User login
ASCO addresses financial barriers to cancer clinical trials
The American Society of Clinical Oncology (ASCO) has issued a policy statement addressing financial barriers to patient participation in cancer clinical trials.
ASCO’s policy statement outlines a series of recommendations designed to address multiple financial barriers that impede access to clinical trials, including patient costs that aren’t covered consistently by health insurance; a lack of information provided to patients about clinical trial costs; and limited available research data on financial hardships related to participation in clinical trials.
“Clinical trials are essential for evaluating the safety and efficacy of new cancer treatments, but cancer researchers have seen consistently low patient participation levels—especially among underserved patient populations—in part, due to the financial burdens facing many patients with cancer,” said ASCO President Monica M. Bertagnolli, MD.
“Addressing financial barriers will help improve the enrollment rate and the efficiency, quality, and applicability of cancer research. By including more—and more diverse—participants in our research studies, we expand our ability to care for all patients.”
The recommendations in ASCO’s policy statement include:
- Improve payer clinical trial coverage policies. Payment policies should be revised to be made consistent, streamlined, and transparent to all stakeholders.
- Payers should have clear definitions of “routine costs.”
- Payers should streamline prior authorization processes and facilitate trial enrollment through provider reimbursement of clinical trial-related services.
- State Medicaid programs should universally guarantee coverage of routine care costs of clinical trials for their beneficiaries.
- The U.S. Centers for Medicare & Medicaid Services (CMS) should revise current policy that requires Medicare Advantage beneficiaries to revert to fee-for-service coverage during clinical trials.
- CMS’s Innovation Center should explore the effectiveness of alternative payment models in support of clinical trial accrual.
- During the clinical trials development and enrollment process, provide patients with clear, transparent information about potential trial-related out-of-pocket costs and include mechanisms to support patient financial/health literacy.
- Clinical trial sponsors should perform—and make available to enrolling institutions—comprehensive, prospective coverage analyses.
- Research sites should consider offering in-house financial navigation/counseling to patients or consider partnering with organizations that provide such services.
- Design clinical trials to minimize incremental costs, consistent with scientific objectives and participant safety.
- Remove impediments to ethically appropriate financial compensation for trial-related out-of-pocket costs. Provision of such financial support should not be considered undue inducement.
- Office for Human Research Protections should develop guidance on targeted financial support.
- Incentivize research that will better characterize patient costs incurred for participating in cancer clinical trials and support the longer-term development of tools to identify and mitigate the risk of trial-associated financial hardship.
“Continued progress against cancer depends on improving patient access to participation in clinical research,” Dr. Bertagnolli said.
“The recommendations in ASCO’s statement aim to ensure that no patient is denied access to a clinical trial for financial reasons and that patients are not harmed financially because of their contributions to advancing science. Ultimately, this is about strengthening the nation’s cancer research enterprise as a whole.”
The American Society of Clinical Oncology (ASCO) has issued a policy statement addressing financial barriers to patient participation in cancer clinical trials.
ASCO’s policy statement outlines a series of recommendations designed to address multiple financial barriers that impede access to clinical trials, including patient costs that aren’t covered consistently by health insurance; a lack of information provided to patients about clinical trial costs; and limited available research data on financial hardships related to participation in clinical trials.
“Clinical trials are essential for evaluating the safety and efficacy of new cancer treatments, but cancer researchers have seen consistently low patient participation levels—especially among underserved patient populations—in part, due to the financial burdens facing many patients with cancer,” said ASCO President Monica M. Bertagnolli, MD.
“Addressing financial barriers will help improve the enrollment rate and the efficiency, quality, and applicability of cancer research. By including more—and more diverse—participants in our research studies, we expand our ability to care for all patients.”
The recommendations in ASCO’s policy statement include:
- Improve payer clinical trial coverage policies. Payment policies should be revised to be made consistent, streamlined, and transparent to all stakeholders.
- Payers should have clear definitions of “routine costs.”
- Payers should streamline prior authorization processes and facilitate trial enrollment through provider reimbursement of clinical trial-related services.
- State Medicaid programs should universally guarantee coverage of routine care costs of clinical trials for their beneficiaries.
- The U.S. Centers for Medicare & Medicaid Services (CMS) should revise current policy that requires Medicare Advantage beneficiaries to revert to fee-for-service coverage during clinical trials.
- CMS’s Innovation Center should explore the effectiveness of alternative payment models in support of clinical trial accrual.
- During the clinical trials development and enrollment process, provide patients with clear, transparent information about potential trial-related out-of-pocket costs and include mechanisms to support patient financial/health literacy.
- Clinical trial sponsors should perform—and make available to enrolling institutions—comprehensive, prospective coverage analyses.
- Research sites should consider offering in-house financial navigation/counseling to patients or consider partnering with organizations that provide such services.
- Design clinical trials to minimize incremental costs, consistent with scientific objectives and participant safety.
- Remove impediments to ethically appropriate financial compensation for trial-related out-of-pocket costs. Provision of such financial support should not be considered undue inducement.
- Office for Human Research Protections should develop guidance on targeted financial support.
- Incentivize research that will better characterize patient costs incurred for participating in cancer clinical trials and support the longer-term development of tools to identify and mitigate the risk of trial-associated financial hardship.
“Continued progress against cancer depends on improving patient access to participation in clinical research,” Dr. Bertagnolli said.
“The recommendations in ASCO’s statement aim to ensure that no patient is denied access to a clinical trial for financial reasons and that patients are not harmed financially because of their contributions to advancing science. Ultimately, this is about strengthening the nation’s cancer research enterprise as a whole.”
The American Society of Clinical Oncology (ASCO) has issued a policy statement addressing financial barriers to patient participation in cancer clinical trials.
ASCO’s policy statement outlines a series of recommendations designed to address multiple financial barriers that impede access to clinical trials, including patient costs that aren’t covered consistently by health insurance; a lack of information provided to patients about clinical trial costs; and limited available research data on financial hardships related to participation in clinical trials.
“Clinical trials are essential for evaluating the safety and efficacy of new cancer treatments, but cancer researchers have seen consistently low patient participation levels—especially among underserved patient populations—in part, due to the financial burdens facing many patients with cancer,” said ASCO President Monica M. Bertagnolli, MD.
“Addressing financial barriers will help improve the enrollment rate and the efficiency, quality, and applicability of cancer research. By including more—and more diverse—participants in our research studies, we expand our ability to care for all patients.”
The recommendations in ASCO’s policy statement include:
- Improve payer clinical trial coverage policies. Payment policies should be revised to be made consistent, streamlined, and transparent to all stakeholders.
- Payers should have clear definitions of “routine costs.”
- Payers should streamline prior authorization processes and facilitate trial enrollment through provider reimbursement of clinical trial-related services.
- State Medicaid programs should universally guarantee coverage of routine care costs of clinical trials for their beneficiaries.
- The U.S. Centers for Medicare & Medicaid Services (CMS) should revise current policy that requires Medicare Advantage beneficiaries to revert to fee-for-service coverage during clinical trials.
- CMS’s Innovation Center should explore the effectiveness of alternative payment models in support of clinical trial accrual.
- During the clinical trials development and enrollment process, provide patients with clear, transparent information about potential trial-related out-of-pocket costs and include mechanisms to support patient financial/health literacy.
- Clinical trial sponsors should perform—and make available to enrolling institutions—comprehensive, prospective coverage analyses.
- Research sites should consider offering in-house financial navigation/counseling to patients or consider partnering with organizations that provide such services.
- Design clinical trials to minimize incremental costs, consistent with scientific objectives and participant safety.
- Remove impediments to ethically appropriate financial compensation for trial-related out-of-pocket costs. Provision of such financial support should not be considered undue inducement.
- Office for Human Research Protections should develop guidance on targeted financial support.
- Incentivize research that will better characterize patient costs incurred for participating in cancer clinical trials and support the longer-term development of tools to identify and mitigate the risk of trial-associated financial hardship.
“Continued progress against cancer depends on improving patient access to participation in clinical research,” Dr. Bertagnolli said.
“The recommendations in ASCO’s statement aim to ensure that no patient is denied access to a clinical trial for financial reasons and that patients are not harmed financially because of their contributions to advancing science. Ultimately, this is about strengthening the nation’s cancer research enterprise as a whole.”
Doc reports ‘very encouraging’ results in penta-refractory MM
HOUSTON—Treatment with selinexor and low-dose dexamethasone can provide a “meaningful clinical benefit” in patients with penta-refractory multiple myeloma (MM), according to the principal investigator of the STORM trial.
Updated results from this phase 2 trial showed that selinexor and low-dose dexamethasone produced an overall response rate of 26.2% and a clinical benefit rate of 39.3%.
The median progression-free survival was 3.7 months, and the median overall survival was 8.6 months.
The trial’s principal investigator, Sundar Jagannath, MBBS, of the Mount Sinai School of Medicine in New York, N.Y., presented these results at the Society of Hematologic Oncology (SOHO) 2018 Annual Meeting as abstract MM-255.*
“The additional phase 2b clinical results ... are very encouraging for the patients suffering from penta-refractory multiple myeloma and their families,” Dr. Jagannath said.
“Of particular significance, for the nearly 40% of patients who had a minimal response or better, the median survival was 15.6 months, which provided the opportunity for a meaningful clinical benefit for patients on the STORM study.”
The study (NCT02336815) included 122 patients with penta-refractory MM. They had previously received bortezomib, carfilzomib, lenalidomide, pomalidomide, daratumumab, alkylating agents, and glucocorticoids. Their disease was refractory to glucocorticoids, at least one proteasome inhibitor, at least one immunomodulatory drug, daratumumab, and their most recent therapy.
The patients had received a median of 7 (range, 3-18) prior treatment regimens. Their median age was 65 (range, 40-86), 58% were male, and 53% had high-risk cytogenetics.
Patients received oral selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.
Response and survival
Two patients (1.6%) achieved stringent complete responses. They also had minimal residual disease negativity, one at the level of 1 x 10-6 and one at 1 x 10-4.
Six patients (4.9%) had very good partial responses, 24 (19.7%) had partial responses (PRs), 16 (13.1%) had minimal responses (MRs), and 48 (39.3%) had stable disease (SD).
Sixteen patients (13.1%) had progressive disease (PD), and 10 (8.2%) were not evaluable for response.
The overall response rate (PR or better) was 26.2% (n=32), the clinical benefit rate (MR or better) was 39.3% (n=48), and the disease control rate (SD or better) was 78.7% (n=98).
The median duration of response was 4.4 months (range, <1 to 12.2 months).
The median progression-free survival was 3.7 months overall, 4.6 months in patients with an MR or better, and 1.1 months in patients who had PD or were not evaluable.
The median overall survival was 8.6 months for the entire cohort. It was 15.6 months in patients with an MR or better and 1.7 months in patients who had PD or were not evaluable (P<0.0001).
Safety
The most common non-hematologic treatment-related adverse events (AEs) were fatigue/asthenia (69.9%), nausea (69.1%), anorexia (52.0%), weight loss (47.2%), vomiting (35.0%), diarrhea (33.3%), and hyponatremia (30.9%).
Hematologic treatment-related AEs included thrombocytopenia (67.5%), anemia (48.0%), neutropenia (35.8%), leukopenia (29.3%), and lymphopenia (13.8%).
The “most important” grade 3/4 AEs, according to Dr. Jagannath, were thrombocytopenia (53.7%), anemia (29.3%), fatigue (22.8%), hyponatremia (16.3%), nausea (9.8%), diarrhea (6.5%), anorexia (3.3%), and emesis (3.3%).
Twenty-three patients (19.5%) discontinued treatment due to a related AE.
This study was sponsored by Karyopharm Therapeutics. Dr. Jagannath reported relationships with Karyopharm, Janssen, Celgene, Amgen, and GSK.
*Information in the abstract differs from the presentation.
HOUSTON—Treatment with selinexor and low-dose dexamethasone can provide a “meaningful clinical benefit” in patients with penta-refractory multiple myeloma (MM), according to the principal investigator of the STORM trial.
Updated results from this phase 2 trial showed that selinexor and low-dose dexamethasone produced an overall response rate of 26.2% and a clinical benefit rate of 39.3%.
The median progression-free survival was 3.7 months, and the median overall survival was 8.6 months.
The trial’s principal investigator, Sundar Jagannath, MBBS, of the Mount Sinai School of Medicine in New York, N.Y., presented these results at the Society of Hematologic Oncology (SOHO) 2018 Annual Meeting as abstract MM-255.*
“The additional phase 2b clinical results ... are very encouraging for the patients suffering from penta-refractory multiple myeloma and their families,” Dr. Jagannath said.
“Of particular significance, for the nearly 40% of patients who had a minimal response or better, the median survival was 15.6 months, which provided the opportunity for a meaningful clinical benefit for patients on the STORM study.”
The study (NCT02336815) included 122 patients with penta-refractory MM. They had previously received bortezomib, carfilzomib, lenalidomide, pomalidomide, daratumumab, alkylating agents, and glucocorticoids. Their disease was refractory to glucocorticoids, at least one proteasome inhibitor, at least one immunomodulatory drug, daratumumab, and their most recent therapy.
The patients had received a median of 7 (range, 3-18) prior treatment regimens. Their median age was 65 (range, 40-86), 58% were male, and 53% had high-risk cytogenetics.
Patients received oral selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.
Response and survival
Two patients (1.6%) achieved stringent complete responses. They also had minimal residual disease negativity, one at the level of 1 x 10-6 and one at 1 x 10-4.
Six patients (4.9%) had very good partial responses, 24 (19.7%) had partial responses (PRs), 16 (13.1%) had minimal responses (MRs), and 48 (39.3%) had stable disease (SD).
Sixteen patients (13.1%) had progressive disease (PD), and 10 (8.2%) were not evaluable for response.
The overall response rate (PR or better) was 26.2% (n=32), the clinical benefit rate (MR or better) was 39.3% (n=48), and the disease control rate (SD or better) was 78.7% (n=98).
The median duration of response was 4.4 months (range, <1 to 12.2 months).
The median progression-free survival was 3.7 months overall, 4.6 months in patients with an MR or better, and 1.1 months in patients who had PD or were not evaluable.
The median overall survival was 8.6 months for the entire cohort. It was 15.6 months in patients with an MR or better and 1.7 months in patients who had PD or were not evaluable (P<0.0001).
Safety
The most common non-hematologic treatment-related adverse events (AEs) were fatigue/asthenia (69.9%), nausea (69.1%), anorexia (52.0%), weight loss (47.2%), vomiting (35.0%), diarrhea (33.3%), and hyponatremia (30.9%).
Hematologic treatment-related AEs included thrombocytopenia (67.5%), anemia (48.0%), neutropenia (35.8%), leukopenia (29.3%), and lymphopenia (13.8%).
The “most important” grade 3/4 AEs, according to Dr. Jagannath, were thrombocytopenia (53.7%), anemia (29.3%), fatigue (22.8%), hyponatremia (16.3%), nausea (9.8%), diarrhea (6.5%), anorexia (3.3%), and emesis (3.3%).
Twenty-three patients (19.5%) discontinued treatment due to a related AE.
This study was sponsored by Karyopharm Therapeutics. Dr. Jagannath reported relationships with Karyopharm, Janssen, Celgene, Amgen, and GSK.
*Information in the abstract differs from the presentation.
HOUSTON—Treatment with selinexor and low-dose dexamethasone can provide a “meaningful clinical benefit” in patients with penta-refractory multiple myeloma (MM), according to the principal investigator of the STORM trial.
Updated results from this phase 2 trial showed that selinexor and low-dose dexamethasone produced an overall response rate of 26.2% and a clinical benefit rate of 39.3%.
The median progression-free survival was 3.7 months, and the median overall survival was 8.6 months.
The trial’s principal investigator, Sundar Jagannath, MBBS, of the Mount Sinai School of Medicine in New York, N.Y., presented these results at the Society of Hematologic Oncology (SOHO) 2018 Annual Meeting as abstract MM-255.*
“The additional phase 2b clinical results ... are very encouraging for the patients suffering from penta-refractory multiple myeloma and their families,” Dr. Jagannath said.
“Of particular significance, for the nearly 40% of patients who had a minimal response or better, the median survival was 15.6 months, which provided the opportunity for a meaningful clinical benefit for patients on the STORM study.”
The study (NCT02336815) included 122 patients with penta-refractory MM. They had previously received bortezomib, carfilzomib, lenalidomide, pomalidomide, daratumumab, alkylating agents, and glucocorticoids. Their disease was refractory to glucocorticoids, at least one proteasome inhibitor, at least one immunomodulatory drug, daratumumab, and their most recent therapy.
The patients had received a median of 7 (range, 3-18) prior treatment regimens. Their median age was 65 (range, 40-86), 58% were male, and 53% had high-risk cytogenetics.
Patients received oral selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.
Response and survival
Two patients (1.6%) achieved stringent complete responses. They also had minimal residual disease negativity, one at the level of 1 x 10-6 and one at 1 x 10-4.
Six patients (4.9%) had very good partial responses, 24 (19.7%) had partial responses (PRs), 16 (13.1%) had minimal responses (MRs), and 48 (39.3%) had stable disease (SD).
Sixteen patients (13.1%) had progressive disease (PD), and 10 (8.2%) were not evaluable for response.
The overall response rate (PR or better) was 26.2% (n=32), the clinical benefit rate (MR or better) was 39.3% (n=48), and the disease control rate (SD or better) was 78.7% (n=98).
The median duration of response was 4.4 months (range, <1 to 12.2 months).
The median progression-free survival was 3.7 months overall, 4.6 months in patients with an MR or better, and 1.1 months in patients who had PD or were not evaluable.
The median overall survival was 8.6 months for the entire cohort. It was 15.6 months in patients with an MR or better and 1.7 months in patients who had PD or were not evaluable (P<0.0001).
Safety
The most common non-hematologic treatment-related adverse events (AEs) were fatigue/asthenia (69.9%), nausea (69.1%), anorexia (52.0%), weight loss (47.2%), vomiting (35.0%), diarrhea (33.3%), and hyponatremia (30.9%).
Hematologic treatment-related AEs included thrombocytopenia (67.5%), anemia (48.0%), neutropenia (35.8%), leukopenia (29.3%), and lymphopenia (13.8%).
The “most important” grade 3/4 AEs, according to Dr. Jagannath, were thrombocytopenia (53.7%), anemia (29.3%), fatigue (22.8%), hyponatremia (16.3%), nausea (9.8%), diarrhea (6.5%), anorexia (3.3%), and emesis (3.3%).
Twenty-three patients (19.5%) discontinued treatment due to a related AE.
This study was sponsored by Karyopharm Therapeutics. Dr. Jagannath reported relationships with Karyopharm, Janssen, Celgene, Amgen, and GSK.
*Information in the abstract differs from the presentation.
CAR T-cell therapy elicits responses in MM
BOSTON—Early results from a phase 1 trial suggest the chimeric antigen receptor (CAR) T-cell therapy P-BCMA-101 can produce responses in patients with relapsed/refractory multiple myeloma (MM).
All 11 patients treated have experienced some clinical response, with 8 patients achieving a partial response (PR) or better.
The most common adverse events were neutropenia and thrombocytopenia. One patient was suspected to have cytokine release syndrome, but the condition resolved without use of tociluzimab or steroids.
These results were presented at the 2018 CAR-TCR Summit by Eric Ostertag, MD, PhD, chief executive officer of Poseida Therapeutics Inc., the company developing P-BCMA-101.
Dr. Ostertag presented data on 11 patients with heavily pretreated MM. They had a median of six prior therapies. Their median age was 60, and 73% were considered high risk.
Prior to receiving P-BCMA-101, patients received conditioning with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) for 3 days.
Patients were then treated across three dose groups with average CAR T-cell doses of 51×106 (n=3), 152×106 (n=7), and 430×106 (n=1).
As of August 10, 2018, all 11 patients were still on study.
There were no dose-limiting toxicities. Eight patients developed neutropenia, and 5 had thrombocytopenia.
Researchers suspected cytokine release syndrome in one patient, but the condition resolved without tociluzimab or steroid treatment. There was no neurotoxicity reported, and none of the patients required admission to an intensive care unit.
All patients showed improvement in biomarkers following treatment.
Ten patients were evaluable for response by International Myeloma Working Group criteria. Seven of these patients achieved at least a PR, including very good partial responses (VGPRs) and stringent complete response (CR).
The eleventh patient also responded to treatment, but this patient has oligosecretory disease and was only evaluable by PET. The patient had a near-CR by PET.
Poseida Therapeutics would not disclose additional details regarding how many patients achieved a PR, VGPR, or CR, but the company plans to release more information on response at an upcoming meeting.
“The latest data results show that P-BCMA-101 induces deep responses in a heavily pretreated population with relapsed/refractory multiple myeloma, with some patients reaching VGPR and even stringent CR at early efficacy assessments,” Dr. Ostertag said.
“We believe our advantages of a purified product, where all cells express the CAR molecule, and a product with high levels of stem cell memory T cells, producing a more gradual and prolonged immune response against tumor cells, provide a significantly better therapeutic index when compared with other CAR-T therapeutics. We are also encouraged that P-BCMA-101 is demonstrating significant efficacy even at doses that have been ineffective for other anti-BCMA CAR-T therapies and that our response rates continue to improve as the dose increases.”
This study (NCT03288493) is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.
BOSTON—Early results from a phase 1 trial suggest the chimeric antigen receptor (CAR) T-cell therapy P-BCMA-101 can produce responses in patients with relapsed/refractory multiple myeloma (MM).
All 11 patients treated have experienced some clinical response, with 8 patients achieving a partial response (PR) or better.
The most common adverse events were neutropenia and thrombocytopenia. One patient was suspected to have cytokine release syndrome, but the condition resolved without use of tociluzimab or steroids.
These results were presented at the 2018 CAR-TCR Summit by Eric Ostertag, MD, PhD, chief executive officer of Poseida Therapeutics Inc., the company developing P-BCMA-101.
Dr. Ostertag presented data on 11 patients with heavily pretreated MM. They had a median of six prior therapies. Their median age was 60, and 73% were considered high risk.
Prior to receiving P-BCMA-101, patients received conditioning with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) for 3 days.
Patients were then treated across three dose groups with average CAR T-cell doses of 51×106 (n=3), 152×106 (n=7), and 430×106 (n=1).
As of August 10, 2018, all 11 patients were still on study.
There were no dose-limiting toxicities. Eight patients developed neutropenia, and 5 had thrombocytopenia.
Researchers suspected cytokine release syndrome in one patient, but the condition resolved without tociluzimab or steroid treatment. There was no neurotoxicity reported, and none of the patients required admission to an intensive care unit.
All patients showed improvement in biomarkers following treatment.
Ten patients were evaluable for response by International Myeloma Working Group criteria. Seven of these patients achieved at least a PR, including very good partial responses (VGPRs) and stringent complete response (CR).
The eleventh patient also responded to treatment, but this patient has oligosecretory disease and was only evaluable by PET. The patient had a near-CR by PET.
Poseida Therapeutics would not disclose additional details regarding how many patients achieved a PR, VGPR, or CR, but the company plans to release more information on response at an upcoming meeting.
“The latest data results show that P-BCMA-101 induces deep responses in a heavily pretreated population with relapsed/refractory multiple myeloma, with some patients reaching VGPR and even stringent CR at early efficacy assessments,” Dr. Ostertag said.
“We believe our advantages of a purified product, where all cells express the CAR molecule, and a product with high levels of stem cell memory T cells, producing a more gradual and prolonged immune response against tumor cells, provide a significantly better therapeutic index when compared with other CAR-T therapeutics. We are also encouraged that P-BCMA-101 is demonstrating significant efficacy even at doses that have been ineffective for other anti-BCMA CAR-T therapies and that our response rates continue to improve as the dose increases.”
This study (NCT03288493) is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.
BOSTON—Early results from a phase 1 trial suggest the chimeric antigen receptor (CAR) T-cell therapy P-BCMA-101 can produce responses in patients with relapsed/refractory multiple myeloma (MM).
All 11 patients treated have experienced some clinical response, with 8 patients achieving a partial response (PR) or better.
The most common adverse events were neutropenia and thrombocytopenia. One patient was suspected to have cytokine release syndrome, but the condition resolved without use of tociluzimab or steroids.
These results were presented at the 2018 CAR-TCR Summit by Eric Ostertag, MD, PhD, chief executive officer of Poseida Therapeutics Inc., the company developing P-BCMA-101.
Dr. Ostertag presented data on 11 patients with heavily pretreated MM. They had a median of six prior therapies. Their median age was 60, and 73% were considered high risk.
Prior to receiving P-BCMA-101, patients received conditioning with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) for 3 days.
Patients were then treated across three dose groups with average CAR T-cell doses of 51×106 (n=3), 152×106 (n=7), and 430×106 (n=1).
As of August 10, 2018, all 11 patients were still on study.
There were no dose-limiting toxicities. Eight patients developed neutropenia, and 5 had thrombocytopenia.
Researchers suspected cytokine release syndrome in one patient, but the condition resolved without tociluzimab or steroid treatment. There was no neurotoxicity reported, and none of the patients required admission to an intensive care unit.
All patients showed improvement in biomarkers following treatment.
Ten patients were evaluable for response by International Myeloma Working Group criteria. Seven of these patients achieved at least a PR, including very good partial responses (VGPRs) and stringent complete response (CR).
The eleventh patient also responded to treatment, but this patient has oligosecretory disease and was only evaluable by PET. The patient had a near-CR by PET.
Poseida Therapeutics would not disclose additional details regarding how many patients achieved a PR, VGPR, or CR, but the company plans to release more information on response at an upcoming meeting.
“The latest data results show that P-BCMA-101 induces deep responses in a heavily pretreated population with relapsed/refractory multiple myeloma, with some patients reaching VGPR and even stringent CR at early efficacy assessments,” Dr. Ostertag said.
“We believe our advantages of a purified product, where all cells express the CAR molecule, and a product with high levels of stem cell memory T cells, producing a more gradual and prolonged immune response against tumor cells, provide a significantly better therapeutic index when compared with other CAR-T therapeutics. We are also encouraged that P-BCMA-101 is demonstrating significant efficacy even at doses that have been ineffective for other anti-BCMA CAR-T therapies and that our response rates continue to improve as the dose increases.”
This study (NCT03288493) is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.
Kids with BCP-ALL exhibit immunological disparities at birth
Patients who develop B-cell precursor acute lymphoblastic leukemia (BCP-ALL) in childhood may have dysregulated immune function at birth, according to a study published in Cancer Research.
Investigators evaluated neonatal concentrations of inflammatory markers and found significant differences between children who were later diagnosed with BCP-ALL and leukemia-free control subjects.
“Our findings suggest that children who develop ALL are immunologically disparate already at birth,” said study author Signe Holst Søegaard, a PhD student at Statens Serum Institut in Copenhagen, Denmark.
“This may link to other observations suggesting that children who develop ALL respond differently to infections in early childhood, potentially promoting subsequent genetic events required for transformation to ALL, or speculations that they are unable to eliminate preleukemic cells.”
“Importantly, our study does not inform about the nature of the associations observed—i.e., whether they are causal or consequential. Accordingly, further studies are needed both to confirm the findings and to identify the underlying mechanisms.”
For this study, Søegaard and her colleagues measured concentrations of 10 inflammatory markers on neonatal dried blood spots from 178 patients with BCP-ALL and 178 matched controls. The patients were diagnosed with BCP-ALL at ages 1 to 9.
The inflammatory markers assessed were interleukin (IL)-6, its soluble receptor sIL-6Rα, IL-8, IL-10, IL-12, IL-17, IL-18, transforming growth factor (TGF)-β1, monocyte chemotactic protein (MCP)-1, and C-reactive protein (CRP).
Results
Compared to controls, children who later developed BCP-ALL had significantly different neonatal concentrations of eight inflammatory markers.
Concentrations of sIL-6Rα, IL-8, TGF-β1, MCP-1, and CRP were significantly lower among the BCP-ALL patients. The adjusted odds ratios (adjusted for birth weight and maternal age) of BCP-ALL were 0.82 for sIL-6Rα, 0.84 for IL-8, 0.83 for TGF-β1, 0.68 for MCP-1, and 0.83 for CRP.
On the other hand, concentrations of IL-6, IL-17, and IL-18 were significantly higher among BCP-ALL patients than controls. The adjusted odds ratios were 1.19 for IL-6, 1.12 for IL-17, and 1.08 for IL-18.
The investigators noted that IL-10 concentrations were too low for accurate measurement in all patients and controls. Additionally, a “large proportion” of patients and controls (31% to 61%) had IL-6 and IL-17 concentrations that were below the limit of detection.
“We also demonstrated that several previously shown ALL risk factors—namely, birth order, gestational age, and sex—were associated with the neonatal concentrations of inflammatory markers,” Søegaard said. “These findings raise the interesting possibility that the effects of some known ALL risk factors partly act through prenatal programming of immune function.”
The investigators found that increasing birth order was associated with significantly higher IL-18 and lower CRP concentrations.
Increasing gestational age was associated with significantly lower sIL-6Rα and TGF-β1 concentrations and higher CRP concentrations. And males had significantly lower sIL-6Rα and IL-8 concentrations and higher CRP concentrations than females.
However, none of the following factors were significantly associated with concentrations of inflammatory biomarkers: maternal age at delivery, maternal hospital contact due to infection during pregnancy, maternal prescription for antimicrobials during pregnancy, birth weight, and mode of delivery.
“Our findings underline the role the child’s baseline immune characteristics may play in the development of ALL,” Søegaard said. “However, we cannot yet use our research results to predict who will develop childhood ALL. In future studies, we will further characterize the relation between immune constitution at birth and risk of childhood ALL with the ultimate goal of developing preventive strategies targeting predisposed children.”
Søegaard noted that this study had its limitations, including the small number of inflammatory markers studied. In addition, the limited sample size made it impossible to detect potential differences between BCP-ALL subtypes.
The study was sponsored by the Dagmar Marshall Foundation, the A.P. Møller Foundation, the Danish Childhood Cancer Foundation, the Arvid Nilsson Foundation, and the Danish Cancer Research Foundation. There were no conflicts of interest disclosed.
Patients who develop B-cell precursor acute lymphoblastic leukemia (BCP-ALL) in childhood may have dysregulated immune function at birth, according to a study published in Cancer Research.
Investigators evaluated neonatal concentrations of inflammatory markers and found significant differences between children who were later diagnosed with BCP-ALL and leukemia-free control subjects.
“Our findings suggest that children who develop ALL are immunologically disparate already at birth,” said study author Signe Holst Søegaard, a PhD student at Statens Serum Institut in Copenhagen, Denmark.
“This may link to other observations suggesting that children who develop ALL respond differently to infections in early childhood, potentially promoting subsequent genetic events required for transformation to ALL, or speculations that they are unable to eliminate preleukemic cells.”
“Importantly, our study does not inform about the nature of the associations observed—i.e., whether they are causal or consequential. Accordingly, further studies are needed both to confirm the findings and to identify the underlying mechanisms.”
For this study, Søegaard and her colleagues measured concentrations of 10 inflammatory markers on neonatal dried blood spots from 178 patients with BCP-ALL and 178 matched controls. The patients were diagnosed with BCP-ALL at ages 1 to 9.
The inflammatory markers assessed were interleukin (IL)-6, its soluble receptor sIL-6Rα, IL-8, IL-10, IL-12, IL-17, IL-18, transforming growth factor (TGF)-β1, monocyte chemotactic protein (MCP)-1, and C-reactive protein (CRP).
Results
Compared to controls, children who later developed BCP-ALL had significantly different neonatal concentrations of eight inflammatory markers.
Concentrations of sIL-6Rα, IL-8, TGF-β1, MCP-1, and CRP were significantly lower among the BCP-ALL patients. The adjusted odds ratios (adjusted for birth weight and maternal age) of BCP-ALL were 0.82 for sIL-6Rα, 0.84 for IL-8, 0.83 for TGF-β1, 0.68 for MCP-1, and 0.83 for CRP.
On the other hand, concentrations of IL-6, IL-17, and IL-18 were significantly higher among BCP-ALL patients than controls. The adjusted odds ratios were 1.19 for IL-6, 1.12 for IL-17, and 1.08 for IL-18.
The investigators noted that IL-10 concentrations were too low for accurate measurement in all patients and controls. Additionally, a “large proportion” of patients and controls (31% to 61%) had IL-6 and IL-17 concentrations that were below the limit of detection.
“We also demonstrated that several previously shown ALL risk factors—namely, birth order, gestational age, and sex—were associated with the neonatal concentrations of inflammatory markers,” Søegaard said. “These findings raise the interesting possibility that the effects of some known ALL risk factors partly act through prenatal programming of immune function.”
The investigators found that increasing birth order was associated with significantly higher IL-18 and lower CRP concentrations.
Increasing gestational age was associated with significantly lower sIL-6Rα and TGF-β1 concentrations and higher CRP concentrations. And males had significantly lower sIL-6Rα and IL-8 concentrations and higher CRP concentrations than females.
However, none of the following factors were significantly associated with concentrations of inflammatory biomarkers: maternal age at delivery, maternal hospital contact due to infection during pregnancy, maternal prescription for antimicrobials during pregnancy, birth weight, and mode of delivery.
“Our findings underline the role the child’s baseline immune characteristics may play in the development of ALL,” Søegaard said. “However, we cannot yet use our research results to predict who will develop childhood ALL. In future studies, we will further characterize the relation between immune constitution at birth and risk of childhood ALL with the ultimate goal of developing preventive strategies targeting predisposed children.”
Søegaard noted that this study had its limitations, including the small number of inflammatory markers studied. In addition, the limited sample size made it impossible to detect potential differences between BCP-ALL subtypes.
The study was sponsored by the Dagmar Marshall Foundation, the A.P. Møller Foundation, the Danish Childhood Cancer Foundation, the Arvid Nilsson Foundation, and the Danish Cancer Research Foundation. There were no conflicts of interest disclosed.
Patients who develop B-cell precursor acute lymphoblastic leukemia (BCP-ALL) in childhood may have dysregulated immune function at birth, according to a study published in Cancer Research.
Investigators evaluated neonatal concentrations of inflammatory markers and found significant differences between children who were later diagnosed with BCP-ALL and leukemia-free control subjects.
“Our findings suggest that children who develop ALL are immunologically disparate already at birth,” said study author Signe Holst Søegaard, a PhD student at Statens Serum Institut in Copenhagen, Denmark.
“This may link to other observations suggesting that children who develop ALL respond differently to infections in early childhood, potentially promoting subsequent genetic events required for transformation to ALL, or speculations that they are unable to eliminate preleukemic cells.”
“Importantly, our study does not inform about the nature of the associations observed—i.e., whether they are causal or consequential. Accordingly, further studies are needed both to confirm the findings and to identify the underlying mechanisms.”
For this study, Søegaard and her colleagues measured concentrations of 10 inflammatory markers on neonatal dried blood spots from 178 patients with BCP-ALL and 178 matched controls. The patients were diagnosed with BCP-ALL at ages 1 to 9.
The inflammatory markers assessed were interleukin (IL)-6, its soluble receptor sIL-6Rα, IL-8, IL-10, IL-12, IL-17, IL-18, transforming growth factor (TGF)-β1, monocyte chemotactic protein (MCP)-1, and C-reactive protein (CRP).
Results
Compared to controls, children who later developed BCP-ALL had significantly different neonatal concentrations of eight inflammatory markers.
Concentrations of sIL-6Rα, IL-8, TGF-β1, MCP-1, and CRP were significantly lower among the BCP-ALL patients. The adjusted odds ratios (adjusted for birth weight and maternal age) of BCP-ALL were 0.82 for sIL-6Rα, 0.84 for IL-8, 0.83 for TGF-β1, 0.68 for MCP-1, and 0.83 for CRP.
On the other hand, concentrations of IL-6, IL-17, and IL-18 were significantly higher among BCP-ALL patients than controls. The adjusted odds ratios were 1.19 for IL-6, 1.12 for IL-17, and 1.08 for IL-18.
The investigators noted that IL-10 concentrations were too low for accurate measurement in all patients and controls. Additionally, a “large proportion” of patients and controls (31% to 61%) had IL-6 and IL-17 concentrations that were below the limit of detection.
“We also demonstrated that several previously shown ALL risk factors—namely, birth order, gestational age, and sex—were associated with the neonatal concentrations of inflammatory markers,” Søegaard said. “These findings raise the interesting possibility that the effects of some known ALL risk factors partly act through prenatal programming of immune function.”
The investigators found that increasing birth order was associated with significantly higher IL-18 and lower CRP concentrations.
Increasing gestational age was associated with significantly lower sIL-6Rα and TGF-β1 concentrations and higher CRP concentrations. And males had significantly lower sIL-6Rα and IL-8 concentrations and higher CRP concentrations than females.
However, none of the following factors were significantly associated with concentrations of inflammatory biomarkers: maternal age at delivery, maternal hospital contact due to infection during pregnancy, maternal prescription for antimicrobials during pregnancy, birth weight, and mode of delivery.
“Our findings underline the role the child’s baseline immune characteristics may play in the development of ALL,” Søegaard said. “However, we cannot yet use our research results to predict who will develop childhood ALL. In future studies, we will further characterize the relation between immune constitution at birth and risk of childhood ALL with the ultimate goal of developing preventive strategies targeting predisposed children.”
Søegaard noted that this study had its limitations, including the small number of inflammatory markers studied. In addition, the limited sample size made it impossible to detect potential differences between BCP-ALL subtypes.
The study was sponsored by the Dagmar Marshall Foundation, the A.P. Møller Foundation, the Danish Childhood Cancer Foundation, the Arvid Nilsson Foundation, and the Danish Cancer Research Foundation. There were no conflicts of interest disclosed.
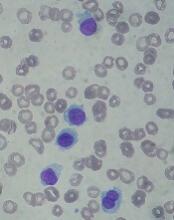
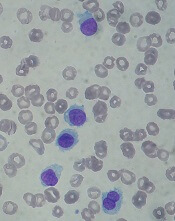
FDA approves drug for hairy cell leukemia
The U.S. Food and Drug Administration (FDA) has approved moxetumomab pasudotox-tdfk (Lumoxiti), a CD22-directed cytotoxin, to treat hairy cell leukemia (HCL).
Moxetumomab pasudotox is approved to treat adults with relapsed or refractory HCL who have received at least two prior systemic therapies, including treatment with a purine nucleoside analog.
The prescribing information for moxetumomab pasudotox includes a Boxed Warning noting that the drug poses risks of capillary leak syndrome (CLS) and hemolytic uremic syndrome (HUS). Treatment with moxetumomab pasudotox should be delayed or discontinued in patients who develop CLS and discontinued in patients with HUS.
The FDA granted the application for moxetumomab pasudotox fast track and priority review designations, and the drug received orphan drug designation from the FDA.
The agency granted the approval of moxetumomab pasudotox to AstraZeneca Pharmaceuticals based on results from a phase 3 trial (NCT01829711).
Data from this study were presented at the 2018 ASCO Annual Meeting (abstract 7004).
The trial included 80 patients with relapsed or refractory HCL who had received at least two prior lines of therapy.
At a median of 16.7 months of follow-up, the objective response rate was 75% (60/80), the complete response (CR) rate was 41% (33/80), and the durable CR rate was 30% (24/80). Durable CR was defined as CR with hematologic remission for more than 180 days.
Most patients with a CR achieved minimal residual disease negativity (82%; 27/33).
The median duration of response was not reached, nor was the median progression-free survival.
The most frequent treatment-related adverse events (AEs) were nausea (28%), peripheral edema (26%), headache (21%), and pyrexia (20%). Other treatment-related AEs included infections (8%) and neutropenia (3%).
Treatment-related AEs that led to discontinuation included HUS (5%), CLS (3%), and increased blood creatinine (3%).
In all, seven patients (9%) had CLS, and seven (9%) had HUS. This includes four (5%) patients who had both. CLS and HUS proved manageable and reversible.
There were three deaths in this trial, but none of them were considered treatment-related.
The U.S. Food and Drug Administration (FDA) has approved moxetumomab pasudotox-tdfk (Lumoxiti), a CD22-directed cytotoxin, to treat hairy cell leukemia (HCL).
Moxetumomab pasudotox is approved to treat adults with relapsed or refractory HCL who have received at least two prior systemic therapies, including treatment with a purine nucleoside analog.
The prescribing information for moxetumomab pasudotox includes a Boxed Warning noting that the drug poses risks of capillary leak syndrome (CLS) and hemolytic uremic syndrome (HUS). Treatment with moxetumomab pasudotox should be delayed or discontinued in patients who develop CLS and discontinued in patients with HUS.
The FDA granted the application for moxetumomab pasudotox fast track and priority review designations, and the drug received orphan drug designation from the FDA.
The agency granted the approval of moxetumomab pasudotox to AstraZeneca Pharmaceuticals based on results from a phase 3 trial (NCT01829711).
Data from this study were presented at the 2018 ASCO Annual Meeting (abstract 7004).
The trial included 80 patients with relapsed or refractory HCL who had received at least two prior lines of therapy.
At a median of 16.7 months of follow-up, the objective response rate was 75% (60/80), the complete response (CR) rate was 41% (33/80), and the durable CR rate was 30% (24/80). Durable CR was defined as CR with hematologic remission for more than 180 days.
Most patients with a CR achieved minimal residual disease negativity (82%; 27/33).
The median duration of response was not reached, nor was the median progression-free survival.
The most frequent treatment-related adverse events (AEs) were nausea (28%), peripheral edema (26%), headache (21%), and pyrexia (20%). Other treatment-related AEs included infections (8%) and neutropenia (3%).
Treatment-related AEs that led to discontinuation included HUS (5%), CLS (3%), and increased blood creatinine (3%).
In all, seven patients (9%) had CLS, and seven (9%) had HUS. This includes four (5%) patients who had both. CLS and HUS proved manageable and reversible.
There were three deaths in this trial, but none of them were considered treatment-related.
The U.S. Food and Drug Administration (FDA) has approved moxetumomab pasudotox-tdfk (Lumoxiti), a CD22-directed cytotoxin, to treat hairy cell leukemia (HCL).
Moxetumomab pasudotox is approved to treat adults with relapsed or refractory HCL who have received at least two prior systemic therapies, including treatment with a purine nucleoside analog.
The prescribing information for moxetumomab pasudotox includes a Boxed Warning noting that the drug poses risks of capillary leak syndrome (CLS) and hemolytic uremic syndrome (HUS). Treatment with moxetumomab pasudotox should be delayed or discontinued in patients who develop CLS and discontinued in patients with HUS.
The FDA granted the application for moxetumomab pasudotox fast track and priority review designations, and the drug received orphan drug designation from the FDA.
The agency granted the approval of moxetumomab pasudotox to AstraZeneca Pharmaceuticals based on results from a phase 3 trial (NCT01829711).
Data from this study were presented at the 2018 ASCO Annual Meeting (abstract 7004).
The trial included 80 patients with relapsed or refractory HCL who had received at least two prior lines of therapy.
At a median of 16.7 months of follow-up, the objective response rate was 75% (60/80), the complete response (CR) rate was 41% (33/80), and the durable CR rate was 30% (24/80). Durable CR was defined as CR with hematologic remission for more than 180 days.
Most patients with a CR achieved minimal residual disease negativity (82%; 27/33).
The median duration of response was not reached, nor was the median progression-free survival.
The most frequent treatment-related adverse events (AEs) were nausea (28%), peripheral edema (26%), headache (21%), and pyrexia (20%). Other treatment-related AEs included infections (8%) and neutropenia (3%).
Treatment-related AEs that led to discontinuation included HUS (5%), CLS (3%), and increased blood creatinine (3%).
In all, seven patients (9%) had CLS, and seven (9%) had HUS. This includes four (5%) patients who had both. CLS and HUS proved manageable and reversible.
There were three deaths in this trial, but none of them were considered treatment-related.
EC approves product for von Willebrand disease
The European Commission (EC) has granted marketing authorization for vonicog alfa (Veyvondi), a recombinant von Willebrand factor (rVWF) product.
The EC approved vonicog alfa for the treatment of bleeding events and treatment/prevention of surgical bleeding in adults (age 18 and older) with von Willebrand disease (VWD) when desmopressin treatment alone is ineffective or not indicated.
The approval means Shire is authorized to market vonicog alfa in the European Union as well as in Iceland, Lichtenstein, and Norway.
The EC’s approval of vonicog alfa was based on outcomes from three clinical trials. This includes a phase 1 study and a pair of phase 3 trials—one in a surgical setting and one in a non-surgical setting.
Data from these studies are available in the Summary of Product Characteristics for vonicog alfa.
Phase 1 trial
This trial (NCT00816660, 070701) enrolled patients with type 3 or severe type 1 VWD.
The goal was to assess the safety and pharmacokinetics of vonicog alfa (rVWF) combined at a fixed ratio with recombinant factor VIII (rFVIII)—referred to as “rVWF-rFVIII.” The researchers compared rVWF-rFVIII to plasma-derived (pd) VWF combined with pdFVIII (pdVWF-pdFVIII).
The safety analysis included 32 patients who received rVWF-rFVIII. There were no thrombotic events, serious adverse events, or new cases of inhibitors to VWF or FVIII in these patients.
The pharmacokinetic analysis included 19 patients. The researchers said the pharmacokinetics of rVWF ristocetin cofactor activity, VWF antigen, and collagen-binding activity were similar with rVWF-rFVIII and pdVWF-pdFVIII.
FVIII levels were higher after infusion with rVWF-rFVIII than with pdVWF-pdFVIII, even after 72 hours. The researchers said this suggests that rVWF alone “could maintain sufficient FVIII activity to treat a bleeding episode once the initial FVIII level has reached a therapeutic threshold.”
These results were published in Blood in 2013.
Phase 3: Non-surgical
This study (NCT01410227, 071001) included 49 patients with VWD who received vonicog alfa with or without rFVIII.
All participants had successful treatment of bleeding episodes. Most (96.9%) treated bleeds (192 bleeds in 22 patients) were given an “excellent” efficacy rating (as good as or better than expected).
Most bleeds (81.8%) were resolved with a single infusion of vonicog alfa, and the treatment had a mean half-life of 21.9 hours.
There were 8 adverse events considered related to vonicog alfa, and 2 were serious. One patient experienced 2 simultaneous serious events—chest discomfort and increased heart rate—but these were resolved.
There were no thrombotic events in this trial, no treatment-related binding or neutralizing antibodies against VWF, and no neutralizing antibodies against FVIII.
These results were published in Blood in 2015.
Phase 3: Surgical setting
This trial (NCT02283268, 071101) enrolled 15 adults with severe VWD who were undergoing elective surgical procedures (10 of them major procedures).
Patients received vonicog alfa at 40 to 60 IU per kg of body weight 12 to 24 hours before surgery. Within 3 hours of surgery, each patient’s FVIII level (FVIII:C) was assessed, with a target of 30 IU/dL for minor surgeries and 60 IU/dL for major surgeries.
Within an hour of surgery, patients received a dose of vonicog alfa, with or without rFVIII, depending on the target FVIII:C levels at the 3-hour assessment.
Ten patients received rVWF alone, 12 did not receive any preoperative FVIII, and 2 did not receive rVWF postoperatively.
Vonicog alfa demonstrated overall hemostatic efficacy, as assessed 24 hours after the last perioperative infusion or the completion of the study visit, whichever occurred earlier.
Intra- and post-operative hemostasis was rated as “excellent” (as good as or better than expected) in 60% of patients and “good” (probably as good as expected) in 40% of patients.
One patient developed deep vein thrombosis 3 days after undergoing hip replacement surgery.
One patient tested positive for binding antibodies to VWF. None of the patients developed binding antibodies against potential impurities such as rFurin, CHO-protein, or mouse IgG.
These results were presented at the WFH 2018 World Congress.
The European Commission (EC) has granted marketing authorization for vonicog alfa (Veyvondi), a recombinant von Willebrand factor (rVWF) product.
The EC approved vonicog alfa for the treatment of bleeding events and treatment/prevention of surgical bleeding in adults (age 18 and older) with von Willebrand disease (VWD) when desmopressin treatment alone is ineffective or not indicated.
The approval means Shire is authorized to market vonicog alfa in the European Union as well as in Iceland, Lichtenstein, and Norway.
The EC’s approval of vonicog alfa was based on outcomes from three clinical trials. This includes a phase 1 study and a pair of phase 3 trials—one in a surgical setting and one in a non-surgical setting.
Data from these studies are available in the Summary of Product Characteristics for vonicog alfa.
Phase 1 trial
This trial (NCT00816660, 070701) enrolled patients with type 3 or severe type 1 VWD.
The goal was to assess the safety and pharmacokinetics of vonicog alfa (rVWF) combined at a fixed ratio with recombinant factor VIII (rFVIII)—referred to as “rVWF-rFVIII.” The researchers compared rVWF-rFVIII to plasma-derived (pd) VWF combined with pdFVIII (pdVWF-pdFVIII).
The safety analysis included 32 patients who received rVWF-rFVIII. There were no thrombotic events, serious adverse events, or new cases of inhibitors to VWF or FVIII in these patients.
The pharmacokinetic analysis included 19 patients. The researchers said the pharmacokinetics of rVWF ristocetin cofactor activity, VWF antigen, and collagen-binding activity were similar with rVWF-rFVIII and pdVWF-pdFVIII.
FVIII levels were higher after infusion with rVWF-rFVIII than with pdVWF-pdFVIII, even after 72 hours. The researchers said this suggests that rVWF alone “could maintain sufficient FVIII activity to treat a bleeding episode once the initial FVIII level has reached a therapeutic threshold.”
These results were published in Blood in 2013.
Phase 3: Non-surgical
This study (NCT01410227, 071001) included 49 patients with VWD who received vonicog alfa with or without rFVIII.
All participants had successful treatment of bleeding episodes. Most (96.9%) treated bleeds (192 bleeds in 22 patients) were given an “excellent” efficacy rating (as good as or better than expected).
Most bleeds (81.8%) were resolved with a single infusion of vonicog alfa, and the treatment had a mean half-life of 21.9 hours.
There were 8 adverse events considered related to vonicog alfa, and 2 were serious. One patient experienced 2 simultaneous serious events—chest discomfort and increased heart rate—but these were resolved.
There were no thrombotic events in this trial, no treatment-related binding or neutralizing antibodies against VWF, and no neutralizing antibodies against FVIII.
These results were published in Blood in 2015.
Phase 3: Surgical setting
This trial (NCT02283268, 071101) enrolled 15 adults with severe VWD who were undergoing elective surgical procedures (10 of them major procedures).
Patients received vonicog alfa at 40 to 60 IU per kg of body weight 12 to 24 hours before surgery. Within 3 hours of surgery, each patient’s FVIII level (FVIII:C) was assessed, with a target of 30 IU/dL for minor surgeries and 60 IU/dL for major surgeries.
Within an hour of surgery, patients received a dose of vonicog alfa, with or without rFVIII, depending on the target FVIII:C levels at the 3-hour assessment.
Ten patients received rVWF alone, 12 did not receive any preoperative FVIII, and 2 did not receive rVWF postoperatively.
Vonicog alfa demonstrated overall hemostatic efficacy, as assessed 24 hours after the last perioperative infusion or the completion of the study visit, whichever occurred earlier.
Intra- and post-operative hemostasis was rated as “excellent” (as good as or better than expected) in 60% of patients and “good” (probably as good as expected) in 40% of patients.
One patient developed deep vein thrombosis 3 days after undergoing hip replacement surgery.
One patient tested positive for binding antibodies to VWF. None of the patients developed binding antibodies against potential impurities such as rFurin, CHO-protein, or mouse IgG.
These results were presented at the WFH 2018 World Congress.
The European Commission (EC) has granted marketing authorization for vonicog alfa (Veyvondi), a recombinant von Willebrand factor (rVWF) product.
The EC approved vonicog alfa for the treatment of bleeding events and treatment/prevention of surgical bleeding in adults (age 18 and older) with von Willebrand disease (VWD) when desmopressin treatment alone is ineffective or not indicated.
The approval means Shire is authorized to market vonicog alfa in the European Union as well as in Iceland, Lichtenstein, and Norway.
The EC’s approval of vonicog alfa was based on outcomes from three clinical trials. This includes a phase 1 study and a pair of phase 3 trials—one in a surgical setting and one in a non-surgical setting.
Data from these studies are available in the Summary of Product Characteristics for vonicog alfa.
Phase 1 trial
This trial (NCT00816660, 070701) enrolled patients with type 3 or severe type 1 VWD.
The goal was to assess the safety and pharmacokinetics of vonicog alfa (rVWF) combined at a fixed ratio with recombinant factor VIII (rFVIII)—referred to as “rVWF-rFVIII.” The researchers compared rVWF-rFVIII to plasma-derived (pd) VWF combined with pdFVIII (pdVWF-pdFVIII).
The safety analysis included 32 patients who received rVWF-rFVIII. There were no thrombotic events, serious adverse events, or new cases of inhibitors to VWF or FVIII in these patients.
The pharmacokinetic analysis included 19 patients. The researchers said the pharmacokinetics of rVWF ristocetin cofactor activity, VWF antigen, and collagen-binding activity were similar with rVWF-rFVIII and pdVWF-pdFVIII.
FVIII levels were higher after infusion with rVWF-rFVIII than with pdVWF-pdFVIII, even after 72 hours. The researchers said this suggests that rVWF alone “could maintain sufficient FVIII activity to treat a bleeding episode once the initial FVIII level has reached a therapeutic threshold.”
These results were published in Blood in 2013.
Phase 3: Non-surgical
This study (NCT01410227, 071001) included 49 patients with VWD who received vonicog alfa with or without rFVIII.
All participants had successful treatment of bleeding episodes. Most (96.9%) treated bleeds (192 bleeds in 22 patients) were given an “excellent” efficacy rating (as good as or better than expected).
Most bleeds (81.8%) were resolved with a single infusion of vonicog alfa, and the treatment had a mean half-life of 21.9 hours.
There were 8 adverse events considered related to vonicog alfa, and 2 were serious. One patient experienced 2 simultaneous serious events—chest discomfort and increased heart rate—but these were resolved.
There were no thrombotic events in this trial, no treatment-related binding or neutralizing antibodies against VWF, and no neutralizing antibodies against FVIII.
These results were published in Blood in 2015.
Phase 3: Surgical setting
This trial (NCT02283268, 071101) enrolled 15 adults with severe VWD who were undergoing elective surgical procedures (10 of them major procedures).
Patients received vonicog alfa at 40 to 60 IU per kg of body weight 12 to 24 hours before surgery. Within 3 hours of surgery, each patient’s FVIII level (FVIII:C) was assessed, with a target of 30 IU/dL for minor surgeries and 60 IU/dL for major surgeries.
Within an hour of surgery, patients received a dose of vonicog alfa, with or without rFVIII, depending on the target FVIII:C levels at the 3-hour assessment.
Ten patients received rVWF alone, 12 did not receive any preoperative FVIII, and 2 did not receive rVWF postoperatively.
Vonicog alfa demonstrated overall hemostatic efficacy, as assessed 24 hours after the last perioperative infusion or the completion of the study visit, whichever occurred earlier.
Intra- and post-operative hemostasis was rated as “excellent” (as good as or better than expected) in 60% of patients and “good” (probably as good as expected) in 40% of patients.
One patient developed deep vein thrombosis 3 days after undergoing hip replacement surgery.
One patient tested positive for binding antibodies to VWF. None of the patients developed binding antibodies against potential impurities such as rFurin, CHO-protein, or mouse IgG.
These results were presented at the WFH 2018 World Congress.
Insights could change treatment, classification of MPAL
An extensive analysis of mixed phenotype acute leukemia (MPAL) has led to new insights that may have implications for disease classification and treatment.
Researchers believe they have identified new subtypes of MPAL that should be included in the World Health Organization (WHO) classification for acute leukemia.
Each of these subtypes shares genomic characteristics with other acute leukemias, which suggests the new subtypes might respond to treatments that are already in use.
This research has also shed light on how MPAL evolves and appears to provide an explanation for why MPAL displays characteristics of both acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL).
“ALL and AML have very different treatments, but MPAL has features of both, so the question of how best to treat patients with MPAL has been challenging the leukemia community worldwide, and long-term survival of patients has been poor,” said Charles Mullighan, MBBS, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
With these issues in mind, Dr. Mullighan and his colleagues conducted their study of MPAL and described their findings in Nature.
New classifications
The researchers used whole-genome, whole-exome, and RNA sequencing to analyze 115 samples from pediatric patients with MPAL.
The analysis revealed mutations that define the two most common subtypes of MPAL—B/myeloid and T/myeloid—and suggested these subtypes share similarities with other leukemia subtypes.
The researchers found that 48% of B/myeloid MPAL cases carried rearrangements in ZNF384, a characteristic that is also found in cases of B-cell ALL. In fact, the team said the gene expression profiles of ZNF384r B-ALL and ZNF384r MPAL were indistinguishable.
“That is biologically and clinically important,” Dr. Mullighan said. “The findings suggest the ZNF384 rearrangement defines a distinct leukemia subtype, and the alteration should be used to guide treatment.”
The researchers noted that patients with ZNF384r exhibited higher FLT3 expression than patients with other types of B/myeloid or T/myeloid MPAL, so patients with ZNF384r MPAL might respond well to treatment with a FLT3 inhibitor.
This study also showed that cases of B/myeloid MPAL without ZNF384r shared genomic features with other B-ALL subtypes, such as Ph-like B-ALL, which may have implications for treatment.
Another of the researchers’ discoveries was that T/myeloid MPAL and early T-cell precursor ALL have similar gene expression profiles.
The team identified several genes that were mutated at similar frequencies in T/myeloid MPAL and early T-cell precursor ALL, including WT1, ETV6, EZH2, and FLT3. WT1 was the most frequently mutated transcription factor gene in T/myeloid MPAL.
Based on these findings, the researchers said the WHO classification of acute leukemia should be updated to include:
- ZNF384r acute leukemia (either B-ALL or MPAL)
- WT1-mutant T/myeloid MPAL
- Ph-like B/myeloid MPAL.
Evolution of MPAL
The researchers’ analyses also revealed leukemia-initiating genetic alterations in early hematopoietic progenitors.
The team said this and other findings—including the common genomic features of ZNF384r MPAL and B-ALL—suggest the ambiguous phenotype of MPAL results from alterations in immature hematopoietic progenitors.
“These findings suggest that the founding mutation occurs early in blood cell development, in some cases in hematopoietic stem cells, and results in an acute leukemia with features of both myeloid and lymphoid cells,” said study author Thomas Alexander, MD, of the University of North Carolina at Chapel Hill.
“One previous theory was that the reason you have two different cancer types within the same patient is that they acquire different mutations that drive them to become AML or ALL, with genomically distinct tumors within the same patient. That doesn’t seem to be the case from our data. Our proposed model is that the mutations occur earlier in development in cells that retain the potential to acquire myeloid or lymphoid features.”
This research was supported by the National Cancer Institute, the National Institutes of Health, Cookies for Kids’ Cancer, and other organizations.
An extensive analysis of mixed phenotype acute leukemia (MPAL) has led to new insights that may have implications for disease classification and treatment.
Researchers believe they have identified new subtypes of MPAL that should be included in the World Health Organization (WHO) classification for acute leukemia.
Each of these subtypes shares genomic characteristics with other acute leukemias, which suggests the new subtypes might respond to treatments that are already in use.
This research has also shed light on how MPAL evolves and appears to provide an explanation for why MPAL displays characteristics of both acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL).
“ALL and AML have very different treatments, but MPAL has features of both, so the question of how best to treat patients with MPAL has been challenging the leukemia community worldwide, and long-term survival of patients has been poor,” said Charles Mullighan, MBBS, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
With these issues in mind, Dr. Mullighan and his colleagues conducted their study of MPAL and described their findings in Nature.
New classifications
The researchers used whole-genome, whole-exome, and RNA sequencing to analyze 115 samples from pediatric patients with MPAL.
The analysis revealed mutations that define the two most common subtypes of MPAL—B/myeloid and T/myeloid—and suggested these subtypes share similarities with other leukemia subtypes.
The researchers found that 48% of B/myeloid MPAL cases carried rearrangements in ZNF384, a characteristic that is also found in cases of B-cell ALL. In fact, the team said the gene expression profiles of ZNF384r B-ALL and ZNF384r MPAL were indistinguishable.
“That is biologically and clinically important,” Dr. Mullighan said. “The findings suggest the ZNF384 rearrangement defines a distinct leukemia subtype, and the alteration should be used to guide treatment.”
The researchers noted that patients with ZNF384r exhibited higher FLT3 expression than patients with other types of B/myeloid or T/myeloid MPAL, so patients with ZNF384r MPAL might respond well to treatment with a FLT3 inhibitor.
This study also showed that cases of B/myeloid MPAL without ZNF384r shared genomic features with other B-ALL subtypes, such as Ph-like B-ALL, which may have implications for treatment.
Another of the researchers’ discoveries was that T/myeloid MPAL and early T-cell precursor ALL have similar gene expression profiles.
The team identified several genes that were mutated at similar frequencies in T/myeloid MPAL and early T-cell precursor ALL, including WT1, ETV6, EZH2, and FLT3. WT1 was the most frequently mutated transcription factor gene in T/myeloid MPAL.
Based on these findings, the researchers said the WHO classification of acute leukemia should be updated to include:
- ZNF384r acute leukemia (either B-ALL or MPAL)
- WT1-mutant T/myeloid MPAL
- Ph-like B/myeloid MPAL.
Evolution of MPAL
The researchers’ analyses also revealed leukemia-initiating genetic alterations in early hematopoietic progenitors.
The team said this and other findings—including the common genomic features of ZNF384r MPAL and B-ALL—suggest the ambiguous phenotype of MPAL results from alterations in immature hematopoietic progenitors.
“These findings suggest that the founding mutation occurs early in blood cell development, in some cases in hematopoietic stem cells, and results in an acute leukemia with features of both myeloid and lymphoid cells,” said study author Thomas Alexander, MD, of the University of North Carolina at Chapel Hill.
“One previous theory was that the reason you have two different cancer types within the same patient is that they acquire different mutations that drive them to become AML or ALL, with genomically distinct tumors within the same patient. That doesn’t seem to be the case from our data. Our proposed model is that the mutations occur earlier in development in cells that retain the potential to acquire myeloid or lymphoid features.”
This research was supported by the National Cancer Institute, the National Institutes of Health, Cookies for Kids’ Cancer, and other organizations.
An extensive analysis of mixed phenotype acute leukemia (MPAL) has led to new insights that may have implications for disease classification and treatment.
Researchers believe they have identified new subtypes of MPAL that should be included in the World Health Organization (WHO) classification for acute leukemia.
Each of these subtypes shares genomic characteristics with other acute leukemias, which suggests the new subtypes might respond to treatments that are already in use.
This research has also shed light on how MPAL evolves and appears to provide an explanation for why MPAL displays characteristics of both acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL).
“ALL and AML have very different treatments, but MPAL has features of both, so the question of how best to treat patients with MPAL has been challenging the leukemia community worldwide, and long-term survival of patients has been poor,” said Charles Mullighan, MBBS, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
With these issues in mind, Dr. Mullighan and his colleagues conducted their study of MPAL and described their findings in Nature.
New classifications
The researchers used whole-genome, whole-exome, and RNA sequencing to analyze 115 samples from pediatric patients with MPAL.
The analysis revealed mutations that define the two most common subtypes of MPAL—B/myeloid and T/myeloid—and suggested these subtypes share similarities with other leukemia subtypes.
The researchers found that 48% of B/myeloid MPAL cases carried rearrangements in ZNF384, a characteristic that is also found in cases of B-cell ALL. In fact, the team said the gene expression profiles of ZNF384r B-ALL and ZNF384r MPAL were indistinguishable.
“That is biologically and clinically important,” Dr. Mullighan said. “The findings suggest the ZNF384 rearrangement defines a distinct leukemia subtype, and the alteration should be used to guide treatment.”
The researchers noted that patients with ZNF384r exhibited higher FLT3 expression than patients with other types of B/myeloid or T/myeloid MPAL, so patients with ZNF384r MPAL might respond well to treatment with a FLT3 inhibitor.
This study also showed that cases of B/myeloid MPAL without ZNF384r shared genomic features with other B-ALL subtypes, such as Ph-like B-ALL, which may have implications for treatment.
Another of the researchers’ discoveries was that T/myeloid MPAL and early T-cell precursor ALL have similar gene expression profiles.
The team identified several genes that were mutated at similar frequencies in T/myeloid MPAL and early T-cell precursor ALL, including WT1, ETV6, EZH2, and FLT3. WT1 was the most frequently mutated transcription factor gene in T/myeloid MPAL.
Based on these findings, the researchers said the WHO classification of acute leukemia should be updated to include:
- ZNF384r acute leukemia (either B-ALL or MPAL)
- WT1-mutant T/myeloid MPAL
- Ph-like B/myeloid MPAL.
Evolution of MPAL
The researchers’ analyses also revealed leukemia-initiating genetic alterations in early hematopoietic progenitors.
The team said this and other findings—including the common genomic features of ZNF384r MPAL and B-ALL—suggest the ambiguous phenotype of MPAL results from alterations in immature hematopoietic progenitors.
“These findings suggest that the founding mutation occurs early in blood cell development, in some cases in hematopoietic stem cells, and results in an acute leukemia with features of both myeloid and lymphoid cells,” said study author Thomas Alexander, MD, of the University of North Carolina at Chapel Hill.
“One previous theory was that the reason you have two different cancer types within the same patient is that they acquire different mutations that drive them to become AML or ALL, with genomically distinct tumors within the same patient. That doesn’t seem to be the case from our data. Our proposed model is that the mutations occur earlier in development in cells that retain the potential to acquire myeloid or lymphoid features.”
This research was supported by the National Cancer Institute, the National Institutes of Health, Cookies for Kids’ Cancer, and other organizations.
MRD data added to venetoclax label
The U.S. Food and Drug Administration (FDA) has expanded the label for venetoclax tablets (Venclexta®) to include data on minimal residual disease (MRD).
The drug’s prescribing information now includes details on MRD negativity in previously treated patients with chronic lymphocytic leukemia (CLL) who received venetoclax in combination with rituximab in the phase 3 MURANO trial.
The combination of venetoclax and rituximab was FDA approved in June for the treatment of patients with CLL or small lymphocytic lymphoma, with or without 17p deletion, who received at least one prior therapy.
The MURANO trial (NCT02005471), which supported the FDA approval, included 389 patients with relapsed or refractory CLL.
The patients were randomized to receive:
- Venetoclax at 400 mg daily for 24 months (after a 5-week ramp-up period) plus rituximab at 375 mg/m2 on day 1 for the first cycle and at 500 mg/m2 on day 1 for cycles 2 to 6 (n=194)
- Bendamustine at 70 mg/m2 on days 1 and 2 for 6 cycles plus rituximab at the same schedule as the venetoclax arm (n=195).
Researchers evaluated MRD in patients who achieved a partial response or better. MRD was assessed using allele-specific oligonucleotide polymerase chain reaction, and the definition of MRD negativity was less than one CLL cell per 10,000 lymphocytes.
The researchers assessed MRD in the peripheral blood 3 months after the last dose of rituximab. At that time, 53% (103/194) of patients in the venetoclax-rituximab arm were MRD negative, as were 12% (23/195) of patients in the bendamustine-rituximab arm.
The researchers also assessed MRD in the peripheral blood of patients with a complete response (CR) or CR with incomplete marrow recovery (CRi). MRD negativity was achieved by 3% (6/194) of these patients in the venetoclax-rituximab arm and 2% (3/195) in the bendamustine-rituximab arm.
Three percent (3/106) of patients in the venetoclax arm who achieved CR/CRi were MRD negative in both the peripheral blood and the bone marrow.
“The rates of MRD negativity seen with Venclexta plus rituximab are very encouraging,” said MURANO investigator John Seymour, MBBS, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Additional results from the MURANO trial were published in The New England Journal of Medicine in March and are included in the prescribing information for venetoclax.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the U.S. and by AbbVie outside the U.S.
The U.S. Food and Drug Administration (FDA) has expanded the label for venetoclax tablets (Venclexta®) to include data on minimal residual disease (MRD).
The drug’s prescribing information now includes details on MRD negativity in previously treated patients with chronic lymphocytic leukemia (CLL) who received venetoclax in combination with rituximab in the phase 3 MURANO trial.
The combination of venetoclax and rituximab was FDA approved in June for the treatment of patients with CLL or small lymphocytic lymphoma, with or without 17p deletion, who received at least one prior therapy.
The MURANO trial (NCT02005471), which supported the FDA approval, included 389 patients with relapsed or refractory CLL.
The patients were randomized to receive:
- Venetoclax at 400 mg daily for 24 months (after a 5-week ramp-up period) plus rituximab at 375 mg/m2 on day 1 for the first cycle and at 500 mg/m2 on day 1 for cycles 2 to 6 (n=194)
- Bendamustine at 70 mg/m2 on days 1 and 2 for 6 cycles plus rituximab at the same schedule as the venetoclax arm (n=195).
Researchers evaluated MRD in patients who achieved a partial response or better. MRD was assessed using allele-specific oligonucleotide polymerase chain reaction, and the definition of MRD negativity was less than one CLL cell per 10,000 lymphocytes.
The researchers assessed MRD in the peripheral blood 3 months after the last dose of rituximab. At that time, 53% (103/194) of patients in the venetoclax-rituximab arm were MRD negative, as were 12% (23/195) of patients in the bendamustine-rituximab arm.
The researchers also assessed MRD in the peripheral blood of patients with a complete response (CR) or CR with incomplete marrow recovery (CRi). MRD negativity was achieved by 3% (6/194) of these patients in the venetoclax-rituximab arm and 2% (3/195) in the bendamustine-rituximab arm.
Three percent (3/106) of patients in the venetoclax arm who achieved CR/CRi were MRD negative in both the peripheral blood and the bone marrow.
“The rates of MRD negativity seen with Venclexta plus rituximab are very encouraging,” said MURANO investigator John Seymour, MBBS, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Additional results from the MURANO trial were published in The New England Journal of Medicine in March and are included in the prescribing information for venetoclax.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the U.S. and by AbbVie outside the U.S.
The U.S. Food and Drug Administration (FDA) has expanded the label for venetoclax tablets (Venclexta®) to include data on minimal residual disease (MRD).
The drug’s prescribing information now includes details on MRD negativity in previously treated patients with chronic lymphocytic leukemia (CLL) who received venetoclax in combination with rituximab in the phase 3 MURANO trial.
The combination of venetoclax and rituximab was FDA approved in June for the treatment of patients with CLL or small lymphocytic lymphoma, with or without 17p deletion, who received at least one prior therapy.
The MURANO trial (NCT02005471), which supported the FDA approval, included 389 patients with relapsed or refractory CLL.
The patients were randomized to receive:
- Venetoclax at 400 mg daily for 24 months (after a 5-week ramp-up period) plus rituximab at 375 mg/m2 on day 1 for the first cycle and at 500 mg/m2 on day 1 for cycles 2 to 6 (n=194)
- Bendamustine at 70 mg/m2 on days 1 and 2 for 6 cycles plus rituximab at the same schedule as the venetoclax arm (n=195).
Researchers evaluated MRD in patients who achieved a partial response or better. MRD was assessed using allele-specific oligonucleotide polymerase chain reaction, and the definition of MRD negativity was less than one CLL cell per 10,000 lymphocytes.
The researchers assessed MRD in the peripheral blood 3 months after the last dose of rituximab. At that time, 53% (103/194) of patients in the venetoclax-rituximab arm were MRD negative, as were 12% (23/195) of patients in the bendamustine-rituximab arm.
The researchers also assessed MRD in the peripheral blood of patients with a complete response (CR) or CR with incomplete marrow recovery (CRi). MRD negativity was achieved by 3% (6/194) of these patients in the venetoclax-rituximab arm and 2% (3/195) in the bendamustine-rituximab arm.
Three percent (3/106) of patients in the venetoclax arm who achieved CR/CRi were MRD negative in both the peripheral blood and the bone marrow.
“The rates of MRD negativity seen with Venclexta plus rituximab are very encouraging,” said MURANO investigator John Seymour, MBBS, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Additional results from the MURANO trial were published in The New England Journal of Medicine in March and are included in the prescribing information for venetoclax.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the U.S. and by AbbVie outside the U.S.
Cell population appears to drive relapse in AML
Researchers believe they have identified cells that are responsible for relapse of acute myeloid leukemia (AML).
These “leukemic-regenerating cells” (LRCs), which are distinct from leukemic stem cells (LSCs), seem to arise in response to chemotherapy.
Experiments in mouse models of AML suggested that targeting LRCs could reduce the risk of relapse, and analyses of AML patient samples suggested LRCs might be used to predict relapse.
Allison Boyd, PhD, of McMaster University in Hamilton, Ontario, Canada, and her colleagues reported these findings in Cancer Cell.
The researchers evaluated the leukemic populations that persist after chemotherapy by analyzing AML patient samples and xenograft AML models. The team found that LSCs were depleted by chemotherapy, and a different cell population, LRCs, appeared to arise in response to treatment.
LRCs are “molecularly distinct from therapy-naïve LSCs,” the researchers said. In fact, the team identified 19 genes that are preferentially expressed by LRCs and could be druggable.
One of these genes is DRD2, and the researchers found they could target LRCs using a small-molecule antagonist of DRD2.
Targeting LRCs
Dr. Boyd and her colleagues compared the effects of treatment with a DRD2 antagonist in AML xenografts populated with therapy-naive LSCs and AML xenografts that harbored LRCs following exposure to cytarabine.
The researchers said DRD2 antagonist therapy “moderately” affected AML progenitors in the LSC model but “had profound effects on regenerating LRCs.”
Treatment with the DRD2 antagonist also improved the efficacy of chemotherapy.
In xenografts derived from one AML patient, treatment with cytarabine alone left 50% of mice with residual disease. However, the addition of the DRD2 antagonist enabled 100% of the mice to achieve disease-free status.
In xenografts derived from a patient with more aggressive AML, all recipient mice had residual disease after receiving cytarabine. Treatment with the DRD2 antagonist slowed leukemic re-growth and nearly doubled the time to relapse.
Targeting LRCs also reduced disease regeneration potential in samples from other AML patients.
“This is a major clinical opportunity because this type of leukemia is very diverse and responds differently across patients,” Dr. Boyd said. “It has been a challenge in a clinical setting to find a commonality for therapeutic targeting across the wide array of patients, and these regenerative cells provide that similarity.”
Predicting relapse
Dr. Boyd and her colleagues also analyzed bone marrow samples collected from AML patients approximately 3 weeks after they completed standard induction chemotherapy.
The team found that progenitor activity was enriched among residual leukemic cells. However, patient cells lacked gene expression signatures related to therapy-naive LSCs.
“Instead, these highly regenerative AML cells preferentially expressed our LRC signature,” the researchers said.
The team also found evidence to suggest that LRC molecular profiles arise temporarily after chemotherapy. The LRC signature was not observed at diagnosis or once AML was re-established at relapse.
“We think there are opportunities here because now we have a window where we can kick the cancer while it’s down,” Dr. Boyd said.
She and her colleagues also found the LRC signature might be useful for predicting relapse in AML patients.
The team assessed expression of SLC2A2, an LRC marker that has overlapping expression with DRD2, in 7 patients who were in clinical remission after induction.
The researchers found that chemotherapy increased expression of SLC2A2 only in the four patients who had residual disease—not in the three patients who remained in disease-free remission for at least 5 years.
“These results suggest that LRC populations represent reservoirs of residual disease, and LRC marker expression levels can be linked to clinical outcomes of AML relapse,” the researchers said.
This study was supported by the Canadian Cancer Society, the Canadian Institutes of Health Research, the Ontario Institute for Cancer Research, and other organizations.
Researchers believe they have identified cells that are responsible for relapse of acute myeloid leukemia (AML).
These “leukemic-regenerating cells” (LRCs), which are distinct from leukemic stem cells (LSCs), seem to arise in response to chemotherapy.
Experiments in mouse models of AML suggested that targeting LRCs could reduce the risk of relapse, and analyses of AML patient samples suggested LRCs might be used to predict relapse.
Allison Boyd, PhD, of McMaster University in Hamilton, Ontario, Canada, and her colleagues reported these findings in Cancer Cell.
The researchers evaluated the leukemic populations that persist after chemotherapy by analyzing AML patient samples and xenograft AML models. The team found that LSCs were depleted by chemotherapy, and a different cell population, LRCs, appeared to arise in response to treatment.
LRCs are “molecularly distinct from therapy-naïve LSCs,” the researchers said. In fact, the team identified 19 genes that are preferentially expressed by LRCs and could be druggable.
One of these genes is DRD2, and the researchers found they could target LRCs using a small-molecule antagonist of DRD2.
Targeting LRCs
Dr. Boyd and her colleagues compared the effects of treatment with a DRD2 antagonist in AML xenografts populated with therapy-naive LSCs and AML xenografts that harbored LRCs following exposure to cytarabine.
The researchers said DRD2 antagonist therapy “moderately” affected AML progenitors in the LSC model but “had profound effects on regenerating LRCs.”
Treatment with the DRD2 antagonist also improved the efficacy of chemotherapy.
In xenografts derived from one AML patient, treatment with cytarabine alone left 50% of mice with residual disease. However, the addition of the DRD2 antagonist enabled 100% of the mice to achieve disease-free status.
In xenografts derived from a patient with more aggressive AML, all recipient mice had residual disease after receiving cytarabine. Treatment with the DRD2 antagonist slowed leukemic re-growth and nearly doubled the time to relapse.
Targeting LRCs also reduced disease regeneration potential in samples from other AML patients.
“This is a major clinical opportunity because this type of leukemia is very diverse and responds differently across patients,” Dr. Boyd said. “It has been a challenge in a clinical setting to find a commonality for therapeutic targeting across the wide array of patients, and these regenerative cells provide that similarity.”
Predicting relapse
Dr. Boyd and her colleagues also analyzed bone marrow samples collected from AML patients approximately 3 weeks after they completed standard induction chemotherapy.
The team found that progenitor activity was enriched among residual leukemic cells. However, patient cells lacked gene expression signatures related to therapy-naive LSCs.
“Instead, these highly regenerative AML cells preferentially expressed our LRC signature,” the researchers said.
The team also found evidence to suggest that LRC molecular profiles arise temporarily after chemotherapy. The LRC signature was not observed at diagnosis or once AML was re-established at relapse.
“We think there are opportunities here because now we have a window where we can kick the cancer while it’s down,” Dr. Boyd said.
She and her colleagues also found the LRC signature might be useful for predicting relapse in AML patients.
The team assessed expression of SLC2A2, an LRC marker that has overlapping expression with DRD2, in 7 patients who were in clinical remission after induction.
The researchers found that chemotherapy increased expression of SLC2A2 only in the four patients who had residual disease—not in the three patients who remained in disease-free remission for at least 5 years.
“These results suggest that LRC populations represent reservoirs of residual disease, and LRC marker expression levels can be linked to clinical outcomes of AML relapse,” the researchers said.
This study was supported by the Canadian Cancer Society, the Canadian Institutes of Health Research, the Ontario Institute for Cancer Research, and other organizations.
Researchers believe they have identified cells that are responsible for relapse of acute myeloid leukemia (AML).
These “leukemic-regenerating cells” (LRCs), which are distinct from leukemic stem cells (LSCs), seem to arise in response to chemotherapy.
Experiments in mouse models of AML suggested that targeting LRCs could reduce the risk of relapse, and analyses of AML patient samples suggested LRCs might be used to predict relapse.
Allison Boyd, PhD, of McMaster University in Hamilton, Ontario, Canada, and her colleagues reported these findings in Cancer Cell.
The researchers evaluated the leukemic populations that persist after chemotherapy by analyzing AML patient samples and xenograft AML models. The team found that LSCs were depleted by chemotherapy, and a different cell population, LRCs, appeared to arise in response to treatment.
LRCs are “molecularly distinct from therapy-naïve LSCs,” the researchers said. In fact, the team identified 19 genes that are preferentially expressed by LRCs and could be druggable.
One of these genes is DRD2, and the researchers found they could target LRCs using a small-molecule antagonist of DRD2.
Targeting LRCs
Dr. Boyd and her colleagues compared the effects of treatment with a DRD2 antagonist in AML xenografts populated with therapy-naive LSCs and AML xenografts that harbored LRCs following exposure to cytarabine.
The researchers said DRD2 antagonist therapy “moderately” affected AML progenitors in the LSC model but “had profound effects on regenerating LRCs.”
Treatment with the DRD2 antagonist also improved the efficacy of chemotherapy.
In xenografts derived from one AML patient, treatment with cytarabine alone left 50% of mice with residual disease. However, the addition of the DRD2 antagonist enabled 100% of the mice to achieve disease-free status.
In xenografts derived from a patient with more aggressive AML, all recipient mice had residual disease after receiving cytarabine. Treatment with the DRD2 antagonist slowed leukemic re-growth and nearly doubled the time to relapse.
Targeting LRCs also reduced disease regeneration potential in samples from other AML patients.
“This is a major clinical opportunity because this type of leukemia is very diverse and responds differently across patients,” Dr. Boyd said. “It has been a challenge in a clinical setting to find a commonality for therapeutic targeting across the wide array of patients, and these regenerative cells provide that similarity.”
Predicting relapse
Dr. Boyd and her colleagues also analyzed bone marrow samples collected from AML patients approximately 3 weeks after they completed standard induction chemotherapy.
The team found that progenitor activity was enriched among residual leukemic cells. However, patient cells lacked gene expression signatures related to therapy-naive LSCs.
“Instead, these highly regenerative AML cells preferentially expressed our LRC signature,” the researchers said.
The team also found evidence to suggest that LRC molecular profiles arise temporarily after chemotherapy. The LRC signature was not observed at diagnosis or once AML was re-established at relapse.
“We think there are opportunities here because now we have a window where we can kick the cancer while it’s down,” Dr. Boyd said.
She and her colleagues also found the LRC signature might be useful for predicting relapse in AML patients.
The team assessed expression of SLC2A2, an LRC marker that has overlapping expression with DRD2, in 7 patients who were in clinical remission after induction.
The researchers found that chemotherapy increased expression of SLC2A2 only in the four patients who had residual disease—not in the three patients who remained in disease-free remission for at least 5 years.
“These results suggest that LRC populations represent reservoirs of residual disease, and LRC marker expression levels can be linked to clinical outcomes of AML relapse,” the researchers said.
This study was supported by the Canadian Cancer Society, the Canadian Institutes of Health Research, the Ontario Institute for Cancer Research, and other organizations.
HIF1A could be therapeutic target for MDS
The transcription factor HIF1A could be a therapeutic target for “a broad spectrum” of patients with myelodysplastic syndromes (MDS), according to researchers.
Preclinical experiments indicated that HIF1A fuels the biological processes that cause different types of MDS.
Researchers also found that inhibiting HIF1A reversed MDS symptoms and prolonged survival in mouse models of MDS.
Gang Huang, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio, and his colleagues reported these findings in Cancer Discovery.
The researchers identified HIF1A’s role in MDS by first analyzing cells from healthy donors and MDS patients, including patients with refractory anemia, refractory anemia with ring sideroblasts, and refractory anemia with excess blasts type 1 and 2.
The researchers observed increased gene expression of HIF1A-induced genes in the cells from MDS patients. The team also found a high frequency of HIF1A-expressing cells in the MDS cohort, regardless of the patients’ IPSS-R risk.
The researchers conducted experiments in mouse models to study the onset of MDS and its genetic and molecular drivers. The results suggested that dysregulation of HIF1A has a central role in the onset of MDS, including different manifestations and symptoms found in patients.
“We know the genomes of MDS patients have recurrent mutations in different transcriptional, epigenetic, and metabolic regulators, but the incidence of these mutations does not directly correspond to the disease when it occurs,” Dr. Huang noted.
“Our study shows that malfunctions in the signaling of HIF1A could be generating the diverse medical problems doctors see in MDS patients.”
Specifically, the researchers found that MDS-associated mutations—DNMT3A, TET2, ASXL1, RUNX1, and MLL1—induced HIF1A signaling. And activation of HIF1A signaling in hematopoietic cells induced MDS phenotypes in mice.
The team said this suggests dysregulation of HIF1A signaling could generate diverse MDS phenotypes by “functioning as a signaling funnel” for MDS driver mutations.
The researchers also showed that inhibition of HIF1A could reverse MDS phenotypes. They said HIF1A deletion rescued dysplasia formation, partially rescued thrombocytopenia, and abrogated MDS development in mouse models.
Treatment with echinomycin, an inhibitor of HIF1A-mediated target gene activation, prolonged survival in mouse models of MDS and decreased MDSL cell numbers in the bone marrow and spleen.
This research was supported by the Kyoto University Foundation, the MDS Foundation, the Cincinnati Children’s Hospital Research Foundation, the Leukemia Research Foundation, and others.
The transcription factor HIF1A could be a therapeutic target for “a broad spectrum” of patients with myelodysplastic syndromes (MDS), according to researchers.
Preclinical experiments indicated that HIF1A fuels the biological processes that cause different types of MDS.
Researchers also found that inhibiting HIF1A reversed MDS symptoms and prolonged survival in mouse models of MDS.
Gang Huang, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio, and his colleagues reported these findings in Cancer Discovery.
The researchers identified HIF1A’s role in MDS by first analyzing cells from healthy donors and MDS patients, including patients with refractory anemia, refractory anemia with ring sideroblasts, and refractory anemia with excess blasts type 1 and 2.
The researchers observed increased gene expression of HIF1A-induced genes in the cells from MDS patients. The team also found a high frequency of HIF1A-expressing cells in the MDS cohort, regardless of the patients’ IPSS-R risk.
The researchers conducted experiments in mouse models to study the onset of MDS and its genetic and molecular drivers. The results suggested that dysregulation of HIF1A has a central role in the onset of MDS, including different manifestations and symptoms found in patients.
“We know the genomes of MDS patients have recurrent mutations in different transcriptional, epigenetic, and metabolic regulators, but the incidence of these mutations does not directly correspond to the disease when it occurs,” Dr. Huang noted.
“Our study shows that malfunctions in the signaling of HIF1A could be generating the diverse medical problems doctors see in MDS patients.”
Specifically, the researchers found that MDS-associated mutations—DNMT3A, TET2, ASXL1, RUNX1, and MLL1—induced HIF1A signaling. And activation of HIF1A signaling in hematopoietic cells induced MDS phenotypes in mice.
The team said this suggests dysregulation of HIF1A signaling could generate diverse MDS phenotypes by “functioning as a signaling funnel” for MDS driver mutations.
The researchers also showed that inhibition of HIF1A could reverse MDS phenotypes. They said HIF1A deletion rescued dysplasia formation, partially rescued thrombocytopenia, and abrogated MDS development in mouse models.
Treatment with echinomycin, an inhibitor of HIF1A-mediated target gene activation, prolonged survival in mouse models of MDS and decreased MDSL cell numbers in the bone marrow and spleen.
This research was supported by the Kyoto University Foundation, the MDS Foundation, the Cincinnati Children’s Hospital Research Foundation, the Leukemia Research Foundation, and others.
The transcription factor HIF1A could be a therapeutic target for “a broad spectrum” of patients with myelodysplastic syndromes (MDS), according to researchers.
Preclinical experiments indicated that HIF1A fuels the biological processes that cause different types of MDS.
Researchers also found that inhibiting HIF1A reversed MDS symptoms and prolonged survival in mouse models of MDS.
Gang Huang, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio, and his colleagues reported these findings in Cancer Discovery.
The researchers identified HIF1A’s role in MDS by first analyzing cells from healthy donors and MDS patients, including patients with refractory anemia, refractory anemia with ring sideroblasts, and refractory anemia with excess blasts type 1 and 2.
The researchers observed increased gene expression of HIF1A-induced genes in the cells from MDS patients. The team also found a high frequency of HIF1A-expressing cells in the MDS cohort, regardless of the patients’ IPSS-R risk.
The researchers conducted experiments in mouse models to study the onset of MDS and its genetic and molecular drivers. The results suggested that dysregulation of HIF1A has a central role in the onset of MDS, including different manifestations and symptoms found in patients.
“We know the genomes of MDS patients have recurrent mutations in different transcriptional, epigenetic, and metabolic regulators, but the incidence of these mutations does not directly correspond to the disease when it occurs,” Dr. Huang noted.
“Our study shows that malfunctions in the signaling of HIF1A could be generating the diverse medical problems doctors see in MDS patients.”
Specifically, the researchers found that MDS-associated mutations—DNMT3A, TET2, ASXL1, RUNX1, and MLL1—induced HIF1A signaling. And activation of HIF1A signaling in hematopoietic cells induced MDS phenotypes in mice.
The team said this suggests dysregulation of HIF1A signaling could generate diverse MDS phenotypes by “functioning as a signaling funnel” for MDS driver mutations.
The researchers also showed that inhibition of HIF1A could reverse MDS phenotypes. They said HIF1A deletion rescued dysplasia formation, partially rescued thrombocytopenia, and abrogated MDS development in mouse models.
Treatment with echinomycin, an inhibitor of HIF1A-mediated target gene activation, prolonged survival in mouse models of MDS and decreased MDSL cell numbers in the bone marrow and spleen.
This research was supported by the Kyoto University Foundation, the MDS Foundation, the Cincinnati Children’s Hospital Research Foundation, the Leukemia Research Foundation, and others.