User login
Chronic papules on the back and extremities
A 45-year-old Caucasian woman presented with pruritic erythematous scaling eruptions on her back and lower extremities. The patient said these skin lesions, which she has had since childhood, become worse in the summer. Additionally, her nails were fragile and often cracked. Her father and son had similar skin lesions.
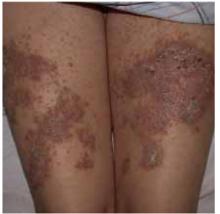
On skin examination, we saw erythematous hyperkeratotic confluent papules and plaques on her back, chest, thighs, and lower legs. Multiple 3- to 5-mm keratotic papules were noted on the dorsa of her hands bilaterally. Fingernail examination revealed longitudinal lines with notching at the distal edges (Figures 1 and 2). Examination of other systems was unremarkable.
FIGURE 1
Papules on the back...
FIGURE 2
...and the thighs
What is your diagnosis?
Are any diagnostic tests Necessary to confirm it?
Diagnosis: darier’s disease
Darier’s disease, also called Darier-White disease or keratosis follicularis, is a genodermatosis that affects 1 in 55,000 to 100,000 persons.1 It is inherited in an autosomal dominant fashion, resulting from a mutation in chromosome 12q23-q24.1, which encodes the gene ATP 2A2, which in turn encodes a SERCA2 (sarco/endoplasmic reticulum calcium)-ATPase pump. This defect results in instability of desmosomes.2-4
With Darier’s disease, skin lesions are often present in the second decade of life but rarely appear in adulthood. The clinical findings are described as yellowish, greasy hyperkeratotic papules coalescing to warty plaques in a seborrheic distribution on the face, scalp, flexures, and groin. The nails can have red and white alternating longitudinal bands, as well as a V-shaped nicking at the distal nail plate, with resultant splitting and subungual hyperkeratosis. Oral and anogenital mucosa can have a cobblestone appearance. Some families have had associated cases of schizophrenia and mental retardation.1,5
The histologic findings on skin biopsies of Darier’s disease show acantholysis (loss of epidermal adhesion) and dyskeratosis (abnormal keratinization) as the 2 main features.
Laboratory tests: biopsy confirms diagnosis
Biopsy of a characteristic papule from the patient’s back revealed diffuse acantholytic dyskeratosis, which confirmed the clinical diagnosis of Darier’s disease.
Two types of dyskeratotic cells are present: corps ronds and grains. Corps ronds, found in the stratum spinosum, are characterized by an irregular eccentric pyknotic nucleus, a clear perinuclear halo, and a brightly eosinophilic cytoplasm. Grains are mostly located in the stratum corneum; they consist of oval cells with elongated cigar-shaped nuclei. The patient declined genetic testing.
Differential diagnosis
For hyperkeratotic plaques on the back and extremities, several diagnoses should be considered.
Psoriasis is a papulosquamous hyperproliferative disorder, with underlying autoimmune mechanisms.
Seborrheic dermatitis is another papulosquamous disorder involving the sebum-rich areas of the scalp, face, and trunk. In addition to sebum, is is linked to Pityrosporum ovale, immunologic abnormalities, and activation of complement.
Transient acantholytic dermatosis, or Grover’s disease, is a benign, self-limited disorder; however, it may be persistent and difficult to manage. The process usually begins as an eruption on the anterior part of the chest, the upper part of the back, and the lower part of the chest.
Familial benign pemphigus is a chronic autosomal dominant disorder with incomplete penetrance, which manifests clinically as vesicles and erythematous plaques with overlying crusts, which typically occur in the genital area, as well as the chest, neck, and axillary areas.
Management: retinoids, laser surgery
Therapeutic options are palliative. A multidisciplinary approach is often necessary; family physicians as well as dermatologists, and occasionally plastic surgeons, have important roles in managing this chronic condition.
Treatment options for Darier’s disease range from topical to systemic medications and laser therapies. Successful topical therapies include corticosteroids, retinoids, urea, salicylic acid, 5-fluorouracil, and topical antibiotics.5,6
The most successful treatment option is systemic use of retinoids, most often acitretin (Soriatane).1,5 This medication, like isotretinoin (Accutane), requires meticulous monitoring and counseling. Women of childbearing age should be instructed to use 2 birth-control methods and, according to current recommendations, instructed not to conceive for 3 years following cessation of treatment (2 years in Europe). Cyclosporine may be used to control acute, severe flares.
Laser excision, excision and grafting, and dermabrasion have been used to treat hypertrophic lesions.1,5 More recently, photodynamic therapy (using photosensitizers in conjunction with a source of visible light) was also used in the treatment of Darier’s disease.7
Keep in mind that patients with Darier’s disease are more susceptible to cutaneous infections with bacteria, herpes simplex virus, and poxvirus. Awareness of this susceptibility can facilitate early diagnosis and treatment.8
Corresponding author
Amor Khachemoune, MD, CWS, Georgetown University Medical Center, Division of Dermatology, 3800 Reservoir Road, NW, 5PHC, Washington, DC 20007. E-mail: [email protected].
Submissions
Richard P. Usatine, Editor, Photo Rounds, University of Texas Health Sciences Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900. E-mail: [email protected].
1. Goldsmith LA, Baden HP. Darier-White disease (keratosis follicularis) and acrokeratosis verruciformis. In Freedberg IM, Eisen AZ, Wolff K, Austen KF, et al, eds: Dermatology in General Medicine. 5th ed. New York, NY: McGraw-Hill; 1999;614-618.
2. Jacobsen NJ, Lyons I, Hoogendoorn B, et al. ATP2A2 mutations in Darier’s disease and their relationship to neuropsychiatric phenotypes. Hum Mol Genet 1999;8:1631-1636.
3. Sakuntabhai A, Ruiz-Perez V, Carter S, et al. Mutations in ATP2A2, encoding a Ca+2 pump, cause Darier disease. Nat Genet 1999;21:271-277.
4. Ahn W, Lee MG, Kim KH, Muallem S. Multiple effects of SERCA2b mutations associated with Darier’s disease. J Biol Chem 2003;278:20795-20801.
5. Cooper SM, Burge SM. Darier’s disease: epidemiology, pathophysiology, and management. Am J Clin Dermatol 2003;4:97-105.
6. Knulst AC, De La Faille HB, Van Vloten WA. Topical 5-fluorouracil in the treatment of Darier’s disease. Br J Dermatol 1995;133:463-466.
7. Exadaktylou D, Kurwa HA, Calonje E, Barlow RJ. Treatment of Darier’s disease with photodynamic therapy. Br J Dermatol 2003;149:606-610.
8. Parslew R, Verbov JL. Kaposi’s varicelliform eruption due to herpes simplex in Darier’s disease. Clin Exp Dermatol 1994;19:428-429.
A 45-year-old Caucasian woman presented with pruritic erythematous scaling eruptions on her back and lower extremities. The patient said these skin lesions, which she has had since childhood, become worse in the summer. Additionally, her nails were fragile and often cracked. Her father and son had similar skin lesions.
On skin examination, we saw erythematous hyperkeratotic confluent papules and plaques on her back, chest, thighs, and lower legs. Multiple 3- to 5-mm keratotic papules were noted on the dorsa of her hands bilaterally. Fingernail examination revealed longitudinal lines with notching at the distal edges (Figures 1 and 2). Examination of other systems was unremarkable.
FIGURE 1
Papules on the back...
FIGURE 2
...and the thighs
What is your diagnosis?
Are any diagnostic tests Necessary to confirm it?
Diagnosis: darier’s disease
Darier’s disease, also called Darier-White disease or keratosis follicularis, is a genodermatosis that affects 1 in 55,000 to 100,000 persons.1 It is inherited in an autosomal dominant fashion, resulting from a mutation in chromosome 12q23-q24.1, which encodes the gene ATP 2A2, which in turn encodes a SERCA2 (sarco/endoplasmic reticulum calcium)-ATPase pump. This defect results in instability of desmosomes.2-4
With Darier’s disease, skin lesions are often present in the second decade of life but rarely appear in adulthood. The clinical findings are described as yellowish, greasy hyperkeratotic papules coalescing to warty plaques in a seborrheic distribution on the face, scalp, flexures, and groin. The nails can have red and white alternating longitudinal bands, as well as a V-shaped nicking at the distal nail plate, with resultant splitting and subungual hyperkeratosis. Oral and anogenital mucosa can have a cobblestone appearance. Some families have had associated cases of schizophrenia and mental retardation.1,5
The histologic findings on skin biopsies of Darier’s disease show acantholysis (loss of epidermal adhesion) and dyskeratosis (abnormal keratinization) as the 2 main features.
Laboratory tests: biopsy confirms diagnosis
Biopsy of a characteristic papule from the patient’s back revealed diffuse acantholytic dyskeratosis, which confirmed the clinical diagnosis of Darier’s disease.
Two types of dyskeratotic cells are present: corps ronds and grains. Corps ronds, found in the stratum spinosum, are characterized by an irregular eccentric pyknotic nucleus, a clear perinuclear halo, and a brightly eosinophilic cytoplasm. Grains are mostly located in the stratum corneum; they consist of oval cells with elongated cigar-shaped nuclei. The patient declined genetic testing.
Differential diagnosis
For hyperkeratotic plaques on the back and extremities, several diagnoses should be considered.
Psoriasis is a papulosquamous hyperproliferative disorder, with underlying autoimmune mechanisms.
Seborrheic dermatitis is another papulosquamous disorder involving the sebum-rich areas of the scalp, face, and trunk. In addition to sebum, is is linked to Pityrosporum ovale, immunologic abnormalities, and activation of complement.
Transient acantholytic dermatosis, or Grover’s disease, is a benign, self-limited disorder; however, it may be persistent and difficult to manage. The process usually begins as an eruption on the anterior part of the chest, the upper part of the back, and the lower part of the chest.
Familial benign pemphigus is a chronic autosomal dominant disorder with incomplete penetrance, which manifests clinically as vesicles and erythematous plaques with overlying crusts, which typically occur in the genital area, as well as the chest, neck, and axillary areas.
Management: retinoids, laser surgery
Therapeutic options are palliative. A multidisciplinary approach is often necessary; family physicians as well as dermatologists, and occasionally plastic surgeons, have important roles in managing this chronic condition.
Treatment options for Darier’s disease range from topical to systemic medications and laser therapies. Successful topical therapies include corticosteroids, retinoids, urea, salicylic acid, 5-fluorouracil, and topical antibiotics.5,6
The most successful treatment option is systemic use of retinoids, most often acitretin (Soriatane).1,5 This medication, like isotretinoin (Accutane), requires meticulous monitoring and counseling. Women of childbearing age should be instructed to use 2 birth-control methods and, according to current recommendations, instructed not to conceive for 3 years following cessation of treatment (2 years in Europe). Cyclosporine may be used to control acute, severe flares.
Laser excision, excision and grafting, and dermabrasion have been used to treat hypertrophic lesions.1,5 More recently, photodynamic therapy (using photosensitizers in conjunction with a source of visible light) was also used in the treatment of Darier’s disease.7
Keep in mind that patients with Darier’s disease are more susceptible to cutaneous infections with bacteria, herpes simplex virus, and poxvirus. Awareness of this susceptibility can facilitate early diagnosis and treatment.8
Corresponding author
Amor Khachemoune, MD, CWS, Georgetown University Medical Center, Division of Dermatology, 3800 Reservoir Road, NW, 5PHC, Washington, DC 20007. E-mail: [email protected].
Submissions
Richard P. Usatine, Editor, Photo Rounds, University of Texas Health Sciences Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900. E-mail: [email protected].
A 45-year-old Caucasian woman presented with pruritic erythematous scaling eruptions on her back and lower extremities. The patient said these skin lesions, which she has had since childhood, become worse in the summer. Additionally, her nails were fragile and often cracked. Her father and son had similar skin lesions.
On skin examination, we saw erythematous hyperkeratotic confluent papules and plaques on her back, chest, thighs, and lower legs. Multiple 3- to 5-mm keratotic papules were noted on the dorsa of her hands bilaterally. Fingernail examination revealed longitudinal lines with notching at the distal edges (Figures 1 and 2). Examination of other systems was unremarkable.
FIGURE 1
Papules on the back...
FIGURE 2
...and the thighs
What is your diagnosis?
Are any diagnostic tests Necessary to confirm it?
Diagnosis: darier’s disease
Darier’s disease, also called Darier-White disease or keratosis follicularis, is a genodermatosis that affects 1 in 55,000 to 100,000 persons.1 It is inherited in an autosomal dominant fashion, resulting from a mutation in chromosome 12q23-q24.1, which encodes the gene ATP 2A2, which in turn encodes a SERCA2 (sarco/endoplasmic reticulum calcium)-ATPase pump. This defect results in instability of desmosomes.2-4
With Darier’s disease, skin lesions are often present in the second decade of life but rarely appear in adulthood. The clinical findings are described as yellowish, greasy hyperkeratotic papules coalescing to warty plaques in a seborrheic distribution on the face, scalp, flexures, and groin. The nails can have red and white alternating longitudinal bands, as well as a V-shaped nicking at the distal nail plate, with resultant splitting and subungual hyperkeratosis. Oral and anogenital mucosa can have a cobblestone appearance. Some families have had associated cases of schizophrenia and mental retardation.1,5
The histologic findings on skin biopsies of Darier’s disease show acantholysis (loss of epidermal adhesion) and dyskeratosis (abnormal keratinization) as the 2 main features.
Laboratory tests: biopsy confirms diagnosis
Biopsy of a characteristic papule from the patient’s back revealed diffuse acantholytic dyskeratosis, which confirmed the clinical diagnosis of Darier’s disease.
Two types of dyskeratotic cells are present: corps ronds and grains. Corps ronds, found in the stratum spinosum, are characterized by an irregular eccentric pyknotic nucleus, a clear perinuclear halo, and a brightly eosinophilic cytoplasm. Grains are mostly located in the stratum corneum; they consist of oval cells with elongated cigar-shaped nuclei. The patient declined genetic testing.
Differential diagnosis
For hyperkeratotic plaques on the back and extremities, several diagnoses should be considered.
Psoriasis is a papulosquamous hyperproliferative disorder, with underlying autoimmune mechanisms.
Seborrheic dermatitis is another papulosquamous disorder involving the sebum-rich areas of the scalp, face, and trunk. In addition to sebum, is is linked to Pityrosporum ovale, immunologic abnormalities, and activation of complement.
Transient acantholytic dermatosis, or Grover’s disease, is a benign, self-limited disorder; however, it may be persistent and difficult to manage. The process usually begins as an eruption on the anterior part of the chest, the upper part of the back, and the lower part of the chest.
Familial benign pemphigus is a chronic autosomal dominant disorder with incomplete penetrance, which manifests clinically as vesicles and erythematous plaques with overlying crusts, which typically occur in the genital area, as well as the chest, neck, and axillary areas.
Management: retinoids, laser surgery
Therapeutic options are palliative. A multidisciplinary approach is often necessary; family physicians as well as dermatologists, and occasionally plastic surgeons, have important roles in managing this chronic condition.
Treatment options for Darier’s disease range from topical to systemic medications and laser therapies. Successful topical therapies include corticosteroids, retinoids, urea, salicylic acid, 5-fluorouracil, and topical antibiotics.5,6
The most successful treatment option is systemic use of retinoids, most often acitretin (Soriatane).1,5 This medication, like isotretinoin (Accutane), requires meticulous monitoring and counseling. Women of childbearing age should be instructed to use 2 birth-control methods and, according to current recommendations, instructed not to conceive for 3 years following cessation of treatment (2 years in Europe). Cyclosporine may be used to control acute, severe flares.
Laser excision, excision and grafting, and dermabrasion have been used to treat hypertrophic lesions.1,5 More recently, photodynamic therapy (using photosensitizers in conjunction with a source of visible light) was also used in the treatment of Darier’s disease.7
Keep in mind that patients with Darier’s disease are more susceptible to cutaneous infections with bacteria, herpes simplex virus, and poxvirus. Awareness of this susceptibility can facilitate early diagnosis and treatment.8
Corresponding author
Amor Khachemoune, MD, CWS, Georgetown University Medical Center, Division of Dermatology, 3800 Reservoir Road, NW, 5PHC, Washington, DC 20007. E-mail: [email protected].
Submissions
Richard P. Usatine, Editor, Photo Rounds, University of Texas Health Sciences Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900. E-mail: [email protected].
1. Goldsmith LA, Baden HP. Darier-White disease (keratosis follicularis) and acrokeratosis verruciformis. In Freedberg IM, Eisen AZ, Wolff K, Austen KF, et al, eds: Dermatology in General Medicine. 5th ed. New York, NY: McGraw-Hill; 1999;614-618.
2. Jacobsen NJ, Lyons I, Hoogendoorn B, et al. ATP2A2 mutations in Darier’s disease and their relationship to neuropsychiatric phenotypes. Hum Mol Genet 1999;8:1631-1636.
3. Sakuntabhai A, Ruiz-Perez V, Carter S, et al. Mutations in ATP2A2, encoding a Ca+2 pump, cause Darier disease. Nat Genet 1999;21:271-277.
4. Ahn W, Lee MG, Kim KH, Muallem S. Multiple effects of SERCA2b mutations associated with Darier’s disease. J Biol Chem 2003;278:20795-20801.
5. Cooper SM, Burge SM. Darier’s disease: epidemiology, pathophysiology, and management. Am J Clin Dermatol 2003;4:97-105.
6. Knulst AC, De La Faille HB, Van Vloten WA. Topical 5-fluorouracil in the treatment of Darier’s disease. Br J Dermatol 1995;133:463-466.
7. Exadaktylou D, Kurwa HA, Calonje E, Barlow RJ. Treatment of Darier’s disease with photodynamic therapy. Br J Dermatol 2003;149:606-610.
8. Parslew R, Verbov JL. Kaposi’s varicelliform eruption due to herpes simplex in Darier’s disease. Clin Exp Dermatol 1994;19:428-429.
1. Goldsmith LA, Baden HP. Darier-White disease (keratosis follicularis) and acrokeratosis verruciformis. In Freedberg IM, Eisen AZ, Wolff K, Austen KF, et al, eds: Dermatology in General Medicine. 5th ed. New York, NY: McGraw-Hill; 1999;614-618.
2. Jacobsen NJ, Lyons I, Hoogendoorn B, et al. ATP2A2 mutations in Darier’s disease and their relationship to neuropsychiatric phenotypes. Hum Mol Genet 1999;8:1631-1636.
3. Sakuntabhai A, Ruiz-Perez V, Carter S, et al. Mutations in ATP2A2, encoding a Ca+2 pump, cause Darier disease. Nat Genet 1999;21:271-277.
4. Ahn W, Lee MG, Kim KH, Muallem S. Multiple effects of SERCA2b mutations associated with Darier’s disease. J Biol Chem 2003;278:20795-20801.
5. Cooper SM, Burge SM. Darier’s disease: epidemiology, pathophysiology, and management. Am J Clin Dermatol 2003;4:97-105.
6. Knulst AC, De La Faille HB, Van Vloten WA. Topical 5-fluorouracil in the treatment of Darier’s disease. Br J Dermatol 1995;133:463-466.
7. Exadaktylou D, Kurwa HA, Calonje E, Barlow RJ. Treatment of Darier’s disease with photodynamic therapy. Br J Dermatol 2003;149:606-610.
8. Parslew R, Verbov JL. Kaposi’s varicelliform eruption due to herpes simplex in Darier’s disease. Clin Exp Dermatol 1994;19:428-429.