User login
Immunostaining Advances Up Melanocyte ID Efficiency
ORLANDO – Mohs surgery is an appropriate choice for lentigo maligna patients because advances in immunostaining allow easier and more efficient identification of melanocytes on frozen sections, said Dr. Basil S. Cherpelis.
Recent literature shows the recommended 5-mm margin for melanoma is often inadequate, Dr. Cherpelis said at the Orlando Dermatology Aesthetic and Clinical conference.
The margins needed for successful treatment of lentigo maligna vary – 5 mm is enough for some melanomas, while others might need a 1-cm margin.
"It makes sense to use a method of intraoperative margin control," said Dr. Cherpelis, of the Moffitt Cancer Center at the University of South Florida in Tampa. "That’s what gives you the flexibility to adjust your margins based on the melanoma that you happen to be treating."
One option for intraoperative margin control is traditional frozen sections, Dr. Cherpelis said. But frozen sections offer a limited view of the margin, and they pose the problem of freeze artifacts, which can make the distinction between melanocytes and keratinocytes difficult. A second option is the square or perimeter method, but this method involves a 1-2 week wait for complete results, which is inconvenient for doctors and patients.
A third option is Mohs surgery. Literature shows that Mohs is effective for melanoma, with the benefits of entire visualization and same-day reconstruction, but it is not widely used, Dr. Cherpelis said. One reason: Melanomas on permanent sections have halos around them, making identification easy, but frozen sections have similar halos around keratinocytes and melanocytes.
Using immunostaining as part of Mohs surgery can solve the identification problem, but until recently immunostain protocols could take at least an hour.
Dr. Cherpelis and his colleagues have streamlined the process.
"We have been able to shorten our protocols down to 19 minutes for MART-1 [melanoma-associated antigen recognized by T cells] and 35 minutes for MITF [microphthalmia-associated transcription factor]," Dr. Cherpelis said (Derm. Surg. 2009;35:207-13; Am. J. Dermatopath. 2010; 32:319-25, respectively). The protocols make Mohs surgery easier because the immunostain helps clinicians easily identify melanocytes.
MART-1 (a cytoplasmic stain) is the most common immunostain, but some data suggest it can falsely label keratinocytes in inflamed skin or in pigmented actinic keratoses, Dr. Cherpelis said. It also can cause pseudo-confluence (the appearance of touching melanocytes). By contrast, MITF is a nuclear stain, so it does not have the problem of pseudo-confluence.
Dr. Cherpelis said he had no relevant financial disclosures.
ORLANDO – Mohs surgery is an appropriate choice for lentigo maligna patients because advances in immunostaining allow easier and more efficient identification of melanocytes on frozen sections, said Dr. Basil S. Cherpelis.
Recent literature shows the recommended 5-mm margin for melanoma is often inadequate, Dr. Cherpelis said at the Orlando Dermatology Aesthetic and Clinical conference.
The margins needed for successful treatment of lentigo maligna vary – 5 mm is enough for some melanomas, while others might need a 1-cm margin.
"It makes sense to use a method of intraoperative margin control," said Dr. Cherpelis, of the Moffitt Cancer Center at the University of South Florida in Tampa. "That’s what gives you the flexibility to adjust your margins based on the melanoma that you happen to be treating."
One option for intraoperative margin control is traditional frozen sections, Dr. Cherpelis said. But frozen sections offer a limited view of the margin, and they pose the problem of freeze artifacts, which can make the distinction between melanocytes and keratinocytes difficult. A second option is the square or perimeter method, but this method involves a 1-2 week wait for complete results, which is inconvenient for doctors and patients.
A third option is Mohs surgery. Literature shows that Mohs is effective for melanoma, with the benefits of entire visualization and same-day reconstruction, but it is not widely used, Dr. Cherpelis said. One reason: Melanomas on permanent sections have halos around them, making identification easy, but frozen sections have similar halos around keratinocytes and melanocytes.
Using immunostaining as part of Mohs surgery can solve the identification problem, but until recently immunostain protocols could take at least an hour.
Dr. Cherpelis and his colleagues have streamlined the process.
"We have been able to shorten our protocols down to 19 minutes for MART-1 [melanoma-associated antigen recognized by T cells] and 35 minutes for MITF [microphthalmia-associated transcription factor]," Dr. Cherpelis said (Derm. Surg. 2009;35:207-13; Am. J. Dermatopath. 2010; 32:319-25, respectively). The protocols make Mohs surgery easier because the immunostain helps clinicians easily identify melanocytes.
MART-1 (a cytoplasmic stain) is the most common immunostain, but some data suggest it can falsely label keratinocytes in inflamed skin or in pigmented actinic keratoses, Dr. Cherpelis said. It also can cause pseudo-confluence (the appearance of touching melanocytes). By contrast, MITF is a nuclear stain, so it does not have the problem of pseudo-confluence.
Dr. Cherpelis said he had no relevant financial disclosures.
ORLANDO – Mohs surgery is an appropriate choice for lentigo maligna patients because advances in immunostaining allow easier and more efficient identification of melanocytes on frozen sections, said Dr. Basil S. Cherpelis.
Recent literature shows the recommended 5-mm margin for melanoma is often inadequate, Dr. Cherpelis said at the Orlando Dermatology Aesthetic and Clinical conference.
The margins needed for successful treatment of lentigo maligna vary – 5 mm is enough for some melanomas, while others might need a 1-cm margin.
"It makes sense to use a method of intraoperative margin control," said Dr. Cherpelis, of the Moffitt Cancer Center at the University of South Florida in Tampa. "That’s what gives you the flexibility to adjust your margins based on the melanoma that you happen to be treating."
One option for intraoperative margin control is traditional frozen sections, Dr. Cherpelis said. But frozen sections offer a limited view of the margin, and they pose the problem of freeze artifacts, which can make the distinction between melanocytes and keratinocytes difficult. A second option is the square or perimeter method, but this method involves a 1-2 week wait for complete results, which is inconvenient for doctors and patients.
A third option is Mohs surgery. Literature shows that Mohs is effective for melanoma, with the benefits of entire visualization and same-day reconstruction, but it is not widely used, Dr. Cherpelis said. One reason: Melanomas on permanent sections have halos around them, making identification easy, but frozen sections have similar halos around keratinocytes and melanocytes.
Using immunostaining as part of Mohs surgery can solve the identification problem, but until recently immunostain protocols could take at least an hour.
Dr. Cherpelis and his colleagues have streamlined the process.
"We have been able to shorten our protocols down to 19 minutes for MART-1 [melanoma-associated antigen recognized by T cells] and 35 minutes for MITF [microphthalmia-associated transcription factor]," Dr. Cherpelis said (Derm. Surg. 2009;35:207-13; Am. J. Dermatopath. 2010; 32:319-25, respectively). The protocols make Mohs surgery easier because the immunostain helps clinicians easily identify melanocytes.
MART-1 (a cytoplasmic stain) is the most common immunostain, but some data suggest it can falsely label keratinocytes in inflamed skin or in pigmented actinic keratoses, Dr. Cherpelis said. It also can cause pseudo-confluence (the appearance of touching melanocytes). By contrast, MITF is a nuclear stain, so it does not have the problem of pseudo-confluence.
Dr. Cherpelis said he had no relevant financial disclosures.
EXPERT ANALYSIS FROM THE ORLANDO DERMATOLOGY AESTHETIC & CLINICAL CONFERENCE
Immunostaining Advances Up Melanocyte ID Efficiency
ORLANDO – Mohs surgery is an appropriate choice for lentigo maligna patients because advances in immunostaining allow easier and more efficient identification of melanocytes on frozen sections, said Dr. Basil S. Cherpelis.
Recent literature shows the recommended 5-mm margin for melanoma is often inadequate, Dr. Cherpelis said at the Orlando Dermatology Aesthetic and Clinical conference.
The margins needed for successful treatment of lentigo maligna vary – 5 mm is enough for some melanomas, while others might need a 1-cm margin.
"It makes sense to use a method of intraoperative margin control," said Dr. Cherpelis, of the Moffitt Cancer Center at the University of South Florida in Tampa. "That’s what gives you the flexibility to adjust your margins based on the melanoma that you happen to be treating."
One option for intraoperative margin control is traditional frozen sections, Dr. Cherpelis said. But frozen sections offer a limited view of the margin, and they pose the problem of freeze artifacts, which can make the distinction between melanocytes and keratinocytes difficult. A second option is the square or perimeter method, but this method involves a 1-2 week wait for complete results, which is inconvenient for doctors and patients.
A third option is Mohs surgery. Literature shows that Mohs is effective for melanoma, with the benefits of entire visualization and same-day reconstruction, but it is not widely used, Dr. Cherpelis said. One reason: Melanomas on permanent sections have halos around them, making identification easy, but frozen sections have similar halos around keratinocytes and melanocytes.
Using immunostaining as part of Mohs surgery can solve the identification problem, but until recently immunostain protocols could take at least an hour.
Dr. Cherpelis and his colleagues have streamlined the process.
"We have been able to shorten our protocols down to 19 minutes for MART-1 [melanoma-associated antigen recognized by T cells] and 35 minutes for MITF [microphthalmia-associated transcription factor]," Dr. Cherpelis said (Derm. Surg. 2009;35:207-13; Am. J. Dermatopath. 2010; 32:319-25, respectively). The protocols make Mohs surgery easier because the immunostain helps clinicians easily identify melanocytes.
MART-1 (a cytoplasmic stain) is the most common immunostain, but some data suggest it can falsely label keratinocytes in inflamed skin or in pigmented actinic keratoses, Dr. Cherpelis said. It also can cause pseudo-confluence (the appearance of touching melanocytes). By contrast, MITF is a nuclear stain, so it does not have the problem of pseudo-confluence.
Dr. Cherpelis said he had no relevant financial disclosures.
ORLANDO – Mohs surgery is an appropriate choice for lentigo maligna patients because advances in immunostaining allow easier and more efficient identification of melanocytes on frozen sections, said Dr. Basil S. Cherpelis.
Recent literature shows the recommended 5-mm margin for melanoma is often inadequate, Dr. Cherpelis said at the Orlando Dermatology Aesthetic and Clinical conference.
The margins needed for successful treatment of lentigo maligna vary – 5 mm is enough for some melanomas, while others might need a 1-cm margin.
"It makes sense to use a method of intraoperative margin control," said Dr. Cherpelis, of the Moffitt Cancer Center at the University of South Florida in Tampa. "That’s what gives you the flexibility to adjust your margins based on the melanoma that you happen to be treating."
One option for intraoperative margin control is traditional frozen sections, Dr. Cherpelis said. But frozen sections offer a limited view of the margin, and they pose the problem of freeze artifacts, which can make the distinction between melanocytes and keratinocytes difficult. A second option is the square or perimeter method, but this method involves a 1-2 week wait for complete results, which is inconvenient for doctors and patients.
A third option is Mohs surgery. Literature shows that Mohs is effective for melanoma, with the benefits of entire visualization and same-day reconstruction, but it is not widely used, Dr. Cherpelis said. One reason: Melanomas on permanent sections have halos around them, making identification easy, but frozen sections have similar halos around keratinocytes and melanocytes.
Using immunostaining as part of Mohs surgery can solve the identification problem, but until recently immunostain protocols could take at least an hour.
Dr. Cherpelis and his colleagues have streamlined the process.
"We have been able to shorten our protocols down to 19 minutes for MART-1 [melanoma-associated antigen recognized by T cells] and 35 minutes for MITF [microphthalmia-associated transcription factor]," Dr. Cherpelis said (Derm. Surg. 2009;35:207-13; Am. J. Dermatopath. 2010; 32:319-25, respectively). The protocols make Mohs surgery easier because the immunostain helps clinicians easily identify melanocytes.
MART-1 (a cytoplasmic stain) is the most common immunostain, but some data suggest it can falsely label keratinocytes in inflamed skin or in pigmented actinic keratoses, Dr. Cherpelis said. It also can cause pseudo-confluence (the appearance of touching melanocytes). By contrast, MITF is a nuclear stain, so it does not have the problem of pseudo-confluence.
Dr. Cherpelis said he had no relevant financial disclosures.
ORLANDO – Mohs surgery is an appropriate choice for lentigo maligna patients because advances in immunostaining allow easier and more efficient identification of melanocytes on frozen sections, said Dr. Basil S. Cherpelis.
Recent literature shows the recommended 5-mm margin for melanoma is often inadequate, Dr. Cherpelis said at the Orlando Dermatology Aesthetic and Clinical conference.
The margins needed for successful treatment of lentigo maligna vary – 5 mm is enough for some melanomas, while others might need a 1-cm margin.
"It makes sense to use a method of intraoperative margin control," said Dr. Cherpelis, of the Moffitt Cancer Center at the University of South Florida in Tampa. "That’s what gives you the flexibility to adjust your margins based on the melanoma that you happen to be treating."
One option for intraoperative margin control is traditional frozen sections, Dr. Cherpelis said. But frozen sections offer a limited view of the margin, and they pose the problem of freeze artifacts, which can make the distinction between melanocytes and keratinocytes difficult. A second option is the square or perimeter method, but this method involves a 1-2 week wait for complete results, which is inconvenient for doctors and patients.
A third option is Mohs surgery. Literature shows that Mohs is effective for melanoma, with the benefits of entire visualization and same-day reconstruction, but it is not widely used, Dr. Cherpelis said. One reason: Melanomas on permanent sections have halos around them, making identification easy, but frozen sections have similar halos around keratinocytes and melanocytes.
Using immunostaining as part of Mohs surgery can solve the identification problem, but until recently immunostain protocols could take at least an hour.
Dr. Cherpelis and his colleagues have streamlined the process.
"We have been able to shorten our protocols down to 19 minutes for MART-1 [melanoma-associated antigen recognized by T cells] and 35 minutes for MITF [microphthalmia-associated transcription factor]," Dr. Cherpelis said (Derm. Surg. 2009;35:207-13; Am. J. Dermatopath. 2010; 32:319-25, respectively). The protocols make Mohs surgery easier because the immunostain helps clinicians easily identify melanocytes.
MART-1 (a cytoplasmic stain) is the most common immunostain, but some data suggest it can falsely label keratinocytes in inflamed skin or in pigmented actinic keratoses, Dr. Cherpelis said. It also can cause pseudo-confluence (the appearance of touching melanocytes). By contrast, MITF is a nuclear stain, so it does not have the problem of pseudo-confluence.
Dr. Cherpelis said he had no relevant financial disclosures.
EXPERT ANAYLSIS FROM THE ORLANDO DERMATOLOGY AESTHETIC & CLINICAL CONFERENCE
Hypertension, Cholesterol Are Largely Uncontrolled in U.S. Adults
Approximately 68 million American adults have high blood pressure and 71 million have high cholesterol, and the conditions are uncontrolled in 37 million and 48 million, respectively, according to a Vital Signs report released by the Centers for Disease Control and Prevention on Feb. 1.
"Heart disease is the leading killer in America, and the bottom line is that high blood pressure and high cholesterol are out of control for most Americans who have these conditions," CDC director Dr. Thomas R. Frieden said during the teleconference accompanying the report’s release.
High blood pressure and high cholesterol remain top risk factors for life-threatening conditions including strokes, heart attacks, and vascular diseases, he added.
Dr. Frieden had a message for physicians: Controlling high blood pressure and cholesterol is one of the most important things you can do for your patients. Know how many of your patients have high blood pressure and high cholesterol, what proportion are controlled, and what can be done to help more patients get these conditions under control, he said.
"We have seen many examples of health systems, health programs, and doctors’ offices using information technology to support patients and drastically improve the levels of control, and that’s something that is needed throughout health care in this country," he added.
The report was based on data from the National Health and Nutrition Examination Survey (NHANES) on adults aged 18 years and older. The findings also indicate that approximately 20 million U.S. adults with high blood pressure and 37 million with high cholesterol are not being treated for these conditions.
The prevalence of control of high blood pressure was 29% among adults without health insurance, and the control of high cholesterol was less than 15% among those with limited access to health care. But at least 80% of individuals with uncontrolled high blood pressure and high cholesterol have health insurance, Dr. Frieden noted.
For those with health insurance, the characteristics of their specific plan are more likely to affect how likely they are to have high blood pressure or high cholesterol under control than are their personal characteristics, he said.
High blood pressure was defined as blood pressure greater than 140/90 mmHg or reported use of blood pressure–lowering medication. The national prevalence of high blood pressure remained stable over the past decade, although 70% of those with hypertension were being treated and 46% were being controlled, according to the report.
The criteria for high cholesterol included anyone taking cholesterol medication or having a LDL cholesterol level of 100 mg/dL or higher for high-risk individuals, 130 mg/dL or higher for intermediate-risk individuals, and 160 mg/dL for those at low risk.
The proportion of adults treated for high cholesterol increased from 28% to 48% over the past decade, and the proportion of those controlling their high cholesterol increased from less than 20% to more than 30%.
The findings were limited by the lack of data on individuals in nursing homes and other institutions that are not included in NHANES databases, the CDC researchers noted in the report.
About 100,000 deaths [in the U.S.] are preventable by simple, low-cost improvements in our ability to control high blood pressure and high cholesterol," said Dr. Frieden. "Better control can save lives and save money."
The report is available online at www.cdc.gov/vitalsigns. More detailed information can be found in the Feb. 1 issue of the weekly Morbidity and Mortality Report (MMWR early release/vol. 60; Feb. 1, 2011).
Approximately 68 million American adults have high blood pressure and 71 million have high cholesterol, and the conditions are uncontrolled in 37 million and 48 million, respectively, according to a Vital Signs report released by the Centers for Disease Control and Prevention on Feb. 1.
"Heart disease is the leading killer in America, and the bottom line is that high blood pressure and high cholesterol are out of control for most Americans who have these conditions," CDC director Dr. Thomas R. Frieden said during the teleconference accompanying the report’s release.
High blood pressure and high cholesterol remain top risk factors for life-threatening conditions including strokes, heart attacks, and vascular diseases, he added.
Dr. Frieden had a message for physicians: Controlling high blood pressure and cholesterol is one of the most important things you can do for your patients. Know how many of your patients have high blood pressure and high cholesterol, what proportion are controlled, and what can be done to help more patients get these conditions under control, he said.
"We have seen many examples of health systems, health programs, and doctors’ offices using information technology to support patients and drastically improve the levels of control, and that’s something that is needed throughout health care in this country," he added.
The report was based on data from the National Health and Nutrition Examination Survey (NHANES) on adults aged 18 years and older. The findings also indicate that approximately 20 million U.S. adults with high blood pressure and 37 million with high cholesterol are not being treated for these conditions.
The prevalence of control of high blood pressure was 29% among adults without health insurance, and the control of high cholesterol was less than 15% among those with limited access to health care. But at least 80% of individuals with uncontrolled high blood pressure and high cholesterol have health insurance, Dr. Frieden noted.
For those with health insurance, the characteristics of their specific plan are more likely to affect how likely they are to have high blood pressure or high cholesterol under control than are their personal characteristics, he said.
High blood pressure was defined as blood pressure greater than 140/90 mmHg or reported use of blood pressure–lowering medication. The national prevalence of high blood pressure remained stable over the past decade, although 70% of those with hypertension were being treated and 46% were being controlled, according to the report.
The criteria for high cholesterol included anyone taking cholesterol medication or having a LDL cholesterol level of 100 mg/dL or higher for high-risk individuals, 130 mg/dL or higher for intermediate-risk individuals, and 160 mg/dL for those at low risk.
The proportion of adults treated for high cholesterol increased from 28% to 48% over the past decade, and the proportion of those controlling their high cholesterol increased from less than 20% to more than 30%.
The findings were limited by the lack of data on individuals in nursing homes and other institutions that are not included in NHANES databases, the CDC researchers noted in the report.
About 100,000 deaths [in the U.S.] are preventable by simple, low-cost improvements in our ability to control high blood pressure and high cholesterol," said Dr. Frieden. "Better control can save lives and save money."
The report is available online at www.cdc.gov/vitalsigns. More detailed information can be found in the Feb. 1 issue of the weekly Morbidity and Mortality Report (MMWR early release/vol. 60; Feb. 1, 2011).
Approximately 68 million American adults have high blood pressure and 71 million have high cholesterol, and the conditions are uncontrolled in 37 million and 48 million, respectively, according to a Vital Signs report released by the Centers for Disease Control and Prevention on Feb. 1.
"Heart disease is the leading killer in America, and the bottom line is that high blood pressure and high cholesterol are out of control for most Americans who have these conditions," CDC director Dr. Thomas R. Frieden said during the teleconference accompanying the report’s release.
High blood pressure and high cholesterol remain top risk factors for life-threatening conditions including strokes, heart attacks, and vascular diseases, he added.
Dr. Frieden had a message for physicians: Controlling high blood pressure and cholesterol is one of the most important things you can do for your patients. Know how many of your patients have high blood pressure and high cholesterol, what proportion are controlled, and what can be done to help more patients get these conditions under control, he said.
"We have seen many examples of health systems, health programs, and doctors’ offices using information technology to support patients and drastically improve the levels of control, and that’s something that is needed throughout health care in this country," he added.
The report was based on data from the National Health and Nutrition Examination Survey (NHANES) on adults aged 18 years and older. The findings also indicate that approximately 20 million U.S. adults with high blood pressure and 37 million with high cholesterol are not being treated for these conditions.
The prevalence of control of high blood pressure was 29% among adults without health insurance, and the control of high cholesterol was less than 15% among those with limited access to health care. But at least 80% of individuals with uncontrolled high blood pressure and high cholesterol have health insurance, Dr. Frieden noted.
For those with health insurance, the characteristics of their specific plan are more likely to affect how likely they are to have high blood pressure or high cholesterol under control than are their personal characteristics, he said.
High blood pressure was defined as blood pressure greater than 140/90 mmHg or reported use of blood pressure–lowering medication. The national prevalence of high blood pressure remained stable over the past decade, although 70% of those with hypertension were being treated and 46% were being controlled, according to the report.
The criteria for high cholesterol included anyone taking cholesterol medication or having a LDL cholesterol level of 100 mg/dL or higher for high-risk individuals, 130 mg/dL or higher for intermediate-risk individuals, and 160 mg/dL for those at low risk.
The proportion of adults treated for high cholesterol increased from 28% to 48% over the past decade, and the proportion of those controlling their high cholesterol increased from less than 20% to more than 30%.
The findings were limited by the lack of data on individuals in nursing homes and other institutions that are not included in NHANES databases, the CDC researchers noted in the report.
About 100,000 deaths [in the U.S.] are preventable by simple, low-cost improvements in our ability to control high blood pressure and high cholesterol," said Dr. Frieden. "Better control can save lives and save money."
The report is available online at www.cdc.gov/vitalsigns. More detailed information can be found in the Feb. 1 issue of the weekly Morbidity and Mortality Report (MMWR early release/vol. 60; Feb. 1, 2011).
FROM A VITAL SIGNS REPORT RELEASED BY THE CENTERS FOR DISEASE CONTROL AND PREVENTION
Hypertension, Cholesterol Are Largely Uncontrolled in U.S. Adults
Approximately 68 million American adults have high blood pressure and 71 million have high cholesterol, and the conditions are uncontrolled in 37 million and 48 million, respectively, according to a Vital Signs report released by the Centers for Disease Control and Prevention on Feb. 1.
"Heart disease is the leading killer in America, and the bottom line is that high blood pressure and high cholesterol are out of control for most Americans who have these conditions," CDC director Dr. Thomas R. Frieden said during the teleconference accompanying the report’s release.
High blood pressure and high cholesterol remain top risk factors for life-threatening conditions including strokes, heart attacks, and vascular diseases, he added.
Dr. Frieden had a message for physicians: Controlling high blood pressure and cholesterol is one of the most important things you can do for your patients. Know how many of your patients have high blood pressure and high cholesterol, what proportion are controlled, and what can be done to help more patients get these conditions under control, he said.
"We have seen many examples of health systems, health programs, and doctors’ offices using information technology to support patients and drastically improve the levels of control, and that’s something that is needed throughout health care in this country," he added.
The report was based on data from the National Health and Nutrition Examination Survey (NHANES) on adults aged 18 years and older. The findings also indicate that approximately 20 million U.S. adults with high blood pressure and 37 million with high cholesterol are not being treated for these conditions.
The prevalence of control of high blood pressure was 29% among adults without health insurance, and the control of high cholesterol was less than 15% among those with limited access to health care. But at least 80% of individuals with uncontrolled high blood pressure and high cholesterol have health insurance, Dr. Frieden noted.
For those with health insurance, the characteristics of their specific plan are more likely to affect how likely they are to have high blood pressure or high cholesterol under control than are their personal characteristics, he said.
High blood pressure was defined as blood pressure greater than 140/90 mmHg or reported use of blood pressure–lowering medication. The national prevalence of high blood pressure remained stable over the past decade, although 70% of those with hypertension were being treated and 46% were being controlled, according to the report.
The criteria for high cholesterol included anyone taking cholesterol medication or having a LDL cholesterol level of 100 mg/dL or higher for high-risk individuals, 130 mg/dL or higher for intermediate-risk individuals, and 160 mg/dL for those at low risk.
The proportion of adults treated for high cholesterol increased from 28% to 48% over the past decade, and the proportion of those controlling their high cholesterol increased from less than 20% to more than 30%.
The findings were limited by the lack of data on individuals in nursing homes and other institutions that are not included in NHANES databases, the CDC researchers noted in the report.
About 100,000 deaths [in the U.S.] are preventable by simple, low-cost improvements in our ability to control high blood pressure and high cholesterol," said Dr. Frieden. "Better control can save lives and save money."
The report is available online. More detailed information can be found in the Feb. 1 issue of the weekly Morbidity and Mortality Report (MMWR early release/vol. 60; Feb. 1, 2011).
Approximately 68 million American adults have high blood pressure and 71 million have high cholesterol, and the conditions are uncontrolled in 37 million and 48 million, respectively, according to a Vital Signs report released by the Centers for Disease Control and Prevention on Feb. 1.
"Heart disease is the leading killer in America, and the bottom line is that high blood pressure and high cholesterol are out of control for most Americans who have these conditions," CDC director Dr. Thomas R. Frieden said during the teleconference accompanying the report’s release.
High blood pressure and high cholesterol remain top risk factors for life-threatening conditions including strokes, heart attacks, and vascular diseases, he added.
Dr. Frieden had a message for physicians: Controlling high blood pressure and cholesterol is one of the most important things you can do for your patients. Know how many of your patients have high blood pressure and high cholesterol, what proportion are controlled, and what can be done to help more patients get these conditions under control, he said.
"We have seen many examples of health systems, health programs, and doctors’ offices using information technology to support patients and drastically improve the levels of control, and that’s something that is needed throughout health care in this country," he added.
The report was based on data from the National Health and Nutrition Examination Survey (NHANES) on adults aged 18 years and older. The findings also indicate that approximately 20 million U.S. adults with high blood pressure and 37 million with high cholesterol are not being treated for these conditions.
The prevalence of control of high blood pressure was 29% among adults without health insurance, and the control of high cholesterol was less than 15% among those with limited access to health care. But at least 80% of individuals with uncontrolled high blood pressure and high cholesterol have health insurance, Dr. Frieden noted.
For those with health insurance, the characteristics of their specific plan are more likely to affect how likely they are to have high blood pressure or high cholesterol under control than are their personal characteristics, he said.
High blood pressure was defined as blood pressure greater than 140/90 mmHg or reported use of blood pressure–lowering medication. The national prevalence of high blood pressure remained stable over the past decade, although 70% of those with hypertension were being treated and 46% were being controlled, according to the report.
The criteria for high cholesterol included anyone taking cholesterol medication or having a LDL cholesterol level of 100 mg/dL or higher for high-risk individuals, 130 mg/dL or higher for intermediate-risk individuals, and 160 mg/dL for those at low risk.
The proportion of adults treated for high cholesterol increased from 28% to 48% over the past decade, and the proportion of those controlling their high cholesterol increased from less than 20% to more than 30%.
The findings were limited by the lack of data on individuals in nursing homes and other institutions that are not included in NHANES databases, the CDC researchers noted in the report.
About 100,000 deaths [in the U.S.] are preventable by simple, low-cost improvements in our ability to control high blood pressure and high cholesterol," said Dr. Frieden. "Better control can save lives and save money."
The report is available online. More detailed information can be found in the Feb. 1 issue of the weekly Morbidity and Mortality Report (MMWR early release/vol. 60; Feb. 1, 2011).
Approximately 68 million American adults have high blood pressure and 71 million have high cholesterol, and the conditions are uncontrolled in 37 million and 48 million, respectively, according to a Vital Signs report released by the Centers for Disease Control and Prevention on Feb. 1.
"Heart disease is the leading killer in America, and the bottom line is that high blood pressure and high cholesterol are out of control for most Americans who have these conditions," CDC director Dr. Thomas R. Frieden said during the teleconference accompanying the report’s release.
High blood pressure and high cholesterol remain top risk factors for life-threatening conditions including strokes, heart attacks, and vascular diseases, he added.
Dr. Frieden had a message for physicians: Controlling high blood pressure and cholesterol is one of the most important things you can do for your patients. Know how many of your patients have high blood pressure and high cholesterol, what proportion are controlled, and what can be done to help more patients get these conditions under control, he said.
"We have seen many examples of health systems, health programs, and doctors’ offices using information technology to support patients and drastically improve the levels of control, and that’s something that is needed throughout health care in this country," he added.
The report was based on data from the National Health and Nutrition Examination Survey (NHANES) on adults aged 18 years and older. The findings also indicate that approximately 20 million U.S. adults with high blood pressure and 37 million with high cholesterol are not being treated for these conditions.
The prevalence of control of high blood pressure was 29% among adults without health insurance, and the control of high cholesterol was less than 15% among those with limited access to health care. But at least 80% of individuals with uncontrolled high blood pressure and high cholesterol have health insurance, Dr. Frieden noted.
For those with health insurance, the characteristics of their specific plan are more likely to affect how likely they are to have high blood pressure or high cholesterol under control than are their personal characteristics, he said.
High blood pressure was defined as blood pressure greater than 140/90 mmHg or reported use of blood pressure–lowering medication. The national prevalence of high blood pressure remained stable over the past decade, although 70% of those with hypertension were being treated and 46% were being controlled, according to the report.
The criteria for high cholesterol included anyone taking cholesterol medication or having a LDL cholesterol level of 100 mg/dL or higher for high-risk individuals, 130 mg/dL or higher for intermediate-risk individuals, and 160 mg/dL for those at low risk.
The proportion of adults treated for high cholesterol increased from 28% to 48% over the past decade, and the proportion of those controlling their high cholesterol increased from less than 20% to more than 30%.
The findings were limited by the lack of data on individuals in nursing homes and other institutions that are not included in NHANES databases, the CDC researchers noted in the report.
About 100,000 deaths [in the U.S.] are preventable by simple, low-cost improvements in our ability to control high blood pressure and high cholesterol," said Dr. Frieden. "Better control can save lives and save money."
The report is available online. More detailed information can be found in the Feb. 1 issue of the weekly Morbidity and Mortality Report (MMWR early release/vol. 60; Feb. 1, 2011).
FROM A VITAL SIGNS REPORT RELEASED BY THE CENTERS FOR DISEASE CONTROL AND PREVENTION
Smoking, Obesity Shortening U.S. Life Spans
The life expectancy of Americans falls short compared to that of their counterparts in other high-income countries, and smoking and obesity are key contributors to the difference, the National Research Council of the National Academies reported.
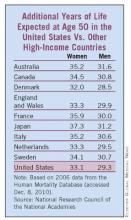
The life expectancy at birth for U.S. men increased from 65 years in 1950 to 76 years in 2006; for U.S. women, it increased from 71 to 81 years. Similarly, life expectancy at age 50 for men in the U.S. increased from 23 to 29 years. For American women, that figure rose from 27 to 33 years. Still, the improved life expectancy in the United States – the world's top spender on health care – fell below that of eight other rich countries, including Australia, Japan, and Canada (see chart).
The National Council on Aging commissioned the report, “Explaining Divergent Levels of Longevity in High-Income Countries,” to identify factors behind the differences in life expectancy. The report focused on life expectancy at age 50, because at least 90% of newborns in high-income countries now survive to age 50 years. The data were based primarily on an analysis of cause-of-death statistics.
“Smoking appears to be responsible for a good deal of the divergence in female life expectancy,” according to the report. The researchers estimated that 78% of the difference in life expectancy between American women and those in other high-income countries was attributable to smoking. Similarly, among men, smoking accounted for 41% of the difference.
The reduction in smoking in the United States over the past 20 years is likely to pay off in improved longevity trends in future decades, the researchers noted. A reduction or increase in smoking rates appears to take 20–30 years to impact mortality, they added.
Obesity also plays a significant role in the lagging U.S. longevity. Based on data from several studies, obesity accounts for approximately 20%–35% of the difference in longevity between Americans and residents of other countries.
Physical inactivity, social integration, and healthcare systems also likely contribute to increased mortality and differences in life expectancy among countries, but evaluation of these risk factors has been limited to observational studies, the researchers noted.
The National Research Council is the principal operating agency of the National Academy of Sciences and the National Academy of Engineering, which are private, nonprofit institutions. The report is available for purchase from the National Academies Press.
Vitals
Source Elsevier Global Medical News
The life expectancy of Americans falls short compared to that of their counterparts in other high-income countries, and smoking and obesity are key contributors to the difference, the National Research Council of the National Academies reported.
The life expectancy at birth for U.S. men increased from 65 years in 1950 to 76 years in 2006; for U.S. women, it increased from 71 to 81 years. Similarly, life expectancy at age 50 for men in the U.S. increased from 23 to 29 years. For American women, that figure rose from 27 to 33 years. Still, the improved life expectancy in the United States – the world's top spender on health care – fell below that of eight other rich countries, including Australia, Japan, and Canada (see chart).
The National Council on Aging commissioned the report, “Explaining Divergent Levels of Longevity in High-Income Countries,” to identify factors behind the differences in life expectancy. The report focused on life expectancy at age 50, because at least 90% of newborns in high-income countries now survive to age 50 years. The data were based primarily on an analysis of cause-of-death statistics.
“Smoking appears to be responsible for a good deal of the divergence in female life expectancy,” according to the report. The researchers estimated that 78% of the difference in life expectancy between American women and those in other high-income countries was attributable to smoking. Similarly, among men, smoking accounted for 41% of the difference.
The reduction in smoking in the United States over the past 20 years is likely to pay off in improved longevity trends in future decades, the researchers noted. A reduction or increase in smoking rates appears to take 20–30 years to impact mortality, they added.
Obesity also plays a significant role in the lagging U.S. longevity. Based on data from several studies, obesity accounts for approximately 20%–35% of the difference in longevity between Americans and residents of other countries.
Physical inactivity, social integration, and healthcare systems also likely contribute to increased mortality and differences in life expectancy among countries, but evaluation of these risk factors has been limited to observational studies, the researchers noted.
The National Research Council is the principal operating agency of the National Academy of Sciences and the National Academy of Engineering, which are private, nonprofit institutions. The report is available for purchase from the National Academies Press.
Vitals
Source Elsevier Global Medical News
The life expectancy of Americans falls short compared to that of their counterparts in other high-income countries, and smoking and obesity are key contributors to the difference, the National Research Council of the National Academies reported.
The life expectancy at birth for U.S. men increased from 65 years in 1950 to 76 years in 2006; for U.S. women, it increased from 71 to 81 years. Similarly, life expectancy at age 50 for men in the U.S. increased from 23 to 29 years. For American women, that figure rose from 27 to 33 years. Still, the improved life expectancy in the United States – the world's top spender on health care – fell below that of eight other rich countries, including Australia, Japan, and Canada (see chart).
The National Council on Aging commissioned the report, “Explaining Divergent Levels of Longevity in High-Income Countries,” to identify factors behind the differences in life expectancy. The report focused on life expectancy at age 50, because at least 90% of newborns in high-income countries now survive to age 50 years. The data were based primarily on an analysis of cause-of-death statistics.
“Smoking appears to be responsible for a good deal of the divergence in female life expectancy,” according to the report. The researchers estimated that 78% of the difference in life expectancy between American women and those in other high-income countries was attributable to smoking. Similarly, among men, smoking accounted for 41% of the difference.
The reduction in smoking in the United States over the past 20 years is likely to pay off in improved longevity trends in future decades, the researchers noted. A reduction or increase in smoking rates appears to take 20–30 years to impact mortality, they added.
Obesity also plays a significant role in the lagging U.S. longevity. Based on data from several studies, obesity accounts for approximately 20%–35% of the difference in longevity between Americans and residents of other countries.
Physical inactivity, social integration, and healthcare systems also likely contribute to increased mortality and differences in life expectancy among countries, but evaluation of these risk factors has been limited to observational studies, the researchers noted.
The National Research Council is the principal operating agency of the National Academy of Sciences and the National Academy of Engineering, which are private, nonprofit institutions. The report is available for purchase from the National Academies Press.
Vitals
Source Elsevier Global Medical News
From the National Research Council
Oral Apixaban Halved VTE Rate After Joint Replacement
ORLANDO — Oral apixaban reduced the incidence of major venous thromboembolism after joint replacement surgery by approximately half compared with enoxaparin, with no increased risk of bleeding, investigators have reported.
Of approximately 7,000 patients who underwent thromboprophylaxis after surgery, major VTE occurred in 0.68% of those who had received apixaban, compared with 1.50% who had been given enoxaparin. This was a significant difference, Gary E. Raskob, Ph.D., said.
Prevention of major venous thromboembolism is “a significant issue in health care in the United States,” where the number of knee and hip replacements is expected to increase, said Dr. Raskob, dean of the College of Public Health at the University of Oklahoma Health Sciences Center in Oklahoma City. To provide more precise estimates of the incidence of major VTE and safety outcomes, the researchers combined data from two phase III, randomized, double-blind trials of patients who had undergone knee (ADVANCE-2 study) or hip (ADVANCE-3) replacement. A total of 8,464 were randomized to apixaban, a novel orally administered factor Xa inhibitor (4,236 patients), or enoxaparin (4,228 patients).
Efficacy results related to VTE were based on 3,394 patients in each group. Major VTE occurred in 23 patients in the apixaban group (0.68%), vs. 51 patients in the enoxaparin group (1.50%).
Bleeding results were based on 4,174 apixaban patients and 4,228 enoxaparin patients. Major bleeding occurred in 31 patients in the apixaban group and 32 in the enoxaparin group (0.74% vs. 0.77%). Major bleeding at the surgical site occurred in 26 in the apixaban group and 27 in the enoxaparin group.
Dr. Raskob has financial relationships with Bristol-Meyers Squibb, Pfizer, Bayer, Johnson & Johnson, Sanofi Aventis, and Daiichi Sankyo.
To see an interview with Dr. Gary E. Raskob, go to
Source Heidi Splete/Elsevier Global Medical Newswww.rheumatologynews.com
ORLANDO — Oral apixaban reduced the incidence of major venous thromboembolism after joint replacement surgery by approximately half compared with enoxaparin, with no increased risk of bleeding, investigators have reported.
Of approximately 7,000 patients who underwent thromboprophylaxis after surgery, major VTE occurred in 0.68% of those who had received apixaban, compared with 1.50% who had been given enoxaparin. This was a significant difference, Gary E. Raskob, Ph.D., said.
Prevention of major venous thromboembolism is “a significant issue in health care in the United States,” where the number of knee and hip replacements is expected to increase, said Dr. Raskob, dean of the College of Public Health at the University of Oklahoma Health Sciences Center in Oklahoma City. To provide more precise estimates of the incidence of major VTE and safety outcomes, the researchers combined data from two phase III, randomized, double-blind trials of patients who had undergone knee (ADVANCE-2 study) or hip (ADVANCE-3) replacement. A total of 8,464 were randomized to apixaban, a novel orally administered factor Xa inhibitor (4,236 patients), or enoxaparin (4,228 patients).
Efficacy results related to VTE were based on 3,394 patients in each group. Major VTE occurred in 23 patients in the apixaban group (0.68%), vs. 51 patients in the enoxaparin group (1.50%).
Bleeding results were based on 4,174 apixaban patients and 4,228 enoxaparin patients. Major bleeding occurred in 31 patients in the apixaban group and 32 in the enoxaparin group (0.74% vs. 0.77%). Major bleeding at the surgical site occurred in 26 in the apixaban group and 27 in the enoxaparin group.
Dr. Raskob has financial relationships with Bristol-Meyers Squibb, Pfizer, Bayer, Johnson & Johnson, Sanofi Aventis, and Daiichi Sankyo.
To see an interview with Dr. Gary E. Raskob, go to
Source Heidi Splete/Elsevier Global Medical Newswww.rheumatologynews.com
ORLANDO — Oral apixaban reduced the incidence of major venous thromboembolism after joint replacement surgery by approximately half compared with enoxaparin, with no increased risk of bleeding, investigators have reported.
Of approximately 7,000 patients who underwent thromboprophylaxis after surgery, major VTE occurred in 0.68% of those who had received apixaban, compared with 1.50% who had been given enoxaparin. This was a significant difference, Gary E. Raskob, Ph.D., said.
Prevention of major venous thromboembolism is “a significant issue in health care in the United States,” where the number of knee and hip replacements is expected to increase, said Dr. Raskob, dean of the College of Public Health at the University of Oklahoma Health Sciences Center in Oklahoma City. To provide more precise estimates of the incidence of major VTE and safety outcomes, the researchers combined data from two phase III, randomized, double-blind trials of patients who had undergone knee (ADVANCE-2 study) or hip (ADVANCE-3) replacement. A total of 8,464 were randomized to apixaban, a novel orally administered factor Xa inhibitor (4,236 patients), or enoxaparin (4,228 patients).
Efficacy results related to VTE were based on 3,394 patients in each group. Major VTE occurred in 23 patients in the apixaban group (0.68%), vs. 51 patients in the enoxaparin group (1.50%).
Bleeding results were based on 4,174 apixaban patients and 4,228 enoxaparin patients. Major bleeding occurred in 31 patients in the apixaban group and 32 in the enoxaparin group (0.74% vs. 0.77%). Major bleeding at the surgical site occurred in 26 in the apixaban group and 27 in the enoxaparin group.
Dr. Raskob has financial relationships with Bristol-Meyers Squibb, Pfizer, Bayer, Johnson & Johnson, Sanofi Aventis, and Daiichi Sankyo.
To see an interview with Dr. Gary E. Raskob, go to
Source Heidi Splete/Elsevier Global Medical Newswww.rheumatologynews.com
New Dietary Guidelines Emphasize Healthy Body Weight As Goal
WASHINGTON – The new Dietary Guidelines for Americans 2010, released Jan. 31, take a four-pronged approach focus to improving American’s dietary habits by recommending balancing calories and exercise to achieve a healthy body weight, restricting sodium and saturated fat, increasing consumption of whole grains and healthy fats, and developing mindful behaviors around eating and food preparation.
"We are putting some of the best information in people’s hands, and that’s a big step forward," said Health and Human Services Secretary Kathleen Sebelius, who presented the guidelines with Department of Agriculture Secretary Tom Vilsack. The guidelines are a joint effort of the U.S. Department of Health and Human Services and the Department of Agriculture.
The guidelines, intended for children aged 2 years and older and adults, include 23 recommendations in four categories, plus six additional recommendations for specific population groups. The guidelines are meant to include those at increased risk of chronic disease. The four categories are:
Balancing calories to reduce weight: Recommendations in this category include getting more exercise and balancing it against calorie intake as appropriate for weight maintenance or weight loss.
• Reducing certain foods and food components: The guidelines call for consuming less than 2,300 mg of sodium daily. The recommendation is no more than 1,500 mg for blacks, people aged 51 years and older, as well as anyone regardless of age who has hypertension, diabetes, or chronic kidney disease. Other recommended reductions include having saturated fats comprise less that 10% of daily calories, and consuming less than 300 mg of cholesterol daily.
• Increasing certain foods and nutrients: The recommendations repeat previous dietary guidelines that call for whole-grain foods to comprise half of Americans’ grain intake. Other recommendations include replacing solid fats , eating more seafood in favor of some red meat and poultry, replacing full-fat dairy products with low-fat or fat-free options, and consuming a variety of protein-rich foods including eggs, beans, nuts, and soy.
• Building healthy eating patterns and behaviors: In addition to 20 recommendations relating to diet and exercise, the new guidelines include 3 recommendations that are less food specific: Select an eating pattern that "meets nutrient needs over time at an appropriate calorie level;" and keep a food journal to assess how food and beverage choices fit into a healthy eating pattern; follow food safety recommendations when cooking and eating to reduce the risk of foodborne illness.
Women of child-bearing age should boost iron intake by eating foods with easily absorbed heme iron and vitamin C–rich foods that enhance iron absorption. Additional recommendations include adding 400 mcg of folic acid daily for women, in addition to the folate found in a healthy diet. Recommendations for women who are pregnant or breast-feeding include eating 8-12 ounces of seafood per week, but limiting tuna consumption to 6 ounces per week and avoiding tilefish, shark, swordfish, and king mackerel because of their high mercury content. Pregnant women also are advised to take an iron supplement as recommended by their health care providers.
One additional recommendation for individuals aged 50 years and older: Consume vitamin B12-fortified foods as part of a daily diet or as supplements. However, the guidelines did not recommend a specific amount of daily B12 for this population.
Over the next few months, USDA and HHS will release consumer tips and tools to help Americans follow the guidelines, including a revised food pyramid.
For more information, check out the complete guidelines.
WASHINGTON – The new Dietary Guidelines for Americans 2010, released Jan. 31, take a four-pronged approach focus to improving American’s dietary habits by recommending balancing calories and exercise to achieve a healthy body weight, restricting sodium and saturated fat, increasing consumption of whole grains and healthy fats, and developing mindful behaviors around eating and food preparation.
"We are putting some of the best information in people’s hands, and that’s a big step forward," said Health and Human Services Secretary Kathleen Sebelius, who presented the guidelines with Department of Agriculture Secretary Tom Vilsack. The guidelines are a joint effort of the U.S. Department of Health and Human Services and the Department of Agriculture.
The guidelines, intended for children aged 2 years and older and adults, include 23 recommendations in four categories, plus six additional recommendations for specific population groups. The guidelines are meant to include those at increased risk of chronic disease. The four categories are:
Balancing calories to reduce weight: Recommendations in this category include getting more exercise and balancing it against calorie intake as appropriate for weight maintenance or weight loss.
• Reducing certain foods and food components: The guidelines call for consuming less than 2,300 mg of sodium daily. The recommendation is no more than 1,500 mg for blacks, people aged 51 years and older, as well as anyone regardless of age who has hypertension, diabetes, or chronic kidney disease. Other recommended reductions include having saturated fats comprise less that 10% of daily calories, and consuming less than 300 mg of cholesterol daily.
• Increasing certain foods and nutrients: The recommendations repeat previous dietary guidelines that call for whole-grain foods to comprise half of Americans’ grain intake. Other recommendations include replacing solid fats , eating more seafood in favor of some red meat and poultry, replacing full-fat dairy products with low-fat or fat-free options, and consuming a variety of protein-rich foods including eggs, beans, nuts, and soy.
• Building healthy eating patterns and behaviors: In addition to 20 recommendations relating to diet and exercise, the new guidelines include 3 recommendations that are less food specific: Select an eating pattern that "meets nutrient needs over time at an appropriate calorie level;" and keep a food journal to assess how food and beverage choices fit into a healthy eating pattern; follow food safety recommendations when cooking and eating to reduce the risk of foodborne illness.
Women of child-bearing age should boost iron intake by eating foods with easily absorbed heme iron and vitamin C–rich foods that enhance iron absorption. Additional recommendations include adding 400 mcg of folic acid daily for women, in addition to the folate found in a healthy diet. Recommendations for women who are pregnant or breast-feeding include eating 8-12 ounces of seafood per week, but limiting tuna consumption to 6 ounces per week and avoiding tilefish, shark, swordfish, and king mackerel because of their high mercury content. Pregnant women also are advised to take an iron supplement as recommended by their health care providers.
One additional recommendation for individuals aged 50 years and older: Consume vitamin B12-fortified foods as part of a daily diet or as supplements. However, the guidelines did not recommend a specific amount of daily B12 for this population.
Over the next few months, USDA and HHS will release consumer tips and tools to help Americans follow the guidelines, including a revised food pyramid.
For more information, check out the complete guidelines.
WASHINGTON – The new Dietary Guidelines for Americans 2010, released Jan. 31, take a four-pronged approach focus to improving American’s dietary habits by recommending balancing calories and exercise to achieve a healthy body weight, restricting sodium and saturated fat, increasing consumption of whole grains and healthy fats, and developing mindful behaviors around eating and food preparation.
"We are putting some of the best information in people’s hands, and that’s a big step forward," said Health and Human Services Secretary Kathleen Sebelius, who presented the guidelines with Department of Agriculture Secretary Tom Vilsack. The guidelines are a joint effort of the U.S. Department of Health and Human Services and the Department of Agriculture.
The guidelines, intended for children aged 2 years and older and adults, include 23 recommendations in four categories, plus six additional recommendations for specific population groups. The guidelines are meant to include those at increased risk of chronic disease. The four categories are:
Balancing calories to reduce weight: Recommendations in this category include getting more exercise and balancing it against calorie intake as appropriate for weight maintenance or weight loss.
• Reducing certain foods and food components: The guidelines call for consuming less than 2,300 mg of sodium daily. The recommendation is no more than 1,500 mg for blacks, people aged 51 years and older, as well as anyone regardless of age who has hypertension, diabetes, or chronic kidney disease. Other recommended reductions include having saturated fats comprise less that 10% of daily calories, and consuming less than 300 mg of cholesterol daily.
• Increasing certain foods and nutrients: The recommendations repeat previous dietary guidelines that call for whole-grain foods to comprise half of Americans’ grain intake. Other recommendations include replacing solid fats , eating more seafood in favor of some red meat and poultry, replacing full-fat dairy products with low-fat or fat-free options, and consuming a variety of protein-rich foods including eggs, beans, nuts, and soy.
• Building healthy eating patterns and behaviors: In addition to 20 recommendations relating to diet and exercise, the new guidelines include 3 recommendations that are less food specific: Select an eating pattern that "meets nutrient needs over time at an appropriate calorie level;" and keep a food journal to assess how food and beverage choices fit into a healthy eating pattern; follow food safety recommendations when cooking and eating to reduce the risk of foodborne illness.
Women of child-bearing age should boost iron intake by eating foods with easily absorbed heme iron and vitamin C–rich foods that enhance iron absorption. Additional recommendations include adding 400 mcg of folic acid daily for women, in addition to the folate found in a healthy diet. Recommendations for women who are pregnant or breast-feeding include eating 8-12 ounces of seafood per week, but limiting tuna consumption to 6 ounces per week and avoiding tilefish, shark, swordfish, and king mackerel because of their high mercury content. Pregnant women also are advised to take an iron supplement as recommended by their health care providers.
One additional recommendation for individuals aged 50 years and older: Consume vitamin B12-fortified foods as part of a daily diet or as supplements. However, the guidelines did not recommend a specific amount of daily B12 for this population.
Over the next few months, USDA and HHS will release consumer tips and tools to help Americans follow the guidelines, including a revised food pyramid.
For more information, check out the complete guidelines.
FROM THE U.S. DEPARTMENTS OF AGRICULTURE AND HEALTH AND HUMAN SERVICES
New Dietary Guidelines Emphasize Healthy Body Weight As Goal
WASHINGTON – The new Dietary Guidelines for Americans 2010, released Jan. 31, take a four-pronged approach focus to improving American’s dietary habits by recommending balancing calories and exercise to achieve a healthy body weight, restricting sodium and saturated fat, increasing consumption of whole grains and healthy fats, and developing mindful behaviors around eating and food preparation.
"We are putting some of the best information in people’s hands, and that’s a big step forward," said Health and Human Services Secretary Kathleen Sebelius, who presented the guidelines with Department of Agriculture Secretary Tom Vilsack. The guidelines are a joint effort of the U.S. Department of Health and Human Services and the Department of Agriculture.
The guidelines, intended for children aged 2 years and older and adults, include 23 recommendations in four categories, plus six additional recommendations for specific population groups. The guidelines are meant to include those at increased risk of chronic disease. The four categories are:
Balancing calories to reduce weight: Recommendations in this category include getting more exercise and balancing it against calorie intake as appropriate for weight maintenance or weight loss.
• Reducing certain foods and food components: The guidelines call for consuming less than 2,300 mg of sodium daily. The recommendation is no more than 1,500 mg for blacks, people aged 51 years and older, as well as anyone regardless of age who has hypertension, diabetes, or chronic kidney disease. Other recommended reductions include having saturated fats comprise less that 10% of daily calories, and consuming less than 300 mg of cholesterol daily.
• Increasing certain foods and nutrients: The recommendations repeat previous dietary guidelines that call for whole-grain foods to comprise half of Americans’ grain intake. Other recommendations include replacing solid fats , eating more seafood in favor of some red meat and poultry, replacing full-fat dairy products with low-fat or fat-free options, and consuming a variety of protein-rich foods including eggs, beans, nuts, and soy.
• Building healthy eating patterns and behaviors: In addition to 20 recommendations relating to diet and exercise, the new guidelines include 3 recommendations that are less food specific: Select an eating pattern that "meets nutrient needs over time at an appropriate calorie level;" and keep a food journal to assess how food and beverage choices fit into a healthy eating pattern; follow food safety recommendations when cooking and eating to reduce the risk of foodborne illness.
Women of child-bearing age should boost iron intake by eating foods with easily absorbed heme iron and vitamin C–rich foods that enhance iron absorption. Additional recommendations include adding 400 mcg of folic acid daily for women, in addition to the folate found in a healthy diet. Recommendations for women who are pregnant or breast-feeding include eating 8-12 ounces of seafood per week, but limiting tuna consumption to 6 ounces per week and avoiding tilefish, shark, swordfish, and king mackerel because of their high mercury content. Pregnant women also are advised to take an iron supplement as recommended by their health care providers.
One additional recommendation for individuals aged 50 years and older: Consume vitamin B12-fortified foods as part of a daily diet or as supplements. However, the guidelines did not recommend a specific amount of daily B12 for this population.
Over the next few months, USDA and HHS will release consumer tips and tools to help Americans follow the guidelines, including a revised food pyramid.
For more information, check out the complete guidelines.
WASHINGTON – The new Dietary Guidelines for Americans 2010, released Jan. 31, take a four-pronged approach focus to improving American’s dietary habits by recommending balancing calories and exercise to achieve a healthy body weight, restricting sodium and saturated fat, increasing consumption of whole grains and healthy fats, and developing mindful behaviors around eating and food preparation.
"We are putting some of the best information in people’s hands, and that’s a big step forward," said Health and Human Services Secretary Kathleen Sebelius, who presented the guidelines with Department of Agriculture Secretary Tom Vilsack. The guidelines are a joint effort of the U.S. Department of Health and Human Services and the Department of Agriculture.
The guidelines, intended for children aged 2 years and older and adults, include 23 recommendations in four categories, plus six additional recommendations for specific population groups. The guidelines are meant to include those at increased risk of chronic disease. The four categories are:
Balancing calories to reduce weight: Recommendations in this category include getting more exercise and balancing it against calorie intake as appropriate for weight maintenance or weight loss.
• Reducing certain foods and food components: The guidelines call for consuming less than 2,300 mg of sodium daily. The recommendation is no more than 1,500 mg for blacks, people aged 51 years and older, as well as anyone regardless of age who has hypertension, diabetes, or chronic kidney disease. Other recommended reductions include having saturated fats comprise less that 10% of daily calories, and consuming less than 300 mg of cholesterol daily.
• Increasing certain foods and nutrients: The recommendations repeat previous dietary guidelines that call for whole-grain foods to comprise half of Americans’ grain intake. Other recommendations include replacing solid fats , eating more seafood in favor of some red meat and poultry, replacing full-fat dairy products with low-fat or fat-free options, and consuming a variety of protein-rich foods including eggs, beans, nuts, and soy.
• Building healthy eating patterns and behaviors: In addition to 20 recommendations relating to diet and exercise, the new guidelines include 3 recommendations that are less food specific: Select an eating pattern that "meets nutrient needs over time at an appropriate calorie level;" and keep a food journal to assess how food and beverage choices fit into a healthy eating pattern; follow food safety recommendations when cooking and eating to reduce the risk of foodborne illness.
Women of child-bearing age should boost iron intake by eating foods with easily absorbed heme iron and vitamin C–rich foods that enhance iron absorption. Additional recommendations include adding 400 mcg of folic acid daily for women, in addition to the folate found in a healthy diet. Recommendations for women who are pregnant or breast-feeding include eating 8-12 ounces of seafood per week, but limiting tuna consumption to 6 ounces per week and avoiding tilefish, shark, swordfish, and king mackerel because of their high mercury content. Pregnant women also are advised to take an iron supplement as recommended by their health care providers.
One additional recommendation for individuals aged 50 years and older: Consume vitamin B12-fortified foods as part of a daily diet or as supplements. However, the guidelines did not recommend a specific amount of daily B12 for this population.
Over the next few months, USDA and HHS will release consumer tips and tools to help Americans follow the guidelines, including a revised food pyramid.
For more information, check out the complete guidelines.
WASHINGTON – The new Dietary Guidelines for Americans 2010, released Jan. 31, take a four-pronged approach focus to improving American’s dietary habits by recommending balancing calories and exercise to achieve a healthy body weight, restricting sodium and saturated fat, increasing consumption of whole grains and healthy fats, and developing mindful behaviors around eating and food preparation.
"We are putting some of the best information in people’s hands, and that’s a big step forward," said Health and Human Services Secretary Kathleen Sebelius, who presented the guidelines with Department of Agriculture Secretary Tom Vilsack. The guidelines are a joint effort of the U.S. Department of Health and Human Services and the Department of Agriculture.
The guidelines, intended for children aged 2 years and older and adults, include 23 recommendations in four categories, plus six additional recommendations for specific population groups. The guidelines are meant to include those at increased risk of chronic disease. The four categories are:
Balancing calories to reduce weight: Recommendations in this category include getting more exercise and balancing it against calorie intake as appropriate for weight maintenance or weight loss.
• Reducing certain foods and food components: The guidelines call for consuming less than 2,300 mg of sodium daily. The recommendation is no more than 1,500 mg for blacks, people aged 51 years and older, as well as anyone regardless of age who has hypertension, diabetes, or chronic kidney disease. Other recommended reductions include having saturated fats comprise less that 10% of daily calories, and consuming less than 300 mg of cholesterol daily.
• Increasing certain foods and nutrients: The recommendations repeat previous dietary guidelines that call for whole-grain foods to comprise half of Americans’ grain intake. Other recommendations include replacing solid fats , eating more seafood in favor of some red meat and poultry, replacing full-fat dairy products with low-fat or fat-free options, and consuming a variety of protein-rich foods including eggs, beans, nuts, and soy.
• Building healthy eating patterns and behaviors: In addition to 20 recommendations relating to diet and exercise, the new guidelines include 3 recommendations that are less food specific: Select an eating pattern that "meets nutrient needs over time at an appropriate calorie level;" and keep a food journal to assess how food and beverage choices fit into a healthy eating pattern; follow food safety recommendations when cooking and eating to reduce the risk of foodborne illness.
Women of child-bearing age should boost iron intake by eating foods with easily absorbed heme iron and vitamin C–rich foods that enhance iron absorption. Additional recommendations include adding 400 mcg of folic acid daily for women, in addition to the folate found in a healthy diet. Recommendations for women who are pregnant or breast-feeding include eating 8-12 ounces of seafood per week, but limiting tuna consumption to 6 ounces per week and avoiding tilefish, shark, swordfish, and king mackerel because of their high mercury content. Pregnant women also are advised to take an iron supplement as recommended by their health care providers.
One additional recommendation for individuals aged 50 years and older: Consume vitamin B12-fortified foods as part of a daily diet or as supplements. However, the guidelines did not recommend a specific amount of daily B12 for this population.
Over the next few months, USDA and HHS will release consumer tips and tools to help Americans follow the guidelines, including a revised food pyramid.
For more information, check out the complete guidelines.
FROM THE U.S. DEPARTMENTS OF AGRICULTURE AND HEALTH AND HUMAN SERVICES
In the Pipeline: Three Novel Drugs Hit Three Different Targets in CLL
ORLANDO – Three novel agents with three different targets cleared phase I hurdles in chronic lymphocytic leukemia.
These investigational agents, still known by their drug company labels, demonstrated varying degrees of activity in heavily pretreated patients. In all three presentations, investigators concluded that further trials are warranted.
PCI-32765 Hits Bruton’s Tyrosine Kinase
In the first presentation, PCI-32765 was described as a novel oral selective inhibitor of Bruton’s tyrosine kinase (Btk), a mediator of B-cell receptor signaling. Btk is not expressed in T cells or NK cells, which makes it "an ideal therapeutic target for B-cell malignancies dependent on BCR [gene] signaling," said Dr. Jan A. Burger of the University of Texas M.D. Anderson Cancer Center in Houston.
Dr. Burger presented pooled data from 54 patients (median age, 68 years), 47 of whom had chronic lymphocytic leukemia (CLL) and 7 of whom had small lymphocytic leukemia (SLL). Outcomes included 1 complete response and 16 partial responses in a population who had had a median of 3 previous therapies (range, 1-10). Nearly all (95%) had previously received a nucleoside analogue and anti-CD20 agents. In addition, 21% had prior bendamustine and 9% had alemtuzumab.
The trial divided these patients into the following two groups:
• Phase IA. Of 23 patients enrolled, 16 were treated in 28-day cycles with 7 days of rest. They received doses from 1.25 mg/kg per day to 12.5 mg/kg per day of the study drug. The other seven patients were treated for cycles of 35 days with no rest. In this group, six received 8.3 mg/kg per day, and one received a fixed dose of 560 mg/day. The median follow-up was 8 months.
Among the 13 evaluable patients in phase IA, 1 patient (8%) had a complete response, 8 (62%) had a partial response, and 2 (15%) had nodal response with lymphocytosis.
• Phase IB. Of 38 patients enrolled, 11 were treatment naive and 27 were relapsed or refractory patients. All received 420 mg/day in 28-day cycles. The median follow-up was 2 months.
Among the 32 evaluable patients in the phase IB group, none had complete response, 8 patients (25%) had a partial response, and 17 patients (53%) had nodal response with lymphocytosis.
All told, of 39 patients who were evaluated for changes in lymph node disease, 87% had a nodal response to PCI-32765. "Rapid lymph node responses are associated with a transient lymphocytosis, indicating a unique phenomenon of BCR-targeted therapy," Dr. Burger commented.
Overall, no renal or hepatic adverse events have been reported, and no evidence has been seen of cumulative toxicity in patients with at least 6 months of follow-up, Dr. Burger said. Reported adverse events included diarrhea, nausea, vomiting, headache, and rash.
Although the numbers are small and the results are preliminary, "the lack of drug-related myelosuppression or cumulative toxicity supports further investigation in various CLL treatment settings," Dr. Burger said.
Pharmacyclics sponsored the trial. Dr. Burger had no financial conflicts to disclose. Several coauthors reported serving as a consultant or receiving honoraria or research funding from the company; four were employees with equity ownership.
CAL-101 Blocks the PI3K-Delta Pathway
Novel CAL-101, an orally bioavailable small molecule, inhibits PI3K-delta activity, according to findings described in the second presentation.
"Constitutive activation of the PI3K-delta pathway drives proliferation, survival, and abnormal trafficking of malignant B-cells in chronic lymphocytic leukemia," said Dr. Richard R. Furman, director of the CLL and Waldenström’s macroglobulinemia programs at Cornell University in New York City.
In this study of patients with previously treated hematologic malignancies, 54 CLL patients received 50 mg to 150 mg of CAL-101 twice daily, with continuous oral dosing for an average of eight 28-day cycles. The median age of the patients was 63 years and 82% were male. All patients had been treated with fludarabine. In addition, 98% had received rituximab, 87% had received an alkylating agent, and 31% had received alemtuzumab.
The overall response rate was 26%, and the lymph node response rate was 80%. In addition, CAL-101 was associated with nodal shrinkage in all patients in an intent-to-treat analysis. Patients with baseline thrombocytopenia (defined as platelet counts less than 100,000/mcL) experienced sustained improvements in platelet count (that is, greater than 100,000/mcL, or greater than 50%), Dr. Furman said.
The most common grade 3/4 hematologic adverse event was neutropenia (24%), and the most common grade 3/4 nonhematologic event was pneumonia (24%). "Grade 3/4 adverse events were largely due to prior therapy or underlying CLL," said Dr. Furman. No pattern of drug-related symptomatic adverse events was observed, and patients showed no dose-limiting toxicities over periods of exposure beyond 1 year.
The results support further studies of CAL-101 at a dosage of 150 mg twice daily as a frontline therapy for CLL patients, or as a single agent or combined with chemoimmunotherapy for CLL patients, Dr. Furman added.
Calistoga Pharmaceuticals sponsored the trial. Dr. Furman had no financial conflicts to disclose. Several coauthors disclosed consultancy for, employment with, or research funding from Calistoga Pharmaceuticals; seven were employees and/or held equity ownership in the company.
TRU-016 Tackles CD37
Dr. Furman also presented results from a dose-escalation study of TRU-016, a novel humanized anti-CD37 small modular immunopharmaceutical (SMIP) protein.
Studies in mice have suggested that CD37 is involved in regulating B-cell function. TRU-016 offers direct apoptosis with greater cell-killing potential than rituximab and greater antibody-dependent cellular cytotoxicity than rituximab or alemtuzumab, he said.
In this dose-finding study, 57 patients with relapsed or refractory CLL or SLL received one of nine dosages, ranging from 0.03 mg/kg to 20 mg/kg, given intravenously once a week for 4-12 weekly doses. In a second dosing schedule, patients received 3, 6, or 10 mg/kg on days 1, 3, and 5 of the first week of treatment, followed by 3-11 weekly doses three times a week. The patients had no organ function problems, and their platelet counts were greater than 30,000/mcL.
The overall response rate was 13%, based on 1996 National Cancer Institute criteria. The overall median reduction in lymphocytes in the intent-to-treat population was 60%.
In the 16 patients with one to two prior therapies, the overall response rate was 40% and the clinical response rate was 44%. No clinical response was noted in patients with three or more prior therapies, but there was an overall median reduction in lymphocytes of 60% from baseline to the end of treatment, Dr. Furman said. The median progression-free survival for all patients was 134 days.
Neutropenia, the most common adverse event, was reported in nine patients (16%). There was no apparent relationship between drug dose and adverse events, and a maximum tolerated dose was not reached in this study.
"Given B-cell selective target, independent single agent activity, and synergy with CLL therapies, TRU-016 combination trials in CLL patients are planned," he said.
Trubion Pharmaceuticals (now Emergent Biosolutions) sponsored the trial. Dr. Furman had no financial conflicts to disclose. Several coinvestigators disclosed consultancy for, employment with equity ownership in, or research funding from Trubion.
ORLANDO – Three novel agents with three different targets cleared phase I hurdles in chronic lymphocytic leukemia.
These investigational agents, still known by their drug company labels, demonstrated varying degrees of activity in heavily pretreated patients. In all three presentations, investigators concluded that further trials are warranted.
PCI-32765 Hits Bruton’s Tyrosine Kinase
In the first presentation, PCI-32765 was described as a novel oral selective inhibitor of Bruton’s tyrosine kinase (Btk), a mediator of B-cell receptor signaling. Btk is not expressed in T cells or NK cells, which makes it "an ideal therapeutic target for B-cell malignancies dependent on BCR [gene] signaling," said Dr. Jan A. Burger of the University of Texas M.D. Anderson Cancer Center in Houston.
Dr. Burger presented pooled data from 54 patients (median age, 68 years), 47 of whom had chronic lymphocytic leukemia (CLL) and 7 of whom had small lymphocytic leukemia (SLL). Outcomes included 1 complete response and 16 partial responses in a population who had had a median of 3 previous therapies (range, 1-10). Nearly all (95%) had previously received a nucleoside analogue and anti-CD20 agents. In addition, 21% had prior bendamustine and 9% had alemtuzumab.
The trial divided these patients into the following two groups:
• Phase IA. Of 23 patients enrolled, 16 were treated in 28-day cycles with 7 days of rest. They received doses from 1.25 mg/kg per day to 12.5 mg/kg per day of the study drug. The other seven patients were treated for cycles of 35 days with no rest. In this group, six received 8.3 mg/kg per day, and one received a fixed dose of 560 mg/day. The median follow-up was 8 months.
Among the 13 evaluable patients in phase IA, 1 patient (8%) had a complete response, 8 (62%) had a partial response, and 2 (15%) had nodal response with lymphocytosis.
• Phase IB. Of 38 patients enrolled, 11 were treatment naive and 27 were relapsed or refractory patients. All received 420 mg/day in 28-day cycles. The median follow-up was 2 months.
Among the 32 evaluable patients in the phase IB group, none had complete response, 8 patients (25%) had a partial response, and 17 patients (53%) had nodal response with lymphocytosis.
All told, of 39 patients who were evaluated for changes in lymph node disease, 87% had a nodal response to PCI-32765. "Rapid lymph node responses are associated with a transient lymphocytosis, indicating a unique phenomenon of BCR-targeted therapy," Dr. Burger commented.
Overall, no renal or hepatic adverse events have been reported, and no evidence has been seen of cumulative toxicity in patients with at least 6 months of follow-up, Dr. Burger said. Reported adverse events included diarrhea, nausea, vomiting, headache, and rash.
Although the numbers are small and the results are preliminary, "the lack of drug-related myelosuppression or cumulative toxicity supports further investigation in various CLL treatment settings," Dr. Burger said.
Pharmacyclics sponsored the trial. Dr. Burger had no financial conflicts to disclose. Several coauthors reported serving as a consultant or receiving honoraria or research funding from the company; four were employees with equity ownership.
CAL-101 Blocks the PI3K-Delta Pathway
Novel CAL-101, an orally bioavailable small molecule, inhibits PI3K-delta activity, according to findings described in the second presentation.
"Constitutive activation of the PI3K-delta pathway drives proliferation, survival, and abnormal trafficking of malignant B-cells in chronic lymphocytic leukemia," said Dr. Richard R. Furman, director of the CLL and Waldenström’s macroglobulinemia programs at Cornell University in New York City.
In this study of patients with previously treated hematologic malignancies, 54 CLL patients received 50 mg to 150 mg of CAL-101 twice daily, with continuous oral dosing for an average of eight 28-day cycles. The median age of the patients was 63 years and 82% were male. All patients had been treated with fludarabine. In addition, 98% had received rituximab, 87% had received an alkylating agent, and 31% had received alemtuzumab.
The overall response rate was 26%, and the lymph node response rate was 80%. In addition, CAL-101 was associated with nodal shrinkage in all patients in an intent-to-treat analysis. Patients with baseline thrombocytopenia (defined as platelet counts less than 100,000/mcL) experienced sustained improvements in platelet count (that is, greater than 100,000/mcL, or greater than 50%), Dr. Furman said.
The most common grade 3/4 hematologic adverse event was neutropenia (24%), and the most common grade 3/4 nonhematologic event was pneumonia (24%). "Grade 3/4 adverse events were largely due to prior therapy or underlying CLL," said Dr. Furman. No pattern of drug-related symptomatic adverse events was observed, and patients showed no dose-limiting toxicities over periods of exposure beyond 1 year.
The results support further studies of CAL-101 at a dosage of 150 mg twice daily as a frontline therapy for CLL patients, or as a single agent or combined with chemoimmunotherapy for CLL patients, Dr. Furman added.
Calistoga Pharmaceuticals sponsored the trial. Dr. Furman had no financial conflicts to disclose. Several coauthors disclosed consultancy for, employment with, or research funding from Calistoga Pharmaceuticals; seven were employees and/or held equity ownership in the company.
TRU-016 Tackles CD37
Dr. Furman also presented results from a dose-escalation study of TRU-016, a novel humanized anti-CD37 small modular immunopharmaceutical (SMIP) protein.
Studies in mice have suggested that CD37 is involved in regulating B-cell function. TRU-016 offers direct apoptosis with greater cell-killing potential than rituximab and greater antibody-dependent cellular cytotoxicity than rituximab or alemtuzumab, he said.
In this dose-finding study, 57 patients with relapsed or refractory CLL or SLL received one of nine dosages, ranging from 0.03 mg/kg to 20 mg/kg, given intravenously once a week for 4-12 weekly doses. In a second dosing schedule, patients received 3, 6, or 10 mg/kg on days 1, 3, and 5 of the first week of treatment, followed by 3-11 weekly doses three times a week. The patients had no organ function problems, and their platelet counts were greater than 30,000/mcL.
The overall response rate was 13%, based on 1996 National Cancer Institute criteria. The overall median reduction in lymphocytes in the intent-to-treat population was 60%.
In the 16 patients with one to two prior therapies, the overall response rate was 40% and the clinical response rate was 44%. No clinical response was noted in patients with three or more prior therapies, but there was an overall median reduction in lymphocytes of 60% from baseline to the end of treatment, Dr. Furman said. The median progression-free survival for all patients was 134 days.
Neutropenia, the most common adverse event, was reported in nine patients (16%). There was no apparent relationship between drug dose and adverse events, and a maximum tolerated dose was not reached in this study.
"Given B-cell selective target, independent single agent activity, and synergy with CLL therapies, TRU-016 combination trials in CLL patients are planned," he said.
Trubion Pharmaceuticals (now Emergent Biosolutions) sponsored the trial. Dr. Furman had no financial conflicts to disclose. Several coinvestigators disclosed consultancy for, employment with equity ownership in, or research funding from Trubion.
ORLANDO – Three novel agents with three different targets cleared phase I hurdles in chronic lymphocytic leukemia.
These investigational agents, still known by their drug company labels, demonstrated varying degrees of activity in heavily pretreated patients. In all three presentations, investigators concluded that further trials are warranted.
PCI-32765 Hits Bruton’s Tyrosine Kinase
In the first presentation, PCI-32765 was described as a novel oral selective inhibitor of Bruton’s tyrosine kinase (Btk), a mediator of B-cell receptor signaling. Btk is not expressed in T cells or NK cells, which makes it "an ideal therapeutic target for B-cell malignancies dependent on BCR [gene] signaling," said Dr. Jan A. Burger of the University of Texas M.D. Anderson Cancer Center in Houston.
Dr. Burger presented pooled data from 54 patients (median age, 68 years), 47 of whom had chronic lymphocytic leukemia (CLL) and 7 of whom had small lymphocytic leukemia (SLL). Outcomes included 1 complete response and 16 partial responses in a population who had had a median of 3 previous therapies (range, 1-10). Nearly all (95%) had previously received a nucleoside analogue and anti-CD20 agents. In addition, 21% had prior bendamustine and 9% had alemtuzumab.
The trial divided these patients into the following two groups:
• Phase IA. Of 23 patients enrolled, 16 were treated in 28-day cycles with 7 days of rest. They received doses from 1.25 mg/kg per day to 12.5 mg/kg per day of the study drug. The other seven patients were treated for cycles of 35 days with no rest. In this group, six received 8.3 mg/kg per day, and one received a fixed dose of 560 mg/day. The median follow-up was 8 months.
Among the 13 evaluable patients in phase IA, 1 patient (8%) had a complete response, 8 (62%) had a partial response, and 2 (15%) had nodal response with lymphocytosis.
• Phase IB. Of 38 patients enrolled, 11 were treatment naive and 27 were relapsed or refractory patients. All received 420 mg/day in 28-day cycles. The median follow-up was 2 months.
Among the 32 evaluable patients in the phase IB group, none had complete response, 8 patients (25%) had a partial response, and 17 patients (53%) had nodal response with lymphocytosis.
All told, of 39 patients who were evaluated for changes in lymph node disease, 87% had a nodal response to PCI-32765. "Rapid lymph node responses are associated with a transient lymphocytosis, indicating a unique phenomenon of BCR-targeted therapy," Dr. Burger commented.
Overall, no renal or hepatic adverse events have been reported, and no evidence has been seen of cumulative toxicity in patients with at least 6 months of follow-up, Dr. Burger said. Reported adverse events included diarrhea, nausea, vomiting, headache, and rash.
Although the numbers are small and the results are preliminary, "the lack of drug-related myelosuppression or cumulative toxicity supports further investigation in various CLL treatment settings," Dr. Burger said.
Pharmacyclics sponsored the trial. Dr. Burger had no financial conflicts to disclose. Several coauthors reported serving as a consultant or receiving honoraria or research funding from the company; four were employees with equity ownership.
CAL-101 Blocks the PI3K-Delta Pathway
Novel CAL-101, an orally bioavailable small molecule, inhibits PI3K-delta activity, according to findings described in the second presentation.
"Constitutive activation of the PI3K-delta pathway drives proliferation, survival, and abnormal trafficking of malignant B-cells in chronic lymphocytic leukemia," said Dr. Richard R. Furman, director of the CLL and Waldenström’s macroglobulinemia programs at Cornell University in New York City.
In this study of patients with previously treated hematologic malignancies, 54 CLL patients received 50 mg to 150 mg of CAL-101 twice daily, with continuous oral dosing for an average of eight 28-day cycles. The median age of the patients was 63 years and 82% were male. All patients had been treated with fludarabine. In addition, 98% had received rituximab, 87% had received an alkylating agent, and 31% had received alemtuzumab.
The overall response rate was 26%, and the lymph node response rate was 80%. In addition, CAL-101 was associated with nodal shrinkage in all patients in an intent-to-treat analysis. Patients with baseline thrombocytopenia (defined as platelet counts less than 100,000/mcL) experienced sustained improvements in platelet count (that is, greater than 100,000/mcL, or greater than 50%), Dr. Furman said.
The most common grade 3/4 hematologic adverse event was neutropenia (24%), and the most common grade 3/4 nonhematologic event was pneumonia (24%). "Grade 3/4 adverse events were largely due to prior therapy or underlying CLL," said Dr. Furman. No pattern of drug-related symptomatic adverse events was observed, and patients showed no dose-limiting toxicities over periods of exposure beyond 1 year.
The results support further studies of CAL-101 at a dosage of 150 mg twice daily as a frontline therapy for CLL patients, or as a single agent or combined with chemoimmunotherapy for CLL patients, Dr. Furman added.
Calistoga Pharmaceuticals sponsored the trial. Dr. Furman had no financial conflicts to disclose. Several coauthors disclosed consultancy for, employment with, or research funding from Calistoga Pharmaceuticals; seven were employees and/or held equity ownership in the company.
TRU-016 Tackles CD37
Dr. Furman also presented results from a dose-escalation study of TRU-016, a novel humanized anti-CD37 small modular immunopharmaceutical (SMIP) protein.
Studies in mice have suggested that CD37 is involved in regulating B-cell function. TRU-016 offers direct apoptosis with greater cell-killing potential than rituximab and greater antibody-dependent cellular cytotoxicity than rituximab or alemtuzumab, he said.
In this dose-finding study, 57 patients with relapsed or refractory CLL or SLL received one of nine dosages, ranging from 0.03 mg/kg to 20 mg/kg, given intravenously once a week for 4-12 weekly doses. In a second dosing schedule, patients received 3, 6, or 10 mg/kg on days 1, 3, and 5 of the first week of treatment, followed by 3-11 weekly doses three times a week. The patients had no organ function problems, and their platelet counts were greater than 30,000/mcL.
The overall response rate was 13%, based on 1996 National Cancer Institute criteria. The overall median reduction in lymphocytes in the intent-to-treat population was 60%.
In the 16 patients with one to two prior therapies, the overall response rate was 40% and the clinical response rate was 44%. No clinical response was noted in patients with three or more prior therapies, but there was an overall median reduction in lymphocytes of 60% from baseline to the end of treatment, Dr. Furman said. The median progression-free survival for all patients was 134 days.
Neutropenia, the most common adverse event, was reported in nine patients (16%). There was no apparent relationship between drug dose and adverse events, and a maximum tolerated dose was not reached in this study.
"Given B-cell selective target, independent single agent activity, and synergy with CLL therapies, TRU-016 combination trials in CLL patients are planned," he said.
Trubion Pharmaceuticals (now Emergent Biosolutions) sponsored the trial. Dr. Furman had no financial conflicts to disclose. Several coinvestigators disclosed consultancy for, employment with equity ownership in, or research funding from Trubion.
Smoking, Obesity Responsible for Shorter U.S. Life Spans
The life expectancy of Americans falls short compared to that of their counterparts in other high-income countries, and smoking and obesity are key contributors to the difference, the National Research Council of the National Academies reported Jan. 25.
The life expectancy at birth for U.S. men increased from 65 years in 1950 to 76 years in 2006; for U.S. women, it increased from 71 to 81 years. Similarly, life expectancy at age 50 for men in the U.S. increased from 23 to 29 years. For American women, that figure rose from 27 to 33 years. Still, the improved life expectancy in the United States –the world’s top spender on health care -- fell below that of approximately nine other countries, including Australia, Japan, and Canada. (See graphic.)
The National Council on Aging commissioned the report, "Explaining Divergent Levels of Longevity in High-Income Countries," to identify factors behind the differences in life expectancy. The report focused on life expectancy at age 50, because at least 90% of newborns in high-income countries now survive to age 50 years. The data were based primarily on an analysis of cause-of-death statistics.
"Smoking appears to be responsible for a good deal of the divergence in female life expectancy," according to the report. The researchers estimated that 78% of the difference in life expectancy between American women and those in other high-income countries was attributable to smoking. Similarly, among men, smoking accounted for 41% of the difference.
The reduction in smoking in the United States over the past 20 years is likely to pay off in improved longevity trends in future decades, the researchers noted. A reduction or increase in smoking rates appears to take 20 to 30 years to impact mortality, they added.
Obesity also plays a significant role in the lagging U.S. longevity. Based on data from several studies, obesity accounts for approximately 20%-35% of the difference in longevity between Americans and residents of countries.
Physical inactivity, social integration, and healthcare systems also likely contribute to increased mortality and differences in life expectancy among countries, but evaluation of these risk factors has been limited to observational studies, the researchers noted.
The report was limited by a lack of markers to directly identify the impact on longevity of risk factors other than smoking, including obesity, physical inactivity, and stress, the researchers said.
The National Research Council is the principal operating agency of the National Academy of Sciences and the National Academy of Engineering, which are private, nonprofit institutions. The report is available for purchase from the National Academies Press.
The life expectancy of Americans falls short compared to that of their counterparts in other high-income countries, and smoking and obesity are key contributors to the difference, the National Research Council of the National Academies reported Jan. 25.
The life expectancy at birth for U.S. men increased from 65 years in 1950 to 76 years in 2006; for U.S. women, it increased from 71 to 81 years. Similarly, life expectancy at age 50 for men in the U.S. increased from 23 to 29 years. For American women, that figure rose from 27 to 33 years. Still, the improved life expectancy in the United States –the world’s top spender on health care -- fell below that of approximately nine other countries, including Australia, Japan, and Canada. (See graphic.)
The National Council on Aging commissioned the report, "Explaining Divergent Levels of Longevity in High-Income Countries," to identify factors behind the differences in life expectancy. The report focused on life expectancy at age 50, because at least 90% of newborns in high-income countries now survive to age 50 years. The data were based primarily on an analysis of cause-of-death statistics.
"Smoking appears to be responsible for a good deal of the divergence in female life expectancy," according to the report. The researchers estimated that 78% of the difference in life expectancy between American women and those in other high-income countries was attributable to smoking. Similarly, among men, smoking accounted for 41% of the difference.
The reduction in smoking in the United States over the past 20 years is likely to pay off in improved longevity trends in future decades, the researchers noted. A reduction or increase in smoking rates appears to take 20 to 30 years to impact mortality, they added.
Obesity also plays a significant role in the lagging U.S. longevity. Based on data from several studies, obesity accounts for approximately 20%-35% of the difference in longevity between Americans and residents of countries.
Physical inactivity, social integration, and healthcare systems also likely contribute to increased mortality and differences in life expectancy among countries, but evaluation of these risk factors has been limited to observational studies, the researchers noted.
The report was limited by a lack of markers to directly identify the impact on longevity of risk factors other than smoking, including obesity, physical inactivity, and stress, the researchers said.
The National Research Council is the principal operating agency of the National Academy of Sciences and the National Academy of Engineering, which are private, nonprofit institutions. The report is available for purchase from the National Academies Press.
The life expectancy of Americans falls short compared to that of their counterparts in other high-income countries, and smoking and obesity are key contributors to the difference, the National Research Council of the National Academies reported Jan. 25.
The life expectancy at birth for U.S. men increased from 65 years in 1950 to 76 years in 2006; for U.S. women, it increased from 71 to 81 years. Similarly, life expectancy at age 50 for men in the U.S. increased from 23 to 29 years. For American women, that figure rose from 27 to 33 years. Still, the improved life expectancy in the United States –the world’s top spender on health care -- fell below that of approximately nine other countries, including Australia, Japan, and Canada. (See graphic.)
The National Council on Aging commissioned the report, "Explaining Divergent Levels of Longevity in High-Income Countries," to identify factors behind the differences in life expectancy. The report focused on life expectancy at age 50, because at least 90% of newborns in high-income countries now survive to age 50 years. The data were based primarily on an analysis of cause-of-death statistics.
"Smoking appears to be responsible for a good deal of the divergence in female life expectancy," according to the report. The researchers estimated that 78% of the difference in life expectancy between American women and those in other high-income countries was attributable to smoking. Similarly, among men, smoking accounted for 41% of the difference.
The reduction in smoking in the United States over the past 20 years is likely to pay off in improved longevity trends in future decades, the researchers noted. A reduction or increase in smoking rates appears to take 20 to 30 years to impact mortality, they added.
Obesity also plays a significant role in the lagging U.S. longevity. Based on data from several studies, obesity accounts for approximately 20%-35% of the difference in longevity between Americans and residents of countries.
Physical inactivity, social integration, and healthcare systems also likely contribute to increased mortality and differences in life expectancy among countries, but evaluation of these risk factors has been limited to observational studies, the researchers noted.
The report was limited by a lack of markers to directly identify the impact on longevity of risk factors other than smoking, including obesity, physical inactivity, and stress, the researchers said.
The National Research Council is the principal operating agency of the National Academy of Sciences and the National Academy of Engineering, which are private, nonprofit institutions. The report is available for purchase from the National Academies Press.
FROM THE NATIONAL RESEARCH COUNCIL