User login
2020 Update on obstetrics
Attributed to the ancient Greek philosopher Heraclitus, and often quoted in contemporary times, is the expression “the only constant is change.” This sentiment rings true for the field of obstetrics this past year, as several bread-and-butter guidelines for managing common obstetric conditions were either challenged or altered.
The publication of the PROLONG trial called into question the use of intramuscular progesterone for the prevention of preterm birth. Prophylaxis guidelines for group B streptococcal disease were updated, including several significant clinical practice changes. Finally, there was a comprehensive overhaul of the guidelines for hypertensive disorders of pregnancy, which replaced a landmark Task Force document from the American College of Obstetricians and Gynecologists (ACOG) that was published only a few years ago.
Change is constant, and in obstetrics it is vital to keep up with the changing guidelines that result as new data become available for digestion and implementation into everyday clinical practice.
Results from the PROLONG trial may shake up treatment options for recurrent preterm birth
Blackwell SC, Gyamfi-Bannerman C, Biggio JR Jr, et al. 17-OHPC to prevent recurrent preterm birth in singleton gestations (PROLONG study): a multicenter, international, randomized double-blind trial. Am J Perinatol. 2019. doi: 10.1055/s-0039-3400227.
The drug 17 α-hydroxyprogesterone caproate (17-OHPC, or 17P; Makena) was approved by the US Food and Drug Administration (FDA) in 2011 for the prevention of spontaneous preterm birth (PTB) in women with a singleton pregnancy and a history of singleton spontaneous PTB. The results of the trial by Meis and colleagues of 17-OHPC played a major role in achieving that approval, as it demonstrated a 34% reduction in recurrent PTB and a reduction in some neonatal morbidities.1 Following the drug's approval, both ACOG and the Society for Maternal-Fetal Medicine (SMFM) published guidelines recommending progesterone therapy, including 17-OHPC, for the prevention of recurrent spontaneous PTB.2
The FDA approval of 17-OHPC was granted under an accelerated conditional pathway that required a confirmatory trial evaluating efficacy, safety, and long-term infant follow-up to be performed by the sponsor. That trial, Progestin's Role in Optimizing Neonatal Gestation (PROLONG), was started in 2009, and its results were published on October 25, 2019.3
Continue to: Design of the trial...
Design of the trial
PROLONG was a multicenter (93 sites), randomized, placebo-controlled, double-blind study conducted in 9 countries (23% of participants were in the United States, 60% were in Russia and Ukraine). The co-primary outcome was PTB < 35 weeks and a composite neonatal morbidity and mortality index. The primary safety outcome was fetal/early infant death.
The study was designed to have 98% power to detect a 30% reduction in PTB < 35 weeks, and 90% power to detect a 35% reduction in the neonatal composite index. It included 1,708 participants (1,130 were treated with 17-OHPC, and 578 received placebo).
Trial outcomes. There was no difference in PTB < 35 weeks between the 17-OHPC and the placebo groups (11.0% vs 11.5%; relative risk [RR], 0.95; 95% confidence interval [CI], 0.71-1.26). There was no difference in PTB < 32 or < 37 weeks.
The study revealed also that there was no difference between groups in the neonatal composite index (5.6% for 17-OHPC vs 5.0% for placebo; RR, 1.12; 95% CI, 0.68-1.61). In addition, there was no difference in fetal/early infant death between the 17-OHPC and placebo groups (1.7% vs 1.9%; RR, 0.87; 95% CI, 0.4-1.81).
Conclusions. The trial investigators concluded that 17-OHPC did not demonstrate a reduction in recurrent PTB and did not decrease neonatal morbidity.
Study limitations included underpowering and selection bias
The investigators noted that the PTB rate in PROLONG was unexpectedly almost 50% lower than that in the Meis trial, and that therefore the PROLONG trial was underpowered to assess the primary outcomes.
Further, the study populations of the 2 trials were very different: The Meis trial included women at higher baseline risk for PTB (> 1 prior PTB and at least 1 other risk factor for PTB). Additionally, while the PROLONG trial included mostly white (90%), married (90%), nonsmoking women (8% smoked), the Meis trial population was 59% black and 50% married, and 20% were smokers.
The availability and common use of 17-OHPC in the United States likely led to a selection bias for the PROLONG trial population, as the highest-risk patients were most likely already receiving treatment and were therefore excluded from the PROLONG trial.
Society, and FDA, responses to the new data
The results of the PROLONG trial call into question what has become standard practice for patients with a history of spontaneous PTB in the United States. While the safety profile of 17-OHPC has not been cited as a concern, whether or not the drug should be used at all has—as has its current FDA-approved status.
In response to the publication of the PROLONG trial results, ACOG released a Practice Advisory that acknowledged the study's findings but did not alter the current recommendations to continue to offer progesterone for the prevention of preterm birth, upholding ACOG's current Practice Bulletin guidance.2,4 Additional considerations for offering 17-OHPC use include the patients' preferences, available resources, and the setting for the intervention.
SMFM's response was more specific, stating that it is reasonable to continue to use 17-OHPC in high-risk patient populations consistent with those in the Meis trial.5 In the rest of the general population at risk for recurrent PTB, SMFM recommends that, due to uncertain benefit with 17-OHPC, the high cost, patient discomfort, and increased visits should be taken into account.
Four days after the publication of the PROLONG study, the FDA Bone, Reproductive, and Urologic Drugs Advisory Committee voted 9-7 to withdraw approval for 17-OHPC.6 In response, SMFM released a statement supporting continued access to 17-OHPC.7 The FDA's final decision on the status of the drug is expected within the next several months from this writing.
17-OHPC continues to be considered safe and still is recommended by both ACOG and SMFM for the prevention of recurrent preterm birth in high-risk patients. The high-risk patient population who may benefit most from this therapy is still not certain, but hopefully future studies will better delineate this. The landscape for 17-OHPC use may change dramatically if FDA approval is not upheld in the future. In my current practice, I am continuing to offer 17-OHPC to patients per the current ACOG guidelines, but I am counseling patients in a shared decision-making model regarding the findings of the PROLONG trial and the potential change in FDA approval.
Continue to: ACOG updates guidance on preventing early-onset GBS disease...
ACOG updates guidance on preventing early-onset GBS disease
American College of Obstetricians and Gynecologists—Committee on Obstetric Practice. ACOG committee opinion no. 782: prevention of early-onset group B streptococcal disease in newborns. Obstet Gynecol. 2019;134:e19-e40.
Group B streptococcus (GBS) is the leading cause of newborn infection and is associated with maternal infections as well as preterm labor and stillbirth. Early-onset GBS disease occurs within 7 days of birth and is linked to vertical transmission via maternal colonization of the genitourinary or gastrointestinal tract and fetal/neonatal aspiration at birth.
Preventing early-onset GBS disease with maternal screening and intrapartum prophylaxis according to the Centers for Disease Control and Prevention (CDC) guidelines has reduced early-onset disease by 80% since the 1990s. By contrast, late-onset GBS infection, which occurs 7 days to 3 months after birth, usually is associated with horizontal maternal transmission or hospital or community infections, and it is not prevented by intrapartum treatment.
In 2018, the CDC transferred responsibility for GBS prophylaxis guidelines to ACOG and the American Academy of Pediatrics (AAP). In July 2019, ACOG released its Committee Opinion on preventing early-onset GBS disease in newborns.8 This guidance replaces and updates the previous guidelines, with 3 notable changes.
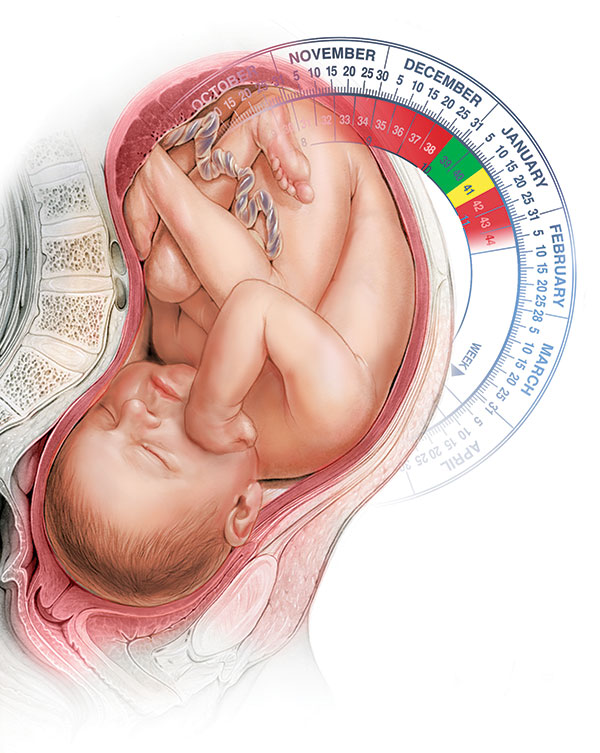
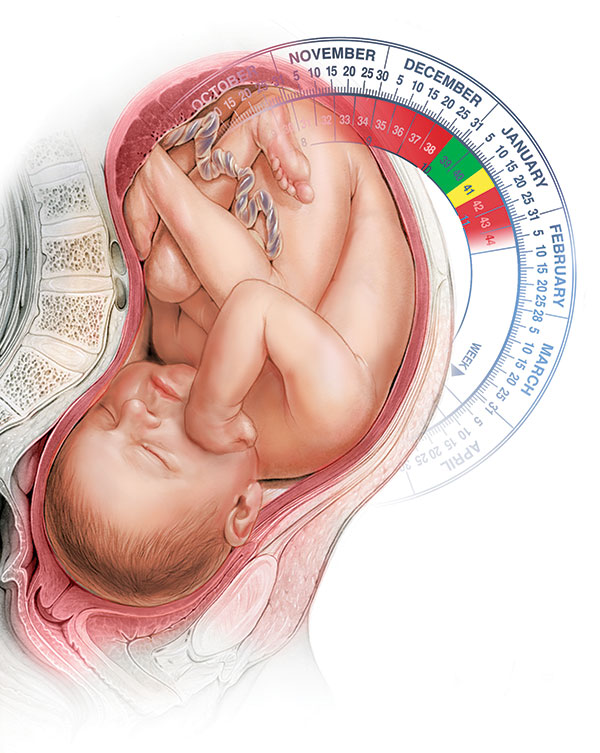
The screening timing has changed
In the CDC's 2010 guidelines, GBS screening was recommended to start at 35 weeks' gestation. The new guidelines recommend universal vaginal-rectal screening at 36 to 37 6/7 weeks' gestation. The new timing of culture will shift the expected 5-week window in which GBS cultures are considered valid up to at least 41 weeks' gestation. The rationale for this change is that any GBS-unknown patient who previously would have been cultured under 37 weeks' would be an automatic candidate for empiric therapy and the lower rate of birth in the 35th versus the 41st week of gestation.
Identifying candidates for intrapartum treatment
The usual indications for intrapartum antibiotic prophylaxis include a GBS-positive culture at 36 weeks or beyond, GBS bacteriuria at any point in pregnancy, a prior GBS-affected child, or unknown GBS status with any of the following: < 37 weeks, rupture of membranes ≥ 18 hours or temperature ≥ 100.4°F (38°C), and a positive rapid GBS culture in labor. In addition, antibiotics now should be considered for patients at term with unknown GBS status but with a history of GBS colonization in a prior pregnancy.
This represents a major practice change for women at ≥ 37 weeks with unknown GBS status and no other traditional risk factors. The rationale for this recommendation is that women who have been positive for GBS in a prior pregnancy have a 50% chance of being colonized in the current pregnancy, and their newborns are therefore at higher risk for early-onset GBS disease.
Managing patients with penicillin allergy
Intravenous penicillin (or ampicillin) remains the antibiotic of choice for intrapartum prophylaxis against GBS due to its efficacy and specific, narrow coverage of gram-positive organisms. The updated recommendations emphasize that it is important to carefully evaluate patients with reported penicillin allergies for several reasons: determining risk of anaphylaxis and clindamycin susceptibility testing in GBS evaluations are often overlooked by obstetric providers, the need for antibiotic stewardship to reduce the development of antibiotic resistance, and clarification of allergy status for future health care needs.
Three recommendations are made:
- Laboratory requisitions for cultures should specifically note a penicillin allergy so that clindamycin susceptibility testing can be performed.
- Penicillin allergy skin testing should be considered for patients at unknown or low risk for anaphylaxis, as it is considered safe in pregnancy and most patients (80%-90%) who report a penicillin allergy are actually penicillin tolerant.
- For patients at high risk for anaphylaxis to penicillin, the recommended vancomycin dosing has been changed from 1 g IV every 12 hours to 20 mg/kg IV every 8 hours (maximum single dose, 2 g). Renal function should be assessed prior to dosing. This weight- and renal function-based dosing increased neonatal therapeutic levels in several studies of different doses.
ACOG's key recommendations for preventing early-onset GBS disease in newborns include:
- Universal vaginal-rectal screening for GBS should be performed at 36 to 37 6/7 weeks' gestation.
- Intrapartum antibiotic prophylaxis should be considered for low-risk patients at term with unknown GBS status and a history of GBS colonization in a prior pregnancy.
- Patients with a reported penicillin allergy require careful evaluation of the nature of their allergy, including consideration of skin testing and GBS susceptibility evaluation in order to promote the best practices for antibiotic use.
- For GBS-positive patients at high risk for penicillin anaphylaxis, vancomycin 20 mg/kg IV every 8 hours (maximum single dose, 2 g) is recommended.
Continue to: Managing hypertension in pregnancy: New recommendations...
Managing hypertension in pregnancy: New recommendations
American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 202. Gestational hypertension and preeclampsia. Obstet Gynecol. 2019;133:e1-e25.
In 2013, ACOG released "Hypertension in pregnancy," a 99-page comprehensive document developed by their Task Force on Hypertension in Pregnancy, to summarize knowledge on the subject, provide guidelines for management, and identify needed areas of research.9 I summarized key points from that document in the 2014 "Update on Obstetrics" (OBG Manag. 2013;26[1]:28-36). Now, ACOG has released 2 Practice Bulletins—"Gestational hypertension and preeclampsia" and "Chronic hypertension in pregnancy"—that replace the 2013 document.10,11 These Practice Bulletins are quite comprehensive and warrant a thorough read. Several noteworthy changes relevant to the practicing obstetrician are summarized below.
Highlights of revised guidance
Expectant management vs early delivery in preeclampsia with fetal growth restriction. Fetal growth restriction, which was removed from the definition of preeclampsia with severe features in 2013, is no longer an indication for delivery in preeclampsia with severe features (previously, if the estimated fetal weight was < 5th percentile for gestational age, delivery after steroid administration was recommended). Rather, expectant management is reasonable if fetal antenatal testing, amniotic fluid, and Doppler ultrasound studies are reassuring. Abnormal umbilical artery Doppler studies continue to be an indication for earlier delivery.
Postpartum NSAID use in hypertension. The 2013 document cautioned against nonsteroidal anti-inflammatory drug (NSAID) use postpartum in women with hypertensive disorders of pregnancy because of concern for exacerbating hypertension. The updated Practice Bulletins recommend NSAIDs as the preferred choice over opioid analgesics as data have not shown these drugs to increase blood pressure, antihypertensive requirements, or other adverse events in postpartum patients with blood pressure issues.
More women will be diagnosed with chronic hypertension. Recently, the American College of Cardiology and the American Heart Association changed the definition of hypertension. Stage 1 hypertension is now defined as a systolic blood pressure of 130-139 mm Hg or a diastolic blood pressure of 80-89 mm Hg. Treatment of stage 1 hypertension is recommended for nonpregnant adults with risk factors for current or future cardiovascular disease. The potential impact is that more women will enter pregnancy with a diagnosis of chronic hypertension, and more may be on prepregnancy antihypertensive therapy that will need to be addressed during the pregnancy.
Blood pressure goals. The target blood pressure range for pregnant women with chronic hypertension is recommended to be ≥ 120/80 mm Hg and < 160/110 mm Hg (this represents a slight change, as previously diastolic blood pressure was to be < 105 mm Hg). Postpartum blood pressure goals of < 150/100 mm Hg remain the same.
Managing acute hypertensive emergencies. Both Practice Bulletins emphasize the importance of aggressive management of acute hypertensive emergency, with options for 3 protocols: labetalol, nifedipine, and hydralazine. The goal is to administer antihypertensive therapy within 30 to 60 minutes, but administration as soon as feasibly possible after diagnosis of severe hypertension is ideal.
Timing of delivery. Recommended delivery timing in patients with chronic hypertension was slightly altered (previous recommendations included a range of 37 to 39 6/7 weeks). The lower limit of gestational age for recommended delivery timing in chronic hypertension has not changed—it remains not before 38 weeks if no antihypertensive therapy and stable, and not before 37 weeks if antihypertensive therapy and stable.
The upper limit of 39 6/7 weeks is challenged, however, because data support that induction of labor at either 38 or 39 weeks reduces the risk of severe hypertensive complications (such as superimposed preeclampsia and eclampsia) without increasing the risk of cesarean delivery. Therefore, for patients with chronic hypertension, expectant management beyond 39 weeks is cautioned, to be done only with careful consideration of risks and with close surveillance.
As with ACOG’s original Task Force document on hypertension, clinicians should thoroughly read these 2 Practice Bulletins on hypertension in pregnancy as there are subtle changes that affect day-to-day practice, such as the definition of hypertension prior to pregnancy, treatment guidelines, and delivery timing recommendations. As always, these are guidelines, and the obstetrician’s clinical judgment and the needs of specific patient populations also must be taken into account.
- Meis PJ, Klebanoff M, Thom E, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348:2379-2385.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins—Obstetrics. Practice bulletin No. 130: prediction and prevention of preterm birth. Obstet Gynecol. 2012;120:964-973.
- Blackwell SC, Gyamfi-Bannerman C, Biggio JR Jr, et al. 17-OHPC to prevent recurrent preterm birth in singleton gestations (PROLONG study): a multicenter, international, randomized double-blind trial. Am J Perinatol. 2019. doi: 10.1055/s-0039-3400227.
- ACOG Practice Advisory. Clinical guidance for integration of the findings of the PROLONG study: progestin’s role in optimizing neonatal gestation. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Clinical-guidance-for-integration-of-the-findings-of-The-PROLONG-study-Progestins-Role-in-Optimizing. Accessed November 10, 2019.
- Society for Maternal-Fetal Medicine Publications Committee. SMFM Statement: use of 17-alpha hydroxyprogesterone caproate for prevention of recurrent preterm birth. https://www.smfm.org/publications/280-smfm-statement-use-of-17-alpha-hydroxyprogesterone-caproate-for-prevention-of-recurrent-preterm-birth. Accessed November 10, 2019.
- US Food and Drug Administration. Bone, Reproductive, and Urologic Drugs Advisory Committee Meeting, October 29, 2019. Advisory Committee Briefing Materials: Available for Public Release. https://www.fda.gov/media/132004/download. Accessed November 19, 2019.
- Society for Maternal-Fetal Medicine. SMFM responds to the FDA’s Bone, Reproductive and Urologic Advisory Committee. https://s3.amazonaws.com/cdn.smfm.org/media/2091/17P_Public_Statement.pdf. Accessed November 19, 2019.
- American College of Obstetricians and Gynecologists—Committee on Obstetric Practice. ACOG committee opinion no. 782: prevention of early-onset group B streptococcal disease in newborns. Obstet Gynecol. 2019;134:e19-e40.
- American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy. Hypertension in Pregnancy. Washington, DC: ACOG; November 2013.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 202: gestational hypertension and preeclampsia. Obstet Gynecol. 2019;133:e1-e25.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 203: chronic hypertension in pregnancy. Obstet Gynecol. 2019;133:e26-e50.
Attributed to the ancient Greek philosopher Heraclitus, and often quoted in contemporary times, is the expression “the only constant is change.” This sentiment rings true for the field of obstetrics this past year, as several bread-and-butter guidelines for managing common obstetric conditions were either challenged or altered.
The publication of the PROLONG trial called into question the use of intramuscular progesterone for the prevention of preterm birth. Prophylaxis guidelines for group B streptococcal disease were updated, including several significant clinical practice changes. Finally, there was a comprehensive overhaul of the guidelines for hypertensive disorders of pregnancy, which replaced a landmark Task Force document from the American College of Obstetricians and Gynecologists (ACOG) that was published only a few years ago.
Change is constant, and in obstetrics it is vital to keep up with the changing guidelines that result as new data become available for digestion and implementation into everyday clinical practice.
Results from the PROLONG trial may shake up treatment options for recurrent preterm birth
Blackwell SC, Gyamfi-Bannerman C, Biggio JR Jr, et al. 17-OHPC to prevent recurrent preterm birth in singleton gestations (PROLONG study): a multicenter, international, randomized double-blind trial. Am J Perinatol. 2019. doi: 10.1055/s-0039-3400227.
The drug 17 α-hydroxyprogesterone caproate (17-OHPC, or 17P; Makena) was approved by the US Food and Drug Administration (FDA) in 2011 for the prevention of spontaneous preterm birth (PTB) in women with a singleton pregnancy and a history of singleton spontaneous PTB. The results of the trial by Meis and colleagues of 17-OHPC played a major role in achieving that approval, as it demonstrated a 34% reduction in recurrent PTB and a reduction in some neonatal morbidities.1 Following the drug's approval, both ACOG and the Society for Maternal-Fetal Medicine (SMFM) published guidelines recommending progesterone therapy, including 17-OHPC, for the prevention of recurrent spontaneous PTB.2
The FDA approval of 17-OHPC was granted under an accelerated conditional pathway that required a confirmatory trial evaluating efficacy, safety, and long-term infant follow-up to be performed by the sponsor. That trial, Progestin's Role in Optimizing Neonatal Gestation (PROLONG), was started in 2009, and its results were published on October 25, 2019.3
Continue to: Design of the trial...
Design of the trial
PROLONG was a multicenter (93 sites), randomized, placebo-controlled, double-blind study conducted in 9 countries (23% of participants were in the United States, 60% were in Russia and Ukraine). The co-primary outcome was PTB < 35 weeks and a composite neonatal morbidity and mortality index. The primary safety outcome was fetal/early infant death.
The study was designed to have 98% power to detect a 30% reduction in PTB < 35 weeks, and 90% power to detect a 35% reduction in the neonatal composite index. It included 1,708 participants (1,130 were treated with 17-OHPC, and 578 received placebo).
Trial outcomes. There was no difference in PTB < 35 weeks between the 17-OHPC and the placebo groups (11.0% vs 11.5%; relative risk [RR], 0.95; 95% confidence interval [CI], 0.71-1.26). There was no difference in PTB < 32 or < 37 weeks.
The study revealed also that there was no difference between groups in the neonatal composite index (5.6% for 17-OHPC vs 5.0% for placebo; RR, 1.12; 95% CI, 0.68-1.61). In addition, there was no difference in fetal/early infant death between the 17-OHPC and placebo groups (1.7% vs 1.9%; RR, 0.87; 95% CI, 0.4-1.81).
Conclusions. The trial investigators concluded that 17-OHPC did not demonstrate a reduction in recurrent PTB and did not decrease neonatal morbidity.
Study limitations included underpowering and selection bias
The investigators noted that the PTB rate in PROLONG was unexpectedly almost 50% lower than that in the Meis trial, and that therefore the PROLONG trial was underpowered to assess the primary outcomes.
Further, the study populations of the 2 trials were very different: The Meis trial included women at higher baseline risk for PTB (> 1 prior PTB and at least 1 other risk factor for PTB). Additionally, while the PROLONG trial included mostly white (90%), married (90%), nonsmoking women (8% smoked), the Meis trial population was 59% black and 50% married, and 20% were smokers.
The availability and common use of 17-OHPC in the United States likely led to a selection bias for the PROLONG trial population, as the highest-risk patients were most likely already receiving treatment and were therefore excluded from the PROLONG trial.
Society, and FDA, responses to the new data
The results of the PROLONG trial call into question what has become standard practice for patients with a history of spontaneous PTB in the United States. While the safety profile of 17-OHPC has not been cited as a concern, whether or not the drug should be used at all has—as has its current FDA-approved status.
In response to the publication of the PROLONG trial results, ACOG released a Practice Advisory that acknowledged the study's findings but did not alter the current recommendations to continue to offer progesterone for the prevention of preterm birth, upholding ACOG's current Practice Bulletin guidance.2,4 Additional considerations for offering 17-OHPC use include the patients' preferences, available resources, and the setting for the intervention.
SMFM's response was more specific, stating that it is reasonable to continue to use 17-OHPC in high-risk patient populations consistent with those in the Meis trial.5 In the rest of the general population at risk for recurrent PTB, SMFM recommends that, due to uncertain benefit with 17-OHPC, the high cost, patient discomfort, and increased visits should be taken into account.
Four days after the publication of the PROLONG study, the FDA Bone, Reproductive, and Urologic Drugs Advisory Committee voted 9-7 to withdraw approval for 17-OHPC.6 In response, SMFM released a statement supporting continued access to 17-OHPC.7 The FDA's final decision on the status of the drug is expected within the next several months from this writing.
17-OHPC continues to be considered safe and still is recommended by both ACOG and SMFM for the prevention of recurrent preterm birth in high-risk patients. The high-risk patient population who may benefit most from this therapy is still not certain, but hopefully future studies will better delineate this. The landscape for 17-OHPC use may change dramatically if FDA approval is not upheld in the future. In my current practice, I am continuing to offer 17-OHPC to patients per the current ACOG guidelines, but I am counseling patients in a shared decision-making model regarding the findings of the PROLONG trial and the potential change in FDA approval.
Continue to: ACOG updates guidance on preventing early-onset GBS disease...
ACOG updates guidance on preventing early-onset GBS disease
American College of Obstetricians and Gynecologists—Committee on Obstetric Practice. ACOG committee opinion no. 782: prevention of early-onset group B streptococcal disease in newborns. Obstet Gynecol. 2019;134:e19-e40.
Group B streptococcus (GBS) is the leading cause of newborn infection and is associated with maternal infections as well as preterm labor and stillbirth. Early-onset GBS disease occurs within 7 days of birth and is linked to vertical transmission via maternal colonization of the genitourinary or gastrointestinal tract and fetal/neonatal aspiration at birth.
Preventing early-onset GBS disease with maternal screening and intrapartum prophylaxis according to the Centers for Disease Control and Prevention (CDC) guidelines has reduced early-onset disease by 80% since the 1990s. By contrast, late-onset GBS infection, which occurs 7 days to 3 months after birth, usually is associated with horizontal maternal transmission or hospital or community infections, and it is not prevented by intrapartum treatment.
In 2018, the CDC transferred responsibility for GBS prophylaxis guidelines to ACOG and the American Academy of Pediatrics (AAP). In July 2019, ACOG released its Committee Opinion on preventing early-onset GBS disease in newborns.8 This guidance replaces and updates the previous guidelines, with 3 notable changes.
The screening timing has changed
In the CDC's 2010 guidelines, GBS screening was recommended to start at 35 weeks' gestation. The new guidelines recommend universal vaginal-rectal screening at 36 to 37 6/7 weeks' gestation. The new timing of culture will shift the expected 5-week window in which GBS cultures are considered valid up to at least 41 weeks' gestation. The rationale for this change is that any GBS-unknown patient who previously would have been cultured under 37 weeks' would be an automatic candidate for empiric therapy and the lower rate of birth in the 35th versus the 41st week of gestation.
Identifying candidates for intrapartum treatment
The usual indications for intrapartum antibiotic prophylaxis include a GBS-positive culture at 36 weeks or beyond, GBS bacteriuria at any point in pregnancy, a prior GBS-affected child, or unknown GBS status with any of the following: < 37 weeks, rupture of membranes ≥ 18 hours or temperature ≥ 100.4°F (38°C), and a positive rapid GBS culture in labor. In addition, antibiotics now should be considered for patients at term with unknown GBS status but with a history of GBS colonization in a prior pregnancy.
This represents a major practice change for women at ≥ 37 weeks with unknown GBS status and no other traditional risk factors. The rationale for this recommendation is that women who have been positive for GBS in a prior pregnancy have a 50% chance of being colonized in the current pregnancy, and their newborns are therefore at higher risk for early-onset GBS disease.
Managing patients with penicillin allergy
Intravenous penicillin (or ampicillin) remains the antibiotic of choice for intrapartum prophylaxis against GBS due to its efficacy and specific, narrow coverage of gram-positive organisms. The updated recommendations emphasize that it is important to carefully evaluate patients with reported penicillin allergies for several reasons: determining risk of anaphylaxis and clindamycin susceptibility testing in GBS evaluations are often overlooked by obstetric providers, the need for antibiotic stewardship to reduce the development of antibiotic resistance, and clarification of allergy status for future health care needs.
Three recommendations are made:
- Laboratory requisitions for cultures should specifically note a penicillin allergy so that clindamycin susceptibility testing can be performed.
- Penicillin allergy skin testing should be considered for patients at unknown or low risk for anaphylaxis, as it is considered safe in pregnancy and most patients (80%-90%) who report a penicillin allergy are actually penicillin tolerant.
- For patients at high risk for anaphylaxis to penicillin, the recommended vancomycin dosing has been changed from 1 g IV every 12 hours to 20 mg/kg IV every 8 hours (maximum single dose, 2 g). Renal function should be assessed prior to dosing. This weight- and renal function-based dosing increased neonatal therapeutic levels in several studies of different doses.
ACOG's key recommendations for preventing early-onset GBS disease in newborns include:
- Universal vaginal-rectal screening for GBS should be performed at 36 to 37 6/7 weeks' gestation.
- Intrapartum antibiotic prophylaxis should be considered for low-risk patients at term with unknown GBS status and a history of GBS colonization in a prior pregnancy.
- Patients with a reported penicillin allergy require careful evaluation of the nature of their allergy, including consideration of skin testing and GBS susceptibility evaluation in order to promote the best practices for antibiotic use.
- For GBS-positive patients at high risk for penicillin anaphylaxis, vancomycin 20 mg/kg IV every 8 hours (maximum single dose, 2 g) is recommended.
Continue to: Managing hypertension in pregnancy: New recommendations...
Managing hypertension in pregnancy: New recommendations
American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 202. Gestational hypertension and preeclampsia. Obstet Gynecol. 2019;133:e1-e25.
In 2013, ACOG released "Hypertension in pregnancy," a 99-page comprehensive document developed by their Task Force on Hypertension in Pregnancy, to summarize knowledge on the subject, provide guidelines for management, and identify needed areas of research.9 I summarized key points from that document in the 2014 "Update on Obstetrics" (OBG Manag. 2013;26[1]:28-36). Now, ACOG has released 2 Practice Bulletins—"Gestational hypertension and preeclampsia" and "Chronic hypertension in pregnancy"—that replace the 2013 document.10,11 These Practice Bulletins are quite comprehensive and warrant a thorough read. Several noteworthy changes relevant to the practicing obstetrician are summarized below.
Highlights of revised guidance
Expectant management vs early delivery in preeclampsia with fetal growth restriction. Fetal growth restriction, which was removed from the definition of preeclampsia with severe features in 2013, is no longer an indication for delivery in preeclampsia with severe features (previously, if the estimated fetal weight was < 5th percentile for gestational age, delivery after steroid administration was recommended). Rather, expectant management is reasonable if fetal antenatal testing, amniotic fluid, and Doppler ultrasound studies are reassuring. Abnormal umbilical artery Doppler studies continue to be an indication for earlier delivery.
Postpartum NSAID use in hypertension. The 2013 document cautioned against nonsteroidal anti-inflammatory drug (NSAID) use postpartum in women with hypertensive disorders of pregnancy because of concern for exacerbating hypertension. The updated Practice Bulletins recommend NSAIDs as the preferred choice over opioid analgesics as data have not shown these drugs to increase blood pressure, antihypertensive requirements, or other adverse events in postpartum patients with blood pressure issues.
More women will be diagnosed with chronic hypertension. Recently, the American College of Cardiology and the American Heart Association changed the definition of hypertension. Stage 1 hypertension is now defined as a systolic blood pressure of 130-139 mm Hg or a diastolic blood pressure of 80-89 mm Hg. Treatment of stage 1 hypertension is recommended for nonpregnant adults with risk factors for current or future cardiovascular disease. The potential impact is that more women will enter pregnancy with a diagnosis of chronic hypertension, and more may be on prepregnancy antihypertensive therapy that will need to be addressed during the pregnancy.
Blood pressure goals. The target blood pressure range for pregnant women with chronic hypertension is recommended to be ≥ 120/80 mm Hg and < 160/110 mm Hg (this represents a slight change, as previously diastolic blood pressure was to be < 105 mm Hg). Postpartum blood pressure goals of < 150/100 mm Hg remain the same.
Managing acute hypertensive emergencies. Both Practice Bulletins emphasize the importance of aggressive management of acute hypertensive emergency, with options for 3 protocols: labetalol, nifedipine, and hydralazine. The goal is to administer antihypertensive therapy within 30 to 60 minutes, but administration as soon as feasibly possible after diagnosis of severe hypertension is ideal.
Timing of delivery. Recommended delivery timing in patients with chronic hypertension was slightly altered (previous recommendations included a range of 37 to 39 6/7 weeks). The lower limit of gestational age for recommended delivery timing in chronic hypertension has not changed—it remains not before 38 weeks if no antihypertensive therapy and stable, and not before 37 weeks if antihypertensive therapy and stable.
The upper limit of 39 6/7 weeks is challenged, however, because data support that induction of labor at either 38 or 39 weeks reduces the risk of severe hypertensive complications (such as superimposed preeclampsia and eclampsia) without increasing the risk of cesarean delivery. Therefore, for patients with chronic hypertension, expectant management beyond 39 weeks is cautioned, to be done only with careful consideration of risks and with close surveillance.
As with ACOG’s original Task Force document on hypertension, clinicians should thoroughly read these 2 Practice Bulletins on hypertension in pregnancy as there are subtle changes that affect day-to-day practice, such as the definition of hypertension prior to pregnancy, treatment guidelines, and delivery timing recommendations. As always, these are guidelines, and the obstetrician’s clinical judgment and the needs of specific patient populations also must be taken into account.
Attributed to the ancient Greek philosopher Heraclitus, and often quoted in contemporary times, is the expression “the only constant is change.” This sentiment rings true for the field of obstetrics this past year, as several bread-and-butter guidelines for managing common obstetric conditions were either challenged or altered.
The publication of the PROLONG trial called into question the use of intramuscular progesterone for the prevention of preterm birth. Prophylaxis guidelines for group B streptococcal disease were updated, including several significant clinical practice changes. Finally, there was a comprehensive overhaul of the guidelines for hypertensive disorders of pregnancy, which replaced a landmark Task Force document from the American College of Obstetricians and Gynecologists (ACOG) that was published only a few years ago.
Change is constant, and in obstetrics it is vital to keep up with the changing guidelines that result as new data become available for digestion and implementation into everyday clinical practice.
Results from the PROLONG trial may shake up treatment options for recurrent preterm birth
Blackwell SC, Gyamfi-Bannerman C, Biggio JR Jr, et al. 17-OHPC to prevent recurrent preterm birth in singleton gestations (PROLONG study): a multicenter, international, randomized double-blind trial. Am J Perinatol. 2019. doi: 10.1055/s-0039-3400227.
The drug 17 α-hydroxyprogesterone caproate (17-OHPC, or 17P; Makena) was approved by the US Food and Drug Administration (FDA) in 2011 for the prevention of spontaneous preterm birth (PTB) in women with a singleton pregnancy and a history of singleton spontaneous PTB. The results of the trial by Meis and colleagues of 17-OHPC played a major role in achieving that approval, as it demonstrated a 34% reduction in recurrent PTB and a reduction in some neonatal morbidities.1 Following the drug's approval, both ACOG and the Society for Maternal-Fetal Medicine (SMFM) published guidelines recommending progesterone therapy, including 17-OHPC, for the prevention of recurrent spontaneous PTB.2
The FDA approval of 17-OHPC was granted under an accelerated conditional pathway that required a confirmatory trial evaluating efficacy, safety, and long-term infant follow-up to be performed by the sponsor. That trial, Progestin's Role in Optimizing Neonatal Gestation (PROLONG), was started in 2009, and its results were published on October 25, 2019.3
Continue to: Design of the trial...
Design of the trial
PROLONG was a multicenter (93 sites), randomized, placebo-controlled, double-blind study conducted in 9 countries (23% of participants were in the United States, 60% were in Russia and Ukraine). The co-primary outcome was PTB < 35 weeks and a composite neonatal morbidity and mortality index. The primary safety outcome was fetal/early infant death.
The study was designed to have 98% power to detect a 30% reduction in PTB < 35 weeks, and 90% power to detect a 35% reduction in the neonatal composite index. It included 1,708 participants (1,130 were treated with 17-OHPC, and 578 received placebo).
Trial outcomes. There was no difference in PTB < 35 weeks between the 17-OHPC and the placebo groups (11.0% vs 11.5%; relative risk [RR], 0.95; 95% confidence interval [CI], 0.71-1.26). There was no difference in PTB < 32 or < 37 weeks.
The study revealed also that there was no difference between groups in the neonatal composite index (5.6% for 17-OHPC vs 5.0% for placebo; RR, 1.12; 95% CI, 0.68-1.61). In addition, there was no difference in fetal/early infant death between the 17-OHPC and placebo groups (1.7% vs 1.9%; RR, 0.87; 95% CI, 0.4-1.81).
Conclusions. The trial investigators concluded that 17-OHPC did not demonstrate a reduction in recurrent PTB and did not decrease neonatal morbidity.
Study limitations included underpowering and selection bias
The investigators noted that the PTB rate in PROLONG was unexpectedly almost 50% lower than that in the Meis trial, and that therefore the PROLONG trial was underpowered to assess the primary outcomes.
Further, the study populations of the 2 trials were very different: The Meis trial included women at higher baseline risk for PTB (> 1 prior PTB and at least 1 other risk factor for PTB). Additionally, while the PROLONG trial included mostly white (90%), married (90%), nonsmoking women (8% smoked), the Meis trial population was 59% black and 50% married, and 20% were smokers.
The availability and common use of 17-OHPC in the United States likely led to a selection bias for the PROLONG trial population, as the highest-risk patients were most likely already receiving treatment and were therefore excluded from the PROLONG trial.
Society, and FDA, responses to the new data
The results of the PROLONG trial call into question what has become standard practice for patients with a history of spontaneous PTB in the United States. While the safety profile of 17-OHPC has not been cited as a concern, whether or not the drug should be used at all has—as has its current FDA-approved status.
In response to the publication of the PROLONG trial results, ACOG released a Practice Advisory that acknowledged the study's findings but did not alter the current recommendations to continue to offer progesterone for the prevention of preterm birth, upholding ACOG's current Practice Bulletin guidance.2,4 Additional considerations for offering 17-OHPC use include the patients' preferences, available resources, and the setting for the intervention.
SMFM's response was more specific, stating that it is reasonable to continue to use 17-OHPC in high-risk patient populations consistent with those in the Meis trial.5 In the rest of the general population at risk for recurrent PTB, SMFM recommends that, due to uncertain benefit with 17-OHPC, the high cost, patient discomfort, and increased visits should be taken into account.
Four days after the publication of the PROLONG study, the FDA Bone, Reproductive, and Urologic Drugs Advisory Committee voted 9-7 to withdraw approval for 17-OHPC.6 In response, SMFM released a statement supporting continued access to 17-OHPC.7 The FDA's final decision on the status of the drug is expected within the next several months from this writing.
17-OHPC continues to be considered safe and still is recommended by both ACOG and SMFM for the prevention of recurrent preterm birth in high-risk patients. The high-risk patient population who may benefit most from this therapy is still not certain, but hopefully future studies will better delineate this. The landscape for 17-OHPC use may change dramatically if FDA approval is not upheld in the future. In my current practice, I am continuing to offer 17-OHPC to patients per the current ACOG guidelines, but I am counseling patients in a shared decision-making model regarding the findings of the PROLONG trial and the potential change in FDA approval.
Continue to: ACOG updates guidance on preventing early-onset GBS disease...
ACOG updates guidance on preventing early-onset GBS disease
American College of Obstetricians and Gynecologists—Committee on Obstetric Practice. ACOG committee opinion no. 782: prevention of early-onset group B streptococcal disease in newborns. Obstet Gynecol. 2019;134:e19-e40.
Group B streptococcus (GBS) is the leading cause of newborn infection and is associated with maternal infections as well as preterm labor and stillbirth. Early-onset GBS disease occurs within 7 days of birth and is linked to vertical transmission via maternal colonization of the genitourinary or gastrointestinal tract and fetal/neonatal aspiration at birth.
Preventing early-onset GBS disease with maternal screening and intrapartum prophylaxis according to the Centers for Disease Control and Prevention (CDC) guidelines has reduced early-onset disease by 80% since the 1990s. By contrast, late-onset GBS infection, which occurs 7 days to 3 months after birth, usually is associated with horizontal maternal transmission or hospital or community infections, and it is not prevented by intrapartum treatment.
In 2018, the CDC transferred responsibility for GBS prophylaxis guidelines to ACOG and the American Academy of Pediatrics (AAP). In July 2019, ACOG released its Committee Opinion on preventing early-onset GBS disease in newborns.8 This guidance replaces and updates the previous guidelines, with 3 notable changes.
The screening timing has changed
In the CDC's 2010 guidelines, GBS screening was recommended to start at 35 weeks' gestation. The new guidelines recommend universal vaginal-rectal screening at 36 to 37 6/7 weeks' gestation. The new timing of culture will shift the expected 5-week window in which GBS cultures are considered valid up to at least 41 weeks' gestation. The rationale for this change is that any GBS-unknown patient who previously would have been cultured under 37 weeks' would be an automatic candidate for empiric therapy and the lower rate of birth in the 35th versus the 41st week of gestation.
Identifying candidates for intrapartum treatment
The usual indications for intrapartum antibiotic prophylaxis include a GBS-positive culture at 36 weeks or beyond, GBS bacteriuria at any point in pregnancy, a prior GBS-affected child, or unknown GBS status with any of the following: < 37 weeks, rupture of membranes ≥ 18 hours or temperature ≥ 100.4°F (38°C), and a positive rapid GBS culture in labor. In addition, antibiotics now should be considered for patients at term with unknown GBS status but with a history of GBS colonization in a prior pregnancy.
This represents a major practice change for women at ≥ 37 weeks with unknown GBS status and no other traditional risk factors. The rationale for this recommendation is that women who have been positive for GBS in a prior pregnancy have a 50% chance of being colonized in the current pregnancy, and their newborns are therefore at higher risk for early-onset GBS disease.
Managing patients with penicillin allergy
Intravenous penicillin (or ampicillin) remains the antibiotic of choice for intrapartum prophylaxis against GBS due to its efficacy and specific, narrow coverage of gram-positive organisms. The updated recommendations emphasize that it is important to carefully evaluate patients with reported penicillin allergies for several reasons: determining risk of anaphylaxis and clindamycin susceptibility testing in GBS evaluations are often overlooked by obstetric providers, the need for antibiotic stewardship to reduce the development of antibiotic resistance, and clarification of allergy status for future health care needs.
Three recommendations are made:
- Laboratory requisitions for cultures should specifically note a penicillin allergy so that clindamycin susceptibility testing can be performed.
- Penicillin allergy skin testing should be considered for patients at unknown or low risk for anaphylaxis, as it is considered safe in pregnancy and most patients (80%-90%) who report a penicillin allergy are actually penicillin tolerant.
- For patients at high risk for anaphylaxis to penicillin, the recommended vancomycin dosing has been changed from 1 g IV every 12 hours to 20 mg/kg IV every 8 hours (maximum single dose, 2 g). Renal function should be assessed prior to dosing. This weight- and renal function-based dosing increased neonatal therapeutic levels in several studies of different doses.
ACOG's key recommendations for preventing early-onset GBS disease in newborns include:
- Universal vaginal-rectal screening for GBS should be performed at 36 to 37 6/7 weeks' gestation.
- Intrapartum antibiotic prophylaxis should be considered for low-risk patients at term with unknown GBS status and a history of GBS colonization in a prior pregnancy.
- Patients with a reported penicillin allergy require careful evaluation of the nature of their allergy, including consideration of skin testing and GBS susceptibility evaluation in order to promote the best practices for antibiotic use.
- For GBS-positive patients at high risk for penicillin anaphylaxis, vancomycin 20 mg/kg IV every 8 hours (maximum single dose, 2 g) is recommended.
Continue to: Managing hypertension in pregnancy: New recommendations...
Managing hypertension in pregnancy: New recommendations
American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 202. Gestational hypertension and preeclampsia. Obstet Gynecol. 2019;133:e1-e25.
In 2013, ACOG released "Hypertension in pregnancy," a 99-page comprehensive document developed by their Task Force on Hypertension in Pregnancy, to summarize knowledge on the subject, provide guidelines for management, and identify needed areas of research.9 I summarized key points from that document in the 2014 "Update on Obstetrics" (OBG Manag. 2013;26[1]:28-36). Now, ACOG has released 2 Practice Bulletins—"Gestational hypertension and preeclampsia" and "Chronic hypertension in pregnancy"—that replace the 2013 document.10,11 These Practice Bulletins are quite comprehensive and warrant a thorough read. Several noteworthy changes relevant to the practicing obstetrician are summarized below.
Highlights of revised guidance
Expectant management vs early delivery in preeclampsia with fetal growth restriction. Fetal growth restriction, which was removed from the definition of preeclampsia with severe features in 2013, is no longer an indication for delivery in preeclampsia with severe features (previously, if the estimated fetal weight was < 5th percentile for gestational age, delivery after steroid administration was recommended). Rather, expectant management is reasonable if fetal antenatal testing, amniotic fluid, and Doppler ultrasound studies are reassuring. Abnormal umbilical artery Doppler studies continue to be an indication for earlier delivery.
Postpartum NSAID use in hypertension. The 2013 document cautioned against nonsteroidal anti-inflammatory drug (NSAID) use postpartum in women with hypertensive disorders of pregnancy because of concern for exacerbating hypertension. The updated Practice Bulletins recommend NSAIDs as the preferred choice over opioid analgesics as data have not shown these drugs to increase blood pressure, antihypertensive requirements, or other adverse events in postpartum patients with blood pressure issues.
More women will be diagnosed with chronic hypertension. Recently, the American College of Cardiology and the American Heart Association changed the definition of hypertension. Stage 1 hypertension is now defined as a systolic blood pressure of 130-139 mm Hg or a diastolic blood pressure of 80-89 mm Hg. Treatment of stage 1 hypertension is recommended for nonpregnant adults with risk factors for current or future cardiovascular disease. The potential impact is that more women will enter pregnancy with a diagnosis of chronic hypertension, and more may be on prepregnancy antihypertensive therapy that will need to be addressed during the pregnancy.
Blood pressure goals. The target blood pressure range for pregnant women with chronic hypertension is recommended to be ≥ 120/80 mm Hg and < 160/110 mm Hg (this represents a slight change, as previously diastolic blood pressure was to be < 105 mm Hg). Postpartum blood pressure goals of < 150/100 mm Hg remain the same.
Managing acute hypertensive emergencies. Both Practice Bulletins emphasize the importance of aggressive management of acute hypertensive emergency, with options for 3 protocols: labetalol, nifedipine, and hydralazine. The goal is to administer antihypertensive therapy within 30 to 60 minutes, but administration as soon as feasibly possible after diagnosis of severe hypertension is ideal.
Timing of delivery. Recommended delivery timing in patients with chronic hypertension was slightly altered (previous recommendations included a range of 37 to 39 6/7 weeks). The lower limit of gestational age for recommended delivery timing in chronic hypertension has not changed—it remains not before 38 weeks if no antihypertensive therapy and stable, and not before 37 weeks if antihypertensive therapy and stable.
The upper limit of 39 6/7 weeks is challenged, however, because data support that induction of labor at either 38 or 39 weeks reduces the risk of severe hypertensive complications (such as superimposed preeclampsia and eclampsia) without increasing the risk of cesarean delivery. Therefore, for patients with chronic hypertension, expectant management beyond 39 weeks is cautioned, to be done only with careful consideration of risks and with close surveillance.
As with ACOG’s original Task Force document on hypertension, clinicians should thoroughly read these 2 Practice Bulletins on hypertension in pregnancy as there are subtle changes that affect day-to-day practice, such as the definition of hypertension prior to pregnancy, treatment guidelines, and delivery timing recommendations. As always, these are guidelines, and the obstetrician’s clinical judgment and the needs of specific patient populations also must be taken into account.
- Meis PJ, Klebanoff M, Thom E, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348:2379-2385.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins—Obstetrics. Practice bulletin No. 130: prediction and prevention of preterm birth. Obstet Gynecol. 2012;120:964-973.
- Blackwell SC, Gyamfi-Bannerman C, Biggio JR Jr, et al. 17-OHPC to prevent recurrent preterm birth in singleton gestations (PROLONG study): a multicenter, international, randomized double-blind trial. Am J Perinatol. 2019. doi: 10.1055/s-0039-3400227.
- ACOG Practice Advisory. Clinical guidance for integration of the findings of the PROLONG study: progestin’s role in optimizing neonatal gestation. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Clinical-guidance-for-integration-of-the-findings-of-The-PROLONG-study-Progestins-Role-in-Optimizing. Accessed November 10, 2019.
- Society for Maternal-Fetal Medicine Publications Committee. SMFM Statement: use of 17-alpha hydroxyprogesterone caproate for prevention of recurrent preterm birth. https://www.smfm.org/publications/280-smfm-statement-use-of-17-alpha-hydroxyprogesterone-caproate-for-prevention-of-recurrent-preterm-birth. Accessed November 10, 2019.
- US Food and Drug Administration. Bone, Reproductive, and Urologic Drugs Advisory Committee Meeting, October 29, 2019. Advisory Committee Briefing Materials: Available for Public Release. https://www.fda.gov/media/132004/download. Accessed November 19, 2019.
- Society for Maternal-Fetal Medicine. SMFM responds to the FDA’s Bone, Reproductive and Urologic Advisory Committee. https://s3.amazonaws.com/cdn.smfm.org/media/2091/17P_Public_Statement.pdf. Accessed November 19, 2019.
- American College of Obstetricians and Gynecologists—Committee on Obstetric Practice. ACOG committee opinion no. 782: prevention of early-onset group B streptococcal disease in newborns. Obstet Gynecol. 2019;134:e19-e40.
- American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy. Hypertension in Pregnancy. Washington, DC: ACOG; November 2013.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 202: gestational hypertension and preeclampsia. Obstet Gynecol. 2019;133:e1-e25.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 203: chronic hypertension in pregnancy. Obstet Gynecol. 2019;133:e26-e50.
- Meis PJ, Klebanoff M, Thom E, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348:2379-2385.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins—Obstetrics. Practice bulletin No. 130: prediction and prevention of preterm birth. Obstet Gynecol. 2012;120:964-973.
- Blackwell SC, Gyamfi-Bannerman C, Biggio JR Jr, et al. 17-OHPC to prevent recurrent preterm birth in singleton gestations (PROLONG study): a multicenter, international, randomized double-blind trial. Am J Perinatol. 2019. doi: 10.1055/s-0039-3400227.
- ACOG Practice Advisory. Clinical guidance for integration of the findings of the PROLONG study: progestin’s role in optimizing neonatal gestation. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Clinical-guidance-for-integration-of-the-findings-of-The-PROLONG-study-Progestins-Role-in-Optimizing. Accessed November 10, 2019.
- Society for Maternal-Fetal Medicine Publications Committee. SMFM Statement: use of 17-alpha hydroxyprogesterone caproate for prevention of recurrent preterm birth. https://www.smfm.org/publications/280-smfm-statement-use-of-17-alpha-hydroxyprogesterone-caproate-for-prevention-of-recurrent-preterm-birth. Accessed November 10, 2019.
- US Food and Drug Administration. Bone, Reproductive, and Urologic Drugs Advisory Committee Meeting, October 29, 2019. Advisory Committee Briefing Materials: Available for Public Release. https://www.fda.gov/media/132004/download. Accessed November 19, 2019.
- Society for Maternal-Fetal Medicine. SMFM responds to the FDA’s Bone, Reproductive and Urologic Advisory Committee. https://s3.amazonaws.com/cdn.smfm.org/media/2091/17P_Public_Statement.pdf. Accessed November 19, 2019.
- American College of Obstetricians and Gynecologists—Committee on Obstetric Practice. ACOG committee opinion no. 782: prevention of early-onset group B streptococcal disease in newborns. Obstet Gynecol. 2019;134:e19-e40.
- American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy. Hypertension in Pregnancy. Washington, DC: ACOG; November 2013.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 202: gestational hypertension and preeclampsia. Obstet Gynecol. 2019;133:e1-e25.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 203: chronic hypertension in pregnancy. Obstet Gynecol. 2019;133:e26-e50.
2019 Update on Obstetrics
The past year was an exciting one in obstetrics. The landmark ARRIVE trial presented at the Society for Maternal-Fetal Medicine’s (SMFM) annual meeting and subsequently published in the New England Journal of Medicine contradicted a long-held belief about the safety of elective labor induction. In a large randomized trial, Cahill and colleagues took a controversial but practical clinical question about second-stage labor management and answered it for the practicing obstetrician in the trenches. Finally, the American College of Obstetricians and Gynecologists (ACOG) placed new emphasis on the oft overlooked but increasingly more complicated postpartum period, offering guidance to support improving care for women in this transitional period.
Ultimately, this was the year of the patient, as research, clinical guidelines, and education focused on how to achieve the best in safety and quality of care for delivery planning, the delivery itself, and the so-called fourth trimester.
ARRIVE: Labor induction at 39 weeks reduces CD rate with no difference in perinatal death or serious outcomes
Grobman WA, Rice MM, Reddy UM, et al; for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
The term "elective induction of labor" has long had a negative connotation because of its association with increased CD rates and adverse perinatal outcomes. This view was based on results from older observational studies that compared outcomes for labor induction with those of spontaneous labor. In more recent observational studies that more appropriately compared labor induction with expectant management, however, elective induction of labor appears to be associated with similar CD rates and perinatal outcomes.
To test the hypothesis that elective induction would have a lower risk for perinatal death or severe neonatal complications than expectant management in low-risk nulliparous women, Grobman and colleagues conducted A Randomized Trial of Induction Versus Expectant Management (ARRIVE).1
Study population, timing of delivery, and trial outcomes
This randomized controlled trial included 6,106 women at 41 US centers in the Maternal-Fetal Medicine Units Network of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Study participants were low-risk nulliparous women with a singleton vertex fetus who were randomly assigned to induction of labor at 39 to 39 4/7 weeks (n = 3,062) or expectant management (n = 3,044) until 40 5/7 to 42 2/7 weeks.
"Low risk" was defined as having no maternal or fetal indication for delivery prior to 40 5/7 weeks. Reliable gestational dating was required.
While no specific protocol for induction of labor management was required, there were 2 requests: 1) Cervical ripening was requested for an unfavorable cervix (63% of participants had a modified Bishop score <5), and 2) a duration of at least 12 hours after cervical ripening, rupture of membranes, and use of uterine stimulant was requested before performing a CD for "failed induction" (if medically appropriate).
The primary outcome was a composite of perinatal death or serious neonatal complications. The main secondary outcome was CD.
Potentially game-changing findings
The investigators found that there was no statistically significant difference between the elective induction and expectant management groups for the primary composite perinatal outcome (4.3% vs 5.4%; P = .049, with P<.046 prespecified for significance). In addition, the rate of CD was significantly lower in the labor induction group than in the expectant management group (18.6% vs 22.2%; P<.001).
Other significant findings in secondary outcomes included the following:
- Hypertensive disorders of pregnancy were significantly lower in the labor induction group compared with the expectant management group (9.1% vs 14.1%; P<.001).
- The labor induction group had a longer length of stay in the labor and delivery unit but a shorter postpartum hospital stay.
- The labor induction group reported less pain and more control during labor.
Results refute negative notion of elective labor induction
The authors concluded that in a low-risk nulliparous patient population, elective induction of labor at 39 weeks does not increase the risk for adverse perinatal outcomes and decreases the rate of CD and hypertensive disorders of pregnancy. Additionally, they noted that induction at 39 weeks should not be avoided with the goal of preventing CD, as even women with an unfavorable cervix had a lower rate of CD in the induction group compared with the expectant management group.
After publication of the ARRIVE trial findings, both ACOG and SMFM released statements supporting elective labor induction at or beyond 39 weeks’ gestation in low-risk nulliparous women with good gestational dating.2,3 They cited the following as important issues: adherence to the trial inclusion criteria except for research purposes, shared decision-making with the patient, consideration of the logistics and impact on the health care facility, and the yet unknown impact on cost. Finally, it should be a priority to avoid the primary CD for a failed induction by allowing a longer latent phase of labor, as long as maternal and fetal conditions allow. In my practice, I actively offer induction of labor to most of my patients at 39 weeks after a discussion of the risks and benefits.
Continue to: Immediate pushing in second stage...
Immediate pushing in second stage offers benefits and is preferable to delayed pushing
Cahill AG, Srinivas SK, Tita AT, et al. Effect of immediate vs delayed pushing on rates of spontaneous vaginal delivery among nulliparous women receiving neuraxial analgesia: a randomized clinical trial. JAMA. 2018;320:1444-1454.
In a randomized trial of 2,414 women, Cahill and colleagues sought to answer a seemingly simple question: What is the best timing for pushing during the second stage of labor--immediate or delayed?
Practical management of the second stage of labor (defined as complete cervical dilation to the delivery of the infant) varies by provider and setting, and previous data on pushing efforts are conflicting. Delayed pushing, or "laboring down," has been suggested to allow passive fetal rotation and to conserve maternal energy for pushing. Older studies have shown that delayed pushing decreases the rate of operative delivery. More recent study data have not demonstrated a difference between immediate and delayed pushing techniques on vaginal delivery rates and have noted that increased maternal and neonatal morbidities are associated with a longer second stage of labor.
The recent trial by Cahill and colleagues was designed to determine the effect of these 2 techniques on spontaneous vaginal delivery rates and on maternal and neonatal morbidities.4
Large study population
This randomized pragmatic trial was conducted at 6 centers in the United States. Study participants (2,404 women completed the study) were nulliparous women at 37 or more weeks' gestation with neuraxial anesthesia who were randomly assigned at complete cervical dilation either to immediate pushing (n = 1,200) or to delayed pushing, that is, instructed to wait 60 minutes before starting to push (n = 1,204). The obstetric provider determined the rest of the labor management.
The primary outcome was the rate of spontaneous vaginal delivery. Secondary outcomes included duration of the second stage of labor, duration of active pushing, operative vaginal delivery, CD, and several maternal assessments (postpartum hemorrhage, chorioamnionitis, endometritis, and perineal lacerations).
Both groups had similar vaginal delivery rates, differences in some measures
There was no difference in the primary outcome between the 2 groups: The spontaneous vaginal delivery rate was 85.9% (n = 1,031) in the immediate pushing group and 86.5% (n = 1,041) in the delayed pushing group (P = .67).
Analysis of secondary outcomes revealed several significant differences:
- decreased total time for the second stage of labor in the immediate pushing group compared with the delayed pushing group (102.4 vs 134.2 minutes) but longer active pushing time (83.7 vs 74.5 minutes)
- a lower rate of postpartum hemorrhage, chorioamnionitis in the second stage, neonatal acidemia, and suspected neonatal sepsis in the immediate pushing group
- a higher rate of third-degree perineal lacerations in the immediate pushing group.
No difference was found between groups in rates of operative vaginal deliveries, CDs, endometritis, overall perineal lacerations, or spontaneous vaginal delivery by fetal station or occiput position.
Authors' takeaway
The authors concluded that since delayed pushing does not increase spontaneous vaginal delivery rates and increases the duration of the second stage of labor and both maternal and neonatal morbidity, immediate pushing may be preferred in this patient population.
After reviewing the available literature in light of this study’s findings, ACOG released a practice advisory in October 2018 stating that “it is reasonable to choose immediate over delayed pushing in nulliparous patients with neuraxial anesthesia.”5 Nulliparous patients with neuraxial anesthesia should be counseled that delayed pushing does not increase the rate of spontaneous vaginal birth and may increase both maternal and neonatal complications. As this may be a practice change for many obstetrics units, the obstetric nursing department should be included in this education and counseling. In my practice, I would recommend immediate pushing, but it is important to include both the patient and her nurse in the discussion.
ACOG aims to optimize postpartum care
American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 736. Optimizing postpartum care. Obstet Gynecol. 2018;131:e140-e150.
In May 2018, ACOG released "Optimizing postpartum care," a committee opinion that proposes a new model of comprehensive postpartum care focused on improving both short- and long-term health outcomes for women and infants. (This replaces the June 2016 committee opinion No. 666.) Described as "the fourth trimester," the postpartum period is a critical transitional period in which both pregnancy-related and pre-existing conditions may affect maternal, neonatal, and family status; half of pregnancy-related maternal deaths occur during the postpartum period.6
The postpartum visit: Often a lost opportunity
ACOG cites that up to 40% of women in the United States do not attend their postpartum visit.6 Many aspects of the postpartum visit, including follow-up for chronic diseases, mental health screening, and contraceptive counseling, provide opportunities for acute intervention as well as establishment of healthy behaviors. Some studies have shown that postpartum depression, breastfeeding, and patient satisfaction outcomes improve as a result of postpartum engagement.
Continue to: ACOG's recommendations...
ACOG's recommendations
Ongoing process. ACOG's first proposed change concerns the structure of the postpartum visit itself, which traditionally has been a single visit with a provider at approximately 6 weeks postpartum. Postpartum care plans actually should be started before birth, during regular prenatal care, and adjusted in the hospital as needed so that the provider can educate patients about the issues they may face and resources they may need during this time. This prenatal preparation hopefully will encourage more patients to attend their postpartum visits.
Increased provider contact. Another proposed change is that after delivery, the patient should have contact with a provider within the first 3 weeks postpartum. For high-risk patients, this may involve an in-person clinic visit as soon as 3 to 10 days postpartum (for hypertensive disorders of pregnancy) or at 1 to 2 weeks (for postpartum depression screening, incision checks, and lactation issues). For lower-risk patients, a phone call may be appropriate and/or preferred. Ongoing follow-up for all patients before the final postpartum visit should be individualized.
Postpartum visit and care transition. ACOG recommends a comprehensive postpartum visit at 4 to 12 weeks to fully evaluate the woman's physical, social, and psychologic well-being and to serve as a transition from pregnancy care to well-woman care. This is a large order and includes evaluation of the following:
- mood and emotional well-being
- infant care and feeding
- sexuality, contraception, and birth spacing
- sleep and fatigue
- physical recovery from birth
- chronic disease management and transition to primary care provider
- health maintenance
- review of labor and delivery course if needed
- review of risks and recommendations for future pregnancies.
After these components are addressed, it is expected that the patient will be transitioned to a primary care provider (who may continue to be the ObGyn, as appropriate) to coordinate her future care in the primary medical home.
Useful resource for adopting new paradigm
ACOG's recommendations are somewhat daunting, and these changes will require education and resources, a significant increase in obstetric provider time and effort, and consideration of policy change regarding such issues as parental leave and postpartum care reimbursement. As a start, ACOG has developed an online aid for health care providers called "Postpartum toolkit" (https://www.acog.org/About-ACOG/ACOG-Departments/Toolkits-for-Health-Care-Providers/Postpartum-Toolkit), which provides education and resources for all steps in the process and can be individualized for each practice and patient.7
Postpartum care should be seen as an ongoing process to address both short- and long-term health outcomes for the patient, her newborn, and their family. This process should begin with planning in the antenatal period, continue with close individualized follow-up within the first 3 weeks of birth, and conclude with a comprehensive postpartum evaluation and transition to well-woman care. Shifting the paradigm of postpartum care will take considerable commitment and resources on the part of obstetric providers and their practices. In my practice, we routinely see hypertensive patients within the first week postpartum and patients at risk for postpartum depression within the first 2 weeks in our clinics. We have a standard 6-week postpartum visit for all patients as well. Going forward, we need to further determine how and when we can implement ACOG’s extensive new recommendations for optimizing postpartum care.
- Grobman WA, Rice MM, Reddy UM, et al; for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
- American College of Obstetricians and Gynecologists. Practice advisory: clinical guidance for integration of the findings of the ARRIVE trial: Labor induction versus expectant management in low-risk nulliparous women. August 2018. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Practice-Advisory-Clinical-guidance-for-integration-of-the-findings-of-The-ARRIVE-Trial. Accessed November 25, 2018.
- Society for Maternal-Fetal Medicine (SMFM) Publications Committee. SMFM statement on elective induction of labor in low-risk nulliparous women at term: the ARRIVE trial. Am J Obstet Gynecol. doi:10.1016/j.ajog.2018.08.009. In press.
- Cahill AG, Srinivas SK, Tita AT, et al. Effect of immediate vs delayed pushing on rates of spontaneous vaginal delivery among nulliparous women receiving neuraxial analgesia: a randomized clinical trial. JAMA. 2018;320:1444-1454.
- American College of Obstetricians and Gynecologists. Practice advisory: immediate versus delayed pushing in nulliparous women receiving neuraxial analgesia. October 2018. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Practice-Advisory-Immediate-vs-delayed-pushing-in-nulliparous-women-receiving-neuraxial-analgesia. Accessed November 25, 2018.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 736. Optimizing postpartum care. Obstet Gynecol. 2018;131:e140-e150.
- American College of Obstetricians and Gynecologists. ACOG Postpartum toolkit. https://www.acog.org/About-ACOG/ACOG-Departments/Toolkits-for-Health-Care-Providers/Postpartum-Toolkit. Accessed November 25, 2018.
The past year was an exciting one in obstetrics. The landmark ARRIVE trial presented at the Society for Maternal-Fetal Medicine’s (SMFM) annual meeting and subsequently published in the New England Journal of Medicine contradicted a long-held belief about the safety of elective labor induction. In a large randomized trial, Cahill and colleagues took a controversial but practical clinical question about second-stage labor management and answered it for the practicing obstetrician in the trenches. Finally, the American College of Obstetricians and Gynecologists (ACOG) placed new emphasis on the oft overlooked but increasingly more complicated postpartum period, offering guidance to support improving care for women in this transitional period.
Ultimately, this was the year of the patient, as research, clinical guidelines, and education focused on how to achieve the best in safety and quality of care for delivery planning, the delivery itself, and the so-called fourth trimester.
ARRIVE: Labor induction at 39 weeks reduces CD rate with no difference in perinatal death or serious outcomes
Grobman WA, Rice MM, Reddy UM, et al; for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
The term "elective induction of labor" has long had a negative connotation because of its association with increased CD rates and adverse perinatal outcomes. This view was based on results from older observational studies that compared outcomes for labor induction with those of spontaneous labor. In more recent observational studies that more appropriately compared labor induction with expectant management, however, elective induction of labor appears to be associated with similar CD rates and perinatal outcomes.
To test the hypothesis that elective induction would have a lower risk for perinatal death or severe neonatal complications than expectant management in low-risk nulliparous women, Grobman and colleagues conducted A Randomized Trial of Induction Versus Expectant Management (ARRIVE).1
Study population, timing of delivery, and trial outcomes
This randomized controlled trial included 6,106 women at 41 US centers in the Maternal-Fetal Medicine Units Network of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Study participants were low-risk nulliparous women with a singleton vertex fetus who were randomly assigned to induction of labor at 39 to 39 4/7 weeks (n = 3,062) or expectant management (n = 3,044) until 40 5/7 to 42 2/7 weeks.
"Low risk" was defined as having no maternal or fetal indication for delivery prior to 40 5/7 weeks. Reliable gestational dating was required.
While no specific protocol for induction of labor management was required, there were 2 requests: 1) Cervical ripening was requested for an unfavorable cervix (63% of participants had a modified Bishop score <5), and 2) a duration of at least 12 hours after cervical ripening, rupture of membranes, and use of uterine stimulant was requested before performing a CD for "failed induction" (if medically appropriate).
The primary outcome was a composite of perinatal death or serious neonatal complications. The main secondary outcome was CD.
Potentially game-changing findings
The investigators found that there was no statistically significant difference between the elective induction and expectant management groups for the primary composite perinatal outcome (4.3% vs 5.4%; P = .049, with P<.046 prespecified for significance). In addition, the rate of CD was significantly lower in the labor induction group than in the expectant management group (18.6% vs 22.2%; P<.001).
Other significant findings in secondary outcomes included the following:
- Hypertensive disorders of pregnancy were significantly lower in the labor induction group compared with the expectant management group (9.1% vs 14.1%; P<.001).
- The labor induction group had a longer length of stay in the labor and delivery unit but a shorter postpartum hospital stay.
- The labor induction group reported less pain and more control during labor.
Results refute negative notion of elective labor induction
The authors concluded that in a low-risk nulliparous patient population, elective induction of labor at 39 weeks does not increase the risk for adverse perinatal outcomes and decreases the rate of CD and hypertensive disorders of pregnancy. Additionally, they noted that induction at 39 weeks should not be avoided with the goal of preventing CD, as even women with an unfavorable cervix had a lower rate of CD in the induction group compared with the expectant management group.
After publication of the ARRIVE trial findings, both ACOG and SMFM released statements supporting elective labor induction at or beyond 39 weeks’ gestation in low-risk nulliparous women with good gestational dating.2,3 They cited the following as important issues: adherence to the trial inclusion criteria except for research purposes, shared decision-making with the patient, consideration of the logistics and impact on the health care facility, and the yet unknown impact on cost. Finally, it should be a priority to avoid the primary CD for a failed induction by allowing a longer latent phase of labor, as long as maternal and fetal conditions allow. In my practice, I actively offer induction of labor to most of my patients at 39 weeks after a discussion of the risks and benefits.
Continue to: Immediate pushing in second stage...
Immediate pushing in second stage offers benefits and is preferable to delayed pushing
Cahill AG, Srinivas SK, Tita AT, et al. Effect of immediate vs delayed pushing on rates of spontaneous vaginal delivery among nulliparous women receiving neuraxial analgesia: a randomized clinical trial. JAMA. 2018;320:1444-1454.
In a randomized trial of 2,414 women, Cahill and colleagues sought to answer a seemingly simple question: What is the best timing for pushing during the second stage of labor--immediate or delayed?
Practical management of the second stage of labor (defined as complete cervical dilation to the delivery of the infant) varies by provider and setting, and previous data on pushing efforts are conflicting. Delayed pushing, or "laboring down," has been suggested to allow passive fetal rotation and to conserve maternal energy for pushing. Older studies have shown that delayed pushing decreases the rate of operative delivery. More recent study data have not demonstrated a difference between immediate and delayed pushing techniques on vaginal delivery rates and have noted that increased maternal and neonatal morbidities are associated with a longer second stage of labor.
The recent trial by Cahill and colleagues was designed to determine the effect of these 2 techniques on spontaneous vaginal delivery rates and on maternal and neonatal morbidities.4
Large study population
This randomized pragmatic trial was conducted at 6 centers in the United States. Study participants (2,404 women completed the study) were nulliparous women at 37 or more weeks' gestation with neuraxial anesthesia who were randomly assigned at complete cervical dilation either to immediate pushing (n = 1,200) or to delayed pushing, that is, instructed to wait 60 minutes before starting to push (n = 1,204). The obstetric provider determined the rest of the labor management.
The primary outcome was the rate of spontaneous vaginal delivery. Secondary outcomes included duration of the second stage of labor, duration of active pushing, operative vaginal delivery, CD, and several maternal assessments (postpartum hemorrhage, chorioamnionitis, endometritis, and perineal lacerations).
Both groups had similar vaginal delivery rates, differences in some measures
There was no difference in the primary outcome between the 2 groups: The spontaneous vaginal delivery rate was 85.9% (n = 1,031) in the immediate pushing group and 86.5% (n = 1,041) in the delayed pushing group (P = .67).
Analysis of secondary outcomes revealed several significant differences:
- decreased total time for the second stage of labor in the immediate pushing group compared with the delayed pushing group (102.4 vs 134.2 minutes) but longer active pushing time (83.7 vs 74.5 minutes)
- a lower rate of postpartum hemorrhage, chorioamnionitis in the second stage, neonatal acidemia, and suspected neonatal sepsis in the immediate pushing group
- a higher rate of third-degree perineal lacerations in the immediate pushing group.
No difference was found between groups in rates of operative vaginal deliveries, CDs, endometritis, overall perineal lacerations, or spontaneous vaginal delivery by fetal station or occiput position.
Authors' takeaway
The authors concluded that since delayed pushing does not increase spontaneous vaginal delivery rates and increases the duration of the second stage of labor and both maternal and neonatal morbidity, immediate pushing may be preferred in this patient population.
After reviewing the available literature in light of this study’s findings, ACOG released a practice advisory in October 2018 stating that “it is reasonable to choose immediate over delayed pushing in nulliparous patients with neuraxial anesthesia.”5 Nulliparous patients with neuraxial anesthesia should be counseled that delayed pushing does not increase the rate of spontaneous vaginal birth and may increase both maternal and neonatal complications. As this may be a practice change for many obstetrics units, the obstetric nursing department should be included in this education and counseling. In my practice, I would recommend immediate pushing, but it is important to include both the patient and her nurse in the discussion.
ACOG aims to optimize postpartum care
American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 736. Optimizing postpartum care. Obstet Gynecol. 2018;131:e140-e150.
In May 2018, ACOG released "Optimizing postpartum care," a committee opinion that proposes a new model of comprehensive postpartum care focused on improving both short- and long-term health outcomes for women and infants. (This replaces the June 2016 committee opinion No. 666.) Described as "the fourth trimester," the postpartum period is a critical transitional period in which both pregnancy-related and pre-existing conditions may affect maternal, neonatal, and family status; half of pregnancy-related maternal deaths occur during the postpartum period.6
The postpartum visit: Often a lost opportunity
ACOG cites that up to 40% of women in the United States do not attend their postpartum visit.6 Many aspects of the postpartum visit, including follow-up for chronic diseases, mental health screening, and contraceptive counseling, provide opportunities for acute intervention as well as establishment of healthy behaviors. Some studies have shown that postpartum depression, breastfeeding, and patient satisfaction outcomes improve as a result of postpartum engagement.
Continue to: ACOG's recommendations...
ACOG's recommendations
Ongoing process. ACOG's first proposed change concerns the structure of the postpartum visit itself, which traditionally has been a single visit with a provider at approximately 6 weeks postpartum. Postpartum care plans actually should be started before birth, during regular prenatal care, and adjusted in the hospital as needed so that the provider can educate patients about the issues they may face and resources they may need during this time. This prenatal preparation hopefully will encourage more patients to attend their postpartum visits.
Increased provider contact. Another proposed change is that after delivery, the patient should have contact with a provider within the first 3 weeks postpartum. For high-risk patients, this may involve an in-person clinic visit as soon as 3 to 10 days postpartum (for hypertensive disorders of pregnancy) or at 1 to 2 weeks (for postpartum depression screening, incision checks, and lactation issues). For lower-risk patients, a phone call may be appropriate and/or preferred. Ongoing follow-up for all patients before the final postpartum visit should be individualized.
Postpartum visit and care transition. ACOG recommends a comprehensive postpartum visit at 4 to 12 weeks to fully evaluate the woman's physical, social, and psychologic well-being and to serve as a transition from pregnancy care to well-woman care. This is a large order and includes evaluation of the following:
- mood and emotional well-being
- infant care and feeding
- sexuality, contraception, and birth spacing
- sleep and fatigue
- physical recovery from birth
- chronic disease management and transition to primary care provider
- health maintenance
- review of labor and delivery course if needed
- review of risks and recommendations for future pregnancies.
After these components are addressed, it is expected that the patient will be transitioned to a primary care provider (who may continue to be the ObGyn, as appropriate) to coordinate her future care in the primary medical home.
Useful resource for adopting new paradigm
ACOG's recommendations are somewhat daunting, and these changes will require education and resources, a significant increase in obstetric provider time and effort, and consideration of policy change regarding such issues as parental leave and postpartum care reimbursement. As a start, ACOG has developed an online aid for health care providers called "Postpartum toolkit" (https://www.acog.org/About-ACOG/ACOG-Departments/Toolkits-for-Health-Care-Providers/Postpartum-Toolkit), which provides education and resources for all steps in the process and can be individualized for each practice and patient.7
Postpartum care should be seen as an ongoing process to address both short- and long-term health outcomes for the patient, her newborn, and their family. This process should begin with planning in the antenatal period, continue with close individualized follow-up within the first 3 weeks of birth, and conclude with a comprehensive postpartum evaluation and transition to well-woman care. Shifting the paradigm of postpartum care will take considerable commitment and resources on the part of obstetric providers and their practices. In my practice, we routinely see hypertensive patients within the first week postpartum and patients at risk for postpartum depression within the first 2 weeks in our clinics. We have a standard 6-week postpartum visit for all patients as well. Going forward, we need to further determine how and when we can implement ACOG’s extensive new recommendations for optimizing postpartum care.
The past year was an exciting one in obstetrics. The landmark ARRIVE trial presented at the Society for Maternal-Fetal Medicine’s (SMFM) annual meeting and subsequently published in the New England Journal of Medicine contradicted a long-held belief about the safety of elective labor induction. In a large randomized trial, Cahill and colleagues took a controversial but practical clinical question about second-stage labor management and answered it for the practicing obstetrician in the trenches. Finally, the American College of Obstetricians and Gynecologists (ACOG) placed new emphasis on the oft overlooked but increasingly more complicated postpartum period, offering guidance to support improving care for women in this transitional period.
Ultimately, this was the year of the patient, as research, clinical guidelines, and education focused on how to achieve the best in safety and quality of care for delivery planning, the delivery itself, and the so-called fourth trimester.
ARRIVE: Labor induction at 39 weeks reduces CD rate with no difference in perinatal death or serious outcomes
Grobman WA, Rice MM, Reddy UM, et al; for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
The term "elective induction of labor" has long had a negative connotation because of its association with increased CD rates and adverse perinatal outcomes. This view was based on results from older observational studies that compared outcomes for labor induction with those of spontaneous labor. In more recent observational studies that more appropriately compared labor induction with expectant management, however, elective induction of labor appears to be associated with similar CD rates and perinatal outcomes.
To test the hypothesis that elective induction would have a lower risk for perinatal death or severe neonatal complications than expectant management in low-risk nulliparous women, Grobman and colleagues conducted A Randomized Trial of Induction Versus Expectant Management (ARRIVE).1
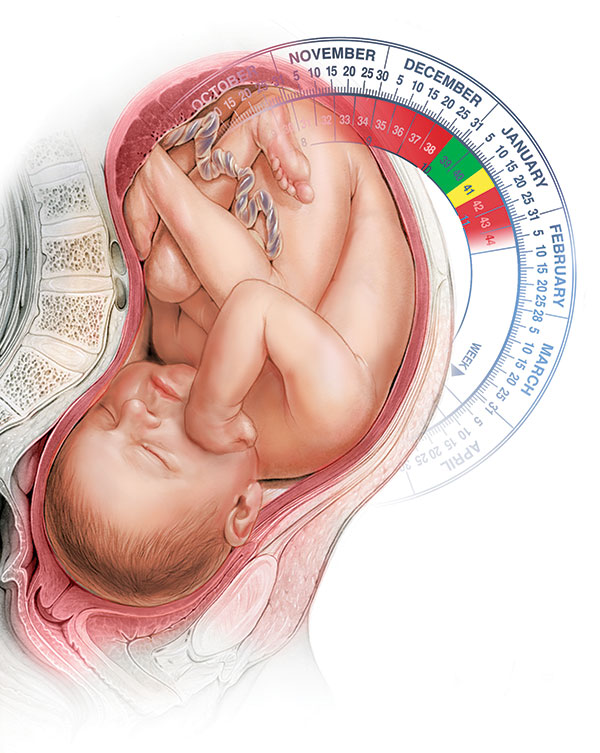
Study population, timing of delivery, and trial outcomes
This randomized controlled trial included 6,106 women at 41 US centers in the Maternal-Fetal Medicine Units Network of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Study participants were low-risk nulliparous women with a singleton vertex fetus who were randomly assigned to induction of labor at 39 to 39 4/7 weeks (n = 3,062) or expectant management (n = 3,044) until 40 5/7 to 42 2/7 weeks.
"Low risk" was defined as having no maternal or fetal indication for delivery prior to 40 5/7 weeks. Reliable gestational dating was required.
While no specific protocol for induction of labor management was required, there were 2 requests: 1) Cervical ripening was requested for an unfavorable cervix (63% of participants had a modified Bishop score <5), and 2) a duration of at least 12 hours after cervical ripening, rupture of membranes, and use of uterine stimulant was requested before performing a CD for "failed induction" (if medically appropriate).
The primary outcome was a composite of perinatal death or serious neonatal complications. The main secondary outcome was CD.
Potentially game-changing findings
The investigators found that there was no statistically significant difference between the elective induction and expectant management groups for the primary composite perinatal outcome (4.3% vs 5.4%; P = .049, with P<.046 prespecified for significance). In addition, the rate of CD was significantly lower in the labor induction group than in the expectant management group (18.6% vs 22.2%; P<.001).
Other significant findings in secondary outcomes included the following:
- Hypertensive disorders of pregnancy were significantly lower in the labor induction group compared with the expectant management group (9.1% vs 14.1%; P<.001).
- The labor induction group had a longer length of stay in the labor and delivery unit but a shorter postpartum hospital stay.
- The labor induction group reported less pain and more control during labor.
Results refute negative notion of elective labor induction
The authors concluded that in a low-risk nulliparous patient population, elective induction of labor at 39 weeks does not increase the risk for adverse perinatal outcomes and decreases the rate of CD and hypertensive disorders of pregnancy. Additionally, they noted that induction at 39 weeks should not be avoided with the goal of preventing CD, as even women with an unfavorable cervix had a lower rate of CD in the induction group compared with the expectant management group.
After publication of the ARRIVE trial findings, both ACOG and SMFM released statements supporting elective labor induction at or beyond 39 weeks’ gestation in low-risk nulliparous women with good gestational dating.2,3 They cited the following as important issues: adherence to the trial inclusion criteria except for research purposes, shared decision-making with the patient, consideration of the logistics and impact on the health care facility, and the yet unknown impact on cost. Finally, it should be a priority to avoid the primary CD for a failed induction by allowing a longer latent phase of labor, as long as maternal and fetal conditions allow. In my practice, I actively offer induction of labor to most of my patients at 39 weeks after a discussion of the risks and benefits.
Continue to: Immediate pushing in second stage...
Immediate pushing in second stage offers benefits and is preferable to delayed pushing
Cahill AG, Srinivas SK, Tita AT, et al. Effect of immediate vs delayed pushing on rates of spontaneous vaginal delivery among nulliparous women receiving neuraxial analgesia: a randomized clinical trial. JAMA. 2018;320:1444-1454.
In a randomized trial of 2,414 women, Cahill and colleagues sought to answer a seemingly simple question: What is the best timing for pushing during the second stage of labor--immediate or delayed?
Practical management of the second stage of labor (defined as complete cervical dilation to the delivery of the infant) varies by provider and setting, and previous data on pushing efforts are conflicting. Delayed pushing, or "laboring down," has been suggested to allow passive fetal rotation and to conserve maternal energy for pushing. Older studies have shown that delayed pushing decreases the rate of operative delivery. More recent study data have not demonstrated a difference between immediate and delayed pushing techniques on vaginal delivery rates and have noted that increased maternal and neonatal morbidities are associated with a longer second stage of labor.
The recent trial by Cahill and colleagues was designed to determine the effect of these 2 techniques on spontaneous vaginal delivery rates and on maternal and neonatal morbidities.4
Large study population
This randomized pragmatic trial was conducted at 6 centers in the United States. Study participants (2,404 women completed the study) were nulliparous women at 37 or more weeks' gestation with neuraxial anesthesia who were randomly assigned at complete cervical dilation either to immediate pushing (n = 1,200) or to delayed pushing, that is, instructed to wait 60 minutes before starting to push (n = 1,204). The obstetric provider determined the rest of the labor management.
The primary outcome was the rate of spontaneous vaginal delivery. Secondary outcomes included duration of the second stage of labor, duration of active pushing, operative vaginal delivery, CD, and several maternal assessments (postpartum hemorrhage, chorioamnionitis, endometritis, and perineal lacerations).
Both groups had similar vaginal delivery rates, differences in some measures
There was no difference in the primary outcome between the 2 groups: The spontaneous vaginal delivery rate was 85.9% (n = 1,031) in the immediate pushing group and 86.5% (n = 1,041) in the delayed pushing group (P = .67).
Analysis of secondary outcomes revealed several significant differences:
- decreased total time for the second stage of labor in the immediate pushing group compared with the delayed pushing group (102.4 vs 134.2 minutes) but longer active pushing time (83.7 vs 74.5 minutes)
- a lower rate of postpartum hemorrhage, chorioamnionitis in the second stage, neonatal acidemia, and suspected neonatal sepsis in the immediate pushing group
- a higher rate of third-degree perineal lacerations in the immediate pushing group.
No difference was found between groups in rates of operative vaginal deliveries, CDs, endometritis, overall perineal lacerations, or spontaneous vaginal delivery by fetal station or occiput position.
Authors' takeaway
The authors concluded that since delayed pushing does not increase spontaneous vaginal delivery rates and increases the duration of the second stage of labor and both maternal and neonatal morbidity, immediate pushing may be preferred in this patient population.
After reviewing the available literature in light of this study’s findings, ACOG released a practice advisory in October 2018 stating that “it is reasonable to choose immediate over delayed pushing in nulliparous patients with neuraxial anesthesia.”5 Nulliparous patients with neuraxial anesthesia should be counseled that delayed pushing does not increase the rate of spontaneous vaginal birth and may increase both maternal and neonatal complications. As this may be a practice change for many obstetrics units, the obstetric nursing department should be included in this education and counseling. In my practice, I would recommend immediate pushing, but it is important to include both the patient and her nurse in the discussion.
ACOG aims to optimize postpartum care
American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 736. Optimizing postpartum care. Obstet Gynecol. 2018;131:e140-e150.
In May 2018, ACOG released "Optimizing postpartum care," a committee opinion that proposes a new model of comprehensive postpartum care focused on improving both short- and long-term health outcomes for women and infants. (This replaces the June 2016 committee opinion No. 666.) Described as "the fourth trimester," the postpartum period is a critical transitional period in which both pregnancy-related and pre-existing conditions may affect maternal, neonatal, and family status; half of pregnancy-related maternal deaths occur during the postpartum period.6
The postpartum visit: Often a lost opportunity
ACOG cites that up to 40% of women in the United States do not attend their postpartum visit.6 Many aspects of the postpartum visit, including follow-up for chronic diseases, mental health screening, and contraceptive counseling, provide opportunities for acute intervention as well as establishment of healthy behaviors. Some studies have shown that postpartum depression, breastfeeding, and patient satisfaction outcomes improve as a result of postpartum engagement.
Continue to: ACOG's recommendations...
ACOG's recommendations
Ongoing process. ACOG's first proposed change concerns the structure of the postpartum visit itself, which traditionally has been a single visit with a provider at approximately 6 weeks postpartum. Postpartum care plans actually should be started before birth, during regular prenatal care, and adjusted in the hospital as needed so that the provider can educate patients about the issues they may face and resources they may need during this time. This prenatal preparation hopefully will encourage more patients to attend their postpartum visits.
Increased provider contact. Another proposed change is that after delivery, the patient should have contact with a provider within the first 3 weeks postpartum. For high-risk patients, this may involve an in-person clinic visit as soon as 3 to 10 days postpartum (for hypertensive disorders of pregnancy) or at 1 to 2 weeks (for postpartum depression screening, incision checks, and lactation issues). For lower-risk patients, a phone call may be appropriate and/or preferred. Ongoing follow-up for all patients before the final postpartum visit should be individualized.
Postpartum visit and care transition. ACOG recommends a comprehensive postpartum visit at 4 to 12 weeks to fully evaluate the woman's physical, social, and psychologic well-being and to serve as a transition from pregnancy care to well-woman care. This is a large order and includes evaluation of the following:
- mood and emotional well-being
- infant care and feeding
- sexuality, contraception, and birth spacing
- sleep and fatigue
- physical recovery from birth
- chronic disease management and transition to primary care provider
- health maintenance
- review of labor and delivery course if needed
- review of risks and recommendations for future pregnancies.
After these components are addressed, it is expected that the patient will be transitioned to a primary care provider (who may continue to be the ObGyn, as appropriate) to coordinate her future care in the primary medical home.
Useful resource for adopting new paradigm
ACOG's recommendations are somewhat daunting, and these changes will require education and resources, a significant increase in obstetric provider time and effort, and consideration of policy change regarding such issues as parental leave and postpartum care reimbursement. As a start, ACOG has developed an online aid for health care providers called "Postpartum toolkit" (https://www.acog.org/About-ACOG/ACOG-Departments/Toolkits-for-Health-Care-Providers/Postpartum-Toolkit), which provides education and resources for all steps in the process and can be individualized for each practice and patient.7
Postpartum care should be seen as an ongoing process to address both short- and long-term health outcomes for the patient, her newborn, and their family. This process should begin with planning in the antenatal period, continue with close individualized follow-up within the first 3 weeks of birth, and conclude with a comprehensive postpartum evaluation and transition to well-woman care. Shifting the paradigm of postpartum care will take considerable commitment and resources on the part of obstetric providers and their practices. In my practice, we routinely see hypertensive patients within the first week postpartum and patients at risk for postpartum depression within the first 2 weeks in our clinics. We have a standard 6-week postpartum visit for all patients as well. Going forward, we need to further determine how and when we can implement ACOG’s extensive new recommendations for optimizing postpartum care.
- Grobman WA, Rice MM, Reddy UM, et al; for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
- American College of Obstetricians and Gynecologists. Practice advisory: clinical guidance for integration of the findings of the ARRIVE trial: Labor induction versus expectant management in low-risk nulliparous women. August 2018. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Practice-Advisory-Clinical-guidance-for-integration-of-the-findings-of-The-ARRIVE-Trial. Accessed November 25, 2018.
- Society for Maternal-Fetal Medicine (SMFM) Publications Committee. SMFM statement on elective induction of labor in low-risk nulliparous women at term: the ARRIVE trial. Am J Obstet Gynecol. doi:10.1016/j.ajog.2018.08.009. In press.
- Cahill AG, Srinivas SK, Tita AT, et al. Effect of immediate vs delayed pushing on rates of spontaneous vaginal delivery among nulliparous women receiving neuraxial analgesia: a randomized clinical trial. JAMA. 2018;320:1444-1454.
- American College of Obstetricians and Gynecologists. Practice advisory: immediate versus delayed pushing in nulliparous women receiving neuraxial analgesia. October 2018. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Practice-Advisory-Immediate-vs-delayed-pushing-in-nulliparous-women-receiving-neuraxial-analgesia. Accessed November 25, 2018.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 736. Optimizing postpartum care. Obstet Gynecol. 2018;131:e140-e150.
- American College of Obstetricians and Gynecologists. ACOG Postpartum toolkit. https://www.acog.org/About-ACOG/ACOG-Departments/Toolkits-for-Health-Care-Providers/Postpartum-Toolkit. Accessed November 25, 2018.
- Grobman WA, Rice MM, Reddy UM, et al; for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
- American College of Obstetricians and Gynecologists. Practice advisory: clinical guidance for integration of the findings of the ARRIVE trial: Labor induction versus expectant management in low-risk nulliparous women. August 2018. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Practice-Advisory-Clinical-guidance-for-integration-of-the-findings-of-The-ARRIVE-Trial. Accessed November 25, 2018.
- Society for Maternal-Fetal Medicine (SMFM) Publications Committee. SMFM statement on elective induction of labor in low-risk nulliparous women at term: the ARRIVE trial. Am J Obstet Gynecol. doi:10.1016/j.ajog.2018.08.009. In press.
- Cahill AG, Srinivas SK, Tita AT, et al. Effect of immediate vs delayed pushing on rates of spontaneous vaginal delivery among nulliparous women receiving neuraxial analgesia: a randomized clinical trial. JAMA. 2018;320:1444-1454.
- American College of Obstetricians and Gynecologists. Practice advisory: immediate versus delayed pushing in nulliparous women receiving neuraxial analgesia. October 2018. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Practice-Advisory-Immediate-vs-delayed-pushing-in-nulliparous-women-receiving-neuraxial-analgesia. Accessed November 25, 2018.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 736. Optimizing postpartum care. Obstet Gynecol. 2018;131:e140-e150.
- American College of Obstetricians and Gynecologists. ACOG Postpartum toolkit. https://www.acog.org/About-ACOG/ACOG-Departments/Toolkits-for-Health-Care-Providers/Postpartum-Toolkit. Accessed November 25, 2018.
2018 Update on obstetrics
The past year brought new information and guidance from the American College of Obstetricians and Gynecologists (ACOG) on many relevant obstetric topics, making it difficult to choose just a few for this Update. Opioid use in pregnancy was an obvious choice given the national media attention and the potential opportunity for intervention in pregnancy for both the mother and the fetus/newborn. Postpartum hemorrhage, an “oldie but goodie,” was chosen for several reasons: It got a new definition, a new focus on multidisciplinary care, and an exciting novel tool for the treatment toolbox. Finally, given the rapidly changing technology, new screening recommendations, and the complexity of counseling, carrier screening was chosen as a genetic hot topic for this year.
Opioids, obstetrics, and opportunities
Reddy UM, Davis JM, Ren Z, Greene MF; Opioid Use in Pregnancy, Neonatal Abstinence Syndrome, and Childhood Outcomes Workshop Invited Speakers. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes: Executive summary of a joint workshop. Obstet Gynecol. 2017;130(1):10-28.
ACOG Committee on Obstetric Practice. ACOG committee opinion No. 711: Opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130(2):e81-e94.
The term "opioid epidemic" is omnipresent in both the lay media and the medical literature. In the past decade, the United States has had a huge increase in the number of opioid prescriptions, the rate of admissions and deaths due to prescription opioid misuse and abuse, and an increased rate of heroin use attributed to prior prescription opioid use.
Obstetrics is unique in that opioid use and abuse disorders affect 2 patients simultaneously (the mother and fetus), and the treatment options are somewhat at odds in that they need to balance a stable maternal status and intrauterine environment with the risk of neonatal abstinence syndrome (NAS). Additionally, pregnancy is an opportunity for a woman with opioid use disorder to have access to medical care (possibly for the first time) leading to the diagnosis and treatment of her disease. As the clinicians on the front line, obstetricians therefore require education and guidance on best practice for management of opioid use in pregnancy.
In 2017, Reddy and colleagues, as part of a joint workshop on opioid use in pregnancy, and a committee opinion from ACOG provided the following recommendations.
Screening
Universally screen for substance use, starting at the first prenatal visit; this is recommended over risk factor-based screening.
Use a validated screening tool. A tool such as a questionnaire is recommended as the first-line screening test (for example, the 4Ps screen, the National Institute on Drug Abuse Quick Screen, and the CRAFFT Screening Interview).
Do not universally screen urine and hair for drugs. This type of screening has many limitations, such as the limited number of substances tested, false-positive results, and inaccurate determination of the frequency or timing of drug use. Information regarding the consequences of the test must be provided, and patient consent must be obtained prior to performing the test.
Treatment
Use medication-assisted treatment with buprenorphine or methadone, which is preferred to medically supervised withdrawal. Medication-assisted treatment prevents withdrawal symptoms and cravings, decreases the risk of relapse, improves compliance with prenatal care and addiction treatment programs, and leads to better obstetric outcomes (higher birth weight, lower rate of preterm birth, lower perinatal mortality).
Know that buprenorphine has several advantages over methadone, including the convenience of an outpatient prescription, a lower risk of overdose, and improved neonatal outcomes (higher birth weight, lower doses of morphine to treat NAS, shorter treatment duration).
Prioritize methadone as the preferred option for pregnant women who are already receiving methadone treatment (changing to buprenorphine may precipitate withdrawal), those with a long-standing history of or multi-substance abuse, and those who have failed other treatment programs.
Prenatal care
Screen for comorbid conditions such as sexually transmitted infections, other medications or substance use, social conditions, and mental health disorders.
Perform ultrasonography serially to monitor fetal growth because of the increased risk of fetal growth restriction.
Consult with anesthesiology for pain control recommendations for labor and delivery and with neonatalogy/pediatrics for NAS counseling.
Intrapartum/postpartum care
Recognize heightened pain. Women with opioid use disorder have increased sensitivity to painful stimuli.
Continue the maintenance dose of methadone or buprenorphine throughout hospitalization, with short-acting opioids added for a brief period for postoperative pain.
Prioritize regional anesthesia for pain control in labor or for cesarean delivery.
Consider alternative therapies such as regional blocks, nonopioid medications (nonsteroidal anti-inflammatory drugs, acetaminophen), or relaxation/mindfulness training.
Avoid mixed antagonist and agonist narcotics (butorphanol, nalbuphine, pentazocine) as they may cause acute withdrawal.
Encourage breastfeeding to decrease the severity of NAS and maternal stress and increase maternal-child bonding and maternal confidence.
Offer contraceptive counseling and services immediately postpartum in the hospital, with strong consideration for long-acting reversible contraception.
Opioid prescribing practices
Opioids are prescribed in excess post–cesarean delivery. Several recent studies have demonstrated that most women are prescribed opioids post–cesarean delivery in excess of the amount they use (median 30–40 tablets prescribed, median 20 tablets used).1,2 The leftover opioid medication usually is not discarded and therefore is at risk for diversion or misuse. A small subset of patients will use all the opioids prescribed and feel as though they have not received enough medication.
Prescribe post–cesarean delivery opioids more appropriately by considering individual inpatient opioid requirements or a shared decision-making model.3
Prioritize acetaminophen and ibuprofen during breastfeeding. In a recent editorial in OBG Management, Robert L. Barbieri, MD, recommended that whenever possible, acetaminophen and ibuprofen should be the first-line treatment for breastfeeding women, and narcotics that are metabolized by CYP2D6 should be avoided to reduce the risk to the newborn.4
Universal screening for substance use should be performed in all pregnant women, and clinicians should offer medication-assisted treatment in conjunction with prenatal care and other supportive services as the standard therapy for opioid use disorder. More selective, patient-specific opioid prescribing practices should be applied in the obstetric population.
Read about new strategies for postpartum hemorrhage.
Postpartum hemorrhage: New definitions and new strategies for stemming the flow
ACOG Committee on Practice Bulletins—Obstetrics. ACOG practice bulletin No. 183: Postpartum hemorrhage. Obstet Gynecol. 2017;130(4):e168-e186.
From the very first sentence of the new ACOG practice bulletin, postpartum hemorrhage (PPH) is redefined as "cumulative blood loss greater than or equal to 1,000 mL or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours after the birth process (includes intrapartum loss) regardless of route of delivery." Although this does not seem to be a huge change from the traditional teaching of a 500-mL blood loss at vaginal delivery and a 1,000-mL loss at cesarean delivery, it reflects a shift in focus from simply responding to a certain amount of bleeding to using a multidisciplinary action plan for treating this leading cause of maternal mortality worldwide.
Focus on developing a PPH action plan
As part of the shift toward a multidisciplinary action plan for PPH, all obstetric team members should be aware of the following:
- For most postpartum women, by the time they begin to show signs of hemodynamic compromise, the amount of blood loss approaches 25% of their total blood volume (1,500 mL). Lactic acidosis, systemic inflammation, and a consumptive coagulopathy result.
- Risk stratification prior to delivery, recognition and identification of the source of bleeding, and aggressive early resuscitation to prevent hypovolemia are paramount. Experience gleaned from trauma massive transfusion protocols suggests that judicious transfusion of packed red blood cells, fresh frozen plasma, and platelets in a 1:1:1 ratio is appropriate for obstetric patients. Additionally, patients with low fibrinogen levels should be treated with cryoprecipitate.
- The use of fixed transfusion ratios and standardized protocols for recognition and management of PPH has been demonstrated to increase earlier intervention and resolution of hemorrhage at an earlier stage, although the maternal outcomes results have been mixed.
- Multidisciplinary team drills and simulation exercises also should be considered to help solidify training of an institution's teams responsible for PPH response.
Novel management option: Tranexamic acid
In addition to these strategies, there is a new recommendation for managing refractory PPH: tranexamic acid, which works by binding to lysine receptors on plasminogen and plasmin, inhibiting plasmin-mediated fibrin degradation.5 Previously, tranexamic acid was known to be effective in trauma, heart surgery, and in patients with thrombophilias. Pacheco and colleagues recently demonstrated reduced mortality from obstetric bleeding if tranexamic acid was given within 3 hours of delivery, without increased thrombotic complications.5 ACOG recommends its use if initial medical therapy fails, while the World Health Organization strongly recommends that tranexamic acid be part of a standard PPH package for all cases of PPH (TABLE).6
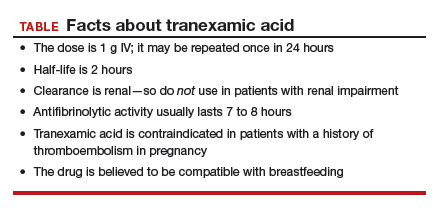
Postpartum hemorrhage requires early, aggressive, and multidisciplinary coordination to ensure that 1) patients at risk for hemorrhage are identified for preventive measures; 2) existing hemorrhage is recognized and quickly treated, first with noninvasive methods and then with more definitive surgical treatments; and 3) blood product replacement follows an evidence-based standardized protocol. Tranexamic acid is recommended as an adjunct treatment for PPH (of any cause) and should be used within 3 hours of delivery.
Read about new ACOG guidance on prepregnancy and prenatal screening.
Carrier screening—choose something
ACOG Committee on Genetics. Committee opinion No. 690: Carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129(3):e35-e40.
ACOG Committee on Genetics. Committee opinion No. 691: Carrier screening for genetic conditions. Obstet Gynecol. 2017;129(3):e41-e55.
Ideally, carrier screening should be offered prior to pregnancy to fully inform couples of their reproductive risks and options for pregnancy. If not performed in the preconception period, carrier screening should be offered to all pregnant women. If a patient chooses screening and screens positive for a particular disorder, her reproductive partner should then be offered screening so that the risk of having an affected child can be determined.
New ACOG guidance on prepregnancy and prenatal screening
Carrier screening recommendations have evolved as the technology available has expanded. All 3 of the following strategies now are considered "acceptable" according to 2 recently published ACOG committee opinions.
Traditional ethnic-specific carrier screening, previously ACOG's sole recommendation, involves offering specific genetic screening to patients from populations with a high prevalence for certain conditions. One such example is Tay-Sachs disease screening in Ashkenazi Jewish patients.
Panethnic screening, which takes into account mixed or uncertain backgrounds, involves screening for a certain panel of disorders and is available to all patients regardless of their background (for example, cystic fibrosis screening offered to all pregnant patients).
Expanded carrier screening is when a large number of disorders can be screened for simultaneously for a lower cost than previous testing strategies. Expanded carrier screening panels vary in number and which conditions are tested by the laboratory. An ideal expanded carrier screening panel has been debated in the literature but not agreed on.7
ObGyns and practices therefore are encouraged to develop a standard counseling and screening protocol to offer to all their patients while being flexible to make available any patient-requested screening that is outside their protocol. Pretest and posttest counseling, including a thorough family history, is essential (as with any genetic testing) and should include residual risk after testing, potential need for specific familial mutation testing instead of general carrier screening, and issues with consanguinity.
Three essential screens
Regardless of the screening strategy chosen from the above options, 3 screening tests should be offered to all pregnant women or couples considering pregnancy (either individually or in the context of an expanded screening panel):
- Cystic fibrosis. At the least, a panel of the 23 most common mutations should be used. More expanded panels, which include hundreds of mutations, increase detection in non-Caucasian populations and for milder forms of the disease or infertility-related mutations.
- Hemoglobinopathies (sickle cell, α- and β-thalassemia). Complete blood count and red blood indices are recommended for all, with hemoglobin electrophoresis recommended for patients of African, Middle Eastern, Mediterranean, or West Indian descent or if mean corpuscular volume is low.
- Spinal muscular atrophy (SMA). The most recent addition to ACOG's recommendations for general carrier screening due to the relatively high carrier frequency (1-in-40 to 1-in-60) and the severity of the disease, SMA causes degeneration of the spinal cord neurons, skeletal muscular atrophy, and overall weakness. Screening is via polymerase chain reaction for SMN1 copy number: 2 copies are normal, and 1 copy indicates a carrier of the SMN1 deletion. About 3% to 4% of patients will screen negative but still will be "carriers" due to having 2 copies of the SMN1 gene on 1 chromosome and no copies on the other chromosome.
All pregnant patients or patients considering pregnancy should be offered carrier screening as standard reproductive care, including screening for cystic fibrosis, hemoglobinopathies, and spinal muscular atrophy. Ethnic, panethnic, or expanded carrier screening (and patient-requested specific screening) all are acceptable options, and a standard screening and counseling protocol should be determined by the ObGyn or practice.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130(1):29–35.
- Osmundson SS, Schornack LA, Grasch JL, Zuckerwise LC, Young JL, Richardson MD. Postdischarge opioid use after cesarean delivery. Obstet Gynecol. 2017;130(1):36–41.
- Prabhu M, McQuaid-Hanson E, Hopp S, et al. A shared decision-making intervention to guide opioid prescribing after cesarean delivery. Obstet Gynecol. 2017;130(1):42–46.
- Barbieri RL. Stop using codeine, oxycodone, hydrocodone, tramadol, and aspirin in women who are breastfeeding. OBG Manag. 2017;29(10):8–12.
- Pacheco LD, Hankins GD, Saad AF, Costantine MM, Chiossi G, Saade GR. Tranexamic acid for the management of obstetric hemorrhage. Obstet Gynecol. 2017;130(4);765–769.
- WHO recommendation on tranexamic acid for the treatment of postpartum haemorrhage. Geneva, Switzerland: World Health Organization; 2017.
- Stevens B, Krstic N, Jones M, Murphy L, Hoskovec J. Finding middle ground in constructing a clinically useful expanded carrier screening panel. Obstet Gynecol. 2017;130(2):279–284.
The past year brought new information and guidance from the American College of Obstetricians and Gynecologists (ACOG) on many relevant obstetric topics, making it difficult to choose just a few for this Update. Opioid use in pregnancy was an obvious choice given the national media attention and the potential opportunity for intervention in pregnancy for both the mother and the fetus/newborn. Postpartum hemorrhage, an “oldie but goodie,” was chosen for several reasons: It got a new definition, a new focus on multidisciplinary care, and an exciting novel tool for the treatment toolbox. Finally, given the rapidly changing technology, new screening recommendations, and the complexity of counseling, carrier screening was chosen as a genetic hot topic for this year.
Opioids, obstetrics, and opportunities
Reddy UM, Davis JM, Ren Z, Greene MF; Opioid Use in Pregnancy, Neonatal Abstinence Syndrome, and Childhood Outcomes Workshop Invited Speakers. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes: Executive summary of a joint workshop. Obstet Gynecol. 2017;130(1):10-28.
ACOG Committee on Obstetric Practice. ACOG committee opinion No. 711: Opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130(2):e81-e94.
The term "opioid epidemic" is omnipresent in both the lay media and the medical literature. In the past decade, the United States has had a huge increase in the number of opioid prescriptions, the rate of admissions and deaths due to prescription opioid misuse and abuse, and an increased rate of heroin use attributed to prior prescription opioid use.
Obstetrics is unique in that opioid use and abuse disorders affect 2 patients simultaneously (the mother and fetus), and the treatment options are somewhat at odds in that they need to balance a stable maternal status and intrauterine environment with the risk of neonatal abstinence syndrome (NAS). Additionally, pregnancy is an opportunity for a woman with opioid use disorder to have access to medical care (possibly for the first time) leading to the diagnosis and treatment of her disease. As the clinicians on the front line, obstetricians therefore require education and guidance on best practice for management of opioid use in pregnancy.
In 2017, Reddy and colleagues, as part of a joint workshop on opioid use in pregnancy, and a committee opinion from ACOG provided the following recommendations.
Screening
Universally screen for substance use, starting at the first prenatal visit; this is recommended over risk factor-based screening.
Use a validated screening tool. A tool such as a questionnaire is recommended as the first-line screening test (for example, the 4Ps screen, the National Institute on Drug Abuse Quick Screen, and the CRAFFT Screening Interview).
Do not universally screen urine and hair for drugs. This type of screening has many limitations, such as the limited number of substances tested, false-positive results, and inaccurate determination of the frequency or timing of drug use. Information regarding the consequences of the test must be provided, and patient consent must be obtained prior to performing the test.
Treatment
Use medication-assisted treatment with buprenorphine or methadone, which is preferred to medically supervised withdrawal. Medication-assisted treatment prevents withdrawal symptoms and cravings, decreases the risk of relapse, improves compliance with prenatal care and addiction treatment programs, and leads to better obstetric outcomes (higher birth weight, lower rate of preterm birth, lower perinatal mortality).
Know that buprenorphine has several advantages over methadone, including the convenience of an outpatient prescription, a lower risk of overdose, and improved neonatal outcomes (higher birth weight, lower doses of morphine to treat NAS, shorter treatment duration).
Prioritize methadone as the preferred option for pregnant women who are already receiving methadone treatment (changing to buprenorphine may precipitate withdrawal), those with a long-standing history of or multi-substance abuse, and those who have failed other treatment programs.
Prenatal care
Screen for comorbid conditions such as sexually transmitted infections, other medications or substance use, social conditions, and mental health disorders.
Perform ultrasonography serially to monitor fetal growth because of the increased risk of fetal growth restriction.
Consult with anesthesiology for pain control recommendations for labor and delivery and with neonatalogy/pediatrics for NAS counseling.
Intrapartum/postpartum care
Recognize heightened pain. Women with opioid use disorder have increased sensitivity to painful stimuli.
Continue the maintenance dose of methadone or buprenorphine throughout hospitalization, with short-acting opioids added for a brief period for postoperative pain.
Prioritize regional anesthesia for pain control in labor or for cesarean delivery.
Consider alternative therapies such as regional blocks, nonopioid medications (nonsteroidal anti-inflammatory drugs, acetaminophen), or relaxation/mindfulness training.
Avoid mixed antagonist and agonist narcotics (butorphanol, nalbuphine, pentazocine) as they may cause acute withdrawal.
Encourage breastfeeding to decrease the severity of NAS and maternal stress and increase maternal-child bonding and maternal confidence.
Offer contraceptive counseling and services immediately postpartum in the hospital, with strong consideration for long-acting reversible contraception.
Opioid prescribing practices
Opioids are prescribed in excess post–cesarean delivery. Several recent studies have demonstrated that most women are prescribed opioids post–cesarean delivery in excess of the amount they use (median 30–40 tablets prescribed, median 20 tablets used).1,2 The leftover opioid medication usually is not discarded and therefore is at risk for diversion or misuse. A small subset of patients will use all the opioids prescribed and feel as though they have not received enough medication.
Prescribe post–cesarean delivery opioids more appropriately by considering individual inpatient opioid requirements or a shared decision-making model.3
Prioritize acetaminophen and ibuprofen during breastfeeding. In a recent editorial in OBG Management, Robert L. Barbieri, MD, recommended that whenever possible, acetaminophen and ibuprofen should be the first-line treatment for breastfeeding women, and narcotics that are metabolized by CYP2D6 should be avoided to reduce the risk to the newborn.4
Universal screening for substance use should be performed in all pregnant women, and clinicians should offer medication-assisted treatment in conjunction with prenatal care and other supportive services as the standard therapy for opioid use disorder. More selective, patient-specific opioid prescribing practices should be applied in the obstetric population.
Read about new strategies for postpartum hemorrhage.
Postpartum hemorrhage: New definitions and new strategies for stemming the flow
ACOG Committee on Practice Bulletins—Obstetrics. ACOG practice bulletin No. 183: Postpartum hemorrhage. Obstet Gynecol. 2017;130(4):e168-e186.
From the very first sentence of the new ACOG practice bulletin, postpartum hemorrhage (PPH) is redefined as "cumulative blood loss greater than or equal to 1,000 mL or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours after the birth process (includes intrapartum loss) regardless of route of delivery." Although this does not seem to be a huge change from the traditional teaching of a 500-mL blood loss at vaginal delivery and a 1,000-mL loss at cesarean delivery, it reflects a shift in focus from simply responding to a certain amount of bleeding to using a multidisciplinary action plan for treating this leading cause of maternal mortality worldwide.
Focus on developing a PPH action plan
As part of the shift toward a multidisciplinary action plan for PPH, all obstetric team members should be aware of the following:
- For most postpartum women, by the time they begin to show signs of hemodynamic compromise, the amount of blood loss approaches 25% of their total blood volume (1,500 mL). Lactic acidosis, systemic inflammation, and a consumptive coagulopathy result.
- Risk stratification prior to delivery, recognition and identification of the source of bleeding, and aggressive early resuscitation to prevent hypovolemia are paramount. Experience gleaned from trauma massive transfusion protocols suggests that judicious transfusion of packed red blood cells, fresh frozen plasma, and platelets in a 1:1:1 ratio is appropriate for obstetric patients. Additionally, patients with low fibrinogen levels should be treated with cryoprecipitate.
- The use of fixed transfusion ratios and standardized protocols for recognition and management of PPH has been demonstrated to increase earlier intervention and resolution of hemorrhage at an earlier stage, although the maternal outcomes results have been mixed.
- Multidisciplinary team drills and simulation exercises also should be considered to help solidify training of an institution's teams responsible for PPH response.
Novel management option: Tranexamic acid
In addition to these strategies, there is a new recommendation for managing refractory PPH: tranexamic acid, which works by binding to lysine receptors on plasminogen and plasmin, inhibiting plasmin-mediated fibrin degradation.5 Previously, tranexamic acid was known to be effective in trauma, heart surgery, and in patients with thrombophilias. Pacheco and colleagues recently demonstrated reduced mortality from obstetric bleeding if tranexamic acid was given within 3 hours of delivery, without increased thrombotic complications.5 ACOG recommends its use if initial medical therapy fails, while the World Health Organization strongly recommends that tranexamic acid be part of a standard PPH package for all cases of PPH (TABLE).6
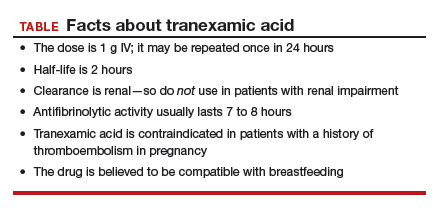
Postpartum hemorrhage requires early, aggressive, and multidisciplinary coordination to ensure that 1) patients at risk for hemorrhage are identified for preventive measures; 2) existing hemorrhage is recognized and quickly treated, first with noninvasive methods and then with more definitive surgical treatments; and 3) blood product replacement follows an evidence-based standardized protocol. Tranexamic acid is recommended as an adjunct treatment for PPH (of any cause) and should be used within 3 hours of delivery.
Read about new ACOG guidance on prepregnancy and prenatal screening.
Carrier screening—choose something
ACOG Committee on Genetics. Committee opinion No. 690: Carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129(3):e35-e40.
ACOG Committee on Genetics. Committee opinion No. 691: Carrier screening for genetic conditions. Obstet Gynecol. 2017;129(3):e41-e55.
Ideally, carrier screening should be offered prior to pregnancy to fully inform couples of their reproductive risks and options for pregnancy. If not performed in the preconception period, carrier screening should be offered to all pregnant women. If a patient chooses screening and screens positive for a particular disorder, her reproductive partner should then be offered screening so that the risk of having an affected child can be determined.
New ACOG guidance on prepregnancy and prenatal screening
Carrier screening recommendations have evolved as the technology available has expanded. All 3 of the following strategies now are considered "acceptable" according to 2 recently published ACOG committee opinions.
Traditional ethnic-specific carrier screening, previously ACOG's sole recommendation, involves offering specific genetic screening to patients from populations with a high prevalence for certain conditions. One such example is Tay-Sachs disease screening in Ashkenazi Jewish patients.
Panethnic screening, which takes into account mixed or uncertain backgrounds, involves screening for a certain panel of disorders and is available to all patients regardless of their background (for example, cystic fibrosis screening offered to all pregnant patients).
Expanded carrier screening is when a large number of disorders can be screened for simultaneously for a lower cost than previous testing strategies. Expanded carrier screening panels vary in number and which conditions are tested by the laboratory. An ideal expanded carrier screening panel has been debated in the literature but not agreed on.7
ObGyns and practices therefore are encouraged to develop a standard counseling and screening protocol to offer to all their patients while being flexible to make available any patient-requested screening that is outside their protocol. Pretest and posttest counseling, including a thorough family history, is essential (as with any genetic testing) and should include residual risk after testing, potential need for specific familial mutation testing instead of general carrier screening, and issues with consanguinity.
Three essential screens
Regardless of the screening strategy chosen from the above options, 3 screening tests should be offered to all pregnant women or couples considering pregnancy (either individually or in the context of an expanded screening panel):
- Cystic fibrosis. At the least, a panel of the 23 most common mutations should be used. More expanded panels, which include hundreds of mutations, increase detection in non-Caucasian populations and for milder forms of the disease or infertility-related mutations.
- Hemoglobinopathies (sickle cell, α- and β-thalassemia). Complete blood count and red blood indices are recommended for all, with hemoglobin electrophoresis recommended for patients of African, Middle Eastern, Mediterranean, or West Indian descent or if mean corpuscular volume is low.
- Spinal muscular atrophy (SMA). The most recent addition to ACOG's recommendations for general carrier screening due to the relatively high carrier frequency (1-in-40 to 1-in-60) and the severity of the disease, SMA causes degeneration of the spinal cord neurons, skeletal muscular atrophy, and overall weakness. Screening is via polymerase chain reaction for SMN1 copy number: 2 copies are normal, and 1 copy indicates a carrier of the SMN1 deletion. About 3% to 4% of patients will screen negative but still will be "carriers" due to having 2 copies of the SMN1 gene on 1 chromosome and no copies on the other chromosome.
All pregnant patients or patients considering pregnancy should be offered carrier screening as standard reproductive care, including screening for cystic fibrosis, hemoglobinopathies, and spinal muscular atrophy. Ethnic, panethnic, or expanded carrier screening (and patient-requested specific screening) all are acceptable options, and a standard screening and counseling protocol should be determined by the ObGyn or practice.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The past year brought new information and guidance from the American College of Obstetricians and Gynecologists (ACOG) on many relevant obstetric topics, making it difficult to choose just a few for this Update. Opioid use in pregnancy was an obvious choice given the national media attention and the potential opportunity for intervention in pregnancy for both the mother and the fetus/newborn. Postpartum hemorrhage, an “oldie but goodie,” was chosen for several reasons: It got a new definition, a new focus on multidisciplinary care, and an exciting novel tool for the treatment toolbox. Finally, given the rapidly changing technology, new screening recommendations, and the complexity of counseling, carrier screening was chosen as a genetic hot topic for this year.
Opioids, obstetrics, and opportunities
Reddy UM, Davis JM, Ren Z, Greene MF; Opioid Use in Pregnancy, Neonatal Abstinence Syndrome, and Childhood Outcomes Workshop Invited Speakers. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes: Executive summary of a joint workshop. Obstet Gynecol. 2017;130(1):10-28.
ACOG Committee on Obstetric Practice. ACOG committee opinion No. 711: Opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130(2):e81-e94.
The term "opioid epidemic" is omnipresent in both the lay media and the medical literature. In the past decade, the United States has had a huge increase in the number of opioid prescriptions, the rate of admissions and deaths due to prescription opioid misuse and abuse, and an increased rate of heroin use attributed to prior prescription opioid use.
Obstetrics is unique in that opioid use and abuse disorders affect 2 patients simultaneously (the mother and fetus), and the treatment options are somewhat at odds in that they need to balance a stable maternal status and intrauterine environment with the risk of neonatal abstinence syndrome (NAS). Additionally, pregnancy is an opportunity for a woman with opioid use disorder to have access to medical care (possibly for the first time) leading to the diagnosis and treatment of her disease. As the clinicians on the front line, obstetricians therefore require education and guidance on best practice for management of opioid use in pregnancy.
In 2017, Reddy and colleagues, as part of a joint workshop on opioid use in pregnancy, and a committee opinion from ACOG provided the following recommendations.
Screening
Universally screen for substance use, starting at the first prenatal visit; this is recommended over risk factor-based screening.
Use a validated screening tool. A tool such as a questionnaire is recommended as the first-line screening test (for example, the 4Ps screen, the National Institute on Drug Abuse Quick Screen, and the CRAFFT Screening Interview).
Do not universally screen urine and hair for drugs. This type of screening has many limitations, such as the limited number of substances tested, false-positive results, and inaccurate determination of the frequency or timing of drug use. Information regarding the consequences of the test must be provided, and patient consent must be obtained prior to performing the test.
Treatment
Use medication-assisted treatment with buprenorphine or methadone, which is preferred to medically supervised withdrawal. Medication-assisted treatment prevents withdrawal symptoms and cravings, decreases the risk of relapse, improves compliance with prenatal care and addiction treatment programs, and leads to better obstetric outcomes (higher birth weight, lower rate of preterm birth, lower perinatal mortality).
Know that buprenorphine has several advantages over methadone, including the convenience of an outpatient prescription, a lower risk of overdose, and improved neonatal outcomes (higher birth weight, lower doses of morphine to treat NAS, shorter treatment duration).
Prioritize methadone as the preferred option for pregnant women who are already receiving methadone treatment (changing to buprenorphine may precipitate withdrawal), those with a long-standing history of or multi-substance abuse, and those who have failed other treatment programs.
Prenatal care
Screen for comorbid conditions such as sexually transmitted infections, other medications or substance use, social conditions, and mental health disorders.
Perform ultrasonography serially to monitor fetal growth because of the increased risk of fetal growth restriction.
Consult with anesthesiology for pain control recommendations for labor and delivery and with neonatalogy/pediatrics for NAS counseling.
Intrapartum/postpartum care
Recognize heightened pain. Women with opioid use disorder have increased sensitivity to painful stimuli.
Continue the maintenance dose of methadone or buprenorphine throughout hospitalization, with short-acting opioids added for a brief period for postoperative pain.
Prioritize regional anesthesia for pain control in labor or for cesarean delivery.
Consider alternative therapies such as regional blocks, nonopioid medications (nonsteroidal anti-inflammatory drugs, acetaminophen), or relaxation/mindfulness training.
Avoid mixed antagonist and agonist narcotics (butorphanol, nalbuphine, pentazocine) as they may cause acute withdrawal.
Encourage breastfeeding to decrease the severity of NAS and maternal stress and increase maternal-child bonding and maternal confidence.
Offer contraceptive counseling and services immediately postpartum in the hospital, with strong consideration for long-acting reversible contraception.
Opioid prescribing practices
Opioids are prescribed in excess post–cesarean delivery. Several recent studies have demonstrated that most women are prescribed opioids post–cesarean delivery in excess of the amount they use (median 30–40 tablets prescribed, median 20 tablets used).1,2 The leftover opioid medication usually is not discarded and therefore is at risk for diversion or misuse. A small subset of patients will use all the opioids prescribed and feel as though they have not received enough medication.
Prescribe post–cesarean delivery opioids more appropriately by considering individual inpatient opioid requirements or a shared decision-making model.3
Prioritize acetaminophen and ibuprofen during breastfeeding. In a recent editorial in OBG Management, Robert L. Barbieri, MD, recommended that whenever possible, acetaminophen and ibuprofen should be the first-line treatment for breastfeeding women, and narcotics that are metabolized by CYP2D6 should be avoided to reduce the risk to the newborn.4
Universal screening for substance use should be performed in all pregnant women, and clinicians should offer medication-assisted treatment in conjunction with prenatal care and other supportive services as the standard therapy for opioid use disorder. More selective, patient-specific opioid prescribing practices should be applied in the obstetric population.
Read about new strategies for postpartum hemorrhage.
Postpartum hemorrhage: New definitions and new strategies for stemming the flow
ACOG Committee on Practice Bulletins—Obstetrics. ACOG practice bulletin No. 183: Postpartum hemorrhage. Obstet Gynecol. 2017;130(4):e168-e186.
From the very first sentence of the new ACOG practice bulletin, postpartum hemorrhage (PPH) is redefined as "cumulative blood loss greater than or equal to 1,000 mL or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours after the birth process (includes intrapartum loss) regardless of route of delivery." Although this does not seem to be a huge change from the traditional teaching of a 500-mL blood loss at vaginal delivery and a 1,000-mL loss at cesarean delivery, it reflects a shift in focus from simply responding to a certain amount of bleeding to using a multidisciplinary action plan for treating this leading cause of maternal mortality worldwide.
Focus on developing a PPH action plan
As part of the shift toward a multidisciplinary action plan for PPH, all obstetric team members should be aware of the following:
- For most postpartum women, by the time they begin to show signs of hemodynamic compromise, the amount of blood loss approaches 25% of their total blood volume (1,500 mL). Lactic acidosis, systemic inflammation, and a consumptive coagulopathy result.
- Risk stratification prior to delivery, recognition and identification of the source of bleeding, and aggressive early resuscitation to prevent hypovolemia are paramount. Experience gleaned from trauma massive transfusion protocols suggests that judicious transfusion of packed red blood cells, fresh frozen plasma, and platelets in a 1:1:1 ratio is appropriate for obstetric patients. Additionally, patients with low fibrinogen levels should be treated with cryoprecipitate.
- The use of fixed transfusion ratios and standardized protocols for recognition and management of PPH has been demonstrated to increase earlier intervention and resolution of hemorrhage at an earlier stage, although the maternal outcomes results have been mixed.
- Multidisciplinary team drills and simulation exercises also should be considered to help solidify training of an institution's teams responsible for PPH response.
Novel management option: Tranexamic acid
In addition to these strategies, there is a new recommendation for managing refractory PPH: tranexamic acid, which works by binding to lysine receptors on plasminogen and plasmin, inhibiting plasmin-mediated fibrin degradation.5 Previously, tranexamic acid was known to be effective in trauma, heart surgery, and in patients with thrombophilias. Pacheco and colleagues recently demonstrated reduced mortality from obstetric bleeding if tranexamic acid was given within 3 hours of delivery, without increased thrombotic complications.5 ACOG recommends its use if initial medical therapy fails, while the World Health Organization strongly recommends that tranexamic acid be part of a standard PPH package for all cases of PPH (TABLE).6
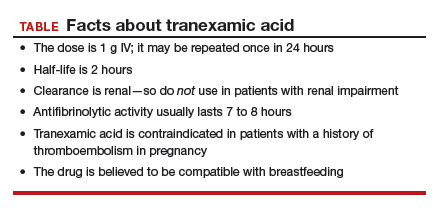
Postpartum hemorrhage requires early, aggressive, and multidisciplinary coordination to ensure that 1) patients at risk for hemorrhage are identified for preventive measures; 2) existing hemorrhage is recognized and quickly treated, first with noninvasive methods and then with more definitive surgical treatments; and 3) blood product replacement follows an evidence-based standardized protocol. Tranexamic acid is recommended as an adjunct treatment for PPH (of any cause) and should be used within 3 hours of delivery.
Read about new ACOG guidance on prepregnancy and prenatal screening.
Carrier screening—choose something
ACOG Committee on Genetics. Committee opinion No. 690: Carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129(3):e35-e40.
ACOG Committee on Genetics. Committee opinion No. 691: Carrier screening for genetic conditions. Obstet Gynecol. 2017;129(3):e41-e55.
Ideally, carrier screening should be offered prior to pregnancy to fully inform couples of their reproductive risks and options for pregnancy. If not performed in the preconception period, carrier screening should be offered to all pregnant women. If a patient chooses screening and screens positive for a particular disorder, her reproductive partner should then be offered screening so that the risk of having an affected child can be determined.
New ACOG guidance on prepregnancy and prenatal screening
Carrier screening recommendations have evolved as the technology available has expanded. All 3 of the following strategies now are considered "acceptable" according to 2 recently published ACOG committee opinions.
Traditional ethnic-specific carrier screening, previously ACOG's sole recommendation, involves offering specific genetic screening to patients from populations with a high prevalence for certain conditions. One such example is Tay-Sachs disease screening in Ashkenazi Jewish patients.
Panethnic screening, which takes into account mixed or uncertain backgrounds, involves screening for a certain panel of disorders and is available to all patients regardless of their background (for example, cystic fibrosis screening offered to all pregnant patients).
Expanded carrier screening is when a large number of disorders can be screened for simultaneously for a lower cost than previous testing strategies. Expanded carrier screening panels vary in number and which conditions are tested by the laboratory. An ideal expanded carrier screening panel has been debated in the literature but not agreed on.7
ObGyns and practices therefore are encouraged to develop a standard counseling and screening protocol to offer to all their patients while being flexible to make available any patient-requested screening that is outside their protocol. Pretest and posttest counseling, including a thorough family history, is essential (as with any genetic testing) and should include residual risk after testing, potential need for specific familial mutation testing instead of general carrier screening, and issues with consanguinity.
Three essential screens
Regardless of the screening strategy chosen from the above options, 3 screening tests should be offered to all pregnant women or couples considering pregnancy (either individually or in the context of an expanded screening panel):
- Cystic fibrosis. At the least, a panel of the 23 most common mutations should be used. More expanded panels, which include hundreds of mutations, increase detection in non-Caucasian populations and for milder forms of the disease or infertility-related mutations.
- Hemoglobinopathies (sickle cell, α- and β-thalassemia). Complete blood count and red blood indices are recommended for all, with hemoglobin electrophoresis recommended for patients of African, Middle Eastern, Mediterranean, or West Indian descent or if mean corpuscular volume is low.
- Spinal muscular atrophy (SMA). The most recent addition to ACOG's recommendations for general carrier screening due to the relatively high carrier frequency (1-in-40 to 1-in-60) and the severity of the disease, SMA causes degeneration of the spinal cord neurons, skeletal muscular atrophy, and overall weakness. Screening is via polymerase chain reaction for SMN1 copy number: 2 copies are normal, and 1 copy indicates a carrier of the SMN1 deletion. About 3% to 4% of patients will screen negative but still will be "carriers" due to having 2 copies of the SMN1 gene on 1 chromosome and no copies on the other chromosome.
All pregnant patients or patients considering pregnancy should be offered carrier screening as standard reproductive care, including screening for cystic fibrosis, hemoglobinopathies, and spinal muscular atrophy. Ethnic, panethnic, or expanded carrier screening (and patient-requested specific screening) all are acceptable options, and a standard screening and counseling protocol should be determined by the ObGyn or practice.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130(1):29–35.
- Osmundson SS, Schornack LA, Grasch JL, Zuckerwise LC, Young JL, Richardson MD. Postdischarge opioid use after cesarean delivery. Obstet Gynecol. 2017;130(1):36–41.
- Prabhu M, McQuaid-Hanson E, Hopp S, et al. A shared decision-making intervention to guide opioid prescribing after cesarean delivery. Obstet Gynecol. 2017;130(1):42–46.
- Barbieri RL. Stop using codeine, oxycodone, hydrocodone, tramadol, and aspirin in women who are breastfeeding. OBG Manag. 2017;29(10):8–12.
- Pacheco LD, Hankins GD, Saad AF, Costantine MM, Chiossi G, Saade GR. Tranexamic acid for the management of obstetric hemorrhage. Obstet Gynecol. 2017;130(4);765–769.
- WHO recommendation on tranexamic acid for the treatment of postpartum haemorrhage. Geneva, Switzerland: World Health Organization; 2017.
- Stevens B, Krstic N, Jones M, Murphy L, Hoskovec J. Finding middle ground in constructing a clinically useful expanded carrier screening panel. Obstet Gynecol. 2017;130(2):279–284.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130(1):29–35.
- Osmundson SS, Schornack LA, Grasch JL, Zuckerwise LC, Young JL, Richardson MD. Postdischarge opioid use after cesarean delivery. Obstet Gynecol. 2017;130(1):36–41.
- Prabhu M, McQuaid-Hanson E, Hopp S, et al. A shared decision-making intervention to guide opioid prescribing after cesarean delivery. Obstet Gynecol. 2017;130(1):42–46.
- Barbieri RL. Stop using codeine, oxycodone, hydrocodone, tramadol, and aspirin in women who are breastfeeding. OBG Manag. 2017;29(10):8–12.
- Pacheco LD, Hankins GD, Saad AF, Costantine MM, Chiossi G, Saade GR. Tranexamic acid for the management of obstetric hemorrhage. Obstet Gynecol. 2017;130(4);765–769.
- WHO recommendation on tranexamic acid for the treatment of postpartum haemorrhage. Geneva, Switzerland: World Health Organization; 2017.
- Stevens B, Krstic N, Jones M, Murphy L, Hoskovec J. Finding middle ground in constructing a clinically useful expanded carrier screening panel. Obstet Gynecol. 2017;130(2):279–284.
2017 Update on obstetrics
In this Update we discuss several exciting new recommendations for preventive treatments in pregnancy and prenatal diagnostic tests. Our A-to-Z coverage includes:
- antenatal steroids in late preterm pregnancy
- expanded list of high-risk conditions warranting low-dose aspirin for preeclampsia prevention
- chromosomal microarray analysis versus karyotype for specific clinical situations
- Zika virus infection evolving information.
Next: New recommendation for timing of late preterm antenatal steroids
New recommendation offered for timing of late preterm antenatal steroids
Gyamfi-Bannerman C, Thom EA, Blackwell SC, et al; for the NICHD Maternal-Fetal Medicine Units Network. Antenatal betamethasone for women at risk for late preterm delivery. N Engl J Med. 2016;374(14):1311-1320.
American College of Obstetricians and Gynecologists. Committee Opinion No. 677. Antenatal corticosteroidtherapy for fetal maturation. Obstet Gynecol. 2016;128(4):e187-e194.
Kamath-Rayne BD, Rozance PJ, Goldenberg RL, Jobe AH. Antenatal corticosteroids beyond 34 weeks gestation: what do we do now? Am J Obstet Gynecol. 2016;215(4):423-430.
A dramatic recommendation for obstetric practice change occurred in 2016: the option of administering antenatal steroids for fetal lung maturity after 34 weeks. In the Antenatal Late Preterm Steroids (ALPS) trial of betamethasone in the late preterm period in patients at "high risk" of imminent delivery, Gyamfi-Bannerman and colleagues demonstrated that the treated group had a significant decrease in the rate of neonatal respiratory complications.
The primary outcome, a composite of respiratory morbidities (including transient tachypnea of the newborn, surfactant use, and need for resuscitation at birth) within the first 72 hours of life, had significant differences between groups, occurring in 165 of 1,427 infants (11.6%) in the betamethasone-treated group and 202 of 1,400 (14.4%) in the placebo group (relative risk in the betamethasone group, 0.80; 95% confidence interval, 0.66-0.97; P = .02). However, there was no statistically significant difference in respiratory distress syndrome, apnea, or pneumonia between groups, and the significant difference noted in bronchopulmonary dysplasia was based on a total number of 11 cases.
In response to these findings, both the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) released practice advisories and interim updates, culminating in a final recommendation for a single course of betamethasone in patients at high risk of preterm delivery between 34 and 36 6/7 weeks who have not received a previous course.
Related article:
When could use of antenatal corticosteroids in the late preterm birth period be beneficial?
In a thorough review of the literature on antenatal steroid use, Kamath-Rayne and colleagues highlighted several factors that should be considered before adopting universal use of steroids at >34 weeks. These include:
- The definition of "high risk of imminent delivery" as preterm labor with at least 3-cm dilation or 75% effacement, or spontaneous rupture of membranes. The effect of less stringent inclusion criteria in real-world clinical practice is not known, and many patients who will go on to deliver at term will receive steroids unnecessarily.
- Multiple gestation, patients with pre-existing diabetes, women who had previously received a course of steroids, and fetuses with anomalies were excluded from the ALPS study. Use of antenatal steroids in these groups at >34 weeks should be evaluated before universal adoption.
Related article:
What is the ideal gestational age for twin delivery to minimize perinatal deaths?
- The incidence of neonatal hypoglycemia in the treated group was significantly increased. This affects our colleagues in pediatrics considerably from a systems standpoint (need for changes to newborn protocols and communication between services).
- The long-term outcomes of patients exposed to steroids in the late preterm period are yet to be delineated, specifically, the potential neurodevelopmental effects of a medication known to alter preterm brain development as well as cardiovascular and metabolic consequences.
Next: Low-dose aspirin for reducing preeclampsia risk
Low-dose aspirin clearly is effective for reducing the risk of preeclampsia
American College of Obstetricians and Gynecologists. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122-1131.
Henderson JT, Whitlock EP, O'Connor E, Senger CA, Thompson JH, Rowland MG. Low-dose aspirin for prevention of morbidity and mortality from preeclampsia: a systematic evidence review for the US Preventive Services Task Force. Ann Intern Med. 2014;160(10):695-703.
LeFevre ML; US Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161(11):819-826.
American College of Obstetricians and Gynecologists. Practice advisory on low-dose aspirin and prevention of preeclampsia: updated recommendations. http://www.acog.org/About-ACOG/News-Room/Practice-Advisories/Practice-Advisory-Low-Dose-Aspirin-and-Prevention-of-Preeclampsia-Updated-Recommendations. Published July 11, 2016. Accessed December 6, 2016.
In the 2013 ACOG Task Force on Hypertension in Pregnancy report, low-dose aspirin (60-80 mg) was recommended to be initiated in the late first trimester to reduce preeclampsia risk for women with:
- prior early onset preeclampsia with preterm delivery at <34 weeks' gestation, or
- preeclampsia in more than one prior pregnancy.
This recommendation was based on several meta-analyses that demonstrated a 10% to 17% reduction in risk with no increase in bleeding, placental abruption, or other adverse events.
In 2014, the US Preventive Services Task Force (USPSTF) conducted a systematic evidence review of low-dose aspirin use for prevention of morbidity and mortality from preeclampsia. That report revealed a 24% risk reduction of preeclampsia in high-risk women treated with low-dose aspirin, as well as a 14% reduction in preterm birth and a 20% reduction in fetal growth restriction. A final statement from the USPSTF in 2014 recommended low-dose aspirin (60-150 mg) starting between 12 and 28 weeks' gestation for women at "high" risk who have:
- a history of preeclampsia, especially if accompanied by an adverse outcome
- multifetal gestation
- chronic hypertension
- diabetes (type 1 or type 2)
- renal disease
- autoimmune disease (such as systematic lupus erythematosus, antiphospholipid syndrome).
Related article:
Start offering aspirin to pregnant women at high risk for preeclampsia
As of July 11, 2016, ACOG supports this expanded list of high-risk conditions. Additionally, the USPSTF identified a "moderate" risk group in which low-dose aspirin may be considered if a patient has several risk factors, such as obesity, nulliparity, family history of preeclampsia, age 35 years or older, or another poor pregnancy outcome. ACOG notes, however, that the evidence supporting this practice is uncertain and does not make a recommendation regarding aspirin use in this population. Further study should be conducted to determine the benefit of low-dose aspirin in these patients as well as the long-term effects of treatment on maternal and child outcomes.
Next: CMA for prenatal genetic diagnosis
Chromosomal microarray analysis is preferable to karyotype in certain situations
Pauli JM, Repke JT. Update on obstetrics. OBG Manag. 2013;25(1):28-32.
Society for Maternal-Fetal Medicine (SMFM), Dugoff L, Norton ME, Kuller JA. The use of chromosomal microarray for prenatal diagnosis. Am J Obstet Gynecol. 2016;215(4):B2-B9.
American College of Obstetricians and Gynecologists. Committee Opinion No. 682. Microarrays and next- generation sequencing technology: the use of advanced genetic diagnostic tools in obstetrics and gynecology.Obstet Gynecol. 2016;128(6):e262-e268.
We previously addressed the use of chromosomal microarray analysis (CMA) for prenatal diagnosis in our 2013 "Update on obstetrics," specifically, the question of whether CMA could replace karyotype. The main differences between karyotype and CMA are that 1) only karyotype can detect balanced translocations/inversions and 2) only CMA can detect copy number variants (CNV). There are some differences in the technology and capabilities of the 2 types of CMA currently available as well.
In our 2013 article we concluded that "The total costs of such an approach--test, interpretation, counseling, and long-term follow-up of uncertain results--are unknown at this time and may prove to be unaffordable on a population-wide basis." Today, the cost of CMA is still higher than karyotype, but it is expected to decrease and insurance coverage for this test is expected to increase.
Related article:
Cell-free DNA screening for women at low risk for fetal aneuploidy
Both SMFM and ACOG released recommendations in 2016 regarding the use of CMA in prenatal genetic diagnosis, summarized as follows:
- CMA is recommended over karyotype for fetuses with structural abnormalities on ultrasound
- The detection rate for clinically relevant abnormal CNVs in this population is about 6%
- CMA is recommended for diagnosis for stillbirth specimens
- CMA does not require dividing cells and may be a quicker and more reliable test in this population
- Karotype or fluorescence in situ hybridization (FISH) is recommended for fetuses with ultrasound findings suggestive of aneuploidy
- If it is negative, then CMA is recommended
- Karyotype or CMA is recommended for patients desiring prenatal diagnostic testing with a normal fetal ultrasound
- The detection rate for clinically relevant CNVs in this population (advanced maternal age, abnormal serum screening, prior aneuploidy, parental anxiety) is about 1%
- Pretest and posttest counseling about the limitations of CMA and a 2% risk of detection of variants of unknown significance (VUS) should be performed by a provider who has expertise in CMA and who has access to databases with genotype/phenotype information for VUS
- This counseling should also include the possibility of diagnosis of nonpaternity, consanguinity, and adult-onset disease
- Karyotype is recommended for couples with recurrent pregnancy loss
- The identification of balanced translocations in this population is most relevant in this patient population
- Prenatal diagnosis with routine use of whole-genome or whole-exome sequencing is not recommended.
Next: Zika virus: Check for updates
Zika virus infection: Check often for the latest updates
American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. Practice advisory on Zika virus. http://www.acog.org/About-ACOG/News-Room/Practice-Advisories/Practice-Advisory-Interim-Guidance-for-Care-of-Obstetric-Patients- During-a-Zika-Virus-Outbreak. Published December 5, 2016. Accessed December 6, 2016.
Centers for Disease Control and Prevention. Zika virus. http://www.cdc.gov/zika/pregnancy/index.html. Updated August 22, 2016. Accessed December 6, 2016.
Petersen EE, Meaney-Delman D, Neblett-Fanfair R, et al. Update: interim guidance for preconception counseling and prevention of sexual transmission of Zika virus for persons with possible Zika virus exposure--United States, September 2016. MMWR Morbid Mortal Wkly Rep. 2016;65(39):1077-1081.
A yearly update on obstetrics would be remiss without mention of the Zika virus and its impact on pregnancy and reproduction. That being said, any recommendations we offer may be out of date by the time this article is published given the rapidly changing picture of Zika virus since it first dominated the headlines in 2016. Here are the basics as summarized from ACOG and the Centers for Disease Control and Prevention (CDC):
Viral spread. Zika virus may be spread in several ways: by an infected Aedes species mosquito, mother to fetus, sexual contact, blood transfusion, or laboratory exposure.
Symptoms of infection include conjunctivitis, fever, rash, and arthralgia, but most patients (4/5) are asymptomatic.
Sequelae. Zika virus infection during pregnancy is believed to cause fetal and neonatal microcephaly, intracranial calcifications, and brain and eye abnormalities. The rate of these findings in infected individuals, as well as the rate of vertical transmission, is not known.
Travel advisory. Pregnant women should not travel to areas with active Zika infection (the CDC website regularly updates these restricted areas).
Preventive measures. If traveling to an area of active Zika infection, pregnant women should take preventative measures day and night against mosquito bites, such as use of insect repellents approved by the Environmental Protection Agency, clothing that covers exposed skin, and staying indoors.
Safe sex. Abstinence or consistent condom use is recommended for pregnant women with partners who travel to or live in areas of active Zika infection.
Delay conception. Conception should be postponed for at least 6 months in men with Zika infection and at least 8 weeks in women with Zika infection.
Testing recommendations. Pregnant women with Zika virus exposure should be tested, regardless of symptoms. Symptomatic exposed nonpregnant women and all men should be tested.
Prenatal surveillance. High-risk consultation and serial ultrasounds for fetal anatomy and growth should be considered in patients with Zika virus infection during pregnancy. Amniocentesis can be considered on a case-by-case basis.
Related article:
Zika virus update: A rapidly moving target
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In this Update we discuss several exciting new recommendations for preventive treatments in pregnancy and prenatal diagnostic tests. Our A-to-Z coverage includes:
- antenatal steroids in late preterm pregnancy
- expanded list of high-risk conditions warranting low-dose aspirin for preeclampsia prevention
- chromosomal microarray analysis versus karyotype for specific clinical situations
- Zika virus infection evolving information.
Next: New recommendation for timing of late preterm antenatal steroids
New recommendation offered for timing of late preterm antenatal steroids
Gyamfi-Bannerman C, Thom EA, Blackwell SC, et al; for the NICHD Maternal-Fetal Medicine Units Network. Antenatal betamethasone for women at risk for late preterm delivery. N Engl J Med. 2016;374(14):1311-1320.
American College of Obstetricians and Gynecologists. Committee Opinion No. 677. Antenatal corticosteroidtherapy for fetal maturation. Obstet Gynecol. 2016;128(4):e187-e194.
Kamath-Rayne BD, Rozance PJ, Goldenberg RL, Jobe AH. Antenatal corticosteroids beyond 34 weeks gestation: what do we do now? Am J Obstet Gynecol. 2016;215(4):423-430.
A dramatic recommendation for obstetric practice change occurred in 2016: the option of administering antenatal steroids for fetal lung maturity after 34 weeks. In the Antenatal Late Preterm Steroids (ALPS) trial of betamethasone in the late preterm period in patients at "high risk" of imminent delivery, Gyamfi-Bannerman and colleagues demonstrated that the treated group had a significant decrease in the rate of neonatal respiratory complications.
The primary outcome, a composite of respiratory morbidities (including transient tachypnea of the newborn, surfactant use, and need for resuscitation at birth) within the first 72 hours of life, had significant differences between groups, occurring in 165 of 1,427 infants (11.6%) in the betamethasone-treated group and 202 of 1,400 (14.4%) in the placebo group (relative risk in the betamethasone group, 0.80; 95% confidence interval, 0.66-0.97; P = .02). However, there was no statistically significant difference in respiratory distress syndrome, apnea, or pneumonia between groups, and the significant difference noted in bronchopulmonary dysplasia was based on a total number of 11 cases.
In response to these findings, both the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) released practice advisories and interim updates, culminating in a final recommendation for a single course of betamethasone in patients at high risk of preterm delivery between 34 and 36 6/7 weeks who have not received a previous course.
Related article:
When could use of antenatal corticosteroids in the late preterm birth period be beneficial?
In a thorough review of the literature on antenatal steroid use, Kamath-Rayne and colleagues highlighted several factors that should be considered before adopting universal use of steroids at >34 weeks. These include:
- The definition of "high risk of imminent delivery" as preterm labor with at least 3-cm dilation or 75% effacement, or spontaneous rupture of membranes. The effect of less stringent inclusion criteria in real-world clinical practice is not known, and many patients who will go on to deliver at term will receive steroids unnecessarily.
- Multiple gestation, patients with pre-existing diabetes, women who had previously received a course of steroids, and fetuses with anomalies were excluded from the ALPS study. Use of antenatal steroids in these groups at >34 weeks should be evaluated before universal adoption.
Related article:
What is the ideal gestational age for twin delivery to minimize perinatal deaths?
- The incidence of neonatal hypoglycemia in the treated group was significantly increased. This affects our colleagues in pediatrics considerably from a systems standpoint (need for changes to newborn protocols and communication between services).
- The long-term outcomes of patients exposed to steroids in the late preterm period are yet to be delineated, specifically, the potential neurodevelopmental effects of a medication known to alter preterm brain development as well as cardiovascular and metabolic consequences.
Next: Low-dose aspirin for reducing preeclampsia risk
Low-dose aspirin clearly is effective for reducing the risk of preeclampsia
American College of Obstetricians and Gynecologists. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122-1131.
Henderson JT, Whitlock EP, O'Connor E, Senger CA, Thompson JH, Rowland MG. Low-dose aspirin for prevention of morbidity and mortality from preeclampsia: a systematic evidence review for the US Preventive Services Task Force. Ann Intern Med. 2014;160(10):695-703.
LeFevre ML; US Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161(11):819-826.
American College of Obstetricians and Gynecologists. Practice advisory on low-dose aspirin and prevention of preeclampsia: updated recommendations. http://www.acog.org/About-ACOG/News-Room/Practice-Advisories/Practice-Advisory-Low-Dose-Aspirin-and-Prevention-of-Preeclampsia-Updated-Recommendations. Published July 11, 2016. Accessed December 6, 2016.
In the 2013 ACOG Task Force on Hypertension in Pregnancy report, low-dose aspirin (60-80 mg) was recommended to be initiated in the late first trimester to reduce preeclampsia risk for women with:
- prior early onset preeclampsia with preterm delivery at <34 weeks' gestation, or
- preeclampsia in more than one prior pregnancy.
This recommendation was based on several meta-analyses that demonstrated a 10% to 17% reduction in risk with no increase in bleeding, placental abruption, or other adverse events.
In 2014, the US Preventive Services Task Force (USPSTF) conducted a systematic evidence review of low-dose aspirin use for prevention of morbidity and mortality from preeclampsia. That report revealed a 24% risk reduction of preeclampsia in high-risk women treated with low-dose aspirin, as well as a 14% reduction in preterm birth and a 20% reduction in fetal growth restriction. A final statement from the USPSTF in 2014 recommended low-dose aspirin (60-150 mg) starting between 12 and 28 weeks' gestation for women at "high" risk who have:
- a history of preeclampsia, especially if accompanied by an adverse outcome
- multifetal gestation
- chronic hypertension
- diabetes (type 1 or type 2)
- renal disease
- autoimmune disease (such as systematic lupus erythematosus, antiphospholipid syndrome).
Related article:
Start offering aspirin to pregnant women at high risk for preeclampsia
As of July 11, 2016, ACOG supports this expanded list of high-risk conditions. Additionally, the USPSTF identified a "moderate" risk group in which low-dose aspirin may be considered if a patient has several risk factors, such as obesity, nulliparity, family history of preeclampsia, age 35 years or older, or another poor pregnancy outcome. ACOG notes, however, that the evidence supporting this practice is uncertain and does not make a recommendation regarding aspirin use in this population. Further study should be conducted to determine the benefit of low-dose aspirin in these patients as well as the long-term effects of treatment on maternal and child outcomes.
Next: CMA for prenatal genetic diagnosis
Chromosomal microarray analysis is preferable to karyotype in certain situations
Pauli JM, Repke JT. Update on obstetrics. OBG Manag. 2013;25(1):28-32.
Society for Maternal-Fetal Medicine (SMFM), Dugoff L, Norton ME, Kuller JA. The use of chromosomal microarray for prenatal diagnosis. Am J Obstet Gynecol. 2016;215(4):B2-B9.
American College of Obstetricians and Gynecologists. Committee Opinion No. 682. Microarrays and next- generation sequencing technology: the use of advanced genetic diagnostic tools in obstetrics and gynecology.Obstet Gynecol. 2016;128(6):e262-e268.
We previously addressed the use of chromosomal microarray analysis (CMA) for prenatal diagnosis in our 2013 "Update on obstetrics," specifically, the question of whether CMA could replace karyotype. The main differences between karyotype and CMA are that 1) only karyotype can detect balanced translocations/inversions and 2) only CMA can detect copy number variants (CNV). There are some differences in the technology and capabilities of the 2 types of CMA currently available as well.
In our 2013 article we concluded that "The total costs of such an approach--test, interpretation, counseling, and long-term follow-up of uncertain results--are unknown at this time and may prove to be unaffordable on a population-wide basis." Today, the cost of CMA is still higher than karyotype, but it is expected to decrease and insurance coverage for this test is expected to increase.
Related article:
Cell-free DNA screening for women at low risk for fetal aneuploidy
Both SMFM and ACOG released recommendations in 2016 regarding the use of CMA in prenatal genetic diagnosis, summarized as follows:
- CMA is recommended over karyotype for fetuses with structural abnormalities on ultrasound
- The detection rate for clinically relevant abnormal CNVs in this population is about 6%
- CMA is recommended for diagnosis for stillbirth specimens
- CMA does not require dividing cells and may be a quicker and more reliable test in this population
- Karotype or fluorescence in situ hybridization (FISH) is recommended for fetuses with ultrasound findings suggestive of aneuploidy
- If it is negative, then CMA is recommended
- Karyotype or CMA is recommended for patients desiring prenatal diagnostic testing with a normal fetal ultrasound
- The detection rate for clinically relevant CNVs in this population (advanced maternal age, abnormal serum screening, prior aneuploidy, parental anxiety) is about 1%
- Pretest and posttest counseling about the limitations of CMA and a 2% risk of detection of variants of unknown significance (VUS) should be performed by a provider who has expertise in CMA and who has access to databases with genotype/phenotype information for VUS
- This counseling should also include the possibility of diagnosis of nonpaternity, consanguinity, and adult-onset disease
- Karyotype is recommended for couples with recurrent pregnancy loss
- The identification of balanced translocations in this population is most relevant in this patient population
- Prenatal diagnosis with routine use of whole-genome or whole-exome sequencing is not recommended.
Next: Zika virus: Check for updates
Zika virus infection: Check often for the latest updates
American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. Practice advisory on Zika virus. http://www.acog.org/About-ACOG/News-Room/Practice-Advisories/Practice-Advisory-Interim-Guidance-for-Care-of-Obstetric-Patients- During-a-Zika-Virus-Outbreak. Published December 5, 2016. Accessed December 6, 2016.
Centers for Disease Control and Prevention. Zika virus. http://www.cdc.gov/zika/pregnancy/index.html. Updated August 22, 2016. Accessed December 6, 2016.
Petersen EE, Meaney-Delman D, Neblett-Fanfair R, et al. Update: interim guidance for preconception counseling and prevention of sexual transmission of Zika virus for persons with possible Zika virus exposure--United States, September 2016. MMWR Morbid Mortal Wkly Rep. 2016;65(39):1077-1081.
A yearly update on obstetrics would be remiss without mention of the Zika virus and its impact on pregnancy and reproduction. That being said, any recommendations we offer may be out of date by the time this article is published given the rapidly changing picture of Zika virus since it first dominated the headlines in 2016. Here are the basics as summarized from ACOG and the Centers for Disease Control and Prevention (CDC):
Viral spread. Zika virus may be spread in several ways: by an infected Aedes species mosquito, mother to fetus, sexual contact, blood transfusion, or laboratory exposure.
Symptoms of infection include conjunctivitis, fever, rash, and arthralgia, but most patients (4/5) are asymptomatic.
Sequelae. Zika virus infection during pregnancy is believed to cause fetal and neonatal microcephaly, intracranial calcifications, and brain and eye abnormalities. The rate of these findings in infected individuals, as well as the rate of vertical transmission, is not known.
Travel advisory. Pregnant women should not travel to areas with active Zika infection (the CDC website regularly updates these restricted areas).
Preventive measures. If traveling to an area of active Zika infection, pregnant women should take preventative measures day and night against mosquito bites, such as use of insect repellents approved by the Environmental Protection Agency, clothing that covers exposed skin, and staying indoors.
Safe sex. Abstinence or consistent condom use is recommended for pregnant women with partners who travel to or live in areas of active Zika infection.
Delay conception. Conception should be postponed for at least 6 months in men with Zika infection and at least 8 weeks in women with Zika infection.
Testing recommendations. Pregnant women with Zika virus exposure should be tested, regardless of symptoms. Symptomatic exposed nonpregnant women and all men should be tested.
Prenatal surveillance. High-risk consultation and serial ultrasounds for fetal anatomy and growth should be considered in patients with Zika virus infection during pregnancy. Amniocentesis can be considered on a case-by-case basis.
Related article:
Zika virus update: A rapidly moving target
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In this Update we discuss several exciting new recommendations for preventive treatments in pregnancy and prenatal diagnostic tests. Our A-to-Z coverage includes:
- antenatal steroids in late preterm pregnancy
- expanded list of high-risk conditions warranting low-dose aspirin for preeclampsia prevention
- chromosomal microarray analysis versus karyotype for specific clinical situations
- Zika virus infection evolving information.
Next: New recommendation for timing of late preterm antenatal steroids
New recommendation offered for timing of late preterm antenatal steroids
Gyamfi-Bannerman C, Thom EA, Blackwell SC, et al; for the NICHD Maternal-Fetal Medicine Units Network. Antenatal betamethasone for women at risk for late preterm delivery. N Engl J Med. 2016;374(14):1311-1320.
American College of Obstetricians and Gynecologists. Committee Opinion No. 677. Antenatal corticosteroidtherapy for fetal maturation. Obstet Gynecol. 2016;128(4):e187-e194.
Kamath-Rayne BD, Rozance PJ, Goldenberg RL, Jobe AH. Antenatal corticosteroids beyond 34 weeks gestation: what do we do now? Am J Obstet Gynecol. 2016;215(4):423-430.
A dramatic recommendation for obstetric practice change occurred in 2016: the option of administering antenatal steroids for fetal lung maturity after 34 weeks. In the Antenatal Late Preterm Steroids (ALPS) trial of betamethasone in the late preterm period in patients at "high risk" of imminent delivery, Gyamfi-Bannerman and colleagues demonstrated that the treated group had a significant decrease in the rate of neonatal respiratory complications.
The primary outcome, a composite of respiratory morbidities (including transient tachypnea of the newborn, surfactant use, and need for resuscitation at birth) within the first 72 hours of life, had significant differences between groups, occurring in 165 of 1,427 infants (11.6%) in the betamethasone-treated group and 202 of 1,400 (14.4%) in the placebo group (relative risk in the betamethasone group, 0.80; 95% confidence interval, 0.66-0.97; P = .02). However, there was no statistically significant difference in respiratory distress syndrome, apnea, or pneumonia between groups, and the significant difference noted in bronchopulmonary dysplasia was based on a total number of 11 cases.
In response to these findings, both the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) released practice advisories and interim updates, culminating in a final recommendation for a single course of betamethasone in patients at high risk of preterm delivery between 34 and 36 6/7 weeks who have not received a previous course.
Related article:
When could use of antenatal corticosteroids in the late preterm birth period be beneficial?
In a thorough review of the literature on antenatal steroid use, Kamath-Rayne and colleagues highlighted several factors that should be considered before adopting universal use of steroids at >34 weeks. These include:
- The definition of "high risk of imminent delivery" as preterm labor with at least 3-cm dilation or 75% effacement, or spontaneous rupture of membranes. The effect of less stringent inclusion criteria in real-world clinical practice is not known, and many patients who will go on to deliver at term will receive steroids unnecessarily.
- Multiple gestation, patients with pre-existing diabetes, women who had previously received a course of steroids, and fetuses with anomalies were excluded from the ALPS study. Use of antenatal steroids in these groups at >34 weeks should be evaluated before universal adoption.
Related article:
What is the ideal gestational age for twin delivery to minimize perinatal deaths?
- The incidence of neonatal hypoglycemia in the treated group was significantly increased. This affects our colleagues in pediatrics considerably from a systems standpoint (need for changes to newborn protocols and communication between services).
- The long-term outcomes of patients exposed to steroids in the late preterm period are yet to be delineated, specifically, the potential neurodevelopmental effects of a medication known to alter preterm brain development as well as cardiovascular and metabolic consequences.
Next: Low-dose aspirin for reducing preeclampsia risk
Low-dose aspirin clearly is effective for reducing the risk of preeclampsia
American College of Obstetricians and Gynecologists. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122-1131.
Henderson JT, Whitlock EP, O'Connor E, Senger CA, Thompson JH, Rowland MG. Low-dose aspirin for prevention of morbidity and mortality from preeclampsia: a systematic evidence review for the US Preventive Services Task Force. Ann Intern Med. 2014;160(10):695-703.
LeFevre ML; US Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161(11):819-826.
American College of Obstetricians and Gynecologists. Practice advisory on low-dose aspirin and prevention of preeclampsia: updated recommendations. http://www.acog.org/About-ACOG/News-Room/Practice-Advisories/Practice-Advisory-Low-Dose-Aspirin-and-Prevention-of-Preeclampsia-Updated-Recommendations. Published July 11, 2016. Accessed December 6, 2016.
In the 2013 ACOG Task Force on Hypertension in Pregnancy report, low-dose aspirin (60-80 mg) was recommended to be initiated in the late first trimester to reduce preeclampsia risk for women with:
- prior early onset preeclampsia with preterm delivery at <34 weeks' gestation, or
- preeclampsia in more than one prior pregnancy.
This recommendation was based on several meta-analyses that demonstrated a 10% to 17% reduction in risk with no increase in bleeding, placental abruption, or other adverse events.
In 2014, the US Preventive Services Task Force (USPSTF) conducted a systematic evidence review of low-dose aspirin use for prevention of morbidity and mortality from preeclampsia. That report revealed a 24% risk reduction of preeclampsia in high-risk women treated with low-dose aspirin, as well as a 14% reduction in preterm birth and a 20% reduction in fetal growth restriction. A final statement from the USPSTF in 2014 recommended low-dose aspirin (60-150 mg) starting between 12 and 28 weeks' gestation for women at "high" risk who have:
- a history of preeclampsia, especially if accompanied by an adverse outcome
- multifetal gestation
- chronic hypertension
- diabetes (type 1 or type 2)
- renal disease
- autoimmune disease (such as systematic lupus erythematosus, antiphospholipid syndrome).
Related article:
Start offering aspirin to pregnant women at high risk for preeclampsia
As of July 11, 2016, ACOG supports this expanded list of high-risk conditions. Additionally, the USPSTF identified a "moderate" risk group in which low-dose aspirin may be considered if a patient has several risk factors, such as obesity, nulliparity, family history of preeclampsia, age 35 years or older, or another poor pregnancy outcome. ACOG notes, however, that the evidence supporting this practice is uncertain and does not make a recommendation regarding aspirin use in this population. Further study should be conducted to determine the benefit of low-dose aspirin in these patients as well as the long-term effects of treatment on maternal and child outcomes.
Next: CMA for prenatal genetic diagnosis
Chromosomal microarray analysis is preferable to karyotype in certain situations
Pauli JM, Repke JT. Update on obstetrics. OBG Manag. 2013;25(1):28-32.
Society for Maternal-Fetal Medicine (SMFM), Dugoff L, Norton ME, Kuller JA. The use of chromosomal microarray for prenatal diagnosis. Am J Obstet Gynecol. 2016;215(4):B2-B9.
American College of Obstetricians and Gynecologists. Committee Opinion No. 682. Microarrays and next- generation sequencing technology: the use of advanced genetic diagnostic tools in obstetrics and gynecology.Obstet Gynecol. 2016;128(6):e262-e268.
We previously addressed the use of chromosomal microarray analysis (CMA) for prenatal diagnosis in our 2013 "Update on obstetrics," specifically, the question of whether CMA could replace karyotype. The main differences between karyotype and CMA are that 1) only karyotype can detect balanced translocations/inversions and 2) only CMA can detect copy number variants (CNV). There are some differences in the technology and capabilities of the 2 types of CMA currently available as well.
In our 2013 article we concluded that "The total costs of such an approach--test, interpretation, counseling, and long-term follow-up of uncertain results--are unknown at this time and may prove to be unaffordable on a population-wide basis." Today, the cost of CMA is still higher than karyotype, but it is expected to decrease and insurance coverage for this test is expected to increase.
Related article:
Cell-free DNA screening for women at low risk for fetal aneuploidy
Both SMFM and ACOG released recommendations in 2016 regarding the use of CMA in prenatal genetic diagnosis, summarized as follows:
- CMA is recommended over karyotype for fetuses with structural abnormalities on ultrasound
- The detection rate for clinically relevant abnormal CNVs in this population is about 6%
- CMA is recommended for diagnosis for stillbirth specimens
- CMA does not require dividing cells and may be a quicker and more reliable test in this population
- Karotype or fluorescence in situ hybridization (FISH) is recommended for fetuses with ultrasound findings suggestive of aneuploidy
- If it is negative, then CMA is recommended
- Karyotype or CMA is recommended for patients desiring prenatal diagnostic testing with a normal fetal ultrasound
- The detection rate for clinically relevant CNVs in this population (advanced maternal age, abnormal serum screening, prior aneuploidy, parental anxiety) is about 1%
- Pretest and posttest counseling about the limitations of CMA and a 2% risk of detection of variants of unknown significance (VUS) should be performed by a provider who has expertise in CMA and who has access to databases with genotype/phenotype information for VUS
- This counseling should also include the possibility of diagnosis of nonpaternity, consanguinity, and adult-onset disease
- Karyotype is recommended for couples with recurrent pregnancy loss
- The identification of balanced translocations in this population is most relevant in this patient population
- Prenatal diagnosis with routine use of whole-genome or whole-exome sequencing is not recommended.
Next: Zika virus: Check for updates
Zika virus infection: Check often for the latest updates
American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. Practice advisory on Zika virus. http://www.acog.org/About-ACOG/News-Room/Practice-Advisories/Practice-Advisory-Interim-Guidance-for-Care-of-Obstetric-Patients- During-a-Zika-Virus-Outbreak. Published December 5, 2016. Accessed December 6, 2016.
Centers for Disease Control and Prevention. Zika virus. http://www.cdc.gov/zika/pregnancy/index.html. Updated August 22, 2016. Accessed December 6, 2016.
Petersen EE, Meaney-Delman D, Neblett-Fanfair R, et al. Update: interim guidance for preconception counseling and prevention of sexual transmission of Zika virus for persons with possible Zika virus exposure--United States, September 2016. MMWR Morbid Mortal Wkly Rep. 2016;65(39):1077-1081.
A yearly update on obstetrics would be remiss without mention of the Zika virus and its impact on pregnancy and reproduction. That being said, any recommendations we offer may be out of date by the time this article is published given the rapidly changing picture of Zika virus since it first dominated the headlines in 2016. Here are the basics as summarized from ACOG and the Centers for Disease Control and Prevention (CDC):
Viral spread. Zika virus may be spread in several ways: by an infected Aedes species mosquito, mother to fetus, sexual contact, blood transfusion, or laboratory exposure.
Symptoms of infection include conjunctivitis, fever, rash, and arthralgia, but most patients (4/5) are asymptomatic.
Sequelae. Zika virus infection during pregnancy is believed to cause fetal and neonatal microcephaly, intracranial calcifications, and brain and eye abnormalities. The rate of these findings in infected individuals, as well as the rate of vertical transmission, is not known.
Travel advisory. Pregnant women should not travel to areas with active Zika infection (the CDC website regularly updates these restricted areas).
Preventive measures. If traveling to an area of active Zika infection, pregnant women should take preventative measures day and night against mosquito bites, such as use of insect repellents approved by the Environmental Protection Agency, clothing that covers exposed skin, and staying indoors.
Safe sex. Abstinence or consistent condom use is recommended for pregnant women with partners who travel to or live in areas of active Zika infection.
Delay conception. Conception should be postponed for at least 6 months in men with Zika infection and at least 8 weeks in women with Zika infection.
Testing recommendations. Pregnant women with Zika virus exposure should be tested, regardless of symptoms. Symptomatic exposed nonpregnant women and all men should be tested.
Prenatal surveillance. High-risk consultation and serial ultrasounds for fetal anatomy and growth should be considered in patients with Zika virus infection during pregnancy. Amniocentesis can be considered on a case-by-case basis.
Related article:
Zika virus update: A rapidly moving target
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
2016 Update on obstetrics
Some areas of obstetric care are not as clearcut as others in this time of rapid medical evolution. In this Update, we discuss 3 of them:
- management of twin gestations
- management of chronic hypertension in pregnancy
- cell-free DNA screening for fetal aneuploidy.
To our benefit, both the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) have weighed in on important aspects of these areas of obstetric care.
Society for Maternal-Fetal Medicine, Simpson LL. Twin-twin transfusion syndrome. Am J Obstet Gynecol. 2013;208(1):3–18.
Society for Maternal-Fetal Medicine. Checklists and Safety Bundles. https://www.smfm.org/mfm-practice/checklists-and-safety-bundles. Published March 2015. Accessed December 7, 2015.
American College of Obstetricians and Gynecologists. Practice bulletin No. 144. Multifetal gestations: twin, triplet, and higher-order multifetal pregnancies. Obstet Gynecol. 2014;123(5):1118–1132.
From the maternal perspective, twin pregnancies are known to have higher risks than their singleton counterparts for such complications as hypertension, preeclampsia, diabetes, hemorrhage, cesarean delivery, postpartum depression, and anemia. These complications are managed essentially the same way regardless of the number of fetuses.
From the fetal/neonatal perspective, twin gestations may carry increased risks of congenital anomalies, preterm birth, and aneuploidy, which are managed similarly to singleton gestations overall, with certain adjustments as necessary.
Twin pregnancies do have unique risks, however, that are managed differently from the time chorionicity is established until delivery. The level of risk increases as the number of chorions and amnions decreases.
A basic management plan for twin gestations consists of a number of components, elucidated below.
1. Determine chorionicity and amnionicityThis determination is most reliably performed late in the first trimester and must be done using ultrasound. The inter-twin membrane should be identified. At 11 to 14 weeks, the presence of the “lambda sign,” a triangular projection of tissue that extends from the chorionic surface, is indicative of a dichorionic pregnancy, while a “T sign” suggests a monochorionic pregnancy (sensitivities 97%–100%; specificities 98%–100%). Alternatively, demonstration of discordant genders or separate placentas may be used later in pregnancy.
2. Monitor growth every 4 weeks in dichorionic twinsDichorionic twins are, by default, diamniotic. After the anatomic survey, growth surveillance should be conducted approximately every 4 weeks.
Discordant growth usually is defined as a difference of 20% or more in weight between the twins, based on the weight of the larger twin. As an isolated finding with both fetuses of normal weight, this discordance has not been demonstrated to increase adverse outcomes. Routine antenatal surveillance is not necessarily indicated.
Fetal growth restriction of one twin or a coexisting abnormality should prompt antenatal testing and/or earlier delivery. Any maternal comorbidities such as hypertension or diabetes also would be indications for testing. Otherwise, delivery is recommended at 38 weeks’ to 38-6/7 weeks’ gestation.
After 32 weeks, the mode of delivery may be vaginal if the presenting twin is vertex and the delivery provider can perform breech extraction or internal podalic version, if necessary.
3. Monochorionic/diamniotic twins also warrant regular surveillanceThe shared placenta places these pregnancies at increased risk for twin-to-twin transfusion syndrome (TTTS), a fetal-placental imbalance in which one twin “transfuses” the other. Ten percent to 15% of monochorionic pregnancies develop TTTS, which is associated with high rates of morbidity and mortality, even when treated.
Antenatal surveillance of these pregnancies involves ultrasonography assessment every 2 weeks, starting at 16 weeks. At each examination, the deepest vertical pocket (DVP) of fluid and presence of each fetal bladder are documented. This limited assessment alternates with a growth assessment every 2 weeks. SMFM recommends this biweekly assessment until 28 weeks, then every 2 to 3 weeks until delivery.
Stage 1 TTTS is defined by the polyhydramnios/oligohydramnios sequence (DVP of one fetus <2 cm, with DVP of the other >8 cm).
Evaluation for treatment of TTTS with laser coagulation (preferred) or amnio‑reduction should take place after the diagnosis is made, along with increased fetal surveillance.
SMFM also recommends fetal echocardiography due to the 9-fold increased risk of cardiac anomalies in monochorionic pregnancies.
Other complications of monochorionic/diamniotic twins include selective fetal growth restriction (due to unequal sharing of the placenta), twin reversed arterial perfusion (TRAP) sequence, and twin anemia-polycythemia sequence (TAPS).
Antenatal surveillance of all monochorionic twins is recommended, given the increased risk of stillbirth; many centers start testing at 32 weeks’ gestation. According to ACOG, uncomplicated monochorionic/diamniotic twins should be delivered at 34 weeks’ to 37-6/7 weeks’ gestation. Fetal growth restriction or other comorbidities may prompt delivery as early as 32 weeks.
4. Know the risks of monoamniotic twin gestationsThese twins are at increased risk for intrauterine fetal death due to cord entanglement, as well as TTTS, TAPS, and fetal growth restriction. Routine growth assessment and evaluation for TTTS are similar to those for monochorionic/diamniotic twins (without the option of polyhydramnios/oligohydramnios measurement), but the overall management of these pregnancies is unknown.
Protocols may range from outpatient antenatal testing to hospitalization to 24 to 28 weeks’ gestation with daily antenatal testing or attempted continuous monitoring. Delivery by cesarean delivery is recommended at 32 to 34 weeks’ gestation.
What this EVIDENCE means for practice Monochorionic twins need specific and frequent monitoring due to significantly increased risk for both fetal and placental complications. They justify late preterm or early term delivery.
Management of chronic hypertension in pregnancy: Reserve therapy for severe hypertension
Cell-free DNA screening for fetal aneuploidy: Strengths and limitations
Some areas of obstetric care are not as clearcut as others in this time of rapid medical evolution. In this Update, we discuss 3 of them:
- management of twin gestations
- management of chronic hypertension in pregnancy
- cell-free DNA screening for fetal aneuploidy.
To our benefit, both the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) have weighed in on important aspects of these areas of obstetric care.
Society for Maternal-Fetal Medicine, Simpson LL. Twin-twin transfusion syndrome. Am J Obstet Gynecol. 2013;208(1):3–18.
Society for Maternal-Fetal Medicine. Checklists and Safety Bundles. https://www.smfm.org/mfm-practice/checklists-and-safety-bundles. Published March 2015. Accessed December 7, 2015.
American College of Obstetricians and Gynecologists. Practice bulletin No. 144. Multifetal gestations: twin, triplet, and higher-order multifetal pregnancies. Obstet Gynecol. 2014;123(5):1118–1132.
From the maternal perspective, twin pregnancies are known to have higher risks than their singleton counterparts for such complications as hypertension, preeclampsia, diabetes, hemorrhage, cesarean delivery, postpartum depression, and anemia. These complications are managed essentially the same way regardless of the number of fetuses.
From the fetal/neonatal perspective, twin gestations may carry increased risks of congenital anomalies, preterm birth, and aneuploidy, which are managed similarly to singleton gestations overall, with certain adjustments as necessary.
Twin pregnancies do have unique risks, however, that are managed differently from the time chorionicity is established until delivery. The level of risk increases as the number of chorions and amnions decreases.
A basic management plan for twin gestations consists of a number of components, elucidated below.
1. Determine chorionicity and amnionicityThis determination is most reliably performed late in the first trimester and must be done using ultrasound. The inter-twin membrane should be identified. At 11 to 14 weeks, the presence of the “lambda sign,” a triangular projection of tissue that extends from the chorionic surface, is indicative of a dichorionic pregnancy, while a “T sign” suggests a monochorionic pregnancy (sensitivities 97%–100%; specificities 98%–100%). Alternatively, demonstration of discordant genders or separate placentas may be used later in pregnancy.
2. Monitor growth every 4 weeks in dichorionic twinsDichorionic twins are, by default, diamniotic. After the anatomic survey, growth surveillance should be conducted approximately every 4 weeks.
Discordant growth usually is defined as a difference of 20% or more in weight between the twins, based on the weight of the larger twin. As an isolated finding with both fetuses of normal weight, this discordance has not been demonstrated to increase adverse outcomes. Routine antenatal surveillance is not necessarily indicated.
Fetal growth restriction of one twin or a coexisting abnormality should prompt antenatal testing and/or earlier delivery. Any maternal comorbidities such as hypertension or diabetes also would be indications for testing. Otherwise, delivery is recommended at 38 weeks’ to 38-6/7 weeks’ gestation.
After 32 weeks, the mode of delivery may be vaginal if the presenting twin is vertex and the delivery provider can perform breech extraction or internal podalic version, if necessary.
3. Monochorionic/diamniotic twins also warrant regular surveillanceThe shared placenta places these pregnancies at increased risk for twin-to-twin transfusion syndrome (TTTS), a fetal-placental imbalance in which one twin “transfuses” the other. Ten percent to 15% of monochorionic pregnancies develop TTTS, which is associated with high rates of morbidity and mortality, even when treated.
Antenatal surveillance of these pregnancies involves ultrasonography assessment every 2 weeks, starting at 16 weeks. At each examination, the deepest vertical pocket (DVP) of fluid and presence of each fetal bladder are documented. This limited assessment alternates with a growth assessment every 2 weeks. SMFM recommends this biweekly assessment until 28 weeks, then every 2 to 3 weeks until delivery.
Stage 1 TTTS is defined by the polyhydramnios/oligohydramnios sequence (DVP of one fetus <2 cm, with DVP of the other >8 cm).
Evaluation for treatment of TTTS with laser coagulation (preferred) or amnio‑reduction should take place after the diagnosis is made, along with increased fetal surveillance.
SMFM also recommends fetal echocardiography due to the 9-fold increased risk of cardiac anomalies in monochorionic pregnancies.
Other complications of monochorionic/diamniotic twins include selective fetal growth restriction (due to unequal sharing of the placenta), twin reversed arterial perfusion (TRAP) sequence, and twin anemia-polycythemia sequence (TAPS).
Antenatal surveillance of all monochorionic twins is recommended, given the increased risk of stillbirth; many centers start testing at 32 weeks’ gestation. According to ACOG, uncomplicated monochorionic/diamniotic twins should be delivered at 34 weeks’ to 37-6/7 weeks’ gestation. Fetal growth restriction or other comorbidities may prompt delivery as early as 32 weeks.
4. Know the risks of monoamniotic twin gestationsThese twins are at increased risk for intrauterine fetal death due to cord entanglement, as well as TTTS, TAPS, and fetal growth restriction. Routine growth assessment and evaluation for TTTS are similar to those for monochorionic/diamniotic twins (without the option of polyhydramnios/oligohydramnios measurement), but the overall management of these pregnancies is unknown.
Protocols may range from outpatient antenatal testing to hospitalization to 24 to 28 weeks’ gestation with daily antenatal testing or attempted continuous monitoring. Delivery by cesarean delivery is recommended at 32 to 34 weeks’ gestation.
What this EVIDENCE means for practice Monochorionic twins need specific and frequent monitoring due to significantly increased risk for both fetal and placental complications. They justify late preterm or early term delivery.
Management of chronic hypertension in pregnancy: Reserve therapy for severe hypertension
Cell-free DNA screening for fetal aneuploidy: Strengths and limitations
Some areas of obstetric care are not as clearcut as others in this time of rapid medical evolution. In this Update, we discuss 3 of them:
- management of twin gestations
- management of chronic hypertension in pregnancy
- cell-free DNA screening for fetal aneuploidy.
To our benefit, both the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) have weighed in on important aspects of these areas of obstetric care.
Society for Maternal-Fetal Medicine, Simpson LL. Twin-twin transfusion syndrome. Am J Obstet Gynecol. 2013;208(1):3–18.
Society for Maternal-Fetal Medicine. Checklists and Safety Bundles. https://www.smfm.org/mfm-practice/checklists-and-safety-bundles. Published March 2015. Accessed December 7, 2015.
American College of Obstetricians and Gynecologists. Practice bulletin No. 144. Multifetal gestations: twin, triplet, and higher-order multifetal pregnancies. Obstet Gynecol. 2014;123(5):1118–1132.
From the maternal perspective, twin pregnancies are known to have higher risks than their singleton counterparts for such complications as hypertension, preeclampsia, diabetes, hemorrhage, cesarean delivery, postpartum depression, and anemia. These complications are managed essentially the same way regardless of the number of fetuses.
From the fetal/neonatal perspective, twin gestations may carry increased risks of congenital anomalies, preterm birth, and aneuploidy, which are managed similarly to singleton gestations overall, with certain adjustments as necessary.
Twin pregnancies do have unique risks, however, that are managed differently from the time chorionicity is established until delivery. The level of risk increases as the number of chorions and amnions decreases.
A basic management plan for twin gestations consists of a number of components, elucidated below.
1. Determine chorionicity and amnionicityThis determination is most reliably performed late in the first trimester and must be done using ultrasound. The inter-twin membrane should be identified. At 11 to 14 weeks, the presence of the “lambda sign,” a triangular projection of tissue that extends from the chorionic surface, is indicative of a dichorionic pregnancy, while a “T sign” suggests a monochorionic pregnancy (sensitivities 97%–100%; specificities 98%–100%). Alternatively, demonstration of discordant genders or separate placentas may be used later in pregnancy.
2. Monitor growth every 4 weeks in dichorionic twinsDichorionic twins are, by default, diamniotic. After the anatomic survey, growth surveillance should be conducted approximately every 4 weeks.
Discordant growth usually is defined as a difference of 20% or more in weight between the twins, based on the weight of the larger twin. As an isolated finding with both fetuses of normal weight, this discordance has not been demonstrated to increase adverse outcomes. Routine antenatal surveillance is not necessarily indicated.
Fetal growth restriction of one twin or a coexisting abnormality should prompt antenatal testing and/or earlier delivery. Any maternal comorbidities such as hypertension or diabetes also would be indications for testing. Otherwise, delivery is recommended at 38 weeks’ to 38-6/7 weeks’ gestation.
After 32 weeks, the mode of delivery may be vaginal if the presenting twin is vertex and the delivery provider can perform breech extraction or internal podalic version, if necessary.
3. Monochorionic/diamniotic twins also warrant regular surveillanceThe shared placenta places these pregnancies at increased risk for twin-to-twin transfusion syndrome (TTTS), a fetal-placental imbalance in which one twin “transfuses” the other. Ten percent to 15% of monochorionic pregnancies develop TTTS, which is associated with high rates of morbidity and mortality, even when treated.
Antenatal surveillance of these pregnancies involves ultrasonography assessment every 2 weeks, starting at 16 weeks. At each examination, the deepest vertical pocket (DVP) of fluid and presence of each fetal bladder are documented. This limited assessment alternates with a growth assessment every 2 weeks. SMFM recommends this biweekly assessment until 28 weeks, then every 2 to 3 weeks until delivery.
Stage 1 TTTS is defined by the polyhydramnios/oligohydramnios sequence (DVP of one fetus <2 cm, with DVP of the other >8 cm).
Evaluation for treatment of TTTS with laser coagulation (preferred) or amnio‑reduction should take place after the diagnosis is made, along with increased fetal surveillance.
SMFM also recommends fetal echocardiography due to the 9-fold increased risk of cardiac anomalies in monochorionic pregnancies.
Other complications of monochorionic/diamniotic twins include selective fetal growth restriction (due to unequal sharing of the placenta), twin reversed arterial perfusion (TRAP) sequence, and twin anemia-polycythemia sequence (TAPS).
Antenatal surveillance of all monochorionic twins is recommended, given the increased risk of stillbirth; many centers start testing at 32 weeks’ gestation. According to ACOG, uncomplicated monochorionic/diamniotic twins should be delivered at 34 weeks’ to 37-6/7 weeks’ gestation. Fetal growth restriction or other comorbidities may prompt delivery as early as 32 weeks.
4. Know the risks of monoamniotic twin gestationsThese twins are at increased risk for intrauterine fetal death due to cord entanglement, as well as TTTS, TAPS, and fetal growth restriction. Routine growth assessment and evaluation for TTTS are similar to those for monochorionic/diamniotic twins (without the option of polyhydramnios/oligohydramnios measurement), but the overall management of these pregnancies is unknown.
Protocols may range from outpatient antenatal testing to hospitalization to 24 to 28 weeks’ gestation with daily antenatal testing or attempted continuous monitoring. Delivery by cesarean delivery is recommended at 32 to 34 weeks’ gestation.
What this EVIDENCE means for practice Monochorionic twins need specific and frequent monitoring due to significantly increased risk for both fetal and placental complications. They justify late preterm or early term delivery.
Management of chronic hypertension in pregnancy: Reserve therapy for severe hypertension
Cell-free DNA screening for fetal aneuploidy: Strengths and limitations
In this article
- Know the risks of monoamniotic twin gestations
- “Less tight” versus “tight” BP control
- Cell-free DNA screening for aneuploidy
2015 Update on obstetrics
Over the past year, much attention has been devoted to labor curves. Is the original Friedman labor curve, which dates to the 1950s, still applicable today? Or do contemporary women labor differently? And if we update our approach to labor management, can we reduce the rate of primary cesarean?
In this Update, we explore these questions, as well as two others:
- How do we minimize infectious morbidity in pregnancy?
- How much prenatal screening is too much?
Is adherence to new labor curves the best way to reduce the rate of primary cesarean?
American College of Obstetricians and Gynecologists. Obstetric Care Consensus No. 1: Safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014;123(3):693–711.
Cohen WR, Friedman EA. Perils of the new labor management guidelines [published online ahead of print September 16, 2014]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2014.09.008.
In 2012, the cesarean delivery rate in the United States remained at 32.8%, a high percentage when one considers the increased risks that major abdominal surgery poses in both the short and long term (blood loss, transfusion, infection, venous thromboembolism, abnormal placentation, hysterectomy).1 The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) have made it a priority to reduce the cesarean delivery rate, focusing their efforts on the primary cesarean. In March 2014, they jointly issued guidelines on the “Safe prevention of the primary cesarean delivery,” highlighting labor dystocia as a top cause.
When contemporary data from the Consortium on Safe Labor were applied to the original Friedman labor curve, investigators found that the active phase of labor may be slower than previously thought.2 The maximum slope for the rate of cervical change was not observed until 6 cm of dilation. This finding potentially changes the point at which arrest of the active phase may be declared. The maximum duration of augmentation with oxytocin also has been extended, based on studies that demonstrated increased vaginal delivery rates.
The Consortium on Safe Labor proposed that, by subjecting a contemporary population to decades-old standards, we have been intervening with primary cesarean too early in the treatment of labor dystocia.
What the guidelines say
The new recommendations from ACOG-SMFM suggest that arrest of the active phase of labor can be declared only when the patient is dilated at least 6 cm with ruptured membranes after either 4 hours of adequate uterine contractions or at least 6 hours of oxytocin administration with inadequate uterine contractions or no cervical change.
Although the recommendations state that there is no maximum duration of the second stage of labor, we may increase the vaginal delivery rate by increasing the duration of pushing to 2 hours for a multiparous patient and 3 hours for a nulliparous patient (with an additional hour when an epidural is given).
Are the recommendations ready for prime time?
In response to the recommendations, Cohen and Friedman (author of the original labor curve) published “Perils of the new labor management guidelines,” cited above. In this commentary, they caution against universal acceptance of the guidelines without further validation. They argue that the analytical method used—and not labor itself—has changed, with possible selection biases and unadjusted confounders altering the shape of the dilatation curve. Cohen and Friedman suggest that serial evaluation of the patient is preferable to an arbitrary cutoff of 6 cm.
They also criticize other aspects of the guidelines, focusing on universal use of intrauterine pressure catheters, amniotomy, and a specific duration of pushing without consideration of descent. A “one size fits all” approach may incur risk to both the mother and the fetus without proven benefit, they contend. Clinical judgment and continuous evaluation of the likelihood and safety of vaginal delivery also are encouraged rather than a reliance on labor curves in isolation.
They urge further validation before adoption of the recommendations. “If we direct our clinical and basic science investigations to the goal of practicing obstetrics in a manner that optimizes maternal and newborn outcomes, the ideal cesarean delivery rate, whatever it may be, will follow,” they write.
What this EVIDENCE means for practice
Proceed with caution when applying labor curves to patients. Use clinical judgment in conjunction with any new guidelines.
Be vigilant for infectious threats to your obstetric population
Jamieson DJ, Uyeki TM, Callaghan WM, Meaney-Delman D, Rasmussen SA. What obstetrician-gynecologists should know about Ebola: a perspective from the Centers for Disease Control and Prevention. Obstet Gynecol. 2014;124(5):1005–1010.
American College of Obstetricians and Gynecologists. Committee Opinion No. 614: Management of pregnant women with presumptive exposure to Listeria monocytogenes. Obstet Gynecol. 2014;124(6):1241–1244.
American College of Obstetricians and Gynecologists. Committee Opinion No. 608: Influenza vaccination during pregnancy. Obstet Gynecol. 2014;124(3):648–651.
We no longer consider pregnancy an immunosuppressed state but, rather, a more immune-modulated system. However, there is no question that the unique physiologic state of pregnancy places a woman and her fetus at increased risk for infection. This was devastatingly obvious during the H1N1 epidemic of 2009 and was reemphasized during a 2014 outbreak of Listeria monocytogenes. We are reminded again during the largest Ebola virus outbreak in history in West Africa, where women have been disproportionately affected.
No neonates have survived Ebola
Although Ebola infections in the United States have been very few, vigilance for people at risk of infection and preparedness to act in the case of infection are vitally important.
The Ebola virus is thought to be spread to humans through contact with infected fruit bats or primates. Human-to-human transmission occurs through direct contact with blood or body fluids (urine, feces, sweat, saliva, breast milk, vomit, semen) of an infected person or contaminated objects (needles, syringes). The incubation period is 2 to 21 days (average, 8–10 days).
Infected people become contagious only upon the appearance of fever and symptoms, which include headache, muscle pain, fatigue, weakness, diarrhea, abdominal pain, vomiting, bleeding, and bruising. The differential diagnosis includes malaria, typhoid, Lassa fever, meningococcal disease, influenza, and Marburg virus.
Treatment of Ebola is supportive care and isolation (standard, contact, and droplet precautions). Prevention is through infection-control precautions and isolation and testing of those exposed, with monitoring for 21 days.
Although pregnant women are not thought to be more susceptible to infection, they are at increased risk of severe illness and mortality, as well as spontaneous abortion and pregnancy-related hemorrhage. No neonates of women infected with Ebola have survived to date.
The CDC recommends that physicians screen patients who have traveled to West Africa and those with fevers and implement appropriate isolation and infection-control precautions. Many hospitals have developed Ebola task forces with this in mind.
Updated information is available at www.cdc.gov/vhf/ebola/index.html.
Pregnant women are highly susceptible to Listeriosis
A nationwide food recall in mid-2014 prompted significant media attention to L monocytogenes, particularly its effect on pregnant women, who have an incidence of Listerial infection 13 times higher than the general population. Although maternal illness is relatively mild, ranging from a complete lack of symptoms to febrile diarrhea, there is an increased risk to the fetus or neonate of loss, preterm labor, neonatal sepsis, meningitis, and death. The perinatal mortality rate is 29%.
The mainstay of prevention during pregnancy is improved food safety and handling, as well as counseling of pregnant women to avoid unpasteurized soft cheeses, raw milk, and unwashed fruits and vegetables, and to avoid or heat thoroughly lunch meats and hot dogs.
When a pregnant woman is exposed to Listeria, management depends on the clinical scenario, as outlined by ACOG:
- Asymptomatic pregnant women do not require testing, treatment, or fetal surveillance. Any development of symptoms within 2 months may justify further evaluation, however.
- Pregnant women with mild gastro-intestinal or flulike symptoms but no fever also can be managed expectantly. Blood cultures may be appropriate; if positive, antibiotic therapy should be initiated.
- A febrile pregnant woman should have blood cultures assessed and be started on antibiotics. The preferred regimen is intravenous ampicillin 6 g/day with or without gentamicin for 14 days. If delivery occurs, placental cultures may be assessed. Listeriosis also can be diagnosed by amniocentesis. Stool cultures are not recommended.
Influenza is largely preventable
It is important to remember that one of the most dangerous viruses for pregnant women can be prevented. However, only 38% to 52% of women who should have received the influenza vaccine around the time of pregnancy actually did so between 2009 and 2013, according to the ACOG Committee Opinion cited above. Pregnant and postpartum women are at increased risk of serious illness, prolonged hospitalization, and death from influenza infection.
The vaccine is safe and effective. Not only does it prevent maternal morbidity and mortality, but it reduces neonatal complications. Inactivated vaccine is recommended for all pregnant women at any gestational age during the flu season.
Because many women are hesitant to accept the vaccine, accurate education is essential to dispel misconceptions about it and its components. It has been shown that if an obstetric clinician recommends the vaccine and makes it available, pregnant patients are five to 50 times more likely to receive it. As obstetricians, we are compelled to make this a priority in our practice.
What this EVIDENCE means for practice
Be alert and ready to act if an infectious threat is noted in your obstetric population. Get your flu shot. Give it to your obstetric patients. And don’t forget that ACOG also supports the administration of one dose of the tetanus, diphtheria, and pertussis vaccine during each pregnancy.
How much prenatal screening is too much?
Goetzinger KR, Odibo AO. Screening for abnormal placentation and adverse pregnancy outcomes with maternal serum biomarkers in the second trimester. Prenatal Diagn. 2014;34(7):635–641.
D’Antonio F, Rijo C, Thilaganathan B, et al. Association between first-trimester maternal serum pregnancy associated plasma protein-A and obstetric complications. Prenatal Diagn. 2013;33(9):839–847.
Dugoff L; Society for Maternal-Fetal Medicine. First- and second-trimester maternal serum markers for aneuploidy and adverse obstetric outcomes. Obstet Gynecol. 2010;115(5):1052–1061.
Martin A, Krishna I, Martina B, et al. Can the quantity of cell-free fetal DNA predict preeclampsia: a systematic review. Prenatal Diagn. 2014;34(7): 685–691.
Audibert F, Boucoiran I, An N, et al. Screening for preeclampsia using first-trimester serum markers and uterine artery Doppler in nulliparous women. Am J Obstet Gynecol. 2010;203(4):383.e1–e8.
Myatt L, Clifton RG, Roberts JM, et al. First-trimester prediction of preeclampsia in nulliparous women at low risk. Obstet Gynecol. 2012;119(6):1234–1242.
The placenta of a normal pregnancy secretes small amounts of a variety of biomarkers such as alpha-fetoprotein (AFP), human chorionic gonadotropin, unconjugated estriol, inhibin A, pregnancy-associated placental protein A (PAPP-A), soluble fms-like tyrosine kinase, and placental growth factor.
The association between abnormal maternal serum biomarkers and abnormal pregnancy outcomes has been known since the 1970s, when elevated AFP was noted in pregnancies with fetal open neural tube defects. Shortly thereafter, low levels of AFP were associated with fetuses with trisomy 21.
One theory is that the abnormality in pregnancy leads to abnormal regulation at the level of the fetal-placental interface and over- or under-secretion of the various biomarkers. An offshoot of this theory is the idea that abnormal placentation (ie, preeclampsia, fetal growth restriction, accreta) also may be reflected in elevated or suppressed secretion of placental biomarkers, which could be used to screen for these conditions during pregnancy.
PAPP-A is a placental serum marker that is a component of first-trimester genetic screening. It is a marker of placental function, and low levels have been associated with fetal growth restriction, preterm birth, preeclampsia, and fetal loss. Another first-trimester marker associated with adverse outcomes is cell-free fetal DNA. This DNA, found in the maternal blood, is a product of placental apoptosis, and elevated levels have been demonstrated in women who develop preeclampsia.
Although many of the biomarkers listed here are not available specifically as a clinical screening test in the United States, the link to common genetic screens makes it tempting to try to add prediction of preeclampsia and other information to an existing test. If specific numbers are reported on the genetic screen for the different markers, that information is already there, and some companies may flag abnormally high or low levels.
However, although the association between abnormal pregnancy outcomes and abnormal biomarkers is well established in the literature, the clinical predictive value is not—nor is there always an effective intervention available. One could argue that low-dose aspirin, which is already recommended for patients with a prior delivery before 34 weeks due to preeclampsia, or more than one prior pregnancy with preeclampsia, could be recommended for patients identified on early screens to be at increased risk for preeclampsia. This approach should be tested in randomized clinical trials before universal adoption.
What this EVIDENCE means for practice
Although it is tempting to use associations to predict adverse events, the clinical value of doing so has not yet been proven. Exercise caution before potentially causing concern for both you and your patient.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews TJ. Births: final data for 2012. Natl Vital Stat Rep. 2013;62(9):1–67.
2. Zhang J, Landy HJ, Branch DW, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Consortium on Safe Labor. Obstet Gynecol. 2010;116(6):1281–1287.
Over the past year, much attention has been devoted to labor curves. Is the original Friedman labor curve, which dates to the 1950s, still applicable today? Or do contemporary women labor differently? And if we update our approach to labor management, can we reduce the rate of primary cesarean?
In this Update, we explore these questions, as well as two others:
- How do we minimize infectious morbidity in pregnancy?
- How much prenatal screening is too much?
Is adherence to new labor curves the best way to reduce the rate of primary cesarean?
American College of Obstetricians and Gynecologists. Obstetric Care Consensus No. 1: Safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014;123(3):693–711.
Cohen WR, Friedman EA. Perils of the new labor management guidelines [published online ahead of print September 16, 2014]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2014.09.008.
In 2012, the cesarean delivery rate in the United States remained at 32.8%, a high percentage when one considers the increased risks that major abdominal surgery poses in both the short and long term (blood loss, transfusion, infection, venous thromboembolism, abnormal placentation, hysterectomy).1 The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) have made it a priority to reduce the cesarean delivery rate, focusing their efforts on the primary cesarean. In March 2014, they jointly issued guidelines on the “Safe prevention of the primary cesarean delivery,” highlighting labor dystocia as a top cause.
When contemporary data from the Consortium on Safe Labor were applied to the original Friedman labor curve, investigators found that the active phase of labor may be slower than previously thought.2 The maximum slope for the rate of cervical change was not observed until 6 cm of dilation. This finding potentially changes the point at which arrest of the active phase may be declared. The maximum duration of augmentation with oxytocin also has been extended, based on studies that demonstrated increased vaginal delivery rates.
The Consortium on Safe Labor proposed that, by subjecting a contemporary population to decades-old standards, we have been intervening with primary cesarean too early in the treatment of labor dystocia.
What the guidelines say
The new recommendations from ACOG-SMFM suggest that arrest of the active phase of labor can be declared only when the patient is dilated at least 6 cm with ruptured membranes after either 4 hours of adequate uterine contractions or at least 6 hours of oxytocin administration with inadequate uterine contractions or no cervical change.
Although the recommendations state that there is no maximum duration of the second stage of labor, we may increase the vaginal delivery rate by increasing the duration of pushing to 2 hours for a multiparous patient and 3 hours for a nulliparous patient (with an additional hour when an epidural is given).
Are the recommendations ready for prime time?
In response to the recommendations, Cohen and Friedman (author of the original labor curve) published “Perils of the new labor management guidelines,” cited above. In this commentary, they caution against universal acceptance of the guidelines without further validation. They argue that the analytical method used—and not labor itself—has changed, with possible selection biases and unadjusted confounders altering the shape of the dilatation curve. Cohen and Friedman suggest that serial evaluation of the patient is preferable to an arbitrary cutoff of 6 cm.
They also criticize other aspects of the guidelines, focusing on universal use of intrauterine pressure catheters, amniotomy, and a specific duration of pushing without consideration of descent. A “one size fits all” approach may incur risk to both the mother and the fetus without proven benefit, they contend. Clinical judgment and continuous evaluation of the likelihood and safety of vaginal delivery also are encouraged rather than a reliance on labor curves in isolation.
They urge further validation before adoption of the recommendations. “If we direct our clinical and basic science investigations to the goal of practicing obstetrics in a manner that optimizes maternal and newborn outcomes, the ideal cesarean delivery rate, whatever it may be, will follow,” they write.
What this EVIDENCE means for practice
Proceed with caution when applying labor curves to patients. Use clinical judgment in conjunction with any new guidelines.
Be vigilant for infectious threats to your obstetric population
Jamieson DJ, Uyeki TM, Callaghan WM, Meaney-Delman D, Rasmussen SA. What obstetrician-gynecologists should know about Ebola: a perspective from the Centers for Disease Control and Prevention. Obstet Gynecol. 2014;124(5):1005–1010.
American College of Obstetricians and Gynecologists. Committee Opinion No. 614: Management of pregnant women with presumptive exposure to Listeria monocytogenes. Obstet Gynecol. 2014;124(6):1241–1244.
American College of Obstetricians and Gynecologists. Committee Opinion No. 608: Influenza vaccination during pregnancy. Obstet Gynecol. 2014;124(3):648–651.
We no longer consider pregnancy an immunosuppressed state but, rather, a more immune-modulated system. However, there is no question that the unique physiologic state of pregnancy places a woman and her fetus at increased risk for infection. This was devastatingly obvious during the H1N1 epidemic of 2009 and was reemphasized during a 2014 outbreak of Listeria monocytogenes. We are reminded again during the largest Ebola virus outbreak in history in West Africa, where women have been disproportionately affected.
No neonates have survived Ebola
Although Ebola infections in the United States have been very few, vigilance for people at risk of infection and preparedness to act in the case of infection are vitally important.
The Ebola virus is thought to be spread to humans through contact with infected fruit bats or primates. Human-to-human transmission occurs through direct contact with blood or body fluids (urine, feces, sweat, saliva, breast milk, vomit, semen) of an infected person or contaminated objects (needles, syringes). The incubation period is 2 to 21 days (average, 8–10 days).
Infected people become contagious only upon the appearance of fever and symptoms, which include headache, muscle pain, fatigue, weakness, diarrhea, abdominal pain, vomiting, bleeding, and bruising. The differential diagnosis includes malaria, typhoid, Lassa fever, meningococcal disease, influenza, and Marburg virus.
Treatment of Ebola is supportive care and isolation (standard, contact, and droplet precautions). Prevention is through infection-control precautions and isolation and testing of those exposed, with monitoring for 21 days.
Although pregnant women are not thought to be more susceptible to infection, they are at increased risk of severe illness and mortality, as well as spontaneous abortion and pregnancy-related hemorrhage. No neonates of women infected with Ebola have survived to date.
The CDC recommends that physicians screen patients who have traveled to West Africa and those with fevers and implement appropriate isolation and infection-control precautions. Many hospitals have developed Ebola task forces with this in mind.
Updated information is available at www.cdc.gov/vhf/ebola/index.html.
Pregnant women are highly susceptible to Listeriosis
A nationwide food recall in mid-2014 prompted significant media attention to L monocytogenes, particularly its effect on pregnant women, who have an incidence of Listerial infection 13 times higher than the general population. Although maternal illness is relatively mild, ranging from a complete lack of symptoms to febrile diarrhea, there is an increased risk to the fetus or neonate of loss, preterm labor, neonatal sepsis, meningitis, and death. The perinatal mortality rate is 29%.
The mainstay of prevention during pregnancy is improved food safety and handling, as well as counseling of pregnant women to avoid unpasteurized soft cheeses, raw milk, and unwashed fruits and vegetables, and to avoid or heat thoroughly lunch meats and hot dogs.
When a pregnant woman is exposed to Listeria, management depends on the clinical scenario, as outlined by ACOG:
- Asymptomatic pregnant women do not require testing, treatment, or fetal surveillance. Any development of symptoms within 2 months may justify further evaluation, however.
- Pregnant women with mild gastro-intestinal or flulike symptoms but no fever also can be managed expectantly. Blood cultures may be appropriate; if positive, antibiotic therapy should be initiated.
- A febrile pregnant woman should have blood cultures assessed and be started on antibiotics. The preferred regimen is intravenous ampicillin 6 g/day with or without gentamicin for 14 days. If delivery occurs, placental cultures may be assessed. Listeriosis also can be diagnosed by amniocentesis. Stool cultures are not recommended.
Influenza is largely preventable
It is important to remember that one of the most dangerous viruses for pregnant women can be prevented. However, only 38% to 52% of women who should have received the influenza vaccine around the time of pregnancy actually did so between 2009 and 2013, according to the ACOG Committee Opinion cited above. Pregnant and postpartum women are at increased risk of serious illness, prolonged hospitalization, and death from influenza infection.
The vaccine is safe and effective. Not only does it prevent maternal morbidity and mortality, but it reduces neonatal complications. Inactivated vaccine is recommended for all pregnant women at any gestational age during the flu season.
Because many women are hesitant to accept the vaccine, accurate education is essential to dispel misconceptions about it and its components. It has been shown that if an obstetric clinician recommends the vaccine and makes it available, pregnant patients are five to 50 times more likely to receive it. As obstetricians, we are compelled to make this a priority in our practice.
What this EVIDENCE means for practice
Be alert and ready to act if an infectious threat is noted in your obstetric population. Get your flu shot. Give it to your obstetric patients. And don’t forget that ACOG also supports the administration of one dose of the tetanus, diphtheria, and pertussis vaccine during each pregnancy.
How much prenatal screening is too much?
Goetzinger KR, Odibo AO. Screening for abnormal placentation and adverse pregnancy outcomes with maternal serum biomarkers in the second trimester. Prenatal Diagn. 2014;34(7):635–641.
D’Antonio F, Rijo C, Thilaganathan B, et al. Association between first-trimester maternal serum pregnancy associated plasma protein-A and obstetric complications. Prenatal Diagn. 2013;33(9):839–847.
Dugoff L; Society for Maternal-Fetal Medicine. First- and second-trimester maternal serum markers for aneuploidy and adverse obstetric outcomes. Obstet Gynecol. 2010;115(5):1052–1061.
Martin A, Krishna I, Martina B, et al. Can the quantity of cell-free fetal DNA predict preeclampsia: a systematic review. Prenatal Diagn. 2014;34(7): 685–691.
Audibert F, Boucoiran I, An N, et al. Screening for preeclampsia using first-trimester serum markers and uterine artery Doppler in nulliparous women. Am J Obstet Gynecol. 2010;203(4):383.e1–e8.
Myatt L, Clifton RG, Roberts JM, et al. First-trimester prediction of preeclampsia in nulliparous women at low risk. Obstet Gynecol. 2012;119(6):1234–1242.
The placenta of a normal pregnancy secretes small amounts of a variety of biomarkers such as alpha-fetoprotein (AFP), human chorionic gonadotropin, unconjugated estriol, inhibin A, pregnancy-associated placental protein A (PAPP-A), soluble fms-like tyrosine kinase, and placental growth factor.
The association between abnormal maternal serum biomarkers and abnormal pregnancy outcomes has been known since the 1970s, when elevated AFP was noted in pregnancies with fetal open neural tube defects. Shortly thereafter, low levels of AFP were associated with fetuses with trisomy 21.
One theory is that the abnormality in pregnancy leads to abnormal regulation at the level of the fetal-placental interface and over- or under-secretion of the various biomarkers. An offshoot of this theory is the idea that abnormal placentation (ie, preeclampsia, fetal growth restriction, accreta) also may be reflected in elevated or suppressed secretion of placental biomarkers, which could be used to screen for these conditions during pregnancy.
PAPP-A is a placental serum marker that is a component of first-trimester genetic screening. It is a marker of placental function, and low levels have been associated with fetal growth restriction, preterm birth, preeclampsia, and fetal loss. Another first-trimester marker associated with adverse outcomes is cell-free fetal DNA. This DNA, found in the maternal blood, is a product of placental apoptosis, and elevated levels have been demonstrated in women who develop preeclampsia.
Although many of the biomarkers listed here are not available specifically as a clinical screening test in the United States, the link to common genetic screens makes it tempting to try to add prediction of preeclampsia and other information to an existing test. If specific numbers are reported on the genetic screen for the different markers, that information is already there, and some companies may flag abnormally high or low levels.
However, although the association between abnormal pregnancy outcomes and abnormal biomarkers is well established in the literature, the clinical predictive value is not—nor is there always an effective intervention available. One could argue that low-dose aspirin, which is already recommended for patients with a prior delivery before 34 weeks due to preeclampsia, or more than one prior pregnancy with preeclampsia, could be recommended for patients identified on early screens to be at increased risk for preeclampsia. This approach should be tested in randomized clinical trials before universal adoption.
What this EVIDENCE means for practice
Although it is tempting to use associations to predict adverse events, the clinical value of doing so has not yet been proven. Exercise caution before potentially causing concern for both you and your patient.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Over the past year, much attention has been devoted to labor curves. Is the original Friedman labor curve, which dates to the 1950s, still applicable today? Or do contemporary women labor differently? And if we update our approach to labor management, can we reduce the rate of primary cesarean?
In this Update, we explore these questions, as well as two others:
- How do we minimize infectious morbidity in pregnancy?
- How much prenatal screening is too much?
Is adherence to new labor curves the best way to reduce the rate of primary cesarean?
American College of Obstetricians and Gynecologists. Obstetric Care Consensus No. 1: Safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014;123(3):693–711.
Cohen WR, Friedman EA. Perils of the new labor management guidelines [published online ahead of print September 16, 2014]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2014.09.008.
In 2012, the cesarean delivery rate in the United States remained at 32.8%, a high percentage when one considers the increased risks that major abdominal surgery poses in both the short and long term (blood loss, transfusion, infection, venous thromboembolism, abnormal placentation, hysterectomy).1 The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) have made it a priority to reduce the cesarean delivery rate, focusing their efforts on the primary cesarean. In March 2014, they jointly issued guidelines on the “Safe prevention of the primary cesarean delivery,” highlighting labor dystocia as a top cause.
When contemporary data from the Consortium on Safe Labor were applied to the original Friedman labor curve, investigators found that the active phase of labor may be slower than previously thought.2 The maximum slope for the rate of cervical change was not observed until 6 cm of dilation. This finding potentially changes the point at which arrest of the active phase may be declared. The maximum duration of augmentation with oxytocin also has been extended, based on studies that demonstrated increased vaginal delivery rates.
The Consortium on Safe Labor proposed that, by subjecting a contemporary population to decades-old standards, we have been intervening with primary cesarean too early in the treatment of labor dystocia.
What the guidelines say
The new recommendations from ACOG-SMFM suggest that arrest of the active phase of labor can be declared only when the patient is dilated at least 6 cm with ruptured membranes after either 4 hours of adequate uterine contractions or at least 6 hours of oxytocin administration with inadequate uterine contractions or no cervical change.
Although the recommendations state that there is no maximum duration of the second stage of labor, we may increase the vaginal delivery rate by increasing the duration of pushing to 2 hours for a multiparous patient and 3 hours for a nulliparous patient (with an additional hour when an epidural is given).
Are the recommendations ready for prime time?
In response to the recommendations, Cohen and Friedman (author of the original labor curve) published “Perils of the new labor management guidelines,” cited above. In this commentary, they caution against universal acceptance of the guidelines without further validation. They argue that the analytical method used—and not labor itself—has changed, with possible selection biases and unadjusted confounders altering the shape of the dilatation curve. Cohen and Friedman suggest that serial evaluation of the patient is preferable to an arbitrary cutoff of 6 cm.
They also criticize other aspects of the guidelines, focusing on universal use of intrauterine pressure catheters, amniotomy, and a specific duration of pushing without consideration of descent. A “one size fits all” approach may incur risk to both the mother and the fetus without proven benefit, they contend. Clinical judgment and continuous evaluation of the likelihood and safety of vaginal delivery also are encouraged rather than a reliance on labor curves in isolation.
They urge further validation before adoption of the recommendations. “If we direct our clinical and basic science investigations to the goal of practicing obstetrics in a manner that optimizes maternal and newborn outcomes, the ideal cesarean delivery rate, whatever it may be, will follow,” they write.
What this EVIDENCE means for practice
Proceed with caution when applying labor curves to patients. Use clinical judgment in conjunction with any new guidelines.
Be vigilant for infectious threats to your obstetric population
Jamieson DJ, Uyeki TM, Callaghan WM, Meaney-Delman D, Rasmussen SA. What obstetrician-gynecologists should know about Ebola: a perspective from the Centers for Disease Control and Prevention. Obstet Gynecol. 2014;124(5):1005–1010.
American College of Obstetricians and Gynecologists. Committee Opinion No. 614: Management of pregnant women with presumptive exposure to Listeria monocytogenes. Obstet Gynecol. 2014;124(6):1241–1244.
American College of Obstetricians and Gynecologists. Committee Opinion No. 608: Influenza vaccination during pregnancy. Obstet Gynecol. 2014;124(3):648–651.
We no longer consider pregnancy an immunosuppressed state but, rather, a more immune-modulated system. However, there is no question that the unique physiologic state of pregnancy places a woman and her fetus at increased risk for infection. This was devastatingly obvious during the H1N1 epidemic of 2009 and was reemphasized during a 2014 outbreak of Listeria monocytogenes. We are reminded again during the largest Ebola virus outbreak in history in West Africa, where women have been disproportionately affected.
No neonates have survived Ebola
Although Ebola infections in the United States have been very few, vigilance for people at risk of infection and preparedness to act in the case of infection are vitally important.
The Ebola virus is thought to be spread to humans through contact with infected fruit bats or primates. Human-to-human transmission occurs through direct contact with blood or body fluids (urine, feces, sweat, saliva, breast milk, vomit, semen) of an infected person or contaminated objects (needles, syringes). The incubation period is 2 to 21 days (average, 8–10 days).
Infected people become contagious only upon the appearance of fever and symptoms, which include headache, muscle pain, fatigue, weakness, diarrhea, abdominal pain, vomiting, bleeding, and bruising. The differential diagnosis includes malaria, typhoid, Lassa fever, meningococcal disease, influenza, and Marburg virus.
Treatment of Ebola is supportive care and isolation (standard, contact, and droplet precautions). Prevention is through infection-control precautions and isolation and testing of those exposed, with monitoring for 21 days.
Although pregnant women are not thought to be more susceptible to infection, they are at increased risk of severe illness and mortality, as well as spontaneous abortion and pregnancy-related hemorrhage. No neonates of women infected with Ebola have survived to date.
The CDC recommends that physicians screen patients who have traveled to West Africa and those with fevers and implement appropriate isolation and infection-control precautions. Many hospitals have developed Ebola task forces with this in mind.
Updated information is available at www.cdc.gov/vhf/ebola/index.html.
Pregnant women are highly susceptible to Listeriosis
A nationwide food recall in mid-2014 prompted significant media attention to L monocytogenes, particularly its effect on pregnant women, who have an incidence of Listerial infection 13 times higher than the general population. Although maternal illness is relatively mild, ranging from a complete lack of symptoms to febrile diarrhea, there is an increased risk to the fetus or neonate of loss, preterm labor, neonatal sepsis, meningitis, and death. The perinatal mortality rate is 29%.
The mainstay of prevention during pregnancy is improved food safety and handling, as well as counseling of pregnant women to avoid unpasteurized soft cheeses, raw milk, and unwashed fruits and vegetables, and to avoid or heat thoroughly lunch meats and hot dogs.
When a pregnant woman is exposed to Listeria, management depends on the clinical scenario, as outlined by ACOG:
- Asymptomatic pregnant women do not require testing, treatment, or fetal surveillance. Any development of symptoms within 2 months may justify further evaluation, however.
- Pregnant women with mild gastro-intestinal or flulike symptoms but no fever also can be managed expectantly. Blood cultures may be appropriate; if positive, antibiotic therapy should be initiated.
- A febrile pregnant woman should have blood cultures assessed and be started on antibiotics. The preferred regimen is intravenous ampicillin 6 g/day with or without gentamicin for 14 days. If delivery occurs, placental cultures may be assessed. Listeriosis also can be diagnosed by amniocentesis. Stool cultures are not recommended.
Influenza is largely preventable
It is important to remember that one of the most dangerous viruses for pregnant women can be prevented. However, only 38% to 52% of women who should have received the influenza vaccine around the time of pregnancy actually did so between 2009 and 2013, according to the ACOG Committee Opinion cited above. Pregnant and postpartum women are at increased risk of serious illness, prolonged hospitalization, and death from influenza infection.
The vaccine is safe and effective. Not only does it prevent maternal morbidity and mortality, but it reduces neonatal complications. Inactivated vaccine is recommended for all pregnant women at any gestational age during the flu season.
Because many women are hesitant to accept the vaccine, accurate education is essential to dispel misconceptions about it and its components. It has been shown that if an obstetric clinician recommends the vaccine and makes it available, pregnant patients are five to 50 times more likely to receive it. As obstetricians, we are compelled to make this a priority in our practice.
What this EVIDENCE means for practice
Be alert and ready to act if an infectious threat is noted in your obstetric population. Get your flu shot. Give it to your obstetric patients. And don’t forget that ACOG also supports the administration of one dose of the tetanus, diphtheria, and pertussis vaccine during each pregnancy.
How much prenatal screening is too much?
Goetzinger KR, Odibo AO. Screening for abnormal placentation and adverse pregnancy outcomes with maternal serum biomarkers in the second trimester. Prenatal Diagn. 2014;34(7):635–641.
D’Antonio F, Rijo C, Thilaganathan B, et al. Association between first-trimester maternal serum pregnancy associated plasma protein-A and obstetric complications. Prenatal Diagn. 2013;33(9):839–847.
Dugoff L; Society for Maternal-Fetal Medicine. First- and second-trimester maternal serum markers for aneuploidy and adverse obstetric outcomes. Obstet Gynecol. 2010;115(5):1052–1061.
Martin A, Krishna I, Martina B, et al. Can the quantity of cell-free fetal DNA predict preeclampsia: a systematic review. Prenatal Diagn. 2014;34(7): 685–691.
Audibert F, Boucoiran I, An N, et al. Screening for preeclampsia using first-trimester serum markers and uterine artery Doppler in nulliparous women. Am J Obstet Gynecol. 2010;203(4):383.e1–e8.
Myatt L, Clifton RG, Roberts JM, et al. First-trimester prediction of preeclampsia in nulliparous women at low risk. Obstet Gynecol. 2012;119(6):1234–1242.
The placenta of a normal pregnancy secretes small amounts of a variety of biomarkers such as alpha-fetoprotein (AFP), human chorionic gonadotropin, unconjugated estriol, inhibin A, pregnancy-associated placental protein A (PAPP-A), soluble fms-like tyrosine kinase, and placental growth factor.
The association between abnormal maternal serum biomarkers and abnormal pregnancy outcomes has been known since the 1970s, when elevated AFP was noted in pregnancies with fetal open neural tube defects. Shortly thereafter, low levels of AFP were associated with fetuses with trisomy 21.
One theory is that the abnormality in pregnancy leads to abnormal regulation at the level of the fetal-placental interface and over- or under-secretion of the various biomarkers. An offshoot of this theory is the idea that abnormal placentation (ie, preeclampsia, fetal growth restriction, accreta) also may be reflected in elevated or suppressed secretion of placental biomarkers, which could be used to screen for these conditions during pregnancy.
PAPP-A is a placental serum marker that is a component of first-trimester genetic screening. It is a marker of placental function, and low levels have been associated with fetal growth restriction, preterm birth, preeclampsia, and fetal loss. Another first-trimester marker associated with adverse outcomes is cell-free fetal DNA. This DNA, found in the maternal blood, is a product of placental apoptosis, and elevated levels have been demonstrated in women who develop preeclampsia.
Although many of the biomarkers listed here are not available specifically as a clinical screening test in the United States, the link to common genetic screens makes it tempting to try to add prediction of preeclampsia and other information to an existing test. If specific numbers are reported on the genetic screen for the different markers, that information is already there, and some companies may flag abnormally high or low levels.
However, although the association between abnormal pregnancy outcomes and abnormal biomarkers is well established in the literature, the clinical predictive value is not—nor is there always an effective intervention available. One could argue that low-dose aspirin, which is already recommended for patients with a prior delivery before 34 weeks due to preeclampsia, or more than one prior pregnancy with preeclampsia, could be recommended for patients identified on early screens to be at increased risk for preeclampsia. This approach should be tested in randomized clinical trials before universal adoption.
What this EVIDENCE means for practice
Although it is tempting to use associations to predict adverse events, the clinical value of doing so has not yet been proven. Exercise caution before potentially causing concern for both you and your patient.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews TJ. Births: final data for 2012. Natl Vital Stat Rep. 2013;62(9):1–67.
2. Zhang J, Landy HJ, Branch DW, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Consortium on Safe Labor. Obstet Gynecol. 2010;116(6):1281–1287.
1. Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews TJ. Births: final data for 2012. Natl Vital Stat Rep. 2013;62(9):1–67.
2. Zhang J, Landy HJ, Branch DW, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Consortium on Safe Labor. Obstet Gynecol. 2010;116(6):1281–1287.
IN THIS ARTICLE
— Is adherence to new labor curves the best way to reduce the rate of primary cesarean?
— Be vigilant for infectious threats to your obstetric population
— How much prenatal screening is too much?
The latest guidance from ACOG on hypertension in pregnancy
In November 2013, the American College of Obstetricians and Gynecologists (ACOG) published a 99-page report on hypertensive disorders in pregnancy. The classification, diagnosis, prediction, prevention, and management of gestational hypertension, preeclampsia, and chronic hypertension were addressed, although preeclampsia was the main focus.
In this audiocast, Dr. Pauli sifts through the guidelines and discusses the changes that will be implemented at her institution.
Dr. Pauli and John T. Repke, MD, are co-authors of the Update on Obstetrics (January 2014).
In November 2013, the American College of Obstetricians and Gynecologists (ACOG) published a 99-page report on hypertensive disorders in pregnancy. The classification, diagnosis, prediction, prevention, and management of gestational hypertension, preeclampsia, and chronic hypertension were addressed, although preeclampsia was the main focus.
In this audiocast, Dr. Pauli sifts through the guidelines and discusses the changes that will be implemented at her institution.
Dr. Pauli and John T. Repke, MD, are co-authors of the Update on Obstetrics (January 2014).
In November 2013, the American College of Obstetricians and Gynecologists (ACOG) published a 99-page report on hypertensive disorders in pregnancy. The classification, diagnosis, prediction, prevention, and management of gestational hypertension, preeclampsia, and chronic hypertension were addressed, although preeclampsia was the main focus.
In this audiocast, Dr. Pauli sifts through the guidelines and discusses the changes that will be implemented at her institution.
Dr. Pauli and John T. Repke, MD, are co-authors of the Update on Obstetrics (January 2014).
Update on Obstetrics
Over the past 20 years, the incidence of preeclampsia in the United States has increased 25%,1 and the disorder is a leading cause of morbidity and death among both mothers and infants. Although considerable progress has been achieved in elucidating the pathophysiology of preeclampsia, greater understanding has not yet carried over into improved clinical practice.
To address this disconnect between data and practice, the American College of Obstetricians and Gynecologists (ACOG) issued a 99-page document in November 2013 to help establish best practices in the diagnosis and management of hypertensive disorders in pregnancy. We begin this article with a look at its major recommendations.
Other notable developments in obstetrics over the past year have been the rapid evolution of noninvasive prenatal testing and the publication of new guidance on screening, diagnosis, and management of gestational diabetes, all of which are addressed in this article.
ACOG AIMS TO CLARIFY BEST PRACTICES IN THE MANAGEMENT OF HYPERTENSION IN PREGNANCY
American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy. Hypertension in Pregnancy. Washington, DC: ACOG; November 2013.
The biggest news of the past year is probably the November 2013 report on hypertension in pregnancy from ACOG, which was developed with three goals in mind:
to summarize current knowledge
to provide best-practice guidelines
to identify areas in which further research is needed.
The classification, diagnosis, prediction, prevention, and management of gestational hypertension, preeclampsia, and chronic hypertension are addressed in the report. Although space constraints prevent us from summarizing the entire document, we would like to highlight the biggest changes and most relevant additions to clinical practice.
Notable recommendations
Classification. Preeclampsia is no longer characterized as “mild” or “severe” but as “preeclampsia without severe features” and “preeclampsia with severe features.” As justification for these changes, the ACOG Task Force on Hypertension in Pregnancy noted that preeclampsia is progressive by nature, so a characterization of “mild” disease is appropriate only at the time of diagnosis. Therefore, “appropriate management mandates frequent reevaluation for severe features.”
Diagnosis of proteinuria. The options are a 24-hour urine collection demonstrating more than 300 mg of protein or a single-specimen urine protein:creatinine ratio of 0.3 mg/dL or higher. Dipstick values should only be used if these quantitative measures are unavailable.
Signs of severe disease. Fetal growth restriction and proteinuria of more than 5 g/24 hr are no longer considered defining features of severe disease.
Severe features now include any of these:
systolic blood pressure (BP) of 160 mm Hg or higher, or diastolic BP of 110 mm Hg or higher on two occasions at least 4 hours apart while the patient is on bed rest (unless antihypertensive therapy is initiated before this time)
thrombocytopenia (platelets <100 x 109/L)
impaired liver function, as indicated by abnormally elevated blood concentrations of liver enzymes (to twice normal concentration) and/or severe, persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses
progressive renal insufficiency (serum creatinine concentration >1.1 mg/dL or a doubling of the serum creatinine concentration in the absence of other renal disease)
pulmonary edema
new-onset visual or central nervous system disturbances.
Related Article: Does an unfavorable cervix preclude induction of labor at term in women who have gestational hypertension or mild preeclampsia? George Macones, MD (Examining the Evidence, December 2012)
Screening for preeclampsia. The use of Doppler studies and serum biomarkers is not recommended, as there is no evidence that early identification translates to improved outcomes.
Prevention of preeclampsia. Low-dose aspirin (60–80 mg/d, starting in the late first trimester) should be offered as primary prevention to:
women with a history of early-onset preeclampsia and delivery before 34 weeks’ gestation
women with a history of preeclampsia in multiple pregnancies
other high-risk patients (chronic hypertension, diabetes).
No other treatments (vitamin C or E, salt restriction, or bed rest) are recommended for the prevention of preeclampsia, although calcium supplementation may be recommended for women with a low baseline dietary intake of calcium.
Use of magnesium sulfate. Universal prophylaxis with magnesium sulfate is not recommended for preeclampsia unless severe features are present or the patient’s clinical condition changes to severe during labor.
Timing of delivery. Recommendations for delivery for patients with hypertensive disorders are:
gestational hypertension or preeclampsia without severe features: 37 weeks’ gestation
preeclampsia with severe features: by 34 weeks
chronic hypertension: not before 38 weeks
chronic hypertension with superimposed preeclampsia: 34 or 37 weeks, depending on the presence of severe features.
All of these recommendations are contingent upon the clinical status of the patient and her fetus. For example, if the fetus develops severe growth restriction (<5%) or oligohydramnios, delivery may be recommended regardless of gestational age, based on fetal testing and maternal stability.
Related Article: A stepwise approach to managing eclampsia and other hypertensive emergencies Baha M. Sibai (October 2013)
Postpartum hypertension. The need for recognition of hypertension in the postpartum period is emphasized, as well as appropriate management, using the following guidelines:
Be aware that BP decreases initially after delivery and then increases 3 to 6 days postpartum, requiring vigilance on the part of the clinician. For this reason, BP monitoring is recommended 72 hours postpartum (inpatient or outpatient) and again in 7 to 10 days in women diagnosed with a hypertensive disorder of pregnancy.
Counsel patients who experience a hypertensive disorder and/or preeclampsia during pregnancy about postpartum preeclampsia, providing strict precautions and explicit instructions regarding its signs and symptoms
If BP remains elevated after the first postpartum day, consider discontinuing nonsteroidal anti-inflammatory drugs (NSAIDs), as they may be related to hypertension
Treat BP that remains above 150/100 mm Hg with antihypertensive therapy
If postpartum preeclampsia is suspected, administer magnesium sulfate for 24 hours.
A culture shift is needed
At our institution, the most significant potential changes to clinical practice may be the elimination of universal magnesium sulfate prophylaxis and the removal of severe fetal growth restriction from the definition of “severe” preeclampsia.
Also, because the use of NSAIDs is widespread for postpartum pain control, a culture change is needed if we are to follow the postpartum recommendations.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Although we suggest that you read the ACOG report thoroughly, remember that its recommendations are only that—recommendations. Also keep in mind that only six of the approximately 60 “recommendations” provided in this report were accompanied by both high-quality evidence and a strong recommendation. There still is room for clinical judgment and individualization of management to specific patient populations.
NONINVASIVE PRENATAL SCREENING IS EXPANDING RAPIDLY—BUT DON’T THROW OUT THAT CVS KIT JUST YET!
ACOG Committee on Genetics.Committee Opinion #545: Noninvasive prenatal testing for fetal aneuploidy. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2012;120(6):1532–1534.
Mennuti MT, Cherry AM, Morrissette JJD, Dugoff L. Is it time to sound an alarm about false-positive cell-free DNA testing for fetal aneuploidy? Am J Obstet Gynecol. 2013;209(5):415–419.
In last year’s Update in Obstetrics, we discussed noninvasive prenatal genetic screening via cell-free fetal DNA, noting that it is a safer (no risk of miscarriage) and faster (starting at 10 weeks’ gestation) way to screen for aneuploidy. The sensitivity and specificity of this test for Trisomy 21 and 18 are over 99%, with slightly lower sensitivity for Trisomy 13 and sex chromosome abnormalities and a false-positive rate of 0.5%.
In a committee opinion published in December 2012, ACOG concluded that
cell-free fetal DNA is an appropriate screening option only for specific groups of patients at risk for aneuploidy:
women older than age 35
women with fetal ultrasonography findings that are concerning for aneuploidy
women with aneuploidy in a prior pregnancy
women with abnormal first- or second-trimester genetic screening tests
parents with a balanced translocation and an increased risk of Trisomy 21 or 13.
Noninvasive aneuploidy testing is for screening only
Negative results are not diagnostic, and all positive results should be confirmed with invasive testing (chorionic villus sampling [CVS] or amniocentesis).
ACOG does not recommend routine use of cell-free fetal DNA without a comprehensive history and adequate patient counseling, as well as a designation of “high risk.”
Over the past year, more options have become available for aneuploidy screening via cell-free fetal DNA, including screening in twin gestations (for Trisomy 21, 18, 13, and the presence of a Y chromosome only) and screening for:
22q deletion (DiGeorge syndrome)
5p– (Cri-du-chat syndrome)
15q (Prader-Willi and Angelman syndromes)
1p (1p36 deletion syndrome)
Trisomy 16
Trisomy 22.
At this rate, the genetic information potentially available via noninvasive testing seems unlimited. It is easy to see how the fact that this is a screening test—not a diagnostic test—could get lost in the excitement.
Other limitations: Noninvasive testing is still not validated in low-risk patients, and the false-positive risk may be higher than original estimates.
Related Article: Noninvasive prenatal DNA testing: A survey of who is using it, and how (Audiocast, June 2013)
The problem of false positives
This issue was addressed by Mennuti and colleagues, who presented eight cases of abnormal cell-free fetal DNA results that were not confirmed by invasive testing.
There are few prospective data about the source of false-positive results; potential mechanisms include an inadequate fetal fraction of cell-free DNA, maternal or placental mosaicism, and a vanishing twin.
Mennuti and colleagues propose that a registry of false-positive and false-negative results be established to gather further data. They also note that as low-risk patients and aneuploidies of lower and lower prevalence are incorporated into noninvasive testing, the false-positive rate will rise. Their findings have implications for patient counseling, patient distress, invasive testing, and reimbursement.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Cell-free fetal DNA is a rapidly expanding screening technology, but it is not ready to replace diagnostic testing. Don’t throw away those CVS and amniocentesis kits just yet—we are a long way from a completely noninvasive world.
WHEN IT COMES TO GESTATIONAL DIABETES, LESS MAY BE MORE
ACOG Committee on Practice Bulletins–Obstetrics. Practice Bulletin #137: Gestational diabetes mellitus. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2013;122(2 Pt 1):406–416.
Gestational diabetes accounts for 90% of diabetic pregnancies, and its incidence has been increasing in the United States along with the obesity epidemic. In recent years, there has been some debate about the best way to screen for, diagnose, and treat gestational diabetes.
Multiple criteria exist for a positive 1-hour (130–140 mg/dL) or 3-hour glucose tolerance test (Carpenter and Coustan vs National Diabetes Data Group), without comparative trials or consensus as to which version is best. Lower cutoffs increase the rate of gestational diabetes by as much as 50%, whereas higher cutoffs lower the false-positive rate and reduce the need for additional tests.
Some groups have recommended moving away from the traditional two-step process to a one-step approach that utilizes the 2-hour, 75-g glucose tolerance test commonly used outside of pregnancy. They argue that this approach would simplify and standardize the process and could improve outcomes in “borderline” pregnancies that would have been missed by less stringent guidelines.
However, the baseline rate of gestational diabetes using this one-step approach would likely increase from 7% to 18% or higher, depending on the patient population. Such an increase would trigger a huge rise in costs and resources needed to care for these patients, without data on outcomes or appropriate therapy for this expanded group of women with gestational diabetes.
Treatment isn't clear-cut, either
Treatment of gestational diabetes centers on labor-intensive glucose monitoring, nutritional interventions, and insulin therapy.
Until recently, the use of oral hypoglycemic agents was not recommended due to limited data. Multiple studies now have been performed to evaluate the safety and efficacy of glyburide and metformin in pregnancy, demonstrating glucose control similar to that achieved with insulin without short-term adverse effects in the mother or newborn. However, as many as 20% to 40% of women using glyburide and 50% of those using metformin require the addition of insulin for adequate glucose control. The long-term effects of these medications are unknown.
Related Article: Does myo-inositol supplementation reduce the rate of gestational diabetes in pregnant women with a family history of type 2 diabetes? E. Albert Reece, MD, PhD, MBA (Examining the Evidence, June 2013)
ACOG weighs in
In an attempt to clarify optimal screening, diagnosis, and treatment, ACOG updated its practice bulletin on gestational diabetes in August 2013. Among its recommendations:
Avoid the 2-hour glucose tolerance test because there is no demonstrated benefit for the increased number of mothers (and their fetuses) that would be identified by this approach. Rather, use the two-step approach of a 1-hour 50-g glucose tolerance test followed by a 3-hour 100-g glucose tolerance test.
In regard to the 1-hour test, ACOG finds either 135 or 140 mg/dL acceptable as a cutoff but recommends that each practice choose one value as a standard and use it consistently. For the 3-hour test, ACOG recommends that each practice choose the version that best fits its population and prevalence of diabetes. At our institution, for example, we have chosen a 1-hour cutoff of 140 mg/dL and the National Diabetes Data Group criteria for the 3-hour test (105, 190, 165, and 145 mg/dL).
Oral glyburide or metformin may be used to treat gestational diabetes, but glyburide (starting at 2.5 mg/d) may be the better choice for glucose control.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Use the two-step screening process to identify gestational diabetes, picking your cutoffs and sticking to them. Oral hypoglycemic agents now are acceptable for treatment, but be prepared to go back to insulin if necessary.
WE WANT TO HEAR FROM YOU. Tell us what you think.
Reference
Wallis AB, Saftlas AF, Hsia J, Atrash HK. Secular trends in the rates of preeclampsia, eclampsia, and gestational hypertension, United States, 1987–2004. Am J Hypertens. 2008;21(5):521–526.
Over the past 20 years, the incidence of preeclampsia in the United States has increased 25%,1 and the disorder is a leading cause of morbidity and death among both mothers and infants. Although considerable progress has been achieved in elucidating the pathophysiology of preeclampsia, greater understanding has not yet carried over into improved clinical practice.
To address this disconnect between data and practice, the American College of Obstetricians and Gynecologists (ACOG) issued a 99-page document in November 2013 to help establish best practices in the diagnosis and management of hypertensive disorders in pregnancy. We begin this article with a look at its major recommendations.
Other notable developments in obstetrics over the past year have been the rapid evolution of noninvasive prenatal testing and the publication of new guidance on screening, diagnosis, and management of gestational diabetes, all of which are addressed in this article.
ACOG AIMS TO CLARIFY BEST PRACTICES IN THE MANAGEMENT OF HYPERTENSION IN PREGNANCY
American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy. Hypertension in Pregnancy. Washington, DC: ACOG; November 2013.
The biggest news of the past year is probably the November 2013 report on hypertension in pregnancy from ACOG, which was developed with three goals in mind:
to summarize current knowledge
to provide best-practice guidelines
to identify areas in which further research is needed.
The classification, diagnosis, prediction, prevention, and management of gestational hypertension, preeclampsia, and chronic hypertension are addressed in the report. Although space constraints prevent us from summarizing the entire document, we would like to highlight the biggest changes and most relevant additions to clinical practice.
Notable recommendations
Classification. Preeclampsia is no longer characterized as “mild” or “severe” but as “preeclampsia without severe features” and “preeclampsia with severe features.” As justification for these changes, the ACOG Task Force on Hypertension in Pregnancy noted that preeclampsia is progressive by nature, so a characterization of “mild” disease is appropriate only at the time of diagnosis. Therefore, “appropriate management mandates frequent reevaluation for severe features.”
Diagnosis of proteinuria. The options are a 24-hour urine collection demonstrating more than 300 mg of protein or a single-specimen urine protein:creatinine ratio of 0.3 mg/dL or higher. Dipstick values should only be used if these quantitative measures are unavailable.
Signs of severe disease. Fetal growth restriction and proteinuria of more than 5 g/24 hr are no longer considered defining features of severe disease.
Severe features now include any of these:
systolic blood pressure (BP) of 160 mm Hg or higher, or diastolic BP of 110 mm Hg or higher on two occasions at least 4 hours apart while the patient is on bed rest (unless antihypertensive therapy is initiated before this time)
thrombocytopenia (platelets <100 x 109/L)
impaired liver function, as indicated by abnormally elevated blood concentrations of liver enzymes (to twice normal concentration) and/or severe, persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses
progressive renal insufficiency (serum creatinine concentration >1.1 mg/dL or a doubling of the serum creatinine concentration in the absence of other renal disease)
pulmonary edema
new-onset visual or central nervous system disturbances.
Related Article: Does an unfavorable cervix preclude induction of labor at term in women who have gestational hypertension or mild preeclampsia? George Macones, MD (Examining the Evidence, December 2012)
Screening for preeclampsia. The use of Doppler studies and serum biomarkers is not recommended, as there is no evidence that early identification translates to improved outcomes.
Prevention of preeclampsia. Low-dose aspirin (60–80 mg/d, starting in the late first trimester) should be offered as primary prevention to:
women with a history of early-onset preeclampsia and delivery before 34 weeks’ gestation
women with a history of preeclampsia in multiple pregnancies
other high-risk patients (chronic hypertension, diabetes).
No other treatments (vitamin C or E, salt restriction, or bed rest) are recommended for the prevention of preeclampsia, although calcium supplementation may be recommended for women with a low baseline dietary intake of calcium.
Use of magnesium sulfate. Universal prophylaxis with magnesium sulfate is not recommended for preeclampsia unless severe features are present or the patient’s clinical condition changes to severe during labor.
Timing of delivery. Recommendations for delivery for patients with hypertensive disorders are:
gestational hypertension or preeclampsia without severe features: 37 weeks’ gestation
preeclampsia with severe features: by 34 weeks
chronic hypertension: not before 38 weeks
chronic hypertension with superimposed preeclampsia: 34 or 37 weeks, depending on the presence of severe features.
All of these recommendations are contingent upon the clinical status of the patient and her fetus. For example, if the fetus develops severe growth restriction (<5%) or oligohydramnios, delivery may be recommended regardless of gestational age, based on fetal testing and maternal stability.
Related Article: A stepwise approach to managing eclampsia and other hypertensive emergencies Baha M. Sibai (October 2013)
Postpartum hypertension. The need for recognition of hypertension in the postpartum period is emphasized, as well as appropriate management, using the following guidelines:
Be aware that BP decreases initially after delivery and then increases 3 to 6 days postpartum, requiring vigilance on the part of the clinician. For this reason, BP monitoring is recommended 72 hours postpartum (inpatient or outpatient) and again in 7 to 10 days in women diagnosed with a hypertensive disorder of pregnancy.
Counsel patients who experience a hypertensive disorder and/or preeclampsia during pregnancy about postpartum preeclampsia, providing strict precautions and explicit instructions regarding its signs and symptoms
If BP remains elevated after the first postpartum day, consider discontinuing nonsteroidal anti-inflammatory drugs (NSAIDs), as they may be related to hypertension
Treat BP that remains above 150/100 mm Hg with antihypertensive therapy
If postpartum preeclampsia is suspected, administer magnesium sulfate for 24 hours.
A culture shift is needed
At our institution, the most significant potential changes to clinical practice may be the elimination of universal magnesium sulfate prophylaxis and the removal of severe fetal growth restriction from the definition of “severe” preeclampsia.
Also, because the use of NSAIDs is widespread for postpartum pain control, a culture change is needed if we are to follow the postpartum recommendations.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Although we suggest that you read the ACOG report thoroughly, remember that its recommendations are only that—recommendations. Also keep in mind that only six of the approximately 60 “recommendations” provided in this report were accompanied by both high-quality evidence and a strong recommendation. There still is room for clinical judgment and individualization of management to specific patient populations.
NONINVASIVE PRENATAL SCREENING IS EXPANDING RAPIDLY—BUT DON’T THROW OUT THAT CVS KIT JUST YET!
ACOG Committee on Genetics.Committee Opinion #545: Noninvasive prenatal testing for fetal aneuploidy. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2012;120(6):1532–1534.
Mennuti MT, Cherry AM, Morrissette JJD, Dugoff L. Is it time to sound an alarm about false-positive cell-free DNA testing for fetal aneuploidy? Am J Obstet Gynecol. 2013;209(5):415–419.
In last year’s Update in Obstetrics, we discussed noninvasive prenatal genetic screening via cell-free fetal DNA, noting that it is a safer (no risk of miscarriage) and faster (starting at 10 weeks’ gestation) way to screen for aneuploidy. The sensitivity and specificity of this test for Trisomy 21 and 18 are over 99%, with slightly lower sensitivity for Trisomy 13 and sex chromosome abnormalities and a false-positive rate of 0.5%.
In a committee opinion published in December 2012, ACOG concluded that
cell-free fetal DNA is an appropriate screening option only for specific groups of patients at risk for aneuploidy:
women older than age 35
women with fetal ultrasonography findings that are concerning for aneuploidy
women with aneuploidy in a prior pregnancy
women with abnormal first- or second-trimester genetic screening tests
parents with a balanced translocation and an increased risk of Trisomy 21 or 13.
Noninvasive aneuploidy testing is for screening only
Negative results are not diagnostic, and all positive results should be confirmed with invasive testing (chorionic villus sampling [CVS] or amniocentesis).
ACOG does not recommend routine use of cell-free fetal DNA without a comprehensive history and adequate patient counseling, as well as a designation of “high risk.”
Over the past year, more options have become available for aneuploidy screening via cell-free fetal DNA, including screening in twin gestations (for Trisomy 21, 18, 13, and the presence of a Y chromosome only) and screening for:
22q deletion (DiGeorge syndrome)
5p– (Cri-du-chat syndrome)
15q (Prader-Willi and Angelman syndromes)
1p (1p36 deletion syndrome)
Trisomy 16
Trisomy 22.
At this rate, the genetic information potentially available via noninvasive testing seems unlimited. It is easy to see how the fact that this is a screening test—not a diagnostic test—could get lost in the excitement.
Other limitations: Noninvasive testing is still not validated in low-risk patients, and the false-positive risk may be higher than original estimates.
Related Article: Noninvasive prenatal DNA testing: A survey of who is using it, and how (Audiocast, June 2013)
The problem of false positives
This issue was addressed by Mennuti and colleagues, who presented eight cases of abnormal cell-free fetal DNA results that were not confirmed by invasive testing.
There are few prospective data about the source of false-positive results; potential mechanisms include an inadequate fetal fraction of cell-free DNA, maternal or placental mosaicism, and a vanishing twin.
Mennuti and colleagues propose that a registry of false-positive and false-negative results be established to gather further data. They also note that as low-risk patients and aneuploidies of lower and lower prevalence are incorporated into noninvasive testing, the false-positive rate will rise. Their findings have implications for patient counseling, patient distress, invasive testing, and reimbursement.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Cell-free fetal DNA is a rapidly expanding screening technology, but it is not ready to replace diagnostic testing. Don’t throw away those CVS and amniocentesis kits just yet—we are a long way from a completely noninvasive world.
WHEN IT COMES TO GESTATIONAL DIABETES, LESS MAY BE MORE
ACOG Committee on Practice Bulletins–Obstetrics. Practice Bulletin #137: Gestational diabetes mellitus. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2013;122(2 Pt 1):406–416.
Gestational diabetes accounts for 90% of diabetic pregnancies, and its incidence has been increasing in the United States along with the obesity epidemic. In recent years, there has been some debate about the best way to screen for, diagnose, and treat gestational diabetes.
Multiple criteria exist for a positive 1-hour (130–140 mg/dL) or 3-hour glucose tolerance test (Carpenter and Coustan vs National Diabetes Data Group), without comparative trials or consensus as to which version is best. Lower cutoffs increase the rate of gestational diabetes by as much as 50%, whereas higher cutoffs lower the false-positive rate and reduce the need for additional tests.
Some groups have recommended moving away from the traditional two-step process to a one-step approach that utilizes the 2-hour, 75-g glucose tolerance test commonly used outside of pregnancy. They argue that this approach would simplify and standardize the process and could improve outcomes in “borderline” pregnancies that would have been missed by less stringent guidelines.
However, the baseline rate of gestational diabetes using this one-step approach would likely increase from 7% to 18% or higher, depending on the patient population. Such an increase would trigger a huge rise in costs and resources needed to care for these patients, without data on outcomes or appropriate therapy for this expanded group of women with gestational diabetes.
Treatment isn't clear-cut, either
Treatment of gestational diabetes centers on labor-intensive glucose monitoring, nutritional interventions, and insulin therapy.
Until recently, the use of oral hypoglycemic agents was not recommended due to limited data. Multiple studies now have been performed to evaluate the safety and efficacy of glyburide and metformin in pregnancy, demonstrating glucose control similar to that achieved with insulin without short-term adverse effects in the mother or newborn. However, as many as 20% to 40% of women using glyburide and 50% of those using metformin require the addition of insulin for adequate glucose control. The long-term effects of these medications are unknown.
Related Article: Does myo-inositol supplementation reduce the rate of gestational diabetes in pregnant women with a family history of type 2 diabetes? E. Albert Reece, MD, PhD, MBA (Examining the Evidence, June 2013)
ACOG weighs in
In an attempt to clarify optimal screening, diagnosis, and treatment, ACOG updated its practice bulletin on gestational diabetes in August 2013. Among its recommendations:
Avoid the 2-hour glucose tolerance test because there is no demonstrated benefit for the increased number of mothers (and their fetuses) that would be identified by this approach. Rather, use the two-step approach of a 1-hour 50-g glucose tolerance test followed by a 3-hour 100-g glucose tolerance test.
In regard to the 1-hour test, ACOG finds either 135 or 140 mg/dL acceptable as a cutoff but recommends that each practice choose one value as a standard and use it consistently. For the 3-hour test, ACOG recommends that each practice choose the version that best fits its population and prevalence of diabetes. At our institution, for example, we have chosen a 1-hour cutoff of 140 mg/dL and the National Diabetes Data Group criteria for the 3-hour test (105, 190, 165, and 145 mg/dL).
Oral glyburide or metformin may be used to treat gestational diabetes, but glyburide (starting at 2.5 mg/d) may be the better choice for glucose control.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Use the two-step screening process to identify gestational diabetes, picking your cutoffs and sticking to them. Oral hypoglycemic agents now are acceptable for treatment, but be prepared to go back to insulin if necessary.
WE WANT TO HEAR FROM YOU. Tell us what you think.
Over the past 20 years, the incidence of preeclampsia in the United States has increased 25%,1 and the disorder is a leading cause of morbidity and death among both mothers and infants. Although considerable progress has been achieved in elucidating the pathophysiology of preeclampsia, greater understanding has not yet carried over into improved clinical practice.
To address this disconnect between data and practice, the American College of Obstetricians and Gynecologists (ACOG) issued a 99-page document in November 2013 to help establish best practices in the diagnosis and management of hypertensive disorders in pregnancy. We begin this article with a look at its major recommendations.
Other notable developments in obstetrics over the past year have been the rapid evolution of noninvasive prenatal testing and the publication of new guidance on screening, diagnosis, and management of gestational diabetes, all of which are addressed in this article.
ACOG AIMS TO CLARIFY BEST PRACTICES IN THE MANAGEMENT OF HYPERTENSION IN PREGNANCY
American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy. Hypertension in Pregnancy. Washington, DC: ACOG; November 2013.
The biggest news of the past year is probably the November 2013 report on hypertension in pregnancy from ACOG, which was developed with three goals in mind:
to summarize current knowledge
to provide best-practice guidelines
to identify areas in which further research is needed.
The classification, diagnosis, prediction, prevention, and management of gestational hypertension, preeclampsia, and chronic hypertension are addressed in the report. Although space constraints prevent us from summarizing the entire document, we would like to highlight the biggest changes and most relevant additions to clinical practice.
Notable recommendations
Classification. Preeclampsia is no longer characterized as “mild” or “severe” but as “preeclampsia without severe features” and “preeclampsia with severe features.” As justification for these changes, the ACOG Task Force on Hypertension in Pregnancy noted that preeclampsia is progressive by nature, so a characterization of “mild” disease is appropriate only at the time of diagnosis. Therefore, “appropriate management mandates frequent reevaluation for severe features.”
Diagnosis of proteinuria. The options are a 24-hour urine collection demonstrating more than 300 mg of protein or a single-specimen urine protein:creatinine ratio of 0.3 mg/dL or higher. Dipstick values should only be used if these quantitative measures are unavailable.
Signs of severe disease. Fetal growth restriction and proteinuria of more than 5 g/24 hr are no longer considered defining features of severe disease.
Severe features now include any of these:
systolic blood pressure (BP) of 160 mm Hg or higher, or diastolic BP of 110 mm Hg or higher on two occasions at least 4 hours apart while the patient is on bed rest (unless antihypertensive therapy is initiated before this time)
thrombocytopenia (platelets <100 x 109/L)
impaired liver function, as indicated by abnormally elevated blood concentrations of liver enzymes (to twice normal concentration) and/or severe, persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses
progressive renal insufficiency (serum creatinine concentration >1.1 mg/dL or a doubling of the serum creatinine concentration in the absence of other renal disease)
pulmonary edema
new-onset visual or central nervous system disturbances.
Related Article: Does an unfavorable cervix preclude induction of labor at term in women who have gestational hypertension or mild preeclampsia? George Macones, MD (Examining the Evidence, December 2012)
Screening for preeclampsia. The use of Doppler studies and serum biomarkers is not recommended, as there is no evidence that early identification translates to improved outcomes.
Prevention of preeclampsia. Low-dose aspirin (60–80 mg/d, starting in the late first trimester) should be offered as primary prevention to:
women with a history of early-onset preeclampsia and delivery before 34 weeks’ gestation
women with a history of preeclampsia in multiple pregnancies
other high-risk patients (chronic hypertension, diabetes).
No other treatments (vitamin C or E, salt restriction, or bed rest) are recommended for the prevention of preeclampsia, although calcium supplementation may be recommended for women with a low baseline dietary intake of calcium.
Use of magnesium sulfate. Universal prophylaxis with magnesium sulfate is not recommended for preeclampsia unless severe features are present or the patient’s clinical condition changes to severe during labor.
Timing of delivery. Recommendations for delivery for patients with hypertensive disorders are:
gestational hypertension or preeclampsia without severe features: 37 weeks’ gestation
preeclampsia with severe features: by 34 weeks
chronic hypertension: not before 38 weeks
chronic hypertension with superimposed preeclampsia: 34 or 37 weeks, depending on the presence of severe features.
All of these recommendations are contingent upon the clinical status of the patient and her fetus. For example, if the fetus develops severe growth restriction (<5%) or oligohydramnios, delivery may be recommended regardless of gestational age, based on fetal testing and maternal stability.
Related Article: A stepwise approach to managing eclampsia and other hypertensive emergencies Baha M. Sibai (October 2013)
Postpartum hypertension. The need for recognition of hypertension in the postpartum period is emphasized, as well as appropriate management, using the following guidelines:
Be aware that BP decreases initially after delivery and then increases 3 to 6 days postpartum, requiring vigilance on the part of the clinician. For this reason, BP monitoring is recommended 72 hours postpartum (inpatient or outpatient) and again in 7 to 10 days in women diagnosed with a hypertensive disorder of pregnancy.
Counsel patients who experience a hypertensive disorder and/or preeclampsia during pregnancy about postpartum preeclampsia, providing strict precautions and explicit instructions regarding its signs and symptoms
If BP remains elevated after the first postpartum day, consider discontinuing nonsteroidal anti-inflammatory drugs (NSAIDs), as they may be related to hypertension
Treat BP that remains above 150/100 mm Hg with antihypertensive therapy
If postpartum preeclampsia is suspected, administer magnesium sulfate for 24 hours.
A culture shift is needed
At our institution, the most significant potential changes to clinical practice may be the elimination of universal magnesium sulfate prophylaxis and the removal of severe fetal growth restriction from the definition of “severe” preeclampsia.
Also, because the use of NSAIDs is widespread for postpartum pain control, a culture change is needed if we are to follow the postpartum recommendations.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Although we suggest that you read the ACOG report thoroughly, remember that its recommendations are only that—recommendations. Also keep in mind that only six of the approximately 60 “recommendations” provided in this report were accompanied by both high-quality evidence and a strong recommendation. There still is room for clinical judgment and individualization of management to specific patient populations.
NONINVASIVE PRENATAL SCREENING IS EXPANDING RAPIDLY—BUT DON’T THROW OUT THAT CVS KIT JUST YET!
ACOG Committee on Genetics.Committee Opinion #545: Noninvasive prenatal testing for fetal aneuploidy. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2012;120(6):1532–1534.
Mennuti MT, Cherry AM, Morrissette JJD, Dugoff L. Is it time to sound an alarm about false-positive cell-free DNA testing for fetal aneuploidy? Am J Obstet Gynecol. 2013;209(5):415–419.
In last year’s Update in Obstetrics, we discussed noninvasive prenatal genetic screening via cell-free fetal DNA, noting that it is a safer (no risk of miscarriage) and faster (starting at 10 weeks’ gestation) way to screen for aneuploidy. The sensitivity and specificity of this test for Trisomy 21 and 18 are over 99%, with slightly lower sensitivity for Trisomy 13 and sex chromosome abnormalities and a false-positive rate of 0.5%.
In a committee opinion published in December 2012, ACOG concluded that
cell-free fetal DNA is an appropriate screening option only for specific groups of patients at risk for aneuploidy:
women older than age 35
women with fetal ultrasonography findings that are concerning for aneuploidy
women with aneuploidy in a prior pregnancy
women with abnormal first- or second-trimester genetic screening tests
parents with a balanced translocation and an increased risk of Trisomy 21 or 13.
Noninvasive aneuploidy testing is for screening only
Negative results are not diagnostic, and all positive results should be confirmed with invasive testing (chorionic villus sampling [CVS] or amniocentesis).
ACOG does not recommend routine use of cell-free fetal DNA without a comprehensive history and adequate patient counseling, as well as a designation of “high risk.”
Over the past year, more options have become available for aneuploidy screening via cell-free fetal DNA, including screening in twin gestations (for Trisomy 21, 18, 13, and the presence of a Y chromosome only) and screening for:
22q deletion (DiGeorge syndrome)
5p– (Cri-du-chat syndrome)
15q (Prader-Willi and Angelman syndromes)
1p (1p36 deletion syndrome)
Trisomy 16
Trisomy 22.
At this rate, the genetic information potentially available via noninvasive testing seems unlimited. It is easy to see how the fact that this is a screening test—not a diagnostic test—could get lost in the excitement.
Other limitations: Noninvasive testing is still not validated in low-risk patients, and the false-positive risk may be higher than original estimates.
Related Article: Noninvasive prenatal DNA testing: A survey of who is using it, and how (Audiocast, June 2013)
The problem of false positives
This issue was addressed by Mennuti and colleagues, who presented eight cases of abnormal cell-free fetal DNA results that were not confirmed by invasive testing.
There are few prospective data about the source of false-positive results; potential mechanisms include an inadequate fetal fraction of cell-free DNA, maternal or placental mosaicism, and a vanishing twin.
Mennuti and colleagues propose that a registry of false-positive and false-negative results be established to gather further data. They also note that as low-risk patients and aneuploidies of lower and lower prevalence are incorporated into noninvasive testing, the false-positive rate will rise. Their findings have implications for patient counseling, patient distress, invasive testing, and reimbursement.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Cell-free fetal DNA is a rapidly expanding screening technology, but it is not ready to replace diagnostic testing. Don’t throw away those CVS and amniocentesis kits just yet—we are a long way from a completely noninvasive world.
WHEN IT COMES TO GESTATIONAL DIABETES, LESS MAY BE MORE
ACOG Committee on Practice Bulletins–Obstetrics. Practice Bulletin #137: Gestational diabetes mellitus. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2013;122(2 Pt 1):406–416.
Gestational diabetes accounts for 90% of diabetic pregnancies, and its incidence has been increasing in the United States along with the obesity epidemic. In recent years, there has been some debate about the best way to screen for, diagnose, and treat gestational diabetes.
Multiple criteria exist for a positive 1-hour (130–140 mg/dL) or 3-hour glucose tolerance test (Carpenter and Coustan vs National Diabetes Data Group), without comparative trials or consensus as to which version is best. Lower cutoffs increase the rate of gestational diabetes by as much as 50%, whereas higher cutoffs lower the false-positive rate and reduce the need for additional tests.
Some groups have recommended moving away from the traditional two-step process to a one-step approach that utilizes the 2-hour, 75-g glucose tolerance test commonly used outside of pregnancy. They argue that this approach would simplify and standardize the process and could improve outcomes in “borderline” pregnancies that would have been missed by less stringent guidelines.
However, the baseline rate of gestational diabetes using this one-step approach would likely increase from 7% to 18% or higher, depending on the patient population. Such an increase would trigger a huge rise in costs and resources needed to care for these patients, without data on outcomes or appropriate therapy for this expanded group of women with gestational diabetes.
Treatment isn't clear-cut, either
Treatment of gestational diabetes centers on labor-intensive glucose monitoring, nutritional interventions, and insulin therapy.
Until recently, the use of oral hypoglycemic agents was not recommended due to limited data. Multiple studies now have been performed to evaluate the safety and efficacy of glyburide and metformin in pregnancy, demonstrating glucose control similar to that achieved with insulin without short-term adverse effects in the mother or newborn. However, as many as 20% to 40% of women using glyburide and 50% of those using metformin require the addition of insulin for adequate glucose control. The long-term effects of these medications are unknown.
Related Article: Does myo-inositol supplementation reduce the rate of gestational diabetes in pregnant women with a family history of type 2 diabetes? E. Albert Reece, MD, PhD, MBA (Examining the Evidence, June 2013)
ACOG weighs in
In an attempt to clarify optimal screening, diagnosis, and treatment, ACOG updated its practice bulletin on gestational diabetes in August 2013. Among its recommendations:
Avoid the 2-hour glucose tolerance test because there is no demonstrated benefit for the increased number of mothers (and their fetuses) that would be identified by this approach. Rather, use the two-step approach of a 1-hour 50-g glucose tolerance test followed by a 3-hour 100-g glucose tolerance test.
In regard to the 1-hour test, ACOG finds either 135 or 140 mg/dL acceptable as a cutoff but recommends that each practice choose one value as a standard and use it consistently. For the 3-hour test, ACOG recommends that each practice choose the version that best fits its population and prevalence of diabetes. At our institution, for example, we have chosen a 1-hour cutoff of 140 mg/dL and the National Diabetes Data Group criteria for the 3-hour test (105, 190, 165, and 145 mg/dL).
Oral glyburide or metformin may be used to treat gestational diabetes, but glyburide (starting at 2.5 mg/d) may be the better choice for glucose control.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Use the two-step screening process to identify gestational diabetes, picking your cutoffs and sticking to them. Oral hypoglycemic agents now are acceptable for treatment, but be prepared to go back to insulin if necessary.
WE WANT TO HEAR FROM YOU. Tell us what you think.
Reference
Wallis AB, Saftlas AF, Hsia J, Atrash HK. Secular trends in the rates of preeclampsia, eclampsia, and gestational hypertension, United States, 1987–2004. Am J Hypertens. 2008;21(5):521–526.
Reference
Wallis AB, Saftlas AF, Hsia J, Atrash HK. Secular trends in the rates of preeclampsia, eclampsia, and gestational hypertension, United States, 1987–2004. Am J Hypertens. 2008;21(5):521–526.
UPDATE ON OBSTETRICS
The authors report no financial relationships relevant to this article.
If there have been overriding themes in obstetrics over the past year, they have been “more,” “sooner,” “faster,” “safer.” Advances in our field have thrilled our scientific curiosity and increased our ability to alleviate suffering—but at what cost? And who will pay that cost?
In this Update, we focus on recent advances in prenatal diagnosis and fetal therapy, as well as the ever-encroaching economic barriers that may limit our ability to get what we want. In particular, we will discuss:
- two technologies in prenatal genetics: noninvasive aneuploidy testing using cell-free DNA and prenatal microarray analysis
- open fetal surgery to reduce mortality and improve the function and quality of life for fetuses with open neural tube defects
- the value and probable impact of bundled payments—that is, one payment for multiple services grouped into one “episode.”
Two noninvasive approaches to prenatal diagnosis offer promise—but practicality and cost are uncertain
Ashoor G, Syngelaki RM, Wagner M, Birdir C, Nicolaides KH. Chromosome-selective sequencing of maternal plasma cell-free DNA for first-trimester detection of trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):322.e1–e5.
Reddy UM, Page GP, Saade GR, et al. Karyotype versus microarray testing for genetic abnormalities after stillbirth. N Engl J Med. 2012;367(23):2185–2193.
Talkowski ME, Ordulu Z, Pillalamarri V, et al. Clinical diagnosis by whole-genome sequencing of a prenatal sample. N Engl J Med. 2012;367(23):2226–2232.
Wapner RJ, Martin CL, Levy B, et al. Chromosomal microarray versus karyotyping for prenatal diagnosis. N Engl J Med. 2012;367(23):2175–2184.
Genetic screening and testing are a standard part of prenatal care in most developed countries. We have come a long way since a maternal age of 35 years was the only variable separating patients into low- and high-risk categories. This year, two technologies have emerged that may change forever the way we approach prenatal genetics:
One argument for using more accurate genetic screening methods: They limit the number of invasive tests that are needed. Chorionic villus sampling (CVS) and amniocentesis, even when performed by the most experienced of operators, pose a small but real risk of fetal injury and pregnancy loss.
Noninvasive aneuploidy diagnosis is now a reality in high-risk population screening
The holy grail of aneuploidy diagnosis would be a noninvasive way to sample fetal cells. Although we have known for decades that fetal cells enter the maternal circulation, it has been impractical to use them for aneuploidy testing because of their scarcity and longevity. In the 1990s, however, cell-free fetal DNA (cffDNA), a compound of DNA fragments of uncertain origin, was identified in maternal plasma. CffDNA is more plentiful than fetal cells. It also disappears within hours of delivery, demonstrating that it is specific to the current pregnancy.
CffDNA is already used in fetal Rh typing and gender determination in disorders such as congenital adrenal hyperplasia. Several studies in high-risk populations have demonstrated high sensitivity and specificity for the detection of Trisomies 21, 18, and 13. Several commercial tests are now available, although neither their accuracy nor their cost has been determined for use in low-risk population screening, compared with traditional testing.
Microarray analysis, paired with karyotyping, can elucidate ultrasound-identified fetal anomalies
Cytogenetic microarray analysis is also being explored in the prenatal period. Microarray analysis is currently used as a first-line test for infants and children who demonstrate developmental delay, autism spectrum disorders, dysmorphic features, and congenital anomalies. As many as 15% of patients with an otherwise normal karyotype will have a clinically significant copy number variant (CNV) on microarray. This finding has led to the use of microarray analysis in conjunction with karyotyping for fetuses with ultrasound-identified anomalies. Both targeted arrays (for syndromes associated with ultrasound anomalies) and whole-genome arrays are available.

Recent data from a study from the National Institute of Child Health and Human Development (NICHD) reveal that the prenatal detection rates for aneuploidy and unbalanced translocations are comparable between microarray analysis and karyotyping. Microarray analysis did not, however, detect triploidies or balanced translocations. As many as 6% of patients with a normal karyotype and structural anomalies and 1.7% of patients with advanced maternal age or positive screening tests had either a known or potentially clinically relevant CNV. This large study concluded that microarray analysis not only provides equal detection of aneuploidy but also more information in the form of CNVs, compared with karyotyping alone.
Microarray analysis also has been used in the study of pregnancy loss and stillbirth because it does not require viable or intact tissue as a source of DNA—an advantage, compared with traditional karyotyping. A recent study from the Stillbirth Collaborative Research Network demonstrated that genetic results in cases involving stillbirth were obtained more frequently via microarray analysis (87.4%) than by karyotype (70.5%). In addition, more genetic abnormalities (aneuploidy, pathogenic CNVs, and CNVs of unknown clinical significance) were detected by microarray analysis. Investigators concluded that microarray analysis may be especially useful in cases involving stillbirth (when a karyotype cannot be obtained) and structural abnormalities.
We want an accurate, completely risk-free genetic test that can be used for anyone. What we have so far is a technology that must be tested before it can be used in most of our patients—that is, the low-risk ones. We also have access to the fetus’ genetic code on a very specific level.
The total costs of such an approach—test, interpretation, counseling, and long-term follow-up of uncertain results—are unknown at this time and may prove to be unaffordable on a population-wide basis.
Should microarray analysis replace routine prenatal genetic testing?
A major dilemma associated with this technology is the significant amount of time that may be needed to counsel patients when the results are of unclear clinical significance.5 If the fetus has an anomaly, and a related CNV is identified, then counseling of the parents is fairly straightforward. However, if the fetus has an anomaly and a CNV that has not yet been defined, what should the parents be told? Some argue that this information should not be shared with the parents, whereas others recommend full disclosure of all results—even if we do not yet know what to make of them.
Another issue with microarray analysis is its inability to detect balanced translocations, triploidies, and low-level mosaicism, which require either a karyotype or whole-genome sequencing. Microarray analysis is also more expensive than karyotyping, although this may change in the future.
>Fetal therapy involves a complex equation of potential benefits and risks
Adzick NS, Thom EA, Spong CY, et al; MOMS Investigators. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011;364(11):993–1104.
Fetal therapy is broadly defined as any intervention administered to or via the mother with a primary indication to improve perinatal or long-term outcomes for the fetus or newborn. The concept of intervening to prevent the death of a fetus by correcting an anatomic anomaly or halting a disease process in utero is not new. Liley performed the first intrauterine fetal transfusion for Rh alloimmunization in the 1960s. Today, we perform fetal interventions routinely to reduce mortality by giving medical therapy to the mother, such as antenatal corticosteroids to enhance fetal lung maturity or anti-arrhythmics for supraventricular tachycardia. More invasive procedures have proved to be lifesaving (placental laser coagulation for twin-twin transfusion syndrome), ameliorating in the short term (shunting for lower urinary tract obstruction to relieve oligohydramnios), or ultimately not helpful (decompression of hydrocephalus).
Most recently, open fetal surgery has taken center stage as an intervention focused not only on reducing mortality but on improving function and quality of life for fetuses with open neural tube defects (ONTDs). This anomaly was targeted for fetal intervention because, although ONTDs are not generally considered lethal, a significant number of patients die before the age of 5, the majority of patients require shunts that leave them vulnerable to complications, and ONTDs generally impose lifelong intellectual and physical limitations. Repair during fetal life was proposed to prevent damage to the spinal cord and reverse hindbrain herniation, with the goal of improving long-term neurologic function.
The Management of Myelomeningocele Study (MOMS) is a prospective, multicenter trial that randomly assigned fetuses with isolated ONTDs to open fetal repair of myelomeningocele via hysterotomy or to postnatal repair of the defect. Forty percent of infants who underwent fetal repair required placement of a shunt, compared with 82% of those who had postnatal repair (relative risk, 0.48; 97.7% CI, 0.36 to 0.64; P<.001). Infants in the fetal-repair group also had significantly improved composite scores for mental development and motor function at 30 months (P = .007), as well as improvement in secondary outcomes such as hindbrain herniation and independent walking at 30 months.
As exciting as these results are, open fetal surgery still has significant limitations. The few centers that perform the most complex surgeries often have strict exclusion criteria, including maternal body mass index (BMI) greater than 35 kg/m2 and other medical comorbidities. The surgery also poses real risks for both mother and fetus. In the MOMS trial, the risk of preterm labor increased in the fetal-repair group, compared with postnatal repair (38% vs 14%), as did the risk of premature rupture of membranes (46% vs 8%). The fetal-repair group delivered more than 3 weeks earlier than the postnatal repair group (34 vs 37 weeks). Twenty-five percent of the fetal-repair group had thinning of the uterine scar, with uterine dehiscence seen in 10%. When myelomeningocele is repaired during fetal life, mothers require two hysterotomies during pregnancy and face an increased risk of uterine rupture and preterm delivery in subsequent pregnancies. The use of tocolytics exposes these mothers to an increased risk of pulmonary edema (6% in the fetal-repair group vs 0% for postnatal repair).
Other issues that should be addressed:
- the need for rigorous study of open fetal surgery for other fetal anomalies
- prognostic factors for success and for complications
- long-term outcomes in neurologic development of children and fertility of mothers
- a comparison of costs between fetal and postnatal treatment.
Although we may want to intervene as early in life as possible (that is, the fetal period) to achieve the best outcomes for the child, we need to weigh the short-term benefits of intervention against the known risks that intervention poses for the mother in the current pregnancy as well as the potential implications for future pregnancies (ie, the need for all future deliveries to be by cesarean section), not to mention the unknown long-term effects of intervention on both the child and society.
Bundled payments may help us deliver higher-quality, more efficient, and less costly care
Centers for Medicare and Medicaid Services, US Department of Health and Human Services. Fact Sheet: Bundled Payments for Care Improvement Initiative. Washington, DC: DHS; 2011. http://innovations.cms.gov/Files/fact-sheet/Bundled-Payment-Fact-Sheet.pdf. Accessed December 6, 2012.
There is little question that health care in the United States needs reform. The culture of “more is better” is not sustainable economically—nor does our health as a whole reflect the amount of money that we spend on health care, compared with other countries. Although the future is not yet clear, one proposed mechanism for reform is the institution of bundled payments—the grouping of multiple services into one “episode” for payment purposes. An episode might include inpatient hospitalization for pneumonia, for example, or the grouping of surgery with post-discharge care. In obstetrics, all pregnancy care could be grouped into one episode. The concept behind bundled payments is to provide incentives to institutions and providers to delivery higher-quality, more efficient, and less costly care.
If bundled payments become the reality for obstetric care in the future, how will that affect the way we care for our patients? Instead of blindly ordering all available tests, we need to consider thoroughly whether the patient truly needs a test to improve pregnancy outcomes. We also need to consider whether other measures might be avoided safely to keep costs within the bundle. A few examples:
- Is a screening fetal echocardiogram really necessary in a diabetic woman if the ultrasound anatomy scan is sufficient to rule out any cardiac anomaly that might require intervention in the delivery room?
- How will we integrate the expense of cell-free fetal DNA aneuploidy testing and microarray analysis, not to mention the extended counseling sessions that will be necessary to explain findings of uncertain clinical significance, into the bundle? Will “low-risk” patients need to pay out of pocket?
Few physicians entered medicine to worry about costs. Most of us want to worry about our patients. Yet, the reality is that scientific curiosity and a desire to do more—and to do it sooner, faster, and safer—are no longer sufficient justifications for many clinical decisions. We soon may need to figure out how to get what we need without spending as much in the process. In doing so, we may find ourselves moving away from the computer screen and back to the bedside—where we belong.
- Will a second ultrasound scan to visualize the fetal spine in a patient with a normal alpha-fetoprotein level be included in the bundle or paid for by the patient?
These issues may seem trivial, but we can no longer afford to order every test available. We will need to spend more time examining and counseling our patients so that they feel they are still getting the best care possible.
We want to hear from you! Tell us what you think.
1. Chiu RWK, Lo YMD. Noninvasive prenatal diagnosis by fetal nucleic acid analysis in maternal plasma: the coming of age. Semin Fetal Neonatal Med. 2011;16(2):88-93.
2. Chiu RWK, Lo YMD. Noninvasive prenatal diagnosis empowered by high-throughput sequencing. Prenat Diagn. 2012;32(4):401-406.
3. Savage MS, Mourad MJ, Wapner RJ. Evolving applications of microarray analysis in prenatal diagnosis. Curr Opin Obstet Gynecol. 2011;23(2):103-108.
4. Dugoff L. Application of genomic technology in prenatal diagnosis [editorial]. N Engl J Med. 2012;367(23):2249-2251.
5. Wapner RJ, Driscoll DA, Simpson JL. Integration of microarray technology into prenatal diagnosis: counseling issues generated during the NICHD clinical trial. Prenat Diagn. 2012;32(4):396-400.
The authors report no financial relationships relevant to this article.
If there have been overriding themes in obstetrics over the past year, they have been “more,” “sooner,” “faster,” “safer.” Advances in our field have thrilled our scientific curiosity and increased our ability to alleviate suffering—but at what cost? And who will pay that cost?
In this Update, we focus on recent advances in prenatal diagnosis and fetal therapy, as well as the ever-encroaching economic barriers that may limit our ability to get what we want. In particular, we will discuss:
- two technologies in prenatal genetics: noninvasive aneuploidy testing using cell-free DNA and prenatal microarray analysis
- open fetal surgery to reduce mortality and improve the function and quality of life for fetuses with open neural tube defects
- the value and probable impact of bundled payments—that is, one payment for multiple services grouped into one “episode.”
Two noninvasive approaches to prenatal diagnosis offer promise—but practicality and cost are uncertain
Ashoor G, Syngelaki RM, Wagner M, Birdir C, Nicolaides KH. Chromosome-selective sequencing of maternal plasma cell-free DNA for first-trimester detection of trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):322.e1–e5.
Reddy UM, Page GP, Saade GR, et al. Karyotype versus microarray testing for genetic abnormalities after stillbirth. N Engl J Med. 2012;367(23):2185–2193.
Talkowski ME, Ordulu Z, Pillalamarri V, et al. Clinical diagnosis by whole-genome sequencing of a prenatal sample. N Engl J Med. 2012;367(23):2226–2232.
Wapner RJ, Martin CL, Levy B, et al. Chromosomal microarray versus karyotyping for prenatal diagnosis. N Engl J Med. 2012;367(23):2175–2184.
Genetic screening and testing are a standard part of prenatal care in most developed countries. We have come a long way since a maternal age of 35 years was the only variable separating patients into low- and high-risk categories. This year, two technologies have emerged that may change forever the way we approach prenatal genetics:
One argument for using more accurate genetic screening methods: They limit the number of invasive tests that are needed. Chorionic villus sampling (CVS) and amniocentesis, even when performed by the most experienced of operators, pose a small but real risk of fetal injury and pregnancy loss.
Noninvasive aneuploidy diagnosis is now a reality in high-risk population screening
The holy grail of aneuploidy diagnosis would be a noninvasive way to sample fetal cells. Although we have known for decades that fetal cells enter the maternal circulation, it has been impractical to use them for aneuploidy testing because of their scarcity and longevity. In the 1990s, however, cell-free fetal DNA (cffDNA), a compound of DNA fragments of uncertain origin, was identified in maternal plasma. CffDNA is more plentiful than fetal cells. It also disappears within hours of delivery, demonstrating that it is specific to the current pregnancy.
CffDNA is already used in fetal Rh typing and gender determination in disorders such as congenital adrenal hyperplasia. Several studies in high-risk populations have demonstrated high sensitivity and specificity for the detection of Trisomies 21, 18, and 13. Several commercial tests are now available, although neither their accuracy nor their cost has been determined for use in low-risk population screening, compared with traditional testing.
Microarray analysis, paired with karyotyping, can elucidate ultrasound-identified fetal anomalies
Cytogenetic microarray analysis is also being explored in the prenatal period. Microarray analysis is currently used as a first-line test for infants and children who demonstrate developmental delay, autism spectrum disorders, dysmorphic features, and congenital anomalies. As many as 15% of patients with an otherwise normal karyotype will have a clinically significant copy number variant (CNV) on microarray. This finding has led to the use of microarray analysis in conjunction with karyotyping for fetuses with ultrasound-identified anomalies. Both targeted arrays (for syndromes associated with ultrasound anomalies) and whole-genome arrays are available.

Recent data from a study from the National Institute of Child Health and Human Development (NICHD) reveal that the prenatal detection rates for aneuploidy and unbalanced translocations are comparable between microarray analysis and karyotyping. Microarray analysis did not, however, detect triploidies or balanced translocations. As many as 6% of patients with a normal karyotype and structural anomalies and 1.7% of patients with advanced maternal age or positive screening tests had either a known or potentially clinically relevant CNV. This large study concluded that microarray analysis not only provides equal detection of aneuploidy but also more information in the form of CNVs, compared with karyotyping alone.
Microarray analysis also has been used in the study of pregnancy loss and stillbirth because it does not require viable or intact tissue as a source of DNA—an advantage, compared with traditional karyotyping. A recent study from the Stillbirth Collaborative Research Network demonstrated that genetic results in cases involving stillbirth were obtained more frequently via microarray analysis (87.4%) than by karyotype (70.5%). In addition, more genetic abnormalities (aneuploidy, pathogenic CNVs, and CNVs of unknown clinical significance) were detected by microarray analysis. Investigators concluded that microarray analysis may be especially useful in cases involving stillbirth (when a karyotype cannot be obtained) and structural abnormalities.
We want an accurate, completely risk-free genetic test that can be used for anyone. What we have so far is a technology that must be tested before it can be used in most of our patients—that is, the low-risk ones. We also have access to the fetus’ genetic code on a very specific level.
The total costs of such an approach—test, interpretation, counseling, and long-term follow-up of uncertain results—are unknown at this time and may prove to be unaffordable on a population-wide basis.
Should microarray analysis replace routine prenatal genetic testing?
A major dilemma associated with this technology is the significant amount of time that may be needed to counsel patients when the results are of unclear clinical significance.5 If the fetus has an anomaly, and a related CNV is identified, then counseling of the parents is fairly straightforward. However, if the fetus has an anomaly and a CNV that has not yet been defined, what should the parents be told? Some argue that this information should not be shared with the parents, whereas others recommend full disclosure of all results—even if we do not yet know what to make of them.
Another issue with microarray analysis is its inability to detect balanced translocations, triploidies, and low-level mosaicism, which require either a karyotype or whole-genome sequencing. Microarray analysis is also more expensive than karyotyping, although this may change in the future.
>Fetal therapy involves a complex equation of potential benefits and risks
Adzick NS, Thom EA, Spong CY, et al; MOMS Investigators. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011;364(11):993–1104.
Fetal therapy is broadly defined as any intervention administered to or via the mother with a primary indication to improve perinatal or long-term outcomes for the fetus or newborn. The concept of intervening to prevent the death of a fetus by correcting an anatomic anomaly or halting a disease process in utero is not new. Liley performed the first intrauterine fetal transfusion for Rh alloimmunization in the 1960s. Today, we perform fetal interventions routinely to reduce mortality by giving medical therapy to the mother, such as antenatal corticosteroids to enhance fetal lung maturity or anti-arrhythmics for supraventricular tachycardia. More invasive procedures have proved to be lifesaving (placental laser coagulation for twin-twin transfusion syndrome), ameliorating in the short term (shunting for lower urinary tract obstruction to relieve oligohydramnios), or ultimately not helpful (decompression of hydrocephalus).
Most recently, open fetal surgery has taken center stage as an intervention focused not only on reducing mortality but on improving function and quality of life for fetuses with open neural tube defects (ONTDs). This anomaly was targeted for fetal intervention because, although ONTDs are not generally considered lethal, a significant number of patients die before the age of 5, the majority of patients require shunts that leave them vulnerable to complications, and ONTDs generally impose lifelong intellectual and physical limitations. Repair during fetal life was proposed to prevent damage to the spinal cord and reverse hindbrain herniation, with the goal of improving long-term neurologic function.
The Management of Myelomeningocele Study (MOMS) is a prospective, multicenter trial that randomly assigned fetuses with isolated ONTDs to open fetal repair of myelomeningocele via hysterotomy or to postnatal repair of the defect. Forty percent of infants who underwent fetal repair required placement of a shunt, compared with 82% of those who had postnatal repair (relative risk, 0.48; 97.7% CI, 0.36 to 0.64; P<.001). Infants in the fetal-repair group also had significantly improved composite scores for mental development and motor function at 30 months (P = .007), as well as improvement in secondary outcomes such as hindbrain herniation and independent walking at 30 months.
As exciting as these results are, open fetal surgery still has significant limitations. The few centers that perform the most complex surgeries often have strict exclusion criteria, including maternal body mass index (BMI) greater than 35 kg/m2 and other medical comorbidities. The surgery also poses real risks for both mother and fetus. In the MOMS trial, the risk of preterm labor increased in the fetal-repair group, compared with postnatal repair (38% vs 14%), as did the risk of premature rupture of membranes (46% vs 8%). The fetal-repair group delivered more than 3 weeks earlier than the postnatal repair group (34 vs 37 weeks). Twenty-five percent of the fetal-repair group had thinning of the uterine scar, with uterine dehiscence seen in 10%. When myelomeningocele is repaired during fetal life, mothers require two hysterotomies during pregnancy and face an increased risk of uterine rupture and preterm delivery in subsequent pregnancies. The use of tocolytics exposes these mothers to an increased risk of pulmonary edema (6% in the fetal-repair group vs 0% for postnatal repair).
Other issues that should be addressed:
- the need for rigorous study of open fetal surgery for other fetal anomalies
- prognostic factors for success and for complications
- long-term outcomes in neurologic development of children and fertility of mothers
- a comparison of costs between fetal and postnatal treatment.
Although we may want to intervene as early in life as possible (that is, the fetal period) to achieve the best outcomes for the child, we need to weigh the short-term benefits of intervention against the known risks that intervention poses for the mother in the current pregnancy as well as the potential implications for future pregnancies (ie, the need for all future deliveries to be by cesarean section), not to mention the unknown long-term effects of intervention on both the child and society.
Bundled payments may help us deliver higher-quality, more efficient, and less costly care
Centers for Medicare and Medicaid Services, US Department of Health and Human Services. Fact Sheet: Bundled Payments for Care Improvement Initiative. Washington, DC: DHS; 2011. http://innovations.cms.gov/Files/fact-sheet/Bundled-Payment-Fact-Sheet.pdf. Accessed December 6, 2012.
There is little question that health care in the United States needs reform. The culture of “more is better” is not sustainable economically—nor does our health as a whole reflect the amount of money that we spend on health care, compared with other countries. Although the future is not yet clear, one proposed mechanism for reform is the institution of bundled payments—the grouping of multiple services into one “episode” for payment purposes. An episode might include inpatient hospitalization for pneumonia, for example, or the grouping of surgery with post-discharge care. In obstetrics, all pregnancy care could be grouped into one episode. The concept behind bundled payments is to provide incentives to institutions and providers to delivery higher-quality, more efficient, and less costly care.
If bundled payments become the reality for obstetric care in the future, how will that affect the way we care for our patients? Instead of blindly ordering all available tests, we need to consider thoroughly whether the patient truly needs a test to improve pregnancy outcomes. We also need to consider whether other measures might be avoided safely to keep costs within the bundle. A few examples:
- Is a screening fetal echocardiogram really necessary in a diabetic woman if the ultrasound anatomy scan is sufficient to rule out any cardiac anomaly that might require intervention in the delivery room?
- How will we integrate the expense of cell-free fetal DNA aneuploidy testing and microarray analysis, not to mention the extended counseling sessions that will be necessary to explain findings of uncertain clinical significance, into the bundle? Will “low-risk” patients need to pay out of pocket?
Few physicians entered medicine to worry about costs. Most of us want to worry about our patients. Yet, the reality is that scientific curiosity and a desire to do more—and to do it sooner, faster, and safer—are no longer sufficient justifications for many clinical decisions. We soon may need to figure out how to get what we need without spending as much in the process. In doing so, we may find ourselves moving away from the computer screen and back to the bedside—where we belong.
- Will a second ultrasound scan to visualize the fetal spine in a patient with a normal alpha-fetoprotein level be included in the bundle or paid for by the patient?
These issues may seem trivial, but we can no longer afford to order every test available. We will need to spend more time examining and counseling our patients so that they feel they are still getting the best care possible.
We want to hear from you! Tell us what you think.
The authors report no financial relationships relevant to this article.
If there have been overriding themes in obstetrics over the past year, they have been “more,” “sooner,” “faster,” “safer.” Advances in our field have thrilled our scientific curiosity and increased our ability to alleviate suffering—but at what cost? And who will pay that cost?
In this Update, we focus on recent advances in prenatal diagnosis and fetal therapy, as well as the ever-encroaching economic barriers that may limit our ability to get what we want. In particular, we will discuss:
- two technologies in prenatal genetics: noninvasive aneuploidy testing using cell-free DNA and prenatal microarray analysis
- open fetal surgery to reduce mortality and improve the function and quality of life for fetuses with open neural tube defects
- the value and probable impact of bundled payments—that is, one payment for multiple services grouped into one “episode.”
Two noninvasive approaches to prenatal diagnosis offer promise—but practicality and cost are uncertain
Ashoor G, Syngelaki RM, Wagner M, Birdir C, Nicolaides KH. Chromosome-selective sequencing of maternal plasma cell-free DNA for first-trimester detection of trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):322.e1–e5.
Reddy UM, Page GP, Saade GR, et al. Karyotype versus microarray testing for genetic abnormalities after stillbirth. N Engl J Med. 2012;367(23):2185–2193.
Talkowski ME, Ordulu Z, Pillalamarri V, et al. Clinical diagnosis by whole-genome sequencing of a prenatal sample. N Engl J Med. 2012;367(23):2226–2232.
Wapner RJ, Martin CL, Levy B, et al. Chromosomal microarray versus karyotyping for prenatal diagnosis. N Engl J Med. 2012;367(23):2175–2184.
Genetic screening and testing are a standard part of prenatal care in most developed countries. We have come a long way since a maternal age of 35 years was the only variable separating patients into low- and high-risk categories. This year, two technologies have emerged that may change forever the way we approach prenatal genetics:
One argument for using more accurate genetic screening methods: They limit the number of invasive tests that are needed. Chorionic villus sampling (CVS) and amniocentesis, even when performed by the most experienced of operators, pose a small but real risk of fetal injury and pregnancy loss.
Noninvasive aneuploidy diagnosis is now a reality in high-risk population screening
The holy grail of aneuploidy diagnosis would be a noninvasive way to sample fetal cells. Although we have known for decades that fetal cells enter the maternal circulation, it has been impractical to use them for aneuploidy testing because of their scarcity and longevity. In the 1990s, however, cell-free fetal DNA (cffDNA), a compound of DNA fragments of uncertain origin, was identified in maternal plasma. CffDNA is more plentiful than fetal cells. It also disappears within hours of delivery, demonstrating that it is specific to the current pregnancy.
CffDNA is already used in fetal Rh typing and gender determination in disorders such as congenital adrenal hyperplasia. Several studies in high-risk populations have demonstrated high sensitivity and specificity for the detection of Trisomies 21, 18, and 13. Several commercial tests are now available, although neither their accuracy nor their cost has been determined for use in low-risk population screening, compared with traditional testing.
Microarray analysis, paired with karyotyping, can elucidate ultrasound-identified fetal anomalies
Cytogenetic microarray analysis is also being explored in the prenatal period. Microarray analysis is currently used as a first-line test for infants and children who demonstrate developmental delay, autism spectrum disorders, dysmorphic features, and congenital anomalies. As many as 15% of patients with an otherwise normal karyotype will have a clinically significant copy number variant (CNV) on microarray. This finding has led to the use of microarray analysis in conjunction with karyotyping for fetuses with ultrasound-identified anomalies. Both targeted arrays (for syndromes associated with ultrasound anomalies) and whole-genome arrays are available.

Recent data from a study from the National Institute of Child Health and Human Development (NICHD) reveal that the prenatal detection rates for aneuploidy and unbalanced translocations are comparable between microarray analysis and karyotyping. Microarray analysis did not, however, detect triploidies or balanced translocations. As many as 6% of patients with a normal karyotype and structural anomalies and 1.7% of patients with advanced maternal age or positive screening tests had either a known or potentially clinically relevant CNV. This large study concluded that microarray analysis not only provides equal detection of aneuploidy but also more information in the form of CNVs, compared with karyotyping alone.
Microarray analysis also has been used in the study of pregnancy loss and stillbirth because it does not require viable or intact tissue as a source of DNA—an advantage, compared with traditional karyotyping. A recent study from the Stillbirth Collaborative Research Network demonstrated that genetic results in cases involving stillbirth were obtained more frequently via microarray analysis (87.4%) than by karyotype (70.5%). In addition, more genetic abnormalities (aneuploidy, pathogenic CNVs, and CNVs of unknown clinical significance) were detected by microarray analysis. Investigators concluded that microarray analysis may be especially useful in cases involving stillbirth (when a karyotype cannot be obtained) and structural abnormalities.
We want an accurate, completely risk-free genetic test that can be used for anyone. What we have so far is a technology that must be tested before it can be used in most of our patients—that is, the low-risk ones. We also have access to the fetus’ genetic code on a very specific level.
The total costs of such an approach—test, interpretation, counseling, and long-term follow-up of uncertain results—are unknown at this time and may prove to be unaffordable on a population-wide basis.
Should microarray analysis replace routine prenatal genetic testing?
A major dilemma associated with this technology is the significant amount of time that may be needed to counsel patients when the results are of unclear clinical significance.5 If the fetus has an anomaly, and a related CNV is identified, then counseling of the parents is fairly straightforward. However, if the fetus has an anomaly and a CNV that has not yet been defined, what should the parents be told? Some argue that this information should not be shared with the parents, whereas others recommend full disclosure of all results—even if we do not yet know what to make of them.
Another issue with microarray analysis is its inability to detect balanced translocations, triploidies, and low-level mosaicism, which require either a karyotype or whole-genome sequencing. Microarray analysis is also more expensive than karyotyping, although this may change in the future.
>Fetal therapy involves a complex equation of potential benefits and risks
Adzick NS, Thom EA, Spong CY, et al; MOMS Investigators. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011;364(11):993–1104.
Fetal therapy is broadly defined as any intervention administered to or via the mother with a primary indication to improve perinatal or long-term outcomes for the fetus or newborn. The concept of intervening to prevent the death of a fetus by correcting an anatomic anomaly or halting a disease process in utero is not new. Liley performed the first intrauterine fetal transfusion for Rh alloimmunization in the 1960s. Today, we perform fetal interventions routinely to reduce mortality by giving medical therapy to the mother, such as antenatal corticosteroids to enhance fetal lung maturity or anti-arrhythmics for supraventricular tachycardia. More invasive procedures have proved to be lifesaving (placental laser coagulation for twin-twin transfusion syndrome), ameliorating in the short term (shunting for lower urinary tract obstruction to relieve oligohydramnios), or ultimately not helpful (decompression of hydrocephalus).
Most recently, open fetal surgery has taken center stage as an intervention focused not only on reducing mortality but on improving function and quality of life for fetuses with open neural tube defects (ONTDs). This anomaly was targeted for fetal intervention because, although ONTDs are not generally considered lethal, a significant number of patients die before the age of 5, the majority of patients require shunts that leave them vulnerable to complications, and ONTDs generally impose lifelong intellectual and physical limitations. Repair during fetal life was proposed to prevent damage to the spinal cord and reverse hindbrain herniation, with the goal of improving long-term neurologic function.
The Management of Myelomeningocele Study (MOMS) is a prospective, multicenter trial that randomly assigned fetuses with isolated ONTDs to open fetal repair of myelomeningocele via hysterotomy or to postnatal repair of the defect. Forty percent of infants who underwent fetal repair required placement of a shunt, compared with 82% of those who had postnatal repair (relative risk, 0.48; 97.7% CI, 0.36 to 0.64; P<.001). Infants in the fetal-repair group also had significantly improved composite scores for mental development and motor function at 30 months (P = .007), as well as improvement in secondary outcomes such as hindbrain herniation and independent walking at 30 months.
As exciting as these results are, open fetal surgery still has significant limitations. The few centers that perform the most complex surgeries often have strict exclusion criteria, including maternal body mass index (BMI) greater than 35 kg/m2 and other medical comorbidities. The surgery also poses real risks for both mother and fetus. In the MOMS trial, the risk of preterm labor increased in the fetal-repair group, compared with postnatal repair (38% vs 14%), as did the risk of premature rupture of membranes (46% vs 8%). The fetal-repair group delivered more than 3 weeks earlier than the postnatal repair group (34 vs 37 weeks). Twenty-five percent of the fetal-repair group had thinning of the uterine scar, with uterine dehiscence seen in 10%. When myelomeningocele is repaired during fetal life, mothers require two hysterotomies during pregnancy and face an increased risk of uterine rupture and preterm delivery in subsequent pregnancies. The use of tocolytics exposes these mothers to an increased risk of pulmonary edema (6% in the fetal-repair group vs 0% for postnatal repair).
Other issues that should be addressed:
- the need for rigorous study of open fetal surgery for other fetal anomalies
- prognostic factors for success and for complications
- long-term outcomes in neurologic development of children and fertility of mothers
- a comparison of costs between fetal and postnatal treatment.
Although we may want to intervene as early in life as possible (that is, the fetal period) to achieve the best outcomes for the child, we need to weigh the short-term benefits of intervention against the known risks that intervention poses for the mother in the current pregnancy as well as the potential implications for future pregnancies (ie, the need for all future deliveries to be by cesarean section), not to mention the unknown long-term effects of intervention on both the child and society.
Bundled payments may help us deliver higher-quality, more efficient, and less costly care
Centers for Medicare and Medicaid Services, US Department of Health and Human Services. Fact Sheet: Bundled Payments for Care Improvement Initiative. Washington, DC: DHS; 2011. http://innovations.cms.gov/Files/fact-sheet/Bundled-Payment-Fact-Sheet.pdf. Accessed December 6, 2012.
There is little question that health care in the United States needs reform. The culture of “more is better” is not sustainable economically—nor does our health as a whole reflect the amount of money that we spend on health care, compared with other countries. Although the future is not yet clear, one proposed mechanism for reform is the institution of bundled payments—the grouping of multiple services into one “episode” for payment purposes. An episode might include inpatient hospitalization for pneumonia, for example, or the grouping of surgery with post-discharge care. In obstetrics, all pregnancy care could be grouped into one episode. The concept behind bundled payments is to provide incentives to institutions and providers to delivery higher-quality, more efficient, and less costly care.
If bundled payments become the reality for obstetric care in the future, how will that affect the way we care for our patients? Instead of blindly ordering all available tests, we need to consider thoroughly whether the patient truly needs a test to improve pregnancy outcomes. We also need to consider whether other measures might be avoided safely to keep costs within the bundle. A few examples:
- Is a screening fetal echocardiogram really necessary in a diabetic woman if the ultrasound anatomy scan is sufficient to rule out any cardiac anomaly that might require intervention in the delivery room?
- How will we integrate the expense of cell-free fetal DNA aneuploidy testing and microarray analysis, not to mention the extended counseling sessions that will be necessary to explain findings of uncertain clinical significance, into the bundle? Will “low-risk” patients need to pay out of pocket?
Few physicians entered medicine to worry about costs. Most of us want to worry about our patients. Yet, the reality is that scientific curiosity and a desire to do more—and to do it sooner, faster, and safer—are no longer sufficient justifications for many clinical decisions. We soon may need to figure out how to get what we need without spending as much in the process. In doing so, we may find ourselves moving away from the computer screen and back to the bedside—where we belong.
- Will a second ultrasound scan to visualize the fetal spine in a patient with a normal alpha-fetoprotein level be included in the bundle or paid for by the patient?
These issues may seem trivial, but we can no longer afford to order every test available. We will need to spend more time examining and counseling our patients so that they feel they are still getting the best care possible.
We want to hear from you! Tell us what you think.
1. Chiu RWK, Lo YMD. Noninvasive prenatal diagnosis by fetal nucleic acid analysis in maternal plasma: the coming of age. Semin Fetal Neonatal Med. 2011;16(2):88-93.
2. Chiu RWK, Lo YMD. Noninvasive prenatal diagnosis empowered by high-throughput sequencing. Prenat Diagn. 2012;32(4):401-406.
3. Savage MS, Mourad MJ, Wapner RJ. Evolving applications of microarray analysis in prenatal diagnosis. Curr Opin Obstet Gynecol. 2011;23(2):103-108.
4. Dugoff L. Application of genomic technology in prenatal diagnosis [editorial]. N Engl J Med. 2012;367(23):2249-2251.
5. Wapner RJ, Driscoll DA, Simpson JL. Integration of microarray technology into prenatal diagnosis: counseling issues generated during the NICHD clinical trial. Prenat Diagn. 2012;32(4):396-400.
1. Chiu RWK, Lo YMD. Noninvasive prenatal diagnosis by fetal nucleic acid analysis in maternal plasma: the coming of age. Semin Fetal Neonatal Med. 2011;16(2):88-93.
2. Chiu RWK, Lo YMD. Noninvasive prenatal diagnosis empowered by high-throughput sequencing. Prenat Diagn. 2012;32(4):401-406.
3. Savage MS, Mourad MJ, Wapner RJ. Evolving applications of microarray analysis in prenatal diagnosis. Curr Opin Obstet Gynecol. 2011;23(2):103-108.
4. Dugoff L. Application of genomic technology in prenatal diagnosis [editorial]. N Engl J Med. 2012;367(23):2249-2251.
5. Wapner RJ, Driscoll DA, Simpson JL. Integration of microarray technology into prenatal diagnosis: counseling issues generated during the NICHD clinical trial. Prenat Diagn. 2012;32(4):396-400.