User login
Interim PET provides limited prognostic value for diffuse large B-cell lymphoma
Results from positron emission tomography after 2 and 4 weeks of standardized, dose-dense chemotherapy in patients with diffuse large B-cell lymphoma (DLBCL) failed to provide sufficient prognostic accuracy to guide therapeutic decisions, according to a report published online in the Journal of Clinical Oncology.
“Our data demonstrate that interim PET-CT fails to deliver a PPV [positive predictive value] or NPV [negative predictive value] that reflects the clinical outcome for patients with DLBCL treated with R-CHOP-14 with sufficient accuracy to guide therapeutic decisions such as treatment intensification/deintensification at the present stage,” wrote Dr. Chrisoph Mamot of the division of haematology/oncology, Cantonal Hospital of Aarau, Switzerland, and colleagues (J. Clin. Onc. 2015 July 6 [doi:10.1200/JCO.2014.58.9846]).
Although the likelihood of 2-year event-free survival (EFS) was significantly lower among patients who had positive PET results after 2 weeks of therapy (PET-2-positive), compared with PET-2-negative patients (48% vs. 74%; P = .004), a large proportion of interim PET-positive patients had favorable outcomes. This may be due to the dose-dense regimen, Dr. Mamot and colleagues said.
Patients underwent six cycles of R-CHOP (rituximab 375 mg/m2, cyclophosphamide 750 mg/m2, doxorubicin 50 mg/m2, vincristine 1.4 mg/m2, and prednisone 100 mg/m2 for 5 days) every 14 days, followed by two cycles of rituximab.
Patients who had a positive PET-2 result received another PET scan after completion of four chemotherapy cycles. The 2-year EFS for PET-4-positive and PET-4-negative patients were not significantly different.
“Our original hypothesis that an interim PET/CT at a later time point might be able to better separate patients with good or poor prognosis was not confirmed,” the authors wrote. The end-of-treatment PET provided the best prediction of good vs. poor prognosis, but this time point is too late to adapt treatment. The authors concluded that interim PET/CT in patients with DLBCL presently is not accurate enough to guide treatment decisions in individual patients.
The multicenter, prospective study evaluated 138 patients, median age 58.5 years, who had untreated DLBCL, Ann Arbor stage I (12%), II (34%), III (23%), or IV (30%).
The study was supported by grants from Amgen (Switzerland) and OncoSuisse. Dr. Christoph Mamot reported consulting or advisory roles with Roche, Novartis, Amgen, and Boehringer-Ingelheim. Several of his coauthors reported ties to industry sources.
Results from positron emission tomography after 2 and 4 weeks of standardized, dose-dense chemotherapy in patients with diffuse large B-cell lymphoma (DLBCL) failed to provide sufficient prognostic accuracy to guide therapeutic decisions, according to a report published online in the Journal of Clinical Oncology.
“Our data demonstrate that interim PET-CT fails to deliver a PPV [positive predictive value] or NPV [negative predictive value] that reflects the clinical outcome for patients with DLBCL treated with R-CHOP-14 with sufficient accuracy to guide therapeutic decisions such as treatment intensification/deintensification at the present stage,” wrote Dr. Chrisoph Mamot of the division of haematology/oncology, Cantonal Hospital of Aarau, Switzerland, and colleagues (J. Clin. Onc. 2015 July 6 [doi:10.1200/JCO.2014.58.9846]).
Although the likelihood of 2-year event-free survival (EFS) was significantly lower among patients who had positive PET results after 2 weeks of therapy (PET-2-positive), compared with PET-2-negative patients (48% vs. 74%; P = .004), a large proportion of interim PET-positive patients had favorable outcomes. This may be due to the dose-dense regimen, Dr. Mamot and colleagues said.
Patients underwent six cycles of R-CHOP (rituximab 375 mg/m2, cyclophosphamide 750 mg/m2, doxorubicin 50 mg/m2, vincristine 1.4 mg/m2, and prednisone 100 mg/m2 for 5 days) every 14 days, followed by two cycles of rituximab.
Patients who had a positive PET-2 result received another PET scan after completion of four chemotherapy cycles. The 2-year EFS for PET-4-positive and PET-4-negative patients were not significantly different.
“Our original hypothesis that an interim PET/CT at a later time point might be able to better separate patients with good or poor prognosis was not confirmed,” the authors wrote. The end-of-treatment PET provided the best prediction of good vs. poor prognosis, but this time point is too late to adapt treatment. The authors concluded that interim PET/CT in patients with DLBCL presently is not accurate enough to guide treatment decisions in individual patients.
The multicenter, prospective study evaluated 138 patients, median age 58.5 years, who had untreated DLBCL, Ann Arbor stage I (12%), II (34%), III (23%), or IV (30%).
The study was supported by grants from Amgen (Switzerland) and OncoSuisse. Dr. Christoph Mamot reported consulting or advisory roles with Roche, Novartis, Amgen, and Boehringer-Ingelheim. Several of his coauthors reported ties to industry sources.
Results from positron emission tomography after 2 and 4 weeks of standardized, dose-dense chemotherapy in patients with diffuse large B-cell lymphoma (DLBCL) failed to provide sufficient prognostic accuracy to guide therapeutic decisions, according to a report published online in the Journal of Clinical Oncology.
“Our data demonstrate that interim PET-CT fails to deliver a PPV [positive predictive value] or NPV [negative predictive value] that reflects the clinical outcome for patients with DLBCL treated with R-CHOP-14 with sufficient accuracy to guide therapeutic decisions such as treatment intensification/deintensification at the present stage,” wrote Dr. Chrisoph Mamot of the division of haematology/oncology, Cantonal Hospital of Aarau, Switzerland, and colleagues (J. Clin. Onc. 2015 July 6 [doi:10.1200/JCO.2014.58.9846]).
Although the likelihood of 2-year event-free survival (EFS) was significantly lower among patients who had positive PET results after 2 weeks of therapy (PET-2-positive), compared with PET-2-negative patients (48% vs. 74%; P = .004), a large proportion of interim PET-positive patients had favorable outcomes. This may be due to the dose-dense regimen, Dr. Mamot and colleagues said.
Patients underwent six cycles of R-CHOP (rituximab 375 mg/m2, cyclophosphamide 750 mg/m2, doxorubicin 50 mg/m2, vincristine 1.4 mg/m2, and prednisone 100 mg/m2 for 5 days) every 14 days, followed by two cycles of rituximab.
Patients who had a positive PET-2 result received another PET scan after completion of four chemotherapy cycles. The 2-year EFS for PET-4-positive and PET-4-negative patients were not significantly different.
“Our original hypothesis that an interim PET/CT at a later time point might be able to better separate patients with good or poor prognosis was not confirmed,” the authors wrote. The end-of-treatment PET provided the best prediction of good vs. poor prognosis, but this time point is too late to adapt treatment. The authors concluded that interim PET/CT in patients with DLBCL presently is not accurate enough to guide treatment decisions in individual patients.
The multicenter, prospective study evaluated 138 patients, median age 58.5 years, who had untreated DLBCL, Ann Arbor stage I (12%), II (34%), III (23%), or IV (30%).
The study was supported by grants from Amgen (Switzerland) and OncoSuisse. Dr. Christoph Mamot reported consulting or advisory roles with Roche, Novartis, Amgen, and Boehringer-Ingelheim. Several of his coauthors reported ties to industry sources.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: After two cycles of standardized, dose-dense chemotherapy in patients with diffuse large B-cell lymphoma (DLBCL), positive results from PET signaled worse 2-year event-free survival (EFS) than negative interim PET results, but overall survival was not significantly different.
Major finding: After two cycles of chemotherapy, 2-year EFS for PET-positive, compared with PET-negative patients was 48.2% vs. 74.2% (P = .004). Overall survival was 87.7% vs. 90.6% (P = .6).
Data source: The multicenter, prospective study evaluated 138 patients, median age 58.5 years, who had untreated DLBCL, Ann Arbor stage I (12%), II (34%), III (23%), or IV (30%).
Disclosures: The study was supported by grants from Amgen (Switzerland) and OncoSuisse. Dr. Christoph Mamot reported consulting or advisory roles with Roche, Novartis, Amgen, and Boehringer-Ingelheim. Several of his coauthors reported ties to industry sources.
Consolidation chemotherapy after concurrent chemoradiation failed to improve outcomes in NSCLC
Results from a large, multinational phase III trial showed that consolidation chemotherapy with docetaxel and cisplatin after concurrent chemoradiation with the same agents failed to improve progression-free survival in patients with locally advanced non–small cell lung cancer (NSCLC), according to a report published online in the Journal of Clinical Oncology.
After a median follow up of 50.7 months, progression-free survival (PFS) for the arm that received consolidation chemotherapy (CC) was 8.1 months, compared with 9.1 months for the arm that did not receive CC (hazard ratio, 0.91; 95% confidence interval, 0.73-1.12; P = .36). Median overall survival (OS) was also similar between groups: 20.6 vs. 21.8 months, respectively (P = .44).
Among patients assigned to the CC arm, only 42.1% received all three planned cycles, 54.1% completed at least two cycles, and 31.6% did not receive any CC.
“The major obstacle in this trial was that many patients could not complete the three planned cycles of CC,” wrote Dr. Jin Seok Ahn of the Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea, and colleagues. A large proportion of patients failed to start CC because of disease progression or death, and many patients had incomplete recovery from the adverse effects of concurrent chemoradiation. “A full-dose doublet regimen of CC in our trial might have further reduced the rate of completing the three planned cycles of CC,” the investigators noted (J. Clin. Onc. 2015 July 6 [doi:10.1200/JCO.2014.60.0130]).
The randomized phase III trial included 420 patients with inoperable stage IIIA or IIIB non–small cell lung cancer, enrolled from 31 centers in Korea, China, and Taiwan from 2005 to 2011.
Patients older than 60 years, who had similar baseline characteristics to younger patients, experienced significant benefit from CC (HR 0.72), for reasons that remain unexplained.
An exploratory biomarker study indicated the expression of ERCC1 and class III beta-tubulin was not correlated with PFS or OS.
The study was supported in part by Sanofi-Aventis Korea. Dr. Jin Seok Ahn reported financial ties to Eli Lilly, Pfizer, and Roche. Several of his coauthors reported ties to industry sources.
Results from a large, multinational phase III trial showed that consolidation chemotherapy with docetaxel and cisplatin after concurrent chemoradiation with the same agents failed to improve progression-free survival in patients with locally advanced non–small cell lung cancer (NSCLC), according to a report published online in the Journal of Clinical Oncology.
After a median follow up of 50.7 months, progression-free survival (PFS) for the arm that received consolidation chemotherapy (CC) was 8.1 months, compared with 9.1 months for the arm that did not receive CC (hazard ratio, 0.91; 95% confidence interval, 0.73-1.12; P = .36). Median overall survival (OS) was also similar between groups: 20.6 vs. 21.8 months, respectively (P = .44).
Among patients assigned to the CC arm, only 42.1% received all three planned cycles, 54.1% completed at least two cycles, and 31.6% did not receive any CC.
“The major obstacle in this trial was that many patients could not complete the three planned cycles of CC,” wrote Dr. Jin Seok Ahn of the Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea, and colleagues. A large proportion of patients failed to start CC because of disease progression or death, and many patients had incomplete recovery from the adverse effects of concurrent chemoradiation. “A full-dose doublet regimen of CC in our trial might have further reduced the rate of completing the three planned cycles of CC,” the investigators noted (J. Clin. Onc. 2015 July 6 [doi:10.1200/JCO.2014.60.0130]).
The randomized phase III trial included 420 patients with inoperable stage IIIA or IIIB non–small cell lung cancer, enrolled from 31 centers in Korea, China, and Taiwan from 2005 to 2011.
Patients older than 60 years, who had similar baseline characteristics to younger patients, experienced significant benefit from CC (HR 0.72), for reasons that remain unexplained.
An exploratory biomarker study indicated the expression of ERCC1 and class III beta-tubulin was not correlated with PFS or OS.
The study was supported in part by Sanofi-Aventis Korea. Dr. Jin Seok Ahn reported financial ties to Eli Lilly, Pfizer, and Roche. Several of his coauthors reported ties to industry sources.
Results from a large, multinational phase III trial showed that consolidation chemotherapy with docetaxel and cisplatin after concurrent chemoradiation with the same agents failed to improve progression-free survival in patients with locally advanced non–small cell lung cancer (NSCLC), according to a report published online in the Journal of Clinical Oncology.
After a median follow up of 50.7 months, progression-free survival (PFS) for the arm that received consolidation chemotherapy (CC) was 8.1 months, compared with 9.1 months for the arm that did not receive CC (hazard ratio, 0.91; 95% confidence interval, 0.73-1.12; P = .36). Median overall survival (OS) was also similar between groups: 20.6 vs. 21.8 months, respectively (P = .44).
Among patients assigned to the CC arm, only 42.1% received all three planned cycles, 54.1% completed at least two cycles, and 31.6% did not receive any CC.
“The major obstacle in this trial was that many patients could not complete the three planned cycles of CC,” wrote Dr. Jin Seok Ahn of the Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea, and colleagues. A large proportion of patients failed to start CC because of disease progression or death, and many patients had incomplete recovery from the adverse effects of concurrent chemoradiation. “A full-dose doublet regimen of CC in our trial might have further reduced the rate of completing the three planned cycles of CC,” the investigators noted (J. Clin. Onc. 2015 July 6 [doi:10.1200/JCO.2014.60.0130]).
The randomized phase III trial included 420 patients with inoperable stage IIIA or IIIB non–small cell lung cancer, enrolled from 31 centers in Korea, China, and Taiwan from 2005 to 2011.
Patients older than 60 years, who had similar baseline characteristics to younger patients, experienced significant benefit from CC (HR 0.72), for reasons that remain unexplained.
An exploratory biomarker study indicated the expression of ERCC1 and class III beta-tubulin was not correlated with PFS or OS.
The study was supported in part by Sanofi-Aventis Korea. Dr. Jin Seok Ahn reported financial ties to Eli Lilly, Pfizer, and Roche. Several of his coauthors reported ties to industry sources.
Key clinical point: Docetaxel and cisplatin consolidation chemotherapy (CC) after concurrent chemoradiation failed to prolong progression-free survival in patients with locally advanced non–small cell lung cancer.
Major finding: PFS was similar for patients who received CC and those who did not, 8.1 vs. 9.1 months, respectively (P = .36).
Data source: The randomized phase III trial included 420 patients with inoperable stage IIIA or IIIB NSCLC, enrolled from 31 centers in Korea, China, and Taiwan.
Disclosures: The study was supported in part by Sanofi-Aventis Korea. Dr. Jin Seok Ahn reported financial ties to Eli Lilly, Pfizer, and Roche. Several of his coauthors reported ties to industry sources.
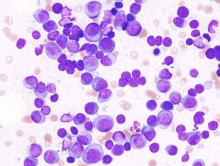
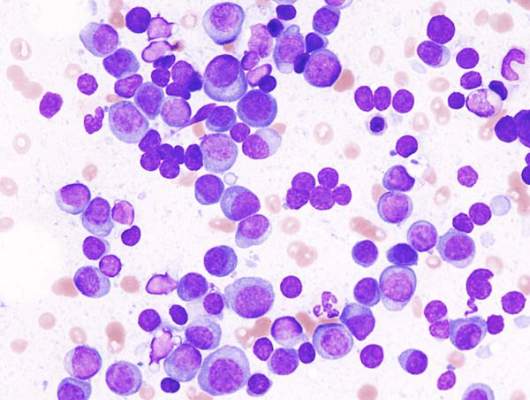
CRd is well tolerated and effective in newly diagnosed and smoldering multiple myeloma
Patients with newly diagnosed multiple myeloma or smoldering multiple myeloma experienced good responses and few severe adverse events from carfilzomib-lenalidomide-dexamethasone with lenalidomide extension (CRd-R), according to a report published online in JAMA Oncology.
The regimen was not associated with peripheral neuropathy of grade 3 or above, and both groups had high rates of minimal residual disease negativity, which has been shown to be associated with improved progression-free survival and overall survival in newly diagnosed patients treated with CRd.
However, the three tools used for measuring patient response differed in their abilities to detect minimal residual disease, the researchers reported.
“Given the high degree of CR [complete response] rates achievable by three-drug combination regimens, there is an increased need for clinical trials to detect MRD [minimal residual disease] beyond traditional methods and characterize optimal MRD technique,” wrote Dr. Neha Korde of the myeloma service at Memorial Sloan Kettering Cancer Center, New York, and colleagues.
The researchers used three measures to assess minimal residual disease: multiparametric flow cytometry, next-generation sequencing, and fluorodeoxyglucose positron-emission tomography/computed tomography.
Based on multiparametric flow cytometry, minimal residual disease was not detected in 62% (28/45) of the patients with newly diagnosed disease and in 92% (11/12) of those with smoldering multiple myeloma, (JAMA Oncol. 2015 July 2 [doi:10.1001/jamaoncol.2015.2010]). Based on flow cytometry, 98% negativity for minimal residual disease was seen in patients with at least nCR. Based on next-generation sequencing, an additional 30% of patients were positive for minimal residual disease, highlighting the potential increased sensitivity of that assay, the researcher said.
In patients with newly diagnosed disease, 98% achieved at least a partial response, 89% had at least a very good partial response, 62% had at least a near complete response, and 56% had at least a complete response or a stringent complete response. Responses improved with more therapy; the median time to CR was 5 (2-17) cycles, and six patients reached CR during the lenalidomide extension. The median duration of response was not reached.
All of the patients with high-risk smoldering multiple myeloma achieved at least a complete response, with median time of 6 (2-20) cycles to CR.
In a 2-year study, 45 patients with newly diagnosed multiple myeloma received a treatment regimen that included eight 28-day cycles of CRd, followed by 24 cycles of lenalidomide extended dosing for those with stable disease. Promising early results led to a pilot study with the same regimen in 12 patients with high-risk SMM, a condition that leads to symptomatic disease within a median of 2 years.
None of the patients with newly diagnosed multiple myeloma had peripheral neuropathy of grade 3 or above, the primary endpoint. Grade 1 peripheral neuropathy affected 33% of patients, and grade 2 was experienced by 9%. Lymphopenia and electrolyte or metabolism abnormalities were the most common adverse events. Grade 3 or 4 cardiac events included two patients with congestive heart failure and three patients with hypertension.
Patients with smoldering multiple myeloma had similar rates of adverse events.
In this pilot study, the CRd combination was well tolerated and yielded deep responses across prognostic groups. However, morphological complete response, in this scenario, was insufficient to characterize tumor reduction.
“With the introduction of highly effective drug combinations, traditional response criteria become less valid because these do not sufficiently assess the deepness of response.” New approaches such as MRD and PET/CT negativity should be introduced to evaluate response in clinical trials and, ultimately, in clinical practice.
Patients with smoldering multiple myeloma, who have more than a 90% probability of disease progression within 2 years, may benefit from early treatment that is effective and does not expose them to an excessive risk of toxicity.
Dr. Pieter Sonneveld is head of the department of hematology at the Erasmus MC Cancer Institute, Rotterdam, the Netherlands. Dr. Sonneveld reported receiving research funding from Celgene, Onyx/Amgen, Janssen, and Karyopharm.
In this pilot study, the CRd combination was well tolerated and yielded deep responses across prognostic groups. However, morphological complete response, in this scenario, was insufficient to characterize tumor reduction.
“With the introduction of highly effective drug combinations, traditional response criteria become less valid because these do not sufficiently assess the deepness of response.” New approaches such as MRD and PET/CT negativity should be introduced to evaluate response in clinical trials and, ultimately, in clinical practice.
Patients with smoldering multiple myeloma, who have more than a 90% probability of disease progression within 2 years, may benefit from early treatment that is effective and does not expose them to an excessive risk of toxicity.
Dr. Pieter Sonneveld is head of the department of hematology at the Erasmus MC Cancer Institute, Rotterdam, the Netherlands. Dr. Sonneveld reported receiving research funding from Celgene, Onyx/Amgen, Janssen, and Karyopharm.
In this pilot study, the CRd combination was well tolerated and yielded deep responses across prognostic groups. However, morphological complete response, in this scenario, was insufficient to characterize tumor reduction.
“With the introduction of highly effective drug combinations, traditional response criteria become less valid because these do not sufficiently assess the deepness of response.” New approaches such as MRD and PET/CT negativity should be introduced to evaluate response in clinical trials and, ultimately, in clinical practice.
Patients with smoldering multiple myeloma, who have more than a 90% probability of disease progression within 2 years, may benefit from early treatment that is effective and does not expose them to an excessive risk of toxicity.
Dr. Pieter Sonneveld is head of the department of hematology at the Erasmus MC Cancer Institute, Rotterdam, the Netherlands. Dr. Sonneveld reported receiving research funding from Celgene, Onyx/Amgen, Janssen, and Karyopharm.
Patients with newly diagnosed multiple myeloma or smoldering multiple myeloma experienced good responses and few severe adverse events from carfilzomib-lenalidomide-dexamethasone with lenalidomide extension (CRd-R), according to a report published online in JAMA Oncology.
The regimen was not associated with peripheral neuropathy of grade 3 or above, and both groups had high rates of minimal residual disease negativity, which has been shown to be associated with improved progression-free survival and overall survival in newly diagnosed patients treated with CRd.
However, the three tools used for measuring patient response differed in their abilities to detect minimal residual disease, the researchers reported.
“Given the high degree of CR [complete response] rates achievable by three-drug combination regimens, there is an increased need for clinical trials to detect MRD [minimal residual disease] beyond traditional methods and characterize optimal MRD technique,” wrote Dr. Neha Korde of the myeloma service at Memorial Sloan Kettering Cancer Center, New York, and colleagues.
The researchers used three measures to assess minimal residual disease: multiparametric flow cytometry, next-generation sequencing, and fluorodeoxyglucose positron-emission tomography/computed tomography.
Based on multiparametric flow cytometry, minimal residual disease was not detected in 62% (28/45) of the patients with newly diagnosed disease and in 92% (11/12) of those with smoldering multiple myeloma, (JAMA Oncol. 2015 July 2 [doi:10.1001/jamaoncol.2015.2010]). Based on flow cytometry, 98% negativity for minimal residual disease was seen in patients with at least nCR. Based on next-generation sequencing, an additional 30% of patients were positive for minimal residual disease, highlighting the potential increased sensitivity of that assay, the researcher said.
In patients with newly diagnosed disease, 98% achieved at least a partial response, 89% had at least a very good partial response, 62% had at least a near complete response, and 56% had at least a complete response or a stringent complete response. Responses improved with more therapy; the median time to CR was 5 (2-17) cycles, and six patients reached CR during the lenalidomide extension. The median duration of response was not reached.
All of the patients with high-risk smoldering multiple myeloma achieved at least a complete response, with median time of 6 (2-20) cycles to CR.
In a 2-year study, 45 patients with newly diagnosed multiple myeloma received a treatment regimen that included eight 28-day cycles of CRd, followed by 24 cycles of lenalidomide extended dosing for those with stable disease. Promising early results led to a pilot study with the same regimen in 12 patients with high-risk SMM, a condition that leads to symptomatic disease within a median of 2 years.
None of the patients with newly diagnosed multiple myeloma had peripheral neuropathy of grade 3 or above, the primary endpoint. Grade 1 peripheral neuropathy affected 33% of patients, and grade 2 was experienced by 9%. Lymphopenia and electrolyte or metabolism abnormalities were the most common adverse events. Grade 3 or 4 cardiac events included two patients with congestive heart failure and three patients with hypertension.
Patients with smoldering multiple myeloma had similar rates of adverse events.
Patients with newly diagnosed multiple myeloma or smoldering multiple myeloma experienced good responses and few severe adverse events from carfilzomib-lenalidomide-dexamethasone with lenalidomide extension (CRd-R), according to a report published online in JAMA Oncology.
The regimen was not associated with peripheral neuropathy of grade 3 or above, and both groups had high rates of minimal residual disease negativity, which has been shown to be associated with improved progression-free survival and overall survival in newly diagnosed patients treated with CRd.
However, the three tools used for measuring patient response differed in their abilities to detect minimal residual disease, the researchers reported.
“Given the high degree of CR [complete response] rates achievable by three-drug combination regimens, there is an increased need for clinical trials to detect MRD [minimal residual disease] beyond traditional methods and characterize optimal MRD technique,” wrote Dr. Neha Korde of the myeloma service at Memorial Sloan Kettering Cancer Center, New York, and colleagues.
The researchers used three measures to assess minimal residual disease: multiparametric flow cytometry, next-generation sequencing, and fluorodeoxyglucose positron-emission tomography/computed tomography.
Based on multiparametric flow cytometry, minimal residual disease was not detected in 62% (28/45) of the patients with newly diagnosed disease and in 92% (11/12) of those with smoldering multiple myeloma, (JAMA Oncol. 2015 July 2 [doi:10.1001/jamaoncol.2015.2010]). Based on flow cytometry, 98% negativity for minimal residual disease was seen in patients with at least nCR. Based on next-generation sequencing, an additional 30% of patients were positive for minimal residual disease, highlighting the potential increased sensitivity of that assay, the researcher said.
In patients with newly diagnosed disease, 98% achieved at least a partial response, 89% had at least a very good partial response, 62% had at least a near complete response, and 56% had at least a complete response or a stringent complete response. Responses improved with more therapy; the median time to CR was 5 (2-17) cycles, and six patients reached CR during the lenalidomide extension. The median duration of response was not reached.
All of the patients with high-risk smoldering multiple myeloma achieved at least a complete response, with median time of 6 (2-20) cycles to CR.
In a 2-year study, 45 patients with newly diagnosed multiple myeloma received a treatment regimen that included eight 28-day cycles of CRd, followed by 24 cycles of lenalidomide extended dosing for those with stable disease. Promising early results led to a pilot study with the same regimen in 12 patients with high-risk SMM, a condition that leads to symptomatic disease within a median of 2 years.
None of the patients with newly diagnosed multiple myeloma had peripheral neuropathy of grade 3 or above, the primary endpoint. Grade 1 peripheral neuropathy affected 33% of patients, and grade 2 was experienced by 9%. Lymphopenia and electrolyte or metabolism abnormalities were the most common adverse events. Grade 3 or 4 cardiac events included two patients with congestive heart failure and three patients with hypertension.
Patients with smoldering multiple myeloma had similar rates of adverse events.
FROM JAMA ONCOLOGY
Key clinical point: Patients with newly diagnosed multiple myeloma or smoldering multiple myeloma had high rates of minimal residual disease negativity and none experienced grade 3 or 4 peripheral neuropathy from carfilzomib-lenalidomide-dexamethasone with lenalidomide extension (CRd-R).
Major finding: Based on multiparametric flow cytometry, minimal residual disease was not detected in 62% (28/45) of the patients with newly diagnosed disease and in 92% (11/12) of those with smoldering multiple myeloma.
Data source: A 2-year pilot study of 45 patients with newly diagnosed multiple myeloma and 12 patients with smoldering multiple myeloma.
Disclosures: The study was partially supported by Onyx and Celgene. Dr. Korde reported consulting for MedScape. Her coauthors reported ties to several industry sources.
Urea cream bests antioxidant ointment to prevent chemo-induced hand-foot syndrome
Urea cream is more effective at preventing hand-foot syndrome (HFS) than is a medical ointment high in antioxidants for patients receiving capecitabine, according to a randomized phase III study published online in the Journal of Clinical Oncology.
During a 6-week treatment period, 17 of 76 patients (22.4%) who used 10% urea cream experienced HFS, compared with 30 of 76 patients (39.5%) who used the new ointment Mapisal, which has been available on the German market since 2011 (odds ratio 2.37; 95% CI 1.14 to 4.84; P = .02). The distribution of HFS grades within the groups was similar, with the majority having grade 1 and about 6% experiencing grade 3 HFS. A secondary endpoint, time to develop HFS, was significantly longer in the urea cream group (J. Clin. Oncol. 2015 June 29 [doi:10.1200/JCO.2014.60.4587]).
The result was unexpected. Mapisal contains several antioxidants and oil extracts and exhibits a high radical protection factor, which was hypothesized to be of benefit due to a decline in antioxidative capacity of the skin in patients using capecitabine. “The most striking explanation for the observed ineffectiveness of Mapisal is that either the hypothesis – that is, that Mapisal’s crucial mode of action against HFS is to act as an antioxidant against free radicals – is incorrect, or that this is not the main mechanism of HFS development, at least in the case of capecitabine,” wrote Dr. Ralf-Dieter Hofheinz of University Hospital Mannheim, Germany, and colleagues.
Between 2012 and 2013, the study enrolled 160 patients with GI tumors or breast cancer who were being treated with capecitabine, and 152 were randomly assigned to receive prophylactic treatment with either Mapisal or 10% urea cream for a 6-week period. Aside from HFS, adverse events were similar between the groups. After the treatment period, skin-related quality of life was significantly lower in the Mapisal vs. urea group.
The results of this study, along with findings from a previous phase II study demonstrating activity of urea cream in patients treated with sorafenib, supports the idea that urea cream is an appropriate prophylaxis for HFS and a reasonable standard for future investigations, the researchers noted.
Urea cream is more effective at preventing hand-foot syndrome (HFS) than is a medical ointment high in antioxidants for patients receiving capecitabine, according to a randomized phase III study published online in the Journal of Clinical Oncology.
During a 6-week treatment period, 17 of 76 patients (22.4%) who used 10% urea cream experienced HFS, compared with 30 of 76 patients (39.5%) who used the new ointment Mapisal, which has been available on the German market since 2011 (odds ratio 2.37; 95% CI 1.14 to 4.84; P = .02). The distribution of HFS grades within the groups was similar, with the majority having grade 1 and about 6% experiencing grade 3 HFS. A secondary endpoint, time to develop HFS, was significantly longer in the urea cream group (J. Clin. Oncol. 2015 June 29 [doi:10.1200/JCO.2014.60.4587]).
The result was unexpected. Mapisal contains several antioxidants and oil extracts and exhibits a high radical protection factor, which was hypothesized to be of benefit due to a decline in antioxidative capacity of the skin in patients using capecitabine. “The most striking explanation for the observed ineffectiveness of Mapisal is that either the hypothesis – that is, that Mapisal’s crucial mode of action against HFS is to act as an antioxidant against free radicals – is incorrect, or that this is not the main mechanism of HFS development, at least in the case of capecitabine,” wrote Dr. Ralf-Dieter Hofheinz of University Hospital Mannheim, Germany, and colleagues.
Between 2012 and 2013, the study enrolled 160 patients with GI tumors or breast cancer who were being treated with capecitabine, and 152 were randomly assigned to receive prophylactic treatment with either Mapisal or 10% urea cream for a 6-week period. Aside from HFS, adverse events were similar between the groups. After the treatment period, skin-related quality of life was significantly lower in the Mapisal vs. urea group.
The results of this study, along with findings from a previous phase II study demonstrating activity of urea cream in patients treated with sorafenib, supports the idea that urea cream is an appropriate prophylaxis for HFS and a reasonable standard for future investigations, the researchers noted.
Urea cream is more effective at preventing hand-foot syndrome (HFS) than is a medical ointment high in antioxidants for patients receiving capecitabine, according to a randomized phase III study published online in the Journal of Clinical Oncology.
During a 6-week treatment period, 17 of 76 patients (22.4%) who used 10% urea cream experienced HFS, compared with 30 of 76 patients (39.5%) who used the new ointment Mapisal, which has been available on the German market since 2011 (odds ratio 2.37; 95% CI 1.14 to 4.84; P = .02). The distribution of HFS grades within the groups was similar, with the majority having grade 1 and about 6% experiencing grade 3 HFS. A secondary endpoint, time to develop HFS, was significantly longer in the urea cream group (J. Clin. Oncol. 2015 June 29 [doi:10.1200/JCO.2014.60.4587]).
The result was unexpected. Mapisal contains several antioxidants and oil extracts and exhibits a high radical protection factor, which was hypothesized to be of benefit due to a decline in antioxidative capacity of the skin in patients using capecitabine. “The most striking explanation for the observed ineffectiveness of Mapisal is that either the hypothesis – that is, that Mapisal’s crucial mode of action against HFS is to act as an antioxidant against free radicals – is incorrect, or that this is not the main mechanism of HFS development, at least in the case of capecitabine,” wrote Dr. Ralf-Dieter Hofheinz of University Hospital Mannheim, Germany, and colleagues.
Between 2012 and 2013, the study enrolled 160 patients with GI tumors or breast cancer who were being treated with capecitabine, and 152 were randomly assigned to receive prophylactic treatment with either Mapisal or 10% urea cream for a 6-week period. Aside from HFS, adverse events were similar between the groups. After the treatment period, skin-related quality of life was significantly lower in the Mapisal vs. urea group.
The results of this study, along with findings from a previous phase II study demonstrating activity of urea cream in patients treated with sorafenib, supports the idea that urea cream is an appropriate prophylaxis for HFS and a reasonable standard for future investigations, the researchers noted.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Urea cream was superior to Mapisal, an antioxidant-containing ointment, in preventing hand-foot syndrome (HFS) among patients receiving capecitabine.
Major finding: A significantly higher proportion of patients using Mapisal experienced HFS compared with urea cream: 39.5% vs. 22.4% (P = .02).
Data source: Between 2012 and 2013, the randomized phase III trial included 152 patients with GI tumors or breast cancer who received HFS prophylactic treatment for 6 weeks.
Disclosures: Medac supported the study. Dr. Hofheinz disclosed ties with Medac, Roche, Amgen, Merck, Eli Lilly, Sanofi, and Bayer AG.
Serial CA-125 measurements better for ovarian cancer screening
A cancer risk algorithm using serial measurements of serum cancer antigen 125 (CA-125) detected more cases of ovarian cancer than did a single-threshold rule, according to a large, prospective screening study published in the Journal of Clinical Oncology.
The findings “highlight the need to examine serial change in biomarker levels in the context of screening and early detection of cancer. Reliance on predefined single-threshold rules may result in biomarkers of value being discarded,” wrote Dr. Usha Menon, professor of gynecological cancer at University College London (J. Clin. Oncol. 2015 June 20 [doi:10.1200/JCO.2014.59.4945]).
The risk of ovarian cancer algorithm (ROCA) compares an individual’s CA-125 serial profile with that of cancer cases and healthy controls to estimate a risk for ovarian cancer. The United Kingdom Collaborative Trial of Ovarian Cancer Screening enrolled 202,638 women and randomly allocated about 50,000 to multimodal screening using CA-125 velocity measurements and ROCA. From 2002 to 2011, 296,911 incident screens were performed, which was a median 7 screens per participant.
Out of 155 women with invasive epithelial ovarian or tubal cancers (iEOC), ROCA detected 85.8%, whereas single measurements of CA-125 as thresholds 35, 30, and 22 U/mL would have identified 41.3%, 48.4%, and 66.5%, respectively. The ROCA had significantly larger area under the receiver operating curve (ROC) 0.915) than did single CA-125 measurements (0.915 vs. 0.869; P = .0027). Most of the screen-detected iEOCs (82.0%) were aggressive type II, contrary to concerns that screening identifies more indolent cancers.
Surgery as a result of positive screen results occurred in 640 women (0.2% of all screens) and of these, 154 (24.1%) had primary ovarian and/or tubal malignancies detected, representing a lower false-positive rate than other screening strategies.
The median time from annual screen to surgery was 20 weeks, but for women who had CA-125 in the normal range (and intermediate ROCA), the median time to surgery was 30 weeks, because of a requirement for repeat tests. Modifications to the screening strategy to decrease this time may be warranted given that this group had a higher proportion of stage I and II iEOCs compared with those who had intermediate ROCA coupled with above-normal CA-125, did not require more testing, and had a median time to surgery of 12 weeks.
Key clinical point: A velocity-based algorithm using serial measures of serum cancer antigen 125 (CA-125) detected more ovarian cancer cases compared with CA-125 single-threshold rules.
Major finding: An algorithm that estimates risk of ovarian cancer based on CA-125 velocity detected 85.8% of 155 women with invasive epithelial ovarian or tubal cancers, while the CA-125 single thresholds of 35, 30, and 22 U/mL would have identified 41.3%, 48.4%, and 66.5%, respectively.
Data source: From 2002 to 2011, participants in the United Kingdom Collaborative Trial of Ovarian Cancer Screening (n = 46,237) underwent 296,911 incident screens (median 7 per person) in a prospective study comparing CA-125 velocity with single-threshold rule for detection of ovarian cancer.
Disclosures: Dr. Menon reported having stock or other ownership in Abcodia. Several of her coauthors reported financial relationships with various industry sources.
Key clinical point: A velocity-based algorithm using serial measures of serum cancer antigen 125 (CA-125) detected more ovarian cancer cases compared with CA-125 single-threshold rules.
Major finding: An algorithm that estimates risk of ovarian cancer based on CA-125 velocity detected 85.8% of 155 women with invasive epithelial ovarian or tubal cancers, while the CA-125 single thresholds of 35, 30, and 22 U/mL would have identified 41.3%, 48.4%, and 66.5%, respectively.
Data source: From 2002 to 2011, participants in the United Kingdom Collaborative Trial of Ovarian Cancer Screening (n = 46,237) underwent 296,911 incident screens (median 7 per person) in a prospective study comparing CA-125 velocity with single-threshold rule for detection of ovarian cancer.
Disclosures: Dr. Menon reported having stock or other ownership in Abcodia. Several of her coauthors reported financial relationships with various industry sources.
Key clinical point: A velocity-based algorithm using serial measures of serum cancer antigen 125 (CA-125) detected more ovarian cancer cases compared with CA-125 single-threshold rules.
Major finding: An algorithm that estimates risk of ovarian cancer based on CA-125 velocity detected 85.8% of 155 women with invasive epithelial ovarian or tubal cancers, while the CA-125 single thresholds of 35, 30, and 22 U/mL would have identified 41.3%, 48.4%, and 66.5%, respectively.
Data source: From 2002 to 2011, participants in the United Kingdom Collaborative Trial of Ovarian Cancer Screening (n = 46,237) underwent 296,911 incident screens (median 7 per person) in a prospective study comparing CA-125 velocity with single-threshold rule for detection of ovarian cancer.
Disclosures: Dr. Menon reported having stock or other ownership in Abcodia. Several of her coauthors reported financial relationships with various industry sources.
A cancer risk algorithm using serial measurements of serum cancer antigen 125 (CA-125) detected more cases of ovarian cancer than did a single-threshold rule, according to a large, prospective screening study published in the Journal of Clinical Oncology.
The findings “highlight the need to examine serial change in biomarker levels in the context of screening and early detection of cancer. Reliance on predefined single-threshold rules may result in biomarkers of value being discarded,” wrote Dr. Usha Menon, professor of gynecological cancer at University College London (J. Clin. Oncol. 2015 June 20 [doi:10.1200/JCO.2014.59.4945]).
The risk of ovarian cancer algorithm (ROCA) compares an individual’s CA-125 serial profile with that of cancer cases and healthy controls to estimate a risk for ovarian cancer. The United Kingdom Collaborative Trial of Ovarian Cancer Screening enrolled 202,638 women and randomly allocated about 50,000 to multimodal screening using CA-125 velocity measurements and ROCA. From 2002 to 2011, 296,911 incident screens were performed, which was a median 7 screens per participant.
Out of 155 women with invasive epithelial ovarian or tubal cancers (iEOC), ROCA detected 85.8%, whereas single measurements of CA-125 as thresholds 35, 30, and 22 U/mL would have identified 41.3%, 48.4%, and 66.5%, respectively. The ROCA had significantly larger area under the receiver operating curve (ROC) 0.915) than did single CA-125 measurements (0.915 vs. 0.869; P = .0027). Most of the screen-detected iEOCs (82.0%) were aggressive type II, contrary to concerns that screening identifies more indolent cancers.
Surgery as a result of positive screen results occurred in 640 women (0.2% of all screens) and of these, 154 (24.1%) had primary ovarian and/or tubal malignancies detected, representing a lower false-positive rate than other screening strategies.
The median time from annual screen to surgery was 20 weeks, but for women who had CA-125 in the normal range (and intermediate ROCA), the median time to surgery was 30 weeks, because of a requirement for repeat tests. Modifications to the screening strategy to decrease this time may be warranted given that this group had a higher proportion of stage I and II iEOCs compared with those who had intermediate ROCA coupled with above-normal CA-125, did not require more testing, and had a median time to surgery of 12 weeks.
A cancer risk algorithm using serial measurements of serum cancer antigen 125 (CA-125) detected more cases of ovarian cancer than did a single-threshold rule, according to a large, prospective screening study published in the Journal of Clinical Oncology.
The findings “highlight the need to examine serial change in biomarker levels in the context of screening and early detection of cancer. Reliance on predefined single-threshold rules may result in biomarkers of value being discarded,” wrote Dr. Usha Menon, professor of gynecological cancer at University College London (J. Clin. Oncol. 2015 June 20 [doi:10.1200/JCO.2014.59.4945]).
The risk of ovarian cancer algorithm (ROCA) compares an individual’s CA-125 serial profile with that of cancer cases and healthy controls to estimate a risk for ovarian cancer. The United Kingdom Collaborative Trial of Ovarian Cancer Screening enrolled 202,638 women and randomly allocated about 50,000 to multimodal screening using CA-125 velocity measurements and ROCA. From 2002 to 2011, 296,911 incident screens were performed, which was a median 7 screens per participant.
Out of 155 women with invasive epithelial ovarian or tubal cancers (iEOC), ROCA detected 85.8%, whereas single measurements of CA-125 as thresholds 35, 30, and 22 U/mL would have identified 41.3%, 48.4%, and 66.5%, respectively. The ROCA had significantly larger area under the receiver operating curve (ROC) 0.915) than did single CA-125 measurements (0.915 vs. 0.869; P = .0027). Most of the screen-detected iEOCs (82.0%) were aggressive type II, contrary to concerns that screening identifies more indolent cancers.
Surgery as a result of positive screen results occurred in 640 women (0.2% of all screens) and of these, 154 (24.1%) had primary ovarian and/or tubal malignancies detected, representing a lower false-positive rate than other screening strategies.
The median time from annual screen to surgery was 20 weeks, but for women who had CA-125 in the normal range (and intermediate ROCA), the median time to surgery was 30 weeks, because of a requirement for repeat tests. Modifications to the screening strategy to decrease this time may be warranted given that this group had a higher proportion of stage I and II iEOCs compared with those who had intermediate ROCA coupled with above-normal CA-125, did not require more testing, and had a median time to surgery of 12 weeks.
FROM JOURNAL OF CLINICAL ONCOLOGY
CD8 cell dose predicts outcomes in allogeneic stem cell transplantation with reduced-intensity conditioning
Peripheral blood stem cell (PBSC) grafts with high doses of CD8 cells were associated with significantly lower relapse risk and improved survival in patients who were treated for hematologic malignancies with reduced-intensity conditioning (RIC) hematopoietic allogeneic stem cell transplantation (allo-HSCT), according to a report online in the Journal of Clinical Oncology.
A multivariate analysis showed that CD8 cell dose was an independent predictor of relapse (adjusted hazard ratio [aHR], 0.43; P = .009), relapse-free survival (aHR, 0.50; P = .006), and overall survival (aHR, 0.57; P = .04). The data showed a linear association between CD8 cell dose and outcomes, and further analysis identified an optimum cutoff of CD8 cell dose (0.72 x 108 CD8 cells per kg) to segregate survival outcomes. Patients who received grafts with CD8 cell doses above the cutoff had significantly improved regression-free and overall survival (P = .005 and P = .007, respectively).
“These findings indicate that improved survival after RIC transplantations could be achieved by optimizing donor selection and PBSC collection to increase the likelihood of mobilizing grafts containing high CD8 cell doses,” wrote Dr. Ran Reshef of the department of medicine at the Hospital of the University of Pennsylvania, Philadelphia, and colleagues (Journ. Clin. Onc. 2015 June 8 [doi:10.1200/JCO.2014.60.1203]).
Younger donors were more likely to have CD8 cell doses above the cutoff (CD8hi), however, only 53% of donors younger than 30 years had CD8hi grafts. To find methods to predict graft composition during donor screening, the investigators studied 21 randomly selected allo-HSCT donors. They found no correlations between CD8 graft content and clinical variables such as weight, sex, viral serologies, or apheresis parameters. Donors with a higher proportion of CD8 cells donated grafts with higher CD8 cell dose, but the presence of higher CD4 counts negated this. Screening for the relative proportions of CD8 and CD4 cells identifies donors most likely to mobilize CD8hi grafts.
“This is also a practical consideration because the assay is rapid, is routinely performed in clinical laboratories, and can easily be done at the time of confirmatory HLA [human leukocyte antigen] typing,” the authors noted. Since the relationship between CD8 dose and survival is linear, the higher the dose the better, even if it is below the cutoff.
Previous studies showed conflicting results regarding the outcome of RIC transplantation with younger unrelated donors versus older sibling donors. Donor age inversely correlates with CD8 cell dose, and the results of this study showed that overall survival was significantly better with younger unrelated donors with a CD8hi graft, compared with older sibling donors (P = .03). No such benefit was observed with younger unrelated donors with CD8lo grafts (P = .28), indicating the benefit may rely on CD8 cell dose.
The study evaluated 200 patients with hematologic malignancy who underwent allo-HSCT with fludarabine plus busulfan conditioning from 2007 to 2014 at the Abramson Cancer Center, University of Pennsylvania in Philadelphia. The cumulative relapse incidence was 42% at 1 year and 47% at 5 years. The most common diseases in the cohort were acute myeloid leukemia, myelodysplastic syndrome, and non-Hodgkin lymphoma.
High CD8 dose was associated with an increased, but nonsignificant risk of chronic graft-versus-host disease (GVHD); the risk for nonrelapse mortality was not associated with cell doses.
Peripheral blood stem cell (PBSC) grafts with high doses of CD8 cells were associated with significantly lower relapse risk and improved survival in patients who were treated for hematologic malignancies with reduced-intensity conditioning (RIC) hematopoietic allogeneic stem cell transplantation (allo-HSCT), according to a report online in the Journal of Clinical Oncology.
A multivariate analysis showed that CD8 cell dose was an independent predictor of relapse (adjusted hazard ratio [aHR], 0.43; P = .009), relapse-free survival (aHR, 0.50; P = .006), and overall survival (aHR, 0.57; P = .04). The data showed a linear association between CD8 cell dose and outcomes, and further analysis identified an optimum cutoff of CD8 cell dose (0.72 x 108 CD8 cells per kg) to segregate survival outcomes. Patients who received grafts with CD8 cell doses above the cutoff had significantly improved regression-free and overall survival (P = .005 and P = .007, respectively).
“These findings indicate that improved survival after RIC transplantations could be achieved by optimizing donor selection and PBSC collection to increase the likelihood of mobilizing grafts containing high CD8 cell doses,” wrote Dr. Ran Reshef of the department of medicine at the Hospital of the University of Pennsylvania, Philadelphia, and colleagues (Journ. Clin. Onc. 2015 June 8 [doi:10.1200/JCO.2014.60.1203]).
Younger donors were more likely to have CD8 cell doses above the cutoff (CD8hi), however, only 53% of donors younger than 30 years had CD8hi grafts. To find methods to predict graft composition during donor screening, the investigators studied 21 randomly selected allo-HSCT donors. They found no correlations between CD8 graft content and clinical variables such as weight, sex, viral serologies, or apheresis parameters. Donors with a higher proportion of CD8 cells donated grafts with higher CD8 cell dose, but the presence of higher CD4 counts negated this. Screening for the relative proportions of CD8 and CD4 cells identifies donors most likely to mobilize CD8hi grafts.
“This is also a practical consideration because the assay is rapid, is routinely performed in clinical laboratories, and can easily be done at the time of confirmatory HLA [human leukocyte antigen] typing,” the authors noted. Since the relationship between CD8 dose and survival is linear, the higher the dose the better, even if it is below the cutoff.
Previous studies showed conflicting results regarding the outcome of RIC transplantation with younger unrelated donors versus older sibling donors. Donor age inversely correlates with CD8 cell dose, and the results of this study showed that overall survival was significantly better with younger unrelated donors with a CD8hi graft, compared with older sibling donors (P = .03). No such benefit was observed with younger unrelated donors with CD8lo grafts (P = .28), indicating the benefit may rely on CD8 cell dose.
The study evaluated 200 patients with hematologic malignancy who underwent allo-HSCT with fludarabine plus busulfan conditioning from 2007 to 2014 at the Abramson Cancer Center, University of Pennsylvania in Philadelphia. The cumulative relapse incidence was 42% at 1 year and 47% at 5 years. The most common diseases in the cohort were acute myeloid leukemia, myelodysplastic syndrome, and non-Hodgkin lymphoma.
High CD8 dose was associated with an increased, but nonsignificant risk of chronic graft-versus-host disease (GVHD); the risk for nonrelapse mortality was not associated with cell doses.
Peripheral blood stem cell (PBSC) grafts with high doses of CD8 cells were associated with significantly lower relapse risk and improved survival in patients who were treated for hematologic malignancies with reduced-intensity conditioning (RIC) hematopoietic allogeneic stem cell transplantation (allo-HSCT), according to a report online in the Journal of Clinical Oncology.
A multivariate analysis showed that CD8 cell dose was an independent predictor of relapse (adjusted hazard ratio [aHR], 0.43; P = .009), relapse-free survival (aHR, 0.50; P = .006), and overall survival (aHR, 0.57; P = .04). The data showed a linear association between CD8 cell dose and outcomes, and further analysis identified an optimum cutoff of CD8 cell dose (0.72 x 108 CD8 cells per kg) to segregate survival outcomes. Patients who received grafts with CD8 cell doses above the cutoff had significantly improved regression-free and overall survival (P = .005 and P = .007, respectively).
“These findings indicate that improved survival after RIC transplantations could be achieved by optimizing donor selection and PBSC collection to increase the likelihood of mobilizing grafts containing high CD8 cell doses,” wrote Dr. Ran Reshef of the department of medicine at the Hospital of the University of Pennsylvania, Philadelphia, and colleagues (Journ. Clin. Onc. 2015 June 8 [doi:10.1200/JCO.2014.60.1203]).
Younger donors were more likely to have CD8 cell doses above the cutoff (CD8hi), however, only 53% of donors younger than 30 years had CD8hi grafts. To find methods to predict graft composition during donor screening, the investigators studied 21 randomly selected allo-HSCT donors. They found no correlations between CD8 graft content and clinical variables such as weight, sex, viral serologies, or apheresis parameters. Donors with a higher proportion of CD8 cells donated grafts with higher CD8 cell dose, but the presence of higher CD4 counts negated this. Screening for the relative proportions of CD8 and CD4 cells identifies donors most likely to mobilize CD8hi grafts.
“This is also a practical consideration because the assay is rapid, is routinely performed in clinical laboratories, and can easily be done at the time of confirmatory HLA [human leukocyte antigen] typing,” the authors noted. Since the relationship between CD8 dose and survival is linear, the higher the dose the better, even if it is below the cutoff.
Previous studies showed conflicting results regarding the outcome of RIC transplantation with younger unrelated donors versus older sibling donors. Donor age inversely correlates with CD8 cell dose, and the results of this study showed that overall survival was significantly better with younger unrelated donors with a CD8hi graft, compared with older sibling donors (P = .03). No such benefit was observed with younger unrelated donors with CD8lo grafts (P = .28), indicating the benefit may rely on CD8 cell dose.
The study evaluated 200 patients with hematologic malignancy who underwent allo-HSCT with fludarabine plus busulfan conditioning from 2007 to 2014 at the Abramson Cancer Center, University of Pennsylvania in Philadelphia. The cumulative relapse incidence was 42% at 1 year and 47% at 5 years. The most common diseases in the cohort were acute myeloid leukemia, myelodysplastic syndrome, and non-Hodgkin lymphoma.
High CD8 dose was associated with an increased, but nonsignificant risk of chronic graft-versus-host disease (GVHD); the risk for nonrelapse mortality was not associated with cell doses.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: High CD8 cell dose in peripheral blood stem cell grafts was associated with reduced risk of relapse and increased survival in allogeneic stem cell transplantation with reduced-intensity conditioning.
Major finding: With a cumulative relapse incidence of 42% at 1 year, CD8 cell dose was an independent predictor of relapse (aHR, 0.43; P = .009), relapse-free survival (0.50; P = .006), and overall survival (0.57; P = .04).
Data source: The retrospective, single-institution study evaluated 200 patients who underwent peripheral blood alloHSCT with fludarabine plus busulfan conditioning from 2007 to 2014. Analysis of graft T-cell content used 21 randomly selected donors.
Disclosures: Dr. Reshef reported having consulting or advisory roles with Celgene, Spectrum Pharmaceuticals, Tobira Therapeutics, and Teva Pharmaceutical Industries. Many of his coauthors reported having financial relationships with industry.
Prostate cancer screening for men over 50 has declined
Subsequent to the 2012 U.S. Preventative Services Task Force recommendation discouraging prostate-specific antigen (PSA)-based screening, prostate cancer screening significantly declined among men age 50 years and older in the United States, according to a study published online in the Journal of Clinical Oncology.
Based on National Health Interview Surveys in 2005, 2010, and 2013, self-reported PSA-testing levels decreased most among men aged 50-59 years, from 33.2% in 2010 to 24.8% in 2013 (odds ratio, 0.66; P < .01). Declines from 2010 to 2013 were also observed among men aged 60-74 years (51.2%-43.6%; OR, 0.74; P < .01); and aged 75 and older (43.9%-37.1%, OR, 0.75; P = .03). Among men aged 40-49 years, the decline from 12.5% to 11.2% was not significant (Journ. Clin. Onc. 2015 June 8 [doi:10.1200/JCO.2015.61.6532]).
The declines may reflect increased adherence by physicians to USPSTF guidelines; nevertheless, in 2013 approximately one-third of men aged 65 or older who had high risk for 9-year mortality (about 1.4 million individuals) were screened.
“Persistently elevated screening rates among men with limited remaining life expectancies are troubling and merit further interventions,” wrote Dr. Michael Drazer of the University of Chicago Medical Center and colleagues. “These may include increasing awareness of initiatives such as Choosing Wisely recommendations from the American Society of Clinical Oncology and recommendations from the American Geriatrics Society,” they wrote.
If these efforts prove unsuccessful, reducing or eliminating reimbursements for screening and interventions may be considered, the authors suggest.
A multivariate model identified factors that predict which men over age 65 are likely to be screened, and these are men who went to college, were married, consumed alcohol, and received a colonoscopy in the last 10 years. They found no significant predictors in the patient population for declines in screening from 2010 to 2013.
Several studies support the use of extended screening intervals (every 2-3 years) for patients at low risk for prostate cancer. Annual screening of men aged 55-67 years has been estimated to result in a 50% overdiagnosis rate.
Drs. Drazer and Huo reported having no financial disclosures. Dr. Eggener reported having consulting or advisory roles with Myriad Genetics, Medivation, Janssen Pharmaceuticals, Genomic Health, OPKO Diagnostics, and MDxHealth.
Subsequent to the 2012 U.S. Preventative Services Task Force recommendation discouraging prostate-specific antigen (PSA)-based screening, prostate cancer screening significantly declined among men age 50 years and older in the United States, according to a study published online in the Journal of Clinical Oncology.
Based on National Health Interview Surveys in 2005, 2010, and 2013, self-reported PSA-testing levels decreased most among men aged 50-59 years, from 33.2% in 2010 to 24.8% in 2013 (odds ratio, 0.66; P < .01). Declines from 2010 to 2013 were also observed among men aged 60-74 years (51.2%-43.6%; OR, 0.74; P < .01); and aged 75 and older (43.9%-37.1%, OR, 0.75; P = .03). Among men aged 40-49 years, the decline from 12.5% to 11.2% was not significant (Journ. Clin. Onc. 2015 June 8 [doi:10.1200/JCO.2015.61.6532]).
The declines may reflect increased adherence by physicians to USPSTF guidelines; nevertheless, in 2013 approximately one-third of men aged 65 or older who had high risk for 9-year mortality (about 1.4 million individuals) were screened.
“Persistently elevated screening rates among men with limited remaining life expectancies are troubling and merit further interventions,” wrote Dr. Michael Drazer of the University of Chicago Medical Center and colleagues. “These may include increasing awareness of initiatives such as Choosing Wisely recommendations from the American Society of Clinical Oncology and recommendations from the American Geriatrics Society,” they wrote.
If these efforts prove unsuccessful, reducing or eliminating reimbursements for screening and interventions may be considered, the authors suggest.
A multivariate model identified factors that predict which men over age 65 are likely to be screened, and these are men who went to college, were married, consumed alcohol, and received a colonoscopy in the last 10 years. They found no significant predictors in the patient population for declines in screening from 2010 to 2013.
Several studies support the use of extended screening intervals (every 2-3 years) for patients at low risk for prostate cancer. Annual screening of men aged 55-67 years has been estimated to result in a 50% overdiagnosis rate.
Drs. Drazer and Huo reported having no financial disclosures. Dr. Eggener reported having consulting or advisory roles with Myriad Genetics, Medivation, Janssen Pharmaceuticals, Genomic Health, OPKO Diagnostics, and MDxHealth.
Subsequent to the 2012 U.S. Preventative Services Task Force recommendation discouraging prostate-specific antigen (PSA)-based screening, prostate cancer screening significantly declined among men age 50 years and older in the United States, according to a study published online in the Journal of Clinical Oncology.
Based on National Health Interview Surveys in 2005, 2010, and 2013, self-reported PSA-testing levels decreased most among men aged 50-59 years, from 33.2% in 2010 to 24.8% in 2013 (odds ratio, 0.66; P < .01). Declines from 2010 to 2013 were also observed among men aged 60-74 years (51.2%-43.6%; OR, 0.74; P < .01); and aged 75 and older (43.9%-37.1%, OR, 0.75; P = .03). Among men aged 40-49 years, the decline from 12.5% to 11.2% was not significant (Journ. Clin. Onc. 2015 June 8 [doi:10.1200/JCO.2015.61.6532]).
The declines may reflect increased adherence by physicians to USPSTF guidelines; nevertheless, in 2013 approximately one-third of men aged 65 or older who had high risk for 9-year mortality (about 1.4 million individuals) were screened.
“Persistently elevated screening rates among men with limited remaining life expectancies are troubling and merit further interventions,” wrote Dr. Michael Drazer of the University of Chicago Medical Center and colleagues. “These may include increasing awareness of initiatives such as Choosing Wisely recommendations from the American Society of Clinical Oncology and recommendations from the American Geriatrics Society,” they wrote.
If these efforts prove unsuccessful, reducing or eliminating reimbursements for screening and interventions may be considered, the authors suggest.
A multivariate model identified factors that predict which men over age 65 are likely to be screened, and these are men who went to college, were married, consumed alcohol, and received a colonoscopy in the last 10 years. They found no significant predictors in the patient population for declines in screening from 2010 to 2013.
Several studies support the use of extended screening intervals (every 2-3 years) for patients at low risk for prostate cancer. Annual screening of men aged 55-67 years has been estimated to result in a 50% overdiagnosis rate.
Drs. Drazer and Huo reported having no financial disclosures. Dr. Eggener reported having consulting or advisory roles with Myriad Genetics, Medivation, Janssen Pharmaceuticals, Genomic Health, OPKO Diagnostics, and MDxHealth.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Prostate cancer screening rates among men aged 50 years and older declined nationwide from 2010 to 2013.
Major finding: From 2010 to 2013 screening rates significantly declined among men aged 50-59 (33.2%-24.8%, P < .01); aged 60-74 (51.2%-43.6%, P < .01); and aged 75 and older (43.9%-37.1%, P = .03).
Data source: The National Health Interview Survey is a face-to-face, cross-sectional survey that included men ≥ 40 years who had seen a physician in the previous year, representing over 60,000,000 men.
Disclosures: Drs. Drazer and Huo reported having no financial disclosures. Dr. Eggener reported having consulting or advisory roles with Myriad Genetics, Medivation, Janssen Pharmaceuticals, Genomic Health, OPKO Diagnostics, and MDxHealth.
Dexrazoxane Tx did not affect overall survival in pediatric leukemia and lymphoma
Exposure to dexrazoxane among pediatric patients with leukemia or lymphoma did not affect overall mortality during a median follow-up period of 12.6 years, according to a report published online in the Journal of Clinical Oncology.
Aggregated data from three Children’s Oncology Group trials showed that among 1,008 pediatric patients who received treatment with doxorubicin with or without dexrazoxane (DRZ) from 1996 to 2001, exposure to DRZ was not associated with an increased risk of relapse (HR, 0.81; 95% CI, 0.60-1.08) or death (HR, 1.03; 0.73-1.45). Comparing DRZ with non-DRZ treatment groups at 10 years, the cumulative incidence of relapse was 16.1% vs. 19.1% (difference, – 3.0%; 95% CI, – 7.9% to 0.2%) and overall mortality was 12.8% vs. 12.2% (difference, – 0.6%; 95% CI, – 3.5% to 4.7%). The three trials (P9404, P9425, and P9426) evaluated individually likewise did not show significant differences in relapse or mortality rates.
Although studies in adults show a positive effect of DRZ on heart failure rates after anthracycline therapy, concern over DRZ interference with cancer therapies and a possible link to second cancers have limited its use in children and prompted Dr. Eric Chow of the Fred Hutchinson Cancer Research Center, Seattle, and his colleagues to assess the effect of DRZ on mortality.
The investigators wrote that DRZ “does not appear to interfere with cancer treatment efficacy, in terms of original cancer mortality or overall risk of relapse. Although the risk for secondary cancer mortality (mainly as a result of AML/MDS [acute myeloid leukemia/myelodysplastic syndrome]) was greater among those exposed to DRZ, the overall number of events was small, and the differences were not statistically significant,” the investigators said. (J. Clin. Oncol. 2015 May 26 [doi:10.1200/JCO.2014.59.4473])
Aggregated data from the three trials shows that the 10-year mortality rate of AML/MDS was 1.4% for those treated with DRZ (seven patients), compared with 0.8% for those treated without DRZ (five patients).
The beneficial effects of DRZ in decreasing the risk of heart failure have been observed in trials of adult patients, but the results for survivors of childhood cancers have been inconclusive because heart failure may develop over a longer time period in children. With the median age of survivors in this study of 24 years, significant differences in cardiac mortality due to DRZ use are not detectable. To evaluate DRZ as a cardioprotectant, a new Children’s Oncology Group study (Effects of Dexrazoxane Hydrochloride on Biomarkers Associated With Cardiomyopathy and Heart Failure After Cancer Treatment [HEART]) will determine the cardiovascular health of individuals in the three trials P9404, P9425, and P9426.
“Given that second cancers and symptomatic cardiac disease appear to be by far the two most common categories of serious late effects (in terms of both absolute and relative risks) among long-term childhood cancer survivors as a group … with cumulative incidences of each approaching 20% by age 50 years, any strategy that offers the promise of reduced cardiotoxicity without being offset by second cancers is highly attractive,” Dr. Chow and his associates wrote.
The study was supported by the National Institutes of Health, St. Baldrick’s Foundation, and the Leukemia and Lymphoma Society. Dr. Chow reported having no relevant financial conflicts. Three of his coauthors reported having financial relationships with industry.
Exposure to dexrazoxane among pediatric patients with leukemia or lymphoma did not affect overall mortality during a median follow-up period of 12.6 years, according to a report published online in the Journal of Clinical Oncology.
Aggregated data from three Children’s Oncology Group trials showed that among 1,008 pediatric patients who received treatment with doxorubicin with or without dexrazoxane (DRZ) from 1996 to 2001, exposure to DRZ was not associated with an increased risk of relapse (HR, 0.81; 95% CI, 0.60-1.08) or death (HR, 1.03; 0.73-1.45). Comparing DRZ with non-DRZ treatment groups at 10 years, the cumulative incidence of relapse was 16.1% vs. 19.1% (difference, – 3.0%; 95% CI, – 7.9% to 0.2%) and overall mortality was 12.8% vs. 12.2% (difference, – 0.6%; 95% CI, – 3.5% to 4.7%). The three trials (P9404, P9425, and P9426) evaluated individually likewise did not show significant differences in relapse or mortality rates.
Although studies in adults show a positive effect of DRZ on heart failure rates after anthracycline therapy, concern over DRZ interference with cancer therapies and a possible link to second cancers have limited its use in children and prompted Dr. Eric Chow of the Fred Hutchinson Cancer Research Center, Seattle, and his colleagues to assess the effect of DRZ on mortality.
The investigators wrote that DRZ “does not appear to interfere with cancer treatment efficacy, in terms of original cancer mortality or overall risk of relapse. Although the risk for secondary cancer mortality (mainly as a result of AML/MDS [acute myeloid leukemia/myelodysplastic syndrome]) was greater among those exposed to DRZ, the overall number of events was small, and the differences were not statistically significant,” the investigators said. (J. Clin. Oncol. 2015 May 26 [doi:10.1200/JCO.2014.59.4473])
Aggregated data from the three trials shows that the 10-year mortality rate of AML/MDS was 1.4% for those treated with DRZ (seven patients), compared with 0.8% for those treated without DRZ (five patients).
The beneficial effects of DRZ in decreasing the risk of heart failure have been observed in trials of adult patients, but the results for survivors of childhood cancers have been inconclusive because heart failure may develop over a longer time period in children. With the median age of survivors in this study of 24 years, significant differences in cardiac mortality due to DRZ use are not detectable. To evaluate DRZ as a cardioprotectant, a new Children’s Oncology Group study (Effects of Dexrazoxane Hydrochloride on Biomarkers Associated With Cardiomyopathy and Heart Failure After Cancer Treatment [HEART]) will determine the cardiovascular health of individuals in the three trials P9404, P9425, and P9426.
“Given that second cancers and symptomatic cardiac disease appear to be by far the two most common categories of serious late effects (in terms of both absolute and relative risks) among long-term childhood cancer survivors as a group … with cumulative incidences of each approaching 20% by age 50 years, any strategy that offers the promise of reduced cardiotoxicity without being offset by second cancers is highly attractive,” Dr. Chow and his associates wrote.
The study was supported by the National Institutes of Health, St. Baldrick’s Foundation, and the Leukemia and Lymphoma Society. Dr. Chow reported having no relevant financial conflicts. Three of his coauthors reported having financial relationships with industry.
Exposure to dexrazoxane among pediatric patients with leukemia or lymphoma did not affect overall mortality during a median follow-up period of 12.6 years, according to a report published online in the Journal of Clinical Oncology.
Aggregated data from three Children’s Oncology Group trials showed that among 1,008 pediatric patients who received treatment with doxorubicin with or without dexrazoxane (DRZ) from 1996 to 2001, exposure to DRZ was not associated with an increased risk of relapse (HR, 0.81; 95% CI, 0.60-1.08) or death (HR, 1.03; 0.73-1.45). Comparing DRZ with non-DRZ treatment groups at 10 years, the cumulative incidence of relapse was 16.1% vs. 19.1% (difference, – 3.0%; 95% CI, – 7.9% to 0.2%) and overall mortality was 12.8% vs. 12.2% (difference, – 0.6%; 95% CI, – 3.5% to 4.7%). The three trials (P9404, P9425, and P9426) evaluated individually likewise did not show significant differences in relapse or mortality rates.
Although studies in adults show a positive effect of DRZ on heart failure rates after anthracycline therapy, concern over DRZ interference with cancer therapies and a possible link to second cancers have limited its use in children and prompted Dr. Eric Chow of the Fred Hutchinson Cancer Research Center, Seattle, and his colleagues to assess the effect of DRZ on mortality.
The investigators wrote that DRZ “does not appear to interfere with cancer treatment efficacy, in terms of original cancer mortality or overall risk of relapse. Although the risk for secondary cancer mortality (mainly as a result of AML/MDS [acute myeloid leukemia/myelodysplastic syndrome]) was greater among those exposed to DRZ, the overall number of events was small, and the differences were not statistically significant,” the investigators said. (J. Clin. Oncol. 2015 May 26 [doi:10.1200/JCO.2014.59.4473])
Aggregated data from the three trials shows that the 10-year mortality rate of AML/MDS was 1.4% for those treated with DRZ (seven patients), compared with 0.8% for those treated without DRZ (five patients).
The beneficial effects of DRZ in decreasing the risk of heart failure have been observed in trials of adult patients, but the results for survivors of childhood cancers have been inconclusive because heart failure may develop over a longer time period in children. With the median age of survivors in this study of 24 years, significant differences in cardiac mortality due to DRZ use are not detectable. To evaluate DRZ as a cardioprotectant, a new Children’s Oncology Group study (Effects of Dexrazoxane Hydrochloride on Biomarkers Associated With Cardiomyopathy and Heart Failure After Cancer Treatment [HEART]) will determine the cardiovascular health of individuals in the three trials P9404, P9425, and P9426.
“Given that second cancers and symptomatic cardiac disease appear to be by far the two most common categories of serious late effects (in terms of both absolute and relative risks) among long-term childhood cancer survivors as a group … with cumulative incidences of each approaching 20% by age 50 years, any strategy that offers the promise of reduced cardiotoxicity without being offset by second cancers is highly attractive,” Dr. Chow and his associates wrote.
The study was supported by the National Institutes of Health, St. Baldrick’s Foundation, and the Leukemia and Lymphoma Society. Dr. Chow reported having no relevant financial conflicts. Three of his coauthors reported having financial relationships with industry.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Treatment with dexrazoxane was not associated with an increased risk for cancer relapse or death.
Major finding: For pediatric patients with leukemia and lymphoma, the cumulative incidence of relapse at 10 years was 16.1% with DRZ, compared with 19.1% without DRZ (difference, – 3.0%; 95% CI, – 7.9% to 0.2%); overall mortality was 12.8% with DRZ vs. 12.2% without DRZ (difference, – 0.6%; 95% CI, – 3.5% to 4.7%).
Data source: Aggregated Children’s Oncology Group trials enrolling 1,008 pediatric patients with leukemia or lymphoma who were randomized to receive doxorubicin with or without DRZ from 1996 to 2001.
Disclosures: The study was supported by the National Institutes of Health, St. Baldrick’s Foundation, and the Leukemia and Lymphoma Society. Dr. Chow reported having no relevant financial conflicts. Three of his coauthors reported having financial relationships with industry.
T-VEC improved durable response rate in advanced melanoma
Treatment with the oncolytic immunotherapy talimogene laherparepvec (T-VEC) resulted in significantly longer rates of durable response and overall response, compared with subcutaneous granulocyte-macrophage colony-stimulating factor (GM-CSF), according to results from the phase III OPTiM trial reported in the Journal of Clinical Oncology.
“To our knowledge, OPTiM is the first randomized, controlled, phase III study evaluating an oncolytic immunotherapy to demonstrate a therapeutic benefit in melanoma,” wrote Dr. Robert Andtbacka, of the Huntsman Cancer Institute, University of Utah, Salt Lake City, and colleagues (J. Clin. Onc. 2015 May 26 [doi:10.1200/JCO.2014.58.3377]).
Patients who received T-VEC vs. subcutaneous GM-CSF had significantly improved rates of durable response, defined as responses lasting 6 months or more, (16.3% vs. 2.1%; P < .001), as well as improved overall response rates (26.4% vs. 5.7% ; P < .001). Complete responses were achieved in 10.8% of the T-VEC arm (32 patients) and < 1% (1 patient) in the GM-CSF arm. Median overall survival was 23.3 months for T-VEC and 18.9 months for GM-CSF (P = .051).
Differences in durable response rates and overall response rates between the T-VEC and GM-CSF arms were greater among patients with stage IIIb or IIIC (33% vs. 0%) and IVM1a disease (16% vs. 2%) than in patients with stage IVM1b (3% vs. 4%) or IVM1c disease (7% vs. 3%). This may be because of insufficient time for the immunotherapy to benefit patients with visceral disease, or because injection of T-VEC into dermal, subcutaneous, and nodal metastases may activate an immune response that preferentially targets metastases in similar anatomic sites.
Among patients in the T-VEC arm who achieved a response, 54% had disease progression prior to response. This pseudoprogression is consistent with other immunotherapies and illustrates the importance of continuing treatment in stable patients despite increasing lesions, the investigators noted.
Based on a modified herpes simplex virus type 1, T-VEC is an oncolytic virus designed to replicate in and lyse tumor cells while promoting an antitumor immune response.
Adverse events more frequently observed in the T-VEC group were flu-like symptoms, including chills, pyrexia, nausea, and fatigue. Incidence of grade 3 or 4 adverse events was 11% for T-VEC and 5% for GM-CSF. The tolerable safety profile of T-VEC is an important factor in considering combined immunotherapy approaches, wrote Dr. Robert Andtbacka and associates.
“The evidence of local and systemic immune responses with T-VEC supports combinations with other immunotherapies as a rational approach. A phase 1b/2 study of T-VEC and ipilimumab is evaluating the safety and efficacy of this combination,” they wrote.
Treatment with the oncolytic immunotherapy talimogene laherparepvec (T-VEC) resulted in significantly longer rates of durable response and overall response, compared with subcutaneous granulocyte-macrophage colony-stimulating factor (GM-CSF), according to results from the phase III OPTiM trial reported in the Journal of Clinical Oncology.
“To our knowledge, OPTiM is the first randomized, controlled, phase III study evaluating an oncolytic immunotherapy to demonstrate a therapeutic benefit in melanoma,” wrote Dr. Robert Andtbacka, of the Huntsman Cancer Institute, University of Utah, Salt Lake City, and colleagues (J. Clin. Onc. 2015 May 26 [doi:10.1200/JCO.2014.58.3377]).
Patients who received T-VEC vs. subcutaneous GM-CSF had significantly improved rates of durable response, defined as responses lasting 6 months or more, (16.3% vs. 2.1%; P < .001), as well as improved overall response rates (26.4% vs. 5.7% ; P < .001). Complete responses were achieved in 10.8% of the T-VEC arm (32 patients) and < 1% (1 patient) in the GM-CSF arm. Median overall survival was 23.3 months for T-VEC and 18.9 months for GM-CSF (P = .051).
Differences in durable response rates and overall response rates between the T-VEC and GM-CSF arms were greater among patients with stage IIIb or IIIC (33% vs. 0%) and IVM1a disease (16% vs. 2%) than in patients with stage IVM1b (3% vs. 4%) or IVM1c disease (7% vs. 3%). This may be because of insufficient time for the immunotherapy to benefit patients with visceral disease, or because injection of T-VEC into dermal, subcutaneous, and nodal metastases may activate an immune response that preferentially targets metastases in similar anatomic sites.
Among patients in the T-VEC arm who achieved a response, 54% had disease progression prior to response. This pseudoprogression is consistent with other immunotherapies and illustrates the importance of continuing treatment in stable patients despite increasing lesions, the investigators noted.
Based on a modified herpes simplex virus type 1, T-VEC is an oncolytic virus designed to replicate in and lyse tumor cells while promoting an antitumor immune response.
Adverse events more frequently observed in the T-VEC group were flu-like symptoms, including chills, pyrexia, nausea, and fatigue. Incidence of grade 3 or 4 adverse events was 11% for T-VEC and 5% for GM-CSF. The tolerable safety profile of T-VEC is an important factor in considering combined immunotherapy approaches, wrote Dr. Robert Andtbacka and associates.
“The evidence of local and systemic immune responses with T-VEC supports combinations with other immunotherapies as a rational approach. A phase 1b/2 study of T-VEC and ipilimumab is evaluating the safety and efficacy of this combination,” they wrote.
Treatment with the oncolytic immunotherapy talimogene laherparepvec (T-VEC) resulted in significantly longer rates of durable response and overall response, compared with subcutaneous granulocyte-macrophage colony-stimulating factor (GM-CSF), according to results from the phase III OPTiM trial reported in the Journal of Clinical Oncology.
“To our knowledge, OPTiM is the first randomized, controlled, phase III study evaluating an oncolytic immunotherapy to demonstrate a therapeutic benefit in melanoma,” wrote Dr. Robert Andtbacka, of the Huntsman Cancer Institute, University of Utah, Salt Lake City, and colleagues (J. Clin. Onc. 2015 May 26 [doi:10.1200/JCO.2014.58.3377]).
Patients who received T-VEC vs. subcutaneous GM-CSF had significantly improved rates of durable response, defined as responses lasting 6 months or more, (16.3% vs. 2.1%; P < .001), as well as improved overall response rates (26.4% vs. 5.7% ; P < .001). Complete responses were achieved in 10.8% of the T-VEC arm (32 patients) and < 1% (1 patient) in the GM-CSF arm. Median overall survival was 23.3 months for T-VEC and 18.9 months for GM-CSF (P = .051).
Differences in durable response rates and overall response rates between the T-VEC and GM-CSF arms were greater among patients with stage IIIb or IIIC (33% vs. 0%) and IVM1a disease (16% vs. 2%) than in patients with stage IVM1b (3% vs. 4%) or IVM1c disease (7% vs. 3%). This may be because of insufficient time for the immunotherapy to benefit patients with visceral disease, or because injection of T-VEC into dermal, subcutaneous, and nodal metastases may activate an immune response that preferentially targets metastases in similar anatomic sites.
Among patients in the T-VEC arm who achieved a response, 54% had disease progression prior to response. This pseudoprogression is consistent with other immunotherapies and illustrates the importance of continuing treatment in stable patients despite increasing lesions, the investigators noted.
Based on a modified herpes simplex virus type 1, T-VEC is an oncolytic virus designed to replicate in and lyse tumor cells while promoting an antitumor immune response.
Adverse events more frequently observed in the T-VEC group were flu-like symptoms, including chills, pyrexia, nausea, and fatigue. Incidence of grade 3 or 4 adverse events was 11% for T-VEC and 5% for GM-CSF. The tolerable safety profile of T-VEC is an important factor in considering combined immunotherapy approaches, wrote Dr. Robert Andtbacka and associates.
“The evidence of local and systemic immune responses with T-VEC supports combinations with other immunotherapies as a rational approach. A phase 1b/2 study of T-VEC and ipilimumab is evaluating the safety and efficacy of this combination,” they wrote.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Compared with granulocyte-macrophage colony-stimulating factor, talimogene laherparepvec significantly improved durable response rates and overall response rates in patients with advanced melanoma.
Major finding: Durable response rates in the T-VEC vs. GM-CSF arms were 16.3% vs. 2.1% (P < .001). Overall response rates were 26.4% vs. 5.7% (P < .001).
Data source: The randomized open-label phase III trial included 437 patients with nonresectable stage IIIB to IV melanoma who received T-VEC (n = 291) or GM-CSF (n = 127).
Disclosures: The study was funded by Amgen. Dr. Andtbacka reported having financial relationships with Amgen, Novartis, Merck, Takeda Pharmaceuticals, and Viralytics. Many of his coauthors reported having financial relationships with industry.
ACOG spells out risk assessment for hereditary cancer syndromes
To identify patients at increased risk for certain types of cancer, ob.gyns. should perform and regularly update hereditary cancer risk assessments, according to a new recommendation from the American College of Obstetricians and Gynecologists.
Patients at increased risk for hereditary cancer syndromes should be referred to a cancer genetics specialist for further assessment and counseling, according to the opinion from ACOG’s Committee on Genetics (Obstet. Gynecol. 2015;125:1538-43).
Personal and family histories provide key information to determine the appropriateness of genetic counseling, which is distinct from genetic testing. Discussed in the counseling visit, the decision for genetic testing is based on family history, pedigree analysis, and, in some cases, pathology reports and confirmation of cancer deaths.
Patient intake forms are used in many office settings to gather relevant information. Online versions of intake forms, such as the Surgeon General’s “My Family Health Portrait,” can facilitate documentation of comprehensive histories. The American Society of Clinical Oncology also has identified some key elements of an adequate family history for assessing cancer risk, including first- and second-degree relatives, maternal and paternal sides, European Jewish ancestry, age of onset and type of cancer, and results of predisposition tests in any relative.
There are several indicators for the presence of hereditary cancer syndromes, including cancer diagnosed at an unusually young age, the presence of several different types of cancer, several close relatives with the same type of cancer, unusual presentation (such as breast cancer in a man), certain birth defects (such as skin growths or skeletal abnormalities associated with inherited cancer syndromes), and Ashkenazi Jewish ancestry.
The ACOG committee opinion identifies common hereditary cancer syndromes involved in gynecologic cancers, including hereditary breast and ovarian cancer syndrome and Lynch, Li-Fraumeni, Cowden, and Peutz-Jeghers syndromes.
Mutations in DNA repair genes BRCA1 and BRCA2 cause hereditary breast and ovarian cancer syndrome and account for 5%-15% of all breast and ovarian cancers in the United States. The carrier frequency in the general population is 1 in 500, but it is much higher (1 in 40) in the Ashkenazi Jewish population. Women with hereditary breast and ovarian cancer syndrome have a 65%-74% lifetime risk of breast cancer and 39%-46% (BRCA1) or 12%-20% (BRCA2) risk of ovarian cancer.
Also caused by DNA repair defects, Lynch syndrome, or hereditary nonpolyposis colorectal cancer, has a prevalence of 1 in 600 to 1 in 3,000. Individuals with Lynch syndrome have increased risk of colon (52%-82%), endometrial (25%-60%), and ovarian (4%-24%) cancers. Malignancies associated with Lynch syndrome include uterine, gastric, small bowel, hepatobiliary, breast, brain, and sebaceous skin cancers.
The presence of Li-Fraumeni syndrome increases the risk of osteosarcoma, breast cancer, colon cancer, adrenocortical carcinoma, leukemia and lymphoma, and brain cancer. Caused by mutations in the tumor suppressor gene TP53, individuals with the syndrome have a 90% risk of cancer by age 60 years. Patients diagnosed with a Li-Fraumeni syndrome–associated malignancy should be referred to a cancer genetics specialist for counseling, according to the committee opinion.
Individuals with the relatively rare (1 in 200,000) Cowden syndrome usually have pathognomonic skin lesions, including papillomatous papules on the face and mucous membranes, by age 30 years. The presence of Cowden syndrome increases the lifetime risk of breast cancer to 25%-50% and endometrial cancer to 5%-10%. Clinicians should consult frequently updated guidelines to determine which patients should be referred for genetic evaluation.
Mutations in serine/threonine kinase 11 cause Peutz-Jehgers syndrome. Two of the following three criteria characterize the syndrome: two or more hamartomatous polyps in the GI tract; mucocutaneous hyperpigmentation of the mouth, lips, nose, eyes, genitalia, or fingers; and a family history of Peutz-Jeghers syndrome. Women with Peutz-Jeghers syndrome have a 50% increased lifetime risk of breast cancer and increased risk of ovarian, uterine, and cervical cancer.
To identify patients at increased risk for certain types of cancer, ob.gyns. should perform and regularly update hereditary cancer risk assessments, according to a new recommendation from the American College of Obstetricians and Gynecologists.
Patients at increased risk for hereditary cancer syndromes should be referred to a cancer genetics specialist for further assessment and counseling, according to the opinion from ACOG’s Committee on Genetics (Obstet. Gynecol. 2015;125:1538-43).
Personal and family histories provide key information to determine the appropriateness of genetic counseling, which is distinct from genetic testing. Discussed in the counseling visit, the decision for genetic testing is based on family history, pedigree analysis, and, in some cases, pathology reports and confirmation of cancer deaths.
Patient intake forms are used in many office settings to gather relevant information. Online versions of intake forms, such as the Surgeon General’s “My Family Health Portrait,” can facilitate documentation of comprehensive histories. The American Society of Clinical Oncology also has identified some key elements of an adequate family history for assessing cancer risk, including first- and second-degree relatives, maternal and paternal sides, European Jewish ancestry, age of onset and type of cancer, and results of predisposition tests in any relative.
There are several indicators for the presence of hereditary cancer syndromes, including cancer diagnosed at an unusually young age, the presence of several different types of cancer, several close relatives with the same type of cancer, unusual presentation (such as breast cancer in a man), certain birth defects (such as skin growths or skeletal abnormalities associated with inherited cancer syndromes), and Ashkenazi Jewish ancestry.
The ACOG committee opinion identifies common hereditary cancer syndromes involved in gynecologic cancers, including hereditary breast and ovarian cancer syndrome and Lynch, Li-Fraumeni, Cowden, and Peutz-Jeghers syndromes.
Mutations in DNA repair genes BRCA1 and BRCA2 cause hereditary breast and ovarian cancer syndrome and account for 5%-15% of all breast and ovarian cancers in the United States. The carrier frequency in the general population is 1 in 500, but it is much higher (1 in 40) in the Ashkenazi Jewish population. Women with hereditary breast and ovarian cancer syndrome have a 65%-74% lifetime risk of breast cancer and 39%-46% (BRCA1) or 12%-20% (BRCA2) risk of ovarian cancer.
Also caused by DNA repair defects, Lynch syndrome, or hereditary nonpolyposis colorectal cancer, has a prevalence of 1 in 600 to 1 in 3,000. Individuals with Lynch syndrome have increased risk of colon (52%-82%), endometrial (25%-60%), and ovarian (4%-24%) cancers. Malignancies associated with Lynch syndrome include uterine, gastric, small bowel, hepatobiliary, breast, brain, and sebaceous skin cancers.
The presence of Li-Fraumeni syndrome increases the risk of osteosarcoma, breast cancer, colon cancer, adrenocortical carcinoma, leukemia and lymphoma, and brain cancer. Caused by mutations in the tumor suppressor gene TP53, individuals with the syndrome have a 90% risk of cancer by age 60 years. Patients diagnosed with a Li-Fraumeni syndrome–associated malignancy should be referred to a cancer genetics specialist for counseling, according to the committee opinion.
Individuals with the relatively rare (1 in 200,000) Cowden syndrome usually have pathognomonic skin lesions, including papillomatous papules on the face and mucous membranes, by age 30 years. The presence of Cowden syndrome increases the lifetime risk of breast cancer to 25%-50% and endometrial cancer to 5%-10%. Clinicians should consult frequently updated guidelines to determine which patients should be referred for genetic evaluation.
Mutations in serine/threonine kinase 11 cause Peutz-Jehgers syndrome. Two of the following three criteria characterize the syndrome: two or more hamartomatous polyps in the GI tract; mucocutaneous hyperpigmentation of the mouth, lips, nose, eyes, genitalia, or fingers; and a family history of Peutz-Jeghers syndrome. Women with Peutz-Jeghers syndrome have a 50% increased lifetime risk of breast cancer and increased risk of ovarian, uterine, and cervical cancer.
To identify patients at increased risk for certain types of cancer, ob.gyns. should perform and regularly update hereditary cancer risk assessments, according to a new recommendation from the American College of Obstetricians and Gynecologists.
Patients at increased risk for hereditary cancer syndromes should be referred to a cancer genetics specialist for further assessment and counseling, according to the opinion from ACOG’s Committee on Genetics (Obstet. Gynecol. 2015;125:1538-43).
Personal and family histories provide key information to determine the appropriateness of genetic counseling, which is distinct from genetic testing. Discussed in the counseling visit, the decision for genetic testing is based on family history, pedigree analysis, and, in some cases, pathology reports and confirmation of cancer deaths.
Patient intake forms are used in many office settings to gather relevant information. Online versions of intake forms, such as the Surgeon General’s “My Family Health Portrait,” can facilitate documentation of comprehensive histories. The American Society of Clinical Oncology also has identified some key elements of an adequate family history for assessing cancer risk, including first- and second-degree relatives, maternal and paternal sides, European Jewish ancestry, age of onset and type of cancer, and results of predisposition tests in any relative.
There are several indicators for the presence of hereditary cancer syndromes, including cancer diagnosed at an unusually young age, the presence of several different types of cancer, several close relatives with the same type of cancer, unusual presentation (such as breast cancer in a man), certain birth defects (such as skin growths or skeletal abnormalities associated with inherited cancer syndromes), and Ashkenazi Jewish ancestry.
The ACOG committee opinion identifies common hereditary cancer syndromes involved in gynecologic cancers, including hereditary breast and ovarian cancer syndrome and Lynch, Li-Fraumeni, Cowden, and Peutz-Jeghers syndromes.
Mutations in DNA repair genes BRCA1 and BRCA2 cause hereditary breast and ovarian cancer syndrome and account for 5%-15% of all breast and ovarian cancers in the United States. The carrier frequency in the general population is 1 in 500, but it is much higher (1 in 40) in the Ashkenazi Jewish population. Women with hereditary breast and ovarian cancer syndrome have a 65%-74% lifetime risk of breast cancer and 39%-46% (BRCA1) or 12%-20% (BRCA2) risk of ovarian cancer.
Also caused by DNA repair defects, Lynch syndrome, or hereditary nonpolyposis colorectal cancer, has a prevalence of 1 in 600 to 1 in 3,000. Individuals with Lynch syndrome have increased risk of colon (52%-82%), endometrial (25%-60%), and ovarian (4%-24%) cancers. Malignancies associated with Lynch syndrome include uterine, gastric, small bowel, hepatobiliary, breast, brain, and sebaceous skin cancers.
The presence of Li-Fraumeni syndrome increases the risk of osteosarcoma, breast cancer, colon cancer, adrenocortical carcinoma, leukemia and lymphoma, and brain cancer. Caused by mutations in the tumor suppressor gene TP53, individuals with the syndrome have a 90% risk of cancer by age 60 years. Patients diagnosed with a Li-Fraumeni syndrome–associated malignancy should be referred to a cancer genetics specialist for counseling, according to the committee opinion.
Individuals with the relatively rare (1 in 200,000) Cowden syndrome usually have pathognomonic skin lesions, including papillomatous papules on the face and mucous membranes, by age 30 years. The presence of Cowden syndrome increases the lifetime risk of breast cancer to 25%-50% and endometrial cancer to 5%-10%. Clinicians should consult frequently updated guidelines to determine which patients should be referred for genetic evaluation.
Mutations in serine/threonine kinase 11 cause Peutz-Jehgers syndrome. Two of the following three criteria characterize the syndrome: two or more hamartomatous polyps in the GI tract; mucocutaneous hyperpigmentation of the mouth, lips, nose, eyes, genitalia, or fingers; and a family history of Peutz-Jeghers syndrome. Women with Peutz-Jeghers syndrome have a 50% increased lifetime risk of breast cancer and increased risk of ovarian, uterine, and cervical cancer.