User login
9/11 firefighters may have higher risk of MGUS, early MM
Exposure to the 9/11 World Trade Center (WTC) disaster site may increase the risk of monoclonal gammopathy of undetermined significance (MGUS) and early development of multiple myeloma (MM).
Researchers found that firefighters exposed to the site had a nearly 2-fold higher risk of MGUS than a control population.
And those firefighters who developed MM were diagnosed 12 years earlier than MM patients in the general US population.
These findings were published in JAMA Oncology.
Previous studies suggested that MGUS and MM tend to develop after exposure to toxic chemicals, and individuals exposed to the WTC disaster site have an increased risk of developing cancers.
The aerosolized dust from the collapsed WTC towers exposed firefighters and other first responders to high levels of polychlorinated biphenyls, polycyclic aromatic hydrocarbons, dioxins, asbestos, and other potential carcinogens, as well as diesel smoke from heavy machinery used in the 10-month rescue and recovery effort.
“With our 2011 study in The Lancet, we were the first to show that first responders were more likely to get many different types of cancer,” said David J. Prezant, MD, of Albert Einstein College of Medicine in Bronx, New York.
“We carried out this new study to do more than just treat cancer. We wanted to find early, predictive signs of cancer that would allow us to screen people and monitor those found to be at risk. By detecting MGUS, which predicts the development of multiple myeloma, we are able to do that.”
For statistical reasons, the study population was limited to 781 white, male WTC-exposed firefighters ages 50 to 79.
The researchers assess the prevalence of MGUS in these firefighters and compared it to the prevalence of MGUS in a non-exposed comparison group—men living in Olmsted County, Minnesota.
The prevalence of MGUS was 1.8-fold higher in the firefighters. There were 7.63 cases of MGUS per 100 firefighters and 4.34 cases per 100 non-exposed men.
The researchers also found the prevalence of light-chain MGUS was 3.1-fold higher in the firefighters than in the controls. The prevalence rate of light-chain MGUS was 3.08 and 0.98 per 100 persons, respectively.
“We saw a significantly higher incidence of MGUS in these first responders, and they’re developing it at a young age,” said study author Amit Verma, MBBS, of Albert Einstein College of Medicine.
The subjects’ early development of MGUS suggests they may face an increased risk for early onset MM as well.
In a separate analysis, the researchers examined 16 cases of MM among white, male WTC-exposed firefighters diagnosed between September 12, 2001, and July 1, 2017.
Their average age at diagnosis was 57, or 12 years younger than the average age for MM diagnosis in the US.
The researchers also found that 7 of 14 evaluable cases were light-chain MM. They said this is more than double the rate observed in other populations—50% vs 20%.
In the population of firefighters screened for MGUS, 38% (18/47) of those who had MGUS were found to have the light-chain subtype.
The researchers said these findings are of interest because previous research revealed associations between light-chain MM/MGUS and exposure to toxins and chronic immune stimulation.
The team also assessed CD20 expression in a subset of 7 MM patients. Five of these patients (71%) had CD20-positive cells, which is associated with poor prognosis.
Based on these findings, the researchers recommend that physicians screen first responders exposed to the WTC disaster site for MGUS.
“Screening for multiple myeloma risk by testing for MGUS is something we can offer these first responders, which is why this study is important,” Dr Prezant said.
Exposure to the 9/11 World Trade Center (WTC) disaster site may increase the risk of monoclonal gammopathy of undetermined significance (MGUS) and early development of multiple myeloma (MM).
Researchers found that firefighters exposed to the site had a nearly 2-fold higher risk of MGUS than a control population.
And those firefighters who developed MM were diagnosed 12 years earlier than MM patients in the general US population.
These findings were published in JAMA Oncology.
Previous studies suggested that MGUS and MM tend to develop after exposure to toxic chemicals, and individuals exposed to the WTC disaster site have an increased risk of developing cancers.
The aerosolized dust from the collapsed WTC towers exposed firefighters and other first responders to high levels of polychlorinated biphenyls, polycyclic aromatic hydrocarbons, dioxins, asbestos, and other potential carcinogens, as well as diesel smoke from heavy machinery used in the 10-month rescue and recovery effort.
“With our 2011 study in The Lancet, we were the first to show that first responders were more likely to get many different types of cancer,” said David J. Prezant, MD, of Albert Einstein College of Medicine in Bronx, New York.
“We carried out this new study to do more than just treat cancer. We wanted to find early, predictive signs of cancer that would allow us to screen people and monitor those found to be at risk. By detecting MGUS, which predicts the development of multiple myeloma, we are able to do that.”
For statistical reasons, the study population was limited to 781 white, male WTC-exposed firefighters ages 50 to 79.
The researchers assess the prevalence of MGUS in these firefighters and compared it to the prevalence of MGUS in a non-exposed comparison group—men living in Olmsted County, Minnesota.
The prevalence of MGUS was 1.8-fold higher in the firefighters. There were 7.63 cases of MGUS per 100 firefighters and 4.34 cases per 100 non-exposed men.
The researchers also found the prevalence of light-chain MGUS was 3.1-fold higher in the firefighters than in the controls. The prevalence rate of light-chain MGUS was 3.08 and 0.98 per 100 persons, respectively.
“We saw a significantly higher incidence of MGUS in these first responders, and they’re developing it at a young age,” said study author Amit Verma, MBBS, of Albert Einstein College of Medicine.
The subjects’ early development of MGUS suggests they may face an increased risk for early onset MM as well.
In a separate analysis, the researchers examined 16 cases of MM among white, male WTC-exposed firefighters diagnosed between September 12, 2001, and July 1, 2017.
Their average age at diagnosis was 57, or 12 years younger than the average age for MM diagnosis in the US.
The researchers also found that 7 of 14 evaluable cases were light-chain MM. They said this is more than double the rate observed in other populations—50% vs 20%.
In the population of firefighters screened for MGUS, 38% (18/47) of those who had MGUS were found to have the light-chain subtype.
The researchers said these findings are of interest because previous research revealed associations between light-chain MM/MGUS and exposure to toxins and chronic immune stimulation.
The team also assessed CD20 expression in a subset of 7 MM patients. Five of these patients (71%) had CD20-positive cells, which is associated with poor prognosis.
Based on these findings, the researchers recommend that physicians screen first responders exposed to the WTC disaster site for MGUS.
“Screening for multiple myeloma risk by testing for MGUS is something we can offer these first responders, which is why this study is important,” Dr Prezant said.
Exposure to the 9/11 World Trade Center (WTC) disaster site may increase the risk of monoclonal gammopathy of undetermined significance (MGUS) and early development of multiple myeloma (MM).
Researchers found that firefighters exposed to the site had a nearly 2-fold higher risk of MGUS than a control population.
And those firefighters who developed MM were diagnosed 12 years earlier than MM patients in the general US population.
These findings were published in JAMA Oncology.
Previous studies suggested that MGUS and MM tend to develop after exposure to toxic chemicals, and individuals exposed to the WTC disaster site have an increased risk of developing cancers.
The aerosolized dust from the collapsed WTC towers exposed firefighters and other first responders to high levels of polychlorinated biphenyls, polycyclic aromatic hydrocarbons, dioxins, asbestos, and other potential carcinogens, as well as diesel smoke from heavy machinery used in the 10-month rescue and recovery effort.
“With our 2011 study in The Lancet, we were the first to show that first responders were more likely to get many different types of cancer,” said David J. Prezant, MD, of Albert Einstein College of Medicine in Bronx, New York.
“We carried out this new study to do more than just treat cancer. We wanted to find early, predictive signs of cancer that would allow us to screen people and monitor those found to be at risk. By detecting MGUS, which predicts the development of multiple myeloma, we are able to do that.”
For statistical reasons, the study population was limited to 781 white, male WTC-exposed firefighters ages 50 to 79.
The researchers assess the prevalence of MGUS in these firefighters and compared it to the prevalence of MGUS in a non-exposed comparison group—men living in Olmsted County, Minnesota.
The prevalence of MGUS was 1.8-fold higher in the firefighters. There were 7.63 cases of MGUS per 100 firefighters and 4.34 cases per 100 non-exposed men.
The researchers also found the prevalence of light-chain MGUS was 3.1-fold higher in the firefighters than in the controls. The prevalence rate of light-chain MGUS was 3.08 and 0.98 per 100 persons, respectively.
“We saw a significantly higher incidence of MGUS in these first responders, and they’re developing it at a young age,” said study author Amit Verma, MBBS, of Albert Einstein College of Medicine.
The subjects’ early development of MGUS suggests they may face an increased risk for early onset MM as well.
In a separate analysis, the researchers examined 16 cases of MM among white, male WTC-exposed firefighters diagnosed between September 12, 2001, and July 1, 2017.
Their average age at diagnosis was 57, or 12 years younger than the average age for MM diagnosis in the US.
The researchers also found that 7 of 14 evaluable cases were light-chain MM. They said this is more than double the rate observed in other populations—50% vs 20%.
In the population of firefighters screened for MGUS, 38% (18/47) of those who had MGUS were found to have the light-chain subtype.
The researchers said these findings are of interest because previous research revealed associations between light-chain MM/MGUS and exposure to toxins and chronic immune stimulation.
The team also assessed CD20 expression in a subset of 7 MM patients. Five of these patients (71%) had CD20-positive cells, which is associated with poor prognosis.
Based on these findings, the researchers recommend that physicians screen first responders exposed to the WTC disaster site for MGUS.
“Screening for multiple myeloma risk by testing for MGUS is something we can offer these first responders, which is why this study is important,” Dr Prezant said.
Radioimmunoconjugate shows activity in NHL
CHICAGO—The radioimmunoconjugate 177Lu-NNV003 has demonstrated activity against non-Hodgkin lymphomas (NHLs).
Experiments showed that 177Lu-NNV003 can inhibit proliferation in mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), and chronic lymphocytic leukemia (CLL) cell lines.
177Lu-NNV003 also exhibited an antitumor effect and prolonged survival in mouse models of MCL, DLBCL, and CLL.
These results were presented at the AACR Annual Meeting 2018 (abstract 848).
This research was conducted by employees of Nordic Nanovector and other researchers. Nordic Nanovector is the company developing 177Lu-NNV003.
177Lu-NNV003 consists of a chimeric antibody targeting CD37 (NNV003) conjugated with p-SCN-Bn-DOTA, which chelates the β-emitting radionuclide lutetium-177.
The researchers found that 177Lu-NNV003 inhibited proliferation in all 3 NHL cell lines tested—MEC-2 (CLL), DOHH2 (DLBCL), and REC-1 (MCL). DOHH2 was the most radiosensitive cell line.
The unlabeled NNV003 antibody, on the other hand, did not exhibit an antiproliferative effect in these cell lines. However, NNV003 did induce antibody-dependent cellular cytotoxicity in MEC-2 and DOHH2 cells and antibody-dependent cellular phagocytosis in MEC-2 cells.
The researchers found that 177Lu-NNV003 targeted CD37-positive cells and demonstrated antitumor effects in mouse models of MCL, CLL, and DLBCL.
REC-1 model
177Lu-NNV003 prolonged survival in CB17 SCID mice injected with REC-1 cells and cured 50% to 60% of the mice.
Median survival times were 55 days in mice that received sodium chloride (NaCl), 85 days in mice that received NNV003 (0.167 mg/kg), and 61 days in mice that received 177Lu-IgG1 (100 MBq/kg).
On the other hand, mice treated with 177Lu-NNV003 had a median survival of 152 days (100 MBq/kg), or the median survival was not reached (50 MBq/kg).
The difference in survival was significant for 177Lu-NNV003 recipients compared to recipients of NaCl (P<0.001) or 177Lu-IgG1 (P<0.002).
MEC-2 model
177Lu-NNV003 also prolonged survival in NRG mice injected with MEC-2 cells.
The median survival was 21 days in mice that received NaCl, NNV003 (2 x 0.33 mg/kg), or 177Lu-IgG1 (200 MBq/kg).
However, mice treated with 177Lu-NNV003 had a median survival of 32 days (200 MBq/kg) or 29 days (2 x 200 MBq/kg).
The difference in survival was significant for 177Lu-NNV003 recipients compared to recipients of 177Lu-IgG1 (P<0.025) or 2 x NNV003 (P<0.02).
DOHH2 model
RAG-2 mice injected with DOHH2 cells had survival times surpassing 200 days after treatment with NNV003 or 177Lu-NNV003.
The median survival was not reached in mice that received NNV003 (at 2 or 30 mg/kg) or 177Lu-NNV003 (at 200, 300, or 400 MBq/kg). But the median survival was 46 days in mice that received NaCl and 47 days in mice that received 177Lu-IgG1 (300 MBq/kg).
The difference in survival was significant for recipients of NNV003 or 177Lu-NNV003 compared to recipients of 177Lu-IgG1 or NaCl (P<0.001 for all).
Toxicity and biodistribution
The researchers noted that the 177Lu-labeled antibodies caused transient hematologic toxicity in the mice.
In the MEC-2 and DOHH2 models, there was no redistribution of 177Lu-NNV003 in organs after initial uptake. (The researchers did not report on biodistribution in the REC-1 model.)
177Lu-NNV003 had low uptake in the liver, spleen, kidneys, and femur. The researchers said this suggests 177Lu-NNV003 is stable in vivo, as free lutetium-177 tends to accumulate in bones.
CHICAGO—The radioimmunoconjugate 177Lu-NNV003 has demonstrated activity against non-Hodgkin lymphomas (NHLs).
Experiments showed that 177Lu-NNV003 can inhibit proliferation in mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), and chronic lymphocytic leukemia (CLL) cell lines.
177Lu-NNV003 also exhibited an antitumor effect and prolonged survival in mouse models of MCL, DLBCL, and CLL.
These results were presented at the AACR Annual Meeting 2018 (abstract 848).
This research was conducted by employees of Nordic Nanovector and other researchers. Nordic Nanovector is the company developing 177Lu-NNV003.
177Lu-NNV003 consists of a chimeric antibody targeting CD37 (NNV003) conjugated with p-SCN-Bn-DOTA, which chelates the β-emitting radionuclide lutetium-177.
The researchers found that 177Lu-NNV003 inhibited proliferation in all 3 NHL cell lines tested—MEC-2 (CLL), DOHH2 (DLBCL), and REC-1 (MCL). DOHH2 was the most radiosensitive cell line.
The unlabeled NNV003 antibody, on the other hand, did not exhibit an antiproliferative effect in these cell lines. However, NNV003 did induce antibody-dependent cellular cytotoxicity in MEC-2 and DOHH2 cells and antibody-dependent cellular phagocytosis in MEC-2 cells.
The researchers found that 177Lu-NNV003 targeted CD37-positive cells and demonstrated antitumor effects in mouse models of MCL, CLL, and DLBCL.
REC-1 model
177Lu-NNV003 prolonged survival in CB17 SCID mice injected with REC-1 cells and cured 50% to 60% of the mice.
Median survival times were 55 days in mice that received sodium chloride (NaCl), 85 days in mice that received NNV003 (0.167 mg/kg), and 61 days in mice that received 177Lu-IgG1 (100 MBq/kg).
On the other hand, mice treated with 177Lu-NNV003 had a median survival of 152 days (100 MBq/kg), or the median survival was not reached (50 MBq/kg).
The difference in survival was significant for 177Lu-NNV003 recipients compared to recipients of NaCl (P<0.001) or 177Lu-IgG1 (P<0.002).
MEC-2 model
177Lu-NNV003 also prolonged survival in NRG mice injected with MEC-2 cells.
The median survival was 21 days in mice that received NaCl, NNV003 (2 x 0.33 mg/kg), or 177Lu-IgG1 (200 MBq/kg).
However, mice treated with 177Lu-NNV003 had a median survival of 32 days (200 MBq/kg) or 29 days (2 x 200 MBq/kg).
The difference in survival was significant for 177Lu-NNV003 recipients compared to recipients of 177Lu-IgG1 (P<0.025) or 2 x NNV003 (P<0.02).
DOHH2 model
RAG-2 mice injected with DOHH2 cells had survival times surpassing 200 days after treatment with NNV003 or 177Lu-NNV003.
The median survival was not reached in mice that received NNV003 (at 2 or 30 mg/kg) or 177Lu-NNV003 (at 200, 300, or 400 MBq/kg). But the median survival was 46 days in mice that received NaCl and 47 days in mice that received 177Lu-IgG1 (300 MBq/kg).
The difference in survival was significant for recipients of NNV003 or 177Lu-NNV003 compared to recipients of 177Lu-IgG1 or NaCl (P<0.001 for all).
Toxicity and biodistribution
The researchers noted that the 177Lu-labeled antibodies caused transient hematologic toxicity in the mice.
In the MEC-2 and DOHH2 models, there was no redistribution of 177Lu-NNV003 in organs after initial uptake. (The researchers did not report on biodistribution in the REC-1 model.)
177Lu-NNV003 had low uptake in the liver, spleen, kidneys, and femur. The researchers said this suggests 177Lu-NNV003 is stable in vivo, as free lutetium-177 tends to accumulate in bones.
CHICAGO—The radioimmunoconjugate 177Lu-NNV003 has demonstrated activity against non-Hodgkin lymphomas (NHLs).
Experiments showed that 177Lu-NNV003 can inhibit proliferation in mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), and chronic lymphocytic leukemia (CLL) cell lines.
177Lu-NNV003 also exhibited an antitumor effect and prolonged survival in mouse models of MCL, DLBCL, and CLL.
These results were presented at the AACR Annual Meeting 2018 (abstract 848).
This research was conducted by employees of Nordic Nanovector and other researchers. Nordic Nanovector is the company developing 177Lu-NNV003.
177Lu-NNV003 consists of a chimeric antibody targeting CD37 (NNV003) conjugated with p-SCN-Bn-DOTA, which chelates the β-emitting radionuclide lutetium-177.
The researchers found that 177Lu-NNV003 inhibited proliferation in all 3 NHL cell lines tested—MEC-2 (CLL), DOHH2 (DLBCL), and REC-1 (MCL). DOHH2 was the most radiosensitive cell line.
The unlabeled NNV003 antibody, on the other hand, did not exhibit an antiproliferative effect in these cell lines. However, NNV003 did induce antibody-dependent cellular cytotoxicity in MEC-2 and DOHH2 cells and antibody-dependent cellular phagocytosis in MEC-2 cells.
The researchers found that 177Lu-NNV003 targeted CD37-positive cells and demonstrated antitumor effects in mouse models of MCL, CLL, and DLBCL.
REC-1 model
177Lu-NNV003 prolonged survival in CB17 SCID mice injected with REC-1 cells and cured 50% to 60% of the mice.
Median survival times were 55 days in mice that received sodium chloride (NaCl), 85 days in mice that received NNV003 (0.167 mg/kg), and 61 days in mice that received 177Lu-IgG1 (100 MBq/kg).
On the other hand, mice treated with 177Lu-NNV003 had a median survival of 152 days (100 MBq/kg), or the median survival was not reached (50 MBq/kg).
The difference in survival was significant for 177Lu-NNV003 recipients compared to recipients of NaCl (P<0.001) or 177Lu-IgG1 (P<0.002).
MEC-2 model
177Lu-NNV003 also prolonged survival in NRG mice injected with MEC-2 cells.
The median survival was 21 days in mice that received NaCl, NNV003 (2 x 0.33 mg/kg), or 177Lu-IgG1 (200 MBq/kg).
However, mice treated with 177Lu-NNV003 had a median survival of 32 days (200 MBq/kg) or 29 days (2 x 200 MBq/kg).
The difference in survival was significant for 177Lu-NNV003 recipients compared to recipients of 177Lu-IgG1 (P<0.025) or 2 x NNV003 (P<0.02).
DOHH2 model
RAG-2 mice injected with DOHH2 cells had survival times surpassing 200 days after treatment with NNV003 or 177Lu-NNV003.
The median survival was not reached in mice that received NNV003 (at 2 or 30 mg/kg) or 177Lu-NNV003 (at 200, 300, or 400 MBq/kg). But the median survival was 46 days in mice that received NaCl and 47 days in mice that received 177Lu-IgG1 (300 MBq/kg).
The difference in survival was significant for recipients of NNV003 or 177Lu-NNV003 compared to recipients of 177Lu-IgG1 or NaCl (P<0.001 for all).
Toxicity and biodistribution
The researchers noted that the 177Lu-labeled antibodies caused transient hematologic toxicity in the mice.
In the MEC-2 and DOHH2 models, there was no redistribution of 177Lu-NNV003 in organs after initial uptake. (The researchers did not report on biodistribution in the REC-1 model.)
177Lu-NNV003 had low uptake in the liver, spleen, kidneys, and femur. The researchers said this suggests 177Lu-NNV003 is stable in vivo, as free lutetium-177 tends to accumulate in bones.
Many believe in unproven causes of cancer, survey shows
A new survey suggests many people believe certain environmental and lifestyle factors cause cancer even though there is insufficient evidence to support these beliefs.
In a survey of 1330 people in England, more than 40% of respondents said that stress and food additives can cause cancer.
More than a third of participants reported that cancer may result from exposure to electromagnetic frequencies and eating genetically modified foods.
“It’s worrying to see so many people endorse risk factors for which there is no convincing evidence,” said Samuel Smith, PhD, of the University of Leeds in the UK.
“Compared to past research, it appears the number of people believing in unproven causes of cancer has increased since the start of the century, which could be a result of changes to how we access news and information through the Internet and social media.”
Dr Smith and his colleagues reported results from the survey in European Journal of Cancer.
The researchers surveyed 1330 people with a mean age of 43.7. Slightly more than half (51.6%) were female, most (84.7%) were white, and most (67%) had post-16 qualifications (education beyond age 16).
The survey included questions about 11 known cancer risk factors, such as being overweight, alcohol consumption, having a relative with cancer, and infection with human papillomavirus (HPV).
The survey also included questions about 12 factors that are commonly believed to cause cancer but for which there is no scientific evidence to confirm the belief. Some of these include eating food containing artificial sweeteners and using mobile phones, cleaning products, and aerosol containers.
Respondents were asked how much they agree that each of the factors increase the risk of cancer. Response options were: strongly disagree, disagree, unsure, agree, and strongly agree.
Results
Participants provided a correct response to more of the questions about proven cancer risk factors than unproven factors—53% and 36%, respectively (P<0.01).
Most respondents knew that active smoking (88%) and exposure to smoking (80%) can cause cancer. However, only 30% of them knew that HPV or low fruit and vegetable consumption are proven cancer risk factors.
The most common unproven factors believed to cause cancer were stress (43%), food additives (42%), electromagnetic frequencies (35%), and genetically modified foods (34%).
In addition, 19% of respondents said using microwave ovens can cause cancer, and 15% said drinking from plastic bottles can cause cancer.
The researchers did note that belief in unproven causes of cancer did not mean a person was more likely to have risky lifestyle habits.
However, respondents who had better knowledge of proven causes were more likely to engage in habits that might reduce their risk of cancer.
“People’s beliefs are so important because they have an impact on the lifestyle choices they make,” said Lion Shahab, PhD, of University College London in the UK.
“Those with better awareness of proven causes of cancer were more likely not to smoke and to eat more fruit and vegetables.”
Dr Smith added, “It’s vital to improve public education about the causes of cancer if we want to help people make informed decisions about their lives and ensure they aren’t worrying unnecessarily.”
A new survey suggests many people believe certain environmental and lifestyle factors cause cancer even though there is insufficient evidence to support these beliefs.
In a survey of 1330 people in England, more than 40% of respondents said that stress and food additives can cause cancer.
More than a third of participants reported that cancer may result from exposure to electromagnetic frequencies and eating genetically modified foods.
“It’s worrying to see so many people endorse risk factors for which there is no convincing evidence,” said Samuel Smith, PhD, of the University of Leeds in the UK.
“Compared to past research, it appears the number of people believing in unproven causes of cancer has increased since the start of the century, which could be a result of changes to how we access news and information through the Internet and social media.”
Dr Smith and his colleagues reported results from the survey in European Journal of Cancer.
The researchers surveyed 1330 people with a mean age of 43.7. Slightly more than half (51.6%) were female, most (84.7%) were white, and most (67%) had post-16 qualifications (education beyond age 16).
The survey included questions about 11 known cancer risk factors, such as being overweight, alcohol consumption, having a relative with cancer, and infection with human papillomavirus (HPV).
The survey also included questions about 12 factors that are commonly believed to cause cancer but for which there is no scientific evidence to confirm the belief. Some of these include eating food containing artificial sweeteners and using mobile phones, cleaning products, and aerosol containers.
Respondents were asked how much they agree that each of the factors increase the risk of cancer. Response options were: strongly disagree, disagree, unsure, agree, and strongly agree.
Results
Participants provided a correct response to more of the questions about proven cancer risk factors than unproven factors—53% and 36%, respectively (P<0.01).
Most respondents knew that active smoking (88%) and exposure to smoking (80%) can cause cancer. However, only 30% of them knew that HPV or low fruit and vegetable consumption are proven cancer risk factors.
The most common unproven factors believed to cause cancer were stress (43%), food additives (42%), electromagnetic frequencies (35%), and genetically modified foods (34%).
In addition, 19% of respondents said using microwave ovens can cause cancer, and 15% said drinking from plastic bottles can cause cancer.
The researchers did note that belief in unproven causes of cancer did not mean a person was more likely to have risky lifestyle habits.
However, respondents who had better knowledge of proven causes were more likely to engage in habits that might reduce their risk of cancer.
“People’s beliefs are so important because they have an impact on the lifestyle choices they make,” said Lion Shahab, PhD, of University College London in the UK.
“Those with better awareness of proven causes of cancer were more likely not to smoke and to eat more fruit and vegetables.”
Dr Smith added, “It’s vital to improve public education about the causes of cancer if we want to help people make informed decisions about their lives and ensure they aren’t worrying unnecessarily.”
A new survey suggests many people believe certain environmental and lifestyle factors cause cancer even though there is insufficient evidence to support these beliefs.
In a survey of 1330 people in England, more than 40% of respondents said that stress and food additives can cause cancer.
More than a third of participants reported that cancer may result from exposure to electromagnetic frequencies and eating genetically modified foods.
“It’s worrying to see so many people endorse risk factors for which there is no convincing evidence,” said Samuel Smith, PhD, of the University of Leeds in the UK.
“Compared to past research, it appears the number of people believing in unproven causes of cancer has increased since the start of the century, which could be a result of changes to how we access news and information through the Internet and social media.”
Dr Smith and his colleagues reported results from the survey in European Journal of Cancer.
The researchers surveyed 1330 people with a mean age of 43.7. Slightly more than half (51.6%) were female, most (84.7%) were white, and most (67%) had post-16 qualifications (education beyond age 16).
The survey included questions about 11 known cancer risk factors, such as being overweight, alcohol consumption, having a relative with cancer, and infection with human papillomavirus (HPV).
The survey also included questions about 12 factors that are commonly believed to cause cancer but for which there is no scientific evidence to confirm the belief. Some of these include eating food containing artificial sweeteners and using mobile phones, cleaning products, and aerosol containers.
Respondents were asked how much they agree that each of the factors increase the risk of cancer. Response options were: strongly disagree, disagree, unsure, agree, and strongly agree.
Results
Participants provided a correct response to more of the questions about proven cancer risk factors than unproven factors—53% and 36%, respectively (P<0.01).
Most respondents knew that active smoking (88%) and exposure to smoking (80%) can cause cancer. However, only 30% of them knew that HPV or low fruit and vegetable consumption are proven cancer risk factors.
The most common unproven factors believed to cause cancer were stress (43%), food additives (42%), electromagnetic frequencies (35%), and genetically modified foods (34%).
In addition, 19% of respondents said using microwave ovens can cause cancer, and 15% said drinking from plastic bottles can cause cancer.
The researchers did note that belief in unproven causes of cancer did not mean a person was more likely to have risky lifestyle habits.
However, respondents who had better knowledge of proven causes were more likely to engage in habits that might reduce their risk of cancer.
“People’s beliefs are so important because they have an impact on the lifestyle choices they make,” said Lion Shahab, PhD, of University College London in the UK.
“Those with better awareness of proven causes of cancer were more likely not to smoke and to eat more fruit and vegetables.”
Dr Smith added, “It’s vital to improve public education about the causes of cancer if we want to help people make informed decisions about their lives and ensure they aren’t worrying unnecessarily.”
Haplo-HSCT regimen can cure SCD, team says
A haploidentical transplant regimen has led to long-term engraftment in adults with sickle cell disease (SCD), according to researchers.
Seven of 8 patients treated with this regimen were still alive at last follow-up, and 6 of them maintained engraftment.
Two patients developed graft-versus-host disease (GVHD). One of them had acute and chronic GVHD and died about 400 days after transplant. The other had acute GVHD that resolved with treatment.
Damiano Rondelli, MD, of the University of Illinois at Chicago, and his colleagues reported these results in Biology of Blood and Marrow Transplantation.
The researchers initially screened 50 adult SCD patients as candidates for haploidentical hematopoietic stem cell transplant (haplo-HSCT) between January 2014 and March 2017. Most patients were ineligible or declined the procedure.
Ultimately, 10 patients received a haplo-HSCT. Unfortunately, the first 2 patients failed to engraft. These patients had received conditioning with alemtuzumab and 3 Gy total body irradiation (TBI) as well as post-transplant cyclophosphamide.
Because of this failure, the researchers used the following regimen for the remaining 8 patients. It’s a modified version of the regimen described in Blood in 2012.
“We modified the transplant protocol by increasing the dose of radiation used before the transplant and by infusing growth factor-mobilized peripheral blood stem cells instead of bone marrow cells,” Dr Rondelli said. “These two modifications helped ensure the patient’s body could accept the healthy donor cells.”
Modified regimen
Patients received growth-factor-mobilized peripheral blood stem cells after conditioning with rabbit antithymocyte globulin (0.5 mg/kg on day -9, 2 mg/kg on day -8 and -7), cyclophosphamide (14.5 mg/kg on day -6 and -5), fludarabine (30 mg/m2 on day -6 to -2), and single-dose TBI (3 Gy on day -1).
For GVHD prophylaxis, patients received intravenous cyclophosphamide (50 mg/kg on day 3 and 4), oral mycophenolate mofetil (15 mg/kg 3 times daily from day 5 to 35), and sirolimus (from day 5 dosed for a target trough of 5 to 15 ng/mL). In patients who had T-cell chimerism greater than 50% at 1 year after HSCT and did not have signs of GVHD, sirolimus was tapered off over 3 months.
Patients stopped taking hydroxyurea on day -9. They received red blood cell exchange transfusion on day -10 (with the goal of getting hemoglobin S below 30%) and received platelet transfusions to maintain platelet counts greater than 50 x 109 cells/L.
Patients also received penicillin V (250 mg twice daily) in addition to standard antimicrobial prophylaxis.
Results
All 8 patients on the modified regimen engrafted. The median time to neutrophil engraftment was 22 days (range, 18 to 23 days). One patient experienced secondary graft failure on day 90.
Seven neutropenic patients with hemoglobin S less than 30% received G-CSF after transplant. They received a median of 7 doses (range, 3 to 14) at 5 μg/kg, starting at day 12 post-HSCT. One of these patients experienced mild bone pain in the lower extremities.
Two patients developed GVHD. At day 83, one patient developed acute or chronic GVHD involving the skin, liver, and eyes. Steroids and sirolimus improved eye and liver symptoms, but the patient died at home on day 407.
The other patient had grade 2, gastrointestinal, acute GVHD that resolved with steroid therapy.
Three patients had grade 2 or higher mucositis, and 2 had cytomegalovirus (CMV) reactivation without CMV infection.
Two patients had small subarachnoid hemorrhages. One of these patients had a history of multiple red blood cell antibodies, became refractory to platelet transfusions, and developed small subarachnoid hemorrhages day 10. The patient’s symptoms and brain imaging resolved after platelet counts were maintained above 50 x 109 cells/L with cross-matched platelets.
The second patient had a history of stroke, experienced a seizure when the platelet count was 68 x 109 cells/L, and was found to have a subarachnoid hemorrhage on day 12. Symptoms and imaging results improved once the patient began levetiracetam and platelet levels were maintained above 100 x 109 cells/L.
At a median follow-up of 17 months (range, 12 to 30), 7 of the 8 patients were still alive.
Six patients had maintained greater than 95% stable donor engraftment with improvements in their hemoglobin concentrations. Three of these patients have stopped immunosuppression, and 3 are being tapered off it.
“These patients are cured of sickle cell disease,” Dr Rondelli said. “The takeaway message is two-fold. First, this transplant protocol may cure many more adult patients with advanced sickle cell disease.”
“Second, despite the increasing safety of the transplant protocols and new compatibility of HLA half-matched donors, many sickle cell patients still face barriers to care. Of the patients we screened, only 20% underwent a transplant.”
Dr Rondelli noted that 20% of the patients screened could not undergo transplant because of insurance denial. Other patients were ineligible because they had high rates of donor-specific antigens, and still others declined transplant.
A haploidentical transplant regimen has led to long-term engraftment in adults with sickle cell disease (SCD), according to researchers.
Seven of 8 patients treated with this regimen were still alive at last follow-up, and 6 of them maintained engraftment.
Two patients developed graft-versus-host disease (GVHD). One of them had acute and chronic GVHD and died about 400 days after transplant. The other had acute GVHD that resolved with treatment.
Damiano Rondelli, MD, of the University of Illinois at Chicago, and his colleagues reported these results in Biology of Blood and Marrow Transplantation.
The researchers initially screened 50 adult SCD patients as candidates for haploidentical hematopoietic stem cell transplant (haplo-HSCT) between January 2014 and March 2017. Most patients were ineligible or declined the procedure.
Ultimately, 10 patients received a haplo-HSCT. Unfortunately, the first 2 patients failed to engraft. These patients had received conditioning with alemtuzumab and 3 Gy total body irradiation (TBI) as well as post-transplant cyclophosphamide.
Because of this failure, the researchers used the following regimen for the remaining 8 patients. It’s a modified version of the regimen described in Blood in 2012.
“We modified the transplant protocol by increasing the dose of radiation used before the transplant and by infusing growth factor-mobilized peripheral blood stem cells instead of bone marrow cells,” Dr Rondelli said. “These two modifications helped ensure the patient’s body could accept the healthy donor cells.”
Modified regimen
Patients received growth-factor-mobilized peripheral blood stem cells after conditioning with rabbit antithymocyte globulin (0.5 mg/kg on day -9, 2 mg/kg on day -8 and -7), cyclophosphamide (14.5 mg/kg on day -6 and -5), fludarabine (30 mg/m2 on day -6 to -2), and single-dose TBI (3 Gy on day -1).
For GVHD prophylaxis, patients received intravenous cyclophosphamide (50 mg/kg on day 3 and 4), oral mycophenolate mofetil (15 mg/kg 3 times daily from day 5 to 35), and sirolimus (from day 5 dosed for a target trough of 5 to 15 ng/mL). In patients who had T-cell chimerism greater than 50% at 1 year after HSCT and did not have signs of GVHD, sirolimus was tapered off over 3 months.
Patients stopped taking hydroxyurea on day -9. They received red blood cell exchange transfusion on day -10 (with the goal of getting hemoglobin S below 30%) and received platelet transfusions to maintain platelet counts greater than 50 x 109 cells/L.
Patients also received penicillin V (250 mg twice daily) in addition to standard antimicrobial prophylaxis.
Results
All 8 patients on the modified regimen engrafted. The median time to neutrophil engraftment was 22 days (range, 18 to 23 days). One patient experienced secondary graft failure on day 90.
Seven neutropenic patients with hemoglobin S less than 30% received G-CSF after transplant. They received a median of 7 doses (range, 3 to 14) at 5 μg/kg, starting at day 12 post-HSCT. One of these patients experienced mild bone pain in the lower extremities.
Two patients developed GVHD. At day 83, one patient developed acute or chronic GVHD involving the skin, liver, and eyes. Steroids and sirolimus improved eye and liver symptoms, but the patient died at home on day 407.
The other patient had grade 2, gastrointestinal, acute GVHD that resolved with steroid therapy.
Three patients had grade 2 or higher mucositis, and 2 had cytomegalovirus (CMV) reactivation without CMV infection.
Two patients had small subarachnoid hemorrhages. One of these patients had a history of multiple red blood cell antibodies, became refractory to platelet transfusions, and developed small subarachnoid hemorrhages day 10. The patient’s symptoms and brain imaging resolved after platelet counts were maintained above 50 x 109 cells/L with cross-matched platelets.
The second patient had a history of stroke, experienced a seizure when the platelet count was 68 x 109 cells/L, and was found to have a subarachnoid hemorrhage on day 12. Symptoms and imaging results improved once the patient began levetiracetam and platelet levels were maintained above 100 x 109 cells/L.
At a median follow-up of 17 months (range, 12 to 30), 7 of the 8 patients were still alive.
Six patients had maintained greater than 95% stable donor engraftment with improvements in their hemoglobin concentrations. Three of these patients have stopped immunosuppression, and 3 are being tapered off it.
“These patients are cured of sickle cell disease,” Dr Rondelli said. “The takeaway message is two-fold. First, this transplant protocol may cure many more adult patients with advanced sickle cell disease.”
“Second, despite the increasing safety of the transplant protocols and new compatibility of HLA half-matched donors, many sickle cell patients still face barriers to care. Of the patients we screened, only 20% underwent a transplant.”
Dr Rondelli noted that 20% of the patients screened could not undergo transplant because of insurance denial. Other patients were ineligible because they had high rates of donor-specific antigens, and still others declined transplant.
A haploidentical transplant regimen has led to long-term engraftment in adults with sickle cell disease (SCD), according to researchers.
Seven of 8 patients treated with this regimen were still alive at last follow-up, and 6 of them maintained engraftment.
Two patients developed graft-versus-host disease (GVHD). One of them had acute and chronic GVHD and died about 400 days after transplant. The other had acute GVHD that resolved with treatment.
Damiano Rondelli, MD, of the University of Illinois at Chicago, and his colleagues reported these results in Biology of Blood and Marrow Transplantation.
The researchers initially screened 50 adult SCD patients as candidates for haploidentical hematopoietic stem cell transplant (haplo-HSCT) between January 2014 and March 2017. Most patients were ineligible or declined the procedure.
Ultimately, 10 patients received a haplo-HSCT. Unfortunately, the first 2 patients failed to engraft. These patients had received conditioning with alemtuzumab and 3 Gy total body irradiation (TBI) as well as post-transplant cyclophosphamide.
Because of this failure, the researchers used the following regimen for the remaining 8 patients. It’s a modified version of the regimen described in Blood in 2012.
“We modified the transplant protocol by increasing the dose of radiation used before the transplant and by infusing growth factor-mobilized peripheral blood stem cells instead of bone marrow cells,” Dr Rondelli said. “These two modifications helped ensure the patient’s body could accept the healthy donor cells.”
Modified regimen
Patients received growth-factor-mobilized peripheral blood stem cells after conditioning with rabbit antithymocyte globulin (0.5 mg/kg on day -9, 2 mg/kg on day -8 and -7), cyclophosphamide (14.5 mg/kg on day -6 and -5), fludarabine (30 mg/m2 on day -6 to -2), and single-dose TBI (3 Gy on day -1).
For GVHD prophylaxis, patients received intravenous cyclophosphamide (50 mg/kg on day 3 and 4), oral mycophenolate mofetil (15 mg/kg 3 times daily from day 5 to 35), and sirolimus (from day 5 dosed for a target trough of 5 to 15 ng/mL). In patients who had T-cell chimerism greater than 50% at 1 year after HSCT and did not have signs of GVHD, sirolimus was tapered off over 3 months.
Patients stopped taking hydroxyurea on day -9. They received red blood cell exchange transfusion on day -10 (with the goal of getting hemoglobin S below 30%) and received platelet transfusions to maintain platelet counts greater than 50 x 109 cells/L.
Patients also received penicillin V (250 mg twice daily) in addition to standard antimicrobial prophylaxis.
Results
All 8 patients on the modified regimen engrafted. The median time to neutrophil engraftment was 22 days (range, 18 to 23 days). One patient experienced secondary graft failure on day 90.
Seven neutropenic patients with hemoglobin S less than 30% received G-CSF after transplant. They received a median of 7 doses (range, 3 to 14) at 5 μg/kg, starting at day 12 post-HSCT. One of these patients experienced mild bone pain in the lower extremities.
Two patients developed GVHD. At day 83, one patient developed acute or chronic GVHD involving the skin, liver, and eyes. Steroids and sirolimus improved eye and liver symptoms, but the patient died at home on day 407.
The other patient had grade 2, gastrointestinal, acute GVHD that resolved with steroid therapy.
Three patients had grade 2 or higher mucositis, and 2 had cytomegalovirus (CMV) reactivation without CMV infection.
Two patients had small subarachnoid hemorrhages. One of these patients had a history of multiple red blood cell antibodies, became refractory to platelet transfusions, and developed small subarachnoid hemorrhages day 10. The patient’s symptoms and brain imaging resolved after platelet counts were maintained above 50 x 109 cells/L with cross-matched platelets.
The second patient had a history of stroke, experienced a seizure when the platelet count was 68 x 109 cells/L, and was found to have a subarachnoid hemorrhage on day 12. Symptoms and imaging results improved once the patient began levetiracetam and platelet levels were maintained above 100 x 109 cells/L.
At a median follow-up of 17 months (range, 12 to 30), 7 of the 8 patients were still alive.
Six patients had maintained greater than 95% stable donor engraftment with improvements in their hemoglobin concentrations. Three of these patients have stopped immunosuppression, and 3 are being tapered off it.
“These patients are cured of sickle cell disease,” Dr Rondelli said. “The takeaway message is two-fold. First, this transplant protocol may cure many more adult patients with advanced sickle cell disease.”
“Second, despite the increasing safety of the transplant protocols and new compatibility of HLA half-matched donors, many sickle cell patients still face barriers to care. Of the patients we screened, only 20% underwent a transplant.”
Dr Rondelli noted that 20% of the patients screened could not undergo transplant because of insurance denial. Other patients were ineligible because they had high rates of donor-specific antigens, and still others declined transplant.
Health Canada approves blood system for platelets
Health Canada has approved commercialization of the INTERCEPT Blood System for platelets, which is used for the ex vivo treatment and storage of platelet components.
The INTERCEPT Blood System for platelets can inactivate a range of pathogens—including viruses, bacteria, and protozoan parasites—to reduce the risk of transfusion-transmitted infections.
The system also inactivates contaminating donor leukocytes to reduce the risk of transfusion-associated graft-versus-host disease.
“[The INTERCEPT Blood System for platelets] provides an important, proactive safety measure to reduce the risk of transfusion-transmitted infections from known and emerging pathogens,” said Carol Moore, of Cerus Corporation, the company marketing the system.
“The approval provides blood centers the flexibility to pathogen-inactivate platelets derived from whole blood or apheresis collections, and stored in either platelet additive solution or plasma. In addition, Canadian blood centers will be able to create larger platelet pools from whole blood collections and use our double-dose INTERCEPT kits to yield 2 therapeutic platelet doses to realize improved operational efficiencies and economics.”
The INTERCEPT Blood System for platelets is Cerus Corporation’s second pathogen-inactivated system to be approved in Canada. The INTERCEPT Blood System for plasma was approved in May 2016.
The platelet and plasma systems use the same illumination device, the same active compound (amotosalen), and very similar production steps.
The INTERCEPT systems target a basic biological difference between the therapeutic components of blood. Platelets, plasma, and red blood cells do not require functional DNA or RNA for therapeutic efficacy. But pathogens and white blood cells do, in order to transmit infection.
The INTERCEPT systems use a proprietary molecule (amotosalen) that, when activated by UVA light, binds to and blocks the replication of DNA and RNA, preventing nucleic acid replication and rendering the pathogen inactive.
The INTERCEPT Blood System for platelets has been approved in Europe since 2002 and in the US since 2014.
Health Canada has approved commercialization of the INTERCEPT Blood System for platelets, which is used for the ex vivo treatment and storage of platelet components.
The INTERCEPT Blood System for platelets can inactivate a range of pathogens—including viruses, bacteria, and protozoan parasites—to reduce the risk of transfusion-transmitted infections.
The system also inactivates contaminating donor leukocytes to reduce the risk of transfusion-associated graft-versus-host disease.
“[The INTERCEPT Blood System for platelets] provides an important, proactive safety measure to reduce the risk of transfusion-transmitted infections from known and emerging pathogens,” said Carol Moore, of Cerus Corporation, the company marketing the system.
“The approval provides blood centers the flexibility to pathogen-inactivate platelets derived from whole blood or apheresis collections, and stored in either platelet additive solution or plasma. In addition, Canadian blood centers will be able to create larger platelet pools from whole blood collections and use our double-dose INTERCEPT kits to yield 2 therapeutic platelet doses to realize improved operational efficiencies and economics.”
The INTERCEPT Blood System for platelets is Cerus Corporation’s second pathogen-inactivated system to be approved in Canada. The INTERCEPT Blood System for plasma was approved in May 2016.
The platelet and plasma systems use the same illumination device, the same active compound (amotosalen), and very similar production steps.
The INTERCEPT systems target a basic biological difference between the therapeutic components of blood. Platelets, plasma, and red blood cells do not require functional DNA or RNA for therapeutic efficacy. But pathogens and white blood cells do, in order to transmit infection.
The INTERCEPT systems use a proprietary molecule (amotosalen) that, when activated by UVA light, binds to and blocks the replication of DNA and RNA, preventing nucleic acid replication and rendering the pathogen inactive.
The INTERCEPT Blood System for platelets has been approved in Europe since 2002 and in the US since 2014.
Health Canada has approved commercialization of the INTERCEPT Blood System for platelets, which is used for the ex vivo treatment and storage of platelet components.
The INTERCEPT Blood System for platelets can inactivate a range of pathogens—including viruses, bacteria, and protozoan parasites—to reduce the risk of transfusion-transmitted infections.
The system also inactivates contaminating donor leukocytes to reduce the risk of transfusion-associated graft-versus-host disease.
“[The INTERCEPT Blood System for platelets] provides an important, proactive safety measure to reduce the risk of transfusion-transmitted infections from known and emerging pathogens,” said Carol Moore, of Cerus Corporation, the company marketing the system.
“The approval provides blood centers the flexibility to pathogen-inactivate platelets derived from whole blood or apheresis collections, and stored in either platelet additive solution or plasma. In addition, Canadian blood centers will be able to create larger platelet pools from whole blood collections and use our double-dose INTERCEPT kits to yield 2 therapeutic platelet doses to realize improved operational efficiencies and economics.”
The INTERCEPT Blood System for platelets is Cerus Corporation’s second pathogen-inactivated system to be approved in Canada. The INTERCEPT Blood System for plasma was approved in May 2016.
The platelet and plasma systems use the same illumination device, the same active compound (amotosalen), and very similar production steps.
The INTERCEPT systems target a basic biological difference between the therapeutic components of blood. Platelets, plasma, and red blood cells do not require functional DNA or RNA for therapeutic efficacy. But pathogens and white blood cells do, in order to transmit infection.
The INTERCEPT systems use a proprietary molecule (amotosalen) that, when activated by UVA light, binds to and blocks the replication of DNA and RNA, preventing nucleic acid replication and rendering the pathogen inactive.
The INTERCEPT Blood System for platelets has been approved in Europe since 2002 and in the US since 2014.
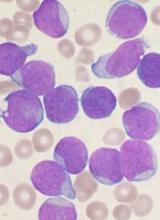
CDK inhibitor synergizes with venetoclax in CLL
CHICAGO—Researchers have reported “strong synergy” between the CDK2/9 inhibitor CYC065 and the Bcl-2 inhibitor venetoclax in chronic lymphocytic leukemia (CLL).
Experiments indicated that CYC065 and venetoclax target parallel mechanisms that promote survival in CLL cells, working together to induce apoptosis.
The drugs demonstrated synergy even in CLL samples that are inherently resistant to each drug alone.
William Plunkett, PhD, of The University of Texas MD Anderson Cancer Center in Houston, Texas, and his colleagues reported these findings at the AACR Annual Meeting 2018 (abstract 3905).
This research was supported by Cyclacel Pharmaceuticals, Inc., the company developing CYC065.
The researchers explained that CYC065 depletes Mcl-1 to induce apoptosis in CLL cells, while venetoclax induces apoptosis via inhibition of Bcl-2. However, upregulation of Mcl-1 is associated with resistance to venetoclax.
Therefore, the researchers theorized that combining CYC065 and venetoclax would serve to target 2 mechanisms that promote survival in CLL cells.
Experiments showed that CYC065 and venetoclax combined synergistically in CLL samples with or without 17p deletion. However, the researchers observed heterogeneity in response across samples.
The team said both drugs appeared to be less potent in some del(17p) samples. However, they also observed “great synergy” in del(17p) samples that were resistant to CYC065 or venetoclax alone.
The researchers noted differences in the kinetics of cell death in response to each drug and said this is consistent with the drugs’ different mechanisms of action.
Maximal cell death was reached at 6 to 8 hours with venetoclax but took at least 24 hours with CYC065.
The researchers also assessed the reversibility of CYC065 and venetoclax. They incubated CLL cells with each drug alone and in combination, then washed and incubated cells in drug-free media.
The team observed no additional cell death after the removal of CYC065, venetoclax, or the combination. They said this suggests an “adequate exposure time” is needed to maximize the induction of apoptosis with these drugs.
“[T]he combination of CYC065 and venetoclax is strongly synergistic in primary CLL cells from patients, including those with 17p deletions,” said Spiro Rombotis, president and chief executive officer of Cyclacel.
“In addition, the combination was active in 2 CLL samples which were resistant to either agent alone. These findings support the hypothesis that dual targeting of the Mcl-1- and Bcl-2-dependent mechanisms could induce synergistic cell death by apoptosis.”
Based on these results, Cyclacel is planning a trial of CYC065 and venetoclax in patients with relapsed/refractory CLL.
CHICAGO—Researchers have reported “strong synergy” between the CDK2/9 inhibitor CYC065 and the Bcl-2 inhibitor venetoclax in chronic lymphocytic leukemia (CLL).
Experiments indicated that CYC065 and venetoclax target parallel mechanisms that promote survival in CLL cells, working together to induce apoptosis.
The drugs demonstrated synergy even in CLL samples that are inherently resistant to each drug alone.
William Plunkett, PhD, of The University of Texas MD Anderson Cancer Center in Houston, Texas, and his colleagues reported these findings at the AACR Annual Meeting 2018 (abstract 3905).
This research was supported by Cyclacel Pharmaceuticals, Inc., the company developing CYC065.
The researchers explained that CYC065 depletes Mcl-1 to induce apoptosis in CLL cells, while venetoclax induces apoptosis via inhibition of Bcl-2. However, upregulation of Mcl-1 is associated with resistance to venetoclax.
Therefore, the researchers theorized that combining CYC065 and venetoclax would serve to target 2 mechanisms that promote survival in CLL cells.
Experiments showed that CYC065 and venetoclax combined synergistically in CLL samples with or without 17p deletion. However, the researchers observed heterogeneity in response across samples.
The team said both drugs appeared to be less potent in some del(17p) samples. However, they also observed “great synergy” in del(17p) samples that were resistant to CYC065 or venetoclax alone.
The researchers noted differences in the kinetics of cell death in response to each drug and said this is consistent with the drugs’ different mechanisms of action.
Maximal cell death was reached at 6 to 8 hours with venetoclax but took at least 24 hours with CYC065.
The researchers also assessed the reversibility of CYC065 and venetoclax. They incubated CLL cells with each drug alone and in combination, then washed and incubated cells in drug-free media.
The team observed no additional cell death after the removal of CYC065, venetoclax, or the combination. They said this suggests an “adequate exposure time” is needed to maximize the induction of apoptosis with these drugs.
“[T]he combination of CYC065 and venetoclax is strongly synergistic in primary CLL cells from patients, including those with 17p deletions,” said Spiro Rombotis, president and chief executive officer of Cyclacel.
“In addition, the combination was active in 2 CLL samples which were resistant to either agent alone. These findings support the hypothesis that dual targeting of the Mcl-1- and Bcl-2-dependent mechanisms could induce synergistic cell death by apoptosis.”
Based on these results, Cyclacel is planning a trial of CYC065 and venetoclax in patients with relapsed/refractory CLL.
CHICAGO—Researchers have reported “strong synergy” between the CDK2/9 inhibitor CYC065 and the Bcl-2 inhibitor venetoclax in chronic lymphocytic leukemia (CLL).
Experiments indicated that CYC065 and venetoclax target parallel mechanisms that promote survival in CLL cells, working together to induce apoptosis.
The drugs demonstrated synergy even in CLL samples that are inherently resistant to each drug alone.
William Plunkett, PhD, of The University of Texas MD Anderson Cancer Center in Houston, Texas, and his colleagues reported these findings at the AACR Annual Meeting 2018 (abstract 3905).
This research was supported by Cyclacel Pharmaceuticals, Inc., the company developing CYC065.
The researchers explained that CYC065 depletes Mcl-1 to induce apoptosis in CLL cells, while venetoclax induces apoptosis via inhibition of Bcl-2. However, upregulation of Mcl-1 is associated with resistance to venetoclax.
Therefore, the researchers theorized that combining CYC065 and venetoclax would serve to target 2 mechanisms that promote survival in CLL cells.
Experiments showed that CYC065 and venetoclax combined synergistically in CLL samples with or without 17p deletion. However, the researchers observed heterogeneity in response across samples.
The team said both drugs appeared to be less potent in some del(17p) samples. However, they also observed “great synergy” in del(17p) samples that were resistant to CYC065 or venetoclax alone.
The researchers noted differences in the kinetics of cell death in response to each drug and said this is consistent with the drugs’ different mechanisms of action.
Maximal cell death was reached at 6 to 8 hours with venetoclax but took at least 24 hours with CYC065.
The researchers also assessed the reversibility of CYC065 and venetoclax. They incubated CLL cells with each drug alone and in combination, then washed and incubated cells in drug-free media.
The team observed no additional cell death after the removal of CYC065, venetoclax, or the combination. They said this suggests an “adequate exposure time” is needed to maximize the induction of apoptosis with these drugs.
“[T]he combination of CYC065 and venetoclax is strongly synergistic in primary CLL cells from patients, including those with 17p deletions,” said Spiro Rombotis, president and chief executive officer of Cyclacel.
“In addition, the combination was active in 2 CLL samples which were resistant to either agent alone. These findings support the hypothesis that dual targeting of the Mcl-1- and Bcl-2-dependent mechanisms could induce synergistic cell death by apoptosis.”
Based on these results, Cyclacel is planning a trial of CYC065 and venetoclax in patients with relapsed/refractory CLL.
Potential therapeutic target for type of AML
New research suggests SHARP1 may be a therapeutic target in MLL-AF6 acute myeloid leukemia (AML).
Researchers found that SHARP1, a circadian clock transcription factor, is overexpressed in MLL-AF6 AML.
In mouse models, suppression of SHARP1 induced apoptosis in leukemic cells, while deletion of SHARP1 delayed AML development and weakened leukemia-initiating potential.
“We found that MLL-AF6 binds with SHARP1, leading to an increase in the level of SHARP1,” explained study author Dan Tenen, MD, of the Cancer Science Institute of Singapore.
“The increase of SHARP1 levels has the 2-fold effect of initiating leukemia development, as well as maintaining the growth of leukemic cells. [O]ur study also revealed that SHARP1 could act upon other target genes of MLL-AF6 to aggravate the progression of AML, but, by removing or reducing the level of SHARP1, the growth of leukemic cells could be stopped.”
Dr Tenen and his colleagues reported these findings in Nature Communications.
The researchers found that SHARP1 was overexpressed in MLL-AF6 AML, but its expression was decreased in most other subtypes of AML analyzed as well as in normal bone marrow CD34+ cells.
Experiments in AML cell lines revealed that SHARP1 expression is regulated by MLL-AF6/DOT1L. The researchers said MLL-AF6 and MEN1/LEDGF directly bind to the SHARP1 gene locus to positively regulate SHARP1 expression through DOT1L activity.
Dr Tenen and his colleagues performed knockdown experiments in mice and found that SHARP1 plays a “critical” role in maintaining clonogenic growth and preventing apoptosis in MLL-AF6 AML cells.
The team also assessed the effects of SHARP1 deletion in mouse models of MLL-AF6 AML.
SHARP1 knockout mice had superior survival compared to wild-type mice. In addition, the knockout mice exhibited signs of less aggressive disease—fewer AML cells, lower white blood cell counts, and higher red blood cell counts.
The researchers also found that SHARP1 deletion reduced MLL-AF6 leukemia-initiating ability but did not affect normal hematopoiesis.
Finally, the team discovered that SHARP1 cooperates with MLL-AF6 to regulate target genes in MLL-AF6 AML cells.
New research suggests SHARP1 may be a therapeutic target in MLL-AF6 acute myeloid leukemia (AML).
Researchers found that SHARP1, a circadian clock transcription factor, is overexpressed in MLL-AF6 AML.
In mouse models, suppression of SHARP1 induced apoptosis in leukemic cells, while deletion of SHARP1 delayed AML development and weakened leukemia-initiating potential.
“We found that MLL-AF6 binds with SHARP1, leading to an increase in the level of SHARP1,” explained study author Dan Tenen, MD, of the Cancer Science Institute of Singapore.
“The increase of SHARP1 levels has the 2-fold effect of initiating leukemia development, as well as maintaining the growth of leukemic cells. [O]ur study also revealed that SHARP1 could act upon other target genes of MLL-AF6 to aggravate the progression of AML, but, by removing or reducing the level of SHARP1, the growth of leukemic cells could be stopped.”
Dr Tenen and his colleagues reported these findings in Nature Communications.
The researchers found that SHARP1 was overexpressed in MLL-AF6 AML, but its expression was decreased in most other subtypes of AML analyzed as well as in normal bone marrow CD34+ cells.
Experiments in AML cell lines revealed that SHARP1 expression is regulated by MLL-AF6/DOT1L. The researchers said MLL-AF6 and MEN1/LEDGF directly bind to the SHARP1 gene locus to positively regulate SHARP1 expression through DOT1L activity.
Dr Tenen and his colleagues performed knockdown experiments in mice and found that SHARP1 plays a “critical” role in maintaining clonogenic growth and preventing apoptosis in MLL-AF6 AML cells.
The team also assessed the effects of SHARP1 deletion in mouse models of MLL-AF6 AML.
SHARP1 knockout mice had superior survival compared to wild-type mice. In addition, the knockout mice exhibited signs of less aggressive disease—fewer AML cells, lower white blood cell counts, and higher red blood cell counts.
The researchers also found that SHARP1 deletion reduced MLL-AF6 leukemia-initiating ability but did not affect normal hematopoiesis.
Finally, the team discovered that SHARP1 cooperates with MLL-AF6 to regulate target genes in MLL-AF6 AML cells.
New research suggests SHARP1 may be a therapeutic target in MLL-AF6 acute myeloid leukemia (AML).
Researchers found that SHARP1, a circadian clock transcription factor, is overexpressed in MLL-AF6 AML.
In mouse models, suppression of SHARP1 induced apoptosis in leukemic cells, while deletion of SHARP1 delayed AML development and weakened leukemia-initiating potential.
“We found that MLL-AF6 binds with SHARP1, leading to an increase in the level of SHARP1,” explained study author Dan Tenen, MD, of the Cancer Science Institute of Singapore.
“The increase of SHARP1 levels has the 2-fold effect of initiating leukemia development, as well as maintaining the growth of leukemic cells. [O]ur study also revealed that SHARP1 could act upon other target genes of MLL-AF6 to aggravate the progression of AML, but, by removing or reducing the level of SHARP1, the growth of leukemic cells could be stopped.”
Dr Tenen and his colleagues reported these findings in Nature Communications.
The researchers found that SHARP1 was overexpressed in MLL-AF6 AML, but its expression was decreased in most other subtypes of AML analyzed as well as in normal bone marrow CD34+ cells.
Experiments in AML cell lines revealed that SHARP1 expression is regulated by MLL-AF6/DOT1L. The researchers said MLL-AF6 and MEN1/LEDGF directly bind to the SHARP1 gene locus to positively regulate SHARP1 expression through DOT1L activity.
Dr Tenen and his colleagues performed knockdown experiments in mice and found that SHARP1 plays a “critical” role in maintaining clonogenic growth and preventing apoptosis in MLL-AF6 AML cells.
The team also assessed the effects of SHARP1 deletion in mouse models of MLL-AF6 AML.
SHARP1 knockout mice had superior survival compared to wild-type mice. In addition, the knockout mice exhibited signs of less aggressive disease—fewer AML cells, lower white blood cell counts, and higher red blood cell counts.
The researchers also found that SHARP1 deletion reduced MLL-AF6 leukemia-initiating ability but did not affect normal hematopoiesis.
Finally, the team discovered that SHARP1 cooperates with MLL-AF6 to regulate target genes in MLL-AF6 AML cells.
FDA places tazemetostat trials on partial hold
The US Food and Drug Administration (FDA) has placed a partial hold on clinical trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas.
The hold has halted enrollment in US-based trials of tazemetostat, but study subjects who have not experienced disease progression may continue to receive the drug.
The hold is due to an adverse event observed in a pediatric patient on a phase 1 study of tazemetostat.
The patient, who had advanced poorly differentiated chordoma, developed a secondary T-cell lymphoma while taking tazemetostat.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. Now, the patient has discontinued tazemetostat and is being treated for T-cell lymphoma.
More than 750 patients have been treated with tazemetostat to date, and this is the only case of secondary lymphoma that has been observed, according to Epizyme, Inc., the company developing tazemetostat.
The company also noted that doses of tazemetostat explored in its phase 1 pediatric study are higher than those used in the phase 2 adult studies.
Epizyme has begun taking steps to address the hold on tazemetostat trials—updating the informed consent, investigator’s brochure, and study protocols.
The company will need to confirm alignment with the FDA in order to resume US enrollment.
“We are working expeditiously with clinical trial investigators and regulatory authorities to initiate the appropriate steps to resume enrollment,” said Robert Bazemore, president and chief executive officer of Epizyme.
“Epizyme, along with our global investigator community, has been very encouraged by the clinical responses and tolerability of tazemetostat observed in pediatric and adult patients with hematological malignancies and solid tumors enrolled in our trials. We remain encouraged by the potential of tazemetostat to address the unmet needs of many patients living with cancer.”
The US Food and Drug Administration (FDA) has placed a partial hold on clinical trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas.
The hold has halted enrollment in US-based trials of tazemetostat, but study subjects who have not experienced disease progression may continue to receive the drug.
The hold is due to an adverse event observed in a pediatric patient on a phase 1 study of tazemetostat.
The patient, who had advanced poorly differentiated chordoma, developed a secondary T-cell lymphoma while taking tazemetostat.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. Now, the patient has discontinued tazemetostat and is being treated for T-cell lymphoma.
More than 750 patients have been treated with tazemetostat to date, and this is the only case of secondary lymphoma that has been observed, according to Epizyme, Inc., the company developing tazemetostat.
The company also noted that doses of tazemetostat explored in its phase 1 pediatric study are higher than those used in the phase 2 adult studies.
Epizyme has begun taking steps to address the hold on tazemetostat trials—updating the informed consent, investigator’s brochure, and study protocols.
The company will need to confirm alignment with the FDA in order to resume US enrollment.
“We are working expeditiously with clinical trial investigators and regulatory authorities to initiate the appropriate steps to resume enrollment,” said Robert Bazemore, president and chief executive officer of Epizyme.
“Epizyme, along with our global investigator community, has been very encouraged by the clinical responses and tolerability of tazemetostat observed in pediatric and adult patients with hematological malignancies and solid tumors enrolled in our trials. We remain encouraged by the potential of tazemetostat to address the unmet needs of many patients living with cancer.”
The US Food and Drug Administration (FDA) has placed a partial hold on clinical trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas.
The hold has halted enrollment in US-based trials of tazemetostat, but study subjects who have not experienced disease progression may continue to receive the drug.
The hold is due to an adverse event observed in a pediatric patient on a phase 1 study of tazemetostat.
The patient, who had advanced poorly differentiated chordoma, developed a secondary T-cell lymphoma while taking tazemetostat.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. Now, the patient has discontinued tazemetostat and is being treated for T-cell lymphoma.
More than 750 patients have been treated with tazemetostat to date, and this is the only case of secondary lymphoma that has been observed, according to Epizyme, Inc., the company developing tazemetostat.
The company also noted that doses of tazemetostat explored in its phase 1 pediatric study are higher than those used in the phase 2 adult studies.
Epizyme has begun taking steps to address the hold on tazemetostat trials—updating the informed consent, investigator’s brochure, and study protocols.
The company will need to confirm alignment with the FDA in order to resume US enrollment.
“We are working expeditiously with clinical trial investigators and regulatory authorities to initiate the appropriate steps to resume enrollment,” said Robert Bazemore, president and chief executive officer of Epizyme.
“Epizyme, along with our global investigator community, has been very encouraged by the clinical responses and tolerability of tazemetostat observed in pediatric and adult patients with hematological malignancies and solid tumors enrolled in our trials. We remain encouraged by the potential of tazemetostat to address the unmet needs of many patients living with cancer.”
Improving education for pediatric cancer caregivers
A new checklist could improve education for parents and other caregivers of children newly diagnosed with cancer, according to a group of nurses.
The checklist is divided into topics that should be taught according to their level of urgency.
The list includes subjects that should be discussed prior to patients’ initial hospital discharge and topics that can be covered later, either within the first month of the patients’ cancer diagnosis or before patients complete therapy.
Cheryl Rodgers, PhD, RN, and her colleagues provided details on this checklist in the Journal of Pediatric Oncology Nursing.
A team of 19 nurses and 2 parent advocates from the Children’s Oncology Group developed the checklist based on existing education checklists, expert recommendations, and team-based activities and discussions.
The checklist is divided into primary, secondary, and tertiary topics.
Primary topics are those that should be discussed with caregivers before they leave the hospital the first time. Examples include home medication dose and frequency, who and when to call for help, preventing infection, and treatment side effects to know before the next appointment.
Secondary topics are those that can be covered during the first month after a child’s cancer diagnosis. Examples include an explanation of what cancer is, an overview of chemotherapy, and more details on the side effects of cancer treatment.
Tertiary topics can be discussed before the child finishes cancer treatment. Examples include details on tests and procedures, risky behaviors to avoid, coping skills, and insurance issues.
Dr Rodgers and her colleagues said this checklist provides nurses with a clear outline of topics that should be discussed with caregivers immediately and topics that can be safely deferred. This could prevent information overload and help caregivers remember the most important information.
A new checklist could improve education for parents and other caregivers of children newly diagnosed with cancer, according to a group of nurses.
The checklist is divided into topics that should be taught according to their level of urgency.
The list includes subjects that should be discussed prior to patients’ initial hospital discharge and topics that can be covered later, either within the first month of the patients’ cancer diagnosis or before patients complete therapy.
Cheryl Rodgers, PhD, RN, and her colleagues provided details on this checklist in the Journal of Pediatric Oncology Nursing.
A team of 19 nurses and 2 parent advocates from the Children’s Oncology Group developed the checklist based on existing education checklists, expert recommendations, and team-based activities and discussions.
The checklist is divided into primary, secondary, and tertiary topics.
Primary topics are those that should be discussed with caregivers before they leave the hospital the first time. Examples include home medication dose and frequency, who and when to call for help, preventing infection, and treatment side effects to know before the next appointment.
Secondary topics are those that can be covered during the first month after a child’s cancer diagnosis. Examples include an explanation of what cancer is, an overview of chemotherapy, and more details on the side effects of cancer treatment.
Tertiary topics can be discussed before the child finishes cancer treatment. Examples include details on tests and procedures, risky behaviors to avoid, coping skills, and insurance issues.
Dr Rodgers and her colleagues said this checklist provides nurses with a clear outline of topics that should be discussed with caregivers immediately and topics that can be safely deferred. This could prevent information overload and help caregivers remember the most important information.
A new checklist could improve education for parents and other caregivers of children newly diagnosed with cancer, according to a group of nurses.
The checklist is divided into topics that should be taught according to their level of urgency.
The list includes subjects that should be discussed prior to patients’ initial hospital discharge and topics that can be covered later, either within the first month of the patients’ cancer diagnosis or before patients complete therapy.
Cheryl Rodgers, PhD, RN, and her colleagues provided details on this checklist in the Journal of Pediatric Oncology Nursing.
A team of 19 nurses and 2 parent advocates from the Children’s Oncology Group developed the checklist based on existing education checklists, expert recommendations, and team-based activities and discussions.
The checklist is divided into primary, secondary, and tertiary topics.
Primary topics are those that should be discussed with caregivers before they leave the hospital the first time. Examples include home medication dose and frequency, who and when to call for help, preventing infection, and treatment side effects to know before the next appointment.
Secondary topics are those that can be covered during the first month after a child’s cancer diagnosis. Examples include an explanation of what cancer is, an overview of chemotherapy, and more details on the side effects of cancer treatment.
Tertiary topics can be discussed before the child finishes cancer treatment. Examples include details on tests and procedures, risky behaviors to avoid, coping skills, and insurance issues.
Dr Rodgers and her colleagues said this checklist provides nurses with a clear outline of topics that should be discussed with caregivers immediately and topics that can be safely deferred. This could prevent information overload and help caregivers remember the most important information.
Drug receives orphan designation for ALL
The US Food and Drug Administration (FDA) has granted orphan drug designation to LBS-007 as a treatment for acute lymphoblastic leukemia (ALL).
LBS-007 is a non-ATP cell-cycle inhibitor targeting a range of cancers.
LBS-007 functions by blocking the kinase activity of CDC7, a key regulator of the cancer cell cycle.
Inhibiting CDC7 stops the proliferation of tumor cells and results in cell death.
Lin BioScience, Inc., the company developing LBS-007, said the drug has demonstrated “very potent activity” against leukemia and solid tumors in preclinical studies.
The company is expected to launch a phase 1 trial of LBS-007 in drug-resistant and refractory acute leukemia in the fourth quarter of 2018.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to LBS-007 as a treatment for acute lymphoblastic leukemia (ALL).
LBS-007 is a non-ATP cell-cycle inhibitor targeting a range of cancers.
LBS-007 functions by blocking the kinase activity of CDC7, a key regulator of the cancer cell cycle.
Inhibiting CDC7 stops the proliferation of tumor cells and results in cell death.
Lin BioScience, Inc., the company developing LBS-007, said the drug has demonstrated “very potent activity” against leukemia and solid tumors in preclinical studies.
The company is expected to launch a phase 1 trial of LBS-007 in drug-resistant and refractory acute leukemia in the fourth quarter of 2018.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to LBS-007 as a treatment for acute lymphoblastic leukemia (ALL).
LBS-007 is a non-ATP cell-cycle inhibitor targeting a range of cancers.
LBS-007 functions by blocking the kinase activity of CDC7, a key regulator of the cancer cell cycle.
Inhibiting CDC7 stops the proliferation of tumor cells and results in cell death.
Lin BioScience, Inc., the company developing LBS-007, said the drug has demonstrated “very potent activity” against leukemia and solid tumors in preclinical studies.
The company is expected to launch a phase 1 trial of LBS-007 in drug-resistant and refractory acute leukemia in the fourth quarter of 2018.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.