User login
Bleomycin can be safely omitted after negative PET2 in HL

Photo by Jens Maus
LUGANO—Results of the RATHL trial indicate that bleomycin can be omitted from ABVD therapy following a negative interim FDG-PET scan in patients with Hodgkin lymphoma.
Progression-free survival (PFS) and overall survival (OS) were the same at 3 years for patients who were PET-negative after 2 cycles of ABVD and then continued therapy with or without bleomycin.
These results were presented at the 13th International Conference on Malignant Lymphoma (13-ICML).
Investigators based the RATHL study on the principles that it’s desirable to de-escalate treatment in the best responders to avoid late toxicity and that PET scans after 2 cycles of ABVD are highly predictive.
The team enrolled 1214 patients from 6 countries, 861 of whom were in the UK. Patients received a PET scan at staging, 2 cycles of ABVD, and then a second PET scan (PET2).
If patients were negative after PET2, they were randomized to receive 4 more cycles of ABVD or AVD and no radiotherapy.
If they were positive after PET2, patients received 4 cycles of BEACOPP-14 or 3 cycles of escalated BEACOPP. These patients then received a third PET scan, and the positive patients went on to receive radiotherapy or a salvage regimen.
The PET3-negative patients received 2 more cycles of BEACOPP-14 or one of escalated BEACOPP without radiotherapy.
Peter W. Johnson, MD, of the University of Southampton in the UK, presented the results of these treatment regimens during the plenary session of 13-ICML as abstract 008.
Patient characteristics
Patients were a median age of 33 (range, 18-79), and 55% were male. They had disease stages of II (41%), III (31%), or IV (28%).
Seventy-four percent of patients had a performance status of 0. Almost half (49%) had an IPS score of 2 to 3, and 18% had an IPS score of 4 or more. Thirty-two percent had bulky disease.
Investigators followed the patients for a median of 34.7 months (range, 1 day to 68.2 months).
Results after PET2
Seventy-seven patients were missing a second PET scan, mostly due to PET protocol violations of having to use the same scanner for the baseline and second scan and the same acquisition time.
“We were very strict on our quality control,” Dr Johnson said, “because we wished to make sure this was reproducible data.”
So the results after 2 cycles of ABVD treatment were based on 1137 patients.
PET-negative patients
More than 80% of patients were PET-negative after 2 cycles. Four hundred and sixty-nine patients were randomized to receive ABVD and 466 to AVD.
The groups were well-balanced in terms of median age, performance status, stage, B symptoms, bulky disease, and IPS score.
There was a significant excess of neutropenic fever (P=0.032) and infection (P=0.040) in those patients continuing on ABVD compared to AVD. And any hematologic toxicity was highly significantly different between the 2 arms (P<0.001).
“So we have demonstrated that continuing with bleomycin beyond cycle 2 is accompanied by significantly more toxicity,” Dr Johnson said.
Ninety-eight percent of patients in both cohorts received at least 6 cycles of therapy post-randomization.
At a median follow-up of 36.3 months, 65% of patients in the ABVD arm and 69% in the AVD arm achieved a complete remission (CR) or unconfirmed CR (CRu).
Fourteen patients died in each of the arms. Seven patients died of their disease in the AVD arm, compared with 1 in the ABVD arm. Slightly more patients died from toxicity in the ABVD arm.
The primary endpoint of PFS showed very little difference between the 2 arms. The 3-year PFS in the intent-to-treat analysis was 85.4% for patients in the ABVD arm and 84.4% for those in the AVD arm.
The investigators observed that the PFS of 85% was somewhat lower than the 95% PFS observed in the literature. So they looked at the association between baseline factors and PFS after negative PET2.
“And what stands out from this is that if you have high-stage disease at presentation, there is a slightly higher chance of treatment failure following a negative PET scan,” Dr Johnson said. “And you can see the trend here, from early stage disease up to advanced-stage disease, the PET scan becomes a less reliable indicator of result.”
The investigators also conducted a subgroup analysis of the PET2-negative patients and found there was no difference in outcome between treatment arms in patients with more advanced disease, with bulky disease, with a high IPS score, or according to the PET score.
“So we have not succeeded in finding any subgroup where it appears to be beneficial to continue bleomycin,” Dr Johnson said.
The OS rate was also the same between the 2 arms, at 97%.
PET2-positive patients
One hundred and seventy-four patients who were positive after the second PET scan received either BEACOPP for 14 days or escalated BEACOPP.
The percentage of patients who experienced grade 3-4 toxicities was largely similar between the 2 regimens, although the patients receiving escalated BEACOPP had more neutropenia (P=0.057), thrombocytopenia (P=0.001), and neutropenic fever (P=0.08).
In terms of efficacy, two-thirds of patients became PET-negative by the third PET scan, and 48% of patients achieved a CR or CRu.
Twenty-one patients died, 8 due to Hodgkin lymphoma.
The PFS was 66.0% in the BEACOPP-14 group and 71.1% in the escalated-BEACOPP group. The 3-year OS was 89.6% in the BEACOPP-14 group and 82.8% in the escalated-BEACOPP group.
For the entire group of 1214 patients, the 3-year PFS was 82.5%, and the OS was 95.4%.
Based on these results, the investigators concluded that it is safe to omit bleomycin and consolidation radiotherapy from subsequent ABVD therapy after a negative interim PET scan. And doing so reduces toxicity, especially dyspnea, thromboembolism, and neutropenic fever.
“[B]y using more selective chemotherapy and much less radiotherapy than we have previously used in our studies, where we’re giving less than 3% of patients consolidation radiotherapy, the results appear to be favorable and an improvement over what we have seen previously,” Dr Johnson said.
Details on lung toxicity in this study were presented separately at 13-ICML as abstract 041. ![]()

Photo by Jens Maus
LUGANO—Results of the RATHL trial indicate that bleomycin can be omitted from ABVD therapy following a negative interim FDG-PET scan in patients with Hodgkin lymphoma.
Progression-free survival (PFS) and overall survival (OS) were the same at 3 years for patients who were PET-negative after 2 cycles of ABVD and then continued therapy with or without bleomycin.
These results were presented at the 13th International Conference on Malignant Lymphoma (13-ICML).
Investigators based the RATHL study on the principles that it’s desirable to de-escalate treatment in the best responders to avoid late toxicity and that PET scans after 2 cycles of ABVD are highly predictive.
The team enrolled 1214 patients from 6 countries, 861 of whom were in the UK. Patients received a PET scan at staging, 2 cycles of ABVD, and then a second PET scan (PET2).
If patients were negative after PET2, they were randomized to receive 4 more cycles of ABVD or AVD and no radiotherapy.
If they were positive after PET2, patients received 4 cycles of BEACOPP-14 or 3 cycles of escalated BEACOPP. These patients then received a third PET scan, and the positive patients went on to receive radiotherapy or a salvage regimen.
The PET3-negative patients received 2 more cycles of BEACOPP-14 or one of escalated BEACOPP without radiotherapy.
Peter W. Johnson, MD, of the University of Southampton in the UK, presented the results of these treatment regimens during the plenary session of 13-ICML as abstract 008.
Patient characteristics
Patients were a median age of 33 (range, 18-79), and 55% were male. They had disease stages of II (41%), III (31%), or IV (28%).
Seventy-four percent of patients had a performance status of 0. Almost half (49%) had an IPS score of 2 to 3, and 18% had an IPS score of 4 or more. Thirty-two percent had bulky disease.
Investigators followed the patients for a median of 34.7 months (range, 1 day to 68.2 months).
Results after PET2
Seventy-seven patients were missing a second PET scan, mostly due to PET protocol violations of having to use the same scanner for the baseline and second scan and the same acquisition time.
“We were very strict on our quality control,” Dr Johnson said, “because we wished to make sure this was reproducible data.”
So the results after 2 cycles of ABVD treatment were based on 1137 patients.
PET-negative patients
More than 80% of patients were PET-negative after 2 cycles. Four hundred and sixty-nine patients were randomized to receive ABVD and 466 to AVD.
The groups were well-balanced in terms of median age, performance status, stage, B symptoms, bulky disease, and IPS score.
There was a significant excess of neutropenic fever (P=0.032) and infection (P=0.040) in those patients continuing on ABVD compared to AVD. And any hematologic toxicity was highly significantly different between the 2 arms (P<0.001).
“So we have demonstrated that continuing with bleomycin beyond cycle 2 is accompanied by significantly more toxicity,” Dr Johnson said.
Ninety-eight percent of patients in both cohorts received at least 6 cycles of therapy post-randomization.
At a median follow-up of 36.3 months, 65% of patients in the ABVD arm and 69% in the AVD arm achieved a complete remission (CR) or unconfirmed CR (CRu).
Fourteen patients died in each of the arms. Seven patients died of their disease in the AVD arm, compared with 1 in the ABVD arm. Slightly more patients died from toxicity in the ABVD arm.
The primary endpoint of PFS showed very little difference between the 2 arms. The 3-year PFS in the intent-to-treat analysis was 85.4% for patients in the ABVD arm and 84.4% for those in the AVD arm.
The investigators observed that the PFS of 85% was somewhat lower than the 95% PFS observed in the literature. So they looked at the association between baseline factors and PFS after negative PET2.
“And what stands out from this is that if you have high-stage disease at presentation, there is a slightly higher chance of treatment failure following a negative PET scan,” Dr Johnson said. “And you can see the trend here, from early stage disease up to advanced-stage disease, the PET scan becomes a less reliable indicator of result.”
The investigators also conducted a subgroup analysis of the PET2-negative patients and found there was no difference in outcome between treatment arms in patients with more advanced disease, with bulky disease, with a high IPS score, or according to the PET score.
“So we have not succeeded in finding any subgroup where it appears to be beneficial to continue bleomycin,” Dr Johnson said.
The OS rate was also the same between the 2 arms, at 97%.
PET2-positive patients
One hundred and seventy-four patients who were positive after the second PET scan received either BEACOPP for 14 days or escalated BEACOPP.
The percentage of patients who experienced grade 3-4 toxicities was largely similar between the 2 regimens, although the patients receiving escalated BEACOPP had more neutropenia (P=0.057), thrombocytopenia (P=0.001), and neutropenic fever (P=0.08).
In terms of efficacy, two-thirds of patients became PET-negative by the third PET scan, and 48% of patients achieved a CR or CRu.
Twenty-one patients died, 8 due to Hodgkin lymphoma.
The PFS was 66.0% in the BEACOPP-14 group and 71.1% in the escalated-BEACOPP group. The 3-year OS was 89.6% in the BEACOPP-14 group and 82.8% in the escalated-BEACOPP group.
For the entire group of 1214 patients, the 3-year PFS was 82.5%, and the OS was 95.4%.
Based on these results, the investigators concluded that it is safe to omit bleomycin and consolidation radiotherapy from subsequent ABVD therapy after a negative interim PET scan. And doing so reduces toxicity, especially dyspnea, thromboembolism, and neutropenic fever.
“[B]y using more selective chemotherapy and much less radiotherapy than we have previously used in our studies, where we’re giving less than 3% of patients consolidation radiotherapy, the results appear to be favorable and an improvement over what we have seen previously,” Dr Johnson said.
Details on lung toxicity in this study were presented separately at 13-ICML as abstract 041. ![]()

Photo by Jens Maus
LUGANO—Results of the RATHL trial indicate that bleomycin can be omitted from ABVD therapy following a negative interim FDG-PET scan in patients with Hodgkin lymphoma.
Progression-free survival (PFS) and overall survival (OS) were the same at 3 years for patients who were PET-negative after 2 cycles of ABVD and then continued therapy with or without bleomycin.
These results were presented at the 13th International Conference on Malignant Lymphoma (13-ICML).
Investigators based the RATHL study on the principles that it’s desirable to de-escalate treatment in the best responders to avoid late toxicity and that PET scans after 2 cycles of ABVD are highly predictive.
The team enrolled 1214 patients from 6 countries, 861 of whom were in the UK. Patients received a PET scan at staging, 2 cycles of ABVD, and then a second PET scan (PET2).
If patients were negative after PET2, they were randomized to receive 4 more cycles of ABVD or AVD and no radiotherapy.
If they were positive after PET2, patients received 4 cycles of BEACOPP-14 or 3 cycles of escalated BEACOPP. These patients then received a third PET scan, and the positive patients went on to receive radiotherapy or a salvage regimen.
The PET3-negative patients received 2 more cycles of BEACOPP-14 or one of escalated BEACOPP without radiotherapy.
Peter W. Johnson, MD, of the University of Southampton in the UK, presented the results of these treatment regimens during the plenary session of 13-ICML as abstract 008.
Patient characteristics
Patients were a median age of 33 (range, 18-79), and 55% were male. They had disease stages of II (41%), III (31%), or IV (28%).
Seventy-four percent of patients had a performance status of 0. Almost half (49%) had an IPS score of 2 to 3, and 18% had an IPS score of 4 or more. Thirty-two percent had bulky disease.
Investigators followed the patients for a median of 34.7 months (range, 1 day to 68.2 months).
Results after PET2
Seventy-seven patients were missing a second PET scan, mostly due to PET protocol violations of having to use the same scanner for the baseline and second scan and the same acquisition time.
“We were very strict on our quality control,” Dr Johnson said, “because we wished to make sure this was reproducible data.”
So the results after 2 cycles of ABVD treatment were based on 1137 patients.
PET-negative patients
More than 80% of patients were PET-negative after 2 cycles. Four hundred and sixty-nine patients were randomized to receive ABVD and 466 to AVD.
The groups were well-balanced in terms of median age, performance status, stage, B symptoms, bulky disease, and IPS score.
There was a significant excess of neutropenic fever (P=0.032) and infection (P=0.040) in those patients continuing on ABVD compared to AVD. And any hematologic toxicity was highly significantly different between the 2 arms (P<0.001).
“So we have demonstrated that continuing with bleomycin beyond cycle 2 is accompanied by significantly more toxicity,” Dr Johnson said.
Ninety-eight percent of patients in both cohorts received at least 6 cycles of therapy post-randomization.
At a median follow-up of 36.3 months, 65% of patients in the ABVD arm and 69% in the AVD arm achieved a complete remission (CR) or unconfirmed CR (CRu).
Fourteen patients died in each of the arms. Seven patients died of their disease in the AVD arm, compared with 1 in the ABVD arm. Slightly more patients died from toxicity in the ABVD arm.
The primary endpoint of PFS showed very little difference between the 2 arms. The 3-year PFS in the intent-to-treat analysis was 85.4% for patients in the ABVD arm and 84.4% for those in the AVD arm.
The investigators observed that the PFS of 85% was somewhat lower than the 95% PFS observed in the literature. So they looked at the association between baseline factors and PFS after negative PET2.
“And what stands out from this is that if you have high-stage disease at presentation, there is a slightly higher chance of treatment failure following a negative PET scan,” Dr Johnson said. “And you can see the trend here, from early stage disease up to advanced-stage disease, the PET scan becomes a less reliable indicator of result.”
The investigators also conducted a subgroup analysis of the PET2-negative patients and found there was no difference in outcome between treatment arms in patients with more advanced disease, with bulky disease, with a high IPS score, or according to the PET score.
“So we have not succeeded in finding any subgroup where it appears to be beneficial to continue bleomycin,” Dr Johnson said.
The OS rate was also the same between the 2 arms, at 97%.
PET2-positive patients
One hundred and seventy-four patients who were positive after the second PET scan received either BEACOPP for 14 days or escalated BEACOPP.
The percentage of patients who experienced grade 3-4 toxicities was largely similar between the 2 regimens, although the patients receiving escalated BEACOPP had more neutropenia (P=0.057), thrombocytopenia (P=0.001), and neutropenic fever (P=0.08).
In terms of efficacy, two-thirds of patients became PET-negative by the third PET scan, and 48% of patients achieved a CR or CRu.
Twenty-one patients died, 8 due to Hodgkin lymphoma.
The PFS was 66.0% in the BEACOPP-14 group and 71.1% in the escalated-BEACOPP group. The 3-year OS was 89.6% in the BEACOPP-14 group and 82.8% in the escalated-BEACOPP group.
For the entire group of 1214 patients, the 3-year PFS was 82.5%, and the OS was 95.4%.
Based on these results, the investigators concluded that it is safe to omit bleomycin and consolidation radiotherapy from subsequent ABVD therapy after a negative interim PET scan. And doing so reduces toxicity, especially dyspnea, thromboembolism, and neutropenic fever.
“[B]y using more selective chemotherapy and much less radiotherapy than we have previously used in our studies, where we’re giving less than 3% of patients consolidation radiotherapy, the results appear to be favorable and an improvement over what we have seen previously,” Dr Johnson said.
Details on lung toxicity in this study were presented separately at 13-ICML as abstract 041. ![]()
Activin receptors continue to show efficacy in ß-thalassemia

Congress of the European
Hematology Association
VIENNA—Two very similar activin receptors, luspatercept and sotatercept, continue to show efficacy in patients with ß-thalassemia, according to research presented at the 20th Congress of the European Hematology Association (EHA).
The “twin compounds” basically differ from each other in the receptor type, but both can increase hemoglobin levels in non-transfusion-dependent (NTD) patients and reduce transfusion burden in transfusion-dependent (TD) patients.
Luspatercept is a recombinant fusion protein containing a modified extracellular domain of the activin receptor type IIB, while sotatercept is an activin receptor type IIA.
Antonio Piga, MD, of Turin University in Italy, presented the most recent results with luspatercept at EHA as abstract S136*. An update on sotatercept was also presented at the meeting.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds.
The phase 2, multicenter, open-label trial of luspatercept now has results on 39 patients, 35 of whom were in the dose-escalation cohorts and 4 who are in the expansion cohort that is currently underway.
Adult patients age 18 and older received luspatercept subcutaneously every 3 weeks for 3 months. Doses in the dose-escalation cohorts increased from 0.2 mg/kg to 1.25 mg/kg.
Patients in the expansion cohort received a starting dose of 0.8 mg/kg, with an individual dose titration up to 1.25 mg/kg, for an additional 12 months of treatment. Twenty of 30 patients were enrolled in the expansion cohort as of June 8.
For all patients, the median age was 40, 82% had had a splenectomy, and 49% were male. Twenty-five patients were NTD, and 14 were TD.
NTD patients
NTD patients had a median baseline hemoglobin level of 8.4 g/dL and liver iron concentration (LIC) of 5.8 ± 3.8 mg/g dry weight (dw).
Four of 8 patients who received luspatercept at doses ranging from 0.8 mg/kg to 1.25 mg/kg saw an increase in their hemoglobin levels of 1.5 g/dL or more for 2 weeks or longer, and 3 patients (38%) had a mean hemoglobin increase of 1.5 g/dL for 9 weeks or longer.
Patients on the higher doses of luspatercept had larger hemoglobin increases, and, with continued treatment, patients sustained their hemoglobin increases.
Increases in hemoglobin correlated with reductions in LIC.
“There was a trend to lower liver iron concentration,” Dr Piga said, “a trend that seems important.”
Patients achieved reductions in LIC with and without iron chelation therapy.
Eight of 12 patients with a baseline LIC of 5 mg/g dw or greater had decreases of 1 mg or more at month 4. And 10 of 10 patients with a baseline LIC of less than 5 mg/g dw were able to maintain that concentration.
TD patients
At baseline, TD patients required a median of 7.5 red blood cell (RBC) units every 12 weeks and had an LIC of 5.2 ± 5.7 mg/g dw.
Ten of 14 patients were treated for 12 weeks or longer and were evaluable for changes in transfusion burden. And all 10 patients had a 40% or greater reduction in transfusion burden.
Two of 3 patients with an LIC of 7 mg/g dw had decreases of 1 mg/g dw or more at month 4. And all 7 patients with a baseline LIC less than 7 mg/g dw were able to maintain that level.
Leg ulcers
Three patients with long-term, persistent leg ulcers experienced rapid healing with luspatercept treatment.
One NTD patient on the 0.4 mg/kg dose experienced complete healing after 6 weeks, and 1 TD patient on the 1.0 mg/kg dose experienced complete healing after 18 weeks.
Safety
Bone pain (23%), myalgia (18%), headache (15%), and asthenia (10%) were the most common drug-related adverse events. None of the related adverse events were serious.
Two patients had treatment-related, grade 3 adverse events of bone pain (2 events) and asthenia (1 event). Six of 39 patients discontinued treatment early due to an adverse event of headache, ankle pain, back pain, spider nevi, superficial thrombosis, or bone pain.
The US Food and Drug Administration recently granted luspatercept fast track designation for the treatment of patients with TD or NTD β-thalassemia.
Dr Piga said a pivotal phase 3 trial of luspatercept in patients with β -thalassemia and myelodysplastic syndromes is planned. ![]()
*Data in the abstract differ from the presentation.

Congress of the European
Hematology Association
VIENNA—Two very similar activin receptors, luspatercept and sotatercept, continue to show efficacy in patients with ß-thalassemia, according to research presented at the 20th Congress of the European Hematology Association (EHA).
The “twin compounds” basically differ from each other in the receptor type, but both can increase hemoglobin levels in non-transfusion-dependent (NTD) patients and reduce transfusion burden in transfusion-dependent (TD) patients.
Luspatercept is a recombinant fusion protein containing a modified extracellular domain of the activin receptor type IIB, while sotatercept is an activin receptor type IIA.
Antonio Piga, MD, of Turin University in Italy, presented the most recent results with luspatercept at EHA as abstract S136*. An update on sotatercept was also presented at the meeting.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds.
The phase 2, multicenter, open-label trial of luspatercept now has results on 39 patients, 35 of whom were in the dose-escalation cohorts and 4 who are in the expansion cohort that is currently underway.
Adult patients age 18 and older received luspatercept subcutaneously every 3 weeks for 3 months. Doses in the dose-escalation cohorts increased from 0.2 mg/kg to 1.25 mg/kg.
Patients in the expansion cohort received a starting dose of 0.8 mg/kg, with an individual dose titration up to 1.25 mg/kg, for an additional 12 months of treatment. Twenty of 30 patients were enrolled in the expansion cohort as of June 8.
For all patients, the median age was 40, 82% had had a splenectomy, and 49% were male. Twenty-five patients were NTD, and 14 were TD.
NTD patients
NTD patients had a median baseline hemoglobin level of 8.4 g/dL and liver iron concentration (LIC) of 5.8 ± 3.8 mg/g dry weight (dw).
Four of 8 patients who received luspatercept at doses ranging from 0.8 mg/kg to 1.25 mg/kg saw an increase in their hemoglobin levels of 1.5 g/dL or more for 2 weeks or longer, and 3 patients (38%) had a mean hemoglobin increase of 1.5 g/dL for 9 weeks or longer.
Patients on the higher doses of luspatercept had larger hemoglobin increases, and, with continued treatment, patients sustained their hemoglobin increases.
Increases in hemoglobin correlated with reductions in LIC.
“There was a trend to lower liver iron concentration,” Dr Piga said, “a trend that seems important.”
Patients achieved reductions in LIC with and without iron chelation therapy.
Eight of 12 patients with a baseline LIC of 5 mg/g dw or greater had decreases of 1 mg or more at month 4. And 10 of 10 patients with a baseline LIC of less than 5 mg/g dw were able to maintain that concentration.
TD patients
At baseline, TD patients required a median of 7.5 red blood cell (RBC) units every 12 weeks and had an LIC of 5.2 ± 5.7 mg/g dw.
Ten of 14 patients were treated for 12 weeks or longer and were evaluable for changes in transfusion burden. And all 10 patients had a 40% or greater reduction in transfusion burden.
Two of 3 patients with an LIC of 7 mg/g dw had decreases of 1 mg/g dw or more at month 4. And all 7 patients with a baseline LIC less than 7 mg/g dw were able to maintain that level.
Leg ulcers
Three patients with long-term, persistent leg ulcers experienced rapid healing with luspatercept treatment.
One NTD patient on the 0.4 mg/kg dose experienced complete healing after 6 weeks, and 1 TD patient on the 1.0 mg/kg dose experienced complete healing after 18 weeks.
Safety
Bone pain (23%), myalgia (18%), headache (15%), and asthenia (10%) were the most common drug-related adverse events. None of the related adverse events were serious.
Two patients had treatment-related, grade 3 adverse events of bone pain (2 events) and asthenia (1 event). Six of 39 patients discontinued treatment early due to an adverse event of headache, ankle pain, back pain, spider nevi, superficial thrombosis, or bone pain.
The US Food and Drug Administration recently granted luspatercept fast track designation for the treatment of patients with TD or NTD β-thalassemia.
Dr Piga said a pivotal phase 3 trial of luspatercept in patients with β -thalassemia and myelodysplastic syndromes is planned. ![]()
*Data in the abstract differ from the presentation.

Congress of the European
Hematology Association
VIENNA—Two very similar activin receptors, luspatercept and sotatercept, continue to show efficacy in patients with ß-thalassemia, according to research presented at the 20th Congress of the European Hematology Association (EHA).
The “twin compounds” basically differ from each other in the receptor type, but both can increase hemoglobin levels in non-transfusion-dependent (NTD) patients and reduce transfusion burden in transfusion-dependent (TD) patients.
Luspatercept is a recombinant fusion protein containing a modified extracellular domain of the activin receptor type IIB, while sotatercept is an activin receptor type IIA.
Antonio Piga, MD, of Turin University in Italy, presented the most recent results with luspatercept at EHA as abstract S136*. An update on sotatercept was also presented at the meeting.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds.
The phase 2, multicenter, open-label trial of luspatercept now has results on 39 patients, 35 of whom were in the dose-escalation cohorts and 4 who are in the expansion cohort that is currently underway.
Adult patients age 18 and older received luspatercept subcutaneously every 3 weeks for 3 months. Doses in the dose-escalation cohorts increased from 0.2 mg/kg to 1.25 mg/kg.
Patients in the expansion cohort received a starting dose of 0.8 mg/kg, with an individual dose titration up to 1.25 mg/kg, for an additional 12 months of treatment. Twenty of 30 patients were enrolled in the expansion cohort as of June 8.
For all patients, the median age was 40, 82% had had a splenectomy, and 49% were male. Twenty-five patients were NTD, and 14 were TD.
NTD patients
NTD patients had a median baseline hemoglobin level of 8.4 g/dL and liver iron concentration (LIC) of 5.8 ± 3.8 mg/g dry weight (dw).
Four of 8 patients who received luspatercept at doses ranging from 0.8 mg/kg to 1.25 mg/kg saw an increase in their hemoglobin levels of 1.5 g/dL or more for 2 weeks or longer, and 3 patients (38%) had a mean hemoglobin increase of 1.5 g/dL for 9 weeks or longer.
Patients on the higher doses of luspatercept had larger hemoglobin increases, and, with continued treatment, patients sustained their hemoglobin increases.
Increases in hemoglobin correlated with reductions in LIC.
“There was a trend to lower liver iron concentration,” Dr Piga said, “a trend that seems important.”
Patients achieved reductions in LIC with and without iron chelation therapy.
Eight of 12 patients with a baseline LIC of 5 mg/g dw or greater had decreases of 1 mg or more at month 4. And 10 of 10 patients with a baseline LIC of less than 5 mg/g dw were able to maintain that concentration.
TD patients
At baseline, TD patients required a median of 7.5 red blood cell (RBC) units every 12 weeks and had an LIC of 5.2 ± 5.7 mg/g dw.
Ten of 14 patients were treated for 12 weeks or longer and were evaluable for changes in transfusion burden. And all 10 patients had a 40% or greater reduction in transfusion burden.
Two of 3 patients with an LIC of 7 mg/g dw had decreases of 1 mg/g dw or more at month 4. And all 7 patients with a baseline LIC less than 7 mg/g dw were able to maintain that level.
Leg ulcers
Three patients with long-term, persistent leg ulcers experienced rapid healing with luspatercept treatment.
One NTD patient on the 0.4 mg/kg dose experienced complete healing after 6 weeks, and 1 TD patient on the 1.0 mg/kg dose experienced complete healing after 18 weeks.
Safety
Bone pain (23%), myalgia (18%), headache (15%), and asthenia (10%) were the most common drug-related adverse events. None of the related adverse events were serious.
Two patients had treatment-related, grade 3 adverse events of bone pain (2 events) and asthenia (1 event). Six of 39 patients discontinued treatment early due to an adverse event of headache, ankle pain, back pain, spider nevi, superficial thrombosis, or bone pain.
The US Food and Drug Administration recently granted luspatercept fast track designation for the treatment of patients with TD or NTD β-thalassemia.
Dr Piga said a pivotal phase 3 trial of luspatercept in patients with β -thalassemia and myelodysplastic syndromes is planned. ![]()
*Data in the abstract differ from the presentation.
Drug won’t advance to phase 3 in ß-thalassemia
thalassemia
VIENNA—Data from a phase 2a trial suggest the activin receptor sotatercept can effectively treat patients with ß-thalassemia.
However, the companies developing the drug have decided not to advance sotatercept to phase 3 trials in this patient population.
Instead, the companies are initiating a phase 3 program with sotatercept’s “twin” activin receptor, luspatercept, in patients with ß-thalassemia or myelodysplastic syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds. The companies plan to continue developing sotatercept for patients with chronic kidney disease.
Maria Domenica Cappellini, MD, of the University of Milan in Italy, presented results from the phase 2a study of sotatercept in ß-thalassemia at the 20th Congress of the European Hematology Association (abstract S137*).
Phase 2 results with luspatercept in ß-thalassemia were also presented at the meeting.
The dose-finding study of sotatercept had enrolled 46 patients at the time of Dr Cappellini’s presentation. The drug was given subcutaneously at doses ranging from 0.1 mg/kg to 1.0 mg/kg every 3 weeks.
The 30 non-transfusion-dependent (NTD) patients received 4 or fewer red blood cell (RBC) units in the 6 months prior to study enrollment. The 16 transfusion-dependent (TD) patients had received 2 or more RBC units every 30 days for 6 months or more prior to study enrollment.
Twenty-five of the 46 patients remain on treatment, with a median exposure time of 12.4 months.
NTD patients
The patients’ median age was 42, and 53% were female. Fifty-three percent had had a splenectomy, and the median baseline hemoglobin level was 8.4 g/dL.
Treatment with sotatercept produced a dose-dependent hemoglobin increase.
“[W]hat I found quite interesting is that the increase is consistent and persistent, [even] after 1 year,” Dr Cappellini said. “And they are still maintained on treatment, of course, but it is a sustained response.”
At the 0.75 mg/kg dose, 86% of patients had a hemoglobin increase of 1 g/dL for 12 weeks or more, and 71% had an increase of 1.5 g/dL.
TD patients
The patients’ median age was 36 years, and 38% were female. Three-quarters of patients had ß-thalassemia major, and a quarter had ß-thalassemia intermedia.
Nearly a third of patients had had a splenectomy, and their transfusion burden at baseline ranged from 8 RBC units to 35 RBC units every 24 weeks.
The mean reduction in transfusion burden among patients treated with sotatercept at doses of 0.5 mg/kg or higher was 32.25%. And the 1.0 mg/kg dose of sotatercept reduced one patient’s transfusion burden by 61.6%.
Dr Cappellini noted that the pharmacokinetic analysis showed a correlation with exposure. The investigators observed no apparent effects of weight, sex, age, or transfusion burden on drug clearance.
“So the relationship was probably more related to long-term exposure than to the real dosage,” she said.
Safety
Hypertension and bone pain were the most common grade 2-4, treatment-related adverse events.
Seven patients discontinued the study due to adverse events, one patient each with bone pain, superficial thrombophlebitis, ventricular extrasystole, spinal extramedullary erythropoietic tissue, and erythema at the injection site/allergic reaction. Two patients discontinued due to hypertension.
Dr Cappellini concluded that sotatercept and the related molecule, luspatercept, may provide a favorable risk-benefit profile for patients with ß-thalassemia.
“These 2 molecules are merging now for a phase 3 trial in either TD or NTD thalassemia cohorts,” she said. “The two drugs are actually very, very similar, and, in fact, for the trial, we decided to use only one. There is no way to go on with 2 molecules.”
In April, Acceleron and Celgene announced plans to initiate a phase 3 program with luspatercept in myelodysplastic syndromes and β-thalassemia by the end of this year. The companies said they will continue to develop sotatercept for patients with chronic kidney disease. ![]()
*Data in the abstract differ from the presentation.
thalassemia
VIENNA—Data from a phase 2a trial suggest the activin receptor sotatercept can effectively treat patients with ß-thalassemia.
However, the companies developing the drug have decided not to advance sotatercept to phase 3 trials in this patient population.
Instead, the companies are initiating a phase 3 program with sotatercept’s “twin” activin receptor, luspatercept, in patients with ß-thalassemia or myelodysplastic syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds. The companies plan to continue developing sotatercept for patients with chronic kidney disease.
Maria Domenica Cappellini, MD, of the University of Milan in Italy, presented results from the phase 2a study of sotatercept in ß-thalassemia at the 20th Congress of the European Hematology Association (abstract S137*).
Phase 2 results with luspatercept in ß-thalassemia were also presented at the meeting.
The dose-finding study of sotatercept had enrolled 46 patients at the time of Dr Cappellini’s presentation. The drug was given subcutaneously at doses ranging from 0.1 mg/kg to 1.0 mg/kg every 3 weeks.
The 30 non-transfusion-dependent (NTD) patients received 4 or fewer red blood cell (RBC) units in the 6 months prior to study enrollment. The 16 transfusion-dependent (TD) patients had received 2 or more RBC units every 30 days for 6 months or more prior to study enrollment.
Twenty-five of the 46 patients remain on treatment, with a median exposure time of 12.4 months.
NTD patients
The patients’ median age was 42, and 53% were female. Fifty-three percent had had a splenectomy, and the median baseline hemoglobin level was 8.4 g/dL.
Treatment with sotatercept produced a dose-dependent hemoglobin increase.
“[W]hat I found quite interesting is that the increase is consistent and persistent, [even] after 1 year,” Dr Cappellini said. “And they are still maintained on treatment, of course, but it is a sustained response.”
At the 0.75 mg/kg dose, 86% of patients had a hemoglobin increase of 1 g/dL for 12 weeks or more, and 71% had an increase of 1.5 g/dL.
TD patients
The patients’ median age was 36 years, and 38% were female. Three-quarters of patients had ß-thalassemia major, and a quarter had ß-thalassemia intermedia.
Nearly a third of patients had had a splenectomy, and their transfusion burden at baseline ranged from 8 RBC units to 35 RBC units every 24 weeks.
The mean reduction in transfusion burden among patients treated with sotatercept at doses of 0.5 mg/kg or higher was 32.25%. And the 1.0 mg/kg dose of sotatercept reduced one patient’s transfusion burden by 61.6%.
Dr Cappellini noted that the pharmacokinetic analysis showed a correlation with exposure. The investigators observed no apparent effects of weight, sex, age, or transfusion burden on drug clearance.
“So the relationship was probably more related to long-term exposure than to the real dosage,” she said.
Safety
Hypertension and bone pain were the most common grade 2-4, treatment-related adverse events.
Seven patients discontinued the study due to adverse events, one patient each with bone pain, superficial thrombophlebitis, ventricular extrasystole, spinal extramedullary erythropoietic tissue, and erythema at the injection site/allergic reaction. Two patients discontinued due to hypertension.
Dr Cappellini concluded that sotatercept and the related molecule, luspatercept, may provide a favorable risk-benefit profile for patients with ß-thalassemia.
“These 2 molecules are merging now for a phase 3 trial in either TD or NTD thalassemia cohorts,” she said. “The two drugs are actually very, very similar, and, in fact, for the trial, we decided to use only one. There is no way to go on with 2 molecules.”
In April, Acceleron and Celgene announced plans to initiate a phase 3 program with luspatercept in myelodysplastic syndromes and β-thalassemia by the end of this year. The companies said they will continue to develop sotatercept for patients with chronic kidney disease. ![]()
*Data in the abstract differ from the presentation.
thalassemia
VIENNA—Data from a phase 2a trial suggest the activin receptor sotatercept can effectively treat patients with ß-thalassemia.
However, the companies developing the drug have decided not to advance sotatercept to phase 3 trials in this patient population.
Instead, the companies are initiating a phase 3 program with sotatercept’s “twin” activin receptor, luspatercept, in patients with ß-thalassemia or myelodysplastic syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds. The companies plan to continue developing sotatercept for patients with chronic kidney disease.
Maria Domenica Cappellini, MD, of the University of Milan in Italy, presented results from the phase 2a study of sotatercept in ß-thalassemia at the 20th Congress of the European Hematology Association (abstract S137*).
Phase 2 results with luspatercept in ß-thalassemia were also presented at the meeting.
The dose-finding study of sotatercept had enrolled 46 patients at the time of Dr Cappellini’s presentation. The drug was given subcutaneously at doses ranging from 0.1 mg/kg to 1.0 mg/kg every 3 weeks.
The 30 non-transfusion-dependent (NTD) patients received 4 or fewer red blood cell (RBC) units in the 6 months prior to study enrollment. The 16 transfusion-dependent (TD) patients had received 2 or more RBC units every 30 days for 6 months or more prior to study enrollment.
Twenty-five of the 46 patients remain on treatment, with a median exposure time of 12.4 months.
NTD patients
The patients’ median age was 42, and 53% were female. Fifty-three percent had had a splenectomy, and the median baseline hemoglobin level was 8.4 g/dL.
Treatment with sotatercept produced a dose-dependent hemoglobin increase.
“[W]hat I found quite interesting is that the increase is consistent and persistent, [even] after 1 year,” Dr Cappellini said. “And they are still maintained on treatment, of course, but it is a sustained response.”
At the 0.75 mg/kg dose, 86% of patients had a hemoglobin increase of 1 g/dL for 12 weeks or more, and 71% had an increase of 1.5 g/dL.
TD patients
The patients’ median age was 36 years, and 38% were female. Three-quarters of patients had ß-thalassemia major, and a quarter had ß-thalassemia intermedia.
Nearly a third of patients had had a splenectomy, and their transfusion burden at baseline ranged from 8 RBC units to 35 RBC units every 24 weeks.
The mean reduction in transfusion burden among patients treated with sotatercept at doses of 0.5 mg/kg or higher was 32.25%. And the 1.0 mg/kg dose of sotatercept reduced one patient’s transfusion burden by 61.6%.
Dr Cappellini noted that the pharmacokinetic analysis showed a correlation with exposure. The investigators observed no apparent effects of weight, sex, age, or transfusion burden on drug clearance.
“So the relationship was probably more related to long-term exposure than to the real dosage,” she said.
Safety
Hypertension and bone pain were the most common grade 2-4, treatment-related adverse events.
Seven patients discontinued the study due to adverse events, one patient each with bone pain, superficial thrombophlebitis, ventricular extrasystole, spinal extramedullary erythropoietic tissue, and erythema at the injection site/allergic reaction. Two patients discontinued due to hypertension.
Dr Cappellini concluded that sotatercept and the related molecule, luspatercept, may provide a favorable risk-benefit profile for patients with ß-thalassemia.
“These 2 molecules are merging now for a phase 3 trial in either TD or NTD thalassemia cohorts,” she said. “The two drugs are actually very, very similar, and, in fact, for the trial, we decided to use only one. There is no way to go on with 2 molecules.”
In April, Acceleron and Celgene announced plans to initiate a phase 3 program with luspatercept in myelodysplastic syndromes and β-thalassemia by the end of this year. The companies said they will continue to develop sotatercept for patients with chronic kidney disease. ![]()
*Data in the abstract differ from the presentation.
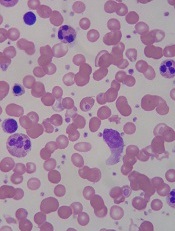
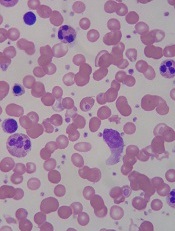
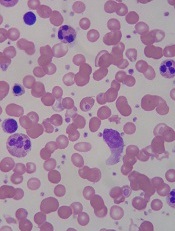
Unsickling red blood cells
VIENNA—Researchers say they have found a way to unsickle red blood cells (RBCs), at least in vitro.
Using pegylated carboxyhemoglobin bovine gas transfer, the team restored sickled RBCs to a more normal, rounder shape in as little as 5 minutes.
Ronald Jubin, PhD, of Prolong Pharmaceuticals, the company developing carboxyhemoglobin, described this process at the 20th Congress of the European Hematology Association (abstract S140).
Pegylated carboxyhemoglobin bovine (Sanguinate [SG]) was designed to reduce vasoconstriction, counteract inflammatory responses, and deliver oxygen to hypoxic cells by releasing carbon monoxide.
The investigators contend that using SG early in a vasooclusive crisis (VOC) can limit the crisis and reduce pain severity.
They evaluated SG treatment using RBCs from healthy volunteers and patients with sickle cell disease (SCD).
The researchers monitored carboxyhemoglobin and oxyhemoglobin levels and analyzed patient samples using light microscopy and image capture flow cytometry. In this manner, they were able to visualize and quantify the effects of SG treatment on reversing the sickling of RBCs.
The investigators found that SG rapidly transferred its carbon monoxide component to oxygenated RBCs along with oxygen loading of SG.
“SG restored more normal RBC shape in as little as 5 minutes,” Dr Jubin said.
SG was also able to continually facilitate gas transfer through multiple exposure events and limited inflammatory marker expression in SCD blood samples.
The researchers concluded that SG can serve as an active gas transport agent, providing either carbon monoxide or oxygen to sickled RBCs. They also noted that image capture flow cytometry allowed for a quantitative measurement of decreased sickling and may provide a way to monitor SG treatment effects on SCD patients in future studies.
Dr Jubin said phase 1 safety trials of SG have been completed, and phase 2 trials are in development for VOC, SCD leg ulcers, delayed cerebral ischemia, prevention of delayed kidney graft function, and pulmonary hypertension in beta-thalassemia.
SG was recently awarded orphan drug status by the US Food and Drug Administration.
Orphan designation provides the company developing a drug with certain benefits and incentives, including a 7-year period of marketing exclusivity upon regulatory approval, potential tax credits for certain activities, eligibility for orphan drug grants, and the waiver of certain administrative fees. ![]()
VIENNA—Researchers say they have found a way to unsickle red blood cells (RBCs), at least in vitro.
Using pegylated carboxyhemoglobin bovine gas transfer, the team restored sickled RBCs to a more normal, rounder shape in as little as 5 minutes.
Ronald Jubin, PhD, of Prolong Pharmaceuticals, the company developing carboxyhemoglobin, described this process at the 20th Congress of the European Hematology Association (abstract S140).
Pegylated carboxyhemoglobin bovine (Sanguinate [SG]) was designed to reduce vasoconstriction, counteract inflammatory responses, and deliver oxygen to hypoxic cells by releasing carbon monoxide.
The investigators contend that using SG early in a vasooclusive crisis (VOC) can limit the crisis and reduce pain severity.
They evaluated SG treatment using RBCs from healthy volunteers and patients with sickle cell disease (SCD).
The researchers monitored carboxyhemoglobin and oxyhemoglobin levels and analyzed patient samples using light microscopy and image capture flow cytometry. In this manner, they were able to visualize and quantify the effects of SG treatment on reversing the sickling of RBCs.
The investigators found that SG rapidly transferred its carbon monoxide component to oxygenated RBCs along with oxygen loading of SG.
“SG restored more normal RBC shape in as little as 5 minutes,” Dr Jubin said.
SG was also able to continually facilitate gas transfer through multiple exposure events and limited inflammatory marker expression in SCD blood samples.
The researchers concluded that SG can serve as an active gas transport agent, providing either carbon monoxide or oxygen to sickled RBCs. They also noted that image capture flow cytometry allowed for a quantitative measurement of decreased sickling and may provide a way to monitor SG treatment effects on SCD patients in future studies.
Dr Jubin said phase 1 safety trials of SG have been completed, and phase 2 trials are in development for VOC, SCD leg ulcers, delayed cerebral ischemia, prevention of delayed kidney graft function, and pulmonary hypertension in beta-thalassemia.
SG was recently awarded orphan drug status by the US Food and Drug Administration.
Orphan designation provides the company developing a drug with certain benefits and incentives, including a 7-year period of marketing exclusivity upon regulatory approval, potential tax credits for certain activities, eligibility for orphan drug grants, and the waiver of certain administrative fees. ![]()
VIENNA—Researchers say they have found a way to unsickle red blood cells (RBCs), at least in vitro.
Using pegylated carboxyhemoglobin bovine gas transfer, the team restored sickled RBCs to a more normal, rounder shape in as little as 5 minutes.
Ronald Jubin, PhD, of Prolong Pharmaceuticals, the company developing carboxyhemoglobin, described this process at the 20th Congress of the European Hematology Association (abstract S140).
Pegylated carboxyhemoglobin bovine (Sanguinate [SG]) was designed to reduce vasoconstriction, counteract inflammatory responses, and deliver oxygen to hypoxic cells by releasing carbon monoxide.
The investigators contend that using SG early in a vasooclusive crisis (VOC) can limit the crisis and reduce pain severity.
They evaluated SG treatment using RBCs from healthy volunteers and patients with sickle cell disease (SCD).
The researchers monitored carboxyhemoglobin and oxyhemoglobin levels and analyzed patient samples using light microscopy and image capture flow cytometry. In this manner, they were able to visualize and quantify the effects of SG treatment on reversing the sickling of RBCs.
The investigators found that SG rapidly transferred its carbon monoxide component to oxygenated RBCs along with oxygen loading of SG.
“SG restored more normal RBC shape in as little as 5 minutes,” Dr Jubin said.
SG was also able to continually facilitate gas transfer through multiple exposure events and limited inflammatory marker expression in SCD blood samples.
The researchers concluded that SG can serve as an active gas transport agent, providing either carbon monoxide or oxygen to sickled RBCs. They also noted that image capture flow cytometry allowed for a quantitative measurement of decreased sickling and may provide a way to monitor SG treatment effects on SCD patients in future studies.
Dr Jubin said phase 1 safety trials of SG have been completed, and phase 2 trials are in development for VOC, SCD leg ulcers, delayed cerebral ischemia, prevention of delayed kidney graft function, and pulmonary hypertension in beta-thalassemia.
SG was recently awarded orphan drug status by the US Food and Drug Administration.
Orphan designation provides the company developing a drug with certain benefits and incentives, including a 7-year period of marketing exclusivity upon regulatory approval, potential tax credits for certain activities, eligibility for orphan drug grants, and the waiver of certain administrative fees. ![]()
Older patients benefit from brentuximab treatment

Credit: NIH
SAN FRANCISCO—Younger patients with Hodgkin lymphoma fare well on brentuximab vedotin, experiencing an overall objective response rate (ORR) of 75% and a complete response (CR) rate of 34% in the pivotal phase 2 study of patients with relapsed/refractory disease.
And a retrospective study of patients older than 60 years showed that single-agent therapy was well tolerated, prompting an ORR of 53% and a CR rate of 40% in a relapsed or refractory population.
So investigators decided to explore in a prospective study whether patients 60 years or older could benefit from up-front treatment with brentuximab as a single agent or in combination.
Andres Forero-Torres, MD, of the University of Alabama in Birmingham, presented the results of this trial at the 2014 ASH Annual Meeting (abstract 294).*
Enrolled patients had classic Hodgkin lymphoma, were treatment-naïve, and were ineligible for or declined conventional front-line treatment. The primary endpoint was ORR.
The study is being conducted in 3 parts—brentuximab as a single agent, brentuximab plus dacarbazine, and brentuximab plus bendamustine. At the time of the ASH presentation, data for the brentuximab-bendamustine combination were not available.
Single-agent brentuximab
Twenty-seven patients on the single-agent arm were evaluable for efficacy and safety. They were a median age of 78 (range, 64 to 92). About half (52%) were male, and 78% had an ECOG performance status of grade 0 or 1.
Forty-four percent had moderate renal function impairment with a creatinine clearance between 30 and 60 mL/min. Thirty percent had B symptoms, 22% had bulky disease, and 52% had extra-nodal involvement.
Patients received 1.8 mg/kg of brentuximab intravenously on day 1 of a 21-day cycle. Response was assessed by CT scan during cycles 2, 4, 8, and 16, and by CT plus PET scan during cycles 2 and 8.
The median follow-up was 8.7 months. Dr Forero-Torres pointed out that, initially, “there were no progressions,” and all patients achieved tumor reduction.
The ORR was 93%, the CR rate was 70%, the partial response rate was 22%, and the rate of stable disease was 7%.
The median duration of response was 9.1 months (range, 0.03 to 13.14), and the median progression-free survival was 10.5 months (range, 2.6 to 14.3). For patients who had a CR, the median progression-free survival was about 12 months, Dr Forero-Torres said.
The median number of treatment cycles administered per patient was 8 (range, 3 to 23). Patients discontinued treatment primarily because of progressive disease (41%) or adverse events (AEs, 37%).
AEs occurring in 20% or more of patients were constipation, decreased appetite, diarrhea, peripheral edema, nausea, fatigue, and peripheral sensory neuropathy. All were grade 1 or 2, except for peripheral sensory neuropathy, which also had about 20% grade 3 events.
Grade 3 or higher treatment-related AEs included peripheral sensory neuropathy (n=7), peripheral motor neuropathy (n=2), rash (n=2), and 1 patient each with anemia, increased aspartate aminotransferase, asthenia, neutropenia, orthostatic hypotension, generalized rash, and maculopapular rash.
Serious AEs (SAEs) were minimal, Dr Forero-Torres said, and included 1 patient each with pyrexia, orthostatic hypotension, asthenia and rash, and deep vein thrombosis.
Seven patients discontinued treatment due to peripheral sensory neuropathy, 2 due to peripheral motor neuropathy, and 1 due to orthostatic hypotension.
Dr Forero-Torres emphasized that there were no grade 4 AEs, no AE-related deaths, and no deaths within 30 days of the last dose of medication.
Brentuximab plus dacarbazine
Fourteen of 18 patients in the combination arm were evaluable for efficacy and safety. Their median age was 72.5 (range, 62 to 87), 72% were male, 67% had an ECOG status of grade 0 or 1, and 56% had normal renal function with a creatinine clearance greater than 80 mL/min.
Forty-four percent exhibited B symptoms, 11% had bulky disease, and 50% had extra-nodal involvement.
They received brentuximab at 1.8 mg/kg plus dacarbazine at 375 mg/m2 for cycles 1-12, followed by monotherapy for cycles 13-16.
At the time of the interim analysis, 83% of patients were still on treatment, “so this is very early preliminary data,” Dr Forero-Torres noted.
All of the patients achieved tumor reduction, and 4 patients achieved a CR.
They had a median treatment duration of 16.7 weeks (range, 3 to 36), received a median of 5.5 cycles (range, 1 to 12), and had a median follow-up time of 19.1 weeks (range, 6.1 to 36.1).
The most common grade 1 or 2 AEs were peripheral sensory neuropathy (33%), nausea (33%), diarrhea (28%), constipation (28%), fatigue (22%), alopecia (22%), arthralgia (22%), and headache (22%).
Grade 3 AEs or SAEs, with 1 patient each, were C difficile colitis (SAE), hypotension (SAE), and hyperglycemia.
Dr Forero-Torres noted that investigators observed “robust antitumor activity” among these older patients receiving front-line brentuximab.
The cohort combining brentuximab with bendamustine is currently enrolling patients.
The study is sponsored by Seattle Genetics, Inc., developer of brentuximab vedotin (Adcetris).![]()
*Information in the abstract differs from that presented at the meeting.

Credit: NIH
SAN FRANCISCO—Younger patients with Hodgkin lymphoma fare well on brentuximab vedotin, experiencing an overall objective response rate (ORR) of 75% and a complete response (CR) rate of 34% in the pivotal phase 2 study of patients with relapsed/refractory disease.
And a retrospective study of patients older than 60 years showed that single-agent therapy was well tolerated, prompting an ORR of 53% and a CR rate of 40% in a relapsed or refractory population.
So investigators decided to explore in a prospective study whether patients 60 years or older could benefit from up-front treatment with brentuximab as a single agent or in combination.
Andres Forero-Torres, MD, of the University of Alabama in Birmingham, presented the results of this trial at the 2014 ASH Annual Meeting (abstract 294).*
Enrolled patients had classic Hodgkin lymphoma, were treatment-naïve, and were ineligible for or declined conventional front-line treatment. The primary endpoint was ORR.
The study is being conducted in 3 parts—brentuximab as a single agent, brentuximab plus dacarbazine, and brentuximab plus bendamustine. At the time of the ASH presentation, data for the brentuximab-bendamustine combination were not available.
Single-agent brentuximab
Twenty-seven patients on the single-agent arm were evaluable for efficacy and safety. They were a median age of 78 (range, 64 to 92). About half (52%) were male, and 78% had an ECOG performance status of grade 0 or 1.
Forty-four percent had moderate renal function impairment with a creatinine clearance between 30 and 60 mL/min. Thirty percent had B symptoms, 22% had bulky disease, and 52% had extra-nodal involvement.
Patients received 1.8 mg/kg of brentuximab intravenously on day 1 of a 21-day cycle. Response was assessed by CT scan during cycles 2, 4, 8, and 16, and by CT plus PET scan during cycles 2 and 8.
The median follow-up was 8.7 months. Dr Forero-Torres pointed out that, initially, “there were no progressions,” and all patients achieved tumor reduction.
The ORR was 93%, the CR rate was 70%, the partial response rate was 22%, and the rate of stable disease was 7%.
The median duration of response was 9.1 months (range, 0.03 to 13.14), and the median progression-free survival was 10.5 months (range, 2.6 to 14.3). For patients who had a CR, the median progression-free survival was about 12 months, Dr Forero-Torres said.
The median number of treatment cycles administered per patient was 8 (range, 3 to 23). Patients discontinued treatment primarily because of progressive disease (41%) or adverse events (AEs, 37%).
AEs occurring in 20% or more of patients were constipation, decreased appetite, diarrhea, peripheral edema, nausea, fatigue, and peripheral sensory neuropathy. All were grade 1 or 2, except for peripheral sensory neuropathy, which also had about 20% grade 3 events.
Grade 3 or higher treatment-related AEs included peripheral sensory neuropathy (n=7), peripheral motor neuropathy (n=2), rash (n=2), and 1 patient each with anemia, increased aspartate aminotransferase, asthenia, neutropenia, orthostatic hypotension, generalized rash, and maculopapular rash.
Serious AEs (SAEs) were minimal, Dr Forero-Torres said, and included 1 patient each with pyrexia, orthostatic hypotension, asthenia and rash, and deep vein thrombosis.
Seven patients discontinued treatment due to peripheral sensory neuropathy, 2 due to peripheral motor neuropathy, and 1 due to orthostatic hypotension.
Dr Forero-Torres emphasized that there were no grade 4 AEs, no AE-related deaths, and no deaths within 30 days of the last dose of medication.
Brentuximab plus dacarbazine
Fourteen of 18 patients in the combination arm were evaluable for efficacy and safety. Their median age was 72.5 (range, 62 to 87), 72% were male, 67% had an ECOG status of grade 0 or 1, and 56% had normal renal function with a creatinine clearance greater than 80 mL/min.
Forty-four percent exhibited B symptoms, 11% had bulky disease, and 50% had extra-nodal involvement.
They received brentuximab at 1.8 mg/kg plus dacarbazine at 375 mg/m2 for cycles 1-12, followed by monotherapy for cycles 13-16.
At the time of the interim analysis, 83% of patients were still on treatment, “so this is very early preliminary data,” Dr Forero-Torres noted.
All of the patients achieved tumor reduction, and 4 patients achieved a CR.
They had a median treatment duration of 16.7 weeks (range, 3 to 36), received a median of 5.5 cycles (range, 1 to 12), and had a median follow-up time of 19.1 weeks (range, 6.1 to 36.1).
The most common grade 1 or 2 AEs were peripheral sensory neuropathy (33%), nausea (33%), diarrhea (28%), constipation (28%), fatigue (22%), alopecia (22%), arthralgia (22%), and headache (22%).
Grade 3 AEs or SAEs, with 1 patient each, were C difficile colitis (SAE), hypotension (SAE), and hyperglycemia.
Dr Forero-Torres noted that investigators observed “robust antitumor activity” among these older patients receiving front-line brentuximab.
The cohort combining brentuximab with bendamustine is currently enrolling patients.
The study is sponsored by Seattle Genetics, Inc., developer of brentuximab vedotin (Adcetris).![]()
*Information in the abstract differs from that presented at the meeting.

Credit: NIH
SAN FRANCISCO—Younger patients with Hodgkin lymphoma fare well on brentuximab vedotin, experiencing an overall objective response rate (ORR) of 75% and a complete response (CR) rate of 34% in the pivotal phase 2 study of patients with relapsed/refractory disease.
And a retrospective study of patients older than 60 years showed that single-agent therapy was well tolerated, prompting an ORR of 53% and a CR rate of 40% in a relapsed or refractory population.
So investigators decided to explore in a prospective study whether patients 60 years or older could benefit from up-front treatment with brentuximab as a single agent or in combination.
Andres Forero-Torres, MD, of the University of Alabama in Birmingham, presented the results of this trial at the 2014 ASH Annual Meeting (abstract 294).*
Enrolled patients had classic Hodgkin lymphoma, were treatment-naïve, and were ineligible for or declined conventional front-line treatment. The primary endpoint was ORR.
The study is being conducted in 3 parts—brentuximab as a single agent, brentuximab plus dacarbazine, and brentuximab plus bendamustine. At the time of the ASH presentation, data for the brentuximab-bendamustine combination were not available.
Single-agent brentuximab
Twenty-seven patients on the single-agent arm were evaluable for efficacy and safety. They were a median age of 78 (range, 64 to 92). About half (52%) were male, and 78% had an ECOG performance status of grade 0 or 1.
Forty-four percent had moderate renal function impairment with a creatinine clearance between 30 and 60 mL/min. Thirty percent had B symptoms, 22% had bulky disease, and 52% had extra-nodal involvement.
Patients received 1.8 mg/kg of brentuximab intravenously on day 1 of a 21-day cycle. Response was assessed by CT scan during cycles 2, 4, 8, and 16, and by CT plus PET scan during cycles 2 and 8.
The median follow-up was 8.7 months. Dr Forero-Torres pointed out that, initially, “there were no progressions,” and all patients achieved tumor reduction.
The ORR was 93%, the CR rate was 70%, the partial response rate was 22%, and the rate of stable disease was 7%.
The median duration of response was 9.1 months (range, 0.03 to 13.14), and the median progression-free survival was 10.5 months (range, 2.6 to 14.3). For patients who had a CR, the median progression-free survival was about 12 months, Dr Forero-Torres said.
The median number of treatment cycles administered per patient was 8 (range, 3 to 23). Patients discontinued treatment primarily because of progressive disease (41%) or adverse events (AEs, 37%).
AEs occurring in 20% or more of patients were constipation, decreased appetite, diarrhea, peripheral edema, nausea, fatigue, and peripheral sensory neuropathy. All were grade 1 or 2, except for peripheral sensory neuropathy, which also had about 20% grade 3 events.
Grade 3 or higher treatment-related AEs included peripheral sensory neuropathy (n=7), peripheral motor neuropathy (n=2), rash (n=2), and 1 patient each with anemia, increased aspartate aminotransferase, asthenia, neutropenia, orthostatic hypotension, generalized rash, and maculopapular rash.
Serious AEs (SAEs) were minimal, Dr Forero-Torres said, and included 1 patient each with pyrexia, orthostatic hypotension, asthenia and rash, and deep vein thrombosis.
Seven patients discontinued treatment due to peripheral sensory neuropathy, 2 due to peripheral motor neuropathy, and 1 due to orthostatic hypotension.
Dr Forero-Torres emphasized that there were no grade 4 AEs, no AE-related deaths, and no deaths within 30 days of the last dose of medication.
Brentuximab plus dacarbazine
Fourteen of 18 patients in the combination arm were evaluable for efficacy and safety. Their median age was 72.5 (range, 62 to 87), 72% were male, 67% had an ECOG status of grade 0 or 1, and 56% had normal renal function with a creatinine clearance greater than 80 mL/min.
Forty-four percent exhibited B symptoms, 11% had bulky disease, and 50% had extra-nodal involvement.
They received brentuximab at 1.8 mg/kg plus dacarbazine at 375 mg/m2 for cycles 1-12, followed by monotherapy for cycles 13-16.
At the time of the interim analysis, 83% of patients were still on treatment, “so this is very early preliminary data,” Dr Forero-Torres noted.
All of the patients achieved tumor reduction, and 4 patients achieved a CR.
They had a median treatment duration of 16.7 weeks (range, 3 to 36), received a median of 5.5 cycles (range, 1 to 12), and had a median follow-up time of 19.1 weeks (range, 6.1 to 36.1).
The most common grade 1 or 2 AEs were peripheral sensory neuropathy (33%), nausea (33%), diarrhea (28%), constipation (28%), fatigue (22%), alopecia (22%), arthralgia (22%), and headache (22%).
Grade 3 AEs or SAEs, with 1 patient each, were C difficile colitis (SAE), hypotension (SAE), and hyperglycemia.
Dr Forero-Torres noted that investigators observed “robust antitumor activity” among these older patients receiving front-line brentuximab.
The cohort combining brentuximab with bendamustine is currently enrolling patients.
The study is sponsored by Seattle Genetics, Inc., developer of brentuximab vedotin (Adcetris).![]()
*Information in the abstract differs from that presented at the meeting.
CARs come in different makes and models

Credit: NIAID
SAN FRANCISCO—CTL019, a chimeric antigen receptor (CAR) T cell targeting CD19, is not the only CAR in the production line.
Investigators at the National Cancer Institute in Bethesda, Maryland, and Memorial Sloan Kettering Cancer Center (MSKCC) in New York City are also pursuing CAR T-cell therapy.
These groups are using a retroviral platform to transduce the T cells rather than a lentiviral one, as is the case with CTL019.
Investigators reported progress to date on these makes of CARs at the 2014 ASH Annual Meeting.
Daniel W. Lee III, MD, of the National Cancer Institute, reported on a phase 1 study of CD19 CAR T cells in children and young adults with CD19+ acute lymphoblastic leukemia or non-Hodgkin lymphoma.
And Jae H. Park, MD, of MSKCC, presented data from a trial of JCAR015—autologous T cells genetically modified to express a 19-28z CAR targeting CD19—in patients with B-cell acute lymphoblastic leukemia.
The study is sponsored by MSKCC, but JCAR015 is a product of Juno Therapeutics. ![]()

Credit: NIAID
SAN FRANCISCO—CTL019, a chimeric antigen receptor (CAR) T cell targeting CD19, is not the only CAR in the production line.
Investigators at the National Cancer Institute in Bethesda, Maryland, and Memorial Sloan Kettering Cancer Center (MSKCC) in New York City are also pursuing CAR T-cell therapy.
These groups are using a retroviral platform to transduce the T cells rather than a lentiviral one, as is the case with CTL019.
Investigators reported progress to date on these makes of CARs at the 2014 ASH Annual Meeting.
Daniel W. Lee III, MD, of the National Cancer Institute, reported on a phase 1 study of CD19 CAR T cells in children and young adults with CD19+ acute lymphoblastic leukemia or non-Hodgkin lymphoma.
And Jae H. Park, MD, of MSKCC, presented data from a trial of JCAR015—autologous T cells genetically modified to express a 19-28z CAR targeting CD19—in patients with B-cell acute lymphoblastic leukemia.
The study is sponsored by MSKCC, but JCAR015 is a product of Juno Therapeutics. ![]()

Credit: NIAID
SAN FRANCISCO—CTL019, a chimeric antigen receptor (CAR) T cell targeting CD19, is not the only CAR in the production line.
Investigators at the National Cancer Institute in Bethesda, Maryland, and Memorial Sloan Kettering Cancer Center (MSKCC) in New York City are also pursuing CAR T-cell therapy.
These groups are using a retroviral platform to transduce the T cells rather than a lentiviral one, as is the case with CTL019.
Investigators reported progress to date on these makes of CARs at the 2014 ASH Annual Meeting.
Daniel W. Lee III, MD, of the National Cancer Institute, reported on a phase 1 study of CD19 CAR T cells in children and young adults with CD19+ acute lymphoblastic leukemia or non-Hodgkin lymphoma.
And Jae H. Park, MD, of MSKCC, presented data from a trial of JCAR015—autologous T cells genetically modified to express a 19-28z CAR targeting CD19—in patients with B-cell acute lymphoblastic leukemia.
The study is sponsored by MSKCC, but JCAR015 is a product of Juno Therapeutics. ![]()
CAR is feasible in majority of ALL patients, team says

Credit: Bill Branson
SAN FRANCISCO—A chimeric antigen receptor (CAR) T-cell therapy is feasible in 90% of heavily pretreated or transplanted patients with acute lymphoblastic leukemia (ALL) and can serve as a bridge to transplant, according to investigators.
Daniel W. Lee III, MD, of the National Cancer Institute in Bethesda, Maryland, reported on a phase 1 study of this CD19 CAR T-cell therapy in children and young adults with CD19+ ALL or non-Hodgkin lymphoma at the 2014 ASH Annual Meeting (abstract 381*).
Twenty-one patients were enrolled on the trial. They had a preparative regimen of fludarabine and cyclophosphamide and were infused with CAR T cells 11 days after the peripheral blood mononuclear cells were collected.
Dose levels were 1 x 106 CAR+ T cells/kg, 3 x 106 CAR+ T cells/kg, or the maximum number of cells generated if below either one of these levels. Two patients received less than the dose assigned and were not evaluated for toxicity.
Patients were a median age of 13 years (range, 5 to 27). Fourteen were male, 20 had ALL, and 1 had diffuse large B-cell lymphoma.
All had detectable disease, and 2 were CNS2 at the time of T-cell infusion. Six had primary refractory disease, 8 had at least 1 prior stem cell transplant, and 4 had prior immunotherapy.
The investigators determined that the maximally tolerated dose was 1 x 106 CAR+ T cells/kg. The dose-limiting toxicities were related to cytokine release syndrome (CRS), which was reversible if managed appropriately with tocilizumab, with or without steroids.
Grade 3 adverse events possibly related to therapy included fever (47%), febrile neutropenia (37%), electrolyte disturbance (29%), CRS (16%), hypotension (11%), transaminitis (16%), and 5% each for hypertension, prolonged QTc, dysphasia, LV systolic dysfunction, multiorgan failure, hypoxia, and pulmonary edema.
Grade 4 events possibly related to treatment included electrolyte disturbance (5%), CRS (16%), hypotension (11%), cardiac arrest (5%), and hypoxia (5%). There was no evidence of graft-vs-host disease.
The complete response (CR) rate was 67% in the intent-to-treat population and 70% in patients with ALL.
“Those patients who responded tended to have some degree of cytokine release syndrome, whereas those patients who did not respond or had stable disease did not have any CRS,” Dr Lee said. “But, also, it’s important to note that you don’t have to have severe grade 3 or grade 4 CRS in order to have significant response.”
Dr Lee also pointed out that in vivo CAR T-cell expansion significantly correlated with response (P=0.0028). And CRS severity correlated with IL-6 (P=0.0002), INF-γ (P=0.0002), C-reactive protein (P=0.0015), and CAR (P=0.0011).
At a median follow-up of 10 months, minimal residual disease-negative patients had a 79% leukemia-free survival. Overall survival was 52% for all patients enrolled. Two patients had CD19-negative relapses.
The investigators also found that CAR T cells can eliminate CNS leukemia, with 11 of 17 patients (65%) having CAR T cells detectable in their cerebrospinal fluid.
The team concluded that this therapy is feasible in 90% of heavily pretreated or transplanted ALL patients and can serve as a bridge to transplant. ![]()
*Information in the abstract differs from that presented at the meeting.

Credit: Bill Branson
SAN FRANCISCO—A chimeric antigen receptor (CAR) T-cell therapy is feasible in 90% of heavily pretreated or transplanted patients with acute lymphoblastic leukemia (ALL) and can serve as a bridge to transplant, according to investigators.
Daniel W. Lee III, MD, of the National Cancer Institute in Bethesda, Maryland, reported on a phase 1 study of this CD19 CAR T-cell therapy in children and young adults with CD19+ ALL or non-Hodgkin lymphoma at the 2014 ASH Annual Meeting (abstract 381*).
Twenty-one patients were enrolled on the trial. They had a preparative regimen of fludarabine and cyclophosphamide and were infused with CAR T cells 11 days after the peripheral blood mononuclear cells were collected.
Dose levels were 1 x 106 CAR+ T cells/kg, 3 x 106 CAR+ T cells/kg, or the maximum number of cells generated if below either one of these levels. Two patients received less than the dose assigned and were not evaluated for toxicity.
Patients were a median age of 13 years (range, 5 to 27). Fourteen were male, 20 had ALL, and 1 had diffuse large B-cell lymphoma.
All had detectable disease, and 2 were CNS2 at the time of T-cell infusion. Six had primary refractory disease, 8 had at least 1 prior stem cell transplant, and 4 had prior immunotherapy.
The investigators determined that the maximally tolerated dose was 1 x 106 CAR+ T cells/kg. The dose-limiting toxicities were related to cytokine release syndrome (CRS), which was reversible if managed appropriately with tocilizumab, with or without steroids.
Grade 3 adverse events possibly related to therapy included fever (47%), febrile neutropenia (37%), electrolyte disturbance (29%), CRS (16%), hypotension (11%), transaminitis (16%), and 5% each for hypertension, prolonged QTc, dysphasia, LV systolic dysfunction, multiorgan failure, hypoxia, and pulmonary edema.
Grade 4 events possibly related to treatment included electrolyte disturbance (5%), CRS (16%), hypotension (11%), cardiac arrest (5%), and hypoxia (5%). There was no evidence of graft-vs-host disease.
The complete response (CR) rate was 67% in the intent-to-treat population and 70% in patients with ALL.
“Those patients who responded tended to have some degree of cytokine release syndrome, whereas those patients who did not respond or had stable disease did not have any CRS,” Dr Lee said. “But, also, it’s important to note that you don’t have to have severe grade 3 or grade 4 CRS in order to have significant response.”
Dr Lee also pointed out that in vivo CAR T-cell expansion significantly correlated with response (P=0.0028). And CRS severity correlated with IL-6 (P=0.0002), INF-γ (P=0.0002), C-reactive protein (P=0.0015), and CAR (P=0.0011).
At a median follow-up of 10 months, minimal residual disease-negative patients had a 79% leukemia-free survival. Overall survival was 52% for all patients enrolled. Two patients had CD19-negative relapses.
The investigators also found that CAR T cells can eliminate CNS leukemia, with 11 of 17 patients (65%) having CAR T cells detectable in their cerebrospinal fluid.
The team concluded that this therapy is feasible in 90% of heavily pretreated or transplanted ALL patients and can serve as a bridge to transplant. ![]()
*Information in the abstract differs from that presented at the meeting.

Credit: Bill Branson
SAN FRANCISCO—A chimeric antigen receptor (CAR) T-cell therapy is feasible in 90% of heavily pretreated or transplanted patients with acute lymphoblastic leukemia (ALL) and can serve as a bridge to transplant, according to investigators.
Daniel W. Lee III, MD, of the National Cancer Institute in Bethesda, Maryland, reported on a phase 1 study of this CD19 CAR T-cell therapy in children and young adults with CD19+ ALL or non-Hodgkin lymphoma at the 2014 ASH Annual Meeting (abstract 381*).
Twenty-one patients were enrolled on the trial. They had a preparative regimen of fludarabine and cyclophosphamide and were infused with CAR T cells 11 days after the peripheral blood mononuclear cells were collected.
Dose levels were 1 x 106 CAR+ T cells/kg, 3 x 106 CAR+ T cells/kg, or the maximum number of cells generated if below either one of these levels. Two patients received less than the dose assigned and were not evaluated for toxicity.
Patients were a median age of 13 years (range, 5 to 27). Fourteen were male, 20 had ALL, and 1 had diffuse large B-cell lymphoma.
All had detectable disease, and 2 were CNS2 at the time of T-cell infusion. Six had primary refractory disease, 8 had at least 1 prior stem cell transplant, and 4 had prior immunotherapy.
The investigators determined that the maximally tolerated dose was 1 x 106 CAR+ T cells/kg. The dose-limiting toxicities were related to cytokine release syndrome (CRS), which was reversible if managed appropriately with tocilizumab, with or without steroids.
Grade 3 adverse events possibly related to therapy included fever (47%), febrile neutropenia (37%), electrolyte disturbance (29%), CRS (16%), hypotension (11%), transaminitis (16%), and 5% each for hypertension, prolonged QTc, dysphasia, LV systolic dysfunction, multiorgan failure, hypoxia, and pulmonary edema.
Grade 4 events possibly related to treatment included electrolyte disturbance (5%), CRS (16%), hypotension (11%), cardiac arrest (5%), and hypoxia (5%). There was no evidence of graft-vs-host disease.
The complete response (CR) rate was 67% in the intent-to-treat population and 70% in patients with ALL.
“Those patients who responded tended to have some degree of cytokine release syndrome, whereas those patients who did not respond or had stable disease did not have any CRS,” Dr Lee said. “But, also, it’s important to note that you don’t have to have severe grade 3 or grade 4 CRS in order to have significant response.”
Dr Lee also pointed out that in vivo CAR T-cell expansion significantly correlated with response (P=0.0028). And CRS severity correlated with IL-6 (P=0.0002), INF-γ (P=0.0002), C-reactive protein (P=0.0015), and CAR (P=0.0011).
At a median follow-up of 10 months, minimal residual disease-negative patients had a 79% leukemia-free survival. Overall survival was 52% for all patients enrolled. Two patients had CD19-negative relapses.
The investigators also found that CAR T cells can eliminate CNS leukemia, with 11 of 17 patients (65%) having CAR T cells detectable in their cerebrospinal fluid.
The team concluded that this therapy is feasible in 90% of heavily pretreated or transplanted ALL patients and can serve as a bridge to transplant.
*Information in the abstract differs from that presented at the meeting.
CAR produces durable responses in B-cell ALL

Credit: Charles Haymond
SAN FRANCISCO—JCAR015, a chimeric antigen receptor (CAR) T-cell therapy, can produce durable responses in patients with B-cell acute lymphoblastic leukemia (ALL) who do not undergo subsequent hematopoietic stem cell transplant (HSCT), new research suggests.
JCAR015 consists of autologous T cells genetically modified to express 19-28z chimeric antigen receptor (19-28z CAR) targeting CD19.
Jae H. Park, MD, of Memorial Sloan Kettering Cancer Center in New York, presented data on JCAR015 at the 2014 ASH Annual Meeting (abstract 382).* The study is sponsored by Memorial Sloan Kettering, but funding has also been provided by Juno Therapeutics, the company developing JCAR015.
JCAR015 was tested at a dose of 1 - 3 x 106 CAR cells/kg in 33 adults with relapsed/refractory B-cell ALL. Twenty-eight patients were evaluable for toxicity, 27 for response, and 5 patients were too early in their treatment to evaluate at the time of data cutoff.
Twenty-one patients were male, and the median age was 55 (range, 23 to 74).
Thirteen patients (46%) had minimal disease (<5% blasts) immediately prior to T-cell infusion, and 15 patients (54%) had morphologic disease of 5% to 100% blasts (median 63%).
Eighteen patients (64%) had received 2 prior lines of therapy, and 5 (18%) each had 3 or more prior lines.
Eight patients (29%) underwent prior allogeneic HSCT, 9 patients (32%) were Philadelphia chromosome positive (Ph+), and 3 (11%) had the T315I mutation.
The overall complete response (CR) rate was 89%, and the minimal residual disease-negative CR rate was 88%. The median time to CR was 22.5 days (range, 9 to 33).
The investigators performed a subgroup analysis and found that 100% of the 13 patients with minimal disease before therapy achieved a CR, compared to 79% of patients with morphologic disease.
Eighty-six percent (6/7) of patients who had a prior HSCT and 90% (18/20) without a prior HSCT achieved a CR. Eighty-nine percent (8/9) of Ph+ patients achieved a CR, and 89% (16/18) of Philadelphia-negative patients (89%) achieved a CR.
At a median follow-up of 6 months (range, 1 to 38 months), 12 patients remained disease-free, including 7 patients who had more than a year of follow-up. Seven patients are disease-free without a subsequent HSCT.
Nine patients relapsed during a follow-up of 3 to 8 months, and 10 patients proceeded to HSCT. Two relapses occurred after HSCT, one in a patient who had CD19-negative blasts, and 7 relapses occurred without HSCT.
The overall survival rate at 6 months was 57%, and the median survival was 8.5 months.
For those patients who had a transplant after CAR therapy, the median survival was 10.8 months, and the survival rate at 6 months was 68%.
Dr Park pointed out that maximum T-cell expansion occurred between days 7 and 14 and correlated with the occurrence of cytokine release syndrome (CRS). The T cells persisted for 1 to 3 months following infusion.
The main adverse events were those associated with CRS and neurologic changes. Severe CRS requiring vasopressors or mechanical ventilation occurred in 5 patients (18%) overall and in 5 patients (33%) with morphologic disease before therapy. Severe CRS did not occur in any patient with minimal disease before therapy.
Grade 3 or 4 neurotoxicity occurred in 7 patients (25%) overall, in 6 patients (40%) with morphologic disease, and in 1 with minimal disease (8%) before therapy.
The investigators observed no graft-vs-host disease exacerbation, and CRS was managed with an IL-6R inhibitor, steroids, or both.
Dr Park noted that the neurologic symptoms are reversible and can occur independently of CRS.
He also pointed out that CR rates were similar regardless of different disease risk factors, and that durable responses have been achieved in patients who did not have a subsequent HSCT.
*Information in the abstract differs from that presented at the meeting.

Credit: Charles Haymond
SAN FRANCISCO—JCAR015, a chimeric antigen receptor (CAR) T-cell therapy, can produce durable responses in patients with B-cell acute lymphoblastic leukemia (ALL) who do not undergo subsequent hematopoietic stem cell transplant (HSCT), new research suggests.
JCAR015 consists of autologous T cells genetically modified to express 19-28z chimeric antigen receptor (19-28z CAR) targeting CD19.
Jae H. Park, MD, of Memorial Sloan Kettering Cancer Center in New York, presented data on JCAR015 at the 2014 ASH Annual Meeting (abstract 382).* The study is sponsored by Memorial Sloan Kettering, but funding has also been provided by Juno Therapeutics, the company developing JCAR015.
JCAR015 was tested at a dose of 1 - 3 x 106 CAR cells/kg in 33 adults with relapsed/refractory B-cell ALL. Twenty-eight patients were evaluable for toxicity, 27 for response, and 5 patients were too early in their treatment to evaluate at the time of data cutoff.
Twenty-one patients were male, and the median age was 55 (range, 23 to 74).
Thirteen patients (46%) had minimal disease (<5% blasts) immediately prior to T-cell infusion, and 15 patients (54%) had morphologic disease of 5% to 100% blasts (median 63%).
Eighteen patients (64%) had received 2 prior lines of therapy, and 5 (18%) each had 3 or more prior lines.
Eight patients (29%) underwent prior allogeneic HSCT, 9 patients (32%) were Philadelphia chromosome positive (Ph+), and 3 (11%) had the T315I mutation.
The overall complete response (CR) rate was 89%, and the minimal residual disease-negative CR rate was 88%. The median time to CR was 22.5 days (range, 9 to 33).
The investigators performed a subgroup analysis and found that 100% of the 13 patients with minimal disease before therapy achieved a CR, compared to 79% of patients with morphologic disease.
Eighty-six percent (6/7) of patients who had a prior HSCT and 90% (18/20) without a prior HSCT achieved a CR. Eighty-nine percent (8/9) of Ph+ patients achieved a CR, and 89% (16/18) of Philadelphia-negative patients (89%) achieved a CR.
At a median follow-up of 6 months (range, 1 to 38 months), 12 patients remained disease-free, including 7 patients who had more than a year of follow-up. Seven patients are disease-free without a subsequent HSCT.
Nine patients relapsed during a follow-up of 3 to 8 months, and 10 patients proceeded to HSCT. Two relapses occurred after HSCT, one in a patient who had CD19-negative blasts, and 7 relapses occurred without HSCT.
The overall survival rate at 6 months was 57%, and the median survival was 8.5 months.
For those patients who had a transplant after CAR therapy, the median survival was 10.8 months, and the survival rate at 6 months was 68%.
Dr Park pointed out that maximum T-cell expansion occurred between days 7 and 14 and correlated with the occurrence of cytokine release syndrome (CRS). The T cells persisted for 1 to 3 months following infusion.
The main adverse events were those associated with CRS and neurologic changes. Severe CRS requiring vasopressors or mechanical ventilation occurred in 5 patients (18%) overall and in 5 patients (33%) with morphologic disease before therapy. Severe CRS did not occur in any patient with minimal disease before therapy.
Grade 3 or 4 neurotoxicity occurred in 7 patients (25%) overall, in 6 patients (40%) with morphologic disease, and in 1 with minimal disease (8%) before therapy.
The investigators observed no graft-vs-host disease exacerbation, and CRS was managed with an IL-6R inhibitor, steroids, or both.
Dr Park noted that the neurologic symptoms are reversible and can occur independently of CRS.
He also pointed out that CR rates were similar regardless of different disease risk factors, and that durable responses have been achieved in patients who did not have a subsequent HSCT.
*Information in the abstract differs from that presented at the meeting.

Credit: Charles Haymond
SAN FRANCISCO—JCAR015, a chimeric antigen receptor (CAR) T-cell therapy, can produce durable responses in patients with B-cell acute lymphoblastic leukemia (ALL) who do not undergo subsequent hematopoietic stem cell transplant (HSCT), new research suggests.
JCAR015 consists of autologous T cells genetically modified to express 19-28z chimeric antigen receptor (19-28z CAR) targeting CD19.
Jae H. Park, MD, of Memorial Sloan Kettering Cancer Center in New York, presented data on JCAR015 at the 2014 ASH Annual Meeting (abstract 382).* The study is sponsored by Memorial Sloan Kettering, but funding has also been provided by Juno Therapeutics, the company developing JCAR015.
JCAR015 was tested at a dose of 1 - 3 x 106 CAR cells/kg in 33 adults with relapsed/refractory B-cell ALL. Twenty-eight patients were evaluable for toxicity, 27 for response, and 5 patients were too early in their treatment to evaluate at the time of data cutoff.
Twenty-one patients were male, and the median age was 55 (range, 23 to 74).
Thirteen patients (46%) had minimal disease (<5% blasts) immediately prior to T-cell infusion, and 15 patients (54%) had morphologic disease of 5% to 100% blasts (median 63%).
Eighteen patients (64%) had received 2 prior lines of therapy, and 5 (18%) each had 3 or more prior lines.
Eight patients (29%) underwent prior allogeneic HSCT, 9 patients (32%) were Philadelphia chromosome positive (Ph+), and 3 (11%) had the T315I mutation.
The overall complete response (CR) rate was 89%, and the minimal residual disease-negative CR rate was 88%. The median time to CR was 22.5 days (range, 9 to 33).
The investigators performed a subgroup analysis and found that 100% of the 13 patients with minimal disease before therapy achieved a CR, compared to 79% of patients with morphologic disease.
Eighty-six percent (6/7) of patients who had a prior HSCT and 90% (18/20) without a prior HSCT achieved a CR. Eighty-nine percent (8/9) of Ph+ patients achieved a CR, and 89% (16/18) of Philadelphia-negative patients (89%) achieved a CR.
At a median follow-up of 6 months (range, 1 to 38 months), 12 patients remained disease-free, including 7 patients who had more than a year of follow-up. Seven patients are disease-free without a subsequent HSCT.
Nine patients relapsed during a follow-up of 3 to 8 months, and 10 patients proceeded to HSCT. Two relapses occurred after HSCT, one in a patient who had CD19-negative blasts, and 7 relapses occurred without HSCT.
The overall survival rate at 6 months was 57%, and the median survival was 8.5 months.
For those patients who had a transplant after CAR therapy, the median survival was 10.8 months, and the survival rate at 6 months was 68%.
Dr Park pointed out that maximum T-cell expansion occurred between days 7 and 14 and correlated with the occurrence of cytokine release syndrome (CRS). The T cells persisted for 1 to 3 months following infusion.
The main adverse events were those associated with CRS and neurologic changes. Severe CRS requiring vasopressors or mechanical ventilation occurred in 5 patients (18%) overall and in 5 patients (33%) with morphologic disease before therapy. Severe CRS did not occur in any patient with minimal disease before therapy.
Grade 3 or 4 neurotoxicity occurred in 7 patients (25%) overall, in 6 patients (40%) with morphologic disease, and in 1 with minimal disease (8%) before therapy.
The investigators observed no graft-vs-host disease exacerbation, and CRS was managed with an IL-6R inhibitor, steroids, or both.
Dr Park noted that the neurologic symptoms are reversible and can occur independently of CRS.
He also pointed out that CR rates were similar regardless of different disease risk factors, and that durable responses have been achieved in patients who did not have a subsequent HSCT.
*Information in the abstract differs from that presented at the meeting.
Classic HL vulnerable to PD-1 blockade therapy
SAN FRANCISCO—Two monoclonal antibodies that block the programmed death-1 (PD-1) pathway are showing promise in early phase trials in relapsed/refractory classic Hodgkin lymphoma (cHL).
Nivolumab prompted an 87% overall response rate (ORR) in heavily pretreated patients, and pembrolizumab elicited a 66% ORR in patients who had failed prior treatment with brentuximab vedotin.
These results were presented in 2 abstracts at the 2014 ASH Annual Meeting.
The rationale for using PD-1 blockade in cHL is that these patients frequently have an alteration in chromosome 9p24.1, which leads to increased expression of the PD-1 ligands, PD-L1 and PD-L2. The ligands engage the PD-1 receptors on activated T cells, inducing T-cell exhaustion. More than 85% of cHL tumors overexpress PD-L1.
Craig H. Moskowitz, MD, who presented the data on pembrolizumab at the meeting, sees nivolumab and pembrolizumab as being very similar.
“My gut feeling is that, at the end of the day, the response rates will be very similar,” he said. “The complete response rates will be similar. I think the toxicity profiles may be slightly dissimilar, and we’ll have to see what happens when these studies are both peer-reviewed.”
Nivolumab
Philippe Armand, MD, of Dana-Farber Cancer Institute in Boston, presented data on nivolumab in cHL (abstract 289), which was an independent expansion cohort of a phase 1b study in hematologic malignancies.
The 23 cHL patients received nivolumab at 3 mg/kg on weeks 1 and 4, then every 2 weeks.
Patients were a median age of 35 years (range, 20 to 54), and about two-thirds had received 4 or more prior systemic therapies. Seventy-eight percent had prior autologous stem cell transplant, and 78% had prior treatment with brentuximab.
“These were extensively pretreated patients” Dr Armand said, “with few options available.”
Twenty patients responded, for an ORR of 87%. Four patients (17%) achieved a complete response (CR), 16 (70%) had a partial response, and 3 (13%) had stable disease.
There were no progressions. And, at 24 weeks, the progression-free survival was 86%.
There were no life-threatening adverse events (AEs), no drug-related deaths, and no drug-related grade 4 AEs. Twenty-two patients (96%) experienced an AE, 18 (78%) had a drug-related AE, 5 (22%) had a grade 3 drug-related AE, and 2 (9%) patients discontinued treatment due to a drug-related AE.
The 2 events leading to discontinuation were myelodysplastic syndromes with grade 3 thrombocytopenia and grade 3 pancreatitis. The other grade 3 drug-related AEs were lymphopenia, increased lipase, GI inflammation, pneumonitis, colitis, and stomatitis.
“Overall, nivolumab has been used in thousands of patients already on clinical trials in solid tumors,” Dr Armand said. “And, overall, this safety profile mirrors that from what we expected in solid tumors.”
“But the interesting thing about that, from our standpoint, is that there was no apparent increase in the incidence of lung toxicity, which is something we worry about for those patients because many of them had had radiation or other drugs that can cause lung injury.”
This study was recently published in NEJM. It was funded by Bristol-Myers Squibb, the company developing nivolumab, and others.
Based on results of this study, the US Food and Drug Administration (FDA) granted nivolumab breakthrough therapy designation to treat HL. The drug recently gained FDA approval to treat advanced melanoma.
Pembrolizumab
Dr Moskowitz, of Memorial Sloan Kettering Cancer Center in New York, presented data on pembrolizumab as abstract 290.*
Investigators enrolled 31 patients onto the cHL cohort of the Keynote 013 trial. Patients were a median age of 32 years (range, 20 to 67).
All patients had failed therapy with brentuximab vedotin, 69% failed prior stem cell transplant, and 28% were transplant ineligible. Patients had to have an ECOG performance status of 0 or 1 and could not have autoimmune disease or interstitial lung disease.
Patients received 10 mg/kg of pembrolizumab intravenously every 2 weeks for up to 24 months or until progression.
Twenty-nine patients were evaluable for efficacy. The ORR was 66%, with a CR rate of 21% and a partial response rate of 45%. Twenty-one percent of patients had stable disease, and 14% had progressive disease. So the clinical benefit rate was 86%.
The median time to response was 12 weeks, and the median duration of response ranged from 1 to 185 days, but the median had not yet been reached.
Nine patients (31%) discontinued therapy, 1 (3%) due to an AE, 7 (24%) due to disease progression, and 1 (3%) after achieving a CR. Twenty patients (69%) were still on therapy at the time of the presentation, and 1 patient went on to transplant.
Sixteen patients (55%) experienced 1 or more treatment-related AE of any grade. Those occurring in 2 or more patients included hypothyroidism (10%), pneumonitis (10%), constipation (7%), diarrhea (7%), nausea (7%), hypercholesterolemia (7%), hypertriglyceridemia (7%), and hematuria (7%).
Treatment-related AEs of grade 3 or higher included axillary pain (3%), hypoxia (3%), joint swelling (3%), and pneumonitis (3%). Three patients experienced 4 grade 3 or higher AEs. There were no grade 4 treatment-related AEs or treatment-related deaths.
“In my opinion,” Dr Moskowitz concluded, “these results support continued development of pembrolizumab in Hodgkin lymphoma.”
“I think that these drugs are here to stay. Where we are going to put them in the armamentarium in Hodgkin lymphoma remains to be seen.”
This study was funded by Merck Sharp & Dohme Corp., the company developing pembrolizumab. ![]()
*Information in the abstract differs from that presented at the meeting.
SAN FRANCISCO—Two monoclonal antibodies that block the programmed death-1 (PD-1) pathway are showing promise in early phase trials in relapsed/refractory classic Hodgkin lymphoma (cHL).
Nivolumab prompted an 87% overall response rate (ORR) in heavily pretreated patients, and pembrolizumab elicited a 66% ORR in patients who had failed prior treatment with brentuximab vedotin.
These results were presented in 2 abstracts at the 2014 ASH Annual Meeting.
The rationale for using PD-1 blockade in cHL is that these patients frequently have an alteration in chromosome 9p24.1, which leads to increased expression of the PD-1 ligands, PD-L1 and PD-L2. The ligands engage the PD-1 receptors on activated T cells, inducing T-cell exhaustion. More than 85% of cHL tumors overexpress PD-L1.
Craig H. Moskowitz, MD, who presented the data on pembrolizumab at the meeting, sees nivolumab and pembrolizumab as being very similar.
“My gut feeling is that, at the end of the day, the response rates will be very similar,” he said. “The complete response rates will be similar. I think the toxicity profiles may be slightly dissimilar, and we’ll have to see what happens when these studies are both peer-reviewed.”
Nivolumab
Philippe Armand, MD, of Dana-Farber Cancer Institute in Boston, presented data on nivolumab in cHL (abstract 289), which was an independent expansion cohort of a phase 1b study in hematologic malignancies.
The 23 cHL patients received nivolumab at 3 mg/kg on weeks 1 and 4, then every 2 weeks.
Patients were a median age of 35 years (range, 20 to 54), and about two-thirds had received 4 or more prior systemic therapies. Seventy-eight percent had prior autologous stem cell transplant, and 78% had prior treatment with brentuximab.
“These were extensively pretreated patients” Dr Armand said, “with few options available.”
Twenty patients responded, for an ORR of 87%. Four patients (17%) achieved a complete response (CR), 16 (70%) had a partial response, and 3 (13%) had stable disease.
There were no progressions. And, at 24 weeks, the progression-free survival was 86%.
There were no life-threatening adverse events (AEs), no drug-related deaths, and no drug-related grade 4 AEs. Twenty-two patients (96%) experienced an AE, 18 (78%) had a drug-related AE, 5 (22%) had a grade 3 drug-related AE, and 2 (9%) patients discontinued treatment due to a drug-related AE.
The 2 events leading to discontinuation were myelodysplastic syndromes with grade 3 thrombocytopenia and grade 3 pancreatitis. The other grade 3 drug-related AEs were lymphopenia, increased lipase, GI inflammation, pneumonitis, colitis, and stomatitis.
“Overall, nivolumab has been used in thousands of patients already on clinical trials in solid tumors,” Dr Armand said. “And, overall, this safety profile mirrors that from what we expected in solid tumors.”
“But the interesting thing about that, from our standpoint, is that there was no apparent increase in the incidence of lung toxicity, which is something we worry about for those patients because many of them had had radiation or other drugs that can cause lung injury.”
This study was recently published in NEJM. It was funded by Bristol-Myers Squibb, the company developing nivolumab, and others.
Based on results of this study, the US Food and Drug Administration (FDA) granted nivolumab breakthrough therapy designation to treat HL. The drug recently gained FDA approval to treat advanced melanoma.
Pembrolizumab
Dr Moskowitz, of Memorial Sloan Kettering Cancer Center in New York, presented data on pembrolizumab as abstract 290.*
Investigators enrolled 31 patients onto the cHL cohort of the Keynote 013 trial. Patients were a median age of 32 years (range, 20 to 67).
All patients had failed therapy with brentuximab vedotin, 69% failed prior stem cell transplant, and 28% were transplant ineligible. Patients had to have an ECOG performance status of 0 or 1 and could not have autoimmune disease or interstitial lung disease.
Patients received 10 mg/kg of pembrolizumab intravenously every 2 weeks for up to 24 months or until progression.
Twenty-nine patients were evaluable for efficacy. The ORR was 66%, with a CR rate of 21% and a partial response rate of 45%. Twenty-one percent of patients had stable disease, and 14% had progressive disease. So the clinical benefit rate was 86%.
The median time to response was 12 weeks, and the median duration of response ranged from 1 to 185 days, but the median had not yet been reached.
Nine patients (31%) discontinued therapy, 1 (3%) due to an AE, 7 (24%) due to disease progression, and 1 (3%) after achieving a CR. Twenty patients (69%) were still on therapy at the time of the presentation, and 1 patient went on to transplant.
Sixteen patients (55%) experienced 1 or more treatment-related AE of any grade. Those occurring in 2 or more patients included hypothyroidism (10%), pneumonitis (10%), constipation (7%), diarrhea (7%), nausea (7%), hypercholesterolemia (7%), hypertriglyceridemia (7%), and hematuria (7%).
Treatment-related AEs of grade 3 or higher included axillary pain (3%), hypoxia (3%), joint swelling (3%), and pneumonitis (3%). Three patients experienced 4 grade 3 or higher AEs. There were no grade 4 treatment-related AEs or treatment-related deaths.
“In my opinion,” Dr Moskowitz concluded, “these results support continued development of pembrolizumab in Hodgkin lymphoma.”
“I think that these drugs are here to stay. Where we are going to put them in the armamentarium in Hodgkin lymphoma remains to be seen.”
This study was funded by Merck Sharp & Dohme Corp., the company developing pembrolizumab. ![]()
*Information in the abstract differs from that presented at the meeting.
SAN FRANCISCO—Two monoclonal antibodies that block the programmed death-1 (PD-1) pathway are showing promise in early phase trials in relapsed/refractory classic Hodgkin lymphoma (cHL).
Nivolumab prompted an 87% overall response rate (ORR) in heavily pretreated patients, and pembrolizumab elicited a 66% ORR in patients who had failed prior treatment with brentuximab vedotin.
These results were presented in 2 abstracts at the 2014 ASH Annual Meeting.
The rationale for using PD-1 blockade in cHL is that these patients frequently have an alteration in chromosome 9p24.1, which leads to increased expression of the PD-1 ligands, PD-L1 and PD-L2. The ligands engage the PD-1 receptors on activated T cells, inducing T-cell exhaustion. More than 85% of cHL tumors overexpress PD-L1.
Craig H. Moskowitz, MD, who presented the data on pembrolizumab at the meeting, sees nivolumab and pembrolizumab as being very similar.
“My gut feeling is that, at the end of the day, the response rates will be very similar,” he said. “The complete response rates will be similar. I think the toxicity profiles may be slightly dissimilar, and we’ll have to see what happens when these studies are both peer-reviewed.”
Nivolumab
Philippe Armand, MD, of Dana-Farber Cancer Institute in Boston, presented data on nivolumab in cHL (abstract 289), which was an independent expansion cohort of a phase 1b study in hematologic malignancies.
The 23 cHL patients received nivolumab at 3 mg/kg on weeks 1 and 4, then every 2 weeks.
Patients were a median age of 35 years (range, 20 to 54), and about two-thirds had received 4 or more prior systemic therapies. Seventy-eight percent had prior autologous stem cell transplant, and 78% had prior treatment with brentuximab.
“These were extensively pretreated patients” Dr Armand said, “with few options available.”
Twenty patients responded, for an ORR of 87%. Four patients (17%) achieved a complete response (CR), 16 (70%) had a partial response, and 3 (13%) had stable disease.
There were no progressions. And, at 24 weeks, the progression-free survival was 86%.
There were no life-threatening adverse events (AEs), no drug-related deaths, and no drug-related grade 4 AEs. Twenty-two patients (96%) experienced an AE, 18 (78%) had a drug-related AE, 5 (22%) had a grade 3 drug-related AE, and 2 (9%) patients discontinued treatment due to a drug-related AE.
The 2 events leading to discontinuation were myelodysplastic syndromes with grade 3 thrombocytopenia and grade 3 pancreatitis. The other grade 3 drug-related AEs were lymphopenia, increased lipase, GI inflammation, pneumonitis, colitis, and stomatitis.
“Overall, nivolumab has been used in thousands of patients already on clinical trials in solid tumors,” Dr Armand said. “And, overall, this safety profile mirrors that from what we expected in solid tumors.”
“But the interesting thing about that, from our standpoint, is that there was no apparent increase in the incidence of lung toxicity, which is something we worry about for those patients because many of them had had radiation or other drugs that can cause lung injury.”
This study was recently published in NEJM. It was funded by Bristol-Myers Squibb, the company developing nivolumab, and others.
Based on results of this study, the US Food and Drug Administration (FDA) granted nivolumab breakthrough therapy designation to treat HL. The drug recently gained FDA approval to treat advanced melanoma.
Pembrolizumab
Dr Moskowitz, of Memorial Sloan Kettering Cancer Center in New York, presented data on pembrolizumab as abstract 290.*
Investigators enrolled 31 patients onto the cHL cohort of the Keynote 013 trial. Patients were a median age of 32 years (range, 20 to 67).
All patients had failed therapy with brentuximab vedotin, 69% failed prior stem cell transplant, and 28% were transplant ineligible. Patients had to have an ECOG performance status of 0 or 1 and could not have autoimmune disease or interstitial lung disease.
Patients received 10 mg/kg of pembrolizumab intravenously every 2 weeks for up to 24 months or until progression.
Twenty-nine patients were evaluable for efficacy. The ORR was 66%, with a CR rate of 21% and a partial response rate of 45%. Twenty-one percent of patients had stable disease, and 14% had progressive disease. So the clinical benefit rate was 86%.
The median time to response was 12 weeks, and the median duration of response ranged from 1 to 185 days, but the median had not yet been reached.
Nine patients (31%) discontinued therapy, 1 (3%) due to an AE, 7 (24%) due to disease progression, and 1 (3%) after achieving a CR. Twenty patients (69%) were still on therapy at the time of the presentation, and 1 patient went on to transplant.
Sixteen patients (55%) experienced 1 or more treatment-related AE of any grade. Those occurring in 2 or more patients included hypothyroidism (10%), pneumonitis (10%), constipation (7%), diarrhea (7%), nausea (7%), hypercholesterolemia (7%), hypertriglyceridemia (7%), and hematuria (7%).
Treatment-related AEs of grade 3 or higher included axillary pain (3%), hypoxia (3%), joint swelling (3%), and pneumonitis (3%). Three patients experienced 4 grade 3 or higher AEs. There were no grade 4 treatment-related AEs or treatment-related deaths.
“In my opinion,” Dr Moskowitz concluded, “these results support continued development of pembrolizumab in Hodgkin lymphoma.”
“I think that these drugs are here to stay. Where we are going to put them in the armamentarium in Hodgkin lymphoma remains to be seen.”
This study was funded by Merck Sharp & Dohme Corp., the company developing pembrolizumab. ![]()
*Information in the abstract differs from that presented at the meeting.
Brentuximab combinations highly active in Hodgkin lymphoma

Photo courtesy of ASH
SAN FRANCISCO—Two recent studies have shown combination therapy with brentuximab vedotin to be highly active in newly diagnosed patients with Hodgkin lymphoma (HL) and in relapsed or refractory patients after frontline therapy.
The first study evaluated brentuximab with ABVD or AVD and the second with bendamustine.
Objective response rates were 95% with ABVD, 96% with AVD, and 96% with bendamustine.
Both studies were presented at the 2014 ASH Annual Meeting, and both were sponsored by Seattle Genetics, Inc., the company developing brentuximab vedotin.
Brentuximab with ABVD or AVD
Standard frontline therapy with ABVD (adriamycin, bleomycin, vinblastine, and dacarbazine) or AVD (the same regimen without bleomycin) fails to cure up to 30% of patients with HL.
So investigators decided to try a new approach to increase efficacy and reduce toxicity—combining brentuximab with standard therapy.
Joseph M. Connors, MD, of the BC Cancer Agency and University of British Columbia in Vancouver, Canada, presented long-term outcomes of the brentuximab-ABVD combination as abstract 292.*
Phase 1 dose-escalation study
The key initial study of the combination determined the maximum tolerated dose of brentuximab to be 1.2 mg/kg delivered on a 2-week schedule to match the other agents in the ABVD regimen. Brentuximab was delivered for up to 6 cycles.
Of the 50 patients treated, 75% were males with an ECOG status of 0 or 1. Their median age was 32.5 years (range, 18 to 59). Approximately 80% were stage III or IV.
“We learned several key lessons from that initial study,” Dr Connors said. “The first was that when one adds brentuximab vedotin to the full-dose combination ABVD, unacceptable levels of pulmonary toxicity occurred, with 44% of the patients eventually experiencing pulmonary toxicity, typically manifest between the third and sixth cycle of treatment.”
The toxicity resolved in 9 of the 11 patients, but was fatal in 2. The median time to resolution was 2.6 weeks.
Eight patients discontinued bleomycin but were able to complete treatment with AVD and brentuximab.
“When we dropped bleomycin from the combination and shifted to AVD without bleomycin, no patients experienced pulmonary toxicity,” Dr Connors added.
Ultimately, the combination produced a response rate of 95% with ABVD and 96% with AVD.
Long-term follow-up
Investigators then assessed the durability of the response and the time distribution of any relapses.
All but 1 patient was available for follow-up. Patients were followed for a median of 45 months in the ABVD arm and 36 months in the AVD arm.
In the ABVD arm, 22 of 24 patients are living, and all 26 patients in the AVD group are alive. Altogether, there have been 5 relapses—3 in the ABVD arm (occurring at 9, 22, and 23 months) and 2 in the AVD arm (occurring at 7 and 22 months).
The 3-year failure-free survival is 79% with ABVD and 92% with AVD. And the 3-year overall survival is 92% in the ABVD arm and 100% in the AVD arm.
No deaths from HL have occurred, and all 5 relapsed patients have undergone autologous stem cell transplant. One of those has subsequently relapsed.
“So far,” Dr Connors said, “survival has been excellent.” And responses are durable.
“This has encouraged activation of the large, international trial,” Dr Connors said, comparing AVD plus brentuximab to standard ABVD in frontline treatment of HL.
Brentuximab with bendamustine
Brentuximab is also active as a single agent in relapsed/refractory HL, producing a 34% complete response (CR) rate. And the alkylating agent bendamustine produces a 33% CR rate in these patients. Furthermore, both agents have manageable safety profiles and different mechanisms of action.
Investigators therefore hypothesized that brentuximab in combination with bendamustine could induce more CRs in HL patients with relapsed or refractory disease after frontline therapy.
Ann LaCasce, MD, of Dana-Farber Cancer Institute in Boston, presented the data at ASH as abstract 293.*
Ten patients were enrolled in the phase 1 portion of the study to determine the optimal dose level of bendamustine and to assess safety and tolerability.
No dose-limiting toxicities were observed. So the investigators used bendamustine at 90 mg/m2 and brentuximab at 1.8 mg/kg. Patients received a median of 2 cycles (range, 1 to 6) of combination therapy.
Patients had the option to proceed to an autologous stem cell transplant at any time after cycle 2 and could receive brentuximab monotherapy thereafter for up to 16 total doses.
The phase 2 expansion portion enrolled 44 patients and assessed the best response, duration of response, and progression-free survival.
Results
Patients were a median age of 37 years (range, 27 to 51), and 57% were male. Ninety-eight percent were ECOG status 0 or 1, and 54% had stage III or IV disease at diagnosis.
The majority of patients had received ABVD as frontline therapy, Dr LaCasce pointed out.
The most common treatment-emergent adverse event was infusion-related reactions, accounting for 96% of the events. Dyspnea (15%), chills (13%), and flushing (13%) were the most common symptoms, and hypotension requiring vasopressor support also occurred.
Most reactions occurred within 24 hours of the cycle 2 infusion and were considered related to both agents. However, delayed hypersensitivity reactions also occurred, Dr LaCasce said, the most common being rash in 14 patients up to 22 days after infusion.
“Based on the number of infusion-related reactions after 24 patients, the protocol was amended to require mandatory corticosteroids and anthistamine premedication,” Dr LaCasce explained. “[T]his resulted in a significant decrease in the severity of the infusion-related reactions.”
The best clinical response for the 48 evaluable patients was 83% CR and 13% partial remission, for an objective response rate of 96%.
The median progression-free survival has not yet been reached, and the combination has had no negative impact on stem cell mobilization or engraftment to date.
The response rate compares very favorably to historical data, Dr LaCasce said, and the combination represents a promising salvage regimen for HL patients. ![]()
*Data in the presentation differ from the abstract.

Photo courtesy of ASH
SAN FRANCISCO—Two recent studies have shown combination therapy with brentuximab vedotin to be highly active in newly diagnosed patients with Hodgkin lymphoma (HL) and in relapsed or refractory patients after frontline therapy.
The first study evaluated brentuximab with ABVD or AVD and the second with bendamustine.
Objective response rates were 95% with ABVD, 96% with AVD, and 96% with bendamustine.
Both studies were presented at the 2014 ASH Annual Meeting, and both were sponsored by Seattle Genetics, Inc., the company developing brentuximab vedotin.
Brentuximab with ABVD or AVD
Standard frontline therapy with ABVD (adriamycin, bleomycin, vinblastine, and dacarbazine) or AVD (the same regimen without bleomycin) fails to cure up to 30% of patients with HL.
So investigators decided to try a new approach to increase efficacy and reduce toxicity—combining brentuximab with standard therapy.
Joseph M. Connors, MD, of the BC Cancer Agency and University of British Columbia in Vancouver, Canada, presented long-term outcomes of the brentuximab-ABVD combination as abstract 292.*
Phase 1 dose-escalation study
The key initial study of the combination determined the maximum tolerated dose of brentuximab to be 1.2 mg/kg delivered on a 2-week schedule to match the other agents in the ABVD regimen. Brentuximab was delivered for up to 6 cycles.
Of the 50 patients treated, 75% were males with an ECOG status of 0 or 1. Their median age was 32.5 years (range, 18 to 59). Approximately 80% were stage III or IV.
“We learned several key lessons from that initial study,” Dr Connors said. “The first was that when one adds brentuximab vedotin to the full-dose combination ABVD, unacceptable levels of pulmonary toxicity occurred, with 44% of the patients eventually experiencing pulmonary toxicity, typically manifest between the third and sixth cycle of treatment.”
The toxicity resolved in 9 of the 11 patients, but was fatal in 2. The median time to resolution was 2.6 weeks.
Eight patients discontinued bleomycin but were able to complete treatment with AVD and brentuximab.
“When we dropped bleomycin from the combination and shifted to AVD without bleomycin, no patients experienced pulmonary toxicity,” Dr Connors added.
Ultimately, the combination produced a response rate of 95% with ABVD and 96% with AVD.
Long-term follow-up
Investigators then assessed the durability of the response and the time distribution of any relapses.
All but 1 patient was available for follow-up. Patients were followed for a median of 45 months in the ABVD arm and 36 months in the AVD arm.
In the ABVD arm, 22 of 24 patients are living, and all 26 patients in the AVD group are alive. Altogether, there have been 5 relapses—3 in the ABVD arm (occurring at 9, 22, and 23 months) and 2 in the AVD arm (occurring at 7 and 22 months).
The 3-year failure-free survival is 79% with ABVD and 92% with AVD. And the 3-year overall survival is 92% in the ABVD arm and 100% in the AVD arm.
No deaths from HL have occurred, and all 5 relapsed patients have undergone autologous stem cell transplant. One of those has subsequently relapsed.
“So far,” Dr Connors said, “survival has been excellent.” And responses are durable.
“This has encouraged activation of the large, international trial,” Dr Connors said, comparing AVD plus brentuximab to standard ABVD in frontline treatment of HL.
Brentuximab with bendamustine
Brentuximab is also active as a single agent in relapsed/refractory HL, producing a 34% complete response (CR) rate. And the alkylating agent bendamustine produces a 33% CR rate in these patients. Furthermore, both agents have manageable safety profiles and different mechanisms of action.
Investigators therefore hypothesized that brentuximab in combination with bendamustine could induce more CRs in HL patients with relapsed or refractory disease after frontline therapy.
Ann LaCasce, MD, of Dana-Farber Cancer Institute in Boston, presented the data at ASH as abstract 293.*
Ten patients were enrolled in the phase 1 portion of the study to determine the optimal dose level of bendamustine and to assess safety and tolerability.
No dose-limiting toxicities were observed. So the investigators used bendamustine at 90 mg/m2 and brentuximab at 1.8 mg/kg. Patients received a median of 2 cycles (range, 1 to 6) of combination therapy.
Patients had the option to proceed to an autologous stem cell transplant at any time after cycle 2 and could receive brentuximab monotherapy thereafter for up to 16 total doses.
The phase 2 expansion portion enrolled 44 patients and assessed the best response, duration of response, and progression-free survival.
Results
Patients were a median age of 37 years (range, 27 to 51), and 57% were male. Ninety-eight percent were ECOG status 0 or 1, and 54% had stage III or IV disease at diagnosis.
The majority of patients had received ABVD as frontline therapy, Dr LaCasce pointed out.
The most common treatment-emergent adverse event was infusion-related reactions, accounting for 96% of the events. Dyspnea (15%), chills (13%), and flushing (13%) were the most common symptoms, and hypotension requiring vasopressor support also occurred.
Most reactions occurred within 24 hours of the cycle 2 infusion and were considered related to both agents. However, delayed hypersensitivity reactions also occurred, Dr LaCasce said, the most common being rash in 14 patients up to 22 days after infusion.
“Based on the number of infusion-related reactions after 24 patients, the protocol was amended to require mandatory corticosteroids and anthistamine premedication,” Dr LaCasce explained. “[T]his resulted in a significant decrease in the severity of the infusion-related reactions.”
The best clinical response for the 48 evaluable patients was 83% CR and 13% partial remission, for an objective response rate of 96%.
The median progression-free survival has not yet been reached, and the combination has had no negative impact on stem cell mobilization or engraftment to date.
The response rate compares very favorably to historical data, Dr LaCasce said, and the combination represents a promising salvage regimen for HL patients. ![]()
*Data in the presentation differ from the abstract.

Photo courtesy of ASH
SAN FRANCISCO—Two recent studies have shown combination therapy with brentuximab vedotin to be highly active in newly diagnosed patients with Hodgkin lymphoma (HL) and in relapsed or refractory patients after frontline therapy.
The first study evaluated brentuximab with ABVD or AVD and the second with bendamustine.
Objective response rates were 95% with ABVD, 96% with AVD, and 96% with bendamustine.
Both studies were presented at the 2014 ASH Annual Meeting, and both were sponsored by Seattle Genetics, Inc., the company developing brentuximab vedotin.
Brentuximab with ABVD or AVD
Standard frontline therapy with ABVD (adriamycin, bleomycin, vinblastine, and dacarbazine) or AVD (the same regimen without bleomycin) fails to cure up to 30% of patients with HL.
So investigators decided to try a new approach to increase efficacy and reduce toxicity—combining brentuximab with standard therapy.
Joseph M. Connors, MD, of the BC Cancer Agency and University of British Columbia in Vancouver, Canada, presented long-term outcomes of the brentuximab-ABVD combination as abstract 292.*
Phase 1 dose-escalation study
The key initial study of the combination determined the maximum tolerated dose of brentuximab to be 1.2 mg/kg delivered on a 2-week schedule to match the other agents in the ABVD regimen. Brentuximab was delivered for up to 6 cycles.
Of the 50 patients treated, 75% were males with an ECOG status of 0 or 1. Their median age was 32.5 years (range, 18 to 59). Approximately 80% were stage III or IV.
“We learned several key lessons from that initial study,” Dr Connors said. “The first was that when one adds brentuximab vedotin to the full-dose combination ABVD, unacceptable levels of pulmonary toxicity occurred, with 44% of the patients eventually experiencing pulmonary toxicity, typically manifest between the third and sixth cycle of treatment.”
The toxicity resolved in 9 of the 11 patients, but was fatal in 2. The median time to resolution was 2.6 weeks.
Eight patients discontinued bleomycin but were able to complete treatment with AVD and brentuximab.
“When we dropped bleomycin from the combination and shifted to AVD without bleomycin, no patients experienced pulmonary toxicity,” Dr Connors added.
Ultimately, the combination produced a response rate of 95% with ABVD and 96% with AVD.
Long-term follow-up
Investigators then assessed the durability of the response and the time distribution of any relapses.
All but 1 patient was available for follow-up. Patients were followed for a median of 45 months in the ABVD arm and 36 months in the AVD arm.
In the ABVD arm, 22 of 24 patients are living, and all 26 patients in the AVD group are alive. Altogether, there have been 5 relapses—3 in the ABVD arm (occurring at 9, 22, and 23 months) and 2 in the AVD arm (occurring at 7 and 22 months).
The 3-year failure-free survival is 79% with ABVD and 92% with AVD. And the 3-year overall survival is 92% in the ABVD arm and 100% in the AVD arm.
No deaths from HL have occurred, and all 5 relapsed patients have undergone autologous stem cell transplant. One of those has subsequently relapsed.
“So far,” Dr Connors said, “survival has been excellent.” And responses are durable.
“This has encouraged activation of the large, international trial,” Dr Connors said, comparing AVD plus brentuximab to standard ABVD in frontline treatment of HL.
Brentuximab with bendamustine
Brentuximab is also active as a single agent in relapsed/refractory HL, producing a 34% complete response (CR) rate. And the alkylating agent bendamustine produces a 33% CR rate in these patients. Furthermore, both agents have manageable safety profiles and different mechanisms of action.
Investigators therefore hypothesized that brentuximab in combination with bendamustine could induce more CRs in HL patients with relapsed or refractory disease after frontline therapy.
Ann LaCasce, MD, of Dana-Farber Cancer Institute in Boston, presented the data at ASH as abstract 293.*
Ten patients were enrolled in the phase 1 portion of the study to determine the optimal dose level of bendamustine and to assess safety and tolerability.
No dose-limiting toxicities were observed. So the investigators used bendamustine at 90 mg/m2 and brentuximab at 1.8 mg/kg. Patients received a median of 2 cycles (range, 1 to 6) of combination therapy.
Patients had the option to proceed to an autologous stem cell transplant at any time after cycle 2 and could receive brentuximab monotherapy thereafter for up to 16 total doses.
The phase 2 expansion portion enrolled 44 patients and assessed the best response, duration of response, and progression-free survival.
Results
Patients were a median age of 37 years (range, 27 to 51), and 57% were male. Ninety-eight percent were ECOG status 0 or 1, and 54% had stage III or IV disease at diagnosis.
The majority of patients had received ABVD as frontline therapy, Dr LaCasce pointed out.
The most common treatment-emergent adverse event was infusion-related reactions, accounting for 96% of the events. Dyspnea (15%), chills (13%), and flushing (13%) were the most common symptoms, and hypotension requiring vasopressor support also occurred.
Most reactions occurred within 24 hours of the cycle 2 infusion and were considered related to both agents. However, delayed hypersensitivity reactions also occurred, Dr LaCasce said, the most common being rash in 14 patients up to 22 days after infusion.
“Based on the number of infusion-related reactions after 24 patients, the protocol was amended to require mandatory corticosteroids and anthistamine premedication,” Dr LaCasce explained. “[T]his resulted in a significant decrease in the severity of the infusion-related reactions.”
The best clinical response for the 48 evaluable patients was 83% CR and 13% partial remission, for an objective response rate of 96%.
The median progression-free survival has not yet been reached, and the combination has had no negative impact on stem cell mobilization or engraftment to date.
The response rate compares very favorably to historical data, Dr LaCasce said, and the combination represents a promising salvage regimen for HL patients. ![]()
*Data in the presentation differ from the abstract.

