User login
Pediatric Orthopedic Basics
Case 1
A mother presented to the ED with her 8-year-old daughter after she witnessed the child fall off her bicycle onto the sidewalk. When she fell, the girl landed onto her outstretched arms and sustained minor abrasions to her palms and knees, but did not hit her head or lose consciousness. Upon falling, the child immediately cried that her left arm hurt and kept holding it guarded near her body.
She was seated on her mother’s lap in the examination room, appearing anxious but in no acute distress. The treating EP observed the superficial abrasions from across the room and obtained a detailed history.
The patient was afebrile, and her vital signs were stable with the exception of mild tachycardia. After a couple of minutes, the EP slowly approached the child and was able to perform a basic examination. There was no obvious deformity to her left upper extremity, and only mild swelling over the wrist. She was able to move her fingers well and had excellent capillary refill distally. The child remained calm during manual palpation of the anatomic snuff box. However, she immediately pulled away and began to cry upon palpation more proximally over the distal forearm. The EP discussed his concerns with the child’s mother and explained that further evaluation was necessary.
Case 2
A mother and father presented to the ED carrying their 6-year-old boy, stating that the child had been limping since they picked him up from a neighbor’s house an hour earlier and was now refusing to walk. The father noted that a group of children had been jumping on a trampoline unsupervised, but he did not witness any injury to his son. Both parents said that the boy had been well up until that day.
At presentation, the child was afebrile and his vital signs were stable. The EP asked the parents to coax the child to walk across the room. During the walk, the boy was reluctant to bear weight on his right foot. Careful inspection of his lower limb revealed no external signs of trauma, and it appeared neurovascularly intact. Careful palpation elicited tenderness directly over the physis at the distal fibula and near the lateral malleolus. While considering the broad differential for a limping child, the physician was primarily concerned with point tenderness on examination and informed the parents that radiographic imaging was warranted.
Overview
Pediatric musculoskeletal (MSK) injury and orthopedic trauma now comprise more than 10% of visits to the ED.1 Fractures in particular are becoming more commonplace with the increasing number of children actively involved in athletic sports and high-risk activities.
The general approach to acute-care management of these children has evolved, trending more toward splinting the fractured extremity and away from traditional casting. There are many benefits to splinting. The most important is arguably the reduced risk of developing compartment syndrome due to a splint’s ability to expand with accompanied swelling.2 This article reviews the unique characteristics of pediatric bone development and initial management of pediatric fractures, as well as basic splinting techniques and unique indications that require further orthopedic consultation.
Physiological Differences in Children
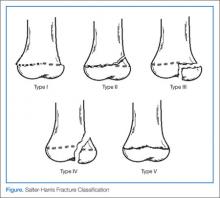
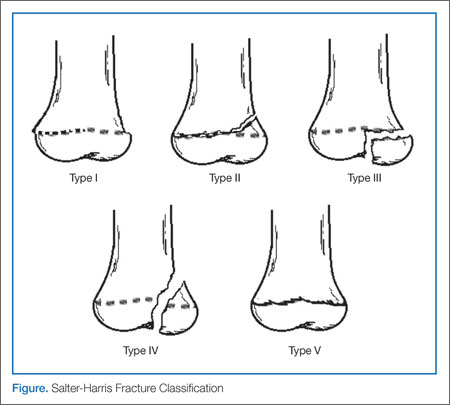
The MSK system of a child differs greatly from that of an adult. The bones themselves are much more porous and malleable during childhood, making them more susceptible to traumatic injury. The growing periosteum and the developing physes are particularly vulnerable, accounting for up to 20% of pediatric fractures (see the Figure illustrating the Salter-Harris classification in the next section).3 This is particularly true at a young age, when ligamentous adherence out-performs the bony integrity itself, making fractures more common than sprains and tears. The opposite is true in adults, who are much more likely to experience sprains before succumbing to fracture. Furthermore, since the periosteum is still very active in children, the fractured bone is much more likely to remodel, lending to less deformity and overall better outcomes in most cases.3 Nonunion is extremely rare in children.
Initial Management
Approaching the Pediatric Patient
Special consideration should be given when initially approaching an injured child, so as not to cause additional undue fear or anxiety to the patient. It is helpful to take an extra moment upon entering the room to simply observe the child’s positioning, posture, or reluctance to move a particular limb. Obtaining a careful, detailed history from a distance is recommended before too quickly approaching the patient. In addition, asking the caregiver to serve as proxy during the initial physical examination may also prove helpful in localizing the pain. In the obscure case, such as the child refusing to bear weight, it is good to keep a broad differential and inspect for non-MSK injury (eg, painful hernia, testicular torsion, foreign body lodged in the bottom of the foot). Utilizing a “log-rolling” technique with the palms of one’s hands on the patient’s thigh may reveal hip pathology. Simply observing the preoccupied child walk around the unit while watching from behind may also aid in the evaluation.
However, when the injury such as an open fracture or severe displacement is obvious, immediate stabilization is critical so as not to permit any additional harm. An arm board is typically used to accomplish this. In addition, pain control should never be overlooked, either with intravenous opioids or more appropriate oral or intranasal analgesia.4,5 In cases of significant trauma, always remember ABC assessment (airway, breathing/oxygenation, and circulation), despite the eagerness to give attention to what may be an obvious fracture.
Workup
Although the use of ultrasound and other modalities is becoming more popular in some settings, it is still commonplace to begin the evaluation of a potential fracture or dislocation with plain film X-rays. Before sending a patient to radiology, always stabilize any unstable fracture to avoid further injury or potentiate neurovascular compromise. In most cases, three views, including anteroposterior, true lateral, and oblique, are obtained. If a fracture is unclear, it may be helpful to image the opposite extremity for comparison. The location of a fracture and its characteristics greatly influence acute-care management, as well as patient disposition, the need for consultation with orthopedics, and follow-up expectations and instructions.
Salter-Harris Fracture Classification
The physes of bones in growing children are particularly vulnerable sites of fracture since they have not yet fused. The five generally accepted types of fracture according to risk of growth disturbance are illustrated in the above Figure and are differentiated as follows:
Type I. This type of fracture is exclusive involvement of the physis itself, separating the metaphysis from the epiphysis. Since plain films may not reveal any visible fracture, the clinician should have a high index of suspicion if the physical examination elicits point tenderness over the growth plate. When in doubt if a fracture is present, always splint. Type I fractures of the physis tend to heal well, without significant consequence.
Type II. As with type I fractures, type II involve the physis, but also have a fragment of displaced metaphysis—the most common of all physeal fractures. Without significant displacement, these fractures also tend to have good outcomes.
Type III. Rather than involving the physis and metaphysis, type III fractures involve the epiphysis and therefore the joint itself. It is because of the epiphyseal displacement that these fractures tend to have a worse prognosis with joint disability and growth arrest. Thus, establishing alignment is imperative. The distal tibial Tillaux fracture is an example and requires internal fixation for optimal healing.
Type IV. Similar to a type III fracture, with the fracture extending proximally through a segment of the metaphysis, type IV fractures are treated similar to type III fractures. Due to joint involvement, an orthopedic consultation is warranted.
Type V. This type represents compression fractures of the physis. As the visibility of these fractures is poor on plain films, diagnosis can be challenging. However, history of axial compression injury may help lead the clinician to an accurate diagnosis. Since there is a high incidence of growth disturbance in type V fractures, compression affecting other areas such as the spine should also be considered.
Certainly not all pediatric fractures will involve a physis. A detailed description and management of other unique types of pediatric fractures is discussed in other articles in this feature.
Splinting Basics
Once the decision is made to apply a splint to a fracture, certain basic precautions should first be taken. Initially, any significant lacerations or abrasions should be thoroughly irrigated, cleansed, and dressed appropriately. Next, the physician should reevaluate and document both neurological status and perfusion of the area, particularly distal to the fracture site.
One commonly overlooked step in management of any fracture is pain control. It is advisable to consider administering medication prior to splinting on a case-by-case basis and for all fractures requiring reduction.
Materials and Methods
Prepackaged fiberglass splints have become a popular, efficient, and less-messy material of choice in pediatric splinting. Alternatively, plaster of Paris—although a bit more cumbersome—has some advantages, including low cost and a tendency to mold more easily to the extremity being splinted.7 When using plaster, strips should be cut a little longer than the anticipated length needed since they may shrink during curing. The unaffected limb should be used to gauge the measurement needed.
Regardless of the material chosen, all splinting should begin with the application of a stockinette tube dressing over the skin, leaving a distal opening over fingers or toes. This should be followed by a padding material (eg, Webril), beginning distally and rolling proximally, being sure to have approximately 50% overlap of each roll. Extra padding should be rolled over any bony prominence (eg, ulnar stylus) to avoid discomfort or pressure sores once the splint is applied.2
Between 8 and 10 layers of plaster (additional layers for lower extremity splints) should be wetted with room-temperature water. Hot water should never be used as this will intensify the exothermic reaction that occurs when curing and could cause burns.2 The limb should be kept in the anatomic position while the plaster is being molded to the shape of the extremity, allowing 15 to 20 minutes to dry.1 Once dry, an elastic bandage such as an Ace wrap may be placed over the entire cast to hold it secure in place. If fiberglass is used, it is helpful to squeeze out extra water before molding to the extremity. Again, an additional padding roll should be employed to avoid any discomfort or pressure beneath the splint.
In both fiberglass and plaster splinting, the edges of either type of material should not be abrasive to the skin; this can be avoided by rolling over excess padding and stockinette to create a round soft edge on either end.7 Finally, the patient should be fitted with a shoulder sling or crutches (if age appropriate) to further immobilize the injured extremity and avoid any movement or weight bearing.
Types of Splints
The type of splint depends of the location and characteristics of the fracture being immobilized. The following are a few examples of the more popular splinting techniques indicated for common pediatric fractures.
Long-Arm Posterior Splint. This splint is useful for most forearm and elbow fractures. The splint length should extend from midlength of the humerus to the palmar crease, and the width should be semicircular. In addition, an anatomic position of 90˚ flexion of the elbow should be maintained, with the hand in a neutral position and slight dorsiflexion. It is generally accepted to slightly pronate the forearm when splinting a supracondylar fracture. Orthopedics should always be consulted if the fracture involves the elbow.
Ulnar “Gutter” Splint. Useful for nondisplaced, minimally-angulated metacarpal “boxer’s fracture” or fourth and fifth phalangeal fractures, the length of the ulnar splint should extend from the distal phalanx to proximal forearm. Splint width should enclose both the volar and dorsum surfaces of the fourth and fifth metacarpals. In addition, padding should be placed between the digits for comfort. The metacarpophalangeal joints should be positioned at 70˚, and the proximal phalangeal angle at approximately 20˚ flexion2; this will help minimize the risk of contractures.
Forearm “Sugar-Tong” Splint. These splints are indicated for immobilization of a distal radius fracture or wrist injury. Distal radial fractures are by far the most common fractures encountered in the pediatric population,8 and splinting for angulation less than 15˚ is preferred.9,10 For proper stabilization, a long U-shaped splint should originate at the palmar crease, wrap around the elbow, and end at the metacarpophalangeal joint dorsally. Again, the hand should be dorsiflexed, and a soft rolled edge should be kept on the palmar crease to allow full finger flexion to near 90˚.
Thumb Spica Splint. A thumb spica splint is useful to immobilize uncomplicated fracture of the first metacarpal or proximal phalanx or when scaphoid (navicular) bone fracture is suspected. A semicircumferential molding of the radial forearm should be formed, extending to the thumbnail bed, and wrapping around the thumb. The proper hand positioning is slightly dorsiflexed, with thumb abducted slightly, as if holding a glass of water.2 If there is any doubt of a navicular fracture (rare in prepubescent children), the clinician should never hesitate to splint!
Long-Leg Posterior Splint. This type of splint is appropriate for immobilization of midshaft tibia/fibula fractures or most knee injuries. Full length of the splint should start beneath the inferior gluteal fold and extend to the ball of the foot, leaving the toes free. The ankle should be at 90˚ flexion and the knee should remain just slightly flexed, never locked straight. Orthopedics should always be consulted in cases of proximal tibia/fibula fractures or knee joint involvement.
Posterior Ankle Splint. Essentially a shorter version of a long-leg splint extending proximally to just below the knee, the posterior ankle splint is useful to immobilize ankle fractures, foot fractures, and severe ankle sprains. The distal fibula and occasional tibia physes are another common site of pediatric fractures, particularly in obese or more active children.11,12 When using either a long- or short-leg posterior ankle splint, it is helpful to hold the foot at 90˚ flexion until the material hardens or the proper angle may be lost. A recall that displaced or Salter-Harris type III or IV physeal fractures justify orthopedics consult. Nonweight-bearing, use of crutches, ice, and elevation are all important points for recovery in 3 to 6 weeks.
Lower Extremity Stirrup “Sugar-Tong” Splint. This splint is indicated for additional ankle stabilization. It runs in a U-shape (not unlike a forearm sugar-tong splint) from just below the knee around the calcaneus, and it must be wide enough to encase the ankle but not so wide that the two sides overlap when molded. It is very important to add extra padding around both malleoli and beneath the calcaneus to reduce the likelihood of pressure sores. Crutches are essential to avoid weight-bearing in patients old enough to use them. Some pediatric orthopedists advise avoiding this type of splint in the smaller, noncompliant, active child.
Complications
Although splinting has many advantages over casting in the acute-care setting, several potential complications may develop. Although rare, thermal burns to the underlying skin may occur if excessively warm or hot water is used on plaster or fiberglass due to the exothermic reaction during the hardening process. Therefore, the use of room-temperature water is always recommended. Despite the noncircumferential nature of a splint, it is still possible to develop significant swelling following splint application, which can lead to neurovascular compromise, compartment syndrome, infection, or pressure ulcers.7 The patient and caregiver should be advised to return to the ED immediately for evaluation if serious signs and symptoms such as pain, numbness, tingling, dusky color of skin, or poor capillary refill develop.
Case 1 Conclusion
The EP in this case elected to obtain plain X-rays of the patient’s left forearm, including the wrist and elbow. The results demonstrated a disruption of the cortical integrity of the distal radius, consistent with a buckle fracture. The angulation was estimated at merely 10˚. The bones of the wrist and elbow appeared normal. The EP concluded that a consult with orthopedics was not required urgently, and immobilized the patient’s arm using a fiberglass sugar-tong splint, keeping her elbow at 90˚, the forearm in a neutral position, and hand slightly dorsiflexed. A nurse assisted in keeping the child still to ensure the splint was shaped around the arm and hardened in this position. The child was provided with a sling, and supportive-care measures, including analgesia with nonsteroidal anti-inflammatory drugs as needed, ice, rest, and the importance of keeping the splint dry, were reviewed with her parents. The EP also stressed the importance of surveying for any loss of sensation or perfusion to the patient’s hand and fingers, and recommended follow up with orthopedics 1 week from discharge.
Case 2 Conclusion
Multiple views of the patient’s ankle were obtained on X-ray and showed no apparent fracture or dislocation. Additional films of the opposite ankle were obtained for comparison, but both appeared quite similar except for mild soft-tissue swelling of the affected side. Since point tenderness was reproducible over the distal fibular physis, the EP elected to place a short-leg posterior splint, maintaining good anatomic position with extra padding around the malleoli. The parents were instructed on proper elevation, ice to reduce inflammation, and the use of pain medication if needed.
One week after discharge, the treating EP received a letter from the child’s orthopedist, informing him that at the follow-up appointment, a repeat ankle film revealed periosteal changes and a type I Salter-Harris distal fibula fracture. Immobilization for an additional 3 weeks and supportive care was indicated.
Dr Del Re is an instructor of pediatrics and an intermediate care pediatrician, Rady Children’s Hospital, San Diego, California. Dr Clingenpeel is a fellowship director, pediatric emergency medicine, and associate professor of pediatrics, Eastern Virginia Medical School, Norfolk.
- Bachman D, Santora S. Musculoskeletal trauma. In: Fleisher GR, Ludwig S, eds. Textbook of Pediatric Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2010:1335-1375.
- Klig JE. Splinting procedures. In: King C, Henretig FM, eds. Texbook of Pediatric Emergency Procedures. 2nd ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2008:919-931.
- Wilkins KE. The incidence of fractures in children. In: Rockwood CA, Wilkins KE, Beaty JH, eds. Fractures in Children. 4th ed. Philadelphia, PA: Lippincott-Raven; 1996:3-17.
- Mahar PJ, Rana JA, Kennedy CS, Christopher NC. A randomized clinical trial of oral transmucosal fentanyl citrate versus intravenous morphine sulfate for initial control of pain in children with extremity injuries. Pediatr Emerg Care. 2007;23(8):544-548.
- Saunders M, Adelgais K, Nelson D. Use of intranasal fentanyl for the relief of pediatric orthopedic trauma pain. Acad Emerg Med. 2010;17(11):1155-1161.
- Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am. 1963;45:587-622.
- Boyd AS, Benjamin HJ, Asplund C. Principles of casting and splinting. Am Fam Physician. 2009;79(1):16-22.
- Solan MC, Rees R, Daly K. Current management of torus fractures of the distal radius. Injury. 2002;33(6):503-505.
- Boutis K, Willan A, Babyn P, Goeree R, Howard A. Cast versus splint in children with minimally angulated fractures of the distal radius: a randomized controlled trial. CMAJ. 2010;182(14):1507-1512.
- Firmin F, Crouch R. Splinting versus casting of “torus” fractures to the distal radius in the paediatric patient presenting at the emergency department (ED): a literature review. Int Emerg Nurs. 2009;17(3):173-178.
- Peterson HA, Madhok R, Benson JT, Ilstrup DM, Melton LJ 3rd. Physeal fractures: Part 1. Epidemiology in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop. 1994;14(4):423-430.
- Blackburn EW, Aronsson DD, Rubright JH, Lisle JW. Ankle fractures in children. J Bone Joint Surg Am. 2012; 94(13):1234-1244.
Case 1
A mother presented to the ED with her 8-year-old daughter after she witnessed the child fall off her bicycle onto the sidewalk. When she fell, the girl landed onto her outstretched arms and sustained minor abrasions to her palms and knees, but did not hit her head or lose consciousness. Upon falling, the child immediately cried that her left arm hurt and kept holding it guarded near her body.
She was seated on her mother’s lap in the examination room, appearing anxious but in no acute distress. The treating EP observed the superficial abrasions from across the room and obtained a detailed history.
The patient was afebrile, and her vital signs were stable with the exception of mild tachycardia. After a couple of minutes, the EP slowly approached the child and was able to perform a basic examination. There was no obvious deformity to her left upper extremity, and only mild swelling over the wrist. She was able to move her fingers well and had excellent capillary refill distally. The child remained calm during manual palpation of the anatomic snuff box. However, she immediately pulled away and began to cry upon palpation more proximally over the distal forearm. The EP discussed his concerns with the child’s mother and explained that further evaluation was necessary.
Case 2
A mother and father presented to the ED carrying their 6-year-old boy, stating that the child had been limping since they picked him up from a neighbor’s house an hour earlier and was now refusing to walk. The father noted that a group of children had been jumping on a trampoline unsupervised, but he did not witness any injury to his son. Both parents said that the boy had been well up until that day.
At presentation, the child was afebrile and his vital signs were stable. The EP asked the parents to coax the child to walk across the room. During the walk, the boy was reluctant to bear weight on his right foot. Careful inspection of his lower limb revealed no external signs of trauma, and it appeared neurovascularly intact. Careful palpation elicited tenderness directly over the physis at the distal fibula and near the lateral malleolus. While considering the broad differential for a limping child, the physician was primarily concerned with point tenderness on examination and informed the parents that radiographic imaging was warranted.
Overview
Pediatric musculoskeletal (MSK) injury and orthopedic trauma now comprise more than 10% of visits to the ED.1 Fractures in particular are becoming more commonplace with the increasing number of children actively involved in athletic sports and high-risk activities.
The general approach to acute-care management of these children has evolved, trending more toward splinting the fractured extremity and away from traditional casting. There are many benefits to splinting. The most important is arguably the reduced risk of developing compartment syndrome due to a splint’s ability to expand with accompanied swelling.2 This article reviews the unique characteristics of pediatric bone development and initial management of pediatric fractures, as well as basic splinting techniques and unique indications that require further orthopedic consultation.
Physiological Differences in Children
The MSK system of a child differs greatly from that of an adult. The bones themselves are much more porous and malleable during childhood, making them more susceptible to traumatic injury. The growing periosteum and the developing physes are particularly vulnerable, accounting for up to 20% of pediatric fractures (see the Figure illustrating the Salter-Harris classification in the next section).3 This is particularly true at a young age, when ligamentous adherence out-performs the bony integrity itself, making fractures more common than sprains and tears. The opposite is true in adults, who are much more likely to experience sprains before succumbing to fracture. Furthermore, since the periosteum is still very active in children, the fractured bone is much more likely to remodel, lending to less deformity and overall better outcomes in most cases.3 Nonunion is extremely rare in children.
Initial Management
Approaching the Pediatric Patient
Special consideration should be given when initially approaching an injured child, so as not to cause additional undue fear or anxiety to the patient. It is helpful to take an extra moment upon entering the room to simply observe the child’s positioning, posture, or reluctance to move a particular limb. Obtaining a careful, detailed history from a distance is recommended before too quickly approaching the patient. In addition, asking the caregiver to serve as proxy during the initial physical examination may also prove helpful in localizing the pain. In the obscure case, such as the child refusing to bear weight, it is good to keep a broad differential and inspect for non-MSK injury (eg, painful hernia, testicular torsion, foreign body lodged in the bottom of the foot). Utilizing a “log-rolling” technique with the palms of one’s hands on the patient’s thigh may reveal hip pathology. Simply observing the preoccupied child walk around the unit while watching from behind may also aid in the evaluation.
However, when the injury such as an open fracture or severe displacement is obvious, immediate stabilization is critical so as not to permit any additional harm. An arm board is typically used to accomplish this. In addition, pain control should never be overlooked, either with intravenous opioids or more appropriate oral or intranasal analgesia.4,5 In cases of significant trauma, always remember ABC assessment (airway, breathing/oxygenation, and circulation), despite the eagerness to give attention to what may be an obvious fracture.
Workup
Although the use of ultrasound and other modalities is becoming more popular in some settings, it is still commonplace to begin the evaluation of a potential fracture or dislocation with plain film X-rays. Before sending a patient to radiology, always stabilize any unstable fracture to avoid further injury or potentiate neurovascular compromise. In most cases, three views, including anteroposterior, true lateral, and oblique, are obtained. If a fracture is unclear, it may be helpful to image the opposite extremity for comparison. The location of a fracture and its characteristics greatly influence acute-care management, as well as patient disposition, the need for consultation with orthopedics, and follow-up expectations and instructions.
Salter-Harris Fracture Classification
The physes of bones in growing children are particularly vulnerable sites of fracture since they have not yet fused. The five generally accepted types of fracture according to risk of growth disturbance are illustrated in the above Figure and are differentiated as follows:
Type I. This type of fracture is exclusive involvement of the physis itself, separating the metaphysis from the epiphysis. Since plain films may not reveal any visible fracture, the clinician should have a high index of suspicion if the physical examination elicits point tenderness over the growth plate. When in doubt if a fracture is present, always splint. Type I fractures of the physis tend to heal well, without significant consequence.
Type II. As with type I fractures, type II involve the physis, but also have a fragment of displaced metaphysis—the most common of all physeal fractures. Without significant displacement, these fractures also tend to have good outcomes.
Type III. Rather than involving the physis and metaphysis, type III fractures involve the epiphysis and therefore the joint itself. It is because of the epiphyseal displacement that these fractures tend to have a worse prognosis with joint disability and growth arrest. Thus, establishing alignment is imperative. The distal tibial Tillaux fracture is an example and requires internal fixation for optimal healing.
Type IV. Similar to a type III fracture, with the fracture extending proximally through a segment of the metaphysis, type IV fractures are treated similar to type III fractures. Due to joint involvement, an orthopedic consultation is warranted.
Type V. This type represents compression fractures of the physis. As the visibility of these fractures is poor on plain films, diagnosis can be challenging. However, history of axial compression injury may help lead the clinician to an accurate diagnosis. Since there is a high incidence of growth disturbance in type V fractures, compression affecting other areas such as the spine should also be considered.
Certainly not all pediatric fractures will involve a physis. A detailed description and management of other unique types of pediatric fractures is discussed in other articles in this feature.
Splinting Basics
Once the decision is made to apply a splint to a fracture, certain basic precautions should first be taken. Initially, any significant lacerations or abrasions should be thoroughly irrigated, cleansed, and dressed appropriately. Next, the physician should reevaluate and document both neurological status and perfusion of the area, particularly distal to the fracture site.
One commonly overlooked step in management of any fracture is pain control. It is advisable to consider administering medication prior to splinting on a case-by-case basis and for all fractures requiring reduction.
Materials and Methods
Prepackaged fiberglass splints have become a popular, efficient, and less-messy material of choice in pediatric splinting. Alternatively, plaster of Paris—although a bit more cumbersome—has some advantages, including low cost and a tendency to mold more easily to the extremity being splinted.7 When using plaster, strips should be cut a little longer than the anticipated length needed since they may shrink during curing. The unaffected limb should be used to gauge the measurement needed.
Regardless of the material chosen, all splinting should begin with the application of a stockinette tube dressing over the skin, leaving a distal opening over fingers or toes. This should be followed by a padding material (eg, Webril), beginning distally and rolling proximally, being sure to have approximately 50% overlap of each roll. Extra padding should be rolled over any bony prominence (eg, ulnar stylus) to avoid discomfort or pressure sores once the splint is applied.2
Between 8 and 10 layers of plaster (additional layers for lower extremity splints) should be wetted with room-temperature water. Hot water should never be used as this will intensify the exothermic reaction that occurs when curing and could cause burns.2 The limb should be kept in the anatomic position while the plaster is being molded to the shape of the extremity, allowing 15 to 20 minutes to dry.1 Once dry, an elastic bandage such as an Ace wrap may be placed over the entire cast to hold it secure in place. If fiberglass is used, it is helpful to squeeze out extra water before molding to the extremity. Again, an additional padding roll should be employed to avoid any discomfort or pressure beneath the splint.
In both fiberglass and plaster splinting, the edges of either type of material should not be abrasive to the skin; this can be avoided by rolling over excess padding and stockinette to create a round soft edge on either end.7 Finally, the patient should be fitted with a shoulder sling or crutches (if age appropriate) to further immobilize the injured extremity and avoid any movement or weight bearing.
Types of Splints
The type of splint depends of the location and characteristics of the fracture being immobilized. The following are a few examples of the more popular splinting techniques indicated for common pediatric fractures.
Long-Arm Posterior Splint. This splint is useful for most forearm and elbow fractures. The splint length should extend from midlength of the humerus to the palmar crease, and the width should be semicircular. In addition, an anatomic position of 90˚ flexion of the elbow should be maintained, with the hand in a neutral position and slight dorsiflexion. It is generally accepted to slightly pronate the forearm when splinting a supracondylar fracture. Orthopedics should always be consulted if the fracture involves the elbow.
Ulnar “Gutter” Splint. Useful for nondisplaced, minimally-angulated metacarpal “boxer’s fracture” or fourth and fifth phalangeal fractures, the length of the ulnar splint should extend from the distal phalanx to proximal forearm. Splint width should enclose both the volar and dorsum surfaces of the fourth and fifth metacarpals. In addition, padding should be placed between the digits for comfort. The metacarpophalangeal joints should be positioned at 70˚, and the proximal phalangeal angle at approximately 20˚ flexion2; this will help minimize the risk of contractures.
Forearm “Sugar-Tong” Splint. These splints are indicated for immobilization of a distal radius fracture or wrist injury. Distal radial fractures are by far the most common fractures encountered in the pediatric population,8 and splinting for angulation less than 15˚ is preferred.9,10 For proper stabilization, a long U-shaped splint should originate at the palmar crease, wrap around the elbow, and end at the metacarpophalangeal joint dorsally. Again, the hand should be dorsiflexed, and a soft rolled edge should be kept on the palmar crease to allow full finger flexion to near 90˚.
Thumb Spica Splint. A thumb spica splint is useful to immobilize uncomplicated fracture of the first metacarpal or proximal phalanx or when scaphoid (navicular) bone fracture is suspected. A semicircumferential molding of the radial forearm should be formed, extending to the thumbnail bed, and wrapping around the thumb. The proper hand positioning is slightly dorsiflexed, with thumb abducted slightly, as if holding a glass of water.2 If there is any doubt of a navicular fracture (rare in prepubescent children), the clinician should never hesitate to splint!
Long-Leg Posterior Splint. This type of splint is appropriate for immobilization of midshaft tibia/fibula fractures or most knee injuries. Full length of the splint should start beneath the inferior gluteal fold and extend to the ball of the foot, leaving the toes free. The ankle should be at 90˚ flexion and the knee should remain just slightly flexed, never locked straight. Orthopedics should always be consulted in cases of proximal tibia/fibula fractures or knee joint involvement.
Posterior Ankle Splint. Essentially a shorter version of a long-leg splint extending proximally to just below the knee, the posterior ankle splint is useful to immobilize ankle fractures, foot fractures, and severe ankle sprains. The distal fibula and occasional tibia physes are another common site of pediatric fractures, particularly in obese or more active children.11,12 When using either a long- or short-leg posterior ankle splint, it is helpful to hold the foot at 90˚ flexion until the material hardens or the proper angle may be lost. A recall that displaced or Salter-Harris type III or IV physeal fractures justify orthopedics consult. Nonweight-bearing, use of crutches, ice, and elevation are all important points for recovery in 3 to 6 weeks.
Lower Extremity Stirrup “Sugar-Tong” Splint. This splint is indicated for additional ankle stabilization. It runs in a U-shape (not unlike a forearm sugar-tong splint) from just below the knee around the calcaneus, and it must be wide enough to encase the ankle but not so wide that the two sides overlap when molded. It is very important to add extra padding around both malleoli and beneath the calcaneus to reduce the likelihood of pressure sores. Crutches are essential to avoid weight-bearing in patients old enough to use them. Some pediatric orthopedists advise avoiding this type of splint in the smaller, noncompliant, active child.
Complications
Although splinting has many advantages over casting in the acute-care setting, several potential complications may develop. Although rare, thermal burns to the underlying skin may occur if excessively warm or hot water is used on plaster or fiberglass due to the exothermic reaction during the hardening process. Therefore, the use of room-temperature water is always recommended. Despite the noncircumferential nature of a splint, it is still possible to develop significant swelling following splint application, which can lead to neurovascular compromise, compartment syndrome, infection, or pressure ulcers.7 The patient and caregiver should be advised to return to the ED immediately for evaluation if serious signs and symptoms such as pain, numbness, tingling, dusky color of skin, or poor capillary refill develop.
Case 1 Conclusion
The EP in this case elected to obtain plain X-rays of the patient’s left forearm, including the wrist and elbow. The results demonstrated a disruption of the cortical integrity of the distal radius, consistent with a buckle fracture. The angulation was estimated at merely 10˚. The bones of the wrist and elbow appeared normal. The EP concluded that a consult with orthopedics was not required urgently, and immobilized the patient’s arm using a fiberglass sugar-tong splint, keeping her elbow at 90˚, the forearm in a neutral position, and hand slightly dorsiflexed. A nurse assisted in keeping the child still to ensure the splint was shaped around the arm and hardened in this position. The child was provided with a sling, and supportive-care measures, including analgesia with nonsteroidal anti-inflammatory drugs as needed, ice, rest, and the importance of keeping the splint dry, were reviewed with her parents. The EP also stressed the importance of surveying for any loss of sensation or perfusion to the patient’s hand and fingers, and recommended follow up with orthopedics 1 week from discharge.
Case 2 Conclusion
Multiple views of the patient’s ankle were obtained on X-ray and showed no apparent fracture or dislocation. Additional films of the opposite ankle were obtained for comparison, but both appeared quite similar except for mild soft-tissue swelling of the affected side. Since point tenderness was reproducible over the distal fibular physis, the EP elected to place a short-leg posterior splint, maintaining good anatomic position with extra padding around the malleoli. The parents were instructed on proper elevation, ice to reduce inflammation, and the use of pain medication if needed.
One week after discharge, the treating EP received a letter from the child’s orthopedist, informing him that at the follow-up appointment, a repeat ankle film revealed periosteal changes and a type I Salter-Harris distal fibula fracture. Immobilization for an additional 3 weeks and supportive care was indicated.
Dr Del Re is an instructor of pediatrics and an intermediate care pediatrician, Rady Children’s Hospital, San Diego, California. Dr Clingenpeel is a fellowship director, pediatric emergency medicine, and associate professor of pediatrics, Eastern Virginia Medical School, Norfolk.
Case 1
A mother presented to the ED with her 8-year-old daughter after she witnessed the child fall off her bicycle onto the sidewalk. When she fell, the girl landed onto her outstretched arms and sustained minor abrasions to her palms and knees, but did not hit her head or lose consciousness. Upon falling, the child immediately cried that her left arm hurt and kept holding it guarded near her body.
She was seated on her mother’s lap in the examination room, appearing anxious but in no acute distress. The treating EP observed the superficial abrasions from across the room and obtained a detailed history.
The patient was afebrile, and her vital signs were stable with the exception of mild tachycardia. After a couple of minutes, the EP slowly approached the child and was able to perform a basic examination. There was no obvious deformity to her left upper extremity, and only mild swelling over the wrist. She was able to move her fingers well and had excellent capillary refill distally. The child remained calm during manual palpation of the anatomic snuff box. However, she immediately pulled away and began to cry upon palpation more proximally over the distal forearm. The EP discussed his concerns with the child’s mother and explained that further evaluation was necessary.
Case 2
A mother and father presented to the ED carrying their 6-year-old boy, stating that the child had been limping since they picked him up from a neighbor’s house an hour earlier and was now refusing to walk. The father noted that a group of children had been jumping on a trampoline unsupervised, but he did not witness any injury to his son. Both parents said that the boy had been well up until that day.
At presentation, the child was afebrile and his vital signs were stable. The EP asked the parents to coax the child to walk across the room. During the walk, the boy was reluctant to bear weight on his right foot. Careful inspection of his lower limb revealed no external signs of trauma, and it appeared neurovascularly intact. Careful palpation elicited tenderness directly over the physis at the distal fibula and near the lateral malleolus. While considering the broad differential for a limping child, the physician was primarily concerned with point tenderness on examination and informed the parents that radiographic imaging was warranted.
Overview
Pediatric musculoskeletal (MSK) injury and orthopedic trauma now comprise more than 10% of visits to the ED.1 Fractures in particular are becoming more commonplace with the increasing number of children actively involved in athletic sports and high-risk activities.
The general approach to acute-care management of these children has evolved, trending more toward splinting the fractured extremity and away from traditional casting. There are many benefits to splinting. The most important is arguably the reduced risk of developing compartment syndrome due to a splint’s ability to expand with accompanied swelling.2 This article reviews the unique characteristics of pediatric bone development and initial management of pediatric fractures, as well as basic splinting techniques and unique indications that require further orthopedic consultation.
Physiological Differences in Children
The MSK system of a child differs greatly from that of an adult. The bones themselves are much more porous and malleable during childhood, making them more susceptible to traumatic injury. The growing periosteum and the developing physes are particularly vulnerable, accounting for up to 20% of pediatric fractures (see the Figure illustrating the Salter-Harris classification in the next section).3 This is particularly true at a young age, when ligamentous adherence out-performs the bony integrity itself, making fractures more common than sprains and tears. The opposite is true in adults, who are much more likely to experience sprains before succumbing to fracture. Furthermore, since the periosteum is still very active in children, the fractured bone is much more likely to remodel, lending to less deformity and overall better outcomes in most cases.3 Nonunion is extremely rare in children.
Initial Management
Approaching the Pediatric Patient
Special consideration should be given when initially approaching an injured child, so as not to cause additional undue fear or anxiety to the patient. It is helpful to take an extra moment upon entering the room to simply observe the child’s positioning, posture, or reluctance to move a particular limb. Obtaining a careful, detailed history from a distance is recommended before too quickly approaching the patient. In addition, asking the caregiver to serve as proxy during the initial physical examination may also prove helpful in localizing the pain. In the obscure case, such as the child refusing to bear weight, it is good to keep a broad differential and inspect for non-MSK injury (eg, painful hernia, testicular torsion, foreign body lodged in the bottom of the foot). Utilizing a “log-rolling” technique with the palms of one’s hands on the patient’s thigh may reveal hip pathology. Simply observing the preoccupied child walk around the unit while watching from behind may also aid in the evaluation.
However, when the injury such as an open fracture or severe displacement is obvious, immediate stabilization is critical so as not to permit any additional harm. An arm board is typically used to accomplish this. In addition, pain control should never be overlooked, either with intravenous opioids or more appropriate oral or intranasal analgesia.4,5 In cases of significant trauma, always remember ABC assessment (airway, breathing/oxygenation, and circulation), despite the eagerness to give attention to what may be an obvious fracture.
Workup
Although the use of ultrasound and other modalities is becoming more popular in some settings, it is still commonplace to begin the evaluation of a potential fracture or dislocation with plain film X-rays. Before sending a patient to radiology, always stabilize any unstable fracture to avoid further injury or potentiate neurovascular compromise. In most cases, three views, including anteroposterior, true lateral, and oblique, are obtained. If a fracture is unclear, it may be helpful to image the opposite extremity for comparison. The location of a fracture and its characteristics greatly influence acute-care management, as well as patient disposition, the need for consultation with orthopedics, and follow-up expectations and instructions.
Salter-Harris Fracture Classification
The physes of bones in growing children are particularly vulnerable sites of fracture since they have not yet fused. The five generally accepted types of fracture according to risk of growth disturbance are illustrated in the above Figure and are differentiated as follows:
Type I. This type of fracture is exclusive involvement of the physis itself, separating the metaphysis from the epiphysis. Since plain films may not reveal any visible fracture, the clinician should have a high index of suspicion if the physical examination elicits point tenderness over the growth plate. When in doubt if a fracture is present, always splint. Type I fractures of the physis tend to heal well, without significant consequence.
Type II. As with type I fractures, type II involve the physis, but also have a fragment of displaced metaphysis—the most common of all physeal fractures. Without significant displacement, these fractures also tend to have good outcomes.
Type III. Rather than involving the physis and metaphysis, type III fractures involve the epiphysis and therefore the joint itself. It is because of the epiphyseal displacement that these fractures tend to have a worse prognosis with joint disability and growth arrest. Thus, establishing alignment is imperative. The distal tibial Tillaux fracture is an example and requires internal fixation for optimal healing.
Type IV. Similar to a type III fracture, with the fracture extending proximally through a segment of the metaphysis, type IV fractures are treated similar to type III fractures. Due to joint involvement, an orthopedic consultation is warranted.
Type V. This type represents compression fractures of the physis. As the visibility of these fractures is poor on plain films, diagnosis can be challenging. However, history of axial compression injury may help lead the clinician to an accurate diagnosis. Since there is a high incidence of growth disturbance in type V fractures, compression affecting other areas such as the spine should also be considered.
Certainly not all pediatric fractures will involve a physis. A detailed description and management of other unique types of pediatric fractures is discussed in other articles in this feature.
Splinting Basics
Once the decision is made to apply a splint to a fracture, certain basic precautions should first be taken. Initially, any significant lacerations or abrasions should be thoroughly irrigated, cleansed, and dressed appropriately. Next, the physician should reevaluate and document both neurological status and perfusion of the area, particularly distal to the fracture site.
One commonly overlooked step in management of any fracture is pain control. It is advisable to consider administering medication prior to splinting on a case-by-case basis and for all fractures requiring reduction.
Materials and Methods
Prepackaged fiberglass splints have become a popular, efficient, and less-messy material of choice in pediatric splinting. Alternatively, plaster of Paris—although a bit more cumbersome—has some advantages, including low cost and a tendency to mold more easily to the extremity being splinted.7 When using plaster, strips should be cut a little longer than the anticipated length needed since they may shrink during curing. The unaffected limb should be used to gauge the measurement needed.
Regardless of the material chosen, all splinting should begin with the application of a stockinette tube dressing over the skin, leaving a distal opening over fingers or toes. This should be followed by a padding material (eg, Webril), beginning distally and rolling proximally, being sure to have approximately 50% overlap of each roll. Extra padding should be rolled over any bony prominence (eg, ulnar stylus) to avoid discomfort or pressure sores once the splint is applied.2
Between 8 and 10 layers of plaster (additional layers for lower extremity splints) should be wetted with room-temperature water. Hot water should never be used as this will intensify the exothermic reaction that occurs when curing and could cause burns.2 The limb should be kept in the anatomic position while the plaster is being molded to the shape of the extremity, allowing 15 to 20 minutes to dry.1 Once dry, an elastic bandage such as an Ace wrap may be placed over the entire cast to hold it secure in place. If fiberglass is used, it is helpful to squeeze out extra water before molding to the extremity. Again, an additional padding roll should be employed to avoid any discomfort or pressure beneath the splint.
In both fiberglass and plaster splinting, the edges of either type of material should not be abrasive to the skin; this can be avoided by rolling over excess padding and stockinette to create a round soft edge on either end.7 Finally, the patient should be fitted with a shoulder sling or crutches (if age appropriate) to further immobilize the injured extremity and avoid any movement or weight bearing.
Types of Splints
The type of splint depends of the location and characteristics of the fracture being immobilized. The following are a few examples of the more popular splinting techniques indicated for common pediatric fractures.
Long-Arm Posterior Splint. This splint is useful for most forearm and elbow fractures. The splint length should extend from midlength of the humerus to the palmar crease, and the width should be semicircular. In addition, an anatomic position of 90˚ flexion of the elbow should be maintained, with the hand in a neutral position and slight dorsiflexion. It is generally accepted to slightly pronate the forearm when splinting a supracondylar fracture. Orthopedics should always be consulted if the fracture involves the elbow.
Ulnar “Gutter” Splint. Useful for nondisplaced, minimally-angulated metacarpal “boxer’s fracture” or fourth and fifth phalangeal fractures, the length of the ulnar splint should extend from the distal phalanx to proximal forearm. Splint width should enclose both the volar and dorsum surfaces of the fourth and fifth metacarpals. In addition, padding should be placed between the digits for comfort. The metacarpophalangeal joints should be positioned at 70˚, and the proximal phalangeal angle at approximately 20˚ flexion2; this will help minimize the risk of contractures.
Forearm “Sugar-Tong” Splint. These splints are indicated for immobilization of a distal radius fracture or wrist injury. Distal radial fractures are by far the most common fractures encountered in the pediatric population,8 and splinting for angulation less than 15˚ is preferred.9,10 For proper stabilization, a long U-shaped splint should originate at the palmar crease, wrap around the elbow, and end at the metacarpophalangeal joint dorsally. Again, the hand should be dorsiflexed, and a soft rolled edge should be kept on the palmar crease to allow full finger flexion to near 90˚.
Thumb Spica Splint. A thumb spica splint is useful to immobilize uncomplicated fracture of the first metacarpal or proximal phalanx or when scaphoid (navicular) bone fracture is suspected. A semicircumferential molding of the radial forearm should be formed, extending to the thumbnail bed, and wrapping around the thumb. The proper hand positioning is slightly dorsiflexed, with thumb abducted slightly, as if holding a glass of water.2 If there is any doubt of a navicular fracture (rare in prepubescent children), the clinician should never hesitate to splint!
Long-Leg Posterior Splint. This type of splint is appropriate for immobilization of midshaft tibia/fibula fractures or most knee injuries. Full length of the splint should start beneath the inferior gluteal fold and extend to the ball of the foot, leaving the toes free. The ankle should be at 90˚ flexion and the knee should remain just slightly flexed, never locked straight. Orthopedics should always be consulted in cases of proximal tibia/fibula fractures or knee joint involvement.
Posterior Ankle Splint. Essentially a shorter version of a long-leg splint extending proximally to just below the knee, the posterior ankle splint is useful to immobilize ankle fractures, foot fractures, and severe ankle sprains. The distal fibula and occasional tibia physes are another common site of pediatric fractures, particularly in obese or more active children.11,12 When using either a long- or short-leg posterior ankle splint, it is helpful to hold the foot at 90˚ flexion until the material hardens or the proper angle may be lost. A recall that displaced or Salter-Harris type III or IV physeal fractures justify orthopedics consult. Nonweight-bearing, use of crutches, ice, and elevation are all important points for recovery in 3 to 6 weeks.
Lower Extremity Stirrup “Sugar-Tong” Splint. This splint is indicated for additional ankle stabilization. It runs in a U-shape (not unlike a forearm sugar-tong splint) from just below the knee around the calcaneus, and it must be wide enough to encase the ankle but not so wide that the two sides overlap when molded. It is very important to add extra padding around both malleoli and beneath the calcaneus to reduce the likelihood of pressure sores. Crutches are essential to avoid weight-bearing in patients old enough to use them. Some pediatric orthopedists advise avoiding this type of splint in the smaller, noncompliant, active child.
Complications
Although splinting has many advantages over casting in the acute-care setting, several potential complications may develop. Although rare, thermal burns to the underlying skin may occur if excessively warm or hot water is used on plaster or fiberglass due to the exothermic reaction during the hardening process. Therefore, the use of room-temperature water is always recommended. Despite the noncircumferential nature of a splint, it is still possible to develop significant swelling following splint application, which can lead to neurovascular compromise, compartment syndrome, infection, or pressure ulcers.7 The patient and caregiver should be advised to return to the ED immediately for evaluation if serious signs and symptoms such as pain, numbness, tingling, dusky color of skin, or poor capillary refill develop.
Case 1 Conclusion
The EP in this case elected to obtain plain X-rays of the patient’s left forearm, including the wrist and elbow. The results demonstrated a disruption of the cortical integrity of the distal radius, consistent with a buckle fracture. The angulation was estimated at merely 10˚. The bones of the wrist and elbow appeared normal. The EP concluded that a consult with orthopedics was not required urgently, and immobilized the patient’s arm using a fiberglass sugar-tong splint, keeping her elbow at 90˚, the forearm in a neutral position, and hand slightly dorsiflexed. A nurse assisted in keeping the child still to ensure the splint was shaped around the arm and hardened in this position. The child was provided with a sling, and supportive-care measures, including analgesia with nonsteroidal anti-inflammatory drugs as needed, ice, rest, and the importance of keeping the splint dry, were reviewed with her parents. The EP also stressed the importance of surveying for any loss of sensation or perfusion to the patient’s hand and fingers, and recommended follow up with orthopedics 1 week from discharge.
Case 2 Conclusion
Multiple views of the patient’s ankle were obtained on X-ray and showed no apparent fracture or dislocation. Additional films of the opposite ankle were obtained for comparison, but both appeared quite similar except for mild soft-tissue swelling of the affected side. Since point tenderness was reproducible over the distal fibular physis, the EP elected to place a short-leg posterior splint, maintaining good anatomic position with extra padding around the malleoli. The parents were instructed on proper elevation, ice to reduce inflammation, and the use of pain medication if needed.
One week after discharge, the treating EP received a letter from the child’s orthopedist, informing him that at the follow-up appointment, a repeat ankle film revealed periosteal changes and a type I Salter-Harris distal fibula fracture. Immobilization for an additional 3 weeks and supportive care was indicated.
Dr Del Re is an instructor of pediatrics and an intermediate care pediatrician, Rady Children’s Hospital, San Diego, California. Dr Clingenpeel is a fellowship director, pediatric emergency medicine, and associate professor of pediatrics, Eastern Virginia Medical School, Norfolk.
- Bachman D, Santora S. Musculoskeletal trauma. In: Fleisher GR, Ludwig S, eds. Textbook of Pediatric Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2010:1335-1375.
- Klig JE. Splinting procedures. In: King C, Henretig FM, eds. Texbook of Pediatric Emergency Procedures. 2nd ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2008:919-931.
- Wilkins KE. The incidence of fractures in children. In: Rockwood CA, Wilkins KE, Beaty JH, eds. Fractures in Children. 4th ed. Philadelphia, PA: Lippincott-Raven; 1996:3-17.
- Mahar PJ, Rana JA, Kennedy CS, Christopher NC. A randomized clinical trial of oral transmucosal fentanyl citrate versus intravenous morphine sulfate for initial control of pain in children with extremity injuries. Pediatr Emerg Care. 2007;23(8):544-548.
- Saunders M, Adelgais K, Nelson D. Use of intranasal fentanyl for the relief of pediatric orthopedic trauma pain. Acad Emerg Med. 2010;17(11):1155-1161.
- Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am. 1963;45:587-622.
- Boyd AS, Benjamin HJ, Asplund C. Principles of casting and splinting. Am Fam Physician. 2009;79(1):16-22.
- Solan MC, Rees R, Daly K. Current management of torus fractures of the distal radius. Injury. 2002;33(6):503-505.
- Boutis K, Willan A, Babyn P, Goeree R, Howard A. Cast versus splint in children with minimally angulated fractures of the distal radius: a randomized controlled trial. CMAJ. 2010;182(14):1507-1512.
- Firmin F, Crouch R. Splinting versus casting of “torus” fractures to the distal radius in the paediatric patient presenting at the emergency department (ED): a literature review. Int Emerg Nurs. 2009;17(3):173-178.
- Peterson HA, Madhok R, Benson JT, Ilstrup DM, Melton LJ 3rd. Physeal fractures: Part 1. Epidemiology in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop. 1994;14(4):423-430.
- Blackburn EW, Aronsson DD, Rubright JH, Lisle JW. Ankle fractures in children. J Bone Joint Surg Am. 2012; 94(13):1234-1244.
- Bachman D, Santora S. Musculoskeletal trauma. In: Fleisher GR, Ludwig S, eds. Textbook of Pediatric Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2010:1335-1375.
- Klig JE. Splinting procedures. In: King C, Henretig FM, eds. Texbook of Pediatric Emergency Procedures. 2nd ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2008:919-931.
- Wilkins KE. The incidence of fractures in children. In: Rockwood CA, Wilkins KE, Beaty JH, eds. Fractures in Children. 4th ed. Philadelphia, PA: Lippincott-Raven; 1996:3-17.
- Mahar PJ, Rana JA, Kennedy CS, Christopher NC. A randomized clinical trial of oral transmucosal fentanyl citrate versus intravenous morphine sulfate for initial control of pain in children with extremity injuries. Pediatr Emerg Care. 2007;23(8):544-548.
- Saunders M, Adelgais K, Nelson D. Use of intranasal fentanyl for the relief of pediatric orthopedic trauma pain. Acad Emerg Med. 2010;17(11):1155-1161.
- Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am. 1963;45:587-622.
- Boyd AS, Benjamin HJ, Asplund C. Principles of casting and splinting. Am Fam Physician. 2009;79(1):16-22.
- Solan MC, Rees R, Daly K. Current management of torus fractures of the distal radius. Injury. 2002;33(6):503-505.
- Boutis K, Willan A, Babyn P, Goeree R, Howard A. Cast versus splint in children with minimally angulated fractures of the distal radius: a randomized controlled trial. CMAJ. 2010;182(14):1507-1512.
- Firmin F, Crouch R. Splinting versus casting of “torus” fractures to the distal radius in the paediatric patient presenting at the emergency department (ED): a literature review. Int Emerg Nurs. 2009;17(3):173-178.
- Peterson HA, Madhok R, Benson JT, Ilstrup DM, Melton LJ 3rd. Physeal fractures: Part 1. Epidemiology in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop. 1994;14(4):423-430.
- Blackburn EW, Aronsson DD, Rubright JH, Lisle JW. Ankle fractures in children. J Bone Joint Surg Am. 2012; 94(13):1234-1244.