User login
Posttraumatic Saphenous Neuroma After Open Tibial Fracture
Neuralgia and neuroma secondary to iatrogenic saphenous nerve injury have been described in the setting of orthopedic surgical interventions using a medial parapatellar approach, and in vascular surgery procedures for harvest of the saphenous vein.1-3 However, postoperative neuropathic pain caused by saphenous neuroma in the setting of orthopedic trauma has not been described.
We present a case of symptomatic posttraumatic saphenous neuroma after a displaced and laterally angulated open distal one-third tibial fracture. This unreported cause of postinjury neuralgia is an important complication to address as other similar and more common conditions, such as peripheral neuropathy and complex regional pain syndrome (CRPS), can present in a similar manner. Reaching the correct diagnosis can be challenging for clinicians unfamiliar with this condition or its clinical presentation. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 43-year-old woman presented to our practice 2 years after an open distal one-third metadiaphyseal fracture of the tibia with associated segmental fibular fracture (Gustilo-Anderson type II)4 after an automobile/bicycle accident. At the time of injury, she was noted to have a complex medial wound in the region of an open fracture at the junction of the middle and distal thirds of her tibial shaft. She underwent definitive treatment at an outside facility with initial irrigation and débridement and primary wound closure, followed by staged intramedullary nail fixation. Both soft-tissue and bony injuries healed within the expected time frame, and the patient was discharged from orthopedic care.
Approximately 1 year after her initial injury, the patient began to complain of progressive and persistent anteromedial knee pain as well as gradual-onset, medial-sided leg pain. The leg pain began at the level of her previous fracture site, at the distal one-third metadiaphyseal tibial junction, and radiated from the site of her previous medial open wound distally to the medial aspect of her foot. The pain was burning and tingling in nature, with associated hyperesthesia of the affected area. A diagnosis of CRPS was made, and the patient was prescribed a course of desensitization therapy, oral neuromodulating agents, and physical therapy. After 3 months’ therapy, she remained symptomatic and underwent removal of her proximal tibial interlocking screw fixation (Figure 1). When these measures failed to provide symptomatic relief, and having seen several therapists and physicians, including physiatrists, pain management specialists, and orthopedic surgeons, she presented to our clinic for consultation.
Diagnostic Assessment
On presentation, the patient’s surgical incisions were well healed. At the junction of the middle and distal thirds of the tibia, a 4-cm oblique scar was noted over the anteromedial border of the tibia, the site of her previous open fracture. She demonstrated decreased sensation along the length of this oblique scar, as well as in the distribution of the saphenous nerve distally. Further examination of the previously injured region revealed a positive Tinel sign over the course of the saphenous nerve, with radiating pain down the medial aspect of her leg, recreating her symptoms. She otherwise had full range of motion at the knee with mild tenderness to palpation at the medial joint line and patellar tendon. Her lower extremity motor examination, reflexes, and the remainder of her sensory examination were benign.
These findings were consistent with isolated saphenous neuralgia, and selective injection of the saphenous distribution over the injury site was performed. This injection provided immediate symptomatic relief, with the patient reporting preinjection and postinjection pain scores of 7/10 and 2/10, respectively. Because of the clinical improvement demonstrated with selective injection, surgical intervention with exploration and neurolysis of the saphenous nerve was recommended.
Therapeutic Intervention
The patient underwent surgical exploration of her saphenous nerve at the level of her original open fracture. This was done concurrently with a left-knee diagnostic arthroscopy and removal of her intramedullary tibial implant both to exclude intra-articular pathology (given her medial joint-line tenderness and the limitation of magnetic resonance imaging to diagnose meniscus tear in the presence of her tibial hardware) and to remove any potential hardware irritation in the setting of her anterior knee pain.5,6
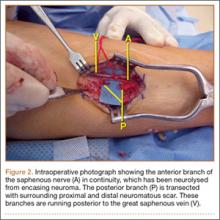
Preoperatively, the path of the saphenous nerve was marked using the saphenous vein as a guide. An incision overlying the presumed saphenous nerve course was made at the site of her previous open wound and clinical Tinel sign. The saphenous nerve was carefully dissected with loupe magnification, and the distal divisions of the anterior and posterior branches were identified. The anterior branch was found to be in continuity but encased in fibrotic neuroma. Selective neurolysis of this anterior branch was performed. The posterior branch was found to have been traumatically severed, with both the proximal and distal ends encased in neuromatous scar (Figure 2). Neurectomy of the posterior branch was performed and the severed proximal end of the nerve was buried into the adjacent medial gastrocnemius muscle beneath the fascia of the superficial posterior compartment.7-9
Postoperative Course and Outcome
Upon transport to the postsurgical care unit and emergence from sedation, the patient experienced immediate resolution of her neuralgic symptoms. Pathology of the operative specimen showed a benign, disorganized arrangement of axons, Schwann cells, and perineural fibroblasts amidst a fibrous stroma, consistent with traumatic neuroma. At 1-month and 6-month follow-up visits, the patient remained symptom-free, aside from some continued anterior left knee pain near the site of intramedullary nail entry. Her positive Tinel sign had completely resolved, as did her neuralgic symptoms down the medial aspect of her leg. This proved consistent with a diagnosis of neuroma as the cause of the majority of her symptoms. Subjectively, she reported excellent overall pain relief and satisfaction with her treatment and postoperative course.
Discussion
Postoperative pain after intramedullary fixation of tibial shaft fractures is common and can be caused by several clinical entities.5,10 Anterior knee pain is a well-known complication present in up to 73% of patients treated with tibial nailing.10 Osteoarthritis of the knee or ankle as well as nonarthritic ipsilateral ankle pain are also common complaints, often resulting from tibial malunion or malrotation, leading to altered joint kinematics.11 Additionally, superficial peroneal nerve and tibial neurovascular bundle injuries have been reported as potential complications of distal interlocking screw placement, and should be considered in such patients.12
Another consideration for the development of postoperative pain is CRPS, which is thought to be caused by postinjury sympathetic activation that produces pain out of proportion to clinical examination findings.13 Although no postoperative incidence of CRPS in the setting of tibial nailing has been reported, it is a known contributor to poor functional outcomes after fractures or crush injuries to the lower extremity.9 When attempting to diagnose and treat chronic postoperative pain after tibial nailing, the clinician must keep these common etiologies in mind as well as an understanding of the adjacent anatomy.
The saphenous nerve originates from the third and fourth lumbar nerve roots, coursing beneath the inguinal ligament as part of the femoral nerve. As the terminal branch of the femoral nerve, the saphenous nerve runs in the Hunter canal beneath the fascia of the sartorius muscle. It is bordered laterally by the vastus medialis muscle, and posteriorly and laterally by the adductor longus and magnus muscles. The saphenous nerve then crosses the femoral artery superficially from medial to lateral as it courses distally in the canal. As it emerges from the adductor hiatus, the saphenous nerve runs superficial to the gracilis muscle around the posterior border of the sartorius muscle with the descending genicular artery, and becomes a subcutaneous structure at the level of the knee joint. The infrapatellar branch of the saphenous nerve provides sensation to the medial knee, and continues in a subcutaneous course just medial to the posterior aspect of the tibial shaft with the great saphenous vein. The nerve distally supplies sensory input from the medial foot and ankle.1,3,14
There are several causes of saphenous neuralgia related to surgical and nonsurgical trauma.2,3,15,16 The most common cause of nerve injury is iatrogenic traction or transection causing neuralgic sequelae from subsequent neuroma formation. The anatomy of the saphenous nerve puts it at particular risk when performing saphenectomy for vascular procedures, and its infrapatellar branch is at particular risk when performing a medial parapatellar approach for total knee arthroplasty.2,3 In the case of the surgically naïve patient, saphenous nerve entrapment syndromes have also been described, and occur most frequently at the level of the adductor hiatus or as the saphenous nerve courses between the sartorius and gracilis muscles proximal to the knee joint.16
As is illustrated in the present case, orthopedic trauma may be an additional cause of saphenous neuroma formation, leading to symptomatic neuralgia. This case suggests that symptomatic neuroma should be included in the differential diagnosis of posttraumatic pain in the orthopedic trauma patient. It is important to note that, although this case occurred after a severe injury, the intimate association of the saphenous nerve with the tibia places it in a vulnerable position, and traumatic transection is possible after closed injuries to the tibial metadiaphyseal junction or tibial shaft.
Neuroma formation occurs in response to damage to the endoneurium and axon. For an axon to repair properly, the damaged proximal segment must join with, and reenter, the distal stump. As axons attempt to regenerate, occasionally the proximal stump can escape into the surrounding tissue and form a painful neuroma consisting of a disorganized mass of Schwann cells, fibroblasts, blood vessels, and axons with various degrees of myelination. The subsequent neuralgia associated with neuroma formation is caused by chemical or mechanical stimulation of the damaged axons or by spontaneously evoked potentials in the damaged axons. These signals can manifest as a variety of symptoms, including paresthesia and allodynia.17,18
Making the diagnosis of neuroma-related neuralgia can be challenging and nebulous. A characteristic history and positive Tinel sign over the affected area are helpful clinical indicators. However, the clinical finding most predictive of favorable surgical outcome is symptomatic relief after local injection of 1% lidocaine to the affected area. This is an important diagnostic test, especially when attempting to differentiate painful neuroma from other causes of posttraumatic lower extremity pain (eg, CRPS). Such an injection should be performed in the diagnosis and treatment of symptomatic neuroma, and some authors would suggest that insufficient relief of symptoms with diagnostic nerve block is a contraindication to surgical treatment.19
Several treatments for painful neuromas have been described, with variable results.19,20 The most widely accepted treatment of a complete nerve transection with associated neuroma is neurectomy with reimplantation of the proximal end into adjacent bone, muscle, or vein.14,15 Balcin and colleagues21 suggest that vein transposition produces the most favorable outcomes. Simple neurolysis of in-continuity neuromas has also been described with favorable results.
Conclusion
Neuralgia-producing neuromas of the saphenous nerve are relatively uncommon but can lead to persistent pain and frustrating symptoms for the patient. As noted, the diagnosis may elude clinicians, especially in patients with less obvious clinical presentations. We suggest the following algorithm to help distinguish between painful neuroma and other causes of posttraumatic leg pain: (1) physical examination (including testing for instability, joint line tenderness, patellofemoral pain, Tinel sign, and Semmes-Weinstein testing) should be performed, and plain radiographs taken of the involved bones and joints; (2) if all of the above reveal no abnormality, and there is a positive Tinel sign directly over the course of a nerve, an injection of lidocaine over the region of the potential neuroma can be diagnostic; (3) should several abnormalities be present, further investigation using magnetic resonance imaging, bone scan, and/or electromyography may provide additional information that leads to a diagnosis.
1. Senegor M. Iatrogenic saphenous neuralgia: successful treatment with neuroma resection. J Neurosurg. 1991;28(2):295-298.
2. Mountney J, Wilkinson GA. Saphenous neuralgia after coronary artery bypass grafting. Eur J Cardiothorac Surg. 1999;16(4):440-443.
3. Kachar SM, Williams KM, Finn HA. Neuroma of the infrapatellar branch of the saphenous nerve: a cause of reversible knee stiffness after total knee arthroplasty. J Arthroplasty. 2008;23(6):927-930.
4. Gustilo RB, Anderson AB. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58(4):453-458.
5. Keating JF, Orfaly R, O’Brien PJ. Knee pain after tibial nailing. J Orthop Trauma. 1997;11(1):10-13.
6. Chen CY, Lin KC, Yang SW, Tarng YW, Hsu CJ, Renn JH. Influence of nail prominence and insertion point on anterior knee pain after tibial intramedullary nailing. Orthopedics. 2014;37(3):e221-e225.
7. Lewin-Kowalik J, Marcol W, Kotulska K, Mandera M, Klimczak A. Prevention and management of painful neuroma. Neurol Med Chir (Tokyo). 2006;46(2):62-67.
8. Otfinowski J, Pawelec A, Kaluza J. Implantation of peripheral neural stump into muscle and its effect on the development of posttraumatic neuroma. Pol J Pathol. 1994;45:195-202.
9. Van Beek AL. Management of nerve compression syndromes and painful neuromas. In: McCarthy JG, May JW Jr, Littler JW, eds. Plastic Surgery. Philadelphia, PA: WB Saunders; 1990:4817-4858.
10. Lefaivre KA, Guy P, Chan H, Blachut PA. Long-term follow-up of tibial shaft fractures treated with intramedullary nailing. J Orthop Trauma. 2008;22(8):525-529.
11. Milner SA, Davis TR, Muir KR, Greenwood DC, Doherty M. Long-term outcome after tibial shaft fracture: is malunion important? J Bone Joint Surg Am. 2002;84(6):971-980.
12. Roberts CS, King D, Wang M, Seligson D, Voor MJ. Should distal interlocking of tibial nails be performed from medial or lateral direction? Anatomical and biomechanical considerations. J Orthop Trauma. 1999;13(1):27-32.
13. Hogan CJ, Hurwitz SR. Treatment of complex regional pain syndrome of the lower extremity. J Am Acad Orthop Surg. 2002;10(4):281-289.
14. Gray H, Lewis WH. Anatomy of the Human Body. Philadelphia, PA: Lea & Febiger, 1918. Bartleby.com website. http://www.bartleby.com/br/107.html. Accessed September 29, 2015.
15. Myerson MS, McGarvey WC, Henderson MR, Hakim J. Morbidity after crush injuries to the foot. J Orthop Trauma. 1994;8(4):343-349.
16. Kalenak A. Saphenous nerve entrapment. Op Tech Sports Med. 1996;4(1):40-45.
17. Wolf SW, Hotchkiss RN, Pederson WC, Kozin SH. The peripheral neuroma. In: Green DP, Wolfe SW, eds. Green’s Operative Hand Surgery. 6th ed. Philadelphia, PA: Elsevier Churchill Livingstone, 2011;1063-1071.
18. Thordarson DB, Shean CJ. Nerve and tendon lacerations about the foot and ankle. J Am Acad Orthop Surg. 2005;13(3):186-196.
19. Stokvis A, van der Avoort DJ, van Neck JW, Hovius SE, Coert JH. Surgical management of neuroma pain: a prospective follow-up study. Pain. 2010;151(3):862-869.
20. Burchiel KJ, Johans TJ, Ochoa J. The surgical treatment of painful traumatic neuromas. J Neurosurg. 1993;78(5):714-719.
21. Balcin H, Erba P, Wettstein R, Schaefer DJ, Pierer G, Kalbermatten DF. A comparative study of two methods of surgical treatment for painful neuroma. J Bone Joint Surg Br. 2009;91(6):803-808.
Neuralgia and neuroma secondary to iatrogenic saphenous nerve injury have been described in the setting of orthopedic surgical interventions using a medial parapatellar approach, and in vascular surgery procedures for harvest of the saphenous vein.1-3 However, postoperative neuropathic pain caused by saphenous neuroma in the setting of orthopedic trauma has not been described.
We present a case of symptomatic posttraumatic saphenous neuroma after a displaced and laterally angulated open distal one-third tibial fracture. This unreported cause of postinjury neuralgia is an important complication to address as other similar and more common conditions, such as peripheral neuropathy and complex regional pain syndrome (CRPS), can present in a similar manner. Reaching the correct diagnosis can be challenging for clinicians unfamiliar with this condition or its clinical presentation. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 43-year-old woman presented to our practice 2 years after an open distal one-third metadiaphyseal fracture of the tibia with associated segmental fibular fracture (Gustilo-Anderson type II)4 after an automobile/bicycle accident. At the time of injury, she was noted to have a complex medial wound in the region of an open fracture at the junction of the middle and distal thirds of her tibial shaft. She underwent definitive treatment at an outside facility with initial irrigation and débridement and primary wound closure, followed by staged intramedullary nail fixation. Both soft-tissue and bony injuries healed within the expected time frame, and the patient was discharged from orthopedic care.
Approximately 1 year after her initial injury, the patient began to complain of progressive and persistent anteromedial knee pain as well as gradual-onset, medial-sided leg pain. The leg pain began at the level of her previous fracture site, at the distal one-third metadiaphyseal tibial junction, and radiated from the site of her previous medial open wound distally to the medial aspect of her foot. The pain was burning and tingling in nature, with associated hyperesthesia of the affected area. A diagnosis of CRPS was made, and the patient was prescribed a course of desensitization therapy, oral neuromodulating agents, and physical therapy. After 3 months’ therapy, she remained symptomatic and underwent removal of her proximal tibial interlocking screw fixation (Figure 1). When these measures failed to provide symptomatic relief, and having seen several therapists and physicians, including physiatrists, pain management specialists, and orthopedic surgeons, she presented to our clinic for consultation.
Diagnostic Assessment
On presentation, the patient’s surgical incisions were well healed. At the junction of the middle and distal thirds of the tibia, a 4-cm oblique scar was noted over the anteromedial border of the tibia, the site of her previous open fracture. She demonstrated decreased sensation along the length of this oblique scar, as well as in the distribution of the saphenous nerve distally. Further examination of the previously injured region revealed a positive Tinel sign over the course of the saphenous nerve, with radiating pain down the medial aspect of her leg, recreating her symptoms. She otherwise had full range of motion at the knee with mild tenderness to palpation at the medial joint line and patellar tendon. Her lower extremity motor examination, reflexes, and the remainder of her sensory examination were benign.
These findings were consistent with isolated saphenous neuralgia, and selective injection of the saphenous distribution over the injury site was performed. This injection provided immediate symptomatic relief, with the patient reporting preinjection and postinjection pain scores of 7/10 and 2/10, respectively. Because of the clinical improvement demonstrated with selective injection, surgical intervention with exploration and neurolysis of the saphenous nerve was recommended.
Therapeutic Intervention
The patient underwent surgical exploration of her saphenous nerve at the level of her original open fracture. This was done concurrently with a left-knee diagnostic arthroscopy and removal of her intramedullary tibial implant both to exclude intra-articular pathology (given her medial joint-line tenderness and the limitation of magnetic resonance imaging to diagnose meniscus tear in the presence of her tibial hardware) and to remove any potential hardware irritation in the setting of her anterior knee pain.5,6
Preoperatively, the path of the saphenous nerve was marked using the saphenous vein as a guide. An incision overlying the presumed saphenous nerve course was made at the site of her previous open wound and clinical Tinel sign. The saphenous nerve was carefully dissected with loupe magnification, and the distal divisions of the anterior and posterior branches were identified. The anterior branch was found to be in continuity but encased in fibrotic neuroma. Selective neurolysis of this anterior branch was performed. The posterior branch was found to have been traumatically severed, with both the proximal and distal ends encased in neuromatous scar (Figure 2). Neurectomy of the posterior branch was performed and the severed proximal end of the nerve was buried into the adjacent medial gastrocnemius muscle beneath the fascia of the superficial posterior compartment.7-9
Postoperative Course and Outcome
Upon transport to the postsurgical care unit and emergence from sedation, the patient experienced immediate resolution of her neuralgic symptoms. Pathology of the operative specimen showed a benign, disorganized arrangement of axons, Schwann cells, and perineural fibroblasts amidst a fibrous stroma, consistent with traumatic neuroma. At 1-month and 6-month follow-up visits, the patient remained symptom-free, aside from some continued anterior left knee pain near the site of intramedullary nail entry. Her positive Tinel sign had completely resolved, as did her neuralgic symptoms down the medial aspect of her leg. This proved consistent with a diagnosis of neuroma as the cause of the majority of her symptoms. Subjectively, she reported excellent overall pain relief and satisfaction with her treatment and postoperative course.
Discussion
Postoperative pain after intramedullary fixation of tibial shaft fractures is common and can be caused by several clinical entities.5,10 Anterior knee pain is a well-known complication present in up to 73% of patients treated with tibial nailing.10 Osteoarthritis of the knee or ankle as well as nonarthritic ipsilateral ankle pain are also common complaints, often resulting from tibial malunion or malrotation, leading to altered joint kinematics.11 Additionally, superficial peroneal nerve and tibial neurovascular bundle injuries have been reported as potential complications of distal interlocking screw placement, and should be considered in such patients.12
Another consideration for the development of postoperative pain is CRPS, which is thought to be caused by postinjury sympathetic activation that produces pain out of proportion to clinical examination findings.13 Although no postoperative incidence of CRPS in the setting of tibial nailing has been reported, it is a known contributor to poor functional outcomes after fractures or crush injuries to the lower extremity.9 When attempting to diagnose and treat chronic postoperative pain after tibial nailing, the clinician must keep these common etiologies in mind as well as an understanding of the adjacent anatomy.
The saphenous nerve originates from the third and fourth lumbar nerve roots, coursing beneath the inguinal ligament as part of the femoral nerve. As the terminal branch of the femoral nerve, the saphenous nerve runs in the Hunter canal beneath the fascia of the sartorius muscle. It is bordered laterally by the vastus medialis muscle, and posteriorly and laterally by the adductor longus and magnus muscles. The saphenous nerve then crosses the femoral artery superficially from medial to lateral as it courses distally in the canal. As it emerges from the adductor hiatus, the saphenous nerve runs superficial to the gracilis muscle around the posterior border of the sartorius muscle with the descending genicular artery, and becomes a subcutaneous structure at the level of the knee joint. The infrapatellar branch of the saphenous nerve provides sensation to the medial knee, and continues in a subcutaneous course just medial to the posterior aspect of the tibial shaft with the great saphenous vein. The nerve distally supplies sensory input from the medial foot and ankle.1,3,14
There are several causes of saphenous neuralgia related to surgical and nonsurgical trauma.2,3,15,16 The most common cause of nerve injury is iatrogenic traction or transection causing neuralgic sequelae from subsequent neuroma formation. The anatomy of the saphenous nerve puts it at particular risk when performing saphenectomy for vascular procedures, and its infrapatellar branch is at particular risk when performing a medial parapatellar approach for total knee arthroplasty.2,3 In the case of the surgically naïve patient, saphenous nerve entrapment syndromes have also been described, and occur most frequently at the level of the adductor hiatus or as the saphenous nerve courses between the sartorius and gracilis muscles proximal to the knee joint.16
As is illustrated in the present case, orthopedic trauma may be an additional cause of saphenous neuroma formation, leading to symptomatic neuralgia. This case suggests that symptomatic neuroma should be included in the differential diagnosis of posttraumatic pain in the orthopedic trauma patient. It is important to note that, although this case occurred after a severe injury, the intimate association of the saphenous nerve with the tibia places it in a vulnerable position, and traumatic transection is possible after closed injuries to the tibial metadiaphyseal junction or tibial shaft.
Neuroma formation occurs in response to damage to the endoneurium and axon. For an axon to repair properly, the damaged proximal segment must join with, and reenter, the distal stump. As axons attempt to regenerate, occasionally the proximal stump can escape into the surrounding tissue and form a painful neuroma consisting of a disorganized mass of Schwann cells, fibroblasts, blood vessels, and axons with various degrees of myelination. The subsequent neuralgia associated with neuroma formation is caused by chemical or mechanical stimulation of the damaged axons or by spontaneously evoked potentials in the damaged axons. These signals can manifest as a variety of symptoms, including paresthesia and allodynia.17,18
Making the diagnosis of neuroma-related neuralgia can be challenging and nebulous. A characteristic history and positive Tinel sign over the affected area are helpful clinical indicators. However, the clinical finding most predictive of favorable surgical outcome is symptomatic relief after local injection of 1% lidocaine to the affected area. This is an important diagnostic test, especially when attempting to differentiate painful neuroma from other causes of posttraumatic lower extremity pain (eg, CRPS). Such an injection should be performed in the diagnosis and treatment of symptomatic neuroma, and some authors would suggest that insufficient relief of symptoms with diagnostic nerve block is a contraindication to surgical treatment.19
Several treatments for painful neuromas have been described, with variable results.19,20 The most widely accepted treatment of a complete nerve transection with associated neuroma is neurectomy with reimplantation of the proximal end into adjacent bone, muscle, or vein.14,15 Balcin and colleagues21 suggest that vein transposition produces the most favorable outcomes. Simple neurolysis of in-continuity neuromas has also been described with favorable results.
Conclusion
Neuralgia-producing neuromas of the saphenous nerve are relatively uncommon but can lead to persistent pain and frustrating symptoms for the patient. As noted, the diagnosis may elude clinicians, especially in patients with less obvious clinical presentations. We suggest the following algorithm to help distinguish between painful neuroma and other causes of posttraumatic leg pain: (1) physical examination (including testing for instability, joint line tenderness, patellofemoral pain, Tinel sign, and Semmes-Weinstein testing) should be performed, and plain radiographs taken of the involved bones and joints; (2) if all of the above reveal no abnormality, and there is a positive Tinel sign directly over the course of a nerve, an injection of lidocaine over the region of the potential neuroma can be diagnostic; (3) should several abnormalities be present, further investigation using magnetic resonance imaging, bone scan, and/or electromyography may provide additional information that leads to a diagnosis.
Neuralgia and neuroma secondary to iatrogenic saphenous nerve injury have been described in the setting of orthopedic surgical interventions using a medial parapatellar approach, and in vascular surgery procedures for harvest of the saphenous vein.1-3 However, postoperative neuropathic pain caused by saphenous neuroma in the setting of orthopedic trauma has not been described.
We present a case of symptomatic posttraumatic saphenous neuroma after a displaced and laterally angulated open distal one-third tibial fracture. This unreported cause of postinjury neuralgia is an important complication to address as other similar and more common conditions, such as peripheral neuropathy and complex regional pain syndrome (CRPS), can present in a similar manner. Reaching the correct diagnosis can be challenging for clinicians unfamiliar with this condition or its clinical presentation. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 43-year-old woman presented to our practice 2 years after an open distal one-third metadiaphyseal fracture of the tibia with associated segmental fibular fracture (Gustilo-Anderson type II)4 after an automobile/bicycle accident. At the time of injury, she was noted to have a complex medial wound in the region of an open fracture at the junction of the middle and distal thirds of her tibial shaft. She underwent definitive treatment at an outside facility with initial irrigation and débridement and primary wound closure, followed by staged intramedullary nail fixation. Both soft-tissue and bony injuries healed within the expected time frame, and the patient was discharged from orthopedic care.
Approximately 1 year after her initial injury, the patient began to complain of progressive and persistent anteromedial knee pain as well as gradual-onset, medial-sided leg pain. The leg pain began at the level of her previous fracture site, at the distal one-third metadiaphyseal tibial junction, and radiated from the site of her previous medial open wound distally to the medial aspect of her foot. The pain was burning and tingling in nature, with associated hyperesthesia of the affected area. A diagnosis of CRPS was made, and the patient was prescribed a course of desensitization therapy, oral neuromodulating agents, and physical therapy. After 3 months’ therapy, she remained symptomatic and underwent removal of her proximal tibial interlocking screw fixation (Figure 1). When these measures failed to provide symptomatic relief, and having seen several therapists and physicians, including physiatrists, pain management specialists, and orthopedic surgeons, she presented to our clinic for consultation.
Diagnostic Assessment
On presentation, the patient’s surgical incisions were well healed. At the junction of the middle and distal thirds of the tibia, a 4-cm oblique scar was noted over the anteromedial border of the tibia, the site of her previous open fracture. She demonstrated decreased sensation along the length of this oblique scar, as well as in the distribution of the saphenous nerve distally. Further examination of the previously injured region revealed a positive Tinel sign over the course of the saphenous nerve, with radiating pain down the medial aspect of her leg, recreating her symptoms. She otherwise had full range of motion at the knee with mild tenderness to palpation at the medial joint line and patellar tendon. Her lower extremity motor examination, reflexes, and the remainder of her sensory examination were benign.
These findings were consistent with isolated saphenous neuralgia, and selective injection of the saphenous distribution over the injury site was performed. This injection provided immediate symptomatic relief, with the patient reporting preinjection and postinjection pain scores of 7/10 and 2/10, respectively. Because of the clinical improvement demonstrated with selective injection, surgical intervention with exploration and neurolysis of the saphenous nerve was recommended.
Therapeutic Intervention
The patient underwent surgical exploration of her saphenous nerve at the level of her original open fracture. This was done concurrently with a left-knee diagnostic arthroscopy and removal of her intramedullary tibial implant both to exclude intra-articular pathology (given her medial joint-line tenderness and the limitation of magnetic resonance imaging to diagnose meniscus tear in the presence of her tibial hardware) and to remove any potential hardware irritation in the setting of her anterior knee pain.5,6
Preoperatively, the path of the saphenous nerve was marked using the saphenous vein as a guide. An incision overlying the presumed saphenous nerve course was made at the site of her previous open wound and clinical Tinel sign. The saphenous nerve was carefully dissected with loupe magnification, and the distal divisions of the anterior and posterior branches were identified. The anterior branch was found to be in continuity but encased in fibrotic neuroma. Selective neurolysis of this anterior branch was performed. The posterior branch was found to have been traumatically severed, with both the proximal and distal ends encased in neuromatous scar (Figure 2). Neurectomy of the posterior branch was performed and the severed proximal end of the nerve was buried into the adjacent medial gastrocnemius muscle beneath the fascia of the superficial posterior compartment.7-9
Postoperative Course and Outcome
Upon transport to the postsurgical care unit and emergence from sedation, the patient experienced immediate resolution of her neuralgic symptoms. Pathology of the operative specimen showed a benign, disorganized arrangement of axons, Schwann cells, and perineural fibroblasts amidst a fibrous stroma, consistent with traumatic neuroma. At 1-month and 6-month follow-up visits, the patient remained symptom-free, aside from some continued anterior left knee pain near the site of intramedullary nail entry. Her positive Tinel sign had completely resolved, as did her neuralgic symptoms down the medial aspect of her leg. This proved consistent with a diagnosis of neuroma as the cause of the majority of her symptoms. Subjectively, she reported excellent overall pain relief and satisfaction with her treatment and postoperative course.
Discussion
Postoperative pain after intramedullary fixation of tibial shaft fractures is common and can be caused by several clinical entities.5,10 Anterior knee pain is a well-known complication present in up to 73% of patients treated with tibial nailing.10 Osteoarthritis of the knee or ankle as well as nonarthritic ipsilateral ankle pain are also common complaints, often resulting from tibial malunion or malrotation, leading to altered joint kinematics.11 Additionally, superficial peroneal nerve and tibial neurovascular bundle injuries have been reported as potential complications of distal interlocking screw placement, and should be considered in such patients.12
Another consideration for the development of postoperative pain is CRPS, which is thought to be caused by postinjury sympathetic activation that produces pain out of proportion to clinical examination findings.13 Although no postoperative incidence of CRPS in the setting of tibial nailing has been reported, it is a known contributor to poor functional outcomes after fractures or crush injuries to the lower extremity.9 When attempting to diagnose and treat chronic postoperative pain after tibial nailing, the clinician must keep these common etiologies in mind as well as an understanding of the adjacent anatomy.
The saphenous nerve originates from the third and fourth lumbar nerve roots, coursing beneath the inguinal ligament as part of the femoral nerve. As the terminal branch of the femoral nerve, the saphenous nerve runs in the Hunter canal beneath the fascia of the sartorius muscle. It is bordered laterally by the vastus medialis muscle, and posteriorly and laterally by the adductor longus and magnus muscles. The saphenous nerve then crosses the femoral artery superficially from medial to lateral as it courses distally in the canal. As it emerges from the adductor hiatus, the saphenous nerve runs superficial to the gracilis muscle around the posterior border of the sartorius muscle with the descending genicular artery, and becomes a subcutaneous structure at the level of the knee joint. The infrapatellar branch of the saphenous nerve provides sensation to the medial knee, and continues in a subcutaneous course just medial to the posterior aspect of the tibial shaft with the great saphenous vein. The nerve distally supplies sensory input from the medial foot and ankle.1,3,14
There are several causes of saphenous neuralgia related to surgical and nonsurgical trauma.2,3,15,16 The most common cause of nerve injury is iatrogenic traction or transection causing neuralgic sequelae from subsequent neuroma formation. The anatomy of the saphenous nerve puts it at particular risk when performing saphenectomy for vascular procedures, and its infrapatellar branch is at particular risk when performing a medial parapatellar approach for total knee arthroplasty.2,3 In the case of the surgically naïve patient, saphenous nerve entrapment syndromes have also been described, and occur most frequently at the level of the adductor hiatus or as the saphenous nerve courses between the sartorius and gracilis muscles proximal to the knee joint.16
As is illustrated in the present case, orthopedic trauma may be an additional cause of saphenous neuroma formation, leading to symptomatic neuralgia. This case suggests that symptomatic neuroma should be included in the differential diagnosis of posttraumatic pain in the orthopedic trauma patient. It is important to note that, although this case occurred after a severe injury, the intimate association of the saphenous nerve with the tibia places it in a vulnerable position, and traumatic transection is possible after closed injuries to the tibial metadiaphyseal junction or tibial shaft.
Neuroma formation occurs in response to damage to the endoneurium and axon. For an axon to repair properly, the damaged proximal segment must join with, and reenter, the distal stump. As axons attempt to regenerate, occasionally the proximal stump can escape into the surrounding tissue and form a painful neuroma consisting of a disorganized mass of Schwann cells, fibroblasts, blood vessels, and axons with various degrees of myelination. The subsequent neuralgia associated with neuroma formation is caused by chemical or mechanical stimulation of the damaged axons or by spontaneously evoked potentials in the damaged axons. These signals can manifest as a variety of symptoms, including paresthesia and allodynia.17,18
Making the diagnosis of neuroma-related neuralgia can be challenging and nebulous. A characteristic history and positive Tinel sign over the affected area are helpful clinical indicators. However, the clinical finding most predictive of favorable surgical outcome is symptomatic relief after local injection of 1% lidocaine to the affected area. This is an important diagnostic test, especially when attempting to differentiate painful neuroma from other causes of posttraumatic lower extremity pain (eg, CRPS). Such an injection should be performed in the diagnosis and treatment of symptomatic neuroma, and some authors would suggest that insufficient relief of symptoms with diagnostic nerve block is a contraindication to surgical treatment.19
Several treatments for painful neuromas have been described, with variable results.19,20 The most widely accepted treatment of a complete nerve transection with associated neuroma is neurectomy with reimplantation of the proximal end into adjacent bone, muscle, or vein.14,15 Balcin and colleagues21 suggest that vein transposition produces the most favorable outcomes. Simple neurolysis of in-continuity neuromas has also been described with favorable results.
Conclusion
Neuralgia-producing neuromas of the saphenous nerve are relatively uncommon but can lead to persistent pain and frustrating symptoms for the patient. As noted, the diagnosis may elude clinicians, especially in patients with less obvious clinical presentations. We suggest the following algorithm to help distinguish between painful neuroma and other causes of posttraumatic leg pain: (1) physical examination (including testing for instability, joint line tenderness, patellofemoral pain, Tinel sign, and Semmes-Weinstein testing) should be performed, and plain radiographs taken of the involved bones and joints; (2) if all of the above reveal no abnormality, and there is a positive Tinel sign directly over the course of a nerve, an injection of lidocaine over the region of the potential neuroma can be diagnostic; (3) should several abnormalities be present, further investigation using magnetic resonance imaging, bone scan, and/or electromyography may provide additional information that leads to a diagnosis.
1. Senegor M. Iatrogenic saphenous neuralgia: successful treatment with neuroma resection. J Neurosurg. 1991;28(2):295-298.
2. Mountney J, Wilkinson GA. Saphenous neuralgia after coronary artery bypass grafting. Eur J Cardiothorac Surg. 1999;16(4):440-443.
3. Kachar SM, Williams KM, Finn HA. Neuroma of the infrapatellar branch of the saphenous nerve: a cause of reversible knee stiffness after total knee arthroplasty. J Arthroplasty. 2008;23(6):927-930.
4. Gustilo RB, Anderson AB. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58(4):453-458.
5. Keating JF, Orfaly R, O’Brien PJ. Knee pain after tibial nailing. J Orthop Trauma. 1997;11(1):10-13.
6. Chen CY, Lin KC, Yang SW, Tarng YW, Hsu CJ, Renn JH. Influence of nail prominence and insertion point on anterior knee pain after tibial intramedullary nailing. Orthopedics. 2014;37(3):e221-e225.
7. Lewin-Kowalik J, Marcol W, Kotulska K, Mandera M, Klimczak A. Prevention and management of painful neuroma. Neurol Med Chir (Tokyo). 2006;46(2):62-67.
8. Otfinowski J, Pawelec A, Kaluza J. Implantation of peripheral neural stump into muscle and its effect on the development of posttraumatic neuroma. Pol J Pathol. 1994;45:195-202.
9. Van Beek AL. Management of nerve compression syndromes and painful neuromas. In: McCarthy JG, May JW Jr, Littler JW, eds. Plastic Surgery. Philadelphia, PA: WB Saunders; 1990:4817-4858.
10. Lefaivre KA, Guy P, Chan H, Blachut PA. Long-term follow-up of tibial shaft fractures treated with intramedullary nailing. J Orthop Trauma. 2008;22(8):525-529.
11. Milner SA, Davis TR, Muir KR, Greenwood DC, Doherty M. Long-term outcome after tibial shaft fracture: is malunion important? J Bone Joint Surg Am. 2002;84(6):971-980.
12. Roberts CS, King D, Wang M, Seligson D, Voor MJ. Should distal interlocking of tibial nails be performed from medial or lateral direction? Anatomical and biomechanical considerations. J Orthop Trauma. 1999;13(1):27-32.
13. Hogan CJ, Hurwitz SR. Treatment of complex regional pain syndrome of the lower extremity. J Am Acad Orthop Surg. 2002;10(4):281-289.
14. Gray H, Lewis WH. Anatomy of the Human Body. Philadelphia, PA: Lea & Febiger, 1918. Bartleby.com website. http://www.bartleby.com/br/107.html. Accessed September 29, 2015.
15. Myerson MS, McGarvey WC, Henderson MR, Hakim J. Morbidity after crush injuries to the foot. J Orthop Trauma. 1994;8(4):343-349.
16. Kalenak A. Saphenous nerve entrapment. Op Tech Sports Med. 1996;4(1):40-45.
17. Wolf SW, Hotchkiss RN, Pederson WC, Kozin SH. The peripheral neuroma. In: Green DP, Wolfe SW, eds. Green’s Operative Hand Surgery. 6th ed. Philadelphia, PA: Elsevier Churchill Livingstone, 2011;1063-1071.
18. Thordarson DB, Shean CJ. Nerve and tendon lacerations about the foot and ankle. J Am Acad Orthop Surg. 2005;13(3):186-196.
19. Stokvis A, van der Avoort DJ, van Neck JW, Hovius SE, Coert JH. Surgical management of neuroma pain: a prospective follow-up study. Pain. 2010;151(3):862-869.
20. Burchiel KJ, Johans TJ, Ochoa J. The surgical treatment of painful traumatic neuromas. J Neurosurg. 1993;78(5):714-719.
21. Balcin H, Erba P, Wettstein R, Schaefer DJ, Pierer G, Kalbermatten DF. A comparative study of two methods of surgical treatment for painful neuroma. J Bone Joint Surg Br. 2009;91(6):803-808.
1. Senegor M. Iatrogenic saphenous neuralgia: successful treatment with neuroma resection. J Neurosurg. 1991;28(2):295-298.
2. Mountney J, Wilkinson GA. Saphenous neuralgia after coronary artery bypass grafting. Eur J Cardiothorac Surg. 1999;16(4):440-443.
3. Kachar SM, Williams KM, Finn HA. Neuroma of the infrapatellar branch of the saphenous nerve: a cause of reversible knee stiffness after total knee arthroplasty. J Arthroplasty. 2008;23(6):927-930.
4. Gustilo RB, Anderson AB. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58(4):453-458.
5. Keating JF, Orfaly R, O’Brien PJ. Knee pain after tibial nailing. J Orthop Trauma. 1997;11(1):10-13.
6. Chen CY, Lin KC, Yang SW, Tarng YW, Hsu CJ, Renn JH. Influence of nail prominence and insertion point on anterior knee pain after tibial intramedullary nailing. Orthopedics. 2014;37(3):e221-e225.
7. Lewin-Kowalik J, Marcol W, Kotulska K, Mandera M, Klimczak A. Prevention and management of painful neuroma. Neurol Med Chir (Tokyo). 2006;46(2):62-67.
8. Otfinowski J, Pawelec A, Kaluza J. Implantation of peripheral neural stump into muscle and its effect on the development of posttraumatic neuroma. Pol J Pathol. 1994;45:195-202.
9. Van Beek AL. Management of nerve compression syndromes and painful neuromas. In: McCarthy JG, May JW Jr, Littler JW, eds. Plastic Surgery. Philadelphia, PA: WB Saunders; 1990:4817-4858.
10. Lefaivre KA, Guy P, Chan H, Blachut PA. Long-term follow-up of tibial shaft fractures treated with intramedullary nailing. J Orthop Trauma. 2008;22(8):525-529.
11. Milner SA, Davis TR, Muir KR, Greenwood DC, Doherty M. Long-term outcome after tibial shaft fracture: is malunion important? J Bone Joint Surg Am. 2002;84(6):971-980.
12. Roberts CS, King D, Wang M, Seligson D, Voor MJ. Should distal interlocking of tibial nails be performed from medial or lateral direction? Anatomical and biomechanical considerations. J Orthop Trauma. 1999;13(1):27-32.
13. Hogan CJ, Hurwitz SR. Treatment of complex regional pain syndrome of the lower extremity. J Am Acad Orthop Surg. 2002;10(4):281-289.
14. Gray H, Lewis WH. Anatomy of the Human Body. Philadelphia, PA: Lea & Febiger, 1918. Bartleby.com website. http://www.bartleby.com/br/107.html. Accessed September 29, 2015.
15. Myerson MS, McGarvey WC, Henderson MR, Hakim J. Morbidity after crush injuries to the foot. J Orthop Trauma. 1994;8(4):343-349.
16. Kalenak A. Saphenous nerve entrapment. Op Tech Sports Med. 1996;4(1):40-45.
17. Wolf SW, Hotchkiss RN, Pederson WC, Kozin SH. The peripheral neuroma. In: Green DP, Wolfe SW, eds. Green’s Operative Hand Surgery. 6th ed. Philadelphia, PA: Elsevier Churchill Livingstone, 2011;1063-1071.
18. Thordarson DB, Shean CJ. Nerve and tendon lacerations about the foot and ankle. J Am Acad Orthop Surg. 2005;13(3):186-196.
19. Stokvis A, van der Avoort DJ, van Neck JW, Hovius SE, Coert JH. Surgical management of neuroma pain: a prospective follow-up study. Pain. 2010;151(3):862-869.
20. Burchiel KJ, Johans TJ, Ochoa J. The surgical treatment of painful traumatic neuromas. J Neurosurg. 1993;78(5):714-719.
21. Balcin H, Erba P, Wettstein R, Schaefer DJ, Pierer G, Kalbermatten DF. A comparative study of two methods of surgical treatment for painful neuroma. J Bone Joint Surg Br. 2009;91(6):803-808.