User login
The Hospital Readmissions Reduction Program and Observation Hospitalizations
The Hospital Readmissions Reduction Program (HRRP) was designed to improve quality and safety for traditional Medicare beneficiaries.1 Since 2012, the program has reduced payments to institutions with excess inpatient rehospitalizations within 30 days of an index inpatient stay for targeted medical conditions. Observation hospitalizations, billed as outpatient and covered under Medicare Part B, are not counted as index or 30-day rehospitalizations under HRRP methods. Historically, observation occurred almost exclusively in observation units. Now, observation hospitalizations commonly occur on hospital wards, even in intensive care units, and are often clinically indistinguishable from inpatient hospitalizations billed under Medicare Part A.2 The Centers for Medicare & Medicaid Services (CMS) state that beneficiaries expected to need 2 or more midnights of hospital care should generally be considered inpatients, yet observation hospitalizations commonly exceed 2 midnights.3,4
The increasing use of observation hospitalizations5,6 raises questions about its impact on HRRP measurements. While observation hospitalizations have been studied as part of 30-day follow-up (numerator) to index inpatient hospitalizations,5,6 little is known about how observation hospitalizations impact rates when they are factored in as both index stays (denominator) and in the 30-day rehospitalization rate (numerator).2,7 We analyzed the complete combinations of observation and inpatient hospitalizations, including observation as index hospitalization, rehospitalization, or both, to determine HRRP impact.
METHODS
Study Cohort
Medicare fee-for-service standard claim files for all beneficiaries (100% population file version) were used to examine qualifying index inpatient and observation hospitalizations between January 1, 2014, and November 30, 2014, as well as 30-day inpatient and observation rehospitalizations. We used CMS’s 30-day methodology, including previously described standard exclusions (Appendix Figure),8 except for the aforementioned inclusion of observation hospitalizations. Observation hospitalizations were identified using established methods,3,9,10 excluding those observation encounters coded with revenue center code 0761 only3,10 in order to be most conservative in identifying observation hospitalizations (Appendix Figure). These methods assign hospitalization type (observation or inpatient) based on the final (billed) status. The terms hospitalization and rehospitalization refer to both inpatient and observation encounters. The University of Wisconsin Health Sciences Institutional Review Board approved this study.
Hospital Readmissions Reduction Program
Index HRRP admissions for congestive heart failure, chronic obstructive pulmonary disease, myocardial infarction, and pneumonia were examined as a prespecified subgroup.1,11 Coronary artery bypass grafting, total hip replacement, and total knee replacement were excluded in this analysis, as no crosswalk exists between International Classification of Diseases, Ninth Revision codes and Current Procedural Terminology codes for these surgical conditions.11
Analysis
Analyses were conducted at the encounter level, consistent with CMS methods.8 Descriptive statistics were used to summarize index and 30-day outcomes.
RESULTS
Of 8,859,534 index hospitalizations for any reason or diagnosis, 1,597,837 (18%) were observation and 7,261,697 (82%) were inpatient. Including all hospitalizations, 23% (390,249/1,689,609) of rehospitalizations were excluded from readmission measurement by virtue of the index hospitalization and/or 30-day rehospitalization being observation (Table 1 and Table 2).
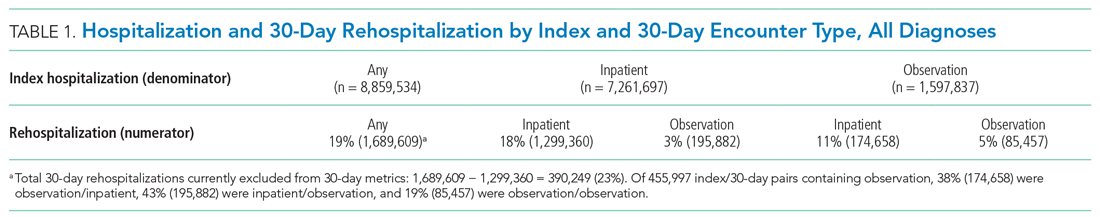
For the subgroup of HRRP conditions, 418,923 (11%) and 3,387,849 (89%) of 3,806,772 index hospitalizations were observation and inpatient, respectively. Including HRRP conditions only, 18% (155,553/876,033) of rehospitalizations were excluded from HRRP reporting owing to observation hospitalization as index, 30-day outcome, or both. Of 188,430 index/30-day pairs containing observation, 34% (63,740) were observation/inpatient, 53% (100,343) were inpatient/observation, and 13% (24,347) were observation/observation (Table 1 and Table 2).
DISCUSSION
By ignoring observation hospitalizations in 30-day HRRP quality metrics, nearly one of five potential rehospitalizations is missed. Observation hospitalizations commonly occur as either the index event or 30-day outcome, so accurately determining 30-day HRRP rates must include observation in both positions. Given hospital variability in observation use,3,7 these findings are critically important to accurately understand rehospitalization risk and indicate that HRRP may not be fulfilling its intended purpose.
Including all hospitalizations for any diagnosis, we found that observation and inpatient hospitalizations commonly occur within 30 days of each other. Nearly one in four hospitalization/rehospitalization pairs include observation as index, 30-day rehospitalization, or both. Although not directly related to HRRP metrics, these data demonstrate the growing importance and presence of outpatient (observation) hospitalizations in the Medicare program.
Our study adds to the evolving body of literature investigating quality measures under a two-tiered hospital system where inpatient hospitalizations are counted and observation hospitalizations are not. Figueroa and colleagues12 found that improvements in avoidable admission rates for patients with ambulatory care–sensitive conditions were largely attributable to a shift from counted inpatient to uncounted observation hospitalizations. In other words, hospitalizations were still occurring, but were not being tallied due to outpatient (observation) classification. Zuckerman et al5 and the Medicare Payment Advisory Commission (MedPAC)6 concluded that readmissions improvements recognized by the HRRP were not explained by a shift to more observation hospitalizations following an index inpatient hospitalization; however, both studies included observation hospitalizations as part of 30-day rehospitalization (numerator) only, not also as part of index hospitalizations (denominator). Our study confirms the importance of including observation hospitalizations in both the index (denominator) and 30-day (numerator) rehospitalization positions to determine the full impact of observation hospitalizations on Medicare’s HRRP metrics.
Our study has limitations. We focused on nonsurgical HRRP conditions, which may have impacted our findings. Additionally, some authors have suggested including emergency department (ED) visits in rehospitalization studies.7 Although ED visits occur at hospitals, they are not hospitalizations; we excluded them as a first step. Had we included ED visits, encounters excluded from HRRP measurements would have increased, suggesting that our findings, while sizeable, are likely conservative. Additionally, we could not determine the merits or medical necessity of hospitalizations (inpatient or outpatient observation), but this is an inherent limitation in a large claims dataset like this one. Finally, we only included a single year of data in this analysis, and it is possible that additional years of data would show different trends. However, we have no reason to believe the study year to be an aberrant year; if anything, observation rates have increased since 2014,6 again pointing out that while our findings are sizable, they are likely conservative. Future research could include additional years of data to confirm even greater proportions of rehospitalizations exempt from HRRP over time due to observation hospitalizations as index and/or 30-day events.
Outpatient observation hospitalizations can occur anywhere in the hospital and are often clinically similar to inpatient hospitalizations, yet observation hospitalizations are essentially invisible under inpatient quality metrics. Requiring the HRRP to include observation hospitalizations is the most obvious solution, but this could require major regulatory and legislative change11,13—change that would fix a metric but fail to address broad policy concerns inherent in the two-tiered observation and inpatient billing distinction. Instead, CMS and Congress might consider this an opportunity to address the oxymoron of “outpatient hospitalizations” by engaging in comprehensive observation reform.
1. Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP). Accessed March 12, 2021. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program
2. Sabbatini AK, Wright B. Excluding observation stays from readmission rates—what quality measures are missing. N Engl J Med. 2018;378(22):2062-2065. https://doi.org/10.1056/NEJMp1800732
3. Sheehy AM, Powell WR, Kaiksow FA, et al. Thirty-day re-observation, chronic re-observation, and neighborhood disadvantage. Mayo Clin Proc. 2020;95(12):2644-2654. https://doi.org/10.1016/j.mayocp.2020.06.059
4. US Department of Health and Human Services. Office of Inspector General. Vulnerabilities remain under Medicare’s 2-midnight hospital policy. December 19, 2016. Accessed February 11, 2021. https://oig.hhs.gov/oei/reports/oei-02-15-00020.asp
5. Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374(16):1543-1551. https://doi.org/10.1056/NEJMsa1513024
6. Medicare Payment Advisory Commission. Mandated report: the effects of the Hospital Readmissions Reduction Program. In: Report to the Congress: Medicare and the Health Care Delivery System. 2018;3-31. Accessed March 17, 2021. Available at: http://www.medpac.gov/docs/default-source/reports/jun18_medpacreporttocongress_rev_nov2019_note_sec.pdf?sfvrsn=0
7. Wadhera RK, Yeh RW, Maddox KEJ. The Hospital Readmissions Reduction Program—time for a reboot. N Engl J Med. 2019;380(24):2289-2291. https://doi.org/10.1056/NEJMp1901225
8. National Quality Forum. Measure #1789: Hospital-wide all-cause unplanned readmission measure. Accessed January 30, 2021. https://www.qualityforum.org/ProjectDescription.aspx?projectID=73619
9. Sheehy AM, Shi F, Kind AJH. Identifying observation stays in Medicare data: policy implications of a definition. J Hosp Med. 2019;14(2):96-100. https://doi.org/10.12788/jhm.3038
10. Powell WR, Kaiksow FA, Kind AJH, Sheehy AM. What is an observation stay? Evaluating the use of hospital observation stays in Medicare. J Am Geriatr Soc. 2020;68(7):1568-1572. https://doi.org/10.1111/jgs.16441
11. Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP) Archives. Accessed February 10, 2021. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/HRRP-Archives
12. Figueroa JF, Burke LG, Zheng J, Orav EJ, Jha AK. Trends in hospitalization vs observation stay for ambulatory care-sensitive conditions. JAMA Intern Med. 2019;179(12): 1714-1716. https://doi.org/10.1001/jamainternmed.2019.3177
13. Public Law 111-148, Patient Protection and Affordable Care Act, 111th Congress. March 23, 2010. Accessed March 12, 2021.https://www.congress.gov/111/plaws/publ148/PLAW-111publ148.pdf
The Hospital Readmissions Reduction Program (HRRP) was designed to improve quality and safety for traditional Medicare beneficiaries.1 Since 2012, the program has reduced payments to institutions with excess inpatient rehospitalizations within 30 days of an index inpatient stay for targeted medical conditions. Observation hospitalizations, billed as outpatient and covered under Medicare Part B, are not counted as index or 30-day rehospitalizations under HRRP methods. Historically, observation occurred almost exclusively in observation units. Now, observation hospitalizations commonly occur on hospital wards, even in intensive care units, and are often clinically indistinguishable from inpatient hospitalizations billed under Medicare Part A.2 The Centers for Medicare & Medicaid Services (CMS) state that beneficiaries expected to need 2 or more midnights of hospital care should generally be considered inpatients, yet observation hospitalizations commonly exceed 2 midnights.3,4
The increasing use of observation hospitalizations5,6 raises questions about its impact on HRRP measurements. While observation hospitalizations have been studied as part of 30-day follow-up (numerator) to index inpatient hospitalizations,5,6 little is known about how observation hospitalizations impact rates when they are factored in as both index stays (denominator) and in the 30-day rehospitalization rate (numerator).2,7 We analyzed the complete combinations of observation and inpatient hospitalizations, including observation as index hospitalization, rehospitalization, or both, to determine HRRP impact.
METHODS
Study Cohort
Medicare fee-for-service standard claim files for all beneficiaries (100% population file version) were used to examine qualifying index inpatient and observation hospitalizations between January 1, 2014, and November 30, 2014, as well as 30-day inpatient and observation rehospitalizations. We used CMS’s 30-day methodology, including previously described standard exclusions (Appendix Figure),8 except for the aforementioned inclusion of observation hospitalizations. Observation hospitalizations were identified using established methods,3,9,10 excluding those observation encounters coded with revenue center code 0761 only3,10 in order to be most conservative in identifying observation hospitalizations (Appendix Figure). These methods assign hospitalization type (observation or inpatient) based on the final (billed) status. The terms hospitalization and rehospitalization refer to both inpatient and observation encounters. The University of Wisconsin Health Sciences Institutional Review Board approved this study.
Hospital Readmissions Reduction Program
Index HRRP admissions for congestive heart failure, chronic obstructive pulmonary disease, myocardial infarction, and pneumonia were examined as a prespecified subgroup.1,11 Coronary artery bypass grafting, total hip replacement, and total knee replacement were excluded in this analysis, as no crosswalk exists between International Classification of Diseases, Ninth Revision codes and Current Procedural Terminology codes for these surgical conditions.11
Analysis
Analyses were conducted at the encounter level, consistent with CMS methods.8 Descriptive statistics were used to summarize index and 30-day outcomes.
RESULTS
Of 8,859,534 index hospitalizations for any reason or diagnosis, 1,597,837 (18%) were observation and 7,261,697 (82%) were inpatient. Including all hospitalizations, 23% (390,249/1,689,609) of rehospitalizations were excluded from readmission measurement by virtue of the index hospitalization and/or 30-day rehospitalization being observation (Table 1 and Table 2).
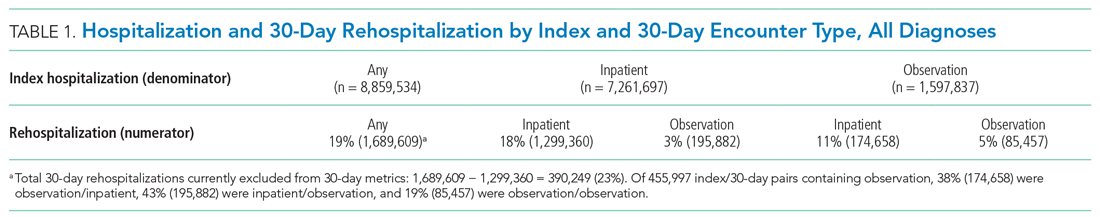
For the subgroup of HRRP conditions, 418,923 (11%) and 3,387,849 (89%) of 3,806,772 index hospitalizations were observation and inpatient, respectively. Including HRRP conditions only, 18% (155,553/876,033) of rehospitalizations were excluded from HRRP reporting owing to observation hospitalization as index, 30-day outcome, or both. Of 188,430 index/30-day pairs containing observation, 34% (63,740) were observation/inpatient, 53% (100,343) were inpatient/observation, and 13% (24,347) were observation/observation (Table 1 and Table 2).
DISCUSSION
By ignoring observation hospitalizations in 30-day HRRP quality metrics, nearly one of five potential rehospitalizations is missed. Observation hospitalizations commonly occur as either the index event or 30-day outcome, so accurately determining 30-day HRRP rates must include observation in both positions. Given hospital variability in observation use,3,7 these findings are critically important to accurately understand rehospitalization risk and indicate that HRRP may not be fulfilling its intended purpose.
Including all hospitalizations for any diagnosis, we found that observation and inpatient hospitalizations commonly occur within 30 days of each other. Nearly one in four hospitalization/rehospitalization pairs include observation as index, 30-day rehospitalization, or both. Although not directly related to HRRP metrics, these data demonstrate the growing importance and presence of outpatient (observation) hospitalizations in the Medicare program.
Our study adds to the evolving body of literature investigating quality measures under a two-tiered hospital system where inpatient hospitalizations are counted and observation hospitalizations are not. Figueroa and colleagues12 found that improvements in avoidable admission rates for patients with ambulatory care–sensitive conditions were largely attributable to a shift from counted inpatient to uncounted observation hospitalizations. In other words, hospitalizations were still occurring, but were not being tallied due to outpatient (observation) classification. Zuckerman et al5 and the Medicare Payment Advisory Commission (MedPAC)6 concluded that readmissions improvements recognized by the HRRP were not explained by a shift to more observation hospitalizations following an index inpatient hospitalization; however, both studies included observation hospitalizations as part of 30-day rehospitalization (numerator) only, not also as part of index hospitalizations (denominator). Our study confirms the importance of including observation hospitalizations in both the index (denominator) and 30-day (numerator) rehospitalization positions to determine the full impact of observation hospitalizations on Medicare’s HRRP metrics.
Our study has limitations. We focused on nonsurgical HRRP conditions, which may have impacted our findings. Additionally, some authors have suggested including emergency department (ED) visits in rehospitalization studies.7 Although ED visits occur at hospitals, they are not hospitalizations; we excluded them as a first step. Had we included ED visits, encounters excluded from HRRP measurements would have increased, suggesting that our findings, while sizeable, are likely conservative. Additionally, we could not determine the merits or medical necessity of hospitalizations (inpatient or outpatient observation), but this is an inherent limitation in a large claims dataset like this one. Finally, we only included a single year of data in this analysis, and it is possible that additional years of data would show different trends. However, we have no reason to believe the study year to be an aberrant year; if anything, observation rates have increased since 2014,6 again pointing out that while our findings are sizable, they are likely conservative. Future research could include additional years of data to confirm even greater proportions of rehospitalizations exempt from HRRP over time due to observation hospitalizations as index and/or 30-day events.
Outpatient observation hospitalizations can occur anywhere in the hospital and are often clinically similar to inpatient hospitalizations, yet observation hospitalizations are essentially invisible under inpatient quality metrics. Requiring the HRRP to include observation hospitalizations is the most obvious solution, but this could require major regulatory and legislative change11,13—change that would fix a metric but fail to address broad policy concerns inherent in the two-tiered observation and inpatient billing distinction. Instead, CMS and Congress might consider this an opportunity to address the oxymoron of “outpatient hospitalizations” by engaging in comprehensive observation reform.
The Hospital Readmissions Reduction Program (HRRP) was designed to improve quality and safety for traditional Medicare beneficiaries.1 Since 2012, the program has reduced payments to institutions with excess inpatient rehospitalizations within 30 days of an index inpatient stay for targeted medical conditions. Observation hospitalizations, billed as outpatient and covered under Medicare Part B, are not counted as index or 30-day rehospitalizations under HRRP methods. Historically, observation occurred almost exclusively in observation units. Now, observation hospitalizations commonly occur on hospital wards, even in intensive care units, and are often clinically indistinguishable from inpatient hospitalizations billed under Medicare Part A.2 The Centers for Medicare & Medicaid Services (CMS) state that beneficiaries expected to need 2 or more midnights of hospital care should generally be considered inpatients, yet observation hospitalizations commonly exceed 2 midnights.3,4
The increasing use of observation hospitalizations5,6 raises questions about its impact on HRRP measurements. While observation hospitalizations have been studied as part of 30-day follow-up (numerator) to index inpatient hospitalizations,5,6 little is known about how observation hospitalizations impact rates when they are factored in as both index stays (denominator) and in the 30-day rehospitalization rate (numerator).2,7 We analyzed the complete combinations of observation and inpatient hospitalizations, including observation as index hospitalization, rehospitalization, or both, to determine HRRP impact.
METHODS
Study Cohort
Medicare fee-for-service standard claim files for all beneficiaries (100% population file version) were used to examine qualifying index inpatient and observation hospitalizations between January 1, 2014, and November 30, 2014, as well as 30-day inpatient and observation rehospitalizations. We used CMS’s 30-day methodology, including previously described standard exclusions (Appendix Figure),8 except for the aforementioned inclusion of observation hospitalizations. Observation hospitalizations were identified using established methods,3,9,10 excluding those observation encounters coded with revenue center code 0761 only3,10 in order to be most conservative in identifying observation hospitalizations (Appendix Figure). These methods assign hospitalization type (observation or inpatient) based on the final (billed) status. The terms hospitalization and rehospitalization refer to both inpatient and observation encounters. The University of Wisconsin Health Sciences Institutional Review Board approved this study.
Hospital Readmissions Reduction Program
Index HRRP admissions for congestive heart failure, chronic obstructive pulmonary disease, myocardial infarction, and pneumonia were examined as a prespecified subgroup.1,11 Coronary artery bypass grafting, total hip replacement, and total knee replacement were excluded in this analysis, as no crosswalk exists between International Classification of Diseases, Ninth Revision codes and Current Procedural Terminology codes for these surgical conditions.11
Analysis
Analyses were conducted at the encounter level, consistent with CMS methods.8 Descriptive statistics were used to summarize index and 30-day outcomes.
RESULTS
Of 8,859,534 index hospitalizations for any reason or diagnosis, 1,597,837 (18%) were observation and 7,261,697 (82%) were inpatient. Including all hospitalizations, 23% (390,249/1,689,609) of rehospitalizations were excluded from readmission measurement by virtue of the index hospitalization and/or 30-day rehospitalization being observation (Table 1 and Table 2).
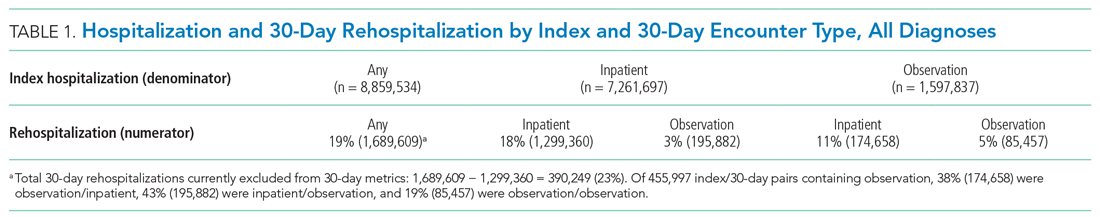
For the subgroup of HRRP conditions, 418,923 (11%) and 3,387,849 (89%) of 3,806,772 index hospitalizations were observation and inpatient, respectively. Including HRRP conditions only, 18% (155,553/876,033) of rehospitalizations were excluded from HRRP reporting owing to observation hospitalization as index, 30-day outcome, or both. Of 188,430 index/30-day pairs containing observation, 34% (63,740) were observation/inpatient, 53% (100,343) were inpatient/observation, and 13% (24,347) were observation/observation (Table 1 and Table 2).
DISCUSSION
By ignoring observation hospitalizations in 30-day HRRP quality metrics, nearly one of five potential rehospitalizations is missed. Observation hospitalizations commonly occur as either the index event or 30-day outcome, so accurately determining 30-day HRRP rates must include observation in both positions. Given hospital variability in observation use,3,7 these findings are critically important to accurately understand rehospitalization risk and indicate that HRRP may not be fulfilling its intended purpose.
Including all hospitalizations for any diagnosis, we found that observation and inpatient hospitalizations commonly occur within 30 days of each other. Nearly one in four hospitalization/rehospitalization pairs include observation as index, 30-day rehospitalization, or both. Although not directly related to HRRP metrics, these data demonstrate the growing importance and presence of outpatient (observation) hospitalizations in the Medicare program.
Our study adds to the evolving body of literature investigating quality measures under a two-tiered hospital system where inpatient hospitalizations are counted and observation hospitalizations are not. Figueroa and colleagues12 found that improvements in avoidable admission rates for patients with ambulatory care–sensitive conditions were largely attributable to a shift from counted inpatient to uncounted observation hospitalizations. In other words, hospitalizations were still occurring, but were not being tallied due to outpatient (observation) classification. Zuckerman et al5 and the Medicare Payment Advisory Commission (MedPAC)6 concluded that readmissions improvements recognized by the HRRP were not explained by a shift to more observation hospitalizations following an index inpatient hospitalization; however, both studies included observation hospitalizations as part of 30-day rehospitalization (numerator) only, not also as part of index hospitalizations (denominator). Our study confirms the importance of including observation hospitalizations in both the index (denominator) and 30-day (numerator) rehospitalization positions to determine the full impact of observation hospitalizations on Medicare’s HRRP metrics.
Our study has limitations. We focused on nonsurgical HRRP conditions, which may have impacted our findings. Additionally, some authors have suggested including emergency department (ED) visits in rehospitalization studies.7 Although ED visits occur at hospitals, they are not hospitalizations; we excluded them as a first step. Had we included ED visits, encounters excluded from HRRP measurements would have increased, suggesting that our findings, while sizeable, are likely conservative. Additionally, we could not determine the merits or medical necessity of hospitalizations (inpatient or outpatient observation), but this is an inherent limitation in a large claims dataset like this one. Finally, we only included a single year of data in this analysis, and it is possible that additional years of data would show different trends. However, we have no reason to believe the study year to be an aberrant year; if anything, observation rates have increased since 2014,6 again pointing out that while our findings are sizable, they are likely conservative. Future research could include additional years of data to confirm even greater proportions of rehospitalizations exempt from HRRP over time due to observation hospitalizations as index and/or 30-day events.
Outpatient observation hospitalizations can occur anywhere in the hospital and are often clinically similar to inpatient hospitalizations, yet observation hospitalizations are essentially invisible under inpatient quality metrics. Requiring the HRRP to include observation hospitalizations is the most obvious solution, but this could require major regulatory and legislative change11,13—change that would fix a metric but fail to address broad policy concerns inherent in the two-tiered observation and inpatient billing distinction. Instead, CMS and Congress might consider this an opportunity to address the oxymoron of “outpatient hospitalizations” by engaging in comprehensive observation reform.
1. Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP). Accessed March 12, 2021. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program
2. Sabbatini AK, Wright B. Excluding observation stays from readmission rates—what quality measures are missing. N Engl J Med. 2018;378(22):2062-2065. https://doi.org/10.1056/NEJMp1800732
3. Sheehy AM, Powell WR, Kaiksow FA, et al. Thirty-day re-observation, chronic re-observation, and neighborhood disadvantage. Mayo Clin Proc. 2020;95(12):2644-2654. https://doi.org/10.1016/j.mayocp.2020.06.059
4. US Department of Health and Human Services. Office of Inspector General. Vulnerabilities remain under Medicare’s 2-midnight hospital policy. December 19, 2016. Accessed February 11, 2021. https://oig.hhs.gov/oei/reports/oei-02-15-00020.asp
5. Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374(16):1543-1551. https://doi.org/10.1056/NEJMsa1513024
6. Medicare Payment Advisory Commission. Mandated report: the effects of the Hospital Readmissions Reduction Program. In: Report to the Congress: Medicare and the Health Care Delivery System. 2018;3-31. Accessed March 17, 2021. Available at: http://www.medpac.gov/docs/default-source/reports/jun18_medpacreporttocongress_rev_nov2019_note_sec.pdf?sfvrsn=0
7. Wadhera RK, Yeh RW, Maddox KEJ. The Hospital Readmissions Reduction Program—time for a reboot. N Engl J Med. 2019;380(24):2289-2291. https://doi.org/10.1056/NEJMp1901225
8. National Quality Forum. Measure #1789: Hospital-wide all-cause unplanned readmission measure. Accessed January 30, 2021. https://www.qualityforum.org/ProjectDescription.aspx?projectID=73619
9. Sheehy AM, Shi F, Kind AJH. Identifying observation stays in Medicare data: policy implications of a definition. J Hosp Med. 2019;14(2):96-100. https://doi.org/10.12788/jhm.3038
10. Powell WR, Kaiksow FA, Kind AJH, Sheehy AM. What is an observation stay? Evaluating the use of hospital observation stays in Medicare. J Am Geriatr Soc. 2020;68(7):1568-1572. https://doi.org/10.1111/jgs.16441
11. Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP) Archives. Accessed February 10, 2021. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/HRRP-Archives
12. Figueroa JF, Burke LG, Zheng J, Orav EJ, Jha AK. Trends in hospitalization vs observation stay for ambulatory care-sensitive conditions. JAMA Intern Med. 2019;179(12): 1714-1716. https://doi.org/10.1001/jamainternmed.2019.3177
13. Public Law 111-148, Patient Protection and Affordable Care Act, 111th Congress. March 23, 2010. Accessed March 12, 2021.https://www.congress.gov/111/plaws/publ148/PLAW-111publ148.pdf
1. Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP). Accessed March 12, 2021. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program
2. Sabbatini AK, Wright B. Excluding observation stays from readmission rates—what quality measures are missing. N Engl J Med. 2018;378(22):2062-2065. https://doi.org/10.1056/NEJMp1800732
3. Sheehy AM, Powell WR, Kaiksow FA, et al. Thirty-day re-observation, chronic re-observation, and neighborhood disadvantage. Mayo Clin Proc. 2020;95(12):2644-2654. https://doi.org/10.1016/j.mayocp.2020.06.059
4. US Department of Health and Human Services. Office of Inspector General. Vulnerabilities remain under Medicare’s 2-midnight hospital policy. December 19, 2016. Accessed February 11, 2021. https://oig.hhs.gov/oei/reports/oei-02-15-00020.asp
5. Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374(16):1543-1551. https://doi.org/10.1056/NEJMsa1513024
6. Medicare Payment Advisory Commission. Mandated report: the effects of the Hospital Readmissions Reduction Program. In: Report to the Congress: Medicare and the Health Care Delivery System. 2018;3-31. Accessed March 17, 2021. Available at: http://www.medpac.gov/docs/default-source/reports/jun18_medpacreporttocongress_rev_nov2019_note_sec.pdf?sfvrsn=0
7. Wadhera RK, Yeh RW, Maddox KEJ. The Hospital Readmissions Reduction Program—time for a reboot. N Engl J Med. 2019;380(24):2289-2291. https://doi.org/10.1056/NEJMp1901225
8. National Quality Forum. Measure #1789: Hospital-wide all-cause unplanned readmission measure. Accessed January 30, 2021. https://www.qualityforum.org/ProjectDescription.aspx?projectID=73619
9. Sheehy AM, Shi F, Kind AJH. Identifying observation stays in Medicare data: policy implications of a definition. J Hosp Med. 2019;14(2):96-100. https://doi.org/10.12788/jhm.3038
10. Powell WR, Kaiksow FA, Kind AJH, Sheehy AM. What is an observation stay? Evaluating the use of hospital observation stays in Medicare. J Am Geriatr Soc. 2020;68(7):1568-1572. https://doi.org/10.1111/jgs.16441
11. Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP) Archives. Accessed February 10, 2021. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/HRRP-Archives
12. Figueroa JF, Burke LG, Zheng J, Orav EJ, Jha AK. Trends in hospitalization vs observation stay for ambulatory care-sensitive conditions. JAMA Intern Med. 2019;179(12): 1714-1716. https://doi.org/10.1001/jamainternmed.2019.3177
13. Public Law 111-148, Patient Protection and Affordable Care Act, 111th Congress. March 23, 2010. Accessed March 12, 2021.https://www.congress.gov/111/plaws/publ148/PLAW-111publ148.pdf
© 2021 Society of Hospital Medicine
Improving Healthcare Value: COVID-19 Emergency Regulatory Relief and Implications for Post-Acute Skilled Nursing Facility Care
Medicare beneficiary who requires skilled care in a nursing home? Better be admitted for at least 3 days in the hospital first if you want the nursing home paid for. Govt doesn’t always make sense. We’re listening to feedback.
—Centers for Medicare & Medicaid Services Administrator Seema Verma, @SeemaCMS, August 4, 2019, via Twitter.1
On March 13, 2020, the president of the United States declared a national health emergency, granting the secretary of the United States Department of Health & Human Services authority to grant waivers intended to ease certain Medicare and Medicaid program requirements.2 Broad waiver categories include those that may be requested by an individual institution, as well as “COVID-19 Emergency Declaration Blanket Waivers,” which automatically apply across all facilities and providers. As stated by the Centers for Medicare & Medicaid Services (CMS), waivers are intended to create “regulatory flexibilities to help healthcare providers contain the spread of 2019 Novel Coronavirus Disease (COVID-19).” These provisions are retroactive to March 1, 2020, expire at the end of the “emergency period or 60 days from the date the waiver . . . is first published” and can be extended by the secretary.2
The issued blanket waivers remove administrative requirements in a wide range of care settings including home health, hospice, hospitals, and skilled nursing facilities (SNF), among others. The waiving of many of these administrative requirements are welcomed by providers and administrators alike in this time of national crisis. For example, relaxation of verbal order signage requirements and expanded coverage of telehealth will, almost certainly, improve accessibility, efficiency, and requisite coordination and care across settings. Emergence of these new “COVID-19” waivers also present rare and valuable opportunities to examine care improvement in areas long believed to need permanent regulatory change. Perhaps the most important of these long over-due changes is the current CMS process for determining Part A eligibility for post-acute skilled nursing facility coverage for traditional Medicare beneficiaries following an inpatient hospitalization. Under COVID-19, CMS has now granted a waiver that “authorizes the Secretary to provide for Skilled Nursing Facilities (SNF) coverage in the absence of a qualifying [three consecutive inpatient midnight] hospital stay. . . .”2 Although demand for SNF placement may shift during the pandemic, hospitals facing capacity issues will more easily be able to discharge Medicare beneficiaries ready for post-acute care.
POST-ACUTE SKILLED NURSING FACILITY COVERAGE
When Medicare was established in 1965, approximately half of Americans over age 65 did not have health insurance, and older adults were the most likely demographic to be living in poverty.3 Originally called “Hospital Insurance” or “Medicare Part A,” these “Inpatient Hospital Services” are described in Social Security statute as “items and services furnished to an inpatient of a hospital” including room and board, nursing services, pharmaceuticals, and medical and surgical services delivered in the hospital.4 In 1967, Medicare beneficiaries staying three consecutive inpatient hospital midnights were also afforded post-acute SNF coverage for up to 100 days. As expected, hospital use increased as seniors had coverage for hospital care and were also, in many cases, able to access higher quality post-hospital care.5
Over the past 50 years, two important changes have shifted Medicare beneficiary SNF coverage. First, due to efficiencies and changes in care delivery, average length of hospital stay for Americans over age 65 has shrunk from 14 days in 1965 to approximately 5 days currently.5,6 Now, fewer beneficiaries spend the necessary three or more nights in the hospital to qualify for post-acute SNF coverage. Second, and most importantly, CMS created “observation status” in the 1980s, which allowed for patients to be observed as “outpatients” in a hospital instead of as inpatients. Notably, these observation nights fall under outpatient status (Part B), and therefore do not count toward the statutory SNF coverage requirement of three inpatient midnights.
According to CMS, observation should be used so that a “decision can be made regarding whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital. . . . In the majority of cases, the decision can be made in less than 48 hours, usually in less than 24 hours.”7 At the time of its development, this concept fit the growing use of Emergency Department observation units, in which patients presented for an acute issue but could usually discharge home in the stated time frame.
OBSERVATION CARE
In reality, outpatient (observation) status is not synonymous with observation units. Because observation is a billing determination, not a specific type of clinical care, observation care may be delivered anywhere in a hospital—including an observation unit, a hospital ward, or even an intensive care unit (ICU). While all hospitals may deliver observation care, only about one-third of hospitals have observation units, and even hospitals with observation units deliver observation care outside of these units. Traditional Medicare beneficiaries who stay three or more nights in the hospital but cannot meet the three inpatient midnight requirement to access their SNF coverage benefits because of outpatient (observation) nights are often left vulnerable and confused, saddling them with an average of $10,503 for each uncovered SNF stay.8 As emergent evidence demonstrates striking racial, geographic, and socioeconomic-based health disparities in COVID-19, renewal of the “three-midnight rule” could have disproportionate and long-lasting ramifications for these populations in particular.9
Hospital observation stays (or observation nights) can look identical to inpatient hospital stays, as defined by the Social Security statute4; yet never count toward the three-inpatient-midnight tally. In 2014, the Office of Inspector General (OIG) found there were 633,148 hospital stays that lasted three midnights or longer but did not contain three consecutive inpatient midnights, which resulted in nonqualifying stays for purposes of SNF coverage, if that coverage was needed.10 A more recent OIG report found that Medicare was paying erroneously for some SNF stays because even CMS could not distinguish between three midnights that were all inpatient or a combination of inpatient and observation.11 Additionally, because care provided is often indistinguishable, status changes between outpatient and inpatient are common; in 2014, 40% of Medicare observation stays occurring within 30 days of an inpatient stay changed to inpatient over the course of a single hospitalization.12 Now, in the time of COVID-19, this untenable decades-long problem has the potential to be definitively addressed by a permanent removal of the three midnight requirement altogether.
PROGRESS TOWARD REFORM
Several recent signals suggest that change is supported by a diverse group of stakeholders. In their 2019 Top 25 Unimplemented Recommendations, the OIG acknowledged the similarity in observation and inpatient care, recommending that “CMS . . . analyze the potential impacts of counting time spent as an outpatient toward the 3-night requirement for skilled nursing facility (SNF) services so that beneficiaries receiving similar hospital care have similar access to these services.”13 The “Improving Access to Medicare Coverage Act of 2019,” reintroduced in the 116th Congress, would count all midnights spent in the hospital, whether those nights are inpatient or observation, toward the three midnight requirement.14 This bill has bipartisan, bicameral support, which demonstrates unified legislative interest across the political spectrum. More recently in March 2020, a federal judge in the class action lawsuit Alexander v Azar determined that Medicare beneficiaries had the right to appeal to Medicare if a physician placed a patient in inpatient status and this decision was overturned administratively by a hospital, resulting in loss of a beneficiary’s SNF coverage.15 Although now under appeal, this judicial decision signals the importance of beneficiary rights to appeal directly to CMS.
Given the mounting support for reform, it is probable that cost concerns and allocation of resources to the Part A vs Part B “buckets” remain the only barrier to permanently reforming the three-midnight inpatient stay policy. Pilot programs testing Medicare SNF waivers more than 30 years ago suggested increased cost and SNF usage.16 However, more contemporary experience from Medicare Advantage programs suggest just the opposite. Grebla et al showed there was no increased SNF use nor SNF length of stay for beneficiaries in Medicare Advantage plans that waived the three inpatient midnight requirement.17
Arguably, the current COVID-19 emergency blanket SNF waiver is not a perfect test of short- or long-term Medicare costs. First, factors such as reduced hospital elective surgeries that may typically drive post-acute SNF admissions, as well as potentially reduced SNF utilization caused by fear of COVID-19 outbreaks, may temporarily lower SNF use and associated Medicare expenditures. The existing waiver of statute is also financially constrained, stipulating that “this action does not increase overall program payments. . . .”2 Longer term, innovations in care delivery prompted by accelerated telehealth reforms may shift more post-acute care from SNFs to the home setting, changing patterns of SNF utilization altogether. Despite these limitations, this regulatory relief will still provide valuable utilization and cost information on SNF use under a system absent the three-midnight requirement.
CONCLUSION
Rarely, if ever, does a national healthcare system experience such a rapid and marked change as that seen with the COVID-19 pandemic. Despite the tragic emergency circumstances prompting CMS’s blanket waivers, it provides CMS and stakeholders with a rare opportunity to evaluate potential improvements revealed by each individual aspect of COVID-19 regulatory relief. CMS has in the past argued the three-midnight SNF requirement is a statutory issue and thus not within their control, yet they have used their regulatory authority to waive this policy to facilitate efficient care in a national health crisis. This is a change that many believe is long overdue, and one that should be maintained even after COVID-19 abates. “Govt doesn’t always make sense,” as Administrator Verma wrote,1 should be a cry for government to make better sense of existing legislation and regulation. Reform of the three-midnight inpatient rule is the right place to start.
1. @SeemaCMS. #Medicare beneficiary who requires skilled care in a nursing home? Better be admitted for at least 3 days in the hospital first if you want the nursing home paid for. [Flushed face emoji] Govt doesn’t always make sense. We’re listening to feedback. #RedTapeTales #TheBoldAndTheBureaucratic. August 4, 2019. Accessed April 17, 2020. https://twitter.com/SeemaCMS/status/1158029830056828928
2. COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers. Centers for Medicare & Medicaid Services, US Dept of Health & Human Services; 2020. Accessed April 17, 2020. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf
3. Medicare & Medicaid Milestones, 1937 to 2015. Centers for Medicare and Medicaid Services, US Dept of Health & Human Services; 2015. Accessed April 17, 2020. https://www.cms.gov/About-CMS/Agency-Information/History/Downloads/Medicare-and-Medicaid-Milestones-1937-2015.pdf
4. Social Security Laws, 42 USC 1395x §1861 (1965). Accessed April 17, 2020. https://www.ssa.gov/OP_Home/ssact/title18/1861.htm
5. Loewenstein R. Early effects of Medicare on the health care of the aged. Social Security Bulletin. April 1971; pp 3-20, 42. Accessed April 14, 2020. https://www.ssa.gov/policy/docs/ssb/v34n4/v34n4p3.pdf
6. Weiss AJ, Elixhauser A. Overview of Hospital Stays in the United States, 2012. Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality, US Dept of Health & Human Services; 2014. Accessed April 16, 2020. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb180-Hospitalizations-United-States-2012.pdf
7. Medicare Benefits Policy Manual, Internet-Only Manuals. Centers for Medicare & Medicaid Services. Pub. 100-02, Chapter 6, § 20.6. Updated April 5, 2012. Accessed April 17, 2020. http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Internet-Only-Manuals-IOMs.html
8. Wright S. Hospitals’ Use of Observation Stays and Short Inpatient Stays for Medicare Beneficiaries. Office of the Inspector General, US Dept of Health & Human Services; 2014. Accessed April 16, 2020. https://oig.hhs.gov/oei/reports/oei-02-12-00040.asp
9. Yancy CW. COVID-19 and African Americans. JAMA. Published online April 15, 2020. https://doi.org/10.1001/jama.2020.6548
10. Levinson DR. Vulnerabilities Remain Under Medicare’s 2-Midnight Hospital Policy. Office of the Inspector General, US Dept of Health & Human Services; 2016. Accessed April 18, 2020. https://oig.hhs.gov/oei/reports/oei-02-15-00020.pdf
11. Levinson DR. CMS Improperly Paid Millions of Dollars for Skilled Nursing Facility Services When the Medicare 3-Day Inpatient Hospital Stay Requirement Was Not Met. Office of the Inspector General, US Dept of Health & Human Services; 2019. Accessed April 16, 2020. https://www.oig.hhs.gov/oas/reports/region5/51600043.pdf
12. Sheehy A, Shi F, Kind A. Identifying observation stays in Medicare data: policy implications of a definition. J Hosp Med. 2019;14(2):96-100. https://doi.org/10.12788/jhm.3038
13. Solutions to Reduce Fraud, Waste, and Abuse in HHS Programs: OIG’s Top Recommendations. Office of the Inspector General, US Dept of Health & Human Services; 2019. Accessed April 18, 2020. https://oig.hhs.gov/reports-and-publications/compendium/files/compendium2019.pdf
14. Improving Access to Medicare Coverage Act of 2019, HR 1682, 116th Congress (2019). Accessed April 16, 2020. https://www.congress.gov/bill/116th-congress/house-bill/1682
15. Alexander v Azar, 396 F Supp 3d 242 (D CT 2019). Accessed May 26, 2020. https://casetext.com/case/alexander-v-azar-1?
16. Lipsitz L. The 3-night hospital stay and Medicare coverage for skilled nursing care. JAMA. 2013;310(14):1441-1442. https://doi.org/10.1001/jama.2013.254845
17. Grebla R, Keohane L, Lee Y, Lipsitz L, Rahman M, Trevedi A. Waiving the three-day rule: admissions and length-of-stay at hospitals and skilled nursing facilities did not increase. Health Affairs (Millwood). 2015;34(8):1324-1330. https://doi.org/10.1377/hlthaff.2015.0054
Medicare beneficiary who requires skilled care in a nursing home? Better be admitted for at least 3 days in the hospital first if you want the nursing home paid for. Govt doesn’t always make sense. We’re listening to feedback.
—Centers for Medicare & Medicaid Services Administrator Seema Verma, @SeemaCMS, August 4, 2019, via Twitter.1
On March 13, 2020, the president of the United States declared a national health emergency, granting the secretary of the United States Department of Health & Human Services authority to grant waivers intended to ease certain Medicare and Medicaid program requirements.2 Broad waiver categories include those that may be requested by an individual institution, as well as “COVID-19 Emergency Declaration Blanket Waivers,” which automatically apply across all facilities and providers. As stated by the Centers for Medicare & Medicaid Services (CMS), waivers are intended to create “regulatory flexibilities to help healthcare providers contain the spread of 2019 Novel Coronavirus Disease (COVID-19).” These provisions are retroactive to March 1, 2020, expire at the end of the “emergency period or 60 days from the date the waiver . . . is first published” and can be extended by the secretary.2
The issued blanket waivers remove administrative requirements in a wide range of care settings including home health, hospice, hospitals, and skilled nursing facilities (SNF), among others. The waiving of many of these administrative requirements are welcomed by providers and administrators alike in this time of national crisis. For example, relaxation of verbal order signage requirements and expanded coverage of telehealth will, almost certainly, improve accessibility, efficiency, and requisite coordination and care across settings. Emergence of these new “COVID-19” waivers also present rare and valuable opportunities to examine care improvement in areas long believed to need permanent regulatory change. Perhaps the most important of these long over-due changes is the current CMS process for determining Part A eligibility for post-acute skilled nursing facility coverage for traditional Medicare beneficiaries following an inpatient hospitalization. Under COVID-19, CMS has now granted a waiver that “authorizes the Secretary to provide for Skilled Nursing Facilities (SNF) coverage in the absence of a qualifying [three consecutive inpatient midnight] hospital stay. . . .”2 Although demand for SNF placement may shift during the pandemic, hospitals facing capacity issues will more easily be able to discharge Medicare beneficiaries ready for post-acute care.
POST-ACUTE SKILLED NURSING FACILITY COVERAGE
When Medicare was established in 1965, approximately half of Americans over age 65 did not have health insurance, and older adults were the most likely demographic to be living in poverty.3 Originally called “Hospital Insurance” or “Medicare Part A,” these “Inpatient Hospital Services” are described in Social Security statute as “items and services furnished to an inpatient of a hospital” including room and board, nursing services, pharmaceuticals, and medical and surgical services delivered in the hospital.4 In 1967, Medicare beneficiaries staying three consecutive inpatient hospital midnights were also afforded post-acute SNF coverage for up to 100 days. As expected, hospital use increased as seniors had coverage for hospital care and were also, in many cases, able to access higher quality post-hospital care.5
Over the past 50 years, two important changes have shifted Medicare beneficiary SNF coverage. First, due to efficiencies and changes in care delivery, average length of hospital stay for Americans over age 65 has shrunk from 14 days in 1965 to approximately 5 days currently.5,6 Now, fewer beneficiaries spend the necessary three or more nights in the hospital to qualify for post-acute SNF coverage. Second, and most importantly, CMS created “observation status” in the 1980s, which allowed for patients to be observed as “outpatients” in a hospital instead of as inpatients. Notably, these observation nights fall under outpatient status (Part B), and therefore do not count toward the statutory SNF coverage requirement of three inpatient midnights.
According to CMS, observation should be used so that a “decision can be made regarding whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital. . . . In the majority of cases, the decision can be made in less than 48 hours, usually in less than 24 hours.”7 At the time of its development, this concept fit the growing use of Emergency Department observation units, in which patients presented for an acute issue but could usually discharge home in the stated time frame.
OBSERVATION CARE
In reality, outpatient (observation) status is not synonymous with observation units. Because observation is a billing determination, not a specific type of clinical care, observation care may be delivered anywhere in a hospital—including an observation unit, a hospital ward, or even an intensive care unit (ICU). While all hospitals may deliver observation care, only about one-third of hospitals have observation units, and even hospitals with observation units deliver observation care outside of these units. Traditional Medicare beneficiaries who stay three or more nights in the hospital but cannot meet the three inpatient midnight requirement to access their SNF coverage benefits because of outpatient (observation) nights are often left vulnerable and confused, saddling them with an average of $10,503 for each uncovered SNF stay.8 As emergent evidence demonstrates striking racial, geographic, and socioeconomic-based health disparities in COVID-19, renewal of the “three-midnight rule” could have disproportionate and long-lasting ramifications for these populations in particular.9
Hospital observation stays (or observation nights) can look identical to inpatient hospital stays, as defined by the Social Security statute4; yet never count toward the three-inpatient-midnight tally. In 2014, the Office of Inspector General (OIG) found there were 633,148 hospital stays that lasted three midnights or longer but did not contain three consecutive inpatient midnights, which resulted in nonqualifying stays for purposes of SNF coverage, if that coverage was needed.10 A more recent OIG report found that Medicare was paying erroneously for some SNF stays because even CMS could not distinguish between three midnights that were all inpatient or a combination of inpatient and observation.11 Additionally, because care provided is often indistinguishable, status changes between outpatient and inpatient are common; in 2014, 40% of Medicare observation stays occurring within 30 days of an inpatient stay changed to inpatient over the course of a single hospitalization.12 Now, in the time of COVID-19, this untenable decades-long problem has the potential to be definitively addressed by a permanent removal of the three midnight requirement altogether.
PROGRESS TOWARD REFORM
Several recent signals suggest that change is supported by a diverse group of stakeholders. In their 2019 Top 25 Unimplemented Recommendations, the OIG acknowledged the similarity in observation and inpatient care, recommending that “CMS . . . analyze the potential impacts of counting time spent as an outpatient toward the 3-night requirement for skilled nursing facility (SNF) services so that beneficiaries receiving similar hospital care have similar access to these services.”13 The “Improving Access to Medicare Coverage Act of 2019,” reintroduced in the 116th Congress, would count all midnights spent in the hospital, whether those nights are inpatient or observation, toward the three midnight requirement.14 This bill has bipartisan, bicameral support, which demonstrates unified legislative interest across the political spectrum. More recently in March 2020, a federal judge in the class action lawsuit Alexander v Azar determined that Medicare beneficiaries had the right to appeal to Medicare if a physician placed a patient in inpatient status and this decision was overturned administratively by a hospital, resulting in loss of a beneficiary’s SNF coverage.15 Although now under appeal, this judicial decision signals the importance of beneficiary rights to appeal directly to CMS.
Given the mounting support for reform, it is probable that cost concerns and allocation of resources to the Part A vs Part B “buckets” remain the only barrier to permanently reforming the three-midnight inpatient stay policy. Pilot programs testing Medicare SNF waivers more than 30 years ago suggested increased cost and SNF usage.16 However, more contemporary experience from Medicare Advantage programs suggest just the opposite. Grebla et al showed there was no increased SNF use nor SNF length of stay for beneficiaries in Medicare Advantage plans that waived the three inpatient midnight requirement.17
Arguably, the current COVID-19 emergency blanket SNF waiver is not a perfect test of short- or long-term Medicare costs. First, factors such as reduced hospital elective surgeries that may typically drive post-acute SNF admissions, as well as potentially reduced SNF utilization caused by fear of COVID-19 outbreaks, may temporarily lower SNF use and associated Medicare expenditures. The existing waiver of statute is also financially constrained, stipulating that “this action does not increase overall program payments. . . .”2 Longer term, innovations in care delivery prompted by accelerated telehealth reforms may shift more post-acute care from SNFs to the home setting, changing patterns of SNF utilization altogether. Despite these limitations, this regulatory relief will still provide valuable utilization and cost information on SNF use under a system absent the three-midnight requirement.
CONCLUSION
Rarely, if ever, does a national healthcare system experience such a rapid and marked change as that seen with the COVID-19 pandemic. Despite the tragic emergency circumstances prompting CMS’s blanket waivers, it provides CMS and stakeholders with a rare opportunity to evaluate potential improvements revealed by each individual aspect of COVID-19 regulatory relief. CMS has in the past argued the three-midnight SNF requirement is a statutory issue and thus not within their control, yet they have used their regulatory authority to waive this policy to facilitate efficient care in a national health crisis. This is a change that many believe is long overdue, and one that should be maintained even after COVID-19 abates. “Govt doesn’t always make sense,” as Administrator Verma wrote,1 should be a cry for government to make better sense of existing legislation and regulation. Reform of the three-midnight inpatient rule is the right place to start.
Medicare beneficiary who requires skilled care in a nursing home? Better be admitted for at least 3 days in the hospital first if you want the nursing home paid for. Govt doesn’t always make sense. We’re listening to feedback.
—Centers for Medicare & Medicaid Services Administrator Seema Verma, @SeemaCMS, August 4, 2019, via Twitter.1
On March 13, 2020, the president of the United States declared a national health emergency, granting the secretary of the United States Department of Health & Human Services authority to grant waivers intended to ease certain Medicare and Medicaid program requirements.2 Broad waiver categories include those that may be requested by an individual institution, as well as “COVID-19 Emergency Declaration Blanket Waivers,” which automatically apply across all facilities and providers. As stated by the Centers for Medicare & Medicaid Services (CMS), waivers are intended to create “regulatory flexibilities to help healthcare providers contain the spread of 2019 Novel Coronavirus Disease (COVID-19).” These provisions are retroactive to March 1, 2020, expire at the end of the “emergency period or 60 days from the date the waiver . . . is first published” and can be extended by the secretary.2
The issued blanket waivers remove administrative requirements in a wide range of care settings including home health, hospice, hospitals, and skilled nursing facilities (SNF), among others. The waiving of many of these administrative requirements are welcomed by providers and administrators alike in this time of national crisis. For example, relaxation of verbal order signage requirements and expanded coverage of telehealth will, almost certainly, improve accessibility, efficiency, and requisite coordination and care across settings. Emergence of these new “COVID-19” waivers also present rare and valuable opportunities to examine care improvement in areas long believed to need permanent regulatory change. Perhaps the most important of these long over-due changes is the current CMS process for determining Part A eligibility for post-acute skilled nursing facility coverage for traditional Medicare beneficiaries following an inpatient hospitalization. Under COVID-19, CMS has now granted a waiver that “authorizes the Secretary to provide for Skilled Nursing Facilities (SNF) coverage in the absence of a qualifying [three consecutive inpatient midnight] hospital stay. . . .”2 Although demand for SNF placement may shift during the pandemic, hospitals facing capacity issues will more easily be able to discharge Medicare beneficiaries ready for post-acute care.
POST-ACUTE SKILLED NURSING FACILITY COVERAGE
When Medicare was established in 1965, approximately half of Americans over age 65 did not have health insurance, and older adults were the most likely demographic to be living in poverty.3 Originally called “Hospital Insurance” or “Medicare Part A,” these “Inpatient Hospital Services” are described in Social Security statute as “items and services furnished to an inpatient of a hospital” including room and board, nursing services, pharmaceuticals, and medical and surgical services delivered in the hospital.4 In 1967, Medicare beneficiaries staying three consecutive inpatient hospital midnights were also afforded post-acute SNF coverage for up to 100 days. As expected, hospital use increased as seniors had coverage for hospital care and were also, in many cases, able to access higher quality post-hospital care.5
Over the past 50 years, two important changes have shifted Medicare beneficiary SNF coverage. First, due to efficiencies and changes in care delivery, average length of hospital stay for Americans over age 65 has shrunk from 14 days in 1965 to approximately 5 days currently.5,6 Now, fewer beneficiaries spend the necessary three or more nights in the hospital to qualify for post-acute SNF coverage. Second, and most importantly, CMS created “observation status” in the 1980s, which allowed for patients to be observed as “outpatients” in a hospital instead of as inpatients. Notably, these observation nights fall under outpatient status (Part B), and therefore do not count toward the statutory SNF coverage requirement of three inpatient midnights.
According to CMS, observation should be used so that a “decision can be made regarding whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital. . . . In the majority of cases, the decision can be made in less than 48 hours, usually in less than 24 hours.”7 At the time of its development, this concept fit the growing use of Emergency Department observation units, in which patients presented for an acute issue but could usually discharge home in the stated time frame.
OBSERVATION CARE
In reality, outpatient (observation) status is not synonymous with observation units. Because observation is a billing determination, not a specific type of clinical care, observation care may be delivered anywhere in a hospital—including an observation unit, a hospital ward, or even an intensive care unit (ICU). While all hospitals may deliver observation care, only about one-third of hospitals have observation units, and even hospitals with observation units deliver observation care outside of these units. Traditional Medicare beneficiaries who stay three or more nights in the hospital but cannot meet the three inpatient midnight requirement to access their SNF coverage benefits because of outpatient (observation) nights are often left vulnerable and confused, saddling them with an average of $10,503 for each uncovered SNF stay.8 As emergent evidence demonstrates striking racial, geographic, and socioeconomic-based health disparities in COVID-19, renewal of the “three-midnight rule” could have disproportionate and long-lasting ramifications for these populations in particular.9
Hospital observation stays (or observation nights) can look identical to inpatient hospital stays, as defined by the Social Security statute4; yet never count toward the three-inpatient-midnight tally. In 2014, the Office of Inspector General (OIG) found there were 633,148 hospital stays that lasted three midnights or longer but did not contain three consecutive inpatient midnights, which resulted in nonqualifying stays for purposes of SNF coverage, if that coverage was needed.10 A more recent OIG report found that Medicare was paying erroneously for some SNF stays because even CMS could not distinguish between three midnights that were all inpatient or a combination of inpatient and observation.11 Additionally, because care provided is often indistinguishable, status changes between outpatient and inpatient are common; in 2014, 40% of Medicare observation stays occurring within 30 days of an inpatient stay changed to inpatient over the course of a single hospitalization.12 Now, in the time of COVID-19, this untenable decades-long problem has the potential to be definitively addressed by a permanent removal of the three midnight requirement altogether.
PROGRESS TOWARD REFORM
Several recent signals suggest that change is supported by a diverse group of stakeholders. In their 2019 Top 25 Unimplemented Recommendations, the OIG acknowledged the similarity in observation and inpatient care, recommending that “CMS . . . analyze the potential impacts of counting time spent as an outpatient toward the 3-night requirement for skilled nursing facility (SNF) services so that beneficiaries receiving similar hospital care have similar access to these services.”13 The “Improving Access to Medicare Coverage Act of 2019,” reintroduced in the 116th Congress, would count all midnights spent in the hospital, whether those nights are inpatient or observation, toward the three midnight requirement.14 This bill has bipartisan, bicameral support, which demonstrates unified legislative interest across the political spectrum. More recently in March 2020, a federal judge in the class action lawsuit Alexander v Azar determined that Medicare beneficiaries had the right to appeal to Medicare if a physician placed a patient in inpatient status and this decision was overturned administratively by a hospital, resulting in loss of a beneficiary’s SNF coverage.15 Although now under appeal, this judicial decision signals the importance of beneficiary rights to appeal directly to CMS.
Given the mounting support for reform, it is probable that cost concerns and allocation of resources to the Part A vs Part B “buckets” remain the only barrier to permanently reforming the three-midnight inpatient stay policy. Pilot programs testing Medicare SNF waivers more than 30 years ago suggested increased cost and SNF usage.16 However, more contemporary experience from Medicare Advantage programs suggest just the opposite. Grebla et al showed there was no increased SNF use nor SNF length of stay for beneficiaries in Medicare Advantage plans that waived the three inpatient midnight requirement.17
Arguably, the current COVID-19 emergency blanket SNF waiver is not a perfect test of short- or long-term Medicare costs. First, factors such as reduced hospital elective surgeries that may typically drive post-acute SNF admissions, as well as potentially reduced SNF utilization caused by fear of COVID-19 outbreaks, may temporarily lower SNF use and associated Medicare expenditures. The existing waiver of statute is also financially constrained, stipulating that “this action does not increase overall program payments. . . .”2 Longer term, innovations in care delivery prompted by accelerated telehealth reforms may shift more post-acute care from SNFs to the home setting, changing patterns of SNF utilization altogether. Despite these limitations, this regulatory relief will still provide valuable utilization and cost information on SNF use under a system absent the three-midnight requirement.
CONCLUSION
Rarely, if ever, does a national healthcare system experience such a rapid and marked change as that seen with the COVID-19 pandemic. Despite the tragic emergency circumstances prompting CMS’s blanket waivers, it provides CMS and stakeholders with a rare opportunity to evaluate potential improvements revealed by each individual aspect of COVID-19 regulatory relief. CMS has in the past argued the three-midnight SNF requirement is a statutory issue and thus not within their control, yet they have used their regulatory authority to waive this policy to facilitate efficient care in a national health crisis. This is a change that many believe is long overdue, and one that should be maintained even after COVID-19 abates. “Govt doesn’t always make sense,” as Administrator Verma wrote,1 should be a cry for government to make better sense of existing legislation and regulation. Reform of the three-midnight inpatient rule is the right place to start.
1. @SeemaCMS. #Medicare beneficiary who requires skilled care in a nursing home? Better be admitted for at least 3 days in the hospital first if you want the nursing home paid for. [Flushed face emoji] Govt doesn’t always make sense. We’re listening to feedback. #RedTapeTales #TheBoldAndTheBureaucratic. August 4, 2019. Accessed April 17, 2020. https://twitter.com/SeemaCMS/status/1158029830056828928
2. COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers. Centers for Medicare & Medicaid Services, US Dept of Health & Human Services; 2020. Accessed April 17, 2020. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf
3. Medicare & Medicaid Milestones, 1937 to 2015. Centers for Medicare and Medicaid Services, US Dept of Health & Human Services; 2015. Accessed April 17, 2020. https://www.cms.gov/About-CMS/Agency-Information/History/Downloads/Medicare-and-Medicaid-Milestones-1937-2015.pdf
4. Social Security Laws, 42 USC 1395x §1861 (1965). Accessed April 17, 2020. https://www.ssa.gov/OP_Home/ssact/title18/1861.htm
5. Loewenstein R. Early effects of Medicare on the health care of the aged. Social Security Bulletin. April 1971; pp 3-20, 42. Accessed April 14, 2020. https://www.ssa.gov/policy/docs/ssb/v34n4/v34n4p3.pdf
6. Weiss AJ, Elixhauser A. Overview of Hospital Stays in the United States, 2012. Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality, US Dept of Health & Human Services; 2014. Accessed April 16, 2020. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb180-Hospitalizations-United-States-2012.pdf
7. Medicare Benefits Policy Manual, Internet-Only Manuals. Centers for Medicare & Medicaid Services. Pub. 100-02, Chapter 6, § 20.6. Updated April 5, 2012. Accessed April 17, 2020. http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Internet-Only-Manuals-IOMs.html
8. Wright S. Hospitals’ Use of Observation Stays and Short Inpatient Stays for Medicare Beneficiaries. Office of the Inspector General, US Dept of Health & Human Services; 2014. Accessed April 16, 2020. https://oig.hhs.gov/oei/reports/oei-02-12-00040.asp
9. Yancy CW. COVID-19 and African Americans. JAMA. Published online April 15, 2020. https://doi.org/10.1001/jama.2020.6548
10. Levinson DR. Vulnerabilities Remain Under Medicare’s 2-Midnight Hospital Policy. Office of the Inspector General, US Dept of Health & Human Services; 2016. Accessed April 18, 2020. https://oig.hhs.gov/oei/reports/oei-02-15-00020.pdf
11. Levinson DR. CMS Improperly Paid Millions of Dollars for Skilled Nursing Facility Services When the Medicare 3-Day Inpatient Hospital Stay Requirement Was Not Met. Office of the Inspector General, US Dept of Health & Human Services; 2019. Accessed April 16, 2020. https://www.oig.hhs.gov/oas/reports/region5/51600043.pdf
12. Sheehy A, Shi F, Kind A. Identifying observation stays in Medicare data: policy implications of a definition. J Hosp Med. 2019;14(2):96-100. https://doi.org/10.12788/jhm.3038
13. Solutions to Reduce Fraud, Waste, and Abuse in HHS Programs: OIG’s Top Recommendations. Office of the Inspector General, US Dept of Health & Human Services; 2019. Accessed April 18, 2020. https://oig.hhs.gov/reports-and-publications/compendium/files/compendium2019.pdf
14. Improving Access to Medicare Coverage Act of 2019, HR 1682, 116th Congress (2019). Accessed April 16, 2020. https://www.congress.gov/bill/116th-congress/house-bill/1682
15. Alexander v Azar, 396 F Supp 3d 242 (D CT 2019). Accessed May 26, 2020. https://casetext.com/case/alexander-v-azar-1?
16. Lipsitz L. The 3-night hospital stay and Medicare coverage for skilled nursing care. JAMA. 2013;310(14):1441-1442. https://doi.org/10.1001/jama.2013.254845
17. Grebla R, Keohane L, Lee Y, Lipsitz L, Rahman M, Trevedi A. Waiving the three-day rule: admissions and length-of-stay at hospitals and skilled nursing facilities did not increase. Health Affairs (Millwood). 2015;34(8):1324-1330. https://doi.org/10.1377/hlthaff.2015.0054
1. @SeemaCMS. #Medicare beneficiary who requires skilled care in a nursing home? Better be admitted for at least 3 days in the hospital first if you want the nursing home paid for. [Flushed face emoji] Govt doesn’t always make sense. We’re listening to feedback. #RedTapeTales #TheBoldAndTheBureaucratic. August 4, 2019. Accessed April 17, 2020. https://twitter.com/SeemaCMS/status/1158029830056828928
2. COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers. Centers for Medicare & Medicaid Services, US Dept of Health & Human Services; 2020. Accessed April 17, 2020. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf
3. Medicare & Medicaid Milestones, 1937 to 2015. Centers for Medicare and Medicaid Services, US Dept of Health & Human Services; 2015. Accessed April 17, 2020. https://www.cms.gov/About-CMS/Agency-Information/History/Downloads/Medicare-and-Medicaid-Milestones-1937-2015.pdf
4. Social Security Laws, 42 USC 1395x §1861 (1965). Accessed April 17, 2020. https://www.ssa.gov/OP_Home/ssact/title18/1861.htm
5. Loewenstein R. Early effects of Medicare on the health care of the aged. Social Security Bulletin. April 1971; pp 3-20, 42. Accessed April 14, 2020. https://www.ssa.gov/policy/docs/ssb/v34n4/v34n4p3.pdf
6. Weiss AJ, Elixhauser A. Overview of Hospital Stays in the United States, 2012. Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality, US Dept of Health & Human Services; 2014. Accessed April 16, 2020. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb180-Hospitalizations-United-States-2012.pdf
7. Medicare Benefits Policy Manual, Internet-Only Manuals. Centers for Medicare & Medicaid Services. Pub. 100-02, Chapter 6, § 20.6. Updated April 5, 2012. Accessed April 17, 2020. http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Internet-Only-Manuals-IOMs.html
8. Wright S. Hospitals’ Use of Observation Stays and Short Inpatient Stays for Medicare Beneficiaries. Office of the Inspector General, US Dept of Health & Human Services; 2014. Accessed April 16, 2020. https://oig.hhs.gov/oei/reports/oei-02-12-00040.asp
9. Yancy CW. COVID-19 and African Americans. JAMA. Published online April 15, 2020. https://doi.org/10.1001/jama.2020.6548
10. Levinson DR. Vulnerabilities Remain Under Medicare’s 2-Midnight Hospital Policy. Office of the Inspector General, US Dept of Health & Human Services; 2016. Accessed April 18, 2020. https://oig.hhs.gov/oei/reports/oei-02-15-00020.pdf
11. Levinson DR. CMS Improperly Paid Millions of Dollars for Skilled Nursing Facility Services When the Medicare 3-Day Inpatient Hospital Stay Requirement Was Not Met. Office of the Inspector General, US Dept of Health & Human Services; 2019. Accessed April 16, 2020. https://www.oig.hhs.gov/oas/reports/region5/51600043.pdf
12. Sheehy A, Shi F, Kind A. Identifying observation stays in Medicare data: policy implications of a definition. J Hosp Med. 2019;14(2):96-100. https://doi.org/10.12788/jhm.3038
13. Solutions to Reduce Fraud, Waste, and Abuse in HHS Programs: OIG’s Top Recommendations. Office of the Inspector General, US Dept of Health & Human Services; 2019. Accessed April 18, 2020. https://oig.hhs.gov/reports-and-publications/compendium/files/compendium2019.pdf
14. Improving Access to Medicare Coverage Act of 2019, HR 1682, 116th Congress (2019). Accessed April 16, 2020. https://www.congress.gov/bill/116th-congress/house-bill/1682
15. Alexander v Azar, 396 F Supp 3d 242 (D CT 2019). Accessed May 26, 2020. https://casetext.com/case/alexander-v-azar-1?
16. Lipsitz L. The 3-night hospital stay and Medicare coverage for skilled nursing care. JAMA. 2013;310(14):1441-1442. https://doi.org/10.1001/jama.2013.254845
17. Grebla R, Keohane L, Lee Y, Lipsitz L, Rahman M, Trevedi A. Waiving the three-day rule: admissions and length-of-stay at hospitals and skilled nursing facilities did not increase. Health Affairs (Millwood). 2015;34(8):1324-1330. https://doi.org/10.1377/hlthaff.2015.0054
© 2020 Society of Hospital Medicine
Policy in Clinical Practice: Medicare Advantage and Observation Hospitalizations
CLINICAL SCENARIO
A 73-year-old man presents to the emergency department with sepsis secondary to community-acquired pneumonia. The patient requires supplemental oxygen and is started on intravenous antibiotics. His admitting physician expects he will need more than two nights of hospital care and suggests that inpatient status, rather than outpatient (observation) status, would be appropriate under Medicare’s “Two-Midnight Rule.” The physician also suspects the patient may need a brief stay in a skilled nursing facility (SNF) following the mentioned hospitalization and notes that the patient has a Medicare Advantage plan (Table) and wonders if the Two-Midnight Rule applies. Further, she questions whether Medicare’s “Three-Midnight Rule” for SNF benefits will factor in the patient’s discharge planning.
BACKGROUND AND HISTORY
Since the 1970s, the Centers for Medicare & Medicaid Services (CMS) has allowed enrollees to receive their Medicare benefits from privately managed health plans through the so-called Medicare Advantage programs. CMS contracts with commercial insurers who, in exchange for a set payment per Medicare enrollee, “accept full responsibility (ie, risk) for the costs of their enrollees’ care.”1 Over the past 20 years the percent of Medicare Advantage enrollees has nearly doubled nationwide, from 18% to 34%, and is projected to grow even further to 42% by 2028.2,3 The reasons beneficiaries choose to enroll in Medicare Advantage over Traditional Medicare have yet to be thoroughly studied; ease of enrollment and plan administration, as well as lower deductibles, copays, and out-of-pocket maximums for in-network services, are thought to be some of the driving factors.
The federal government has asserted two goals for the development of Medicare Advantage: beneficiary choice and economic efficiency.1 Medicare Advantage plans must be actuarially equal to Traditional Medicare but do not have to cover services in precisely the same way. Medicare Advantage plans may achieve cost savings through narrower networks, strict control of access to SNF services and acute care inpatient rehabilitation, and prior authorization requirements, the latter of which has received recent congressional attention.4,5 On the other hand, many Medicare Advantage plans offer dental, fitness, optical, and caregiver benefits that are not included under Traditional Medicare. Beneficiaries can theoretically compare the coverage and costs of Traditional Medicare to Medicare Advantage programs and make informed choices based on their individualized needs. The second stated goal for the Medicare Advantage option assumes that privately managed plans provide care at lower costs compared with CMS; this assumption has yet to be confirmed with solid data. Indeed, a recent analysis comparing the overall costs of Medicare Advantage to those of Traditional Medicare concluded that Medicare Advantage costs CMS more than Traditional Medicare,6 perhaps in part due to risk adjustment practices.7
POLICY IN PRACTICE
There are a number of areas of uncertainty regarding the specifics of how Medicare Advantage plans work, including Medicare Advantage programs’ use of outpatient (observation) stays. CMS has tried to provide guidance to healthcare organizations and clinicians regarding the appropriate use of inpatient hospitalizations for patients with Traditional Medicare, including the implementation of the Two-Midnight Rule in 2013. According to the rule, clinicians should place inpatient admission orders when they reasonably expect a patient’s care to extend across two midnights.8 Such admission decisions are subject to review by Medicare contractors and Quality Improvement Organizations.
In contrast, Medicare Advantage plans which enter into contracts with specific healthcare systems are not required to abide by CMS’ guidelines for the Two-Midnight Rule.9 When Medicare Advantage firms negotiate contracts with individual hospitals and healthcare organizations, CMS has been clear that such contracts are not required to include the Two-Midnight Rule when it comes to making hospitalization status decisions.10 Instead, in these instances, Medicare Advantage plans often use proprietary decision tools containing clinical criteria, such as Milliman Care Guidelines or InterQual, and/or their own plan’s internal criteria as part of the decision-making process to grant inpatient or outpatient (observation) status. More importantly, CMS has stated that for hospitals and healthcare systems that do not contract with Medicare Advantage programs, the Two-Midnight Rule should apply when it comes to making hospitalization status decisions.10
Implications for Patients
Currently, there are no data available to compare between Medicare Advantage enrollees and traditional medicine beneficiaries in terms of the frequency of observation use and out-of-pocket cost for observation stays. As alluded to in the patient’s case, the use of outpatient (observation) status has implications for a patient’s posthospitalization SNF benefit. Under Traditional Medicare, patients must be hospitalized for three consecutive inpatient midnights in order to qualify for the SNF benefit. Time spent under outpatient (observation) status does not count toward this three-day requirement. Interestingly, some Medicare Advantage programs have demonstrated innovation in this area, waiving the three inpatient midnight requirement for their beneficiaries;11 there is evidence, however, that compared with their Traditional Medicare counterparts, Medicare Advantage beneficiaries are admitted to lower quality SNFs.12 The posthospitalization consequences of an inpatient versus outpatient (observation) status determination for a Medicare Advantage beneficiary is thus unclear, further complicating the decision-making process for patients when it comes to choosing a Medicare policy, and for providers when it comes to choosing an admission status.
Implications for Clinicians and Healthcare Systems
After performing an initial history and physical exam, if a healthcare provider determines that a patient requires hospitalization, an order is placed to classify the stay as inpatient or outpatient (observation). For beneficiaries with Traditional Medicare or a Medicare Advantage plan that has not contracted with the hospital, clinicians should follow the Two-Midnight Rule for making this determination. For contracted Medicare Advantage, the rules are variable. Under Medicare’s Conditions of Participation, hospitals and healthcare organizations are required to have utilization management (UM) programs to assist physicians in making appropriate admission decisions. UM reviews can happen at any point during or after a patient’s stay, however, and physicians may have to make decisions using their best judgment at the time of admission without real-time input from UM teams.
Outpatient (observation) care and the challenges surrounding appropriate status orders have complicated the admission decision. In one study of 2014 Traditional Medicare claims, almost half of outpatient (observation) stays contained a status change.13 Based on a recent survey of hospitalist physicians, about two-thirds of hospitalists report at least monthly requests from patients to change their status.14 Hospital medicine physicians report that these requests “can severely damage the therapeutic bond”14 between provider and patient because the provider must assign status based on CMS rules, not patient request.
COMMENTARY AND RECOMMENDATIONS
CMS could improve the current system in one of two ways. First, CMS could require that all Medicare Advantage plans follow the same polices as Traditional Medicare policies regarding the Two- and Three-Midnight Rules. This would eliminate the need for both hospitals and healthcare organizations to dedicate time and resources to negotiating with each Medicare Advantage program and to managing each Medicare Advantage patient admission based on a specific contract. Ideally, CMS could completely eliminate its outpatient (observation) policy so that all hospitalizations are treated exactly the same, classified under the same billing status and with beneficiaries having the same postacute benefit. This would be consistent with the sentiment behind the recent Office of Inspector General’s (OIG) report suggesting that CMS consider counting outpatient midnights toward the three-midnight requirement for postacute SNF care “so that beneficiaries receiving similar hospital care have similar access to these services.”15
WHAT SHOULD I TELL MY PATIENT?
The physician in the example above should tell their patient that they will be admitted as an inpatient given her expectation that the patient will need hospitalization for oxygen support, parenteral antibiotics, and evaluation by physical therapy to determine a medically appropriate discharge plan. The physician should document the medical necessity for the admission, specifically her expectation that the patient will require at least two midnights of medically necessary hospital care. If the patient has Traditional Medicare, this documentation, along with the inpatient status order, will fulfill the requirements for an inpatient stay. If the patient has a Medicare Advantage plan, the physician can advise the patient that the plan administrators will ultimately determine if an inpatient stay will be covered or denied.
CONCLUSIONS
In the proposed clinical scenario, the rules determining the patient’s hospitalization status depend on whether the hospital contracts with the patient’s Medicare Advantage plan, and if so, what the contracted criteria are in determining inpatient and outpatient (observation) status. The physician could consider real-time input from the hospital’s UM team, if available. Regardless of UM input, if the physician hospitalizes the patient as an inpatient, the Medicare Advantage plan administrators will make a determination regarding the appropriateness of the admission status, as well as whether the patient qualifies for posthospitalization Medicare SNF benefits (if requested) and, additionally, which SNFs will be covered. If denied, the hospitalist will have the option of a peer-to-peer discussion with the insurance company to overturn the denial. Given the confusion, complexity, and implications presented by this admission status decision-making process, standardization across Traditional Medicare and Medicare Advantage plans, or a budget-neutral plan to eliminate status distinction altogether, is certainly warranted.
1.McGuire TG, Newhouse JP, Sinaiko AD. An economic history of Medicare Part C. Millbank Q. 2011;89(2):289-332. https://doi.org/10.1111/j.1468-0009.2011.00629.x.
2. Medicare Advantage. Available at: https://www.kff.org/medicare/fact-sheet/medicare-advantage/.
3. Neuman P, Jacobson G. Medicare Advantage checkup. N Engl J Med. 2018;379(22):2163-2172. https://doi.org/10.1056/NEJMhpr1804089.
4. HR 3107: improving seniors’ timely access to Care Act of 2019. Available at: https://www.congress.gov/bill/116th-congress/house-bill/3107/text?q=%7B%22search%22%3A%5B%22prior+authorization%22%5D%7D&r=1&s=1.
5. Gadbois EA, Tyler DA, Shield RR, et al. Medicare Advantage control of postacute costs: perspective from stakeholders. Am J Manag Care. 2018;24(12):e386-e392.
6. Rooke-Ley H, Broome T, Mostashari F, Cavanaugh S. Evaluating Medicare programs against saving taxpayer dollars. Health Affairs, August 16, 2019. Available at: https://www.healthaffairs.org/do/10.1377/hblog20190813.223707/full/.
7. Office of Inspector General. Billions in estimated Medicare Advantage payments from chart reviews raise concerns. December 2019. Available at: https://oig.hhs.gov/oei/reports/oei-03-17-00470.pdf. Accessed December 15, 2019.
8. Fact sheet: two-midnight rule. Available at: https://www.cms.gov/newsroom/fact-sheets/fact-sheet-two-midnight-rule-0.
9. Locke C, Hu E. Medicare’s two-midnight rule: what hospitalists must know. Available at: https://www.the-hospitalist.org/hospitalist/article/194971/medicares-two-midnight-rule.
10. Announcement of calendar year (CY) 2019 Medicare Advantage capitation rates and Medicare Advantage and part D payment policies and final call letter. Page 206. Available at: https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Downloads/Announcement2019.pdf. Accessed November 18, 2019.
11. Grebla R, Keohane L, Lee Y, Lipsitz L, Rahman M, Trivedi A. Waiving the three-day rule: admissions and length-of-stay at hospitals and skilled nursing facilities did not increase. Health Aff. 2015;34(8):1324-1330. https://doi.org/10.1377/hlthaff.2015.0054.
12. Meyers D, Mor V, Rahman M. Medicare Advantage enrollees more likely to enter lower-quality nursing homes compared to fee-for-service enrollees. Health Aff. 2018;37(1):78-85. https://doi.org/10.1377/hlthaff.2017.0714.
13. Sheehy A, Shi F, Kind AJH. Identifying observation stays in Medicare data: Policy implications of a definition. J Hosp Med. 2019;14(2):96-100. https://doi.org/10.12788/jhm.3038
14. The hospital observation care problem: perspectives and solutions from the Society of Hospital Medicine. Available at: https://www.hospitalmedicine.org/globalassets/policy-and-advocacy/advocacy-pdf/shms-observation-white-paper-2017. Accessed November 18, 2019.
15. U.S. Department of Health & Human Services, Office of Inspector General. Solutions to reduce fraud, waste and abuse in HHS programs: OIG’s top recommendations. Available at: https://oig.hhs.gov/reports-and-publications/compendium/. Accessed November 22, 2019.
CLINICAL SCENARIO
A 73-year-old man presents to the emergency department with sepsis secondary to community-acquired pneumonia. The patient requires supplemental oxygen and is started on intravenous antibiotics. His admitting physician expects he will need more than two nights of hospital care and suggests that inpatient status, rather than outpatient (observation) status, would be appropriate under Medicare’s “Two-Midnight Rule.” The physician also suspects the patient may need a brief stay in a skilled nursing facility (SNF) following the mentioned hospitalization and notes that the patient has a Medicare Advantage plan (Table) and wonders if the Two-Midnight Rule applies. Further, she questions whether Medicare’s “Three-Midnight Rule” for SNF benefits will factor in the patient’s discharge planning.
BACKGROUND AND HISTORY
Since the 1970s, the Centers for Medicare & Medicaid Services (CMS) has allowed enrollees to receive their Medicare benefits from privately managed health plans through the so-called Medicare Advantage programs. CMS contracts with commercial insurers who, in exchange for a set payment per Medicare enrollee, “accept full responsibility (ie, risk) for the costs of their enrollees’ care.”1 Over the past 20 years the percent of Medicare Advantage enrollees has nearly doubled nationwide, from 18% to 34%, and is projected to grow even further to 42% by 2028.2,3 The reasons beneficiaries choose to enroll in Medicare Advantage over Traditional Medicare have yet to be thoroughly studied; ease of enrollment and plan administration, as well as lower deductibles, copays, and out-of-pocket maximums for in-network services, are thought to be some of the driving factors.
The federal government has asserted two goals for the development of Medicare Advantage: beneficiary choice and economic efficiency.1 Medicare Advantage plans must be actuarially equal to Traditional Medicare but do not have to cover services in precisely the same way. Medicare Advantage plans may achieve cost savings through narrower networks, strict control of access to SNF services and acute care inpatient rehabilitation, and prior authorization requirements, the latter of which has received recent congressional attention.4,5 On the other hand, many Medicare Advantage plans offer dental, fitness, optical, and caregiver benefits that are not included under Traditional Medicare. Beneficiaries can theoretically compare the coverage and costs of Traditional Medicare to Medicare Advantage programs and make informed choices based on their individualized needs. The second stated goal for the Medicare Advantage option assumes that privately managed plans provide care at lower costs compared with CMS; this assumption has yet to be confirmed with solid data. Indeed, a recent analysis comparing the overall costs of Medicare Advantage to those of Traditional Medicare concluded that Medicare Advantage costs CMS more than Traditional Medicare,6 perhaps in part due to risk adjustment practices.7
POLICY IN PRACTICE
There are a number of areas of uncertainty regarding the specifics of how Medicare Advantage plans work, including Medicare Advantage programs’ use of outpatient (observation) stays. CMS has tried to provide guidance to healthcare organizations and clinicians regarding the appropriate use of inpatient hospitalizations for patients with Traditional Medicare, including the implementation of the Two-Midnight Rule in 2013. According to the rule, clinicians should place inpatient admission orders when they reasonably expect a patient’s care to extend across two midnights.8 Such admission decisions are subject to review by Medicare contractors and Quality Improvement Organizations.
In contrast, Medicare Advantage plans which enter into contracts with specific healthcare systems are not required to abide by CMS’ guidelines for the Two-Midnight Rule.9 When Medicare Advantage firms negotiate contracts with individual hospitals and healthcare organizations, CMS has been clear that such contracts are not required to include the Two-Midnight Rule when it comes to making hospitalization status decisions.10 Instead, in these instances, Medicare Advantage plans often use proprietary decision tools containing clinical criteria, such as Milliman Care Guidelines or InterQual, and/or their own plan’s internal criteria as part of the decision-making process to grant inpatient or outpatient (observation) status. More importantly, CMS has stated that for hospitals and healthcare systems that do not contract with Medicare Advantage programs, the Two-Midnight Rule should apply when it comes to making hospitalization status decisions.10
Implications for Patients
Currently, there are no data available to compare between Medicare Advantage enrollees and traditional medicine beneficiaries in terms of the frequency of observation use and out-of-pocket cost for observation stays. As alluded to in the patient’s case, the use of outpatient (observation) status has implications for a patient’s posthospitalization SNF benefit. Under Traditional Medicare, patients must be hospitalized for three consecutive inpatient midnights in order to qualify for the SNF benefit. Time spent under outpatient (observation) status does not count toward this three-day requirement. Interestingly, some Medicare Advantage programs have demonstrated innovation in this area, waiving the three inpatient midnight requirement for their beneficiaries;11 there is evidence, however, that compared with their Traditional Medicare counterparts, Medicare Advantage beneficiaries are admitted to lower quality SNFs.12 The posthospitalization consequences of an inpatient versus outpatient (observation) status determination for a Medicare Advantage beneficiary is thus unclear, further complicating the decision-making process for patients when it comes to choosing a Medicare policy, and for providers when it comes to choosing an admission status.
Implications for Clinicians and Healthcare Systems
After performing an initial history and physical exam, if a healthcare provider determines that a patient requires hospitalization, an order is placed to classify the stay as inpatient or outpatient (observation). For beneficiaries with Traditional Medicare or a Medicare Advantage plan that has not contracted with the hospital, clinicians should follow the Two-Midnight Rule for making this determination. For contracted Medicare Advantage, the rules are variable. Under Medicare’s Conditions of Participation, hospitals and healthcare organizations are required to have utilization management (UM) programs to assist physicians in making appropriate admission decisions. UM reviews can happen at any point during or after a patient’s stay, however, and physicians may have to make decisions using their best judgment at the time of admission without real-time input from UM teams.
Outpatient (observation) care and the challenges surrounding appropriate status orders have complicated the admission decision. In one study of 2014 Traditional Medicare claims, almost half of outpatient (observation) stays contained a status change.13 Based on a recent survey of hospitalist physicians, about two-thirds of hospitalists report at least monthly requests from patients to change their status.14 Hospital medicine physicians report that these requests “can severely damage the therapeutic bond”14 between provider and patient because the provider must assign status based on CMS rules, not patient request.
COMMENTARY AND RECOMMENDATIONS
CMS could improve the current system in one of two ways. First, CMS could require that all Medicare Advantage plans follow the same polices as Traditional Medicare policies regarding the Two- and Three-Midnight Rules. This would eliminate the need for both hospitals and healthcare organizations to dedicate time and resources to negotiating with each Medicare Advantage program and to managing each Medicare Advantage patient admission based on a specific contract. Ideally, CMS could completely eliminate its outpatient (observation) policy so that all hospitalizations are treated exactly the same, classified under the same billing status and with beneficiaries having the same postacute benefit. This would be consistent with the sentiment behind the recent Office of Inspector General’s (OIG) report suggesting that CMS consider counting outpatient midnights toward the three-midnight requirement for postacute SNF care “so that beneficiaries receiving similar hospital care have similar access to these services.”15
WHAT SHOULD I TELL MY PATIENT?
The physician in the example above should tell their patient that they will be admitted as an inpatient given her expectation that the patient will need hospitalization for oxygen support, parenteral antibiotics, and evaluation by physical therapy to determine a medically appropriate discharge plan. The physician should document the medical necessity for the admission, specifically her expectation that the patient will require at least two midnights of medically necessary hospital care. If the patient has Traditional Medicare, this documentation, along with the inpatient status order, will fulfill the requirements for an inpatient stay. If the patient has a Medicare Advantage plan, the physician can advise the patient that the plan administrators will ultimately determine if an inpatient stay will be covered or denied.
CONCLUSIONS
In the proposed clinical scenario, the rules determining the patient’s hospitalization status depend on whether the hospital contracts with the patient’s Medicare Advantage plan, and if so, what the contracted criteria are in determining inpatient and outpatient (observation) status. The physician could consider real-time input from the hospital’s UM team, if available. Regardless of UM input, if the physician hospitalizes the patient as an inpatient, the Medicare Advantage plan administrators will make a determination regarding the appropriateness of the admission status, as well as whether the patient qualifies for posthospitalization Medicare SNF benefits (if requested) and, additionally, which SNFs will be covered. If denied, the hospitalist will have the option of a peer-to-peer discussion with the insurance company to overturn the denial. Given the confusion, complexity, and implications presented by this admission status decision-making process, standardization across Traditional Medicare and Medicare Advantage plans, or a budget-neutral plan to eliminate status distinction altogether, is certainly warranted.
CLINICAL SCENARIO
A 73-year-old man presents to the emergency department with sepsis secondary to community-acquired pneumonia. The patient requires supplemental oxygen and is started on intravenous antibiotics. His admitting physician expects he will need more than two nights of hospital care and suggests that inpatient status, rather than outpatient (observation) status, would be appropriate under Medicare’s “Two-Midnight Rule.” The physician also suspects the patient may need a brief stay in a skilled nursing facility (SNF) following the mentioned hospitalization and notes that the patient has a Medicare Advantage plan (Table) and wonders if the Two-Midnight Rule applies. Further, she questions whether Medicare’s “Three-Midnight Rule” for SNF benefits will factor in the patient’s discharge planning.
BACKGROUND AND HISTORY
Since the 1970s, the Centers for Medicare & Medicaid Services (CMS) has allowed enrollees to receive their Medicare benefits from privately managed health plans through the so-called Medicare Advantage programs. CMS contracts with commercial insurers who, in exchange for a set payment per Medicare enrollee, “accept full responsibility (ie, risk) for the costs of their enrollees’ care.”1 Over the past 20 years the percent of Medicare Advantage enrollees has nearly doubled nationwide, from 18% to 34%, and is projected to grow even further to 42% by 2028.2,3 The reasons beneficiaries choose to enroll in Medicare Advantage over Traditional Medicare have yet to be thoroughly studied; ease of enrollment and plan administration, as well as lower deductibles, copays, and out-of-pocket maximums for in-network services, are thought to be some of the driving factors.
The federal government has asserted two goals for the development of Medicare Advantage: beneficiary choice and economic efficiency.1 Medicare Advantage plans must be actuarially equal to Traditional Medicare but do not have to cover services in precisely the same way. Medicare Advantage plans may achieve cost savings through narrower networks, strict control of access to SNF services and acute care inpatient rehabilitation, and prior authorization requirements, the latter of which has received recent congressional attention.4,5 On the other hand, many Medicare Advantage plans offer dental, fitness, optical, and caregiver benefits that are not included under Traditional Medicare. Beneficiaries can theoretically compare the coverage and costs of Traditional Medicare to Medicare Advantage programs and make informed choices based on their individualized needs. The second stated goal for the Medicare Advantage option assumes that privately managed plans provide care at lower costs compared with CMS; this assumption has yet to be confirmed with solid data. Indeed, a recent analysis comparing the overall costs of Medicare Advantage to those of Traditional Medicare concluded that Medicare Advantage costs CMS more than Traditional Medicare,6 perhaps in part due to risk adjustment practices.7
POLICY IN PRACTICE
There are a number of areas of uncertainty regarding the specifics of how Medicare Advantage plans work, including Medicare Advantage programs’ use of outpatient (observation) stays. CMS has tried to provide guidance to healthcare organizations and clinicians regarding the appropriate use of inpatient hospitalizations for patients with Traditional Medicare, including the implementation of the Two-Midnight Rule in 2013. According to the rule, clinicians should place inpatient admission orders when they reasonably expect a patient’s care to extend across two midnights.8 Such admission decisions are subject to review by Medicare contractors and Quality Improvement Organizations.
In contrast, Medicare Advantage plans which enter into contracts with specific healthcare systems are not required to abide by CMS’ guidelines for the Two-Midnight Rule.9 When Medicare Advantage firms negotiate contracts with individual hospitals and healthcare organizations, CMS has been clear that such contracts are not required to include the Two-Midnight Rule when it comes to making hospitalization status decisions.10 Instead, in these instances, Medicare Advantage plans often use proprietary decision tools containing clinical criteria, such as Milliman Care Guidelines or InterQual, and/or their own plan’s internal criteria as part of the decision-making process to grant inpatient or outpatient (observation) status. More importantly, CMS has stated that for hospitals and healthcare systems that do not contract with Medicare Advantage programs, the Two-Midnight Rule should apply when it comes to making hospitalization status decisions.10
Implications for Patients
Currently, there are no data available to compare between Medicare Advantage enrollees and traditional medicine beneficiaries in terms of the frequency of observation use and out-of-pocket cost for observation stays. As alluded to in the patient’s case, the use of outpatient (observation) status has implications for a patient’s posthospitalization SNF benefit. Under Traditional Medicare, patients must be hospitalized for three consecutive inpatient midnights in order to qualify for the SNF benefit. Time spent under outpatient (observation) status does not count toward this three-day requirement. Interestingly, some Medicare Advantage programs have demonstrated innovation in this area, waiving the three inpatient midnight requirement for their beneficiaries;11 there is evidence, however, that compared with their Traditional Medicare counterparts, Medicare Advantage beneficiaries are admitted to lower quality SNFs.12 The posthospitalization consequences of an inpatient versus outpatient (observation) status determination for a Medicare Advantage beneficiary is thus unclear, further complicating the decision-making process for patients when it comes to choosing a Medicare policy, and for providers when it comes to choosing an admission status.
Implications for Clinicians and Healthcare Systems
After performing an initial history and physical exam, if a healthcare provider determines that a patient requires hospitalization, an order is placed to classify the stay as inpatient or outpatient (observation). For beneficiaries with Traditional Medicare or a Medicare Advantage plan that has not contracted with the hospital, clinicians should follow the Two-Midnight Rule for making this determination. For contracted Medicare Advantage, the rules are variable. Under Medicare’s Conditions of Participation, hospitals and healthcare organizations are required to have utilization management (UM) programs to assist physicians in making appropriate admission decisions. UM reviews can happen at any point during or after a patient’s stay, however, and physicians may have to make decisions using their best judgment at the time of admission without real-time input from UM teams.
Outpatient (observation) care and the challenges surrounding appropriate status orders have complicated the admission decision. In one study of 2014 Traditional Medicare claims, almost half of outpatient (observation) stays contained a status change.13 Based on a recent survey of hospitalist physicians, about two-thirds of hospitalists report at least monthly requests from patients to change their status.14 Hospital medicine physicians report that these requests “can severely damage the therapeutic bond”14 between provider and patient because the provider must assign status based on CMS rules, not patient request.
COMMENTARY AND RECOMMENDATIONS
CMS could improve the current system in one of two ways. First, CMS could require that all Medicare Advantage plans follow the same polices as Traditional Medicare policies regarding the Two- and Three-Midnight Rules. This would eliminate the need for both hospitals and healthcare organizations to dedicate time and resources to negotiating with each Medicare Advantage program and to managing each Medicare Advantage patient admission based on a specific contract. Ideally, CMS could completely eliminate its outpatient (observation) policy so that all hospitalizations are treated exactly the same, classified under the same billing status and with beneficiaries having the same postacute benefit. This would be consistent with the sentiment behind the recent Office of Inspector General’s (OIG) report suggesting that CMS consider counting outpatient midnights toward the three-midnight requirement for postacute SNF care “so that beneficiaries receiving similar hospital care have similar access to these services.”15
WHAT SHOULD I TELL MY PATIENT?
The physician in the example above should tell their patient that they will be admitted as an inpatient given her expectation that the patient will need hospitalization for oxygen support, parenteral antibiotics, and evaluation by physical therapy to determine a medically appropriate discharge plan. The physician should document the medical necessity for the admission, specifically her expectation that the patient will require at least two midnights of medically necessary hospital care. If the patient has Traditional Medicare, this documentation, along with the inpatient status order, will fulfill the requirements for an inpatient stay. If the patient has a Medicare Advantage plan, the physician can advise the patient that the plan administrators will ultimately determine if an inpatient stay will be covered or denied.
CONCLUSIONS
In the proposed clinical scenario, the rules determining the patient’s hospitalization status depend on whether the hospital contracts with the patient’s Medicare Advantage plan, and if so, what the contracted criteria are in determining inpatient and outpatient (observation) status. The physician could consider real-time input from the hospital’s UM team, if available. Regardless of UM input, if the physician hospitalizes the patient as an inpatient, the Medicare Advantage plan administrators will make a determination regarding the appropriateness of the admission status, as well as whether the patient qualifies for posthospitalization Medicare SNF benefits (if requested) and, additionally, which SNFs will be covered. If denied, the hospitalist will have the option of a peer-to-peer discussion with the insurance company to overturn the denial. Given the confusion, complexity, and implications presented by this admission status decision-making process, standardization across Traditional Medicare and Medicare Advantage plans, or a budget-neutral plan to eliminate status distinction altogether, is certainly warranted.
1.McGuire TG, Newhouse JP, Sinaiko AD. An economic history of Medicare Part C. Millbank Q. 2011;89(2):289-332. https://doi.org/10.1111/j.1468-0009.2011.00629.x.
2. Medicare Advantage. Available at: https://www.kff.org/medicare/fact-sheet/medicare-advantage/.
3. Neuman P, Jacobson G. Medicare Advantage checkup. N Engl J Med. 2018;379(22):2163-2172. https://doi.org/10.1056/NEJMhpr1804089.
4. HR 3107: improving seniors’ timely access to Care Act of 2019. Available at: https://www.congress.gov/bill/116th-congress/house-bill/3107/text?q=%7B%22search%22%3A%5B%22prior+authorization%22%5D%7D&r=1&s=1.
5. Gadbois EA, Tyler DA, Shield RR, et al. Medicare Advantage control of postacute costs: perspective from stakeholders. Am J Manag Care. 2018;24(12):e386-e392.
6. Rooke-Ley H, Broome T, Mostashari F, Cavanaugh S. Evaluating Medicare programs against saving taxpayer dollars. Health Affairs, August 16, 2019. Available at: https://www.healthaffairs.org/do/10.1377/hblog20190813.223707/full/.
7. Office of Inspector General. Billions in estimated Medicare Advantage payments from chart reviews raise concerns. December 2019. Available at: https://oig.hhs.gov/oei/reports/oei-03-17-00470.pdf. Accessed December 15, 2019.
8. Fact sheet: two-midnight rule. Available at: https://www.cms.gov/newsroom/fact-sheets/fact-sheet-two-midnight-rule-0.
9. Locke C, Hu E. Medicare’s two-midnight rule: what hospitalists must know. Available at: https://www.the-hospitalist.org/hospitalist/article/194971/medicares-two-midnight-rule.
10. Announcement of calendar year (CY) 2019 Medicare Advantage capitation rates and Medicare Advantage and part D payment policies and final call letter. Page 206. Available at: https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Downloads/Announcement2019.pdf. Accessed November 18, 2019.
11. Grebla R, Keohane L, Lee Y, Lipsitz L, Rahman M, Trivedi A. Waiving the three-day rule: admissions and length-of-stay at hospitals and skilled nursing facilities did not increase. Health Aff. 2015;34(8):1324-1330. https://doi.org/10.1377/hlthaff.2015.0054.
12. Meyers D, Mor V, Rahman M. Medicare Advantage enrollees more likely to enter lower-quality nursing homes compared to fee-for-service enrollees. Health Aff. 2018;37(1):78-85. https://doi.org/10.1377/hlthaff.2017.0714.
13. Sheehy A, Shi F, Kind AJH. Identifying observation stays in Medicare data: Policy implications of a definition. J Hosp Med. 2019;14(2):96-100. https://doi.org/10.12788/jhm.3038
14. The hospital observation care problem: perspectives and solutions from the Society of Hospital Medicine. Available at: https://www.hospitalmedicine.org/globalassets/policy-and-advocacy/advocacy-pdf/shms-observation-white-paper-2017. Accessed November 18, 2019.
15. U.S. Department of Health & Human Services, Office of Inspector General. Solutions to reduce fraud, waste and abuse in HHS programs: OIG’s top recommendations. Available at: https://oig.hhs.gov/reports-and-publications/compendium/. Accessed November 22, 2019.
1.McGuire TG, Newhouse JP, Sinaiko AD. An economic history of Medicare Part C. Millbank Q. 2011;89(2):289-332. https://doi.org/10.1111/j.1468-0009.2011.00629.x.
2. Medicare Advantage. Available at: https://www.kff.org/medicare/fact-sheet/medicare-advantage/.
3. Neuman P, Jacobson G. Medicare Advantage checkup. N Engl J Med. 2018;379(22):2163-2172. https://doi.org/10.1056/NEJMhpr1804089.
4. HR 3107: improving seniors’ timely access to Care Act of 2019. Available at: https://www.congress.gov/bill/116th-congress/house-bill/3107/text?q=%7B%22search%22%3A%5B%22prior+authorization%22%5D%7D&r=1&s=1.
5. Gadbois EA, Tyler DA, Shield RR, et al. Medicare Advantage control of postacute costs: perspective from stakeholders. Am J Manag Care. 2018;24(12):e386-e392.
6. Rooke-Ley H, Broome T, Mostashari F, Cavanaugh S. Evaluating Medicare programs against saving taxpayer dollars. Health Affairs, August 16, 2019. Available at: https://www.healthaffairs.org/do/10.1377/hblog20190813.223707/full/.
7. Office of Inspector General. Billions in estimated Medicare Advantage payments from chart reviews raise concerns. December 2019. Available at: https://oig.hhs.gov/oei/reports/oei-03-17-00470.pdf. Accessed December 15, 2019.
8. Fact sheet: two-midnight rule. Available at: https://www.cms.gov/newsroom/fact-sheets/fact-sheet-two-midnight-rule-0.
9. Locke C, Hu E. Medicare’s two-midnight rule: what hospitalists must know. Available at: https://www.the-hospitalist.org/hospitalist/article/194971/medicares-two-midnight-rule.
10. Announcement of calendar year (CY) 2019 Medicare Advantage capitation rates and Medicare Advantage and part D payment policies and final call letter. Page 206. Available at: https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Downloads/Announcement2019.pdf. Accessed November 18, 2019.
11. Grebla R, Keohane L, Lee Y, Lipsitz L, Rahman M, Trivedi A. Waiving the three-day rule: admissions and length-of-stay at hospitals and skilled nursing facilities did not increase. Health Aff. 2015;34(8):1324-1330. https://doi.org/10.1377/hlthaff.2015.0054.
12. Meyers D, Mor V, Rahman M. Medicare Advantage enrollees more likely to enter lower-quality nursing homes compared to fee-for-service enrollees. Health Aff. 2018;37(1):78-85. https://doi.org/10.1377/hlthaff.2017.0714.
13. Sheehy A, Shi F, Kind AJH. Identifying observation stays in Medicare data: Policy implications of a definition. J Hosp Med. 2019;14(2):96-100. https://doi.org/10.12788/jhm.3038
14. The hospital observation care problem: perspectives and solutions from the Society of Hospital Medicine. Available at: https://www.hospitalmedicine.org/globalassets/policy-and-advocacy/advocacy-pdf/shms-observation-white-paper-2017. Accessed November 18, 2019.
15. U.S. Department of Health & Human Services, Office of Inspector General. Solutions to reduce fraud, waste and abuse in HHS programs: OIG’s top recommendations. Available at: https://oig.hhs.gov/reports-and-publications/compendium/. Accessed November 22, 2019.
© 2020 Society of Hospital Medicine
Next Steps for Next Steps: The Intersection of Health Policy with Clinical Decision-Making
The Journal of Hospital Medicine introduced the Choosing Wisely®: Next Steps in Improving Healthcare Value series in 20151 as a companion to the popular Choosing Wisely®: Things We Do For No Reason™ series2 that was introduced in October in the same year. Both series were created in partnership with the American Board of Internal Medicine Foundation and were designed in the spirit of the Choosing Wisely® campaign’s mission to “promote conversations between clinicians and patients” in choosing care supported by evidence that minimizes harm, including avoidance of unnecessary treatments and tests.3 The Choosing Wisely®: Next Steps in Improving Healthcare Value series extends these principles as a forum for manuscripts that focus on translating value-based concepts into daily operations, including systems-level care delivery redesign initiatives, payment model innovations, and analyses of relevant policies or practice trends.
INITIAL EXPERIENCE
Since its inception, 16 Choosing Wisely®: Next Steps in Improving Healthcare Value manuscripts have been published, encompassing a wide range of topics such as postacute care transitions,4 the role of hospital medicine practice within accountable care organizations (ACOs),5 and quality and value at end-of-life.6
NEXT STEPS WITH NEXT STEPS
Few physicians receive health policy training.7,8 Hospital medicine practitioners are a core component of the workforce, driving change and value-based improvements at almost every inpatient facility across the country. Regardless of their background or experience, hospital medicine practitioners must interface with legislation, regulation, and other policies every day while providing patient care. Intentional, value-based improvements are more likely to succeed if those providing direct patient care understand health policies, particularly the effects of those policies on transactional, point-of-care decisions.
We are pleased to expand the Choosing Wisely®: Next Steps in Improving Healthcare Value series to include articles exploring health policy implications at the bedside. These articles will use common clinical scenarios to illuminate health policies most germane to hospital medicine practitioners and present applications of the policies as they relate to value at the level of patient–provider interactions. Each article will present a clinical scenario, explain key policy terms, address implications of specific policies in clinical practice, and propose how those policies can be improved (Appendix). Going forward, Choosing Wisely®: Next Steps in Improving Healthcare Value manuscript titles will include either “Policy in Clinical Practice” or “Improving Healthcare Value” to better establish a connection to the series and distinguish between the two article types.
The first Choosing Wisely®: Next Steps in Improving Healthcare Value—Implications of Health Policy on Clinical Decision-Making manuscript appears in this issue of the Journal of Hospital Medicine.9 As is the current practice for Choosing Wisely®: Next Steps in Improving Healthcare Value, authors are requested to send series editors a 500-word precis for review to ensure topic suitability before submission of a full manuscript. The precis, as well as any questions pertaining to the new series, can be directed to [email protected].
The authors thank the American Board of Internal Medicine Foundation for supporting this series.
1. Horwitz L, Masica A, Auerbach A. Introducing choosing wisely: Next steps in improving healthcare value. J Hosp Med. 2015;10(3): 187-189.
2. Feldman L. Choosing wisely: Things we do for no reasons. J Hosp Med. 2015;10(10):696. https://doi.org/10.1002/jhm.2425.
3. Choosing wisely: An initiative of the ABIM Foundation. Available at: http://www.choosingwisely.org/. Accessed July 8, 2019.
4. Conway S, Parekh A, Hughes A, et al. Next steps in improving healthcare value: Postacute care transitions: Developing a skilled nursing facility collaborative within an academic health system. J Hosp Med. 2019;14(3):174-177. https://doi.org/10.12788/jhm.3117.
5. Li J, Williams M. Hospitalist value in an ACO world. J Hosp Med. 2018;13(4):272-276. https://doi.org/10.12788/jhm.2965.
6. Fail R, Meier D. Improving quality of care for seriously ill patients: Opportunities for hospitalists. J Hosp Med. 2018;13(3):194-197. https://doi.org/10.12788/jhm.2896.
7. Fry C, Buntin M, Jain S. Medical schools and health policy: Adapting to the changing health care system. NEJM Catalyst, 2017. Available at: https://catalyst.nejm.org/medical-schools-health-policy-research/. Accessed July 10, 2019.
8. For doctors-in-training, a dose of health policy helps the medicine go down. National Public Radio (NPR), 2016. Available at: https://www.npr.org/sections/health-shots/2016/06/09/481207153/for-doctors-in-training-a-dose-of-health-policy-helps-the-medicine-go-down. Accessed July 10, 2019.
9. Kaiksow FA, Powell WR, Ankuda CK, et al. Policy in clinical practice: Medicare advantage and observation hospitalizations. J Hosp Med. 2020;15(1):6-8. https://doi.org/10.12788/jhm.3364.
The Journal of Hospital Medicine introduced the Choosing Wisely®: Next Steps in Improving Healthcare Value series in 20151 as a companion to the popular Choosing Wisely®: Things We Do For No Reason™ series2 that was introduced in October in the same year. Both series were created in partnership with the American Board of Internal Medicine Foundation and were designed in the spirit of the Choosing Wisely® campaign’s mission to “promote conversations between clinicians and patients” in choosing care supported by evidence that minimizes harm, including avoidance of unnecessary treatments and tests.3 The Choosing Wisely®: Next Steps in Improving Healthcare Value series extends these principles as a forum for manuscripts that focus on translating value-based concepts into daily operations, including systems-level care delivery redesign initiatives, payment model innovations, and analyses of relevant policies or practice trends.
INITIAL EXPERIENCE
Since its inception, 16 Choosing Wisely®: Next Steps in Improving Healthcare Value manuscripts have been published, encompassing a wide range of topics such as postacute care transitions,4 the role of hospital medicine practice within accountable care organizations (ACOs),5 and quality and value at end-of-life.6
NEXT STEPS WITH NEXT STEPS
Few physicians receive health policy training.7,8 Hospital medicine practitioners are a core component of the workforce, driving change and value-based improvements at almost every inpatient facility across the country. Regardless of their background or experience, hospital medicine practitioners must interface with legislation, regulation, and other policies every day while providing patient care. Intentional, value-based improvements are more likely to succeed if those providing direct patient care understand health policies, particularly the effects of those policies on transactional, point-of-care decisions.
We are pleased to expand the Choosing Wisely®: Next Steps in Improving Healthcare Value series to include articles exploring health policy implications at the bedside. These articles will use common clinical scenarios to illuminate health policies most germane to hospital medicine practitioners and present applications of the policies as they relate to value at the level of patient–provider interactions. Each article will present a clinical scenario, explain key policy terms, address implications of specific policies in clinical practice, and propose how those policies can be improved (Appendix). Going forward, Choosing Wisely®: Next Steps in Improving Healthcare Value manuscript titles will include either “Policy in Clinical Practice” or “Improving Healthcare Value” to better establish a connection to the series and distinguish between the two article types.
The first Choosing Wisely®: Next Steps in Improving Healthcare Value—Implications of Health Policy on Clinical Decision-Making manuscript appears in this issue of the Journal of Hospital Medicine.9 As is the current practice for Choosing Wisely®: Next Steps in Improving Healthcare Value, authors are requested to send series editors a 500-word precis for review to ensure topic suitability before submission of a full manuscript. The precis, as well as any questions pertaining to the new series, can be directed to [email protected].
The authors thank the American Board of Internal Medicine Foundation for supporting this series.
The Journal of Hospital Medicine introduced the Choosing Wisely®: Next Steps in Improving Healthcare Value series in 20151 as a companion to the popular Choosing Wisely®: Things We Do For No Reason™ series2 that was introduced in October in the same year. Both series were created in partnership with the American Board of Internal Medicine Foundation and were designed in the spirit of the Choosing Wisely® campaign’s mission to “promote conversations between clinicians and patients” in choosing care supported by evidence that minimizes harm, including avoidance of unnecessary treatments and tests.3 The Choosing Wisely®: Next Steps in Improving Healthcare Value series extends these principles as a forum for manuscripts that focus on translating value-based concepts into daily operations, including systems-level care delivery redesign initiatives, payment model innovations, and analyses of relevant policies or practice trends.
INITIAL EXPERIENCE
Since its inception, 16 Choosing Wisely®: Next Steps in Improving Healthcare Value manuscripts have been published, encompassing a wide range of topics such as postacute care transitions,4 the role of hospital medicine practice within accountable care organizations (ACOs),5 and quality and value at end-of-life.6
NEXT STEPS WITH NEXT STEPS
Few physicians receive health policy training.7,8 Hospital medicine practitioners are a core component of the workforce, driving change and value-based improvements at almost every inpatient facility across the country. Regardless of their background or experience, hospital medicine practitioners must interface with legislation, regulation, and other policies every day while providing patient care. Intentional, value-based improvements are more likely to succeed if those providing direct patient care understand health policies, particularly the effects of those policies on transactional, point-of-care decisions.
We are pleased to expand the Choosing Wisely®: Next Steps in Improving Healthcare Value series to include articles exploring health policy implications at the bedside. These articles will use common clinical scenarios to illuminate health policies most germane to hospital medicine practitioners and present applications of the policies as they relate to value at the level of patient–provider interactions. Each article will present a clinical scenario, explain key policy terms, address implications of specific policies in clinical practice, and propose how those policies can be improved (Appendix). Going forward, Choosing Wisely®: Next Steps in Improving Healthcare Value manuscript titles will include either “Policy in Clinical Practice” or “Improving Healthcare Value” to better establish a connection to the series and distinguish between the two article types.
The first Choosing Wisely®: Next Steps in Improving Healthcare Value—Implications of Health Policy on Clinical Decision-Making manuscript appears in this issue of the Journal of Hospital Medicine.9 As is the current practice for Choosing Wisely®: Next Steps in Improving Healthcare Value, authors are requested to send series editors a 500-word precis for review to ensure topic suitability before submission of a full manuscript. The precis, as well as any questions pertaining to the new series, can be directed to [email protected].
The authors thank the American Board of Internal Medicine Foundation for supporting this series.
1. Horwitz L, Masica A, Auerbach A. Introducing choosing wisely: Next steps in improving healthcare value. J Hosp Med. 2015;10(3): 187-189.
2. Feldman L. Choosing wisely: Things we do for no reasons. J Hosp Med. 2015;10(10):696. https://doi.org/10.1002/jhm.2425.
3. Choosing wisely: An initiative of the ABIM Foundation. Available at: http://www.choosingwisely.org/. Accessed July 8, 2019.
4. Conway S, Parekh A, Hughes A, et al. Next steps in improving healthcare value: Postacute care transitions: Developing a skilled nursing facility collaborative within an academic health system. J Hosp Med. 2019;14(3):174-177. https://doi.org/10.12788/jhm.3117.
5. Li J, Williams M. Hospitalist value in an ACO world. J Hosp Med. 2018;13(4):272-276. https://doi.org/10.12788/jhm.2965.
6. Fail R, Meier D. Improving quality of care for seriously ill patients: Opportunities for hospitalists. J Hosp Med. 2018;13(3):194-197. https://doi.org/10.12788/jhm.2896.
7. Fry C, Buntin M, Jain S. Medical schools and health policy: Adapting to the changing health care system. NEJM Catalyst, 2017. Available at: https://catalyst.nejm.org/medical-schools-health-policy-research/. Accessed July 10, 2019.
8. For doctors-in-training, a dose of health policy helps the medicine go down. National Public Radio (NPR), 2016. Available at: https://www.npr.org/sections/health-shots/2016/06/09/481207153/for-doctors-in-training-a-dose-of-health-policy-helps-the-medicine-go-down. Accessed July 10, 2019.
9. Kaiksow FA, Powell WR, Ankuda CK, et al. Policy in clinical practice: Medicare advantage and observation hospitalizations. J Hosp Med. 2020;15(1):6-8. https://doi.org/10.12788/jhm.3364.
1. Horwitz L, Masica A, Auerbach A. Introducing choosing wisely: Next steps in improving healthcare value. J Hosp Med. 2015;10(3): 187-189.
2. Feldman L. Choosing wisely: Things we do for no reasons. J Hosp Med. 2015;10(10):696. https://doi.org/10.1002/jhm.2425.
3. Choosing wisely: An initiative of the ABIM Foundation. Available at: http://www.choosingwisely.org/. Accessed July 8, 2019.
4. Conway S, Parekh A, Hughes A, et al. Next steps in improving healthcare value: Postacute care transitions: Developing a skilled nursing facility collaborative within an academic health system. J Hosp Med. 2019;14(3):174-177. https://doi.org/10.12788/jhm.3117.
5. Li J, Williams M. Hospitalist value in an ACO world. J Hosp Med. 2018;13(4):272-276. https://doi.org/10.12788/jhm.2965.
6. Fail R, Meier D. Improving quality of care for seriously ill patients: Opportunities for hospitalists. J Hosp Med. 2018;13(3):194-197. https://doi.org/10.12788/jhm.2896.
7. Fry C, Buntin M, Jain S. Medical schools and health policy: Adapting to the changing health care system. NEJM Catalyst, 2017. Available at: https://catalyst.nejm.org/medical-schools-health-policy-research/. Accessed July 10, 2019.
8. For doctors-in-training, a dose of health policy helps the medicine go down. National Public Radio (NPR), 2016. Available at: https://www.npr.org/sections/health-shots/2016/06/09/481207153/for-doctors-in-training-a-dose-of-health-policy-helps-the-medicine-go-down. Accessed July 10, 2019.
9. Kaiksow FA, Powell WR, Ankuda CK, et al. Policy in clinical practice: Medicare advantage and observation hospitalizations. J Hosp Med. 2020;15(1):6-8. https://doi.org/10.12788/jhm.3364.
© 2020 Society of Hospital Medicine
