User login
Outpatient treatment of heart failure
- Control the risks for the development and progression of heart failure (HF) by controlling hypertension, diabetes, myocardial ischemia, and tobacco and alcohol use.
- Treat HF with angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, or beta-blockers, used alone or in combination; add spironolactone and carvedilol (or change current beta-blocker to carvedilol) in severe HF; institute aerobic exercise program.
- Control symptoms with diuretics, restricted dietary sodium intake, and digoxin.
- Provide close follow-up that is comprehensive and multidisciplinary, including intensive patient education; self-monitoring of weight, symptoms, and blood pressure; and periodic telephone or in-home follow-up between scheduled office visits.
Heart failure (HF) affects more than 2 million adults in the United States.1 This common, costly, and disabling disorder mainly affects the elderly, with prevalence rates of up to 10% in patients older than 65 years.2,3 The management of HF is responsible for millions of outpatient visits per year,4 is the most common discharge diagnosis for Medicare beneficiaries,5 and accounts for more than 5% of total health care dollars spent.6
Treatment
Major advances in the pharmacologic treatment of heart failure (HF) have emerged in recent years. An approach to the diagnosis and evaluation of HF is described elsewhere.7 This article summarizes the evidence for outpatient treatment of HF. Current intervention trials do not distinguish between systolic and diastolic heart failure; it is therefore unknown whether or how drug therapy should be tailored according to the type of HF. The treatment of cardiac dysrhythmias in the setting of HF is beyond the scope of this article and is presented elsewhere.8Table 1 compares the available outpatient treatments of HF and includes the levels of evidence, numbers needed to treat, and appropriate situations for use. In the remainder of this article, we will discuss pharmacologic and nonpharmacologic management, including identification of ineffective treatments.
TABLE 1
Treatment options in heart failure
| Strength of recommendation (level of evidence)* | Treatment | NNT (Time)† | Use in NYHA class | Comments |
|---|---|---|---|---|
| A (1a) | Angiotensin-converting9-14 enzyme (ACE) inhibitors | 24 (90 days to 2 years) | I–IV | Even moderate doses (equivalent to 10 to 20 mg enalapril per day) provide benefit |
| A (1b) | Angiotensin-receptor blockers (ARBs)15,16 | Similar to ACE inhibitors | I–IV | Useful in patients who do not tolerate ACE inhibitors; may be combined with ACE inhibitors or beta-blockers, but not both |
| A (1a) | Beta-blockers (metoprolol, bisoprolol, carvedilol)17-20 | 24 (1 to 2 years) | I–IV | Usually added to ACE inhibitors or ARBs. May also be useful if concomitant tachydysrhythmias are present and in the post-MI period |
| A (1b) | Carvedilol21 | 18 (10 months) | III–IV | Add carvedilol if not already taking beta-blocker or change current beta-blocker to carvedilol |
| A (1b) | Spironolactone23 | 9 (2 years) | III–IV | NNT = 4 (2 years) to prevent hospitalization for HF. Severe hyperkalemia important safety concern (NNH = 195 over 2 years) |
| A (1b) | Hydralazine + isosorbide dinitrate (ISDN)24,25 | 19 (6 years) | I–IV | Use limited by poor tolerability |
| B (1a) | Digoxin26-28 | N/A | I–IV | No mortality benefit. NNT = 22 to prevent 1 hospitalization over 3 years. Increased risk of hospitalization for digoxin toxicity (NNH = 94 over 3 years) |
| B (2b) | Diuretics (furosemide, bumetanide, torsemide)29-32 | N/A | I–IV | Used for fluid, sodium, and symptom control. No data on mortality benefit |
| A (1b) | Aerobic exercise38-40 | 4 (14 months) | I–IV | Decreases hospitalization for HF (NNT = 5). Even brief symptom-limited exercise in severe HF has benefit in improving quality of life |
| A (1b) | Comprehensive, multi-disciplinary outpatient visits | N/A | I–IV | No mortality benefit. NNT = 5 for 3 months to prevent repeat hospitalization. Includes some combination of intensive education, medication monitoring, individualized diet modification, telephone/home visit follow-up between scheduled outpatient visits |
| B (5) | Dietary sodium restriction8,36,37 | N/A | I–IV | Recommended as standard practice, but no morbidity or mortality data from RCTs |
| C (2a) | Antiplatelet therapy and anticoagulation in HF with sinus rhythm33,35,58 | N/A | N/A | Antiplatelet therapy not useful. No data to support routine anticoagulation, although may be useful in severe HF. Patients with concomitant atrial fibrillation should be anticoagulated if no contraindications |
| D (1b) | Calcium channel blockers (CCBs)46-50 | N/A | N/A | Short-acting CCBs worsen HF. Newer, long-acting CCBs do not worsen HF, but there is no evidence of morbidity or mortality benefit |
| D (1b) | Intermittent positive inotrope (oral or intravenous)(dobutamine, milrinone)51-53 | N/A | N/A | Increased mortality (NNH = 17 over 5 months), increased hospitalizations for worsening HF (NNH = 20), and serious adverse reactions (NNH = 25) |
| *Based on the guidelines for evidence quality outlined by the Center for Evidence-Based Medicine. Available at http://cebm.jr2.ox.ac.uk/docs/levels.html. | ||||
| †NNT = number needed to treat to prevent 1 death over specified time period unless otherwise noted. | ||||
| HF, heart failure; MI, myocardial infarction; NNH, number needed to harm; NNT, number needed to treat; NYHA, New York Heart Association classification; RCT, randomized controlled trial. | ||||
Pharmacologic treatment
Angiotensin-converting enzyme inhibitors. A systematic review9 of 32 trials with a total of 7105 patients demonstrated that mortality rates were lower in patients taking an angiotensin-converting enzyme (ACE) inhibitor than in those not taking one (number needed to treat [NNT] = 24 for > 90 days, meaning that 1 fewer death occurs for every 24 patients who take an ACE inhibitor for more than 90 days). In addition, there is a reduction in the combined endpoints of death and hospitalization because of HF (NNT = 11). Although most of this benefit was realized in the first 90 days of therapy, benefits lasted for 4 to 5 years and were more pronounced in patients categorized in more severe New York Heart Association (NYHA) HF classes10 (class I: no limitation of activities; class II: slight limitation of activity; class III: marked limitation of activity and comfortable only at rest; class IV: symptoms at rest).
Dosage comparison studies demonstrate that HF patients can benefit from even moderate doses of ACE inhibitors. A recent multicenter trial comparing moderate dose enalapril (10 mg twice a day) with a higher dose (30 mg twice a day) in patients with a left ventricular ejection fraction (LVEF) of less than 20% found no differences in mortality at 1 year between the 2 groups.11 In addition, both groups achieved similar increases in functional status and LVEF.
Several trials have demonstrated good tolerability of ACE inhibitors.12-14 Dropout rates of 15% to 30% were similar between patients in the ACE inhibitor and placebo groups, mainly because of side effects, including dizziness, altered taste, hypotension, hyperkalemia, and cough.
Angiotensin-receptor blockers. Angiotensin-receptor blockers (ARBs) reduce all-cause mortality and HF-related hospitalizations in patients with NYHA class II and III HF at rates comparable with those of ACE inhibitors.15,16 Cough is not a side effect of ARBs. Although they are more expensive, ARBs offer a reasonable alternative for patients who do not tolerate ACE inhibitors.
Beta-blockers. The beta-blockers carvedilol, metoprolol, and bisoprolol have a proven mortality benefit for patients with HF.17-19 Pooled results of 6 randomized controlled trials (RCTs), including more than 9000 patients already taking ACE inhibitors, showed a significant reduction in total mortality (NNT = 24 over 1–2 years) and sudden death (NNT = 35), regardless of NYHA classification.20 The average dropout rate of 16% was similar in the betablocker and placebo groups.
Early beta-blocker studies included few NYHA class IV patients until a recent study of the use of carvedilol in severe chronic HF.21 In this study, all patients were taking diuretics plus either an ACE inhibitor or ARB and were permitted to take digoxin, nitrates, hydralazine, spironolactone, or amiodarone. Carvedilol at an average dose of 37 mg per day decreased mortality (NNT = 18 for 10 months) and lowered combined mortality and hospitalization for worsening HF (NNT = 13). Study patients taking carvedilol withdrew from the study at a lower rate (approximately 15%) than placebo.
Because the pharmacologic properties of betablockers vary, clinicians have wondered which are most beneficial. The investigators in a study comparing metoprolol (a beta-1 antagonist) with carvedilol (a beta-1, beta-2, and alpha-1 antagonist) in NYHA class II or III patients found no differences in quality-of-life measures or changes in NYHA classification.22
Spironolactone. The addition of spironolactone to standard care can help patients with severe HF.23 In NYHA class III and IV HF patients, spironolactone at doses ranging from 25 mg every other day to 50 mg per day reduces mortality (NNT = 9 for 2 years), reduces hospitalization from all cardiac causes (NNT = 4), and reduces hospitalization for worsening HF (NNT = 3). The most common serious adverse event in the spironolactone group was severe hyperkalemia (number needed to harm [NNH] = 195). Ten percent of men taking spironolactone experienced breast pain and gynecomastia.
Hydralazine and isosorbide dinitrate. The combination of hydralazine and isosorbide dinitrate (ISDN) reduces mortality in HF patients, but tolerability is an issue. In earlier trials, men with HF symptoms that were optimally controlled with digoxin and diuretics and treated with hydralazine (average dose = 270 mg/day) plus ISDN (average dose = 136 mg/day) had a decrease in all-cause mortality of 28% (NNT = 19 for 6 years).24 A more recent trial comparing hydralazine plus ISDN with enalapril25 (average daily doses of hydralazine = 300 mg/day; ISDN = 160 mg/day; enalapril = 20 mg/day) in NYHA class II–III patients showed no differences in mortality between the 2 groups over 3 years. Tolerability was a problem in these trials; more than 30% of patients stopped taking hydralazine, nitrate, or both.
Digoxin. Digoxin is effective for treating the symptoms of HF in the absence of dysrhythmias but there are no data demonstrating a mortality benefit. Digoxin increases functional capacity in NYHA class II–III patients and heart failure symptoms worsen if digoxin is withdrawn.26 Although there are no differences in all-cause mortality with the use of digoxin, there are fewer hospitalizations due to worsening HF (NNT = 27–114 over 3 years) and a lower rate of clinical deterioration (NNT = 4–75).27 In a randomized trial comparing digoxin and placebo, patients taking digoxin were twice as likely to be hospitalized for suspected digoxin toxicity (2.0% vs 0.9%; P < .001; NNH = 52).28
Diuretics. Diuretics are a mainstay of the symptomatic treatment of heart failure. Short-term studies have shown that diuretics improve the symptoms of sodium and fluid retention and increase exercise tolerance and cardiac function regardless of NYHA classification.29-32 No studies that examine their effects on morbidity and mortality are available.
Antiplatelet therapy and anticoagulation. Patients with HF have an increased risk for thromboembolic events of 1.6% to 3.2% per year.33 One systematic review concluded that antiplatelet therapy is not useful in preventing thromboembolism in patients with HF in sinus rhythm and may even be harmful.34 Another systematic review also concluded that the data do not support the routine use of anticoagulants (eg, warfarin) in patients with HF and sinus rhythm.35 Anticoagulation may be beneficial, however, if there is echocardiographic visualization of a left ventricular thrombus or in cases of “severe” HF or concomitant atrial fibrillation.35
Nonpharmacologic management
Dietary sodium restriction. There is consensus that dietary sodium restriction is important in the treatment of HF36 and is recommended in published guidelines.8,37 Sodium restriction assists with fluid volume control and minimizes the dosages of HF drugs used. These recommendations are based on the retention of sodium and water in symptomatic HF. No studies, however, have examined the effect of dietary sodium restriction on morbidity or mortality, either alone or in combination with pharmacologic treatments.
Exercise training. Moderate exercise training improves quality of life and decreases mortality in patients with stable chronic HF. A recent RCT demonstrated a decrease in mortality (NNT = 4 for 14 months) and hospital readmission for HF (NNT = 5) with only moderate exercise on a stationary bicycle (60% of maximum exercise capacity) for 2 to 3 hours per week.38 Other studies have demonstrated improvements in physiologic markers39 and in quality-of-life ratings with short-term, symptom-limited exercise.40
Multidisciplinary or case-management approach. A case-based or disease-management approach to patients with HF decreases the frequency of unplanned and repeat hospitalizations, increases functional status, and increases quality of life.41 Even a single in-home visit by a clinical pharmacist and a nurse results in fewer unplanned readmissions and fewer days of hospitalization up to 18 months after discharge.42,43 A small study of 27 patients in a Veterans Affairs hospital demonstrated that patient instruction in the self-monitoring of weight and blood pressure, combined with frequent telephone follow-up from a nurse, lowered repeat hospitalizations over 1 year, with the effect more pronounced in patients with more severe NYHA classifications.44 A large RCT demonstrated that a multidisciplinary management approach (intensive patient education about HF and its treatment, dietary assessment and instruction, medication analysis and elimination of unnecessary medications, and telephone and home visit follow-up) results in fewer hospitalizations (NNT = 5 for 3 months) and reduced costs of care.45
Treatments that have no benefit or are harmful
Calcium-channel blockers. Although some of the newer, longer-acting calcium-channel blockers (CCBs) appear to be safe in the treatment of heart failure,46-49 no trials are available demonstrating that they lower mortality, decrease hospitalizations, or improve quality of life in patients with a failing heart. Older, short-acting CCBs can worsen HF.50
Positive inotropic therapy. Intermittent positive inotropic therapy, either orally (milrinone) or intravenously (dobutamine), should be avoided. Although short-term studies have shown some increase in cardiac function and symptoms,51 long-term studies demonstrate no mortality benefit.52 One RCT of milrinone demonstrated an increase in mortality (NNH = 17 for 5 months), an increased rate of hospitalization for worsening HF (NNH = 20), and more serious side effects (NNH = 25).53
Prognosis
Despite the increased longevity in Western developed nations and increased survival from coronary artery disease over recent decades, the overall prognosis of HF has improved very little.6,54 Mortality data derived from several different sources, the largest being the Framingham Heart Study,2,55 have shown that HF remains highly lethal, with a 5-year survival rate of 25% in men and 38% in women with NYHA II–IV heart failure. Mortality data from the placebo arms of intervention trials show an average 1-year mortality of 18%.9,17,19,20,56 A recent population-based study of patients with a new diagnosis of HF showed survival rates of only 62% at 12 months and 57% at 18 months.57 Despite these dismal population-based data, predicting the likelihood of survival in individuals with HF is largely unreliable.8 Estimating individual prognosis is only somewhat useful in making end-of-life care and hospice decisions for patients with very advanced HF. Table 2 summarizes specific prognostic factors for patients with HF.
TABLE 2
Factors that affect prognosis in patients with heart failure (HF)
| Factor | Result | Comment |
|---|---|---|
| Age1,2,6,59 | Increasing age and age older than 55 years decreases survival | Framingham data: survival rates of older women are twice as long as those of older men despite significant age difference (women: 72 years; men: 68 years). |
| Sex56,60-62 | Mortality higher in men | Women are underrepresented in HF trials and frequently have HF associated with diastolic dysfunction. Women rate their quality of inpatient care lower than men do. |
| Race63-65 | African Americans have higher mortality rates and higher rates of recurrent hospitalization | HF affects approximately 3% of all African Americans. They develop symptoms at an earlier tage. The disease progresses more rapidly than in whites. African Americans are underrepresented in HF trials. |
| Attending physician specialty66-68 | No difference in 6-month cardiac and all-cause mortality between family physician or generalist and cardiologist care | Family physician or generalist: Twofold increased risk of readmission in 6 months; tend to overestimate risks of ACE inhibitors and therefore under-prescribe them. |
| Cardiologist (as attending or consultant): Increased testing, hospital lengths of stay, and hospital charges, but better patient-perceived quality of life. |
Suggested management of patients with heart failure
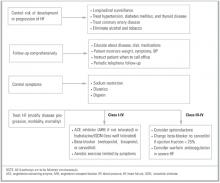
Although the optimal sequence of pharmacologic interventions for treating HF has not been examined in RCTs, recommendations can be made on the basis of existing evidence in HF management (Figure). This approach can be divided into 4 steps performed simultaneously: (1) control risks for the development and progression of HF (treat concomitant diseases); (2) HF treatment; (3) symptom control; (4) close follow-up.
Control risks. Risks for the development and worsening of HF should be addressed as described else-where.8 Steps include longitudinal surveillance; identification and treatment of hypertension, diabetes and thyroid diseases; management of atherosclerotic and coronary artery disease and myocardial ischemia; and the elimination of alcohol and tobacco use.
Heart failure treatment. All patients with HF should take a drug or a combination of drugs that affects the disease process. Drugs shown by the preponderance of evidence to decrease morbidity and mortality include ACE inhibitors, beta-blockers, and ARBs. For most HF patients, regardless of NYHA class, ACE inhibitors should be the initial baseline treatment because of their proven track record and the observation that most recent HF trials include patients who are already taking these medications. ARBs are similar in efficacy to ACE inhibitors and, therefore, are an adequate alternative when ACE inhibitors are not tolerated. Beta-blockers (metoprolol and bisoprolol) added to ACE inhibitors are also useful as a baseline treatment in most HF patients and may be especially useful in the case of tachydysrhythmias and in the postmyocardial infarction period.
For severe HF (NYHA III–IV), spironolactone and carvedilol are useful additions to baseline drug therapy. Carvedilol may be added if a beta-blocker is not currently used. If the patient is currently taking a beta-blocker, the drug should be discontinued before the patient is switched to carvedilol.
The hydralazine–nitrate combination has been proved effective, but tolerability and ease-of-use issues limit its usefulness. No data are available to support the use of nitrates other than isosorbide dinitrate. Nitrates may be useful, however, for concomitant chronic myocardial ischemia.
Patients with stable HF should be encouraged to begin and maintain a regular aerobic exercise program. The level of exercise can range from brief, symptom-limited exercise to moderate exercise (60% capacity) for 3 or more hours per week.
The use of antiplatelet therapy or the routine use of anticoagulation in patients with HF who are in sinus rhythm provides no benefit. Anticoagulation may be useful if the patient has severe HF or has a known mural thrombus. HF patients with atrial fibrillation should be considered for antiplatelet or anticoagulation therapy as described elsewhere.58
Short-acting CCBs may worsen HF. No data support the use of any CCB in the primary treatment of HF. Similarly, intermittent use of milrinone or dobutamine is not indicated.
Symptom control. The symptomatic treatment of HF includes the use of diuretics and dietary sodium restriction to control sodium levels and volume status. Symptom control should be accomplished along with the pharmacologic disease management outlined above.
The role of digoxin in the failing heart without dysrhythmias is unclear. Digoxin may be most useful in symptom control, as it reduces hospitalizations attributed to worsening HF. This benefit must be balanced against an increased risk of hospitalization caused by digoxin toxicity. Patients who are already taking digoxin should probably continue to do so. The role of digoxin in newly diagnosed HF patients is unknown.
Close follow-up. Comprehensive follow-up, with the patient as a more active participant and in which care is extended beyond the hospital or office to the home, is a key strategy in the long-term care of HF patients. This aspect of HF management should include educating patients about their disease process and their dietary and pharmacologic treatments; teaching them how to monitor their weight, symptoms, and blood pressure and to understand when to seek care; and following up periodically by telephone between scheduled office visits.
FIGURE
Management of adults with heart failure
1. Schocken DD, Arrieta MI, Leaverton PE, Ross EA. Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol 1992;20:301-6.
2. McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure. The Framingham study. N Engl J Med 1971;285:1442-6.
3. Kannel WB, Plehn JF, Cupples LA. Cardiac failure and sudden death in the Framingham Study. Am Heart J 1988;115:869-75.
4. Schappert SM. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 1997. Vital Health Stat 13. 1999;No. 143:i-iv,1-39.
5. Krumholz HM, Parent EM, Tu N, et al. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med 1997;157:99-104.
6. McMurray JJ, Stewart S. Heart failure. Epidemiology, etiology, and prognosis of heart failure. Heart 2000;83:596-602.
7. Mair FS, Lloyd-Williams F. Evaluation of suspected left ventricular systolic dysfunction. J Fam Pract 2002;51:466-471.
8. Hunt SA, Baker DW, Chin MH, et al. ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). 2001. American College of Cardiology Web site. Available at: http://www.acc.org/clinical/guidelines/failure/hf_index.htm.
9. Garg R, Yusuf S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. JAMA 1995;273:1450-6.
10. The Criteria Committee of the New York Heart Association. Diseases of the Heart and Blood Vessels: Nomenclature and Criteria for Diagnosis. 6th ed. Boston, MA: Little, Brown; 1964.
11. Nanas JN, Alexopoulus G, Anastasiou-Nana MI, et al. Outcome of patients with congestive heart failure treated with standard versus high doses of enalapril: a multicenter study. J Am Coll Cardiol 2000;36:2090-5.
12. CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. N Engl J Med 1987;316:1429-35.
13. SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1991;325:293-302.
14. Pfeffer MA, Braunwald E, Moye LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement (SAVE) trial. N Engl J Med 1992;327:659-77.
15. Pitt B, Poole-Wilson PA, Segal R, et al. Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: a randomized trial. The losartan heart failure survival study (ELITE II). Lancet 2000;355:1582-7.
16. Cohn JN, Tognoni G. for the Valsartan Heart Failure Trial Investigators. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med 2001;345:1667-75.
17. Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. N Engl J Med 1996;334:1349-55.
18. MERIT-HF Study Group. Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet 1999;353:2001-7.
19. CIBIS-II Investigators. The cardiac insufficiency bisoprolol study II (CIBIS-II): a randomized trial. Lancet 1999;353:9-13.
20. Lee S, Spencer A. Beta-blockers to reduce mortality in patients with systolic dysfunction. J Fam Pract 2001;6:499-504.
21. Packer M, Coats AJS, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001;344:1651-8.
22. Metra M, Giubbini R, Nodari S, et al. Differential effects of betablockers in patients with heart failure: a prospective, randomized, double-blind comparison of the long-term effects of metoprolol versus carvedilol. Circulation 2000;102:546-51.
23. Pitt B, Zannad F, Remm WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med 1999;341:707-17.
24. Cohn J, Archibald DG, Ziesche S, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. N Engl J Med 1986;314:1547-52.
25. Cohn JN, Johnson G, Ziesche S, et al. Comparison of enalapril with hydralazine–isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med 1991;325:303-10.
26. Packer M, Gheorghiade M, Young JB, et al. Withdrawal of digoxin from patients with chronic heart failure treated with angiotensin-converting enzyme inhibitors. N Engl J Med 1993;329:1-7.
27. Hood WB, Jr, Dans A, Guyatt GH, Jaescke R, McMurray JV. Digitalis for treatment of congestive heart failure in patients in sinus rhythm. In: The Cochrane Library, Issue 4, 2001. Oxford, England: Update Software.
28. The Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med 1997;336:525-33.
29. Brater DC. Diuretic therapy. N Engl J Med 1998;339:387-95.
30. Cody RJ, Kubo SH, Pickworth KK. Diuretic treatment for the sodium retention of congestive heart failure. Arch Intern Med 1994;154:1905-14.
31. Wilson JR, Reichek N, Dunkman WB, Goldberg S. Effect of diuresis on the performance of the failing left ventricle in man. Am J Med 1981;70:234-9.
32. Richardson A, Bayliss J, Scriven AJ, Parameshwar J, Poole-Wilson PA, Sutton GC. Double-blind comparison of captopril alone against furosemide plus amiloride in mild heart failure. Lancet 1987;2:709-11.
33. Dunkman WB. Thromboembolism and antithrombotic therapy in congestive heart failure. J Cardiovasc Risk 1995;2:107-17.
34. Lip GYH, Gibbs CR. Antiplatelet agents versus control or anticoagulation for heart failure in sinus rhythm. In: The Cochrane Library, Issue 4, 2001. Oxford, England: Update Software.
35. Lip GYH, Gibbs CR. Anticoagulation for heart failure in sinus rhythm. In: The Cochrane Library, Issue 4, 2001. Oxford, England: Update Software.
36. Lenihan DJ, Uretsky BF. Nonpharmacologic treatment of heart failure in the elderly. Clin Geriatr Med 2000;16:477-87.
37. Williams JF, Bristow MR, Fowler MB, et al. Guidelines for the evaluation and management of chronic heart failure. Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Evaluation and Management of Heart Failure). Circulation 1995;92:2764-84.
38. Belardinelli R, Georgiou D, Ciance G, Purcaro A. Randomized controlled trial of long-term moderate exercise training in chronic heart failure. Effects on functional capacity, quality of life, and clinical outcome. Circulation 1999;99:1173-82.
39. Sullivan MJ, Higginbotham MB, Cobb FR. Exercise training in patients with severe left ventricular dysfunction. Hemodynamic and metabolic effects. Circulation 1988;78:506-15.
40. Tokmakova M, Dobreva B, Kostianev S. Effects of short-term exercise training in patients with heart failure. Folia Medica (Plovdiv) 1999;41:68-71. Abstract.
41. Rich MW. Heart failure disease management: a critical review. J Card Fail 1999;5:64-75.
42. Stewart S, Pearson S, Horowitz JD. Effects of a home-based intervention among patients with congestive heart failure discharged from acute hospital care. Arch Intern Med 1998;158:1067-72.
43. Stewart S, Vandenbroek AJ, Pearson S, Horowitz JD. Prolonged beneficial effects of a home-based intervention on unplanned readmissions and mortality among patients with congestive heart failure. Arch Intern Med 1999;159:257-61.
44. Shah NB, Der E, Ruggerio C, Heidenreich PA, Massie BM. Prevention of hospitalizations for heart failure with an interactive home monitoring program. Am Heart J 1998;135:373-8.
45. Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med 1995;333:1190-5.
46. Levine TN, Bernink PJ, Caspi A, et al. Effect of mibefradil, a T-type calcium channel blocker, on morbidity and mortality in moderate to severe congestive heart failure: the MACH-1 study. Mortality Assessment in Congestive Heart Failure Trial. Circulation 2000;101:758-64.
47. Mahon N, McKenna WJ. Calcium-channel blockers in cardiac failure. Prog Card Dis 1998;41:191-206.
48. deVries RJ, van Veldhuisen DJ, Dunselman PH. Efficacy and safety of calcium channel blockers in heart failure: focus on recent trials with second-generation dihydropyridines. Am Heart J 2000;139(2 pt 1):185-94.
49. O’Connor CM, Carson PE, Miller AB, et al. Effect of amlodipine on mode of death among patients with advanced heart failure in the PRAISE trial. Prospective randomized amlodipine survival evaluation. Am J Cardiol 1998;82:881-7.
50. Packer M, Kessler PD, Lee WH. Calcium-channel blockade in the management of severe chronic congestive heart failure: a bridge too far. Circulation 1987;75:V56-64.
51. Anderson JL. Hemodynamic and clinical benefits with intravenous milrinone in severe chronic heart failure: results of a multicenter study in the United States. Am Heart J 1991;121:1956-64.
52. Elis A, Bental T, Kimchi O, Ravid M, Lishner M. Intermittent dobutamine treatment in patients with chronic refractory congestive heart failure: a randomized, double-blind, placebo-controlled study. Clin Pharmacol Ther 1998;63:682-5.
53. Packer M, Carver JR, Rodeheffer RJ, et al. Effect of oral milrinone on mortality in severe chronic heart failure. The PROMISE Study Research Group. N Engl J Med 1991;325:1468-75.
54. Cleland JGF, Clark A. Has the survival of the heart failure population changed? Lessons from trials. Am J Cardiol 1999;83:112D-19D.
55. Ho KKL, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: the Framingham study. J Am Coll Cardiol 1993;22(suppl A):6A-13A.
56. Clinical Quality Improvement Network Investigators. Mortality risk and patterns of practice in 4606 acute care patients with congestive heart failure. The relative importance of age, sex, and medical therapy. Arch Intern Med 1996;156:1669-73.
57. Cowie MR, Wood DA, Coats AJ, et al. Survival of patients with a new diagnosis of heart failure: a population-based study. Heart 2000;83:505-10.
58. Albers GW, Dalen JE, Laupacis A, Manning WJ, Petersen P, Singer DE. Antithrombotic therapy in atrial fibrillation. Chest 2001;119:194S-206S.
59. Doba N, Tomiyama H, Nakayama T. Drugs, heart failure and quality of life: what are we achieving? What should we be trying to achieve? Drugs Aging 1999;14:153-63.
60. Petrie MC, Dawson NF, Murdoch DR, Davie AP, McMurray JJV. Failure of women’s hearts. Circulation 1999;99:2334-41.
61. Burns RB, McCarthy EP, Moskowitz MA, Ash A, Kane RL, Finch M. Outcomes for older men and women with congestive heart failure. J Am Geriatr Soc 1997;45:276-80.
62. Chin MH, Goldman L. Gender differences in 1-year survival and quality of life among patients admitted with congestive heart failure. Med Care 1998;36:1033-46.
63. Dries DL, Exner DV, Gersh BJ, Cooper HA, Carson PE, Domanski MJ. Racial differences in the outcome of left ventricular dysfunction [published erratum appears in N Engl J Med 1999; 341:298]. N Engl J Med 1999;340:609-16.
64. Alexander M, Grumbach K, Remy L, Rowell R, Massie BM. Congestive heart failure hospitalizations and survival in California: patterns according to race/ethnicity. Am Heart J 1999;137:919-27.
65. Philbin EF, DiSalvo TG. Influence of race and gender on care process, resource use, and hospital-based outcomes in congestive heart failure. Am J Cardiol 1998;82:76-81.
66. Reis SE, Holubkov R, Edmundowicz D, et al. Treatment of patients admitted to the hospital with congestive heart failure: specialty-related disparities in practice patterns and outcomes. J Am Coll Cardiol 1997;30:733-8.
67. Philbin EF, Weil HFC, Erb TA, Jenkins PL. Cardiology or primary care for heart failure in the community setting. Process of care and clinical outcomes. Chest 1999;116:346-54.
68. Baker DW, Hayes RP, Massie BM, Craig CA. Variations in family physicians’ and cardiologists’ care for patients with heart failure. Am Heart J 1999;138:826-34.
- Control the risks for the development and progression of heart failure (HF) by controlling hypertension, diabetes, myocardial ischemia, and tobacco and alcohol use.
- Treat HF with angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, or beta-blockers, used alone or in combination; add spironolactone and carvedilol (or change current beta-blocker to carvedilol) in severe HF; institute aerobic exercise program.
- Control symptoms with diuretics, restricted dietary sodium intake, and digoxin.
- Provide close follow-up that is comprehensive and multidisciplinary, including intensive patient education; self-monitoring of weight, symptoms, and blood pressure; and periodic telephone or in-home follow-up between scheduled office visits.
Heart failure (HF) affects more than 2 million adults in the United States.1 This common, costly, and disabling disorder mainly affects the elderly, with prevalence rates of up to 10% in patients older than 65 years.2,3 The management of HF is responsible for millions of outpatient visits per year,4 is the most common discharge diagnosis for Medicare beneficiaries,5 and accounts for more than 5% of total health care dollars spent.6
Treatment
Major advances in the pharmacologic treatment of heart failure (HF) have emerged in recent years. An approach to the diagnosis and evaluation of HF is described elsewhere.7 This article summarizes the evidence for outpatient treatment of HF. Current intervention trials do not distinguish between systolic and diastolic heart failure; it is therefore unknown whether or how drug therapy should be tailored according to the type of HF. The treatment of cardiac dysrhythmias in the setting of HF is beyond the scope of this article and is presented elsewhere.8Table 1 compares the available outpatient treatments of HF and includes the levels of evidence, numbers needed to treat, and appropriate situations for use. In the remainder of this article, we will discuss pharmacologic and nonpharmacologic management, including identification of ineffective treatments.
TABLE 1
Treatment options in heart failure
| Strength of recommendation (level of evidence)* | Treatment | NNT (Time)† | Use in NYHA class | Comments |
|---|---|---|---|---|
| A (1a) | Angiotensin-converting9-14 enzyme (ACE) inhibitors | 24 (90 days to 2 years) | I–IV | Even moderate doses (equivalent to 10 to 20 mg enalapril per day) provide benefit |
| A (1b) | Angiotensin-receptor blockers (ARBs)15,16 | Similar to ACE inhibitors | I–IV | Useful in patients who do not tolerate ACE inhibitors; may be combined with ACE inhibitors or beta-blockers, but not both |
| A (1a) | Beta-blockers (metoprolol, bisoprolol, carvedilol)17-20 | 24 (1 to 2 years) | I–IV | Usually added to ACE inhibitors or ARBs. May also be useful if concomitant tachydysrhythmias are present and in the post-MI period |
| A (1b) | Carvedilol21 | 18 (10 months) | III–IV | Add carvedilol if not already taking beta-blocker or change current beta-blocker to carvedilol |
| A (1b) | Spironolactone23 | 9 (2 years) | III–IV | NNT = 4 (2 years) to prevent hospitalization for HF. Severe hyperkalemia important safety concern (NNH = 195 over 2 years) |
| A (1b) | Hydralazine + isosorbide dinitrate (ISDN)24,25 | 19 (6 years) | I–IV | Use limited by poor tolerability |
| B (1a) | Digoxin26-28 | N/A | I–IV | No mortality benefit. NNT = 22 to prevent 1 hospitalization over 3 years. Increased risk of hospitalization for digoxin toxicity (NNH = 94 over 3 years) |
| B (2b) | Diuretics (furosemide, bumetanide, torsemide)29-32 | N/A | I–IV | Used for fluid, sodium, and symptom control. No data on mortality benefit |
| A (1b) | Aerobic exercise38-40 | 4 (14 months) | I–IV | Decreases hospitalization for HF (NNT = 5). Even brief symptom-limited exercise in severe HF has benefit in improving quality of life |
| A (1b) | Comprehensive, multi-disciplinary outpatient visits | N/A | I–IV | No mortality benefit. NNT = 5 for 3 months to prevent repeat hospitalization. Includes some combination of intensive education, medication monitoring, individualized diet modification, telephone/home visit follow-up between scheduled outpatient visits |
| B (5) | Dietary sodium restriction8,36,37 | N/A | I–IV | Recommended as standard practice, but no morbidity or mortality data from RCTs |
| C (2a) | Antiplatelet therapy and anticoagulation in HF with sinus rhythm33,35,58 | N/A | N/A | Antiplatelet therapy not useful. No data to support routine anticoagulation, although may be useful in severe HF. Patients with concomitant atrial fibrillation should be anticoagulated if no contraindications |
| D (1b) | Calcium channel blockers (CCBs)46-50 | N/A | N/A | Short-acting CCBs worsen HF. Newer, long-acting CCBs do not worsen HF, but there is no evidence of morbidity or mortality benefit |
| D (1b) | Intermittent positive inotrope (oral or intravenous)(dobutamine, milrinone)51-53 | N/A | N/A | Increased mortality (NNH = 17 over 5 months), increased hospitalizations for worsening HF (NNH = 20), and serious adverse reactions (NNH = 25) |
| *Based on the guidelines for evidence quality outlined by the Center for Evidence-Based Medicine. Available at http://cebm.jr2.ox.ac.uk/docs/levels.html. | ||||
| †NNT = number needed to treat to prevent 1 death over specified time period unless otherwise noted. | ||||
| HF, heart failure; MI, myocardial infarction; NNH, number needed to harm; NNT, number needed to treat; NYHA, New York Heart Association classification; RCT, randomized controlled trial. | ||||
Pharmacologic treatment
Angiotensin-converting enzyme inhibitors. A systematic review9 of 32 trials with a total of 7105 patients demonstrated that mortality rates were lower in patients taking an angiotensin-converting enzyme (ACE) inhibitor than in those not taking one (number needed to treat [NNT] = 24 for > 90 days, meaning that 1 fewer death occurs for every 24 patients who take an ACE inhibitor for more than 90 days). In addition, there is a reduction in the combined endpoints of death and hospitalization because of HF (NNT = 11). Although most of this benefit was realized in the first 90 days of therapy, benefits lasted for 4 to 5 years and were more pronounced in patients categorized in more severe New York Heart Association (NYHA) HF classes10 (class I: no limitation of activities; class II: slight limitation of activity; class III: marked limitation of activity and comfortable only at rest; class IV: symptoms at rest).
Dosage comparison studies demonstrate that HF patients can benefit from even moderate doses of ACE inhibitors. A recent multicenter trial comparing moderate dose enalapril (10 mg twice a day) with a higher dose (30 mg twice a day) in patients with a left ventricular ejection fraction (LVEF) of less than 20% found no differences in mortality at 1 year between the 2 groups.11 In addition, both groups achieved similar increases in functional status and LVEF.
Several trials have demonstrated good tolerability of ACE inhibitors.12-14 Dropout rates of 15% to 30% were similar between patients in the ACE inhibitor and placebo groups, mainly because of side effects, including dizziness, altered taste, hypotension, hyperkalemia, and cough.
Angiotensin-receptor blockers. Angiotensin-receptor blockers (ARBs) reduce all-cause mortality and HF-related hospitalizations in patients with NYHA class II and III HF at rates comparable with those of ACE inhibitors.15,16 Cough is not a side effect of ARBs. Although they are more expensive, ARBs offer a reasonable alternative for patients who do not tolerate ACE inhibitors.
Beta-blockers. The beta-blockers carvedilol, metoprolol, and bisoprolol have a proven mortality benefit for patients with HF.17-19 Pooled results of 6 randomized controlled trials (RCTs), including more than 9000 patients already taking ACE inhibitors, showed a significant reduction in total mortality (NNT = 24 over 1–2 years) and sudden death (NNT = 35), regardless of NYHA classification.20 The average dropout rate of 16% was similar in the betablocker and placebo groups.
Early beta-blocker studies included few NYHA class IV patients until a recent study of the use of carvedilol in severe chronic HF.21 In this study, all patients were taking diuretics plus either an ACE inhibitor or ARB and were permitted to take digoxin, nitrates, hydralazine, spironolactone, or amiodarone. Carvedilol at an average dose of 37 mg per day decreased mortality (NNT = 18 for 10 months) and lowered combined mortality and hospitalization for worsening HF (NNT = 13). Study patients taking carvedilol withdrew from the study at a lower rate (approximately 15%) than placebo.
Because the pharmacologic properties of betablockers vary, clinicians have wondered which are most beneficial. The investigators in a study comparing metoprolol (a beta-1 antagonist) with carvedilol (a beta-1, beta-2, and alpha-1 antagonist) in NYHA class II or III patients found no differences in quality-of-life measures or changes in NYHA classification.22
Spironolactone. The addition of spironolactone to standard care can help patients with severe HF.23 In NYHA class III and IV HF patients, spironolactone at doses ranging from 25 mg every other day to 50 mg per day reduces mortality (NNT = 9 for 2 years), reduces hospitalization from all cardiac causes (NNT = 4), and reduces hospitalization for worsening HF (NNT = 3). The most common serious adverse event in the spironolactone group was severe hyperkalemia (number needed to harm [NNH] = 195). Ten percent of men taking spironolactone experienced breast pain and gynecomastia.
Hydralazine and isosorbide dinitrate. The combination of hydralazine and isosorbide dinitrate (ISDN) reduces mortality in HF patients, but tolerability is an issue. In earlier trials, men with HF symptoms that were optimally controlled with digoxin and diuretics and treated with hydralazine (average dose = 270 mg/day) plus ISDN (average dose = 136 mg/day) had a decrease in all-cause mortality of 28% (NNT = 19 for 6 years).24 A more recent trial comparing hydralazine plus ISDN with enalapril25 (average daily doses of hydralazine = 300 mg/day; ISDN = 160 mg/day; enalapril = 20 mg/day) in NYHA class II–III patients showed no differences in mortality between the 2 groups over 3 years. Tolerability was a problem in these trials; more than 30% of patients stopped taking hydralazine, nitrate, or both.
Digoxin. Digoxin is effective for treating the symptoms of HF in the absence of dysrhythmias but there are no data demonstrating a mortality benefit. Digoxin increases functional capacity in NYHA class II–III patients and heart failure symptoms worsen if digoxin is withdrawn.26 Although there are no differences in all-cause mortality with the use of digoxin, there are fewer hospitalizations due to worsening HF (NNT = 27–114 over 3 years) and a lower rate of clinical deterioration (NNT = 4–75).27 In a randomized trial comparing digoxin and placebo, patients taking digoxin were twice as likely to be hospitalized for suspected digoxin toxicity (2.0% vs 0.9%; P < .001; NNH = 52).28
Diuretics. Diuretics are a mainstay of the symptomatic treatment of heart failure. Short-term studies have shown that diuretics improve the symptoms of sodium and fluid retention and increase exercise tolerance and cardiac function regardless of NYHA classification.29-32 No studies that examine their effects on morbidity and mortality are available.
Antiplatelet therapy and anticoagulation. Patients with HF have an increased risk for thromboembolic events of 1.6% to 3.2% per year.33 One systematic review concluded that antiplatelet therapy is not useful in preventing thromboembolism in patients with HF in sinus rhythm and may even be harmful.34 Another systematic review also concluded that the data do not support the routine use of anticoagulants (eg, warfarin) in patients with HF and sinus rhythm.35 Anticoagulation may be beneficial, however, if there is echocardiographic visualization of a left ventricular thrombus or in cases of “severe” HF or concomitant atrial fibrillation.35
Nonpharmacologic management
Dietary sodium restriction. There is consensus that dietary sodium restriction is important in the treatment of HF36 and is recommended in published guidelines.8,37 Sodium restriction assists with fluid volume control and minimizes the dosages of HF drugs used. These recommendations are based on the retention of sodium and water in symptomatic HF. No studies, however, have examined the effect of dietary sodium restriction on morbidity or mortality, either alone or in combination with pharmacologic treatments.
Exercise training. Moderate exercise training improves quality of life and decreases mortality in patients with stable chronic HF. A recent RCT demonstrated a decrease in mortality (NNT = 4 for 14 months) and hospital readmission for HF (NNT = 5) with only moderate exercise on a stationary bicycle (60% of maximum exercise capacity) for 2 to 3 hours per week.38 Other studies have demonstrated improvements in physiologic markers39 and in quality-of-life ratings with short-term, symptom-limited exercise.40
Multidisciplinary or case-management approach. A case-based or disease-management approach to patients with HF decreases the frequency of unplanned and repeat hospitalizations, increases functional status, and increases quality of life.41 Even a single in-home visit by a clinical pharmacist and a nurse results in fewer unplanned readmissions and fewer days of hospitalization up to 18 months after discharge.42,43 A small study of 27 patients in a Veterans Affairs hospital demonstrated that patient instruction in the self-monitoring of weight and blood pressure, combined with frequent telephone follow-up from a nurse, lowered repeat hospitalizations over 1 year, with the effect more pronounced in patients with more severe NYHA classifications.44 A large RCT demonstrated that a multidisciplinary management approach (intensive patient education about HF and its treatment, dietary assessment and instruction, medication analysis and elimination of unnecessary medications, and telephone and home visit follow-up) results in fewer hospitalizations (NNT = 5 for 3 months) and reduced costs of care.45
Treatments that have no benefit or are harmful
Calcium-channel blockers. Although some of the newer, longer-acting calcium-channel blockers (CCBs) appear to be safe in the treatment of heart failure,46-49 no trials are available demonstrating that they lower mortality, decrease hospitalizations, or improve quality of life in patients with a failing heart. Older, short-acting CCBs can worsen HF.50
Positive inotropic therapy. Intermittent positive inotropic therapy, either orally (milrinone) or intravenously (dobutamine), should be avoided. Although short-term studies have shown some increase in cardiac function and symptoms,51 long-term studies demonstrate no mortality benefit.52 One RCT of milrinone demonstrated an increase in mortality (NNH = 17 for 5 months), an increased rate of hospitalization for worsening HF (NNH = 20), and more serious side effects (NNH = 25).53
Prognosis
Despite the increased longevity in Western developed nations and increased survival from coronary artery disease over recent decades, the overall prognosis of HF has improved very little.6,54 Mortality data derived from several different sources, the largest being the Framingham Heart Study,2,55 have shown that HF remains highly lethal, with a 5-year survival rate of 25% in men and 38% in women with NYHA II–IV heart failure. Mortality data from the placebo arms of intervention trials show an average 1-year mortality of 18%.9,17,19,20,56 A recent population-based study of patients with a new diagnosis of HF showed survival rates of only 62% at 12 months and 57% at 18 months.57 Despite these dismal population-based data, predicting the likelihood of survival in individuals with HF is largely unreliable.8 Estimating individual prognosis is only somewhat useful in making end-of-life care and hospice decisions for patients with very advanced HF. Table 2 summarizes specific prognostic factors for patients with HF.
TABLE 2
Factors that affect prognosis in patients with heart failure (HF)
| Factor | Result | Comment |
|---|---|---|
| Age1,2,6,59 | Increasing age and age older than 55 years decreases survival | Framingham data: survival rates of older women are twice as long as those of older men despite significant age difference (women: 72 years; men: 68 years). |
| Sex56,60-62 | Mortality higher in men | Women are underrepresented in HF trials and frequently have HF associated with diastolic dysfunction. Women rate their quality of inpatient care lower than men do. |
| Race63-65 | African Americans have higher mortality rates and higher rates of recurrent hospitalization | HF affects approximately 3% of all African Americans. They develop symptoms at an earlier tage. The disease progresses more rapidly than in whites. African Americans are underrepresented in HF trials. |
| Attending physician specialty66-68 | No difference in 6-month cardiac and all-cause mortality between family physician or generalist and cardiologist care | Family physician or generalist: Twofold increased risk of readmission in 6 months; tend to overestimate risks of ACE inhibitors and therefore under-prescribe them. |
| Cardiologist (as attending or consultant): Increased testing, hospital lengths of stay, and hospital charges, but better patient-perceived quality of life. |
Suggested management of patients with heart failure
Although the optimal sequence of pharmacologic interventions for treating HF has not been examined in RCTs, recommendations can be made on the basis of existing evidence in HF management (Figure). This approach can be divided into 4 steps performed simultaneously: (1) control risks for the development and progression of HF (treat concomitant diseases); (2) HF treatment; (3) symptom control; (4) close follow-up.
Control risks. Risks for the development and worsening of HF should be addressed as described else-where.8 Steps include longitudinal surveillance; identification and treatment of hypertension, diabetes and thyroid diseases; management of atherosclerotic and coronary artery disease and myocardial ischemia; and the elimination of alcohol and tobacco use.
Heart failure treatment. All patients with HF should take a drug or a combination of drugs that affects the disease process. Drugs shown by the preponderance of evidence to decrease morbidity and mortality include ACE inhibitors, beta-blockers, and ARBs. For most HF patients, regardless of NYHA class, ACE inhibitors should be the initial baseline treatment because of their proven track record and the observation that most recent HF trials include patients who are already taking these medications. ARBs are similar in efficacy to ACE inhibitors and, therefore, are an adequate alternative when ACE inhibitors are not tolerated. Beta-blockers (metoprolol and bisoprolol) added to ACE inhibitors are also useful as a baseline treatment in most HF patients and may be especially useful in the case of tachydysrhythmias and in the postmyocardial infarction period.
For severe HF (NYHA III–IV), spironolactone and carvedilol are useful additions to baseline drug therapy. Carvedilol may be added if a beta-blocker is not currently used. If the patient is currently taking a beta-blocker, the drug should be discontinued before the patient is switched to carvedilol.
The hydralazine–nitrate combination has been proved effective, but tolerability and ease-of-use issues limit its usefulness. No data are available to support the use of nitrates other than isosorbide dinitrate. Nitrates may be useful, however, for concomitant chronic myocardial ischemia.
Patients with stable HF should be encouraged to begin and maintain a regular aerobic exercise program. The level of exercise can range from brief, symptom-limited exercise to moderate exercise (60% capacity) for 3 or more hours per week.
The use of antiplatelet therapy or the routine use of anticoagulation in patients with HF who are in sinus rhythm provides no benefit. Anticoagulation may be useful if the patient has severe HF or has a known mural thrombus. HF patients with atrial fibrillation should be considered for antiplatelet or anticoagulation therapy as described elsewhere.58
Short-acting CCBs may worsen HF. No data support the use of any CCB in the primary treatment of HF. Similarly, intermittent use of milrinone or dobutamine is not indicated.
Symptom control. The symptomatic treatment of HF includes the use of diuretics and dietary sodium restriction to control sodium levels and volume status. Symptom control should be accomplished along with the pharmacologic disease management outlined above.
The role of digoxin in the failing heart without dysrhythmias is unclear. Digoxin may be most useful in symptom control, as it reduces hospitalizations attributed to worsening HF. This benefit must be balanced against an increased risk of hospitalization caused by digoxin toxicity. Patients who are already taking digoxin should probably continue to do so. The role of digoxin in newly diagnosed HF patients is unknown.
Close follow-up. Comprehensive follow-up, with the patient as a more active participant and in which care is extended beyond the hospital or office to the home, is a key strategy in the long-term care of HF patients. This aspect of HF management should include educating patients about their disease process and their dietary and pharmacologic treatments; teaching them how to monitor their weight, symptoms, and blood pressure and to understand when to seek care; and following up periodically by telephone between scheduled office visits.
FIGURE
Management of adults with heart failure
- Control the risks for the development and progression of heart failure (HF) by controlling hypertension, diabetes, myocardial ischemia, and tobacco and alcohol use.
- Treat HF with angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, or beta-blockers, used alone or in combination; add spironolactone and carvedilol (or change current beta-blocker to carvedilol) in severe HF; institute aerobic exercise program.
- Control symptoms with diuretics, restricted dietary sodium intake, and digoxin.
- Provide close follow-up that is comprehensive and multidisciplinary, including intensive patient education; self-monitoring of weight, symptoms, and blood pressure; and periodic telephone or in-home follow-up between scheduled office visits.
Heart failure (HF) affects more than 2 million adults in the United States.1 This common, costly, and disabling disorder mainly affects the elderly, with prevalence rates of up to 10% in patients older than 65 years.2,3 The management of HF is responsible for millions of outpatient visits per year,4 is the most common discharge diagnosis for Medicare beneficiaries,5 and accounts for more than 5% of total health care dollars spent.6
Treatment
Major advances in the pharmacologic treatment of heart failure (HF) have emerged in recent years. An approach to the diagnosis and evaluation of HF is described elsewhere.7 This article summarizes the evidence for outpatient treatment of HF. Current intervention trials do not distinguish between systolic and diastolic heart failure; it is therefore unknown whether or how drug therapy should be tailored according to the type of HF. The treatment of cardiac dysrhythmias in the setting of HF is beyond the scope of this article and is presented elsewhere.8Table 1 compares the available outpatient treatments of HF and includes the levels of evidence, numbers needed to treat, and appropriate situations for use. In the remainder of this article, we will discuss pharmacologic and nonpharmacologic management, including identification of ineffective treatments.
TABLE 1
Treatment options in heart failure
| Strength of recommendation (level of evidence)* | Treatment | NNT (Time)† | Use in NYHA class | Comments |
|---|---|---|---|---|
| A (1a) | Angiotensin-converting9-14 enzyme (ACE) inhibitors | 24 (90 days to 2 years) | I–IV | Even moderate doses (equivalent to 10 to 20 mg enalapril per day) provide benefit |
| A (1b) | Angiotensin-receptor blockers (ARBs)15,16 | Similar to ACE inhibitors | I–IV | Useful in patients who do not tolerate ACE inhibitors; may be combined with ACE inhibitors or beta-blockers, but not both |
| A (1a) | Beta-blockers (metoprolol, bisoprolol, carvedilol)17-20 | 24 (1 to 2 years) | I–IV | Usually added to ACE inhibitors or ARBs. May also be useful if concomitant tachydysrhythmias are present and in the post-MI period |
| A (1b) | Carvedilol21 | 18 (10 months) | III–IV | Add carvedilol if not already taking beta-blocker or change current beta-blocker to carvedilol |
| A (1b) | Spironolactone23 | 9 (2 years) | III–IV | NNT = 4 (2 years) to prevent hospitalization for HF. Severe hyperkalemia important safety concern (NNH = 195 over 2 years) |
| A (1b) | Hydralazine + isosorbide dinitrate (ISDN)24,25 | 19 (6 years) | I–IV | Use limited by poor tolerability |
| B (1a) | Digoxin26-28 | N/A | I–IV | No mortality benefit. NNT = 22 to prevent 1 hospitalization over 3 years. Increased risk of hospitalization for digoxin toxicity (NNH = 94 over 3 years) |
| B (2b) | Diuretics (furosemide, bumetanide, torsemide)29-32 | N/A | I–IV | Used for fluid, sodium, and symptom control. No data on mortality benefit |
| A (1b) | Aerobic exercise38-40 | 4 (14 months) | I–IV | Decreases hospitalization for HF (NNT = 5). Even brief symptom-limited exercise in severe HF has benefit in improving quality of life |
| A (1b) | Comprehensive, multi-disciplinary outpatient visits | N/A | I–IV | No mortality benefit. NNT = 5 for 3 months to prevent repeat hospitalization. Includes some combination of intensive education, medication monitoring, individualized diet modification, telephone/home visit follow-up between scheduled outpatient visits |
| B (5) | Dietary sodium restriction8,36,37 | N/A | I–IV | Recommended as standard practice, but no morbidity or mortality data from RCTs |
| C (2a) | Antiplatelet therapy and anticoagulation in HF with sinus rhythm33,35,58 | N/A | N/A | Antiplatelet therapy not useful. No data to support routine anticoagulation, although may be useful in severe HF. Patients with concomitant atrial fibrillation should be anticoagulated if no contraindications |
| D (1b) | Calcium channel blockers (CCBs)46-50 | N/A | N/A | Short-acting CCBs worsen HF. Newer, long-acting CCBs do not worsen HF, but there is no evidence of morbidity or mortality benefit |
| D (1b) | Intermittent positive inotrope (oral or intravenous)(dobutamine, milrinone)51-53 | N/A | N/A | Increased mortality (NNH = 17 over 5 months), increased hospitalizations for worsening HF (NNH = 20), and serious adverse reactions (NNH = 25) |
| *Based on the guidelines for evidence quality outlined by the Center for Evidence-Based Medicine. Available at http://cebm.jr2.ox.ac.uk/docs/levels.html. | ||||
| †NNT = number needed to treat to prevent 1 death over specified time period unless otherwise noted. | ||||
| HF, heart failure; MI, myocardial infarction; NNH, number needed to harm; NNT, number needed to treat; NYHA, New York Heart Association classification; RCT, randomized controlled trial. | ||||
Pharmacologic treatment
Angiotensin-converting enzyme inhibitors. A systematic review9 of 32 trials with a total of 7105 patients demonstrated that mortality rates were lower in patients taking an angiotensin-converting enzyme (ACE) inhibitor than in those not taking one (number needed to treat [NNT] = 24 for > 90 days, meaning that 1 fewer death occurs for every 24 patients who take an ACE inhibitor for more than 90 days). In addition, there is a reduction in the combined endpoints of death and hospitalization because of HF (NNT = 11). Although most of this benefit was realized in the first 90 days of therapy, benefits lasted for 4 to 5 years and were more pronounced in patients categorized in more severe New York Heart Association (NYHA) HF classes10 (class I: no limitation of activities; class II: slight limitation of activity; class III: marked limitation of activity and comfortable only at rest; class IV: symptoms at rest).
Dosage comparison studies demonstrate that HF patients can benefit from even moderate doses of ACE inhibitors. A recent multicenter trial comparing moderate dose enalapril (10 mg twice a day) with a higher dose (30 mg twice a day) in patients with a left ventricular ejection fraction (LVEF) of less than 20% found no differences in mortality at 1 year between the 2 groups.11 In addition, both groups achieved similar increases in functional status and LVEF.
Several trials have demonstrated good tolerability of ACE inhibitors.12-14 Dropout rates of 15% to 30% were similar between patients in the ACE inhibitor and placebo groups, mainly because of side effects, including dizziness, altered taste, hypotension, hyperkalemia, and cough.
Angiotensin-receptor blockers. Angiotensin-receptor blockers (ARBs) reduce all-cause mortality and HF-related hospitalizations in patients with NYHA class II and III HF at rates comparable with those of ACE inhibitors.15,16 Cough is not a side effect of ARBs. Although they are more expensive, ARBs offer a reasonable alternative for patients who do not tolerate ACE inhibitors.
Beta-blockers. The beta-blockers carvedilol, metoprolol, and bisoprolol have a proven mortality benefit for patients with HF.17-19 Pooled results of 6 randomized controlled trials (RCTs), including more than 9000 patients already taking ACE inhibitors, showed a significant reduction in total mortality (NNT = 24 over 1–2 years) and sudden death (NNT = 35), regardless of NYHA classification.20 The average dropout rate of 16% was similar in the betablocker and placebo groups.
Early beta-blocker studies included few NYHA class IV patients until a recent study of the use of carvedilol in severe chronic HF.21 In this study, all patients were taking diuretics plus either an ACE inhibitor or ARB and were permitted to take digoxin, nitrates, hydralazine, spironolactone, or amiodarone. Carvedilol at an average dose of 37 mg per day decreased mortality (NNT = 18 for 10 months) and lowered combined mortality and hospitalization for worsening HF (NNT = 13). Study patients taking carvedilol withdrew from the study at a lower rate (approximately 15%) than placebo.
Because the pharmacologic properties of betablockers vary, clinicians have wondered which are most beneficial. The investigators in a study comparing metoprolol (a beta-1 antagonist) with carvedilol (a beta-1, beta-2, and alpha-1 antagonist) in NYHA class II or III patients found no differences in quality-of-life measures or changes in NYHA classification.22
Spironolactone. The addition of spironolactone to standard care can help patients with severe HF.23 In NYHA class III and IV HF patients, spironolactone at doses ranging from 25 mg every other day to 50 mg per day reduces mortality (NNT = 9 for 2 years), reduces hospitalization from all cardiac causes (NNT = 4), and reduces hospitalization for worsening HF (NNT = 3). The most common serious adverse event in the spironolactone group was severe hyperkalemia (number needed to harm [NNH] = 195). Ten percent of men taking spironolactone experienced breast pain and gynecomastia.
Hydralazine and isosorbide dinitrate. The combination of hydralazine and isosorbide dinitrate (ISDN) reduces mortality in HF patients, but tolerability is an issue. In earlier trials, men with HF symptoms that were optimally controlled with digoxin and diuretics and treated with hydralazine (average dose = 270 mg/day) plus ISDN (average dose = 136 mg/day) had a decrease in all-cause mortality of 28% (NNT = 19 for 6 years).24 A more recent trial comparing hydralazine plus ISDN with enalapril25 (average daily doses of hydralazine = 300 mg/day; ISDN = 160 mg/day; enalapril = 20 mg/day) in NYHA class II–III patients showed no differences in mortality between the 2 groups over 3 years. Tolerability was a problem in these trials; more than 30% of patients stopped taking hydralazine, nitrate, or both.
Digoxin. Digoxin is effective for treating the symptoms of HF in the absence of dysrhythmias but there are no data demonstrating a mortality benefit. Digoxin increases functional capacity in NYHA class II–III patients and heart failure symptoms worsen if digoxin is withdrawn.26 Although there are no differences in all-cause mortality with the use of digoxin, there are fewer hospitalizations due to worsening HF (NNT = 27–114 over 3 years) and a lower rate of clinical deterioration (NNT = 4–75).27 In a randomized trial comparing digoxin and placebo, patients taking digoxin were twice as likely to be hospitalized for suspected digoxin toxicity (2.0% vs 0.9%; P < .001; NNH = 52).28
Diuretics. Diuretics are a mainstay of the symptomatic treatment of heart failure. Short-term studies have shown that diuretics improve the symptoms of sodium and fluid retention and increase exercise tolerance and cardiac function regardless of NYHA classification.29-32 No studies that examine their effects on morbidity and mortality are available.
Antiplatelet therapy and anticoagulation. Patients with HF have an increased risk for thromboembolic events of 1.6% to 3.2% per year.33 One systematic review concluded that antiplatelet therapy is not useful in preventing thromboembolism in patients with HF in sinus rhythm and may even be harmful.34 Another systematic review also concluded that the data do not support the routine use of anticoagulants (eg, warfarin) in patients with HF and sinus rhythm.35 Anticoagulation may be beneficial, however, if there is echocardiographic visualization of a left ventricular thrombus or in cases of “severe” HF or concomitant atrial fibrillation.35
Nonpharmacologic management
Dietary sodium restriction. There is consensus that dietary sodium restriction is important in the treatment of HF36 and is recommended in published guidelines.8,37 Sodium restriction assists with fluid volume control and minimizes the dosages of HF drugs used. These recommendations are based on the retention of sodium and water in symptomatic HF. No studies, however, have examined the effect of dietary sodium restriction on morbidity or mortality, either alone or in combination with pharmacologic treatments.
Exercise training. Moderate exercise training improves quality of life and decreases mortality in patients with stable chronic HF. A recent RCT demonstrated a decrease in mortality (NNT = 4 for 14 months) and hospital readmission for HF (NNT = 5) with only moderate exercise on a stationary bicycle (60% of maximum exercise capacity) for 2 to 3 hours per week.38 Other studies have demonstrated improvements in physiologic markers39 and in quality-of-life ratings with short-term, symptom-limited exercise.40
Multidisciplinary or case-management approach. A case-based or disease-management approach to patients with HF decreases the frequency of unplanned and repeat hospitalizations, increases functional status, and increases quality of life.41 Even a single in-home visit by a clinical pharmacist and a nurse results in fewer unplanned readmissions and fewer days of hospitalization up to 18 months after discharge.42,43 A small study of 27 patients in a Veterans Affairs hospital demonstrated that patient instruction in the self-monitoring of weight and blood pressure, combined with frequent telephone follow-up from a nurse, lowered repeat hospitalizations over 1 year, with the effect more pronounced in patients with more severe NYHA classifications.44 A large RCT demonstrated that a multidisciplinary management approach (intensive patient education about HF and its treatment, dietary assessment and instruction, medication analysis and elimination of unnecessary medications, and telephone and home visit follow-up) results in fewer hospitalizations (NNT = 5 for 3 months) and reduced costs of care.45
Treatments that have no benefit or are harmful
Calcium-channel blockers. Although some of the newer, longer-acting calcium-channel blockers (CCBs) appear to be safe in the treatment of heart failure,46-49 no trials are available demonstrating that they lower mortality, decrease hospitalizations, or improve quality of life in patients with a failing heart. Older, short-acting CCBs can worsen HF.50
Positive inotropic therapy. Intermittent positive inotropic therapy, either orally (milrinone) or intravenously (dobutamine), should be avoided. Although short-term studies have shown some increase in cardiac function and symptoms,51 long-term studies demonstrate no mortality benefit.52 One RCT of milrinone demonstrated an increase in mortality (NNH = 17 for 5 months), an increased rate of hospitalization for worsening HF (NNH = 20), and more serious side effects (NNH = 25).53
Prognosis
Despite the increased longevity in Western developed nations and increased survival from coronary artery disease over recent decades, the overall prognosis of HF has improved very little.6,54 Mortality data derived from several different sources, the largest being the Framingham Heart Study,2,55 have shown that HF remains highly lethal, with a 5-year survival rate of 25% in men and 38% in women with NYHA II–IV heart failure. Mortality data from the placebo arms of intervention trials show an average 1-year mortality of 18%.9,17,19,20,56 A recent population-based study of patients with a new diagnosis of HF showed survival rates of only 62% at 12 months and 57% at 18 months.57 Despite these dismal population-based data, predicting the likelihood of survival in individuals with HF is largely unreliable.8 Estimating individual prognosis is only somewhat useful in making end-of-life care and hospice decisions for patients with very advanced HF. Table 2 summarizes specific prognostic factors for patients with HF.
TABLE 2
Factors that affect prognosis in patients with heart failure (HF)
| Factor | Result | Comment |
|---|---|---|
| Age1,2,6,59 | Increasing age and age older than 55 years decreases survival | Framingham data: survival rates of older women are twice as long as those of older men despite significant age difference (women: 72 years; men: 68 years). |
| Sex56,60-62 | Mortality higher in men | Women are underrepresented in HF trials and frequently have HF associated with diastolic dysfunction. Women rate their quality of inpatient care lower than men do. |
| Race63-65 | African Americans have higher mortality rates and higher rates of recurrent hospitalization | HF affects approximately 3% of all African Americans. They develop symptoms at an earlier tage. The disease progresses more rapidly than in whites. African Americans are underrepresented in HF trials. |
| Attending physician specialty66-68 | No difference in 6-month cardiac and all-cause mortality between family physician or generalist and cardiologist care | Family physician or generalist: Twofold increased risk of readmission in 6 months; tend to overestimate risks of ACE inhibitors and therefore under-prescribe them. |
| Cardiologist (as attending or consultant): Increased testing, hospital lengths of stay, and hospital charges, but better patient-perceived quality of life. |
Suggested management of patients with heart failure
Although the optimal sequence of pharmacologic interventions for treating HF has not been examined in RCTs, recommendations can be made on the basis of existing evidence in HF management (Figure). This approach can be divided into 4 steps performed simultaneously: (1) control risks for the development and progression of HF (treat concomitant diseases); (2) HF treatment; (3) symptom control; (4) close follow-up.
Control risks. Risks for the development and worsening of HF should be addressed as described else-where.8 Steps include longitudinal surveillance; identification and treatment of hypertension, diabetes and thyroid diseases; management of atherosclerotic and coronary artery disease and myocardial ischemia; and the elimination of alcohol and tobacco use.
Heart failure treatment. All patients with HF should take a drug or a combination of drugs that affects the disease process. Drugs shown by the preponderance of evidence to decrease morbidity and mortality include ACE inhibitors, beta-blockers, and ARBs. For most HF patients, regardless of NYHA class, ACE inhibitors should be the initial baseline treatment because of their proven track record and the observation that most recent HF trials include patients who are already taking these medications. ARBs are similar in efficacy to ACE inhibitors and, therefore, are an adequate alternative when ACE inhibitors are not tolerated. Beta-blockers (metoprolol and bisoprolol) added to ACE inhibitors are also useful as a baseline treatment in most HF patients and may be especially useful in the case of tachydysrhythmias and in the postmyocardial infarction period.
For severe HF (NYHA III–IV), spironolactone and carvedilol are useful additions to baseline drug therapy. Carvedilol may be added if a beta-blocker is not currently used. If the patient is currently taking a beta-blocker, the drug should be discontinued before the patient is switched to carvedilol.
The hydralazine–nitrate combination has been proved effective, but tolerability and ease-of-use issues limit its usefulness. No data are available to support the use of nitrates other than isosorbide dinitrate. Nitrates may be useful, however, for concomitant chronic myocardial ischemia.
Patients with stable HF should be encouraged to begin and maintain a regular aerobic exercise program. The level of exercise can range from brief, symptom-limited exercise to moderate exercise (60% capacity) for 3 or more hours per week.
The use of antiplatelet therapy or the routine use of anticoagulation in patients with HF who are in sinus rhythm provides no benefit. Anticoagulation may be useful if the patient has severe HF or has a known mural thrombus. HF patients with atrial fibrillation should be considered for antiplatelet or anticoagulation therapy as described elsewhere.58
Short-acting CCBs may worsen HF. No data support the use of any CCB in the primary treatment of HF. Similarly, intermittent use of milrinone or dobutamine is not indicated.
Symptom control. The symptomatic treatment of HF includes the use of diuretics and dietary sodium restriction to control sodium levels and volume status. Symptom control should be accomplished along with the pharmacologic disease management outlined above.
The role of digoxin in the failing heart without dysrhythmias is unclear. Digoxin may be most useful in symptom control, as it reduces hospitalizations attributed to worsening HF. This benefit must be balanced against an increased risk of hospitalization caused by digoxin toxicity. Patients who are already taking digoxin should probably continue to do so. The role of digoxin in newly diagnosed HF patients is unknown.
Close follow-up. Comprehensive follow-up, with the patient as a more active participant and in which care is extended beyond the hospital or office to the home, is a key strategy in the long-term care of HF patients. This aspect of HF management should include educating patients about their disease process and their dietary and pharmacologic treatments; teaching them how to monitor their weight, symptoms, and blood pressure and to understand when to seek care; and following up periodically by telephone between scheduled office visits.
FIGURE
Management of adults with heart failure
1. Schocken DD, Arrieta MI, Leaverton PE, Ross EA. Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol 1992;20:301-6.
2. McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure. The Framingham study. N Engl J Med 1971;285:1442-6.
3. Kannel WB, Plehn JF, Cupples LA. Cardiac failure and sudden death in the Framingham Study. Am Heart J 1988;115:869-75.
4. Schappert SM. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 1997. Vital Health Stat 13. 1999;No. 143:i-iv,1-39.
5. Krumholz HM, Parent EM, Tu N, et al. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med 1997;157:99-104.
6. McMurray JJ, Stewart S. Heart failure. Epidemiology, etiology, and prognosis of heart failure. Heart 2000;83:596-602.
7. Mair FS, Lloyd-Williams F. Evaluation of suspected left ventricular systolic dysfunction. J Fam Pract 2002;51:466-471.
8. Hunt SA, Baker DW, Chin MH, et al. ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). 2001. American College of Cardiology Web site. Available at: http://www.acc.org/clinical/guidelines/failure/hf_index.htm.
9. Garg R, Yusuf S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. JAMA 1995;273:1450-6.
10. The Criteria Committee of the New York Heart Association. Diseases of the Heart and Blood Vessels: Nomenclature and Criteria for Diagnosis. 6th ed. Boston, MA: Little, Brown; 1964.
11. Nanas JN, Alexopoulus G, Anastasiou-Nana MI, et al. Outcome of patients with congestive heart failure treated with standard versus high doses of enalapril: a multicenter study. J Am Coll Cardiol 2000;36:2090-5.
12. CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. N Engl J Med 1987;316:1429-35.
13. SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1991;325:293-302.
14. Pfeffer MA, Braunwald E, Moye LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement (SAVE) trial. N Engl J Med 1992;327:659-77.
15. Pitt B, Poole-Wilson PA, Segal R, et al. Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: a randomized trial. The losartan heart failure survival study (ELITE II). Lancet 2000;355:1582-7.
16. Cohn JN, Tognoni G. for the Valsartan Heart Failure Trial Investigators. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med 2001;345:1667-75.
17. Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. N Engl J Med 1996;334:1349-55.
18. MERIT-HF Study Group. Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet 1999;353:2001-7.
19. CIBIS-II Investigators. The cardiac insufficiency bisoprolol study II (CIBIS-II): a randomized trial. Lancet 1999;353:9-13.
20. Lee S, Spencer A. Beta-blockers to reduce mortality in patients with systolic dysfunction. J Fam Pract 2001;6:499-504.
21. Packer M, Coats AJS, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001;344:1651-8.
22. Metra M, Giubbini R, Nodari S, et al. Differential effects of betablockers in patients with heart failure: a prospective, randomized, double-blind comparison of the long-term effects of metoprolol versus carvedilol. Circulation 2000;102:546-51.
23. Pitt B, Zannad F, Remm WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med 1999;341:707-17.
24. Cohn J, Archibald DG, Ziesche S, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. N Engl J Med 1986;314:1547-52.
25. Cohn JN, Johnson G, Ziesche S, et al. Comparison of enalapril with hydralazine–isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med 1991;325:303-10.
26. Packer M, Gheorghiade M, Young JB, et al. Withdrawal of digoxin from patients with chronic heart failure treated with angiotensin-converting enzyme inhibitors. N Engl J Med 1993;329:1-7.
27. Hood WB, Jr, Dans A, Guyatt GH, Jaescke R, McMurray JV. Digitalis for treatment of congestive heart failure in patients in sinus rhythm. In: The Cochrane Library, Issue 4, 2001. Oxford, England: Update Software.
28. The Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med 1997;336:525-33.
29. Brater DC. Diuretic therapy. N Engl J Med 1998;339:387-95.
30. Cody RJ, Kubo SH, Pickworth KK. Diuretic treatment for the sodium retention of congestive heart failure. Arch Intern Med 1994;154:1905-14.
31. Wilson JR, Reichek N, Dunkman WB, Goldberg S. Effect of diuresis on the performance of the failing left ventricle in man. Am J Med 1981;70:234-9.
32. Richardson A, Bayliss J, Scriven AJ, Parameshwar J, Poole-Wilson PA, Sutton GC. Double-blind comparison of captopril alone against furosemide plus amiloride in mild heart failure. Lancet 1987;2:709-11.
33. Dunkman WB. Thromboembolism and antithrombotic therapy in congestive heart failure. J Cardiovasc Risk 1995;2:107-17.
34. Lip GYH, Gibbs CR. Antiplatelet agents versus control or anticoagulation for heart failure in sinus rhythm. In: The Cochrane Library, Issue 4, 2001. Oxford, England: Update Software.
35. Lip GYH, Gibbs CR. Anticoagulation for heart failure in sinus rhythm. In: The Cochrane Library, Issue 4, 2001. Oxford, England: Update Software.
36. Lenihan DJ, Uretsky BF. Nonpharmacologic treatment of heart failure in the elderly. Clin Geriatr Med 2000;16:477-87.
37. Williams JF, Bristow MR, Fowler MB, et al. Guidelines for the evaluation and management of chronic heart failure. Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Evaluation and Management of Heart Failure). Circulation 1995;92:2764-84.
38. Belardinelli R, Georgiou D, Ciance G, Purcaro A. Randomized controlled trial of long-term moderate exercise training in chronic heart failure. Effects on functional capacity, quality of life, and clinical outcome. Circulation 1999;99:1173-82.
39. Sullivan MJ, Higginbotham MB, Cobb FR. Exercise training in patients with severe left ventricular dysfunction. Hemodynamic and metabolic effects. Circulation 1988;78:506-15.
40. Tokmakova M, Dobreva B, Kostianev S. Effects of short-term exercise training in patients with heart failure. Folia Medica (Plovdiv) 1999;41:68-71. Abstract.
41. Rich MW. Heart failure disease management: a critical review. J Card Fail 1999;5:64-75.
42. Stewart S, Pearson S, Horowitz JD. Effects of a home-based intervention among patients with congestive heart failure discharged from acute hospital care. Arch Intern Med 1998;158:1067-72.
43. Stewart S, Vandenbroek AJ, Pearson S, Horowitz JD. Prolonged beneficial effects of a home-based intervention on unplanned readmissions and mortality among patients with congestive heart failure. Arch Intern Med 1999;159:257-61.
44. Shah NB, Der E, Ruggerio C, Heidenreich PA, Massie BM. Prevention of hospitalizations for heart failure with an interactive home monitoring program. Am Heart J 1998;135:373-8.
45. Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med 1995;333:1190-5.
46. Levine TN, Bernink PJ, Caspi A, et al. Effect of mibefradil, a T-type calcium channel blocker, on morbidity and mortality in moderate to severe congestive heart failure: the MACH-1 study. Mortality Assessment in Congestive Heart Failure Trial. Circulation 2000;101:758-64.
47. Mahon N, McKenna WJ. Calcium-channel blockers in cardiac failure. Prog Card Dis 1998;41:191-206.
48. deVries RJ, van Veldhuisen DJ, Dunselman PH. Efficacy and safety of calcium channel blockers in heart failure: focus on recent trials with second-generation dihydropyridines. Am Heart J 2000;139(2 pt 1):185-94.
49. O’Connor CM, Carson PE, Miller AB, et al. Effect of amlodipine on mode of death among patients with advanced heart failure in the PRAISE trial. Prospective randomized amlodipine survival evaluation. Am J Cardiol 1998;82:881-7.
50. Packer M, Kessler PD, Lee WH. Calcium-channel blockade in the management of severe chronic congestive heart failure: a bridge too far. Circulation 1987;75:V56-64.
51. Anderson JL. Hemodynamic and clinical benefits with intravenous milrinone in severe chronic heart failure: results of a multicenter study in the United States. Am Heart J 1991;121:1956-64.
52. Elis A, Bental T, Kimchi O, Ravid M, Lishner M. Intermittent dobutamine treatment in patients with chronic refractory congestive heart failure: a randomized, double-blind, placebo-controlled study. Clin Pharmacol Ther 1998;63:682-5.
53. Packer M, Carver JR, Rodeheffer RJ, et al. Effect of oral milrinone on mortality in severe chronic heart failure. The PROMISE Study Research Group. N Engl J Med 1991;325:1468-75.
54. Cleland JGF, Clark A. Has the survival of the heart failure population changed? Lessons from trials. Am J Cardiol 1999;83:112D-19D.
55. Ho KKL, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: the Framingham study. J Am Coll Cardiol 1993;22(suppl A):6A-13A.
56. Clinical Quality Improvement Network Investigators. Mortality risk and patterns of practice in 4606 acute care patients with congestive heart failure. The relative importance of age, sex, and medical therapy. Arch Intern Med 1996;156:1669-73.
57. Cowie MR, Wood DA, Coats AJ, et al. Survival of patients with a new diagnosis of heart failure: a population-based study. Heart 2000;83:505-10.
58. Albers GW, Dalen JE, Laupacis A, Manning WJ, Petersen P, Singer DE. Antithrombotic therapy in atrial fibrillation. Chest 2001;119:194S-206S.
59. Doba N, Tomiyama H, Nakayama T. Drugs, heart failure and quality of life: what are we achieving? What should we be trying to achieve? Drugs Aging 1999;14:153-63.
60. Petrie MC, Dawson NF, Murdoch DR, Davie AP, McMurray JJV. Failure of women’s hearts. Circulation 1999;99:2334-41.
61. Burns RB, McCarthy EP, Moskowitz MA, Ash A, Kane RL, Finch M. Outcomes for older men and women with congestive heart failure. J Am Geriatr Soc 1997;45:276-80.
62. Chin MH, Goldman L. Gender differences in 1-year survival and quality of life among patients admitted with congestive heart failure. Med Care 1998;36:1033-46.
63. Dries DL, Exner DV, Gersh BJ, Cooper HA, Carson PE, Domanski MJ. Racial differences in the outcome of left ventricular dysfunction [published erratum appears in N Engl J Med 1999; 341:298]. N Engl J Med 1999;340:609-16.
64. Alexander M, Grumbach K, Remy L, Rowell R, Massie BM. Congestive heart failure hospitalizations and survival in California: patterns according to race/ethnicity. Am Heart J 1999;137:919-27.
65. Philbin EF, DiSalvo TG. Influence of race and gender on care process, resource use, and hospital-based outcomes in congestive heart failure. Am J Cardiol 1998;82:76-81.
66. Reis SE, Holubkov R, Edmundowicz D, et al. Treatment of patients admitted to the hospital with congestive heart failure: specialty-related disparities in practice patterns and outcomes. J Am Coll Cardiol 1997;30:733-8.
67. Philbin EF, Weil HFC, Erb TA, Jenkins PL. Cardiology or primary care for heart failure in the community setting. Process of care and clinical outcomes. Chest 1999;116:346-54.
68. Baker DW, Hayes RP, Massie BM, Craig CA. Variations in family physicians’ and cardiologists’ care for patients with heart failure. Am Heart J 1999;138:826-34.
1. Schocken DD, Arrieta MI, Leaverton PE, Ross EA. Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol 1992;20:301-6.
2. McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure. The Framingham study. N Engl J Med 1971;285:1442-6.
3. Kannel WB, Plehn JF, Cupples LA. Cardiac failure and sudden death in the Framingham Study. Am Heart J 1988;115:869-75.
4. Schappert SM. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 1997. Vital Health Stat 13. 1999;No. 143:i-iv,1-39.
5. Krumholz HM, Parent EM, Tu N, et al. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med 1997;157:99-104.
6. McMurray JJ, Stewart S. Heart failure. Epidemiology, etiology, and prognosis of heart failure. Heart 2000;83:596-602.
7. Mair FS, Lloyd-Williams F. Evaluation of suspected left ventricular systolic dysfunction. J Fam Pract 2002;51:466-471.
8. Hunt SA, Baker DW, Chin MH, et al. ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). 2001. American College of Cardiology Web site. Available at: http://www.acc.org/clinical/guidelines/failure/hf_index.htm.
9. Garg R, Yusuf S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. JAMA 1995;273:1450-6.
10. The Criteria Committee of the New York Heart Association. Diseases of the Heart and Blood Vessels: Nomenclature and Criteria for Diagnosis. 6th ed. Boston, MA: Little, Brown; 1964.
11. Nanas JN, Alexopoulus G, Anastasiou-Nana MI, et al. Outcome of patients with congestive heart failure treated with standard versus high doses of enalapril: a multicenter study. J Am Coll Cardiol 2000;36:2090-5.
12. CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. N Engl J Med 1987;316:1429-35.
13. SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1991;325:293-302.
14. Pfeffer MA, Braunwald E, Moye LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement (SAVE) trial. N Engl J Med 1992;327:659-77.
15. Pitt B, Poole-Wilson PA, Segal R, et al. Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: a randomized trial. The losartan heart failure survival study (ELITE II). Lancet 2000;355:1582-7.
16. Cohn JN, Tognoni G. for the Valsartan Heart Failure Trial Investigators. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med 2001;345:1667-75.
17. Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. N Engl J Med 1996;334:1349-55.
18. MERIT-HF Study Group. Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet 1999;353:2001-7.
19. CIBIS-II Investigators. The cardiac insufficiency bisoprolol study II (CIBIS-II): a randomized trial. Lancet 1999;353:9-13.
20. Lee S, Spencer A. Beta-blockers to reduce mortality in patients with systolic dysfunction. J Fam Pract 2001;6:499-504.
21. Packer M, Coats AJS, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001;344:1651-8.
22. Metra M, Giubbini R, Nodari S, et al. Differential effects of betablockers in patients with heart failure: a prospective, randomized, double-blind comparison of the long-term effects of metoprolol versus carvedilol. Circulation 2000;102:546-51.
23. Pitt B, Zannad F, Remm WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med 1999;341:707-17.
24. Cohn J, Archibald DG, Ziesche S, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. N Engl J Med 1986;314:1547-52.
25. Cohn JN, Johnson G, Ziesche S, et al. Comparison of enalapril with hydralazine–isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med 1991;325:303-10.
26. Packer M, Gheorghiade M, Young JB, et al. Withdrawal of digoxin from patients with chronic heart failure treated with angiotensin-converting enzyme inhibitors. N Engl J Med 1993;329:1-7.
27. Hood WB, Jr, Dans A, Guyatt GH, Jaescke R, McMurray JV. Digitalis for treatment of congestive heart failure in patients in sinus rhythm. In: The Cochrane Library, Issue 4, 2001. Oxford, England: Update Software.
28. The Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med 1997;336:525-33.
29. Brater DC. Diuretic therapy. N Engl J Med 1998;339:387-95.
30. Cody RJ, Kubo SH, Pickworth KK. Diuretic treatment for the sodium retention of congestive heart failure. Arch Intern Med 1994;154:1905-14.
31. Wilson JR, Reichek N, Dunkman WB, Goldberg S. Effect of diuresis on the performance of the failing left ventricle in man. Am J Med 1981;70:234-9.
32. Richardson A, Bayliss J, Scriven AJ, Parameshwar J, Poole-Wilson PA, Sutton GC. Double-blind comparison of captopril alone against furosemide plus amiloride in mild heart failure. Lancet 1987;2:709-11.
33. Dunkman WB. Thromboembolism and antithrombotic therapy in congestive heart failure. J Cardiovasc Risk 1995;2:107-17.
34. Lip GYH, Gibbs CR. Antiplatelet agents versus control or anticoagulation for heart failure in sinus rhythm. In: The Cochrane Library, Issue 4, 2001. Oxford, England: Update Software.
35. Lip GYH, Gibbs CR. Anticoagulation for heart failure in sinus rhythm. In: The Cochrane Library, Issue 4, 2001. Oxford, England: Update Software.
36. Lenihan DJ, Uretsky BF. Nonpharmacologic treatment of heart failure in the elderly. Clin Geriatr Med 2000;16:477-87.
37. Williams JF, Bristow MR, Fowler MB, et al. Guidelines for the evaluation and management of chronic heart failure. Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Evaluation and Management of Heart Failure). Circulation 1995;92:2764-84.
38. Belardinelli R, Georgiou D, Ciance G, Purcaro A. Randomized controlled trial of long-term moderate exercise training in chronic heart failure. Effects on functional capacity, quality of life, and clinical outcome. Circulation 1999;99:1173-82.
39. Sullivan MJ, Higginbotham MB, Cobb FR. Exercise training in patients with severe left ventricular dysfunction. Hemodynamic and metabolic effects. Circulation 1988;78:506-15.
40. Tokmakova M, Dobreva B, Kostianev S. Effects of short-term exercise training in patients with heart failure. Folia Medica (Plovdiv) 1999;41:68-71. Abstract.
41. Rich MW. Heart failure disease management: a critical review. J Card Fail 1999;5:64-75.
42. Stewart S, Pearson S, Horowitz JD. Effects of a home-based intervention among patients with congestive heart failure discharged from acute hospital care. Arch Intern Med 1998;158:1067-72.
43. Stewart S, Vandenbroek AJ, Pearson S, Horowitz JD. Prolonged beneficial effects of a home-based intervention on unplanned readmissions and mortality among patients with congestive heart failure. Arch Intern Med 1999;159:257-61.
44. Shah NB, Der E, Ruggerio C, Heidenreich PA, Massie BM. Prevention of hospitalizations for heart failure with an interactive home monitoring program. Am Heart J 1998;135:373-8.
45. Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med 1995;333:1190-5.
46. Levine TN, Bernink PJ, Caspi A, et al. Effect of mibefradil, a T-type calcium channel blocker, on morbidity and mortality in moderate to severe congestive heart failure: the MACH-1 study. Mortality Assessment in Congestive Heart Failure Trial. Circulation 2000;101:758-64.
47. Mahon N, McKenna WJ. Calcium-channel blockers in cardiac failure. Prog Card Dis 1998;41:191-206.
48. deVries RJ, van Veldhuisen DJ, Dunselman PH. Efficacy and safety of calcium channel blockers in heart failure: focus on recent trials with second-generation dihydropyridines. Am Heart J 2000;139(2 pt 1):185-94.
49. O’Connor CM, Carson PE, Miller AB, et al. Effect of amlodipine on mode of death among patients with advanced heart failure in the PRAISE trial. Prospective randomized amlodipine survival evaluation. Am J Cardiol 1998;82:881-7.
50. Packer M, Kessler PD, Lee WH. Calcium-channel blockade in the management of severe chronic congestive heart failure: a bridge too far. Circulation 1987;75:V56-64.
51. Anderson JL. Hemodynamic and clinical benefits with intravenous milrinone in severe chronic heart failure: results of a multicenter study in the United States. Am Heart J 1991;121:1956-64.
52. Elis A, Bental T, Kimchi O, Ravid M, Lishner M. Intermittent dobutamine treatment in patients with chronic refractory congestive heart failure: a randomized, double-blind, placebo-controlled study. Clin Pharmacol Ther 1998;63:682-5.
53. Packer M, Carver JR, Rodeheffer RJ, et al. Effect of oral milrinone on mortality in severe chronic heart failure. The PROMISE Study Research Group. N Engl J Med 1991;325:1468-75.
54. Cleland JGF, Clark A. Has the survival of the heart failure population changed? Lessons from trials. Am J Cardiol 1999;83:112D-19D.
55. Ho KKL, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: the Framingham study. J Am Coll Cardiol 1993;22(suppl A):6A-13A.
56. Clinical Quality Improvement Network Investigators. Mortality risk and patterns of practice in 4606 acute care patients with congestive heart failure. The relative importance of age, sex, and medical therapy. Arch Intern Med 1996;156:1669-73.
57. Cowie MR, Wood DA, Coats AJ, et al. Survival of patients with a new diagnosis of heart failure: a population-based study. Heart 2000;83:505-10.
58. Albers GW, Dalen JE, Laupacis A, Manning WJ, Petersen P, Singer DE. Antithrombotic therapy in atrial fibrillation. Chest 2001;119:194S-206S.
59. Doba N, Tomiyama H, Nakayama T. Drugs, heart failure and quality of life: what are we achieving? What should we be trying to achieve? Drugs Aging 1999;14:153-63.
60. Petrie MC, Dawson NF, Murdoch DR, Davie AP, McMurray JJV. Failure of women’s hearts. Circulation 1999;99:2334-41.
61. Burns RB, McCarthy EP, Moskowitz MA, Ash A, Kane RL, Finch M. Outcomes for older men and women with congestive heart failure. J Am Geriatr Soc 1997;45:276-80.
62. Chin MH, Goldman L. Gender differences in 1-year survival and quality of life among patients admitted with congestive heart failure. Med Care 1998;36:1033-46.
63. Dries DL, Exner DV, Gersh BJ, Cooper HA, Carson PE, Domanski MJ. Racial differences in the outcome of left ventricular dysfunction [published erratum appears in N Engl J Med 1999; 341:298]. N Engl J Med 1999;340:609-16.
64. Alexander M, Grumbach K, Remy L, Rowell R, Massie BM. Congestive heart failure hospitalizations and survival in California: patterns according to race/ethnicity. Am Heart J 1999;137:919-27.
65. Philbin EF, DiSalvo TG. Influence of race and gender on care process, resource use, and hospital-based outcomes in congestive heart failure. Am J Cardiol 1998;82:76-81.
66. Reis SE, Holubkov R, Edmundowicz D, et al. Treatment of patients admitted to the hospital with congestive heart failure: specialty-related disparities in practice patterns and outcomes. J Am Coll Cardiol 1997;30:733-8.
67. Philbin EF, Weil HFC, Erb TA, Jenkins PL. Cardiology or primary care for heart failure in the community setting. Process of care and clinical outcomes. Chest 1999;116:346-54.
68. Baker DW, Hayes RP, Massie BM, Craig CA. Variations in family physicians’ and cardiologists’ care for patients with heart failure. Am Heart J 1999;138:826-34.
What is the best treatment for slowing the progression to end-stage renal disease (ESRD) in African Americans with hypertensive nephropathy?
BACKGROUND: Deaths in African Americans from hypertensive renal disease have risen in recent years. The effects of various antihypertensives on mortality are unknown, since studies have included few African Americans.
POPULATION STUDIED: This study included 1094 African Americans between the ages of 18 and 70 years with hypertensive renal disease, defined as a glomerular filtration rate (GFR) of 20 to 65 mL per minute. The patients included in this study had no other identified causes of renal disease, and were excluded if they had diabetes mellitus, malignant hypertension, secondary hypertension, or congestive heart failure. The average age of the participants was 54 years, and they had a history of hypertension for a mean of 14 years. Nearly half were women with a mean arterial pressure (MAP) of 115. Patients with more than 2.5 g per day of urinary protein excretion were excluded; however, approximately one third of the study participants had proteinuria greater than 300 mg per day, with the average being 600 mg per day. Half of the subjects had a history of heart disease. At enrollment, 40% were taking an angiotensin-converting enzyme (ACE) inhibitor, 27% a b-blocker, 60% a calcium channel blocker (CCB), and 45% a dihydropyridine calcium channel blocker (DHP-CCB).
STUDY DESIGN AND VALIDITY: The patients were randomized to 1 of 3 antihypertensive medications: the ACE inhibitor ramipril 2.5 to 10 mg per day, the sustained-release b-blocker metoprolol 50 to 200 mg per day, or the DHP-CCB amlodipine 5 to 10 mg per day. Each of these groups was further divided into 2 target blood pressure groups: “usual” (MAP) goal of 102 or a “low” MAP goal of 92. Blood pressures were checked and medications adjusted monthly to achieve target MAPs, and GFR was evaluated at baseline and every 3 months. Data were analyzed using an intention-to-treat approach. This is an interim analysis of the African American Study of Kidney Disease and Hypertension (AASK) trial, a multicentered and double-blinded study. Allocation concealment was maintained for study drug assignments but not for the blood pressure goals. Because interim analysis showed large differences between the ramipril and metoprolol groups compared with the amlodipine group, the amlodipine arm was terminated. Follow-up of patients in the remaining arms is ongoing and will be reported at a later time.
OUTCOMES MEASURED: The primary outcome measured was the effect of the study drugs on the long-term rate of decline of GFR. Secondary outcomes were “GFR events” (a decrease of GFR greater than 50%), progression to ESRD, death, and combinations of these.
RESULTS: Baseline characteristics were similar between the amlodipine and ramipril groups, and the average follow-up was 3 years. Overall, the rate of decline in GFR was 36% slower in the ramipril group compared with the amlodipine group (P=.002). This slowed decline in GFR was more pronounced in the subgroup of participants with proteinuria and in the subgroup that had a baseline GFR of less than 40 mL per minute.
Although African Americans have traditionally been thought to be less responsive to ACE inhibitors, in this study ramipril (2.5-10 mg/day) was useful in the treatment of already established hypertensive nephropathy in this population. Ramipril slowed progression to ESRD, especially in those patients with preexisting proteinuria and in those with more advanced renal failure (GFR less than 40 mg/minute). Interestingly, amlodipine was inferior to both ramipril and metoprolol in the treatment of hypertensive renal disease. The question of which is better, ramipril or metoprolol, is currently under study.
BACKGROUND: Deaths in African Americans from hypertensive renal disease have risen in recent years. The effects of various antihypertensives on mortality are unknown, since studies have included few African Americans.
POPULATION STUDIED: This study included 1094 African Americans between the ages of 18 and 70 years with hypertensive renal disease, defined as a glomerular filtration rate (GFR) of 20 to 65 mL per minute. The patients included in this study had no other identified causes of renal disease, and were excluded if they had diabetes mellitus, malignant hypertension, secondary hypertension, or congestive heart failure. The average age of the participants was 54 years, and they had a history of hypertension for a mean of 14 years. Nearly half were women with a mean arterial pressure (MAP) of 115. Patients with more than 2.5 g per day of urinary protein excretion were excluded; however, approximately one third of the study participants had proteinuria greater than 300 mg per day, with the average being 600 mg per day. Half of the subjects had a history of heart disease. At enrollment, 40% were taking an angiotensin-converting enzyme (ACE) inhibitor, 27% a b-blocker, 60% a calcium channel blocker (CCB), and 45% a dihydropyridine calcium channel blocker (DHP-CCB).
STUDY DESIGN AND VALIDITY: The patients were randomized to 1 of 3 antihypertensive medications: the ACE inhibitor ramipril 2.5 to 10 mg per day, the sustained-release b-blocker metoprolol 50 to 200 mg per day, or the DHP-CCB amlodipine 5 to 10 mg per day. Each of these groups was further divided into 2 target blood pressure groups: “usual” (MAP) goal of 102 or a “low” MAP goal of 92. Blood pressures were checked and medications adjusted monthly to achieve target MAPs, and GFR was evaluated at baseline and every 3 months. Data were analyzed using an intention-to-treat approach. This is an interim analysis of the African American Study of Kidney Disease and Hypertension (AASK) trial, a multicentered and double-blinded study. Allocation concealment was maintained for study drug assignments but not for the blood pressure goals. Because interim analysis showed large differences between the ramipril and metoprolol groups compared with the amlodipine group, the amlodipine arm was terminated. Follow-up of patients in the remaining arms is ongoing and will be reported at a later time.
OUTCOMES MEASURED: The primary outcome measured was the effect of the study drugs on the long-term rate of decline of GFR. Secondary outcomes were “GFR events” (a decrease of GFR greater than 50%), progression to ESRD, death, and combinations of these.
RESULTS: Baseline characteristics were similar between the amlodipine and ramipril groups, and the average follow-up was 3 years. Overall, the rate of decline in GFR was 36% slower in the ramipril group compared with the amlodipine group (P=.002). This slowed decline in GFR was more pronounced in the subgroup of participants with proteinuria and in the subgroup that had a baseline GFR of less than 40 mL per minute.
Although African Americans have traditionally been thought to be less responsive to ACE inhibitors, in this study ramipril (2.5-10 mg/day) was useful in the treatment of already established hypertensive nephropathy in this population. Ramipril slowed progression to ESRD, especially in those patients with preexisting proteinuria and in those with more advanced renal failure (GFR less than 40 mg/minute). Interestingly, amlodipine was inferior to both ramipril and metoprolol in the treatment of hypertensive renal disease. The question of which is better, ramipril or metoprolol, is currently under study.
BACKGROUND: Deaths in African Americans from hypertensive renal disease have risen in recent years. The effects of various antihypertensives on mortality are unknown, since studies have included few African Americans.
POPULATION STUDIED: This study included 1094 African Americans between the ages of 18 and 70 years with hypertensive renal disease, defined as a glomerular filtration rate (GFR) of 20 to 65 mL per minute. The patients included in this study had no other identified causes of renal disease, and were excluded if they had diabetes mellitus, malignant hypertension, secondary hypertension, or congestive heart failure. The average age of the participants was 54 years, and they had a history of hypertension for a mean of 14 years. Nearly half were women with a mean arterial pressure (MAP) of 115. Patients with more than 2.5 g per day of urinary protein excretion were excluded; however, approximately one third of the study participants had proteinuria greater than 300 mg per day, with the average being 600 mg per day. Half of the subjects had a history of heart disease. At enrollment, 40% were taking an angiotensin-converting enzyme (ACE) inhibitor, 27% a b-blocker, 60% a calcium channel blocker (CCB), and 45% a dihydropyridine calcium channel blocker (DHP-CCB).
STUDY DESIGN AND VALIDITY: The patients were randomized to 1 of 3 antihypertensive medications: the ACE inhibitor ramipril 2.5 to 10 mg per day, the sustained-release b-blocker metoprolol 50 to 200 mg per day, or the DHP-CCB amlodipine 5 to 10 mg per day. Each of these groups was further divided into 2 target blood pressure groups: “usual” (MAP) goal of 102 or a “low” MAP goal of 92. Blood pressures were checked and medications adjusted monthly to achieve target MAPs, and GFR was evaluated at baseline and every 3 months. Data were analyzed using an intention-to-treat approach. This is an interim analysis of the African American Study of Kidney Disease and Hypertension (AASK) trial, a multicentered and double-blinded study. Allocation concealment was maintained for study drug assignments but not for the blood pressure goals. Because interim analysis showed large differences between the ramipril and metoprolol groups compared with the amlodipine group, the amlodipine arm was terminated. Follow-up of patients in the remaining arms is ongoing and will be reported at a later time.
OUTCOMES MEASURED: The primary outcome measured was the effect of the study drugs on the long-term rate of decline of GFR. Secondary outcomes were “GFR events” (a decrease of GFR greater than 50%), progression to ESRD, death, and combinations of these.
RESULTS: Baseline characteristics were similar between the amlodipine and ramipril groups, and the average follow-up was 3 years. Overall, the rate of decline in GFR was 36% slower in the ramipril group compared with the amlodipine group (P=.002). This slowed decline in GFR was more pronounced in the subgroup of participants with proteinuria and in the subgroup that had a baseline GFR of less than 40 mL per minute.
Although African Americans have traditionally been thought to be less responsive to ACE inhibitors, in this study ramipril (2.5-10 mg/day) was useful in the treatment of already established hypertensive nephropathy in this population. Ramipril slowed progression to ESRD, especially in those patients with preexisting proteinuria and in those with more advanced renal failure (GFR less than 40 mg/minute). Interestingly, amlodipine was inferior to both ramipril and metoprolol in the treatment of hypertensive renal disease. The question of which is better, ramipril or metoprolol, is currently under study.
The Evaluation and Treatment of Children with Acute Otitis Media
Between 1993 and 1995 more than 20 million visits were provided to children younger than 15 years for otitis media; 77% of these were for children aged 4 years and younger.1 Acute otitis media (AOM) is the most frequent primary diagnosis in preschool children and accounts for almost 20% of ambulatory care visits in this age group. By the age of 3 months, 10% of children will be given at least 1 diagnosis of otitis media and more than 90% by the age of 2 years.2 Peak incidence occurs between the ages 6 and 15 months, although there is a second peak at approximately age 5 years that is thought to be associated with entrance into school.3 In the mid-1990s, treatment of otitis media cost $3.8 billion per year4; 20% of the more than 110 million prescriptions for oral antibiotics are for otitis media.5
The most important contributor to AOM is a dysfunction of the eustachian tube, allowing reflux of fluid and bacteria into the middle ear space from the nasopharynx.6 This dysfunction is usually multifactorial and is likely a combination of anatomy (shorter and more flexible eustachian tubes) and function (inefficiency at clearing secretions and equilibrating negative intratympanic pressures) in younger children.7 Acute viral upper respiratory infections create inflammation and secretions that magnify this eustachian tube dysfunction and predispose to or induce AOM.
The 3 most common bacteria in AOM are Streptococcus pneumoniae, Haemophilus species, and Branhamella catarrhalis. A recent study showed that both bacteria and viruses were isolated in the middle ear fluid of 65% of children with otitis media. In fact, 35% had viruses isolated as the sole middle ear pathogen.8 Other studies have failed to identify a specific infectious agent in a significant number of middle ear fluid aspirates.9
Diagnosis
The diagnosis of AOM in children is often based on a combination of symptoms and physical findings. It is usually defined as bulging or opacification of the tympanic membrane with or without erythema, middle ear effusion, marked decrease or absence of tympanic membrane mobility, and accompanied by at least one of the following signs and symptoms of acute infection: fever, otalgia, irritability, otorrhea, lethargy, anorexia, vomiting, or diarrhea.10 Although the best reference standard for the diagnosis of AOM is myringotomy or tympanocentesis, no published studies were identified in which this reference was performed in all study patients. Most published studies use pneumatic otoscopy combined with tympanocentesis or myringotomy as the reference standard when middle ear effusion is suspected.
Most symptoms are not specific for AOM. In a survey of patients seeing general practitioners in Finland,11 the symptoms that most increased the likelihood of diagnosing AOM were earache (relative risk [RR]=5.4; 95% confidence interval [CI], 3.3-8.9), rubbing of the ear (RR=5.0; 95% CI, 2.9-8.6), and excessive crying (RR=2.8; 95% CI, 1.8-4.3). Although fever, earache, or excessive crying were present in 90% of children considered to have AOM, one or more of these symptoms were also present in 72% of children who did not have otitis media. In another survey of children aged younger than 4 years with a diagnosis of AOM, 40% did not have otalgia, and 30% did not have fever.12
Physical examination findings are of variable reliability. Findings that physicians rely on to diagnose AOM, such as a bulging or erythematous tympanic membrane, may occasionally be found in normal ears.13 One study compared the 3 most commonly documented otoscopic findings (color, position, and mobility of the tympanic membrane) with those of pneumatic otoscopy and myringotomy.14 Only 65% of patients with a distinctly red tympanic membrane and 16% with a slightly red tympanic membrane had AOM. A cloudy tympanic membrane was the most predictive color change, with an 80% positive predictive value (PPV), the percentage of patients with the symptom who have AOM. A bulging tympanic membrane was most predictive of AOM (PPV=89%), despite its 27% false-negative rate. Retraction was found in only 19% of children with AOM and had a PPV of only 50%. Distinctly impaired mobility was predictive of otitis media (PPV=78%), but diminished mobility was also found in 30% of children without middle ear effusion. These data and those presented in Table 1 show that each of these otoscopic examination elements (color, position, mobility) alone is inadequate for discriminating between cases in which the diagnosis of AOM is uncertain.
However, combining these signs can be useful.15 A cloudy (opaque), bulging, and immobile tympanic membrane on pneumatic otoscopy was nearly 100% predictive of otitis media in children with acute symptoms. In addition, 94% of children with the combination of distinctly red erythema, bulging, and immobility had AOM. No combination of findings that included only slight redness was more than 53% predictive of AOM.
In children aged younger than 1 year in whom otoscopy can be quite difficult, tympanometry can be a useful tool for detecting a middle ear effusion.16 An abnormal type B tympanogram (flat curve with no distinct peak) in infants presenting with acute symptoms is strong evidence in favor of AOM, although a normal test is not helpful in ruling out the diagnosis.
The diagnosis of AOM can be influenced by the physician’s perception of parental expectations for antibiotics.17 A study of children presenting with ear pain or other upper respiratory symptoms found that physicians diagnosed AOM 49% of the time when they perceived parents wanted antibiotics and only 13% of the time when they thought parents did not want antibiotics. Physicians were 23 times more likely to prescribe an antibiotic for an upper respiratory illness if they perceived that parents expected antimicrobials.
Treatment
A recent systematic review18 found that the symptoms of AOM (mainly otalgia) spontaneously resolved in two thirds of children by 24 hours and in 80% at 2 to 7 days. This was also observed in 2 earlier meta-analyses.10,19 Seventeen children would need to be treated with antibiotics (vs placebo) for 1 child to have less pain at 2 to 7 days (number needed to treat [NNT]=17). There were no differences between antibiotic and placebo groups in other clinical outcomes, such as tympanometry findings, perforation, and recurrences. Also, children treated with antibiotics were almost twice as likely to have vomiting, diarrhea, or a rash.
Initially not treating uncomplicated AOM with antibiotics is an acceptable alternative. In a study by van Buchem and colleagues,20 90% of children with AOM recovered (symptoms resolved) in the first 4 days with nose drops and oral analgesics and without the use of antibiotics. Only 3% of the 4860 children in this study had a clinical course that required further treatment with antibiotics or myringotomy. A recent randomized controlled trial of 315 children demonstrated that children treated immediately with antibiotics had 1 less day of symptoms, but that 1 in 5 of these had diarrhea.21 The group not treated with antibiotics had no serious sequellae and used more analgesics. There were no differences in the number of missed school days, and more than 75% of the parents were satisfied with this “wait and see” approach. These studies also emphasize that antibiotics have a very modest effect on the clinical course of AOM and seem to decrease the duration of symptoms only to a small degree.
Physicians often recommend other symptomatic treatments for ear infections. Non–aspirin analgesics are effective in relieving pain,21 as are ibuprofen22 and Auralgan.23 Antihistamine-decongestant preparations offer no added benefit in resolution of symptoms and have no effect on clinical outcomes when given with antibiotics.24,25
If antibiotics are used, the meta-analysis by Rosenfeld and colleagues10 showed there were no differences in outcomes between treatment with cefaclor, cefixime, erythromycin, trimethoprim-sulfamethoxazole, amoxicillin clavulanate, or erythromycin sulfisoxazole, and treatment with amoxicillin or ampicillin. Broader spectrum and/or more expensive antibiotics therefore offer no advantage over amoxicillin for the initial treatment of AOM. In another meta-analysis, Kozyrskyj and coworkers26 showed that a 5-day antibiotic course was an acceptable alternative to a 8- to 14-day treatment course. There was a slightly increased risk of treatment failure at 1-month follow-up with the shortened course of antibiotics; the NNT to prevent 1 excess failure at 30 days was 17. There were no differences in long-term outcomes (2-3 months) or medication side effects (vomiting, diarrhea, rash) between the short and long antibiotic courses. The broader spectrum azithromycin and intramuscular ceftriaxone offered no advantage over amoxicillin. Children aged younger than 2 years deserve special mention, since they are at higher risk for treatment failures,27,28 persistent symptoms,29 and recurrent otitis media.30 Few well-designed studies exist to guide treatment in this age group. Although children aged younger than 2 years were not excluded, neither review by Glasziou and colleagues18 or Rosenfeld and coworkers10 specifically examined this age group.
Another review demonstrated that (as with older children) routinely using antibiotics initially does not seem to add any clinical benefit.31 A recent randomized controlled trial of 240 children demonstrated that 8 children in this age group would have to be treated with amoxicillin for 1 child to have fewer symptoms (fever, crying, irritability) at 4 days (NNT=8).32 The major benefit of amoxicillin in this study was 1 day less of fever (P=.004). Adverse effects were almost twice as likely in the amoxicillin group, although this difference was not statistically significant. There were also no differences between the groups in clinical failure rates at 11 days or in the likelihood of recurrent otitis media, antibiotic use, specialist referrals, or surgery at 6 weeks. Effects on hearing were not measured. The authors conclude that “this modest effect does not justify prescription of antibiotics at the first visit, provided close surveillance can be guaranteed.” Also, Kozyrskyj and colleagues26 demonstrated in their meta-analysis that as a subgroup there were no differences in clinical failures between 5 and 10 days of antibiotics in children aged younger than 2 years. However, there were only 118 children in this age group. Table 2 shows treatment options for AOM.
In recent years, there has been an increasing concern about worldwide bacterial resistance to antimicrobial drugs33-35 by the World Health Organization36 and the Centers for Disease Control and Prevention (CDC).37 In response to the increasing antimicrobial resistance patterns seen in the common middle ear pathogens, especially S pneumoniae, the CDC Drug-resistant Streptococcus pneumoniae Therapeutic Working Group recommends doubling the dosage of amoxicillin to 80 to 90 mg per kg per day in the empiric treatment of AOM.38 These recommendations are based on in vitro mean inhibitory concentration data of S pneumoniae cultures from middle ear fluid and nasopharyngeal swabs. However, there currently is no patient-oriented evidence to suggest that increasing the amoxicillin dosage actually decreases suppurative or invasive complications of AOM (meningitis, mastoiditis, and so forth), affects recurrence rates or treatment success, affects long-term outcomes of AOM, or even decreases the rate of drug-resistant S pneumoniae. Also, bacteriologic outcomes do not correlate with clinical outcomes. In the meta-analysis by Rosenfeld and coworkers,10 89% of middle ear pathogens from treatment failures were susceptible in vitro to the antibiotic prescribed, and 13% of isolates from clinical cures were resistant in vitro to the prescribed antibiotic. We must use extreme caution in extrapolating the microbiologic findings to the clinical care of the child with AOM.
Prognosis
There are insufficient data to suggest that routine antibiotic use in AOM results in fewer cases of mastoiditis or meningitis. In the systematic reviews cited, the incidence of these suppurative complications was rare. In the Cochrane review by Glasziou and colleagues,18 only 1 case of mastoiditis developed in 2202 children, and this was in a child treated with penicillin. In the Netherlands among 4860 consecutive children with AOM, 2 experienced mastoiditis (both responded to outpatient antibiotic therapy), and there were no cases of meningitis.20 In the meta-analysis by Rosenfeld and coworkers,10 there were no suppurative complications in the 5400 children studied. Although mastoiditis has been quoted as being more common in the preantibiotic era, it is unclear if the current rarity of this condition is due to antibiotic treatment, changes in organism virulence or host defenses, or the assertion that uncomplicated otitis media was often not reported, thus increasing the relative rate of mastoiditis.27 In a recent review,39 antibiotics did not seem to have an appreciable effect on complication rates, leading the authors to conclude that “antibiotic treatment for AOM cannot be considered as a safeguard against the development of complications.” Even in developing countries where the burden of otitis media is great, mastoiditis is quite rare, with a prevalence rate of much less than 1%.40
Antibiotic use does influence bacterial resistance rates. In children previously treated with antibiotics for AOM, there is a 3-fold increased risk of isolating drug-resistant organisms from middle ear effusions with subsequent bouts of otitis media.41,42 In the Netherlands and Iceland, routinely not treating AOM with antibiotics has resulted in a reduction in antibiotic resistance.33,43 The most important risk factors for a poor outcome are age younger than 2 years and attendance at a daycare center.40 Children in daycare have a higher risk of requiring a hospital admission and up to a 50% increased risk of repeated or recurrent ear infections.44,45 Children with chronic underlying illnesses or chronic otitis media with effusion have added risks of poor outcomes that are beyond the scope of this review.
Conclusions
Thus, the natural course of AOM in children is quite favorable. If left untreated, 80% will recover spontaneously within 2 weeks. The addition of antibiotics provides at best a modest reduction in symptoms, while adding cost, adverse drug effects, and increasing bacterial resistance in the patient and community. Minimizing the use of antibiotics in patients with AOM does not increase the risks of perforation, deafness, or contralateral or recurrent AOM.
1. Freid VM, Makuc DM, Rooks RN. Ambulatory health care visits by children: principal diagnosis and place of visit. Vital Health Stat Series 13: data from the National Health Survey. 1998;137:1-23.
2. Klein J. Epidemiology of acute otitis media. Infect Dis 1989;8(suppl 1):89.-
3. Daly KA, Giebink GS. Clinical epidemiology of otitis media. Pediatr Infect Dis J 2000;19:S31-36.
4. Gates GA. Cost-effectiveness considerations in otitis media treatment. Otolaryngol Head Neck Surg 1996;114:525-30.
5. McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA 1995;273:214-19.
6. Taylor RB, ed. Family medicine. Principles and practice. 4th ed. Heidelberg, Germany: Springer-Verlag; 1994.
7. Bluestone CD, Doyle WJ. Anatomy and physiology of eustachian tube and middle ear related to otitis media. J Allergy Clin Immunol 1988;81:997-1003.
8. Heikkinen T, Thint M, Chonmaitree T. Prevalence of various respiratory viruses in the middle ear during acute otitis media. N Engl J Med 1999;340:260-64.
9. Ruuskanen O, Heikkinin AM, Ziegler T. Viruses in acute otitis media: increasing evidence for clinical significance. Pediatr Infect Dis J 1991;10:425-27.
10. Rosenfeld RM, Vertrees JE, Carr J, et al. Clinical efficacy of antimicrobial drugs for acute otitis media: meta-analysis of 5400 children from thirty-three randomized trials. J Pediatr 1994;124:355-67.
11. Niemela M, Uhari M, Juonio-Ervasti K, Luotonen J, Alho O, Vierimaa E. Lack of specific symptomatology in children with acute otitis media. Pediatr Infect Dis J 1994;13:765-68.
12. Heikkinen T, Ruuskanen O. Signs and symptoms predicting acute otitis media. Arch Pediatr Adolesc Med 1995;149:26-29.
13. Aorla M, Ruuskanen O, Ziegler T, et al. Clinical role of respiratory virus infection in acute otitis media. Pediatrics 1990;86:848-55.
14. Karma PH, Penttila MA, Sipila MM, Kataja MJ. Otoscopic diagnosis of middle ear effusion in acute and non-acute otitis media. I. The value of different otoscopic findings. Int J Pediatr Otolaryngol 1989;17:37-49.
15. Karma PH, Sipila MM, Kataja MJ, Penttila MA. Pneumatic otoscopy and otitis media: the value of different tympanic membrane findings and their combinations. In: Kim DJ, Bluestone CD, Klein JO, Nelson JD, Ogra PL, eds. Recent advances in otitis media: proceedings of the Fifth International Symposium. Burlington, Ontario, Canada: Decker; 1993;41-45.
16. Palmu A, Puhakka H, Rahko T, Takala AK. Diagnostic value of tympanometry in infants in clinical practice. Int J Ped Otorhinolaryngol 1999;49:207-13.
17. Mangione-Smith R, McGlynn EA, Elliott MN, Krogstad P, Brook RH. The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior. Pediatrics 1999;103:711-18.
18. Glasziou PP, Del Mar CB, Hayem M, Sanders SL. Antibiotics for acute otitis media in children (Cochrane review). In: The Cochrane library Issue 4. Oxford, England: Update Software; 2000.
19. Del Mar C, Glasziou P, Hayem M. Are antibiotics indicated as initial treatment for children with acute otitis media? A meta-analysis. BMJ 1997;314:1526-29.
20. Van Buchem FL, Peeters MF, van’t Hof MA. Acute otitis media: a new treatment strategy. BMJ 1985;290:1033-37.
21. Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ 2001;332:336-42.
22. Bertin L, Pons G, d’Athis P, et al. A randomized double blind multicentre controlled trial of ibuprofen versus acetaminophen and placebo for symptoms of acute otitis media in children. Fundam Clin Parmacol 1996;10:387-92.
23. Hoberman A, Paradise JL, Reynolds EA, Urkin J. Efficacy of Auralgan for treating ear pain in children with acute otitis media. Arch Pediatr Adolesc Med 1997;151:675-78.
24. Schnore SK, Sangster JF, Gerace TM, Bass MJ. Are antihistamine-decongestants of value in the treatment of acute otitis media in children? J Fam Pract 1986;22:39-43.
25. Bhambhani K, Foulds DM, Swamy KN, Eldis FE, Fischel JE. Acute otitis media in children: are decongestants or antihistamines necessary? Ann Emerg Med 1983;12:13-16.
26. Kozyrskyj AL, Hildes-Ripstein GE, Longstaffe SEA, et al. Short course antibiotics for acute otitis media (Cochrane review). In: The Cochrane library Issue 4. Oxford, England: Update Software; 2000.
27. Froom J, Culpepper L, Jacobs M, et al. Antimicrobials for acute otitis media? A review from the International Primary Care Network. BMJ 1997;315:98-102.
28. Iino Y, Nakamura Y, Koizumi T, Toriyama M. Prognostic factors for persistent middle ear effusion after acute otitis media in children. Acta Oto-Laryngologica 1993;113:761-65.
29. Paradise JL. Short-course antimicrobial treatment for acute otitis media: not best for infants and young children. JAMA 1997;278:1640-42.
30. Rasmussen F. Recurrence of acute otitis media at preschool age in Sweden. J Epidemiol Comm Health. 1994;48:33-35.
31. Damoiseaux RA, van Balen FA, Hoes AW, de Melker RA. Antibiotic treatment of acute otitis media in children under two years of age: evidence based? Br J Gen Pract 1998;48:1861-64.
32. Damoiseaux RAMJ, van Balen FAM, Hoes AW, Verheij TJM, de Melker RA. Primary care based randomised, double blind trial of amoxicillin versus placebo for acute otitis media in children aged under 2 years. BMJ 2000;320:350-54.
33. Neu HC. The crisis in antibiotic resistance. Science 1992; 257:1036-38. 34. Breiman RF, Butler JC, Tenover FC, Elliott JA, Facklan RR. Emergence of drug-resistant pneumococcal infections in the United States. JAMA 1994;271:1831-35.
35. Cohen ML. Epidemiology of drug-resistance: implications for the post-antimicrobial era. Science 1992;257:1050-55.
36. LeDuc JW. World Health Organization strategy for emerging infectious diseases. JAMA 1996;275:318-20.
37. Interagency Task Force on Antimicrobial Resistance. A public health action plan to combat antimicrobial resistance. Available at: www.cdc.gov/drugresistance/actionplan/index.htm.
38. Dowell SF, Butler JC, Giebink GS, et al. Acute otitis media: management and surveillance in an era of pneumococcal resistance—a report from the Drug-resistant Streptococcus pneumoniae Therapeutic Working group. Ped Infect Dis J 1999;18:1-9.
39. Dhooge IJM, Albers FWJ, van Cauwenberge PB. Intratemporal and intracranial complications of acute suppurative otitis media in children: renewed interest. Internat J Ped Otorhinolaryngol 1999;49:S109-14.
40. Berman S. Otitis media in developing countries. Pediatrics 1995;96:126-31.
41. Harrison CJ, Marks MI, Welch DF. Microbiology of recently treated acute otitis media compared with previously untreated acute otitis media. Pediatr Infect Dis J 1985;4:641-46.
42. Ford KL, Mason EO, Jr, Kaplan SL, Lamberth LB, Tillman J. Factors associated with middle ear isolates of Streptococcus pneumoniae resistant to penicillin in a children’s hospital. J Pediatrics 1991;119:941-44.
43. Stephenson J. Icelandic researchers are showing the way to bring down rates of antibiotic-resistant bacteria. JAMA 1996;275:175.
44. Hardy AM, Fowler MG. Child care arrangements and repeated ear infections in young children. Am J Public Health 1993;83:1321-25.
45. Louhiala PJ, Jaakkola N, Ruotsalainen R, Jaakkola JJ. Form of day care and respiratory infection among Finnish children. Am J Public 1995;85:1109-12. 46.
Between 1993 and 1995 more than 20 million visits were provided to children younger than 15 years for otitis media; 77% of these were for children aged 4 years and younger.1 Acute otitis media (AOM) is the most frequent primary diagnosis in preschool children and accounts for almost 20% of ambulatory care visits in this age group. By the age of 3 months, 10% of children will be given at least 1 diagnosis of otitis media and more than 90% by the age of 2 years.2 Peak incidence occurs between the ages 6 and 15 months, although there is a second peak at approximately age 5 years that is thought to be associated with entrance into school.3 In the mid-1990s, treatment of otitis media cost $3.8 billion per year4; 20% of the more than 110 million prescriptions for oral antibiotics are for otitis media.5
The most important contributor to AOM is a dysfunction of the eustachian tube, allowing reflux of fluid and bacteria into the middle ear space from the nasopharynx.6 This dysfunction is usually multifactorial and is likely a combination of anatomy (shorter and more flexible eustachian tubes) and function (inefficiency at clearing secretions and equilibrating negative intratympanic pressures) in younger children.7 Acute viral upper respiratory infections create inflammation and secretions that magnify this eustachian tube dysfunction and predispose to or induce AOM.
The 3 most common bacteria in AOM are Streptococcus pneumoniae, Haemophilus species, and Branhamella catarrhalis. A recent study showed that both bacteria and viruses were isolated in the middle ear fluid of 65% of children with otitis media. In fact, 35% had viruses isolated as the sole middle ear pathogen.8 Other studies have failed to identify a specific infectious agent in a significant number of middle ear fluid aspirates.9
Diagnosis
The diagnosis of AOM in children is often based on a combination of symptoms and physical findings. It is usually defined as bulging or opacification of the tympanic membrane with or without erythema, middle ear effusion, marked decrease or absence of tympanic membrane mobility, and accompanied by at least one of the following signs and symptoms of acute infection: fever, otalgia, irritability, otorrhea, lethargy, anorexia, vomiting, or diarrhea.10 Although the best reference standard for the diagnosis of AOM is myringotomy or tympanocentesis, no published studies were identified in which this reference was performed in all study patients. Most published studies use pneumatic otoscopy combined with tympanocentesis or myringotomy as the reference standard when middle ear effusion is suspected.
Most symptoms are not specific for AOM. In a survey of patients seeing general practitioners in Finland,11 the symptoms that most increased the likelihood of diagnosing AOM were earache (relative risk [RR]=5.4; 95% confidence interval [CI], 3.3-8.9), rubbing of the ear (RR=5.0; 95% CI, 2.9-8.6), and excessive crying (RR=2.8; 95% CI, 1.8-4.3). Although fever, earache, or excessive crying were present in 90% of children considered to have AOM, one or more of these symptoms were also present in 72% of children who did not have otitis media. In another survey of children aged younger than 4 years with a diagnosis of AOM, 40% did not have otalgia, and 30% did not have fever.12
Physical examination findings are of variable reliability. Findings that physicians rely on to diagnose AOM, such as a bulging or erythematous tympanic membrane, may occasionally be found in normal ears.13 One study compared the 3 most commonly documented otoscopic findings (color, position, and mobility of the tympanic membrane) with those of pneumatic otoscopy and myringotomy.14 Only 65% of patients with a distinctly red tympanic membrane and 16% with a slightly red tympanic membrane had AOM. A cloudy tympanic membrane was the most predictive color change, with an 80% positive predictive value (PPV), the percentage of patients with the symptom who have AOM. A bulging tympanic membrane was most predictive of AOM (PPV=89%), despite its 27% false-negative rate. Retraction was found in only 19% of children with AOM and had a PPV of only 50%. Distinctly impaired mobility was predictive of otitis media (PPV=78%), but diminished mobility was also found in 30% of children without middle ear effusion. These data and those presented in Table 1 show that each of these otoscopic examination elements (color, position, mobility) alone is inadequate for discriminating between cases in which the diagnosis of AOM is uncertain.
However, combining these signs can be useful.15 A cloudy (opaque), bulging, and immobile tympanic membrane on pneumatic otoscopy was nearly 100% predictive of otitis media in children with acute symptoms. In addition, 94% of children with the combination of distinctly red erythema, bulging, and immobility had AOM. No combination of findings that included only slight redness was more than 53% predictive of AOM.
In children aged younger than 1 year in whom otoscopy can be quite difficult, tympanometry can be a useful tool for detecting a middle ear effusion.16 An abnormal type B tympanogram (flat curve with no distinct peak) in infants presenting with acute symptoms is strong evidence in favor of AOM, although a normal test is not helpful in ruling out the diagnosis.
The diagnosis of AOM can be influenced by the physician’s perception of parental expectations for antibiotics.17 A study of children presenting with ear pain or other upper respiratory symptoms found that physicians diagnosed AOM 49% of the time when they perceived parents wanted antibiotics and only 13% of the time when they thought parents did not want antibiotics. Physicians were 23 times more likely to prescribe an antibiotic for an upper respiratory illness if they perceived that parents expected antimicrobials.
Treatment
A recent systematic review18 found that the symptoms of AOM (mainly otalgia) spontaneously resolved in two thirds of children by 24 hours and in 80% at 2 to 7 days. This was also observed in 2 earlier meta-analyses.10,19 Seventeen children would need to be treated with antibiotics (vs placebo) for 1 child to have less pain at 2 to 7 days (number needed to treat [NNT]=17). There were no differences between antibiotic and placebo groups in other clinical outcomes, such as tympanometry findings, perforation, and recurrences. Also, children treated with antibiotics were almost twice as likely to have vomiting, diarrhea, or a rash.
Initially not treating uncomplicated AOM with antibiotics is an acceptable alternative. In a study by van Buchem and colleagues,20 90% of children with AOM recovered (symptoms resolved) in the first 4 days with nose drops and oral analgesics and without the use of antibiotics. Only 3% of the 4860 children in this study had a clinical course that required further treatment with antibiotics or myringotomy. A recent randomized controlled trial of 315 children demonstrated that children treated immediately with antibiotics had 1 less day of symptoms, but that 1 in 5 of these had diarrhea.21 The group not treated with antibiotics had no serious sequellae and used more analgesics. There were no differences in the number of missed school days, and more than 75% of the parents were satisfied with this “wait and see” approach. These studies also emphasize that antibiotics have a very modest effect on the clinical course of AOM and seem to decrease the duration of symptoms only to a small degree.
Physicians often recommend other symptomatic treatments for ear infections. Non–aspirin analgesics are effective in relieving pain,21 as are ibuprofen22 and Auralgan.23 Antihistamine-decongestant preparations offer no added benefit in resolution of symptoms and have no effect on clinical outcomes when given with antibiotics.24,25
If antibiotics are used, the meta-analysis by Rosenfeld and colleagues10 showed there were no differences in outcomes between treatment with cefaclor, cefixime, erythromycin, trimethoprim-sulfamethoxazole, amoxicillin clavulanate, or erythromycin sulfisoxazole, and treatment with amoxicillin or ampicillin. Broader spectrum and/or more expensive antibiotics therefore offer no advantage over amoxicillin for the initial treatment of AOM. In another meta-analysis, Kozyrskyj and coworkers26 showed that a 5-day antibiotic course was an acceptable alternative to a 8- to 14-day treatment course. There was a slightly increased risk of treatment failure at 1-month follow-up with the shortened course of antibiotics; the NNT to prevent 1 excess failure at 30 days was 17. There were no differences in long-term outcomes (2-3 months) or medication side effects (vomiting, diarrhea, rash) between the short and long antibiotic courses. The broader spectrum azithromycin and intramuscular ceftriaxone offered no advantage over amoxicillin. Children aged younger than 2 years deserve special mention, since they are at higher risk for treatment failures,27,28 persistent symptoms,29 and recurrent otitis media.30 Few well-designed studies exist to guide treatment in this age group. Although children aged younger than 2 years were not excluded, neither review by Glasziou and colleagues18 or Rosenfeld and coworkers10 specifically examined this age group.
Another review demonstrated that (as with older children) routinely using antibiotics initially does not seem to add any clinical benefit.31 A recent randomized controlled trial of 240 children demonstrated that 8 children in this age group would have to be treated with amoxicillin for 1 child to have fewer symptoms (fever, crying, irritability) at 4 days (NNT=8).32 The major benefit of amoxicillin in this study was 1 day less of fever (P=.004). Adverse effects were almost twice as likely in the amoxicillin group, although this difference was not statistically significant. There were also no differences between the groups in clinical failure rates at 11 days or in the likelihood of recurrent otitis media, antibiotic use, specialist referrals, or surgery at 6 weeks. Effects on hearing were not measured. The authors conclude that “this modest effect does not justify prescription of antibiotics at the first visit, provided close surveillance can be guaranteed.” Also, Kozyrskyj and colleagues26 demonstrated in their meta-analysis that as a subgroup there were no differences in clinical failures between 5 and 10 days of antibiotics in children aged younger than 2 years. However, there were only 118 children in this age group. Table 2 shows treatment options for AOM.
In recent years, there has been an increasing concern about worldwide bacterial resistance to antimicrobial drugs33-35 by the World Health Organization36 and the Centers for Disease Control and Prevention (CDC).37 In response to the increasing antimicrobial resistance patterns seen in the common middle ear pathogens, especially S pneumoniae, the CDC Drug-resistant Streptococcus pneumoniae Therapeutic Working Group recommends doubling the dosage of amoxicillin to 80 to 90 mg per kg per day in the empiric treatment of AOM.38 These recommendations are based on in vitro mean inhibitory concentration data of S pneumoniae cultures from middle ear fluid and nasopharyngeal swabs. However, there currently is no patient-oriented evidence to suggest that increasing the amoxicillin dosage actually decreases suppurative or invasive complications of AOM (meningitis, mastoiditis, and so forth), affects recurrence rates or treatment success, affects long-term outcomes of AOM, or even decreases the rate of drug-resistant S pneumoniae. Also, bacteriologic outcomes do not correlate with clinical outcomes. In the meta-analysis by Rosenfeld and coworkers,10 89% of middle ear pathogens from treatment failures were susceptible in vitro to the antibiotic prescribed, and 13% of isolates from clinical cures were resistant in vitro to the prescribed antibiotic. We must use extreme caution in extrapolating the microbiologic findings to the clinical care of the child with AOM.
Prognosis
There are insufficient data to suggest that routine antibiotic use in AOM results in fewer cases of mastoiditis or meningitis. In the systematic reviews cited, the incidence of these suppurative complications was rare. In the Cochrane review by Glasziou and colleagues,18 only 1 case of mastoiditis developed in 2202 children, and this was in a child treated with penicillin. In the Netherlands among 4860 consecutive children with AOM, 2 experienced mastoiditis (both responded to outpatient antibiotic therapy), and there were no cases of meningitis.20 In the meta-analysis by Rosenfeld and coworkers,10 there were no suppurative complications in the 5400 children studied. Although mastoiditis has been quoted as being more common in the preantibiotic era, it is unclear if the current rarity of this condition is due to antibiotic treatment, changes in organism virulence or host defenses, or the assertion that uncomplicated otitis media was often not reported, thus increasing the relative rate of mastoiditis.27 In a recent review,39 antibiotics did not seem to have an appreciable effect on complication rates, leading the authors to conclude that “antibiotic treatment for AOM cannot be considered as a safeguard against the development of complications.” Even in developing countries where the burden of otitis media is great, mastoiditis is quite rare, with a prevalence rate of much less than 1%.40
Antibiotic use does influence bacterial resistance rates. In children previously treated with antibiotics for AOM, there is a 3-fold increased risk of isolating drug-resistant organisms from middle ear effusions with subsequent bouts of otitis media.41,42 In the Netherlands and Iceland, routinely not treating AOM with antibiotics has resulted in a reduction in antibiotic resistance.33,43 The most important risk factors for a poor outcome are age younger than 2 years and attendance at a daycare center.40 Children in daycare have a higher risk of requiring a hospital admission and up to a 50% increased risk of repeated or recurrent ear infections.44,45 Children with chronic underlying illnesses or chronic otitis media with effusion have added risks of poor outcomes that are beyond the scope of this review.
Conclusions
Thus, the natural course of AOM in children is quite favorable. If left untreated, 80% will recover spontaneously within 2 weeks. The addition of antibiotics provides at best a modest reduction in symptoms, while adding cost, adverse drug effects, and increasing bacterial resistance in the patient and community. Minimizing the use of antibiotics in patients with AOM does not increase the risks of perforation, deafness, or contralateral or recurrent AOM.
Between 1993 and 1995 more than 20 million visits were provided to children younger than 15 years for otitis media; 77% of these were for children aged 4 years and younger.1 Acute otitis media (AOM) is the most frequent primary diagnosis in preschool children and accounts for almost 20% of ambulatory care visits in this age group. By the age of 3 months, 10% of children will be given at least 1 diagnosis of otitis media and more than 90% by the age of 2 years.2 Peak incidence occurs between the ages 6 and 15 months, although there is a second peak at approximately age 5 years that is thought to be associated with entrance into school.3 In the mid-1990s, treatment of otitis media cost $3.8 billion per year4; 20% of the more than 110 million prescriptions for oral antibiotics are for otitis media.5
The most important contributor to AOM is a dysfunction of the eustachian tube, allowing reflux of fluid and bacteria into the middle ear space from the nasopharynx.6 This dysfunction is usually multifactorial and is likely a combination of anatomy (shorter and more flexible eustachian tubes) and function (inefficiency at clearing secretions and equilibrating negative intratympanic pressures) in younger children.7 Acute viral upper respiratory infections create inflammation and secretions that magnify this eustachian tube dysfunction and predispose to or induce AOM.
The 3 most common bacteria in AOM are Streptococcus pneumoniae, Haemophilus species, and Branhamella catarrhalis. A recent study showed that both bacteria and viruses were isolated in the middle ear fluid of 65% of children with otitis media. In fact, 35% had viruses isolated as the sole middle ear pathogen.8 Other studies have failed to identify a specific infectious agent in a significant number of middle ear fluid aspirates.9
Diagnosis
The diagnosis of AOM in children is often based on a combination of symptoms and physical findings. It is usually defined as bulging or opacification of the tympanic membrane with or without erythema, middle ear effusion, marked decrease or absence of tympanic membrane mobility, and accompanied by at least one of the following signs and symptoms of acute infection: fever, otalgia, irritability, otorrhea, lethargy, anorexia, vomiting, or diarrhea.10 Although the best reference standard for the diagnosis of AOM is myringotomy or tympanocentesis, no published studies were identified in which this reference was performed in all study patients. Most published studies use pneumatic otoscopy combined with tympanocentesis or myringotomy as the reference standard when middle ear effusion is suspected.
Most symptoms are not specific for AOM. In a survey of patients seeing general practitioners in Finland,11 the symptoms that most increased the likelihood of diagnosing AOM were earache (relative risk [RR]=5.4; 95% confidence interval [CI], 3.3-8.9), rubbing of the ear (RR=5.0; 95% CI, 2.9-8.6), and excessive crying (RR=2.8; 95% CI, 1.8-4.3). Although fever, earache, or excessive crying were present in 90% of children considered to have AOM, one or more of these symptoms were also present in 72% of children who did not have otitis media. In another survey of children aged younger than 4 years with a diagnosis of AOM, 40% did not have otalgia, and 30% did not have fever.12
Physical examination findings are of variable reliability. Findings that physicians rely on to diagnose AOM, such as a bulging or erythematous tympanic membrane, may occasionally be found in normal ears.13 One study compared the 3 most commonly documented otoscopic findings (color, position, and mobility of the tympanic membrane) with those of pneumatic otoscopy and myringotomy.14 Only 65% of patients with a distinctly red tympanic membrane and 16% with a slightly red tympanic membrane had AOM. A cloudy tympanic membrane was the most predictive color change, with an 80% positive predictive value (PPV), the percentage of patients with the symptom who have AOM. A bulging tympanic membrane was most predictive of AOM (PPV=89%), despite its 27% false-negative rate. Retraction was found in only 19% of children with AOM and had a PPV of only 50%. Distinctly impaired mobility was predictive of otitis media (PPV=78%), but diminished mobility was also found in 30% of children without middle ear effusion. These data and those presented in Table 1 show that each of these otoscopic examination elements (color, position, mobility) alone is inadequate for discriminating between cases in which the diagnosis of AOM is uncertain.
However, combining these signs can be useful.15 A cloudy (opaque), bulging, and immobile tympanic membrane on pneumatic otoscopy was nearly 100% predictive of otitis media in children with acute symptoms. In addition, 94% of children with the combination of distinctly red erythema, bulging, and immobility had AOM. No combination of findings that included only slight redness was more than 53% predictive of AOM.
In children aged younger than 1 year in whom otoscopy can be quite difficult, tympanometry can be a useful tool for detecting a middle ear effusion.16 An abnormal type B tympanogram (flat curve with no distinct peak) in infants presenting with acute symptoms is strong evidence in favor of AOM, although a normal test is not helpful in ruling out the diagnosis.
The diagnosis of AOM can be influenced by the physician’s perception of parental expectations for antibiotics.17 A study of children presenting with ear pain or other upper respiratory symptoms found that physicians diagnosed AOM 49% of the time when they perceived parents wanted antibiotics and only 13% of the time when they thought parents did not want antibiotics. Physicians were 23 times more likely to prescribe an antibiotic for an upper respiratory illness if they perceived that parents expected antimicrobials.
Treatment
A recent systematic review18 found that the symptoms of AOM (mainly otalgia) spontaneously resolved in two thirds of children by 24 hours and in 80% at 2 to 7 days. This was also observed in 2 earlier meta-analyses.10,19 Seventeen children would need to be treated with antibiotics (vs placebo) for 1 child to have less pain at 2 to 7 days (number needed to treat [NNT]=17). There were no differences between antibiotic and placebo groups in other clinical outcomes, such as tympanometry findings, perforation, and recurrences. Also, children treated with antibiotics were almost twice as likely to have vomiting, diarrhea, or a rash.
Initially not treating uncomplicated AOM with antibiotics is an acceptable alternative. In a study by van Buchem and colleagues,20 90% of children with AOM recovered (symptoms resolved) in the first 4 days with nose drops and oral analgesics and without the use of antibiotics. Only 3% of the 4860 children in this study had a clinical course that required further treatment with antibiotics or myringotomy. A recent randomized controlled trial of 315 children demonstrated that children treated immediately with antibiotics had 1 less day of symptoms, but that 1 in 5 of these had diarrhea.21 The group not treated with antibiotics had no serious sequellae and used more analgesics. There were no differences in the number of missed school days, and more than 75% of the parents were satisfied with this “wait and see” approach. These studies also emphasize that antibiotics have a very modest effect on the clinical course of AOM and seem to decrease the duration of symptoms only to a small degree.
Physicians often recommend other symptomatic treatments for ear infections. Non–aspirin analgesics are effective in relieving pain,21 as are ibuprofen22 and Auralgan.23 Antihistamine-decongestant preparations offer no added benefit in resolution of symptoms and have no effect on clinical outcomes when given with antibiotics.24,25
If antibiotics are used, the meta-analysis by Rosenfeld and colleagues10 showed there were no differences in outcomes between treatment with cefaclor, cefixime, erythromycin, trimethoprim-sulfamethoxazole, amoxicillin clavulanate, or erythromycin sulfisoxazole, and treatment with amoxicillin or ampicillin. Broader spectrum and/or more expensive antibiotics therefore offer no advantage over amoxicillin for the initial treatment of AOM. In another meta-analysis, Kozyrskyj and coworkers26 showed that a 5-day antibiotic course was an acceptable alternative to a 8- to 14-day treatment course. There was a slightly increased risk of treatment failure at 1-month follow-up with the shortened course of antibiotics; the NNT to prevent 1 excess failure at 30 days was 17. There were no differences in long-term outcomes (2-3 months) or medication side effects (vomiting, diarrhea, rash) between the short and long antibiotic courses. The broader spectrum azithromycin and intramuscular ceftriaxone offered no advantage over amoxicillin. Children aged younger than 2 years deserve special mention, since they are at higher risk for treatment failures,27,28 persistent symptoms,29 and recurrent otitis media.30 Few well-designed studies exist to guide treatment in this age group. Although children aged younger than 2 years were not excluded, neither review by Glasziou and colleagues18 or Rosenfeld and coworkers10 specifically examined this age group.
Another review demonstrated that (as with older children) routinely using antibiotics initially does not seem to add any clinical benefit.31 A recent randomized controlled trial of 240 children demonstrated that 8 children in this age group would have to be treated with amoxicillin for 1 child to have fewer symptoms (fever, crying, irritability) at 4 days (NNT=8).32 The major benefit of amoxicillin in this study was 1 day less of fever (P=.004). Adverse effects were almost twice as likely in the amoxicillin group, although this difference was not statistically significant. There were also no differences between the groups in clinical failure rates at 11 days or in the likelihood of recurrent otitis media, antibiotic use, specialist referrals, or surgery at 6 weeks. Effects on hearing were not measured. The authors conclude that “this modest effect does not justify prescription of antibiotics at the first visit, provided close surveillance can be guaranteed.” Also, Kozyrskyj and colleagues26 demonstrated in their meta-analysis that as a subgroup there were no differences in clinical failures between 5 and 10 days of antibiotics in children aged younger than 2 years. However, there were only 118 children in this age group. Table 2 shows treatment options for AOM.
In recent years, there has been an increasing concern about worldwide bacterial resistance to antimicrobial drugs33-35 by the World Health Organization36 and the Centers for Disease Control and Prevention (CDC).37 In response to the increasing antimicrobial resistance patterns seen in the common middle ear pathogens, especially S pneumoniae, the CDC Drug-resistant Streptococcus pneumoniae Therapeutic Working Group recommends doubling the dosage of amoxicillin to 80 to 90 mg per kg per day in the empiric treatment of AOM.38 These recommendations are based on in vitro mean inhibitory concentration data of S pneumoniae cultures from middle ear fluid and nasopharyngeal swabs. However, there currently is no patient-oriented evidence to suggest that increasing the amoxicillin dosage actually decreases suppurative or invasive complications of AOM (meningitis, mastoiditis, and so forth), affects recurrence rates or treatment success, affects long-term outcomes of AOM, or even decreases the rate of drug-resistant S pneumoniae. Also, bacteriologic outcomes do not correlate with clinical outcomes. In the meta-analysis by Rosenfeld and coworkers,10 89% of middle ear pathogens from treatment failures were susceptible in vitro to the antibiotic prescribed, and 13% of isolates from clinical cures were resistant in vitro to the prescribed antibiotic. We must use extreme caution in extrapolating the microbiologic findings to the clinical care of the child with AOM.
Prognosis
There are insufficient data to suggest that routine antibiotic use in AOM results in fewer cases of mastoiditis or meningitis. In the systematic reviews cited, the incidence of these suppurative complications was rare. In the Cochrane review by Glasziou and colleagues,18 only 1 case of mastoiditis developed in 2202 children, and this was in a child treated with penicillin. In the Netherlands among 4860 consecutive children with AOM, 2 experienced mastoiditis (both responded to outpatient antibiotic therapy), and there were no cases of meningitis.20 In the meta-analysis by Rosenfeld and coworkers,10 there were no suppurative complications in the 5400 children studied. Although mastoiditis has been quoted as being more common in the preantibiotic era, it is unclear if the current rarity of this condition is due to antibiotic treatment, changes in organism virulence or host defenses, or the assertion that uncomplicated otitis media was often not reported, thus increasing the relative rate of mastoiditis.27 In a recent review,39 antibiotics did not seem to have an appreciable effect on complication rates, leading the authors to conclude that “antibiotic treatment for AOM cannot be considered as a safeguard against the development of complications.” Even in developing countries where the burden of otitis media is great, mastoiditis is quite rare, with a prevalence rate of much less than 1%.40
Antibiotic use does influence bacterial resistance rates. In children previously treated with antibiotics for AOM, there is a 3-fold increased risk of isolating drug-resistant organisms from middle ear effusions with subsequent bouts of otitis media.41,42 In the Netherlands and Iceland, routinely not treating AOM with antibiotics has resulted in a reduction in antibiotic resistance.33,43 The most important risk factors for a poor outcome are age younger than 2 years and attendance at a daycare center.40 Children in daycare have a higher risk of requiring a hospital admission and up to a 50% increased risk of repeated or recurrent ear infections.44,45 Children with chronic underlying illnesses or chronic otitis media with effusion have added risks of poor outcomes that are beyond the scope of this review.
Conclusions
Thus, the natural course of AOM in children is quite favorable. If left untreated, 80% will recover spontaneously within 2 weeks. The addition of antibiotics provides at best a modest reduction in symptoms, while adding cost, adverse drug effects, and increasing bacterial resistance in the patient and community. Minimizing the use of antibiotics in patients with AOM does not increase the risks of perforation, deafness, or contralateral or recurrent AOM.
1. Freid VM, Makuc DM, Rooks RN. Ambulatory health care visits by children: principal diagnosis and place of visit. Vital Health Stat Series 13: data from the National Health Survey. 1998;137:1-23.
2. Klein J. Epidemiology of acute otitis media. Infect Dis 1989;8(suppl 1):89.-
3. Daly KA, Giebink GS. Clinical epidemiology of otitis media. Pediatr Infect Dis J 2000;19:S31-36.
4. Gates GA. Cost-effectiveness considerations in otitis media treatment. Otolaryngol Head Neck Surg 1996;114:525-30.
5. McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA 1995;273:214-19.
6. Taylor RB, ed. Family medicine. Principles and practice. 4th ed. Heidelberg, Germany: Springer-Verlag; 1994.
7. Bluestone CD, Doyle WJ. Anatomy and physiology of eustachian tube and middle ear related to otitis media. J Allergy Clin Immunol 1988;81:997-1003.
8. Heikkinen T, Thint M, Chonmaitree T. Prevalence of various respiratory viruses in the middle ear during acute otitis media. N Engl J Med 1999;340:260-64.
9. Ruuskanen O, Heikkinin AM, Ziegler T. Viruses in acute otitis media: increasing evidence for clinical significance. Pediatr Infect Dis J 1991;10:425-27.
10. Rosenfeld RM, Vertrees JE, Carr J, et al. Clinical efficacy of antimicrobial drugs for acute otitis media: meta-analysis of 5400 children from thirty-three randomized trials. J Pediatr 1994;124:355-67.
11. Niemela M, Uhari M, Juonio-Ervasti K, Luotonen J, Alho O, Vierimaa E. Lack of specific symptomatology in children with acute otitis media. Pediatr Infect Dis J 1994;13:765-68.
12. Heikkinen T, Ruuskanen O. Signs and symptoms predicting acute otitis media. Arch Pediatr Adolesc Med 1995;149:26-29.
13. Aorla M, Ruuskanen O, Ziegler T, et al. Clinical role of respiratory virus infection in acute otitis media. Pediatrics 1990;86:848-55.
14. Karma PH, Penttila MA, Sipila MM, Kataja MJ. Otoscopic diagnosis of middle ear effusion in acute and non-acute otitis media. I. The value of different otoscopic findings. Int J Pediatr Otolaryngol 1989;17:37-49.
15. Karma PH, Sipila MM, Kataja MJ, Penttila MA. Pneumatic otoscopy and otitis media: the value of different tympanic membrane findings and their combinations. In: Kim DJ, Bluestone CD, Klein JO, Nelson JD, Ogra PL, eds. Recent advances in otitis media: proceedings of the Fifth International Symposium. Burlington, Ontario, Canada: Decker; 1993;41-45.
16. Palmu A, Puhakka H, Rahko T, Takala AK. Diagnostic value of tympanometry in infants in clinical practice. Int J Ped Otorhinolaryngol 1999;49:207-13.
17. Mangione-Smith R, McGlynn EA, Elliott MN, Krogstad P, Brook RH. The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior. Pediatrics 1999;103:711-18.
18. Glasziou PP, Del Mar CB, Hayem M, Sanders SL. Antibiotics for acute otitis media in children (Cochrane review). In: The Cochrane library Issue 4. Oxford, England: Update Software; 2000.
19. Del Mar C, Glasziou P, Hayem M. Are antibiotics indicated as initial treatment for children with acute otitis media? A meta-analysis. BMJ 1997;314:1526-29.
20. Van Buchem FL, Peeters MF, van’t Hof MA. Acute otitis media: a new treatment strategy. BMJ 1985;290:1033-37.
21. Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ 2001;332:336-42.
22. Bertin L, Pons G, d’Athis P, et al. A randomized double blind multicentre controlled trial of ibuprofen versus acetaminophen and placebo for symptoms of acute otitis media in children. Fundam Clin Parmacol 1996;10:387-92.
23. Hoberman A, Paradise JL, Reynolds EA, Urkin J. Efficacy of Auralgan for treating ear pain in children with acute otitis media. Arch Pediatr Adolesc Med 1997;151:675-78.
24. Schnore SK, Sangster JF, Gerace TM, Bass MJ. Are antihistamine-decongestants of value in the treatment of acute otitis media in children? J Fam Pract 1986;22:39-43.
25. Bhambhani K, Foulds DM, Swamy KN, Eldis FE, Fischel JE. Acute otitis media in children: are decongestants or antihistamines necessary? Ann Emerg Med 1983;12:13-16.
26. Kozyrskyj AL, Hildes-Ripstein GE, Longstaffe SEA, et al. Short course antibiotics for acute otitis media (Cochrane review). In: The Cochrane library Issue 4. Oxford, England: Update Software; 2000.
27. Froom J, Culpepper L, Jacobs M, et al. Antimicrobials for acute otitis media? A review from the International Primary Care Network. BMJ 1997;315:98-102.
28. Iino Y, Nakamura Y, Koizumi T, Toriyama M. Prognostic factors for persistent middle ear effusion after acute otitis media in children. Acta Oto-Laryngologica 1993;113:761-65.
29. Paradise JL. Short-course antimicrobial treatment for acute otitis media: not best for infants and young children. JAMA 1997;278:1640-42.
30. Rasmussen F. Recurrence of acute otitis media at preschool age in Sweden. J Epidemiol Comm Health. 1994;48:33-35.
31. Damoiseaux RA, van Balen FA, Hoes AW, de Melker RA. Antibiotic treatment of acute otitis media in children under two years of age: evidence based? Br J Gen Pract 1998;48:1861-64.
32. Damoiseaux RAMJ, van Balen FAM, Hoes AW, Verheij TJM, de Melker RA. Primary care based randomised, double blind trial of amoxicillin versus placebo for acute otitis media in children aged under 2 years. BMJ 2000;320:350-54.
33. Neu HC. The crisis in antibiotic resistance. Science 1992; 257:1036-38. 34. Breiman RF, Butler JC, Tenover FC, Elliott JA, Facklan RR. Emergence of drug-resistant pneumococcal infections in the United States. JAMA 1994;271:1831-35.
35. Cohen ML. Epidemiology of drug-resistance: implications for the post-antimicrobial era. Science 1992;257:1050-55.
36. LeDuc JW. World Health Organization strategy for emerging infectious diseases. JAMA 1996;275:318-20.
37. Interagency Task Force on Antimicrobial Resistance. A public health action plan to combat antimicrobial resistance. Available at: www.cdc.gov/drugresistance/actionplan/index.htm.
38. Dowell SF, Butler JC, Giebink GS, et al. Acute otitis media: management and surveillance in an era of pneumococcal resistance—a report from the Drug-resistant Streptococcus pneumoniae Therapeutic Working group. Ped Infect Dis J 1999;18:1-9.
39. Dhooge IJM, Albers FWJ, van Cauwenberge PB. Intratemporal and intracranial complications of acute suppurative otitis media in children: renewed interest. Internat J Ped Otorhinolaryngol 1999;49:S109-14.
40. Berman S. Otitis media in developing countries. Pediatrics 1995;96:126-31.
41. Harrison CJ, Marks MI, Welch DF. Microbiology of recently treated acute otitis media compared with previously untreated acute otitis media. Pediatr Infect Dis J 1985;4:641-46.
42. Ford KL, Mason EO, Jr, Kaplan SL, Lamberth LB, Tillman J. Factors associated with middle ear isolates of Streptococcus pneumoniae resistant to penicillin in a children’s hospital. J Pediatrics 1991;119:941-44.
43. Stephenson J. Icelandic researchers are showing the way to bring down rates of antibiotic-resistant bacteria. JAMA 1996;275:175.
44. Hardy AM, Fowler MG. Child care arrangements and repeated ear infections in young children. Am J Public Health 1993;83:1321-25.
45. Louhiala PJ, Jaakkola N, Ruotsalainen R, Jaakkola JJ. Form of day care and respiratory infection among Finnish children. Am J Public 1995;85:1109-12. 46.
1. Freid VM, Makuc DM, Rooks RN. Ambulatory health care visits by children: principal diagnosis and place of visit. Vital Health Stat Series 13: data from the National Health Survey. 1998;137:1-23.
2. Klein J. Epidemiology of acute otitis media. Infect Dis 1989;8(suppl 1):89.-
3. Daly KA, Giebink GS. Clinical epidemiology of otitis media. Pediatr Infect Dis J 2000;19:S31-36.
4. Gates GA. Cost-effectiveness considerations in otitis media treatment. Otolaryngol Head Neck Surg 1996;114:525-30.
5. McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA 1995;273:214-19.
6. Taylor RB, ed. Family medicine. Principles and practice. 4th ed. Heidelberg, Germany: Springer-Verlag; 1994.
7. Bluestone CD, Doyle WJ. Anatomy and physiology of eustachian tube and middle ear related to otitis media. J Allergy Clin Immunol 1988;81:997-1003.
8. Heikkinen T, Thint M, Chonmaitree T. Prevalence of various respiratory viruses in the middle ear during acute otitis media. N Engl J Med 1999;340:260-64.
9. Ruuskanen O, Heikkinin AM, Ziegler T. Viruses in acute otitis media: increasing evidence for clinical significance. Pediatr Infect Dis J 1991;10:425-27.
10. Rosenfeld RM, Vertrees JE, Carr J, et al. Clinical efficacy of antimicrobial drugs for acute otitis media: meta-analysis of 5400 children from thirty-three randomized trials. J Pediatr 1994;124:355-67.
11. Niemela M, Uhari M, Juonio-Ervasti K, Luotonen J, Alho O, Vierimaa E. Lack of specific symptomatology in children with acute otitis media. Pediatr Infect Dis J 1994;13:765-68.
12. Heikkinen T, Ruuskanen O. Signs and symptoms predicting acute otitis media. Arch Pediatr Adolesc Med 1995;149:26-29.
13. Aorla M, Ruuskanen O, Ziegler T, et al. Clinical role of respiratory virus infection in acute otitis media. Pediatrics 1990;86:848-55.
14. Karma PH, Penttila MA, Sipila MM, Kataja MJ. Otoscopic diagnosis of middle ear effusion in acute and non-acute otitis media. I. The value of different otoscopic findings. Int J Pediatr Otolaryngol 1989;17:37-49.
15. Karma PH, Sipila MM, Kataja MJ, Penttila MA. Pneumatic otoscopy and otitis media: the value of different tympanic membrane findings and their combinations. In: Kim DJ, Bluestone CD, Klein JO, Nelson JD, Ogra PL, eds. Recent advances in otitis media: proceedings of the Fifth International Symposium. Burlington, Ontario, Canada: Decker; 1993;41-45.
16. Palmu A, Puhakka H, Rahko T, Takala AK. Diagnostic value of tympanometry in infants in clinical practice. Int J Ped Otorhinolaryngol 1999;49:207-13.
17. Mangione-Smith R, McGlynn EA, Elliott MN, Krogstad P, Brook RH. The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior. Pediatrics 1999;103:711-18.
18. Glasziou PP, Del Mar CB, Hayem M, Sanders SL. Antibiotics for acute otitis media in children (Cochrane review). In: The Cochrane library Issue 4. Oxford, England: Update Software; 2000.
19. Del Mar C, Glasziou P, Hayem M. Are antibiotics indicated as initial treatment for children with acute otitis media? A meta-analysis. BMJ 1997;314:1526-29.
20. Van Buchem FL, Peeters MF, van’t Hof MA. Acute otitis media: a new treatment strategy. BMJ 1985;290:1033-37.
21. Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ 2001;332:336-42.
22. Bertin L, Pons G, d’Athis P, et al. A randomized double blind multicentre controlled trial of ibuprofen versus acetaminophen and placebo for symptoms of acute otitis media in children. Fundam Clin Parmacol 1996;10:387-92.
23. Hoberman A, Paradise JL, Reynolds EA, Urkin J. Efficacy of Auralgan for treating ear pain in children with acute otitis media. Arch Pediatr Adolesc Med 1997;151:675-78.
24. Schnore SK, Sangster JF, Gerace TM, Bass MJ. Are antihistamine-decongestants of value in the treatment of acute otitis media in children? J Fam Pract 1986;22:39-43.
25. Bhambhani K, Foulds DM, Swamy KN, Eldis FE, Fischel JE. Acute otitis media in children: are decongestants or antihistamines necessary? Ann Emerg Med 1983;12:13-16.
26. Kozyrskyj AL, Hildes-Ripstein GE, Longstaffe SEA, et al. Short course antibiotics for acute otitis media (Cochrane review). In: The Cochrane library Issue 4. Oxford, England: Update Software; 2000.
27. Froom J, Culpepper L, Jacobs M, et al. Antimicrobials for acute otitis media? A review from the International Primary Care Network. BMJ 1997;315:98-102.
28. Iino Y, Nakamura Y, Koizumi T, Toriyama M. Prognostic factors for persistent middle ear effusion after acute otitis media in children. Acta Oto-Laryngologica 1993;113:761-65.
29. Paradise JL. Short-course antimicrobial treatment for acute otitis media: not best for infants and young children. JAMA 1997;278:1640-42.
30. Rasmussen F. Recurrence of acute otitis media at preschool age in Sweden. J Epidemiol Comm Health. 1994;48:33-35.
31. Damoiseaux RA, van Balen FA, Hoes AW, de Melker RA. Antibiotic treatment of acute otitis media in children under two years of age: evidence based? Br J Gen Pract 1998;48:1861-64.
32. Damoiseaux RAMJ, van Balen FAM, Hoes AW, Verheij TJM, de Melker RA. Primary care based randomised, double blind trial of amoxicillin versus placebo for acute otitis media in children aged under 2 years. BMJ 2000;320:350-54.
33. Neu HC. The crisis in antibiotic resistance. Science 1992; 257:1036-38. 34. Breiman RF, Butler JC, Tenover FC, Elliott JA, Facklan RR. Emergence of drug-resistant pneumococcal infections in the United States. JAMA 1994;271:1831-35.
35. Cohen ML. Epidemiology of drug-resistance: implications for the post-antimicrobial era. Science 1992;257:1050-55.
36. LeDuc JW. World Health Organization strategy for emerging infectious diseases. JAMA 1996;275:318-20.
37. Interagency Task Force on Antimicrobial Resistance. A public health action plan to combat antimicrobial resistance. Available at: www.cdc.gov/drugresistance/actionplan/index.htm.
38. Dowell SF, Butler JC, Giebink GS, et al. Acute otitis media: management and surveillance in an era of pneumococcal resistance—a report from the Drug-resistant Streptococcus pneumoniae Therapeutic Working group. Ped Infect Dis J 1999;18:1-9.
39. Dhooge IJM, Albers FWJ, van Cauwenberge PB. Intratemporal and intracranial complications of acute suppurative otitis media in children: renewed interest. Internat J Ped Otorhinolaryngol 1999;49:S109-14.
40. Berman S. Otitis media in developing countries. Pediatrics 1995;96:126-31.
41. Harrison CJ, Marks MI, Welch DF. Microbiology of recently treated acute otitis media compared with previously untreated acute otitis media. Pediatr Infect Dis J 1985;4:641-46.
42. Ford KL, Mason EO, Jr, Kaplan SL, Lamberth LB, Tillman J. Factors associated with middle ear isolates of Streptococcus pneumoniae resistant to penicillin in a children’s hospital. J Pediatrics 1991;119:941-44.
43. Stephenson J. Icelandic researchers are showing the way to bring down rates of antibiotic-resistant bacteria. JAMA 1996;275:175.
44. Hardy AM, Fowler MG. Child care arrangements and repeated ear infections in young children. Am J Public Health 1993;83:1321-25.
45. Louhiala PJ, Jaakkola N, Ruotsalainen R, Jaakkola JJ. Form of day care and respiratory infection among Finnish children. Am J Public 1995;85:1109-12. 46.
Is treatment of hypertension with acetylcholine esterase inhibitors (ACEIs) superior to other antihypertensives in preventing significant cardiovascular events and death in patients with type 2 diabetes?
BACKGROUND: Strong evidence exists that the greater the blood pressure reduction in patients with type 2 diabetes, the greater the clinical benefit in reducing significant cardiovascular events and death.1 It is not known whether these benefits are actually due to the lowering of blood pressure or if there is a drug class effect, particularly among ACEIs.
POPULATION STUDIED: The average age of participants in the 4 studies was 58 years, and 60% were men. The study settings (primary care or referral) were not reported. Baseline blood pressures ranged from 155 to 170 systolic and 93 to 98 diastolic. The duration of diabetes was 8.5 to 10.7 years in 2 studies, 2.7 years in 1 study, and was not reported in 1 study.
STUDY DESIGN AND VALIDITY: This was a meta-analysis. The authors performed a MEDLINE search for studies pertaining to ACEIs, diabetes, and hypertension but did not search any other databases such as the Cochrane Controlled Trials Register. Studies were included if they were randomized controlled trials of patients with type 2 diabetes that evaluated an ACEI versus another antihypertensive medication with a minimum follow-up of 2 years. There was no indication whether retrieved studies were reviewed independently by 2 or more authors for inclusion. Tests for heterogeneity were appropriately applied to assure that only data from similar studies were combined. A fixed effects model, which assumes homogeneity, was used to combine data.
OUTCOMES MEASURED: The outcomes measured were acute myocardial infarction (AMI), stroke, combined cardiovascular events, and all-cause mortality. The combined cardiovascular events varied depending on the particular trial and could include cardiovascular death, fatal and nonfatal MI, fatal and nonfatal stroke, angina, congestive heart failure, and pulmonary infarction.
RESULTS: The initial search identified 195 articles of which 4 studies with a total of 2180 patients met the inclusion criteria. After applying tests for heterogeneity, only data from 3 trials (which studied enalopril vs nisoldipine, captopril vs diuretic/b-blocker, and fosinopril vs amlodipine) were used in the meta-analysis. In one of these trials (captopril vs diuretic/b-blocker), the number of events in persons with diabetes was not reported; it was therefore estimated by the authors of this review. This is a limitation of this meta-analysis. The relative risk calculations for these 3 studies showed that using ACEIs versus other antihypertensives lowered the number of AMIs (summary risk ratio [RR]=0.37; 95% confidence interval [CI], 0.24-0.57), had no affect on the incidence of stroke (RR=0.76; 95% CI, 0.48-1.22), lowered the number of combined cardiovascular events (RR=0.49; 95% CI, 0.36-0.67), and lowered overall cardiovascular mortality (RR=0.57; 95% CI, 0.38-0.87). On the basis of these data, to prevent an additional AMI, cardiovascular event, or death one would have to treat 17, 13, and 40 patients respectively with an ACEI instead of another agent for approximately 4.5 years. The study excluded from the meta-analysis compared outcomes in patients taking an ACEI versus atenolol and found no statistically significant differences between the groups for the 4 clinical outcomes.1
Lowering blood pressure in patients with type 2 diabetes who have hypertension has clear benefits in terms of reducing the number of AMIs, cardiovascular events, and deaths. Although the data presented in this meta-analysis suggest that ACEIs may be more effective than calcium-channel blockers or the combination of a diuretic and a b-blocker, they are not conclusive. In particular, atenolol may have a similar benefit to ACEIs. The decision to use ACEIs in people with diabetes who have hypertension should continue to be made based on patient-specific clinical factors, their effectiveness in lowering blood pressure, and current evidence of benefit in patients with comorbid conditions (eg, microalbuminuria and congestive heart failure).
BACKGROUND: Strong evidence exists that the greater the blood pressure reduction in patients with type 2 diabetes, the greater the clinical benefit in reducing significant cardiovascular events and death.1 It is not known whether these benefits are actually due to the lowering of blood pressure or if there is a drug class effect, particularly among ACEIs.
POPULATION STUDIED: The average age of participants in the 4 studies was 58 years, and 60% were men. The study settings (primary care or referral) were not reported. Baseline blood pressures ranged from 155 to 170 systolic and 93 to 98 diastolic. The duration of diabetes was 8.5 to 10.7 years in 2 studies, 2.7 years in 1 study, and was not reported in 1 study.
STUDY DESIGN AND VALIDITY: This was a meta-analysis. The authors performed a MEDLINE search for studies pertaining to ACEIs, diabetes, and hypertension but did not search any other databases such as the Cochrane Controlled Trials Register. Studies were included if they were randomized controlled trials of patients with type 2 diabetes that evaluated an ACEI versus another antihypertensive medication with a minimum follow-up of 2 years. There was no indication whether retrieved studies were reviewed independently by 2 or more authors for inclusion. Tests for heterogeneity were appropriately applied to assure that only data from similar studies were combined. A fixed effects model, which assumes homogeneity, was used to combine data.
OUTCOMES MEASURED: The outcomes measured were acute myocardial infarction (AMI), stroke, combined cardiovascular events, and all-cause mortality. The combined cardiovascular events varied depending on the particular trial and could include cardiovascular death, fatal and nonfatal MI, fatal and nonfatal stroke, angina, congestive heart failure, and pulmonary infarction.
RESULTS: The initial search identified 195 articles of which 4 studies with a total of 2180 patients met the inclusion criteria. After applying tests for heterogeneity, only data from 3 trials (which studied enalopril vs nisoldipine, captopril vs diuretic/b-blocker, and fosinopril vs amlodipine) were used in the meta-analysis. In one of these trials (captopril vs diuretic/b-blocker), the number of events in persons with diabetes was not reported; it was therefore estimated by the authors of this review. This is a limitation of this meta-analysis. The relative risk calculations for these 3 studies showed that using ACEIs versus other antihypertensives lowered the number of AMIs (summary risk ratio [RR]=0.37; 95% confidence interval [CI], 0.24-0.57), had no affect on the incidence of stroke (RR=0.76; 95% CI, 0.48-1.22), lowered the number of combined cardiovascular events (RR=0.49; 95% CI, 0.36-0.67), and lowered overall cardiovascular mortality (RR=0.57; 95% CI, 0.38-0.87). On the basis of these data, to prevent an additional AMI, cardiovascular event, or death one would have to treat 17, 13, and 40 patients respectively with an ACEI instead of another agent for approximately 4.5 years. The study excluded from the meta-analysis compared outcomes in patients taking an ACEI versus atenolol and found no statistically significant differences between the groups for the 4 clinical outcomes.1
Lowering blood pressure in patients with type 2 diabetes who have hypertension has clear benefits in terms of reducing the number of AMIs, cardiovascular events, and deaths. Although the data presented in this meta-analysis suggest that ACEIs may be more effective than calcium-channel blockers or the combination of a diuretic and a b-blocker, they are not conclusive. In particular, atenolol may have a similar benefit to ACEIs. The decision to use ACEIs in people with diabetes who have hypertension should continue to be made based on patient-specific clinical factors, their effectiveness in lowering blood pressure, and current evidence of benefit in patients with comorbid conditions (eg, microalbuminuria and congestive heart failure).
BACKGROUND: Strong evidence exists that the greater the blood pressure reduction in patients with type 2 diabetes, the greater the clinical benefit in reducing significant cardiovascular events and death.1 It is not known whether these benefits are actually due to the lowering of blood pressure or if there is a drug class effect, particularly among ACEIs.
POPULATION STUDIED: The average age of participants in the 4 studies was 58 years, and 60% were men. The study settings (primary care or referral) were not reported. Baseline blood pressures ranged from 155 to 170 systolic and 93 to 98 diastolic. The duration of diabetes was 8.5 to 10.7 years in 2 studies, 2.7 years in 1 study, and was not reported in 1 study.
STUDY DESIGN AND VALIDITY: This was a meta-analysis. The authors performed a MEDLINE search for studies pertaining to ACEIs, diabetes, and hypertension but did not search any other databases such as the Cochrane Controlled Trials Register. Studies were included if they were randomized controlled trials of patients with type 2 diabetes that evaluated an ACEI versus another antihypertensive medication with a minimum follow-up of 2 years. There was no indication whether retrieved studies were reviewed independently by 2 or more authors for inclusion. Tests for heterogeneity were appropriately applied to assure that only data from similar studies were combined. A fixed effects model, which assumes homogeneity, was used to combine data.
OUTCOMES MEASURED: The outcomes measured were acute myocardial infarction (AMI), stroke, combined cardiovascular events, and all-cause mortality. The combined cardiovascular events varied depending on the particular trial and could include cardiovascular death, fatal and nonfatal MI, fatal and nonfatal stroke, angina, congestive heart failure, and pulmonary infarction.
RESULTS: The initial search identified 195 articles of which 4 studies with a total of 2180 patients met the inclusion criteria. After applying tests for heterogeneity, only data from 3 trials (which studied enalopril vs nisoldipine, captopril vs diuretic/b-blocker, and fosinopril vs amlodipine) were used in the meta-analysis. In one of these trials (captopril vs diuretic/b-blocker), the number of events in persons with diabetes was not reported; it was therefore estimated by the authors of this review. This is a limitation of this meta-analysis. The relative risk calculations for these 3 studies showed that using ACEIs versus other antihypertensives lowered the number of AMIs (summary risk ratio [RR]=0.37; 95% confidence interval [CI], 0.24-0.57), had no affect on the incidence of stroke (RR=0.76; 95% CI, 0.48-1.22), lowered the number of combined cardiovascular events (RR=0.49; 95% CI, 0.36-0.67), and lowered overall cardiovascular mortality (RR=0.57; 95% CI, 0.38-0.87). On the basis of these data, to prevent an additional AMI, cardiovascular event, or death one would have to treat 17, 13, and 40 patients respectively with an ACEI instead of another agent for approximately 4.5 years. The study excluded from the meta-analysis compared outcomes in patients taking an ACEI versus atenolol and found no statistically significant differences between the groups for the 4 clinical outcomes.1
Lowering blood pressure in patients with type 2 diabetes who have hypertension has clear benefits in terms of reducing the number of AMIs, cardiovascular events, and deaths. Although the data presented in this meta-analysis suggest that ACEIs may be more effective than calcium-channel blockers or the combination of a diuretic and a b-blocker, they are not conclusive. In particular, atenolol may have a similar benefit to ACEIs. The decision to use ACEIs in people with diabetes who have hypertension should continue to be made based on patient-specific clinical factors, their effectiveness in lowering blood pressure, and current evidence of benefit in patients with comorbid conditions (eg, microalbuminuria and congestive heart failure).