User login
Novel antibody drug conjugate shows promise in SCLC
CHICAGO – The antibody drug conjugate rovalpituzumab tesirine (Rova-T) is active in DLL3-expressing recurrent and refractory small–cell lung cancer, according to results of a small, first-in-human trial.
Nearly a fifth of the 60 evaluable patients studied experienced tumor shrinkage, and 41% achieved clinical benefit, lead author Dr. Charles M. Rudin of Memorial Sloan Kettering Cancer Center, New York, reported at the annual meeting of the American Society of Clinical Oncology.
“We have demonstrated activity in recurrent and refractory small–cell lung cancer and comparable responses in the second- and third-line settings,” he summarized. “Responses and survival numerically improve [upon] historical controls.”
“This was an early but interesting study of a novel antibody drug conjugate demonstrating activity in progressive small–cell lung cancer which is a very aggressive disease with limited treatment options,” commented moderator Dr. Smitha Krishnamurthi of University Hospitals Case Medical Center, Cleveland.
“What we were focusing on was a new target in small–cell lung cancer, which we believe may be a predictive biomarker for therapeutics. DLL3 is expressed in many small–cell lung cancers and is not expressed in any normal adult tissue,” Dr. Rudin explained. Rova-T contains an anti-DLL3 antibody and pyrrolobenzodiazepine, which together selectively kill DLL3-expressing cells. The study focused on safety and efficacy.
Of the 74 patients enrolled in the study, 60 had tumor tissue samples and were selected for further study. DLL3 was detected in 88% of the patients, and 67% had high-level expression, which was defined as having measurable DLL3 in at least 50% of cells.
All patients received Rova-T as a first-, second-, or third-line therapy. Eleven out of the 60 patients experienced tumor shrinkage and 68% achieved clinical benefit. Among the high–DLL3-expressing patients, 89% achieved and maintained stable disease for at least two scans taken every 6 weeks.
Among the 26 patients with the highest levels of DLL3, 39% responded to the drug, while 32% achieved 1-year survival.
The 12 patients who received Rova-T as a third-line therapy responded “particularly well, with 50% having tumor shrinkage,” reported Dr. Rudin.
“Most importantly, this is the first biomarker-directed therapy to be defined for the treatment of small–cell lung cancer, and this is a biomarker that is expressed in a large majority of small–cell lung cancers so a biomarker that may [have] utility for small–cell lung cancer. Small–cell lung cancer is a terrible disease and is really unchanged in clinically meaningful endpoints for patients. ... Median survival [is] 9-10 months from time of diagnosis, and for recurrent disease, there is really one approved drug … so a lot of room for improvement here,” Dr. Rudin said. Although based on a small cohort, Dr. Rudin noted, “these data really look promising to us as a novel therapeutic for small–cell lung cancer.”
“These results clearly justify further clinical development. We are currently enrolling to those studies,” he said referring to TRINITY, a third-line, single-arm study with no comparative drug. TRINITY is currently enrolling patients in multiple centers. There are also several other trials in the works to look at other diseases with DLL3 expression and to assess Rova-T’s efficacy and safety in combination with other drugs.
Dr. Rudin disclosed that he has a consulting or advisory role with AbbVie, AVEO, Boehringer Ingelheim, GlaxoSmithKline, Merck, Celgene, Novartis, and has received funding from Biomarin. This study was funded by Stemcentrx.
CHICAGO – The antibody drug conjugate rovalpituzumab tesirine (Rova-T) is active in DLL3-expressing recurrent and refractory small–cell lung cancer, according to results of a small, first-in-human trial.
Nearly a fifth of the 60 evaluable patients studied experienced tumor shrinkage, and 41% achieved clinical benefit, lead author Dr. Charles M. Rudin of Memorial Sloan Kettering Cancer Center, New York, reported at the annual meeting of the American Society of Clinical Oncology.
“We have demonstrated activity in recurrent and refractory small–cell lung cancer and comparable responses in the second- and third-line settings,” he summarized. “Responses and survival numerically improve [upon] historical controls.”
“This was an early but interesting study of a novel antibody drug conjugate demonstrating activity in progressive small–cell lung cancer which is a very aggressive disease with limited treatment options,” commented moderator Dr. Smitha Krishnamurthi of University Hospitals Case Medical Center, Cleveland.
“What we were focusing on was a new target in small–cell lung cancer, which we believe may be a predictive biomarker for therapeutics. DLL3 is expressed in many small–cell lung cancers and is not expressed in any normal adult tissue,” Dr. Rudin explained. Rova-T contains an anti-DLL3 antibody and pyrrolobenzodiazepine, which together selectively kill DLL3-expressing cells. The study focused on safety and efficacy.
Of the 74 patients enrolled in the study, 60 had tumor tissue samples and were selected for further study. DLL3 was detected in 88% of the patients, and 67% had high-level expression, which was defined as having measurable DLL3 in at least 50% of cells.
All patients received Rova-T as a first-, second-, or third-line therapy. Eleven out of the 60 patients experienced tumor shrinkage and 68% achieved clinical benefit. Among the high–DLL3-expressing patients, 89% achieved and maintained stable disease for at least two scans taken every 6 weeks.
Among the 26 patients with the highest levels of DLL3, 39% responded to the drug, while 32% achieved 1-year survival.
The 12 patients who received Rova-T as a third-line therapy responded “particularly well, with 50% having tumor shrinkage,” reported Dr. Rudin.
“Most importantly, this is the first biomarker-directed therapy to be defined for the treatment of small–cell lung cancer, and this is a biomarker that is expressed in a large majority of small–cell lung cancers so a biomarker that may [have] utility for small–cell lung cancer. Small–cell lung cancer is a terrible disease and is really unchanged in clinically meaningful endpoints for patients. ... Median survival [is] 9-10 months from time of diagnosis, and for recurrent disease, there is really one approved drug … so a lot of room for improvement here,” Dr. Rudin said. Although based on a small cohort, Dr. Rudin noted, “these data really look promising to us as a novel therapeutic for small–cell lung cancer.”
“These results clearly justify further clinical development. We are currently enrolling to those studies,” he said referring to TRINITY, a third-line, single-arm study with no comparative drug. TRINITY is currently enrolling patients in multiple centers. There are also several other trials in the works to look at other diseases with DLL3 expression and to assess Rova-T’s efficacy and safety in combination with other drugs.
Dr. Rudin disclosed that he has a consulting or advisory role with AbbVie, AVEO, Boehringer Ingelheim, GlaxoSmithKline, Merck, Celgene, Novartis, and has received funding from Biomarin. This study was funded by Stemcentrx.
CHICAGO – The antibody drug conjugate rovalpituzumab tesirine (Rova-T) is active in DLL3-expressing recurrent and refractory small–cell lung cancer, according to results of a small, first-in-human trial.
Nearly a fifth of the 60 evaluable patients studied experienced tumor shrinkage, and 41% achieved clinical benefit, lead author Dr. Charles M. Rudin of Memorial Sloan Kettering Cancer Center, New York, reported at the annual meeting of the American Society of Clinical Oncology.
“We have demonstrated activity in recurrent and refractory small–cell lung cancer and comparable responses in the second- and third-line settings,” he summarized. “Responses and survival numerically improve [upon] historical controls.”
“This was an early but interesting study of a novel antibody drug conjugate demonstrating activity in progressive small–cell lung cancer which is a very aggressive disease with limited treatment options,” commented moderator Dr. Smitha Krishnamurthi of University Hospitals Case Medical Center, Cleveland.
“What we were focusing on was a new target in small–cell lung cancer, which we believe may be a predictive biomarker for therapeutics. DLL3 is expressed in many small–cell lung cancers and is not expressed in any normal adult tissue,” Dr. Rudin explained. Rova-T contains an anti-DLL3 antibody and pyrrolobenzodiazepine, which together selectively kill DLL3-expressing cells. The study focused on safety and efficacy.
Of the 74 patients enrolled in the study, 60 had tumor tissue samples and were selected for further study. DLL3 was detected in 88% of the patients, and 67% had high-level expression, which was defined as having measurable DLL3 in at least 50% of cells.
All patients received Rova-T as a first-, second-, or third-line therapy. Eleven out of the 60 patients experienced tumor shrinkage and 68% achieved clinical benefit. Among the high–DLL3-expressing patients, 89% achieved and maintained stable disease for at least two scans taken every 6 weeks.
Among the 26 patients with the highest levels of DLL3, 39% responded to the drug, while 32% achieved 1-year survival.
The 12 patients who received Rova-T as a third-line therapy responded “particularly well, with 50% having tumor shrinkage,” reported Dr. Rudin.
“Most importantly, this is the first biomarker-directed therapy to be defined for the treatment of small–cell lung cancer, and this is a biomarker that is expressed in a large majority of small–cell lung cancers so a biomarker that may [have] utility for small–cell lung cancer. Small–cell lung cancer is a terrible disease and is really unchanged in clinically meaningful endpoints for patients. ... Median survival [is] 9-10 months from time of diagnosis, and for recurrent disease, there is really one approved drug … so a lot of room for improvement here,” Dr. Rudin said. Although based on a small cohort, Dr. Rudin noted, “these data really look promising to us as a novel therapeutic for small–cell lung cancer.”
“These results clearly justify further clinical development. We are currently enrolling to those studies,” he said referring to TRINITY, a third-line, single-arm study with no comparative drug. TRINITY is currently enrolling patients in multiple centers. There are also several other trials in the works to look at other diseases with DLL3 expression and to assess Rova-T’s efficacy and safety in combination with other drugs.
Dr. Rudin disclosed that he has a consulting or advisory role with AbbVie, AVEO, Boehringer Ingelheim, GlaxoSmithKline, Merck, Celgene, Novartis, and has received funding from Biomarin. This study was funded by Stemcentrx.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Rova-T is active in DLL3-expressing recurrent and refractory small–cell lung cancer.
Major finding: The clinical benefit rate of Rova-T was 68% with 32% of patients achieving 1-year survival.
Data source: A first-in-human trial of 74 patients with SCLC.
Disclosures: This study was funded by Stemcentrx. Dr. Rudin disclosed that he has a consulting or advisory role with AbbVie, AVEO, Boehringer Ingelheim, GlaxoSmithKline, Merck, Celgene, Novartis, and has received funding from BioMarin.
VIDEO: Direct-to-patient study empowers patients, accelerates research
CHICAGO – The Metastatic Breast Cancer Project is an innovative direct-to-patient initiative that allows metastatic breast cancer patients from around the country – often found through social media – to enroll themselves into a research study, primary investigator Dr. Nikhil Wagle said at the annual meeting of the American Society of Clinical Oncology.
Patients interested in participating can visit the project’s website and consent themselves into the study. Patients then fill out a questionnaire about their cancer and their treatments and provide a saliva sample using an at-home kit. Meanwhile, researchers obtain medical records and collect portions of stored tumor samples if available. The overarching goal of the project is to expedite metastatic breast cancer (MBC) genomics research by gaining access to a larger pool of patients with MBC and to generate novel research questions. Over 1,100 patients have already enrolled in the study, and many of them fall into groups of patients – such as those with extraordinary response to treatment or those of racial/ethnic minorities – that are normally challenging to capture in traditional studies.
In a video interview, Dr. Wagle of the Dana-Farber Cancer Institute in Boston and the Broad Institute in Cambridge, Mass., summarizes the unique benefits of the project and discusses future plans, which include gathering patient genomic data from blood biopsy samples and expanding the project to other types of cancers.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – The Metastatic Breast Cancer Project is an innovative direct-to-patient initiative that allows metastatic breast cancer patients from around the country – often found through social media – to enroll themselves into a research study, primary investigator Dr. Nikhil Wagle said at the annual meeting of the American Society of Clinical Oncology.
Patients interested in participating can visit the project’s website and consent themselves into the study. Patients then fill out a questionnaire about their cancer and their treatments and provide a saliva sample using an at-home kit. Meanwhile, researchers obtain medical records and collect portions of stored tumor samples if available. The overarching goal of the project is to expedite metastatic breast cancer (MBC) genomics research by gaining access to a larger pool of patients with MBC and to generate novel research questions. Over 1,100 patients have already enrolled in the study, and many of them fall into groups of patients – such as those with extraordinary response to treatment or those of racial/ethnic minorities – that are normally challenging to capture in traditional studies.
In a video interview, Dr. Wagle of the Dana-Farber Cancer Institute in Boston and the Broad Institute in Cambridge, Mass., summarizes the unique benefits of the project and discusses future plans, which include gathering patient genomic data from blood biopsy samples and expanding the project to other types of cancers.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – The Metastatic Breast Cancer Project is an innovative direct-to-patient initiative that allows metastatic breast cancer patients from around the country – often found through social media – to enroll themselves into a research study, primary investigator Dr. Nikhil Wagle said at the annual meeting of the American Society of Clinical Oncology.
Patients interested in participating can visit the project’s website and consent themselves into the study. Patients then fill out a questionnaire about their cancer and their treatments and provide a saliva sample using an at-home kit. Meanwhile, researchers obtain medical records and collect portions of stored tumor samples if available. The overarching goal of the project is to expedite metastatic breast cancer (MBC) genomics research by gaining access to a larger pool of patients with MBC and to generate novel research questions. Over 1,100 patients have already enrolled in the study, and many of them fall into groups of patients – such as those with extraordinary response to treatment or those of racial/ethnic minorities – that are normally challenging to capture in traditional studies.
In a video interview, Dr. Wagle of the Dana-Farber Cancer Institute in Boston and the Broad Institute in Cambridge, Mass., summarizes the unique benefits of the project and discusses future plans, which include gathering patient genomic data from blood biopsy samples and expanding the project to other types of cancers.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE 2016 ASCO ANNUAL MEETING
VIDEO: Dr. Rugo discusses regulatory future for trastuzumab biosimilar
CHICAGO – Dr. Hope Rugo presented results from a phase III trial comparing the safety and efficacy of the trastuzumab biosimilar MYL-1401O and the FDA-approved trastuzumab (Herceptin), indicating the two were comparable. After 24 weeks, the objective response rates were 69.6% (95% CI: 63.62 to 75.51) for MYL-1401O and 64% (95% CI: 57.81 to 70.26) for trastuzumab. Rates of serious adverse events were comparable at 38.1% among patients receiving MYL-1401O and 36.2% among patients receiving Herceptin.
In a video interview at the annual meeting of the American Society of Clinical Oncology, Dr. Rugo discusses the regulatory future of the biosimilar and prospects for other cancer drug biosimilars. Dr. Rugo is a professor of medicine at the University of California, San Francisco.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Dr. Hope Rugo presented results from a phase III trial comparing the safety and efficacy of the trastuzumab biosimilar MYL-1401O and the FDA-approved trastuzumab (Herceptin), indicating the two were comparable. After 24 weeks, the objective response rates were 69.6% (95% CI: 63.62 to 75.51) for MYL-1401O and 64% (95% CI: 57.81 to 70.26) for trastuzumab. Rates of serious adverse events were comparable at 38.1% among patients receiving MYL-1401O and 36.2% among patients receiving Herceptin.
In a video interview at the annual meeting of the American Society of Clinical Oncology, Dr. Rugo discusses the regulatory future of the biosimilar and prospects for other cancer drug biosimilars. Dr. Rugo is a professor of medicine at the University of California, San Francisco.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Dr. Hope Rugo presented results from a phase III trial comparing the safety and efficacy of the trastuzumab biosimilar MYL-1401O and the FDA-approved trastuzumab (Herceptin), indicating the two were comparable. After 24 weeks, the objective response rates were 69.6% (95% CI: 63.62 to 75.51) for MYL-1401O and 64% (95% CI: 57.81 to 70.26) for trastuzumab. Rates of serious adverse events were comparable at 38.1% among patients receiving MYL-1401O and 36.2% among patients receiving Herceptin.
In a video interview at the annual meeting of the American Society of Clinical Oncology, Dr. Rugo discusses the regulatory future of the biosimilar and prospects for other cancer drug biosimilars. Dr. Rugo is a professor of medicine at the University of California, San Francisco.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE 2016 ASCO ANNUAL MEETING
Biosimilar trastuzumab comparable on safety, efficacy
CHICAGO – The biosimilar trastuzumab antibody MYL-1401O is comparable in safety and efficacy to the FDA-approved trastuzumab (Herceptin) in women with HER2-positive advanced breast cancer, finds a phase III trial reported at the annual meeting of the American Society for Clinical Oncology.
Objective response rates at 24 weeks, the primary endpoint, were 69.6% with MYL-14010 compared to 64% with trastuzumab, reported lead author Dr. Hope Rugo of University of California, San Francisco.
A total of 500 patients with metastatic HER2-positive breast cancer were randomized in the Heritage trial to receive taxane chemotherapy with either trastuzumab or MYL-14010 for at least 8 cycles, followed by trastuzumab alone until disease progression. Response rates were assessed at 24 weeks and 458 patients were evaluable. Patients were enrolled at 95 centers in Asia, Latin America, Africa, and Europe.
Safety was comparable between the two arms; 38.1% of patients receiving MYL-1401O and 36.2% of patients receiving trastuzumab experienced at least one serious adverse event. There were four treatment-related deaths in each arm. Neutropenia was the most common adverse event.
“The Heritage study has demonstrated efficacy equivalence between the trastuzumab biosimilar MYL-1401O [and] Herceptin in combinations with taxanes as first-line therapies for HER2-positive metastatic breast cancer at 24 weeks. We also demonstrated similar safety, immunogenicity and pharmokinetics. This proposed biosimilar has the potential to meet the need for an affordable treatment option with HER2-positive breast cancer,” Dr. Rugo said.
She also said that she would readily adopt MYL-1401O as an alternative once it gains FDA approval.
Mylan, makers of MYL-14010, funded the study. Ten investigators reported serving in advisory roles for, having ownership or stock interest in, or receiving financial compensation or honoraria from multiple companies, including Mylan.
On Twitter @JessCraig_OP
CHICAGO – The biosimilar trastuzumab antibody MYL-1401O is comparable in safety and efficacy to the FDA-approved trastuzumab (Herceptin) in women with HER2-positive advanced breast cancer, finds a phase III trial reported at the annual meeting of the American Society for Clinical Oncology.
Objective response rates at 24 weeks, the primary endpoint, were 69.6% with MYL-14010 compared to 64% with trastuzumab, reported lead author Dr. Hope Rugo of University of California, San Francisco.
A total of 500 patients with metastatic HER2-positive breast cancer were randomized in the Heritage trial to receive taxane chemotherapy with either trastuzumab or MYL-14010 for at least 8 cycles, followed by trastuzumab alone until disease progression. Response rates were assessed at 24 weeks and 458 patients were evaluable. Patients were enrolled at 95 centers in Asia, Latin America, Africa, and Europe.
Safety was comparable between the two arms; 38.1% of patients receiving MYL-1401O and 36.2% of patients receiving trastuzumab experienced at least one serious adverse event. There were four treatment-related deaths in each arm. Neutropenia was the most common adverse event.
“The Heritage study has demonstrated efficacy equivalence between the trastuzumab biosimilar MYL-1401O [and] Herceptin in combinations with taxanes as first-line therapies for HER2-positive metastatic breast cancer at 24 weeks. We also demonstrated similar safety, immunogenicity and pharmokinetics. This proposed biosimilar has the potential to meet the need for an affordable treatment option with HER2-positive breast cancer,” Dr. Rugo said.
She also said that she would readily adopt MYL-1401O as an alternative once it gains FDA approval.
Mylan, makers of MYL-14010, funded the study. Ten investigators reported serving in advisory roles for, having ownership or stock interest in, or receiving financial compensation or honoraria from multiple companies, including Mylan.
On Twitter @JessCraig_OP
CHICAGO – The biosimilar trastuzumab antibody MYL-1401O is comparable in safety and efficacy to the FDA-approved trastuzumab (Herceptin) in women with HER2-positive advanced breast cancer, finds a phase III trial reported at the annual meeting of the American Society for Clinical Oncology.
Objective response rates at 24 weeks, the primary endpoint, were 69.6% with MYL-14010 compared to 64% with trastuzumab, reported lead author Dr. Hope Rugo of University of California, San Francisco.
A total of 500 patients with metastatic HER2-positive breast cancer were randomized in the Heritage trial to receive taxane chemotherapy with either trastuzumab or MYL-14010 for at least 8 cycles, followed by trastuzumab alone until disease progression. Response rates were assessed at 24 weeks and 458 patients were evaluable. Patients were enrolled at 95 centers in Asia, Latin America, Africa, and Europe.
Safety was comparable between the two arms; 38.1% of patients receiving MYL-1401O and 36.2% of patients receiving trastuzumab experienced at least one serious adverse event. There were four treatment-related deaths in each arm. Neutropenia was the most common adverse event.
“The Heritage study has demonstrated efficacy equivalence between the trastuzumab biosimilar MYL-1401O [and] Herceptin in combinations with taxanes as first-line therapies for HER2-positive metastatic breast cancer at 24 weeks. We also demonstrated similar safety, immunogenicity and pharmokinetics. This proposed biosimilar has the potential to meet the need for an affordable treatment option with HER2-positive breast cancer,” Dr. Rugo said.
She also said that she would readily adopt MYL-1401O as an alternative once it gains FDA approval.
Mylan, makers of MYL-14010, funded the study. Ten investigators reported serving in advisory roles for, having ownership or stock interest in, or receiving financial compensation or honoraria from multiple companies, including Mylan.
On Twitter @JessCraig_OP
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: MYL-1401O is comparable in safety and efficacy to trastuzumab for women with HER2-positive advanced breast cancer.
Major finding: The objective response rates at 24 weeks were 69.6% with MYL-1401O and 64% for trastuzumab. Overall, 38.1% of patients receiving MYL-1401O and 36.2% of patients receiving trastuzumab experienced at least one serious adverse event.
Data source: A randomized phase III clinical study of 500 patients with HER2-positive advanced breast cancer enrolled at 95 sites worldwide.
Disclosures: This study was sponsored by Mylan. Ten investigators reported serving in advisory roles for, having ownership or stock interest in, or receiving financial compensation or honoraria from multiple companies, including Mylan.
Early results positive for treating high-grade gliomas with virus-based therapy
An investigational virus-based therapy was safely given to patients with high-grade or recurrent gliomas in a phase I study, improving survival for some, investigators report.
In the phase I trial of Toca 511 (vocimagene amiretrorepvec) in combination with surgical resection, median overall survival was 13.6 months (95% confidence interval, 10.8-20.0) among all evaluable patients with high-grade glioblastoma (n = 43) and 14.4 months (95% CI, 11.3-32.3) for patients with first or second recurrence (n = 32), Dr. Timothy Cloughesy of the University of California, Los Angeles, and his associates reported (Sci Transl Med. 2016;8:1-11).
Investigators compared their data to those of external controls with glioblastoma at first and second recurrence treated with lomustine and saw an almost twofold improvement in overall survival (13.6 months vs. 7.1 months (hazard ratio, 0.45; P = .003).
Toca 511 dispatches a virus to rapidly dividing cancer cells, then delivers a gene encoding an enzyme that converts a nontoxic prodrug, Toca FC (extended-release 5-fluorocytosine), into its active form, 5-fluorouracil.
There were no treatment-related deaths, and there were fewer grade 3 adverse events, compared with the external lomustine control group.
“Recurrent HGG [high-grade glioblastoma] is associated with dismal clinical outcomes, and patients are in need of safe and more efficacious therapy. The nonlytic RRV [retroviral replicating vector] Toca 511 and an extended-release 5-FC [5-fluorocytosine] have the potential to fill this medical need,” the researchers said.
A randomized phase II/III trial in patients with recurrent glioblastoma and anaplastic astrocytoma is underway, they said.
This study was supported by the Accelerate Brain Cancer Cure Foundation, the National Brain Tumor Society, the American Brain Tumor Association, the Musela Foundation, Voices Against Brain Cancer, and the National Institute of Neurological Disorders and Stroke. Thirteen investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies.
On Twitter @JessCraig_OP
An investigational virus-based therapy was safely given to patients with high-grade or recurrent gliomas in a phase I study, improving survival for some, investigators report.
In the phase I trial of Toca 511 (vocimagene amiretrorepvec) in combination with surgical resection, median overall survival was 13.6 months (95% confidence interval, 10.8-20.0) among all evaluable patients with high-grade glioblastoma (n = 43) and 14.4 months (95% CI, 11.3-32.3) for patients with first or second recurrence (n = 32), Dr. Timothy Cloughesy of the University of California, Los Angeles, and his associates reported (Sci Transl Med. 2016;8:1-11).
Investigators compared their data to those of external controls with glioblastoma at first and second recurrence treated with lomustine and saw an almost twofold improvement in overall survival (13.6 months vs. 7.1 months (hazard ratio, 0.45; P = .003).
Toca 511 dispatches a virus to rapidly dividing cancer cells, then delivers a gene encoding an enzyme that converts a nontoxic prodrug, Toca FC (extended-release 5-fluorocytosine), into its active form, 5-fluorouracil.
There were no treatment-related deaths, and there were fewer grade 3 adverse events, compared with the external lomustine control group.
“Recurrent HGG [high-grade glioblastoma] is associated with dismal clinical outcomes, and patients are in need of safe and more efficacious therapy. The nonlytic RRV [retroviral replicating vector] Toca 511 and an extended-release 5-FC [5-fluorocytosine] have the potential to fill this medical need,” the researchers said.
A randomized phase II/III trial in patients with recurrent glioblastoma and anaplastic astrocytoma is underway, they said.
This study was supported by the Accelerate Brain Cancer Cure Foundation, the National Brain Tumor Society, the American Brain Tumor Association, the Musela Foundation, Voices Against Brain Cancer, and the National Institute of Neurological Disorders and Stroke. Thirteen investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies.
On Twitter @JessCraig_OP
An investigational virus-based therapy was safely given to patients with high-grade or recurrent gliomas in a phase I study, improving survival for some, investigators report.
In the phase I trial of Toca 511 (vocimagene amiretrorepvec) in combination with surgical resection, median overall survival was 13.6 months (95% confidence interval, 10.8-20.0) among all evaluable patients with high-grade glioblastoma (n = 43) and 14.4 months (95% CI, 11.3-32.3) for patients with first or second recurrence (n = 32), Dr. Timothy Cloughesy of the University of California, Los Angeles, and his associates reported (Sci Transl Med. 2016;8:1-11).
Investigators compared their data to those of external controls with glioblastoma at first and second recurrence treated with lomustine and saw an almost twofold improvement in overall survival (13.6 months vs. 7.1 months (hazard ratio, 0.45; P = .003).
Toca 511 dispatches a virus to rapidly dividing cancer cells, then delivers a gene encoding an enzyme that converts a nontoxic prodrug, Toca FC (extended-release 5-fluorocytosine), into its active form, 5-fluorouracil.
There were no treatment-related deaths, and there were fewer grade 3 adverse events, compared with the external lomustine control group.
“Recurrent HGG [high-grade glioblastoma] is associated with dismal clinical outcomes, and patients are in need of safe and more efficacious therapy. The nonlytic RRV [retroviral replicating vector] Toca 511 and an extended-release 5-FC [5-fluorocytosine] have the potential to fill this medical need,” the researchers said.
A randomized phase II/III trial in patients with recurrent glioblastoma and anaplastic astrocytoma is underway, they said.
This study was supported by the Accelerate Brain Cancer Cure Foundation, the National Brain Tumor Society, the American Brain Tumor Association, the Musela Foundation, Voices Against Brain Cancer, and the National Institute of Neurological Disorders and Stroke. Thirteen investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies.
On Twitter @JessCraig_OP
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point: A phase I trial indicates that Toca 511 is safe and shows activity in treating patients with high-grade or recurrent glioblastoma.
Major finding: Median overall survival was 13.6 months (95% CI, 10.8-20.0) for patients with high-grade glioblastoma (n = 43), almost twice as long as that of similar patients from a separate trial treated with standard therapy (hazard ratio, 0.45; P = .003).
Data source: A phase I trial of 45 patients with glioblastoma, compared with an external control group.
Disclosures: This study was supported by the Accelerate Brain Cancer Cure Foundation, the National Brain Tumor Society, the American Brain Tumor Association, the Musela Foundation, Voices Against Brain Cancer, and the National Institute of Neurological Disorders and Stroke. Thirteen investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies.
ASCO issues clinical practice guidelines for invasive cervical cancer
The American Society of Clinical Oncology (ASCO) has issued its first clinical practice guidelines on treating invasive cervical cancer, the first of its kind linking recommendations to resource availability.
“Access to cervical cancer care varies between regions of the world, both among and within countries. Lower resource settings tend to have limited or no cervical cancer screening programs. As a result, women often have advanced cervical cancer at diagnosis, which requires treatments that may not be readily available in these areas,” ASCO said in a written statement.
The recommendations, developed by a multidisciplinary panel from the United States, Spain, Mexico, Turkey, Canada, Argentina, Zambia, Uganda, South Korea, China, and India, provide guidance for four resource tiers: basic, limited, enhanced, and maximal. Optimal therapy and palliative care are recommended for each setting and for each stage of cervical cancer.
Concurrent radiotherapy and chemotherapy should be standard in enhanced and maximal settings for women with stage IB to IVA disease. In basic settings where patients cannot be treated with radiation therapy, extrafascial hysterectomy either alone or after neoadjuvant chemotherapy may be an option, the guidelines state. Other key recommendations can be found in the ASCO statement.
On Twitter @JessCraig_OP
The American Society of Clinical Oncology (ASCO) has issued its first clinical practice guidelines on treating invasive cervical cancer, the first of its kind linking recommendations to resource availability.
“Access to cervical cancer care varies between regions of the world, both among and within countries. Lower resource settings tend to have limited or no cervical cancer screening programs. As a result, women often have advanced cervical cancer at diagnosis, which requires treatments that may not be readily available in these areas,” ASCO said in a written statement.
The recommendations, developed by a multidisciplinary panel from the United States, Spain, Mexico, Turkey, Canada, Argentina, Zambia, Uganda, South Korea, China, and India, provide guidance for four resource tiers: basic, limited, enhanced, and maximal. Optimal therapy and palliative care are recommended for each setting and for each stage of cervical cancer.
Concurrent radiotherapy and chemotherapy should be standard in enhanced and maximal settings for women with stage IB to IVA disease. In basic settings where patients cannot be treated with radiation therapy, extrafascial hysterectomy either alone or after neoadjuvant chemotherapy may be an option, the guidelines state. Other key recommendations can be found in the ASCO statement.
On Twitter @JessCraig_OP
The American Society of Clinical Oncology (ASCO) has issued its first clinical practice guidelines on treating invasive cervical cancer, the first of its kind linking recommendations to resource availability.
“Access to cervical cancer care varies between regions of the world, both among and within countries. Lower resource settings tend to have limited or no cervical cancer screening programs. As a result, women often have advanced cervical cancer at diagnosis, which requires treatments that may not be readily available in these areas,” ASCO said in a written statement.
The recommendations, developed by a multidisciplinary panel from the United States, Spain, Mexico, Turkey, Canada, Argentina, Zambia, Uganda, South Korea, China, and India, provide guidance for four resource tiers: basic, limited, enhanced, and maximal. Optimal therapy and palliative care are recommended for each setting and for each stage of cervical cancer.
Concurrent radiotherapy and chemotherapy should be standard in enhanced and maximal settings for women with stage IB to IVA disease. In basic settings where patients cannot be treated with radiation therapy, extrafascial hysterectomy either alone or after neoadjuvant chemotherapy may be an option, the guidelines state. Other key recommendations can be found in the ASCO statement.
On Twitter @JessCraig_OP
Investigational CDK4/6 inhibitor shows activity, less toxicity
Abemaciclib, a CDK4/6 inhibitor, showed durable clinical activity when given as continuous single-agent therapy to patients with advanced cancer, including breast cancer and non–small-cell lung cancer, according to investigators.
Neutropenia was rarely observed in patients treated with abemaciclib, the toxicity observed in some patients who receive the only Food and Drug Administration–approved CDK4/6 inhibitor, palbociclib.
“Abemaciclib is a small-molecule inhibitor of CDK4 and CDK6 that is structurally distinct from other dual inhibitors (such as palbociclib and ribociclib) and notably exhibits greater selectivity for CDK4 compared with CDK6,” wrote Dr. Amita Patnaik of South Texas Accelerated Research Therapeutics and her associates (Cancer Discov. 2016 May 23. doi: 10.1158/2159-8290.CD-16-0095).
Furthermore, preclinical models indicate that the drug can cross the blood-brain barrier, suggesting potential efficacy against primary and metastatic tumors involving the central nervous system, they said.
A total of 225 patients with various types of advanced cancers were enrolled in this multicohort phase I study (dose escalation, n = 33; single-agent abemaciclib therapy for breast cancer, n = 47; non–small-cell lung cancer, n = 68; glioblastoma, n = 17; melanoma, n = 26; colorectal cancer, n = 15; abemaciclib plus fulvestrant combination therapy for hormone receptor–positive breast cancer, n = 19). Abemaciclib was given orally to all patients.
Neither dose-limiting toxicity nor maximum tolerated dose was reached in patients treated at levels of 50 mg, 100 mg, 150 mg, or 225 mg once daily. The maximum tolerated dose was 200 mg for patients treated with abemaciclib twice daily.
In the single-agent breast cancer cohort, the disease control rate was 81% for hormone receptor–positive (HR-positive) tumors, 33% for HR-negative tumors, 100% for HR-positive HER2-positive tumors, 72% for HR-positive HER2-negative tumors, and 70% overall. The response rate was 31% for HR-positive tumors, 0% for HR-negative tumors, 36% for HR-positive HER2-positive tumors, 28% for HR-positive HER2-negative tumors, and 23% overall.
The overall response rate was 21% for breast cancer patients receiving abemaciclib plus fulvestrant.
Among the 68 patients with non–small-cell lung cancer, 2 had a partial response and 31 had stable disease. Of the 26 patients with melanoma, 1 had a partial response and 6 had stable disease. Of the 17 patients with glioblastoma, 3 had stable disease.
Overall, there were no study-related deaths. Diarrhea, nausea, and fatigue were the most common adverse events; all were reversible.
Neutropenia was observed in 39 patients (23% of 173 patients in the single-agent tumor-specific cohort) – 2 were grade 4 events. Grade 3 neutropenia occurred in 6 patients (32% of 19 patients with HR-positive breast cancer receiving combination therapy with abemaciclib plus fulvestrant).
“Previous reports have identified neutropenia as an adverse event associated with dual inhibition of CDK4 and CDK6. However, abemaciclib given as a single agent on a continuous schedule in the tumor-specific cohorts was associated with an acceptable incidence of investigator-reported grade 3 (9%, 16 of 173 patients) or grade 4 (1%, 2 of 173 patients) neutropenia,” wrote the investigators.
“In summary, the results of this clinical trial demonstrate the safety and antitumor activity of abemaciclib as a single agent and support its further development both as monotherapy and in rational combinations. Furthermore, these findings validate CDK4 and CDK6 as anticancer drug targets and translate preclinical predictions regarding therapeutic targeting of cell-cycle derangements in cancer into clinical efficacy,”they wrote.
Eli Lilly funded the study. Eight investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies including Eli Lilly.
On Twitter @JessCraig_OP
Abemaciclib, a CDK4/6 inhibitor, showed durable clinical activity when given as continuous single-agent therapy to patients with advanced cancer, including breast cancer and non–small-cell lung cancer, according to investigators.
Neutropenia was rarely observed in patients treated with abemaciclib, the toxicity observed in some patients who receive the only Food and Drug Administration–approved CDK4/6 inhibitor, palbociclib.
“Abemaciclib is a small-molecule inhibitor of CDK4 and CDK6 that is structurally distinct from other dual inhibitors (such as palbociclib and ribociclib) and notably exhibits greater selectivity for CDK4 compared with CDK6,” wrote Dr. Amita Patnaik of South Texas Accelerated Research Therapeutics and her associates (Cancer Discov. 2016 May 23. doi: 10.1158/2159-8290.CD-16-0095).
Furthermore, preclinical models indicate that the drug can cross the blood-brain barrier, suggesting potential efficacy against primary and metastatic tumors involving the central nervous system, they said.
A total of 225 patients with various types of advanced cancers were enrolled in this multicohort phase I study (dose escalation, n = 33; single-agent abemaciclib therapy for breast cancer, n = 47; non–small-cell lung cancer, n = 68; glioblastoma, n = 17; melanoma, n = 26; colorectal cancer, n = 15; abemaciclib plus fulvestrant combination therapy for hormone receptor–positive breast cancer, n = 19). Abemaciclib was given orally to all patients.
Neither dose-limiting toxicity nor maximum tolerated dose was reached in patients treated at levels of 50 mg, 100 mg, 150 mg, or 225 mg once daily. The maximum tolerated dose was 200 mg for patients treated with abemaciclib twice daily.
In the single-agent breast cancer cohort, the disease control rate was 81% for hormone receptor–positive (HR-positive) tumors, 33% for HR-negative tumors, 100% for HR-positive HER2-positive tumors, 72% for HR-positive HER2-negative tumors, and 70% overall. The response rate was 31% for HR-positive tumors, 0% for HR-negative tumors, 36% for HR-positive HER2-positive tumors, 28% for HR-positive HER2-negative tumors, and 23% overall.
The overall response rate was 21% for breast cancer patients receiving abemaciclib plus fulvestrant.
Among the 68 patients with non–small-cell lung cancer, 2 had a partial response and 31 had stable disease. Of the 26 patients with melanoma, 1 had a partial response and 6 had stable disease. Of the 17 patients with glioblastoma, 3 had stable disease.
Overall, there were no study-related deaths. Diarrhea, nausea, and fatigue were the most common adverse events; all were reversible.
Neutropenia was observed in 39 patients (23% of 173 patients in the single-agent tumor-specific cohort) – 2 were grade 4 events. Grade 3 neutropenia occurred in 6 patients (32% of 19 patients with HR-positive breast cancer receiving combination therapy with abemaciclib plus fulvestrant).
“Previous reports have identified neutropenia as an adverse event associated with dual inhibition of CDK4 and CDK6. However, abemaciclib given as a single agent on a continuous schedule in the tumor-specific cohorts was associated with an acceptable incidence of investigator-reported grade 3 (9%, 16 of 173 patients) or grade 4 (1%, 2 of 173 patients) neutropenia,” wrote the investigators.
“In summary, the results of this clinical trial demonstrate the safety and antitumor activity of abemaciclib as a single agent and support its further development both as monotherapy and in rational combinations. Furthermore, these findings validate CDK4 and CDK6 as anticancer drug targets and translate preclinical predictions regarding therapeutic targeting of cell-cycle derangements in cancer into clinical efficacy,”they wrote.
Eli Lilly funded the study. Eight investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies including Eli Lilly.
On Twitter @JessCraig_OP
Abemaciclib, a CDK4/6 inhibitor, showed durable clinical activity when given as continuous single-agent therapy to patients with advanced cancer, including breast cancer and non–small-cell lung cancer, according to investigators.
Neutropenia was rarely observed in patients treated with abemaciclib, the toxicity observed in some patients who receive the only Food and Drug Administration–approved CDK4/6 inhibitor, palbociclib.
“Abemaciclib is a small-molecule inhibitor of CDK4 and CDK6 that is structurally distinct from other dual inhibitors (such as palbociclib and ribociclib) and notably exhibits greater selectivity for CDK4 compared with CDK6,” wrote Dr. Amita Patnaik of South Texas Accelerated Research Therapeutics and her associates (Cancer Discov. 2016 May 23. doi: 10.1158/2159-8290.CD-16-0095).
Furthermore, preclinical models indicate that the drug can cross the blood-brain barrier, suggesting potential efficacy against primary and metastatic tumors involving the central nervous system, they said.
A total of 225 patients with various types of advanced cancers were enrolled in this multicohort phase I study (dose escalation, n = 33; single-agent abemaciclib therapy for breast cancer, n = 47; non–small-cell lung cancer, n = 68; glioblastoma, n = 17; melanoma, n = 26; colorectal cancer, n = 15; abemaciclib plus fulvestrant combination therapy for hormone receptor–positive breast cancer, n = 19). Abemaciclib was given orally to all patients.
Neither dose-limiting toxicity nor maximum tolerated dose was reached in patients treated at levels of 50 mg, 100 mg, 150 mg, or 225 mg once daily. The maximum tolerated dose was 200 mg for patients treated with abemaciclib twice daily.
In the single-agent breast cancer cohort, the disease control rate was 81% for hormone receptor–positive (HR-positive) tumors, 33% for HR-negative tumors, 100% for HR-positive HER2-positive tumors, 72% for HR-positive HER2-negative tumors, and 70% overall. The response rate was 31% for HR-positive tumors, 0% for HR-negative tumors, 36% for HR-positive HER2-positive tumors, 28% for HR-positive HER2-negative tumors, and 23% overall.
The overall response rate was 21% for breast cancer patients receiving abemaciclib plus fulvestrant.
Among the 68 patients with non–small-cell lung cancer, 2 had a partial response and 31 had stable disease. Of the 26 patients with melanoma, 1 had a partial response and 6 had stable disease. Of the 17 patients with glioblastoma, 3 had stable disease.
Overall, there were no study-related deaths. Diarrhea, nausea, and fatigue were the most common adverse events; all were reversible.
Neutropenia was observed in 39 patients (23% of 173 patients in the single-agent tumor-specific cohort) – 2 were grade 4 events. Grade 3 neutropenia occurred in 6 patients (32% of 19 patients with HR-positive breast cancer receiving combination therapy with abemaciclib plus fulvestrant).
“Previous reports have identified neutropenia as an adverse event associated with dual inhibition of CDK4 and CDK6. However, abemaciclib given as a single agent on a continuous schedule in the tumor-specific cohorts was associated with an acceptable incidence of investigator-reported grade 3 (9%, 16 of 173 patients) or grade 4 (1%, 2 of 173 patients) neutropenia,” wrote the investigators.
“In summary, the results of this clinical trial demonstrate the safety and antitumor activity of abemaciclib as a single agent and support its further development both as monotherapy and in rational combinations. Furthermore, these findings validate CDK4 and CDK6 as anticancer drug targets and translate preclinical predictions regarding therapeutic targeting of cell-cycle derangements in cancer into clinical efficacy,”they wrote.
Eli Lilly funded the study. Eight investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies including Eli Lilly.
On Twitter @JessCraig_OP
FROM CANCER DISCOVERY
Key clinical point: A phase I trial indicates that abemaciclib is safe and shows activity in treating patients with advanced breast and other cancers.
Major finding: In the single-agent breast cancer cohort, the overall disease control rate was 70%. Incidence of neutropenia was 9% for grade 3 and 1% for grade 4.
Data source: A multicenter phase I dose-escalation and tumor-specific cohort study of 225 patients with advanced cancers.
Disclosures: Eli Lilly funded the study. Eight investigators reported serving in advisory roles, having ownership or stock interest in, or receiving financial compensation from multiple companies including Eli Lilly.
Exercise Linked to Fewer Cardiovascular Events in Nonmetastatic Breast Cancer Patients
More rigorous and/or more frequent exercise was associated with a significantly reduced risk of cardiovascular events in women with nonmetastatic breast cancer, regardless of age and type of anticancer therapy received, investigators reported.
“CVD [Cardiovascular disease] is now the leading cause of death among women with nonmetastatic breast cancer, especially for those older than 65 years of age and with preexisting CVD risk factors (eg., hypertension, obesity, history of cardiovascular disease) at diagnosis. Moreover, patients with nonmetastatic breast cancer may be at increased risk of CVD, compared with age-matched women without a history of breast cancer because of the direct toxic effects of anticancer therapy,” wrote Dr. Lee Jones of the Memorial Sloan Kettering Cancer Center, New York, and associates (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.65.6603).
To see whether exercise reduces risk, investigators gave the Arizona Activity Frequency Questionnaire to 2,973 women diagnosed with nonmetastatic breast cancer who were participating in two cohort studies. Frequency, duration, and type of exercise were standardized into metabolic equivalent tasks (MET), which were quartiled into the following categories: less than or equal to 2 h/wk, 2.1-10.3 h/wk, 10.4-24.5 h/wk, and greater than 24.6 h/wk. Cardiovascular events, defined as coronary artery disease, nonfatal myocardial infarction, heart failure, valve abnormality, arrhythmia, stroke or cardiovascular disease–related death, were monitored via electronic medical records.
Median follow-up time was 8.6 years. In age-adjusted analysis, the risk of cardiovascular events declined across increasing quartiles of total MET h/wk (1.00, 0.83, 0.72, 0.57, respectively, P less than .001).
Adherence to national exercise guidelines for adult patients (MET score equal to or greater than 9) was associated with a significant 23% reduction in cardiovascular events. Patients who met the national exercise guidelines had a significant reduction in cardiovascular events regardless of age, menopausal status, type of anticancer therapy, or cardiovascular risk factors at cancer diagnosis when compared with patients who not did meet the national exercise guidelines.
“Irrespective of therapy-induced risk, CVD will remain a leading cause of mortality in early-stage breast cancer given continual improvements in cancer-specific mortality together with the rapidly aging population. Thus, our finding that the cardioprotective effects of exercise are comparable in middle-aged women irrespective of exposure to anticancer therapies is novel and important. … Nevertheless, at present, at least in the United States, exercise treatment is not considered an aspect of first-line therapy for the adverse CV consequences of breast cancer adjuvant therapy, similar to that for the primary or secondary prevention of CVD. As such, confirmatory data from randomized trials are urgently required,” the investigators wrote.
This study was supported by a National Institute of Health Award and research grants from the National Cancer Institute and the Memorial Sloan Kettering Cancer Center. One investigator reported having stock or ownership interests in Exercise by Science. Two investigators reported serving in advisory roles or receiving financial compensation from various companies. The other investigators reported having no disclosures.
More rigorous and/or more frequent exercise was associated with a significantly reduced risk of cardiovascular events in women with nonmetastatic breast cancer, regardless of age and type of anticancer therapy received, investigators reported.
“CVD [Cardiovascular disease] is now the leading cause of death among women with nonmetastatic breast cancer, especially for those older than 65 years of age and with preexisting CVD risk factors (eg., hypertension, obesity, history of cardiovascular disease) at diagnosis. Moreover, patients with nonmetastatic breast cancer may be at increased risk of CVD, compared with age-matched women without a history of breast cancer because of the direct toxic effects of anticancer therapy,” wrote Dr. Lee Jones of the Memorial Sloan Kettering Cancer Center, New York, and associates (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.65.6603).
To see whether exercise reduces risk, investigators gave the Arizona Activity Frequency Questionnaire to 2,973 women diagnosed with nonmetastatic breast cancer who were participating in two cohort studies. Frequency, duration, and type of exercise were standardized into metabolic equivalent tasks (MET), which were quartiled into the following categories: less than or equal to 2 h/wk, 2.1-10.3 h/wk, 10.4-24.5 h/wk, and greater than 24.6 h/wk. Cardiovascular events, defined as coronary artery disease, nonfatal myocardial infarction, heart failure, valve abnormality, arrhythmia, stroke or cardiovascular disease–related death, were monitored via electronic medical records.
Median follow-up time was 8.6 years. In age-adjusted analysis, the risk of cardiovascular events declined across increasing quartiles of total MET h/wk (1.00, 0.83, 0.72, 0.57, respectively, P less than .001).
Adherence to national exercise guidelines for adult patients (MET score equal to or greater than 9) was associated with a significant 23% reduction in cardiovascular events. Patients who met the national exercise guidelines had a significant reduction in cardiovascular events regardless of age, menopausal status, type of anticancer therapy, or cardiovascular risk factors at cancer diagnosis when compared with patients who not did meet the national exercise guidelines.
“Irrespective of therapy-induced risk, CVD will remain a leading cause of mortality in early-stage breast cancer given continual improvements in cancer-specific mortality together with the rapidly aging population. Thus, our finding that the cardioprotective effects of exercise are comparable in middle-aged women irrespective of exposure to anticancer therapies is novel and important. … Nevertheless, at present, at least in the United States, exercise treatment is not considered an aspect of first-line therapy for the adverse CV consequences of breast cancer adjuvant therapy, similar to that for the primary or secondary prevention of CVD. As such, confirmatory data from randomized trials are urgently required,” the investigators wrote.
This study was supported by a National Institute of Health Award and research grants from the National Cancer Institute and the Memorial Sloan Kettering Cancer Center. One investigator reported having stock or ownership interests in Exercise by Science. Two investigators reported serving in advisory roles or receiving financial compensation from various companies. The other investigators reported having no disclosures.
More rigorous and/or more frequent exercise was associated with a significantly reduced risk of cardiovascular events in women with nonmetastatic breast cancer, regardless of age and type of anticancer therapy received, investigators reported.
“CVD [Cardiovascular disease] is now the leading cause of death among women with nonmetastatic breast cancer, especially for those older than 65 years of age and with preexisting CVD risk factors (eg., hypertension, obesity, history of cardiovascular disease) at diagnosis. Moreover, patients with nonmetastatic breast cancer may be at increased risk of CVD, compared with age-matched women without a history of breast cancer because of the direct toxic effects of anticancer therapy,” wrote Dr. Lee Jones of the Memorial Sloan Kettering Cancer Center, New York, and associates (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.65.6603).
To see whether exercise reduces risk, investigators gave the Arizona Activity Frequency Questionnaire to 2,973 women diagnosed with nonmetastatic breast cancer who were participating in two cohort studies. Frequency, duration, and type of exercise were standardized into metabolic equivalent tasks (MET), which were quartiled into the following categories: less than or equal to 2 h/wk, 2.1-10.3 h/wk, 10.4-24.5 h/wk, and greater than 24.6 h/wk. Cardiovascular events, defined as coronary artery disease, nonfatal myocardial infarction, heart failure, valve abnormality, arrhythmia, stroke or cardiovascular disease–related death, were monitored via electronic medical records.
Median follow-up time was 8.6 years. In age-adjusted analysis, the risk of cardiovascular events declined across increasing quartiles of total MET h/wk (1.00, 0.83, 0.72, 0.57, respectively, P less than .001).
Adherence to national exercise guidelines for adult patients (MET score equal to or greater than 9) was associated with a significant 23% reduction in cardiovascular events. Patients who met the national exercise guidelines had a significant reduction in cardiovascular events regardless of age, menopausal status, type of anticancer therapy, or cardiovascular risk factors at cancer diagnosis when compared with patients who not did meet the national exercise guidelines.
“Irrespective of therapy-induced risk, CVD will remain a leading cause of mortality in early-stage breast cancer given continual improvements in cancer-specific mortality together with the rapidly aging population. Thus, our finding that the cardioprotective effects of exercise are comparable in middle-aged women irrespective of exposure to anticancer therapies is novel and important. … Nevertheless, at present, at least in the United States, exercise treatment is not considered an aspect of first-line therapy for the adverse CV consequences of breast cancer adjuvant therapy, similar to that for the primary or secondary prevention of CVD. As such, confirmatory data from randomized trials are urgently required,” the investigators wrote.
This study was supported by a National Institute of Health Award and research grants from the National Cancer Institute and the Memorial Sloan Kettering Cancer Center. One investigator reported having stock or ownership interests in Exercise by Science. Two investigators reported serving in advisory roles or receiving financial compensation from various companies. The other investigators reported having no disclosures.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Exercise linked to fewer cardiovascular events in nonmetastatic breast cancer patients
More rigorous and/or more frequent exercise was associated with a significantly reduced risk of cardiovascular events in women with nonmetastatic breast cancer, regardless of age and type of anticancer therapy received, investigators reported.
“CVD [Cardiovascular disease] is now the leading cause of death among women with nonmetastatic breast cancer, especially for those older than 65 years of age and with preexisting CVD risk factors (eg., hypertension, obesity, history of cardiovascular disease) at diagnosis. Moreover, patients with nonmetastatic breast cancer may be at increased risk of CVD, compared with age-matched women without a history of breast cancer because of the direct toxic effects of anticancer therapy,” wrote Dr. Lee Jones of the Memorial Sloan Kettering Cancer Center, New York, and associates (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.65.6603).
To see whether exercise reduces risk, investigators gave the Arizona Activity Frequency Questionnaire to 2,973 women diagnosed with nonmetastatic breast cancer who were participating in two cohort studies. Frequency, duration, and type of exercise were standardized into metabolic equivalent tasks (MET), which were quartiled into the following categories: less than or equal to 2 h/wk, 2.1-10.3 h/wk, 10.4-24.5 h/wk, and greater than 24.6 h/wk. Cardiovascular events, defined as coronary artery disease, nonfatal myocardial infarction, heart failure, valve abnormality, arrhythmia, stroke or cardiovascular disease–related death, were monitored via electronic medical records.
Median follow-up time was 8.6 years. In age-adjusted analysis, the risk of cardiovascular events declined across increasing quartiles of total MET h/wk (1.00, 0.83, 0.72, 0.57, respectively, P less than .001).
Adherence to national exercise guidelines for adult patients (MET score equal to or greater than 9) was associated with a significant 23% reduction in cardiovascular events. Patients who met the national exercise guidelines had a significant reduction in cardiovascular events regardless of age, menopausal status, type of anticancer therapy, or cardiovascular risk factors at cancer diagnosis when compared with patients who not did meet the national exercise guidelines.
“Irrespective of therapy-induced risk, CVD will remain a leading cause of mortality in early-stage breast cancer given continual improvements in cancer-specific mortality together with the rapidly aging population. Thus, our finding that the cardioprotective effects of exercise are comparable in middle-aged women irrespective of exposure to anticancer therapies is novel and important. … Nevertheless, at present, at least in the United States, exercise treatment is not considered an aspect of first-line therapy for the adverse CV consequences of breast cancer adjuvant therapy, similar to that for the primary or secondary prevention of CVD. As such, confirmatory data from randomized trials are urgently required,” the investigators wrote.
This study was supported by a National Institute of Health Award and research grants from the National Cancer Institute and the Memorial Sloan Kettering Cancer Center. One investigator reported having stock or ownership interests in Exercise by Science. Two investigators reported serving in advisory roles or receiving financial compensation from various companies. The other investigators reported having no disclosures.
On Twitter @JessCraig_OP
More rigorous and/or more frequent exercise was associated with a significantly reduced risk of cardiovascular events in women with nonmetastatic breast cancer, regardless of age and type of anticancer therapy received, investigators reported.
“CVD [Cardiovascular disease] is now the leading cause of death among women with nonmetastatic breast cancer, especially for those older than 65 years of age and with preexisting CVD risk factors (eg., hypertension, obesity, history of cardiovascular disease) at diagnosis. Moreover, patients with nonmetastatic breast cancer may be at increased risk of CVD, compared with age-matched women without a history of breast cancer because of the direct toxic effects of anticancer therapy,” wrote Dr. Lee Jones of the Memorial Sloan Kettering Cancer Center, New York, and associates (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.65.6603).
To see whether exercise reduces risk, investigators gave the Arizona Activity Frequency Questionnaire to 2,973 women diagnosed with nonmetastatic breast cancer who were participating in two cohort studies. Frequency, duration, and type of exercise were standardized into metabolic equivalent tasks (MET), which were quartiled into the following categories: less than or equal to 2 h/wk, 2.1-10.3 h/wk, 10.4-24.5 h/wk, and greater than 24.6 h/wk. Cardiovascular events, defined as coronary artery disease, nonfatal myocardial infarction, heart failure, valve abnormality, arrhythmia, stroke or cardiovascular disease–related death, were monitored via electronic medical records.
Median follow-up time was 8.6 years. In age-adjusted analysis, the risk of cardiovascular events declined across increasing quartiles of total MET h/wk (1.00, 0.83, 0.72, 0.57, respectively, P less than .001).
Adherence to national exercise guidelines for adult patients (MET score equal to or greater than 9) was associated with a significant 23% reduction in cardiovascular events. Patients who met the national exercise guidelines had a significant reduction in cardiovascular events regardless of age, menopausal status, type of anticancer therapy, or cardiovascular risk factors at cancer diagnosis when compared with patients who not did meet the national exercise guidelines.
“Irrespective of therapy-induced risk, CVD will remain a leading cause of mortality in early-stage breast cancer given continual improvements in cancer-specific mortality together with the rapidly aging population. Thus, our finding that the cardioprotective effects of exercise are comparable in middle-aged women irrespective of exposure to anticancer therapies is novel and important. … Nevertheless, at present, at least in the United States, exercise treatment is not considered an aspect of first-line therapy for the adverse CV consequences of breast cancer adjuvant therapy, similar to that for the primary or secondary prevention of CVD. As such, confirmatory data from randomized trials are urgently required,” the investigators wrote.
This study was supported by a National Institute of Health Award and research grants from the National Cancer Institute and the Memorial Sloan Kettering Cancer Center. One investigator reported having stock or ownership interests in Exercise by Science. Two investigators reported serving in advisory roles or receiving financial compensation from various companies. The other investigators reported having no disclosures.
On Twitter @JessCraig_OP
More rigorous and/or more frequent exercise was associated with a significantly reduced risk of cardiovascular events in women with nonmetastatic breast cancer, regardless of age and type of anticancer therapy received, investigators reported.
“CVD [Cardiovascular disease] is now the leading cause of death among women with nonmetastatic breast cancer, especially for those older than 65 years of age and with preexisting CVD risk factors (eg., hypertension, obesity, history of cardiovascular disease) at diagnosis. Moreover, patients with nonmetastatic breast cancer may be at increased risk of CVD, compared with age-matched women without a history of breast cancer because of the direct toxic effects of anticancer therapy,” wrote Dr. Lee Jones of the Memorial Sloan Kettering Cancer Center, New York, and associates (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.65.6603).
To see whether exercise reduces risk, investigators gave the Arizona Activity Frequency Questionnaire to 2,973 women diagnosed with nonmetastatic breast cancer who were participating in two cohort studies. Frequency, duration, and type of exercise were standardized into metabolic equivalent tasks (MET), which were quartiled into the following categories: less than or equal to 2 h/wk, 2.1-10.3 h/wk, 10.4-24.5 h/wk, and greater than 24.6 h/wk. Cardiovascular events, defined as coronary artery disease, nonfatal myocardial infarction, heart failure, valve abnormality, arrhythmia, stroke or cardiovascular disease–related death, were monitored via electronic medical records.
Median follow-up time was 8.6 years. In age-adjusted analysis, the risk of cardiovascular events declined across increasing quartiles of total MET h/wk (1.00, 0.83, 0.72, 0.57, respectively, P less than .001).
Adherence to national exercise guidelines for adult patients (MET score equal to or greater than 9) was associated with a significant 23% reduction in cardiovascular events. Patients who met the national exercise guidelines had a significant reduction in cardiovascular events regardless of age, menopausal status, type of anticancer therapy, or cardiovascular risk factors at cancer diagnosis when compared with patients who not did meet the national exercise guidelines.
“Irrespective of therapy-induced risk, CVD will remain a leading cause of mortality in early-stage breast cancer given continual improvements in cancer-specific mortality together with the rapidly aging population. Thus, our finding that the cardioprotective effects of exercise are comparable in middle-aged women irrespective of exposure to anticancer therapies is novel and important. … Nevertheless, at present, at least in the United States, exercise treatment is not considered an aspect of first-line therapy for the adverse CV consequences of breast cancer adjuvant therapy, similar to that for the primary or secondary prevention of CVD. As such, confirmatory data from randomized trials are urgently required,” the investigators wrote.
This study was supported by a National Institute of Health Award and research grants from the National Cancer Institute and the Memorial Sloan Kettering Cancer Center. One investigator reported having stock or ownership interests in Exercise by Science. Two investigators reported serving in advisory roles or receiving financial compensation from various companies. The other investigators reported having no disclosures.
On Twitter @JessCraig_OP
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Exercise was linked to significantly reduced risk of cardiovascular events in women with nonmetastatic breast cancer, regardless of age and type of anticancer therapy received.
Major finding: Adherence to national exercise guidelines for adult patients (MET score equal to or greater than 9) was associated with a significant 23% reduction in cardiovascular events.
Data source: Retrospective survey of exercise and prospective monitoring of cardiovascular events in 2,973 women with nonmetastatic breast cancer.
Disclosures: This study was supported by a National Institute of Health Award and research grants from the National Cancer Institute and the Memorial Sloan Kettering Cancer Center. One investigator reported having stock or ownership interests in Exercise by Science. Two investigators reported serving in advisory roles or receiving financial compensation from various companies. The other investigators reported having no disclosures.
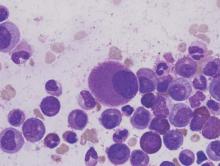
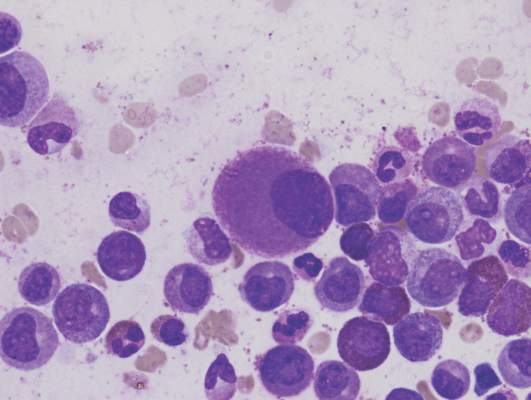
Dasatinib bests imatinib on molecular, cytogenic response rates in CML
Overall survival and progression-free survival were similar at 5 years in chronic myeloid leukemia patients receiving dasatinib or imatinib, but those given dasatinib had higher major molecular response rates and complete cytogenic response rates without a higher rate of adverse events, based on an extension study of previously published data from the DASISION trial.
The DASISION phase III clinical trial included 519 patients with newly diagnosed and treatment-naive chronic myeloid leukemia. Participants were randomly assigned to receive either 100 mg of dasatinib daily (259 patients) or 400 mg of imatinib daily (260 patients). Dosage was altered on a per-patient basis if adverse events or suboptimal responses were observed. The median average daily dose was 99 mg for dasatinib and 400 mg for imatinib after 5 years.
“Initial results showed that dasatinib had met its primary end point of superior efficacy compared with imatinib and had an acceptable safety profile, leading to its approval for first-line use,” reported Dr. Jorge Cortes of the University of Texas MD Anderson Cancer Center, Houston, and his associates (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.64.8899). Given the faster and deeper molecular responses seen in patients taking dasatinib, “dasatinib should continue to be considered a standard first-line therapy for patients with newly diagnosed” chronic myeloid leukemia, they wrote.
In DASISION (Dasatinib Versus Imatinib Study in Treatment-Naive Chronic Myeloid Leukemia Patients), complete cytogenic response, major molecular response, overall survival, and progression-free survival were measured.
The major molecular response rate was significantly higher for patients receiving dasatinib, compared with patients receiving imatinib (76% vs. 64%, P = .0022).
The rate of complete cytogenic response was 28% for dasatinib and 26% for imatinib.
The 5-year overall survival for patients receiving dasatinib was 91% and was not significantly different than the overall survival rate for patients receiving imatinib (90%, P = .1192). Five-year progression-free survival was 85% for patients receiving dasatinib and 86% for patients receiving imatinib.
Grade 3 or 4 adverse events were seen in 15% of patients receiving dasatinib and 11% of patients receiving imatinib. After 5 years, 26 patients had died in each experimental group.
This study was supported by Bristol-Myers Squibb. Eleven investigators reported serving in advisory roles or receiving financial compensation from multiple companies. One investigator had no disclosures to report.
On Twitter @JessCraig_OP
Overall survival and progression-free survival were similar at 5 years in chronic myeloid leukemia patients receiving dasatinib or imatinib, but those given dasatinib had higher major molecular response rates and complete cytogenic response rates without a higher rate of adverse events, based on an extension study of previously published data from the DASISION trial.
The DASISION phase III clinical trial included 519 patients with newly diagnosed and treatment-naive chronic myeloid leukemia. Participants were randomly assigned to receive either 100 mg of dasatinib daily (259 patients) or 400 mg of imatinib daily (260 patients). Dosage was altered on a per-patient basis if adverse events or suboptimal responses were observed. The median average daily dose was 99 mg for dasatinib and 400 mg for imatinib after 5 years.
“Initial results showed that dasatinib had met its primary end point of superior efficacy compared with imatinib and had an acceptable safety profile, leading to its approval for first-line use,” reported Dr. Jorge Cortes of the University of Texas MD Anderson Cancer Center, Houston, and his associates (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.64.8899). Given the faster and deeper molecular responses seen in patients taking dasatinib, “dasatinib should continue to be considered a standard first-line therapy for patients with newly diagnosed” chronic myeloid leukemia, they wrote.
In DASISION (Dasatinib Versus Imatinib Study in Treatment-Naive Chronic Myeloid Leukemia Patients), complete cytogenic response, major molecular response, overall survival, and progression-free survival were measured.
The major molecular response rate was significantly higher for patients receiving dasatinib, compared with patients receiving imatinib (76% vs. 64%, P = .0022).
The rate of complete cytogenic response was 28% for dasatinib and 26% for imatinib.
The 5-year overall survival for patients receiving dasatinib was 91% and was not significantly different than the overall survival rate for patients receiving imatinib (90%, P = .1192). Five-year progression-free survival was 85% for patients receiving dasatinib and 86% for patients receiving imatinib.
Grade 3 or 4 adverse events were seen in 15% of patients receiving dasatinib and 11% of patients receiving imatinib. After 5 years, 26 patients had died in each experimental group.
This study was supported by Bristol-Myers Squibb. Eleven investigators reported serving in advisory roles or receiving financial compensation from multiple companies. One investigator had no disclosures to report.
On Twitter @JessCraig_OP
Overall survival and progression-free survival were similar at 5 years in chronic myeloid leukemia patients receiving dasatinib or imatinib, but those given dasatinib had higher major molecular response rates and complete cytogenic response rates without a higher rate of adverse events, based on an extension study of previously published data from the DASISION trial.
The DASISION phase III clinical trial included 519 patients with newly diagnosed and treatment-naive chronic myeloid leukemia. Participants were randomly assigned to receive either 100 mg of dasatinib daily (259 patients) or 400 mg of imatinib daily (260 patients). Dosage was altered on a per-patient basis if adverse events or suboptimal responses were observed. The median average daily dose was 99 mg for dasatinib and 400 mg for imatinib after 5 years.
“Initial results showed that dasatinib had met its primary end point of superior efficacy compared with imatinib and had an acceptable safety profile, leading to its approval for first-line use,” reported Dr. Jorge Cortes of the University of Texas MD Anderson Cancer Center, Houston, and his associates (J Clin Oncol. 2016 May 23. doi: 10.1200/JCO.2015.64.8899). Given the faster and deeper molecular responses seen in patients taking dasatinib, “dasatinib should continue to be considered a standard first-line therapy for patients with newly diagnosed” chronic myeloid leukemia, they wrote.
In DASISION (Dasatinib Versus Imatinib Study in Treatment-Naive Chronic Myeloid Leukemia Patients), complete cytogenic response, major molecular response, overall survival, and progression-free survival were measured.
The major molecular response rate was significantly higher for patients receiving dasatinib, compared with patients receiving imatinib (76% vs. 64%, P = .0022).
The rate of complete cytogenic response was 28% for dasatinib and 26% for imatinib.
The 5-year overall survival for patients receiving dasatinib was 91% and was not significantly different than the overall survival rate for patients receiving imatinib (90%, P = .1192). Five-year progression-free survival was 85% for patients receiving dasatinib and 86% for patients receiving imatinib.
Grade 3 or 4 adverse events were seen in 15% of patients receiving dasatinib and 11% of patients receiving imatinib. After 5 years, 26 patients had died in each experimental group.
This study was supported by Bristol-Myers Squibb. Eleven investigators reported serving in advisory roles or receiving financial compensation from multiple companies. One investigator had no disclosures to report.
On Twitter @JessCraig_OP
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Patients with chronic myeloid leukemia who received dasatinib experienced higher rates of major molecular response and cytogenic response than did patients treated with imatinib. The improvement in response rate did not come with significantly more adverse events.
Major finding: The major molecular response rate was significantly higher at 76% for patients receiving dasatinib, compared with 64% for patients receiving imatinib (P = .0022).
Data source: A multinational, open-label, phase III trial of 519 patients with treatment-naive myeloid leukemia.
Disclosures: This study was supported by Bristol-Myers Squibb. Eleven investigators reported serving in advisory roles or receiving financial compensation from multiple companies. One investigator had no disclosures to report.