User login
Smoking, Obesity Responsible for Shorter U.S. Life Spans
The life expectancy of Americans falls short compared to that of their counterparts in other high-income countries, and smoking and obesity are key contributors to the difference, the National Research Council of the National Academies reported Jan. 25.
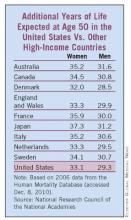
The life expectancy at birth for U.S. men increased from 65 years in 1950 to 76 years in 2006; for U.S. women, it increased from 71 to 81 years. Similarly, life expectancy at age 50 for men in the U.S. increased from 23 to 29 years. For American women, that figure rose from 27 to 33 years. Still, the improved life expectancy in the United States –the world’s top spender on health care -- fell below that of approximately nine other countries, including Australia, Japan, and Canada. (See graphic.)
The National Council on Aging commissioned the report, "Explaining Divergent Levels of Longevity in High-Income Countries," to identify factors behind the differences in life expectancy. The report focused on life expectancy at age 50, because at least 90% of newborns in high-income countries now survive to age 50 years. The data were based primarily on an analysis of cause-of-death statistics.
"Smoking appears to be responsible for a good deal of the divergence in female life expectancy," according to the report. The researchers estimated that 78% of the difference in life expectancy between American women and those in other high-income countries was attributable to smoking. Similarly, among men, smoking accounted for 41% of the difference.
The reduction in smoking in the United States over the past 20 years is likely to pay off in improved longevity trends in future decades, the researchers noted. A reduction or increase in smoking rates appears to take 20 to 30 years to impact mortality, they added.
Obesity also plays a significant role in the lagging U.S. longevity. Based on data from several studies, obesity accounts for approximately 20%-35% of the difference in longevity between Americans and residents of countries.
Physical inactivity, social integration, and healthcare systems also likely contribute to increased mortality and differences in life expectancy among countries, but evaluation of these risk factors has been limited to observational studies, the researchers noted.
The report was limited by a lack of markers to directly identify the impact on longevity of risk factors other than smoking, including obesity, physical inactivity, and stress, the researchers said.
The National Research Council is the principal operating agency of the National Academy of Sciences and the National Academy of Engineering, which are private, nonprofit institutions. The report is available for purchase from the National Academies Press.
The life expectancy of Americans falls short compared to that of their counterparts in other high-income countries, and smoking and obesity are key contributors to the difference, the National Research Council of the National Academies reported Jan. 25.
The life expectancy at birth for U.S. men increased from 65 years in 1950 to 76 years in 2006; for U.S. women, it increased from 71 to 81 years. Similarly, life expectancy at age 50 for men in the U.S. increased from 23 to 29 years. For American women, that figure rose from 27 to 33 years. Still, the improved life expectancy in the United States –the world’s top spender on health care -- fell below that of approximately nine other countries, including Australia, Japan, and Canada. (See graphic.)
The National Council on Aging commissioned the report, "Explaining Divergent Levels of Longevity in High-Income Countries," to identify factors behind the differences in life expectancy. The report focused on life expectancy at age 50, because at least 90% of newborns in high-income countries now survive to age 50 years. The data were based primarily on an analysis of cause-of-death statistics.
"Smoking appears to be responsible for a good deal of the divergence in female life expectancy," according to the report. The researchers estimated that 78% of the difference in life expectancy between American women and those in other high-income countries was attributable to smoking. Similarly, among men, smoking accounted for 41% of the difference.
The reduction in smoking in the United States over the past 20 years is likely to pay off in improved longevity trends in future decades, the researchers noted. A reduction or increase in smoking rates appears to take 20 to 30 years to impact mortality, they added.
Obesity also plays a significant role in the lagging U.S. longevity. Based on data from several studies, obesity accounts for approximately 20%-35% of the difference in longevity between Americans and residents of countries.
Physical inactivity, social integration, and healthcare systems also likely contribute to increased mortality and differences in life expectancy among countries, but evaluation of these risk factors has been limited to observational studies, the researchers noted.
The report was limited by a lack of markers to directly identify the impact on longevity of risk factors other than smoking, including obesity, physical inactivity, and stress, the researchers said.
The National Research Council is the principal operating agency of the National Academy of Sciences and the National Academy of Engineering, which are private, nonprofit institutions. The report is available for purchase from the National Academies Press.
The life expectancy of Americans falls short compared to that of their counterparts in other high-income countries, and smoking and obesity are key contributors to the difference, the National Research Council of the National Academies reported Jan. 25.
The life expectancy at birth for U.S. men increased from 65 years in 1950 to 76 years in 2006; for U.S. women, it increased from 71 to 81 years. Similarly, life expectancy at age 50 for men in the U.S. increased from 23 to 29 years. For American women, that figure rose from 27 to 33 years. Still, the improved life expectancy in the United States –the world’s top spender on health care -- fell below that of approximately nine other countries, including Australia, Japan, and Canada. (See graphic.)
The National Council on Aging commissioned the report, "Explaining Divergent Levels of Longevity in High-Income Countries," to identify factors behind the differences in life expectancy. The report focused on life expectancy at age 50, because at least 90% of newborns in high-income countries now survive to age 50 years. The data were based primarily on an analysis of cause-of-death statistics.
"Smoking appears to be responsible for a good deal of the divergence in female life expectancy," according to the report. The researchers estimated that 78% of the difference in life expectancy between American women and those in other high-income countries was attributable to smoking. Similarly, among men, smoking accounted for 41% of the difference.
The reduction in smoking in the United States over the past 20 years is likely to pay off in improved longevity trends in future decades, the researchers noted. A reduction or increase in smoking rates appears to take 20 to 30 years to impact mortality, they added.
Obesity also plays a significant role in the lagging U.S. longevity. Based on data from several studies, obesity accounts for approximately 20%-35% of the difference in longevity between Americans and residents of countries.
Physical inactivity, social integration, and healthcare systems also likely contribute to increased mortality and differences in life expectancy among countries, but evaluation of these risk factors has been limited to observational studies, the researchers noted.
The report was limited by a lack of markers to directly identify the impact on longevity of risk factors other than smoking, including obesity, physical inactivity, and stress, the researchers said.
The National Research Council is the principal operating agency of the National Academy of Sciences and the National Academy of Engineering, which are private, nonprofit institutions. The report is available for purchase from the National Academies Press.
FROM THE NATIONAL RESEARCH COUNCIL
AHA: More Than One-Third of U.S. Could Have Cardiovascular Disease by 2030
WASHINGTON – Approximately 40% of the United States population could have some form of cardiovascular disease by the year 2030, based on data from a prediction model created by the American Heart Association. The findings were published online on Jan. 24 in an American Heart Association policy statement in Circulation.
If there’s a silver lining in these figures, it is that they are projections," Nancy Brown, chief executive officer of the AHA, said at a press conference. However, if current policies and prevention strategies go unchanged, the United States is facing "a cardiovascular crisis of alarming proportions," she said.
The aging U.S. population and the increase in medical spending are the main forces driving the disease prevalence and cost, wrote Dr. Paul Heidenreich, of the VA Palo Alto (Calif.) Health Care System, and colleagues.
Without changes in current prevention and treatment trends, the prevalence of cardiovascular disease in the United States will increase by about 10% over the next 20 years, and direct medical costs of cardiovascular disease will triple, from $273 billion to $818 billion, according to the policy statement.
The AHA statement projects an additional 27 million Americans with hypertension, 8 million with coronary heart disease, 4 million with stroke, and 3 million with heart failure between 2010 and 2030 (Circulation 2011 Jan. 24 [Epub doi: 10.1161/CIR.0b013e31820a55f5]).
According to the projections, hypertension will be the most expensive component of cardiovascular disease (CVD), with an estimated annual direct medical cost of $200 billion by 2030. The estimated direct medical cost for stroke is $96 billion, compared with $28 billion in 2010, but stroke represents the greatest relative increase in costs over the next 20 years (238%).
In addition, the indirect costs of all types of cardiovascular disease could increase by 61% (from $172 billion in 2010 to $276 billion in 2030).
However, previous studies have shown that many CVD cases are preventable, and individuals who maintain a healthy lifestyle and favorable levels of atherosclerotic risk are less likely to develop CVD. "Therefore, a greater focus on prevention may alter these CVD projections in the future," according to the statement.
Guidelines have been shown to have "a substantial impact on prevention and treatment and will be an important tool for limiting the burden of CVD," according to the statement. The AHA, the American College of Cardiology, and other organizations have previously published prevention-oriented CVD guidelines, but the implementation of such guidelines is often slow, the writing group noted.
Other factors that could hamper the improvement of CVD risk factors include a reported shortage of cardiologists, they added. Other shortages exist in nursing, pharmacy, and primary care, all of which are needed for a team approach to preventing CVD.
The take-home message for cardiologists is that they can "expect to see more demand for their services," Dr. Heidenreich said in an interview. In addition, primary care physicians will be seeing more patients with forms of heart disease. But the solution includes increasing the number of health professionals across all fields, not only cardiology, said Dr. Heidenreich. "The whole medical complex is insufficient to meet the demand" of the potential increases in CVD, he emphasized.
But, "through a combination of improved prevention of risk factors, and treatment of established risk factors, the dire projection of the health and economic impact of CVD can be diminished," the statement concluded.
The projections of CVD prevalence were based on data from the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2006 and Census Bureau projections from 2010 to 2030. Projections of direct medical costs of CVD were based on data from the Medical Expenditure Panel Survey from 2001 to 2005. Indirect costs of CVD included lost productivity from morbidity and early mortality.
Dr. Heidenreich, chair of the writing group, had no financial conflicts to disclose. Several members of the writing group disclosed research funding from pharmaceutical companies including Boston Scientific, Eli Lilly and Company, Pfizer, Procter & Gamble, and Medtronic. Some members disclosed serving as consultants or advisory board members to companies including Sanofi-Aventis, Bristol Myers Squibb, and Daiichi Sankyo. Some members of the group received research support from organizations including the National Institutes of Health and the National Heart, Lung and Blood Institute.
WASHINGTON – Approximately 40% of the United States population could have some form of cardiovascular disease by the year 2030, based on data from a prediction model created by the American Heart Association. The findings were published online on Jan. 24 in an American Heart Association policy statement in Circulation.
If there’s a silver lining in these figures, it is that they are projections," Nancy Brown, chief executive officer of the AHA, said at a press conference. However, if current policies and prevention strategies go unchanged, the United States is facing "a cardiovascular crisis of alarming proportions," she said.
The aging U.S. population and the increase in medical spending are the main forces driving the disease prevalence and cost, wrote Dr. Paul Heidenreich, of the VA Palo Alto (Calif.) Health Care System, and colleagues.
Without changes in current prevention and treatment trends, the prevalence of cardiovascular disease in the United States will increase by about 10% over the next 20 years, and direct medical costs of cardiovascular disease will triple, from $273 billion to $818 billion, according to the policy statement.
The AHA statement projects an additional 27 million Americans with hypertension, 8 million with coronary heart disease, 4 million with stroke, and 3 million with heart failure between 2010 and 2030 (Circulation 2011 Jan. 24 [Epub doi: 10.1161/CIR.0b013e31820a55f5]).
According to the projections, hypertension will be the most expensive component of cardiovascular disease (CVD), with an estimated annual direct medical cost of $200 billion by 2030. The estimated direct medical cost for stroke is $96 billion, compared with $28 billion in 2010, but stroke represents the greatest relative increase in costs over the next 20 years (238%).
In addition, the indirect costs of all types of cardiovascular disease could increase by 61% (from $172 billion in 2010 to $276 billion in 2030).
However, previous studies have shown that many CVD cases are preventable, and individuals who maintain a healthy lifestyle and favorable levels of atherosclerotic risk are less likely to develop CVD. "Therefore, a greater focus on prevention may alter these CVD projections in the future," according to the statement.
Guidelines have been shown to have "a substantial impact on prevention and treatment and will be an important tool for limiting the burden of CVD," according to the statement. The AHA, the American College of Cardiology, and other organizations have previously published prevention-oriented CVD guidelines, but the implementation of such guidelines is often slow, the writing group noted.
Other factors that could hamper the improvement of CVD risk factors include a reported shortage of cardiologists, they added. Other shortages exist in nursing, pharmacy, and primary care, all of which are needed for a team approach to preventing CVD.
The take-home message for cardiologists is that they can "expect to see more demand for their services," Dr. Heidenreich said in an interview. In addition, primary care physicians will be seeing more patients with forms of heart disease. But the solution includes increasing the number of health professionals across all fields, not only cardiology, said Dr. Heidenreich. "The whole medical complex is insufficient to meet the demand" of the potential increases in CVD, he emphasized.
But, "through a combination of improved prevention of risk factors, and treatment of established risk factors, the dire projection of the health and economic impact of CVD can be diminished," the statement concluded.
The projections of CVD prevalence were based on data from the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2006 and Census Bureau projections from 2010 to 2030. Projections of direct medical costs of CVD were based on data from the Medical Expenditure Panel Survey from 2001 to 2005. Indirect costs of CVD included lost productivity from morbidity and early mortality.
Dr. Heidenreich, chair of the writing group, had no financial conflicts to disclose. Several members of the writing group disclosed research funding from pharmaceutical companies including Boston Scientific, Eli Lilly and Company, Pfizer, Procter & Gamble, and Medtronic. Some members disclosed serving as consultants or advisory board members to companies including Sanofi-Aventis, Bristol Myers Squibb, and Daiichi Sankyo. Some members of the group received research support from organizations including the National Institutes of Health and the National Heart, Lung and Blood Institute.
WASHINGTON – Approximately 40% of the United States population could have some form of cardiovascular disease by the year 2030, based on data from a prediction model created by the American Heart Association. The findings were published online on Jan. 24 in an American Heart Association policy statement in Circulation.
If there’s a silver lining in these figures, it is that they are projections," Nancy Brown, chief executive officer of the AHA, said at a press conference. However, if current policies and prevention strategies go unchanged, the United States is facing "a cardiovascular crisis of alarming proportions," she said.
The aging U.S. population and the increase in medical spending are the main forces driving the disease prevalence and cost, wrote Dr. Paul Heidenreich, of the VA Palo Alto (Calif.) Health Care System, and colleagues.
Without changes in current prevention and treatment trends, the prevalence of cardiovascular disease in the United States will increase by about 10% over the next 20 years, and direct medical costs of cardiovascular disease will triple, from $273 billion to $818 billion, according to the policy statement.
The AHA statement projects an additional 27 million Americans with hypertension, 8 million with coronary heart disease, 4 million with stroke, and 3 million with heart failure between 2010 and 2030 (Circulation 2011 Jan. 24 [Epub doi: 10.1161/CIR.0b013e31820a55f5]).
According to the projections, hypertension will be the most expensive component of cardiovascular disease (CVD), with an estimated annual direct medical cost of $200 billion by 2030. The estimated direct medical cost for stroke is $96 billion, compared with $28 billion in 2010, but stroke represents the greatest relative increase in costs over the next 20 years (238%).
In addition, the indirect costs of all types of cardiovascular disease could increase by 61% (from $172 billion in 2010 to $276 billion in 2030).
However, previous studies have shown that many CVD cases are preventable, and individuals who maintain a healthy lifestyle and favorable levels of atherosclerotic risk are less likely to develop CVD. "Therefore, a greater focus on prevention may alter these CVD projections in the future," according to the statement.
Guidelines have been shown to have "a substantial impact on prevention and treatment and will be an important tool for limiting the burden of CVD," according to the statement. The AHA, the American College of Cardiology, and other organizations have previously published prevention-oriented CVD guidelines, but the implementation of such guidelines is often slow, the writing group noted.
Other factors that could hamper the improvement of CVD risk factors include a reported shortage of cardiologists, they added. Other shortages exist in nursing, pharmacy, and primary care, all of which are needed for a team approach to preventing CVD.
The take-home message for cardiologists is that they can "expect to see more demand for their services," Dr. Heidenreich said in an interview. In addition, primary care physicians will be seeing more patients with forms of heart disease. But the solution includes increasing the number of health professionals across all fields, not only cardiology, said Dr. Heidenreich. "The whole medical complex is insufficient to meet the demand" of the potential increases in CVD, he emphasized.
But, "through a combination of improved prevention of risk factors, and treatment of established risk factors, the dire projection of the health and economic impact of CVD can be diminished," the statement concluded.
The projections of CVD prevalence were based on data from the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2006 and Census Bureau projections from 2010 to 2030. Projections of direct medical costs of CVD were based on data from the Medical Expenditure Panel Survey from 2001 to 2005. Indirect costs of CVD included lost productivity from morbidity and early mortality.
Dr. Heidenreich, chair of the writing group, had no financial conflicts to disclose. Several members of the writing group disclosed research funding from pharmaceutical companies including Boston Scientific, Eli Lilly and Company, Pfizer, Procter & Gamble, and Medtronic. Some members disclosed serving as consultants or advisory board members to companies including Sanofi-Aventis, Bristol Myers Squibb, and Daiichi Sankyo. Some members of the group received research support from organizations including the National Institutes of Health and the National Heart, Lung and Blood Institute.
AHA: More Than One-Third of U.S. Could Have Cardiovascular Disease by 2030
WASHINGTON - Approximately 40% of the United States population could have some form of cardiovascular disease by the year 2030, based on data from a prediction model created by the American Heart Association. The findings were published online on Jan. 24 in an American Heart Association policy statement in Circulation.
If there’s a silver lining in these figures, it is that they are projections," Nancy Brown, chief executive officer of the AHA, said at a press conference. However, if current policies and prevention strategies go unchanged, the United States is facing "a cardiovascular crisis of alarming proportions," she said.
The aging U.S. population and the increase in medical spending are the main forces driving the disease prevalence and cost, wrote Dr. Paul Heidenreich, of the VA Palo Alto (Calif.) Health Care System, and colleagues.
Without changes in current prevention and treatment trends, the prevalence of cardiovascular disease in the United States will increase by about 10% over the next 20 years, and direct medical costs of cardiovascular disease will triple, from $273 billion to $818 billion, according to the policy statement.
The AHA statement projects an additional 27 million Americans with hypertension, 8 million with coronary heart disease, 4 million with stroke, and 3 million with heart failure between 2010 and 2030 (Circulation 2011 Jan. 24 [Epub doi: 10.1161/CIR.0b013e31820a55f5]).
According to the projections, hypertension will be the most expensive component of cardiovascular disease (CVD), with an estimated annual direct medical cost of $200 billion by 2030. The estimated direct medical cost for stroke is $96 billion, compared with $28 billion in 2010, but stroke represents the greatest relative increase in costs over the next 20 years (238%).
In addition, the indirect costs of all types of cardiovascular disease could increase by 61% (from $172 billion in 2010 to $276 billion in 2030).
However, previous studies have shown that many CVD cases are preventable, and individuals who maintain a healthy lifestyle and favorable levels of atherosclerotic risk are less likely to develop CVD. "Therefore, a greater focus on prevention may alter these CVD projections in the future," according to the statement.
Guidelines have been shown to have "a substantial impact on prevention and treatment and will be an important tool for limiting the burden of CVD," according to the statement. The AHA, the American College of Cardiology, and other organizations have previously published prevention-oriented CVD guidelines, but the implementation of such guidelines is often slow, the writing group noted.
Other factors that could hamper the improvement of CVD risk factors include a reported shortage of cardiologists, they added. Other shortages exist in nursing, pharmacy, and primary care, all of which are needed for a team approach to preventing CVD.
The take-home message for cardiologists is that they can "expect to see more demand for their services," Dr. Heidenreich said in an interview. In addition, primary care physicians will be seeing more patients with forms of heart disease. But the solution includes increasing the number of health professionals across all fields, not only cardiology, said Dr. Heidenreich. "The whole medical complex is insufficient to meet the demand" of the potential increases in CVD, he emphasized.
But, "through a combination of improved prevention of risk factors, and treatment of established risk factors, the dire projection of the health and economic impact of CVD can be diminished," the statement concluded.
The projections of CVD prevalence were based on data from the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2006 and Census Bureau projections from 2010 to 2030. Projections of direct medical costs of CVD were based on data from the Medical Expenditure Panel Survey from 2001 to 2005. Indirect costs of CVD included lost productivity from morbidity and early mortality.
Dr. Heidenreich, chair of the writing group, had no financial conflicts to disclose. Several members of the writing group disclosed research funding from pharmaceutical companies including Boston Scientific, Eli Lilly and Company, Pfizer, Procter & Gamble, and Medtronic. Some members disclosed serving as consultants or advisory board members to companies including Sanofi-Aventis, Bristol Myers Squibb, and Daiichi Sankyo. Some members of the group received research support from organizations including the National Institutes of Health and the National Heart, Lung and Blood Institute.
WASHINGTON - Approximately 40% of the United States population could have some form of cardiovascular disease by the year 2030, based on data from a prediction model created by the American Heart Association. The findings were published online on Jan. 24 in an American Heart Association policy statement in Circulation.
If there’s a silver lining in these figures, it is that they are projections," Nancy Brown, chief executive officer of the AHA, said at a press conference. However, if current policies and prevention strategies go unchanged, the United States is facing "a cardiovascular crisis of alarming proportions," she said.
The aging U.S. population and the increase in medical spending are the main forces driving the disease prevalence and cost, wrote Dr. Paul Heidenreich, of the VA Palo Alto (Calif.) Health Care System, and colleagues.
Without changes in current prevention and treatment trends, the prevalence of cardiovascular disease in the United States will increase by about 10% over the next 20 years, and direct medical costs of cardiovascular disease will triple, from $273 billion to $818 billion, according to the policy statement.
The AHA statement projects an additional 27 million Americans with hypertension, 8 million with coronary heart disease, 4 million with stroke, and 3 million with heart failure between 2010 and 2030 (Circulation 2011 Jan. 24 [Epub doi: 10.1161/CIR.0b013e31820a55f5]).
According to the projections, hypertension will be the most expensive component of cardiovascular disease (CVD), with an estimated annual direct medical cost of $200 billion by 2030. The estimated direct medical cost for stroke is $96 billion, compared with $28 billion in 2010, but stroke represents the greatest relative increase in costs over the next 20 years (238%).
In addition, the indirect costs of all types of cardiovascular disease could increase by 61% (from $172 billion in 2010 to $276 billion in 2030).
However, previous studies have shown that many CVD cases are preventable, and individuals who maintain a healthy lifestyle and favorable levels of atherosclerotic risk are less likely to develop CVD. "Therefore, a greater focus on prevention may alter these CVD projections in the future," according to the statement.
Guidelines have been shown to have "a substantial impact on prevention and treatment and will be an important tool for limiting the burden of CVD," according to the statement. The AHA, the American College of Cardiology, and other organizations have previously published prevention-oriented CVD guidelines, but the implementation of such guidelines is often slow, the writing group noted.
Other factors that could hamper the improvement of CVD risk factors include a reported shortage of cardiologists, they added. Other shortages exist in nursing, pharmacy, and primary care, all of which are needed for a team approach to preventing CVD.
The take-home message for cardiologists is that they can "expect to see more demand for their services," Dr. Heidenreich said in an interview. In addition, primary care physicians will be seeing more patients with forms of heart disease. But the solution includes increasing the number of health professionals across all fields, not only cardiology, said Dr. Heidenreich. "The whole medical complex is insufficient to meet the demand" of the potential increases in CVD, he emphasized.
But, "through a combination of improved prevention of risk factors, and treatment of established risk factors, the dire projection of the health and economic impact of CVD can be diminished," the statement concluded.
The projections of CVD prevalence were based on data from the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2006 and Census Bureau projections from 2010 to 2030. Projections of direct medical costs of CVD were based on data from the Medical Expenditure Panel Survey from 2001 to 2005. Indirect costs of CVD included lost productivity from morbidity and early mortality.
Dr. Heidenreich, chair of the writing group, had no financial conflicts to disclose. Several members of the writing group disclosed research funding from pharmaceutical companies including Boston Scientific, Eli Lilly and Company, Pfizer, Procter & Gamble, and Medtronic. Some members disclosed serving as consultants or advisory board members to companies including Sanofi-Aventis, Bristol Myers Squibb, and Daiichi Sankyo. Some members of the group received research support from organizations including the National Institutes of Health and the National Heart, Lung and Blood Institute.
WASHINGTON - Approximately 40% of the United States population could have some form of cardiovascular disease by the year 2030, based on data from a prediction model created by the American Heart Association. The findings were published online on Jan. 24 in an American Heart Association policy statement in Circulation.
If there’s a silver lining in these figures, it is that they are projections," Nancy Brown, chief executive officer of the AHA, said at a press conference. However, if current policies and prevention strategies go unchanged, the United States is facing "a cardiovascular crisis of alarming proportions," she said.
The aging U.S. population and the increase in medical spending are the main forces driving the disease prevalence and cost, wrote Dr. Paul Heidenreich, of the VA Palo Alto (Calif.) Health Care System, and colleagues.
Without changes in current prevention and treatment trends, the prevalence of cardiovascular disease in the United States will increase by about 10% over the next 20 years, and direct medical costs of cardiovascular disease will triple, from $273 billion to $818 billion, according to the policy statement.
The AHA statement projects an additional 27 million Americans with hypertension, 8 million with coronary heart disease, 4 million with stroke, and 3 million with heart failure between 2010 and 2030 (Circulation 2011 Jan. 24 [Epub doi: 10.1161/CIR.0b013e31820a55f5]).
According to the projections, hypertension will be the most expensive component of cardiovascular disease (CVD), with an estimated annual direct medical cost of $200 billion by 2030. The estimated direct medical cost for stroke is $96 billion, compared with $28 billion in 2010, but stroke represents the greatest relative increase in costs over the next 20 years (238%).
In addition, the indirect costs of all types of cardiovascular disease could increase by 61% (from $172 billion in 2010 to $276 billion in 2030).
However, previous studies have shown that many CVD cases are preventable, and individuals who maintain a healthy lifestyle and favorable levels of atherosclerotic risk are less likely to develop CVD. "Therefore, a greater focus on prevention may alter these CVD projections in the future," according to the statement.
Guidelines have been shown to have "a substantial impact on prevention and treatment and will be an important tool for limiting the burden of CVD," according to the statement. The AHA, the American College of Cardiology, and other organizations have previously published prevention-oriented CVD guidelines, but the implementation of such guidelines is often slow, the writing group noted.
Other factors that could hamper the improvement of CVD risk factors include a reported shortage of cardiologists, they added. Other shortages exist in nursing, pharmacy, and primary care, all of which are needed for a team approach to preventing CVD.
The take-home message for cardiologists is that they can "expect to see more demand for their services," Dr. Heidenreich said in an interview. In addition, primary care physicians will be seeing more patients with forms of heart disease. But the solution includes increasing the number of health professionals across all fields, not only cardiology, said Dr. Heidenreich. "The whole medical complex is insufficient to meet the demand" of the potential increases in CVD, he emphasized.
But, "through a combination of improved prevention of risk factors, and treatment of established risk factors, the dire projection of the health and economic impact of CVD can be diminished," the statement concluded.
The projections of CVD prevalence were based on data from the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2006 and Census Bureau projections from 2010 to 2030. Projections of direct medical costs of CVD were based on data from the Medical Expenditure Panel Survey from 2001 to 2005. Indirect costs of CVD included lost productivity from morbidity and early mortality.
Dr. Heidenreich, chair of the writing group, had no financial conflicts to disclose. Several members of the writing group disclosed research funding from pharmaceutical companies including Boston Scientific, Eli Lilly and Company, Pfizer, Procter & Gamble, and Medtronic. Some members disclosed serving as consultants or advisory board members to companies including Sanofi-Aventis, Bristol Myers Squibb, and Daiichi Sankyo. Some members of the group received research support from organizations including the National Institutes of Health and the National Heart, Lung and Blood Institute.
Habitual Heavy Drinking Increases Atrial Fibrillation Risk
Habitual heavy drinking is associated with a 51% increased risk of atrial fibrillation, according to findings from a meta-analysis of more than 130,000 adults, published online Jan. 17.
The impact of occasional heavy alcohol intake on AF, known as "holiday heart syndrome," is well known. The impact of consistent heavy alcohol intake on AF risk, however, has not been well studied, said Dr. Satoru Kodama of the University of Tsukuba Institute of Clinical Medicine in Ibaraki, Japan.
Dr. Kodama and colleagues analyzed data from 14 studies, involving a total of 130,820 participants and 7,558 cases of AF. Across the studies, a common scale of grams per day was used as the standard measure of alcohol intake.
Overall, participants who consumed the most alcohol were significantly more likely to have AF than were those who consumed the least, based on a pooled assessment of odds ratio and relative risk (1.51).
The lowest amount of alcohol consumed in the highest intake category for each of the studies ranged from 1.5 to 6 drinks daily.
Within the highest alcohol intake category, the AF risk was not significantly different between participants who consumed fewer than 4 alcoholic drinks daily, defined as 48 g (OR/RR 1.32), and those who had 4 or more drinks per day (1.74) (J. Am. Coll. Cardiol. 2011;57:427-36).
From an analysis of nine of the studies (involving 126,051 participants and 6,341 cases of AF), the researchers found a significant dose-response relationship between alcohol intake and AF risk, which translated into an increase in relative risk of 1.08 per 10 g of alcohol consumed per day.
Stratified analyses of the data, according to study methods, supported the significant association between the highest category of alcohol intake and AF risk.
The study is the first systematic review of habitual alcohol consumption and AF risk. Although the meta-analysis cannot prove causality, the researchers proposed two hypotheses for a cause and effect relationship. One theory, suggested by biological studies, is that high alcohol intake makes it more difficult for the body to maintain a normal heart rhythm.
"Another speculation is based on reports suggesting that the development of chronic heart failure accompanied by long-term alcohol consumption may result in elevated AF risk," the researchers said.
The results suggest that avoiding alcohol completely, as opposed to drinking moderately, is the best way to reduce AF risk, the researchers concluded.
The analysis was limited by the inability to adjust for various confounders across multiple studies, including the presence of hypertension, diabetes, and obstructive sleep apnea, they wrote. In addition, the strength of the findings is limited by the various definitions of heavy drinking, the lack of information about the validation of alcohol intake, and limited consideration of racial differences among study participants.
Further investigation is needed to determine a possible causal relationship between daily alcohol intake and AF risk, the authors wrote.
The researchers reported having no financial conflicts of interest.
Habitual heavy drinking is associated with a 51% increased risk of atrial fibrillation, according to findings from a meta-analysis of more than 130,000 adults, published online Jan. 17.
The impact of occasional heavy alcohol intake on AF, known as "holiday heart syndrome," is well known. The impact of consistent heavy alcohol intake on AF risk, however, has not been well studied, said Dr. Satoru Kodama of the University of Tsukuba Institute of Clinical Medicine in Ibaraki, Japan.
Dr. Kodama and colleagues analyzed data from 14 studies, involving a total of 130,820 participants and 7,558 cases of AF. Across the studies, a common scale of grams per day was used as the standard measure of alcohol intake.
Overall, participants who consumed the most alcohol were significantly more likely to have AF than were those who consumed the least, based on a pooled assessment of odds ratio and relative risk (1.51).
The lowest amount of alcohol consumed in the highest intake category for each of the studies ranged from 1.5 to 6 drinks daily.
Within the highest alcohol intake category, the AF risk was not significantly different between participants who consumed fewer than 4 alcoholic drinks daily, defined as 48 g (OR/RR 1.32), and those who had 4 or more drinks per day (1.74) (J. Am. Coll. Cardiol. 2011;57:427-36).
From an analysis of nine of the studies (involving 126,051 participants and 6,341 cases of AF), the researchers found a significant dose-response relationship between alcohol intake and AF risk, which translated into an increase in relative risk of 1.08 per 10 g of alcohol consumed per day.
Stratified analyses of the data, according to study methods, supported the significant association between the highest category of alcohol intake and AF risk.
The study is the first systematic review of habitual alcohol consumption and AF risk. Although the meta-analysis cannot prove causality, the researchers proposed two hypotheses for a cause and effect relationship. One theory, suggested by biological studies, is that high alcohol intake makes it more difficult for the body to maintain a normal heart rhythm.
"Another speculation is based on reports suggesting that the development of chronic heart failure accompanied by long-term alcohol consumption may result in elevated AF risk," the researchers said.
The results suggest that avoiding alcohol completely, as opposed to drinking moderately, is the best way to reduce AF risk, the researchers concluded.
The analysis was limited by the inability to adjust for various confounders across multiple studies, including the presence of hypertension, diabetes, and obstructive sleep apnea, they wrote. In addition, the strength of the findings is limited by the various definitions of heavy drinking, the lack of information about the validation of alcohol intake, and limited consideration of racial differences among study participants.
Further investigation is needed to determine a possible causal relationship between daily alcohol intake and AF risk, the authors wrote.
The researchers reported having no financial conflicts of interest.
Habitual heavy drinking is associated with a 51% increased risk of atrial fibrillation, according to findings from a meta-analysis of more than 130,000 adults, published online Jan. 17.
The impact of occasional heavy alcohol intake on AF, known as "holiday heart syndrome," is well known. The impact of consistent heavy alcohol intake on AF risk, however, has not been well studied, said Dr. Satoru Kodama of the University of Tsukuba Institute of Clinical Medicine in Ibaraki, Japan.
Dr. Kodama and colleagues analyzed data from 14 studies, involving a total of 130,820 participants and 7,558 cases of AF. Across the studies, a common scale of grams per day was used as the standard measure of alcohol intake.
Overall, participants who consumed the most alcohol were significantly more likely to have AF than were those who consumed the least, based on a pooled assessment of odds ratio and relative risk (1.51).
The lowest amount of alcohol consumed in the highest intake category for each of the studies ranged from 1.5 to 6 drinks daily.
Within the highest alcohol intake category, the AF risk was not significantly different between participants who consumed fewer than 4 alcoholic drinks daily, defined as 48 g (OR/RR 1.32), and those who had 4 or more drinks per day (1.74) (J. Am. Coll. Cardiol. 2011;57:427-36).
From an analysis of nine of the studies (involving 126,051 participants and 6,341 cases of AF), the researchers found a significant dose-response relationship between alcohol intake and AF risk, which translated into an increase in relative risk of 1.08 per 10 g of alcohol consumed per day.
Stratified analyses of the data, according to study methods, supported the significant association between the highest category of alcohol intake and AF risk.
The study is the first systematic review of habitual alcohol consumption and AF risk. Although the meta-analysis cannot prove causality, the researchers proposed two hypotheses for a cause and effect relationship. One theory, suggested by biological studies, is that high alcohol intake makes it more difficult for the body to maintain a normal heart rhythm.
"Another speculation is based on reports suggesting that the development of chronic heart failure accompanied by long-term alcohol consumption may result in elevated AF risk," the researchers said.
The results suggest that avoiding alcohol completely, as opposed to drinking moderately, is the best way to reduce AF risk, the researchers concluded.
The analysis was limited by the inability to adjust for various confounders across multiple studies, including the presence of hypertension, diabetes, and obstructive sleep apnea, they wrote. In addition, the strength of the findings is limited by the various definitions of heavy drinking, the lack of information about the validation of alcohol intake, and limited consideration of racial differences among study participants.
Further investigation is needed to determine a possible causal relationship between daily alcohol intake and AF risk, the authors wrote.
The researchers reported having no financial conflicts of interest.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Habitual Heavy Drinking Increases Atrial Fibrillation Risk
Habitual heavy drinking is associated with a 51% increased risk of atrial fibrillation, according to findings from a meta-analysis of more than 130,000 adults, published online Jan. 17.
The impact of occasional heavy alcohol intake on AF, known as "holiday heart syndrome," is well known. The impact of consistent heavy alcohol intake on AF risk, however, has not been well studied, said Dr. Satoru Kodama of the University of Tsukuba Institute of Clinical Medicine in Ibaraki, Japan.
Dr. Kodama and colleagues analyzed data from 14 studies, involving a total of 130,820 participants and 7,558 cases of AF. Across the studies, a common scale of grams per day was used as the standard measure of alcohol intake.
Overall, participants who consumed the most alcohol were significantly more likely to have AF than were those who consumed the least, based on a pooled assessment of odds ratio and relative risk (1.51).
The lowest amount of alcohol consumed in the highest intake category for each of the studies ranged from 1.5 to 6 drinks daily.
Within the highest alcohol intake category, the AF risk was not significantly different between participants who consumed fewer than 4 alcoholic drinks daily, defined as 48 g (OR/RR 1.32), and those who had 4 or more drinks per day (1.74) (J. Am. Coll. Cardiol. 2011;57:427-36).
From an analysis of nine of the studies (involving 126,051 participants and 6,341 cases of AF), the researchers found a significant dose-response relationship between alcohol intake and AF risk, which translated into an increase in relative risk of 1.08 per 10 g of alcohol consumed per day.
Stratified analyses of the data, according to study methods, supported the significant association between the highest category of alcohol intake and AF risk.
The study is the first systematic review of habitual alcohol consumption and AF risk. Although the meta-analysis cannot prove causality, the researchers proposed two hypotheses for a cause and effect relationship. One theory, suggested by biological studies, is that high alcohol intake makes it more difficult for the body to maintain a normal heart rhythm.
"Another speculation is based on reports suggesting that the development of chronic heart failure accompanied by long-term alcohol consumption may result in elevated AF risk," the researchers said.
The results suggest that avoiding alcohol completely, as opposed to drinking moderately, is the best way to reduce AF risk, the researchers concluded.
The analysis was limited by the inability to adjust for various confounders across multiple studies, including the presence of hypertension, diabetes, and obstructive sleep apnea, they wrote. In addition, the strength of the findings is limited by the various definitions of heavy drinking, the lack of information about the validation of alcohol intake, and limited consideration of racial differences among study participants.
Further investigation is needed to determine a possible causal relationship between daily alcohol intake and AF risk, the authors wrote.
The researchers reported having no financial conflicts of interest.
Habitual heavy drinking is associated with a 51% increased risk of atrial fibrillation, according to findings from a meta-analysis of more than 130,000 adults, published online Jan. 17.
The impact of occasional heavy alcohol intake on AF, known as "holiday heart syndrome," is well known. The impact of consistent heavy alcohol intake on AF risk, however, has not been well studied, said Dr. Satoru Kodama of the University of Tsukuba Institute of Clinical Medicine in Ibaraki, Japan.
Dr. Kodama and colleagues analyzed data from 14 studies, involving a total of 130,820 participants and 7,558 cases of AF. Across the studies, a common scale of grams per day was used as the standard measure of alcohol intake.
Overall, participants who consumed the most alcohol were significantly more likely to have AF than were those who consumed the least, based on a pooled assessment of odds ratio and relative risk (1.51).
The lowest amount of alcohol consumed in the highest intake category for each of the studies ranged from 1.5 to 6 drinks daily.
Within the highest alcohol intake category, the AF risk was not significantly different between participants who consumed fewer than 4 alcoholic drinks daily, defined as 48 g (OR/RR 1.32), and those who had 4 or more drinks per day (1.74) (J. Am. Coll. Cardiol. 2011;57:427-36).
From an analysis of nine of the studies (involving 126,051 participants and 6,341 cases of AF), the researchers found a significant dose-response relationship between alcohol intake and AF risk, which translated into an increase in relative risk of 1.08 per 10 g of alcohol consumed per day.
Stratified analyses of the data, according to study methods, supported the significant association between the highest category of alcohol intake and AF risk.
The study is the first systematic review of habitual alcohol consumption and AF risk. Although the meta-analysis cannot prove causality, the researchers proposed two hypotheses for a cause and effect relationship. One theory, suggested by biological studies, is that high alcohol intake makes it more difficult for the body to maintain a normal heart rhythm.
"Another speculation is based on reports suggesting that the development of chronic heart failure accompanied by long-term alcohol consumption may result in elevated AF risk," the researchers said.
The results suggest that avoiding alcohol completely, as opposed to drinking moderately, is the best way to reduce AF risk, the researchers concluded.
The analysis was limited by the inability to adjust for various confounders across multiple studies, including the presence of hypertension, diabetes, and obstructive sleep apnea, they wrote. In addition, the strength of the findings is limited by the various definitions of heavy drinking, the lack of information about the validation of alcohol intake, and limited consideration of racial differences among study participants.
Further investigation is needed to determine a possible causal relationship between daily alcohol intake and AF risk, the authors wrote.
The researchers reported having no financial conflicts of interest.
Habitual heavy drinking is associated with a 51% increased risk of atrial fibrillation, according to findings from a meta-analysis of more than 130,000 adults, published online Jan. 17.
The impact of occasional heavy alcohol intake on AF, known as "holiday heart syndrome," is well known. The impact of consistent heavy alcohol intake on AF risk, however, has not been well studied, said Dr. Satoru Kodama of the University of Tsukuba Institute of Clinical Medicine in Ibaraki, Japan.
Dr. Kodama and colleagues analyzed data from 14 studies, involving a total of 130,820 participants and 7,558 cases of AF. Across the studies, a common scale of grams per day was used as the standard measure of alcohol intake.
Overall, participants who consumed the most alcohol were significantly more likely to have AF than were those who consumed the least, based on a pooled assessment of odds ratio and relative risk (1.51).
The lowest amount of alcohol consumed in the highest intake category for each of the studies ranged from 1.5 to 6 drinks daily.
Within the highest alcohol intake category, the AF risk was not significantly different between participants who consumed fewer than 4 alcoholic drinks daily, defined as 48 g (OR/RR 1.32), and those who had 4 or more drinks per day (1.74) (J. Am. Coll. Cardiol. 2011;57:427-36).
From an analysis of nine of the studies (involving 126,051 participants and 6,341 cases of AF), the researchers found a significant dose-response relationship between alcohol intake and AF risk, which translated into an increase in relative risk of 1.08 per 10 g of alcohol consumed per day.
Stratified analyses of the data, according to study methods, supported the significant association between the highest category of alcohol intake and AF risk.
The study is the first systematic review of habitual alcohol consumption and AF risk. Although the meta-analysis cannot prove causality, the researchers proposed two hypotheses for a cause and effect relationship. One theory, suggested by biological studies, is that high alcohol intake makes it more difficult for the body to maintain a normal heart rhythm.
"Another speculation is based on reports suggesting that the development of chronic heart failure accompanied by long-term alcohol consumption may result in elevated AF risk," the researchers said.
The results suggest that avoiding alcohol completely, as opposed to drinking moderately, is the best way to reduce AF risk, the researchers concluded.
The analysis was limited by the inability to adjust for various confounders across multiple studies, including the presence of hypertension, diabetes, and obstructive sleep apnea, they wrote. In addition, the strength of the findings is limited by the various definitions of heavy drinking, the lack of information about the validation of alcohol intake, and limited consideration of racial differences among study participants.
Further investigation is needed to determine a possible causal relationship between daily alcohol intake and AF risk, the authors wrote.
The researchers reported having no financial conflicts of interest.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Major Finding: Individuals who consumed the most alcohol (1.5 to 6 drinks daily) were significantly more likely to have atrial fibrillation compared with those who consumed the least, based on a pooled assessment of odds ratio and relative risk (1.51).
Data Source: A meta-analysis of 14 studies involving a total of 130,820 participants and 7,558 AF cases.
Disclosures: The researchers reported having no financial conflicts of interest.
Enoxaparin Equals Aspirin for Preventing VTE in Myeloma
ORLANDO – Enoxaparin and aspirin were equally effective at preventing thrombotic events in young, newly diagnosed myeloma patients who were treated with a lenalidomide-based regimen in a randomized trial.
Previous studies have shown that this patient population is at least three times as likely to develop thrombosis as patients not on a lenalidomide-based regimen, said Dr. Alberto Rocci of the University of Torino (Italy). "Randomized trials comparing different therapies for [venous thromboembolism] prophylaxis in young, newly diagnosed myeloma patients are still lacking," he said at the annual meeting of the American Society of Hematology.
[Check out our comprehensive coverage of the American Society of Hematology's annual meeting.]
In this study, Dr. Rocci and his colleagues enrolled 402 patients younger than 65 years from 62 cancer centers. All patients had symptomatic and measurable disease, with organ damage.
All patients underwent four 28-day cycles of lenalidomide (25 mg/day on days 1-21) and dexamethasone (40 mg/day on days 1, 8, 15, and 22). After this treatment, 202 patients were randomized to six 28-day cycles of melphalan (0.18 mg/kg on days 1-4), prednisone (2 mg/kg on days 1-4), and lenalidomide (10 mg/day on days 1-21); and 200 patients were randomized to two courses of melphalan (200 mg/m2, plus stem cell support). These groups were designated MPR and MEL 200, respectively.
In this substudy, the researchers further randomized eligible patients who received lenalidomide during induction and in the MPR consolidation regimen: 166 patients were assigned to 40 mg of enoxaparin (Lovenox) per day and 176 patients to 100 mg of aspirin per day. Sixty patients were excluded from this randomization because they had a high risk of bleeding or indications for anticoagulant or antiplatelet therapy. Patient demographics and risk factors for thrombotic events were similar between the two groups assessed for venous thromboembolism (VTE) prophylaxis.
The cumulative incidence of all thrombosis, major bleeding, acute cardiovascular events, and sudden deaths was 1.8% in the enoxaparin group and 5.2% in the aspirin group (P = .06). No incidents of major bleeding or sudden death were reported during the study.
During the induction phase of therapy, the incidence of any thrombosis was 1.2% in the enoxaparin group vs. 1.7% in the aspirin group. The events included three cases of deep vein thrombosis (two in the enoxaparin group and one in the aspirin group) and three pulmonary embolisms in the aspirin group.
The time to onset of any thrombotic events was similar between the groups, and the results suggest that the risk of thrombosis is highest during the first 4-6 months of treatment, Dr. Rocci noted.
The relatively low incidence of thrombosis confirms the safety of the dexamethasone/lenalidomide regimen, said Dr. Rocci. The findings also confirm the safety of low-molecular-weight heparin as the standard for preventing thrombosis in newly diagnosed multiple myeloma patients, he said. Aspirin can be a possible alternative in multiple myeloma patients with low risk for developing VTE, he added.
Dr. Rocci had no financial conflicts to disclose. Several of his coauthors disclosed receiving honoraria or research funding from, or serving as a consultant or member of an advisory committee or on the board of directors for, Celgene and Janssen-Cilag.
ORLANDO – Enoxaparin and aspirin were equally effective at preventing thrombotic events in young, newly diagnosed myeloma patients who were treated with a lenalidomide-based regimen in a randomized trial.
Previous studies have shown that this patient population is at least three times as likely to develop thrombosis as patients not on a lenalidomide-based regimen, said Dr. Alberto Rocci of the University of Torino (Italy). "Randomized trials comparing different therapies for [venous thromboembolism] prophylaxis in young, newly diagnosed myeloma patients are still lacking," he said at the annual meeting of the American Society of Hematology.
[Check out our comprehensive coverage of the American Society of Hematology's annual meeting.]
In this study, Dr. Rocci and his colleagues enrolled 402 patients younger than 65 years from 62 cancer centers. All patients had symptomatic and measurable disease, with organ damage.
All patients underwent four 28-day cycles of lenalidomide (25 mg/day on days 1-21) and dexamethasone (40 mg/day on days 1, 8, 15, and 22). After this treatment, 202 patients were randomized to six 28-day cycles of melphalan (0.18 mg/kg on days 1-4), prednisone (2 mg/kg on days 1-4), and lenalidomide (10 mg/day on days 1-21); and 200 patients were randomized to two courses of melphalan (200 mg/m2, plus stem cell support). These groups were designated MPR and MEL 200, respectively.
In this substudy, the researchers further randomized eligible patients who received lenalidomide during induction and in the MPR consolidation regimen: 166 patients were assigned to 40 mg of enoxaparin (Lovenox) per day and 176 patients to 100 mg of aspirin per day. Sixty patients were excluded from this randomization because they had a high risk of bleeding or indications for anticoagulant or antiplatelet therapy. Patient demographics and risk factors for thrombotic events were similar between the two groups assessed for venous thromboembolism (VTE) prophylaxis.
The cumulative incidence of all thrombosis, major bleeding, acute cardiovascular events, and sudden deaths was 1.8% in the enoxaparin group and 5.2% in the aspirin group (P = .06). No incidents of major bleeding or sudden death were reported during the study.
During the induction phase of therapy, the incidence of any thrombosis was 1.2% in the enoxaparin group vs. 1.7% in the aspirin group. The events included three cases of deep vein thrombosis (two in the enoxaparin group and one in the aspirin group) and three pulmonary embolisms in the aspirin group.
The time to onset of any thrombotic events was similar between the groups, and the results suggest that the risk of thrombosis is highest during the first 4-6 months of treatment, Dr. Rocci noted.
The relatively low incidence of thrombosis confirms the safety of the dexamethasone/lenalidomide regimen, said Dr. Rocci. The findings also confirm the safety of low-molecular-weight heparin as the standard for preventing thrombosis in newly diagnosed multiple myeloma patients, he said. Aspirin can be a possible alternative in multiple myeloma patients with low risk for developing VTE, he added.
Dr. Rocci had no financial conflicts to disclose. Several of his coauthors disclosed receiving honoraria or research funding from, or serving as a consultant or member of an advisory committee or on the board of directors for, Celgene and Janssen-Cilag.
ORLANDO – Enoxaparin and aspirin were equally effective at preventing thrombotic events in young, newly diagnosed myeloma patients who were treated with a lenalidomide-based regimen in a randomized trial.
Previous studies have shown that this patient population is at least three times as likely to develop thrombosis as patients not on a lenalidomide-based regimen, said Dr. Alberto Rocci of the University of Torino (Italy). "Randomized trials comparing different therapies for [venous thromboembolism] prophylaxis in young, newly diagnosed myeloma patients are still lacking," he said at the annual meeting of the American Society of Hematology.
[Check out our comprehensive coverage of the American Society of Hematology's annual meeting.]
In this study, Dr. Rocci and his colleagues enrolled 402 patients younger than 65 years from 62 cancer centers. All patients had symptomatic and measurable disease, with organ damage.
All patients underwent four 28-day cycles of lenalidomide (25 mg/day on days 1-21) and dexamethasone (40 mg/day on days 1, 8, 15, and 22). After this treatment, 202 patients were randomized to six 28-day cycles of melphalan (0.18 mg/kg on days 1-4), prednisone (2 mg/kg on days 1-4), and lenalidomide (10 mg/day on days 1-21); and 200 patients were randomized to two courses of melphalan (200 mg/m2, plus stem cell support). These groups were designated MPR and MEL 200, respectively.
In this substudy, the researchers further randomized eligible patients who received lenalidomide during induction and in the MPR consolidation regimen: 166 patients were assigned to 40 mg of enoxaparin (Lovenox) per day and 176 patients to 100 mg of aspirin per day. Sixty patients were excluded from this randomization because they had a high risk of bleeding or indications for anticoagulant or antiplatelet therapy. Patient demographics and risk factors for thrombotic events were similar between the two groups assessed for venous thromboembolism (VTE) prophylaxis.
The cumulative incidence of all thrombosis, major bleeding, acute cardiovascular events, and sudden deaths was 1.8% in the enoxaparin group and 5.2% in the aspirin group (P = .06). No incidents of major bleeding or sudden death were reported during the study.
During the induction phase of therapy, the incidence of any thrombosis was 1.2% in the enoxaparin group vs. 1.7% in the aspirin group. The events included three cases of deep vein thrombosis (two in the enoxaparin group and one in the aspirin group) and three pulmonary embolisms in the aspirin group.
The time to onset of any thrombotic events was similar between the groups, and the results suggest that the risk of thrombosis is highest during the first 4-6 months of treatment, Dr. Rocci noted.
The relatively low incidence of thrombosis confirms the safety of the dexamethasone/lenalidomide regimen, said Dr. Rocci. The findings also confirm the safety of low-molecular-weight heparin as the standard for preventing thrombosis in newly diagnosed multiple myeloma patients, he said. Aspirin can be a possible alternative in multiple myeloma patients with low risk for developing VTE, he added.
Dr. Rocci had no financial conflicts to disclose. Several of his coauthors disclosed receiving honoraria or research funding from, or serving as a consultant or member of an advisory committee or on the board of directors for, Celgene and Janssen-Cilag.
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF HEMATOLOGY
Major Finding: The cumulative incidence of all thrombosis, major bleeding, acute cardiovascular events, and sudden deaths was 1.8% in the enoxaparin group and 5.2% in the aspirin group (P = .06).
Data Source: A randomized trial of 402 young, newly diagnosed patients with multiple myeloma.
Disclosures: Dr. Rocci had no financial conflicts to disclose. Several of his coauthors disclosed receiving honoraria or research funding from, or serving as a consultant or member of an advisory committee or on the board of directors for, Celgene and Janssen-Cilag.
Young Adult AML Patients Fare Better on Children's Protocol
ORLANDO – Ten-year overall survival and event-free survival were significantly higher in adolescents and young adults with acute myeloid leukemia who were treated with a pediatric regimen vs. an adult regimen, based on data from 517 patients aged 16-21 years.
Previous studies have shown improved survival in young adults with acute lymphoblastic leukemia who were treated with a pediatric regimen, said Dr. Anna R.K. Franklin of the University of Texas M.D. Anderson Cancer Center in Houston at the annual meeting of the American Society of Hematology. Dr. Franklin and her coauthors hypothesized that survival trends might be similar in acute myeloid leukemia patients.
The researchers compared 281 young adult patients with AML in Children’s Oncology Group (COG) trials, all of whom received a pediatric regimen, vs. 149 young adults in Cancer and Leukemia Group B (CALGB) trials and 87 young adults in Southwest Oncology Group (SWOG) trials, all of whom received an adult regimen. The patients were treated in 1986-2008.
Overall survival 10 years after study entry was 45% in the COG patients vs. 34% in the CALGB/SWOG patients (P less than .05). A subgroup analysis breaking down the combined population by age showed that overall survival after 10 years was 43% in younger patients (aged 16-18 years) vs. 32% in older patients (aged 19-21 years).
The median age was 18 years overall, but the median age in the COG patients was significantly younger than the median age in the CALGB/SWOG patients (17 years vs. 20 years).
The 10-year overall survival rates by age and group were 45% for younger COG patients, 44% for older COG patients, 40% for younger CALGB/SWOG patients, and 31% for older CALGB/SWOG patients.
Overall, the 10-year event-free survival rates were 39% for younger COG patients and 17% for older COG patients vs. 23%, and 22% for younger and older CALGB/SWOG patients, respectively.
In contrast, 10-year treatment-related mortality rates were significantly higher in COG patients than CALGB/SWOG patients. The rates were 26% for younger COG patients and 30% for older COG patients vs. a constant 12% for younger and older CALGB/SWOG patients.
In this study, age was a confounding variable that made comparison of patients on adult vs. child regimens difficult, because 94% of the COG patients were younger than 19 years, Dr. Franklin noted. However, "COG studies have significantly more [treatment-related mortality] and significantly less risk of relapse than the adult trials," she said.
Significant improvements occurred in 10-year overall survival, event-free survival, and relapse risk in more recent studies compared with earlier studies, but treatment-related mortality also increased, said Dr. Franklin. Multivariate analysis of the data is ongoing to determine which specific factors impact patient outcomes in adult vs. pediatric protocols, she said.
Dr. Franklin had no financial conflicts to disclose.
ORLANDO – Ten-year overall survival and event-free survival were significantly higher in adolescents and young adults with acute myeloid leukemia who were treated with a pediatric regimen vs. an adult regimen, based on data from 517 patients aged 16-21 years.
Previous studies have shown improved survival in young adults with acute lymphoblastic leukemia who were treated with a pediatric regimen, said Dr. Anna R.K. Franklin of the University of Texas M.D. Anderson Cancer Center in Houston at the annual meeting of the American Society of Hematology. Dr. Franklin and her coauthors hypothesized that survival trends might be similar in acute myeloid leukemia patients.
The researchers compared 281 young adult patients with AML in Children’s Oncology Group (COG) trials, all of whom received a pediatric regimen, vs. 149 young adults in Cancer and Leukemia Group B (CALGB) trials and 87 young adults in Southwest Oncology Group (SWOG) trials, all of whom received an adult regimen. The patients were treated in 1986-2008.
Overall survival 10 years after study entry was 45% in the COG patients vs. 34% in the CALGB/SWOG patients (P less than .05). A subgroup analysis breaking down the combined population by age showed that overall survival after 10 years was 43% in younger patients (aged 16-18 years) vs. 32% in older patients (aged 19-21 years).
The median age was 18 years overall, but the median age in the COG patients was significantly younger than the median age in the CALGB/SWOG patients (17 years vs. 20 years).
The 10-year overall survival rates by age and group were 45% for younger COG patients, 44% for older COG patients, 40% for younger CALGB/SWOG patients, and 31% for older CALGB/SWOG patients.
Overall, the 10-year event-free survival rates were 39% for younger COG patients and 17% for older COG patients vs. 23%, and 22% for younger and older CALGB/SWOG patients, respectively.
In contrast, 10-year treatment-related mortality rates were significantly higher in COG patients than CALGB/SWOG patients. The rates were 26% for younger COG patients and 30% for older COG patients vs. a constant 12% for younger and older CALGB/SWOG patients.
In this study, age was a confounding variable that made comparison of patients on adult vs. child regimens difficult, because 94% of the COG patients were younger than 19 years, Dr. Franklin noted. However, "COG studies have significantly more [treatment-related mortality] and significantly less risk of relapse than the adult trials," she said.
Significant improvements occurred in 10-year overall survival, event-free survival, and relapse risk in more recent studies compared with earlier studies, but treatment-related mortality also increased, said Dr. Franklin. Multivariate analysis of the data is ongoing to determine which specific factors impact patient outcomes in adult vs. pediatric protocols, she said.
Dr. Franklin had no financial conflicts to disclose.
ORLANDO – Ten-year overall survival and event-free survival were significantly higher in adolescents and young adults with acute myeloid leukemia who were treated with a pediatric regimen vs. an adult regimen, based on data from 517 patients aged 16-21 years.
Previous studies have shown improved survival in young adults with acute lymphoblastic leukemia who were treated with a pediatric regimen, said Dr. Anna R.K. Franklin of the University of Texas M.D. Anderson Cancer Center in Houston at the annual meeting of the American Society of Hematology. Dr. Franklin and her coauthors hypothesized that survival trends might be similar in acute myeloid leukemia patients.
The researchers compared 281 young adult patients with AML in Children’s Oncology Group (COG) trials, all of whom received a pediatric regimen, vs. 149 young adults in Cancer and Leukemia Group B (CALGB) trials and 87 young adults in Southwest Oncology Group (SWOG) trials, all of whom received an adult regimen. The patients were treated in 1986-2008.
Overall survival 10 years after study entry was 45% in the COG patients vs. 34% in the CALGB/SWOG patients (P less than .05). A subgroup analysis breaking down the combined population by age showed that overall survival after 10 years was 43% in younger patients (aged 16-18 years) vs. 32% in older patients (aged 19-21 years).
The median age was 18 years overall, but the median age in the COG patients was significantly younger than the median age in the CALGB/SWOG patients (17 years vs. 20 years).
The 10-year overall survival rates by age and group were 45% for younger COG patients, 44% for older COG patients, 40% for younger CALGB/SWOG patients, and 31% for older CALGB/SWOG patients.
Overall, the 10-year event-free survival rates were 39% for younger COG patients and 17% for older COG patients vs. 23%, and 22% for younger and older CALGB/SWOG patients, respectively.
In contrast, 10-year treatment-related mortality rates were significantly higher in COG patients than CALGB/SWOG patients. The rates were 26% for younger COG patients and 30% for older COG patients vs. a constant 12% for younger and older CALGB/SWOG patients.
In this study, age was a confounding variable that made comparison of patients on adult vs. child regimens difficult, because 94% of the COG patients were younger than 19 years, Dr. Franklin noted. However, "COG studies have significantly more [treatment-related mortality] and significantly less risk of relapse than the adult trials," she said.
Significant improvements occurred in 10-year overall survival, event-free survival, and relapse risk in more recent studies compared with earlier studies, but treatment-related mortality also increased, said Dr. Franklin. Multivariate analysis of the data is ongoing to determine which specific factors impact patient outcomes in adult vs. pediatric protocols, she said.
Dr. Franklin had no financial conflicts to disclose.
Young Adult AML Patients Fare Better on Children's Protocol
ORLANDO – Ten-year overall survival and event-free survival were significantly higher in adolescents and young adults with acute myeloid leukemia who were treated with a pediatric regimen vs. an adult regimen, based on data from 517 patients aged 16-21 years.
Previous studies have shown improved survival in young adults with acute lymphoblastic leukemia who were treated with a pediatric regimen, said Dr. Anna R.K. Franklin of the University of Texas M.D. Anderson Cancer Center in Houston at the annual meeting of the American Society of Hematology. Dr. Franklin and her coauthors hypothesized that survival trends might be similar in acute myeloid leukemia patients.
The researchers compared 281 young adult patients with AML in Children’s Oncology Group (COG) trials, all of whom received a pediatric regimen, vs. 149 young adults in Cancer and Leukemia Group B (CALGB) trials and 87 young adults in Southwest Oncology Group (SWOG) trials, all of whom received an adult regimen. The patients were treated in 1986-2008.
Overall survival 10 years after study entry was 45% in the COG patients vs. 34% in the CALGB/SWOG patients (P less than .05). A subgroup analysis breaking down the combined population by age showed that overall survival after 10 years was 43% in younger patients (aged 16-18 years) vs. 32% in older patients (aged 19-21 years).
The median age was 18 years overall, but the median age in the COG patients was significantly younger than the median age in the CALGB/SWOG patients (17 years vs. 20 years).
The 10-year overall survival rates by age and group were 45% for younger COG patients, 44% for older COG patients, 40% for younger CALGB/SWOG patients, and 31% for older CALGB/SWOG patients.
Overall, the 10-year event-free survival rates were 39% for younger COG patients and 17% for older COG patients vs. 23%, and 22% for younger and older CALGB/SWOG patients, respectively.
In contrast, 10-year treatment-related mortality rates were significantly higher in COG patients than CALGB/SWOG patients. The rates were 26% for younger COG patients and 30% for older COG patients vs. a constant 12% for younger and older CALGB/SWOG patients.
In this study, age was a confounding variable that made comparison of patients on adult vs. child regimens difficult, because 94% of the COG patients were younger than 19 years, Dr. Franklin noted. However, "COG studies have significantly more [treatment-related mortality] and significantly less risk of relapse than the adult trials," she said.
Significant improvements occurred in 10-year overall survival, event-free survival, and relapse risk in more recent studies compared with earlier studies, but treatment-related mortality also increased, said Dr. Franklin. Multivariate analysis of the data is ongoing to determine which specific factors impact patient outcomes in adult vs. pediatric protocols, she said.
Dr. Franklin had no financial conflicts to disclose.
ORLANDO – Ten-year overall survival and event-free survival were significantly higher in adolescents and young adults with acute myeloid leukemia who were treated with a pediatric regimen vs. an adult regimen, based on data from 517 patients aged 16-21 years.
Previous studies have shown improved survival in young adults with acute lymphoblastic leukemia who were treated with a pediatric regimen, said Dr. Anna R.K. Franklin of the University of Texas M.D. Anderson Cancer Center in Houston at the annual meeting of the American Society of Hematology. Dr. Franklin and her coauthors hypothesized that survival trends might be similar in acute myeloid leukemia patients.
The researchers compared 281 young adult patients with AML in Children’s Oncology Group (COG) trials, all of whom received a pediatric regimen, vs. 149 young adults in Cancer and Leukemia Group B (CALGB) trials and 87 young adults in Southwest Oncology Group (SWOG) trials, all of whom received an adult regimen. The patients were treated in 1986-2008.
Overall survival 10 years after study entry was 45% in the COG patients vs. 34% in the CALGB/SWOG patients (P less than .05). A subgroup analysis breaking down the combined population by age showed that overall survival after 10 years was 43% in younger patients (aged 16-18 years) vs. 32% in older patients (aged 19-21 years).
The median age was 18 years overall, but the median age in the COG patients was significantly younger than the median age in the CALGB/SWOG patients (17 years vs. 20 years).
The 10-year overall survival rates by age and group were 45% for younger COG patients, 44% for older COG patients, 40% for younger CALGB/SWOG patients, and 31% for older CALGB/SWOG patients.
Overall, the 10-year event-free survival rates were 39% for younger COG patients and 17% for older COG patients vs. 23%, and 22% for younger and older CALGB/SWOG patients, respectively.
In contrast, 10-year treatment-related mortality rates were significantly higher in COG patients than CALGB/SWOG patients. The rates were 26% for younger COG patients and 30% for older COG patients vs. a constant 12% for younger and older CALGB/SWOG patients.
In this study, age was a confounding variable that made comparison of patients on adult vs. child regimens difficult, because 94% of the COG patients were younger than 19 years, Dr. Franklin noted. However, "COG studies have significantly more [treatment-related mortality] and significantly less risk of relapse than the adult trials," she said.
Significant improvements occurred in 10-year overall survival, event-free survival, and relapse risk in more recent studies compared with earlier studies, but treatment-related mortality also increased, said Dr. Franklin. Multivariate analysis of the data is ongoing to determine which specific factors impact patient outcomes in adult vs. pediatric protocols, she said.
Dr. Franklin had no financial conflicts to disclose.
ORLANDO – Ten-year overall survival and event-free survival were significantly higher in adolescents and young adults with acute myeloid leukemia who were treated with a pediatric regimen vs. an adult regimen, based on data from 517 patients aged 16-21 years.
Previous studies have shown improved survival in young adults with acute lymphoblastic leukemia who were treated with a pediatric regimen, said Dr. Anna R.K. Franklin of the University of Texas M.D. Anderson Cancer Center in Houston at the annual meeting of the American Society of Hematology. Dr. Franklin and her coauthors hypothesized that survival trends might be similar in acute myeloid leukemia patients.
The researchers compared 281 young adult patients with AML in Children’s Oncology Group (COG) trials, all of whom received a pediatric regimen, vs. 149 young adults in Cancer and Leukemia Group B (CALGB) trials and 87 young adults in Southwest Oncology Group (SWOG) trials, all of whom received an adult regimen. The patients were treated in 1986-2008.
Overall survival 10 years after study entry was 45% in the COG patients vs. 34% in the CALGB/SWOG patients (P less than .05). A subgroup analysis breaking down the combined population by age showed that overall survival after 10 years was 43% in younger patients (aged 16-18 years) vs. 32% in older patients (aged 19-21 years).
The median age was 18 years overall, but the median age in the COG patients was significantly younger than the median age in the CALGB/SWOG patients (17 years vs. 20 years).
The 10-year overall survival rates by age and group were 45% for younger COG patients, 44% for older COG patients, 40% for younger CALGB/SWOG patients, and 31% for older CALGB/SWOG patients.
Overall, the 10-year event-free survival rates were 39% for younger COG patients and 17% for older COG patients vs. 23%, and 22% for younger and older CALGB/SWOG patients, respectively.
In contrast, 10-year treatment-related mortality rates were significantly higher in COG patients than CALGB/SWOG patients. The rates were 26% for younger COG patients and 30% for older COG patients vs. a constant 12% for younger and older CALGB/SWOG patients.
In this study, age was a confounding variable that made comparison of patients on adult vs. child regimens difficult, because 94% of the COG patients were younger than 19 years, Dr. Franklin noted. However, "COG studies have significantly more [treatment-related mortality] and significantly less risk of relapse than the adult trials," she said.
Significant improvements occurred in 10-year overall survival, event-free survival, and relapse risk in more recent studies compared with earlier studies, but treatment-related mortality also increased, said Dr. Franklin. Multivariate analysis of the data is ongoing to determine which specific factors impact patient outcomes in adult vs. pediatric protocols, she said.
Dr. Franklin had no financial conflicts to disclose.
Major Finding: Overall survival 10 years after study entry was 45% in Children’s Oncology Group trials vs. 34% for the same age group in adult trials conducted by the Cancer and Leukemia Group B and Southwest Oncology Group (P less than .05).
Data Source: A study of 571 young adults aged 16-21 years with AML.
Disclosures: Dr. Franklin had no financial conflicts to disclose.
Alemtuzumab Reduces Minimal Residual Disease in CLL Patients
ORLANDO – Alemtuzumab treatment for 6 weeks following chemotherapy eliminated detectable levels of minimal residual disease in 83% of chronic lymphocytic leukemia patients in a phase II study presented at the annual meeting of the American Society of Hematology.
Previous studies have shown that the length of remission in chronic lymphocytic leukemia (CLL) patients depends on the level of minimal residual disease (MRD) at the end of therapy, regardless of the therapeutic regimen, said Dr. Abraham Varghese of St. James’s University Hospital in Leeds, England. Additional studies have shown that alemtuzumab (Campath) can be used as a consolidation therapy after chemotherapy in these patients, but toxicity remains a concern.
To assess the response of CLL patients to alemtuzumab consolidation, Dr. Varghese and his colleagues in the U.K. National Cancer Research Institute’s CLL trials subgroup conducted the prospective National Cancer Research Network CLL207 trial in 47 patients who received alemtuzumab for at least 6 weeks, starting at 6-24 months after chemotherapy. The patients had undergone one to four previous therapies; 51% had complete responses, and the remaining 49% had partial responses. The average age of the 35 men and 12 women was 58 years. About half had received one prior therapy, and 30% had received two therapies. All but one patient had prior fludarabine. The next most common treatment was rituximab, which nine patients (19%) had received.
Overall, 39 patients (83%) were MRD negative at the end of alemtuzumab treatment. At 6 months after treatment, 20 patients were MRD negative, and at 12 months after treatment, 13 patients remained negative, which suggests improved odds for long-term remission, especially in patients who were MRD negative at 6 weeks.
Prior to alemtuzumab treatment, 24 patients were in complete remission and 23 were in partial remission. In the complete remission group, 22 were MRD negative at the end of treatment, 15 were negative 6 months after treatment, and 8 were negative 12 months after treatment. In the partial remission group, 17 patients were MRD negative at the end of treatment, 5 were negative 6 months after treatment, and 5 were negative 12 months after treatment.
Dr. Varghese reported 351 adverse events, 23 of which were severe. Four patients (9%) experienced unacceptable severe adverse reactions: pneumocystis pneumonia that lasted for 1.3 days; Epstein-Barr virus–driven, high-grade B-cell lymphoma of the bowel leading to hematemesis; parainfluenza leading to death; and EBV-driven, high-grade B-cell lymphoma leading to death. Serious adverse events included 14 infections, 3 hematologic disorders, 2 general disorders and administration site conditions, and 1 cardiovascular disorder, Dr. Varghese said.
Although the toxicity was significant, the study results are encouraging, he said. All 47 patients who received treatment were part of the final analysis. In addition, the target number of patients who were negative for MRD in the study was 14, but 39 patients in the study achieved MRD negativity, he noted.
The results suggest that alemtuzumab consolidation therapy should be further studied in a randomized phase III trial, Dr. Varghese said. A randomized phase III trial will compare alemtuzumab consolidation with observation in CLL patients.
Dr. Varghese had no financial conflicts to disclose. Several of his coauthors disclosed receiving honoraria or research funding, serving on the board of directors or advisory committee, or receiving patent and royalty funds from multiple companies including Genzyme, which makes Campath.
ORLANDO – Alemtuzumab treatment for 6 weeks following chemotherapy eliminated detectable levels of minimal residual disease in 83% of chronic lymphocytic leukemia patients in a phase II study presented at the annual meeting of the American Society of Hematology.
Previous studies have shown that the length of remission in chronic lymphocytic leukemia (CLL) patients depends on the level of minimal residual disease (MRD) at the end of therapy, regardless of the therapeutic regimen, said Dr. Abraham Varghese of St. James’s University Hospital in Leeds, England. Additional studies have shown that alemtuzumab (Campath) can be used as a consolidation therapy after chemotherapy in these patients, but toxicity remains a concern.
To assess the response of CLL patients to alemtuzumab consolidation, Dr. Varghese and his colleagues in the U.K. National Cancer Research Institute’s CLL trials subgroup conducted the prospective National Cancer Research Network CLL207 trial in 47 patients who received alemtuzumab for at least 6 weeks, starting at 6-24 months after chemotherapy. The patients had undergone one to four previous therapies; 51% had complete responses, and the remaining 49% had partial responses. The average age of the 35 men and 12 women was 58 years. About half had received one prior therapy, and 30% had received two therapies. All but one patient had prior fludarabine. The next most common treatment was rituximab, which nine patients (19%) had received.
Overall, 39 patients (83%) were MRD negative at the end of alemtuzumab treatment. At 6 months after treatment, 20 patients were MRD negative, and at 12 months after treatment, 13 patients remained negative, which suggests improved odds for long-term remission, especially in patients who were MRD negative at 6 weeks.
Prior to alemtuzumab treatment, 24 patients were in complete remission and 23 were in partial remission. In the complete remission group, 22 were MRD negative at the end of treatment, 15 were negative 6 months after treatment, and 8 were negative 12 months after treatment. In the partial remission group, 17 patients were MRD negative at the end of treatment, 5 were negative 6 months after treatment, and 5 were negative 12 months after treatment.
Dr. Varghese reported 351 adverse events, 23 of which were severe. Four patients (9%) experienced unacceptable severe adverse reactions: pneumocystis pneumonia that lasted for 1.3 days; Epstein-Barr virus–driven, high-grade B-cell lymphoma of the bowel leading to hematemesis; parainfluenza leading to death; and EBV-driven, high-grade B-cell lymphoma leading to death. Serious adverse events included 14 infections, 3 hematologic disorders, 2 general disorders and administration site conditions, and 1 cardiovascular disorder, Dr. Varghese said.
Although the toxicity was significant, the study results are encouraging, he said. All 47 patients who received treatment were part of the final analysis. In addition, the target number of patients who were negative for MRD in the study was 14, but 39 patients in the study achieved MRD negativity, he noted.
The results suggest that alemtuzumab consolidation therapy should be further studied in a randomized phase III trial, Dr. Varghese said. A randomized phase III trial will compare alemtuzumab consolidation with observation in CLL patients.
Dr. Varghese had no financial conflicts to disclose. Several of his coauthors disclosed receiving honoraria or research funding, serving on the board of directors or advisory committee, or receiving patent and royalty funds from multiple companies including Genzyme, which makes Campath.
ORLANDO – Alemtuzumab treatment for 6 weeks following chemotherapy eliminated detectable levels of minimal residual disease in 83% of chronic lymphocytic leukemia patients in a phase II study presented at the annual meeting of the American Society of Hematology.
Previous studies have shown that the length of remission in chronic lymphocytic leukemia (CLL) patients depends on the level of minimal residual disease (MRD) at the end of therapy, regardless of the therapeutic regimen, said Dr. Abraham Varghese of St. James’s University Hospital in Leeds, England. Additional studies have shown that alemtuzumab (Campath) can be used as a consolidation therapy after chemotherapy in these patients, but toxicity remains a concern.
To assess the response of CLL patients to alemtuzumab consolidation, Dr. Varghese and his colleagues in the U.K. National Cancer Research Institute’s CLL trials subgroup conducted the prospective National Cancer Research Network CLL207 trial in 47 patients who received alemtuzumab for at least 6 weeks, starting at 6-24 months after chemotherapy. The patients had undergone one to four previous therapies; 51% had complete responses, and the remaining 49% had partial responses. The average age of the 35 men and 12 women was 58 years. About half had received one prior therapy, and 30% had received two therapies. All but one patient had prior fludarabine. The next most common treatment was rituximab, which nine patients (19%) had received.
Overall, 39 patients (83%) were MRD negative at the end of alemtuzumab treatment. At 6 months after treatment, 20 patients were MRD negative, and at 12 months after treatment, 13 patients remained negative, which suggests improved odds for long-term remission, especially in patients who were MRD negative at 6 weeks.
Prior to alemtuzumab treatment, 24 patients were in complete remission and 23 were in partial remission. In the complete remission group, 22 were MRD negative at the end of treatment, 15 were negative 6 months after treatment, and 8 were negative 12 months after treatment. In the partial remission group, 17 patients were MRD negative at the end of treatment, 5 were negative 6 months after treatment, and 5 were negative 12 months after treatment.
Dr. Varghese reported 351 adverse events, 23 of which were severe. Four patients (9%) experienced unacceptable severe adverse reactions: pneumocystis pneumonia that lasted for 1.3 days; Epstein-Barr virus–driven, high-grade B-cell lymphoma of the bowel leading to hematemesis; parainfluenza leading to death; and EBV-driven, high-grade B-cell lymphoma leading to death. Serious adverse events included 14 infections, 3 hematologic disorders, 2 general disorders and administration site conditions, and 1 cardiovascular disorder, Dr. Varghese said.
Although the toxicity was significant, the study results are encouraging, he said. All 47 patients who received treatment were part of the final analysis. In addition, the target number of patients who were negative for MRD in the study was 14, but 39 patients in the study achieved MRD negativity, he noted.
The results suggest that alemtuzumab consolidation therapy should be further studied in a randomized phase III trial, Dr. Varghese said. A randomized phase III trial will compare alemtuzumab consolidation with observation in CLL patients.
Dr. Varghese had no financial conflicts to disclose. Several of his coauthors disclosed receiving honoraria or research funding, serving on the board of directors or advisory committee, or receiving patent and royalty funds from multiple companies including Genzyme, which makes Campath.
Major Finding: Alemtuzumab was associated with negative MRD in 83% of patients with CLL when it was used for 6 weeks after conclusion of chemotherapy.
Data Source: A phase II study of 47 adults with CLL.
Disclosures: Dr. Varghese had no financial conflicts to disclose. Several coauthors disclosed receiving honoraria or research funding, serving on the board of directors or advisory committee, or receiving patent and royalty funds from multiple companies including Genzyme, which makes Campath.
FDA Tightens Rules for Tobacco Products
Certain tobacco products – including cigarettes, roll-your-own, and smokeless varieties – that were introduced or changed in the United States after Feb. 15, 2007, must be reviewed by the U.S. Food and Drug Administration to show that they are "substantially equivalent" to existing products, Dr. Lawrence Deyton, director of the agency’s Center for Tobacco Products, said in a press briefing on Jan. 5.
The FDA action is driven by the Family Smoking Prevention and Tobacco Control Act, which became law in June 2009. The law allows the FDA to regulate tobacco products with the goal of protecting public health.
The substantial equivalence provisions are "meant to ensure that new tobacco products or changes to existing products are evaluated by the FDA before they enter the marketplace and are consumed by millions of people," Dr. Deyton said. "Up to now, tobacco products have been the only mass-consumed products for which users do not know what they are consuming," he said.
The Tobacco Control Act allows tobacco companies to market products that were available after Feb. 15, 2007, if the companies submit at least a preliminary report to the FDA by March 22, 2011, to show that these products are not significantly different from pre-existing products. Products in existence before Feb. 15, 2007, are not subject to the new FDA review, said Ann Simoneau, director of the Center for Tobacco Products’ Office of Compliance and Enforcement.
Completely new products introduced after March 22 will follow a different regulatory pathway, Dr. Deyton said.
Physicians should know that the FDA is now examining certain tobacco products and that manufacturers are required to submit information to the FDA about the products and changes to them, "particularly if those changes might raise new questions about public health," Dr. Deyton said.
"FDA’s role does not indicate that these products are safe. There are no tobacco products that are safe," Dr. Deyton emphasized. "The Tobacco Control Act is very clear that this is an important public health tool," he said. "The ingredients of these products have not ever been known to those people who consume them."
"The standard we work under when looking at these products is a public health standard," said David Ashley, Ph.D., director of the Center for Tobacco Products’ Office of Science. "That is at the center of all the decisions we are making," he said. "We will be looking at the possible impact on users and nonusers."
Certain tobacco products – including cigarettes, roll-your-own, and smokeless varieties – that were introduced or changed in the United States after Feb. 15, 2007, must be reviewed by the U.S. Food and Drug Administration to show that they are "substantially equivalent" to existing products, Dr. Lawrence Deyton, director of the agency’s Center for Tobacco Products, said in a press briefing on Jan. 5.
The FDA action is driven by the Family Smoking Prevention and Tobacco Control Act, which became law in June 2009. The law allows the FDA to regulate tobacco products with the goal of protecting public health.
The substantial equivalence provisions are "meant to ensure that new tobacco products or changes to existing products are evaluated by the FDA before they enter the marketplace and are consumed by millions of people," Dr. Deyton said. "Up to now, tobacco products have been the only mass-consumed products for which users do not know what they are consuming," he said.
The Tobacco Control Act allows tobacco companies to market products that were available after Feb. 15, 2007, if the companies submit at least a preliminary report to the FDA by March 22, 2011, to show that these products are not significantly different from pre-existing products. Products in existence before Feb. 15, 2007, are not subject to the new FDA review, said Ann Simoneau, director of the Center for Tobacco Products’ Office of Compliance and Enforcement.
Completely new products introduced after March 22 will follow a different regulatory pathway, Dr. Deyton said.
Physicians should know that the FDA is now examining certain tobacco products and that manufacturers are required to submit information to the FDA about the products and changes to them, "particularly if those changes might raise new questions about public health," Dr. Deyton said.
"FDA’s role does not indicate that these products are safe. There are no tobacco products that are safe," Dr. Deyton emphasized. "The Tobacco Control Act is very clear that this is an important public health tool," he said. "The ingredients of these products have not ever been known to those people who consume them."
"The standard we work under when looking at these products is a public health standard," said David Ashley, Ph.D., director of the Center for Tobacco Products’ Office of Science. "That is at the center of all the decisions we are making," he said. "We will be looking at the possible impact on users and nonusers."
Certain tobacco products – including cigarettes, roll-your-own, and smokeless varieties – that were introduced or changed in the United States after Feb. 15, 2007, must be reviewed by the U.S. Food and Drug Administration to show that they are "substantially equivalent" to existing products, Dr. Lawrence Deyton, director of the agency’s Center for Tobacco Products, said in a press briefing on Jan. 5.
The FDA action is driven by the Family Smoking Prevention and Tobacco Control Act, which became law in June 2009. The law allows the FDA to regulate tobacco products with the goal of protecting public health.
The substantial equivalence provisions are "meant to ensure that new tobacco products or changes to existing products are evaluated by the FDA before they enter the marketplace and are consumed by millions of people," Dr. Deyton said. "Up to now, tobacco products have been the only mass-consumed products for which users do not know what they are consuming," he said.
The Tobacco Control Act allows tobacco companies to market products that were available after Feb. 15, 2007, if the companies submit at least a preliminary report to the FDA by March 22, 2011, to show that these products are not significantly different from pre-existing products. Products in existence before Feb. 15, 2007, are not subject to the new FDA review, said Ann Simoneau, director of the Center for Tobacco Products’ Office of Compliance and Enforcement.
Completely new products introduced after March 22 will follow a different regulatory pathway, Dr. Deyton said.
Physicians should know that the FDA is now examining certain tobacco products and that manufacturers are required to submit information to the FDA about the products and changes to them, "particularly if those changes might raise new questions about public health," Dr. Deyton said.
"FDA’s role does not indicate that these products are safe. There are no tobacco products that are safe," Dr. Deyton emphasized. "The Tobacco Control Act is very clear that this is an important public health tool," he said. "The ingredients of these products have not ever been known to those people who consume them."
"The standard we work under when looking at these products is a public health standard," said David Ashley, Ph.D., director of the Center for Tobacco Products’ Office of Science. "That is at the center of all the decisions we are making," he said. "We will be looking at the possible impact on users and nonusers."