User login
Jennifer Smith is the editor of Oncology Practice, part of MDedge Hematology/Oncology. She was previously the editor of Hematology Times, an editor at Principal Investigators Association, and a reporter at The Oneida Daily Dispatch. She has a BS in journalism.
FDA approves ibrutinib plus obinutuzumab for CLL/SLL
The Food and Drug Administration has approved ibrutinib (Imbruvica) for use in combination with obinutuzumab to treat adults with previously untreated chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
This is the tenth FDA approval for ibrutinib, a Bruton tyrosine kinase inhibitor jointly developed and commercialized by Pharmacyclics, an AbbVie company, and Janssen Biotech.
The approval is supported by the phase 3 iLLUMINATE trial (NCT02264574).
Results from this study were recently presented at the annual meeting of the American Society of Hematology (Blood. 2018;132:691) and published in the Lancet Oncology (2019 Jan;20[1]:43-56).
The iLLUMINATE trial enrolled newly diagnosed CLL patients who were randomized to receive ibrutinib plus obinutuzumab (n = 113) or chlorambucil plus obinutuzumab (n = 116).
The median follow-up was 31.3 months. The overall response rate was 88% in the ibrutinib arm and 73% in the chlorambucil arm. The complete response rate, including complete response with incomplete marrow recovery, was 19% and 8%, respectively.
The median progression-free survival was not reached in the ibrutinib arm and was 19.0 months in the chlorambucil arm (hazard ratio, 0.23; 95% confidence interval, 0.15-0.37; P less than .0001). The estimated 30-month progression-free survival was 79% and 31%, respectively.
The most common grade 3/4 adverse events in both arms were neutropenia (36% in the ibrutinib arm and 46% in the chlorambucil arm) and thrombocytopenia (19% and 10%, respectively).
There were 10 deaths caused by adverse events in the ibrutinib arm and 3 in the chlorambucil arm. One death was considered possibly related to ibrutinib (sudden death), and another was considered possibly related to chlorambucil (neuroendocrine carcinoma of the skin).
The Food and Drug Administration has approved ibrutinib (Imbruvica) for use in combination with obinutuzumab to treat adults with previously untreated chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
This is the tenth FDA approval for ibrutinib, a Bruton tyrosine kinase inhibitor jointly developed and commercialized by Pharmacyclics, an AbbVie company, and Janssen Biotech.
The approval is supported by the phase 3 iLLUMINATE trial (NCT02264574).
Results from this study were recently presented at the annual meeting of the American Society of Hematology (Blood. 2018;132:691) and published in the Lancet Oncology (2019 Jan;20[1]:43-56).
The iLLUMINATE trial enrolled newly diagnosed CLL patients who were randomized to receive ibrutinib plus obinutuzumab (n = 113) or chlorambucil plus obinutuzumab (n = 116).
The median follow-up was 31.3 months. The overall response rate was 88% in the ibrutinib arm and 73% in the chlorambucil arm. The complete response rate, including complete response with incomplete marrow recovery, was 19% and 8%, respectively.
The median progression-free survival was not reached in the ibrutinib arm and was 19.0 months in the chlorambucil arm (hazard ratio, 0.23; 95% confidence interval, 0.15-0.37; P less than .0001). The estimated 30-month progression-free survival was 79% and 31%, respectively.
The most common grade 3/4 adverse events in both arms were neutropenia (36% in the ibrutinib arm and 46% in the chlorambucil arm) and thrombocytopenia (19% and 10%, respectively).
There were 10 deaths caused by adverse events in the ibrutinib arm and 3 in the chlorambucil arm. One death was considered possibly related to ibrutinib (sudden death), and another was considered possibly related to chlorambucil (neuroendocrine carcinoma of the skin).
The Food and Drug Administration has approved ibrutinib (Imbruvica) for use in combination with obinutuzumab to treat adults with previously untreated chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
This is the tenth FDA approval for ibrutinib, a Bruton tyrosine kinase inhibitor jointly developed and commercialized by Pharmacyclics, an AbbVie company, and Janssen Biotech.
The approval is supported by the phase 3 iLLUMINATE trial (NCT02264574).
Results from this study were recently presented at the annual meeting of the American Society of Hematology (Blood. 2018;132:691) and published in the Lancet Oncology (2019 Jan;20[1]:43-56).
The iLLUMINATE trial enrolled newly diagnosed CLL patients who were randomized to receive ibrutinib plus obinutuzumab (n = 113) or chlorambucil plus obinutuzumab (n = 116).
The median follow-up was 31.3 months. The overall response rate was 88% in the ibrutinib arm and 73% in the chlorambucil arm. The complete response rate, including complete response with incomplete marrow recovery, was 19% and 8%, respectively.
The median progression-free survival was not reached in the ibrutinib arm and was 19.0 months in the chlorambucil arm (hazard ratio, 0.23; 95% confidence interval, 0.15-0.37; P less than .0001). The estimated 30-month progression-free survival was 79% and 31%, respectively.
The most common grade 3/4 adverse events in both arms were neutropenia (36% in the ibrutinib arm and 46% in the chlorambucil arm) and thrombocytopenia (19% and 10%, respectively).
There were 10 deaths caused by adverse events in the ibrutinib arm and 3 in the chlorambucil arm. One death was considered possibly related to ibrutinib (sudden death), and another was considered possibly related to chlorambucil (neuroendocrine carcinoma of the skin).
EC approves blinatumomab for MRD-positive BCP-ALL
The European Commission (EC) has expanded the approved indication for blinatumomab (Blincyto).
The drug is now approved in Europe to treat adults with Philadelphia chromosome–negative (Ph–), CD19-positive B-cell precursor acute lymphoblastic leukemia (BCP-ALL) in first or second complete remission with minimal residual disease (MRD) of at least 0.1%.
Blinatumomab is already approved in Europe to treat adults with Ph–, CD19-positive relapsed/refractory BCP-ALL and children aged 1 year or older who have relapsed/refractory Ph–, CD19-positive BCP-ALL and have received at least two prior therapies or relapsed after allogeneic hematopoietic stem cell transplant.
The drug was approved in the United States in March 2018 for the treatment of adults and children with BCP-ALL in first or second complete remission with MRD of at least 0.1%.
The EC’s decision to approve blinatumomab in MRD-positive patients was supported by the phase 2 BLAST trial (Blood. 2018;131[14]:1522-31).
The EC’s approval is also based on a positive opinion from the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
That opinion, issued in November 2018, was a reversal of the opinion the committee issued in July 2018. At that time, the CHMP said the available data did not support approval for blinatumomab to treat MRD-positive BCP-ALL.
The CHMP acknowledged that blinatumomab produced MRD negativity in many patients in the BLAST trial but said there was no strong evidence that this led to improved survival. As a result, the CHMP said the benefits of blinatumomab do not outweigh its risks in MRD-positive BCP-ALL patients.
However, Amgen requested a reexamination of the CHMP’s opinion. During the reexamination, the CHMP reviewed all the data and consulted a group of experts.
The experts echoed the CHMP’s prior sentiment that there was no strong evidence of improved survival in MRD-positive patients treated with blinatumomab. However, they also said the data indicate a good response to blinatumomab, with around 78% of patients becoming negative for MRD after treatment.
Noting that MRD-positive patients have a high risk of relapse and few treatment options, the CHMP concluded that the benefits of blinatumomab outweigh its risks in this patient population.
The CHMP recommended expanding the approved indication for blinatumomab but also requested that Amgen provide data from ongoing studies of the drug in MRD-positive patients.
The European Commission (EC) has expanded the approved indication for blinatumomab (Blincyto).
The drug is now approved in Europe to treat adults with Philadelphia chromosome–negative (Ph–), CD19-positive B-cell precursor acute lymphoblastic leukemia (BCP-ALL) in first or second complete remission with minimal residual disease (MRD) of at least 0.1%.
Blinatumomab is already approved in Europe to treat adults with Ph–, CD19-positive relapsed/refractory BCP-ALL and children aged 1 year or older who have relapsed/refractory Ph–, CD19-positive BCP-ALL and have received at least two prior therapies or relapsed after allogeneic hematopoietic stem cell transplant.
The drug was approved in the United States in March 2018 for the treatment of adults and children with BCP-ALL in first or second complete remission with MRD of at least 0.1%.
The EC’s decision to approve blinatumomab in MRD-positive patients was supported by the phase 2 BLAST trial (Blood. 2018;131[14]:1522-31).
The EC’s approval is also based on a positive opinion from the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
That opinion, issued in November 2018, was a reversal of the opinion the committee issued in July 2018. At that time, the CHMP said the available data did not support approval for blinatumomab to treat MRD-positive BCP-ALL.
The CHMP acknowledged that blinatumomab produced MRD negativity in many patients in the BLAST trial but said there was no strong evidence that this led to improved survival. As a result, the CHMP said the benefits of blinatumomab do not outweigh its risks in MRD-positive BCP-ALL patients.
However, Amgen requested a reexamination of the CHMP’s opinion. During the reexamination, the CHMP reviewed all the data and consulted a group of experts.
The experts echoed the CHMP’s prior sentiment that there was no strong evidence of improved survival in MRD-positive patients treated with blinatumomab. However, they also said the data indicate a good response to blinatumomab, with around 78% of patients becoming negative for MRD after treatment.
Noting that MRD-positive patients have a high risk of relapse and few treatment options, the CHMP concluded that the benefits of blinatumomab outweigh its risks in this patient population.
The CHMP recommended expanding the approved indication for blinatumomab but also requested that Amgen provide data from ongoing studies of the drug in MRD-positive patients.
The European Commission (EC) has expanded the approved indication for blinatumomab (Blincyto).
The drug is now approved in Europe to treat adults with Philadelphia chromosome–negative (Ph–), CD19-positive B-cell precursor acute lymphoblastic leukemia (BCP-ALL) in first or second complete remission with minimal residual disease (MRD) of at least 0.1%.
Blinatumomab is already approved in Europe to treat adults with Ph–, CD19-positive relapsed/refractory BCP-ALL and children aged 1 year or older who have relapsed/refractory Ph–, CD19-positive BCP-ALL and have received at least two prior therapies or relapsed after allogeneic hematopoietic stem cell transplant.
The drug was approved in the United States in March 2018 for the treatment of adults and children with BCP-ALL in first or second complete remission with MRD of at least 0.1%.
The EC’s decision to approve blinatumomab in MRD-positive patients was supported by the phase 2 BLAST trial (Blood. 2018;131[14]:1522-31).
The EC’s approval is also based on a positive opinion from the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
That opinion, issued in November 2018, was a reversal of the opinion the committee issued in July 2018. At that time, the CHMP said the available data did not support approval for blinatumomab to treat MRD-positive BCP-ALL.
The CHMP acknowledged that blinatumomab produced MRD negativity in many patients in the BLAST trial but said there was no strong evidence that this led to improved survival. As a result, the CHMP said the benefits of blinatumomab do not outweigh its risks in MRD-positive BCP-ALL patients.
However, Amgen requested a reexamination of the CHMP’s opinion. During the reexamination, the CHMP reviewed all the data and consulted a group of experts.
The experts echoed the CHMP’s prior sentiment that there was no strong evidence of improved survival in MRD-positive patients treated with blinatumomab. However, they also said the data indicate a good response to blinatumomab, with around 78% of patients becoming negative for MRD after treatment.
Noting that MRD-positive patients have a high risk of relapse and few treatment options, the CHMP concluded that the benefits of blinatumomab outweigh its risks in this patient population.
The CHMP recommended expanding the approved indication for blinatumomab but also requested that Amgen provide data from ongoing studies of the drug in MRD-positive patients.
Umbralisib gains FDA breakthrough designation for MZL
The who have received at least one prior anti-CD20 regimen.
Umbralisib (formerly TGR-1202) is a PI3K-delta inhibitor being developed by TG Therapeutics.
Breakthrough designation entitles the company developing a therapy to more intensive FDA guidance and other actions that may expedite FDA review. For a treatment to earn breakthrough designation, early clinical results must show that it provides improvement over available therapies or fulfills an unmet need.
The breakthrough designation for umbralisib was based on interim data from the MZL cohort in the ongoing, phase 2b UNITY-NHL trial (NCT02793583).
In this trial, researchers are testing umbralisib alone or in combination with ublituximab, with or without bendamustine, in patients with previously treated non-Hodgkin lymphoma.
“The MZL single-agent umbralisib cohort of the UNITY-NHL study is fully enrolled, and we look forward to reporting topline results from this cohort by mid-year and presenting the data at a major medical meeting in 2019,” Michael S. Weiss, chief executive officer of TG Therapeutics, said in a statement.
Umbralisib monotherapy was previously evaluated in a phase 1 trial (NCT01767766) of patients with relapsed or refractory B-cell malignancies (Lancet Oncol. 2018 Apr;19[4]:486-96).
The trial enrolled 90 patients, and five of them had MZL. A total of 33 patients achieved a response to umbralisib. This includes one MZL patient who achieved a partial response.
The most common treatment-emergent adverse events (AEs) in this trial were diarrhea, nausea, and fatigue. The most common grade 3/4 AEs were neutropenia, anemia, and thrombocytopenia.
Serious AEs considered at least possibly related to umbralisib were pneumonia, lung infection, febrile neutropenia, and colitis. There were no treatment-related deaths.
The who have received at least one prior anti-CD20 regimen.
Umbralisib (formerly TGR-1202) is a PI3K-delta inhibitor being developed by TG Therapeutics.
Breakthrough designation entitles the company developing a therapy to more intensive FDA guidance and other actions that may expedite FDA review. For a treatment to earn breakthrough designation, early clinical results must show that it provides improvement over available therapies or fulfills an unmet need.
The breakthrough designation for umbralisib was based on interim data from the MZL cohort in the ongoing, phase 2b UNITY-NHL trial (NCT02793583).
In this trial, researchers are testing umbralisib alone or in combination with ublituximab, with or without bendamustine, in patients with previously treated non-Hodgkin lymphoma.
“The MZL single-agent umbralisib cohort of the UNITY-NHL study is fully enrolled, and we look forward to reporting topline results from this cohort by mid-year and presenting the data at a major medical meeting in 2019,” Michael S. Weiss, chief executive officer of TG Therapeutics, said in a statement.
Umbralisib monotherapy was previously evaluated in a phase 1 trial (NCT01767766) of patients with relapsed or refractory B-cell malignancies (Lancet Oncol. 2018 Apr;19[4]:486-96).
The trial enrolled 90 patients, and five of them had MZL. A total of 33 patients achieved a response to umbralisib. This includes one MZL patient who achieved a partial response.
The most common treatment-emergent adverse events (AEs) in this trial were diarrhea, nausea, and fatigue. The most common grade 3/4 AEs were neutropenia, anemia, and thrombocytopenia.
Serious AEs considered at least possibly related to umbralisib were pneumonia, lung infection, febrile neutropenia, and colitis. There were no treatment-related deaths.
The who have received at least one prior anti-CD20 regimen.
Umbralisib (formerly TGR-1202) is a PI3K-delta inhibitor being developed by TG Therapeutics.
Breakthrough designation entitles the company developing a therapy to more intensive FDA guidance and other actions that may expedite FDA review. For a treatment to earn breakthrough designation, early clinical results must show that it provides improvement over available therapies or fulfills an unmet need.
The breakthrough designation for umbralisib was based on interim data from the MZL cohort in the ongoing, phase 2b UNITY-NHL trial (NCT02793583).
In this trial, researchers are testing umbralisib alone or in combination with ublituximab, with or without bendamustine, in patients with previously treated non-Hodgkin lymphoma.
“The MZL single-agent umbralisib cohort of the UNITY-NHL study is fully enrolled, and we look forward to reporting topline results from this cohort by mid-year and presenting the data at a major medical meeting in 2019,” Michael S. Weiss, chief executive officer of TG Therapeutics, said in a statement.
Umbralisib monotherapy was previously evaluated in a phase 1 trial (NCT01767766) of patients with relapsed or refractory B-cell malignancies (Lancet Oncol. 2018 Apr;19[4]:486-96).
The trial enrolled 90 patients, and five of them had MZL. A total of 33 patients achieved a response to umbralisib. This includes one MZL patient who achieved a partial response.
The most common treatment-emergent adverse events (AEs) in this trial were diarrhea, nausea, and fatigue. The most common grade 3/4 AEs were neutropenia, anemia, and thrombocytopenia.
Serious AEs considered at least possibly related to umbralisib were pneumonia, lung infection, febrile neutropenia, and colitis. There were no treatment-related deaths.
Combo treatment may improve quality of life in CTCL
LA JOLLA, CALIF. — Treatment with brentuximab vedotin (BV) and lenalidomide (len) may improve quality of life (QOL) for patients with cutaneous T-cell lymphoma (CTCL), according to the principal investigator of a phase 2 trial.

In this small trial, most CTCL patients experienced relief from pruritus after one cycle of treatment with BV-len.
Investigators also observed durable responses to the combination, although two patients experienced tumor flare prior to response.
“Because of the tumor flare, we decreased the dose of lenalidomide ... and, since then, it has not been a major problem,” said Basem M. William, MD, principal investigator of the trial and a professor at Ohio State University in Columbus.
“We’re trying to be more reassuring to patients that, if they experience a little bit of tumor flare, as long as it’s not dangerous or life-threatening, if they can hold on with the treatment, this might translate to a later durable response.”
Dr. William and his colleagues presented results from this ongoing, phase 2 trial (NCT03409432) at the annual T-cell Lymphoma Forum.
Thus far, the investigators have treated 12 patients with relapsed or refractory CTCL or peripheral T-cell lymphoma (PTCL). The CTCL patients had received at least two lines of skin-directed therapy or one line of systemic therapy, and the PTCL patients had received at least one line of systemic therapy.
Dr. William and his colleagues reported results for 10 patients. Six patients had mycosis fungoides (MF), two had Sézary syndrome (SS), one had CD30+ lymphoproliferative disorder, and one had systemic anaplastic large-cell lymphoma (ALCL).
The patients’ median age was 59 (range, 49-74), there were nine males, and patients had received a median of 2 (range, 1-10) prior therapies.
The first seven patients received BV at 1.2 mg/kg and len at 20 mg daily every 3 weeks. However, after the investigators observed tumor flare in two patients, the dose of len was lowered to 10 mg.
Safety
The investigators said all adverse events (AEs) were reversible by stopping therapy, there were no grade 4 AEs, and none of the patients had grade 3 or higher neuropathy.
“We have not seen an excess of neuropathy, which is very important because both brentuximab and lenalidomide are known to cause neuropathy,” Dr. William said. “So we were fairly concerned that there would be a synergistic neurotoxic effect, which we don’t want, but we haven’t seen that.”
The most common treatment-related AE was neutropenia. Grade 3 neutropenia occurred in four patients.
Other grade 3 AEs, which occurred in patients on the 20 mg dose of len, were thrombocytopenia (n = 1), dyspnea (n = 1), vertigo (n = 1), drug rash with eosinophilia and systemic symptoms (DRESS) syndrome (n = 1), and tumor flare (n = 1).
Three patients discontinued treatment because of AEs — thrombocytopenia, tumor flare, and DRESS syndrome.
Tumor flare and response
“We did see tumor flare in two initial patients treated with the higher dose of lenalidomide, and we had to remove them from the study for their safety,” Dr. William said. “One of them had a full-blown DRESS syndrome. For their safety, we did have to remove them, but both did experience durable remissions after.”
One of the patients with tumor flare, who had MF, didn’t require treatment for 6 months after going off study. The other patient, who had SS, cleared the clone from his blood but developed DRESS syndrome.
In all, three patients achieved a response to treatment. The ALCL patient had a complete response, and two MF patients achieved a partial response.
Two MF patients and one SS patient had stable disease. The remaining four patients — two with MF, one with SS, and one with lymphoproliferative disorder — progressed.
QOL
The investigators used the Skindex-16 to assess the effect of treatment on QOL.
Five of six evaluable patients with CTCL had a 50% or greater reduction in their Skindex-16 scores after two cycles of treatment. In fact, most patients had relief from pruritus after one cycle, Dr. William said.
“Patients with cutaneous T-cell lymphoma, their biggest problem is with the symptom burden, with pruritus,” he said. “They’re really miserable from all the itching they have. They cannot sleep at night. So we’re fairly excited that most of the patients we’ve treated so far had relief from pruritus just after one cycle.”
Dr. William said he and his colleagues are excited about the overall results they have observed with BV-len, although it’s “still pretty early” in the trial. The investigators are planning to enroll a total of 42 patients and may open the trial at a second center.
The study is sponsored by Ohio State University and the lenalidomide is provided by Celgene. Dr. William reported relationships with miRagen Therapeutics, GuidePoint, Kyowa Kirin, and Celgene.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Treatment with brentuximab vedotin (BV) and lenalidomide (len) may improve quality of life (QOL) for patients with cutaneous T-cell lymphoma (CTCL), according to the principal investigator of a phase 2 trial.

In this small trial, most CTCL patients experienced relief from pruritus after one cycle of treatment with BV-len.
Investigators also observed durable responses to the combination, although two patients experienced tumor flare prior to response.
“Because of the tumor flare, we decreased the dose of lenalidomide ... and, since then, it has not been a major problem,” said Basem M. William, MD, principal investigator of the trial and a professor at Ohio State University in Columbus.
“We’re trying to be more reassuring to patients that, if they experience a little bit of tumor flare, as long as it’s not dangerous or life-threatening, if they can hold on with the treatment, this might translate to a later durable response.”
Dr. William and his colleagues presented results from this ongoing, phase 2 trial (NCT03409432) at the annual T-cell Lymphoma Forum.
Thus far, the investigators have treated 12 patients with relapsed or refractory CTCL or peripheral T-cell lymphoma (PTCL). The CTCL patients had received at least two lines of skin-directed therapy or one line of systemic therapy, and the PTCL patients had received at least one line of systemic therapy.
Dr. William and his colleagues reported results for 10 patients. Six patients had mycosis fungoides (MF), two had Sézary syndrome (SS), one had CD30+ lymphoproliferative disorder, and one had systemic anaplastic large-cell lymphoma (ALCL).
The patients’ median age was 59 (range, 49-74), there were nine males, and patients had received a median of 2 (range, 1-10) prior therapies.
The first seven patients received BV at 1.2 mg/kg and len at 20 mg daily every 3 weeks. However, after the investigators observed tumor flare in two patients, the dose of len was lowered to 10 mg.
Safety
The investigators said all adverse events (AEs) were reversible by stopping therapy, there were no grade 4 AEs, and none of the patients had grade 3 or higher neuropathy.
“We have not seen an excess of neuropathy, which is very important because both brentuximab and lenalidomide are known to cause neuropathy,” Dr. William said. “So we were fairly concerned that there would be a synergistic neurotoxic effect, which we don’t want, but we haven’t seen that.”
The most common treatment-related AE was neutropenia. Grade 3 neutropenia occurred in four patients.
Other grade 3 AEs, which occurred in patients on the 20 mg dose of len, were thrombocytopenia (n = 1), dyspnea (n = 1), vertigo (n = 1), drug rash with eosinophilia and systemic symptoms (DRESS) syndrome (n = 1), and tumor flare (n = 1).
Three patients discontinued treatment because of AEs — thrombocytopenia, tumor flare, and DRESS syndrome.
Tumor flare and response
“We did see tumor flare in two initial patients treated with the higher dose of lenalidomide, and we had to remove them from the study for their safety,” Dr. William said. “One of them had a full-blown DRESS syndrome. For their safety, we did have to remove them, but both did experience durable remissions after.”
One of the patients with tumor flare, who had MF, didn’t require treatment for 6 months after going off study. The other patient, who had SS, cleared the clone from his blood but developed DRESS syndrome.
In all, three patients achieved a response to treatment. The ALCL patient had a complete response, and two MF patients achieved a partial response.
Two MF patients and one SS patient had stable disease. The remaining four patients — two with MF, one with SS, and one with lymphoproliferative disorder — progressed.
QOL
The investigators used the Skindex-16 to assess the effect of treatment on QOL.
Five of six evaluable patients with CTCL had a 50% or greater reduction in their Skindex-16 scores after two cycles of treatment. In fact, most patients had relief from pruritus after one cycle, Dr. William said.
“Patients with cutaneous T-cell lymphoma, their biggest problem is with the symptom burden, with pruritus,” he said. “They’re really miserable from all the itching they have. They cannot sleep at night. So we’re fairly excited that most of the patients we’ve treated so far had relief from pruritus just after one cycle.”
Dr. William said he and his colleagues are excited about the overall results they have observed with BV-len, although it’s “still pretty early” in the trial. The investigators are planning to enroll a total of 42 patients and may open the trial at a second center.
The study is sponsored by Ohio State University and the lenalidomide is provided by Celgene. Dr. William reported relationships with miRagen Therapeutics, GuidePoint, Kyowa Kirin, and Celgene.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Treatment with brentuximab vedotin (BV) and lenalidomide (len) may improve quality of life (QOL) for patients with cutaneous T-cell lymphoma (CTCL), according to the principal investigator of a phase 2 trial.

In this small trial, most CTCL patients experienced relief from pruritus after one cycle of treatment with BV-len.
Investigators also observed durable responses to the combination, although two patients experienced tumor flare prior to response.
“Because of the tumor flare, we decreased the dose of lenalidomide ... and, since then, it has not been a major problem,” said Basem M. William, MD, principal investigator of the trial and a professor at Ohio State University in Columbus.
“We’re trying to be more reassuring to patients that, if they experience a little bit of tumor flare, as long as it’s not dangerous or life-threatening, if they can hold on with the treatment, this might translate to a later durable response.”
Dr. William and his colleagues presented results from this ongoing, phase 2 trial (NCT03409432) at the annual T-cell Lymphoma Forum.
Thus far, the investigators have treated 12 patients with relapsed or refractory CTCL or peripheral T-cell lymphoma (PTCL). The CTCL patients had received at least two lines of skin-directed therapy or one line of systemic therapy, and the PTCL patients had received at least one line of systemic therapy.
Dr. William and his colleagues reported results for 10 patients. Six patients had mycosis fungoides (MF), two had Sézary syndrome (SS), one had CD30+ lymphoproliferative disorder, and one had systemic anaplastic large-cell lymphoma (ALCL).
The patients’ median age was 59 (range, 49-74), there were nine males, and patients had received a median of 2 (range, 1-10) prior therapies.
The first seven patients received BV at 1.2 mg/kg and len at 20 mg daily every 3 weeks. However, after the investigators observed tumor flare in two patients, the dose of len was lowered to 10 mg.
Safety
The investigators said all adverse events (AEs) were reversible by stopping therapy, there were no grade 4 AEs, and none of the patients had grade 3 or higher neuropathy.
“We have not seen an excess of neuropathy, which is very important because both brentuximab and lenalidomide are known to cause neuropathy,” Dr. William said. “So we were fairly concerned that there would be a synergistic neurotoxic effect, which we don’t want, but we haven’t seen that.”
The most common treatment-related AE was neutropenia. Grade 3 neutropenia occurred in four patients.
Other grade 3 AEs, which occurred in patients on the 20 mg dose of len, were thrombocytopenia (n = 1), dyspnea (n = 1), vertigo (n = 1), drug rash with eosinophilia and systemic symptoms (DRESS) syndrome (n = 1), and tumor flare (n = 1).
Three patients discontinued treatment because of AEs — thrombocytopenia, tumor flare, and DRESS syndrome.
Tumor flare and response
“We did see tumor flare in two initial patients treated with the higher dose of lenalidomide, and we had to remove them from the study for their safety,” Dr. William said. “One of them had a full-blown DRESS syndrome. For their safety, we did have to remove them, but both did experience durable remissions after.”
One of the patients with tumor flare, who had MF, didn’t require treatment for 6 months after going off study. The other patient, who had SS, cleared the clone from his blood but developed DRESS syndrome.
In all, three patients achieved a response to treatment. The ALCL patient had a complete response, and two MF patients achieved a partial response.
Two MF patients and one SS patient had stable disease. The remaining four patients — two with MF, one with SS, and one with lymphoproliferative disorder — progressed.
QOL
The investigators used the Skindex-16 to assess the effect of treatment on QOL.
Five of six evaluable patients with CTCL had a 50% or greater reduction in their Skindex-16 scores after two cycles of treatment. In fact, most patients had relief from pruritus after one cycle, Dr. William said.
“Patients with cutaneous T-cell lymphoma, their biggest problem is with the symptom burden, with pruritus,” he said. “They’re really miserable from all the itching they have. They cannot sleep at night. So we’re fairly excited that most of the patients we’ve treated so far had relief from pruritus just after one cycle.”
Dr. William said he and his colleagues are excited about the overall results they have observed with BV-len, although it’s “still pretty early” in the trial. The investigators are planning to enroll a total of 42 patients and may open the trial at a second center.
The study is sponsored by Ohio State University and the lenalidomide is provided by Celgene. Dr. William reported relationships with miRagen Therapeutics, GuidePoint, Kyowa Kirin, and Celgene.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
REPORTING FROM TCLF 2019
Key clinical point:
Major finding: Five of six evaluable CTCL patients had a 50% or greater reduction in their Skindex-16 scores after two cycles of treatment.
Study details: A phase 2 study with results reported for 10 patients.
Disclosures: The study is sponsored by Ohio State University and the lenalidomide is provided by Celgene. The principal investigator reported relationships with miRagen Therapeutics, GuidePoint, Kyowa Kirin, and Celgene.
Are single agents better than chemo for relapsed/refractory PTCL?
LA JOLLA, CALIF. — Results from the COMPLETE registry suggest newer single agents may be more effective than combination chemotherapy for patients with relapsed/refractory peripheral T-cell lymphoma (PTCL).
Complete response (CR) rates and median survival times were significantly better among patients who received single agents than among those who received combination therapy.
Although researchers don’t know what is driving these differences in outcomes, they did find that outcomes were best among patients who received single-agent brentuximab vedotin (BV), and a disproportionate number of patients received BV.
The researchers also found that patients who received single-agent therapy were more likely to proceed to stem cell transplant.
Therefore, it’s still unclear if single-agent treatment is superior to combination therapy for relapsed/refractory PTCL, according to Robert Stuver, MD, of Beth Israel Deaconess Medical Center in Boston.
Dr. Stuver presented data from the COMPLETE (Comprehensive Oncology Measures for Peripheral T-cell Lymphoma Treatment) registry at the annual T-cell Lymphoma Forum.
The registry (NCT01110733) enrolled patients newly diagnosed with PTCL. Dr. Stuver presented results among patients who had relapsed after, or were refractory to, upfront therapy and went on to receive single-agent therapy or any combination regimen excluding those single agents. Outcome data were collected for 5 years or until death.
Patients and treatment
There were 26 patients in the combination treatment group — 10 with PTCL not otherwise specified (NOS), 6 with angioimmunoblastic T-cell lymphoma (AITL), 5 with natural killer T-cell lymphoma (NKTL), 3 with anaplastic large-cell lymphoma (ALCL), 1 with enteropathy-associated T-cell lymphoma (EATL), and 1 with hepatosplenic T-cell lymphoma (HSTCL).
Patients in the combination group received gemcitabine-based therapy (n = 10), ifosfamide-based therapy (n = 7), platinum-based therapy (n = 4), CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone)-like therapy (n = 1), DHAP (dexamethasone, high-dose cytarabine, and cisplatin; n = 1), and other combinations (n = 3).
There were 31 patients in the single-agent group – 13 with PTCL-NOS, 7 with ALCL, 5 with AITL, 2 with EATL, 2 with NKTL, and 2 with HSTCL.
These patients were treated with BV (n = 12), romidepsin (n = 8), pralatrexate (n = 5), alisertib (n = 3), bendamustine (n = 1), denileukin diftitox (n = 1), and lenalidomide (n = 1).
Response
The CR rates were significantly higher among patients who received single-agent treatment than among those who received combination therapy — 41.4% (12/31) and 19.2% (5/26), respectively (P = .02). The partial response rates were 17.2% (5/31) and 26.9% (7/26), respectively. Rates of stable disease were 3.4% (1/31) and 30.8% (8/26), respectively.
Complete responders in the single-agent arm were treated with BV (n = 7), romidepsin (n = 2), pralatrexate (n = 1), alisertib (n = 1), and bendamustine (n = 1). Four of the patients treated with BV had ALCL.
“We had an enrichment of patients treated with brentuximab,” Dr. Stuver said. “So the obvious question this begs is, ‘Are the favorable results that were seen for single agents over combination therapy solely due to patients treated with brentuximab?’ ”
To investigate, Dr. Stuver and his colleagues compared responses among patients who received BV with patients who received other single agents or combination therapies.
The CR rate was 58.3% (7/12) among BV recipients, 29.4% (5/17) among patients who received other single agents, and 19.2% (5/26) among patients who received combination therapy.
“The takeaway here is that, when you do divide the single-agent group into BV and other single agents, you’re seeing that BV is doing much better than every other group,” Dr. Stuver said. “And all the other single agents are doing somewhat similarly to the combination group, although there’s still a 10% difference, 29% versus 19%.”
Survival
The median progression-free survival (PFS) and overall survival (OS) were significantly better among patients who received single-agent therapy. The median PFS was 11.7 months in the single-agent group and 6.7 months in the combination group (P = .0197). The median OS was 38.9 months and 17.1 months, respectively (P = .0170).
A factor that may have affected survival is that patients were more likely to undergo stem cell transplant after single-agent therapy (25.8%, 8/31), compared with those who had received combination therapy (7.7%, 2/26).
Another factor that may have affected the survival differences is the enrichment of patients treated with BV.
The researchers found the median PFS was 11.9 months among BV recipients, 10.4 months among patients who received other single agents, and 6.7 months in the combination-therapy group. The median OS was 44.5 months, 19.1 months, and 17.1 months, respectively.
Dr. Stuver said these results suggest there is a role for single agents as first retreatment in the salvage setting. However, this analysis was limited by the small sample size and the enrichment of patients treated with BV.
Larger, randomized studies are needed to identify the “truly superior” treatment strategy for relapsed/refractory PTCL, Dr. Stuver said.
The COMPLETE registry is sponsored by Spectrum Pharmaceuticals. Dr. Stuver did not declare any conflicts of interest.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Results from the COMPLETE registry suggest newer single agents may be more effective than combination chemotherapy for patients with relapsed/refractory peripheral T-cell lymphoma (PTCL).
Complete response (CR) rates and median survival times were significantly better among patients who received single agents than among those who received combination therapy.
Although researchers don’t know what is driving these differences in outcomes, they did find that outcomes were best among patients who received single-agent brentuximab vedotin (BV), and a disproportionate number of patients received BV.
The researchers also found that patients who received single-agent therapy were more likely to proceed to stem cell transplant.
Therefore, it’s still unclear if single-agent treatment is superior to combination therapy for relapsed/refractory PTCL, according to Robert Stuver, MD, of Beth Israel Deaconess Medical Center in Boston.
Dr. Stuver presented data from the COMPLETE (Comprehensive Oncology Measures for Peripheral T-cell Lymphoma Treatment) registry at the annual T-cell Lymphoma Forum.
The registry (NCT01110733) enrolled patients newly diagnosed with PTCL. Dr. Stuver presented results among patients who had relapsed after, or were refractory to, upfront therapy and went on to receive single-agent therapy or any combination regimen excluding those single agents. Outcome data were collected for 5 years or until death.
Patients and treatment
There were 26 patients in the combination treatment group — 10 with PTCL not otherwise specified (NOS), 6 with angioimmunoblastic T-cell lymphoma (AITL), 5 with natural killer T-cell lymphoma (NKTL), 3 with anaplastic large-cell lymphoma (ALCL), 1 with enteropathy-associated T-cell lymphoma (EATL), and 1 with hepatosplenic T-cell lymphoma (HSTCL).
Patients in the combination group received gemcitabine-based therapy (n = 10), ifosfamide-based therapy (n = 7), platinum-based therapy (n = 4), CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone)-like therapy (n = 1), DHAP (dexamethasone, high-dose cytarabine, and cisplatin; n = 1), and other combinations (n = 3).
There were 31 patients in the single-agent group – 13 with PTCL-NOS, 7 with ALCL, 5 with AITL, 2 with EATL, 2 with NKTL, and 2 with HSTCL.
These patients were treated with BV (n = 12), romidepsin (n = 8), pralatrexate (n = 5), alisertib (n = 3), bendamustine (n = 1), denileukin diftitox (n = 1), and lenalidomide (n = 1).
Response
The CR rates were significantly higher among patients who received single-agent treatment than among those who received combination therapy — 41.4% (12/31) and 19.2% (5/26), respectively (P = .02). The partial response rates were 17.2% (5/31) and 26.9% (7/26), respectively. Rates of stable disease were 3.4% (1/31) and 30.8% (8/26), respectively.
Complete responders in the single-agent arm were treated with BV (n = 7), romidepsin (n = 2), pralatrexate (n = 1), alisertib (n = 1), and bendamustine (n = 1). Four of the patients treated with BV had ALCL.
“We had an enrichment of patients treated with brentuximab,” Dr. Stuver said. “So the obvious question this begs is, ‘Are the favorable results that were seen for single agents over combination therapy solely due to patients treated with brentuximab?’ ”
To investigate, Dr. Stuver and his colleagues compared responses among patients who received BV with patients who received other single agents or combination therapies.
The CR rate was 58.3% (7/12) among BV recipients, 29.4% (5/17) among patients who received other single agents, and 19.2% (5/26) among patients who received combination therapy.
“The takeaway here is that, when you do divide the single-agent group into BV and other single agents, you’re seeing that BV is doing much better than every other group,” Dr. Stuver said. “And all the other single agents are doing somewhat similarly to the combination group, although there’s still a 10% difference, 29% versus 19%.”
Survival
The median progression-free survival (PFS) and overall survival (OS) were significantly better among patients who received single-agent therapy. The median PFS was 11.7 months in the single-agent group and 6.7 months in the combination group (P = .0197). The median OS was 38.9 months and 17.1 months, respectively (P = .0170).
A factor that may have affected survival is that patients were more likely to undergo stem cell transplant after single-agent therapy (25.8%, 8/31), compared with those who had received combination therapy (7.7%, 2/26).
Another factor that may have affected the survival differences is the enrichment of patients treated with BV.
The researchers found the median PFS was 11.9 months among BV recipients, 10.4 months among patients who received other single agents, and 6.7 months in the combination-therapy group. The median OS was 44.5 months, 19.1 months, and 17.1 months, respectively.
Dr. Stuver said these results suggest there is a role for single agents as first retreatment in the salvage setting. However, this analysis was limited by the small sample size and the enrichment of patients treated with BV.
Larger, randomized studies are needed to identify the “truly superior” treatment strategy for relapsed/refractory PTCL, Dr. Stuver said.
The COMPLETE registry is sponsored by Spectrum Pharmaceuticals. Dr. Stuver did not declare any conflicts of interest.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Results from the COMPLETE registry suggest newer single agents may be more effective than combination chemotherapy for patients with relapsed/refractory peripheral T-cell lymphoma (PTCL).
Complete response (CR) rates and median survival times were significantly better among patients who received single agents than among those who received combination therapy.
Although researchers don’t know what is driving these differences in outcomes, they did find that outcomes were best among patients who received single-agent brentuximab vedotin (BV), and a disproportionate number of patients received BV.
The researchers also found that patients who received single-agent therapy were more likely to proceed to stem cell transplant.
Therefore, it’s still unclear if single-agent treatment is superior to combination therapy for relapsed/refractory PTCL, according to Robert Stuver, MD, of Beth Israel Deaconess Medical Center in Boston.
Dr. Stuver presented data from the COMPLETE (Comprehensive Oncology Measures for Peripheral T-cell Lymphoma Treatment) registry at the annual T-cell Lymphoma Forum.
The registry (NCT01110733) enrolled patients newly diagnosed with PTCL. Dr. Stuver presented results among patients who had relapsed after, or were refractory to, upfront therapy and went on to receive single-agent therapy or any combination regimen excluding those single agents. Outcome data were collected for 5 years or until death.
Patients and treatment
There were 26 patients in the combination treatment group — 10 with PTCL not otherwise specified (NOS), 6 with angioimmunoblastic T-cell lymphoma (AITL), 5 with natural killer T-cell lymphoma (NKTL), 3 with anaplastic large-cell lymphoma (ALCL), 1 with enteropathy-associated T-cell lymphoma (EATL), and 1 with hepatosplenic T-cell lymphoma (HSTCL).
Patients in the combination group received gemcitabine-based therapy (n = 10), ifosfamide-based therapy (n = 7), platinum-based therapy (n = 4), CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone)-like therapy (n = 1), DHAP (dexamethasone, high-dose cytarabine, and cisplatin; n = 1), and other combinations (n = 3).
There were 31 patients in the single-agent group – 13 with PTCL-NOS, 7 with ALCL, 5 with AITL, 2 with EATL, 2 with NKTL, and 2 with HSTCL.
These patients were treated with BV (n = 12), romidepsin (n = 8), pralatrexate (n = 5), alisertib (n = 3), bendamustine (n = 1), denileukin diftitox (n = 1), and lenalidomide (n = 1).
Response
The CR rates were significantly higher among patients who received single-agent treatment than among those who received combination therapy — 41.4% (12/31) and 19.2% (5/26), respectively (P = .02). The partial response rates were 17.2% (5/31) and 26.9% (7/26), respectively. Rates of stable disease were 3.4% (1/31) and 30.8% (8/26), respectively.
Complete responders in the single-agent arm were treated with BV (n = 7), romidepsin (n = 2), pralatrexate (n = 1), alisertib (n = 1), and bendamustine (n = 1). Four of the patients treated with BV had ALCL.
“We had an enrichment of patients treated with brentuximab,” Dr. Stuver said. “So the obvious question this begs is, ‘Are the favorable results that were seen for single agents over combination therapy solely due to patients treated with brentuximab?’ ”
To investigate, Dr. Stuver and his colleagues compared responses among patients who received BV with patients who received other single agents or combination therapies.
The CR rate was 58.3% (7/12) among BV recipients, 29.4% (5/17) among patients who received other single agents, and 19.2% (5/26) among patients who received combination therapy.
“The takeaway here is that, when you do divide the single-agent group into BV and other single agents, you’re seeing that BV is doing much better than every other group,” Dr. Stuver said. “And all the other single agents are doing somewhat similarly to the combination group, although there’s still a 10% difference, 29% versus 19%.”
Survival
The median progression-free survival (PFS) and overall survival (OS) were significantly better among patients who received single-agent therapy. The median PFS was 11.7 months in the single-agent group and 6.7 months in the combination group (P = .0197). The median OS was 38.9 months and 17.1 months, respectively (P = .0170).
A factor that may have affected survival is that patients were more likely to undergo stem cell transplant after single-agent therapy (25.8%, 8/31), compared with those who had received combination therapy (7.7%, 2/26).
Another factor that may have affected the survival differences is the enrichment of patients treated with BV.
The researchers found the median PFS was 11.9 months among BV recipients, 10.4 months among patients who received other single agents, and 6.7 months in the combination-therapy group. The median OS was 44.5 months, 19.1 months, and 17.1 months, respectively.
Dr. Stuver said these results suggest there is a role for single agents as first retreatment in the salvage setting. However, this analysis was limited by the small sample size and the enrichment of patients treated with BV.
Larger, randomized studies are needed to identify the “truly superior” treatment strategy for relapsed/refractory PTCL, Dr. Stuver said.
The COMPLETE registry is sponsored by Spectrum Pharmaceuticals. Dr. Stuver did not declare any conflicts of interest.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
REPORTING FROM TCLF 2019
Key clinical point:
Major finding: The complete response rate was significantly higher among patients who received single-agent treatment than it was among those who received combination therapy – 41.4% and 19.2%, respectively (P = .02).
Study details: Analysis of 57 patients with relapsed/refractory PTCL in the COMPLETE registry.
Disclosures: The COMPLETE registry is sponsored by Spectrum Pharmaceuticals. Dr. Stuver did not declare any conflicts of interest.
Four-drug combo shows durable responses in relapsed/refractory lymphomas
LA JOLLA, CALIF. — Results of a phase 1 trial suggest a four-drug combination can produce durable responses in patients with relapsed or refractory T- and B-cell lymphomas.
Seven of 15 patients responded to treatment with romidepsin, gemcitabine, oxaliplatin, and dexamethasone, including six patients who achieved a complete response (CR).
The median duration of response was 8.5 months, and three patients had responses lasting more than 24 months.
Patients with angioimmunoblastic T-cell lymphoma (AITL) in particular responded well to the combination.
Neha Mehta-Shah, MD, of Washington University in St. Louis, and her colleagues presented these results in a poster at the annual T-cell Lymphoma Forum.
“[I]t was thought that the addition of histone deacetylase inhibitors to traditional platinum-based chemotherapies, which tend to cause DNA damage, would increase the response of platinum-based therapies,” Dr. Shah said.
With that in mind, she and her colleagues added romidepsin to gemcitabine, oxaliplatin, and dexamethasone and evaluated this combination in patients with relapsed/refractory lymphomas.
The trial (NCT02181218) enrolled 15 patients — 6 with peripheral T-cell lymphoma not otherwise specified (PTCL-NOS), 6 with diffuse large B-cell lymphoma (DLBCL), and 3 with AITL.
The patients’ median age was 66 (range, 55-83), and they had received a median of 2 (range, 1-4) prior therapies.
The researchers tested three dose levels of romidepsin — 8 mg/m2, 10 mg/m2, and 12 mg/m2 — given on day 2 of a 21-day cycle. The study originally included romidepsin on day 8 as well. However, the researchers discontinued the day 8 dose after patients developed grade 4 thrombocytopenia.
Patients also received gemcitabine at 1,000 mg/m2 (day 1), oxaliplatin at 100 mg/m2 (day 1), and dexamethasone at 20 mg (days 1-4). All patients received pegfilgrastim at 6 mg (day 3) as well.
The patients could receive up to eight cycles of treatment if they had stable disease or better and did not experience significant toxicity.
Safety
There was one dose-limiting toxicity (DLT) — pneumonia — at the 8 mg/m2 dose of romidepsin (given on days 2 and 8). There was one DLT — bleeding — at the 10 mg/m2 dose (day 2 only).
Two patients experienced DLTs — neutropenic fever and grade 4 thrombocytopenia — at the 12 mg/m2 dose (day 2 only).
Based on these events, 10 mg/m2 was considered the maximum-tolerated dose of romidepsin.
The most common adverse events (AEs) in this trial were thrombocytopenia (n = 13), electrolyte abnormalities (n = 12), liver function abnormalities (n = 10), anemia (n = 9), neutropenia (n = 8), fatigue (n = 7), nausea (n = 7), and creatinine increase (n = 5).
Grade 3/4 AEs included thrombocytopenia (n = 13), neutropenia (n = 5), anemia (n = 3), hyperglycemia (n = 2), hyperuricemia (n = 2), febrile neutropenia (n = 1), tumor lysis syndrome (n = 1), vomiting (n = 1), peripheral sensory neuropathy (n = 1), pneumonia (n = 1), sepsis (n = 1), bleeding (n = 1), and elevated troponin (n = 1).
Serious AEs requiring hospitalization included pneumonia (n = 1), nausea and vomiting (n = 1), tumor lysis syndrome (n = 1), and complications of disease progression (n = 4).
Efficacy
The overall response rate was 47% (7/15). CRs occurred in all three patients with AITL and two patients with DLBCL. One patient with PTCL-NOS had a CR, and one had a partial response.
The median duration of response was 8.5 months (range, 1.2-36.6 months). Four patients remain in CR — two with AITL, one with PTCL-NOS, and one with DLBCL.
Dr. Shah noted that the CRs in the AITL patients “have been quite prolonged.” One patient had a CR lasting 27 months, and another had a CR lasting 29 months.
Dr. Shah said these results are particularly exciting because patients discontinued study treatment after eight cycles or two cycles after they achieved a CR.
“[S]ome of these patients remained in remission for 2 years without any therapy thereafter, which is quite impressive in a population where the median survival — for patients with relapsed/refractory AITL — is thought to be 6-10 months,” Dr. Shah said.
She noted that this study is ongoing with an expansion cohort of patients with T-cell lymphomas.
This research was supported by Celgene. Dr. Shah reported relationships with Celgene, Kyowa Kirin, Bristol-Myers Squibb, Verastem, and Genentech.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Results of a phase 1 trial suggest a four-drug combination can produce durable responses in patients with relapsed or refractory T- and B-cell lymphomas.
Seven of 15 patients responded to treatment with romidepsin, gemcitabine, oxaliplatin, and dexamethasone, including six patients who achieved a complete response (CR).
The median duration of response was 8.5 months, and three patients had responses lasting more than 24 months.
Patients with angioimmunoblastic T-cell lymphoma (AITL) in particular responded well to the combination.
Neha Mehta-Shah, MD, of Washington University in St. Louis, and her colleagues presented these results in a poster at the annual T-cell Lymphoma Forum.
“[I]t was thought that the addition of histone deacetylase inhibitors to traditional platinum-based chemotherapies, which tend to cause DNA damage, would increase the response of platinum-based therapies,” Dr. Shah said.
With that in mind, she and her colleagues added romidepsin to gemcitabine, oxaliplatin, and dexamethasone and evaluated this combination in patients with relapsed/refractory lymphomas.
The trial (NCT02181218) enrolled 15 patients — 6 with peripheral T-cell lymphoma not otherwise specified (PTCL-NOS), 6 with diffuse large B-cell lymphoma (DLBCL), and 3 with AITL.
The patients’ median age was 66 (range, 55-83), and they had received a median of 2 (range, 1-4) prior therapies.
The researchers tested three dose levels of romidepsin — 8 mg/m2, 10 mg/m2, and 12 mg/m2 — given on day 2 of a 21-day cycle. The study originally included romidepsin on day 8 as well. However, the researchers discontinued the day 8 dose after patients developed grade 4 thrombocytopenia.
Patients also received gemcitabine at 1,000 mg/m2 (day 1), oxaliplatin at 100 mg/m2 (day 1), and dexamethasone at 20 mg (days 1-4). All patients received pegfilgrastim at 6 mg (day 3) as well.
The patients could receive up to eight cycles of treatment if they had stable disease or better and did not experience significant toxicity.
Safety
There was one dose-limiting toxicity (DLT) — pneumonia — at the 8 mg/m2 dose of romidepsin (given on days 2 and 8). There was one DLT — bleeding — at the 10 mg/m2 dose (day 2 only).
Two patients experienced DLTs — neutropenic fever and grade 4 thrombocytopenia — at the 12 mg/m2 dose (day 2 only).
Based on these events, 10 mg/m2 was considered the maximum-tolerated dose of romidepsin.
The most common adverse events (AEs) in this trial were thrombocytopenia (n = 13), electrolyte abnormalities (n = 12), liver function abnormalities (n = 10), anemia (n = 9), neutropenia (n = 8), fatigue (n = 7), nausea (n = 7), and creatinine increase (n = 5).
Grade 3/4 AEs included thrombocytopenia (n = 13), neutropenia (n = 5), anemia (n = 3), hyperglycemia (n = 2), hyperuricemia (n = 2), febrile neutropenia (n = 1), tumor lysis syndrome (n = 1), vomiting (n = 1), peripheral sensory neuropathy (n = 1), pneumonia (n = 1), sepsis (n = 1), bleeding (n = 1), and elevated troponin (n = 1).
Serious AEs requiring hospitalization included pneumonia (n = 1), nausea and vomiting (n = 1), tumor lysis syndrome (n = 1), and complications of disease progression (n = 4).
Efficacy
The overall response rate was 47% (7/15). CRs occurred in all three patients with AITL and two patients with DLBCL. One patient with PTCL-NOS had a CR, and one had a partial response.
The median duration of response was 8.5 months (range, 1.2-36.6 months). Four patients remain in CR — two with AITL, one with PTCL-NOS, and one with DLBCL.
Dr. Shah noted that the CRs in the AITL patients “have been quite prolonged.” One patient had a CR lasting 27 months, and another had a CR lasting 29 months.
Dr. Shah said these results are particularly exciting because patients discontinued study treatment after eight cycles or two cycles after they achieved a CR.
“[S]ome of these patients remained in remission for 2 years without any therapy thereafter, which is quite impressive in a population where the median survival — for patients with relapsed/refractory AITL — is thought to be 6-10 months,” Dr. Shah said.
She noted that this study is ongoing with an expansion cohort of patients with T-cell lymphomas.
This research was supported by Celgene. Dr. Shah reported relationships with Celgene, Kyowa Kirin, Bristol-Myers Squibb, Verastem, and Genentech.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Results of a phase 1 trial suggest a four-drug combination can produce durable responses in patients with relapsed or refractory T- and B-cell lymphomas.
Seven of 15 patients responded to treatment with romidepsin, gemcitabine, oxaliplatin, and dexamethasone, including six patients who achieved a complete response (CR).
The median duration of response was 8.5 months, and three patients had responses lasting more than 24 months.
Patients with angioimmunoblastic T-cell lymphoma (AITL) in particular responded well to the combination.
Neha Mehta-Shah, MD, of Washington University in St. Louis, and her colleagues presented these results in a poster at the annual T-cell Lymphoma Forum.
“[I]t was thought that the addition of histone deacetylase inhibitors to traditional platinum-based chemotherapies, which tend to cause DNA damage, would increase the response of platinum-based therapies,” Dr. Shah said.
With that in mind, she and her colleagues added romidepsin to gemcitabine, oxaliplatin, and dexamethasone and evaluated this combination in patients with relapsed/refractory lymphomas.
The trial (NCT02181218) enrolled 15 patients — 6 with peripheral T-cell lymphoma not otherwise specified (PTCL-NOS), 6 with diffuse large B-cell lymphoma (DLBCL), and 3 with AITL.
The patients’ median age was 66 (range, 55-83), and they had received a median of 2 (range, 1-4) prior therapies.
The researchers tested three dose levels of romidepsin — 8 mg/m2, 10 mg/m2, and 12 mg/m2 — given on day 2 of a 21-day cycle. The study originally included romidepsin on day 8 as well. However, the researchers discontinued the day 8 dose after patients developed grade 4 thrombocytopenia.
Patients also received gemcitabine at 1,000 mg/m2 (day 1), oxaliplatin at 100 mg/m2 (day 1), and dexamethasone at 20 mg (days 1-4). All patients received pegfilgrastim at 6 mg (day 3) as well.
The patients could receive up to eight cycles of treatment if they had stable disease or better and did not experience significant toxicity.
Safety
There was one dose-limiting toxicity (DLT) — pneumonia — at the 8 mg/m2 dose of romidepsin (given on days 2 and 8). There was one DLT — bleeding — at the 10 mg/m2 dose (day 2 only).
Two patients experienced DLTs — neutropenic fever and grade 4 thrombocytopenia — at the 12 mg/m2 dose (day 2 only).
Based on these events, 10 mg/m2 was considered the maximum-tolerated dose of romidepsin.
The most common adverse events (AEs) in this trial were thrombocytopenia (n = 13), electrolyte abnormalities (n = 12), liver function abnormalities (n = 10), anemia (n = 9), neutropenia (n = 8), fatigue (n = 7), nausea (n = 7), and creatinine increase (n = 5).
Grade 3/4 AEs included thrombocytopenia (n = 13), neutropenia (n = 5), anemia (n = 3), hyperglycemia (n = 2), hyperuricemia (n = 2), febrile neutropenia (n = 1), tumor lysis syndrome (n = 1), vomiting (n = 1), peripheral sensory neuropathy (n = 1), pneumonia (n = 1), sepsis (n = 1), bleeding (n = 1), and elevated troponin (n = 1).
Serious AEs requiring hospitalization included pneumonia (n = 1), nausea and vomiting (n = 1), tumor lysis syndrome (n = 1), and complications of disease progression (n = 4).
Efficacy
The overall response rate was 47% (7/15). CRs occurred in all three patients with AITL and two patients with DLBCL. One patient with PTCL-NOS had a CR, and one had a partial response.
The median duration of response was 8.5 months (range, 1.2-36.6 months). Four patients remain in CR — two with AITL, one with PTCL-NOS, and one with DLBCL.
Dr. Shah noted that the CRs in the AITL patients “have been quite prolonged.” One patient had a CR lasting 27 months, and another had a CR lasting 29 months.
Dr. Shah said these results are particularly exciting because patients discontinued study treatment after eight cycles or two cycles after they achieved a CR.
“[S]ome of these patients remained in remission for 2 years without any therapy thereafter, which is quite impressive in a population where the median survival — for patients with relapsed/refractory AITL — is thought to be 6-10 months,” Dr. Shah said.
She noted that this study is ongoing with an expansion cohort of patients with T-cell lymphomas.
This research was supported by Celgene. Dr. Shah reported relationships with Celgene, Kyowa Kirin, Bristol-Myers Squibb, Verastem, and Genentech.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
REPORTING FROM TCLF 2019
Key clinical point:
Major finding: Seven patients responded, and three patients had responses lasting more than 24 months.
Study details: Phase 1 trial of 15 patients.
Disclosures: This research was supported by Celgene. The presenter reported relationships with Celgene, Kyowa Kirin, Bristol-Myers Squibb, Verastem, and Genentech.
FDA approves third trastuzumab biosimilar
The Food and Drug Administration .
Ontruzant (trastuzumab-dttb), marketed by Samsung Bioepis, is the third approved biosimilar to Genentech’s Herceptin in the United States.
Patients should be selected for treatment with Ontruzant using an FDA-approved companion diagnostic for a trastuzumab product.
The prescribing information for the newly approved biosimilar includes a boxed warning highlighting the risk of cardiomyopathy, infusion reactions, embryo-fetal toxicity, and pulmonary toxicity associated with the drug.
Ontruzant was shown to be equivalent to Herceptin in a phase 3 study (Eur J Cancer. 2018 Apr;93:19-27).
The trial included 875 patients with HER2-positive early breast cancer. Patients were randomized to receive Ontruzant or Herceptin for eight cycles concurrently with chemotherapy. The chemotherapy consisted of four cycles of docetaxel followed by four cycles of 5-fluorouracil/epirubicin/cyclophosphamide.
The patients then underwent surgery, which was followed by 10 cycles of Ontruzant (n=380) or Herceptin (n=384).
The median follow-up was 437 days in the Ontruzant arm and 438 days in the Herceptin arm. Safety and efficacy results were similar between the treatment arms.
Treatment-emergent adverse events occurred in 97.5% of patients in the Ontruzant arm and 96.1% of those in the Herceptin arm.
The 12-month event-free survival rate was 93.7% in the Ontruzant arm and 93.4% in the Herceptin arm.
The Food and Drug Administration .
Ontruzant (trastuzumab-dttb), marketed by Samsung Bioepis, is the third approved biosimilar to Genentech’s Herceptin in the United States.
Patients should be selected for treatment with Ontruzant using an FDA-approved companion diagnostic for a trastuzumab product.
The prescribing information for the newly approved biosimilar includes a boxed warning highlighting the risk of cardiomyopathy, infusion reactions, embryo-fetal toxicity, and pulmonary toxicity associated with the drug.
Ontruzant was shown to be equivalent to Herceptin in a phase 3 study (Eur J Cancer. 2018 Apr;93:19-27).
The trial included 875 patients with HER2-positive early breast cancer. Patients were randomized to receive Ontruzant or Herceptin for eight cycles concurrently with chemotherapy. The chemotherapy consisted of four cycles of docetaxel followed by four cycles of 5-fluorouracil/epirubicin/cyclophosphamide.
The patients then underwent surgery, which was followed by 10 cycles of Ontruzant (n=380) or Herceptin (n=384).
The median follow-up was 437 days in the Ontruzant arm and 438 days in the Herceptin arm. Safety and efficacy results were similar between the treatment arms.
Treatment-emergent adverse events occurred in 97.5% of patients in the Ontruzant arm and 96.1% of those in the Herceptin arm.
The 12-month event-free survival rate was 93.7% in the Ontruzant arm and 93.4% in the Herceptin arm.
The Food and Drug Administration .
Ontruzant (trastuzumab-dttb), marketed by Samsung Bioepis, is the third approved biosimilar to Genentech’s Herceptin in the United States.
Patients should be selected for treatment with Ontruzant using an FDA-approved companion diagnostic for a trastuzumab product.
The prescribing information for the newly approved biosimilar includes a boxed warning highlighting the risk of cardiomyopathy, infusion reactions, embryo-fetal toxicity, and pulmonary toxicity associated with the drug.
Ontruzant was shown to be equivalent to Herceptin in a phase 3 study (Eur J Cancer. 2018 Apr;93:19-27).
The trial included 875 patients with HER2-positive early breast cancer. Patients were randomized to receive Ontruzant or Herceptin for eight cycles concurrently with chemotherapy. The chemotherapy consisted of four cycles of docetaxel followed by four cycles of 5-fluorouracil/epirubicin/cyclophosphamide.
The patients then underwent surgery, which was followed by 10 cycles of Ontruzant (n=380) or Herceptin (n=384).
The median follow-up was 437 days in the Ontruzant arm and 438 days in the Herceptin arm. Safety and efficacy results were similar between the treatment arms.
Treatment-emergent adverse events occurred in 97.5% of patients in the Ontruzant arm and 96.1% of those in the Herceptin arm.
The 12-month event-free survival rate was 93.7% in the Ontruzant arm and 93.4% in the Herceptin arm.
Long-term mogamulizumab appears safe, effective in CTCL
LA JOLLA, CALIF. — Prolonged exposure to mogamulizumab can improve responses without compromising safety in patients with cutaneous T-cell lymphoma (CTCL), according to a post hoc analysis of the MAVORIC trial.
Investigators found that exposure to mogamulizumab correlated with response. The highest response rate — 75.6% — was observed in patients exposed to the drug for at least 351 days, and the lowest — 1.9% — was observed in patients exposed to mogamulizumab for less than 72 days.
On the other hand, rates of adverse events (AEs) were similar regardless of how long patients were treated with mogamulizumab.
Youn H. Kim, MD, of Stanford Cancer Institute at Stanford (Calif.) University, and her colleagues presented these findings at the annual T-cell Lymphoma Forum.
The phase 3 MAVORIC trial (NCT01728805) included 372 adults with CTCL who had failed at least one systemic therapy. The patients were randomized to treatment with mogamulizumab or vorinostat.
Results from this comparison were previously reported at the 10th annual T-cell Lymphoma Forum.
At this year’s meeting, Dr. Kim and her colleagues reported results in 184 patients who were randomized to mogamulizumab — 105 of whom had mycosis fungoides (MF) and 79 of whom had Sézary syndrome (SS).
Patients were exposed to mogamulizumab for a mean of 275.2 days and a median of 170.0 days (range, 1-1,617 days).
The investigators divided patients into the following quartiles according to mogamulizumab exposure:
- Less than 72 days — 52 patients (28%)
- 72-170 days — 40 patients (22%)
- 171-351 days — 47 patients (26%)
- More than 351 days — 45 patients (24%).
Patients exposed to mogamulizumab for longer were more likely to have SS, stage III/IV disease, blood involvement, and a performance status of 0.
Dr. Kim said the SS patients “benefited a lot” from mogamulizumab and therefore remained on treatment longer.
Response
As expected, patients exposed to mogamulizumab for the longest period had the highest global response rates. Confirmed response rates according to drug exposure were as follows:
- Less than 72 days: 1.9% overall, 0% for SS, and 2.9% for MF
- 72-170 days: 10% overall, 18.8% for SS, and 4.2% for MF
- 171-351 days: 29.8% overall, 36.4% for SS, and 24% for MF
- More than 351 days: 75.6% overall, 83.3% for SS, and 66.7% for MF.
In addition, rates of complete response (CR) and partial response (PR) tended to increase with mogamulizumab exposure. Rates of CR, PR, and stable disease (SD) according to exposure time were as follows:
- Less than 72 days: 0% CR, 7.7% PR, and 38.5% SD
- 72-170 days: 2.5% CR, 20% PR, and 62.5% SD
- 171-351 days: 2.1% CR, 34% PR, and 57.4% SD
- More than 351 days: 6.7% CR, 71.1% PR, and 17.8% SD.
Safety
“The percentage of patients reporting adverse events was not different in the long-term treatment-exposure patients, compared to the short-term,” Dr. Kim said.
Percentages of treatment-emergent AEs (TEAEs) and serious AEs (SAEs) according to mogamulizumab exposure were as follows:
- Less than 72 days: 26.6% TEAEs and 6.5% SAEs
- 72-170 days: 18.5% TEAEs and 3.3% SAEs
- 171-351 days: 23.4% TEAEs and 6.0% SAEs
- More than 351 days: 21.7% TEAEs and 4.3% SAEs.
“The majority of the grade 3 events occurred in the first two quartiles, not later, which is important to show,” Dr. Kim said.
Most grade 3 AEs occurred within 170 days of treatment initiation, and the median time to a grade 3 or higher AE was 109 days.
The most common treatment-related AEs in the longest exposure cohort were drug eruption (20.0%), thrombocytopenia (11.1%), stomatitis (8.9%), and anemia (8.9%).
Of all patients in this analysis, 45 experienced drug eruption, which was defined as a skin rash possibly, probably, or definitely related to the study drug.
Nine drug eruption events were grade 3, and the rest were grade 1 or 2. The median time to drug eruption was 107 days.
While drug eruption “didn’t show up early,” there is no cumulative risk with longer exposure to mogamulizumab, Dr. Kim said. Likewise, she said, autoimmune AEs were not dose-cumulative events.
There were two patients with definite autoimmune disease — a 65-year-old man with Miller Fisher syndrome (occurring 199 days after mogamulizumab initiation) and a 40-year-old woman with myositis (151 days) and myocarditis (310 days).
The investigators also identified three patients with possible autoimmune disease, including:
- Pneumonitis (310 days) in a 74-year-old woman
- Polymyalgia rheumatica (209 days) and myopathy (not available) in an 84-year-old man
- Hepatitis (144 days), pneumonitis (about 174 days), and polymyositis (about 174 days) in a 73-year-old man.
Dr. Kim and her colleagues said these data suggest prolonged treatment with mogamulizumab is not associated with an increased safety risk in patients with MF or SS. And the manageable safety profile of mogamulizumab meant that patients who derived a clinical benefit could remain on the drug for an extended period of time.
The MAVORIC trial was sponsored by Kyowa Hakko Kirin Pharma. Dr. Kim reported relationships with Merck, Portola Pharmaceuticals, Soligenix, Takeda, TetraLogic Pharmaceuticals, Kyowa Kirin, Seattle Genetics, Medivir, Neumedicines, Eisai, Innate Pharma, Galderma, Miragen Therapeutics, Forty Seven, and Horizon Pharma. Her coinvestigators reported relationships with several companies.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Prolonged exposure to mogamulizumab can improve responses without compromising safety in patients with cutaneous T-cell lymphoma (CTCL), according to a post hoc analysis of the MAVORIC trial.
Investigators found that exposure to mogamulizumab correlated with response. The highest response rate — 75.6% — was observed in patients exposed to the drug for at least 351 days, and the lowest — 1.9% — was observed in patients exposed to mogamulizumab for less than 72 days.
On the other hand, rates of adverse events (AEs) were similar regardless of how long patients were treated with mogamulizumab.
Youn H. Kim, MD, of Stanford Cancer Institute at Stanford (Calif.) University, and her colleagues presented these findings at the annual T-cell Lymphoma Forum.
The phase 3 MAVORIC trial (NCT01728805) included 372 adults with CTCL who had failed at least one systemic therapy. The patients were randomized to treatment with mogamulizumab or vorinostat.
Results from this comparison were previously reported at the 10th annual T-cell Lymphoma Forum.
At this year’s meeting, Dr. Kim and her colleagues reported results in 184 patients who were randomized to mogamulizumab — 105 of whom had mycosis fungoides (MF) and 79 of whom had Sézary syndrome (SS).
Patients were exposed to mogamulizumab for a mean of 275.2 days and a median of 170.0 days (range, 1-1,617 days).
The investigators divided patients into the following quartiles according to mogamulizumab exposure:
- Less than 72 days — 52 patients (28%)
- 72-170 days — 40 patients (22%)
- 171-351 days — 47 patients (26%)
- More than 351 days — 45 patients (24%).
Patients exposed to mogamulizumab for longer were more likely to have SS, stage III/IV disease, blood involvement, and a performance status of 0.
Dr. Kim said the SS patients “benefited a lot” from mogamulizumab and therefore remained on treatment longer.
Response
As expected, patients exposed to mogamulizumab for the longest period had the highest global response rates. Confirmed response rates according to drug exposure were as follows:
- Less than 72 days: 1.9% overall, 0% for SS, and 2.9% for MF
- 72-170 days: 10% overall, 18.8% for SS, and 4.2% for MF
- 171-351 days: 29.8% overall, 36.4% for SS, and 24% for MF
- More than 351 days: 75.6% overall, 83.3% for SS, and 66.7% for MF.
In addition, rates of complete response (CR) and partial response (PR) tended to increase with mogamulizumab exposure. Rates of CR, PR, and stable disease (SD) according to exposure time were as follows:
- Less than 72 days: 0% CR, 7.7% PR, and 38.5% SD
- 72-170 days: 2.5% CR, 20% PR, and 62.5% SD
- 171-351 days: 2.1% CR, 34% PR, and 57.4% SD
- More than 351 days: 6.7% CR, 71.1% PR, and 17.8% SD.
Safety
“The percentage of patients reporting adverse events was not different in the long-term treatment-exposure patients, compared to the short-term,” Dr. Kim said.
Percentages of treatment-emergent AEs (TEAEs) and serious AEs (SAEs) according to mogamulizumab exposure were as follows:
- Less than 72 days: 26.6% TEAEs and 6.5% SAEs
- 72-170 days: 18.5% TEAEs and 3.3% SAEs
- 171-351 days: 23.4% TEAEs and 6.0% SAEs
- More than 351 days: 21.7% TEAEs and 4.3% SAEs.
“The majority of the grade 3 events occurred in the first two quartiles, not later, which is important to show,” Dr. Kim said.
Most grade 3 AEs occurred within 170 days of treatment initiation, and the median time to a grade 3 or higher AE was 109 days.
The most common treatment-related AEs in the longest exposure cohort were drug eruption (20.0%), thrombocytopenia (11.1%), stomatitis (8.9%), and anemia (8.9%).
Of all patients in this analysis, 45 experienced drug eruption, which was defined as a skin rash possibly, probably, or definitely related to the study drug.
Nine drug eruption events were grade 3, and the rest were grade 1 or 2. The median time to drug eruption was 107 days.
While drug eruption “didn’t show up early,” there is no cumulative risk with longer exposure to mogamulizumab, Dr. Kim said. Likewise, she said, autoimmune AEs were not dose-cumulative events.
There were two patients with definite autoimmune disease — a 65-year-old man with Miller Fisher syndrome (occurring 199 days after mogamulizumab initiation) and a 40-year-old woman with myositis (151 days) and myocarditis (310 days).
The investigators also identified three patients with possible autoimmune disease, including:
- Pneumonitis (310 days) in a 74-year-old woman
- Polymyalgia rheumatica (209 days) and myopathy (not available) in an 84-year-old man
- Hepatitis (144 days), pneumonitis (about 174 days), and polymyositis (about 174 days) in a 73-year-old man.
Dr. Kim and her colleagues said these data suggest prolonged treatment with mogamulizumab is not associated with an increased safety risk in patients with MF or SS. And the manageable safety profile of mogamulizumab meant that patients who derived a clinical benefit could remain on the drug for an extended period of time.
The MAVORIC trial was sponsored by Kyowa Hakko Kirin Pharma. Dr. Kim reported relationships with Merck, Portola Pharmaceuticals, Soligenix, Takeda, TetraLogic Pharmaceuticals, Kyowa Kirin, Seattle Genetics, Medivir, Neumedicines, Eisai, Innate Pharma, Galderma, Miragen Therapeutics, Forty Seven, and Horizon Pharma. Her coinvestigators reported relationships with several companies.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Prolonged exposure to mogamulizumab can improve responses without compromising safety in patients with cutaneous T-cell lymphoma (CTCL), according to a post hoc analysis of the MAVORIC trial.
Investigators found that exposure to mogamulizumab correlated with response. The highest response rate — 75.6% — was observed in patients exposed to the drug for at least 351 days, and the lowest — 1.9% — was observed in patients exposed to mogamulizumab for less than 72 days.
On the other hand, rates of adverse events (AEs) were similar regardless of how long patients were treated with mogamulizumab.
Youn H. Kim, MD, of Stanford Cancer Institute at Stanford (Calif.) University, and her colleagues presented these findings at the annual T-cell Lymphoma Forum.
The phase 3 MAVORIC trial (NCT01728805) included 372 adults with CTCL who had failed at least one systemic therapy. The patients were randomized to treatment with mogamulizumab or vorinostat.
Results from this comparison were previously reported at the 10th annual T-cell Lymphoma Forum.
At this year’s meeting, Dr. Kim and her colleagues reported results in 184 patients who were randomized to mogamulizumab — 105 of whom had mycosis fungoides (MF) and 79 of whom had Sézary syndrome (SS).
Patients were exposed to mogamulizumab for a mean of 275.2 days and a median of 170.0 days (range, 1-1,617 days).
The investigators divided patients into the following quartiles according to mogamulizumab exposure:
- Less than 72 days — 52 patients (28%)
- 72-170 days — 40 patients (22%)
- 171-351 days — 47 patients (26%)
- More than 351 days — 45 patients (24%).
Patients exposed to mogamulizumab for longer were more likely to have SS, stage III/IV disease, blood involvement, and a performance status of 0.
Dr. Kim said the SS patients “benefited a lot” from mogamulizumab and therefore remained on treatment longer.
Response
As expected, patients exposed to mogamulizumab for the longest period had the highest global response rates. Confirmed response rates according to drug exposure were as follows:
- Less than 72 days: 1.9% overall, 0% for SS, and 2.9% for MF
- 72-170 days: 10% overall, 18.8% for SS, and 4.2% for MF
- 171-351 days: 29.8% overall, 36.4% for SS, and 24% for MF
- More than 351 days: 75.6% overall, 83.3% for SS, and 66.7% for MF.
In addition, rates of complete response (CR) and partial response (PR) tended to increase with mogamulizumab exposure. Rates of CR, PR, and stable disease (SD) according to exposure time were as follows:
- Less than 72 days: 0% CR, 7.7% PR, and 38.5% SD
- 72-170 days: 2.5% CR, 20% PR, and 62.5% SD
- 171-351 days: 2.1% CR, 34% PR, and 57.4% SD
- More than 351 days: 6.7% CR, 71.1% PR, and 17.8% SD.
Safety
“The percentage of patients reporting adverse events was not different in the long-term treatment-exposure patients, compared to the short-term,” Dr. Kim said.
Percentages of treatment-emergent AEs (TEAEs) and serious AEs (SAEs) according to mogamulizumab exposure were as follows:
- Less than 72 days: 26.6% TEAEs and 6.5% SAEs
- 72-170 days: 18.5% TEAEs and 3.3% SAEs
- 171-351 days: 23.4% TEAEs and 6.0% SAEs
- More than 351 days: 21.7% TEAEs and 4.3% SAEs.
“The majority of the grade 3 events occurred in the first two quartiles, not later, which is important to show,” Dr. Kim said.
Most grade 3 AEs occurred within 170 days of treatment initiation, and the median time to a grade 3 or higher AE was 109 days.
The most common treatment-related AEs in the longest exposure cohort were drug eruption (20.0%), thrombocytopenia (11.1%), stomatitis (8.9%), and anemia (8.9%).
Of all patients in this analysis, 45 experienced drug eruption, which was defined as a skin rash possibly, probably, or definitely related to the study drug.
Nine drug eruption events were grade 3, and the rest were grade 1 or 2. The median time to drug eruption was 107 days.
While drug eruption “didn’t show up early,” there is no cumulative risk with longer exposure to mogamulizumab, Dr. Kim said. Likewise, she said, autoimmune AEs were not dose-cumulative events.
There were two patients with definite autoimmune disease — a 65-year-old man with Miller Fisher syndrome (occurring 199 days after mogamulizumab initiation) and a 40-year-old woman with myositis (151 days) and myocarditis (310 days).
The investigators also identified three patients with possible autoimmune disease, including:
- Pneumonitis (310 days) in a 74-year-old woman
- Polymyalgia rheumatica (209 days) and myopathy (not available) in an 84-year-old man
- Hepatitis (144 days), pneumonitis (about 174 days), and polymyositis (about 174 days) in a 73-year-old man.
Dr. Kim and her colleagues said these data suggest prolonged treatment with mogamulizumab is not associated with an increased safety risk in patients with MF or SS. And the manageable safety profile of mogamulizumab meant that patients who derived a clinical benefit could remain on the drug for an extended period of time.
The MAVORIC trial was sponsored by Kyowa Hakko Kirin Pharma. Dr. Kim reported relationships with Merck, Portola Pharmaceuticals, Soligenix, Takeda, TetraLogic Pharmaceuticals, Kyowa Kirin, Seattle Genetics, Medivir, Neumedicines, Eisai, Innate Pharma, Galderma, Miragen Therapeutics, Forty Seven, and Horizon Pharma. Her coinvestigators reported relationships with several companies.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
REPORTING FROM TCLF 2019
Key clinical point:
Major finding: The highest response rate – 75.6% – was observed in patients exposed to mogamulizumab for at least 351 days.
Study details: A post hoc analysis of the MAVORIC trial, including 184 patients treated with mogamulizumab.
Disclosures: The MAVORIC trial was sponsored by Kyowa Hakko Kirin Pharma. Investigators disclosed relationships with several companies.
Zanubrutinib receives breakthrough designation for MCL
The (MCL) who have received at least one prior therapy.
Zanubrutinib (BGB-3111) is a Bruton’s tyrosine kinase inhibitor being developed by BeiGene as a potential treatment for B-cell malignancies.
Researchers have evaluated zanubrutinib in a phase 2 trial (NCT03206970) of patients with relapsed/refractory MCL. Results from this trial were presented at the 2018 annual meeting of the American Society of Hematology (Abstract 148).
As of March 27, 2018, 86 patients had been enrolled in the trial and received treatment. They had a median of two prior lines of therapy and they received zanubrutinib at 160 mg twice daily.
Eighty-five patients were evaluable for efficacy. The overall response rate was 83.5% (71/85), and the complete response rate was 58.8% (50/85). At a median follow-up of 24.1 weeks, the median duration of response and median progression-free survival had not been reached. The estimated 24-week progression-free survival rate was 82%. The most common adverse events (AEs) in this trial were decrease in neutrophil count (31.4%), rash (29.1%), upper respiratory tract infection (29.1%), and decrease in platelet count (22.1%). Common grade 3 or higher AEs included neutrophil count decrease (11.6%) and lung infection (5.8%).
Four patients had fatal treatment-emergent AEs. One death was caused by a traffic accident, one was due to cerebral hemorrhage, and one resulted from pneumonia. The fourth death occurred in a patient with infection, but the cause of death was unknown.
Breakthrough therapy designation is designed to expedite the development and review of a therapy for a serious or life-threatening disease, following preliminary clinical evidence indicating it demonstrates substantial improvement over existing therapies.
The (MCL) who have received at least one prior therapy.
Zanubrutinib (BGB-3111) is a Bruton’s tyrosine kinase inhibitor being developed by BeiGene as a potential treatment for B-cell malignancies.
Researchers have evaluated zanubrutinib in a phase 2 trial (NCT03206970) of patients with relapsed/refractory MCL. Results from this trial were presented at the 2018 annual meeting of the American Society of Hematology (Abstract 148).
As of March 27, 2018, 86 patients had been enrolled in the trial and received treatment. They had a median of two prior lines of therapy and they received zanubrutinib at 160 mg twice daily.
Eighty-five patients were evaluable for efficacy. The overall response rate was 83.5% (71/85), and the complete response rate was 58.8% (50/85). At a median follow-up of 24.1 weeks, the median duration of response and median progression-free survival had not been reached. The estimated 24-week progression-free survival rate was 82%. The most common adverse events (AEs) in this trial were decrease in neutrophil count (31.4%), rash (29.1%), upper respiratory tract infection (29.1%), and decrease in platelet count (22.1%). Common grade 3 or higher AEs included neutrophil count decrease (11.6%) and lung infection (5.8%).
Four patients had fatal treatment-emergent AEs. One death was caused by a traffic accident, one was due to cerebral hemorrhage, and one resulted from pneumonia. The fourth death occurred in a patient with infection, but the cause of death was unknown.
Breakthrough therapy designation is designed to expedite the development and review of a therapy for a serious or life-threatening disease, following preliminary clinical evidence indicating it demonstrates substantial improvement over existing therapies.
The (MCL) who have received at least one prior therapy.
Zanubrutinib (BGB-3111) is a Bruton’s tyrosine kinase inhibitor being developed by BeiGene as a potential treatment for B-cell malignancies.
Researchers have evaluated zanubrutinib in a phase 2 trial (NCT03206970) of patients with relapsed/refractory MCL. Results from this trial were presented at the 2018 annual meeting of the American Society of Hematology (Abstract 148).
As of March 27, 2018, 86 patients had been enrolled in the trial and received treatment. They had a median of two prior lines of therapy and they received zanubrutinib at 160 mg twice daily.
Eighty-five patients were evaluable for efficacy. The overall response rate was 83.5% (71/85), and the complete response rate was 58.8% (50/85). At a median follow-up of 24.1 weeks, the median duration of response and median progression-free survival had not been reached. The estimated 24-week progression-free survival rate was 82%. The most common adverse events (AEs) in this trial were decrease in neutrophil count (31.4%), rash (29.1%), upper respiratory tract infection (29.1%), and decrease in platelet count (22.1%). Common grade 3 or higher AEs included neutrophil count decrease (11.6%) and lung infection (5.8%).
Four patients had fatal treatment-emergent AEs. One death was caused by a traffic accident, one was due to cerebral hemorrhage, and one resulted from pneumonia. The fourth death occurred in a patient with infection, but the cause of death was unknown.
Breakthrough therapy designation is designed to expedite the development and review of a therapy for a serious or life-threatening disease, following preliminary clinical evidence indicating it demonstrates substantial improvement over existing therapies.
Chidamide may be more effective in PTCL than previously thought
LA JOLLA, CALIF. – Real-world data suggest chidamide may be more effective against relapsed or refractory peripheral T-cell lymphoma (PTCL) than a pivotal study indicated.
Single-agent chidamide produced an overall response rate of 47.0% in a real-world study of more than 1,000 patients, compared with the 28.0% overall response rate that was observed in the phase 2 study of chidamide (Ann Oncol. 2015 Aug;26[8]:1766-71).
Yuqin Song, MD, PhD, of Peking University Cancer Hospital and Institute in Beijing, China, presented data from the real-world study at the annual T-cell Lymphoma Forum.
Dr. Song said this study is the largest cohort of real-world patients with relapsed or refractory PTCL. She and her colleagues analyzed data on 1,064 patients treated at 216 sites across China between February 2015 and December 2017.
The patients had a median age of 54 years, 63.9% were male, and 88.1% had stage III-IV disease.
Disease subtypes included PTCL not otherwise specified (NOS, 38.0%), angioimmunoblastic T-cell lymphoma (AITL, 29.1%), extranodal natural killer T-cell lymphoma (ENKTL, 13.4%), anaplastic large-cell lymphoma (ALCL, 9.1%), and others (10.3%), including cutaneous T-cell lymphoma (CTCL).
Fifty-two percent of patients (n = 553) received chidamide as a single agent, and 48% (n = 511) received the drug with other agents. The most common treatment regimens combined with chidamide were the following
- Cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP, 20.7%).
- Gemcitabine, dexamethasone, and cisplatin (GDP, 11.8%).
- Etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin (EPOCH, 9.8%).
- Patients with ENKTL received chidamide with L-asparaginase (35.4%) or without it (64.5%).
The median follow-up was 4.9 months (range, 0-36.2 months). Across disease subtypes, the overall response rate was 47.0% with single-agent chidamide and 65.4% when chidamide was given in combination with other agents (P less than .01).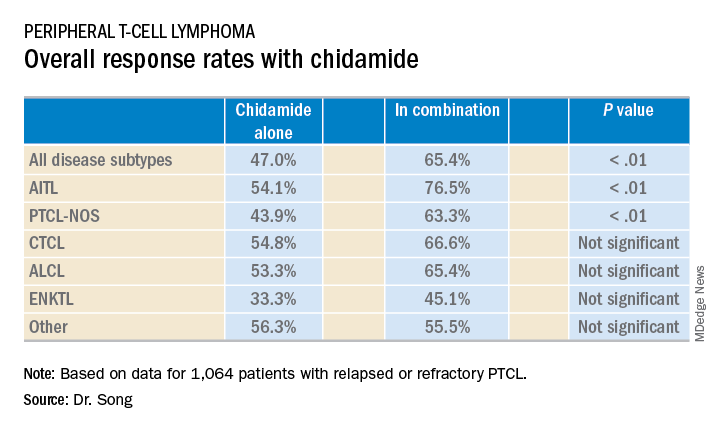
The median overall survival was 400 days for all patients, 342 days for patients treated with chidamide alone, and 457 days for patients who received combination therapy. The 1-year overall survival rates were 52%, 48%, and 56%, respectively.
Dr. Song said these data verify the efficacy of chidamide as a single agent and suggest chidamide might lead to improved survival in refractory or relapsed PTCLs.
Chidamide was generally well tolerated in this study, Dr. Song said. There were no unexpected adverse events (AEs) and most were grade 1 or 2.
The most common AEs (of any grade) observed with single-agent chidamide were neutropenia (42.9%), thrombocytopenia (40.5%), fatigue (38.3%), anemia (31.6%), and nausea/vomiting (21.0%).
The most common AEs observed with chidamide in combination were neutropenia (61.4%), thrombocytopenia (58.5%), fatigue (56.2%), anemia (54.2%), nausea/vomiting (30.7%), and fever (22.1%).
This study was supported by the Union for China Lymphoma Investigators and the Chinese Society of Clinical Oncology. Dr. Song did not disclose any conflicts of interest.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. – Real-world data suggest chidamide may be more effective against relapsed or refractory peripheral T-cell lymphoma (PTCL) than a pivotal study indicated.
Single-agent chidamide produced an overall response rate of 47.0% in a real-world study of more than 1,000 patients, compared with the 28.0% overall response rate that was observed in the phase 2 study of chidamide (Ann Oncol. 2015 Aug;26[8]:1766-71).
Yuqin Song, MD, PhD, of Peking University Cancer Hospital and Institute in Beijing, China, presented data from the real-world study at the annual T-cell Lymphoma Forum.
Dr. Song said this study is the largest cohort of real-world patients with relapsed or refractory PTCL. She and her colleagues analyzed data on 1,064 patients treated at 216 sites across China between February 2015 and December 2017.
The patients had a median age of 54 years, 63.9% were male, and 88.1% had stage III-IV disease.
Disease subtypes included PTCL not otherwise specified (NOS, 38.0%), angioimmunoblastic T-cell lymphoma (AITL, 29.1%), extranodal natural killer T-cell lymphoma (ENKTL, 13.4%), anaplastic large-cell lymphoma (ALCL, 9.1%), and others (10.3%), including cutaneous T-cell lymphoma (CTCL).
Fifty-two percent of patients (n = 553) received chidamide as a single agent, and 48% (n = 511) received the drug with other agents. The most common treatment regimens combined with chidamide were the following
- Cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP, 20.7%).
- Gemcitabine, dexamethasone, and cisplatin (GDP, 11.8%).
- Etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin (EPOCH, 9.8%).
- Patients with ENKTL received chidamide with L-asparaginase (35.4%) or without it (64.5%).
The median follow-up was 4.9 months (range, 0-36.2 months). Across disease subtypes, the overall response rate was 47.0% with single-agent chidamide and 65.4% when chidamide was given in combination with other agents (P less than .01).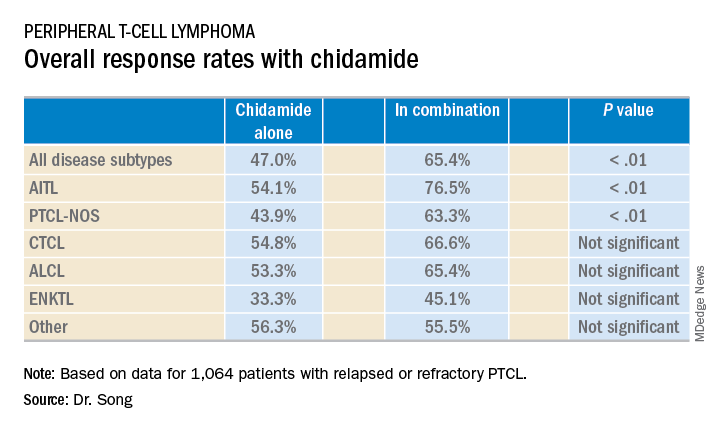
The median overall survival was 400 days for all patients, 342 days for patients treated with chidamide alone, and 457 days for patients who received combination therapy. The 1-year overall survival rates were 52%, 48%, and 56%, respectively.
Dr. Song said these data verify the efficacy of chidamide as a single agent and suggest chidamide might lead to improved survival in refractory or relapsed PTCLs.
Chidamide was generally well tolerated in this study, Dr. Song said. There were no unexpected adverse events (AEs) and most were grade 1 or 2.
The most common AEs (of any grade) observed with single-agent chidamide were neutropenia (42.9%), thrombocytopenia (40.5%), fatigue (38.3%), anemia (31.6%), and nausea/vomiting (21.0%).
The most common AEs observed with chidamide in combination were neutropenia (61.4%), thrombocytopenia (58.5%), fatigue (56.2%), anemia (54.2%), nausea/vomiting (30.7%), and fever (22.1%).
This study was supported by the Union for China Lymphoma Investigators and the Chinese Society of Clinical Oncology. Dr. Song did not disclose any conflicts of interest.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. – Real-world data suggest chidamide may be more effective against relapsed or refractory peripheral T-cell lymphoma (PTCL) than a pivotal study indicated.
Single-agent chidamide produced an overall response rate of 47.0% in a real-world study of more than 1,000 patients, compared with the 28.0% overall response rate that was observed in the phase 2 study of chidamide (Ann Oncol. 2015 Aug;26[8]:1766-71).
Yuqin Song, MD, PhD, of Peking University Cancer Hospital and Institute in Beijing, China, presented data from the real-world study at the annual T-cell Lymphoma Forum.
Dr. Song said this study is the largest cohort of real-world patients with relapsed or refractory PTCL. She and her colleagues analyzed data on 1,064 patients treated at 216 sites across China between February 2015 and December 2017.
The patients had a median age of 54 years, 63.9% were male, and 88.1% had stage III-IV disease.
Disease subtypes included PTCL not otherwise specified (NOS, 38.0%), angioimmunoblastic T-cell lymphoma (AITL, 29.1%), extranodal natural killer T-cell lymphoma (ENKTL, 13.4%), anaplastic large-cell lymphoma (ALCL, 9.1%), and others (10.3%), including cutaneous T-cell lymphoma (CTCL).
Fifty-two percent of patients (n = 553) received chidamide as a single agent, and 48% (n = 511) received the drug with other agents. The most common treatment regimens combined with chidamide were the following
- Cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP, 20.7%).
- Gemcitabine, dexamethasone, and cisplatin (GDP, 11.8%).
- Etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin (EPOCH, 9.8%).
- Patients with ENKTL received chidamide with L-asparaginase (35.4%) or without it (64.5%).
The median follow-up was 4.9 months (range, 0-36.2 months). Across disease subtypes, the overall response rate was 47.0% with single-agent chidamide and 65.4% when chidamide was given in combination with other agents (P less than .01).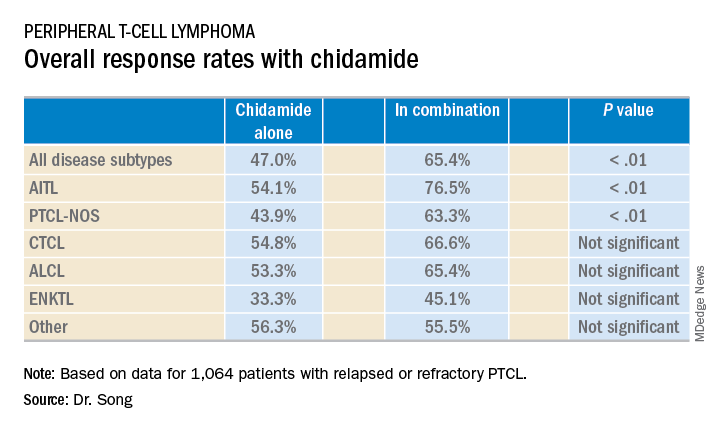
The median overall survival was 400 days for all patients, 342 days for patients treated with chidamide alone, and 457 days for patients who received combination therapy. The 1-year overall survival rates were 52%, 48%, and 56%, respectively.
Dr. Song said these data verify the efficacy of chidamide as a single agent and suggest chidamide might lead to improved survival in refractory or relapsed PTCLs.
Chidamide was generally well tolerated in this study, Dr. Song said. There were no unexpected adverse events (AEs) and most were grade 1 or 2.
The most common AEs (of any grade) observed with single-agent chidamide were neutropenia (42.9%), thrombocytopenia (40.5%), fatigue (38.3%), anemia (31.6%), and nausea/vomiting (21.0%).
The most common AEs observed with chidamide in combination were neutropenia (61.4%), thrombocytopenia (58.5%), fatigue (56.2%), anemia (54.2%), nausea/vomiting (30.7%), and fever (22.1%).
This study was supported by the Union for China Lymphoma Investigators and the Chinese Society of Clinical Oncology. Dr. Song did not disclose any conflicts of interest.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
REPORTING FROM TCLF 2019
Key clinical point:
Major finding: Single-agent chidamide had an overall response rate of 47.0% among relapsed/refractory PTCL patients, compared with 65.4% when used in combination with other agents (P less than .01).
Study details: A real-world cohort of 1,064 relapsed/refractory PTCL patients treated at 216 sites across China between February 2015 and December 2017.
Disclosures: The study was supported by the Union for China Lymphoma Investigators and the Chinese Society of Clinical Oncology. Dr. Song did not disclose any conflicts of interest.







