User login
A Bariatric Surgery Primer for Orthopedic Surgeons
An estimated 220,000 bariatric surgeries are performed annually in the United States and Canada, and 344,221 procedures worldwide.1 Not only are orthopedic surgeons seeing more patients who have had bariatric surgery, they are also referring morbidly obese patients to bariatric surgeons before elective procedures.2 Patients with body mass index (BMI) over 40 kg/m2 are candidates for surgical treatment of obesity. Comorbid conditions directly related to obesity, including diabetes, respiratory insufficiency, and pseudotumor cerebri, decrease the BMI of eligibility to 35 kg/m2. Other considerations are failure of nonsurgical weight-loss methods, such as dietary programs for weight reduction, behavioral modification programs, and pharmacotherapy. Patients’ psychological stability is extremely important given the rigorous dietary changes required after surgery.3 Although weight-loss surgery can eliminate many of the complications of obesity, bariatric patients even with weight loss have increased operative and postoperative risks, likely because of alterations in nutrient absorption. Knowledge of the pathophysiology associated with bariatric surgery can assist orthopedic surgeons in optimizing medical and surgical management of patients’ musculoskeletal issues.
Bariatric Surgery
Surgically induced weight loss works by reducing quantity of food consumed and absorption of calories. Jejunoileal bypass, one of the first procedures used, significantly decreased the absorptive area for nutrients, which led to complications such as diarrhea, cirrhosis, and nephrolithiasis.4 This surgery is no longer performed, and current procedures try to minimize the risks of malabsorption.5
The 2 types of bariatric surgeries now available in the United States are gastroplasty and gastric bypass, both of which are performed laparoscopically.6 Gastroplasties are purely restrictive procedures, which reduce stomach volume. In gastric banding, the most common gastroplasty, a silicone band is placed around the proximal stomach to create a 15-mL pouch in the cardia. Sleeve gastrectomy also reduces stomach volume, to about 25%, by stapling along the greater curvature. In both procedures, consumed calories are restricted, but the gastrointestinal tract is left in continuity, and essential nutrients are properly absorbed.7 However, failure rates are higher, and weight loss more variable, than with gastric bypass procedures.8
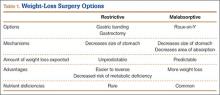
Gastric bypass uses both restriction and malabsorption to increase weight loss.7 A gastric pouch (15-30 mL) is created by stapling across the cardia of the stomach. The jejunum is then divided, and the distal portion of the divided jejunum anastomosed to the small proximal stomach pouch. This creates the roux limb where food passes. The duodenum is excluded, and the proximal portion of the jejunum is attached to the roux limb to provide a conduit for biliary and pancreatic digestive secretions. Weight loss is caused by both reduction in stomach size and malabsorption of calories owing to the diversion of digestive enzymes and the decrease in absorptive surface area. Only 28% of ingested fat and 57% of ingested protein are absorbed9 (Table 1).
Metabolic Consequences
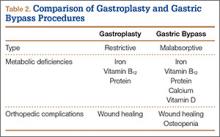
Nutrient deficiencies are seen more often in the malabsorptive procedures; however, patients with restrictive procedures may have poor eating habits and are therefore also at risk.10 In fact, many patients have nutritional deficiencies predating their bariatric surgery, as obesity creates a chronic inflammatory state that leads to anemia of chronic disease. Schweiger and colleagues11 assessed the nutritional status of bariatric surgery candidates and noted a high incidence of iron and folic acid deficiencies with corresponding anemia. They concluded these deficiencies stemmed from calorie-dense diets high in carbohydrates and fats. Although patients may improve their diet after surgery with concomitant nutritional counseling, deficiencies in iron, calcium, vitamin B12, folate, and vitamin D are common12 (Table 2).
Iron deficiency continues after bariatric surgery because dietary iron must be converted to its absorbable form by hydrochloric acid secreted from the stomach. As stomach volume is reduced, there is a corresponding decrease in acid secretion. The result is that iron deficiency occurs in both restrictive and malabsorptive procedures.13 Moreover, with the diversion from the duodenum and the proximal jejunum in bypass surgery, the main areas of absorption are excluded.10 Patients may require intravenous therapy for iron-deficiency anemia—or oral supplementation combined with ascorbic acid to increase stomach acidity.
As calcium is absorbed mainly in the duodenum and the jejunum, patients who undergo malabsorptive procedures can absorb only 20% of the amount ingested.14 Restrictive procedures do not have the same effect on calcium absorption; however, patients may have reduced dietary lactose intake and be at risk for deficiency.
A study by Ducloux and colleagues15 found that 96% of bariatric surgery patients had vitamin D deficiency before the procedure. After malabsorptive procedures, the decrease in bile salts leads to an inability to break down fat-soluble vitamins and to uncoordinated mixing of food and bile secretions.16 Restrictive procedures do not carry this risk, though many patients still require supplementation because of their underlying deficiency.
The decrease in stomach size causes a decrease in intrinsic factor from parietal cells, with subsequent inability to appropriately transport vitamin B12. Exclusion of the duodenum also eliminates the site of absorption; therefore, B12 should be replaced orally.11 Megaloblastic anemia is a rarely reported sequela.17,18 Folate deficiency is less common because it can take place in the entire intestine after surgery, even though absorption occurs primarily in the proximal portion of the small intestine.10
Protein deficiency can result in loss of muscle mass and subsequent muscle weakness, edema, and anomalies of the skin, mucosa, and nails.12 It is seen after both types of procedures because of decreased dietary intake from intolerance. Malabsorptive procedures also decrease pepsinogen secretion and reduce the intestinal absorption surface.
Considerations for Orthopedic Surgeons
Wound Healing
Much of our knowledge of the effects of bariatric surgery on skin and wound healing has been gleaned from samples obtained from patients during abdominoplasty or other body-contouring procedures. These samples have all shown a decrease in hydroxyproline, the major constituent of collagen and the main factor in determining the tensile strength of a wound.19 D’Ettorre and colleagues20 performed biopsies of abdominal skin before and after biliopancreatic diversion and noted that tissue proteins, including hydroxyproline, were significantly reduced. Histologic examination revealed disorganized dermal elastic and collagen fibers. In addition, all patients involved in the study had wound-healing problems, with delayed healing of 25 days, compared with 12 days in nonbariatric patients. Deficiencies in vitamins B12, D, and E, as well as folate and total tissue protein, were implicated as causative factors.
Effects on Bone
Malabsorptive procedures decrease bone mineral density (BMD) through their effects on calcium and vitamin D. BMD is also decreased because these procedures lower levels of plasma leptin and ghrelin, increase adiponectin, and reduce estrogen in women.21 The BMD decline correlates with amount of weight lost.22 This complication is not seen in restrictive procedures, even though patients may have decreased calcium and vitamin D levels.23 The exact effect on BMD and on subsequent risk for osteopenia and osteoporosis is difficult to quantify, as obese patients have higher BMD than age-matched controls do, because of increased mechanical loading. In a prospective study, Vilarrasa and colleagues24 found a 10.9% decrease in femoral neck BMD in women 1 year after Roux-en-Y with 34% weight loss, despite supplementation with 800 IU of vitamin D and 1200 mg of calcium daily.
Fracture Healing
Although BMD is decreased in patients after gastric bypass surgery, there has been only 1 recorded case of fracture nonunion after bariatric surgery—involving a distal radius fracture in a patient who had undergone jejunoileal bypass surgery.25 Hypovitaminosis has a detrimental effect on bone repair and BMD, increasing the risk for fracture from minor trauma; however, delayed union and nonunion have not been reported as consequences.26
Pharmacology
Both restrictive and malabsorptive procedures decrease drug bioavailabilty from tablet preparations by shortening the surface area available for absorption and diminishing stomach acidity.27 These consequences pose a problem particularly for extended-release formulations, as these formulations are not given enough time to dissolve and reach therapeutic concentrations.28 Also affected is warfarin, which requires a larger dose to maintain therapeutic international normalized ratio. Antibiotics may have reduced bioavailability because of decreased transit time. Therefore, liquid preparations are preferred, as they need not be dissolved.
As there is no reported change in intravenous bioavailability with preoperative and postoperative antimicrobial prophylaxis, this is the preferred administration method.29 However, obese patients in general may have altered pharmacokinetics, including increased glomerular filtration rate, and in most cases they should be treated with higher levels of antibiotics.30
Nonsteroidal anti-inflammatory drugs (NSAIDs) should be avoided in all patients. The acidic composition of NSAIDs causes direct injury to the gastric pouch. NSAIDs also injure the gastrointestinal lining by inhibiting prostaglandin synthesis, which thins the mucosa. In turn, erosions and ulcers may form in the epithelial layer.31 Acetaminophen or a centrally acting agent (eg, tramadol) is recommended instead. Aspirin has a chemical structure similar to that of NSAIDs and should not be used either. Alendronate causes esophageal ulceration; however, no such complication has been reported with teriparatide32 (Table 3).
Preoperative Evaluation
As already discussed, patients who undergo weight-loss surgery are at higher risk for wound-healing complications because of nutritional deficiencies. Total protein, albumin, and prealbumin levels and total lymphocyte count should be used to identify protein deficiency, which can decrease the likelihood of organized collagen formation. Huang and colleagues33 noted a statistically significant increase in complications after total knee arthroplasty (TKA) in patients with a prealbumin level under 3.5 mg/dL or a transferrin level under 200 mg/dL. Rates of prosthetic joint infection and development of hematoma or seroma requiring operative management were much higher, as were rates of postoperative neurovascular, renal, and cardiovascular complications.
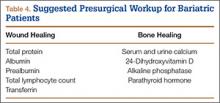
Serum levels of vitamin A, folate, vitamin B12, and vitamin C should also be ordered, as many patients are deficient. Transferrin levels should be checked before surgery, as iron-deficiency anemia is common. Naghshineh and colleagues34 noted an anecdotal decrease in wound-healing complications in body-contouring surgery after correction of subclinical and clinical deficiencies in protein, arginine, glutamine, vitamin A, vitamin B12, vitamin C, folate, thiamine, iron, zinc, and selenium. Zinc deficiency was similarly implicated in wound-healing complications by Zorrilla and colleagues,35,36 who found a statistically significant delay in wound healing in patients with serum zinc levels under 95 mg/dL after total hip arthroplasty (THA)35 and hip hemiarthroplasty.36 To facilitate bone healing, physicians should give patients a thorough workup of levels of serum and urine calcium, 24-hydroxyvitamin D, and alkaline phosphatase. Osteomalacia typically presents with high alkaline phosphatase levels37 and secondary hyperparathyroidism. Therefore, physicians should monitor for these conditions. Although nonunion and aseptic loosening have not been reported as consequences of bariatric surgery, bone health should nevertheless be optimized when possible (Table 4).
Elective Orthopedic Surgery
Little is known about the true effect of weight-loss surgery on subsequent orthopedic procedures. Few investigators have explored the effect of surgery on arthrodesis, and the only recommendation for orthopedic surgeons is to be prepared for poor bone healing and the possibility of nonunion.38 Hidalgo and colleagues39 studied laparoscopic sleeve gastrectomy performed a minimum of 6 months before another elective surgery. Two patients had lumbar laminectomies, 2 had lumbar discectomies, 1 had a cervical discectomy, and 1 had a rotator cuff repair. By most recent follow-up, there were no complications of any of the orthopedic procedures, and all patients had healed.
There is no recommended amount of time between bariatric surgery and elective orthopedic surgery. Maximum weight loss and stabilization are typically achieved 2 years after surgery.40 However, elective orthopedic surgery has been performed as early as 6 months after bariatric surgery. Inacio and colleagues41 studied 3 groups of patients who underwent total joint arthroplasty (TJA): those who had it less than 2 years after bariatric surgery, those who had it more than 2 years after bariatric surgery, and those who were obese but did not have bariatric surgery. Complications of TJA occurred within the first year in 2.9% of the patients who had it more than 2 years after bariatric surgery, in 5.9% of the patients who had it less than 2 years after bariatric surgery, and in 4.1% of the patients who did not undergo bariatric surgery. Similarly, Severson and colleagues2 evaluated intraoperative and postoperative complications of TKA in 3 groups of obese patients: those who had TKA before bariatric surgery, those who had TKA less than 2 years after bariatric surgery, and those who had TKA more than 2 years after bariatric surgery. Gastroplasty and bypass patients were included. BMI was statistically significantly higher in the preoperative group than in the other 2 groups, though mean BMI for all groups was above 35 kg/m2. Operative time and tourniquet time were reduced in patients who had TKA more than 2 years after bariatric surgery, but there was no significant difference in anesthesia time. There was also no difference in 90-day complication rates between patients who had TKA before bariatric surgery and those who had it afterward. Severson and colleagues2 recommended communicating the risks to all obese patients, whether they undergo weight-loss surgery or not.
Arthroplasty
Obese patients have a higher rate of complications after arthroplasty—hence the referrals to bariatric surgeons. Bariatric surgery and its associated weight loss might improve joint pain and delay the need for arthroplasty in some cases.42 Obese people are prone to joint degeneration from the excess weight, and from altered gait patterns (eg, exaggerated step width, slower walking speed, increased time in double-limb stance).43 Gait changes are reversible after weight loss.44 Hooper and colleagues45 found a 37% decrease in lower extremity complaints after surgical weight loss, even though mean BMI at final follow-up was still in the obese range.
Obesity itself is a risk factor for ligamentous instability, but it is unclear whether the risk is mitigated by bariatric surgery. Disruption of the anterior fibers of the medial collateral ligament is more common in obese patients, as are complications involving the extensor mechanism (eg, patellofemoral dislocation). As a result, slower postoperative rehabilitation is recommended.46 Although there is no recorded link between bariatric surgery and the development of ligamentous laxity, surgeons should be aware of the potential for medial collateral ligament avulsion in obese and formerly obese patients and have appropriate implants available.
Kulkarni and colleagues47 compared the rates of hip and knee arthroplasty complications in patients who were obese before bariatric surgery and patients who were still obese after bariatric surgery. Gastroplasty and bypass patients were included. Data on superficial wound infections were excluded; however, the bariatric surgery group’s deep wound infection rate was 3.5 times lower, and its 30-day readmission rate was 7 times lower. There was no difference in dislocation and hip revision rates at 1 year. Although 1 patient in the bariatric surgery group died of an unknown cause 9 days after surgery, Kulkarni and colleagues47 concluded it is safer to operate on obese patients after versus before bariatric surgery. However, their study did not include mean BMI, so no conclusion can be drawn about the risk of operating on patients who were still obese after bariatric surgery.
Studies of weight loss in primary TJA patients have had conflicting findings.48 Trofa and colleagues49 reported that 15 patients who underwent arthroplasty a mean of 42.4 months after bariatric surgery lost 27.9% more of their original BMI compared with patients who underwent bariatric surgery but not arthroplasty. This relationship between arthroplasty and weight loss was strongest in patients who underwent knee arthroplasty, with an average of 43.9% more BMI lost compared to patients who did not undergo TKA. There was no significant change in BMI in patients who underwent THA and bariatric surgery compared with patients who underwent bariatric surgery but not THA.
Parvizi and colleagues50 assessed the results of 20 arthroplasties (8 THAs, 12 TKAs) performed in 14 patients a mean of 23 months after bariatric surgery (2 gastroplasties, 12 bypass surgeries). Mean BMI was 29 kg/m2. At final follow-up, 1 patient required revision THA for aseptic loosening, but all the others showed no evidence of radiographic loosening or wear. One patient had a superficial wound infection, and 1 had a deep wound infection. Parvizi and colleagues50 reported that arthroplasty after bariatric surgery is a viable option and is preferable to operating on morbidly obese patients.
Summary
Orthopedic surgeons are increasingly performing elective hip and knee arthroplasties on patients who have undergone bariatric surgery. Although bariatric surgery may alleviate some of the complications associated with surgery on morbidly obese patients, it should be approached with caution. Studies have shown that bariatric surgery patients are at increased risk for wound-healing and other complications, often caused by unrecognized preoperative nutrient deficiencies. In addition, patients are often unable to tolerate commonly used medications. The exact timing of bariatric surgery relative to elective orthopedic procedures is unclear. Surgeons should perform a preoperative evaluation based on type of bariatric surgery in order to reduce the likelihood of adverse events. Such preemptive therapy may improve the short- and long-term results of major reconstructive surgery. Further research is needed to determine the true effect of bariatric surgery on orthopedic procedures.
1. Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19(12):1605-1611.
2. Severson EP, Singh JA, Browne JA, Trousdale RT, Sarr MG, Lewallen DG. Total knee arthroplasty in morbidly obese patients treated with bariatric surgery. J Arthroplasty. 2012;27(9):1696-1700.
3. Mechanick JI, Kushner RF, Sugerman HJ, et al. American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient [published correction appears in Endocr Pract. 2009;15(7):768]. Endocr Pract. 2008;14(suppl 1):1-83.
4. Hocking MP, Duerson MC, O’Leary JP, Woodward ER. Jejunoilial bypass for morbid obesity. Late follow-up in 100 cases. N Engl J Med. 1983;308(17):995-999.
5. DeMaria EJ. Morbid obesity. In: Mulholland MW, Lillemoe KD, Doherty GM, et al, eds. Greenfield’s Surgery: Scientific Principles & Practice. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:736-743.
6. O’Brien PE. Bariatric surgery: mechanisms, indications and outcomes. J Gastroenterol Hepatol. 2010;25(8):1358-1365.
7. Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724-1737.
8. DeMaria EJ, Sugerman HJ, Meador JG, et al. High failure rate after laparoscopic adjustable silicone gastric banding for treatment of morbid obesity. Ann Surg. 2001;233(6):809-818.
9. Slater GH, Ren CJ, Siegel N, et al. Serum fat-soluble vitamin deficiency and abnormal calcium metabolism after malabsorptive bariatric surgery. J Gastrointest Surg. 2004;8(1):48-55.
10. Alvarez-Leite JI. Nutrient deficiencies secondary to bariatric surgery. Curr Opin Clin Nutr Metab Care. 2004;7(5):569-575.
11. Schweiger C, Weiss R, Berry E, Keidar A. Nutritional deficiencies in bariatric surgery candidates. Obes Surg. 2010;20(2):193-197.
12. Poitou Bernert C, Ciangura C, Coupaye M, Czernichow S, Bouillot JL, Basdevant A. Nutritional deficiency after gastric bypass: diagnosis, prevention and treatment. Diabetes Metab. 2007;33(1):13-24.
13. Gehrer S, Kern B, Peters T, Christoffel-Courtin C, Peterli R. Fewer nutrient deficiencies after laparoscopic sleeve gastrectomy (LSG) than after laparoscopic Roux-Y-gastric bypass (LRYGB)—a prospective study. Obes Surg. 2010;20(4):447-453.
14. Goode LR, Brolin RE, Chowdhury HA, Shapses SA. Bone and gastric bypass surgery: effects of dietary calcium and vitamin D. Obes Res. 2004;12(1):40-47.
15. Ducloux R, Nobécourt E, Chevallier JM, Ducloux H, Elian N, Altman JJ. Vitamin D deficiency before bariatric surgery: should supplement intake be routinely prescribed? Obes Surg. 2011;21(5):556-560.
16. Wang A, Powell A. The effects of obesity surgery on bone metabolism: what orthopedic surgeons need to know. Am J Orthop. 2009;38(2):77-79.
17. Baghdasarian KL. Gastric bypass and megaloblastic anemia. J Am Diet Assoc. 1982;80(4):368-371.
18. Crowley LV, Olson RW. Megaloblastic anemia after gastric bypass for obesity. Am J Gastroenterol. 1983;78(7):406-410.
19. Sorg H, Schulz T, Krueger C, Vollmar B. Consequences of surgical stress on the kinetics of skin wound healing: partial hepatectomy delays and functionally alters dermal repair. Wound Repair Regen. 2009;17(3):367-377.
20. D’Ettorre M, Gniuli D, Iaconelli A, Massi G, Mingrone G, Bracaglia R. Wound healing process in post-bariatric patients: an experimental evaluation. Obes Surg. 2010;20(11):1552-1558.
21. Carrasco F, Ruz M, Rojas P, et al. Changes in bone mineral density, body composition and adiponectin levels in morbidly obese patients after bariatric surgery. Obes Surg. 2009;19(1);41-46.
22. Fleischer J, Stein EM, Bessler M, et al. The decline in hip bone density after gastric bypass surgery is associated with extent of weight loss. J Clin Endocrinol Metab. 2008;93(10):3735-3740.
23. von Mach MA, Stoeckli R, Bilz S, Kraenzlin M, Langer I, Keller U. Changes in bone mineral content after surgical treatment of morbid obesity. Metabolism. 2004;53(7):918-921.
24. Vilarrasa N, Gómez JM, Elio I, et al. Evaluation of bone disease in morbidly obese women after gastric bypass and risk factors implicated in bone loss. Obes Surg. 2009;19(7):860-866.
25. Hey H, Lund B, Sørensen OH, Lund B. Delayed fracture healing following jejunoileal bypass surgery for obesity. Calcif Tissue Int. 1982;34(1):13-15.
26. Borrelli J Jr, Pape C, Hak D, et al. Physiological challenges of bone repair. J Orthop Trauma. 2012;26(12):708-711.
27. Sardo P, Walker JH. Bariatric surgery: impact on medication management. Hosp Pharm. 2008;43(2):113-120.
28. Lizer MH, Papageorgeon H, Glembot TM. Nutritional and pharmacologic challenges in the bariatric surgery patient. Obes Surg. 2010;20(12):1654-1659.
29. Chopra T, Zhao JJ, Alangaden G, Wood MH, Kaye KS. Preventing surgical site infections after bariatric surgery: value of perioperative antibiotic regimens. Expert Rev Pharmacoecon Outcomes Res. 2010;10(3):317-328.
30. Payne KD, Hall RG 2nd. Dosing of antibacterial agents in obese adults: does one size fit all? Expert Rev Anti Infect Ther. 2014;12(7):829-854.
31. Sasse KC, Ganser J, Kozar M, et al. Seven cases of gastric perforation in Roux-en-Y gastric bypass patients: what lessons can we learn? Obes Surg. 2008;18(5):530-534.
32. Miller AD, Smith KM. Medication use in bariatric surgery patients: what orthopedists need to know. Orthopedics. 2006;29(2):121-123.
33. Huang R, Greenky M, Kerr GJ, Austin MS, Parvizi J. The effect of malnutrition on patients undergoing elective joint arthroplasty. J Arthroplasty. 2013;28(8 suppl):21-24.
34. Naghshineh N, O’Brien Coon D, McTigue K, Courcoulas AP, Fernstrom M, Rubin JP. Nutritional assessment of bariatric surgery patients presenting for plastic surgery: a prospective analysis. Plast Reconstr Surg. 2010;126(2):602-610.
35. Zorrilla P, Gómez LA, Salido JA, Silva A, López-Alonso A. Low serum zinc level as a predictive factor of delayed wound healing in total hip replacement. Wound Repair Regen. 2006;14(2):119-122.
36. Zorrilla P, Salido JA, López-Alonso A, Silva A. Serum zinc as a prognostic tool for wound healing in hip hemiarthroplasty. Clin Orthop Relat Res. 2004;(420):304-308.
37. Williams SE, Cooper K, Richmond B, Schauer P. Perioperative management of bariatric surgery patients: focus on metabolic bone disease. Cleve Clin J Med. 2008;75(5):333-349.
38. Kini S, Kannan U. Effect of bariatric surgery on future general surgical procedures. J Minim Access Surg. 2011;7(2):126-131.
39. Hidalgo JE, Roy M, Ramirez A, Szomstein S, Rosenthal RJ. Laparoscopic sleeve gastrectomy: a first step for rapid weight loss in morbidly obese patients requiring a second non-bariatric procedure. Obes Surg. 2012;22(4):555-559.
40. O’Brien PE, McPhail T, Chaston TB, Dixon JB. Systematic review of medium-term weight loss after bariatric operations. Obes Surg. 2006;16(8):1032-1040.
41. Inacio MC, Paxton EW, Fisher D, Li RA, Barber TC, Singh JA. Bariatric surgery prior to total joint arthroplasty may not provide dramatic improvements in post-arthroplasty surgical outcomes. J Arthroplasty. 2014;29(7):1359-1364.
42. Gill RS, Al‐Adra DP, Shi X, Sharma AM, Birch DW, Karmali S. The benefits of bariatric surgery in obese patients with hip and knee osteoarthritis: a systematic review. Obes Rev. 2011;12(12):1083-1089.
43. Vartiainen P, Bragge T, Lyytinen T, Hakkarainen M, Karjalainen PA, Arokoski JP. Kinematic and kinetic changes in obese gait in bariatric surgery–induced weight loss. J Biomech. 2012;45(10):1769-1774.
44. Vincent HK, Ben-David K, Conrad BP, Lamb KM, Seay AN, Vincent KR. Rapid changes in gait, musculoskeletal pain, and quality of life after bariatric surgery. Surg Obes Relat Dis. 2012;8(3):346-354.
45. Hooper MM, Stellato TA, Hallowell PT, Seitz BA, Moskowitz RW. Musculoskeletal findings in obese subjects before and after weight loss following bariatric surgery. Int J Obes. 2007;31(1):114-120.
46. Booth RE Jr. Total knee arthroplasty in the obese patient: tips and quips. J Arthroplasty. 2002;17(4 suppl 1):69-70.
47. Kulkarni A, Jameson SS, James P, Woodcock S, Muller S, Reed MR. Does bariatric surgery prior to lower limb joint replacement reduce complications? Surgeon. 2011;9(1):18-21.
48. Inacio MC, Silverstein DK, Raman R, et al. Weight patterns before and after total joint arthroplasty and characteristics associated with weight change. Perm J. 2014;18(1):25-31.
49. Trofa D, Smith EL, Shah V, Shikora S. Total weight loss associated with increased physical activity after bariatric surgery may increase the need for total joint arthroplasty. Surg Obes Relat Dis. 2014;10(2):335-339.
50. Parvizi J, Trousdale RT, Sarr MG. Total joint arthroplasty in patients surgically treated for morbid obesity. J Arthroplasty. 2000;15(8):1003-1008.
An estimated 220,000 bariatric surgeries are performed annually in the United States and Canada, and 344,221 procedures worldwide.1 Not only are orthopedic surgeons seeing more patients who have had bariatric surgery, they are also referring morbidly obese patients to bariatric surgeons before elective procedures.2 Patients with body mass index (BMI) over 40 kg/m2 are candidates for surgical treatment of obesity. Comorbid conditions directly related to obesity, including diabetes, respiratory insufficiency, and pseudotumor cerebri, decrease the BMI of eligibility to 35 kg/m2. Other considerations are failure of nonsurgical weight-loss methods, such as dietary programs for weight reduction, behavioral modification programs, and pharmacotherapy. Patients’ psychological stability is extremely important given the rigorous dietary changes required after surgery.3 Although weight-loss surgery can eliminate many of the complications of obesity, bariatric patients even with weight loss have increased operative and postoperative risks, likely because of alterations in nutrient absorption. Knowledge of the pathophysiology associated with bariatric surgery can assist orthopedic surgeons in optimizing medical and surgical management of patients’ musculoskeletal issues.
Bariatric Surgery
Surgically induced weight loss works by reducing quantity of food consumed and absorption of calories. Jejunoileal bypass, one of the first procedures used, significantly decreased the absorptive area for nutrients, which led to complications such as diarrhea, cirrhosis, and nephrolithiasis.4 This surgery is no longer performed, and current procedures try to minimize the risks of malabsorption.5
The 2 types of bariatric surgeries now available in the United States are gastroplasty and gastric bypass, both of which are performed laparoscopically.6 Gastroplasties are purely restrictive procedures, which reduce stomach volume. In gastric banding, the most common gastroplasty, a silicone band is placed around the proximal stomach to create a 15-mL pouch in the cardia. Sleeve gastrectomy also reduces stomach volume, to about 25%, by stapling along the greater curvature. In both procedures, consumed calories are restricted, but the gastrointestinal tract is left in continuity, and essential nutrients are properly absorbed.7 However, failure rates are higher, and weight loss more variable, than with gastric bypass procedures.8
Gastric bypass uses both restriction and malabsorption to increase weight loss.7 A gastric pouch (15-30 mL) is created by stapling across the cardia of the stomach. The jejunum is then divided, and the distal portion of the divided jejunum anastomosed to the small proximal stomach pouch. This creates the roux limb where food passes. The duodenum is excluded, and the proximal portion of the jejunum is attached to the roux limb to provide a conduit for biliary and pancreatic digestive secretions. Weight loss is caused by both reduction in stomach size and malabsorption of calories owing to the diversion of digestive enzymes and the decrease in absorptive surface area. Only 28% of ingested fat and 57% of ingested protein are absorbed9 (Table 1).
Metabolic Consequences
Nutrient deficiencies are seen more often in the malabsorptive procedures; however, patients with restrictive procedures may have poor eating habits and are therefore also at risk.10 In fact, many patients have nutritional deficiencies predating their bariatric surgery, as obesity creates a chronic inflammatory state that leads to anemia of chronic disease. Schweiger and colleagues11 assessed the nutritional status of bariatric surgery candidates and noted a high incidence of iron and folic acid deficiencies with corresponding anemia. They concluded these deficiencies stemmed from calorie-dense diets high in carbohydrates and fats. Although patients may improve their diet after surgery with concomitant nutritional counseling, deficiencies in iron, calcium, vitamin B12, folate, and vitamin D are common12 (Table 2).
Iron deficiency continues after bariatric surgery because dietary iron must be converted to its absorbable form by hydrochloric acid secreted from the stomach. As stomach volume is reduced, there is a corresponding decrease in acid secretion. The result is that iron deficiency occurs in both restrictive and malabsorptive procedures.13 Moreover, with the diversion from the duodenum and the proximal jejunum in bypass surgery, the main areas of absorption are excluded.10 Patients may require intravenous therapy for iron-deficiency anemia—or oral supplementation combined with ascorbic acid to increase stomach acidity.
As calcium is absorbed mainly in the duodenum and the jejunum, patients who undergo malabsorptive procedures can absorb only 20% of the amount ingested.14 Restrictive procedures do not have the same effect on calcium absorption; however, patients may have reduced dietary lactose intake and be at risk for deficiency.
A study by Ducloux and colleagues15 found that 96% of bariatric surgery patients had vitamin D deficiency before the procedure. After malabsorptive procedures, the decrease in bile salts leads to an inability to break down fat-soluble vitamins and to uncoordinated mixing of food and bile secretions.16 Restrictive procedures do not carry this risk, though many patients still require supplementation because of their underlying deficiency.
The decrease in stomach size causes a decrease in intrinsic factor from parietal cells, with subsequent inability to appropriately transport vitamin B12. Exclusion of the duodenum also eliminates the site of absorption; therefore, B12 should be replaced orally.11 Megaloblastic anemia is a rarely reported sequela.17,18 Folate deficiency is less common because it can take place in the entire intestine after surgery, even though absorption occurs primarily in the proximal portion of the small intestine.10
Protein deficiency can result in loss of muscle mass and subsequent muscle weakness, edema, and anomalies of the skin, mucosa, and nails.12 It is seen after both types of procedures because of decreased dietary intake from intolerance. Malabsorptive procedures also decrease pepsinogen secretion and reduce the intestinal absorption surface.
Considerations for Orthopedic Surgeons
Wound Healing
Much of our knowledge of the effects of bariatric surgery on skin and wound healing has been gleaned from samples obtained from patients during abdominoplasty or other body-contouring procedures. These samples have all shown a decrease in hydroxyproline, the major constituent of collagen and the main factor in determining the tensile strength of a wound.19 D’Ettorre and colleagues20 performed biopsies of abdominal skin before and after biliopancreatic diversion and noted that tissue proteins, including hydroxyproline, were significantly reduced. Histologic examination revealed disorganized dermal elastic and collagen fibers. In addition, all patients involved in the study had wound-healing problems, with delayed healing of 25 days, compared with 12 days in nonbariatric patients. Deficiencies in vitamins B12, D, and E, as well as folate and total tissue protein, were implicated as causative factors.
Effects on Bone
Malabsorptive procedures decrease bone mineral density (BMD) through their effects on calcium and vitamin D. BMD is also decreased because these procedures lower levels of plasma leptin and ghrelin, increase adiponectin, and reduce estrogen in women.21 The BMD decline correlates with amount of weight lost.22 This complication is not seen in restrictive procedures, even though patients may have decreased calcium and vitamin D levels.23 The exact effect on BMD and on subsequent risk for osteopenia and osteoporosis is difficult to quantify, as obese patients have higher BMD than age-matched controls do, because of increased mechanical loading. In a prospective study, Vilarrasa and colleagues24 found a 10.9% decrease in femoral neck BMD in women 1 year after Roux-en-Y with 34% weight loss, despite supplementation with 800 IU of vitamin D and 1200 mg of calcium daily.
Fracture Healing
Although BMD is decreased in patients after gastric bypass surgery, there has been only 1 recorded case of fracture nonunion after bariatric surgery—involving a distal radius fracture in a patient who had undergone jejunoileal bypass surgery.25 Hypovitaminosis has a detrimental effect on bone repair and BMD, increasing the risk for fracture from minor trauma; however, delayed union and nonunion have not been reported as consequences.26
Pharmacology
Both restrictive and malabsorptive procedures decrease drug bioavailabilty from tablet preparations by shortening the surface area available for absorption and diminishing stomach acidity.27 These consequences pose a problem particularly for extended-release formulations, as these formulations are not given enough time to dissolve and reach therapeutic concentrations.28 Also affected is warfarin, which requires a larger dose to maintain therapeutic international normalized ratio. Antibiotics may have reduced bioavailability because of decreased transit time. Therefore, liquid preparations are preferred, as they need not be dissolved.
As there is no reported change in intravenous bioavailability with preoperative and postoperative antimicrobial prophylaxis, this is the preferred administration method.29 However, obese patients in general may have altered pharmacokinetics, including increased glomerular filtration rate, and in most cases they should be treated with higher levels of antibiotics.30
Nonsteroidal anti-inflammatory drugs (NSAIDs) should be avoided in all patients. The acidic composition of NSAIDs causes direct injury to the gastric pouch. NSAIDs also injure the gastrointestinal lining by inhibiting prostaglandin synthesis, which thins the mucosa. In turn, erosions and ulcers may form in the epithelial layer.31 Acetaminophen or a centrally acting agent (eg, tramadol) is recommended instead. Aspirin has a chemical structure similar to that of NSAIDs and should not be used either. Alendronate causes esophageal ulceration; however, no such complication has been reported with teriparatide32 (Table 3).
Preoperative Evaluation
As already discussed, patients who undergo weight-loss surgery are at higher risk for wound-healing complications because of nutritional deficiencies. Total protein, albumin, and prealbumin levels and total lymphocyte count should be used to identify protein deficiency, which can decrease the likelihood of organized collagen formation. Huang and colleagues33 noted a statistically significant increase in complications after total knee arthroplasty (TKA) in patients with a prealbumin level under 3.5 mg/dL or a transferrin level under 200 mg/dL. Rates of prosthetic joint infection and development of hematoma or seroma requiring operative management were much higher, as were rates of postoperative neurovascular, renal, and cardiovascular complications.
Serum levels of vitamin A, folate, vitamin B12, and vitamin C should also be ordered, as many patients are deficient. Transferrin levels should be checked before surgery, as iron-deficiency anemia is common. Naghshineh and colleagues34 noted an anecdotal decrease in wound-healing complications in body-contouring surgery after correction of subclinical and clinical deficiencies in protein, arginine, glutamine, vitamin A, vitamin B12, vitamin C, folate, thiamine, iron, zinc, and selenium. Zinc deficiency was similarly implicated in wound-healing complications by Zorrilla and colleagues,35,36 who found a statistically significant delay in wound healing in patients with serum zinc levels under 95 mg/dL after total hip arthroplasty (THA)35 and hip hemiarthroplasty.36 To facilitate bone healing, physicians should give patients a thorough workup of levels of serum and urine calcium, 24-hydroxyvitamin D, and alkaline phosphatase. Osteomalacia typically presents with high alkaline phosphatase levels37 and secondary hyperparathyroidism. Therefore, physicians should monitor for these conditions. Although nonunion and aseptic loosening have not been reported as consequences of bariatric surgery, bone health should nevertheless be optimized when possible (Table 4).
Elective Orthopedic Surgery
Little is known about the true effect of weight-loss surgery on subsequent orthopedic procedures. Few investigators have explored the effect of surgery on arthrodesis, and the only recommendation for orthopedic surgeons is to be prepared for poor bone healing and the possibility of nonunion.38 Hidalgo and colleagues39 studied laparoscopic sleeve gastrectomy performed a minimum of 6 months before another elective surgery. Two patients had lumbar laminectomies, 2 had lumbar discectomies, 1 had a cervical discectomy, and 1 had a rotator cuff repair. By most recent follow-up, there were no complications of any of the orthopedic procedures, and all patients had healed.
There is no recommended amount of time between bariatric surgery and elective orthopedic surgery. Maximum weight loss and stabilization are typically achieved 2 years after surgery.40 However, elective orthopedic surgery has been performed as early as 6 months after bariatric surgery. Inacio and colleagues41 studied 3 groups of patients who underwent total joint arthroplasty (TJA): those who had it less than 2 years after bariatric surgery, those who had it more than 2 years after bariatric surgery, and those who were obese but did not have bariatric surgery. Complications of TJA occurred within the first year in 2.9% of the patients who had it more than 2 years after bariatric surgery, in 5.9% of the patients who had it less than 2 years after bariatric surgery, and in 4.1% of the patients who did not undergo bariatric surgery. Similarly, Severson and colleagues2 evaluated intraoperative and postoperative complications of TKA in 3 groups of obese patients: those who had TKA before bariatric surgery, those who had TKA less than 2 years after bariatric surgery, and those who had TKA more than 2 years after bariatric surgery. Gastroplasty and bypass patients were included. BMI was statistically significantly higher in the preoperative group than in the other 2 groups, though mean BMI for all groups was above 35 kg/m2. Operative time and tourniquet time were reduced in patients who had TKA more than 2 years after bariatric surgery, but there was no significant difference in anesthesia time. There was also no difference in 90-day complication rates between patients who had TKA before bariatric surgery and those who had it afterward. Severson and colleagues2 recommended communicating the risks to all obese patients, whether they undergo weight-loss surgery or not.
Arthroplasty
Obese patients have a higher rate of complications after arthroplasty—hence the referrals to bariatric surgeons. Bariatric surgery and its associated weight loss might improve joint pain and delay the need for arthroplasty in some cases.42 Obese people are prone to joint degeneration from the excess weight, and from altered gait patterns (eg, exaggerated step width, slower walking speed, increased time in double-limb stance).43 Gait changes are reversible after weight loss.44 Hooper and colleagues45 found a 37% decrease in lower extremity complaints after surgical weight loss, even though mean BMI at final follow-up was still in the obese range.
Obesity itself is a risk factor for ligamentous instability, but it is unclear whether the risk is mitigated by bariatric surgery. Disruption of the anterior fibers of the medial collateral ligament is more common in obese patients, as are complications involving the extensor mechanism (eg, patellofemoral dislocation). As a result, slower postoperative rehabilitation is recommended.46 Although there is no recorded link between bariatric surgery and the development of ligamentous laxity, surgeons should be aware of the potential for medial collateral ligament avulsion in obese and formerly obese patients and have appropriate implants available.
Kulkarni and colleagues47 compared the rates of hip and knee arthroplasty complications in patients who were obese before bariatric surgery and patients who were still obese after bariatric surgery. Gastroplasty and bypass patients were included. Data on superficial wound infections were excluded; however, the bariatric surgery group’s deep wound infection rate was 3.5 times lower, and its 30-day readmission rate was 7 times lower. There was no difference in dislocation and hip revision rates at 1 year. Although 1 patient in the bariatric surgery group died of an unknown cause 9 days after surgery, Kulkarni and colleagues47 concluded it is safer to operate on obese patients after versus before bariatric surgery. However, their study did not include mean BMI, so no conclusion can be drawn about the risk of operating on patients who were still obese after bariatric surgery.
Studies of weight loss in primary TJA patients have had conflicting findings.48 Trofa and colleagues49 reported that 15 patients who underwent arthroplasty a mean of 42.4 months after bariatric surgery lost 27.9% more of their original BMI compared with patients who underwent bariatric surgery but not arthroplasty. This relationship between arthroplasty and weight loss was strongest in patients who underwent knee arthroplasty, with an average of 43.9% more BMI lost compared to patients who did not undergo TKA. There was no significant change in BMI in patients who underwent THA and bariatric surgery compared with patients who underwent bariatric surgery but not THA.
Parvizi and colleagues50 assessed the results of 20 arthroplasties (8 THAs, 12 TKAs) performed in 14 patients a mean of 23 months after bariatric surgery (2 gastroplasties, 12 bypass surgeries). Mean BMI was 29 kg/m2. At final follow-up, 1 patient required revision THA for aseptic loosening, but all the others showed no evidence of radiographic loosening or wear. One patient had a superficial wound infection, and 1 had a deep wound infection. Parvizi and colleagues50 reported that arthroplasty after bariatric surgery is a viable option and is preferable to operating on morbidly obese patients.
Summary
Orthopedic surgeons are increasingly performing elective hip and knee arthroplasties on patients who have undergone bariatric surgery. Although bariatric surgery may alleviate some of the complications associated with surgery on morbidly obese patients, it should be approached with caution. Studies have shown that bariatric surgery patients are at increased risk for wound-healing and other complications, often caused by unrecognized preoperative nutrient deficiencies. In addition, patients are often unable to tolerate commonly used medications. The exact timing of bariatric surgery relative to elective orthopedic procedures is unclear. Surgeons should perform a preoperative evaluation based on type of bariatric surgery in order to reduce the likelihood of adverse events. Such preemptive therapy may improve the short- and long-term results of major reconstructive surgery. Further research is needed to determine the true effect of bariatric surgery on orthopedic procedures.
An estimated 220,000 bariatric surgeries are performed annually in the United States and Canada, and 344,221 procedures worldwide.1 Not only are orthopedic surgeons seeing more patients who have had bariatric surgery, they are also referring morbidly obese patients to bariatric surgeons before elective procedures.2 Patients with body mass index (BMI) over 40 kg/m2 are candidates for surgical treatment of obesity. Comorbid conditions directly related to obesity, including diabetes, respiratory insufficiency, and pseudotumor cerebri, decrease the BMI of eligibility to 35 kg/m2. Other considerations are failure of nonsurgical weight-loss methods, such as dietary programs for weight reduction, behavioral modification programs, and pharmacotherapy. Patients’ psychological stability is extremely important given the rigorous dietary changes required after surgery.3 Although weight-loss surgery can eliminate many of the complications of obesity, bariatric patients even with weight loss have increased operative and postoperative risks, likely because of alterations in nutrient absorption. Knowledge of the pathophysiology associated with bariatric surgery can assist orthopedic surgeons in optimizing medical and surgical management of patients’ musculoskeletal issues.
Bariatric Surgery
Surgically induced weight loss works by reducing quantity of food consumed and absorption of calories. Jejunoileal bypass, one of the first procedures used, significantly decreased the absorptive area for nutrients, which led to complications such as diarrhea, cirrhosis, and nephrolithiasis.4 This surgery is no longer performed, and current procedures try to minimize the risks of malabsorption.5
The 2 types of bariatric surgeries now available in the United States are gastroplasty and gastric bypass, both of which are performed laparoscopically.6 Gastroplasties are purely restrictive procedures, which reduce stomach volume. In gastric banding, the most common gastroplasty, a silicone band is placed around the proximal stomach to create a 15-mL pouch in the cardia. Sleeve gastrectomy also reduces stomach volume, to about 25%, by stapling along the greater curvature. In both procedures, consumed calories are restricted, but the gastrointestinal tract is left in continuity, and essential nutrients are properly absorbed.7 However, failure rates are higher, and weight loss more variable, than with gastric bypass procedures.8
Gastric bypass uses both restriction and malabsorption to increase weight loss.7 A gastric pouch (15-30 mL) is created by stapling across the cardia of the stomach. The jejunum is then divided, and the distal portion of the divided jejunum anastomosed to the small proximal stomach pouch. This creates the roux limb where food passes. The duodenum is excluded, and the proximal portion of the jejunum is attached to the roux limb to provide a conduit for biliary and pancreatic digestive secretions. Weight loss is caused by both reduction in stomach size and malabsorption of calories owing to the diversion of digestive enzymes and the decrease in absorptive surface area. Only 28% of ingested fat and 57% of ingested protein are absorbed9 (Table 1).
Metabolic Consequences
Nutrient deficiencies are seen more often in the malabsorptive procedures; however, patients with restrictive procedures may have poor eating habits and are therefore also at risk.10 In fact, many patients have nutritional deficiencies predating their bariatric surgery, as obesity creates a chronic inflammatory state that leads to anemia of chronic disease. Schweiger and colleagues11 assessed the nutritional status of bariatric surgery candidates and noted a high incidence of iron and folic acid deficiencies with corresponding anemia. They concluded these deficiencies stemmed from calorie-dense diets high in carbohydrates and fats. Although patients may improve their diet after surgery with concomitant nutritional counseling, deficiencies in iron, calcium, vitamin B12, folate, and vitamin D are common12 (Table 2).
Iron deficiency continues after bariatric surgery because dietary iron must be converted to its absorbable form by hydrochloric acid secreted from the stomach. As stomach volume is reduced, there is a corresponding decrease in acid secretion. The result is that iron deficiency occurs in both restrictive and malabsorptive procedures.13 Moreover, with the diversion from the duodenum and the proximal jejunum in bypass surgery, the main areas of absorption are excluded.10 Patients may require intravenous therapy for iron-deficiency anemia—or oral supplementation combined with ascorbic acid to increase stomach acidity.
As calcium is absorbed mainly in the duodenum and the jejunum, patients who undergo malabsorptive procedures can absorb only 20% of the amount ingested.14 Restrictive procedures do not have the same effect on calcium absorption; however, patients may have reduced dietary lactose intake and be at risk for deficiency.
A study by Ducloux and colleagues15 found that 96% of bariatric surgery patients had vitamin D deficiency before the procedure. After malabsorptive procedures, the decrease in bile salts leads to an inability to break down fat-soluble vitamins and to uncoordinated mixing of food and bile secretions.16 Restrictive procedures do not carry this risk, though many patients still require supplementation because of their underlying deficiency.
The decrease in stomach size causes a decrease in intrinsic factor from parietal cells, with subsequent inability to appropriately transport vitamin B12. Exclusion of the duodenum also eliminates the site of absorption; therefore, B12 should be replaced orally.11 Megaloblastic anemia is a rarely reported sequela.17,18 Folate deficiency is less common because it can take place in the entire intestine after surgery, even though absorption occurs primarily in the proximal portion of the small intestine.10
Protein deficiency can result in loss of muscle mass and subsequent muscle weakness, edema, and anomalies of the skin, mucosa, and nails.12 It is seen after both types of procedures because of decreased dietary intake from intolerance. Malabsorptive procedures also decrease pepsinogen secretion and reduce the intestinal absorption surface.
Considerations for Orthopedic Surgeons
Wound Healing
Much of our knowledge of the effects of bariatric surgery on skin and wound healing has been gleaned from samples obtained from patients during abdominoplasty or other body-contouring procedures. These samples have all shown a decrease in hydroxyproline, the major constituent of collagen and the main factor in determining the tensile strength of a wound.19 D’Ettorre and colleagues20 performed biopsies of abdominal skin before and after biliopancreatic diversion and noted that tissue proteins, including hydroxyproline, were significantly reduced. Histologic examination revealed disorganized dermal elastic and collagen fibers. In addition, all patients involved in the study had wound-healing problems, with delayed healing of 25 days, compared with 12 days in nonbariatric patients. Deficiencies in vitamins B12, D, and E, as well as folate and total tissue protein, were implicated as causative factors.
Effects on Bone
Malabsorptive procedures decrease bone mineral density (BMD) through their effects on calcium and vitamin D. BMD is also decreased because these procedures lower levels of plasma leptin and ghrelin, increase adiponectin, and reduce estrogen in women.21 The BMD decline correlates with amount of weight lost.22 This complication is not seen in restrictive procedures, even though patients may have decreased calcium and vitamin D levels.23 The exact effect on BMD and on subsequent risk for osteopenia and osteoporosis is difficult to quantify, as obese patients have higher BMD than age-matched controls do, because of increased mechanical loading. In a prospective study, Vilarrasa and colleagues24 found a 10.9% decrease in femoral neck BMD in women 1 year after Roux-en-Y with 34% weight loss, despite supplementation with 800 IU of vitamin D and 1200 mg of calcium daily.
Fracture Healing
Although BMD is decreased in patients after gastric bypass surgery, there has been only 1 recorded case of fracture nonunion after bariatric surgery—involving a distal radius fracture in a patient who had undergone jejunoileal bypass surgery.25 Hypovitaminosis has a detrimental effect on bone repair and BMD, increasing the risk for fracture from minor trauma; however, delayed union and nonunion have not been reported as consequences.26
Pharmacology
Both restrictive and malabsorptive procedures decrease drug bioavailabilty from tablet preparations by shortening the surface area available for absorption and diminishing stomach acidity.27 These consequences pose a problem particularly for extended-release formulations, as these formulations are not given enough time to dissolve and reach therapeutic concentrations.28 Also affected is warfarin, which requires a larger dose to maintain therapeutic international normalized ratio. Antibiotics may have reduced bioavailability because of decreased transit time. Therefore, liquid preparations are preferred, as they need not be dissolved.
As there is no reported change in intravenous bioavailability with preoperative and postoperative antimicrobial prophylaxis, this is the preferred administration method.29 However, obese patients in general may have altered pharmacokinetics, including increased glomerular filtration rate, and in most cases they should be treated with higher levels of antibiotics.30
Nonsteroidal anti-inflammatory drugs (NSAIDs) should be avoided in all patients. The acidic composition of NSAIDs causes direct injury to the gastric pouch. NSAIDs also injure the gastrointestinal lining by inhibiting prostaglandin synthesis, which thins the mucosa. In turn, erosions and ulcers may form in the epithelial layer.31 Acetaminophen or a centrally acting agent (eg, tramadol) is recommended instead. Aspirin has a chemical structure similar to that of NSAIDs and should not be used either. Alendronate causes esophageal ulceration; however, no such complication has been reported with teriparatide32 (Table 3).
Preoperative Evaluation
As already discussed, patients who undergo weight-loss surgery are at higher risk for wound-healing complications because of nutritional deficiencies. Total protein, albumin, and prealbumin levels and total lymphocyte count should be used to identify protein deficiency, which can decrease the likelihood of organized collagen formation. Huang and colleagues33 noted a statistically significant increase in complications after total knee arthroplasty (TKA) in patients with a prealbumin level under 3.5 mg/dL or a transferrin level under 200 mg/dL. Rates of prosthetic joint infection and development of hematoma or seroma requiring operative management were much higher, as were rates of postoperative neurovascular, renal, and cardiovascular complications.
Serum levels of vitamin A, folate, vitamin B12, and vitamin C should also be ordered, as many patients are deficient. Transferrin levels should be checked before surgery, as iron-deficiency anemia is common. Naghshineh and colleagues34 noted an anecdotal decrease in wound-healing complications in body-contouring surgery after correction of subclinical and clinical deficiencies in protein, arginine, glutamine, vitamin A, vitamin B12, vitamin C, folate, thiamine, iron, zinc, and selenium. Zinc deficiency was similarly implicated in wound-healing complications by Zorrilla and colleagues,35,36 who found a statistically significant delay in wound healing in patients with serum zinc levels under 95 mg/dL after total hip arthroplasty (THA)35 and hip hemiarthroplasty.36 To facilitate bone healing, physicians should give patients a thorough workup of levels of serum and urine calcium, 24-hydroxyvitamin D, and alkaline phosphatase. Osteomalacia typically presents with high alkaline phosphatase levels37 and secondary hyperparathyroidism. Therefore, physicians should monitor for these conditions. Although nonunion and aseptic loosening have not been reported as consequences of bariatric surgery, bone health should nevertheless be optimized when possible (Table 4).
Elective Orthopedic Surgery
Little is known about the true effect of weight-loss surgery on subsequent orthopedic procedures. Few investigators have explored the effect of surgery on arthrodesis, and the only recommendation for orthopedic surgeons is to be prepared for poor bone healing and the possibility of nonunion.38 Hidalgo and colleagues39 studied laparoscopic sleeve gastrectomy performed a minimum of 6 months before another elective surgery. Two patients had lumbar laminectomies, 2 had lumbar discectomies, 1 had a cervical discectomy, and 1 had a rotator cuff repair. By most recent follow-up, there were no complications of any of the orthopedic procedures, and all patients had healed.
There is no recommended amount of time between bariatric surgery and elective orthopedic surgery. Maximum weight loss and stabilization are typically achieved 2 years after surgery.40 However, elective orthopedic surgery has been performed as early as 6 months after bariatric surgery. Inacio and colleagues41 studied 3 groups of patients who underwent total joint arthroplasty (TJA): those who had it less than 2 years after bariatric surgery, those who had it more than 2 years after bariatric surgery, and those who were obese but did not have bariatric surgery. Complications of TJA occurred within the first year in 2.9% of the patients who had it more than 2 years after bariatric surgery, in 5.9% of the patients who had it less than 2 years after bariatric surgery, and in 4.1% of the patients who did not undergo bariatric surgery. Similarly, Severson and colleagues2 evaluated intraoperative and postoperative complications of TKA in 3 groups of obese patients: those who had TKA before bariatric surgery, those who had TKA less than 2 years after bariatric surgery, and those who had TKA more than 2 years after bariatric surgery. Gastroplasty and bypass patients were included. BMI was statistically significantly higher in the preoperative group than in the other 2 groups, though mean BMI for all groups was above 35 kg/m2. Operative time and tourniquet time were reduced in patients who had TKA more than 2 years after bariatric surgery, but there was no significant difference in anesthesia time. There was also no difference in 90-day complication rates between patients who had TKA before bariatric surgery and those who had it afterward. Severson and colleagues2 recommended communicating the risks to all obese patients, whether they undergo weight-loss surgery or not.
Arthroplasty
Obese patients have a higher rate of complications after arthroplasty—hence the referrals to bariatric surgeons. Bariatric surgery and its associated weight loss might improve joint pain and delay the need for arthroplasty in some cases.42 Obese people are prone to joint degeneration from the excess weight, and from altered gait patterns (eg, exaggerated step width, slower walking speed, increased time in double-limb stance).43 Gait changes are reversible after weight loss.44 Hooper and colleagues45 found a 37% decrease in lower extremity complaints after surgical weight loss, even though mean BMI at final follow-up was still in the obese range.
Obesity itself is a risk factor for ligamentous instability, but it is unclear whether the risk is mitigated by bariatric surgery. Disruption of the anterior fibers of the medial collateral ligament is more common in obese patients, as are complications involving the extensor mechanism (eg, patellofemoral dislocation). As a result, slower postoperative rehabilitation is recommended.46 Although there is no recorded link between bariatric surgery and the development of ligamentous laxity, surgeons should be aware of the potential for medial collateral ligament avulsion in obese and formerly obese patients and have appropriate implants available.
Kulkarni and colleagues47 compared the rates of hip and knee arthroplasty complications in patients who were obese before bariatric surgery and patients who were still obese after bariatric surgery. Gastroplasty and bypass patients were included. Data on superficial wound infections were excluded; however, the bariatric surgery group’s deep wound infection rate was 3.5 times lower, and its 30-day readmission rate was 7 times lower. There was no difference in dislocation and hip revision rates at 1 year. Although 1 patient in the bariatric surgery group died of an unknown cause 9 days after surgery, Kulkarni and colleagues47 concluded it is safer to operate on obese patients after versus before bariatric surgery. However, their study did not include mean BMI, so no conclusion can be drawn about the risk of operating on patients who were still obese after bariatric surgery.
Studies of weight loss in primary TJA patients have had conflicting findings.48 Trofa and colleagues49 reported that 15 patients who underwent arthroplasty a mean of 42.4 months after bariatric surgery lost 27.9% more of their original BMI compared with patients who underwent bariatric surgery but not arthroplasty. This relationship between arthroplasty and weight loss was strongest in patients who underwent knee arthroplasty, with an average of 43.9% more BMI lost compared to patients who did not undergo TKA. There was no significant change in BMI in patients who underwent THA and bariatric surgery compared with patients who underwent bariatric surgery but not THA.
Parvizi and colleagues50 assessed the results of 20 arthroplasties (8 THAs, 12 TKAs) performed in 14 patients a mean of 23 months after bariatric surgery (2 gastroplasties, 12 bypass surgeries). Mean BMI was 29 kg/m2. At final follow-up, 1 patient required revision THA for aseptic loosening, but all the others showed no evidence of radiographic loosening or wear. One patient had a superficial wound infection, and 1 had a deep wound infection. Parvizi and colleagues50 reported that arthroplasty after bariatric surgery is a viable option and is preferable to operating on morbidly obese patients.
Summary
Orthopedic surgeons are increasingly performing elective hip and knee arthroplasties on patients who have undergone bariatric surgery. Although bariatric surgery may alleviate some of the complications associated with surgery on morbidly obese patients, it should be approached with caution. Studies have shown that bariatric surgery patients are at increased risk for wound-healing and other complications, often caused by unrecognized preoperative nutrient deficiencies. In addition, patients are often unable to tolerate commonly used medications. The exact timing of bariatric surgery relative to elective orthopedic procedures is unclear. Surgeons should perform a preoperative evaluation based on type of bariatric surgery in order to reduce the likelihood of adverse events. Such preemptive therapy may improve the short- and long-term results of major reconstructive surgery. Further research is needed to determine the true effect of bariatric surgery on orthopedic procedures.
1. Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19(12):1605-1611.
2. Severson EP, Singh JA, Browne JA, Trousdale RT, Sarr MG, Lewallen DG. Total knee arthroplasty in morbidly obese patients treated with bariatric surgery. J Arthroplasty. 2012;27(9):1696-1700.
3. Mechanick JI, Kushner RF, Sugerman HJ, et al. American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient [published correction appears in Endocr Pract. 2009;15(7):768]. Endocr Pract. 2008;14(suppl 1):1-83.
4. Hocking MP, Duerson MC, O’Leary JP, Woodward ER. Jejunoilial bypass for morbid obesity. Late follow-up in 100 cases. N Engl J Med. 1983;308(17):995-999.
5. DeMaria EJ. Morbid obesity. In: Mulholland MW, Lillemoe KD, Doherty GM, et al, eds. Greenfield’s Surgery: Scientific Principles & Practice. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:736-743.
6. O’Brien PE. Bariatric surgery: mechanisms, indications and outcomes. J Gastroenterol Hepatol. 2010;25(8):1358-1365.
7. Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724-1737.
8. DeMaria EJ, Sugerman HJ, Meador JG, et al. High failure rate after laparoscopic adjustable silicone gastric banding for treatment of morbid obesity. Ann Surg. 2001;233(6):809-818.
9. Slater GH, Ren CJ, Siegel N, et al. Serum fat-soluble vitamin deficiency and abnormal calcium metabolism after malabsorptive bariatric surgery. J Gastrointest Surg. 2004;8(1):48-55.
10. Alvarez-Leite JI. Nutrient deficiencies secondary to bariatric surgery. Curr Opin Clin Nutr Metab Care. 2004;7(5):569-575.
11. Schweiger C, Weiss R, Berry E, Keidar A. Nutritional deficiencies in bariatric surgery candidates. Obes Surg. 2010;20(2):193-197.
12. Poitou Bernert C, Ciangura C, Coupaye M, Czernichow S, Bouillot JL, Basdevant A. Nutritional deficiency after gastric bypass: diagnosis, prevention and treatment. Diabetes Metab. 2007;33(1):13-24.
13. Gehrer S, Kern B, Peters T, Christoffel-Courtin C, Peterli R. Fewer nutrient deficiencies after laparoscopic sleeve gastrectomy (LSG) than after laparoscopic Roux-Y-gastric bypass (LRYGB)—a prospective study. Obes Surg. 2010;20(4):447-453.
14. Goode LR, Brolin RE, Chowdhury HA, Shapses SA. Bone and gastric bypass surgery: effects of dietary calcium and vitamin D. Obes Res. 2004;12(1):40-47.
15. Ducloux R, Nobécourt E, Chevallier JM, Ducloux H, Elian N, Altman JJ. Vitamin D deficiency before bariatric surgery: should supplement intake be routinely prescribed? Obes Surg. 2011;21(5):556-560.
16. Wang A, Powell A. The effects of obesity surgery on bone metabolism: what orthopedic surgeons need to know. Am J Orthop. 2009;38(2):77-79.
17. Baghdasarian KL. Gastric bypass and megaloblastic anemia. J Am Diet Assoc. 1982;80(4):368-371.
18. Crowley LV, Olson RW. Megaloblastic anemia after gastric bypass for obesity. Am J Gastroenterol. 1983;78(7):406-410.
19. Sorg H, Schulz T, Krueger C, Vollmar B. Consequences of surgical stress on the kinetics of skin wound healing: partial hepatectomy delays and functionally alters dermal repair. Wound Repair Regen. 2009;17(3):367-377.
20. D’Ettorre M, Gniuli D, Iaconelli A, Massi G, Mingrone G, Bracaglia R. Wound healing process in post-bariatric patients: an experimental evaluation. Obes Surg. 2010;20(11):1552-1558.
21. Carrasco F, Ruz M, Rojas P, et al. Changes in bone mineral density, body composition and adiponectin levels in morbidly obese patients after bariatric surgery. Obes Surg. 2009;19(1);41-46.
22. Fleischer J, Stein EM, Bessler M, et al. The decline in hip bone density after gastric bypass surgery is associated with extent of weight loss. J Clin Endocrinol Metab. 2008;93(10):3735-3740.
23. von Mach MA, Stoeckli R, Bilz S, Kraenzlin M, Langer I, Keller U. Changes in bone mineral content after surgical treatment of morbid obesity. Metabolism. 2004;53(7):918-921.
24. Vilarrasa N, Gómez JM, Elio I, et al. Evaluation of bone disease in morbidly obese women after gastric bypass and risk factors implicated in bone loss. Obes Surg. 2009;19(7):860-866.
25. Hey H, Lund B, Sørensen OH, Lund B. Delayed fracture healing following jejunoileal bypass surgery for obesity. Calcif Tissue Int. 1982;34(1):13-15.
26. Borrelli J Jr, Pape C, Hak D, et al. Physiological challenges of bone repair. J Orthop Trauma. 2012;26(12):708-711.
27. Sardo P, Walker JH. Bariatric surgery: impact on medication management. Hosp Pharm. 2008;43(2):113-120.
28. Lizer MH, Papageorgeon H, Glembot TM. Nutritional and pharmacologic challenges in the bariatric surgery patient. Obes Surg. 2010;20(12):1654-1659.
29. Chopra T, Zhao JJ, Alangaden G, Wood MH, Kaye KS. Preventing surgical site infections after bariatric surgery: value of perioperative antibiotic regimens. Expert Rev Pharmacoecon Outcomes Res. 2010;10(3):317-328.
30. Payne KD, Hall RG 2nd. Dosing of antibacterial agents in obese adults: does one size fit all? Expert Rev Anti Infect Ther. 2014;12(7):829-854.
31. Sasse KC, Ganser J, Kozar M, et al. Seven cases of gastric perforation in Roux-en-Y gastric bypass patients: what lessons can we learn? Obes Surg. 2008;18(5):530-534.
32. Miller AD, Smith KM. Medication use in bariatric surgery patients: what orthopedists need to know. Orthopedics. 2006;29(2):121-123.
33. Huang R, Greenky M, Kerr GJ, Austin MS, Parvizi J. The effect of malnutrition on patients undergoing elective joint arthroplasty. J Arthroplasty. 2013;28(8 suppl):21-24.
34. Naghshineh N, O’Brien Coon D, McTigue K, Courcoulas AP, Fernstrom M, Rubin JP. Nutritional assessment of bariatric surgery patients presenting for plastic surgery: a prospective analysis. Plast Reconstr Surg. 2010;126(2):602-610.
35. Zorrilla P, Gómez LA, Salido JA, Silva A, López-Alonso A. Low serum zinc level as a predictive factor of delayed wound healing in total hip replacement. Wound Repair Regen. 2006;14(2):119-122.
36. Zorrilla P, Salido JA, López-Alonso A, Silva A. Serum zinc as a prognostic tool for wound healing in hip hemiarthroplasty. Clin Orthop Relat Res. 2004;(420):304-308.
37. Williams SE, Cooper K, Richmond B, Schauer P. Perioperative management of bariatric surgery patients: focus on metabolic bone disease. Cleve Clin J Med. 2008;75(5):333-349.
38. Kini S, Kannan U. Effect of bariatric surgery on future general surgical procedures. J Minim Access Surg. 2011;7(2):126-131.
39. Hidalgo JE, Roy M, Ramirez A, Szomstein S, Rosenthal RJ. Laparoscopic sleeve gastrectomy: a first step for rapid weight loss in morbidly obese patients requiring a second non-bariatric procedure. Obes Surg. 2012;22(4):555-559.
40. O’Brien PE, McPhail T, Chaston TB, Dixon JB. Systematic review of medium-term weight loss after bariatric operations. Obes Surg. 2006;16(8):1032-1040.
41. Inacio MC, Paxton EW, Fisher D, Li RA, Barber TC, Singh JA. Bariatric surgery prior to total joint arthroplasty may not provide dramatic improvements in post-arthroplasty surgical outcomes. J Arthroplasty. 2014;29(7):1359-1364.
42. Gill RS, Al‐Adra DP, Shi X, Sharma AM, Birch DW, Karmali S. The benefits of bariatric surgery in obese patients with hip and knee osteoarthritis: a systematic review. Obes Rev. 2011;12(12):1083-1089.
43. Vartiainen P, Bragge T, Lyytinen T, Hakkarainen M, Karjalainen PA, Arokoski JP. Kinematic and kinetic changes in obese gait in bariatric surgery–induced weight loss. J Biomech. 2012;45(10):1769-1774.
44. Vincent HK, Ben-David K, Conrad BP, Lamb KM, Seay AN, Vincent KR. Rapid changes in gait, musculoskeletal pain, and quality of life after bariatric surgery. Surg Obes Relat Dis. 2012;8(3):346-354.
45. Hooper MM, Stellato TA, Hallowell PT, Seitz BA, Moskowitz RW. Musculoskeletal findings in obese subjects before and after weight loss following bariatric surgery. Int J Obes. 2007;31(1):114-120.
46. Booth RE Jr. Total knee arthroplasty in the obese patient: tips and quips. J Arthroplasty. 2002;17(4 suppl 1):69-70.
47. Kulkarni A, Jameson SS, James P, Woodcock S, Muller S, Reed MR. Does bariatric surgery prior to lower limb joint replacement reduce complications? Surgeon. 2011;9(1):18-21.
48. Inacio MC, Silverstein DK, Raman R, et al. Weight patterns before and after total joint arthroplasty and characteristics associated with weight change. Perm J. 2014;18(1):25-31.
49. Trofa D, Smith EL, Shah V, Shikora S. Total weight loss associated with increased physical activity after bariatric surgery may increase the need for total joint arthroplasty. Surg Obes Relat Dis. 2014;10(2):335-339.
50. Parvizi J, Trousdale RT, Sarr MG. Total joint arthroplasty in patients surgically treated for morbid obesity. J Arthroplasty. 2000;15(8):1003-1008.
1. Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19(12):1605-1611.
2. Severson EP, Singh JA, Browne JA, Trousdale RT, Sarr MG, Lewallen DG. Total knee arthroplasty in morbidly obese patients treated with bariatric surgery. J Arthroplasty. 2012;27(9):1696-1700.
3. Mechanick JI, Kushner RF, Sugerman HJ, et al. American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient [published correction appears in Endocr Pract. 2009;15(7):768]. Endocr Pract. 2008;14(suppl 1):1-83.
4. Hocking MP, Duerson MC, O’Leary JP, Woodward ER. Jejunoilial bypass for morbid obesity. Late follow-up in 100 cases. N Engl J Med. 1983;308(17):995-999.
5. DeMaria EJ. Morbid obesity. In: Mulholland MW, Lillemoe KD, Doherty GM, et al, eds. Greenfield’s Surgery: Scientific Principles & Practice. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:736-743.
6. O’Brien PE. Bariatric surgery: mechanisms, indications and outcomes. J Gastroenterol Hepatol. 2010;25(8):1358-1365.
7. Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724-1737.
8. DeMaria EJ, Sugerman HJ, Meador JG, et al. High failure rate after laparoscopic adjustable silicone gastric banding for treatment of morbid obesity. Ann Surg. 2001;233(6):809-818.
9. Slater GH, Ren CJ, Siegel N, et al. Serum fat-soluble vitamin deficiency and abnormal calcium metabolism after malabsorptive bariatric surgery. J Gastrointest Surg. 2004;8(1):48-55.
10. Alvarez-Leite JI. Nutrient deficiencies secondary to bariatric surgery. Curr Opin Clin Nutr Metab Care. 2004;7(5):569-575.
11. Schweiger C, Weiss R, Berry E, Keidar A. Nutritional deficiencies in bariatric surgery candidates. Obes Surg. 2010;20(2):193-197.
12. Poitou Bernert C, Ciangura C, Coupaye M, Czernichow S, Bouillot JL, Basdevant A. Nutritional deficiency after gastric bypass: diagnosis, prevention and treatment. Diabetes Metab. 2007;33(1):13-24.
13. Gehrer S, Kern B, Peters T, Christoffel-Courtin C, Peterli R. Fewer nutrient deficiencies after laparoscopic sleeve gastrectomy (LSG) than after laparoscopic Roux-Y-gastric bypass (LRYGB)—a prospective study. Obes Surg. 2010;20(4):447-453.
14. Goode LR, Brolin RE, Chowdhury HA, Shapses SA. Bone and gastric bypass surgery: effects of dietary calcium and vitamin D. Obes Res. 2004;12(1):40-47.
15. Ducloux R, Nobécourt E, Chevallier JM, Ducloux H, Elian N, Altman JJ. Vitamin D deficiency before bariatric surgery: should supplement intake be routinely prescribed? Obes Surg. 2011;21(5):556-560.
16. Wang A, Powell A. The effects of obesity surgery on bone metabolism: what orthopedic surgeons need to know. Am J Orthop. 2009;38(2):77-79.
17. Baghdasarian KL. Gastric bypass and megaloblastic anemia. J Am Diet Assoc. 1982;80(4):368-371.
18. Crowley LV, Olson RW. Megaloblastic anemia after gastric bypass for obesity. Am J Gastroenterol. 1983;78(7):406-410.
19. Sorg H, Schulz T, Krueger C, Vollmar B. Consequences of surgical stress on the kinetics of skin wound healing: partial hepatectomy delays and functionally alters dermal repair. Wound Repair Regen. 2009;17(3):367-377.
20. D’Ettorre M, Gniuli D, Iaconelli A, Massi G, Mingrone G, Bracaglia R. Wound healing process in post-bariatric patients: an experimental evaluation. Obes Surg. 2010;20(11):1552-1558.
21. Carrasco F, Ruz M, Rojas P, et al. Changes in bone mineral density, body composition and adiponectin levels in morbidly obese patients after bariatric surgery. Obes Surg. 2009;19(1);41-46.
22. Fleischer J, Stein EM, Bessler M, et al. The decline in hip bone density after gastric bypass surgery is associated with extent of weight loss. J Clin Endocrinol Metab. 2008;93(10):3735-3740.
23. von Mach MA, Stoeckli R, Bilz S, Kraenzlin M, Langer I, Keller U. Changes in bone mineral content after surgical treatment of morbid obesity. Metabolism. 2004;53(7):918-921.
24. Vilarrasa N, Gómez JM, Elio I, et al. Evaluation of bone disease in morbidly obese women after gastric bypass and risk factors implicated in bone loss. Obes Surg. 2009;19(7):860-866.
25. Hey H, Lund B, Sørensen OH, Lund B. Delayed fracture healing following jejunoileal bypass surgery for obesity. Calcif Tissue Int. 1982;34(1):13-15.
26. Borrelli J Jr, Pape C, Hak D, et al. Physiological challenges of bone repair. J Orthop Trauma. 2012;26(12):708-711.
27. Sardo P, Walker JH. Bariatric surgery: impact on medication management. Hosp Pharm. 2008;43(2):113-120.
28. Lizer MH, Papageorgeon H, Glembot TM. Nutritional and pharmacologic challenges in the bariatric surgery patient. Obes Surg. 2010;20(12):1654-1659.
29. Chopra T, Zhao JJ, Alangaden G, Wood MH, Kaye KS. Preventing surgical site infections after bariatric surgery: value of perioperative antibiotic regimens. Expert Rev Pharmacoecon Outcomes Res. 2010;10(3):317-328.
30. Payne KD, Hall RG 2nd. Dosing of antibacterial agents in obese adults: does one size fit all? Expert Rev Anti Infect Ther. 2014;12(7):829-854.
31. Sasse KC, Ganser J, Kozar M, et al. Seven cases of gastric perforation in Roux-en-Y gastric bypass patients: what lessons can we learn? Obes Surg. 2008;18(5):530-534.
32. Miller AD, Smith KM. Medication use in bariatric surgery patients: what orthopedists need to know. Orthopedics. 2006;29(2):121-123.
33. Huang R, Greenky M, Kerr GJ, Austin MS, Parvizi J. The effect of malnutrition on patients undergoing elective joint arthroplasty. J Arthroplasty. 2013;28(8 suppl):21-24.
34. Naghshineh N, O’Brien Coon D, McTigue K, Courcoulas AP, Fernstrom M, Rubin JP. Nutritional assessment of bariatric surgery patients presenting for plastic surgery: a prospective analysis. Plast Reconstr Surg. 2010;126(2):602-610.
35. Zorrilla P, Gómez LA, Salido JA, Silva A, López-Alonso A. Low serum zinc level as a predictive factor of delayed wound healing in total hip replacement. Wound Repair Regen. 2006;14(2):119-122.
36. Zorrilla P, Salido JA, López-Alonso A, Silva A. Serum zinc as a prognostic tool for wound healing in hip hemiarthroplasty. Clin Orthop Relat Res. 2004;(420):304-308.
37. Williams SE, Cooper K, Richmond B, Schauer P. Perioperative management of bariatric surgery patients: focus on metabolic bone disease. Cleve Clin J Med. 2008;75(5):333-349.
38. Kini S, Kannan U. Effect of bariatric surgery on future general surgical procedures. J Minim Access Surg. 2011;7(2):126-131.
39. Hidalgo JE, Roy M, Ramirez A, Szomstein S, Rosenthal RJ. Laparoscopic sleeve gastrectomy: a first step for rapid weight loss in morbidly obese patients requiring a second non-bariatric procedure. Obes Surg. 2012;22(4):555-559.
40. O’Brien PE, McPhail T, Chaston TB, Dixon JB. Systematic review of medium-term weight loss after bariatric operations. Obes Surg. 2006;16(8):1032-1040.
41. Inacio MC, Paxton EW, Fisher D, Li RA, Barber TC, Singh JA. Bariatric surgery prior to total joint arthroplasty may not provide dramatic improvements in post-arthroplasty surgical outcomes. J Arthroplasty. 2014;29(7):1359-1364.
42. Gill RS, Al‐Adra DP, Shi X, Sharma AM, Birch DW, Karmali S. The benefits of bariatric surgery in obese patients with hip and knee osteoarthritis: a systematic review. Obes Rev. 2011;12(12):1083-1089.
43. Vartiainen P, Bragge T, Lyytinen T, Hakkarainen M, Karjalainen PA, Arokoski JP. Kinematic and kinetic changes in obese gait in bariatric surgery–induced weight loss. J Biomech. 2012;45(10):1769-1774.
44. Vincent HK, Ben-David K, Conrad BP, Lamb KM, Seay AN, Vincent KR. Rapid changes in gait, musculoskeletal pain, and quality of life after bariatric surgery. Surg Obes Relat Dis. 2012;8(3):346-354.
45. Hooper MM, Stellato TA, Hallowell PT, Seitz BA, Moskowitz RW. Musculoskeletal findings in obese subjects before and after weight loss following bariatric surgery. Int J Obes. 2007;31(1):114-120.
46. Booth RE Jr. Total knee arthroplasty in the obese patient: tips and quips. J Arthroplasty. 2002;17(4 suppl 1):69-70.
47. Kulkarni A, Jameson SS, James P, Woodcock S, Muller S, Reed MR. Does bariatric surgery prior to lower limb joint replacement reduce complications? Surgeon. 2011;9(1):18-21.
48. Inacio MC, Silverstein DK, Raman R, et al. Weight patterns before and after total joint arthroplasty and characteristics associated with weight change. Perm J. 2014;18(1):25-31.
49. Trofa D, Smith EL, Shah V, Shikora S. Total weight loss associated with increased physical activity after bariatric surgery may increase the need for total joint arthroplasty. Surg Obes Relat Dis. 2014;10(2):335-339.
50. Parvizi J, Trousdale RT, Sarr MG. Total joint arthroplasty in patients surgically treated for morbid obesity. J Arthroplasty. 2000;15(8):1003-1008.