User login
Evaluating Pharmacists’ Time Collecting Self-Monitoring Blood Glucose Data
The American Diabetes Association recommends that patients on intensive insulin regimens self-monitor blood glucose (SMBG) to assist in therapy optimization.1 To be useful, SMBG data must be captured by patients, shared with care teams, and used and interpreted by patients and practitioners.2,3 Communication of SMBG data from the patient to practitioner can be challenging. Although technology can help in this process, limitations exist, such as manual data entry into systems, patient and/or practitioner technological challenges (eg, accessing interface), and compatibility and integration between SMBG devices and electronic health record (EHR) systems.4
The Boise Veterans Affairs Medical Center (BVAMC) in Idaho serves more than 100,000 veterans. It includes a main site, community-based outpatient clinics, and a clinical resource hub that provides telehealth services to veterans residing in rural neighboring states. The BVAMC pharmacy department provides both inpatient and outpatient services. At the BVAMC, clinical pharmacist practitioners (CPPs) are independent practitioners who support their care teams in comprehensive medication management and have the ability to initiate, modify, and discontinue drug therapy for referred patients.5 A prominent role of CPPs in primary care teams is to manage patients with uncontrolled diabetes and intensive insulin regimens in which SMBG data are vital to therapy optimization. As collecting SMBG data from patients is seen anecdotally as time intensive, we determined the mean time spent by CPPs collecting patient SMBG data and its potential implications.
Methods
Pharmacists at BVAMC were asked to estimate and record the following: SMBG data collection method, time spent collecting data, extra time spent documenting or formatting SMBG readings, total patient visit time, and visit type. Time was collected in minutes. Extra time spent documenting or formatting SMBG readings included any additional time formatting or entering data in the clinical note after talking to the patient; if this was done while multitasking and talking to the patient, it was not considered extra time. For total patient visit time, pharmacists were asked to estimate only time spent discussing diabetes care and collecting SMBG data. Visit types were categorized as in-person/face-to-face, telephone, and telehealth using clinical video telehealth (CVT)/VA Video Connect (VVC). Data were collected using a standardized spreadsheet. The spreadsheet was pilot tested by a CPP before distribution to all pharmacists.
CPPs were educated about the project in March 2021 and were asked to record data for a 1-week period between April 5, 2021, and April 30, 2021. One CPP also provided delayed data collected from May 17 to 21, 2021, and these data were included in our analysis.
Descriptive statistics were used to determine the mean time spent by CPPs collecting SMBG data. Unpaired t tests were used to compare time spent collecting SMBG data by different collection methods and patient visit types. A P value of ≤ .05 was considered statistically significant. Data were organized in Microsoft Excel, and statistics were completed with JMP Pro v15.
Results
Eight CPPs provided data from 120 patient encounters. For all pa
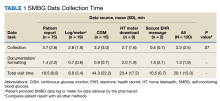
When compared by the SMBG collection method, the longest time spent collecting SMBG data was with patient report (3.7 minutes), and the longest time spent documenting/formatting time was with meter download/home telehealth (2 minutes). There was no statistically significant difference in the time to collect SMBG data between patient report and other methods (3.7 minutes vs 2.8 minutes; P = .07).
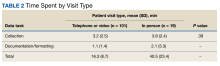
When compared by visit type, there was not a statistically significant difference between time spent collecting in person vs telephone or video SMBG data (3.8 minutes vs 3.2 minutes; P = .39) (Table 2). The most common SMBG collection method for in-person/face-to-face visits was continuous glucose monitor (CGM) (n = 10), followed by meter download/home telehealth (n = 5), patient report (n = 3), and directly from log/meter (n = 1). For telephone or video visits, the most common collection method was patient report (n = 72), followed by directly from log/meter (n = 18), CGM (n = 5), meter download/home telehealth (n = 4), and secure message (n = 2).
Discussion
We found that the mean amount of time spent collecting and documenting/formatting SMBG data was only 4.6 minutes; however, this still represented a substantial portion of visit time. For telephone and CVT/VVC appointments, this represented > 25% of total visit time. While CPPs make important contributions to interprofessional team management of patients with diabetes, their cost is not trivial.6-8 It is worth exploring the most effective and efficient ways to use CPPs. Our results indicate that streamlining SMBG data collection may be beneficial.
Pharmacy technicians, licensed practical nurses/clinical associates, registered nurses/nurse care managers, or other team members could help improve SMBG data collection. Using other team members is also an opportunity for comanagement, for team collaboration, and for more patients to be seen. For example, if a CPP currently has 12 patient encounters that last 20 minutes each, this results in about 240 minutes of direct patient care. If patient encounters were 16 minutes, CPPs could have 15 patient encounters in 240 minutes. Saved time could be used for other clinical tasks involved in disease management or clinical reminder reviews. While there are benefits to CPPs collecting SMBG data, such as further inquiry about patient-reported values, other team members could be trained to ask appropriate follow-up questions for abnormal blood glucose readings. In addition, leveraging current team members and optimizing their roles could prevent the need to acquire additional full-time equivalent employees.
Another opportunity to increase efficiency in SMBG data collection is with SMBG devices and EHR integration.4,9 However, integration can be difficult with different types of SMBG devices and EHR platforms. Education for patients and practitioners could help to ensure accurate and reliable data uploads; patient internet availability; data protection, privacy, and sharing; workflow management; and clear patient-practitioner expectations.10 For example, if patient SMBG data are automatically uploaded to practitioners, patients’ expectations for practitioner review of data and follow-up need to be determined.
We found a subset of 23 patient encounters where data collection and documenting/formatting represented more than half of the total visit time. In this subset, 13 SMBG reports were pulled from a log or meter, 8 were patient reported, and 3 were meter download or home telehealth.
Limitations
A potential reason for the lack of statistically significant differences in SMBG collection method or visit type in this study includes the small sample size. Participation in this work was voluntary, and all participating CPPs had ≥ 3 years of practice in their current setting, which includes a heavy workload of diabetes management. These pharmacists noted self-established procedures/systems for SMBG data collection, including the use of Excel spreadsheets with pregenerated formulas. For less experienced CPPs, SMBG data collection time may be even longer. Pharmacists also noted that they may limit time spent collecting SMBG data depending on the patient encounter and whether they have gathered sufficient data to guide clinical care. Other limitations of this work include data collection from a single institution and that the time documented represented estimates; there was no external monitor.
Conclusions
In this analysis, we found that CPPs spend about 3 minutes collecting SMBG data from patients and about an additional 1 minute documenting and formatting data. While 4 to 5 minutes may not represent a substantial amount of time for 1 patient, it can be when multiplied by several patient encounters. The time spent collecting SMBG data did not significantly differ by collection method or visit type. Opportunities to increase efficiency in SMBG data collection, such as the use of nonpharmacist team members, are worth exploring.
Acknowledgments
Thank you to the pharmacists at the Boise Veterans Affairs Medical Center for their time and support of this work: Danielle Ahlstrom, Paul Black, Robyn Cruz, Sarah Naidoo, Anthony Nelson, Laura Spoutz, Eileen Twomey, Donovan Victorine, and Michelle Wilkin.
1. American Diabetes Association. 7. Diabetes Technology: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(suppl 1):S85-S99. doi:10.2337/dc21-S007
2. Austin MM. The two skill sets of self-monitoring of blood glucose education: the operational and the interpretive. Diabetes Spectr. 2013;26(2):83-90. doi:10.2337/diaspect.26.2.83
3. Gallichan M. Self monitoring of glucose by people with diabetes: evidence based practice. BMJ. 1997;314(7085):964-967. doi:10.1136/bmj.314.7085.964
4. Lewinski AA, Drake C, Shaw RJ, et al. Bridging the integration gap between patient-generated blood glucose data and electronic health records. J Am Med Inform Assoc. 2019;26(7):667-672. doi:10.1093/jamia/ocz039
5. McFarland MS, Groppi J, Jorgenson T, et al. Role of the US Veterans Health Administration clinical pharmacy specialist provider: shaping the future of comprehensive medication management. Can J Hosp Pharm. 2020;73(2):152-158. doi:10.4212/cjhp.v73i2.2982
6. Schmidt K, Caudill J. Hamilton T. Impact of clinical pharmacy specialists on glycemic control in veterans with type 2 diabetes. Am J Health Syst Pharm. 2019;76(suppl 1):S9-S14. doi:10.1093/ajhp/zxy015
7. Sullivan J, Jett BP, Cradick M, Zuber J. Effect of clinical pharmacist intervention on hemoglobin A1c reduction in veteran patients with type 2 diabetes in a rural setting. Ann Pharmacother. 2016;50(12):1023-1027. doi:10.1177/1060028016663564
8. Bloom CI, Ku M, Williams M. Clinical pharmacy specialists’ impact in patient aligned care teams for type 2 diabetes management. J Am Pharm Assoc (2003). 2019;59(5):717-721. doi:10.1016/j.japh.2019.05.002
9. Kumar RB, Goren ND, Stark DE, Wall DP, Longhurst CA. Automated integration of continuous glucose monitor data in the electronic health record using consumer technology. J Am Med Inform Assoc. 2016;23(3):532-537. doi:10.1093/jamia/ocv206
10. Reading MJ, Merrill JA. Converging and diverging needs between patients and providers who are collecting and using patient-generated health data: an integrative review. J Am Med Inform Assoc. 2018;25(6):759-771. doi:10.1093/jamia/ocy006
The American Diabetes Association recommends that patients on intensive insulin regimens self-monitor blood glucose (SMBG) to assist in therapy optimization.1 To be useful, SMBG data must be captured by patients, shared with care teams, and used and interpreted by patients and practitioners.2,3 Communication of SMBG data from the patient to practitioner can be challenging. Although technology can help in this process, limitations exist, such as manual data entry into systems, patient and/or practitioner technological challenges (eg, accessing interface), and compatibility and integration between SMBG devices and electronic health record (EHR) systems.4
The Boise Veterans Affairs Medical Center (BVAMC) in Idaho serves more than 100,000 veterans. It includes a main site, community-based outpatient clinics, and a clinical resource hub that provides telehealth services to veterans residing in rural neighboring states. The BVAMC pharmacy department provides both inpatient and outpatient services. At the BVAMC, clinical pharmacist practitioners (CPPs) are independent practitioners who support their care teams in comprehensive medication management and have the ability to initiate, modify, and discontinue drug therapy for referred patients.5 A prominent role of CPPs in primary care teams is to manage patients with uncontrolled diabetes and intensive insulin regimens in which SMBG data are vital to therapy optimization. As collecting SMBG data from patients is seen anecdotally as time intensive, we determined the mean time spent by CPPs collecting patient SMBG data and its potential implications.
Methods
Pharmacists at BVAMC were asked to estimate and record the following: SMBG data collection method, time spent collecting data, extra time spent documenting or formatting SMBG readings, total patient visit time, and visit type. Time was collected in minutes. Extra time spent documenting or formatting SMBG readings included any additional time formatting or entering data in the clinical note after talking to the patient; if this was done while multitasking and talking to the patient, it was not considered extra time. For total patient visit time, pharmacists were asked to estimate only time spent discussing diabetes care and collecting SMBG data. Visit types were categorized as in-person/face-to-face, telephone, and telehealth using clinical video telehealth (CVT)/VA Video Connect (VVC). Data were collected using a standardized spreadsheet. The spreadsheet was pilot tested by a CPP before distribution to all pharmacists.
CPPs were educated about the project in March 2021 and were asked to record data for a 1-week period between April 5, 2021, and April 30, 2021. One CPP also provided delayed data collected from May 17 to 21, 2021, and these data were included in our analysis.
Descriptive statistics were used to determine the mean time spent by CPPs collecting SMBG data. Unpaired t tests were used to compare time spent collecting SMBG data by different collection methods and patient visit types. A P value of ≤ .05 was considered statistically significant. Data were organized in Microsoft Excel, and statistics were completed with JMP Pro v15.
Results
Eight CPPs provided data from 120 patient encounters. For all pa
When compared by the SMBG collection method, the longest time spent collecting SMBG data was with patient report (3.7 minutes), and the longest time spent documenting/formatting time was with meter download/home telehealth (2 minutes). There was no statistically significant difference in the time to collect SMBG data between patient report and other methods (3.7 minutes vs 2.8 minutes; P = .07).
When compared by visit type, there was not a statistically significant difference between time spent collecting in person vs telephone or video SMBG data (3.8 minutes vs 3.2 minutes; P = .39) (Table 2). The most common SMBG collection method for in-person/face-to-face visits was continuous glucose monitor (CGM) (n = 10), followed by meter download/home telehealth (n = 5), patient report (n = 3), and directly from log/meter (n = 1). For telephone or video visits, the most common collection method was patient report (n = 72), followed by directly from log/meter (n = 18), CGM (n = 5), meter download/home telehealth (n = 4), and secure message (n = 2).
Discussion
We found that the mean amount of time spent collecting and documenting/formatting SMBG data was only 4.6 minutes; however, this still represented a substantial portion of visit time. For telephone and CVT/VVC appointments, this represented > 25% of total visit time. While CPPs make important contributions to interprofessional team management of patients with diabetes, their cost is not trivial.6-8 It is worth exploring the most effective and efficient ways to use CPPs. Our results indicate that streamlining SMBG data collection may be beneficial.
Pharmacy technicians, licensed practical nurses/clinical associates, registered nurses/nurse care managers, or other team members could help improve SMBG data collection. Using other team members is also an opportunity for comanagement, for team collaboration, and for more patients to be seen. For example, if a CPP currently has 12 patient encounters that last 20 minutes each, this results in about 240 minutes of direct patient care. If patient encounters were 16 minutes, CPPs could have 15 patient encounters in 240 minutes. Saved time could be used for other clinical tasks involved in disease management or clinical reminder reviews. While there are benefits to CPPs collecting SMBG data, such as further inquiry about patient-reported values, other team members could be trained to ask appropriate follow-up questions for abnormal blood glucose readings. In addition, leveraging current team members and optimizing their roles could prevent the need to acquire additional full-time equivalent employees.
Another opportunity to increase efficiency in SMBG data collection is with SMBG devices and EHR integration.4,9 However, integration can be difficult with different types of SMBG devices and EHR platforms. Education for patients and practitioners could help to ensure accurate and reliable data uploads; patient internet availability; data protection, privacy, and sharing; workflow management; and clear patient-practitioner expectations.10 For example, if patient SMBG data are automatically uploaded to practitioners, patients’ expectations for practitioner review of data and follow-up need to be determined.
We found a subset of 23 patient encounters where data collection and documenting/formatting represented more than half of the total visit time. In this subset, 13 SMBG reports were pulled from a log or meter, 8 were patient reported, and 3 were meter download or home telehealth.
Limitations
A potential reason for the lack of statistically significant differences in SMBG collection method or visit type in this study includes the small sample size. Participation in this work was voluntary, and all participating CPPs had ≥ 3 years of practice in their current setting, which includes a heavy workload of diabetes management. These pharmacists noted self-established procedures/systems for SMBG data collection, including the use of Excel spreadsheets with pregenerated formulas. For less experienced CPPs, SMBG data collection time may be even longer. Pharmacists also noted that they may limit time spent collecting SMBG data depending on the patient encounter and whether they have gathered sufficient data to guide clinical care. Other limitations of this work include data collection from a single institution and that the time documented represented estimates; there was no external monitor.
Conclusions
In this analysis, we found that CPPs spend about 3 minutes collecting SMBG data from patients and about an additional 1 minute documenting and formatting data. While 4 to 5 minutes may not represent a substantial amount of time for 1 patient, it can be when multiplied by several patient encounters. The time spent collecting SMBG data did not significantly differ by collection method or visit type. Opportunities to increase efficiency in SMBG data collection, such as the use of nonpharmacist team members, are worth exploring.
Acknowledgments
Thank you to the pharmacists at the Boise Veterans Affairs Medical Center for their time and support of this work: Danielle Ahlstrom, Paul Black, Robyn Cruz, Sarah Naidoo, Anthony Nelson, Laura Spoutz, Eileen Twomey, Donovan Victorine, and Michelle Wilkin.
The American Diabetes Association recommends that patients on intensive insulin regimens self-monitor blood glucose (SMBG) to assist in therapy optimization.1 To be useful, SMBG data must be captured by patients, shared with care teams, and used and interpreted by patients and practitioners.2,3 Communication of SMBG data from the patient to practitioner can be challenging. Although technology can help in this process, limitations exist, such as manual data entry into systems, patient and/or practitioner technological challenges (eg, accessing interface), and compatibility and integration between SMBG devices and electronic health record (EHR) systems.4
The Boise Veterans Affairs Medical Center (BVAMC) in Idaho serves more than 100,000 veterans. It includes a main site, community-based outpatient clinics, and a clinical resource hub that provides telehealth services to veterans residing in rural neighboring states. The BVAMC pharmacy department provides both inpatient and outpatient services. At the BVAMC, clinical pharmacist practitioners (CPPs) are independent practitioners who support their care teams in comprehensive medication management and have the ability to initiate, modify, and discontinue drug therapy for referred patients.5 A prominent role of CPPs in primary care teams is to manage patients with uncontrolled diabetes and intensive insulin regimens in which SMBG data are vital to therapy optimization. As collecting SMBG data from patients is seen anecdotally as time intensive, we determined the mean time spent by CPPs collecting patient SMBG data and its potential implications.
Methods
Pharmacists at BVAMC were asked to estimate and record the following: SMBG data collection method, time spent collecting data, extra time spent documenting or formatting SMBG readings, total patient visit time, and visit type. Time was collected in minutes. Extra time spent documenting or formatting SMBG readings included any additional time formatting or entering data in the clinical note after talking to the patient; if this was done while multitasking and talking to the patient, it was not considered extra time. For total patient visit time, pharmacists were asked to estimate only time spent discussing diabetes care and collecting SMBG data. Visit types were categorized as in-person/face-to-face, telephone, and telehealth using clinical video telehealth (CVT)/VA Video Connect (VVC). Data were collected using a standardized spreadsheet. The spreadsheet was pilot tested by a CPP before distribution to all pharmacists.
CPPs were educated about the project in March 2021 and were asked to record data for a 1-week period between April 5, 2021, and April 30, 2021. One CPP also provided delayed data collected from May 17 to 21, 2021, and these data were included in our analysis.
Descriptive statistics were used to determine the mean time spent by CPPs collecting SMBG data. Unpaired t tests were used to compare time spent collecting SMBG data by different collection methods and patient visit types. A P value of ≤ .05 was considered statistically significant. Data were organized in Microsoft Excel, and statistics were completed with JMP Pro v15.
Results
Eight CPPs provided data from 120 patient encounters. For all pa
When compared by the SMBG collection method, the longest time spent collecting SMBG data was with patient report (3.7 minutes), and the longest time spent documenting/formatting time was with meter download/home telehealth (2 minutes). There was no statistically significant difference in the time to collect SMBG data between patient report and other methods (3.7 minutes vs 2.8 minutes; P = .07).
When compared by visit type, there was not a statistically significant difference between time spent collecting in person vs telephone or video SMBG data (3.8 minutes vs 3.2 minutes; P = .39) (Table 2). The most common SMBG collection method for in-person/face-to-face visits was continuous glucose monitor (CGM) (n = 10), followed by meter download/home telehealth (n = 5), patient report (n = 3), and directly from log/meter (n = 1). For telephone or video visits, the most common collection method was patient report (n = 72), followed by directly from log/meter (n = 18), CGM (n = 5), meter download/home telehealth (n = 4), and secure message (n = 2).
Discussion
We found that the mean amount of time spent collecting and documenting/formatting SMBG data was only 4.6 minutes; however, this still represented a substantial portion of visit time. For telephone and CVT/VVC appointments, this represented > 25% of total visit time. While CPPs make important contributions to interprofessional team management of patients with diabetes, their cost is not trivial.6-8 It is worth exploring the most effective and efficient ways to use CPPs. Our results indicate that streamlining SMBG data collection may be beneficial.
Pharmacy technicians, licensed practical nurses/clinical associates, registered nurses/nurse care managers, or other team members could help improve SMBG data collection. Using other team members is also an opportunity for comanagement, for team collaboration, and for more patients to be seen. For example, if a CPP currently has 12 patient encounters that last 20 minutes each, this results in about 240 minutes of direct patient care. If patient encounters were 16 minutes, CPPs could have 15 patient encounters in 240 minutes. Saved time could be used for other clinical tasks involved in disease management or clinical reminder reviews. While there are benefits to CPPs collecting SMBG data, such as further inquiry about patient-reported values, other team members could be trained to ask appropriate follow-up questions for abnormal blood glucose readings. In addition, leveraging current team members and optimizing their roles could prevent the need to acquire additional full-time equivalent employees.
Another opportunity to increase efficiency in SMBG data collection is with SMBG devices and EHR integration.4,9 However, integration can be difficult with different types of SMBG devices and EHR platforms. Education for patients and practitioners could help to ensure accurate and reliable data uploads; patient internet availability; data protection, privacy, and sharing; workflow management; and clear patient-practitioner expectations.10 For example, if patient SMBG data are automatically uploaded to practitioners, patients’ expectations for practitioner review of data and follow-up need to be determined.
We found a subset of 23 patient encounters where data collection and documenting/formatting represented more than half of the total visit time. In this subset, 13 SMBG reports were pulled from a log or meter, 8 were patient reported, and 3 were meter download or home telehealth.
Limitations
A potential reason for the lack of statistically significant differences in SMBG collection method or visit type in this study includes the small sample size. Participation in this work was voluntary, and all participating CPPs had ≥ 3 years of practice in their current setting, which includes a heavy workload of diabetes management. These pharmacists noted self-established procedures/systems for SMBG data collection, including the use of Excel spreadsheets with pregenerated formulas. For less experienced CPPs, SMBG data collection time may be even longer. Pharmacists also noted that they may limit time spent collecting SMBG data depending on the patient encounter and whether they have gathered sufficient data to guide clinical care. Other limitations of this work include data collection from a single institution and that the time documented represented estimates; there was no external monitor.
Conclusions
In this analysis, we found that CPPs spend about 3 minutes collecting SMBG data from patients and about an additional 1 minute documenting and formatting data. While 4 to 5 minutes may not represent a substantial amount of time for 1 patient, it can be when multiplied by several patient encounters. The time spent collecting SMBG data did not significantly differ by collection method or visit type. Opportunities to increase efficiency in SMBG data collection, such as the use of nonpharmacist team members, are worth exploring.
Acknowledgments
Thank you to the pharmacists at the Boise Veterans Affairs Medical Center for their time and support of this work: Danielle Ahlstrom, Paul Black, Robyn Cruz, Sarah Naidoo, Anthony Nelson, Laura Spoutz, Eileen Twomey, Donovan Victorine, and Michelle Wilkin.
1. American Diabetes Association. 7. Diabetes Technology: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(suppl 1):S85-S99. doi:10.2337/dc21-S007
2. Austin MM. The two skill sets of self-monitoring of blood glucose education: the operational and the interpretive. Diabetes Spectr. 2013;26(2):83-90. doi:10.2337/diaspect.26.2.83
3. Gallichan M. Self monitoring of glucose by people with diabetes: evidence based practice. BMJ. 1997;314(7085):964-967. doi:10.1136/bmj.314.7085.964
4. Lewinski AA, Drake C, Shaw RJ, et al. Bridging the integration gap between patient-generated blood glucose data and electronic health records. J Am Med Inform Assoc. 2019;26(7):667-672. doi:10.1093/jamia/ocz039
5. McFarland MS, Groppi J, Jorgenson T, et al. Role of the US Veterans Health Administration clinical pharmacy specialist provider: shaping the future of comprehensive medication management. Can J Hosp Pharm. 2020;73(2):152-158. doi:10.4212/cjhp.v73i2.2982
6. Schmidt K, Caudill J. Hamilton T. Impact of clinical pharmacy specialists on glycemic control in veterans with type 2 diabetes. Am J Health Syst Pharm. 2019;76(suppl 1):S9-S14. doi:10.1093/ajhp/zxy015
7. Sullivan J, Jett BP, Cradick M, Zuber J. Effect of clinical pharmacist intervention on hemoglobin A1c reduction in veteran patients with type 2 diabetes in a rural setting. Ann Pharmacother. 2016;50(12):1023-1027. doi:10.1177/1060028016663564
8. Bloom CI, Ku M, Williams M. Clinical pharmacy specialists’ impact in patient aligned care teams for type 2 diabetes management. J Am Pharm Assoc (2003). 2019;59(5):717-721. doi:10.1016/j.japh.2019.05.002
9. Kumar RB, Goren ND, Stark DE, Wall DP, Longhurst CA. Automated integration of continuous glucose monitor data in the electronic health record using consumer technology. J Am Med Inform Assoc. 2016;23(3):532-537. doi:10.1093/jamia/ocv206
10. Reading MJ, Merrill JA. Converging and diverging needs between patients and providers who are collecting and using patient-generated health data: an integrative review. J Am Med Inform Assoc. 2018;25(6):759-771. doi:10.1093/jamia/ocy006
1. American Diabetes Association. 7. Diabetes Technology: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(suppl 1):S85-S99. doi:10.2337/dc21-S007
2. Austin MM. The two skill sets of self-monitoring of blood glucose education: the operational and the interpretive. Diabetes Spectr. 2013;26(2):83-90. doi:10.2337/diaspect.26.2.83
3. Gallichan M. Self monitoring of glucose by people with diabetes: evidence based practice. BMJ. 1997;314(7085):964-967. doi:10.1136/bmj.314.7085.964
4. Lewinski AA, Drake C, Shaw RJ, et al. Bridging the integration gap between patient-generated blood glucose data and electronic health records. J Am Med Inform Assoc. 2019;26(7):667-672. doi:10.1093/jamia/ocz039
5. McFarland MS, Groppi J, Jorgenson T, et al. Role of the US Veterans Health Administration clinical pharmacy specialist provider: shaping the future of comprehensive medication management. Can J Hosp Pharm. 2020;73(2):152-158. doi:10.4212/cjhp.v73i2.2982
6. Schmidt K, Caudill J. Hamilton T. Impact of clinical pharmacy specialists on glycemic control in veterans with type 2 diabetes. Am J Health Syst Pharm. 2019;76(suppl 1):S9-S14. doi:10.1093/ajhp/zxy015
7. Sullivan J, Jett BP, Cradick M, Zuber J. Effect of clinical pharmacist intervention on hemoglobin A1c reduction in veteran patients with type 2 diabetes in a rural setting. Ann Pharmacother. 2016;50(12):1023-1027. doi:10.1177/1060028016663564
8. Bloom CI, Ku M, Williams M. Clinical pharmacy specialists’ impact in patient aligned care teams for type 2 diabetes management. J Am Pharm Assoc (2003). 2019;59(5):717-721. doi:10.1016/j.japh.2019.05.002
9. Kumar RB, Goren ND, Stark DE, Wall DP, Longhurst CA. Automated integration of continuous glucose monitor data in the electronic health record using consumer technology. J Am Med Inform Assoc. 2016;23(3):532-537. doi:10.1093/jamia/ocv206
10. Reading MJ, Merrill JA. Converging and diverging needs between patients and providers who are collecting and using patient-generated health data: an integrative review. J Am Med Inform Assoc. 2018;25(6):759-771. doi:10.1093/jamia/ocy006
Evaluating Pharmacists’ Time Collecting Self-Monitoring Blood Glucose Data
The American Diabetes Association recommends that patients on intensive insulin regimens self-monitor blood glucose (SMBG) to assist in therapy optimization.1 To be useful, SMBG data must be captured by patients, shared with care teams, and used and interpreted by patients and practitioners.2,3 Communication of SMBG data from the patient to practitioner can be challenging. Although technology can help in this process, limitations exist, such as manual data entry into systems, patient and/or practitioner technological challenges (eg, accessing interface), and compatibility and integration between SMBG devices and electronic health record (EHR) systems.4
The Boise Veterans Affairs Medical Center (BVAMC) in Idaho serves more than 100,000 veterans. It includes a main site, community-based outpatient clinics, and a clinical resource hub that provides telehealth services to veterans residing in rural neighboring states. The BVAMC pharmacy department provides both inpatient and outpatient services. At the BVAMC, clinical pharmacist practitioners (CPPs) are independent practitioners who support their care teams in comprehensive medication management and have the ability to initiate, modify, and discontinue drug therapy for referred patients.5 A prominent role of CPPs in primary care teams is to manage patients with uncontrolled diabetes and intensive insulin regimens, in which SMBG data are vital to therapy optimization. As collecting SMBG data from patients is seen anecdotally as time intensive, we determined the mean time spent by CPPs collecting patient SMBG data and its potential implications.
Methods
Pharmacists at BVAMC were asked to estimate and record the following: SMBG data collection method, time spent collecting data, extra time spent documenting or formatting SMBG readings, total patient visit time, and visit type. Time was collected in minutes. Extra time spent documenting or formatting SMBG readings included any additional time formatting or entering data in the clinical note after talking to the patient; if this was done while multitasking and talking to the patient, it was not considered extra time. For total patient visit time, pharmacists were asked to estimate only time spent discussing diabetes care and collecting SMBG data. Visit types were categorized as in-person/face-to-face, telephone, and telehealth using clinical video telehealth (CVT)/VA Video Connect (VVC). Data were collected using a standardized spreadsheet. The spreadsheet was pilot tested by a CPP before distribution to all pharmacists.
CPPs were educated about the project in March 2021 and were asked to record data for a 1-week period between April 5, 2021, and April 30, 2021. One CPP also provided delayed data collected from May 17 to 21, 2021, and these data were included in our analysis.
Descriptive statistics were used to determine the mean time spent by CPPs collecting SMBG data. Unpaired t tests were used to compare time spent collecting SMBG data by different collection methods and patient visit types. A P value of ≤ .05 was considered statistically significant. Data were organized in Microsoft Excel, and statistics were completed with JMP Pro v15.
Results
Eight CPPs provided data from 120 patient encounters. For all pa
When compared by the SMBG collection method, the longest time spent collecting SMBG data was with patient report (3.7 minutes), and the longest time spent documenting/formatting time was with meter download/home telehealth (2 minutes). There was no statistically significant difference in the time to collect SMBG data between patient report and other methods (3.7 minutes vs 2.8 minutes; P = .07).
When compared by visit type, there was not a statistically significant difference between time spent collecting SMBG data (3.8 minutes vs 3.2 minutes; P = .39) (Table 2).
Discussion
We found that the mean amount of time spent collecting and documenting/formatting SMBG data was only 4.6 minutes; however, this still represented a substantial portion of visit time. For telephone and CVT/VVC appointments, this represented > 25% of total visit time. While CPPs make important contributions to interprofessional team management of patients with diabetes, their cost is not trivial.6-8 It is worth exploring the most effective and efficient ways to use CPPs. Our results indicate that streamlining SMBG data collection may be beneficial.
Pharmacy technicians, licensed practical nurses/clinical associates, registered nurses/nurse care managers, or other team members could help improve SMBG data collection. Using other team members is also an opportunity for comanagement, for team collaboration, and for more patients to be seen. For example, if a CPP currently has 12 patient encounters that last 20 minutes each, this results in about 240 minutes of direct patient care. If patient encounters were 16 minutes, CPPS could have 15 patient encounters in 240 minutes. Saved time could be used for other clinical tasks involved in disease management or clinical reminder reviews. While there are benefits to CPPs collecting SMBG data, such as further inquiry about patient-reported values, other team members could also be trained to ask appropriate follow-up questions for abnormal blood glucose readings. In addition, leveraging current team members and optimizing their roles could prevent the need to acquire additional full-time equivalent employees.
Another opportunity to increase efficiency in SMBG data collection is with SMBG devices and EHR integration.4,9 However, integration can be difficult with different types of SMBG devices and EHR platforms. Education for patients and practitioners could help to ensure accurate and reliable data uploads; patient internet availability; data protection, privacy, and sharing; workflow management; and clear patient-practitioner expectations.10 For example, if patient SMBG data are automatically uploaded to practitioners, patients’ expectations for practitioner review of data and follow-up need to be determined.
We found a subset of patient encounters (n = 23) where data collection and documenting/formatting represented more than half of the total visit time. In this subset, 13 SMBG reports were pulled from a log or meter, 8 were patient reported, and 3 were meter download or home telehealth.
Limitations
A potential reason for the lack of statistically significant differences in SMBG collection method or visit type in this study includes the small sample size. Participation in this work was voluntary, and all participating CPPs had ≥ 3 years of practice in their current setting, which includes a heavy workload of diabetes management. These pharmacists noted self-established procedures/systems for SMBG data collection, including the use of Excel spreadsheets with pregenerated formulas. For less experienced CPPs, SMBG data collection time may be even longer. Pharmacists also noted that they may limit time spent collecting SMBG data depending on the patient encounter and whether they have gathered sufficient data to guide clinical care. Other limitations of this work include data collection from a single institution and that the time documented represented estimates; there was no external monitor.
Conclusions
In this analysis, we found that CPPs spend about 3 minutes collecting SMBG data from patients, and about an additional 1 minute documenting and formatting data. While 4 to 5 minutes may not represent a substantial amount of time for one patient, it can be when multiplied by several patient encounters. The time spent collecting SMBG data did not significantly differ by collection method or visit type. Opportunities to increase efficiency in SMBG data collection, such as the use of nonpharmacist team members are worth exploring.
Acknowledgments
Thank you to the pharmacists at the Boise Veterans Affairs Medical Center for their time and support of this work: Danielle Ahlstrom, Paul Black, Robyn Cruz, Sarah Naidoo, Anthony Nelson, Laura Spoutz, Eileen Twomey, Donovan Victorine, and Michelle Wilkin.
1. American Diabetes Association. 7. Diabetes Technology: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(suppl 1):S85-S99. doi:10.2337/dc21-S007
2. Austin MM. The two skill sets of self-monitoring of blood glucose education: the operational and the interpretive. Diabetes Spectr. 2013;26(2):83-90. doi:10.2337/diaspect.26.2.83
3. Gallichan M. Self monitoring of glucose by people with diabetes: evidence based practice. BMJ. 1997;314(7085):964-967. doi:10.1136/bmj.314.7085.964
4. Lewinski AA, Drake C, Shaw RJ, et al. Bridging the integration gap between patient-generated blood glucose data and electronic health records. J Am Med Inform Assoc. 2019;26(7):667-672. doi:10.1093/jamia/ocz039
5. McFarland MS, Groppi J, Jorgenson T, et al. Role of the US Veterans Health Administration clinical pharmacy specialist provider: shaping the future of comprehensive medication management. Can J Hosp Pharm. 2020;73(2):152-158. doi:10.4212/cjhp.v73i2.2982
6. Schmidt K, Caudill J. Hamilton T. Impact of clinical pharmacy specialists on glycemic control in veterans with type 2 diabetes. Am J Health Syst Pharm. 2019;76(suppl 1):S9-S14. doi:10.1093/ajhp/zxy015
7. Sullivan J, Jett BP, Cradick M, Zuber J. Effect of clinical pharmacist intervention on hemoglobin A1c reduction in veteran patients with type 2 diabetes in a rural setting. Ann Pharmacother. 2016;50(12):1023-1027. doi:10.1177/1060028016663564
8. Bloom CI, Ku M, Williams M. Clinical pharmacy specialists’ impact in patient aligned care teams for type 2 diabetes management. J Am Pharm Assoc (2003). 2019;59(5):717-721. doi:10.1016/j.japh.2019.05.002
9. Kumar RB, Goren ND, Stark DE, Wall DP, Longhurst CA. Automated integration of continuous glucose monitor data in the electronic health record using consumer technology. J Am Med Inform Assoc. 2016;23(3):532-537. doi:10.1093/jamia/ocv206
10. Reading MJ, Merrill JA. Converging and diverging needs between patients and providers who are collecting and using patient-generated health data: an integrative review. J Am Med Inform Assoc. 2018;25(6):759-771. doi:10.1093/jamia/ocy006
The American Diabetes Association recommends that patients on intensive insulin regimens self-monitor blood glucose (SMBG) to assist in therapy optimization.1 To be useful, SMBG data must be captured by patients, shared with care teams, and used and interpreted by patients and practitioners.2,3 Communication of SMBG data from the patient to practitioner can be challenging. Although technology can help in this process, limitations exist, such as manual data entry into systems, patient and/or practitioner technological challenges (eg, accessing interface), and compatibility and integration between SMBG devices and electronic health record (EHR) systems.4
The Boise Veterans Affairs Medical Center (BVAMC) in Idaho serves more than 100,000 veterans. It includes a main site, community-based outpatient clinics, and a clinical resource hub that provides telehealth services to veterans residing in rural neighboring states. The BVAMC pharmacy department provides both inpatient and outpatient services. At the BVAMC, clinical pharmacist practitioners (CPPs) are independent practitioners who support their care teams in comprehensive medication management and have the ability to initiate, modify, and discontinue drug therapy for referred patients.5 A prominent role of CPPs in primary care teams is to manage patients with uncontrolled diabetes and intensive insulin regimens, in which SMBG data are vital to therapy optimization. As collecting SMBG data from patients is seen anecdotally as time intensive, we determined the mean time spent by CPPs collecting patient SMBG data and its potential implications.
Methods
Pharmacists at BVAMC were asked to estimate and record the following: SMBG data collection method, time spent collecting data, extra time spent documenting or formatting SMBG readings, total patient visit time, and visit type. Time was collected in minutes. Extra time spent documenting or formatting SMBG readings included any additional time formatting or entering data in the clinical note after talking to the patient; if this was done while multitasking and talking to the patient, it was not considered extra time. For total patient visit time, pharmacists were asked to estimate only time spent discussing diabetes care and collecting SMBG data. Visit types were categorized as in-person/face-to-face, telephone, and telehealth using clinical video telehealth (CVT)/VA Video Connect (VVC). Data were collected using a standardized spreadsheet. The spreadsheet was pilot tested by a CPP before distribution to all pharmacists.
CPPs were educated about the project in March 2021 and were asked to record data for a 1-week period between April 5, 2021, and April 30, 2021. One CPP also provided delayed data collected from May 17 to 21, 2021, and these data were included in our analysis.
Descriptive statistics were used to determine the mean time spent by CPPs collecting SMBG data. Unpaired t tests were used to compare time spent collecting SMBG data by different collection methods and patient visit types. A P value of ≤ .05 was considered statistically significant. Data were organized in Microsoft Excel, and statistics were completed with JMP Pro v15.
Results
Eight CPPs provided data from 120 patient encounters. For all pa
When compared by the SMBG collection method, the longest time spent collecting SMBG data was with patient report (3.7 minutes), and the longest time spent documenting/formatting time was with meter download/home telehealth (2 minutes). There was no statistically significant difference in the time to collect SMBG data between patient report and other methods (3.7 minutes vs 2.8 minutes; P = .07).
When compared by visit type, there was not a statistically significant difference between time spent collecting SMBG data (3.8 minutes vs 3.2 minutes; P = .39) (Table 2).
Discussion
We found that the mean amount of time spent collecting and documenting/formatting SMBG data was only 4.6 minutes; however, this still represented a substantial portion of visit time. For telephone and CVT/VVC appointments, this represented > 25% of total visit time. While CPPs make important contributions to interprofessional team management of patients with diabetes, their cost is not trivial.6-8 It is worth exploring the most effective and efficient ways to use CPPs. Our results indicate that streamlining SMBG data collection may be beneficial.
Pharmacy technicians, licensed practical nurses/clinical associates, registered nurses/nurse care managers, or other team members could help improve SMBG data collection. Using other team members is also an opportunity for comanagement, for team collaboration, and for more patients to be seen. For example, if a CPP currently has 12 patient encounters that last 20 minutes each, this results in about 240 minutes of direct patient care. If patient encounters were 16 minutes, CPPS could have 15 patient encounters in 240 minutes. Saved time could be used for other clinical tasks involved in disease management or clinical reminder reviews. While there are benefits to CPPs collecting SMBG data, such as further inquiry about patient-reported values, other team members could also be trained to ask appropriate follow-up questions for abnormal blood glucose readings. In addition, leveraging current team members and optimizing their roles could prevent the need to acquire additional full-time equivalent employees.
Another opportunity to increase efficiency in SMBG data collection is with SMBG devices and EHR integration.4,9 However, integration can be difficult with different types of SMBG devices and EHR platforms. Education for patients and practitioners could help to ensure accurate and reliable data uploads; patient internet availability; data protection, privacy, and sharing; workflow management; and clear patient-practitioner expectations.10 For example, if patient SMBG data are automatically uploaded to practitioners, patients’ expectations for practitioner review of data and follow-up need to be determined.
We found a subset of patient encounters (n = 23) where data collection and documenting/formatting represented more than half of the total visit time. In this subset, 13 SMBG reports were pulled from a log or meter, 8 were patient reported, and 3 were meter download or home telehealth.
Limitations
A potential reason for the lack of statistically significant differences in SMBG collection method or visit type in this study includes the small sample size. Participation in this work was voluntary, and all participating CPPs had ≥ 3 years of practice in their current setting, which includes a heavy workload of diabetes management. These pharmacists noted self-established procedures/systems for SMBG data collection, including the use of Excel spreadsheets with pregenerated formulas. For less experienced CPPs, SMBG data collection time may be even longer. Pharmacists also noted that they may limit time spent collecting SMBG data depending on the patient encounter and whether they have gathered sufficient data to guide clinical care. Other limitations of this work include data collection from a single institution and that the time documented represented estimates; there was no external monitor.
Conclusions
In this analysis, we found that CPPs spend about 3 minutes collecting SMBG data from patients, and about an additional 1 minute documenting and formatting data. While 4 to 5 minutes may not represent a substantial amount of time for one patient, it can be when multiplied by several patient encounters. The time spent collecting SMBG data did not significantly differ by collection method or visit type. Opportunities to increase efficiency in SMBG data collection, such as the use of nonpharmacist team members are worth exploring.
Acknowledgments
Thank you to the pharmacists at the Boise Veterans Affairs Medical Center for their time and support of this work: Danielle Ahlstrom, Paul Black, Robyn Cruz, Sarah Naidoo, Anthony Nelson, Laura Spoutz, Eileen Twomey, Donovan Victorine, and Michelle Wilkin.
The American Diabetes Association recommends that patients on intensive insulin regimens self-monitor blood glucose (SMBG) to assist in therapy optimization.1 To be useful, SMBG data must be captured by patients, shared with care teams, and used and interpreted by patients and practitioners.2,3 Communication of SMBG data from the patient to practitioner can be challenging. Although technology can help in this process, limitations exist, such as manual data entry into systems, patient and/or practitioner technological challenges (eg, accessing interface), and compatibility and integration between SMBG devices and electronic health record (EHR) systems.4
The Boise Veterans Affairs Medical Center (BVAMC) in Idaho serves more than 100,000 veterans. It includes a main site, community-based outpatient clinics, and a clinical resource hub that provides telehealth services to veterans residing in rural neighboring states. The BVAMC pharmacy department provides both inpatient and outpatient services. At the BVAMC, clinical pharmacist practitioners (CPPs) are independent practitioners who support their care teams in comprehensive medication management and have the ability to initiate, modify, and discontinue drug therapy for referred patients.5 A prominent role of CPPs in primary care teams is to manage patients with uncontrolled diabetes and intensive insulin regimens, in which SMBG data are vital to therapy optimization. As collecting SMBG data from patients is seen anecdotally as time intensive, we determined the mean time spent by CPPs collecting patient SMBG data and its potential implications.
Methods
Pharmacists at BVAMC were asked to estimate and record the following: SMBG data collection method, time spent collecting data, extra time spent documenting or formatting SMBG readings, total patient visit time, and visit type. Time was collected in minutes. Extra time spent documenting or formatting SMBG readings included any additional time formatting or entering data in the clinical note after talking to the patient; if this was done while multitasking and talking to the patient, it was not considered extra time. For total patient visit time, pharmacists were asked to estimate only time spent discussing diabetes care and collecting SMBG data. Visit types were categorized as in-person/face-to-face, telephone, and telehealth using clinical video telehealth (CVT)/VA Video Connect (VVC). Data were collected using a standardized spreadsheet. The spreadsheet was pilot tested by a CPP before distribution to all pharmacists.
CPPs were educated about the project in March 2021 and were asked to record data for a 1-week period between April 5, 2021, and April 30, 2021. One CPP also provided delayed data collected from May 17 to 21, 2021, and these data were included in our analysis.
Descriptive statistics were used to determine the mean time spent by CPPs collecting SMBG data. Unpaired t tests were used to compare time spent collecting SMBG data by different collection methods and patient visit types. A P value of ≤ .05 was considered statistically significant. Data were organized in Microsoft Excel, and statistics were completed with JMP Pro v15.
Results
Eight CPPs provided data from 120 patient encounters. For all pa
When compared by the SMBG collection method, the longest time spent collecting SMBG data was with patient report (3.7 minutes), and the longest time spent documenting/formatting time was with meter download/home telehealth (2 minutes). There was no statistically significant difference in the time to collect SMBG data between patient report and other methods (3.7 minutes vs 2.8 minutes; P = .07).
When compared by visit type, there was not a statistically significant difference between time spent collecting SMBG data (3.8 minutes vs 3.2 minutes; P = .39) (Table 2).
Discussion
We found that the mean amount of time spent collecting and documenting/formatting SMBG data was only 4.6 minutes; however, this still represented a substantial portion of visit time. For telephone and CVT/VVC appointments, this represented > 25% of total visit time. While CPPs make important contributions to interprofessional team management of patients with diabetes, their cost is not trivial.6-8 It is worth exploring the most effective and efficient ways to use CPPs. Our results indicate that streamlining SMBG data collection may be beneficial.
Pharmacy technicians, licensed practical nurses/clinical associates, registered nurses/nurse care managers, or other team members could help improve SMBG data collection. Using other team members is also an opportunity for comanagement, for team collaboration, and for more patients to be seen. For example, if a CPP currently has 12 patient encounters that last 20 minutes each, this results in about 240 minutes of direct patient care. If patient encounters were 16 minutes, CPPS could have 15 patient encounters in 240 minutes. Saved time could be used for other clinical tasks involved in disease management or clinical reminder reviews. While there are benefits to CPPs collecting SMBG data, such as further inquiry about patient-reported values, other team members could also be trained to ask appropriate follow-up questions for abnormal blood glucose readings. In addition, leveraging current team members and optimizing their roles could prevent the need to acquire additional full-time equivalent employees.
Another opportunity to increase efficiency in SMBG data collection is with SMBG devices and EHR integration.4,9 However, integration can be difficult with different types of SMBG devices and EHR platforms. Education for patients and practitioners could help to ensure accurate and reliable data uploads; patient internet availability; data protection, privacy, and sharing; workflow management; and clear patient-practitioner expectations.10 For example, if patient SMBG data are automatically uploaded to practitioners, patients’ expectations for practitioner review of data and follow-up need to be determined.
We found a subset of patient encounters (n = 23) where data collection and documenting/formatting represented more than half of the total visit time. In this subset, 13 SMBG reports were pulled from a log or meter, 8 were patient reported, and 3 were meter download or home telehealth.
Limitations
A potential reason for the lack of statistically significant differences in SMBG collection method or visit type in this study includes the small sample size. Participation in this work was voluntary, and all participating CPPs had ≥ 3 years of practice in their current setting, which includes a heavy workload of diabetes management. These pharmacists noted self-established procedures/systems for SMBG data collection, including the use of Excel spreadsheets with pregenerated formulas. For less experienced CPPs, SMBG data collection time may be even longer. Pharmacists also noted that they may limit time spent collecting SMBG data depending on the patient encounter and whether they have gathered sufficient data to guide clinical care. Other limitations of this work include data collection from a single institution and that the time documented represented estimates; there was no external monitor.
Conclusions
In this analysis, we found that CPPs spend about 3 minutes collecting SMBG data from patients, and about an additional 1 minute documenting and formatting data. While 4 to 5 minutes may not represent a substantial amount of time for one patient, it can be when multiplied by several patient encounters. The time spent collecting SMBG data did not significantly differ by collection method or visit type. Opportunities to increase efficiency in SMBG data collection, such as the use of nonpharmacist team members are worth exploring.
Acknowledgments
Thank you to the pharmacists at the Boise Veterans Affairs Medical Center for their time and support of this work: Danielle Ahlstrom, Paul Black, Robyn Cruz, Sarah Naidoo, Anthony Nelson, Laura Spoutz, Eileen Twomey, Donovan Victorine, and Michelle Wilkin.
1. American Diabetes Association. 7. Diabetes Technology: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(suppl 1):S85-S99. doi:10.2337/dc21-S007
2. Austin MM. The two skill sets of self-monitoring of blood glucose education: the operational and the interpretive. Diabetes Spectr. 2013;26(2):83-90. doi:10.2337/diaspect.26.2.83
3. Gallichan M. Self monitoring of glucose by people with diabetes: evidence based practice. BMJ. 1997;314(7085):964-967. doi:10.1136/bmj.314.7085.964
4. Lewinski AA, Drake C, Shaw RJ, et al. Bridging the integration gap between patient-generated blood glucose data and electronic health records. J Am Med Inform Assoc. 2019;26(7):667-672. doi:10.1093/jamia/ocz039
5. McFarland MS, Groppi J, Jorgenson T, et al. Role of the US Veterans Health Administration clinical pharmacy specialist provider: shaping the future of comprehensive medication management. Can J Hosp Pharm. 2020;73(2):152-158. doi:10.4212/cjhp.v73i2.2982
6. Schmidt K, Caudill J. Hamilton T. Impact of clinical pharmacy specialists on glycemic control in veterans with type 2 diabetes. Am J Health Syst Pharm. 2019;76(suppl 1):S9-S14. doi:10.1093/ajhp/zxy015
7. Sullivan J, Jett BP, Cradick M, Zuber J. Effect of clinical pharmacist intervention on hemoglobin A1c reduction in veteran patients with type 2 diabetes in a rural setting. Ann Pharmacother. 2016;50(12):1023-1027. doi:10.1177/1060028016663564
8. Bloom CI, Ku M, Williams M. Clinical pharmacy specialists’ impact in patient aligned care teams for type 2 diabetes management. J Am Pharm Assoc (2003). 2019;59(5):717-721. doi:10.1016/j.japh.2019.05.002
9. Kumar RB, Goren ND, Stark DE, Wall DP, Longhurst CA. Automated integration of continuous glucose monitor data in the electronic health record using consumer technology. J Am Med Inform Assoc. 2016;23(3):532-537. doi:10.1093/jamia/ocv206
10. Reading MJ, Merrill JA. Converging and diverging needs between patients and providers who are collecting and using patient-generated health data: an integrative review. J Am Med Inform Assoc. 2018;25(6):759-771. doi:10.1093/jamia/ocy006
1. American Diabetes Association. 7. Diabetes Technology: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(suppl 1):S85-S99. doi:10.2337/dc21-S007
2. Austin MM. The two skill sets of self-monitoring of blood glucose education: the operational and the interpretive. Diabetes Spectr. 2013;26(2):83-90. doi:10.2337/diaspect.26.2.83
3. Gallichan M. Self monitoring of glucose by people with diabetes: evidence based practice. BMJ. 1997;314(7085):964-967. doi:10.1136/bmj.314.7085.964
4. Lewinski AA, Drake C, Shaw RJ, et al. Bridging the integration gap between patient-generated blood glucose data and electronic health records. J Am Med Inform Assoc. 2019;26(7):667-672. doi:10.1093/jamia/ocz039
5. McFarland MS, Groppi J, Jorgenson T, et al. Role of the US Veterans Health Administration clinical pharmacy specialist provider: shaping the future of comprehensive medication management. Can J Hosp Pharm. 2020;73(2):152-158. doi:10.4212/cjhp.v73i2.2982
6. Schmidt K, Caudill J. Hamilton T. Impact of clinical pharmacy specialists on glycemic control in veterans with type 2 diabetes. Am J Health Syst Pharm. 2019;76(suppl 1):S9-S14. doi:10.1093/ajhp/zxy015
7. Sullivan J, Jett BP, Cradick M, Zuber J. Effect of clinical pharmacist intervention on hemoglobin A1c reduction in veteran patients with type 2 diabetes in a rural setting. Ann Pharmacother. 2016;50(12):1023-1027. doi:10.1177/1060028016663564
8. Bloom CI, Ku M, Williams M. Clinical pharmacy specialists’ impact in patient aligned care teams for type 2 diabetes management. J Am Pharm Assoc (2003). 2019;59(5):717-721. doi:10.1016/j.japh.2019.05.002
9. Kumar RB, Goren ND, Stark DE, Wall DP, Longhurst CA. Automated integration of continuous glucose monitor data in the electronic health record using consumer technology. J Am Med Inform Assoc. 2016;23(3):532-537. doi:10.1093/jamia/ocv206
10. Reading MJ, Merrill JA. Converging and diverging needs between patients and providers who are collecting and using patient-generated health data: an integrative review. J Am Med Inform Assoc. 2018;25(6):759-771. doi:10.1093/jamia/ocy006
Creating a Sustainable and Reliable Emergency Preparedness Program to Promote Appropriate Health Care Resources Use
Over the past decade, natural disasters and health care emergencies have increased 74%, averaging 400 documented events per year.1 These unpredictable and sometimes devastating events negatively impact the physical and mental health of communities, taxing already stretched health care system resources and the economy.2,3 During many of these events, patients inappropriately use hospitals, emergency departments (EDs), and critical care resources for chronic disease and elective health care management, resulting in medication shortages, health care access concerns, and treatment delays.4
Most available emergency preparedness programs rely solely on volunteers and/or public health providers to address the resultant coverage gap; however, instability in state and federal funding can make it difficult to maintain and sustain focused preparedness and response efforts. Alaska’s vast geography, low population density (1.2 people per square mile), and access limitations (about 200 villages only reachable by air or boat) make it especially challenging to provide reliable and sustained emergency preparedness and response support. Therefore, all eligible health care providers (HCPs) in Alaska must be involved in preparedness and response efforts.
Despite being the most accessible HCPs, pharmacists and student pharmacists, have not been actively involved in statewide emergency preparedness planning and disaster management efforts in Alaska. In preparation for and during disasters, for example, pharmacists may administer vaccinations, conduct point of care testing, dispense emergency medications, provide emergency medication refills, help mitigate medication shortages, and provide reliable health information to other health care professionals, patients, and their families as they prepare for and manage care during the event.4
The goal of this paper is to share the experience at the University of Alaska Anchorage/Idaho State University College of Pharmacy (UAA/ISU) in the development and implementation of a sustainable emergency preparedness and response support network (EPRSN) model; leveraging an established university student leadership structure and Doctor of Pharmacy (PharmD) students to support sharing of information among community pharmacies, state emergency response teams, and community members.
2018 Alaska Earthquake
On November 30, 2018, southcentral Alaska experienced a magnitude 7.1 earthquake, affecting nearly 295,000 people (approximately 40% of Alaska’s population) damaging roads, buildings, homes, and health care facilities. Emergency response efforts were quickly overwhelmed and hospital EDs became overburdened with patients seeking not only emergent, but also chronic care along with requests for prescription refills.
During disasters, disruptions in medication access and adherence are common. Disruptions can lead to disease exacerbation or progression, hospitalization, and/or death; all of which further contribute to the health care system and economic health burden. For example, after Hurricane Katrina, 46% of patients on hypertension medications had less than perfect adherence due to a variety of reasons (eg, not bringing any or enough medications during evacuation, lack of access to refills).5 Nonadherence to prescription hypertension medication specifically can lead to stroke, heart attack, and more rapidly progressing kidney dysfunction. Patients with diabetes mellitus (DM) also experience negative consequences due to disruptions in medication adherence.6 Lack of access to medications and supplies for DM can likewise lead to significant health sequelae, including acute hyperglycemic events, which can be life-threatening; ongoing hyperglycemia can lead to higher rates of cardiovascular disease, kidney disease, nerve damage, and diabetic retinopathy.7 However, the long-term effects of a natural disaster on health in terms of morbidity and mortality often go unreported, and their impact on chronic health conditions may be underestimated and last for years after the event.
As future health care professionals, student pharmacists continually seek opportunities to engage with and support communities; including preparing for, responding to, mitigating against, and recovering from disasters that affect the health care system and access to needed drug therapies. After the earthquake, student pharmacists reached out to state and local emergency response programs detailed within The State of Alaska Emergency Operations Plan to find opportunities to volunteer.
Agencies contacted included the Office of Emergency Management (OEM) for the Municipality of Anchorage. OEM partners with local health, fire, and police departments, the Alaska Department of Health and Social Services and Emergency Management, the Federal Emergency Management Agency, Centers for Disease Control and Prevention, American Red Cross, and the Salvation Army. It is important to note, due to lack of funding, Alaska no longer has a Medical Reserve Corps, which significantly impacts community emergency response and resilience efforts. After the earthquake, the emergency program manager extended an invitation to student pharmacists to join the joint medical emergency conference call, where local HCPs discuss emergency protocols, identify gaps, and work together to identify solutions.
During this call there was a consensus among HCPs that many patients were inappropriately seeking to fill and refill prescription medications in the ED, and staff were ill-prepared to guide patients to the appropriate services, unaware of which pharmacies were impacted by the earthquake; therefore unable to direct patients to still-operational pharmacies in the area. Together faculty and students discussed how student pharmacists could be involved in filling these identified information gaps and enhance communication among HCPs and entities. It was determined that if student pharmacists established and maintained open lines of communication with community pharmacists, they could efficiently determine which pharmacies were open and operational after disasters and disseminate that information to EDs and health care facilities in order to better direct patients to appropriate health care services.
Observations
A question/answer format and time line approach was used to review the steps leading to EPRSN program development and establishment of project/model deliverables.
Identified gaps
Chronic disease management. According to interviews conducted by the National Center for Disaster Preparedness, people often inappropriately use EDs during disasters.8 EDs do not stock enough medications to refill prescriptions for patients outside of their emergent care needs and are typically ill-suited for patients’ chronic disease management. At the time of the earthquake in Alaska no specific place/organization had been established to collect, store, or disseminate information regarding available pharmacy resources in an emergency. Had such a system been in place to actively inform HCPs and community members which pharmacies were open and operational, it is likely that many negative consequences related to health care utilization could have been reduced or avoided, including the number of people inappropriately using EDs for chronic prescription medication refills. This would not only reduce the burden on the health care system but allow for patients with both emergency and chronic needs to be seen quickly and prevent unnecessary health care costs.
Pharmacists play a vital role in managing chronic diseases.9 Due to extensive education and training, they are considered medication experts, ideally suited to manage chronic medication therapy, help prevent or minimize disease exacerbation and/or progression, reduce preventable health care costs, improve patient quality of life, and reduce morbidity and mortality.9 Pharmacists are accessible and strategically located throughout communities and provide patients with continuity of care other HCPs may be unable to provide. For example, during the COVID-19 pandemic, pharmacies remained open when other primary care providers (PCPs) were not. In addition, during times of natural disasters pharmacies tend to remain open unless there are extenuating circumstances (eg, unsafe building infrastructure, unsafe drug supply).
Emergency Response. To determine the role pharmacists play in emergency preparedness efforts we looked initially to the peer-reviewed literature (search terms: emergency preparedness, natural disasters, pharmacy/pharmacies) then turned to materials and research produced by organizations outside of the traditional commercial and academic publishing channels; however, most emergency preparedness protocols and standard operating procedures (SOPs) did not pertain to pharmacies or acknowledge the contribution of pharmacists. Researchers urge both state and federal governments to foster relationships with and use community pharmacist’s expertise and expanded roles in order to improve the nation’s public health.10
Historically, pharmacists within the US Public Health Service (PHS) have responded alongside local HCPs to meet the needs of communities during public health emergencies. Pharmacists were pivotal in the 2009 response to H1N1 influenza and the 2015 Ebola response, both abroad and within the United States.6 Pharmacists screened and triaged patients, provided life-saving vaccinations, and supported community and health care system education initiatives. However, as the COVID-19 pandemic has demonstrated, responding to a public health crisis takes more than the 1,000 pharmacists serving in the PHS.11 The American Society of Health-System Pharmacists argues that all pharmacists should be involved in working with public health planners.12
Community and health-systems pharmacists are vital to current and future public health responses and represent a largely untapped resource. Pharmacists across the country, especially in rural and underserved communities, have the potential to significantly impact emergency preparedness and response efforts. The > 319,000 US pharmacists comprise a sizable portion of the population and can play vital roles during emergency situations or disasters.13 Often after catastrophic events, community pharmacists provide first-aid, emergency refills, medication counseling, point of care testing, triage patients and serve on emergency response teams.14 However, pharmacists alone cannot address all medication-related patient needs and student pharmacists likewise have a role in emergency preparedness and response efforts. By participating in these efforts and learning these roles as students, they are better prepared to engage in emergency efforts as pharmacists.
Student pharmacist support. There are more than 140 accredited pharmacy schools across the United States, employing > 6,500 pharmacy faculty, and teaching > 63,000 student pharmacists.15 The majority of schools provide free and volunteer-based health care services and collaborate with local, regional, and national entities such as state boards of pharmacy, professional pharmacy organizations, and the American Pharmacist Association (APhA). Through the APhA Academy of Student Pharmacists (ASP), in 2018 and 2019 Operation Heart Campaign, 4,239 patients were referred to a PCP for follow-up care, 117,251 patients received health and wellness services, and 2,772,179 patients were educated regarding cardiovascular disease, the most common noncommunicable disease in the United States.16,17 Also, in 2018 and 2019, APhA-ASPs Operation Diabetes Campaign referred 3,785 patients to their PCP, provided health and wellness services to 36,334 patients, and educated 1,114,281 patients regarding DM.18
Student pharmacists are positioned across the country with reach to rural and underserved communities and have student organizational structures in place to manage student volunteers and support health care service opportunities. These structures could readily be used to augment and provide emergency pharmacy services and the coordination of chronic care services during times of emergency or disaster. Student leaders are well situated to coordinate communication and cooperation across health care disciplines and to facilitate local community pharmacy resource information collection and distribution.
Emergency Preparation Program
To address gaps in emergency preparedness and response, student pharmacists at UAA/ISU took the following steps to develop the EPRSN. Planning involved a multistep process. Step 1 identified important uncaptured data (eg, operational status, staffing, hours of operation, continuity and safety of drug supply chain, building/parking lot damage) required to direct patients to the appropriate medication-related care during an emergency. For step 2, student pharmacists obtained a list of the 138 pharmacies in Alaska from the state board of pharmacy. Pharmacies were contacted by student pharmacists using an established telephone script and updated contact information collected was stored on a secure, online drive accessible to UAA/ISU College of Pharmacy faculty and students using their UAA/ISU email address. In step 3, the APhA-ASP president elect and 3 leaders in each of the 16 APhA-ASP operation in charge of the EPRSN Alaska initiative, surveyed student leaders to determine student willingness to participate. Step 4 was to develop an organizational structure using established leadership structure to collect, capture, update, and share pharmacy data with state emergency response teams. Sustainability from year to year will be ensured through incorporation into the APhA-ASP student engagement framework (eg, annual training led by the president elect, contact information updated biyearly by student leaders, and oversight provided by College of Pharmacy faculty). Step 5 was to create SOPs, flowcharts, telephone scripts, talking points, and student training materials. And in the final preparatory step, plan documents and deliverables were provided to faculty administration and advisors within the College of Pharmacy for initial approval and presented to the student leadership for final approval.
EPRSN will be activated in the case of a natural disaster or state of emergency. Pharmacy students will contact all pharmacies within the designated area to collect up-to-date vital information (eg, operational status, staffing, hours of operation, safe drug supply, building/parking lot damage). Collected information will be disseminated to appropriate community members, HCPs, health care facilities, and emergency preparedness officials, under the direction of the Emergency Program Manager.
Discussion
In order to make informed and timely decisions during emergency situations, patients, HCPs, and health care systems must have appropriate situational awareness. The ability of decision makers to respond is directly dependent on timeliness and relevance of the information collected and shared and greatly contributes to this awareness. Accurate, effective, and consistent information collection has historically been one of the greatest challenges to situational awareness. This is particularly important in times of disaster when necessary emergency situation data may not exist, tools to collect data are inefficient and/or ineffective, and/or current data are inaccessible to relevant parties.19 This was the case in the Alaska earthquake of 2018 and more recently the COVID-19 pandemic of 2020 where information sharing deficits and structural barriers became even more evident.
Transfer of knowledge and information is especially critical during an emergency situation. Ineffective communication and information sharing results in transfer gaps. Gaps that result from inadequate transfers of care between HCPs are referred to as hand-off gaps. Training gaps result from inadequate preparation on the part of HCPs and civic leaders as well as in public health policies and procedures and in understanding of needs in emergent situations. Organization gaps occur when an individual changes positions or leaves a given institution and the acquired knowledge is not shared with others before departure or the replacement individual does not receive necessary training.
In both the Alaska earthquake and the COVID-19 pandemic, gaps in hand-offs, training, and organization were identified. Pharmacists were involved in the solution, providing care, addressing unmet health needs, and supporting the health care system. Many patients and HCPs remain unaware of the services pharmacists are capable and willing to provide, but at even a more basic level they are unsure of what services may be needed in emergency situations. Pharmacists are often used and considered vital HCPs after natural disasters or emergency situations, providing services that extend beyond their normal duties, yet remain within their SOP and expertise and address the medication management needs of their patients, ensuring safe, effective, and continuous access to needed pharmaceuticals.
It is vital that pharmacists and student pharmacists take an active role in emergency preparedness, that students get involved early in outreach and engagement initiatives for which they are ideally suited to coordinate in their communities, and that College of Pharmacy faculty support student pharmacist efforts to continue to highlight the professional roles of pharmacists, in routine health care as well as during times of crisis or disaster. It is important to note that an indirect but important cause of patient mortality related to an emergency event is the inability to access routine health care. If pharmacists and student pharmacists were more involved in emergency preparedness and response efforts, they could play an even greater role in providing much needed health care to patients during times when the health care system is overtaxed (facilitating medication refills and providing administrative and health care support).
Conclusions
Emergency and disaster preparedness are vital to promote the appropriate use of health care resources and prevent health-related complications. Student pharmacists represent a sustainable resource, uniquely positioned to identify community needs, support emergency efforts, coordinate with local pharmacies, and work with pharmacists and others to ensure patients receive the care they need. This work has the potential to improve utilization of health care resources and service delivery during natural disasters and emergencies, on a local, state, and regional level, with the overall goal of maintaining patient health and well-being.
1. Ritchie H, Roser M. Natural disasters. Updated November 2019. Accessed March 12, 2021. https://ourworldindata.org/natural-disasters
2. Freedy JR, Simpson WM Jr. Disaster-related physical and mental health: a role for the family physician. Am Fam Physician. 2007;75(6):841-846.
3. Martin U. Health after disaster: a perspective of psychological/health reactions to disaster. Cogent Psychol. 2015;2(1):1053741. doi:10.1080/23311908.2015.1053741
4. Joy K. Ripple effect: how hurricanes and other disasters affect hospital care. Published September 11, 2017. Accessed March 12, 2021. https://labblog.uofmhealth.org/industry-dx/ripple-effect-how-hurricanes-and-other-disasters-affect-hospital-care
5. Krousel-Wood MA, Islam T, Muntner P, et al. Medication adherence in older clinic patients with hypertension after Hurricane Katrina: implications for clinical practice and disaster management. Am J Med Sci. 2008;336(2):99-104. doi:10.1097/MAJ.0b013e318180f14f
6. Cefalu WT, Smith SR, Blonde L, Fonseca V. The Hurricane Katrina aftermath and its impact on diabetes care: observations from “ground zero”: lessons in disaster preparedness of people with diabetes. Diabetes Care. 2006;29(1):158-160. doi:10.2337/diacare.29.1.158
7. Fonseca VA, Smith H, Kuhadiya N, et al. Impact of a natural disaster on diabetes: exacerbation of disparities and long-term consequences. Diabetes Care. 2009;32(9):1632-1638. doi:10.2337/dc09-0670
8. Suneja A, Chandler TE, Schlegelmilch J, May M, Redlener IE; Columbia University Earth Institute. Chronic disease after natural disasters: public health, policy, and provider perspectives. Published November 12, 2018. Accessed March 12, 2021. doi:10.7916/D8ZP5Q23
9. Kehrer JP, Eberhart G, Wing M, Horon K. Pharmacy’s role in a modern health continuum. Can Pharm J (Ott). 2013;146(6):321-324. doi:10.1177/1715163513506370
10. Shearer MP, Geleta A, Adalja A, Gronvall GK; Johns Hopkins Bloomberg School of Public Health Center for Health Security. Serving the greater good: public health & community pharmacy partnerships. Published October 2017. Accessed March 12, 2021. https://www.centerforhealthsecurity.org/our-work/pubs_archive/pubs-pdfs/2017/public-health-and-community-pharmacy-partnerships-report.pdf
11. Flowers L, Wick J, Figg WD Sr, et al. U.S. Public Health Service Commissioned Corps pharmacists: making a difference in advancing the nation’s health. J Am Pharm Assoc (2003). 2009;49(3):446-452. doi:10.1331/JAPhA.2009.08036
12. American Society of Health-System Pharmacists. ASHP Statement on the Role of Health-System Pharmacists in Public Health. Am J Health Syst Pharm. 2008;65(5):462-467. doi:10.2146/ajhp070399
13. Deloitte. Data USA: pharmacists. Accessed June 2, 2020. https://datausa.io/profile/soc/pharmacists
14. Menighan TE. Pharmacists have major role in emergency response. Pharmacy Today. 2016;22(8):8. doi:10.1016/j.ptdy.2016.07.009
15. American Association of Colleges of Pharmacy. Academic pharmacy’s vital statistics. Updated July 2020. Accessed March 12, 2021. https://www.aacp.org/article/academic-pharmacys-vital-statistics
16. American Pharmacists Association. APhA-ASP Operation Heart. Accessed March 12, 2021. https://www.pharmacist.com/apha-asp-operation-heart
17. World Health Organization. Noncommunicable diseases. Updated June 1, 2018. Accessed March 12, 2021. https://www.who.int/en/news-room/fact-sheets/detail/noncommunicable-diseases
18. American Pharmacists Association. APhA-ASP Operation Diabetes. Accessed March 12, 2021. https://www.pharmacist.com/apha-asp-operation-diabetes
19. Reeve M, Wizemann T, Altevogt B. Enabling Rapid and Sustainable Public Health Research During Disasters: Summary of a Joint Workshop by the Institute of Medicine and the U.S. Department of Health and Human Services. National Academies Press; 2015.
Over the past decade, natural disasters and health care emergencies have increased 74%, averaging 400 documented events per year.1 These unpredictable and sometimes devastating events negatively impact the physical and mental health of communities, taxing already stretched health care system resources and the economy.2,3 During many of these events, patients inappropriately use hospitals, emergency departments (EDs), and critical care resources for chronic disease and elective health care management, resulting in medication shortages, health care access concerns, and treatment delays.4
Most available emergency preparedness programs rely solely on volunteers and/or public health providers to address the resultant coverage gap; however, instability in state and federal funding can make it difficult to maintain and sustain focused preparedness and response efforts. Alaska’s vast geography, low population density (1.2 people per square mile), and access limitations (about 200 villages only reachable by air or boat) make it especially challenging to provide reliable and sustained emergency preparedness and response support. Therefore, all eligible health care providers (HCPs) in Alaska must be involved in preparedness and response efforts.
Despite being the most accessible HCPs, pharmacists and student pharmacists, have not been actively involved in statewide emergency preparedness planning and disaster management efforts in Alaska. In preparation for and during disasters, for example, pharmacists may administer vaccinations, conduct point of care testing, dispense emergency medications, provide emergency medication refills, help mitigate medication shortages, and provide reliable health information to other health care professionals, patients, and their families as they prepare for and manage care during the event.4
The goal of this paper is to share the experience at the University of Alaska Anchorage/Idaho State University College of Pharmacy (UAA/ISU) in the development and implementation of a sustainable emergency preparedness and response support network (EPRSN) model; leveraging an established university student leadership structure and Doctor of Pharmacy (PharmD) students to support sharing of information among community pharmacies, state emergency response teams, and community members.
2018 Alaska Earthquake
On November 30, 2018, southcentral Alaska experienced a magnitude 7.1 earthquake, affecting nearly 295,000 people (approximately 40% of Alaska’s population) damaging roads, buildings, homes, and health care facilities. Emergency response efforts were quickly overwhelmed and hospital EDs became overburdened with patients seeking not only emergent, but also chronic care along with requests for prescription refills.
During disasters, disruptions in medication access and adherence are common. Disruptions can lead to disease exacerbation or progression, hospitalization, and/or death; all of which further contribute to the health care system and economic health burden. For example, after Hurricane Katrina, 46% of patients on hypertension medications had less than perfect adherence due to a variety of reasons (eg, not bringing any or enough medications during evacuation, lack of access to refills).5 Nonadherence to prescription hypertension medication specifically can lead to stroke, heart attack, and more rapidly progressing kidney dysfunction. Patients with diabetes mellitus (DM) also experience negative consequences due to disruptions in medication adherence.6 Lack of access to medications and supplies for DM can likewise lead to significant health sequelae, including acute hyperglycemic events, which can be life-threatening; ongoing hyperglycemia can lead to higher rates of cardiovascular disease, kidney disease, nerve damage, and diabetic retinopathy.7 However, the long-term effects of a natural disaster on health in terms of morbidity and mortality often go unreported, and their impact on chronic health conditions may be underestimated and last for years after the event.
As future health care professionals, student pharmacists continually seek opportunities to engage with and support communities; including preparing for, responding to, mitigating against, and recovering from disasters that affect the health care system and access to needed drug therapies. After the earthquake, student pharmacists reached out to state and local emergency response programs detailed within The State of Alaska Emergency Operations Plan to find opportunities to volunteer.
Agencies contacted included the Office of Emergency Management (OEM) for the Municipality of Anchorage. OEM partners with local health, fire, and police departments, the Alaska Department of Health and Social Services and Emergency Management, the Federal Emergency Management Agency, Centers for Disease Control and Prevention, American Red Cross, and the Salvation Army. It is important to note, due to lack of funding, Alaska no longer has a Medical Reserve Corps, which significantly impacts community emergency response and resilience efforts. After the earthquake, the emergency program manager extended an invitation to student pharmacists to join the joint medical emergency conference call, where local HCPs discuss emergency protocols, identify gaps, and work together to identify solutions.
During this call there was a consensus among HCPs that many patients were inappropriately seeking to fill and refill prescription medications in the ED, and staff were ill-prepared to guide patients to the appropriate services, unaware of which pharmacies were impacted by the earthquake; therefore unable to direct patients to still-operational pharmacies in the area. Together faculty and students discussed how student pharmacists could be involved in filling these identified information gaps and enhance communication among HCPs and entities. It was determined that if student pharmacists established and maintained open lines of communication with community pharmacists, they could efficiently determine which pharmacies were open and operational after disasters and disseminate that information to EDs and health care facilities in order to better direct patients to appropriate health care services.
Observations
A question/answer format and time line approach was used to review the steps leading to EPRSN program development and establishment of project/model deliverables.
Identified gaps
Chronic disease management. According to interviews conducted by the National Center for Disaster Preparedness, people often inappropriately use EDs during disasters.8 EDs do not stock enough medications to refill prescriptions for patients outside of their emergent care needs and are typically ill-suited for patients’ chronic disease management. At the time of the earthquake in Alaska no specific place/organization had been established to collect, store, or disseminate information regarding available pharmacy resources in an emergency. Had such a system been in place to actively inform HCPs and community members which pharmacies were open and operational, it is likely that many negative consequences related to health care utilization could have been reduced or avoided, including the number of people inappropriately using EDs for chronic prescription medication refills. This would not only reduce the burden on the health care system but allow for patients with both emergency and chronic needs to be seen quickly and prevent unnecessary health care costs.
Pharmacists play a vital role in managing chronic diseases.9 Due to extensive education and training, they are considered medication experts, ideally suited to manage chronic medication therapy, help prevent or minimize disease exacerbation and/or progression, reduce preventable health care costs, improve patient quality of life, and reduce morbidity and mortality.9 Pharmacists are accessible and strategically located throughout communities and provide patients with continuity of care other HCPs may be unable to provide. For example, during the COVID-19 pandemic, pharmacies remained open when other primary care providers (PCPs) were not. In addition, during times of natural disasters pharmacies tend to remain open unless there are extenuating circumstances (eg, unsafe building infrastructure, unsafe drug supply).
Emergency Response. To determine the role pharmacists play in emergency preparedness efforts we looked initially to the peer-reviewed literature (search terms: emergency preparedness, natural disasters, pharmacy/pharmacies) then turned to materials and research produced by organizations outside of the traditional commercial and academic publishing channels; however, most emergency preparedness protocols and standard operating procedures (SOPs) did not pertain to pharmacies or acknowledge the contribution of pharmacists. Researchers urge both state and federal governments to foster relationships with and use community pharmacist’s expertise and expanded roles in order to improve the nation’s public health.10
Historically, pharmacists within the US Public Health Service (PHS) have responded alongside local HCPs to meet the needs of communities during public health emergencies. Pharmacists were pivotal in the 2009 response to H1N1 influenza and the 2015 Ebola response, both abroad and within the United States.6 Pharmacists screened and triaged patients, provided life-saving vaccinations, and supported community and health care system education initiatives. However, as the COVID-19 pandemic has demonstrated, responding to a public health crisis takes more than the 1,000 pharmacists serving in the PHS.11 The American Society of Health-System Pharmacists argues that all pharmacists should be involved in working with public health planners.12
Community and health-systems pharmacists are vital to current and future public health responses and represent a largely untapped resource. Pharmacists across the country, especially in rural and underserved communities, have the potential to significantly impact emergency preparedness and response efforts. The > 319,000 US pharmacists comprise a sizable portion of the population and can play vital roles during emergency situations or disasters.13 Often after catastrophic events, community pharmacists provide first-aid, emergency refills, medication counseling, point of care testing, triage patients and serve on emergency response teams.14 However, pharmacists alone cannot address all medication-related patient needs and student pharmacists likewise have a role in emergency preparedness and response efforts. By participating in these efforts and learning these roles as students, they are better prepared to engage in emergency efforts as pharmacists.
Student pharmacist support. There are more than 140 accredited pharmacy schools across the United States, employing > 6,500 pharmacy faculty, and teaching > 63,000 student pharmacists.15 The majority of schools provide free and volunteer-based health care services and collaborate with local, regional, and national entities such as state boards of pharmacy, professional pharmacy organizations, and the American Pharmacist Association (APhA). Through the APhA Academy of Student Pharmacists (ASP), in 2018 and 2019 Operation Heart Campaign, 4,239 patients were referred to a PCP for follow-up care, 117,251 patients received health and wellness services, and 2,772,179 patients were educated regarding cardiovascular disease, the most common noncommunicable disease in the United States.16,17 Also, in 2018 and 2019, APhA-ASPs Operation Diabetes Campaign referred 3,785 patients to their PCP, provided health and wellness services to 36,334 patients, and educated 1,114,281 patients regarding DM.18
Student pharmacists are positioned across the country with reach to rural and underserved communities and have student organizational structures in place to manage student volunteers and support health care service opportunities. These structures could readily be used to augment and provide emergency pharmacy services and the coordination of chronic care services during times of emergency or disaster. Student leaders are well situated to coordinate communication and cooperation across health care disciplines and to facilitate local community pharmacy resource information collection and distribution.
Emergency Preparation Program
To address gaps in emergency preparedness and response, student pharmacists at UAA/ISU took the following steps to develop the EPRSN. Planning involved a multistep process. Step 1 identified important uncaptured data (eg, operational status, staffing, hours of operation, continuity and safety of drug supply chain, building/parking lot damage) required to direct patients to the appropriate medication-related care during an emergency. For step 2, student pharmacists obtained a list of the 138 pharmacies in Alaska from the state board of pharmacy. Pharmacies were contacted by student pharmacists using an established telephone script and updated contact information collected was stored on a secure, online drive accessible to UAA/ISU College of Pharmacy faculty and students using their UAA/ISU email address. In step 3, the APhA-ASP president elect and 3 leaders in each of the 16 APhA-ASP operation in charge of the EPRSN Alaska initiative, surveyed student leaders to determine student willingness to participate. Step 4 was to develop an organizational structure using established leadership structure to collect, capture, update, and share pharmacy data with state emergency response teams. Sustainability from year to year will be ensured through incorporation into the APhA-ASP student engagement framework (eg, annual training led by the president elect, contact information updated biyearly by student leaders, and oversight provided by College of Pharmacy faculty). Step 5 was to create SOPs, flowcharts, telephone scripts, talking points, and student training materials. And in the final preparatory step, plan documents and deliverables were provided to faculty administration and advisors within the College of Pharmacy for initial approval and presented to the student leadership for final approval.
EPRSN will be activated in the case of a natural disaster or state of emergency. Pharmacy students will contact all pharmacies within the designated area to collect up-to-date vital information (eg, operational status, staffing, hours of operation, safe drug supply, building/parking lot damage). Collected information will be disseminated to appropriate community members, HCPs, health care facilities, and emergency preparedness officials, under the direction of the Emergency Program Manager.
Discussion
In order to make informed and timely decisions during emergency situations, patients, HCPs, and health care systems must have appropriate situational awareness. The ability of decision makers to respond is directly dependent on timeliness and relevance of the information collected and shared and greatly contributes to this awareness. Accurate, effective, and consistent information collection has historically been one of the greatest challenges to situational awareness. This is particularly important in times of disaster when necessary emergency situation data may not exist, tools to collect data are inefficient and/or ineffective, and/or current data are inaccessible to relevant parties.19 This was the case in the Alaska earthquake of 2018 and more recently the COVID-19 pandemic of 2020 where information sharing deficits and structural barriers became even more evident.
Transfer of knowledge and information is especially critical during an emergency situation. Ineffective communication and information sharing results in transfer gaps. Gaps that result from inadequate transfers of care between HCPs are referred to as hand-off gaps. Training gaps result from inadequate preparation on the part of HCPs and civic leaders as well as in public health policies and procedures and in understanding of needs in emergent situations. Organization gaps occur when an individual changes positions or leaves a given institution and the acquired knowledge is not shared with others before departure or the replacement individual does not receive necessary training.
In both the Alaska earthquake and the COVID-19 pandemic, gaps in hand-offs, training, and organization were identified. Pharmacists were involved in the solution, providing care, addressing unmet health needs, and supporting the health care system. Many patients and HCPs remain unaware of the services pharmacists are capable and willing to provide, but at even a more basic level they are unsure of what services may be needed in emergency situations. Pharmacists are often used and considered vital HCPs after natural disasters or emergency situations, providing services that extend beyond their normal duties, yet remain within their SOP and expertise and address the medication management needs of their patients, ensuring safe, effective, and continuous access to needed pharmaceuticals.
It is vital that pharmacists and student pharmacists take an active role in emergency preparedness, that students get involved early in outreach and engagement initiatives for which they are ideally suited to coordinate in their communities, and that College of Pharmacy faculty support student pharmacist efforts to continue to highlight the professional roles of pharmacists, in routine health care as well as during times of crisis or disaster. It is important to note that an indirect but important cause of patient mortality related to an emergency event is the inability to access routine health care. If pharmacists and student pharmacists were more involved in emergency preparedness and response efforts, they could play an even greater role in providing much needed health care to patients during times when the health care system is overtaxed (facilitating medication refills and providing administrative and health care support).
Conclusions
Emergency and disaster preparedness are vital to promote the appropriate use of health care resources and prevent health-related complications. Student pharmacists represent a sustainable resource, uniquely positioned to identify community needs, support emergency efforts, coordinate with local pharmacies, and work with pharmacists and others to ensure patients receive the care they need. This work has the potential to improve utilization of health care resources and service delivery during natural disasters and emergencies, on a local, state, and regional level, with the overall goal of maintaining patient health and well-being.
Over the past decade, natural disasters and health care emergencies have increased 74%, averaging 400 documented events per year.1 These unpredictable and sometimes devastating events negatively impact the physical and mental health of communities, taxing already stretched health care system resources and the economy.2,3 During many of these events, patients inappropriately use hospitals, emergency departments (EDs), and critical care resources for chronic disease and elective health care management, resulting in medication shortages, health care access concerns, and treatment delays.4
Most available emergency preparedness programs rely solely on volunteers and/or public health providers to address the resultant coverage gap; however, instability in state and federal funding can make it difficult to maintain and sustain focused preparedness and response efforts. Alaska’s vast geography, low population density (1.2 people per square mile), and access limitations (about 200 villages only reachable by air or boat) make it especially challenging to provide reliable and sustained emergency preparedness and response support. Therefore, all eligible health care providers (HCPs) in Alaska must be involved in preparedness and response efforts.
Despite being the most accessible HCPs, pharmacists and student pharmacists, have not been actively involved in statewide emergency preparedness planning and disaster management efforts in Alaska. In preparation for and during disasters, for example, pharmacists may administer vaccinations, conduct point of care testing, dispense emergency medications, provide emergency medication refills, help mitigate medication shortages, and provide reliable health information to other health care professionals, patients, and their families as they prepare for and manage care during the event.4
The goal of this paper is to share the experience at the University of Alaska Anchorage/Idaho State University College of Pharmacy (UAA/ISU) in the development and implementation of a sustainable emergency preparedness and response support network (EPRSN) model; leveraging an established university student leadership structure and Doctor of Pharmacy (PharmD) students to support sharing of information among community pharmacies, state emergency response teams, and community members.
2018 Alaska Earthquake
On November 30, 2018, southcentral Alaska experienced a magnitude 7.1 earthquake, affecting nearly 295,000 people (approximately 40% of Alaska’s population) damaging roads, buildings, homes, and health care facilities. Emergency response efforts were quickly overwhelmed and hospital EDs became overburdened with patients seeking not only emergent, but also chronic care along with requests for prescription refills.
During disasters, disruptions in medication access and adherence are common. Disruptions can lead to disease exacerbation or progression, hospitalization, and/or death; all of which further contribute to the health care system and economic health burden. For example, after Hurricane Katrina, 46% of patients on hypertension medications had less than perfect adherence due to a variety of reasons (eg, not bringing any or enough medications during evacuation, lack of access to refills).5 Nonadherence to prescription hypertension medication specifically can lead to stroke, heart attack, and more rapidly progressing kidney dysfunction. Patients with diabetes mellitus (DM) also experience negative consequences due to disruptions in medication adherence.6 Lack of access to medications and supplies for DM can likewise lead to significant health sequelae, including acute hyperglycemic events, which can be life-threatening; ongoing hyperglycemia can lead to higher rates of cardiovascular disease, kidney disease, nerve damage, and diabetic retinopathy.7 However, the long-term effects of a natural disaster on health in terms of morbidity and mortality often go unreported, and their impact on chronic health conditions may be underestimated and last for years after the event.
As future health care professionals, student pharmacists continually seek opportunities to engage with and support communities; including preparing for, responding to, mitigating against, and recovering from disasters that affect the health care system and access to needed drug therapies. After the earthquake, student pharmacists reached out to state and local emergency response programs detailed within The State of Alaska Emergency Operations Plan to find opportunities to volunteer.
Agencies contacted included the Office of Emergency Management (OEM) for the Municipality of Anchorage. OEM partners with local health, fire, and police departments, the Alaska Department of Health and Social Services and Emergency Management, the Federal Emergency Management Agency, Centers for Disease Control and Prevention, American Red Cross, and the Salvation Army. It is important to note, due to lack of funding, Alaska no longer has a Medical Reserve Corps, which significantly impacts community emergency response and resilience efforts. After the earthquake, the emergency program manager extended an invitation to student pharmacists to join the joint medical emergency conference call, where local HCPs discuss emergency protocols, identify gaps, and work together to identify solutions.
During this call there was a consensus among HCPs that many patients were inappropriately seeking to fill and refill prescription medications in the ED, and staff were ill-prepared to guide patients to the appropriate services, unaware of which pharmacies were impacted by the earthquake; therefore unable to direct patients to still-operational pharmacies in the area. Together faculty and students discussed how student pharmacists could be involved in filling these identified information gaps and enhance communication among HCPs and entities. It was determined that if student pharmacists established and maintained open lines of communication with community pharmacists, they could efficiently determine which pharmacies were open and operational after disasters and disseminate that information to EDs and health care facilities in order to better direct patients to appropriate health care services.
Observations
A question/answer format and time line approach was used to review the steps leading to EPRSN program development and establishment of project/model deliverables.
Identified gaps
Chronic disease management. According to interviews conducted by the National Center for Disaster Preparedness, people often inappropriately use EDs during disasters.8 EDs do not stock enough medications to refill prescriptions for patients outside of their emergent care needs and are typically ill-suited for patients’ chronic disease management. At the time of the earthquake in Alaska no specific place/organization had been established to collect, store, or disseminate information regarding available pharmacy resources in an emergency. Had such a system been in place to actively inform HCPs and community members which pharmacies were open and operational, it is likely that many negative consequences related to health care utilization could have been reduced or avoided, including the number of people inappropriately using EDs for chronic prescription medication refills. This would not only reduce the burden on the health care system but allow for patients with both emergency and chronic needs to be seen quickly and prevent unnecessary health care costs.
Pharmacists play a vital role in managing chronic diseases.9 Due to extensive education and training, they are considered medication experts, ideally suited to manage chronic medication therapy, help prevent or minimize disease exacerbation and/or progression, reduce preventable health care costs, improve patient quality of life, and reduce morbidity and mortality.9 Pharmacists are accessible and strategically located throughout communities and provide patients with continuity of care other HCPs may be unable to provide. For example, during the COVID-19 pandemic, pharmacies remained open when other primary care providers (PCPs) were not. In addition, during times of natural disasters pharmacies tend to remain open unless there are extenuating circumstances (eg, unsafe building infrastructure, unsafe drug supply).
Emergency Response. To determine the role pharmacists play in emergency preparedness efforts we looked initially to the peer-reviewed literature (search terms: emergency preparedness, natural disasters, pharmacy/pharmacies) then turned to materials and research produced by organizations outside of the traditional commercial and academic publishing channels; however, most emergency preparedness protocols and standard operating procedures (SOPs) did not pertain to pharmacies or acknowledge the contribution of pharmacists. Researchers urge both state and federal governments to foster relationships with and use community pharmacist’s expertise and expanded roles in order to improve the nation’s public health.10
Historically, pharmacists within the US Public Health Service (PHS) have responded alongside local HCPs to meet the needs of communities during public health emergencies. Pharmacists were pivotal in the 2009 response to H1N1 influenza and the 2015 Ebola response, both abroad and within the United States.6 Pharmacists screened and triaged patients, provided life-saving vaccinations, and supported community and health care system education initiatives. However, as the COVID-19 pandemic has demonstrated, responding to a public health crisis takes more than the 1,000 pharmacists serving in the PHS.11 The American Society of Health-System Pharmacists argues that all pharmacists should be involved in working with public health planners.12
Community and health-systems pharmacists are vital to current and future public health responses and represent a largely untapped resource. Pharmacists across the country, especially in rural and underserved communities, have the potential to significantly impact emergency preparedness and response efforts. The > 319,000 US pharmacists comprise a sizable portion of the population and can play vital roles during emergency situations or disasters.13 Often after catastrophic events, community pharmacists provide first-aid, emergency refills, medication counseling, point of care testing, triage patients and serve on emergency response teams.14 However, pharmacists alone cannot address all medication-related patient needs and student pharmacists likewise have a role in emergency preparedness and response efforts. By participating in these efforts and learning these roles as students, they are better prepared to engage in emergency efforts as pharmacists.
Student pharmacist support. There are more than 140 accredited pharmacy schools across the United States, employing > 6,500 pharmacy faculty, and teaching > 63,000 student pharmacists.15 The majority of schools provide free and volunteer-based health care services and collaborate with local, regional, and national entities such as state boards of pharmacy, professional pharmacy organizations, and the American Pharmacist Association (APhA). Through the APhA Academy of Student Pharmacists (ASP), in 2018 and 2019 Operation Heart Campaign, 4,239 patients were referred to a PCP for follow-up care, 117,251 patients received health and wellness services, and 2,772,179 patients were educated regarding cardiovascular disease, the most common noncommunicable disease in the United States.16,17 Also, in 2018 and 2019, APhA-ASPs Operation Diabetes Campaign referred 3,785 patients to their PCP, provided health and wellness services to 36,334 patients, and educated 1,114,281 patients regarding DM.18
Student pharmacists are positioned across the country with reach to rural and underserved communities and have student organizational structures in place to manage student volunteers and support health care service opportunities. These structures could readily be used to augment and provide emergency pharmacy services and the coordination of chronic care services during times of emergency or disaster. Student leaders are well situated to coordinate communication and cooperation across health care disciplines and to facilitate local community pharmacy resource information collection and distribution.
Emergency Preparation Program
To address gaps in emergency preparedness and response, student pharmacists at UAA/ISU took the following steps to develop the EPRSN. Planning involved a multistep process. Step 1 identified important uncaptured data (eg, operational status, staffing, hours of operation, continuity and safety of drug supply chain, building/parking lot damage) required to direct patients to the appropriate medication-related care during an emergency. For step 2, student pharmacists obtained a list of the 138 pharmacies in Alaska from the state board of pharmacy. Pharmacies were contacted by student pharmacists using an established telephone script and updated contact information collected was stored on a secure, online drive accessible to UAA/ISU College of Pharmacy faculty and students using their UAA/ISU email address. In step 3, the APhA-ASP president elect and 3 leaders in each of the 16 APhA-ASP operation in charge of the EPRSN Alaska initiative, surveyed student leaders to determine student willingness to participate. Step 4 was to develop an organizational structure using established leadership structure to collect, capture, update, and share pharmacy data with state emergency response teams. Sustainability from year to year will be ensured through incorporation into the APhA-ASP student engagement framework (eg, annual training led by the president elect, contact information updated biyearly by student leaders, and oversight provided by College of Pharmacy faculty). Step 5 was to create SOPs, flowcharts, telephone scripts, talking points, and student training materials. And in the final preparatory step, plan documents and deliverables were provided to faculty administration and advisors within the College of Pharmacy for initial approval and presented to the student leadership for final approval.
EPRSN will be activated in the case of a natural disaster or state of emergency. Pharmacy students will contact all pharmacies within the designated area to collect up-to-date vital information (eg, operational status, staffing, hours of operation, safe drug supply, building/parking lot damage). Collected information will be disseminated to appropriate community members, HCPs, health care facilities, and emergency preparedness officials, under the direction of the Emergency Program Manager.
Discussion
In order to make informed and timely decisions during emergency situations, patients, HCPs, and health care systems must have appropriate situational awareness. The ability of decision makers to respond is directly dependent on timeliness and relevance of the information collected and shared and greatly contributes to this awareness. Accurate, effective, and consistent information collection has historically been one of the greatest challenges to situational awareness. This is particularly important in times of disaster when necessary emergency situation data may not exist, tools to collect data are inefficient and/or ineffective, and/or current data are inaccessible to relevant parties.19 This was the case in the Alaska earthquake of 2018 and more recently the COVID-19 pandemic of 2020 where information sharing deficits and structural barriers became even more evident.
Transfer of knowledge and information is especially critical during an emergency situation. Ineffective communication and information sharing results in transfer gaps. Gaps that result from inadequate transfers of care between HCPs are referred to as hand-off gaps. Training gaps result from inadequate preparation on the part of HCPs and civic leaders as well as in public health policies and procedures and in understanding of needs in emergent situations. Organization gaps occur when an individual changes positions or leaves a given institution and the acquired knowledge is not shared with others before departure or the replacement individual does not receive necessary training.
In both the Alaska earthquake and the COVID-19 pandemic, gaps in hand-offs, training, and organization were identified. Pharmacists were involved in the solution, providing care, addressing unmet health needs, and supporting the health care system. Many patients and HCPs remain unaware of the services pharmacists are capable and willing to provide, but at even a more basic level they are unsure of what services may be needed in emergency situations. Pharmacists are often used and considered vital HCPs after natural disasters or emergency situations, providing services that extend beyond their normal duties, yet remain within their SOP and expertise and address the medication management needs of their patients, ensuring safe, effective, and continuous access to needed pharmaceuticals.
It is vital that pharmacists and student pharmacists take an active role in emergency preparedness, that students get involved early in outreach and engagement initiatives for which they are ideally suited to coordinate in their communities, and that College of Pharmacy faculty support student pharmacist efforts to continue to highlight the professional roles of pharmacists, in routine health care as well as during times of crisis or disaster. It is important to note that an indirect but important cause of patient mortality related to an emergency event is the inability to access routine health care. If pharmacists and student pharmacists were more involved in emergency preparedness and response efforts, they could play an even greater role in providing much needed health care to patients during times when the health care system is overtaxed (facilitating medication refills and providing administrative and health care support).
Conclusions
Emergency and disaster preparedness are vital to promote the appropriate use of health care resources and prevent health-related complications. Student pharmacists represent a sustainable resource, uniquely positioned to identify community needs, support emergency efforts, coordinate with local pharmacies, and work with pharmacists and others to ensure patients receive the care they need. This work has the potential to improve utilization of health care resources and service delivery during natural disasters and emergencies, on a local, state, and regional level, with the overall goal of maintaining patient health and well-being.
1. Ritchie H, Roser M. Natural disasters. Updated November 2019. Accessed March 12, 2021. https://ourworldindata.org/natural-disasters
2. Freedy JR, Simpson WM Jr. Disaster-related physical and mental health: a role for the family physician. Am Fam Physician. 2007;75(6):841-846.
3. Martin U. Health after disaster: a perspective of psychological/health reactions to disaster. Cogent Psychol. 2015;2(1):1053741. doi:10.1080/23311908.2015.1053741
4. Joy K. Ripple effect: how hurricanes and other disasters affect hospital care. Published September 11, 2017. Accessed March 12, 2021. https://labblog.uofmhealth.org/industry-dx/ripple-effect-how-hurricanes-and-other-disasters-affect-hospital-care
5. Krousel-Wood MA, Islam T, Muntner P, et al. Medication adherence in older clinic patients with hypertension after Hurricane Katrina: implications for clinical practice and disaster management. Am J Med Sci. 2008;336(2):99-104. doi:10.1097/MAJ.0b013e318180f14f
6. Cefalu WT, Smith SR, Blonde L, Fonseca V. The Hurricane Katrina aftermath and its impact on diabetes care: observations from “ground zero”: lessons in disaster preparedness of people with diabetes. Diabetes Care. 2006;29(1):158-160. doi:10.2337/diacare.29.1.158
7. Fonseca VA, Smith H, Kuhadiya N, et al. Impact of a natural disaster on diabetes: exacerbation of disparities and long-term consequences. Diabetes Care. 2009;32(9):1632-1638. doi:10.2337/dc09-0670
8. Suneja A, Chandler TE, Schlegelmilch J, May M, Redlener IE; Columbia University Earth Institute. Chronic disease after natural disasters: public health, policy, and provider perspectives. Published November 12, 2018. Accessed March 12, 2021. doi:10.7916/D8ZP5Q23
9. Kehrer JP, Eberhart G, Wing M, Horon K. Pharmacy’s role in a modern health continuum. Can Pharm J (Ott). 2013;146(6):321-324. doi:10.1177/1715163513506370
10. Shearer MP, Geleta A, Adalja A, Gronvall GK; Johns Hopkins Bloomberg School of Public Health Center for Health Security. Serving the greater good: public health & community pharmacy partnerships. Published October 2017. Accessed March 12, 2021. https://www.centerforhealthsecurity.org/our-work/pubs_archive/pubs-pdfs/2017/public-health-and-community-pharmacy-partnerships-report.pdf
11. Flowers L, Wick J, Figg WD Sr, et al. U.S. Public Health Service Commissioned Corps pharmacists: making a difference in advancing the nation’s health. J Am Pharm Assoc (2003). 2009;49(3):446-452. doi:10.1331/JAPhA.2009.08036
12. American Society of Health-System Pharmacists. ASHP Statement on the Role of Health-System Pharmacists in Public Health. Am J Health Syst Pharm. 2008;65(5):462-467. doi:10.2146/ajhp070399
13. Deloitte. Data USA: pharmacists. Accessed June 2, 2020. https://datausa.io/profile/soc/pharmacists
14. Menighan TE. Pharmacists have major role in emergency response. Pharmacy Today. 2016;22(8):8. doi:10.1016/j.ptdy.2016.07.009
15. American Association of Colleges of Pharmacy. Academic pharmacy’s vital statistics. Updated July 2020. Accessed March 12, 2021. https://www.aacp.org/article/academic-pharmacys-vital-statistics
16. American Pharmacists Association. APhA-ASP Operation Heart. Accessed March 12, 2021. https://www.pharmacist.com/apha-asp-operation-heart
17. World Health Organization. Noncommunicable diseases. Updated June 1, 2018. Accessed March 12, 2021. https://www.who.int/en/news-room/fact-sheets/detail/noncommunicable-diseases
18. American Pharmacists Association. APhA-ASP Operation Diabetes. Accessed March 12, 2021. https://www.pharmacist.com/apha-asp-operation-diabetes
19. Reeve M, Wizemann T, Altevogt B. Enabling Rapid and Sustainable Public Health Research During Disasters: Summary of a Joint Workshop by the Institute of Medicine and the U.S. Department of Health and Human Services. National Academies Press; 2015.
1. Ritchie H, Roser M. Natural disasters. Updated November 2019. Accessed March 12, 2021. https://ourworldindata.org/natural-disasters
2. Freedy JR, Simpson WM Jr. Disaster-related physical and mental health: a role for the family physician. Am Fam Physician. 2007;75(6):841-846.
3. Martin U. Health after disaster: a perspective of psychological/health reactions to disaster. Cogent Psychol. 2015;2(1):1053741. doi:10.1080/23311908.2015.1053741
4. Joy K. Ripple effect: how hurricanes and other disasters affect hospital care. Published September 11, 2017. Accessed March 12, 2021. https://labblog.uofmhealth.org/industry-dx/ripple-effect-how-hurricanes-and-other-disasters-affect-hospital-care
5. Krousel-Wood MA, Islam T, Muntner P, et al. Medication adherence in older clinic patients with hypertension after Hurricane Katrina: implications for clinical practice and disaster management. Am J Med Sci. 2008;336(2):99-104. doi:10.1097/MAJ.0b013e318180f14f
6. Cefalu WT, Smith SR, Blonde L, Fonseca V. The Hurricane Katrina aftermath and its impact on diabetes care: observations from “ground zero”: lessons in disaster preparedness of people with diabetes. Diabetes Care. 2006;29(1):158-160. doi:10.2337/diacare.29.1.158
7. Fonseca VA, Smith H, Kuhadiya N, et al. Impact of a natural disaster on diabetes: exacerbation of disparities and long-term consequences. Diabetes Care. 2009;32(9):1632-1638. doi:10.2337/dc09-0670
8. Suneja A, Chandler TE, Schlegelmilch J, May M, Redlener IE; Columbia University Earth Institute. Chronic disease after natural disasters: public health, policy, and provider perspectives. Published November 12, 2018. Accessed March 12, 2021. doi:10.7916/D8ZP5Q23
9. Kehrer JP, Eberhart G, Wing M, Horon K. Pharmacy’s role in a modern health continuum. Can Pharm J (Ott). 2013;146(6):321-324. doi:10.1177/1715163513506370
10. Shearer MP, Geleta A, Adalja A, Gronvall GK; Johns Hopkins Bloomberg School of Public Health Center for Health Security. Serving the greater good: public health & community pharmacy partnerships. Published October 2017. Accessed March 12, 2021. https://www.centerforhealthsecurity.org/our-work/pubs_archive/pubs-pdfs/2017/public-health-and-community-pharmacy-partnerships-report.pdf
11. Flowers L, Wick J, Figg WD Sr, et al. U.S. Public Health Service Commissioned Corps pharmacists: making a difference in advancing the nation’s health. J Am Pharm Assoc (2003). 2009;49(3):446-452. doi:10.1331/JAPhA.2009.08036
12. American Society of Health-System Pharmacists. ASHP Statement on the Role of Health-System Pharmacists in Public Health. Am J Health Syst Pharm. 2008;65(5):462-467. doi:10.2146/ajhp070399
13. Deloitte. Data USA: pharmacists. Accessed June 2, 2020. https://datausa.io/profile/soc/pharmacists
14. Menighan TE. Pharmacists have major role in emergency response. Pharmacy Today. 2016;22(8):8. doi:10.1016/j.ptdy.2016.07.009
15. American Association of Colleges of Pharmacy. Academic pharmacy’s vital statistics. Updated July 2020. Accessed March 12, 2021. https://www.aacp.org/article/academic-pharmacys-vital-statistics
16. American Pharmacists Association. APhA-ASP Operation Heart. Accessed March 12, 2021. https://www.pharmacist.com/apha-asp-operation-heart
17. World Health Organization. Noncommunicable diseases. Updated June 1, 2018. Accessed March 12, 2021. https://www.who.int/en/news-room/fact-sheets/detail/noncommunicable-diseases
18. American Pharmacists Association. APhA-ASP Operation Diabetes. Accessed March 12, 2021. https://www.pharmacist.com/apha-asp-operation-diabetes
19. Reeve M, Wizemann T, Altevogt B. Enabling Rapid and Sustainable Public Health Research During Disasters: Summary of a Joint Workshop by the Institute of Medicine and the U.S. Department of Health and Human Services. National Academies Press; 2015.