User login
Clinical trial registries don’t match up
A new study has revealed discrepancies in completion status for trials listed on ClinicalTrials.gov and the EU Clinical Trials Register (EUCTR).
Researchers evaluated nearly 10,500 trials listed on both registries and found that roughly 16% of them were marked as “completed” on one registry and “ongoing” on the other.
Most of these (91%) were listed as “ongoing” on EUCTR but “completed” on ClinicalTrials.gov.
“Trial registries are important public documents,” said Ben Goldacre, of the University of Oxford in the UK.
“Doctors, researchers, and patients rely on the information that trialists post about their clinical trial. Concerningly, we now show that this data is commonly inaccurate.”
Goldacre and his colleague, Jessica Fleminger, also from the University of Oxford, reported these findings in PLOS ONE.
The researchers looked at 10,492 clinical trials that were registered on both ClinicalTrials.gov and EUCTR.
For most of these trials (83.8%, n=8794), completion status was the same on both registries. But there were 1698 trials (16.2%) that were listed as “completed” on one registry and “ongoing” on another.
A majority of the discrepant trials (90.5%, n=1536) were “ongoing” on EUCTR and “complete” on ClinicalTrials.gov.
Overall, 43.1% (4530/10,492) of dual-registered trials were listed as “ongoing” on EUCTR, and 33.9% of these (1536/4530) were listed as “completed” on ClinicalTrials.gov.
Thirty percent (3156/10,492) of dual-registered trials were marked as “ongoing” on ClinicalTrials.gov, and 5.1% (162/3156) of these were marked as “completed” on EUCTR.
Goldacre and Fleminger said it is unclear whether researchers, registry owners, or both are responsible for these errors. Regardless, researchers identifying discrepancies should request clarifications from the trialists, and registry owners should undertake simple cross-checks of data to ensure that completion status is accurate.
A new study has revealed discrepancies in completion status for trials listed on ClinicalTrials.gov and the EU Clinical Trials Register (EUCTR).
Researchers evaluated nearly 10,500 trials listed on both registries and found that roughly 16% of them were marked as “completed” on one registry and “ongoing” on the other.
Most of these (91%) were listed as “ongoing” on EUCTR but “completed” on ClinicalTrials.gov.
“Trial registries are important public documents,” said Ben Goldacre, of the University of Oxford in the UK.
“Doctors, researchers, and patients rely on the information that trialists post about their clinical trial. Concerningly, we now show that this data is commonly inaccurate.”
Goldacre and his colleague, Jessica Fleminger, also from the University of Oxford, reported these findings in PLOS ONE.
The researchers looked at 10,492 clinical trials that were registered on both ClinicalTrials.gov and EUCTR.
For most of these trials (83.8%, n=8794), completion status was the same on both registries. But there were 1698 trials (16.2%) that were listed as “completed” on one registry and “ongoing” on another.
A majority of the discrepant trials (90.5%, n=1536) were “ongoing” on EUCTR and “complete” on ClinicalTrials.gov.
Overall, 43.1% (4530/10,492) of dual-registered trials were listed as “ongoing” on EUCTR, and 33.9% of these (1536/4530) were listed as “completed” on ClinicalTrials.gov.
Thirty percent (3156/10,492) of dual-registered trials were marked as “ongoing” on ClinicalTrials.gov, and 5.1% (162/3156) of these were marked as “completed” on EUCTR.
Goldacre and Fleminger said it is unclear whether researchers, registry owners, or both are responsible for these errors. Regardless, researchers identifying discrepancies should request clarifications from the trialists, and registry owners should undertake simple cross-checks of data to ensure that completion status is accurate.
A new study has revealed discrepancies in completion status for trials listed on ClinicalTrials.gov and the EU Clinical Trials Register (EUCTR).
Researchers evaluated nearly 10,500 trials listed on both registries and found that roughly 16% of them were marked as “completed” on one registry and “ongoing” on the other.
Most of these (91%) were listed as “ongoing” on EUCTR but “completed” on ClinicalTrials.gov.
“Trial registries are important public documents,” said Ben Goldacre, of the University of Oxford in the UK.
“Doctors, researchers, and patients rely on the information that trialists post about their clinical trial. Concerningly, we now show that this data is commonly inaccurate.”
Goldacre and his colleague, Jessica Fleminger, also from the University of Oxford, reported these findings in PLOS ONE.
The researchers looked at 10,492 clinical trials that were registered on both ClinicalTrials.gov and EUCTR.
For most of these trials (83.8%, n=8794), completion status was the same on both registries. But there were 1698 trials (16.2%) that were listed as “completed” on one registry and “ongoing” on another.
A majority of the discrepant trials (90.5%, n=1536) were “ongoing” on EUCTR and “complete” on ClinicalTrials.gov.
Overall, 43.1% (4530/10,492) of dual-registered trials were listed as “ongoing” on EUCTR, and 33.9% of these (1536/4530) were listed as “completed” on ClinicalTrials.gov.
Thirty percent (3156/10,492) of dual-registered trials were marked as “ongoing” on ClinicalTrials.gov, and 5.1% (162/3156) of these were marked as “completed” on EUCTR.
Goldacre and Fleminger said it is unclear whether researchers, registry owners, or both are responsible for these errors. Regardless, researchers identifying discrepancies should request clarifications from the trialists, and registry owners should undertake simple cross-checks of data to ensure that completion status is accurate.
Researchers question validity of NCCN guidelines
New research suggests guidelines from the National Comprehensive Cancer Network (NCCN) may sometimes be supported by low-quality evidence or no evidence at all.
Researchers compared NCCN recommendations for cancer drugs to US cancer drug approvals over a 5-year period.
Thirty-nine percent of NCCN’s treatment recommendations did not coincide with uses approved by the US Food and Drug Administration (FDA).
For most of these recommendations (84%), NCCN did not provide supporting data from randomized, phase 3 trials.
For 36% of the recommendations, NCCN gave no supporting evidence.
Vinay Prasad, MD, of Oregon Health & Science University in Portland, Oregon, and his colleagues reported these findings in The BMJ.
Dr Prasad and his colleagues compared FDA approvals of cancer drugs between 2011 and 2015 with NCCN recommendations as of March 25, 2016.
When NCCN made recommendations beyond FDA approvals, the researchers evaluated the evidence used to support those recommendations.
Forty-seven new cancer drugs were approved by the FDA for 69 indications between 2011 and 2015. NCCN recommended the 47 drugs for 113 indications, including the 69 FDA-approved indications.
So 39% (n=44) of NCCN’s recommendations were not approved by the FDA, and NCCN gave the following evidence to support these recommendations:
- No evidence—36% (n=16)
- Phase 2 trial without randomization—30% (n=13)
- Randomized, phase 3 trial—16% (n=7)
- Phase 2 trial with randomization—7% (n=3)
- Case report or series of less than 5 patients—5% (n=2)
- Book chapter or review article—2% (n=1)
- Phase 1 trial—2% (n=1)
- Ongoing trial—2% (n=1).
Dr Prasad and his colleagues did point out that not all FDA approvals are supported by randomized, phase 3 trials.
And when the team followed-up 21 months after their initial analysis, they found that 6 of the 44 (14%) additional recommendations by NCCN had received FDA approval.
The researchers also noted that they did not search for independent evidence to support NCCN recommendations beyond the references NCCN provided. So some of the recommendations may have had more or better supporting evidence than what was provided.
Still, the team said these results suggest NCCN “frequently” makes recommendations that go beyond FDA approvals and “often fails to cite evidence or relies on low levels of evidence.” Therefore, NCCN should cite all evidence used to formulate its recommendations.
NCCN argues that it does provide ample evidence to support the recommendations in its guidelines.
“The NCCN guidelines contain more than 24,500 references to inform users of the evidence used in making its decisions,” said Robert W. Carlson, MD, chief executive officer of NCCN.
“These data are supplemented by the analysis of the available evidence by expert clinician researchers and patient advocates who evaluate each recommendation and come to consensus. Each recommendation is labeled with a Category of Evidence, and the vast majority of those for systemic therapies are accompanied by Evidence Blocks, which outline, on 1-5 scales, the efficacy, safety, quality of the evidence, consistency of the evidence, and affordability of the treatment.”
New research suggests guidelines from the National Comprehensive Cancer Network (NCCN) may sometimes be supported by low-quality evidence or no evidence at all.
Researchers compared NCCN recommendations for cancer drugs to US cancer drug approvals over a 5-year period.
Thirty-nine percent of NCCN’s treatment recommendations did not coincide with uses approved by the US Food and Drug Administration (FDA).
For most of these recommendations (84%), NCCN did not provide supporting data from randomized, phase 3 trials.
For 36% of the recommendations, NCCN gave no supporting evidence.
Vinay Prasad, MD, of Oregon Health & Science University in Portland, Oregon, and his colleagues reported these findings in The BMJ.
Dr Prasad and his colleagues compared FDA approvals of cancer drugs between 2011 and 2015 with NCCN recommendations as of March 25, 2016.
When NCCN made recommendations beyond FDA approvals, the researchers evaluated the evidence used to support those recommendations.
Forty-seven new cancer drugs were approved by the FDA for 69 indications between 2011 and 2015. NCCN recommended the 47 drugs for 113 indications, including the 69 FDA-approved indications.
So 39% (n=44) of NCCN’s recommendations were not approved by the FDA, and NCCN gave the following evidence to support these recommendations:
- No evidence—36% (n=16)
- Phase 2 trial without randomization—30% (n=13)
- Randomized, phase 3 trial—16% (n=7)
- Phase 2 trial with randomization—7% (n=3)
- Case report or series of less than 5 patients—5% (n=2)
- Book chapter or review article—2% (n=1)
- Phase 1 trial—2% (n=1)
- Ongoing trial—2% (n=1).
Dr Prasad and his colleagues did point out that not all FDA approvals are supported by randomized, phase 3 trials.
And when the team followed-up 21 months after their initial analysis, they found that 6 of the 44 (14%) additional recommendations by NCCN had received FDA approval.
The researchers also noted that they did not search for independent evidence to support NCCN recommendations beyond the references NCCN provided. So some of the recommendations may have had more or better supporting evidence than what was provided.
Still, the team said these results suggest NCCN “frequently” makes recommendations that go beyond FDA approvals and “often fails to cite evidence or relies on low levels of evidence.” Therefore, NCCN should cite all evidence used to formulate its recommendations.
NCCN argues that it does provide ample evidence to support the recommendations in its guidelines.
“The NCCN guidelines contain more than 24,500 references to inform users of the evidence used in making its decisions,” said Robert W. Carlson, MD, chief executive officer of NCCN.
“These data are supplemented by the analysis of the available evidence by expert clinician researchers and patient advocates who evaluate each recommendation and come to consensus. Each recommendation is labeled with a Category of Evidence, and the vast majority of those for systemic therapies are accompanied by Evidence Blocks, which outline, on 1-5 scales, the efficacy, safety, quality of the evidence, consistency of the evidence, and affordability of the treatment.”
New research suggests guidelines from the National Comprehensive Cancer Network (NCCN) may sometimes be supported by low-quality evidence or no evidence at all.
Researchers compared NCCN recommendations for cancer drugs to US cancer drug approvals over a 5-year period.
Thirty-nine percent of NCCN’s treatment recommendations did not coincide with uses approved by the US Food and Drug Administration (FDA).
For most of these recommendations (84%), NCCN did not provide supporting data from randomized, phase 3 trials.
For 36% of the recommendations, NCCN gave no supporting evidence.
Vinay Prasad, MD, of Oregon Health & Science University in Portland, Oregon, and his colleagues reported these findings in The BMJ.
Dr Prasad and his colleagues compared FDA approvals of cancer drugs between 2011 and 2015 with NCCN recommendations as of March 25, 2016.
When NCCN made recommendations beyond FDA approvals, the researchers evaluated the evidence used to support those recommendations.
Forty-seven new cancer drugs were approved by the FDA for 69 indications between 2011 and 2015. NCCN recommended the 47 drugs for 113 indications, including the 69 FDA-approved indications.
So 39% (n=44) of NCCN’s recommendations were not approved by the FDA, and NCCN gave the following evidence to support these recommendations:
- No evidence—36% (n=16)
- Phase 2 trial without randomization—30% (n=13)
- Randomized, phase 3 trial—16% (n=7)
- Phase 2 trial with randomization—7% (n=3)
- Case report or series of less than 5 patients—5% (n=2)
- Book chapter or review article—2% (n=1)
- Phase 1 trial—2% (n=1)
- Ongoing trial—2% (n=1).
Dr Prasad and his colleagues did point out that not all FDA approvals are supported by randomized, phase 3 trials.
And when the team followed-up 21 months after their initial analysis, they found that 6 of the 44 (14%) additional recommendations by NCCN had received FDA approval.
The researchers also noted that they did not search for independent evidence to support NCCN recommendations beyond the references NCCN provided. So some of the recommendations may have had more or better supporting evidence than what was provided.
Still, the team said these results suggest NCCN “frequently” makes recommendations that go beyond FDA approvals and “often fails to cite evidence or relies on low levels of evidence.” Therefore, NCCN should cite all evidence used to formulate its recommendations.
NCCN argues that it does provide ample evidence to support the recommendations in its guidelines.
“The NCCN guidelines contain more than 24,500 references to inform users of the evidence used in making its decisions,” said Robert W. Carlson, MD, chief executive officer of NCCN.
“These data are supplemented by the analysis of the available evidence by expert clinician researchers and patient advocates who evaluate each recommendation and come to consensus. Each recommendation is labeled with a Category of Evidence, and the vast majority of those for systemic therapies are accompanied by Evidence Blocks, which outline, on 1-5 scales, the efficacy, safety, quality of the evidence, consistency of the evidence, and affordability of the treatment.”
FDA approves first donor screening tests for Babesia
The US Food and Drug Administration (FDA) has approved the first tests to screen blood donors for Babesia parasites.
The Imugen Babesia microti Arrayed Fluorescent Immunoassay (AFIA) is approved for the detection of antibodies to Babesia microti in plasma samples, and the Imugen Babesia microti Nucleic Acid Test (NAT) is approved for the detection of Babesia microti DNA in whole blood samples.
These tests are intended to be used on samples from volunteer donors of whole blood and blood components as well as living organ and tissue donors.
The tests are not intended for use in the diagnosis of babesiosis infections.
The approval of the Imugen Babesia microti AFIA and NAT tests was granted to Oxford Immunotec, Inc. Both assays are in-house tests that can only be performed at the Norwood, Massachusetts facility.
The applications for the tests were granted priority review. The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products expected to significantly improve the safety or effectiveness of treating, diagnosing, or preventing a serious condition.
“While babesiosis is both preventable and treatable, until today, there was no way to screen for infections amongst blood donors,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research.
“Today’s actions represent the first approvals of Babesia detection tests for use in screening donors of whole blood and blood components, and other living donors.”
About babesiosis
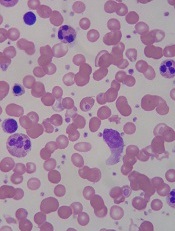
Babesiosis is caused by Babesia parasites that are transmitted by Ixodes scapularis ticks, also known as blacklegged or deer ticks. Babesia microti is the main species of parasite that causes infection in the US.
There are about 1000 to 2000 cases of babesiosis reported in the US each year, with the majority reported from states in the Northeast and upper Midwest.
Most people infected with Babesia microti do not have symptoms and are never diagnosed. Some people develop flu-like symptoms, such as fever, headache, and body aches.
For certain people, especially those with a weak immune system, babesiosis can be a severe, life-threatening disease. And although blood-borne transmission of babesiosis is thought to be uncommon, it is the most frequently reported transfusion-transmitted parasitic infection in the US.
At present, there is no FDA guidance for the testing of donor samples for Babesia. However, the FDA is planning to issue a draft guidance later this year that will include recommendations for reducing the risk of transfusion-transmitted babesiosis.
The US Food and Drug Administration (FDA) has approved the first tests to screen blood donors for Babesia parasites.
The Imugen Babesia microti Arrayed Fluorescent Immunoassay (AFIA) is approved for the detection of antibodies to Babesia microti in plasma samples, and the Imugen Babesia microti Nucleic Acid Test (NAT) is approved for the detection of Babesia microti DNA in whole blood samples.
These tests are intended to be used on samples from volunteer donors of whole blood and blood components as well as living organ and tissue donors.
The tests are not intended for use in the diagnosis of babesiosis infections.
The approval of the Imugen Babesia microti AFIA and NAT tests was granted to Oxford Immunotec, Inc. Both assays are in-house tests that can only be performed at the Norwood, Massachusetts facility.
The applications for the tests were granted priority review. The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products expected to significantly improve the safety or effectiveness of treating, diagnosing, or preventing a serious condition.
“While babesiosis is both preventable and treatable, until today, there was no way to screen for infections amongst blood donors,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research.
“Today’s actions represent the first approvals of Babesia detection tests for use in screening donors of whole blood and blood components, and other living donors.”
About babesiosis
Babesiosis is caused by Babesia parasites that are transmitted by Ixodes scapularis ticks, also known as blacklegged or deer ticks. Babesia microti is the main species of parasite that causes infection in the US.
There are about 1000 to 2000 cases of babesiosis reported in the US each year, with the majority reported from states in the Northeast and upper Midwest.
Most people infected with Babesia microti do not have symptoms and are never diagnosed. Some people develop flu-like symptoms, such as fever, headache, and body aches.
For certain people, especially those with a weak immune system, babesiosis can be a severe, life-threatening disease. And although blood-borne transmission of babesiosis is thought to be uncommon, it is the most frequently reported transfusion-transmitted parasitic infection in the US.
At present, there is no FDA guidance for the testing of donor samples for Babesia. However, the FDA is planning to issue a draft guidance later this year that will include recommendations for reducing the risk of transfusion-transmitted babesiosis.
The US Food and Drug Administration (FDA) has approved the first tests to screen blood donors for Babesia parasites.
The Imugen Babesia microti Arrayed Fluorescent Immunoassay (AFIA) is approved for the detection of antibodies to Babesia microti in plasma samples, and the Imugen Babesia microti Nucleic Acid Test (NAT) is approved for the detection of Babesia microti DNA in whole blood samples.
These tests are intended to be used on samples from volunteer donors of whole blood and blood components as well as living organ and tissue donors.
The tests are not intended for use in the diagnosis of babesiosis infections.
The approval of the Imugen Babesia microti AFIA and NAT tests was granted to Oxford Immunotec, Inc. Both assays are in-house tests that can only be performed at the Norwood, Massachusetts facility.
The applications for the tests were granted priority review. The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products expected to significantly improve the safety or effectiveness of treating, diagnosing, or preventing a serious condition.
“While babesiosis is both preventable and treatable, until today, there was no way to screen for infections amongst blood donors,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research.
“Today’s actions represent the first approvals of Babesia detection tests for use in screening donors of whole blood and blood components, and other living donors.”
About babesiosis
Babesiosis is caused by Babesia parasites that are transmitted by Ixodes scapularis ticks, also known as blacklegged or deer ticks. Babesia microti is the main species of parasite that causes infection in the US.
There are about 1000 to 2000 cases of babesiosis reported in the US each year, with the majority reported from states in the Northeast and upper Midwest.
Most people infected with Babesia microti do not have symptoms and are never diagnosed. Some people develop flu-like symptoms, such as fever, headache, and body aches.
For certain people, especially those with a weak immune system, babesiosis can be a severe, life-threatening disease. And although blood-borne transmission of babesiosis is thought to be uncommon, it is the most frequently reported transfusion-transmitted parasitic infection in the US.
At present, there is no FDA guidance for the testing of donor samples for Babesia. However, the FDA is planning to issue a draft guidance later this year that will include recommendations for reducing the risk of transfusion-transmitted babesiosis.
Drug nets orphan designation for beta-thalassemia
The US Food and Drug Administration (FDA) has granted orphan drug designation to PTG-300, a subcutaneous injectable hepcidin mimetic, for the treatment of beta-thalassemia.
Protagonist Therapeutics, the company developing PTG-300, recently completed a phase 1 trial of the drug.
In this study, healthy volunteers treated with PTG-300 achieved dose-related and sustained reductions in serum iron levels.
In addition, PTG-300 was considered well tolerated, producing no serious adverse events or dose-limiting toxicities.
Protagonist Therapeutics intends to initiate a global clinical trial of PTG-300 in patients with beta-thalassemia following upcoming meetings with the FDA and European Medicines Agency.
“Beta-thalassemia is a rare genetic blood disorder that is characterized by impaired red blood cell production that can result in life-threatening chronic anemia, usually requiring regular and life-long blood transfusions for survival,” said David Y. Liu, PhD, chief scientific officer and head of research and development at Protagonist Therapeutics.
“Over time, these transfusions can lead to excessive iron levels in the body, which can be toxic and consequently lead to end-stage damage to vital organs such as the liver and the heart. As a hepcidin mimetic, PTG-300 is designed to help reduce these excessive iron levels, and, thereby, it may lead to improvements in anemia and decreased need for blood transfusions and chelation therapy.”
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to PTG-300, a subcutaneous injectable hepcidin mimetic, for the treatment of beta-thalassemia.
Protagonist Therapeutics, the company developing PTG-300, recently completed a phase 1 trial of the drug.
In this study, healthy volunteers treated with PTG-300 achieved dose-related and sustained reductions in serum iron levels.
In addition, PTG-300 was considered well tolerated, producing no serious adverse events or dose-limiting toxicities.
Protagonist Therapeutics intends to initiate a global clinical trial of PTG-300 in patients with beta-thalassemia following upcoming meetings with the FDA and European Medicines Agency.
“Beta-thalassemia is a rare genetic blood disorder that is characterized by impaired red blood cell production that can result in life-threatening chronic anemia, usually requiring regular and life-long blood transfusions for survival,” said David Y. Liu, PhD, chief scientific officer and head of research and development at Protagonist Therapeutics.
“Over time, these transfusions can lead to excessive iron levels in the body, which can be toxic and consequently lead to end-stage damage to vital organs such as the liver and the heart. As a hepcidin mimetic, PTG-300 is designed to help reduce these excessive iron levels, and, thereby, it may lead to improvements in anemia and decreased need for blood transfusions and chelation therapy.”
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to PTG-300, a subcutaneous injectable hepcidin mimetic, for the treatment of beta-thalassemia.
Protagonist Therapeutics, the company developing PTG-300, recently completed a phase 1 trial of the drug.
In this study, healthy volunteers treated with PTG-300 achieved dose-related and sustained reductions in serum iron levels.
In addition, PTG-300 was considered well tolerated, producing no serious adverse events or dose-limiting toxicities.
Protagonist Therapeutics intends to initiate a global clinical trial of PTG-300 in patients with beta-thalassemia following upcoming meetings with the FDA and European Medicines Agency.
“Beta-thalassemia is a rare genetic blood disorder that is characterized by impaired red blood cell production that can result in life-threatening chronic anemia, usually requiring regular and life-long blood transfusions for survival,” said David Y. Liu, PhD, chief scientific officer and head of research and development at Protagonist Therapeutics.
“Over time, these transfusions can lead to excessive iron levels in the body, which can be toxic and consequently lead to end-stage damage to vital organs such as the liver and the heart. As a hepcidin mimetic, PTG-300 is designed to help reduce these excessive iron levels, and, thereby, it may lead to improvements in anemia and decreased need for blood transfusions and chelation therapy.”
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
FDA approves label update for nivolumab
The US Food and Drug Administration (FDA) has updated the label for nivolumab (Opdivo®) to include new dosing and administration information.
Nivolumab can now be given at 480 mg infused every 4 weeks for most approved indications, in addition to the previously approved dosing schedule of 240 mg every 2 weeks.
The FDA also approved a shorter 30-minute infusion across all approved indications of nivolumab.
The 480 mg dose option can be used for nearly all approved indications of nivolumab. The exceptions are patients with microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer.
Nivolumab is FDA-approved for the following indications:
- To treat adults with classical Hodgkin lymphoma that has relapsed or progressed after autologous hematopoietic stem cell transplant (HSCT) and brentuximab vedotin or after 3 or more lines of systemic therapy that includes autologous HSCT.
- As monotherapy for patients with BRAF V600 mutation-positive unresectable or metastatic melanoma as well as BRAF V600 wild-type unresectable or metastatic melanoma.
- In combination with ipilimumab for the treatment of patients with unresectable or metastatic melanoma.
- To treat patients with metastatic non-small cell lung cancer with progression on or after platinum-based chemotherapy. Patients with EGFR or ALK genomic tumor aberrations should have disease progression on FDA-approved therapy for these aberrations prior to receiving nivolumab.
- For patients with advanced renal cell carcinoma who have received prior anti-angiogenic therapy.
- To treat patients with recurrent or metastatic squamous cell carcinoma of the head and neck with disease progression on or after platinum-based therapy.
- For patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or after platinum-containing chemotherapy or have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
- To treat adult and pediatric (12 years and older) patients with microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer that has progressed following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
- For patients with hepatocellular carcinoma who have been previously treated with sorafenib.
- For the adjuvant treatment of patients with melanoma with involvement of lymph nodes or metastatic disease who have undergone complete resection.
The US Food and Drug Administration (FDA) has updated the label for nivolumab (Opdivo®) to include new dosing and administration information.
Nivolumab can now be given at 480 mg infused every 4 weeks for most approved indications, in addition to the previously approved dosing schedule of 240 mg every 2 weeks.
The FDA also approved a shorter 30-minute infusion across all approved indications of nivolumab.
The 480 mg dose option can be used for nearly all approved indications of nivolumab. The exceptions are patients with microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer.
Nivolumab is FDA-approved for the following indications:
- To treat adults with classical Hodgkin lymphoma that has relapsed or progressed after autologous hematopoietic stem cell transplant (HSCT) and brentuximab vedotin or after 3 or more lines of systemic therapy that includes autologous HSCT.
- As monotherapy for patients with BRAF V600 mutation-positive unresectable or metastatic melanoma as well as BRAF V600 wild-type unresectable or metastatic melanoma.
- In combination with ipilimumab for the treatment of patients with unresectable or metastatic melanoma.
- To treat patients with metastatic non-small cell lung cancer with progression on or after platinum-based chemotherapy. Patients with EGFR or ALK genomic tumor aberrations should have disease progression on FDA-approved therapy for these aberrations prior to receiving nivolumab.
- For patients with advanced renal cell carcinoma who have received prior anti-angiogenic therapy.
- To treat patients with recurrent or metastatic squamous cell carcinoma of the head and neck with disease progression on or after platinum-based therapy.
- For patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or after platinum-containing chemotherapy or have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
- To treat adult and pediatric (12 years and older) patients with microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer that has progressed following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
- For patients with hepatocellular carcinoma who have been previously treated with sorafenib.
- For the adjuvant treatment of patients with melanoma with involvement of lymph nodes or metastatic disease who have undergone complete resection.
The US Food and Drug Administration (FDA) has updated the label for nivolumab (Opdivo®) to include new dosing and administration information.
Nivolumab can now be given at 480 mg infused every 4 weeks for most approved indications, in addition to the previously approved dosing schedule of 240 mg every 2 weeks.
The FDA also approved a shorter 30-minute infusion across all approved indications of nivolumab.
The 480 mg dose option can be used for nearly all approved indications of nivolumab. The exceptions are patients with microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer.
Nivolumab is FDA-approved for the following indications:
- To treat adults with classical Hodgkin lymphoma that has relapsed or progressed after autologous hematopoietic stem cell transplant (HSCT) and brentuximab vedotin or after 3 or more lines of systemic therapy that includes autologous HSCT.
- As monotherapy for patients with BRAF V600 mutation-positive unresectable or metastatic melanoma as well as BRAF V600 wild-type unresectable or metastatic melanoma.
- In combination with ipilimumab for the treatment of patients with unresectable or metastatic melanoma.
- To treat patients with metastatic non-small cell lung cancer with progression on or after platinum-based chemotherapy. Patients with EGFR or ALK genomic tumor aberrations should have disease progression on FDA-approved therapy for these aberrations prior to receiving nivolumab.
- For patients with advanced renal cell carcinoma who have received prior anti-angiogenic therapy.
- To treat patients with recurrent or metastatic squamous cell carcinoma of the head and neck with disease progression on or after platinum-based therapy.
- For patients with locally advanced or metastatic urothelial carcinoma who have disease progression during or after platinum-containing chemotherapy or have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
- To treat adult and pediatric (12 years and older) patients with microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer that has progressed following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
- For patients with hepatocellular carcinoma who have been previously treated with sorafenib.
- For the adjuvant treatment of patients with melanoma with involvement of lymph nodes or metastatic disease who have undergone complete resection.
Drug could improve treatment of CML, team says
A microRNA-targeting drug could improve the effectiveness of tyrosine kinase inhibitors (TKIs) against chronic myelogenous leukemia (CML), according to preclinical research published in Nature Medicine.
The drug, miristen, targets miR-126, a microRNA expressed in leukemia stem cells (LSCs).
Researchers found that miristen “enhanced the anti-leukemic effects of TKI treatment” in mouse models of CML and “strongly diminished LSC leukemia-initiating capacity.”
“This could be a major breakthrough for people who are in remission for CML because there is always a concern that the disease will come back if TKI treatment is stopped,” said study author Bin Zhang, PhD, of City of Hope Medical Center in Duarte, California.
“Miristen could be the drug that sends the disease into permanent remission.”
For this study, Dr Zhang and her colleagues tested miristen alone and in combination with the TKI nilotinib in mouse models of CML.
The best results were seen in mice treated with miristen and nilotinib. Transplantation of bone marrow cells collected from mice treated with miristen and nilotinib resulted in no sign of leukemia in the healthy recipient mice, meaning all LSCs were eliminated.
The researchers believe miristen simply makes TKIs more effective in killing LSCs. The team also thinks they have discovered the key to the treatment’s success.
The researchers found that endothelial cells in the blood vessels of the bone marrow contain high levels of miR-126. These endothelial cells transfer miR-126 to LSCs, essentially feeding the leukemia what it needs to survive and grow.
The team hypothesized that to eliminate CML, miristen had to lower miR-126 in both the LSCs and the endothelial cells. Testing proved this theory correct.
“What we have discovered is how the microenvironment surrounding the leukemia stem cells supports them and how you need to target miR-126 in the leukemia stem cells and the microenvironment to completely eradicate the disease,” said study author Guido Marcucci, MD, of City of Hope.
“Our current study showed these findings may also apply to other types of leukemia.”
A microRNA-targeting drug could improve the effectiveness of tyrosine kinase inhibitors (TKIs) against chronic myelogenous leukemia (CML), according to preclinical research published in Nature Medicine.
The drug, miristen, targets miR-126, a microRNA expressed in leukemia stem cells (LSCs).
Researchers found that miristen “enhanced the anti-leukemic effects of TKI treatment” in mouse models of CML and “strongly diminished LSC leukemia-initiating capacity.”
“This could be a major breakthrough for people who are in remission for CML because there is always a concern that the disease will come back if TKI treatment is stopped,” said study author Bin Zhang, PhD, of City of Hope Medical Center in Duarte, California.
“Miristen could be the drug that sends the disease into permanent remission.”
For this study, Dr Zhang and her colleagues tested miristen alone and in combination with the TKI nilotinib in mouse models of CML.
The best results were seen in mice treated with miristen and nilotinib. Transplantation of bone marrow cells collected from mice treated with miristen and nilotinib resulted in no sign of leukemia in the healthy recipient mice, meaning all LSCs were eliminated.
The researchers believe miristen simply makes TKIs more effective in killing LSCs. The team also thinks they have discovered the key to the treatment’s success.
The researchers found that endothelial cells in the blood vessels of the bone marrow contain high levels of miR-126. These endothelial cells transfer miR-126 to LSCs, essentially feeding the leukemia what it needs to survive and grow.
The team hypothesized that to eliminate CML, miristen had to lower miR-126 in both the LSCs and the endothelial cells. Testing proved this theory correct.
“What we have discovered is how the microenvironment surrounding the leukemia stem cells supports them and how you need to target miR-126 in the leukemia stem cells and the microenvironment to completely eradicate the disease,” said study author Guido Marcucci, MD, of City of Hope.
“Our current study showed these findings may also apply to other types of leukemia.”
A microRNA-targeting drug could improve the effectiveness of tyrosine kinase inhibitors (TKIs) against chronic myelogenous leukemia (CML), according to preclinical research published in Nature Medicine.
The drug, miristen, targets miR-126, a microRNA expressed in leukemia stem cells (LSCs).
Researchers found that miristen “enhanced the anti-leukemic effects of TKI treatment” in mouse models of CML and “strongly diminished LSC leukemia-initiating capacity.”
“This could be a major breakthrough for people who are in remission for CML because there is always a concern that the disease will come back if TKI treatment is stopped,” said study author Bin Zhang, PhD, of City of Hope Medical Center in Duarte, California.
“Miristen could be the drug that sends the disease into permanent remission.”
For this study, Dr Zhang and her colleagues tested miristen alone and in combination with the TKI nilotinib in mouse models of CML.
The best results were seen in mice treated with miristen and nilotinib. Transplantation of bone marrow cells collected from mice treated with miristen and nilotinib resulted in no sign of leukemia in the healthy recipient mice, meaning all LSCs were eliminated.
The researchers believe miristen simply makes TKIs more effective in killing LSCs. The team also thinks they have discovered the key to the treatment’s success.
The researchers found that endothelial cells in the blood vessels of the bone marrow contain high levels of miR-126. These endothelial cells transfer miR-126 to LSCs, essentially feeding the leukemia what it needs to survive and grow.
The team hypothesized that to eliminate CML, miristen had to lower miR-126 in both the LSCs and the endothelial cells. Testing proved this theory correct.
“What we have discovered is how the microenvironment surrounding the leukemia stem cells supports them and how you need to target miR-126 in the leukemia stem cells and the microenvironment to completely eradicate the disease,” said study author Guido Marcucci, MD, of City of Hope.
“Our current study showed these findings may also apply to other types of leukemia.”
Giving patients control of their healthcare data
The US Centers for Medicare & Medicaid Services (CMS) has announced new initiatives designed to give patients control of their healthcare data.
One initiative, MyHealthEData, is intended to “break down the barriers” that prevent patients from having electronic access to, and control of, their own health records, according to CMS Administrator Seema Verma.
The other initiative, Medicare’s Blue Button 2.0, is a new way for Medicare beneficiaries to access and share their personal health data in a universal digital format.
Verma discussed these programs and other changes CMS is making in a speech at the HIMSS18 Conference in Las Vegas.
MyHealthEData
The Trump Administration is launching MyHealthEData, a government-wide initiative intended to give patients electronic access to their healthcare data and allow patients to take that data with them from healthcare provider to healthcare provider.
The idea is that patients will be able to choose the provider that best meets their needs and give that provider secure access to their data.
“MyHealthEData makes it clear that patients should have access and control to share their data with whomever they want, making the patient the center of our healthcare system,” Verma said.
“Patients need to be able to control their information and know that it’s secure and private. Having access to their medical information will help them make decisions about their care and have a better understanding of their health.”
The MyHealthEData initiative is led by the White House Office of American Innovation, with participation from the Department of Health and Human Services and its CMS, Office of the National Coordinator for Health Information Technology, and National Institutes of Health, as well as the Department of Veterans Affairs.
Blue Button 2.0
Verma said Medicare’s Blue Button 2.0 will enable patients who participate in the traditional Medicare program to connect their claims data to the secure applications, providers, services, and research programs they trust.
“Beneficiaries will maintain complete control in how and when their data is used . . .,” Verma said.
In addition, Medicare’s Blue Button 2.0 is expected to foster increased competition among technology innovators to serve Medicare patients and their caregivers. More than 100 organizations have signed on to use Medicare’s Blue Button 2.0 to develop applications that will provide new tools to help patients manage their health.
“CMS serves more than 130 million beneficiaries through our programs, which means we are uniquely positioned to transform how important healthcare data is shared between patients and their doctors,” Verma said.
“Today, we are calling on private health plans to join us in sharing their data with patients because enabling patients to control their Medicare data so that they can quickly obtain and share it is critical to creating more patient empowerment.”
Additional changes
Verma announced that CMS intends to overhaul its Electronic Health Record (EHR) Incentive Programs to refocus them on interoperability and reduce the time and cost required of providers to comply with the programs’ requirements.
Verma also noted that CMS has implemented laws regarding information blocking, a practice in which providers prevent patients from accessing their data. Under some CMS programs, hospitals and clinicians must show they have not engaged in information-blocking activities.
Other ways in which CMS plans to empower patients with data include:
- Requiring providers to update their systems to ensure data sharing
- Requiring that patients’ data follow them after they are discharged from the hospital
- Working to streamline documentation and billing requirements for providers to allow doctors to spend more time with their patients
- Working to reduce the incidence of unnecessary and duplicative testing, which occurs as a result of providers not sharing data.
The US Centers for Medicare & Medicaid Services (CMS) has announced new initiatives designed to give patients control of their healthcare data.
One initiative, MyHealthEData, is intended to “break down the barriers” that prevent patients from having electronic access to, and control of, their own health records, according to CMS Administrator Seema Verma.
The other initiative, Medicare’s Blue Button 2.0, is a new way for Medicare beneficiaries to access and share their personal health data in a universal digital format.
Verma discussed these programs and other changes CMS is making in a speech at the HIMSS18 Conference in Las Vegas.
MyHealthEData
The Trump Administration is launching MyHealthEData, a government-wide initiative intended to give patients electronic access to their healthcare data and allow patients to take that data with them from healthcare provider to healthcare provider.
The idea is that patients will be able to choose the provider that best meets their needs and give that provider secure access to their data.
“MyHealthEData makes it clear that patients should have access and control to share their data with whomever they want, making the patient the center of our healthcare system,” Verma said.
“Patients need to be able to control their information and know that it’s secure and private. Having access to their medical information will help them make decisions about their care and have a better understanding of their health.”
The MyHealthEData initiative is led by the White House Office of American Innovation, with participation from the Department of Health and Human Services and its CMS, Office of the National Coordinator for Health Information Technology, and National Institutes of Health, as well as the Department of Veterans Affairs.
Blue Button 2.0
Verma said Medicare’s Blue Button 2.0 will enable patients who participate in the traditional Medicare program to connect their claims data to the secure applications, providers, services, and research programs they trust.
“Beneficiaries will maintain complete control in how and when their data is used . . .,” Verma said.
In addition, Medicare’s Blue Button 2.0 is expected to foster increased competition among technology innovators to serve Medicare patients and their caregivers. More than 100 organizations have signed on to use Medicare’s Blue Button 2.0 to develop applications that will provide new tools to help patients manage their health.
“CMS serves more than 130 million beneficiaries through our programs, which means we are uniquely positioned to transform how important healthcare data is shared between patients and their doctors,” Verma said.
“Today, we are calling on private health plans to join us in sharing their data with patients because enabling patients to control their Medicare data so that they can quickly obtain and share it is critical to creating more patient empowerment.”
Additional changes
Verma announced that CMS intends to overhaul its Electronic Health Record (EHR) Incentive Programs to refocus them on interoperability and reduce the time and cost required of providers to comply with the programs’ requirements.
Verma also noted that CMS has implemented laws regarding information blocking, a practice in which providers prevent patients from accessing their data. Under some CMS programs, hospitals and clinicians must show they have not engaged in information-blocking activities.
Other ways in which CMS plans to empower patients with data include:
- Requiring providers to update their systems to ensure data sharing
- Requiring that patients’ data follow them after they are discharged from the hospital
- Working to streamline documentation and billing requirements for providers to allow doctors to spend more time with their patients
- Working to reduce the incidence of unnecessary and duplicative testing, which occurs as a result of providers not sharing data.
The US Centers for Medicare & Medicaid Services (CMS) has announced new initiatives designed to give patients control of their healthcare data.
One initiative, MyHealthEData, is intended to “break down the barriers” that prevent patients from having electronic access to, and control of, their own health records, according to CMS Administrator Seema Verma.
The other initiative, Medicare’s Blue Button 2.0, is a new way for Medicare beneficiaries to access and share their personal health data in a universal digital format.
Verma discussed these programs and other changes CMS is making in a speech at the HIMSS18 Conference in Las Vegas.
MyHealthEData
The Trump Administration is launching MyHealthEData, a government-wide initiative intended to give patients electronic access to their healthcare data and allow patients to take that data with them from healthcare provider to healthcare provider.
The idea is that patients will be able to choose the provider that best meets their needs and give that provider secure access to their data.
“MyHealthEData makes it clear that patients should have access and control to share their data with whomever they want, making the patient the center of our healthcare system,” Verma said.
“Patients need to be able to control their information and know that it’s secure and private. Having access to their medical information will help them make decisions about their care and have a better understanding of their health.”
The MyHealthEData initiative is led by the White House Office of American Innovation, with participation from the Department of Health and Human Services and its CMS, Office of the National Coordinator for Health Information Technology, and National Institutes of Health, as well as the Department of Veterans Affairs.
Blue Button 2.0
Verma said Medicare’s Blue Button 2.0 will enable patients who participate in the traditional Medicare program to connect their claims data to the secure applications, providers, services, and research programs they trust.
“Beneficiaries will maintain complete control in how and when their data is used . . .,” Verma said.
In addition, Medicare’s Blue Button 2.0 is expected to foster increased competition among technology innovators to serve Medicare patients and their caregivers. More than 100 organizations have signed on to use Medicare’s Blue Button 2.0 to develop applications that will provide new tools to help patients manage their health.
“CMS serves more than 130 million beneficiaries through our programs, which means we are uniquely positioned to transform how important healthcare data is shared between patients and their doctors,” Verma said.
“Today, we are calling on private health plans to join us in sharing their data with patients because enabling patients to control their Medicare data so that they can quickly obtain and share it is critical to creating more patient empowerment.”
Additional changes
Verma announced that CMS intends to overhaul its Electronic Health Record (EHR) Incentive Programs to refocus them on interoperability and reduce the time and cost required of providers to comply with the programs’ requirements.
Verma also noted that CMS has implemented laws regarding information blocking, a practice in which providers prevent patients from accessing their data. Under some CMS programs, hospitals and clinicians must show they have not engaged in information-blocking activities.
Other ways in which CMS plans to empower patients with data include:
- Requiring providers to update their systems to ensure data sharing
- Requiring that patients’ data follow them after they are discharged from the hospital
- Working to streamline documentation and billing requirements for providers to allow doctors to spend more time with their patients
- Working to reduce the incidence of unnecessary and duplicative testing, which occurs as a result of providers not sharing data.
Method may predict relapse at BCP-ALL diagnosis
Researchers say they have developed a technique that can help them determine, at diagnosis, whether children with B-cell precursor acute lymphoblastic leukemia (BCP-ALL) will relapse after treatment.
The method involves examining individual leukemia cells using mass cytometry.
In looking at the cells’ stage of development and signaling behavior, the researchers were able to identify a subset of malignant cells that predispose a patient to relapse.
The team described this method, which they termed “developmentally dependent predictor of relapse (DDPR),” in Nature Medicine.
Prior research suggested relapse may be driven by treatment-resistant cells that are present from the beginning of disease development.
“We wondered, can we identify those cells at the time the patient first presents to the clinic, and can we treat patients with a specific therapy to target them?” said study author Kara Davis, DO, of Stanford University in California.
Dr Davis and her colleagues used mass cytometry to analyze diagnostic bone marrow samples from 60 patients with BCP-ALL.
To pinpoint the problematic cells among the millions of cells in each patient’s sample, the researchers had to figure out how to organize the data.
“Every patient has vastly different features to their cancer,” Dr Davis said, “and we had to ask, ‘Is there any common thread between them?’”
The solution, the researchers found, was to match BCP-ALL cells and healthy B cells according to their developmental states, comparing the leukemic cells to the healthy cells.
The comparison revealed 6 features of leukemic cell populations that were associated with relapse.
Broadly, the features suggested that pro-BII cells with activated mTOR signaling were associated with relapse, as were pre-BI cells with activated and unresponsive pre-B-cell receptor signaling.
“We do not understand the mechanisms by which malignant cells from the pro-BII and pre-BI stages of development resist treatment,” Dr Davis noted.
However, she and her colleagues were able to show the leukemic cell features identified by DDPR could predict relapse in the BCP-ALL patients.
Of the 60 patients analyzed, there were 54 with at least 3 years of follow-up. The researchers divided these patients into a training cohort (n=44) and a validation cohort (n=10).
The team used an integrated cumulative/dynamic area under the curve (iAUC) and a C-statistic to assess DDPR performance in both cohorts.
In the training cohort, DDPR had an iAUC value of 0.92 and a C-statistic of 0.87. In the validation cohort, DDPR had an iAUC value of 0.85 and a C-statistic of 0.87.
The researchers also said DDPR “performed well” in predicting relapse-free survival in a retrospective analysis of both cohorts (P = 2.8 × 10−7).
Now, the researchers plan to validate DDPR in a larger number of patients and evaluate whether the same general approach could predict relapse in other cancers.
Researchers say they have developed a technique that can help them determine, at diagnosis, whether children with B-cell precursor acute lymphoblastic leukemia (BCP-ALL) will relapse after treatment.
The method involves examining individual leukemia cells using mass cytometry.
In looking at the cells’ stage of development and signaling behavior, the researchers were able to identify a subset of malignant cells that predispose a patient to relapse.
The team described this method, which they termed “developmentally dependent predictor of relapse (DDPR),” in Nature Medicine.
Prior research suggested relapse may be driven by treatment-resistant cells that are present from the beginning of disease development.
“We wondered, can we identify those cells at the time the patient first presents to the clinic, and can we treat patients with a specific therapy to target them?” said study author Kara Davis, DO, of Stanford University in California.
Dr Davis and her colleagues used mass cytometry to analyze diagnostic bone marrow samples from 60 patients with BCP-ALL.
To pinpoint the problematic cells among the millions of cells in each patient’s sample, the researchers had to figure out how to organize the data.
“Every patient has vastly different features to their cancer,” Dr Davis said, “and we had to ask, ‘Is there any common thread between them?’”
The solution, the researchers found, was to match BCP-ALL cells and healthy B cells according to their developmental states, comparing the leukemic cells to the healthy cells.
The comparison revealed 6 features of leukemic cell populations that were associated with relapse.
Broadly, the features suggested that pro-BII cells with activated mTOR signaling were associated with relapse, as were pre-BI cells with activated and unresponsive pre-B-cell receptor signaling.
“We do not understand the mechanisms by which malignant cells from the pro-BII and pre-BI stages of development resist treatment,” Dr Davis noted.
However, she and her colleagues were able to show the leukemic cell features identified by DDPR could predict relapse in the BCP-ALL patients.
Of the 60 patients analyzed, there were 54 with at least 3 years of follow-up. The researchers divided these patients into a training cohort (n=44) and a validation cohort (n=10).
The team used an integrated cumulative/dynamic area under the curve (iAUC) and a C-statistic to assess DDPR performance in both cohorts.
In the training cohort, DDPR had an iAUC value of 0.92 and a C-statistic of 0.87. In the validation cohort, DDPR had an iAUC value of 0.85 and a C-statistic of 0.87.
The researchers also said DDPR “performed well” in predicting relapse-free survival in a retrospective analysis of both cohorts (P = 2.8 × 10−7).
Now, the researchers plan to validate DDPR in a larger number of patients and evaluate whether the same general approach could predict relapse in other cancers.
Researchers say they have developed a technique that can help them determine, at diagnosis, whether children with B-cell precursor acute lymphoblastic leukemia (BCP-ALL) will relapse after treatment.
The method involves examining individual leukemia cells using mass cytometry.
In looking at the cells’ stage of development and signaling behavior, the researchers were able to identify a subset of malignant cells that predispose a patient to relapse.
The team described this method, which they termed “developmentally dependent predictor of relapse (DDPR),” in Nature Medicine.
Prior research suggested relapse may be driven by treatment-resistant cells that are present from the beginning of disease development.
“We wondered, can we identify those cells at the time the patient first presents to the clinic, and can we treat patients with a specific therapy to target them?” said study author Kara Davis, DO, of Stanford University in California.
Dr Davis and her colleagues used mass cytometry to analyze diagnostic bone marrow samples from 60 patients with BCP-ALL.
To pinpoint the problematic cells among the millions of cells in each patient’s sample, the researchers had to figure out how to organize the data.
“Every patient has vastly different features to their cancer,” Dr Davis said, “and we had to ask, ‘Is there any common thread between them?’”
The solution, the researchers found, was to match BCP-ALL cells and healthy B cells according to their developmental states, comparing the leukemic cells to the healthy cells.
The comparison revealed 6 features of leukemic cell populations that were associated with relapse.
Broadly, the features suggested that pro-BII cells with activated mTOR signaling were associated with relapse, as were pre-BI cells with activated and unresponsive pre-B-cell receptor signaling.
“We do not understand the mechanisms by which malignant cells from the pro-BII and pre-BI stages of development resist treatment,” Dr Davis noted.
However, she and her colleagues were able to show the leukemic cell features identified by DDPR could predict relapse in the BCP-ALL patients.
Of the 60 patients analyzed, there were 54 with at least 3 years of follow-up. The researchers divided these patients into a training cohort (n=44) and a validation cohort (n=10).
The team used an integrated cumulative/dynamic area under the curve (iAUC) and a C-statistic to assess DDPR performance in both cohorts.
In the training cohort, DDPR had an iAUC value of 0.92 and a C-statistic of 0.87. In the validation cohort, DDPR had an iAUC value of 0.85 and a C-statistic of 0.87.
The researchers also said DDPR “performed well” in predicting relapse-free survival in a retrospective analysis of both cohorts (P = 2.8 × 10−7).
Now, the researchers plan to validate DDPR in a larger number of patients and evaluate whether the same general approach could predict relapse in other cancers.
PK dosing software available in US
Pharmacokinetic (PK) dosing software intended for use in patients with hemophilia A is now available in the US.
This free, web-based, prescription software—myPKFiT for ADVATE—is intended to aid healthcare professionals in personalizing the dose and schedule of ADVATE, a full-length recombinant factor VIII product.
The software was cleared by the US Food and Drug Administration (FDA) for use in hemophilia A patients age 16 and older who weigh at least 45 kg and are receiving prophylaxis with ADVATE.
The myPKFiT software generates ADVATE dosage amount and frequency recommendations using a patient’s age and body weight information, as well as local laboratory factor VIII one-stage clotting activity measurements of sparse samples collected from the patient.
A minimum of 2 sparse sampling points are required at the recommended 3 to 4 hours (± 30 minutes) and at 24 to 32 hours (±1 hour) post-infusion.
The software output may be used to guide ADVATE use to maintain factor VIII activity levels at or above a user-specified minimum of 1% to 3% above natural baseline, in accordance with the FDA-approved dosing recommendations for ADVATE.
myPKFiT should only be used to evaluate prophylactic dosing regimens for hemophilia A patients treated with ADVATE.
The software should not be used for patients who have developed neutralizing antibodies to factor VIII products and is not indicated for use in patients with von Willebrand disease.
“A version of myPKFiT has already been widely adopted in Europe since 2014, and we’ve seen how important it has been in helping physicians develop personalized dosing regimens tailored to the specific needs of their patients,” said Andreas Busch, global head of research and development at Shire, the company behind myPKFiT for ADVATE.
“As part of our commitment to precision medicine, we are pleased to bring this innovative application to physicians and patients in the United States.”
More information on the myPKFiT software is available on the ADVATE website and the myPKFiT site.
Pharmacokinetic (PK) dosing software intended for use in patients with hemophilia A is now available in the US.
This free, web-based, prescription software—myPKFiT for ADVATE—is intended to aid healthcare professionals in personalizing the dose and schedule of ADVATE, a full-length recombinant factor VIII product.
The software was cleared by the US Food and Drug Administration (FDA) for use in hemophilia A patients age 16 and older who weigh at least 45 kg and are receiving prophylaxis with ADVATE.
The myPKFiT software generates ADVATE dosage amount and frequency recommendations using a patient’s age and body weight information, as well as local laboratory factor VIII one-stage clotting activity measurements of sparse samples collected from the patient.
A minimum of 2 sparse sampling points are required at the recommended 3 to 4 hours (± 30 minutes) and at 24 to 32 hours (±1 hour) post-infusion.
The software output may be used to guide ADVATE use to maintain factor VIII activity levels at or above a user-specified minimum of 1% to 3% above natural baseline, in accordance with the FDA-approved dosing recommendations for ADVATE.
myPKFiT should only be used to evaluate prophylactic dosing regimens for hemophilia A patients treated with ADVATE.
The software should not be used for patients who have developed neutralizing antibodies to factor VIII products and is not indicated for use in patients with von Willebrand disease.
“A version of myPKFiT has already been widely adopted in Europe since 2014, and we’ve seen how important it has been in helping physicians develop personalized dosing regimens tailored to the specific needs of their patients,” said Andreas Busch, global head of research and development at Shire, the company behind myPKFiT for ADVATE.
“As part of our commitment to precision medicine, we are pleased to bring this innovative application to physicians and patients in the United States.”
More information on the myPKFiT software is available on the ADVATE website and the myPKFiT site.
Pharmacokinetic (PK) dosing software intended for use in patients with hemophilia A is now available in the US.
This free, web-based, prescription software—myPKFiT for ADVATE—is intended to aid healthcare professionals in personalizing the dose and schedule of ADVATE, a full-length recombinant factor VIII product.
The software was cleared by the US Food and Drug Administration (FDA) for use in hemophilia A patients age 16 and older who weigh at least 45 kg and are receiving prophylaxis with ADVATE.
The myPKFiT software generates ADVATE dosage amount and frequency recommendations using a patient’s age and body weight information, as well as local laboratory factor VIII one-stage clotting activity measurements of sparse samples collected from the patient.
A minimum of 2 sparse sampling points are required at the recommended 3 to 4 hours (± 30 minutes) and at 24 to 32 hours (±1 hour) post-infusion.
The software output may be used to guide ADVATE use to maintain factor VIII activity levels at or above a user-specified minimum of 1% to 3% above natural baseline, in accordance with the FDA-approved dosing recommendations for ADVATE.
myPKFiT should only be used to evaluate prophylactic dosing regimens for hemophilia A patients treated with ADVATE.
The software should not be used for patients who have developed neutralizing antibodies to factor VIII products and is not indicated for use in patients with von Willebrand disease.
“A version of myPKFiT has already been widely adopted in Europe since 2014, and we’ve seen how important it has been in helping physicians develop personalized dosing regimens tailored to the specific needs of their patients,” said Andreas Busch, global head of research and development at Shire, the company behind myPKFiT for ADVATE.
“As part of our commitment to precision medicine, we are pleased to bring this innovative application to physicians and patients in the United States.”
More information on the myPKFiT software is available on the ADVATE website and the myPKFiT site.
Agent can reveal HSC engraftment faster
An imaging agent can safely show engraftment of hematopoietic stem cells (HSCs) just days after transplant, according to research published in The Lancet Haematology.
The agent is 18F-fluorothymidine (18F-FLT), a radio-labeled analogue of thymidine.
Past studies have shown that 18F-FLT is incorporated into HSCs.
With the current study, researchers wanted to determine if 18F-FLT could allow them to safely visualize transplanted HSCs.
Kirsten M. Williams, MD, of Children’s National Health System in Washington, DC, and her colleagues tested 18F-FLT in 23 patients undergoing HSC transplant to treat high-risk hematologic malignancies.
The patients first underwent total body irradiation to destroy their own HSCs and then received donor HSCs.
The patients underwent PET/CT scans 1 day before they were infused with HSCs as well as post-transplant at 5 or 9 days, 28 days, and 1 year.
Results
All patients engrafted, a finding that was reflected in blood tests conducted 2 to 4 weeks after transplant. However, imaging results revealed more details.
“Through the images we took, these patients could see the new cells growing in their bodies,” Dr Williams said. “They loved that.”
The researchers and the patients saw the HSCs take a complex journey as they engrafted.
First, HSCs migrated to the patients’ livers and spleens. Next, the cells went to the thoracic spine, the axial spine, the sternum, and the arms and legs.
By 1 year, most of the HSCs were concentrated in the bones that make up the trunk of the body, including the hip, where most biopsies to assess marrow function take place.
This pathway is the same one HSCs take in the fetus when they first form.
The researchers also found the radiation in 18F-FLT did not adversely affect engraftment.
And imaging could reveal successful engraftment at 5 days post-transplant, “which was up to 20 days before engraftment became clinically evident,” according to the researchers.
Dr Williams and her colleagues believe use of 18F-FLT could potentially help patients avoid bone marrow biopsies or, at the very least, help target those biopsies.
And the agent might be helpful for taking stock of HSCs in conditions such as aplastic anemia.
“What happens with HSCs always has been a mystery,” Dr Williams said. “Now, we can start to open that black box.”
An imaging agent can safely show engraftment of hematopoietic stem cells (HSCs) just days after transplant, according to research published in The Lancet Haematology.
The agent is 18F-fluorothymidine (18F-FLT), a radio-labeled analogue of thymidine.
Past studies have shown that 18F-FLT is incorporated into HSCs.
With the current study, researchers wanted to determine if 18F-FLT could allow them to safely visualize transplanted HSCs.
Kirsten M. Williams, MD, of Children’s National Health System in Washington, DC, and her colleagues tested 18F-FLT in 23 patients undergoing HSC transplant to treat high-risk hematologic malignancies.
The patients first underwent total body irradiation to destroy their own HSCs and then received donor HSCs.
The patients underwent PET/CT scans 1 day before they were infused with HSCs as well as post-transplant at 5 or 9 days, 28 days, and 1 year.
Results
All patients engrafted, a finding that was reflected in blood tests conducted 2 to 4 weeks after transplant. However, imaging results revealed more details.
“Through the images we took, these patients could see the new cells growing in their bodies,” Dr Williams said. “They loved that.”
The researchers and the patients saw the HSCs take a complex journey as they engrafted.
First, HSCs migrated to the patients’ livers and spleens. Next, the cells went to the thoracic spine, the axial spine, the sternum, and the arms and legs.
By 1 year, most of the HSCs were concentrated in the bones that make up the trunk of the body, including the hip, where most biopsies to assess marrow function take place.
This pathway is the same one HSCs take in the fetus when they first form.
The researchers also found the radiation in 18F-FLT did not adversely affect engraftment.
And imaging could reveal successful engraftment at 5 days post-transplant, “which was up to 20 days before engraftment became clinically evident,” according to the researchers.
Dr Williams and her colleagues believe use of 18F-FLT could potentially help patients avoid bone marrow biopsies or, at the very least, help target those biopsies.
And the agent might be helpful for taking stock of HSCs in conditions such as aplastic anemia.
“What happens with HSCs always has been a mystery,” Dr Williams said. “Now, we can start to open that black box.”
An imaging agent can safely show engraftment of hematopoietic stem cells (HSCs) just days after transplant, according to research published in The Lancet Haematology.
The agent is 18F-fluorothymidine (18F-FLT), a radio-labeled analogue of thymidine.
Past studies have shown that 18F-FLT is incorporated into HSCs.
With the current study, researchers wanted to determine if 18F-FLT could allow them to safely visualize transplanted HSCs.
Kirsten M. Williams, MD, of Children’s National Health System in Washington, DC, and her colleagues tested 18F-FLT in 23 patients undergoing HSC transplant to treat high-risk hematologic malignancies.
The patients first underwent total body irradiation to destroy their own HSCs and then received donor HSCs.
The patients underwent PET/CT scans 1 day before they were infused with HSCs as well as post-transplant at 5 or 9 days, 28 days, and 1 year.
Results
All patients engrafted, a finding that was reflected in blood tests conducted 2 to 4 weeks after transplant. However, imaging results revealed more details.
“Through the images we took, these patients could see the new cells growing in their bodies,” Dr Williams said. “They loved that.”
The researchers and the patients saw the HSCs take a complex journey as they engrafted.
First, HSCs migrated to the patients’ livers and spleens. Next, the cells went to the thoracic spine, the axial spine, the sternum, and the arms and legs.
By 1 year, most of the HSCs were concentrated in the bones that make up the trunk of the body, including the hip, where most biopsies to assess marrow function take place.
This pathway is the same one HSCs take in the fetus when they first form.
The researchers also found the radiation in 18F-FLT did not adversely affect engraftment.
And imaging could reveal successful engraftment at 5 days post-transplant, “which was up to 20 days before engraftment became clinically evident,” according to the researchers.
Dr Williams and her colleagues believe use of 18F-FLT could potentially help patients avoid bone marrow biopsies or, at the very least, help target those biopsies.
And the agent might be helpful for taking stock of HSCs in conditions such as aplastic anemia.
“What happens with HSCs always has been a mystery,” Dr Williams said. “Now, we can start to open that black box.”