exist in modern medicine. In psychiatry, one of the tenets of the Recovery Movement is to focus on strengths and a positive sense of identity that is not linked to a psychiatric diagnosis. Communities such as Alcoholics Anonymous, Narcotics Anonymous, and Al-Anon foster resilience through communion and sharing. Narrative therapy, developed by Australian therapist Michael White and his collaborator David Epston of New Zealand in 1989 (Context 2009;105:57-58), is a type of psychotherapy that seeks and promotes a healthy, successful personal narrative to replace a dominant repressive illness narrative.
How can the psychiatrist, during a routine office visit, help patients develop a positive, resilient family narrative? Patients can benefit from an exploration of patterns of behavior or ways of relating that might have been passed down through the generations. Understanding the motivations, difficulties, and aspirations of their parents and grandparents provides patients with a historical perspective on their current difficulties. If patients can understand their difficulties in the context of the larger family system, they develop a more nuanced and less harsh understanding of the challenges they face.
When Sarah presented with depression, it became clear that her family dynamics were troubling. She felt happy and competent at work. In passing, she remarked that she felt intimidated by her teenage daughter, so I inquired about her family system to see what generational narratives might be at play. Over several sessions, we uncovered the covert negative messages she had received as a child. She had fought not to pass these on to her children, by being "more permissive and hands off." In response, her children chided her for being overly anxious, sensing that she was conflicted and troubled, although the source remained mysterious to everyone. Using a family systems approach to understand the intergenerational inheritance, the family came to understand the strong generational forces at work. This lessened her guilt and anguish, and increased the children’s understanding and empathy for their mother.
A family systems approach allows a family legacy to be revealed, reworked, and rewritten. A new family narrative that carries the family forward and allows the telling of a positive family narrative can be created. We can guide patients to find the positive aspects of their family stories and thus promote family resilience.
Here are a few questions we should ask our patients: "What did your parents teach you that you want to pass along? What values did your parents have? How have you lived or not lived those values? How has the relationship with your parents affected your relationship with your children? How did your parents resolve problems, and how do you resolve problems? How do your children resolve problems? What were the motivations that drove your parents? What countries do your relatives come from? What was it like for them growing up? Did they experience deprivation? War? How has that affected you and your siblings? Are there family secrets? What do you want to take away from this legacy? What do you want to pass along to the next generation?" Asking these questions allows the patient to see their current struggles and conflicts with a longer lens.
The novelist Laila Lalami, who did not know her mother, was surprised when her husband gave her a DNA test kit so that she could find out her genetic inheritance. When the results came in, Laila remarked: "So it was that, in just a few moments, I found myself returning to those childhood days when I used to dream up different families, and different fates, for my mother. What science gave me, in the end, was no different from what my own imagination had fed me for many years – stories. The search was not over. The search would never be over. And not even science could help fill out the abyss I grew up with. Only stories could." ("My Fictional Grandparents," The New York Times, July 26, 2013)
We are all part of our own family narrative that stretches back in time and forward into the future. We are creating a family story for ourselves in the present that our children will carry forward with them into their future. These narratives have many strands. Let’s help our patients pick out the strands that help them build family resilience.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Carmen Bugan read her poems to her family. Her father had been imprisoned by Securitate, the Romanian secret police, for anticommunist rhetoric that he distributed on leaflets to people’s mailboxes. Securitate tracked him down by examining the leaflets for identifying typescript that they linked to one of his typewriters. He buried his other typewriter in the garden to escape detection. He would dig it up when he wanted to write serious anticommunist literature, then rebury it again in the garden.
"It is not important that the poem stays or goes," Carmen writes. "I discover a way to relieve our family’s suffering even though when I read the poems to Mom and my sister it seems that I create more pain at first.
"Mom loves the words, loves explanations of feelings to negotiate pain, and I can provide this for her. My sister says her feelings are exteriorized, articulated by the emotions in the poem and I can help bring things out" ("Burying the Typewriter," Minneapolis: Graywolf Press, 2012, p. 124).
Carmen created a poetic narrative to help her family manage their suffering. In this way, she helped her family become close and share a sense of belonging together. Carmen was able to transmute the family’s experience of trauma into a story that articulated their survival. Her poems became a written narrative of her family’s history. Resilience was created and passed along through the generations. This is the intergenerational transmission of resilience.
Intergenerational transmission has been shown in trauma; antisocial behavior; violence; religion; politics; substance abuse (J. Res. Adolesc. 1995;5:225-52); depression (J. Fam. Psychol. 2003;17:545-56); attachment (Psychol. Bull. 1995;117:387-403); perfectionism (J. Fam. Psychol. 2005;19:358-66); poverty; being on welfare; teenage pregnancy; education; and family life trajectories ("Intergenerational Transmission of Behavioral Patterns: Similarity of Parents’ and Children’s Family-Life Trajectories," Netherlands Interdisciplinary Demographical Institute, The Hague, 2006).
In short, there is evidence for the intergenerational transmission of everything bad. It is time to create evidence of the intergenerational transmission of resilience.
Researchers who study intergenerational legacies have discovered that children who know the most about their families have a strong sense of control over their lives, higher self-esteem, and the strongest "intergenerational self," compared with children who know less about their families. Marshall P. Duke, Ph.D., and his colleagues developed a measure called "Do You Know?" that asks children questions about their family. Examples of questions are "Do you know where your grandparents grew up? Do you know where your mom and dad went to high school?" (Psychotherapy 2008;45,268-72).
Dr. Duke identifies three common family narratives:
• The ascending family narrative: "Son, when we came to this country, we had nothing. Our family worked. We opened a store. Your grandfather went to high school. Your father went to college. And now you ... "
• The descending narrative: "Sweetheart, we used to have it all. Then we lost everything."
• The oscillating family narrative: "Dear, let me tell you, we’ve had ups and downs in our family. We built a family business. Your grandfather was a pillar of the community. Your mother was on the board of the hospital. But we also had setbacks. You had an uncle who was once arrested. We had a house burn down. Your father lost a job. But no matter what happened, we always stuck together as a family."
Healing narratives are prominent in American Indian and folk medicine traditions but also exist in modern medicine. In psychiatry, one of the tenets of the Recovery Movement is to focus on strengths and a positive sense of identity that is not linked to a psychiatric diagnosis. Communities such as Alcoholics Anonymous, Narcotics Anonymous, and Al-Anon foster resilience through communion and sharing. Narrative therapy, developed by Australian therapist Michael White and his collaborator David Epston of New Zealand in 1989 (Context 2009;105:57-58), is a type of psychotherapy that seeks and promotes a healthy, successful personal narrative to replace a dominant repressive illness narrative.
How can the psychiatrist, during a routine office visit, help patients develop a positive, resilient family narrative? Patients can benefit from an exploration of patterns of behavior or ways of relating that might have been passed down through the generations. Understanding the motivations, difficulties, and aspirations of their parents and grandparents provides patients with a historical perspective on their current difficulties. If patients can understand their difficulties in the context of the larger family system, they develop a more nuanced and less harsh understanding of the challenges they face.
When Sarah presented with depression, it became clear that her family dynamics were troubling. She felt happy and competent at work. In passing, she remarked that she felt intimidated by her teenage daughter, so I inquired about her family system to see what generational narratives might be at play. Over several sessions, we uncovered the covert negative messages she had received as a child. She had fought not to pass these on to her children, by being "more permissive and hands off." In response, her children chided her for being overly anxious, sensing that she was conflicted and troubled, although the source remained mysterious to everyone. Using a family systems approach to understand the intergenerational inheritance, the family came to understand the strong generational forces at work. This lessened her guilt and anguish, and increased the children’s understanding and empathy for their mother.
A family systems approach allows a family legacy to be revealed, reworked, and rewritten. A new family narrative that carries the family forward and allows the telling of a positive family narrative can be created. We can guide patients to find the positive aspects of their family stories and thus promote family resilience.
Here are a few questions we should ask our patients: "What did your parents teach you that you want to pass along? What values did your parents have? How have you lived or not lived those values? How has the relationship with your parents affected your relationship with your children? How did your parents resolve problems, and how do you resolve problems? How do your children resolve problems? What were the motivations that drove your parents? What countries do your relatives come from? What was it like for them growing up? Did they experience deprivation? War? How has that affected you and your siblings? Are there family secrets? What do you want to take away from this legacy? What do you want to pass along to the next generation?" Asking these questions allows the patient to see their current struggles and conflicts with a longer lens.
The novelist Laila Lalami, who did not know her mother, was surprised when her husband gave her a DNA test kit so that she could find out her genetic inheritance. When the results came in, Laila remarked: "So it was that, in just a few moments, I found myself returning to those childhood days when I used to dream up different families, and different fates, for my mother. What science gave me, in the end, was no different from what my own imagination had fed me for many years – stories. The search was not over. The search would never be over. And not even science could help fill out the abyss I grew up with. Only stories could." ("My Fictional Grandparents," The New York Times, July 26, 2013)
We are all part of our own family narrative that stretches back in time and forward into the future. We are creating a family story for ourselves in the present that our children will carry forward with them into their future. These narratives have many strands. Let’s help our patients pick out the strands that help them build family resilience.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Carmen Bugan read her poems to her family. Her father had been imprisoned by Securitate, the Romanian secret police, for anticommunist rhetoric that he distributed on leaflets to people’s mailboxes. Securitate tracked him down by examining the leaflets for identifying typescript that they linked to one of his typewriters. He buried his other typewriter in the garden to escape detection. He would dig it up when he wanted to write serious anticommunist literature, then rebury it again in the garden.
"It is not important that the poem stays or goes," Carmen writes. "I discover a way to relieve our family’s suffering even though when I read the poems to Mom and my sister it seems that I create more pain at first.
"Mom loves the words, loves explanations of feelings to negotiate pain, and I can provide this for her. My sister says her feelings are exteriorized, articulated by the emotions in the poem and I can help bring things out" ("Burying the Typewriter," Minneapolis: Graywolf Press, 2012, p. 124).
Carmen created a poetic narrative to help her family manage their suffering. In this way, she helped her family become close and share a sense of belonging together. Carmen was able to transmute the family’s experience of trauma into a story that articulated their survival. Her poems became a written narrative of her family’s history. Resilience was created and passed along through the generations. This is the intergenerational transmission of resilience.
Intergenerational transmission has been shown in trauma; antisocial behavior; violence; religion; politics; substance abuse (J. Res. Adolesc. 1995;5:225-52); depression (J. Fam. Psychol. 2003;17:545-56); attachment (Psychol. Bull. 1995;117:387-403); perfectionism (J. Fam. Psychol. 2005;19:358-66); poverty; being on welfare; teenage pregnancy; education; and family life trajectories ("Intergenerational Transmission of Behavioral Patterns: Similarity of Parents’ and Children’s Family-Life Trajectories," Netherlands Interdisciplinary Demographical Institute, The Hague, 2006).
In short, there is evidence for the intergenerational transmission of everything bad. It is time to create evidence of the intergenerational transmission of resilience.
Researchers who study intergenerational legacies have discovered that children who know the most about their families have a strong sense of control over their lives, higher self-esteem, and the strongest "intergenerational self," compared with children who know less about their families. Marshall P. Duke, Ph.D., and his colleagues developed a measure called "Do You Know?" that asks children questions about their family. Examples of questions are "Do you know where your grandparents grew up? Do you know where your mom and dad went to high school?" (Psychotherapy 2008;45,268-72).
Dr. Duke identifies three common family narratives:
• The ascending family narrative: "Son, when we came to this country, we had nothing. Our family worked. We opened a store. Your grandfather went to high school. Your father went to college. And now you ... "
• The descending narrative: "Sweetheart, we used to have it all. Then we lost everything."
• The oscillating family narrative: "Dear, let me tell you, we’ve had ups and downs in our family. We built a family business. Your grandfather was a pillar of the community. Your mother was on the board of the hospital. But we also had setbacks. You had an uncle who was once arrested. We had a house burn down. Your father lost a job. But no matter what happened, we always stuck together as a family."
Healing narratives are prominent in American Indian and folk medicine traditions but also exist in modern medicine. In psychiatry, one of the tenets of the Recovery Movement is to focus on strengths and a positive sense of identity that is not linked to a psychiatric diagnosis. Communities such as Alcoholics Anonymous, Narcotics Anonymous, and Al-Anon foster resilience through communion and sharing. Narrative therapy, developed by Australian therapist Michael White and his collaborator David Epston of New Zealand in 1989 (Context 2009;105:57-58), is a type of psychotherapy that seeks and promotes a healthy, successful personal narrative to replace a dominant repressive illness narrative.
How can the psychiatrist, during a routine office visit, help patients develop a positive, resilient family narrative? Patients can benefit from an exploration of patterns of behavior or ways of relating that might have been passed down through the generations. Understanding the motivations, difficulties, and aspirations of their parents and grandparents provides patients with a historical perspective on their current difficulties. If patients can understand their difficulties in the context of the larger family system, they develop a more nuanced and less harsh understanding of the challenges they face.
When Sarah presented with depression, it became clear that her family dynamics were troubling. She felt happy and competent at work. In passing, she remarked that she felt intimidated by her teenage daughter, so I inquired about her family system to see what generational narratives might be at play. Over several sessions, we uncovered the covert negative messages she had received as a child. She had fought not to pass these on to her children, by being "more permissive and hands off." In response, her children chided her for being overly anxious, sensing that she was conflicted and troubled, although the source remained mysterious to everyone. Using a family systems approach to understand the intergenerational inheritance, the family came to understand the strong generational forces at work. This lessened her guilt and anguish, and increased the children’s understanding and empathy for their mother.
A family systems approach allows a family legacy to be revealed, reworked, and rewritten. A new family narrative that carries the family forward and allows the telling of a positive family narrative can be created. We can guide patients to find the positive aspects of their family stories and thus promote family resilience.
Here are a few questions we should ask our patients: "What did your parents teach you that you want to pass along? What values did your parents have? How have you lived or not lived those values? How has the relationship with your parents affected your relationship with your children? How did your parents resolve problems, and how do you resolve problems? How do your children resolve problems? What were the motivations that drove your parents? What countries do your relatives come from? What was it like for them growing up? Did they experience deprivation? War? How has that affected you and your siblings? Are there family secrets? What do you want to take away from this legacy? What do you want to pass along to the next generation?" Asking these questions allows the patient to see their current struggles and conflicts with a longer lens.
The novelist Laila Lalami, who did not know her mother, was surprised when her husband gave her a DNA test kit so that she could find out her genetic inheritance. When the results came in, Laila remarked: "So it was that, in just a few moments, I found myself returning to those childhood days when I used to dream up different families, and different fates, for my mother. What science gave me, in the end, was no different from what my own imagination had fed me for many years – stories. The search was not over. The search would never be over. And not even science could help fill out the abyss I grew up with. Only stories could." ("My Fictional Grandparents," The New York Times, July 26, 2013)
We are all part of our own family narrative that stretches back in time and forward into the future. We are creating a family story for ourselves in the present that our children will carry forward with them into their future. These narratives have many strands. Let’s help our patients pick out the strands that help them build family resilience.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Family therapy in Romania and lessons for the West
In the United States, family psychiatrists continue to deal with the fallout from the 1950s and 1960s, when the early family therapists located mental illness within the family and then touted family therapy as the cure. Families felt blamed and shied away from "family therapy."
Yet, research shows that family treatment for many psychiatric and medical illnesses, whether it is family inclusion or psychoeducation, is very effective in reducing morbidity. Stigma and fear about family involvement have resulted in family treatment lagging behind other psychotherapies in its acceptance as a valid therapeutic intervention.
As a contrast, it is therefore interesting to look at Romania, a postcommunist country, where all psychotherapies were deemed "unnecessary" under communism. According to Dr. Ileana-Mihaela Botezat-Antonescu, "Psychotherapy and psychoanalysis were known as the studies of the soul during the communist regime and went underground. Secret psychotherapy meetings were held in Sibiu and Timisoara, but after the 1989 revolution, we had access to information from abroad," she said during a presentation this year at the World Psychiatric Association meeting in Bucharest, Romania.
"In 1990, freedom occurs, but nobody tells you what to do. You cannot count on anything. It alienated people seeking help. It was a process that took time," said Dr. Botezat-Antonescu, a psychiatrist and psychoanalyst who was trained in the mid-1990s by trainers from the Dutch Psychoanalytic Association and serves as chair of the National Center for Mental Health.
Psychotherapists in Romania must somehow address the traumatic environment that lasted a generation. Young people strive to gain their sense of identity and belonging and, at the same time, are challenged with reestablishing a connection between the generations. The sense of intergenerational trauma and loss extends back to grandparents who lost their farms, houses, and social position.
An understanding of the intergenerational transmission of trauma can inform psychotherapists across the globe in their care of young people. Family therapy is a type of psychotherapy that is well suited to address this intergenerational trauma.
Psychological trauma is passed down through the generations in subtle and unspoken ways. It is important for therapists to recognize when this is occurring and work with the whole family. Family therapy that specifically addresses the intergenerational transmission of trauma can help move a family from feelings of helplessness toward resilience.
Development of family therapy
Family therapy developed in Romania through training courses in Cluj, Târgu Mures, and Timisoara. As there were no Romanian trainers, these courses were taught by family therapists from countries such as Ireland, France, and Yugoslavia. Families and trainees spoke Romanian or Hungarian, and during live supervision, simultaneous translation occurred. All courses, readings, and assignments were in English. Family therapy developed in Romania through training courses in Cluj, Târgu Mures and Timisoara.
Trainees saw families in their own work contexts, for example, psychotherapy centers; psychiatry hospitals; and community centers, such as family planning clinics and domestic violence shelters. Currently, there are 16 family therapy professional organizations (Contemp. Fam. Ther. 2013;35:275-87), including:
• Systemic Family Therapy Association in Cluj
• Association of Family Therapy in Bucharest
• Romanian Association for Family and Systemic Therapy in Timisoara
• Association Crisdu Areopagus in Timisoara
• Pro Familia – Family Therapy Association in Miercurea-Ciuc
• Association for Couple and Family Psychotherapy in Iasi
• Association for Family Counselling and Therapy in Iasi
Dr. Zoltán Kónya and Dr. Ágnes Kónya run the family therapy center in Cluj and have written about the challenges of practicing family therapy in Romania (Context 2007;92:2-4 and Contemporary Family Therapy 2013;35:1). Since family therapy training courses developed at different times, in different places, with trainers invited from different countries, the sense of what constitutes family therapy varies across Romania.
The meaning of the word "systemic" has proved particularly contentious. For some, systemic is synonymous with the Milan approach – which is based on the notion that "families are self-regulating systems that function based on self-developed rules tested over time through a process of trial and error" (Case Conceptualization in Family Therapy, Boston: Pearson, 2013). However, others consider family therapy as more than a systemic approach. Some promote systemic thinking as an all-encompassing epistemological frame for consultation with individuals, families, and organizations, but others do not attach much importance to the term "systemic."
The challenge of organizing into one Romanian family therapy institution with one outlook is great. This challenge also replicates one of the major problems in our field – the idea that family therapy means different things to different people. In Romania, well-meaning outside attempts ended up in a fractured national family therapy identity.
The Kónyas, trained by Irish family therapists, identify additional challenges of introducing family therapy into a culture unfamiliar with the concept. "The fit between systemic therapy and Romanian culture has been a concern of ours since the beginning of our training," they wrote in 2003. "There had been no tradition of people seeing psychotherapists in times of distress. Also, the vast majority of health care professionals had not even heard about family therapy. Would families come to therapy?"
They found that not only did clients come to therapy, but they also were ready to work hard when they did.
"We admire our clients’ courage in facing a series of challenges involved in the therapy process: consulting an outsider for a family problem, participating in sessions as a family, being asked unusual questions, being videotaped and, sometimes, being observed by a team and/or supervisors from abroad," they said.
In their work with patients, the Kónyas write, they have encountered difficulties tied to the use of words and phrases used in systemic therapy.
"For example, the Batesonian phrase 'a difference that makes a difference' is very difficult, if not impossible to properly translate into Romanian – of course, this may only be a problem in a training context, not in therapy. In response to the Romanian or Hungarian translation of the question: ‘And how has this been a problem for you?’ clients almost invariably demonstrate a lack of comprehension: ‘Would you please say that again? I didn’t understand.’ The difficulty here is not that the question makes no sense, but that it is culturally unusual – and therefore potentially therapeutic," they write (Context 2007)
"Also, certain words that might sound neutral in the West sometimes trigger strong emotions in our country. For example, monitoring progress on a 1-10 scale might recall painful experiences connected with school, because in Romania, marks are from 1 to 10. Also, talking about ‘systems’ may trigger discomfort, as this is the word people used during communism to describe the oppressive dictatorial regime. People who challenged the dominant ideas used to be called ‘the enemies of the system.’ "
The communist ideal of "systemization" broke families. Women were encouraged to give birth in a pronatal policy that resulted in orphans and unwanted children. After the 1989 revolution, more than 300,000 Romanians were living in psychiatric institutions. Communist factories were closed, and displaced workers had no place. Raising a voice against the regime risked imprisonment as an enemy of the system. The word "system" is associated with oppression in Romania.
Are there lessons for us in the West? I think the answer is yes and that the Romanian experience highlights several imperatives that are useful for Western mental health professionals. Among those imperatives:
• Family psychiatry needs to agree on a definition of family therapy. Is it any approach that includes families? Do we need to be systemic to be considered family therapists? Does family support qualify as family therapy? Does family psychoeducation qualify as family therapy? Can we embrace these two levels, as well as a third, more-skilled level, a systemic family therapy? Can we accept a three-level definition of family treatment?
• Can we incorporate all the family therapy models into one approach that people will recognize as a generic approach to families? Can we use the common factors approach described by Douglas H. Sprenkle, Ph.D., Sean D. Davis, Ph.D., and Jay L. Lebow, Ph.D., in "Common Factors in Couple and Family Therapy" (New York: The Guilford Press, 2009)? For couples and family therapists, common factors over and above the well-recognized individual psychotherapy factors are conceptualizing the problems in relational terms, using therapy that aims to disrupt dysfunctional relational patterns, expanding treatment to include family members of the index patient, and fostering an expanded therapeutic alliance, according to Dr. Sprenkle, Dr. Davis, and Dr. Lebow.
• Can we develop a protocol that beginners can follow? Aaron Beck’s cognitive-behavioral therapy (CBT) provides a basic template that is easy for the novice therapist and the patient to use, yet brings a unique perspective to psychotherapy. CBT has gone on to develop in several diverse directions, but all CBT models have the same basic set of beliefs. Can a family approach or protocol be both simple AND allow for more sophisticated elaboration? Can we develop a set of basic steps that define family treatment?
• Should there be an approach to families that all disciplines can follow? Family therapy is practiced by physicians, nurses, social workers, and marriage and family therapists. Each discipline tends to work with different populations. Physicians tend to see families in which one person is the identified patient. Social workers tend to see families that have been referred for social services, families who are frequently struggling with such problems as housing, financial, and legal difficulties. Marriage and family therapists are often employed by community and hospital agencies as health care extenders and might work alongside other health care professionals. Would a single approach to families be useful?
In summary, if family therapy is to endure, it must be teachable, translatable, and relevant across disciplines and national boundaries. The systemic paradigm is an important perspective from which all practitioners can benefit. We must continue to disseminate evidence-based family treatments and teach family principles that can be incorporated on a daily basis by all mental health professionals.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
In the United States, family psychiatrists continue to deal with the fallout from the 1950s and 1960s, when the early family therapists located mental illness within the family and then touted family therapy as the cure. Families felt blamed and shied away from "family therapy."
Yet, research shows that family treatment for many psychiatric and medical illnesses, whether it is family inclusion or psychoeducation, is very effective in reducing morbidity. Stigma and fear about family involvement have resulted in family treatment lagging behind other psychotherapies in its acceptance as a valid therapeutic intervention.
As a contrast, it is therefore interesting to look at Romania, a postcommunist country, where all psychotherapies were deemed "unnecessary" under communism. According to Dr. Ileana-Mihaela Botezat-Antonescu, "Psychotherapy and psychoanalysis were known as the studies of the soul during the communist regime and went underground. Secret psychotherapy meetings were held in Sibiu and Timisoara, but after the 1989 revolution, we had access to information from abroad," she said during a presentation this year at the World Psychiatric Association meeting in Bucharest, Romania.
"In 1990, freedom occurs, but nobody tells you what to do. You cannot count on anything. It alienated people seeking help. It was a process that took time," said Dr. Botezat-Antonescu, a psychiatrist and psychoanalyst who was trained in the mid-1990s by trainers from the Dutch Psychoanalytic Association and serves as chair of the National Center for Mental Health.
Psychotherapists in Romania must somehow address the traumatic environment that lasted a generation. Young people strive to gain their sense of identity and belonging and, at the same time, are challenged with reestablishing a connection between the generations. The sense of intergenerational trauma and loss extends back to grandparents who lost their farms, houses, and social position.
An understanding of the intergenerational transmission of trauma can inform psychotherapists across the globe in their care of young people. Family therapy is a type of psychotherapy that is well suited to address this intergenerational trauma.
Psychological trauma is passed down through the generations in subtle and unspoken ways. It is important for therapists to recognize when this is occurring and work with the whole family. Family therapy that specifically addresses the intergenerational transmission of trauma can help move a family from feelings of helplessness toward resilience.
Development of family therapy
Family therapy developed in Romania through training courses in Cluj, Târgu Mures, and Timisoara. As there were no Romanian trainers, these courses were taught by family therapists from countries such as Ireland, France, and Yugoslavia. Families and trainees spoke Romanian or Hungarian, and during live supervision, simultaneous translation occurred. All courses, readings, and assignments were in English. Family therapy developed in Romania through training courses in Cluj, Târgu Mures and Timisoara.
Trainees saw families in their own work contexts, for example, psychotherapy centers; psychiatry hospitals; and community centers, such as family planning clinics and domestic violence shelters. Currently, there are 16 family therapy professional organizations (Contemp. Fam. Ther. 2013;35:275-87), including:
• Systemic Family Therapy Association in Cluj
• Association of Family Therapy in Bucharest
• Romanian Association for Family and Systemic Therapy in Timisoara
• Association Crisdu Areopagus in Timisoara
• Pro Familia – Family Therapy Association in Miercurea-Ciuc
• Association for Couple and Family Psychotherapy in Iasi
• Association for Family Counselling and Therapy in Iasi
Dr. Zoltán Kónya and Dr. Ágnes Kónya run the family therapy center in Cluj and have written about the challenges of practicing family therapy in Romania (Context 2007;92:2-4 and Contemporary Family Therapy 2013;35:1). Since family therapy training courses developed at different times, in different places, with trainers invited from different countries, the sense of what constitutes family therapy varies across Romania.
The meaning of the word "systemic" has proved particularly contentious. For some, systemic is synonymous with the Milan approach – which is based on the notion that "families are self-regulating systems that function based on self-developed rules tested over time through a process of trial and error" (Case Conceptualization in Family Therapy, Boston: Pearson, 2013). However, others consider family therapy as more than a systemic approach. Some promote systemic thinking as an all-encompassing epistemological frame for consultation with individuals, families, and organizations, but others do not attach much importance to the term "systemic."
The challenge of organizing into one Romanian family therapy institution with one outlook is great. This challenge also replicates one of the major problems in our field – the idea that family therapy means different things to different people. In Romania, well-meaning outside attempts ended up in a fractured national family therapy identity.
The Kónyas, trained by Irish family therapists, identify additional challenges of introducing family therapy into a culture unfamiliar with the concept. "The fit between systemic therapy and Romanian culture has been a concern of ours since the beginning of our training," they wrote in 2003. "There had been no tradition of people seeing psychotherapists in times of distress. Also, the vast majority of health care professionals had not even heard about family therapy. Would families come to therapy?"
They found that not only did clients come to therapy, but they also were ready to work hard when they did.
"We admire our clients’ courage in facing a series of challenges involved in the therapy process: consulting an outsider for a family problem, participating in sessions as a family, being asked unusual questions, being videotaped and, sometimes, being observed by a team and/or supervisors from abroad," they said.
In their work with patients, the Kónyas write, they have encountered difficulties tied to the use of words and phrases used in systemic therapy.
"For example, the Batesonian phrase 'a difference that makes a difference' is very difficult, if not impossible to properly translate into Romanian – of course, this may only be a problem in a training context, not in therapy. In response to the Romanian or Hungarian translation of the question: ‘And how has this been a problem for you?’ clients almost invariably demonstrate a lack of comprehension: ‘Would you please say that again? I didn’t understand.’ The difficulty here is not that the question makes no sense, but that it is culturally unusual – and therefore potentially therapeutic," they write (Context 2007)
"Also, certain words that might sound neutral in the West sometimes trigger strong emotions in our country. For example, monitoring progress on a 1-10 scale might recall painful experiences connected with school, because in Romania, marks are from 1 to 10. Also, talking about ‘systems’ may trigger discomfort, as this is the word people used during communism to describe the oppressive dictatorial regime. People who challenged the dominant ideas used to be called ‘the enemies of the system.’ "
The communist ideal of "systemization" broke families. Women were encouraged to give birth in a pronatal policy that resulted in orphans and unwanted children. After the 1989 revolution, more than 300,000 Romanians were living in psychiatric institutions. Communist factories were closed, and displaced workers had no place. Raising a voice against the regime risked imprisonment as an enemy of the system. The word "system" is associated with oppression in Romania.
Are there lessons for us in the West? I think the answer is yes and that the Romanian experience highlights several imperatives that are useful for Western mental health professionals. Among those imperatives:
• Family psychiatry needs to agree on a definition of family therapy. Is it any approach that includes families? Do we need to be systemic to be considered family therapists? Does family support qualify as family therapy? Does family psychoeducation qualify as family therapy? Can we embrace these two levels, as well as a third, more-skilled level, a systemic family therapy? Can we accept a three-level definition of family treatment?
• Can we incorporate all the family therapy models into one approach that people will recognize as a generic approach to families? Can we use the common factors approach described by Douglas H. Sprenkle, Ph.D., Sean D. Davis, Ph.D., and Jay L. Lebow, Ph.D., in "Common Factors in Couple and Family Therapy" (New York: The Guilford Press, 2009)? For couples and family therapists, common factors over and above the well-recognized individual psychotherapy factors are conceptualizing the problems in relational terms, using therapy that aims to disrupt dysfunctional relational patterns, expanding treatment to include family members of the index patient, and fostering an expanded therapeutic alliance, according to Dr. Sprenkle, Dr. Davis, and Dr. Lebow.
• Can we develop a protocol that beginners can follow? Aaron Beck’s cognitive-behavioral therapy (CBT) provides a basic template that is easy for the novice therapist and the patient to use, yet brings a unique perspective to psychotherapy. CBT has gone on to develop in several diverse directions, but all CBT models have the same basic set of beliefs. Can a family approach or protocol be both simple AND allow for more sophisticated elaboration? Can we develop a set of basic steps that define family treatment?
• Should there be an approach to families that all disciplines can follow? Family therapy is practiced by physicians, nurses, social workers, and marriage and family therapists. Each discipline tends to work with different populations. Physicians tend to see families in which one person is the identified patient. Social workers tend to see families that have been referred for social services, families who are frequently struggling with such problems as housing, financial, and legal difficulties. Marriage and family therapists are often employed by community and hospital agencies as health care extenders and might work alongside other health care professionals. Would a single approach to families be useful?
In summary, if family therapy is to endure, it must be teachable, translatable, and relevant across disciplines and national boundaries. The systemic paradigm is an important perspective from which all practitioners can benefit. We must continue to disseminate evidence-based family treatments and teach family principles that can be incorporated on a daily basis by all mental health professionals.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
In the United States, family psychiatrists continue to deal with the fallout from the 1950s and 1960s, when the early family therapists located mental illness within the family and then touted family therapy as the cure. Families felt blamed and shied away from "family therapy."
Yet, research shows that family treatment for many psychiatric and medical illnesses, whether it is family inclusion or psychoeducation, is very effective in reducing morbidity. Stigma and fear about family involvement have resulted in family treatment lagging behind other psychotherapies in its acceptance as a valid therapeutic intervention.
As a contrast, it is therefore interesting to look at Romania, a postcommunist country, where all psychotherapies were deemed "unnecessary" under communism. According to Dr. Ileana-Mihaela Botezat-Antonescu, "Psychotherapy and psychoanalysis were known as the studies of the soul during the communist regime and went underground. Secret psychotherapy meetings were held in Sibiu and Timisoara, but after the 1989 revolution, we had access to information from abroad," she said during a presentation this year at the World Psychiatric Association meeting in Bucharest, Romania.
"In 1990, freedom occurs, but nobody tells you what to do. You cannot count on anything. It alienated people seeking help. It was a process that took time," said Dr. Botezat-Antonescu, a psychiatrist and psychoanalyst who was trained in the mid-1990s by trainers from the Dutch Psychoanalytic Association and serves as chair of the National Center for Mental Health.
Psychotherapists in Romania must somehow address the traumatic environment that lasted a generation. Young people strive to gain their sense of identity and belonging and, at the same time, are challenged with reestablishing a connection between the generations. The sense of intergenerational trauma and loss extends back to grandparents who lost their farms, houses, and social position.
An understanding of the intergenerational transmission of trauma can inform psychotherapists across the globe in their care of young people. Family therapy is a type of psychotherapy that is well suited to address this intergenerational trauma.
Psychological trauma is passed down through the generations in subtle and unspoken ways. It is important for therapists to recognize when this is occurring and work with the whole family. Family therapy that specifically addresses the intergenerational transmission of trauma can help move a family from feelings of helplessness toward resilience.
Development of family therapy
Family therapy developed in Romania through training courses in Cluj, Târgu Mures, and Timisoara. As there were no Romanian trainers, these courses were taught by family therapists from countries such as Ireland, France, and Yugoslavia. Families and trainees spoke Romanian or Hungarian, and during live supervision, simultaneous translation occurred. All courses, readings, and assignments were in English. Family therapy developed in Romania through training courses in Cluj, Târgu Mures and Timisoara.
Trainees saw families in their own work contexts, for example, psychotherapy centers; psychiatry hospitals; and community centers, such as family planning clinics and domestic violence shelters. Currently, there are 16 family therapy professional organizations (Contemp. Fam. Ther. 2013;35:275-87), including:
• Systemic Family Therapy Association in Cluj
• Association of Family Therapy in Bucharest
• Romanian Association for Family and Systemic Therapy in Timisoara
• Association Crisdu Areopagus in Timisoara
• Pro Familia – Family Therapy Association in Miercurea-Ciuc
• Association for Couple and Family Psychotherapy in Iasi
• Association for Family Counselling and Therapy in Iasi
Dr. Zoltán Kónya and Dr. Ágnes Kónya run the family therapy center in Cluj and have written about the challenges of practicing family therapy in Romania (Context 2007;92:2-4 and Contemporary Family Therapy 2013;35:1). Since family therapy training courses developed at different times, in different places, with trainers invited from different countries, the sense of what constitutes family therapy varies across Romania.
The meaning of the word "systemic" has proved particularly contentious. For some, systemic is synonymous with the Milan approach – which is based on the notion that "families are self-regulating systems that function based on self-developed rules tested over time through a process of trial and error" (Case Conceptualization in Family Therapy, Boston: Pearson, 2013). However, others consider family therapy as more than a systemic approach. Some promote systemic thinking as an all-encompassing epistemological frame for consultation with individuals, families, and organizations, but others do not attach much importance to the term "systemic."
The challenge of organizing into one Romanian family therapy institution with one outlook is great. This challenge also replicates one of the major problems in our field – the idea that family therapy means different things to different people. In Romania, well-meaning outside attempts ended up in a fractured national family therapy identity.
The Kónyas, trained by Irish family therapists, identify additional challenges of introducing family therapy into a culture unfamiliar with the concept. "The fit between systemic therapy and Romanian culture has been a concern of ours since the beginning of our training," they wrote in 2003. "There had been no tradition of people seeing psychotherapists in times of distress. Also, the vast majority of health care professionals had not even heard about family therapy. Would families come to therapy?"
They found that not only did clients come to therapy, but they also were ready to work hard when they did.
"We admire our clients’ courage in facing a series of challenges involved in the therapy process: consulting an outsider for a family problem, participating in sessions as a family, being asked unusual questions, being videotaped and, sometimes, being observed by a team and/or supervisors from abroad," they said.
In their work with patients, the Kónyas write, they have encountered difficulties tied to the use of words and phrases used in systemic therapy.
"For example, the Batesonian phrase 'a difference that makes a difference' is very difficult, if not impossible to properly translate into Romanian – of course, this may only be a problem in a training context, not in therapy. In response to the Romanian or Hungarian translation of the question: ‘And how has this been a problem for you?’ clients almost invariably demonstrate a lack of comprehension: ‘Would you please say that again? I didn’t understand.’ The difficulty here is not that the question makes no sense, but that it is culturally unusual – and therefore potentially therapeutic," they write (Context 2007)
"Also, certain words that might sound neutral in the West sometimes trigger strong emotions in our country. For example, monitoring progress on a 1-10 scale might recall painful experiences connected with school, because in Romania, marks are from 1 to 10. Also, talking about ‘systems’ may trigger discomfort, as this is the word people used during communism to describe the oppressive dictatorial regime. People who challenged the dominant ideas used to be called ‘the enemies of the system.’ "
The communist ideal of "systemization" broke families. Women were encouraged to give birth in a pronatal policy that resulted in orphans and unwanted children. After the 1989 revolution, more than 300,000 Romanians were living in psychiatric institutions. Communist factories were closed, and displaced workers had no place. Raising a voice against the regime risked imprisonment as an enemy of the system. The word "system" is associated with oppression in Romania.
Are there lessons for us in the West? I think the answer is yes and that the Romanian experience highlights several imperatives that are useful for Western mental health professionals. Among those imperatives:
• Family psychiatry needs to agree on a definition of family therapy. Is it any approach that includes families? Do we need to be systemic to be considered family therapists? Does family support qualify as family therapy? Does family psychoeducation qualify as family therapy? Can we embrace these two levels, as well as a third, more-skilled level, a systemic family therapy? Can we accept a three-level definition of family treatment?
• Can we incorporate all the family therapy models into one approach that people will recognize as a generic approach to families? Can we use the common factors approach described by Douglas H. Sprenkle, Ph.D., Sean D. Davis, Ph.D., and Jay L. Lebow, Ph.D., in "Common Factors in Couple and Family Therapy" (New York: The Guilford Press, 2009)? For couples and family therapists, common factors over and above the well-recognized individual psychotherapy factors are conceptualizing the problems in relational terms, using therapy that aims to disrupt dysfunctional relational patterns, expanding treatment to include family members of the index patient, and fostering an expanded therapeutic alliance, according to Dr. Sprenkle, Dr. Davis, and Dr. Lebow.
• Can we develop a protocol that beginners can follow? Aaron Beck’s cognitive-behavioral therapy (CBT) provides a basic template that is easy for the novice therapist and the patient to use, yet brings a unique perspective to psychotherapy. CBT has gone on to develop in several diverse directions, but all CBT models have the same basic set of beliefs. Can a family approach or protocol be both simple AND allow for more sophisticated elaboration? Can we develop a set of basic steps that define family treatment?
• Should there be an approach to families that all disciplines can follow? Family therapy is practiced by physicians, nurses, social workers, and marriage and family therapists. Each discipline tends to work with different populations. Physicians tend to see families in which one person is the identified patient. Social workers tend to see families that have been referred for social services, families who are frequently struggling with such problems as housing, financial, and legal difficulties. Marriage and family therapists are often employed by community and hospital agencies as health care extenders and might work alongside other health care professionals. Would a single approach to families be useful?
In summary, if family therapy is to endure, it must be teachable, translatable, and relevant across disciplines and national boundaries. The systemic paradigm is an important perspective from which all practitioners can benefit. We must continue to disseminate evidence-based family treatments and teach family principles that can be incorporated on a daily basis by all mental health professionals.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Including caregivers in patient care is an ethical imperative
Ms. Stout is a 58-year-old divorced mother of two. Her eldest son, Paul, aged 35, has cystic fibrosis and is the recipient of a lung transplant. He has several developmental delays, and his comprehension of medicolegal documents becomes quite limited when he is medically ill and on narcotics. His outpatient medical team is aware of this and includes his mother in all treatment decisions.
However, in the hospital, the medical teams do not appreciate his limitations. In the inpatient hospital setting, he does not retain information presented to him. They question his mother’s continual presence and see her as "overinvolved and enmeshed with her adult son." Ms. Stout says that she has to fight with each new physician team to get them to understand that they need to involve her in all her son’s health care decisions. The younger male physicians, especially, identify with Paul.
Paul presents as a well-adjusted young man. He is agreeable, open, and friendly with the staff. Paul has limited social contacts outside of the hospital. Because of his lengthy involvement in the hospital care system, he is comfortable in the hospital and especially enjoys his interaction with the female nurses. He understands basic procedures because they have been repeated so many times. However, he does not understand his complex health care needs. Unless his comprehension is specifically tested, his deficits go unrecognized.
His mother knows the details of his history and is a better resource than the chart. She insists on being present at all times, despite the demands of her other commitments. Each time her son is admitted, she faces scrutiny, and repeatedly has to explain herself and her son’s limitations to each new physician. She finds this situation exhausting and humiliating. She does not understand why her presence cannot be accepted as helpful.
The toll of caregiving
Family caregivers face many physical, emotional, and financial demands that make them vulnerable to stress-related conditions, both physical and psychological. Caregiving affects caregivers’ health, which, in turn, affects their ability to provide care. The Caregiver Health Effects Study demonstrated a strong link between caregiving and mortality risk, finding that elderly caregivers supporting disabled spouses at home were 63% more likely to die within 4 years than noncaregiving elderly spouses (JAMA 1999;282:2215-9). In addition, family caregivers often lack the time and energy to prepare their own meals, exercise, or engage in their own preventive medical care. Physicians must stress the importance of caregiver self-care for the benefit of both the caregiver and the patient, and identify appropriate sources of community support services, such as home health aides, respite, or adult day care.
In 2008, according to Suzanne Mintz, a cofounder of the National Family Caregivers Association, the estimated market value of the family caregivers’ services was $375 billion annually. Almost one-third of the U.S. population provides care for a chronically ill, disabled, or aged family member or friend during any given year and spends an average of 20 hours per week providing care for loved ones. Two-thirds of caregivers are women, and 13% of family caregivers are providing 40 hours of care a week or more.
The American Psychological Association has a "Caregiver Briefcase." The briefcase contains caregiving facts; a practice section with common caregiver problems and interventions; and sections on research, education, and advocacy. The website and its contents are useful for family members as well as professionals.
In addition, the American Psychological Association offers ways for family members to integrate into health care teams. For example, electronic medical records can allow family members access to portions such as the patient’s problem and medication lists and most recent laboratory findings. Family caregivers can provide ongoing, real-time observations about the patient through the portal, as well as share information about what it is like to be a family caregiver. Those secure messages become part of the patient’s permanent medical record.
Shifting patient decision making to family members is a delicate negotiation between the patient’s ability to make independent decisions and the family’s desire to protect the patient from potentially poor decisions. At critical times, the family has to step up and assume decision-making responsibility for the patient.
To help physicians understand the ethics of this process, the American College of Physicians offers guidelines to help the physician know how best to collaborate with the patient and the caregiver (J. Gen. Intern. Med. 2010;25:255-60). These guidelines are endorsed by 10 medical professional societies, including the Society of General Internal Medicine, the American Academy of Neurology, and the American Academy of Hospice and Palliative Medicine.
Ethical guidelines for collaboration
When working with patients, making sure that six factors are met will help us do a better job of ensuring that the relationship with caregivers is productive for all three parties involved. Here is a listing:
• Respect the patient’s dignity, rights, and values in all patient-physician-caregiver interactions.
• Recognize that physician accessibility and excellent communication are fundamental to supporting the patient and family caregiver.
• Recognize the value of family caregivers as a source of continuity regarding the patient’s medical and psychosocial history.
• Facilitate end of life adjustments for the family.
• Ensure appropriate boundaries when the caregiver is a health care professional.
• Ensure the caregiver receives appropriate support, referrals, and services.
Our failure to use patient and family-centered care (PFCC) is tied to attitudinal, educational, and organizational barriers. The first attitudinal barrier is the expectation that families will be unreasonable. The second is that families will compromise confidentiality. The third is that physicians are largely unaware of research on the benefits of PFCC. Finally, physicians believe that PFCC is time consuming and costs too much.
Educational barriers include the lack of skills needed for collaboration among professionals, administrators, patients, and families.
Organizational barriers that get in the way of PFCC are the lack of guiding vision, the top-down approach with insufficient effort to build staff commitment; grassroots effort that lacks leadership, commitment, and support; scarce fiscal resources and competing priorities; and the absence of a funded coordinator.
Psychiatric illnesses are chronic medical illnesses. As more people have experiences as patients and caregivers, the pressure to involve family members such as Ms. Stout increases. Where does the resistance to involving family members in patient care come from? There is an unfounded, unspoken fear on the part of health professionals that families want something that the health care provider cannot guarantee – that their relative "will get well and everything will be fine." Health care providers might limit what they say to family members in order "not to upset them." If the family members perceive that they are being brushed off and dismissed, they can develop feelings of apprehension. A small upset or misunderstanding can then unleash repressed feelings, resulting in family members lashing out. When health care teams include the family and develop collaborative relationships with families, the likelihood of this kind of conflict is reduced.
Resistance also comes from the perception that family involvement is not necessary for patient care. Many of the consequences of isolating patients from their family are invisible, such as relationship strain, role changes, and caregiver burden. The reality is that, for patients such as Ms. Stout’s son, his mother’s involvement helps his medical team do a better job of managing his care.
It is time that psychiatry, and specifically the American Psychiatric Association, develop ethical guidelines outlining how to work with families of patients with chronic psychiatric illness. At the very least, we should sign on with other medical specialties by endorsing the American College of Physicians’ ethical guidelines described above. We have lagged behind the rest of medicine by failing to address this important issue.
This column, "Families in Psychiatry," appears regularly in Clinical Psychiatry News, a publication of IMNG Medical Media. Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Ms. Stout is a 58-year-old divorced mother of two. Her eldest son, Paul, aged 35, has cystic fibrosis and is the recipient of a lung transplant. He has several developmental delays, and his comprehension of medicolegal documents becomes quite limited when he is medically ill and on narcotics. His outpatient medical team is aware of this and includes his mother in all treatment decisions.
However, in the hospital, the medical teams do not appreciate his limitations. In the inpatient hospital setting, he does not retain information presented to him. They question his mother’s continual presence and see her as "overinvolved and enmeshed with her adult son." Ms. Stout says that she has to fight with each new physician team to get them to understand that they need to involve her in all her son’s health care decisions. The younger male physicians, especially, identify with Paul.
Paul presents as a well-adjusted young man. He is agreeable, open, and friendly with the staff. Paul has limited social contacts outside of the hospital. Because of his lengthy involvement in the hospital care system, he is comfortable in the hospital and especially enjoys his interaction with the female nurses. He understands basic procedures because they have been repeated so many times. However, he does not understand his complex health care needs. Unless his comprehension is specifically tested, his deficits go unrecognized.
His mother knows the details of his history and is a better resource than the chart. She insists on being present at all times, despite the demands of her other commitments. Each time her son is admitted, she faces scrutiny, and repeatedly has to explain herself and her son’s limitations to each new physician. She finds this situation exhausting and humiliating. She does not understand why her presence cannot be accepted as helpful.
The toll of caregiving
Family caregivers face many physical, emotional, and financial demands that make them vulnerable to stress-related conditions, both physical and psychological. Caregiving affects caregivers’ health, which, in turn, affects their ability to provide care. The Caregiver Health Effects Study demonstrated a strong link between caregiving and mortality risk, finding that elderly caregivers supporting disabled spouses at home were 63% more likely to die within 4 years than noncaregiving elderly spouses (JAMA 1999;282:2215-9). In addition, family caregivers often lack the time and energy to prepare their own meals, exercise, or engage in their own preventive medical care. Physicians must stress the importance of caregiver self-care for the benefit of both the caregiver and the patient, and identify appropriate sources of community support services, such as home health aides, respite, or adult day care.
In 2008, according to Suzanne Mintz, a cofounder of the National Family Caregivers Association, the estimated market value of the family caregivers’ services was $375 billion annually. Almost one-third of the U.S. population provides care for a chronically ill, disabled, or aged family member or friend during any given year and spends an average of 20 hours per week providing care for loved ones. Two-thirds of caregivers are women, and 13% of family caregivers are providing 40 hours of care a week or more.
The American Psychological Association has a "Caregiver Briefcase." The briefcase contains caregiving facts; a practice section with common caregiver problems and interventions; and sections on research, education, and advocacy. The website and its contents are useful for family members as well as professionals.
In addition, the American Psychological Association offers ways for family members to integrate into health care teams. For example, electronic medical records can allow family members access to portions such as the patient’s problem and medication lists and most recent laboratory findings. Family caregivers can provide ongoing, real-time observations about the patient through the portal, as well as share information about what it is like to be a family caregiver. Those secure messages become part of the patient’s permanent medical record.
Shifting patient decision making to family members is a delicate negotiation between the patient’s ability to make independent decisions and the family’s desire to protect the patient from potentially poor decisions. At critical times, the family has to step up and assume decision-making responsibility for the patient.
To help physicians understand the ethics of this process, the American College of Physicians offers guidelines to help the physician know how best to collaborate with the patient and the caregiver (J. Gen. Intern. Med. 2010;25:255-60). These guidelines are endorsed by 10 medical professional societies, including the Society of General Internal Medicine, the American Academy of Neurology, and the American Academy of Hospice and Palliative Medicine.
Ethical guidelines for collaboration
When working with patients, making sure that six factors are met will help us do a better job of ensuring that the relationship with caregivers is productive for all three parties involved. Here is a listing:
• Respect the patient’s dignity, rights, and values in all patient-physician-caregiver interactions.
• Recognize that physician accessibility and excellent communication are fundamental to supporting the patient and family caregiver.
• Recognize the value of family caregivers as a source of continuity regarding the patient’s medical and psychosocial history.
• Facilitate end of life adjustments for the family.
• Ensure appropriate boundaries when the caregiver is a health care professional.
• Ensure the caregiver receives appropriate support, referrals, and services.
Our failure to use patient and family-centered care (PFCC) is tied to attitudinal, educational, and organizational barriers. The first attitudinal barrier is the expectation that families will be unreasonable. The second is that families will compromise confidentiality. The third is that physicians are largely unaware of research on the benefits of PFCC. Finally, physicians believe that PFCC is time consuming and costs too much.
Educational barriers include the lack of skills needed for collaboration among professionals, administrators, patients, and families.
Organizational barriers that get in the way of PFCC are the lack of guiding vision, the top-down approach with insufficient effort to build staff commitment; grassroots effort that lacks leadership, commitment, and support; scarce fiscal resources and competing priorities; and the absence of a funded coordinator.
Psychiatric illnesses are chronic medical illnesses. As more people have experiences as patients and caregivers, the pressure to involve family members such as Ms. Stout increases. Where does the resistance to involving family members in patient care come from? There is an unfounded, unspoken fear on the part of health professionals that families want something that the health care provider cannot guarantee – that their relative "will get well and everything will be fine." Health care providers might limit what they say to family members in order "not to upset them." If the family members perceive that they are being brushed off and dismissed, they can develop feelings of apprehension. A small upset or misunderstanding can then unleash repressed feelings, resulting in family members lashing out. When health care teams include the family and develop collaborative relationships with families, the likelihood of this kind of conflict is reduced.
Resistance also comes from the perception that family involvement is not necessary for patient care. Many of the consequences of isolating patients from their family are invisible, such as relationship strain, role changes, and caregiver burden. The reality is that, for patients such as Ms. Stout’s son, his mother’s involvement helps his medical team do a better job of managing his care.
It is time that psychiatry, and specifically the American Psychiatric Association, develop ethical guidelines outlining how to work with families of patients with chronic psychiatric illness. At the very least, we should sign on with other medical specialties by endorsing the American College of Physicians’ ethical guidelines described above. We have lagged behind the rest of medicine by failing to address this important issue.
This column, "Families in Psychiatry," appears regularly in Clinical Psychiatry News, a publication of IMNG Medical Media. Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Ms. Stout is a 58-year-old divorced mother of two. Her eldest son, Paul, aged 35, has cystic fibrosis and is the recipient of a lung transplant. He has several developmental delays, and his comprehension of medicolegal documents becomes quite limited when he is medically ill and on narcotics. His outpatient medical team is aware of this and includes his mother in all treatment decisions.
However, in the hospital, the medical teams do not appreciate his limitations. In the inpatient hospital setting, he does not retain information presented to him. They question his mother’s continual presence and see her as "overinvolved and enmeshed with her adult son." Ms. Stout says that she has to fight with each new physician team to get them to understand that they need to involve her in all her son’s health care decisions. The younger male physicians, especially, identify with Paul.
Paul presents as a well-adjusted young man. He is agreeable, open, and friendly with the staff. Paul has limited social contacts outside of the hospital. Because of his lengthy involvement in the hospital care system, he is comfortable in the hospital and especially enjoys his interaction with the female nurses. He understands basic procedures because they have been repeated so many times. However, he does not understand his complex health care needs. Unless his comprehension is specifically tested, his deficits go unrecognized.
His mother knows the details of his history and is a better resource than the chart. She insists on being present at all times, despite the demands of her other commitments. Each time her son is admitted, she faces scrutiny, and repeatedly has to explain herself and her son’s limitations to each new physician. She finds this situation exhausting and humiliating. She does not understand why her presence cannot be accepted as helpful.
The toll of caregiving
Family caregivers face many physical, emotional, and financial demands that make them vulnerable to stress-related conditions, both physical and psychological. Caregiving affects caregivers’ health, which, in turn, affects their ability to provide care. The Caregiver Health Effects Study demonstrated a strong link between caregiving and mortality risk, finding that elderly caregivers supporting disabled spouses at home were 63% more likely to die within 4 years than noncaregiving elderly spouses (JAMA 1999;282:2215-9). In addition, family caregivers often lack the time and energy to prepare their own meals, exercise, or engage in their own preventive medical care. Physicians must stress the importance of caregiver self-care for the benefit of both the caregiver and the patient, and identify appropriate sources of community support services, such as home health aides, respite, or adult day care.
In 2008, according to Suzanne Mintz, a cofounder of the National Family Caregivers Association, the estimated market value of the family caregivers’ services was $375 billion annually. Almost one-third of the U.S. population provides care for a chronically ill, disabled, or aged family member or friend during any given year and spends an average of 20 hours per week providing care for loved ones. Two-thirds of caregivers are women, and 13% of family caregivers are providing 40 hours of care a week or more.
The American Psychological Association has a "Caregiver Briefcase." The briefcase contains caregiving facts; a practice section with common caregiver problems and interventions; and sections on research, education, and advocacy. The website and its contents are useful for family members as well as professionals.
In addition, the American Psychological Association offers ways for family members to integrate into health care teams. For example, electronic medical records can allow family members access to portions such as the patient’s problem and medication lists and most recent laboratory findings. Family caregivers can provide ongoing, real-time observations about the patient through the portal, as well as share information about what it is like to be a family caregiver. Those secure messages become part of the patient’s permanent medical record.
Shifting patient decision making to family members is a delicate negotiation between the patient’s ability to make independent decisions and the family’s desire to protect the patient from potentially poor decisions. At critical times, the family has to step up and assume decision-making responsibility for the patient.
To help physicians understand the ethics of this process, the American College of Physicians offers guidelines to help the physician know how best to collaborate with the patient and the caregiver (J. Gen. Intern. Med. 2010;25:255-60). These guidelines are endorsed by 10 medical professional societies, including the Society of General Internal Medicine, the American Academy of Neurology, and the American Academy of Hospice and Palliative Medicine.
Ethical guidelines for collaboration
When working with patients, making sure that six factors are met will help us do a better job of ensuring that the relationship with caregivers is productive for all three parties involved. Here is a listing:
• Respect the patient’s dignity, rights, and values in all patient-physician-caregiver interactions.
• Recognize that physician accessibility and excellent communication are fundamental to supporting the patient and family caregiver.
• Recognize the value of family caregivers as a source of continuity regarding the patient’s medical and psychosocial history.
• Facilitate end of life adjustments for the family.
• Ensure appropriate boundaries when the caregiver is a health care professional.
• Ensure the caregiver receives appropriate support, referrals, and services.
Our failure to use patient and family-centered care (PFCC) is tied to attitudinal, educational, and organizational barriers. The first attitudinal barrier is the expectation that families will be unreasonable. The second is that families will compromise confidentiality. The third is that physicians are largely unaware of research on the benefits of PFCC. Finally, physicians believe that PFCC is time consuming and costs too much.
Educational barriers include the lack of skills needed for collaboration among professionals, administrators, patients, and families.
Organizational barriers that get in the way of PFCC are the lack of guiding vision, the top-down approach with insufficient effort to build staff commitment; grassroots effort that lacks leadership, commitment, and support; scarce fiscal resources and competing priorities; and the absence of a funded coordinator.
Psychiatric illnesses are chronic medical illnesses. As more people have experiences as patients and caregivers, the pressure to involve family members such as Ms. Stout increases. Where does the resistance to involving family members in patient care come from? There is an unfounded, unspoken fear on the part of health professionals that families want something that the health care provider cannot guarantee – that their relative "will get well and everything will be fine." Health care providers might limit what they say to family members in order "not to upset them." If the family members perceive that they are being brushed off and dismissed, they can develop feelings of apprehension. A small upset or misunderstanding can then unleash repressed feelings, resulting in family members lashing out. When health care teams include the family and develop collaborative relationships with families, the likelihood of this kind of conflict is reduced.
Resistance also comes from the perception that family involvement is not necessary for patient care. Many of the consequences of isolating patients from their family are invisible, such as relationship strain, role changes, and caregiver burden. The reality is that, for patients such as Ms. Stout’s son, his mother’s involvement helps his medical team do a better job of managing his care.
It is time that psychiatry, and specifically the American Psychiatric Association, develop ethical guidelines outlining how to work with families of patients with chronic psychiatric illness. At the very least, we should sign on with other medical specialties by endorsing the American College of Physicians’ ethical guidelines described above. We have lagged behind the rest of medicine by failing to address this important issue.
This column, "Families in Psychiatry," appears regularly in Clinical Psychiatry News, a publication of IMNG Medical Media. Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013).
Homage to Dr. Murray Bowen
Dr. Denis Fiallos Montero, who describes himself as "an old-time psychiatrist" who grew up during the Family Therapy days, wrote to me to point out "a great omission" in my recent discussion about some of the pioneers in our field ("Dr. Minuchin and the Ashtray," October 2012, p. 4).
Whom did I fail to mention? The late Dr. Murray Bowen.
Dr. Bowen was the originator of the American Family Therapy Association and served as the group’s first president, from 1978 to 1982. (See the Bowen Center website for details of his enduring legacy.)
This column is dedicated to these two gentlemen.
Individuation as a concept
The spirit of Murray Bowen sits in the corner at every family therapist’s family gathering and reminds us about triangulation! He told us clearly that one of the main tasks of individuation is finding the right level of differentiation from our parents.
Concepts of emotional fusion and emotional cutoff are helpful at this time of year, as many of us struggle with conflicted thoughts and feelings about our families of origin.
At one end of the differentiation spectrum is emotional fusion (overly close fused relationships); at the other end of the spectrum is emotional cutoff (disconnection between family members or refusal to engage with certain family members).
Bowen described emotional cutoffs as "the natural mechanisms people use to counter high anxiety or high emotional fusion that arise from unresolved issues with our family of origin" (Family Evaluation, New York: W.W. Norton and Co., 1988). He and his longtime colleague Dr. Michael E. Kerr noted that unresolved family issues get passed down through the generations, with successive generations being affected by seemingly mysterious emotional patterns and behaviors.
Common laments at this time of year are "I feel like a child when I go home," "I feel guilty when I go home," and "I want to take care of those parents of mine and make them do the right thing!" Or we think things like: "I feel angry that my parents do not understand or approve of me." Friends give advice: "Just go home for a short time. Try to avoid sensitive issues. Try to not get into things with them, and then you all will get along."
Gritting your teeth and powering through a family visit is exhausting. However, what is the alternative?
Bowen thought that to develop a healthy sense of self, you must be in good relation with your family of origin, and that all adults in the family should be in "comfortable emotional contact." A self-report scale called the Differentiation of Self Inventory (DSI) is based on Bowen’s theory, and measures emotional functioning, intimacy, and autonomy in interpersonal relationships.
Its subscales assess interpersonal (i.e., fusion and emotional cutoff) and intrapsychic dimensions of differentiation problems (i.e., emotional reactivity and difficulty taking an "I" position) (J. Counseling Psychol. 1998;45:235-46). The DSI has questions like: "I would never consider turning to any of my family members for emotional support," and "I often feel unsure when others are not around to help me make a decision."
Personal connections to theory
Bowen’s theories are helpful to me in thinking about my family of origin. I recently returned to Scotland to visit my Aunt Charlotte. My aunt is the living embodiment of an emotional cutoff.
The original family insult occurred before she was born. Her beloved brother Charlie, the first-born son, was killed in a car accident when he was a young child. Charlotte was the "replacement child," prescribed by the general practitioner to help my grandmother recover from the grief and loss of her son.
Of course, this was not a successful prescription, and the grief and sense of loss continued. However, more tragically, Aunt Charlotte’s mere presence triggered feelings of grief, anger, and guilt for her parents and sister.
Aunt Charlotte was the weakest and most sensitive member of our family. She suffered from asthma and, as an adult, was the victim of a car accident that left her cognitively impaired. (No one seemed to think it was ironic that the accident heightened the family’s anger and distaste for her, rather than provoke sympathy that she could now no longer live a productive life.)
Mentioning Aunt Charlotte’s name in our household raised everyone’s blood pressure. As a young teenager, I was acutely aware of the "unfairness" of the family’s responses to her. Although we all knew about Charlie’s death, we had little understanding of the connection between his death and how Aunt Charlotte was perceived.
I do remember the strong negative feelings in the house at holiday times, but neither my family nor I, as an adolescent, understood what was being enacted. As an adult, I have come to understand that the grief, anger, and emotional tension experienced by Charlie’s death were shifted and projected onto Aunt Charlotte.
Encouraged to seek a life of her own, she eventually moved away, to a small town, close to where her mother had been born and raised. She enjoyed volunteering at the house where Mary, Queen of Scots, had lived, a woman who herself was one of Scotland’s most tragic figures. The best way the family could function, it seemed, was to use emotional cutoff.
As an adult, I have been able to go back and talk with her and her friends, discussing the grief and trauma in the family. Understanding that an emotional cutoff was used to manage the unbearable emotional tensions in the family brings understanding and a way to think about what happened over the years. How much better if her parents and sister had been able to understand this, too!
Forerunner of the genogram
Bowen focused on helping family members develop emotional objectivity about their family relationships. Bowen would draw a family diagram, the forerunner of the genogram, and talk through the family influences on each member. His goal was to help the patient develop emotional object and a greater intellectual understanding about their family of origin. He wanted to help the patient understand the emotional tasks of differentiation.
In the case of Aunt Charlotte, therapy might not have been able to restore her to the family, but at least therapy would have given her and our family a deeper appreciation of the impact of trauma on family relationships and subsequent generations.
Healthy relationships with one’s family of origin mean having the right amount of differentiation. You know you have it when you can relate to your family members without regressing to the "child" position or the "parent" position – and when going home feels good, not fraught with angst, anger, or other strong and difficult emotions.
However, if it still doesn’t feel good because of unresolved problems, it is still possible to develop greater emotional objectivity and a deeper intellectual understanding.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She has been a member of the Association of Family Psychiatrists since 2002 and currently serves as the organization’s treasurer. In addition, she is the coauthor of two books on working with families and is the author of numerous articles on this topic.
Dr. Denis Fiallos Montero, who describes himself as "an old-time psychiatrist" who grew up during the Family Therapy days, wrote to me to point out "a great omission" in my recent discussion about some of the pioneers in our field ("Dr. Minuchin and the Ashtray," October 2012, p. 4).
Whom did I fail to mention? The late Dr. Murray Bowen.
Dr. Bowen was the originator of the American Family Therapy Association and served as the group’s first president, from 1978 to 1982. (See the Bowen Center website for details of his enduring legacy.)
This column is dedicated to these two gentlemen.
Individuation as a concept
The spirit of Murray Bowen sits in the corner at every family therapist’s family gathering and reminds us about triangulation! He told us clearly that one of the main tasks of individuation is finding the right level of differentiation from our parents.
Concepts of emotional fusion and emotional cutoff are helpful at this time of year, as many of us struggle with conflicted thoughts and feelings about our families of origin.
At one end of the differentiation spectrum is emotional fusion (overly close fused relationships); at the other end of the spectrum is emotional cutoff (disconnection between family members or refusal to engage with certain family members).
Bowen described emotional cutoffs as "the natural mechanisms people use to counter high anxiety or high emotional fusion that arise from unresolved issues with our family of origin" (Family Evaluation, New York: W.W. Norton and Co., 1988). He and his longtime colleague Dr. Michael E. Kerr noted that unresolved family issues get passed down through the generations, with successive generations being affected by seemingly mysterious emotional patterns and behaviors.
Common laments at this time of year are "I feel like a child when I go home," "I feel guilty when I go home," and "I want to take care of those parents of mine and make them do the right thing!" Or we think things like: "I feel angry that my parents do not understand or approve of me." Friends give advice: "Just go home for a short time. Try to avoid sensitive issues. Try to not get into things with them, and then you all will get along."
Gritting your teeth and powering through a family visit is exhausting. However, what is the alternative?
Bowen thought that to develop a healthy sense of self, you must be in good relation with your family of origin, and that all adults in the family should be in "comfortable emotional contact." A self-report scale called the Differentiation of Self Inventory (DSI) is based on Bowen’s theory, and measures emotional functioning, intimacy, and autonomy in interpersonal relationships.
Its subscales assess interpersonal (i.e., fusion and emotional cutoff) and intrapsychic dimensions of differentiation problems (i.e., emotional reactivity and difficulty taking an "I" position) (J. Counseling Psychol. 1998;45:235-46). The DSI has questions like: "I would never consider turning to any of my family members for emotional support," and "I often feel unsure when others are not around to help me make a decision."
Personal connections to theory
Bowen’s theories are helpful to me in thinking about my family of origin. I recently returned to Scotland to visit my Aunt Charlotte. My aunt is the living embodiment of an emotional cutoff.
The original family insult occurred before she was born. Her beloved brother Charlie, the first-born son, was killed in a car accident when he was a young child. Charlotte was the "replacement child," prescribed by the general practitioner to help my grandmother recover from the grief and loss of her son.
Of course, this was not a successful prescription, and the grief and sense of loss continued. However, more tragically, Aunt Charlotte’s mere presence triggered feelings of grief, anger, and guilt for her parents and sister.
Aunt Charlotte was the weakest and most sensitive member of our family. She suffered from asthma and, as an adult, was the victim of a car accident that left her cognitively impaired. (No one seemed to think it was ironic that the accident heightened the family’s anger and distaste for her, rather than provoke sympathy that she could now no longer live a productive life.)
Mentioning Aunt Charlotte’s name in our household raised everyone’s blood pressure. As a young teenager, I was acutely aware of the "unfairness" of the family’s responses to her. Although we all knew about Charlie’s death, we had little understanding of the connection between his death and how Aunt Charlotte was perceived.
I do remember the strong negative feelings in the house at holiday times, but neither my family nor I, as an adolescent, understood what was being enacted. As an adult, I have come to understand that the grief, anger, and emotional tension experienced by Charlie’s death were shifted and projected onto Aunt Charlotte.
Encouraged to seek a life of her own, she eventually moved away, to a small town, close to where her mother had been born and raised. She enjoyed volunteering at the house where Mary, Queen of Scots, had lived, a woman who herself was one of Scotland’s most tragic figures. The best way the family could function, it seemed, was to use emotional cutoff.
As an adult, I have been able to go back and talk with her and her friends, discussing the grief and trauma in the family. Understanding that an emotional cutoff was used to manage the unbearable emotional tensions in the family brings understanding and a way to think about what happened over the years. How much better if her parents and sister had been able to understand this, too!
Forerunner of the genogram
Bowen focused on helping family members develop emotional objectivity about their family relationships. Bowen would draw a family diagram, the forerunner of the genogram, and talk through the family influences on each member. His goal was to help the patient develop emotional object and a greater intellectual understanding about their family of origin. He wanted to help the patient understand the emotional tasks of differentiation.
In the case of Aunt Charlotte, therapy might not have been able to restore her to the family, but at least therapy would have given her and our family a deeper appreciation of the impact of trauma on family relationships and subsequent generations.
Healthy relationships with one’s family of origin mean having the right amount of differentiation. You know you have it when you can relate to your family members without regressing to the "child" position or the "parent" position – and when going home feels good, not fraught with angst, anger, or other strong and difficult emotions.
However, if it still doesn’t feel good because of unresolved problems, it is still possible to develop greater emotional objectivity and a deeper intellectual understanding.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She has been a member of the Association of Family Psychiatrists since 2002 and currently serves as the organization’s treasurer. In addition, she is the coauthor of two books on working with families and is the author of numerous articles on this topic.
Dr. Denis Fiallos Montero, who describes himself as "an old-time psychiatrist" who grew up during the Family Therapy days, wrote to me to point out "a great omission" in my recent discussion about some of the pioneers in our field ("Dr. Minuchin and the Ashtray," October 2012, p. 4).
Whom did I fail to mention? The late Dr. Murray Bowen.
Dr. Bowen was the originator of the American Family Therapy Association and served as the group’s first president, from 1978 to 1982. (See the Bowen Center website for details of his enduring legacy.)
This column is dedicated to these two gentlemen.
Individuation as a concept
The spirit of Murray Bowen sits in the corner at every family therapist’s family gathering and reminds us about triangulation! He told us clearly that one of the main tasks of individuation is finding the right level of differentiation from our parents.
Concepts of emotional fusion and emotional cutoff are helpful at this time of year, as many of us struggle with conflicted thoughts and feelings about our families of origin.
At one end of the differentiation spectrum is emotional fusion (overly close fused relationships); at the other end of the spectrum is emotional cutoff (disconnection between family members or refusal to engage with certain family members).
Bowen described emotional cutoffs as "the natural mechanisms people use to counter high anxiety or high emotional fusion that arise from unresolved issues with our family of origin" (Family Evaluation, New York: W.W. Norton and Co., 1988). He and his longtime colleague Dr. Michael E. Kerr noted that unresolved family issues get passed down through the generations, with successive generations being affected by seemingly mysterious emotional patterns and behaviors.
Common laments at this time of year are "I feel like a child when I go home," "I feel guilty when I go home," and "I want to take care of those parents of mine and make them do the right thing!" Or we think things like: "I feel angry that my parents do not understand or approve of me." Friends give advice: "Just go home for a short time. Try to avoid sensitive issues. Try to not get into things with them, and then you all will get along."
Gritting your teeth and powering through a family visit is exhausting. However, what is the alternative?
Bowen thought that to develop a healthy sense of self, you must be in good relation with your family of origin, and that all adults in the family should be in "comfortable emotional contact." A self-report scale called the Differentiation of Self Inventory (DSI) is based on Bowen’s theory, and measures emotional functioning, intimacy, and autonomy in interpersonal relationships.
Its subscales assess interpersonal (i.e., fusion and emotional cutoff) and intrapsychic dimensions of differentiation problems (i.e., emotional reactivity and difficulty taking an "I" position) (J. Counseling Psychol. 1998;45:235-46). The DSI has questions like: "I would never consider turning to any of my family members for emotional support," and "I often feel unsure when others are not around to help me make a decision."
Personal connections to theory
Bowen’s theories are helpful to me in thinking about my family of origin. I recently returned to Scotland to visit my Aunt Charlotte. My aunt is the living embodiment of an emotional cutoff.
The original family insult occurred before she was born. Her beloved brother Charlie, the first-born son, was killed in a car accident when he was a young child. Charlotte was the "replacement child," prescribed by the general practitioner to help my grandmother recover from the grief and loss of her son.
Of course, this was not a successful prescription, and the grief and sense of loss continued. However, more tragically, Aunt Charlotte’s mere presence triggered feelings of grief, anger, and guilt for her parents and sister.
Aunt Charlotte was the weakest and most sensitive member of our family. She suffered from asthma and, as an adult, was the victim of a car accident that left her cognitively impaired. (No one seemed to think it was ironic that the accident heightened the family’s anger and distaste for her, rather than provoke sympathy that she could now no longer live a productive life.)
Mentioning Aunt Charlotte’s name in our household raised everyone’s blood pressure. As a young teenager, I was acutely aware of the "unfairness" of the family’s responses to her. Although we all knew about Charlie’s death, we had little understanding of the connection between his death and how Aunt Charlotte was perceived.
I do remember the strong negative feelings in the house at holiday times, but neither my family nor I, as an adolescent, understood what was being enacted. As an adult, I have come to understand that the grief, anger, and emotional tension experienced by Charlie’s death were shifted and projected onto Aunt Charlotte.
Encouraged to seek a life of her own, she eventually moved away, to a small town, close to where her mother had been born and raised. She enjoyed volunteering at the house where Mary, Queen of Scots, had lived, a woman who herself was one of Scotland’s most tragic figures. The best way the family could function, it seemed, was to use emotional cutoff.
As an adult, I have been able to go back and talk with her and her friends, discussing the grief and trauma in the family. Understanding that an emotional cutoff was used to manage the unbearable emotional tensions in the family brings understanding and a way to think about what happened over the years. How much better if her parents and sister had been able to understand this, too!
Forerunner of the genogram
Bowen focused on helping family members develop emotional objectivity about their family relationships. Bowen would draw a family diagram, the forerunner of the genogram, and talk through the family influences on each member. His goal was to help the patient develop emotional object and a greater intellectual understanding about their family of origin. He wanted to help the patient understand the emotional tasks of differentiation.
In the case of Aunt Charlotte, therapy might not have been able to restore her to the family, but at least therapy would have given her and our family a deeper appreciation of the impact of trauma on family relationships and subsequent generations.
Healthy relationships with one’s family of origin mean having the right amount of differentiation. You know you have it when you can relate to your family members without regressing to the "child" position or the "parent" position – and when going home feels good, not fraught with angst, anger, or other strong and difficult emotions.
However, if it still doesn’t feel good because of unresolved problems, it is still possible to develop greater emotional objectivity and a deeper intellectual understanding.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She has been a member of the Association of Family Psychiatrists since 2002 and currently serves as the organization’s treasurer. In addition, she is the coauthor of two books on working with families and is the author of numerous articles on this topic.
Life in Romanian village offers lessons for our patients
BREB, ROMANIA – While strolling through this village in the Maramures region in the northwest corner of Romania, I ask Ileana, "How many live in this village?" Ileana has just come home from high school in the nearest town and is wearing brightly colored sneakers, blue jeans, and a pink sweatshirt with the word "LOVE" emblazed in sparkles across her chest. She is touring us proudly around her village.
"400."
"400 people?"
"No, 400 families."
"How many in each family?"
"About six or seven."
On the large ornate wooden gate to the family homestead is the inscription: "Familie Hermann." All seven members of the Hermann family live in a three-room traditional wooden house. The house has a large porch, where the family eats, works, and sometimes sleeps in the warm weather.
Maria, the 82-year-old grandmother, sits outside the gate on a small bench and watches the villagers stroll home from the fields with scythes and rakes on their shoulders. She welcomes her daughter and son-in-law back home. It is spring, and the villagers are cleaning the fields in preparation for the summer grass growing. In the fall, they will harvest the grass to feed their animals throughout the winter.
On the porch, in the quiet of a late afternoon, as 9-year-old Ioanna is doing her homework, her mother, Raluca, works on the intricacies of beading the border of Ioanna’s traditional costume to be worn on Easter Sunday. Ioanna watches her mother pin the black velvet jacket to her skirt and load the needle with the gold beads to make the stems for the purple and red flowers. She sees how to turn the green rows into leaves. She shows her mother her school work, as equally neat and carefully calligraphied as her mother’s beading. Concern for accuracy and aesthetics are the skills and values passed down through the generations.
Maria comes in from the gate and resumes shelling beans on the front porch. She doesn’t do as much work in the fields anymore. Instead, she sweeps the house, tends to the flower garden, and helps with the two children. Maria takes the clothes down from the clothesline that stretches across the front of the porch. These handmade, intricately stitched works of art have been washed in preparation for Easter.
Maria shows us the gown she will wear at her funeral. She wove the linen, and smocked the neck and wrists with traditional village colors. She is proud of her work, and we admire it. She takes her gown inside, along with all the other freshly laundered white blouses that men and women will wear during the traditional events throughout the year.
After Easter, when the weather warms, most of the village will make the pilgrimage up the mountain accompanying the shepherds taking the sheep to summer grazing. The milking of the sheep is a defining village event, and precise measures are recorded in a book or on a stick to indicate each person’s anticipated portion of future milkings. This is Stina, a serious celebration, and the villagers wear traditional dress for the feasting, drinking, and dancing.
Life in rural villages is physically hard, and family and communal living are not idyllic. There is no privacy in the village, perhaps no secrets.
There is no privileging of the individual over the family. The family functions as a unit, getting work done by the seasons, so the family can eat throughout the year. The sense of belonging is irrefutable.
There is room for individual pride, however, and this is expressed as skill in raking a straight row, making the best plum brandy, wood carving, and doing embroidery. Everyone has an opinion on which family is the best at their craft in the village. The Hermann family is recognized for their skill in textiles – particularly their embroidery.
The village has its characters: the most devout, the "bad boy," the lazy person, and the man who can’t hold his liquor. This man, the village drunk, frequently makes a trip to the psychiatric hospital in the town of Sighetu Marmatieti, when he gets out of hand. After a few weeks, he comes home quieter, and his good behavior will last for the best part of a year. There is no physician or nurse in the village, only a veterinarian who visits, when called, to care for the animals.
The darker stories of the village lie hidden, because for now, it is early spring, and the village flows with optimism, celebration, and courtship. The white, hand-crafted blouses manifest the feelings of anticipation as they billow and dance on each clothesline throughout the village. Belonging to the village means feeling the seasons unfold intuitively. These feelings sustain and nourish the village families throughout their lives.
Outside of the village, in the "real world," we try to create a sense of belonging. As a country of immigrants, we in America have sense of belonging that is scattered. Still, connecting with our past is too often beyond our grasp. What is belonging? What are its components?
Ways to think about belonging
Studies on belonging extend across many disciplines: psychoanalysis, attachment psychology, social and cultural studies to philosophy. How does a family psychiatrist think about belonging? What aspects of belonging can be incorporated into psychiatric care?
An unmet need for belonging leads to loneliness and lower life satisfaction. This finding came from a study of 436 participants from the Australian Unity Wellbeing database who completed several measurements, including the Need to Belong Scale according to David Mellor, Ph.D., and his colleagues(Pers. Individ. Dif. 2008;45:213-8). Dr. Vincenzo Di Nicola, a psychiatrist who has written extensively about family relationships, also has offered valuable perspective on belongingness: "Belonging is a way of rethinking relational being, how we define mental health, how we understand the expression of its vicissitudes, and how we organize care and healing for sufferers. To do this, we need to recognize how belonging is experienced and negotiated, free of the constraints of our habitual patterns of practice and thought, to imagine belonging without borders for settlers, sojourners, and travelers in the 21st century."
Belongingness traditionally has been seen as a core of family life. If your values are different from those of your family, if you have moved from the village to the city and don’t want to be a farmer, what values do you uphold? Do you now have a new set of people and values? Do you belong to a group/club/school? Belonging to a guild or religious order means that the guild or order becomes your new family. However, belongingness is more transient and a less substantial part of life, as people change jobs and careers, get divorced and remarried, move to other countries.
Who serves as the family for people with psychiatric illness? In a recent study, people with serious mental illness were interviewed and asked about the "communities" to which they belonged (Psychiatr. Serv. [doi: 10.1176/appi.ps.201200235]). The researchers found four "patterns of experience" that made up communities for the respondents. Communities were places where people with mental illness could receive help, especially in times of vulnerability.
In addition, communities were places to manage risk and minimize the anxiety felt in public setting by people with mental illness. The stigma experienced in the general community or even within their families led many respondents to identify more strongly with peers who had mental illness.
Communities also were seen as places where those with serious mental illness could "give back" and help others. So perhaps, in the same way as these respondents defined belongingness for themselves, we can define belongingness for all our patients.
Several components must be satisfied for a person to have a sense of belongingness.
• A community in which the person’s beliefs and values are upheld as sacred (meaningfulness).
• Rituals that bring people together and support the meaningfulness of their lives (meaningfulness).
• People who provide emotional and practical support for others (attachment).
• People who allow others to provide them with support (sense of self-efficacy).
• Generational transmission of skills, crafts, values, and beliefs (generativity).
A sense of place is another component that has been associated with a sense of belonging. After the Boston Marathon bombings, some people affirmed that their sense of belonging was consolidated by that event. For others, a sense of belonging becomes fixed in their sense of tragedy as a victim of an event. We see many patients with posttraumatic stress disorder who have been bound by the traumatizing event(s), and who find it difficult or impossible to move beyond that experience.
For Americans, perhaps the notion of "family values" can be parsed to include the idea and study of belongingness. Understanding what belongingness encompasses can help us discuss relational being with our patients. Where do you find that sense of belonging? For Ioanna, her sense of belonging is felt in the seasonal ebb and flow of village life. Her sense of belonging shows in her skill as she works with her crafts with her hands. Breb belongs to her, even as it opens its large wooden doors to the world.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013.
BREB, ROMANIA – While strolling through this village in the Maramures region in the northwest corner of Romania, I ask Ileana, "How many live in this village?" Ileana has just come home from high school in the nearest town and is wearing brightly colored sneakers, blue jeans, and a pink sweatshirt with the word "LOVE" emblazed in sparkles across her chest. She is touring us proudly around her village.
"400."
"400 people?"
"No, 400 families."
"How many in each family?"
"About six or seven."
On the large ornate wooden gate to the family homestead is the inscription: "Familie Hermann." All seven members of the Hermann family live in a three-room traditional wooden house. The house has a large porch, where the family eats, works, and sometimes sleeps in the warm weather.
Maria, the 82-year-old grandmother, sits outside the gate on a small bench and watches the villagers stroll home from the fields with scythes and rakes on their shoulders. She welcomes her daughter and son-in-law back home. It is spring, and the villagers are cleaning the fields in preparation for the summer grass growing. In the fall, they will harvest the grass to feed their animals throughout the winter.
On the porch, in the quiet of a late afternoon, as 9-year-old Ioanna is doing her homework, her mother, Raluca, works on the intricacies of beading the border of Ioanna’s traditional costume to be worn on Easter Sunday. Ioanna watches her mother pin the black velvet jacket to her skirt and load the needle with the gold beads to make the stems for the purple and red flowers. She sees how to turn the green rows into leaves. She shows her mother her school work, as equally neat and carefully calligraphied as her mother’s beading. Concern for accuracy and aesthetics are the skills and values passed down through the generations.
Maria comes in from the gate and resumes shelling beans on the front porch. She doesn’t do as much work in the fields anymore. Instead, she sweeps the house, tends to the flower garden, and helps with the two children. Maria takes the clothes down from the clothesline that stretches across the front of the porch. These handmade, intricately stitched works of art have been washed in preparation for Easter.
Maria shows us the gown she will wear at her funeral. She wove the linen, and smocked the neck and wrists with traditional village colors. She is proud of her work, and we admire it. She takes her gown inside, along with all the other freshly laundered white blouses that men and women will wear during the traditional events throughout the year.
After Easter, when the weather warms, most of the village will make the pilgrimage up the mountain accompanying the shepherds taking the sheep to summer grazing. The milking of the sheep is a defining village event, and precise measures are recorded in a book or on a stick to indicate each person’s anticipated portion of future milkings. This is Stina, a serious celebration, and the villagers wear traditional dress for the feasting, drinking, and dancing.
Life in rural villages is physically hard, and family and communal living are not idyllic. There is no privacy in the village, perhaps no secrets.
There is no privileging of the individual over the family. The family functions as a unit, getting work done by the seasons, so the family can eat throughout the year. The sense of belonging is irrefutable.
There is room for individual pride, however, and this is expressed as skill in raking a straight row, making the best plum brandy, wood carving, and doing embroidery. Everyone has an opinion on which family is the best at their craft in the village. The Hermann family is recognized for their skill in textiles – particularly their embroidery.
The village has its characters: the most devout, the "bad boy," the lazy person, and the man who can’t hold his liquor. This man, the village drunk, frequently makes a trip to the psychiatric hospital in the town of Sighetu Marmatieti, when he gets out of hand. After a few weeks, he comes home quieter, and his good behavior will last for the best part of a year. There is no physician or nurse in the village, only a veterinarian who visits, when called, to care for the animals.
The darker stories of the village lie hidden, because for now, it is early spring, and the village flows with optimism, celebration, and courtship. The white, hand-crafted blouses manifest the feelings of anticipation as they billow and dance on each clothesline throughout the village. Belonging to the village means feeling the seasons unfold intuitively. These feelings sustain and nourish the village families throughout their lives.
Outside of the village, in the "real world," we try to create a sense of belonging. As a country of immigrants, we in America have sense of belonging that is scattered. Still, connecting with our past is too often beyond our grasp. What is belonging? What are its components?
Ways to think about belonging
Studies on belonging extend across many disciplines: psychoanalysis, attachment psychology, social and cultural studies to philosophy. How does a family psychiatrist think about belonging? What aspects of belonging can be incorporated into psychiatric care?
An unmet need for belonging leads to loneliness and lower life satisfaction. This finding came from a study of 436 participants from the Australian Unity Wellbeing database who completed several measurements, including the Need to Belong Scale according to David Mellor, Ph.D., and his colleagues(Pers. Individ. Dif. 2008;45:213-8). Dr. Vincenzo Di Nicola, a psychiatrist who has written extensively about family relationships, also has offered valuable perspective on belongingness: "Belonging is a way of rethinking relational being, how we define mental health, how we understand the expression of its vicissitudes, and how we organize care and healing for sufferers. To do this, we need to recognize how belonging is experienced and negotiated, free of the constraints of our habitual patterns of practice and thought, to imagine belonging without borders for settlers, sojourners, and travelers in the 21st century."
Belongingness traditionally has been seen as a core of family life. If your values are different from those of your family, if you have moved from the village to the city and don’t want to be a farmer, what values do you uphold? Do you now have a new set of people and values? Do you belong to a group/club/school? Belonging to a guild or religious order means that the guild or order becomes your new family. However, belongingness is more transient and a less substantial part of life, as people change jobs and careers, get divorced and remarried, move to other countries.
Who serves as the family for people with psychiatric illness? In a recent study, people with serious mental illness were interviewed and asked about the "communities" to which they belonged (Psychiatr. Serv. [doi: 10.1176/appi.ps.201200235]). The researchers found four "patterns of experience" that made up communities for the respondents. Communities were places where people with mental illness could receive help, especially in times of vulnerability.
In addition, communities were places to manage risk and minimize the anxiety felt in public setting by people with mental illness. The stigma experienced in the general community or even within their families led many respondents to identify more strongly with peers who had mental illness.
Communities also were seen as places where those with serious mental illness could "give back" and help others. So perhaps, in the same way as these respondents defined belongingness for themselves, we can define belongingness for all our patients.
Several components must be satisfied for a person to have a sense of belongingness.
• A community in which the person’s beliefs and values are upheld as sacred (meaningfulness).
• Rituals that bring people together and support the meaningfulness of their lives (meaningfulness).
• People who provide emotional and practical support for others (attachment).
• People who allow others to provide them with support (sense of self-efficacy).
• Generational transmission of skills, crafts, values, and beliefs (generativity).
A sense of place is another component that has been associated with a sense of belonging. After the Boston Marathon bombings, some people affirmed that their sense of belonging was consolidated by that event. For others, a sense of belonging becomes fixed in their sense of tragedy as a victim of an event. We see many patients with posttraumatic stress disorder who have been bound by the traumatizing event(s), and who find it difficult or impossible to move beyond that experience.
For Americans, perhaps the notion of "family values" can be parsed to include the idea and study of belongingness. Understanding what belongingness encompasses can help us discuss relational being with our patients. Where do you find that sense of belonging? For Ioanna, her sense of belonging is felt in the seasonal ebb and flow of village life. Her sense of belonging shows in her skill as she works with her crafts with her hands. Breb belongs to her, even as it opens its large wooden doors to the world.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013.
BREB, ROMANIA – While strolling through this village in the Maramures region in the northwest corner of Romania, I ask Ileana, "How many live in this village?" Ileana has just come home from high school in the nearest town and is wearing brightly colored sneakers, blue jeans, and a pink sweatshirt with the word "LOVE" emblazed in sparkles across her chest. She is touring us proudly around her village.
"400."
"400 people?"
"No, 400 families."
"How many in each family?"
"About six or seven."
On the large ornate wooden gate to the family homestead is the inscription: "Familie Hermann." All seven members of the Hermann family live in a three-room traditional wooden house. The house has a large porch, where the family eats, works, and sometimes sleeps in the warm weather.
Maria, the 82-year-old grandmother, sits outside the gate on a small bench and watches the villagers stroll home from the fields with scythes and rakes on their shoulders. She welcomes her daughter and son-in-law back home. It is spring, and the villagers are cleaning the fields in preparation for the summer grass growing. In the fall, they will harvest the grass to feed their animals throughout the winter.
On the porch, in the quiet of a late afternoon, as 9-year-old Ioanna is doing her homework, her mother, Raluca, works on the intricacies of beading the border of Ioanna’s traditional costume to be worn on Easter Sunday. Ioanna watches her mother pin the black velvet jacket to her skirt and load the needle with the gold beads to make the stems for the purple and red flowers. She sees how to turn the green rows into leaves. She shows her mother her school work, as equally neat and carefully calligraphied as her mother’s beading. Concern for accuracy and aesthetics are the skills and values passed down through the generations.
Maria comes in from the gate and resumes shelling beans on the front porch. She doesn’t do as much work in the fields anymore. Instead, she sweeps the house, tends to the flower garden, and helps with the two children. Maria takes the clothes down from the clothesline that stretches across the front of the porch. These handmade, intricately stitched works of art have been washed in preparation for Easter.
Maria shows us the gown she will wear at her funeral. She wove the linen, and smocked the neck and wrists with traditional village colors. She is proud of her work, and we admire it. She takes her gown inside, along with all the other freshly laundered white blouses that men and women will wear during the traditional events throughout the year.
After Easter, when the weather warms, most of the village will make the pilgrimage up the mountain accompanying the shepherds taking the sheep to summer grazing. The milking of the sheep is a defining village event, and precise measures are recorded in a book or on a stick to indicate each person’s anticipated portion of future milkings. This is Stina, a serious celebration, and the villagers wear traditional dress for the feasting, drinking, and dancing.
Life in rural villages is physically hard, and family and communal living are not idyllic. There is no privacy in the village, perhaps no secrets.
There is no privileging of the individual over the family. The family functions as a unit, getting work done by the seasons, so the family can eat throughout the year. The sense of belonging is irrefutable.
There is room for individual pride, however, and this is expressed as skill in raking a straight row, making the best plum brandy, wood carving, and doing embroidery. Everyone has an opinion on which family is the best at their craft in the village. The Hermann family is recognized for their skill in textiles – particularly their embroidery.
The village has its characters: the most devout, the "bad boy," the lazy person, and the man who can’t hold his liquor. This man, the village drunk, frequently makes a trip to the psychiatric hospital in the town of Sighetu Marmatieti, when he gets out of hand. After a few weeks, he comes home quieter, and his good behavior will last for the best part of a year. There is no physician or nurse in the village, only a veterinarian who visits, when called, to care for the animals.
The darker stories of the village lie hidden, because for now, it is early spring, and the village flows with optimism, celebration, and courtship. The white, hand-crafted blouses manifest the feelings of anticipation as they billow and dance on each clothesline throughout the village. Belonging to the village means feeling the seasons unfold intuitively. These feelings sustain and nourish the village families throughout their lives.
Outside of the village, in the "real world," we try to create a sense of belonging. As a country of immigrants, we in America have sense of belonging that is scattered. Still, connecting with our past is too often beyond our grasp. What is belonging? What are its components?
Ways to think about belonging
Studies on belonging extend across many disciplines: psychoanalysis, attachment psychology, social and cultural studies to philosophy. How does a family psychiatrist think about belonging? What aspects of belonging can be incorporated into psychiatric care?
An unmet need for belonging leads to loneliness and lower life satisfaction. This finding came from a study of 436 participants from the Australian Unity Wellbeing database who completed several measurements, including the Need to Belong Scale according to David Mellor, Ph.D., and his colleagues(Pers. Individ. Dif. 2008;45:213-8). Dr. Vincenzo Di Nicola, a psychiatrist who has written extensively about family relationships, also has offered valuable perspective on belongingness: "Belonging is a way of rethinking relational being, how we define mental health, how we understand the expression of its vicissitudes, and how we organize care and healing for sufferers. To do this, we need to recognize how belonging is experienced and negotiated, free of the constraints of our habitual patterns of practice and thought, to imagine belonging without borders for settlers, sojourners, and travelers in the 21st century."
Belongingness traditionally has been seen as a core of family life. If your values are different from those of your family, if you have moved from the village to the city and don’t want to be a farmer, what values do you uphold? Do you now have a new set of people and values? Do you belong to a group/club/school? Belonging to a guild or religious order means that the guild or order becomes your new family. However, belongingness is more transient and a less substantial part of life, as people change jobs and careers, get divorced and remarried, move to other countries.
Who serves as the family for people with psychiatric illness? In a recent study, people with serious mental illness were interviewed and asked about the "communities" to which they belonged (Psychiatr. Serv. [doi: 10.1176/appi.ps.201200235]). The researchers found four "patterns of experience" that made up communities for the respondents. Communities were places where people with mental illness could receive help, especially in times of vulnerability.
In addition, communities were places to manage risk and minimize the anxiety felt in public setting by people with mental illness. The stigma experienced in the general community or even within their families led many respondents to identify more strongly with peers who had mental illness.
Communities also were seen as places where those with serious mental illness could "give back" and help others. So perhaps, in the same way as these respondents defined belongingness for themselves, we can define belongingness for all our patients.
Several components must be satisfied for a person to have a sense of belongingness.
• A community in which the person’s beliefs and values are upheld as sacred (meaningfulness).
• Rituals that bring people together and support the meaningfulness of their lives (meaningfulness).
• People who provide emotional and practical support for others (attachment).
• People who allow others to provide them with support (sense of self-efficacy).
• Generational transmission of skills, crafts, values, and beliefs (generativity).
A sense of place is another component that has been associated with a sense of belonging. After the Boston Marathon bombings, some people affirmed that their sense of belonging was consolidated by that event. For others, a sense of belonging becomes fixed in their sense of tragedy as a victim of an event. We see many patients with posttraumatic stress disorder who have been bound by the traumatizing event(s), and who find it difficult or impossible to move beyond that experience.
For Americans, perhaps the notion of "family values" can be parsed to include the idea and study of belongingness. Understanding what belongingness encompasses can help us discuss relational being with our patients. Where do you find that sense of belonging? For Ioanna, her sense of belonging is felt in the seasonal ebb and flow of village life. Her sense of belonging shows in her skill as she works with her crafts with her hands. Breb belongs to her, even as it opens its large wooden doors to the world.
Dr. Heru is with the department of psychiatry at the University of Colorado at Denver, Aurora. She is editor of the recently published book, "Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals" (New York: Routledge, 2013.