User login
Improving Antibiotic Utilization among Hospitalists
Inappropriate antibiotic use is a major public health concern and demonstrates the need for quality improvement initiatives in the delivery of health care.16 Each year nearly 2 million patients in the United States acquire an infection in the hospital, and about 90,000 of them die from these infections.7 More than 70% of the bacteria that cause hospital‐acquired infections are resistant to at least one commonly used drug.7 Persons infected with drug‐resistant organisms have longer hospital stays and higher mortality rates.7
Inappropriate antibiotic use in the inpatient hospital setting can be classified into 5 categories. First, antibiotics may be given for illnesses for which they are not indicated (eg, viral infections). Second, broad‐spectrum antibiotics (such as piperacillin‐tazobactam and quinolones) may be overused in the empiric treatment of common infections.8 Overuse of broad‐spectrum drugs increases selective pressure for antimicrobial resistance and exposes patients to the side effects of some of these drugs, such as Clostridium difficile colitis.8 Third, clinicians occasionally prescribe intravenous (IV) antibiotics when the efficacy of oral agents would be similar. Inappropriate intravenous therapy increases the cost of care and also exposes the patient to the risk of intravenous catheters.8 Fourth, when the correct antibiotic choice is made, inappropriate antibiotic dosage, schedule, and/or duration of treatment can threaten patient safety.8 Fifth, bug‐drug mismatch occurs when susceptibility studies indicate that the drug being used is ineffective or only marginally effective.8 Beyond antimicrobial resistance and safety, these practices also usually increase costs to both the patient and the hospital.7, 910
Influencing providers' prescribing patterns is difficult.11 In this project we assessed the prescribing patterns of hospitalists in an active inpatient environment and then developed an intervention to improve the providers' use of antibiotics. The intervention utilized public health methodologyprior to implementation, we defined the problem, determined its magnitude, identified a behavior change model, and constructed a conceptual framework that identifyied the key determinants. A pilot academic detailing project addressing many determinants was developed, implemented, and evaluated.
Conceptual Model
To change prescribing behaviors is to change learned behaviors. Changing behavior is a complex process affected by several factors including beliefs, expectations, motivations, and the psychosocial environments of the target groups.12 Each of these factors must be considered when attempting to bring about behavior changes. In doing so, a theory that can be depicted in a model often emerges.13 This approach is widely used in understanding and developing public health interventions.
Formulating the Model
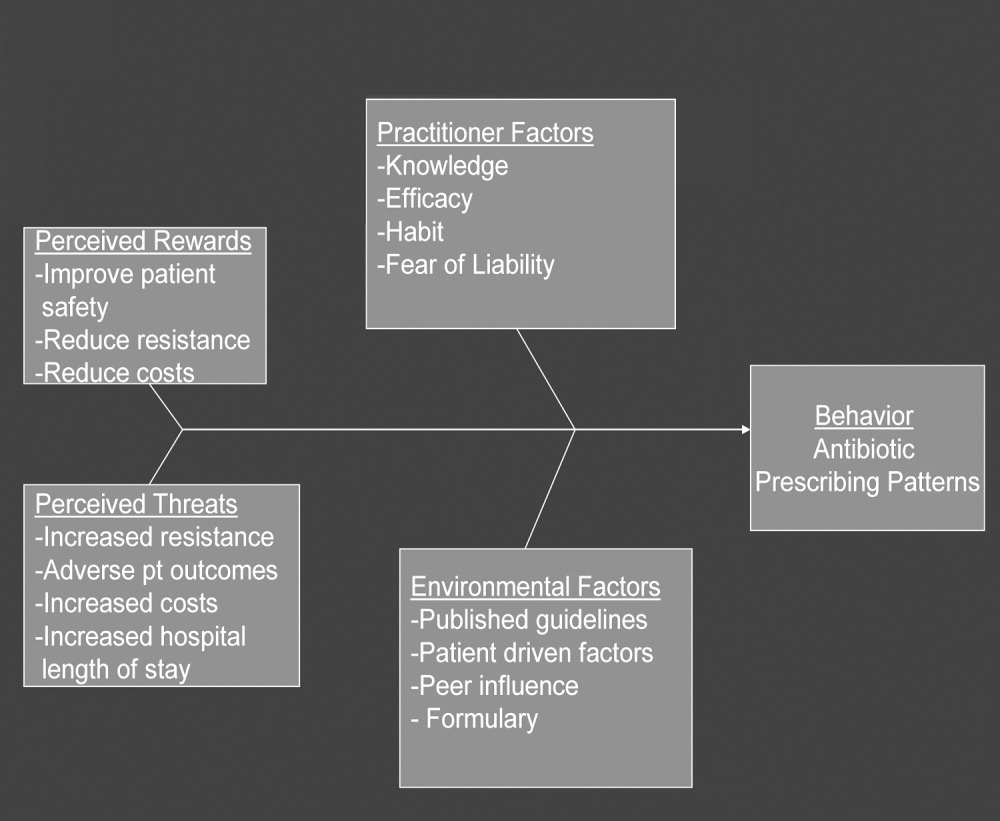
In any public health intervention, recognizing and engaging key stakeholders is a critical step. We identified the following stakeholders: (1) hospitalist practitioners and other prescribing providers including residents and infectious disease specialists; (2) nurses; (3) administrators who are focused on cost effectiveness; (4) patients and their families, who want to get well affordably, without side effects; (5) pharmacists; (6) risk management; and (7) society, which is fearful of the propagation of resistant microbes. In consulting with some of the stakeholders, 4 factors that influence hospitalists' prescribing patterns became apparent. These are practitioner factors, environmental factors, perceived rewards, and perceived threats (Fig. 1).
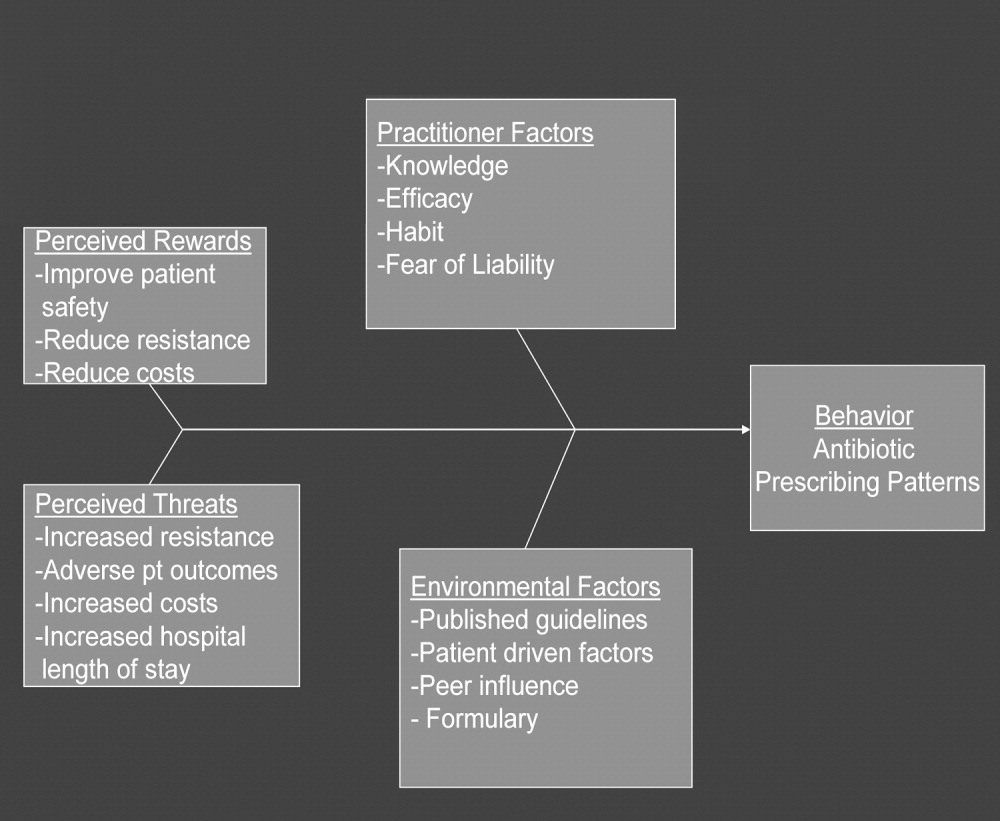
The practitioner factors shaping prescribing are: (1) knowledge of current best care; (2) self‐efficacy, which determines whether a provider is confident in his or her knowledge to adequately treat a specific infection; (3) habit, which causes providers to pick from a narrow repertoire of antibiotics when treating an infection; and (4) fear of liability, which forces some providers to be cautious. Four environmental factors affecting antibiotic prescriptions are: (1) published guidelines regarding organisms' sensitivity to antibiotics; (2) patient‐driven factors such as affordability, compliance with dosing regimens, side effects, and interactions between the antibiotics and other medications; (3) peer influence, in that providers are reluctant to change a prescription started by another provider (eg, emergency room physician); and (4) the formulary of the hospital, as it forces providers to prescribe within specific parameters. The perceived rewards of specific prescribing practices may include improving patient safety and reducing antibiotic resistance and costs, whereas the perceived threats are increasing antimicrobial resistance, having adverse patient outcomes, and increasing costs and hospital length of stay. We selected a high‐yield, low‐effort intervention in order to have an impact on some of the factors underlying hospitalists' prescribing patterns.
METHODS
Participants
The study participants were 17 hospitalist practitioners including physicians, nurse‐practitioners, and physician assistants who make up the Collaborative Inpatient Medical Service (CIMS) at Johns Hopkins Bayview Medical Center (JHBMC; Table 1). All consented to participate. The study was approved by the institutional review board.
| Age in years, mean (SD) | 36 (6) |
| Female, n (%) | 13 (76%) |
| Physician, n (%) | 9 (53%) |
| Nurse‐practitioner, n (%) | 5 (29%) |
| Physician assistant, n (%) | 3 (18%) |
| Years in practice, mean (SD) | 5.1 (2.8) |
| Number of pharmaceutical representatives exposed to in past year, mean | 1 |
| Number of shifts worked per month, mean (SD) | 14 (4) |
| Primarily works days, n (%) | 13 (76%) |
Data Collection
We collected and assessed prescription patterns over 3 periods: preintervention, interim, and postintervention.
Assessing Appropriateness of Antibiotics
For each order that was assessed in the preintervention, interim, and postintervention periods, the following information was collected: (1) drug ordered, (2) clinical diagnosis, (3) microbiology results available at the time of the order (including relevant results from recent cultures), (4) other medical diagnoses (ICD9 codes), (5) allergies, and (6) exposure to health care facilities (within the past 30 days). The computerized medical record allowed access to the discharge summaries of a patient's hospitalization. These records summarized the patient's hospitalization, allowing the investigators to understand the reasons for a provider's choice of antibiotics. If the rationale was not clear about how to categorize a prescription from reading the data, the investigators performed a chart review. From the information culled from these reviews, the primary investigator and an infectious disease specialist classified each prescription order by consensus as appropriate, effective but inappropriate, or inappropriate therapy.
Prescriptions were classified as appropriate when they were indicated and correlated with sensitivities, if available, or were of a narrow‐enough spectrum and recommended as a first‐line treatment for specific illnesses by either the Johns Hopkins Antibiotic Guide14 or the Stanford Guide to Antimicrobial Therapy.15 For example, cephalexin to treat uncomplicated cellulitis was considered appropriate therapy. Effective but inappropriate prescriptions were broad‐spectrum antibiotics used to treat an infection when a narrower‐spectrum antibiotic would have sufficed. For example, piperacillin‐tazobactam would be effective in treating a simple urinary tract infection but inappropriate to use because of its broad spectrum. Other examples of effective but inappropriate prescriptions were giving an IV when an oral alternative would be equally effective and tolerated or prescribing antibiotic treatment whose duration was too long. Finally, inappropriate prescriptions were those written for conditions for which antibiotics are not indicated or for which the prescribed antibiotic was ineffective for the specified infection (bug‐drug mismatch).
Preintervention
In January 2006 the investigators retrospectively reviewed the prescribing patterns of the 17 providers over the previous year. Using the computerized medical record and physician order entry, consecutive prescriptions of each provider were evaluated, beginning December 31, 2005, going back reverse chronologically until 20 prescriptions had been identified. For 12 of the providers, it was actually possible to review 20 prescriptions. For 2 other providers, both new, part‐time additions to the hospitalist group, only 1 and 7 prescriptions were found for the entire year. The prescribing history of the 3 remaining providers who participated in the study, all physician assistants, could not be evaluated (during any period) because all their orders were linked only to physicians, making it impossible to determine their specific prescriptions using the physician order entry system.
Interim
During the interim period between obtaining informed consent and completing the academic detailing (January 3, 2006, to March 23, 2006), provider prescribing patterns were reviewed to determine if the mere knowledge of the project would produce changes in prescribing behavior.
Postintervention
After the academic detailing was completed (March 23, 2006), the prescribing patterns of the hospitalists were followed through April 23, 2006. Each week after the detailing session, the hospitalists received reminders to prescribe appropriately (including pens with the message Reduce the Overuse).
Detailing Procedures
After the review, a profile was assembled for each of the CIMS providers. The study team detailers (a physician and a pharmacist) met with the individual providers for 30 to 45 minutes. Each hospitalist participant completed a short survey that collected demographic information and was asked about the rationale for his or her antibiotic prescribing pattern. Next, the appraisal of the provider's prescribing pattern was reviewed. This review included looking at the costs of the prescribed antibiotics compared with those of the appropriate alternatives and a reexamination of the guidelines for the selected target drugspiperacillin‐tazobactam, vancomycin, and extended‐spectrum quinolones. These 3 antibiotics were picked because our providers had been particularly vulnerable to inappropriately prescribing them. The hospitalists were provided an antibiotic guide developed specifically for this project and based on the Johns Hopkins Antibiotic Guide14 that summarizes the consensus guidelines.
Data Analysis
The primary outcome variable was the aggregate proportion of inappropriate antibiotic prescribed (as defined earlier) before the intervention, during the interim between obtaining informed consent and intervening on all study subjects, and after the intervention. The percentage of appropriate prescriptions versus total not appropriate prescriptions (combining of the effective but inappropriate and inappropriate categories) were compared across the 3 periods. Ninety‐five percent confidence intervals for comparisons of the proportions were determined using Stata 9.0 (College Station, TX). The difference between the proportions of total not appropriate prescriptions before and after academic detailing was computed in Stata using Fisher's exact test to assess significance.
RESULTS
Demographic information and professional characteristics of the 17 providers are shown in Table 1. Their mean age was 36 years, and 76% were female. The top 4 reasons the providers gave for their prescribing practices were: (1) published guidelines, (2) easier dosing schedule for patient when discharged, (3) continuing an antibiotic course initiated in the emergency room, and (4) broad‐spectrum antibiotics cover all possible microbes.
Comparison of Preintervention, Interim, and Postintervention Periods
Table 2 depicts the results of the prescription appraisals from the retrospective reviews. Of the 14 providers who had ordered antibiotics, 8 (57%) had more prescriptions that were total not appropriate than were appropriate in the preintervention period compared with 3 providers (25%) with this prescribing pattern in the postintervention period (P = .13).
| Provider | Preintervention | Postintervention | ||||
|---|---|---|---|---|---|---|
| Prescriptions (n) | Appropriate, n (%) | Total not appropriate, n (%) | Prescriptions (n) | Appropriate, n (%) | Total not appropriate, n (%) | |
| ||||||
| 1 | 20 | 7 (35%) | 13 (65%) | 24 | 17 (70.8%) | 7 (29.2%) |
| 2 | 20 | 10 (50%) | 10 (50%) | 12 | 11 (91.7%) | 1 (8.3%) |
| 3 | 20 | 6 (30%) | 14 (70%) | 8 | 8 (100%) | 0 (0%) |
| 4* | 19 | 10 (52.6%) | 9 (47.4%) | 4 | 3 (75%) | 1 (25%) |
| 5 | 20 | 9 (45%) | 11 (55%) | 10 | 4 (40%) | 6 (60%) |
| 6 | 20 | 5 (25%) | 15 (75%) | 3 | 1 (33.3%) | 2 (66.7%) |
| 7 | 20 | 8 (40%) | 12 (60%) | 8 | 7 (87.5%) | 1 (12.5%) |
| 8* | 1 | 0 (0%) | 1 (100%) | 0 | 0 (0%) | 0 (0%) |
| 9 | 20 | 11 (55%) | 9 (45%) | 5 | 2 (40%) | 3 (60%) |
| 10* | 7 | 3 (42.9%) | 4 (57.1%) | 0 | 0 (0%) | 0 (0%) |
| 11 | 20 | 10 (50%) | 10 (50%) | 17 | 13 (76.5%) | 4 (23.5%) |
| 12 | 20 | 6 (30%) | 14 (70%) | 16 | 14 (87.5%) | 2 (12.5%) |
| 13 | 20 | 12 (60%) | 8 (40%) | 15 | 11 (73.3%) | 4 (26.7%) |
| 14 | 20 | 10 (50%) | 10 (50%) | 7 | 4 (57.1%) | 3 (42.9%) |
| Total | 247 | 107 (43%) | 140 (57%) | 129 | 95 (73.6%) | 34 (26.4%) |
Table 3 shows the proportions of appropriate, effective but inappropriate, and total not appropriate prescriptions in the retrospective, interim, and postintervention periods. Forty‐three percent (95% CI 37%‐49%) of prescriptions were judged to be appropriate, and 57% (95% CI 51%‐63%) to be not appropriate prior to the academic detailing. In the interim period, 59% (95% CI 52%‐65%) of the prescriptions were appropriate, and 41% (95% CI 35%‐48%) were not appropriate; P = .0003. After the intervention, 74% (95% CI 65%‐81%) of the prescriptions were appropriate, and 26% (95% CI 19%‐35%) were not appropriate; P < .0001.
| Period | Appropriate, n (%) | 95% CI | Effective but inappropriate, n (%) | Inappropriate, n (%) | Total not appropriate, n (%) | 95% CI | P value* |
|---|---|---|---|---|---|---|---|
| |||||||
| Retrospective review (pre) | 107 (43%) | 37%‐49% | 75 (30.4%) | 65 (26.6%) | 140 (57%) | 51%‐63% | |
| Interim | 146 (59%) | 52%‐65% | 37 (15%) | 65 (26%) | 102 (41%) | 35%‐48% | .0003 |
| Postintervention | 95 (74%) | 65%‐81% | 8 (6%) | 26 (20%) | 34 (26%) | 19%‐35% | < .0001 |
DISCUSSION
We have demonstrated that academic detailing had a positive impact on the prescribing patterns of hospitalists. The aggregated improvement in antibiotic prescribing patterns can be attributed to improvement in the prescribing patterns of almost every hospitalist practitioner (Table 2). This study focused on aggregate prescriptions as the primary outcome measure because the hospitalists at JHBMC, like at many other institutions, function as a team, with a patient routinely having multiple providers over the course of the hospital stay. The improved prescribing patterns noted during the interim period suggest that the mere knowledge of a project can have an impact on providers. Providers informed the investigators that they were more thoughtful about their choice of antibiotics when they knew that they were being studied. The further statistically significant improvement in prescribing patterns with the intervention shows that the academic detailing itself was successful.
The greatest absolute change in practice was seen in effective but inappropriate prescribing (from 30.4% to 6%), whereas inappropriate prescribing only decreased from 26.6% to 20.6%. Although we aimed to have an impact on all inappropriate antibiotic prescribing patterns, we specifically reviewed the prescribing guidelines for piperacillin‐tazobactam, extended‐spectrum quinolones, and vancomycin. These 3 antibiotics were targeted because our providers had been particularly susceptible to inappropriately prescribing them. The focus on these antibiotics may have resulted in the larger absolute change noted in effective but inappropriate prescribing. We did not collect any data to determine if having an impact on effective but inappropriate prescribing changed the clinical course of the patients, such as shortening their hospital stays. Anecdotal evidence, however, suggests that it does. At our institution it is not uncommon for patients to be kept in the hospital for an extra day to ensure they are stable when transitioned from extended‐spectrum to narrower‐spectrum antibiotics prior to discharge. The effect of reducing effective but inappropriate prescriptions on the clinical course of patients could be an outcome measure assessed by a future, larger study.
Our one‐on‐one appraisal of each provider's prescribing patterns included a review of the cost of the prescribed antibiotics compared with that of the appropriate alternatives. Although decisions on antibiotic choice should be driven by clinical guidelines and appropriateness rather than price, we believed it was relevant to include education about costs and pricing so that providers would be reminded to ascertain whether patients would be able to afford their antibiotics. Antibiotic resistance is influenced by a patient's failure to complete the course of treatment, and noncompliance may be caused by an inability to afford the medication. Often, there are affordable, appropriate alternatives to the newest and most expensive drugs.
A hospitalist‐based academic detailing approach to improving antibiotic prescribing may have far‐reaching benefits and influence. First, it has the potential to affect other practitioners by setting an example and role modeling. In addition to that with their immediate peer group, hospitalists have close and repeated contact with house officers and emergency room physicians and often act as consultants to physicians in other departments such as surgery and psychiatry. Furthermore, some community hospitals have no infectious disease specialists readily available. So this represents an opportunity for hospitalists to promote quality in antibiotic prescribing. Practice‐based learning was very effective because it brought the practitioners face to face with their prescribing patterns. Although intellectually everyone agreed that antibiotics are often misused, this approach forced the providers to stop and reflect on their individual practices. This peer‐delivered intervention allowed for a collaborative approach to solving the problem; the peer (detailer) was approachable, nonjudgmental, and available for further discussion and guidance.
The public health quality improvement approach that we used for our intervention helped us to realize and appreciate the factors underlying prescribing patterns. Only by understanding the motivations for prescribing patterns can we hope to make sustainable changes. This coincides with our previous assertion that hospitalists are engaging in some public health practice.16 In pubic health, the programs, services, and institutions involved emphasize the prevention of disease and the health needs of the population as a whole.17 Hospitalist teams aim to make sure that the high‐quality services needed for protecting the health of their community (hospitalized patients) are available and that this population receives proper consideration in the allocation of resources. Antibiotic optimization is a key role that could fall within the mantra of public health practice for the hospitalist.
Several limitations of this pilot should be considered. First, the intervention is labor intensive. However, it is essential to use the problem‐solving paradigm and incorporate behavior change theories in order to identify interventions that can lead to sustainable change. Second, this was not a randomized controlled trial, and it is possible that there might have been some contamination by external forces. However, in reviewing the educational events at our institution, the press, and articles published during the study period, we could not identify any external factors that would have influenced antibiotic prescribing patterns. It would not have been possible to conduct a randomized trial at our institution because the hospitalists work so closely together that we could not ensure complete separation if the subjects were randomized. There would have been contamination from the intervention group to the control group. A trial with randomization at the institution level is the next step. Third, the number of months retrospectively reviewed in order to identify 20 prescriptions of a provider varied. This study assumed there were no other differences during those months that could have affected provider prescribing behavior; this may have introduced some bias. Fourth, the sustainability of this intervention's positive impact is unknown. We assessed outcome soon after the intervention, and it is unknown whether continual booster sessions are required to maintain the positive impact on prescribing patterns.
This pilot was a good starting place to show that behavior change can be realized with a well‐conceived and methodically executed intervention, even among the busiest of physicians. Audit and feedback, or practice‐based learning, appears to be a powerful educational intervention among professionals who take great pride in their work.
- ,.Improving antibiotic use in low‐income countries: an overview of evidence on determinants.Soc Sci Med.2003;57:733–744.
- .Mechanisms of antimicrobial resistance in bacteria.Am J Med.2006;119(6A):S3–S10.
- .Antimicrobial resistance in gram‐positive bacteria.Am J Med.2006;119(6A):S11–S19.
- .Resistance in Gram‐negative bacteria: enterobacteriaceae.Am J Med.2006;119(6A):S20–S28.
- .Pharmacodynamics: relation to antimicrobial resistance.Am J Med.2006;119(6A):S37–S44.
- .Managing methicillin‐resistant staphylococci: a paradigm for preventing nosocomial transmission of resistant organisms.Am J Med.2006;119(6A):S45–S52.
- NIH. The Problem of Antibiotic Resistance. Available at: http://www.niaid.nih.gov.
- ,,,.Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) colloquium, 2002.Lancet Infect Dis.2004;4:44–53.
- ,,, et al.The rate and cost of hospital‐acquired infections occurring in patients admitted to selected specialties of a district general hospital in England and the national burden imposed.J Hosp Infect.2001;47:198–209.
- ,.The impact of hospital‐acquired bloodstream infections.Emerg Infect Dis.2001;7(2):174–177.
- .Antimicrobial stewardship.Am J Med.2006;119(6A):S53–S61
- ,,, et al.Changing provider behavior: an overview of systemic reviews of interventions.Med Care.2001;39:II–2‐II‐45.
- .A review of current health education theories.Calif J Health Promot.2004;2:74–87
- The Johns Hopkins Hospital Antibiotic Management Program. 2005 Antibiotic Guidelines: Treatment Recommendations for Adult Inpatients. Johns Hopkins Medicine.
- ,,,.The Sanford Guide to Antimicrobial Therapy 2005.35th ed.Hyde Park, VT:Antimicrobial Therapy, Inc.;2005.
- ,,,.Expanding the roles of hospitalist physicians to include public health.J Hosp Med.2007;2:93–101.
- ,.Principles of Public Health Practice.Albany, NY:Delmar Publishing;1997.
Inappropriate antibiotic use is a major public health concern and demonstrates the need for quality improvement initiatives in the delivery of health care.16 Each year nearly 2 million patients in the United States acquire an infection in the hospital, and about 90,000 of them die from these infections.7 More than 70% of the bacteria that cause hospital‐acquired infections are resistant to at least one commonly used drug.7 Persons infected with drug‐resistant organisms have longer hospital stays and higher mortality rates.7
Inappropriate antibiotic use in the inpatient hospital setting can be classified into 5 categories. First, antibiotics may be given for illnesses for which they are not indicated (eg, viral infections). Second, broad‐spectrum antibiotics (such as piperacillin‐tazobactam and quinolones) may be overused in the empiric treatment of common infections.8 Overuse of broad‐spectrum drugs increases selective pressure for antimicrobial resistance and exposes patients to the side effects of some of these drugs, such as Clostridium difficile colitis.8 Third, clinicians occasionally prescribe intravenous (IV) antibiotics when the efficacy of oral agents would be similar. Inappropriate intravenous therapy increases the cost of care and also exposes the patient to the risk of intravenous catheters.8 Fourth, when the correct antibiotic choice is made, inappropriate antibiotic dosage, schedule, and/or duration of treatment can threaten patient safety.8 Fifth, bug‐drug mismatch occurs when susceptibility studies indicate that the drug being used is ineffective or only marginally effective.8 Beyond antimicrobial resistance and safety, these practices also usually increase costs to both the patient and the hospital.7, 910
Influencing providers' prescribing patterns is difficult.11 In this project we assessed the prescribing patterns of hospitalists in an active inpatient environment and then developed an intervention to improve the providers' use of antibiotics. The intervention utilized public health methodologyprior to implementation, we defined the problem, determined its magnitude, identified a behavior change model, and constructed a conceptual framework that identifyied the key determinants. A pilot academic detailing project addressing many determinants was developed, implemented, and evaluated.
Conceptual Model
To change prescribing behaviors is to change learned behaviors. Changing behavior is a complex process affected by several factors including beliefs, expectations, motivations, and the psychosocial environments of the target groups.12 Each of these factors must be considered when attempting to bring about behavior changes. In doing so, a theory that can be depicted in a model often emerges.13 This approach is widely used in understanding and developing public health interventions.
Formulating the Model
In any public health intervention, recognizing and engaging key stakeholders is a critical step. We identified the following stakeholders: (1) hospitalist practitioners and other prescribing providers including residents and infectious disease specialists; (2) nurses; (3) administrators who are focused on cost effectiveness; (4) patients and their families, who want to get well affordably, without side effects; (5) pharmacists; (6) risk management; and (7) society, which is fearful of the propagation of resistant microbes. In consulting with some of the stakeholders, 4 factors that influence hospitalists' prescribing patterns became apparent. These are practitioner factors, environmental factors, perceived rewards, and perceived threats (Fig. 1).
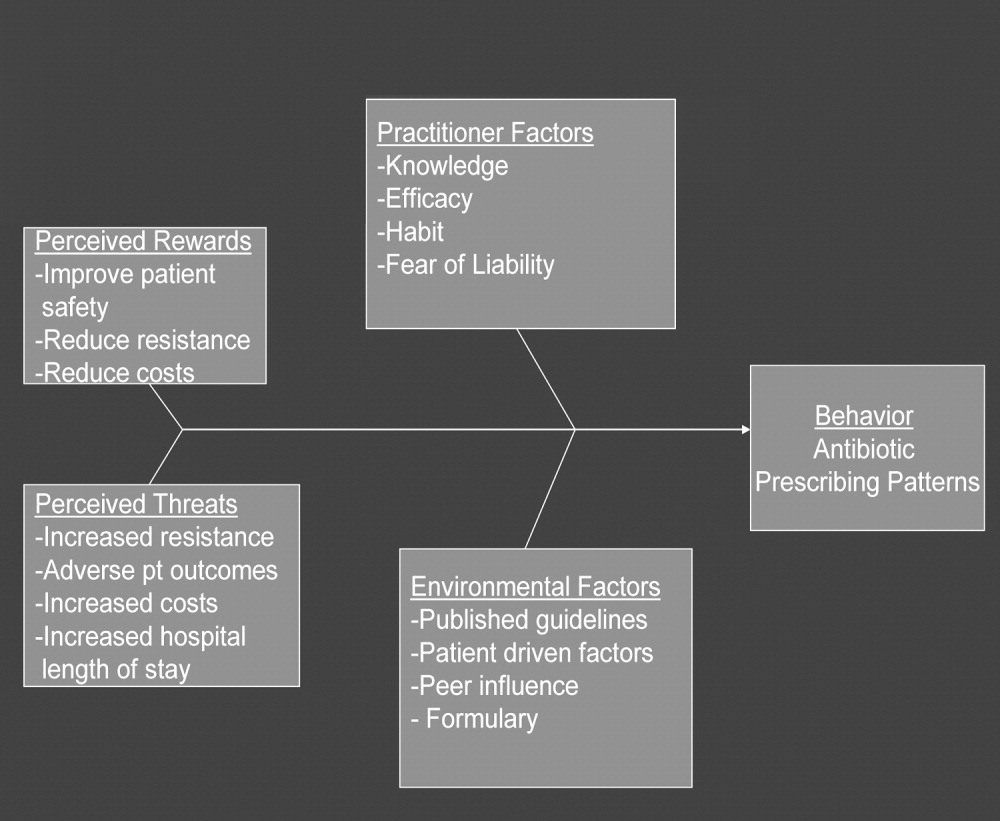
The practitioner factors shaping prescribing are: (1) knowledge of current best care; (2) self‐efficacy, which determines whether a provider is confident in his or her knowledge to adequately treat a specific infection; (3) habit, which causes providers to pick from a narrow repertoire of antibiotics when treating an infection; and (4) fear of liability, which forces some providers to be cautious. Four environmental factors affecting antibiotic prescriptions are: (1) published guidelines regarding organisms' sensitivity to antibiotics; (2) patient‐driven factors such as affordability, compliance with dosing regimens, side effects, and interactions between the antibiotics and other medications; (3) peer influence, in that providers are reluctant to change a prescription started by another provider (eg, emergency room physician); and (4) the formulary of the hospital, as it forces providers to prescribe within specific parameters. The perceived rewards of specific prescribing practices may include improving patient safety and reducing antibiotic resistance and costs, whereas the perceived threats are increasing antimicrobial resistance, having adverse patient outcomes, and increasing costs and hospital length of stay. We selected a high‐yield, low‐effort intervention in order to have an impact on some of the factors underlying hospitalists' prescribing patterns.
METHODS
Participants
The study participants were 17 hospitalist practitioners including physicians, nurse‐practitioners, and physician assistants who make up the Collaborative Inpatient Medical Service (CIMS) at Johns Hopkins Bayview Medical Center (JHBMC; Table 1). All consented to participate. The study was approved by the institutional review board.
| Age in years, mean (SD) | 36 (6) |
| Female, n (%) | 13 (76%) |
| Physician, n (%) | 9 (53%) |
| Nurse‐practitioner, n (%) | 5 (29%) |
| Physician assistant, n (%) | 3 (18%) |
| Years in practice, mean (SD) | 5.1 (2.8) |
| Number of pharmaceutical representatives exposed to in past year, mean | 1 |
| Number of shifts worked per month, mean (SD) | 14 (4) |
| Primarily works days, n (%) | 13 (76%) |
Data Collection
We collected and assessed prescription patterns over 3 periods: preintervention, interim, and postintervention.
Assessing Appropriateness of Antibiotics
For each order that was assessed in the preintervention, interim, and postintervention periods, the following information was collected: (1) drug ordered, (2) clinical diagnosis, (3) microbiology results available at the time of the order (including relevant results from recent cultures), (4) other medical diagnoses (ICD9 codes), (5) allergies, and (6) exposure to health care facilities (within the past 30 days). The computerized medical record allowed access to the discharge summaries of a patient's hospitalization. These records summarized the patient's hospitalization, allowing the investigators to understand the reasons for a provider's choice of antibiotics. If the rationale was not clear about how to categorize a prescription from reading the data, the investigators performed a chart review. From the information culled from these reviews, the primary investigator and an infectious disease specialist classified each prescription order by consensus as appropriate, effective but inappropriate, or inappropriate therapy.
Prescriptions were classified as appropriate when they were indicated and correlated with sensitivities, if available, or were of a narrow‐enough spectrum and recommended as a first‐line treatment for specific illnesses by either the Johns Hopkins Antibiotic Guide14 or the Stanford Guide to Antimicrobial Therapy.15 For example, cephalexin to treat uncomplicated cellulitis was considered appropriate therapy. Effective but inappropriate prescriptions were broad‐spectrum antibiotics used to treat an infection when a narrower‐spectrum antibiotic would have sufficed. For example, piperacillin‐tazobactam would be effective in treating a simple urinary tract infection but inappropriate to use because of its broad spectrum. Other examples of effective but inappropriate prescriptions were giving an IV when an oral alternative would be equally effective and tolerated or prescribing antibiotic treatment whose duration was too long. Finally, inappropriate prescriptions were those written for conditions for which antibiotics are not indicated or for which the prescribed antibiotic was ineffective for the specified infection (bug‐drug mismatch).
Preintervention
In January 2006 the investigators retrospectively reviewed the prescribing patterns of the 17 providers over the previous year. Using the computerized medical record and physician order entry, consecutive prescriptions of each provider were evaluated, beginning December 31, 2005, going back reverse chronologically until 20 prescriptions had been identified. For 12 of the providers, it was actually possible to review 20 prescriptions. For 2 other providers, both new, part‐time additions to the hospitalist group, only 1 and 7 prescriptions were found for the entire year. The prescribing history of the 3 remaining providers who participated in the study, all physician assistants, could not be evaluated (during any period) because all their orders were linked only to physicians, making it impossible to determine their specific prescriptions using the physician order entry system.
Interim
During the interim period between obtaining informed consent and completing the academic detailing (January 3, 2006, to March 23, 2006), provider prescribing patterns were reviewed to determine if the mere knowledge of the project would produce changes in prescribing behavior.
Postintervention
After the academic detailing was completed (March 23, 2006), the prescribing patterns of the hospitalists were followed through April 23, 2006. Each week after the detailing session, the hospitalists received reminders to prescribe appropriately (including pens with the message Reduce the Overuse).
Detailing Procedures
After the review, a profile was assembled for each of the CIMS providers. The study team detailers (a physician and a pharmacist) met with the individual providers for 30 to 45 minutes. Each hospitalist participant completed a short survey that collected demographic information and was asked about the rationale for his or her antibiotic prescribing pattern. Next, the appraisal of the provider's prescribing pattern was reviewed. This review included looking at the costs of the prescribed antibiotics compared with those of the appropriate alternatives and a reexamination of the guidelines for the selected target drugspiperacillin‐tazobactam, vancomycin, and extended‐spectrum quinolones. These 3 antibiotics were picked because our providers had been particularly vulnerable to inappropriately prescribing them. The hospitalists were provided an antibiotic guide developed specifically for this project and based on the Johns Hopkins Antibiotic Guide14 that summarizes the consensus guidelines.
Data Analysis
The primary outcome variable was the aggregate proportion of inappropriate antibiotic prescribed (as defined earlier) before the intervention, during the interim between obtaining informed consent and intervening on all study subjects, and after the intervention. The percentage of appropriate prescriptions versus total not appropriate prescriptions (combining of the effective but inappropriate and inappropriate categories) were compared across the 3 periods. Ninety‐five percent confidence intervals for comparisons of the proportions were determined using Stata 9.0 (College Station, TX). The difference between the proportions of total not appropriate prescriptions before and after academic detailing was computed in Stata using Fisher's exact test to assess significance.
RESULTS
Demographic information and professional characteristics of the 17 providers are shown in Table 1. Their mean age was 36 years, and 76% were female. The top 4 reasons the providers gave for their prescribing practices were: (1) published guidelines, (2) easier dosing schedule for patient when discharged, (3) continuing an antibiotic course initiated in the emergency room, and (4) broad‐spectrum antibiotics cover all possible microbes.
Comparison of Preintervention, Interim, and Postintervention Periods
Table 2 depicts the results of the prescription appraisals from the retrospective reviews. Of the 14 providers who had ordered antibiotics, 8 (57%) had more prescriptions that were total not appropriate than were appropriate in the preintervention period compared with 3 providers (25%) with this prescribing pattern in the postintervention period (P = .13).
| Provider | Preintervention | Postintervention | ||||
|---|---|---|---|---|---|---|
| Prescriptions (n) | Appropriate, n (%) | Total not appropriate, n (%) | Prescriptions (n) | Appropriate, n (%) | Total not appropriate, n (%) | |
| ||||||
| 1 | 20 | 7 (35%) | 13 (65%) | 24 | 17 (70.8%) | 7 (29.2%) |
| 2 | 20 | 10 (50%) | 10 (50%) | 12 | 11 (91.7%) | 1 (8.3%) |
| 3 | 20 | 6 (30%) | 14 (70%) | 8 | 8 (100%) | 0 (0%) |
| 4* | 19 | 10 (52.6%) | 9 (47.4%) | 4 | 3 (75%) | 1 (25%) |
| 5 | 20 | 9 (45%) | 11 (55%) | 10 | 4 (40%) | 6 (60%) |
| 6 | 20 | 5 (25%) | 15 (75%) | 3 | 1 (33.3%) | 2 (66.7%) |
| 7 | 20 | 8 (40%) | 12 (60%) | 8 | 7 (87.5%) | 1 (12.5%) |
| 8* | 1 | 0 (0%) | 1 (100%) | 0 | 0 (0%) | 0 (0%) |
| 9 | 20 | 11 (55%) | 9 (45%) | 5 | 2 (40%) | 3 (60%) |
| 10* | 7 | 3 (42.9%) | 4 (57.1%) | 0 | 0 (0%) | 0 (0%) |
| 11 | 20 | 10 (50%) | 10 (50%) | 17 | 13 (76.5%) | 4 (23.5%) |
| 12 | 20 | 6 (30%) | 14 (70%) | 16 | 14 (87.5%) | 2 (12.5%) |
| 13 | 20 | 12 (60%) | 8 (40%) | 15 | 11 (73.3%) | 4 (26.7%) |
| 14 | 20 | 10 (50%) | 10 (50%) | 7 | 4 (57.1%) | 3 (42.9%) |
| Total | 247 | 107 (43%) | 140 (57%) | 129 | 95 (73.6%) | 34 (26.4%) |
Table 3 shows the proportions of appropriate, effective but inappropriate, and total not appropriate prescriptions in the retrospective, interim, and postintervention periods. Forty‐three percent (95% CI 37%‐49%) of prescriptions were judged to be appropriate, and 57% (95% CI 51%‐63%) to be not appropriate prior to the academic detailing. In the interim period, 59% (95% CI 52%‐65%) of the prescriptions were appropriate, and 41% (95% CI 35%‐48%) were not appropriate; P = .0003. After the intervention, 74% (95% CI 65%‐81%) of the prescriptions were appropriate, and 26% (95% CI 19%‐35%) were not appropriate; P < .0001.
| Period | Appropriate, n (%) | 95% CI | Effective but inappropriate, n (%) | Inappropriate, n (%) | Total not appropriate, n (%) | 95% CI | P value* |
|---|---|---|---|---|---|---|---|
| |||||||
| Retrospective review (pre) | 107 (43%) | 37%‐49% | 75 (30.4%) | 65 (26.6%) | 140 (57%) | 51%‐63% | |
| Interim | 146 (59%) | 52%‐65% | 37 (15%) | 65 (26%) | 102 (41%) | 35%‐48% | .0003 |
| Postintervention | 95 (74%) | 65%‐81% | 8 (6%) | 26 (20%) | 34 (26%) | 19%‐35% | < .0001 |
DISCUSSION
We have demonstrated that academic detailing had a positive impact on the prescribing patterns of hospitalists. The aggregated improvement in antibiotic prescribing patterns can be attributed to improvement in the prescribing patterns of almost every hospitalist practitioner (Table 2). This study focused on aggregate prescriptions as the primary outcome measure because the hospitalists at JHBMC, like at many other institutions, function as a team, with a patient routinely having multiple providers over the course of the hospital stay. The improved prescribing patterns noted during the interim period suggest that the mere knowledge of a project can have an impact on providers. Providers informed the investigators that they were more thoughtful about their choice of antibiotics when they knew that they were being studied. The further statistically significant improvement in prescribing patterns with the intervention shows that the academic detailing itself was successful.
The greatest absolute change in practice was seen in effective but inappropriate prescribing (from 30.4% to 6%), whereas inappropriate prescribing only decreased from 26.6% to 20.6%. Although we aimed to have an impact on all inappropriate antibiotic prescribing patterns, we specifically reviewed the prescribing guidelines for piperacillin‐tazobactam, extended‐spectrum quinolones, and vancomycin. These 3 antibiotics were targeted because our providers had been particularly susceptible to inappropriately prescribing them. The focus on these antibiotics may have resulted in the larger absolute change noted in effective but inappropriate prescribing. We did not collect any data to determine if having an impact on effective but inappropriate prescribing changed the clinical course of the patients, such as shortening their hospital stays. Anecdotal evidence, however, suggests that it does. At our institution it is not uncommon for patients to be kept in the hospital for an extra day to ensure they are stable when transitioned from extended‐spectrum to narrower‐spectrum antibiotics prior to discharge. The effect of reducing effective but inappropriate prescriptions on the clinical course of patients could be an outcome measure assessed by a future, larger study.
Our one‐on‐one appraisal of each provider's prescribing patterns included a review of the cost of the prescribed antibiotics compared with that of the appropriate alternatives. Although decisions on antibiotic choice should be driven by clinical guidelines and appropriateness rather than price, we believed it was relevant to include education about costs and pricing so that providers would be reminded to ascertain whether patients would be able to afford their antibiotics. Antibiotic resistance is influenced by a patient's failure to complete the course of treatment, and noncompliance may be caused by an inability to afford the medication. Often, there are affordable, appropriate alternatives to the newest and most expensive drugs.
A hospitalist‐based academic detailing approach to improving antibiotic prescribing may have far‐reaching benefits and influence. First, it has the potential to affect other practitioners by setting an example and role modeling. In addition to that with their immediate peer group, hospitalists have close and repeated contact with house officers and emergency room physicians and often act as consultants to physicians in other departments such as surgery and psychiatry. Furthermore, some community hospitals have no infectious disease specialists readily available. So this represents an opportunity for hospitalists to promote quality in antibiotic prescribing. Practice‐based learning was very effective because it brought the practitioners face to face with their prescribing patterns. Although intellectually everyone agreed that antibiotics are often misused, this approach forced the providers to stop and reflect on their individual practices. This peer‐delivered intervention allowed for a collaborative approach to solving the problem; the peer (detailer) was approachable, nonjudgmental, and available for further discussion and guidance.
The public health quality improvement approach that we used for our intervention helped us to realize and appreciate the factors underlying prescribing patterns. Only by understanding the motivations for prescribing patterns can we hope to make sustainable changes. This coincides with our previous assertion that hospitalists are engaging in some public health practice.16 In pubic health, the programs, services, and institutions involved emphasize the prevention of disease and the health needs of the population as a whole.17 Hospitalist teams aim to make sure that the high‐quality services needed for protecting the health of their community (hospitalized patients) are available and that this population receives proper consideration in the allocation of resources. Antibiotic optimization is a key role that could fall within the mantra of public health practice for the hospitalist.
Several limitations of this pilot should be considered. First, the intervention is labor intensive. However, it is essential to use the problem‐solving paradigm and incorporate behavior change theories in order to identify interventions that can lead to sustainable change. Second, this was not a randomized controlled trial, and it is possible that there might have been some contamination by external forces. However, in reviewing the educational events at our institution, the press, and articles published during the study period, we could not identify any external factors that would have influenced antibiotic prescribing patterns. It would not have been possible to conduct a randomized trial at our institution because the hospitalists work so closely together that we could not ensure complete separation if the subjects were randomized. There would have been contamination from the intervention group to the control group. A trial with randomization at the institution level is the next step. Third, the number of months retrospectively reviewed in order to identify 20 prescriptions of a provider varied. This study assumed there were no other differences during those months that could have affected provider prescribing behavior; this may have introduced some bias. Fourth, the sustainability of this intervention's positive impact is unknown. We assessed outcome soon after the intervention, and it is unknown whether continual booster sessions are required to maintain the positive impact on prescribing patterns.
This pilot was a good starting place to show that behavior change can be realized with a well‐conceived and methodically executed intervention, even among the busiest of physicians. Audit and feedback, or practice‐based learning, appears to be a powerful educational intervention among professionals who take great pride in their work.
Inappropriate antibiotic use is a major public health concern and demonstrates the need for quality improvement initiatives in the delivery of health care.16 Each year nearly 2 million patients in the United States acquire an infection in the hospital, and about 90,000 of them die from these infections.7 More than 70% of the bacteria that cause hospital‐acquired infections are resistant to at least one commonly used drug.7 Persons infected with drug‐resistant organisms have longer hospital stays and higher mortality rates.7
Inappropriate antibiotic use in the inpatient hospital setting can be classified into 5 categories. First, antibiotics may be given for illnesses for which they are not indicated (eg, viral infections). Second, broad‐spectrum antibiotics (such as piperacillin‐tazobactam and quinolones) may be overused in the empiric treatment of common infections.8 Overuse of broad‐spectrum drugs increases selective pressure for antimicrobial resistance and exposes patients to the side effects of some of these drugs, such as Clostridium difficile colitis.8 Third, clinicians occasionally prescribe intravenous (IV) antibiotics when the efficacy of oral agents would be similar. Inappropriate intravenous therapy increases the cost of care and also exposes the patient to the risk of intravenous catheters.8 Fourth, when the correct antibiotic choice is made, inappropriate antibiotic dosage, schedule, and/or duration of treatment can threaten patient safety.8 Fifth, bug‐drug mismatch occurs when susceptibility studies indicate that the drug being used is ineffective or only marginally effective.8 Beyond antimicrobial resistance and safety, these practices also usually increase costs to both the patient and the hospital.7, 910
Influencing providers' prescribing patterns is difficult.11 In this project we assessed the prescribing patterns of hospitalists in an active inpatient environment and then developed an intervention to improve the providers' use of antibiotics. The intervention utilized public health methodologyprior to implementation, we defined the problem, determined its magnitude, identified a behavior change model, and constructed a conceptual framework that identifyied the key determinants. A pilot academic detailing project addressing many determinants was developed, implemented, and evaluated.
Conceptual Model
To change prescribing behaviors is to change learned behaviors. Changing behavior is a complex process affected by several factors including beliefs, expectations, motivations, and the psychosocial environments of the target groups.12 Each of these factors must be considered when attempting to bring about behavior changes. In doing so, a theory that can be depicted in a model often emerges.13 This approach is widely used in understanding and developing public health interventions.
Formulating the Model
In any public health intervention, recognizing and engaging key stakeholders is a critical step. We identified the following stakeholders: (1) hospitalist practitioners and other prescribing providers including residents and infectious disease specialists; (2) nurses; (3) administrators who are focused on cost effectiveness; (4) patients and their families, who want to get well affordably, without side effects; (5) pharmacists; (6) risk management; and (7) society, which is fearful of the propagation of resistant microbes. In consulting with some of the stakeholders, 4 factors that influence hospitalists' prescribing patterns became apparent. These are practitioner factors, environmental factors, perceived rewards, and perceived threats (Fig. 1).
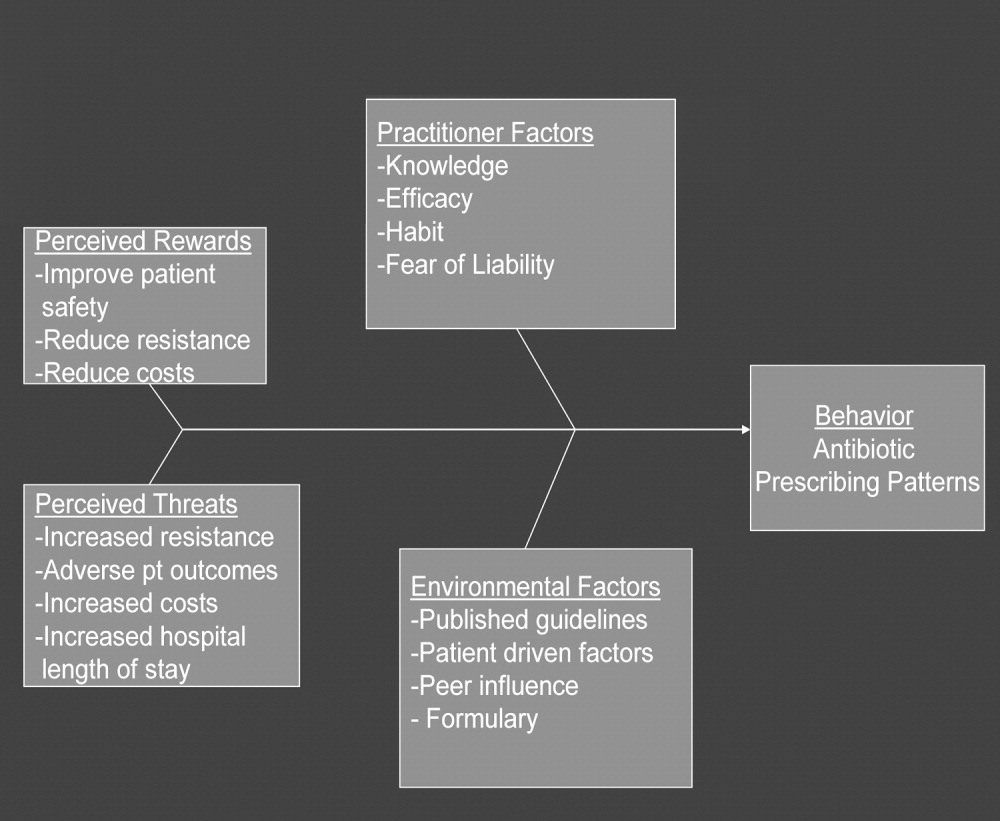
The practitioner factors shaping prescribing are: (1) knowledge of current best care; (2) self‐efficacy, which determines whether a provider is confident in his or her knowledge to adequately treat a specific infection; (3) habit, which causes providers to pick from a narrow repertoire of antibiotics when treating an infection; and (4) fear of liability, which forces some providers to be cautious. Four environmental factors affecting antibiotic prescriptions are: (1) published guidelines regarding organisms' sensitivity to antibiotics; (2) patient‐driven factors such as affordability, compliance with dosing regimens, side effects, and interactions between the antibiotics and other medications; (3) peer influence, in that providers are reluctant to change a prescription started by another provider (eg, emergency room physician); and (4) the formulary of the hospital, as it forces providers to prescribe within specific parameters. The perceived rewards of specific prescribing practices may include improving patient safety and reducing antibiotic resistance and costs, whereas the perceived threats are increasing antimicrobial resistance, having adverse patient outcomes, and increasing costs and hospital length of stay. We selected a high‐yield, low‐effort intervention in order to have an impact on some of the factors underlying hospitalists' prescribing patterns.
METHODS
Participants
The study participants were 17 hospitalist practitioners including physicians, nurse‐practitioners, and physician assistants who make up the Collaborative Inpatient Medical Service (CIMS) at Johns Hopkins Bayview Medical Center (JHBMC; Table 1). All consented to participate. The study was approved by the institutional review board.
| Age in years, mean (SD) | 36 (6) |
| Female, n (%) | 13 (76%) |
| Physician, n (%) | 9 (53%) |
| Nurse‐practitioner, n (%) | 5 (29%) |
| Physician assistant, n (%) | 3 (18%) |
| Years in practice, mean (SD) | 5.1 (2.8) |
| Number of pharmaceutical representatives exposed to in past year, mean | 1 |
| Number of shifts worked per month, mean (SD) | 14 (4) |
| Primarily works days, n (%) | 13 (76%) |
Data Collection
We collected and assessed prescription patterns over 3 periods: preintervention, interim, and postintervention.
Assessing Appropriateness of Antibiotics
For each order that was assessed in the preintervention, interim, and postintervention periods, the following information was collected: (1) drug ordered, (2) clinical diagnosis, (3) microbiology results available at the time of the order (including relevant results from recent cultures), (4) other medical diagnoses (ICD9 codes), (5) allergies, and (6) exposure to health care facilities (within the past 30 days). The computerized medical record allowed access to the discharge summaries of a patient's hospitalization. These records summarized the patient's hospitalization, allowing the investigators to understand the reasons for a provider's choice of antibiotics. If the rationale was not clear about how to categorize a prescription from reading the data, the investigators performed a chart review. From the information culled from these reviews, the primary investigator and an infectious disease specialist classified each prescription order by consensus as appropriate, effective but inappropriate, or inappropriate therapy.
Prescriptions were classified as appropriate when they were indicated and correlated with sensitivities, if available, or were of a narrow‐enough spectrum and recommended as a first‐line treatment for specific illnesses by either the Johns Hopkins Antibiotic Guide14 or the Stanford Guide to Antimicrobial Therapy.15 For example, cephalexin to treat uncomplicated cellulitis was considered appropriate therapy. Effective but inappropriate prescriptions were broad‐spectrum antibiotics used to treat an infection when a narrower‐spectrum antibiotic would have sufficed. For example, piperacillin‐tazobactam would be effective in treating a simple urinary tract infection but inappropriate to use because of its broad spectrum. Other examples of effective but inappropriate prescriptions were giving an IV when an oral alternative would be equally effective and tolerated or prescribing antibiotic treatment whose duration was too long. Finally, inappropriate prescriptions were those written for conditions for which antibiotics are not indicated or for which the prescribed antibiotic was ineffective for the specified infection (bug‐drug mismatch).
Preintervention
In January 2006 the investigators retrospectively reviewed the prescribing patterns of the 17 providers over the previous year. Using the computerized medical record and physician order entry, consecutive prescriptions of each provider were evaluated, beginning December 31, 2005, going back reverse chronologically until 20 prescriptions had been identified. For 12 of the providers, it was actually possible to review 20 prescriptions. For 2 other providers, both new, part‐time additions to the hospitalist group, only 1 and 7 prescriptions were found for the entire year. The prescribing history of the 3 remaining providers who participated in the study, all physician assistants, could not be evaluated (during any period) because all their orders were linked only to physicians, making it impossible to determine their specific prescriptions using the physician order entry system.
Interim
During the interim period between obtaining informed consent and completing the academic detailing (January 3, 2006, to March 23, 2006), provider prescribing patterns were reviewed to determine if the mere knowledge of the project would produce changes in prescribing behavior.
Postintervention
After the academic detailing was completed (March 23, 2006), the prescribing patterns of the hospitalists were followed through April 23, 2006. Each week after the detailing session, the hospitalists received reminders to prescribe appropriately (including pens with the message Reduce the Overuse).
Detailing Procedures
After the review, a profile was assembled for each of the CIMS providers. The study team detailers (a physician and a pharmacist) met with the individual providers for 30 to 45 minutes. Each hospitalist participant completed a short survey that collected demographic information and was asked about the rationale for his or her antibiotic prescribing pattern. Next, the appraisal of the provider's prescribing pattern was reviewed. This review included looking at the costs of the prescribed antibiotics compared with those of the appropriate alternatives and a reexamination of the guidelines for the selected target drugspiperacillin‐tazobactam, vancomycin, and extended‐spectrum quinolones. These 3 antibiotics were picked because our providers had been particularly vulnerable to inappropriately prescribing them. The hospitalists were provided an antibiotic guide developed specifically for this project and based on the Johns Hopkins Antibiotic Guide14 that summarizes the consensus guidelines.
Data Analysis
The primary outcome variable was the aggregate proportion of inappropriate antibiotic prescribed (as defined earlier) before the intervention, during the interim between obtaining informed consent and intervening on all study subjects, and after the intervention. The percentage of appropriate prescriptions versus total not appropriate prescriptions (combining of the effective but inappropriate and inappropriate categories) were compared across the 3 periods. Ninety‐five percent confidence intervals for comparisons of the proportions were determined using Stata 9.0 (College Station, TX). The difference between the proportions of total not appropriate prescriptions before and after academic detailing was computed in Stata using Fisher's exact test to assess significance.
RESULTS
Demographic information and professional characteristics of the 17 providers are shown in Table 1. Their mean age was 36 years, and 76% were female. The top 4 reasons the providers gave for their prescribing practices were: (1) published guidelines, (2) easier dosing schedule for patient when discharged, (3) continuing an antibiotic course initiated in the emergency room, and (4) broad‐spectrum antibiotics cover all possible microbes.
Comparison of Preintervention, Interim, and Postintervention Periods
Table 2 depicts the results of the prescription appraisals from the retrospective reviews. Of the 14 providers who had ordered antibiotics, 8 (57%) had more prescriptions that were total not appropriate than were appropriate in the preintervention period compared with 3 providers (25%) with this prescribing pattern in the postintervention period (P = .13).
| Provider | Preintervention | Postintervention | ||||
|---|---|---|---|---|---|---|
| Prescriptions (n) | Appropriate, n (%) | Total not appropriate, n (%) | Prescriptions (n) | Appropriate, n (%) | Total not appropriate, n (%) | |
| ||||||
| 1 | 20 | 7 (35%) | 13 (65%) | 24 | 17 (70.8%) | 7 (29.2%) |
| 2 | 20 | 10 (50%) | 10 (50%) | 12 | 11 (91.7%) | 1 (8.3%) |
| 3 | 20 | 6 (30%) | 14 (70%) | 8 | 8 (100%) | 0 (0%) |
| 4* | 19 | 10 (52.6%) | 9 (47.4%) | 4 | 3 (75%) | 1 (25%) |
| 5 | 20 | 9 (45%) | 11 (55%) | 10 | 4 (40%) | 6 (60%) |
| 6 | 20 | 5 (25%) | 15 (75%) | 3 | 1 (33.3%) | 2 (66.7%) |
| 7 | 20 | 8 (40%) | 12 (60%) | 8 | 7 (87.5%) | 1 (12.5%) |
| 8* | 1 | 0 (0%) | 1 (100%) | 0 | 0 (0%) | 0 (0%) |
| 9 | 20 | 11 (55%) | 9 (45%) | 5 | 2 (40%) | 3 (60%) |
| 10* | 7 | 3 (42.9%) | 4 (57.1%) | 0 | 0 (0%) | 0 (0%) |
| 11 | 20 | 10 (50%) | 10 (50%) | 17 | 13 (76.5%) | 4 (23.5%) |
| 12 | 20 | 6 (30%) | 14 (70%) | 16 | 14 (87.5%) | 2 (12.5%) |
| 13 | 20 | 12 (60%) | 8 (40%) | 15 | 11 (73.3%) | 4 (26.7%) |
| 14 | 20 | 10 (50%) | 10 (50%) | 7 | 4 (57.1%) | 3 (42.9%) |
| Total | 247 | 107 (43%) | 140 (57%) | 129 | 95 (73.6%) | 34 (26.4%) |
Table 3 shows the proportions of appropriate, effective but inappropriate, and total not appropriate prescriptions in the retrospective, interim, and postintervention periods. Forty‐three percent (95% CI 37%‐49%) of prescriptions were judged to be appropriate, and 57% (95% CI 51%‐63%) to be not appropriate prior to the academic detailing. In the interim period, 59% (95% CI 52%‐65%) of the prescriptions were appropriate, and 41% (95% CI 35%‐48%) were not appropriate; P = .0003. After the intervention, 74% (95% CI 65%‐81%) of the prescriptions were appropriate, and 26% (95% CI 19%‐35%) were not appropriate; P < .0001.
| Period | Appropriate, n (%) | 95% CI | Effective but inappropriate, n (%) | Inappropriate, n (%) | Total not appropriate, n (%) | 95% CI | P value* |
|---|---|---|---|---|---|---|---|
| |||||||
| Retrospective review (pre) | 107 (43%) | 37%‐49% | 75 (30.4%) | 65 (26.6%) | 140 (57%) | 51%‐63% | |
| Interim | 146 (59%) | 52%‐65% | 37 (15%) | 65 (26%) | 102 (41%) | 35%‐48% | .0003 |
| Postintervention | 95 (74%) | 65%‐81% | 8 (6%) | 26 (20%) | 34 (26%) | 19%‐35% | < .0001 |
DISCUSSION
We have demonstrated that academic detailing had a positive impact on the prescribing patterns of hospitalists. The aggregated improvement in antibiotic prescribing patterns can be attributed to improvement in the prescribing patterns of almost every hospitalist practitioner (Table 2). This study focused on aggregate prescriptions as the primary outcome measure because the hospitalists at JHBMC, like at many other institutions, function as a team, with a patient routinely having multiple providers over the course of the hospital stay. The improved prescribing patterns noted during the interim period suggest that the mere knowledge of a project can have an impact on providers. Providers informed the investigators that they were more thoughtful about their choice of antibiotics when they knew that they were being studied. The further statistically significant improvement in prescribing patterns with the intervention shows that the academic detailing itself was successful.
The greatest absolute change in practice was seen in effective but inappropriate prescribing (from 30.4% to 6%), whereas inappropriate prescribing only decreased from 26.6% to 20.6%. Although we aimed to have an impact on all inappropriate antibiotic prescribing patterns, we specifically reviewed the prescribing guidelines for piperacillin‐tazobactam, extended‐spectrum quinolones, and vancomycin. These 3 antibiotics were targeted because our providers had been particularly susceptible to inappropriately prescribing them. The focus on these antibiotics may have resulted in the larger absolute change noted in effective but inappropriate prescribing. We did not collect any data to determine if having an impact on effective but inappropriate prescribing changed the clinical course of the patients, such as shortening their hospital stays. Anecdotal evidence, however, suggests that it does. At our institution it is not uncommon for patients to be kept in the hospital for an extra day to ensure they are stable when transitioned from extended‐spectrum to narrower‐spectrum antibiotics prior to discharge. The effect of reducing effective but inappropriate prescriptions on the clinical course of patients could be an outcome measure assessed by a future, larger study.
Our one‐on‐one appraisal of each provider's prescribing patterns included a review of the cost of the prescribed antibiotics compared with that of the appropriate alternatives. Although decisions on antibiotic choice should be driven by clinical guidelines and appropriateness rather than price, we believed it was relevant to include education about costs and pricing so that providers would be reminded to ascertain whether patients would be able to afford their antibiotics. Antibiotic resistance is influenced by a patient's failure to complete the course of treatment, and noncompliance may be caused by an inability to afford the medication. Often, there are affordable, appropriate alternatives to the newest and most expensive drugs.
A hospitalist‐based academic detailing approach to improving antibiotic prescribing may have far‐reaching benefits and influence. First, it has the potential to affect other practitioners by setting an example and role modeling. In addition to that with their immediate peer group, hospitalists have close and repeated contact with house officers and emergency room physicians and often act as consultants to physicians in other departments such as surgery and psychiatry. Furthermore, some community hospitals have no infectious disease specialists readily available. So this represents an opportunity for hospitalists to promote quality in antibiotic prescribing. Practice‐based learning was very effective because it brought the practitioners face to face with their prescribing patterns. Although intellectually everyone agreed that antibiotics are often misused, this approach forced the providers to stop and reflect on their individual practices. This peer‐delivered intervention allowed for a collaborative approach to solving the problem; the peer (detailer) was approachable, nonjudgmental, and available for further discussion and guidance.
The public health quality improvement approach that we used for our intervention helped us to realize and appreciate the factors underlying prescribing patterns. Only by understanding the motivations for prescribing patterns can we hope to make sustainable changes. This coincides with our previous assertion that hospitalists are engaging in some public health practice.16 In pubic health, the programs, services, and institutions involved emphasize the prevention of disease and the health needs of the population as a whole.17 Hospitalist teams aim to make sure that the high‐quality services needed for protecting the health of their community (hospitalized patients) are available and that this population receives proper consideration in the allocation of resources. Antibiotic optimization is a key role that could fall within the mantra of public health practice for the hospitalist.
Several limitations of this pilot should be considered. First, the intervention is labor intensive. However, it is essential to use the problem‐solving paradigm and incorporate behavior change theories in order to identify interventions that can lead to sustainable change. Second, this was not a randomized controlled trial, and it is possible that there might have been some contamination by external forces. However, in reviewing the educational events at our institution, the press, and articles published during the study period, we could not identify any external factors that would have influenced antibiotic prescribing patterns. It would not have been possible to conduct a randomized trial at our institution because the hospitalists work so closely together that we could not ensure complete separation if the subjects were randomized. There would have been contamination from the intervention group to the control group. A trial with randomization at the institution level is the next step. Third, the number of months retrospectively reviewed in order to identify 20 prescriptions of a provider varied. This study assumed there were no other differences during those months that could have affected provider prescribing behavior; this may have introduced some bias. Fourth, the sustainability of this intervention's positive impact is unknown. We assessed outcome soon after the intervention, and it is unknown whether continual booster sessions are required to maintain the positive impact on prescribing patterns.
This pilot was a good starting place to show that behavior change can be realized with a well‐conceived and methodically executed intervention, even among the busiest of physicians. Audit and feedback, or practice‐based learning, appears to be a powerful educational intervention among professionals who take great pride in their work.
- ,.Improving antibiotic use in low‐income countries: an overview of evidence on determinants.Soc Sci Med.2003;57:733–744.
- .Mechanisms of antimicrobial resistance in bacteria.Am J Med.2006;119(6A):S3–S10.
- .Antimicrobial resistance in gram‐positive bacteria.Am J Med.2006;119(6A):S11–S19.
- .Resistance in Gram‐negative bacteria: enterobacteriaceae.Am J Med.2006;119(6A):S20–S28.
- .Pharmacodynamics: relation to antimicrobial resistance.Am J Med.2006;119(6A):S37–S44.
- .Managing methicillin‐resistant staphylococci: a paradigm for preventing nosocomial transmission of resistant organisms.Am J Med.2006;119(6A):S45–S52.
- NIH. The Problem of Antibiotic Resistance. Available at: http://www.niaid.nih.gov.
- ,,,.Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) colloquium, 2002.Lancet Infect Dis.2004;4:44–53.
- ,,, et al.The rate and cost of hospital‐acquired infections occurring in patients admitted to selected specialties of a district general hospital in England and the national burden imposed.J Hosp Infect.2001;47:198–209.
- ,.The impact of hospital‐acquired bloodstream infections.Emerg Infect Dis.2001;7(2):174–177.
- .Antimicrobial stewardship.Am J Med.2006;119(6A):S53–S61
- ,,, et al.Changing provider behavior: an overview of systemic reviews of interventions.Med Care.2001;39:II–2‐II‐45.
- .A review of current health education theories.Calif J Health Promot.2004;2:74–87
- The Johns Hopkins Hospital Antibiotic Management Program. 2005 Antibiotic Guidelines: Treatment Recommendations for Adult Inpatients. Johns Hopkins Medicine.
- ,,,.The Sanford Guide to Antimicrobial Therapy 2005.35th ed.Hyde Park, VT:Antimicrobial Therapy, Inc.;2005.
- ,,,.Expanding the roles of hospitalist physicians to include public health.J Hosp Med.2007;2:93–101.
- ,.Principles of Public Health Practice.Albany, NY:Delmar Publishing;1997.
- ,.Improving antibiotic use in low‐income countries: an overview of evidence on determinants.Soc Sci Med.2003;57:733–744.
- .Mechanisms of antimicrobial resistance in bacteria.Am J Med.2006;119(6A):S3–S10.
- .Antimicrobial resistance in gram‐positive bacteria.Am J Med.2006;119(6A):S11–S19.
- .Resistance in Gram‐negative bacteria: enterobacteriaceae.Am J Med.2006;119(6A):S20–S28.
- .Pharmacodynamics: relation to antimicrobial resistance.Am J Med.2006;119(6A):S37–S44.
- .Managing methicillin‐resistant staphylococci: a paradigm for preventing nosocomial transmission of resistant organisms.Am J Med.2006;119(6A):S45–S52.
- NIH. The Problem of Antibiotic Resistance. Available at: http://www.niaid.nih.gov.
- ,,,.Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) colloquium, 2002.Lancet Infect Dis.2004;4:44–53.
- ,,, et al.The rate and cost of hospital‐acquired infections occurring in patients admitted to selected specialties of a district general hospital in England and the national burden imposed.J Hosp Infect.2001;47:198–209.
- ,.The impact of hospital‐acquired bloodstream infections.Emerg Infect Dis.2001;7(2):174–177.
- .Antimicrobial stewardship.Am J Med.2006;119(6A):S53–S61
- ,,, et al.Changing provider behavior: an overview of systemic reviews of interventions.Med Care.2001;39:II–2‐II‐45.
- .A review of current health education theories.Calif J Health Promot.2004;2:74–87
- The Johns Hopkins Hospital Antibiotic Management Program. 2005 Antibiotic Guidelines: Treatment Recommendations for Adult Inpatients. Johns Hopkins Medicine.
- ,,,.The Sanford Guide to Antimicrobial Therapy 2005.35th ed.Hyde Park, VT:Antimicrobial Therapy, Inc.;2005.
- ,,,.Expanding the roles of hospitalist physicians to include public health.J Hosp Med.2007;2:93–101.
- ,.Principles of Public Health Practice.Albany, NY:Delmar Publishing;1997.
Copyright © 2008 Society of Hospital Medicine
Expanding Hospitalist Roles to Public Health
The field of hospital medicine came into being in response to numerous factors involving physicians, patients, and hospitals themselves1 Now, years later, hospital medicine is a specialty that is growing, both in size and sophistication such that the role of the hospitalist is constantly evolving.2 A compelling function that has not yet been clearly articulated is the opportunity for hospitalists to serve as public health practitioners in their unique clinical environment. There is precedence for the power of collaboration between medicine and public health as has been seen with emergency medicine's willingness to embrace opportunities to advance public health.35
In public health, the programs, services, and institutions involved emphasize the prevention of disease and the health needs of the population as a whole. Public health activities vary with changing technology and social values, but the goals remain the same: to reduce the amount of disease, premature death, and disease‐associated discomfort and disability in the population.6 The authors of a leading textbook of public health, Scutchfield and Keck, contend that the most important skill for public health practice is the capacity to visualize the potential for health that exists in a community.6
Hospitalists care for a distinct subset of the general populationinpatients, only a small percentage of society in a given year. Yet over time hospitalists affect a substantial subset of the larger population that uses considerable health care resources.79 Furthermore, hospitalization can be a sentinel event with public health implications (eg, newly diagnosed HIV infection or acute myocardial infarction in a patient with an extended family of cigarette smokers). This presents an opportunity to educate and counsel both the patient and the patient's social network. One model of public health practice by hospitalists is to influence the patient, his or her family, and the community by touching and inspiring the hospitalized patient.
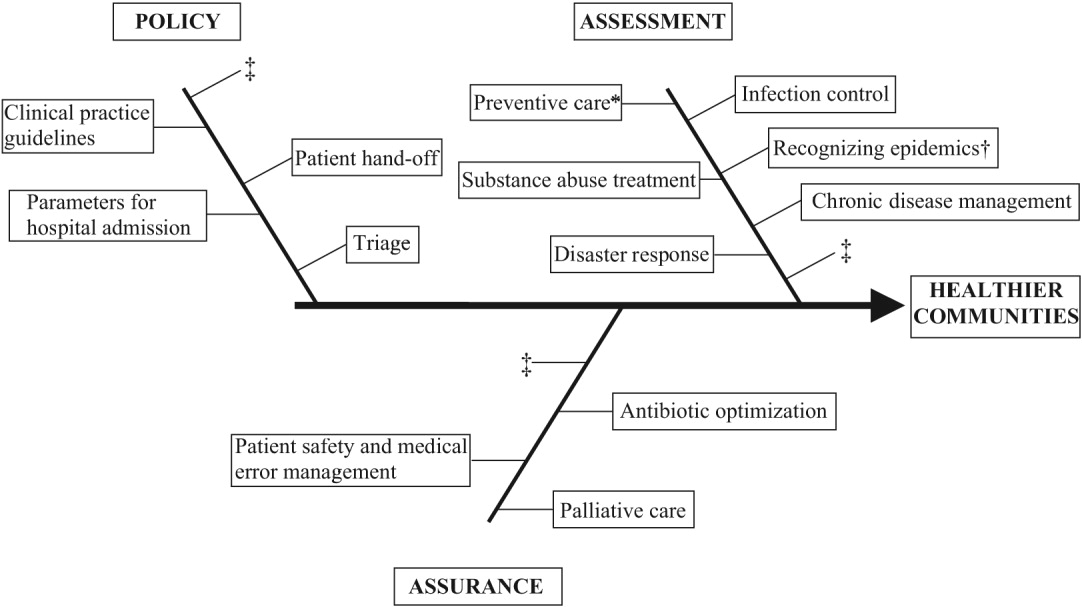
Hospitalists are already involved in many of the core functions of public health (assessment, assurance, and policy development; Fig. 1).10 Achieving ongoing success in this arena means developing hospitalists who are consciously in tune with their roles as public health practitioners.
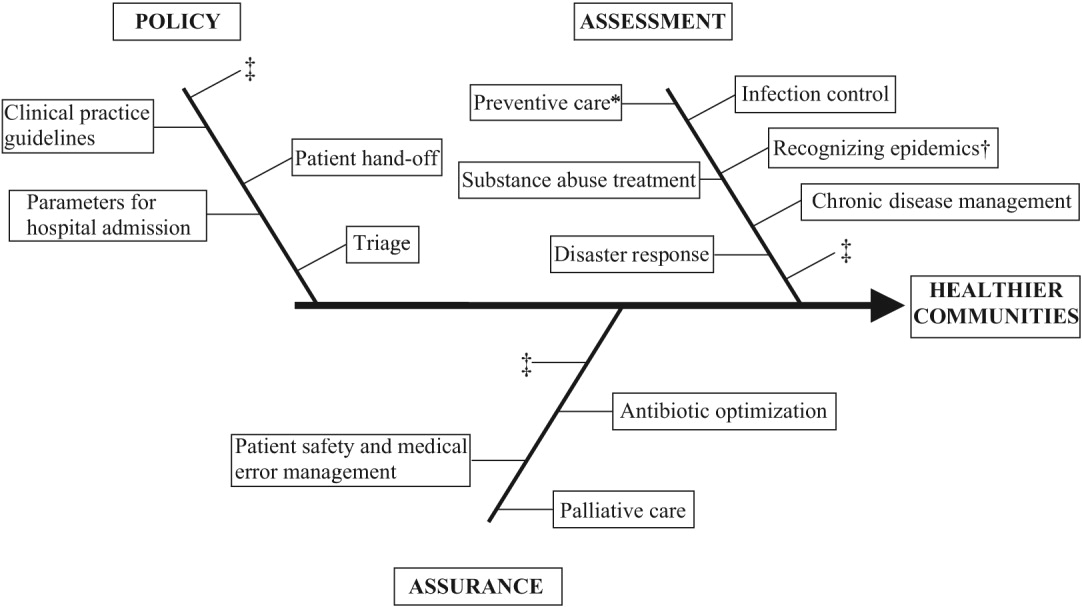
In this article we define the specific public health contributions that hospitalists have made and describe the possibilities for further innovative advances. To this end, we outline specific public health roles under the broad categories of assessment, assurance, and policy. We point to advances in public health accomplished by hospitalists as well as those being performed by nonhospitalists in the hospital setting. We conclude by describing some of the barriers to and implications of hospitalists taking on public health roles.
ASSESSMENT
Assessment is the systematic collection, analysis, and dissemination of health status information.10 These activities include disease surveillance and investigation of acute outbreaks or changes in the epidemiology of chronic diseases. Assessment also involves understanding the health of a population and the key determinants of a population's health from a variety of perspectives: physical, biological, behavioral, social, cultural, and spiritual.6 Human health has been defined as a state characterized by anatomic integrity; ability to perform personally valued family work and community roles; ability to deal with physical, biologic, and social stress; a feeling of well‐being; and freedom from the risk of disease and untimely death.6 Hospitalists interact with individuals at times of stress and acute illness and thus have a unique opportunity to assess the strength, viability, and resources available to individuals. Key roles that may fall within the auspices of assessment in hospital medicine are infection control, epidemic recognition, disaster response, preventive care, substance abuse treatment, and chronic disease management.
Infection Control
Physicians caring for inpatients have a crucial stake in controlling hospital infection as exemplified by the work of Flanders et al. on preventing nosocomial infections, especially nosocomial pneumonia.11 They describe specific strategies to prevent iatrogenic spread such as washing hands before and after patient contact, establishing guidelines against the use of artificial fingernails, using indwelling devices such as catheters only when absolutely necessary, and using sterile barriers.11 Hospitalists such as Sanjay Saint have led the way in studying methods to reduce bladder catheterization, which has been associated with urinary tract infections12; others have collaborated on work to prevent infections in nursing homes.13 Given the importance of this field, there is room for further hospitalist involvement. Novel methods for infection control in hospitals have been studied by nonhospitalists such as Wisnivesky, who prospectively validated a clinical decision rule to predict the need for respiratory isolation of inpatients with suspected tuberculosis (TB). This prediction rule, which is based on clinical and chest radiographic findings, was able to accurately identify patients at low risk for TB from among inpatients with suspected active pulmonary TB isolated on admission to the hospital.14 Retrospective application of the prediction rule showed respiratory precautions were inappropriately implemented for a third of patients.14 These studies are examples of empiric public health research performed in the inpatient setting. In the infection control domain, candidate issues for further study could include interventions aimed at reducing rates of Clostridium difficile, developing programs for standardized surveillance of hospital infection, validating electronic markers for nosocomial infection, and taking innovative approaches to improving hand‐washing practices in the hospital.15, 16
Recognizing Epidemics
An excellent example of the importance of hospitalists embracing public health and remembering their patients are part of a community was the severe acute respiratory syndrome (SARS) outbreak in Toronto, Ontario, Canada. The outbreak is thought to have begun with a single traveler. With the transfer of patients and the movement of visitors and health care workers among facilities, SARS quickly spread through Toronto, making it the largest SARS‐affected area outside Asia.17 Approximately a month after the outbreak was recognized in Toronto, it was thought to be over, and the World Health Organization (WHO) removed Toronto from its SARS‐affected list.17 Unfortunately, patients with unrecognized SARS remained in health care institutions, including a patient transferred to a rehabilitation center. Infection quickly spread again, resulting in a second phase of the outbreak.17
The SARS outbreak served as a reminder that a global public health system is essential and taught many lessons17 germane to pandemics that recur annually (eg, influenza viruses) as well those that episodically threaten the health of the population (eg, avian flu). Proposed actions to prevent a repeat of the scenario that occurred with SARS in Toronto include assessing the current facilities (eg, isolation rooms and respiratory masks) at each institution, identifying health care workers willing to serve as an outbreak team, and the hiring staff to train hospital personnel in personal protective equipment (PPE) and infection control policies.18 The Centers for Disease Control and Prevention (CDC) contends that planning for the possibility of a virulent pandemic at the local, national, and global levels is critical to limiting the mortality and morbidity should such occur.19, 20 In a previous article, Pile and Gordon declared hospitalists are key players in institutional efforts to prepare for a viral pandemic such as influenza and should be aware of lessons that may be applied from responses to pandemics such as SARS.19 Well placed to recognize clinical trends that may herald epidemics, hospitalists can fulfill some of the necessary public health responsibilities delineated above.
Disaster Response
Natural disasters and terrorism are in the forefront of the popular press and are also high priorities in health care and public health.21 Terrorism and natural disasters cause significant injury, illness, and death.22 Hospital‐based health care providers fulfill a variety of roles when terrorist acts and disasters occur, including reporting, diagnosing, and managing illness, providing preventive measures (eg, vaccines and preparedness kits), preventing the secondary spread of disease, assisting in the investigation of the causes of disease outbreaks, participating in preparedness planning, and evaluating preparedness policies and programs.22 The experience gained in the aftermaths of Hurricanes Katrina and Rita with their unprecedented death, injury, destruction, and displacement should help to guide future response and recovery activities.23 Hospitalists were at the forefront of delivering care, living in their hospitals for days after Hurricane Katrina. Without question, hospitalists will be called on again to serve those affected by disasters.
Preventive Care
For many patients admitted to the hospital, meeting a hospitalist is their first encounter with a physician in years.24, 25 In these instances, hospitalists must ensure that patients' immunizations are up‐to‐date and arrange appropriate follow‐up care with primary care providers. Greenwald described an important role that hospitalists could play in HIV prevention by promoting HIV testing in the hospital.26 The CDC recently confirmed the wisdom of this approach and estimates that the 250,000 to 1.2 million people in the United States with HIV infection who do not know their serostatus play a significant role in HIV transmission.26, 27 In an effort to promote testing, the CDC has initiated a program aimed at incorporating HIV testing into routine medical care, as recommended by others.28 More than a quarter of patients with HIV in the United States are diagnosed in the hospital, and for many other patients, hospitalization is their only real opportunity to be tested.26, 29 Similarly, when hospitalists find elevated cholesterol or triglycerides in routine evaluations of patients who present with chest pain, they have to decide whether to initiate lipid‐lowering medications.30 The hospitalist is sometimes the only physician that patients repeatedly admitted, may see over prolonged periods. It follows that if hospitalists are remiss in delivering preventive care to such patients, they lose the opportunity to positively affect their long‐term health. In practice, hospitalists perform myriad preventive‐care functions, although there is scant literature supporting this role. Hospitalists have an opportunity to collaborate in research projects of hospital‐initiated preventive care that measure outcomes at the community level.
Substance Abuse
In the Unites States, 25%‐40% of hospital admissions are related to substance abuse and its sequelae.31 These patients frequently are admitted to general medicine services for detoxification or treatment of substance‐abuse‐related morbidity, although some American hospitals have specialized treatment and detoxification centers. There is a pressing need for more models of comprehensive care that address the complex issues of addiction, including the biological, social, cultural, spiritual, and developmental needs of patients.32
Hospitalists routinely counsel their patients with substance abuse problems and often consult a chemical dependency counselor, who provides patients with additional information about outpatient or inpatient facilities that may help them after their hospitalization. Unfortunately, because of the natural history of substance abuse, many of these patients are rehospitalized with the same problems even after going through rehabilitation. The adoption of a public health philosophy and approach by hospitalists may assist patients who have addictions through innovative multidisciplinary interventions while these patient are being detoxified. Traditionally, these responsibilities have fallen to primary care providers and psychologists in substance abuse medicine; but, as mentioned previously, many such patients are rehospitalized before they make it to their follow‐up appointments.
In a study examining smoking cessation practices among Norwegian hospital physicians, 98% of the doctors stated they ask their patients about their smoking habits, but fewer than 7% of these physicians regularly offer smoking‐cessation counseling, hand out materials, or give patients other advice about smoking cessation.33 That study illustrates that hospital doctors often ask about problems but can certainly improve in terms of intervention and follow‐up. Other works by nonhospitalist physicians have examined the real potential of inpatient interventions for smoking cessation. Most of this work involves a multidisciplinary approach that relies heavily on nurses. For example, Davies et al. evaluated the effectiveness of a hospital‐based intervention for smoking cessation among low‐income smokers using public health methodologies. The intervention was effective and promising as a way to affect smokers in underserved communities.34
Chronic Disease Management
Public health roles involving chronic disease management include surveillance, intervention design, and implementation of control programs.6 Given their access to data on hospitalized patients, hospitalists can carry out surveillance and empirical population‐based research about hospitalized patients with chronic illnesses. Thoughtfully designed protocols can measure the success of interventions initiated in patients while hospitalized, with further data collection and follow‐up after patients have returned to the community.35 Such endeavors can improve the likelihood that patients with chronic conditions are effectively referred to programs that will maintain their health and functional status.36 If hospitalists consider themselves public health providers, encounters with these hospitalized patients will go beyond noting that their chronic conditions are stable and instead will lay the groundwork to prospectively control these conditions. This approach would have the potential to reduce the number of future hospitalizations and lead to healthier communities.37 To truly carry this out effectively, coordinated collaboration between primary care providers and hospitalists will be necessary.
ASSURANCE
Assurance is the provision of access to necessary health services. It entails efforts to solve problems that threaten the health of populations and empowers individuals to maintain their own health. This is accomplished by either encouraging action, delegating to other entities (private or public sector), mandating specific requirements through regulation, or providing services directly.10 Hospitalist teams aim to ensure that the high‐quality services needed to protect the health of their community (hospitalized patients) are available and that this population receives proper consideration in the allocation of resources. The few studies to date that have directly examined the quality of care that hospitalists provide38 have done so using evidence‐based measures believed to correlate with improved health care outcomes.38 The ambiguities in assessing quality may in part limit such studies.39 Specific hospitalist roles that fall under the assurance umbrella include antibiotic optimization, palliative care, patient safety, and medical error management.
Antibiotic Optimization
Inappropriate use of antimicrobial treatment for infectious diseases has cost and public health implications.40 These inappropriate uses include giving antibiotics when not indicated, overusing broad‐spectrum antibiotics, making mismatches between microbes and medicines when cultures and information on test sensitivity are available, and using intravenous formulations when oral therapy would suffice.41 The public health impact goes way beyond increasing selective pressure for antimicrobial resistance to include safety, adverse events, and increased costs to both patient and hospitals.40 At our institution, the hospital medicine service and infectious disease division have jointly developed and implemented an intervention to reduce inappropriate antibiotic use. At other institutions, hospitalist teams have developed protocols for treating infectious diseases commonly encountered in the hospitalized patient.42 The recommendations of both Amin and Reddy for management of community‐ and hospital‐acquired pneumonia acknowledged that through establishment of clinical care pathways, variation in prescribing patterns among hospitalists can be decreased while optimizing outcomes.42 The work of Williams and colleagues is another example of advances by hospitalists. They reviewed the literature to determine that the use of combination antibiotics as empiric therapy for community‐acquired pneumonia is superior to the use of a single effective antibiotic in treating bacteremic patients with pneumococcal community‐acquired pneumonia.43
Palliative Care
Mortality is a vital outcome measure of public health research and interventions. Not surprisingly, many people are hospitalized in the final months of their life and often die in a hospital. Pantilat showed that hospitalists can respond to these circumstances and have the opportunity to improve care of the dying.4446 Muir et al. evaluated the convergence of the fields of palliative care medicine and hospital medicine and reviewed the opportunities for mutual education and improved patient care.47 They described how the confluence of the changing nature and site of death in the United States coupled with the reorganization of hospital care provides a strategic opportunity to improve end‐of‐life care.47 Hospitalists can ensure that care of the dying is delivered with skill, compassion, and expertise. And so it is imperative they be trained to accomplish this objective.47, 49
Fortunately, hospitalists already appear to enhance patientphysician communication. Auerbach looked at communication, care patterns, and outcomes of dying patients, comparing patients being cared for by hospitalists with those being care for by community‐based physicians. Hospitalists had discussions with patients or their families about care more often than did nonhospitalist physicians (91% versus 73%, respectively, P = .006).49 Because the delivery of high‐quality palliative care is time consuming and complex, alternative models for billing or the use of physician extenders or consultants may be necessary at some institutions.
Patient Safety and Medical Error Management
Hospitalists have been in the forefront of promoting a culture of patient safety.50 Their continuous presence in the hospital and their interactions with members of health care teams from multiple disciplines who share this goal make them important facilitators. Hospitalists have increasing involvement in systems‐based efforts aimed at reducing medical errors.50 Hospitalists are being asked to lead committees that adopt multidisciplinary approaches to reduce adverse events, morbidity, and mortality.50 These committees often have representation from pharmacy, nursing, and other key hospital stakeholders including from the administration.51 Quality assurance activities assess locally collected data and compare results with local and national benchmarks. There are several published examples of hospitalists engaged in patient safety and medical error management. For example, Shojania et al compiled evidence based safety practices in an effort to promote patient safety.52, 53 Schnipper studied the role of pharmacist counseling in preventing adverse drug events (ADEs) after hospitalization and found that pharmacist medication review, patient counseling, and telephone follow‐up were associated with a lower rate of preventable ADEs 30 days after hospital discharge.54 Moreover, Syed paired hospitalists and pharmacists to collaboratively prescribe medications appropriately. In one study there were fewer medication errors and adverse drug reactions in patients treated by a team led by hospitalists than in those treated by the control group, made up of nonhospitalist attendings.55
POLICY
Policy development defines health control goals and objectives and develops implementation plans for those goals.10 By necessity, it operates at the intersection of legislative, political, and regulatory processes.10 At many institutions, hospitalists have been involved in the development of policies ensuring that the core functions of assessment and assurance are addressed and maintained. In fact, hospitalists report that development of quality assurance and practice guidelines accounts for most of their nonclinical time.56 This role of hospitalists is supported by anecdotal reports rather than published empiric evidence.57 For example, at Johns Hopkins Bayview Medical Center, hospitalist‐led teams have developed triage and patient handoff policies designed to improve patient safety. Parameters for admission to the general medicine ward have been elaborated and are periodically refined by the hospitalist team.
Another area that falls within the genre of policy is development of clinical practice guidelines. Guidelines for the treatment of pneumonia, congestive heart failure, deep‐vein thrombosis prophylaxis, alcohol and drug withdrawal, pain management, delirium, and chronic obstructive pulmonary disease have been developed by nonhospitalists.58, 59 These areas are considered core competencies in hospital medicine, and as such, hospitalists have an obligation to review and refine these guidelines to ensure the best provision of care to our patients.59
Hospitalists have been engaged in upholding guidelines that affect community practice. For example, in a study comparing treatment of patients admitted with congestive heart failure by hospitalists compared with that by nonhospitalists, hospitalists were found to be more likely to document left ventricular function, a core measure of quality as defined by JCAHO.39, 60 Knowledge about cardiac function can direct future care for patients when they return to the community and into the care of their primary care providers. In another example, Rifkin found that patients with community‐acquired pneumonia treated by hospitalists were more rapidly converted to oral antibiotics from intravenous antibiotics, facilitating a shorter length of stay,61 which reduced the opportunity for nosocomial infections to propagate. Because hospitalists are skilled at following guidelines,59 it follows that they should seize the opportunity to develop more of them.
As the hospitalist movement continues to grow, hospitalists will likely be engaged in implementing citywide, statewide, and even national policies that ensure optimal care of the hospitalized patient.
BARRIERS TO HOSPITALISTS FOCUSING ON PUBLIC HEALTH
Hospitalists are involved in public health activities even though they may not recognize the extent of this involvement. However, there may be some drawbacks to hospitalists viewing each patient encounter as an opportunity for a public health intervention. First, in viewing a patient as part of a cohort, the individual needs of the patient may be overlooked. There is inherent tension between population‐based and individual‐based care, which is a challenge. Second, hospitalists are busy clinicians who may be most highly valued because of their focus on efficiency and cost savings in the acute care setting. This factor alone may prevent substantive involvement by hospitalists in public health practice. Moving beyond the management of an acute illness may interfere with this efficiency and cost effectiveness from the hospital's perspective. However, interventions that promote health and prevent or reduce rehospitalizations may be cost effective to society in the long run. Third, current billing systems do not adequately reward or reimburse providers for the extra time that may be necessary to engage in public health practice. Fourth, hospitalists may not have the awareness, interest, training, or commitment to engage in public health practice. Finally, there may not be effective collaboration and communication systems between primary care providers and hospitalists. This barrier limits or hinders many possibilities for the effective execution of several public health initiatives.
CONCLUSIONS AND IMPLICATIONS
Hospitalists and the specialty of hospital medicine materialized because of myriad economic forces and the need to provide safe, high‐quality care to hospitalized patients. In this article we have described the ways in which hospitalists can be explicitly involved in public health practice. Traditionally, physicians caring for hospitalized patients have collected information through histories and physical examinations, interpreted laboratory data and tests, and formulated assessments and plans of care. To become public health practitioners, hospitalists have to go beyond these tasks and consider public health thought processes, such as problem‐solving paradigms and theories of behavior change. In adopting this public health perspective, hospitalists may begin to think of a patient in the context of the larger community in order to define the problems facing the community, not just the patient, determine the magnitude of such problems, identify key stakeholders, create intervention/prevention strategies, set priorities and recommend interventions, and implement and evaluate those interventions. This approach forces providers to move beyond the physicianpatient model and draw on public health models to invoke change. Hopefully, future research will further convince hospitalists of the benefits of this approach. Although it may be easier to defer care and management decisions to an outpatient physician, data suggest that intervening when patients are in the hospital may be most effective.62, 63 For example, is it possible that patients are more likely to quit smoking when they are sick in the hospital than when they are in their usual state of health on a routine visit at their primary care provider's office?64 Further, although deferring care to a primary care provider (PCP) may be easier, it is not always possible given these barriers: (1) some patients are routinely rehospitalized, precluding primary care visits, (2) some recommendations may not be received by PCPs, and (3) PCPpatient encounters are brief and the agendas full, and there are limited resources to address recommendations from the hospital.
As hospitalists become more involved in public health practice, their collaboration with physicians and researchers in other fields, nurses, policymakers, and administrators will expand. Succeeding in this arena requires integrity, motivation, capacity, understanding, knowledge, and experience.65 It is hoped that hospitalists will embrace the opportunity and master the requisite skill set necessary to practice in and advance this field. As hospitalist fellowship programs are developed, public health practice skills could be incorporated into the curriculum. Currently 6 of 16 fellowship programs offer either a master of public health degree or public health courses.66 Public health skills can also be taught at Society of Hospital Medicine meetings and other continuing medical education events.
With the evolution of hospital medicine, hospitalists have to be malleable in order to optimally meet the needs of the population they serve. The possibilities are endless.
- ,.The Hospitalist movement 5 years later.JAMA.2002;287:487–494.
- Hospitals and Health Networks. Hospitalists: a specialty coming into its own. Available at: http://www.hhmag.com. Accessed February 27,2006.
- ,,.Emergency medicine and public health: new steps in old directions.Ann Emerg Med.2001;38:675–683.
- ,, et al.A public health approach to emergency medicine: preparing for the twenty‐first century.Acad Emerg Med.1994;1:277–286.
- ,.Emergency medicine in population‐based systems of care.Ann Emerg Med.1997;30:800–803.
- ,.Principles of Public Health Practice.Albany, NY:Delmar Publishing;1997.
- Centers for Medicare and Medicaid. Health care spending and growth rate continue to decline in 2004. Available at: http://www.cms.hhs.gov. Accessed October 31,2006.
- ,,, et al.National health expenditures, 2002.Health Care Financ Rev. Summer2004;25:4.
- ,,, et al.Health spending Projections Through 2015: Changes on the Horizon.Health Affairs2006;25:w61–w73.
- Institute of Medicine.Recommendations from the Future of Public Health. InThe Future of the Public's Health.Washington, DC:National Academic Press;2003:411–420.
- ,,.Nosocomial pneumonia: state of the science.Am J Infect Control.2006;34:84–93.
- ,,,,.A reminder reduces urinary catheterization in hospitalized patients.Jt Comm J Qual Patient Saf.2005;31:455–462.
- ,,,.Preventing infections in nursing homes: A survey of infection control practices in southeast Michigan.Am J Infect Control.2005;33:489–492.
- ,,,.Prospective validation of a prediction model for isolating inpatients with suspected pulmonary tuberculosis.Arch Intern Med.2005;165:453–457.
- ,.The Hospital Infection Standardised Surveillance (HISS) programme: analysis of a two‐year pilot.J Hosp Infect.2003;53:259–267.
- ,,,.A Laboratory‐Based, Hospital‐Wide, Electronic Marker for Nosocomial Infection.Am J Clin Pathol.2006;125:34–39.
- ,,.Severe acute respiratory syndrome.Arch Pathol Lab Med.2004;128:1346–1350.
- ,,.Severe acute respiratory syndrome: responses of the healthcare system to a global epidemic.Curr Opin Otolaryngol Head Neck Surg.2005;13:161–164.
- ,.Pandemic influenza and the hospitalist: apocalypse when?J Hosp Med.2006;1:118–123.
- Center for Disease Control and Prevention. Pandemic Influenza information for Health Professionals. Available at: http://www.cdc.gov/flu/pandemic/. Accessed October 31,2006.
- .US health policy in the aftermath of Hurricane Katrina.JAMA.2006;295:437–40
- Levy B,Sidel V, eds.Terrorism and Public Health.New York:Oxford University Press;2003.
- Centers for Disease Control and Prevention (CDC).Public health response to Hurricanes Katrina and Rita—United States 2005.MMWR Morb Mortal Wkly Rep.2006;55:229–231.
- ,,,,,.Racial and ethnic disparities in health: a view from the South Bronx.J Health Care Poor Underserved.2006;17:116–127.
- ,.Williams E. Health Seeking behaviors of African Americans: implications for health administration.J Health Hum Serv Adm.2005;28(1):68–95.
- .Routine rapid HIV testing in hospitals: another opportunity for hospitalists to improve care.J Hosp Med.2006;1:106–112.
- Centers for Disease Control and Prevention.Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003.MMWR Morb Mortal Wkly Rep.2003;52:329–332.
- ,,, et al.Expanded screening for HIV in the United States—an analysis of cost‐effectiveness.N Engl J Med.2005;352:586–595.
- ,,,.Identifying undiagnosed human immunodeficiency virus: the yield for routine, voluntary, inpatient testing.Arch Intern Med.2002;162:887–892.
- ,,,,.Insufficient treatment of hypercholestrolemia among patients hospitalized with chest pain.Clin Cardiol.2006;29:259–262.
- .Medical management of alcoholic patients. In:Kissen B,Besleiter H, eds.Treatment and Rehabilitation of the Chronic Alcoholic.New York:Plenum Publishing Co.;1997.
- ,,.An integral approach to substance abuse.J Psychoactive Drugs.2005;37:363–371.
- ,,, et al.Smoking cessation practice among Norwegian hospital physicians.Tiddskr Nor laegeforen.2000;120:1629–1632.
- ,, et al.Evaluation of an intervention for hospitalized African American smokers.Am J Health Behav.2005;29:228–239.
- .Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs [review].J Am Geriatr Soc.2003;51:549–555.
- ,,,,.Advances in hospital medicine: a review of key articles from the literature.Med Clin N Am.2002;86:797–823.
- ,,,,,.Comprehensive discharge planning with post discharge support for older patients with congestive heart failure.JAMA.2004;291:1358–1367.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis.Med Care Res Rev.2005;62:379–406.
- ,,,,,Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists.Arch Intern Med.2002;162:1251–1256.
- ,,,.Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) colloquim, 2002.Lancet Infect Dis.2004;4:44–53.
- ,,, et al.Systematic review of antimicrobial drug prescribing in hospitals.Emerg Infect Dis.2006;12:211–216.
- ,,,,,,.Recommendations for management of community and hospital acquired pneumonia‐the hospitalist perspective.Curr Opin Pulm Med.2004;10(suppl 1):S23–S27.
- ,,,,.Advances in hospital medicine: a review of key articles from the literature.Med Clin N Am.2002;86:797–823.
- .End‐of‐life care for the hospitalized patient.Med Clin N Am.2002;86:749–770.
- ,.Palliative care for patients with heart failure.JAMA.2004;291:2476–2482.
- ,.Prevalence and structure of palliative care services in California hospitals.Arch Intern Med.2003;163:1084–1088.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.J Med.2001;111:10S–14S.
- .Palliative care in hospitals.J Hosp Med.2006;1:21–28.
- ,.End‐of‐life care in a voluntary hospitalist model: effects on communication, process of care, and patient symptoms.Am J Med.2004;116:669–675.
- ,,,Understanding medical error and improving patient safety in the inpatient setting,Med Clin N Am2002;86:847–867.
- , The hospitalist movement: ten issues to consider, hospital practice. Available at: http://www.hosppract.com/issues/1999/02/wachter.htm. Accessed March 14,2006.
- Shojania KG,Duncan BW,McDonald KM,Wachter RM, eds.Making health care safer: a critical analysis of patient safety practices. Evidence Report/Technology Assessment No. 43 from the Agency for Healthcare Research and Quality: AHRQ Publication No. 01‐E058;2001. Available at: http://www.ahrq.gov/clinic/ptsafety/.
- ,,,.Safe but sound: patient safety meets evidence‐based medicine.JAMA.2002;288:508–513.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- Hospitalists, pharmacists partner to cut errors: shorter lengths of stay, lower med costs result. HealthCare Benchmarks and Quality Improvement.American Health Consultants, Inc.,2005.
- ,,,.Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians.Ann Intern Med.1999;130:343–349.
- ,,,,.Core competencies in hospital medicine: Development and methodology.J Hosp Med.2006;1:48–56.
- National guideline clearing house. Available at: http://www.guideline.gov. Accessed June 26,2006.
- ,,,,, eds.The core competencies in hospital medicine.J Hosp Med.2006;1(suppl 1).
- Joint Commission on Accreditation of Healthcare Organizations. Core Measures overview. Available at: http://www.jcaho.org/perfeas/coremeas/cm.ovrvw.html. Accessed February 1,2006.
- ,,,.,Comparison of processes and outcomes of pneumonia care between hospitalists and community‐based primary care physicians.Mayo Clin Proc.2002;77:1053–1058.
- ,.The effectiveness of a nursing inpatient smoking cessation program in individuals with cardiovascular disease.Nurs Res.2005;54:243–254.
- ,,,,,.Evaluation of an intervention for hospitalized African American smokers.Am J Health Behav.2005;29:228–239.
- .Smoking cessation: the case for hospital‐based interventions.Prof Nurse.2003;19(3):145–148..
- . Dee Hock's management principles, in his own words. Fast Company.1996;5:79. Available at: http://www.fastcompany.com/magazine/05/dee2.html.
- ,,,.Hospital Medicine Fellowships: Works in progress.Am J Med.2006;119(1):72.e1–e7.
The field of hospital medicine came into being in response to numerous factors involving physicians, patients, and hospitals themselves1 Now, years later, hospital medicine is a specialty that is growing, both in size and sophistication such that the role of the hospitalist is constantly evolving.2 A compelling function that has not yet been clearly articulated is the opportunity for hospitalists to serve as public health practitioners in their unique clinical environment. There is precedence for the power of collaboration between medicine and public health as has been seen with emergency medicine's willingness to embrace opportunities to advance public health.35
In public health, the programs, services, and institutions involved emphasize the prevention of disease and the health needs of the population as a whole. Public health activities vary with changing technology and social values, but the goals remain the same: to reduce the amount of disease, premature death, and disease‐associated discomfort and disability in the population.6 The authors of a leading textbook of public health, Scutchfield and Keck, contend that the most important skill for public health practice is the capacity to visualize the potential for health that exists in a community.6
Hospitalists care for a distinct subset of the general populationinpatients, only a small percentage of society in a given year. Yet over time hospitalists affect a substantial subset of the larger population that uses considerable health care resources.79 Furthermore, hospitalization can be a sentinel event with public health implications (eg, newly diagnosed HIV infection or acute myocardial infarction in a patient with an extended family of cigarette smokers). This presents an opportunity to educate and counsel both the patient and the patient's social network. One model of public health practice by hospitalists is to influence the patient, his or her family, and the community by touching and inspiring the hospitalized patient.
Hospitalists are already involved in many of the core functions of public health (assessment, assurance, and policy development; Fig. 1).10 Achieving ongoing success in this arena means developing hospitalists who are consciously in tune with their roles as public health practitioners.
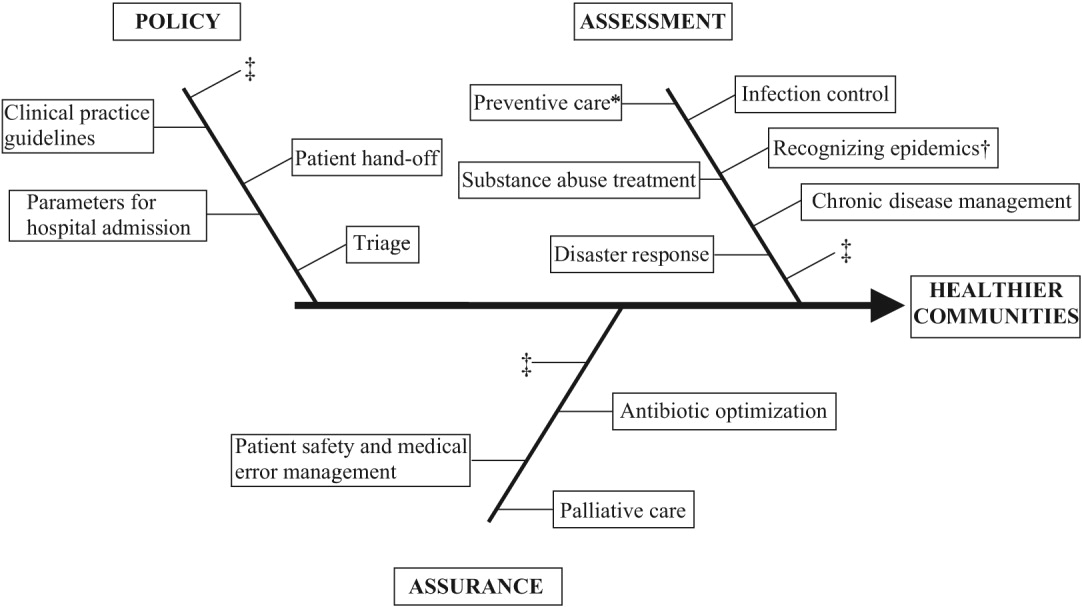
In this article we define the specific public health contributions that hospitalists have made and describe the possibilities for further innovative advances. To this end, we outline specific public health roles under the broad categories of assessment, assurance, and policy. We point to advances in public health accomplished by hospitalists as well as those being performed by nonhospitalists in the hospital setting. We conclude by describing some of the barriers to and implications of hospitalists taking on public health roles.
ASSESSMENT
Assessment is the systematic collection, analysis, and dissemination of health status information.10 These activities include disease surveillance and investigation of acute outbreaks or changes in the epidemiology of chronic diseases. Assessment also involves understanding the health of a population and the key determinants of a population's health from a variety of perspectives: physical, biological, behavioral, social, cultural, and spiritual.6 Human health has been defined as a state characterized by anatomic integrity; ability to perform personally valued family work and community roles; ability to deal with physical, biologic, and social stress; a feeling of well‐being; and freedom from the risk of disease and untimely death.6 Hospitalists interact with individuals at times of stress and acute illness and thus have a unique opportunity to assess the strength, viability, and resources available to individuals. Key roles that may fall within the auspices of assessment in hospital medicine are infection control, epidemic recognition, disaster response, preventive care, substance abuse treatment, and chronic disease management.
Infection Control
Physicians caring for inpatients have a crucial stake in controlling hospital infection as exemplified by the work of Flanders et al. on preventing nosocomial infections, especially nosocomial pneumonia.11 They describe specific strategies to prevent iatrogenic spread such as washing hands before and after patient contact, establishing guidelines against the use of artificial fingernails, using indwelling devices such as catheters only when absolutely necessary, and using sterile barriers.11 Hospitalists such as Sanjay Saint have led the way in studying methods to reduce bladder catheterization, which has been associated with urinary tract infections12; others have collaborated on work to prevent infections in nursing homes.13 Given the importance of this field, there is room for further hospitalist involvement. Novel methods for infection control in hospitals have been studied by nonhospitalists such as Wisnivesky, who prospectively validated a clinical decision rule to predict the need for respiratory isolation of inpatients with suspected tuberculosis (TB). This prediction rule, which is based on clinical and chest radiographic findings, was able to accurately identify patients at low risk for TB from among inpatients with suspected active pulmonary TB isolated on admission to the hospital.14 Retrospective application of the prediction rule showed respiratory precautions were inappropriately implemented for a third of patients.14 These studies are examples of empiric public health research performed in the inpatient setting. In the infection control domain, candidate issues for further study could include interventions aimed at reducing rates of Clostridium difficile, developing programs for standardized surveillance of hospital infection, validating electronic markers for nosocomial infection, and taking innovative approaches to improving hand‐washing practices in the hospital.15, 16
Recognizing Epidemics
An excellent example of the importance of hospitalists embracing public health and remembering their patients are part of a community was the severe acute respiratory syndrome (SARS) outbreak in Toronto, Ontario, Canada. The outbreak is thought to have begun with a single traveler. With the transfer of patients and the movement of visitors and health care workers among facilities, SARS quickly spread through Toronto, making it the largest SARS‐affected area outside Asia.17 Approximately a month after the outbreak was recognized in Toronto, it was thought to be over, and the World Health Organization (WHO) removed Toronto from its SARS‐affected list.17 Unfortunately, patients with unrecognized SARS remained in health care institutions, including a patient transferred to a rehabilitation center. Infection quickly spread again, resulting in a second phase of the outbreak.17
The SARS outbreak served as a reminder that a global public health system is essential and taught many lessons17 germane to pandemics that recur annually (eg, influenza viruses) as well those that episodically threaten the health of the population (eg, avian flu). Proposed actions to prevent a repeat of the scenario that occurred with SARS in Toronto include assessing the current facilities (eg, isolation rooms and respiratory masks) at each institution, identifying health care workers willing to serve as an outbreak team, and the hiring staff to train hospital personnel in personal protective equipment (PPE) and infection control policies.18 The Centers for Disease Control and Prevention (CDC) contends that planning for the possibility of a virulent pandemic at the local, national, and global levels is critical to limiting the mortality and morbidity should such occur.19, 20 In a previous article, Pile and Gordon declared hospitalists are key players in institutional efforts to prepare for a viral pandemic such as influenza and should be aware of lessons that may be applied from responses to pandemics such as SARS.19 Well placed to recognize clinical trends that may herald epidemics, hospitalists can fulfill some of the necessary public health responsibilities delineated above.
Disaster Response
Natural disasters and terrorism are in the forefront of the popular press and are also high priorities in health care and public health.21 Terrorism and natural disasters cause significant injury, illness, and death.22 Hospital‐based health care providers fulfill a variety of roles when terrorist acts and disasters occur, including reporting, diagnosing, and managing illness, providing preventive measures (eg, vaccines and preparedness kits), preventing the secondary spread of disease, assisting in the investigation of the causes of disease outbreaks, participating in preparedness planning, and evaluating preparedness policies and programs.22 The experience gained in the aftermaths of Hurricanes Katrina and Rita with their unprecedented death, injury, destruction, and displacement should help to guide future response and recovery activities.23 Hospitalists were at the forefront of delivering care, living in their hospitals for days after Hurricane Katrina. Without question, hospitalists will be called on again to serve those affected by disasters.
Preventive Care
For many patients admitted to the hospital, meeting a hospitalist is their first encounter with a physician in years.24, 25 In these instances, hospitalists must ensure that patients' immunizations are up‐to‐date and arrange appropriate follow‐up care with primary care providers. Greenwald described an important role that hospitalists could play in HIV prevention by promoting HIV testing in the hospital.26 The CDC recently confirmed the wisdom of this approach and estimates that the 250,000 to 1.2 million people in the United States with HIV infection who do not know their serostatus play a significant role in HIV transmission.26, 27 In an effort to promote testing, the CDC has initiated a program aimed at incorporating HIV testing into routine medical care, as recommended by others.28 More than a quarter of patients with HIV in the United States are diagnosed in the hospital, and for many other patients, hospitalization is their only real opportunity to be tested.26, 29 Similarly, when hospitalists find elevated cholesterol or triglycerides in routine evaluations of patients who present with chest pain, they have to decide whether to initiate lipid‐lowering medications.30 The hospitalist is sometimes the only physician that patients repeatedly admitted, may see over prolonged periods. It follows that if hospitalists are remiss in delivering preventive care to such patients, they lose the opportunity to positively affect their long‐term health. In practice, hospitalists perform myriad preventive‐care functions, although there is scant literature supporting this role. Hospitalists have an opportunity to collaborate in research projects of hospital‐initiated preventive care that measure outcomes at the community level.
Substance Abuse
In the Unites States, 25%‐40% of hospital admissions are related to substance abuse and its sequelae.31 These patients frequently are admitted to general medicine services for detoxification or treatment of substance‐abuse‐related morbidity, although some American hospitals have specialized treatment and detoxification centers. There is a pressing need for more models of comprehensive care that address the complex issues of addiction, including the biological, social, cultural, spiritual, and developmental needs of patients.32
Hospitalists routinely counsel their patients with substance abuse problems and often consult a chemical dependency counselor, who provides patients with additional information about outpatient or inpatient facilities that may help them after their hospitalization. Unfortunately, because of the natural history of substance abuse, many of these patients are rehospitalized with the same problems even after going through rehabilitation. The adoption of a public health philosophy and approach by hospitalists may assist patients who have addictions through innovative multidisciplinary interventions while these patient are being detoxified. Traditionally, these responsibilities have fallen to primary care providers and psychologists in substance abuse medicine; but, as mentioned previously, many such patients are rehospitalized before they make it to their follow‐up appointments.
In a study examining smoking cessation practices among Norwegian hospital physicians, 98% of the doctors stated they ask their patients about their smoking habits, but fewer than 7% of these physicians regularly offer smoking‐cessation counseling, hand out materials, or give patients other advice about smoking cessation.33 That study illustrates that hospital doctors often ask about problems but can certainly improve in terms of intervention and follow‐up. Other works by nonhospitalist physicians have examined the real potential of inpatient interventions for smoking cessation. Most of this work involves a multidisciplinary approach that relies heavily on nurses. For example, Davies et al. evaluated the effectiveness of a hospital‐based intervention for smoking cessation among low‐income smokers using public health methodologies. The intervention was effective and promising as a way to affect smokers in underserved communities.34
Chronic Disease Management
Public health roles involving chronic disease management include surveillance, intervention design, and implementation of control programs.6 Given their access to data on hospitalized patients, hospitalists can carry out surveillance and empirical population‐based research about hospitalized patients with chronic illnesses. Thoughtfully designed protocols can measure the success of interventions initiated in patients while hospitalized, with further data collection and follow‐up after patients have returned to the community.35 Such endeavors can improve the likelihood that patients with chronic conditions are effectively referred to programs that will maintain their health and functional status.36 If hospitalists consider themselves public health providers, encounters with these hospitalized patients will go beyond noting that their chronic conditions are stable and instead will lay the groundwork to prospectively control these conditions. This approach would have the potential to reduce the number of future hospitalizations and lead to healthier communities.37 To truly carry this out effectively, coordinated collaboration between primary care providers and hospitalists will be necessary.
ASSURANCE
Assurance is the provision of access to necessary health services. It entails efforts to solve problems that threaten the health of populations and empowers individuals to maintain their own health. This is accomplished by either encouraging action, delegating to other entities (private or public sector), mandating specific requirements through regulation, or providing services directly.10 Hospitalist teams aim to ensure that the high‐quality services needed to protect the health of their community (hospitalized patients) are available and that this population receives proper consideration in the allocation of resources. The few studies to date that have directly examined the quality of care that hospitalists provide38 have done so using evidence‐based measures believed to correlate with improved health care outcomes.38 The ambiguities in assessing quality may in part limit such studies.39 Specific hospitalist roles that fall under the assurance umbrella include antibiotic optimization, palliative care, patient safety, and medical error management.
Antibiotic Optimization
Inappropriate use of antimicrobial treatment for infectious diseases has cost and public health implications.40 These inappropriate uses include giving antibiotics when not indicated, overusing broad‐spectrum antibiotics, making mismatches between microbes and medicines when cultures and information on test sensitivity are available, and using intravenous formulations when oral therapy would suffice.41 The public health impact goes way beyond increasing selective pressure for antimicrobial resistance to include safety, adverse events, and increased costs to both patient and hospitals.40 At our institution, the hospital medicine service and infectious disease division have jointly developed and implemented an intervention to reduce inappropriate antibiotic use. At other institutions, hospitalist teams have developed protocols for treating infectious diseases commonly encountered in the hospitalized patient.42 The recommendations of both Amin and Reddy for management of community‐ and hospital‐acquired pneumonia acknowledged that through establishment of clinical care pathways, variation in prescribing patterns among hospitalists can be decreased while optimizing outcomes.42 The work of Williams and colleagues is another example of advances by hospitalists. They reviewed the literature to determine that the use of combination antibiotics as empiric therapy for community‐acquired pneumonia is superior to the use of a single effective antibiotic in treating bacteremic patients with pneumococcal community‐acquired pneumonia.43
Palliative Care
Mortality is a vital outcome measure of public health research and interventions. Not surprisingly, many people are hospitalized in the final months of their life and often die in a hospital. Pantilat showed that hospitalists can respond to these circumstances and have the opportunity to improve care of the dying.4446 Muir et al. evaluated the convergence of the fields of palliative care medicine and hospital medicine and reviewed the opportunities for mutual education and improved patient care.47 They described how the confluence of the changing nature and site of death in the United States coupled with the reorganization of hospital care provides a strategic opportunity to improve end‐of‐life care.47 Hospitalists can ensure that care of the dying is delivered with skill, compassion, and expertise. And so it is imperative they be trained to accomplish this objective.47, 49
Fortunately, hospitalists already appear to enhance patientphysician communication. Auerbach looked at communication, care patterns, and outcomes of dying patients, comparing patients being cared for by hospitalists with those being care for by community‐based physicians. Hospitalists had discussions with patients or their families about care more often than did nonhospitalist physicians (91% versus 73%, respectively, P = .006).49 Because the delivery of high‐quality palliative care is time consuming and complex, alternative models for billing or the use of physician extenders or consultants may be necessary at some institutions.
Patient Safety and Medical Error Management
Hospitalists have been in the forefront of promoting a culture of patient safety.50 Their continuous presence in the hospital and their interactions with members of health care teams from multiple disciplines who share this goal make them important facilitators. Hospitalists have increasing involvement in systems‐based efforts aimed at reducing medical errors.50 Hospitalists are being asked to lead committees that adopt multidisciplinary approaches to reduce adverse events, morbidity, and mortality.50 These committees often have representation from pharmacy, nursing, and other key hospital stakeholders including from the administration.51 Quality assurance activities assess locally collected data and compare results with local and national benchmarks. There are several published examples of hospitalists engaged in patient safety and medical error management. For example, Shojania et al compiled evidence based safety practices in an effort to promote patient safety.52, 53 Schnipper studied the role of pharmacist counseling in preventing adverse drug events (ADEs) after hospitalization and found that pharmacist medication review, patient counseling, and telephone follow‐up were associated with a lower rate of preventable ADEs 30 days after hospital discharge.54 Moreover, Syed paired hospitalists and pharmacists to collaboratively prescribe medications appropriately. In one study there were fewer medication errors and adverse drug reactions in patients treated by a team led by hospitalists than in those treated by the control group, made up of nonhospitalist attendings.55
POLICY
Policy development defines health control goals and objectives and develops implementation plans for those goals.10 By necessity, it operates at the intersection of legislative, political, and regulatory processes.10 At many institutions, hospitalists have been involved in the development of policies ensuring that the core functions of assessment and assurance are addressed and maintained. In fact, hospitalists report that development of quality assurance and practice guidelines accounts for most of their nonclinical time.56 This role of hospitalists is supported by anecdotal reports rather than published empiric evidence.57 For example, at Johns Hopkins Bayview Medical Center, hospitalist‐led teams have developed triage and patient handoff policies designed to improve patient safety. Parameters for admission to the general medicine ward have been elaborated and are periodically refined by the hospitalist team.
Another area that falls within the genre of policy is development of clinical practice guidelines. Guidelines for the treatment of pneumonia, congestive heart failure, deep‐vein thrombosis prophylaxis, alcohol and drug withdrawal, pain management, delirium, and chronic obstructive pulmonary disease have been developed by nonhospitalists.58, 59 These areas are considered core competencies in hospital medicine, and as such, hospitalists have an obligation to review and refine these guidelines to ensure the best provision of care to our patients.59
Hospitalists have been engaged in upholding guidelines that affect community practice. For example, in a study comparing treatment of patients admitted with congestive heart failure by hospitalists compared with that by nonhospitalists, hospitalists were found to be more likely to document left ventricular function, a core measure of quality as defined by JCAHO.39, 60 Knowledge about cardiac function can direct future care for patients when they return to the community and into the care of their primary care providers. In another example, Rifkin found that patients with community‐acquired pneumonia treated by hospitalists were more rapidly converted to oral antibiotics from intravenous antibiotics, facilitating a shorter length of stay,61 which reduced the opportunity for nosocomial infections to propagate. Because hospitalists are skilled at following guidelines,59 it follows that they should seize the opportunity to develop more of them.
As the hospitalist movement continues to grow, hospitalists will likely be engaged in implementing citywide, statewide, and even national policies that ensure optimal care of the hospitalized patient.
BARRIERS TO HOSPITALISTS FOCUSING ON PUBLIC HEALTH
Hospitalists are involved in public health activities even though they may not recognize the extent of this involvement. However, there may be some drawbacks to hospitalists viewing each patient encounter as an opportunity for a public health intervention. First, in viewing a patient as part of a cohort, the individual needs of the patient may be overlooked. There is inherent tension between population‐based and individual‐based care, which is a challenge. Second, hospitalists are busy clinicians who may be most highly valued because of their focus on efficiency and cost savings in the acute care setting. This factor alone may prevent substantive involvement by hospitalists in public health practice. Moving beyond the management of an acute illness may interfere with this efficiency and cost effectiveness from the hospital's perspective. However, interventions that promote health and prevent or reduce rehospitalizations may be cost effective to society in the long run. Third, current billing systems do not adequately reward or reimburse providers for the extra time that may be necessary to engage in public health practice. Fourth, hospitalists may not have the awareness, interest, training, or commitment to engage in public health practice. Finally, there may not be effective collaboration and communication systems between primary care providers and hospitalists. This barrier limits or hinders many possibilities for the effective execution of several public health initiatives.
CONCLUSIONS AND IMPLICATIONS
Hospitalists and the specialty of hospital medicine materialized because of myriad economic forces and the need to provide safe, high‐quality care to hospitalized patients. In this article we have described the ways in which hospitalists can be explicitly involved in public health practice. Traditionally, physicians caring for hospitalized patients have collected information through histories and physical examinations, interpreted laboratory data and tests, and formulated assessments and plans of care. To become public health practitioners, hospitalists have to go beyond these tasks and consider public health thought processes, such as problem‐solving paradigms and theories of behavior change. In adopting this public health perspective, hospitalists may begin to think of a patient in the context of the larger community in order to define the problems facing the community, not just the patient, determine the magnitude of such problems, identify key stakeholders, create intervention/prevention strategies, set priorities and recommend interventions, and implement and evaluate those interventions. This approach forces providers to move beyond the physicianpatient model and draw on public health models to invoke change. Hopefully, future research will further convince hospitalists of the benefits of this approach. Although it may be easier to defer care and management decisions to an outpatient physician, data suggest that intervening when patients are in the hospital may be most effective.62, 63 For example, is it possible that patients are more likely to quit smoking when they are sick in the hospital than when they are in their usual state of health on a routine visit at their primary care provider's office?64 Further, although deferring care to a primary care provider (PCP) may be easier, it is not always possible given these barriers: (1) some patients are routinely rehospitalized, precluding primary care visits, (2) some recommendations may not be received by PCPs, and (3) PCPpatient encounters are brief and the agendas full, and there are limited resources to address recommendations from the hospital.
As hospitalists become more involved in public health practice, their collaboration with physicians and researchers in other fields, nurses, policymakers, and administrators will expand. Succeeding in this arena requires integrity, motivation, capacity, understanding, knowledge, and experience.65 It is hoped that hospitalists will embrace the opportunity and master the requisite skill set necessary to practice in and advance this field. As hospitalist fellowship programs are developed, public health practice skills could be incorporated into the curriculum. Currently 6 of 16 fellowship programs offer either a master of public health degree or public health courses.66 Public health skills can also be taught at Society of Hospital Medicine meetings and other continuing medical education events.
With the evolution of hospital medicine, hospitalists have to be malleable in order to optimally meet the needs of the population they serve. The possibilities are endless.
The field of hospital medicine came into being in response to numerous factors involving physicians, patients, and hospitals themselves1 Now, years later, hospital medicine is a specialty that is growing, both in size and sophistication such that the role of the hospitalist is constantly evolving.2 A compelling function that has not yet been clearly articulated is the opportunity for hospitalists to serve as public health practitioners in their unique clinical environment. There is precedence for the power of collaboration between medicine and public health as has been seen with emergency medicine's willingness to embrace opportunities to advance public health.35
In public health, the programs, services, and institutions involved emphasize the prevention of disease and the health needs of the population as a whole. Public health activities vary with changing technology and social values, but the goals remain the same: to reduce the amount of disease, premature death, and disease‐associated discomfort and disability in the population.6 The authors of a leading textbook of public health, Scutchfield and Keck, contend that the most important skill for public health practice is the capacity to visualize the potential for health that exists in a community.6
Hospitalists care for a distinct subset of the general populationinpatients, only a small percentage of society in a given year. Yet over time hospitalists affect a substantial subset of the larger population that uses considerable health care resources.79 Furthermore, hospitalization can be a sentinel event with public health implications (eg, newly diagnosed HIV infection or acute myocardial infarction in a patient with an extended family of cigarette smokers). This presents an opportunity to educate and counsel both the patient and the patient's social network. One model of public health practice by hospitalists is to influence the patient, his or her family, and the community by touching and inspiring the hospitalized patient.
Hospitalists are already involved in many of the core functions of public health (assessment, assurance, and policy development; Fig. 1).10 Achieving ongoing success in this arena means developing hospitalists who are consciously in tune with their roles as public health practitioners.
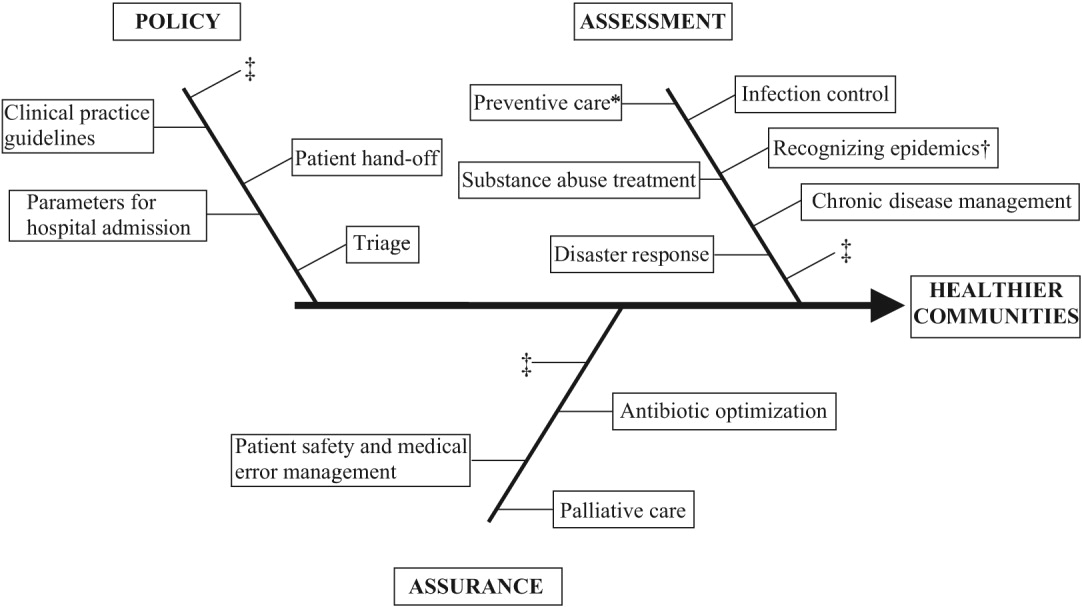
In this article we define the specific public health contributions that hospitalists have made and describe the possibilities for further innovative advances. To this end, we outline specific public health roles under the broad categories of assessment, assurance, and policy. We point to advances in public health accomplished by hospitalists as well as those being performed by nonhospitalists in the hospital setting. We conclude by describing some of the barriers to and implications of hospitalists taking on public health roles.
ASSESSMENT
Assessment is the systematic collection, analysis, and dissemination of health status information.10 These activities include disease surveillance and investigation of acute outbreaks or changes in the epidemiology of chronic diseases. Assessment also involves understanding the health of a population and the key determinants of a population's health from a variety of perspectives: physical, biological, behavioral, social, cultural, and spiritual.6 Human health has been defined as a state characterized by anatomic integrity; ability to perform personally valued family work and community roles; ability to deal with physical, biologic, and social stress; a feeling of well‐being; and freedom from the risk of disease and untimely death.6 Hospitalists interact with individuals at times of stress and acute illness and thus have a unique opportunity to assess the strength, viability, and resources available to individuals. Key roles that may fall within the auspices of assessment in hospital medicine are infection control, epidemic recognition, disaster response, preventive care, substance abuse treatment, and chronic disease management.
Infection Control
Physicians caring for inpatients have a crucial stake in controlling hospital infection as exemplified by the work of Flanders et al. on preventing nosocomial infections, especially nosocomial pneumonia.11 They describe specific strategies to prevent iatrogenic spread such as washing hands before and after patient contact, establishing guidelines against the use of artificial fingernails, using indwelling devices such as catheters only when absolutely necessary, and using sterile barriers.11 Hospitalists such as Sanjay Saint have led the way in studying methods to reduce bladder catheterization, which has been associated with urinary tract infections12; others have collaborated on work to prevent infections in nursing homes.13 Given the importance of this field, there is room for further hospitalist involvement. Novel methods for infection control in hospitals have been studied by nonhospitalists such as Wisnivesky, who prospectively validated a clinical decision rule to predict the need for respiratory isolation of inpatients with suspected tuberculosis (TB). This prediction rule, which is based on clinical and chest radiographic findings, was able to accurately identify patients at low risk for TB from among inpatients with suspected active pulmonary TB isolated on admission to the hospital.14 Retrospective application of the prediction rule showed respiratory precautions were inappropriately implemented for a third of patients.14 These studies are examples of empiric public health research performed in the inpatient setting. In the infection control domain, candidate issues for further study could include interventions aimed at reducing rates of Clostridium difficile, developing programs for standardized surveillance of hospital infection, validating electronic markers for nosocomial infection, and taking innovative approaches to improving hand‐washing practices in the hospital.15, 16
Recognizing Epidemics
An excellent example of the importance of hospitalists embracing public health and remembering their patients are part of a community was the severe acute respiratory syndrome (SARS) outbreak in Toronto, Ontario, Canada. The outbreak is thought to have begun with a single traveler. With the transfer of patients and the movement of visitors and health care workers among facilities, SARS quickly spread through Toronto, making it the largest SARS‐affected area outside Asia.17 Approximately a month after the outbreak was recognized in Toronto, it was thought to be over, and the World Health Organization (WHO) removed Toronto from its SARS‐affected list.17 Unfortunately, patients with unrecognized SARS remained in health care institutions, including a patient transferred to a rehabilitation center. Infection quickly spread again, resulting in a second phase of the outbreak.17
The SARS outbreak served as a reminder that a global public health system is essential and taught many lessons17 germane to pandemics that recur annually (eg, influenza viruses) as well those that episodically threaten the health of the population (eg, avian flu). Proposed actions to prevent a repeat of the scenario that occurred with SARS in Toronto include assessing the current facilities (eg, isolation rooms and respiratory masks) at each institution, identifying health care workers willing to serve as an outbreak team, and the hiring staff to train hospital personnel in personal protective equipment (PPE) and infection control policies.18 The Centers for Disease Control and Prevention (CDC) contends that planning for the possibility of a virulent pandemic at the local, national, and global levels is critical to limiting the mortality and morbidity should such occur.19, 20 In a previous article, Pile and Gordon declared hospitalists are key players in institutional efforts to prepare for a viral pandemic such as influenza and should be aware of lessons that may be applied from responses to pandemics such as SARS.19 Well placed to recognize clinical trends that may herald epidemics, hospitalists can fulfill some of the necessary public health responsibilities delineated above.
Disaster Response
Natural disasters and terrorism are in the forefront of the popular press and are also high priorities in health care and public health.21 Terrorism and natural disasters cause significant injury, illness, and death.22 Hospital‐based health care providers fulfill a variety of roles when terrorist acts and disasters occur, including reporting, diagnosing, and managing illness, providing preventive measures (eg, vaccines and preparedness kits), preventing the secondary spread of disease, assisting in the investigation of the causes of disease outbreaks, participating in preparedness planning, and evaluating preparedness policies and programs.22 The experience gained in the aftermaths of Hurricanes Katrina and Rita with their unprecedented death, injury, destruction, and displacement should help to guide future response and recovery activities.23 Hospitalists were at the forefront of delivering care, living in their hospitals for days after Hurricane Katrina. Without question, hospitalists will be called on again to serve those affected by disasters.
Preventive Care
For many patients admitted to the hospital, meeting a hospitalist is their first encounter with a physician in years.24, 25 In these instances, hospitalists must ensure that patients' immunizations are up‐to‐date and arrange appropriate follow‐up care with primary care providers. Greenwald described an important role that hospitalists could play in HIV prevention by promoting HIV testing in the hospital.26 The CDC recently confirmed the wisdom of this approach and estimates that the 250,000 to 1.2 million people in the United States with HIV infection who do not know their serostatus play a significant role in HIV transmission.26, 27 In an effort to promote testing, the CDC has initiated a program aimed at incorporating HIV testing into routine medical care, as recommended by others.28 More than a quarter of patients with HIV in the United States are diagnosed in the hospital, and for many other patients, hospitalization is their only real opportunity to be tested.26, 29 Similarly, when hospitalists find elevated cholesterol or triglycerides in routine evaluations of patients who present with chest pain, they have to decide whether to initiate lipid‐lowering medications.30 The hospitalist is sometimes the only physician that patients repeatedly admitted, may see over prolonged periods. It follows that if hospitalists are remiss in delivering preventive care to such patients, they lose the opportunity to positively affect their long‐term health. In practice, hospitalists perform myriad preventive‐care functions, although there is scant literature supporting this role. Hospitalists have an opportunity to collaborate in research projects of hospital‐initiated preventive care that measure outcomes at the community level.
Substance Abuse
In the Unites States, 25%‐40% of hospital admissions are related to substance abuse and its sequelae.31 These patients frequently are admitted to general medicine services for detoxification or treatment of substance‐abuse‐related morbidity, although some American hospitals have specialized treatment and detoxification centers. There is a pressing need for more models of comprehensive care that address the complex issues of addiction, including the biological, social, cultural, spiritual, and developmental needs of patients.32
Hospitalists routinely counsel their patients with substance abuse problems and often consult a chemical dependency counselor, who provides patients with additional information about outpatient or inpatient facilities that may help them after their hospitalization. Unfortunately, because of the natural history of substance abuse, many of these patients are rehospitalized with the same problems even after going through rehabilitation. The adoption of a public health philosophy and approach by hospitalists may assist patients who have addictions through innovative multidisciplinary interventions while these patient are being detoxified. Traditionally, these responsibilities have fallen to primary care providers and psychologists in substance abuse medicine; but, as mentioned previously, many such patients are rehospitalized before they make it to their follow‐up appointments.
In a study examining smoking cessation practices among Norwegian hospital physicians, 98% of the doctors stated they ask their patients about their smoking habits, but fewer than 7% of these physicians regularly offer smoking‐cessation counseling, hand out materials, or give patients other advice about smoking cessation.33 That study illustrates that hospital doctors often ask about problems but can certainly improve in terms of intervention and follow‐up. Other works by nonhospitalist physicians have examined the real potential of inpatient interventions for smoking cessation. Most of this work involves a multidisciplinary approach that relies heavily on nurses. For example, Davies et al. evaluated the effectiveness of a hospital‐based intervention for smoking cessation among low‐income smokers using public health methodologies. The intervention was effective and promising as a way to affect smokers in underserved communities.34
Chronic Disease Management
Public health roles involving chronic disease management include surveillance, intervention design, and implementation of control programs.6 Given their access to data on hospitalized patients, hospitalists can carry out surveillance and empirical population‐based research about hospitalized patients with chronic illnesses. Thoughtfully designed protocols can measure the success of interventions initiated in patients while hospitalized, with further data collection and follow‐up after patients have returned to the community.35 Such endeavors can improve the likelihood that patients with chronic conditions are effectively referred to programs that will maintain their health and functional status.36 If hospitalists consider themselves public health providers, encounters with these hospitalized patients will go beyond noting that their chronic conditions are stable and instead will lay the groundwork to prospectively control these conditions. This approach would have the potential to reduce the number of future hospitalizations and lead to healthier communities.37 To truly carry this out effectively, coordinated collaboration between primary care providers and hospitalists will be necessary.
ASSURANCE
Assurance is the provision of access to necessary health services. It entails efforts to solve problems that threaten the health of populations and empowers individuals to maintain their own health. This is accomplished by either encouraging action, delegating to other entities (private or public sector), mandating specific requirements through regulation, or providing services directly.10 Hospitalist teams aim to ensure that the high‐quality services needed to protect the health of their community (hospitalized patients) are available and that this population receives proper consideration in the allocation of resources. The few studies to date that have directly examined the quality of care that hospitalists provide38 have done so using evidence‐based measures believed to correlate with improved health care outcomes.38 The ambiguities in assessing quality may in part limit such studies.39 Specific hospitalist roles that fall under the assurance umbrella include antibiotic optimization, palliative care, patient safety, and medical error management.
Antibiotic Optimization
Inappropriate use of antimicrobial treatment for infectious diseases has cost and public health implications.40 These inappropriate uses include giving antibiotics when not indicated, overusing broad‐spectrum antibiotics, making mismatches between microbes and medicines when cultures and information on test sensitivity are available, and using intravenous formulations when oral therapy would suffice.41 The public health impact goes way beyond increasing selective pressure for antimicrobial resistance to include safety, adverse events, and increased costs to both patient and hospitals.40 At our institution, the hospital medicine service and infectious disease division have jointly developed and implemented an intervention to reduce inappropriate antibiotic use. At other institutions, hospitalist teams have developed protocols for treating infectious diseases commonly encountered in the hospitalized patient.42 The recommendations of both Amin and Reddy for management of community‐ and hospital‐acquired pneumonia acknowledged that through establishment of clinical care pathways, variation in prescribing patterns among hospitalists can be decreased while optimizing outcomes.42 The work of Williams and colleagues is another example of advances by hospitalists. They reviewed the literature to determine that the use of combination antibiotics as empiric therapy for community‐acquired pneumonia is superior to the use of a single effective antibiotic in treating bacteremic patients with pneumococcal community‐acquired pneumonia.43
Palliative Care
Mortality is a vital outcome measure of public health research and interventions. Not surprisingly, many people are hospitalized in the final months of their life and often die in a hospital. Pantilat showed that hospitalists can respond to these circumstances and have the opportunity to improve care of the dying.4446 Muir et al. evaluated the convergence of the fields of palliative care medicine and hospital medicine and reviewed the opportunities for mutual education and improved patient care.47 They described how the confluence of the changing nature and site of death in the United States coupled with the reorganization of hospital care provides a strategic opportunity to improve end‐of‐life care.47 Hospitalists can ensure that care of the dying is delivered with skill, compassion, and expertise. And so it is imperative they be trained to accomplish this objective.47, 49
Fortunately, hospitalists already appear to enhance patientphysician communication. Auerbach looked at communication, care patterns, and outcomes of dying patients, comparing patients being cared for by hospitalists with those being care for by community‐based physicians. Hospitalists had discussions with patients or their families about care more often than did nonhospitalist physicians (91% versus 73%, respectively, P = .006).49 Because the delivery of high‐quality palliative care is time consuming and complex, alternative models for billing or the use of physician extenders or consultants may be necessary at some institutions.
Patient Safety and Medical Error Management
Hospitalists have been in the forefront of promoting a culture of patient safety.50 Their continuous presence in the hospital and their interactions with members of health care teams from multiple disciplines who share this goal make them important facilitators. Hospitalists have increasing involvement in systems‐based efforts aimed at reducing medical errors.50 Hospitalists are being asked to lead committees that adopt multidisciplinary approaches to reduce adverse events, morbidity, and mortality.50 These committees often have representation from pharmacy, nursing, and other key hospital stakeholders including from the administration.51 Quality assurance activities assess locally collected data and compare results with local and national benchmarks. There are several published examples of hospitalists engaged in patient safety and medical error management. For example, Shojania et al compiled evidence based safety practices in an effort to promote patient safety.52, 53 Schnipper studied the role of pharmacist counseling in preventing adverse drug events (ADEs) after hospitalization and found that pharmacist medication review, patient counseling, and telephone follow‐up were associated with a lower rate of preventable ADEs 30 days after hospital discharge.54 Moreover, Syed paired hospitalists and pharmacists to collaboratively prescribe medications appropriately. In one study there were fewer medication errors and adverse drug reactions in patients treated by a team led by hospitalists than in those treated by the control group, made up of nonhospitalist attendings.55
POLICY
Policy development defines health control goals and objectives and develops implementation plans for those goals.10 By necessity, it operates at the intersection of legislative, political, and regulatory processes.10 At many institutions, hospitalists have been involved in the development of policies ensuring that the core functions of assessment and assurance are addressed and maintained. In fact, hospitalists report that development of quality assurance and practice guidelines accounts for most of their nonclinical time.56 This role of hospitalists is supported by anecdotal reports rather than published empiric evidence.57 For example, at Johns Hopkins Bayview Medical Center, hospitalist‐led teams have developed triage and patient handoff policies designed to improve patient safety. Parameters for admission to the general medicine ward have been elaborated and are periodically refined by the hospitalist team.
Another area that falls within the genre of policy is development of clinical practice guidelines. Guidelines for the treatment of pneumonia, congestive heart failure, deep‐vein thrombosis prophylaxis, alcohol and drug withdrawal, pain management, delirium, and chronic obstructive pulmonary disease have been developed by nonhospitalists.58, 59 These areas are considered core competencies in hospital medicine, and as such, hospitalists have an obligation to review and refine these guidelines to ensure the best provision of care to our patients.59
Hospitalists have been engaged in upholding guidelines that affect community practice. For example, in a study comparing treatment of patients admitted with congestive heart failure by hospitalists compared with that by nonhospitalists, hospitalists were found to be more likely to document left ventricular function, a core measure of quality as defined by JCAHO.39, 60 Knowledge about cardiac function can direct future care for patients when they return to the community and into the care of their primary care providers. In another example, Rifkin found that patients with community‐acquired pneumonia treated by hospitalists were more rapidly converted to oral antibiotics from intravenous antibiotics, facilitating a shorter length of stay,61 which reduced the opportunity for nosocomial infections to propagate. Because hospitalists are skilled at following guidelines,59 it follows that they should seize the opportunity to develop more of them.
As the hospitalist movement continues to grow, hospitalists will likely be engaged in implementing citywide, statewide, and even national policies that ensure optimal care of the hospitalized patient.
BARRIERS TO HOSPITALISTS FOCUSING ON PUBLIC HEALTH
Hospitalists are involved in public health activities even though they may not recognize the extent of this involvement. However, there may be some drawbacks to hospitalists viewing each patient encounter as an opportunity for a public health intervention. First, in viewing a patient as part of a cohort, the individual needs of the patient may be overlooked. There is inherent tension between population‐based and individual‐based care, which is a challenge. Second, hospitalists are busy clinicians who may be most highly valued because of their focus on efficiency and cost savings in the acute care setting. This factor alone may prevent substantive involvement by hospitalists in public health practice. Moving beyond the management of an acute illness may interfere with this efficiency and cost effectiveness from the hospital's perspective. However, interventions that promote health and prevent or reduce rehospitalizations may be cost effective to society in the long run. Third, current billing systems do not adequately reward or reimburse providers for the extra time that may be necessary to engage in public health practice. Fourth, hospitalists may not have the awareness, interest, training, or commitment to engage in public health practice. Finally, there may not be effective collaboration and communication systems between primary care providers and hospitalists. This barrier limits or hinders many possibilities for the effective execution of several public health initiatives.
CONCLUSIONS AND IMPLICATIONS
Hospitalists and the specialty of hospital medicine materialized because of myriad economic forces and the need to provide safe, high‐quality care to hospitalized patients. In this article we have described the ways in which hospitalists can be explicitly involved in public health practice. Traditionally, physicians caring for hospitalized patients have collected information through histories and physical examinations, interpreted laboratory data and tests, and formulated assessments and plans of care. To become public health practitioners, hospitalists have to go beyond these tasks and consider public health thought processes, such as problem‐solving paradigms and theories of behavior change. In adopting this public health perspective, hospitalists may begin to think of a patient in the context of the larger community in order to define the problems facing the community, not just the patient, determine the magnitude of such problems, identify key stakeholders, create intervention/prevention strategies, set priorities and recommend interventions, and implement and evaluate those interventions. This approach forces providers to move beyond the physicianpatient model and draw on public health models to invoke change. Hopefully, future research will further convince hospitalists of the benefits of this approach. Although it may be easier to defer care and management decisions to an outpatient physician, data suggest that intervening when patients are in the hospital may be most effective.62, 63 For example, is it possible that patients are more likely to quit smoking when they are sick in the hospital than when they are in their usual state of health on a routine visit at their primary care provider's office?64 Further, although deferring care to a primary care provider (PCP) may be easier, it is not always possible given these barriers: (1) some patients are routinely rehospitalized, precluding primary care visits, (2) some recommendations may not be received by PCPs, and (3) PCPpatient encounters are brief and the agendas full, and there are limited resources to address recommendations from the hospital.
As hospitalists become more involved in public health practice, their collaboration with physicians and researchers in other fields, nurses, policymakers, and administrators will expand. Succeeding in this arena requires integrity, motivation, capacity, understanding, knowledge, and experience.65 It is hoped that hospitalists will embrace the opportunity and master the requisite skill set necessary to practice in and advance this field. As hospitalist fellowship programs are developed, public health practice skills could be incorporated into the curriculum. Currently 6 of 16 fellowship programs offer either a master of public health degree or public health courses.66 Public health skills can also be taught at Society of Hospital Medicine meetings and other continuing medical education events.
With the evolution of hospital medicine, hospitalists have to be malleable in order to optimally meet the needs of the population they serve. The possibilities are endless.
- ,.The Hospitalist movement 5 years later.JAMA.2002;287:487–494.
- Hospitals and Health Networks. Hospitalists: a specialty coming into its own. Available at: http://www.hhmag.com. Accessed February 27,2006.
- ,,.Emergency medicine and public health: new steps in old directions.Ann Emerg Med.2001;38:675–683.
- ,, et al.A public health approach to emergency medicine: preparing for the twenty‐first century.Acad Emerg Med.1994;1:277–286.
- ,.Emergency medicine in population‐based systems of care.Ann Emerg Med.1997;30:800–803.
- ,.Principles of Public Health Practice.Albany, NY:Delmar Publishing;1997.
- Centers for Medicare and Medicaid. Health care spending and growth rate continue to decline in 2004. Available at: http://www.cms.hhs.gov. Accessed October 31,2006.
- ,,, et al.National health expenditures, 2002.Health Care Financ Rev. Summer2004;25:4.
- ,,, et al.Health spending Projections Through 2015: Changes on the Horizon.Health Affairs2006;25:w61–w73.
- Institute of Medicine.Recommendations from the Future of Public Health. InThe Future of the Public's Health.Washington, DC:National Academic Press;2003:411–420.
- ,,.Nosocomial pneumonia: state of the science.Am J Infect Control.2006;34:84–93.
- ,,,,.A reminder reduces urinary catheterization in hospitalized patients.Jt Comm J Qual Patient Saf.2005;31:455–462.
- ,,,.Preventing infections in nursing homes: A survey of infection control practices in southeast Michigan.Am J Infect Control.2005;33:489–492.
- ,,,.Prospective validation of a prediction model for isolating inpatients with suspected pulmonary tuberculosis.Arch Intern Med.2005;165:453–457.
- ,.The Hospital Infection Standardised Surveillance (HISS) programme: analysis of a two‐year pilot.J Hosp Infect.2003;53:259–267.
- ,,,.A Laboratory‐Based, Hospital‐Wide, Electronic Marker for Nosocomial Infection.Am J Clin Pathol.2006;125:34–39.
- ,,.Severe acute respiratory syndrome.Arch Pathol Lab Med.2004;128:1346–1350.
- ,,.Severe acute respiratory syndrome: responses of the healthcare system to a global epidemic.Curr Opin Otolaryngol Head Neck Surg.2005;13:161–164.
- ,.Pandemic influenza and the hospitalist: apocalypse when?J Hosp Med.2006;1:118–123.
- Center for Disease Control and Prevention. Pandemic Influenza information for Health Professionals. Available at: http://www.cdc.gov/flu/pandemic/. Accessed October 31,2006.
- .US health policy in the aftermath of Hurricane Katrina.JAMA.2006;295:437–40
- Levy B,Sidel V, eds.Terrorism and Public Health.New York:Oxford University Press;2003.
- Centers for Disease Control and Prevention (CDC).Public health response to Hurricanes Katrina and Rita—United States 2005.MMWR Morb Mortal Wkly Rep.2006;55:229–231.
- ,,,,,.Racial and ethnic disparities in health: a view from the South Bronx.J Health Care Poor Underserved.2006;17:116–127.
- ,.Williams E. Health Seeking behaviors of African Americans: implications for health administration.J Health Hum Serv Adm.2005;28(1):68–95.
- .Routine rapid HIV testing in hospitals: another opportunity for hospitalists to improve care.J Hosp Med.2006;1:106–112.
- Centers for Disease Control and Prevention.Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003.MMWR Morb Mortal Wkly Rep.2003;52:329–332.
- ,,, et al.Expanded screening for HIV in the United States—an analysis of cost‐effectiveness.N Engl J Med.2005;352:586–595.
- ,,,.Identifying undiagnosed human immunodeficiency virus: the yield for routine, voluntary, inpatient testing.Arch Intern Med.2002;162:887–892.
- ,,,,.Insufficient treatment of hypercholestrolemia among patients hospitalized with chest pain.Clin Cardiol.2006;29:259–262.
- .Medical management of alcoholic patients. In:Kissen B,Besleiter H, eds.Treatment and Rehabilitation of the Chronic Alcoholic.New York:Plenum Publishing Co.;1997.
- ,,.An integral approach to substance abuse.J Psychoactive Drugs.2005;37:363–371.
- ,,, et al.Smoking cessation practice among Norwegian hospital physicians.Tiddskr Nor laegeforen.2000;120:1629–1632.
- ,, et al.Evaluation of an intervention for hospitalized African American smokers.Am J Health Behav.2005;29:228–239.
- .Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs [review].J Am Geriatr Soc.2003;51:549–555.
- ,,,,.Advances in hospital medicine: a review of key articles from the literature.Med Clin N Am.2002;86:797–823.
- ,,,,,.Comprehensive discharge planning with post discharge support for older patients with congestive heart failure.JAMA.2004;291:1358–1367.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis.Med Care Res Rev.2005;62:379–406.
- ,,,,,Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists.Arch Intern Med.2002;162:1251–1256.
- ,,,.Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) colloquim, 2002.Lancet Infect Dis.2004;4:44–53.
- ,,, et al.Systematic review of antimicrobial drug prescribing in hospitals.Emerg Infect Dis.2006;12:211–216.
- ,,,,,,.Recommendations for management of community and hospital acquired pneumonia‐the hospitalist perspective.Curr Opin Pulm Med.2004;10(suppl 1):S23–S27.
- ,,,,.Advances in hospital medicine: a review of key articles from the literature.Med Clin N Am.2002;86:797–823.
- .End‐of‐life care for the hospitalized patient.Med Clin N Am.2002;86:749–770.
- ,.Palliative care for patients with heart failure.JAMA.2004;291:2476–2482.
- ,.Prevalence and structure of palliative care services in California hospitals.Arch Intern Med.2003;163:1084–1088.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.J Med.2001;111:10S–14S.
- .Palliative care in hospitals.J Hosp Med.2006;1:21–28.
- ,.End‐of‐life care in a voluntary hospitalist model: effects on communication, process of care, and patient symptoms.Am J Med.2004;116:669–675.
- ,,,Understanding medical error and improving patient safety in the inpatient setting,Med Clin N Am2002;86:847–867.
- , The hospitalist movement: ten issues to consider, hospital practice. Available at: http://www.hosppract.com/issues/1999/02/wachter.htm. Accessed March 14,2006.
- Shojania KG,Duncan BW,McDonald KM,Wachter RM, eds.Making health care safer: a critical analysis of patient safety practices. Evidence Report/Technology Assessment No. 43 from the Agency for Healthcare Research and Quality: AHRQ Publication No. 01‐E058;2001. Available at: http://www.ahrq.gov/clinic/ptsafety/.
- ,,,.Safe but sound: patient safety meets evidence‐based medicine.JAMA.2002;288:508–513.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- Hospitalists, pharmacists partner to cut errors: shorter lengths of stay, lower med costs result. HealthCare Benchmarks and Quality Improvement.American Health Consultants, Inc.,2005.
- ,,,.Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians.Ann Intern Med.1999;130:343–349.
- ,,,,.Core competencies in hospital medicine: Development and methodology.J Hosp Med.2006;1:48–56.
- National guideline clearing house. Available at: http://www.guideline.gov. Accessed June 26,2006.
- ,,,,, eds.The core competencies in hospital medicine.J Hosp Med.2006;1(suppl 1).
- Joint Commission on Accreditation of Healthcare Organizations. Core Measures overview. Available at: http://www.jcaho.org/perfeas/coremeas/cm.ovrvw.html. Accessed February 1,2006.
- ,,,.,Comparison of processes and outcomes of pneumonia care between hospitalists and community‐based primary care physicians.Mayo Clin Proc.2002;77:1053–1058.
- ,.The effectiveness of a nursing inpatient smoking cessation program in individuals with cardiovascular disease.Nurs Res.2005;54:243–254.
- ,,,,,.Evaluation of an intervention for hospitalized African American smokers.Am J Health Behav.2005;29:228–239.
- .Smoking cessation: the case for hospital‐based interventions.Prof Nurse.2003;19(3):145–148..
- . Dee Hock's management principles, in his own words. Fast Company.1996;5:79. Available at: http://www.fastcompany.com/magazine/05/dee2.html.
- ,,,.Hospital Medicine Fellowships: Works in progress.Am J Med.2006;119(1):72.e1–e7.
- ,.The Hospitalist movement 5 years later.JAMA.2002;287:487–494.
- Hospitals and Health Networks. Hospitalists: a specialty coming into its own. Available at: http://www.hhmag.com. Accessed February 27,2006.
- ,,.Emergency medicine and public health: new steps in old directions.Ann Emerg Med.2001;38:675–683.
- ,, et al.A public health approach to emergency medicine: preparing for the twenty‐first century.Acad Emerg Med.1994;1:277–286.
- ,.Emergency medicine in population‐based systems of care.Ann Emerg Med.1997;30:800–803.
- ,.Principles of Public Health Practice.Albany, NY:Delmar Publishing;1997.
- Centers for Medicare and Medicaid. Health care spending and growth rate continue to decline in 2004. Available at: http://www.cms.hhs.gov. Accessed October 31,2006.
- ,,, et al.National health expenditures, 2002.Health Care Financ Rev. Summer2004;25:4.
- ,,, et al.Health spending Projections Through 2015: Changes on the Horizon.Health Affairs2006;25:w61–w73.
- Institute of Medicine.Recommendations from the Future of Public Health. InThe Future of the Public's Health.Washington, DC:National Academic Press;2003:411–420.
- ,,.Nosocomial pneumonia: state of the science.Am J Infect Control.2006;34:84–93.
- ,,,,.A reminder reduces urinary catheterization in hospitalized patients.Jt Comm J Qual Patient Saf.2005;31:455–462.
- ,,,.Preventing infections in nursing homes: A survey of infection control practices in southeast Michigan.Am J Infect Control.2005;33:489–492.
- ,,,.Prospective validation of a prediction model for isolating inpatients with suspected pulmonary tuberculosis.Arch Intern Med.2005;165:453–457.
- ,.The Hospital Infection Standardised Surveillance (HISS) programme: analysis of a two‐year pilot.J Hosp Infect.2003;53:259–267.
- ,,,.A Laboratory‐Based, Hospital‐Wide, Electronic Marker for Nosocomial Infection.Am J Clin Pathol.2006;125:34–39.
- ,,.Severe acute respiratory syndrome.Arch Pathol Lab Med.2004;128:1346–1350.
- ,,.Severe acute respiratory syndrome: responses of the healthcare system to a global epidemic.Curr Opin Otolaryngol Head Neck Surg.2005;13:161–164.
- ,.Pandemic influenza and the hospitalist: apocalypse when?J Hosp Med.2006;1:118–123.
- Center for Disease Control and Prevention. Pandemic Influenza information for Health Professionals. Available at: http://www.cdc.gov/flu/pandemic/. Accessed October 31,2006.
- .US health policy in the aftermath of Hurricane Katrina.JAMA.2006;295:437–40
- Levy B,Sidel V, eds.Terrorism and Public Health.New York:Oxford University Press;2003.
- Centers for Disease Control and Prevention (CDC).Public health response to Hurricanes Katrina and Rita—United States 2005.MMWR Morb Mortal Wkly Rep.2006;55:229–231.
- ,,,,,.Racial and ethnic disparities in health: a view from the South Bronx.J Health Care Poor Underserved.2006;17:116–127.
- ,.Williams E. Health Seeking behaviors of African Americans: implications for health administration.J Health Hum Serv Adm.2005;28(1):68–95.
- .Routine rapid HIV testing in hospitals: another opportunity for hospitalists to improve care.J Hosp Med.2006;1:106–112.
- Centers for Disease Control and Prevention.Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003.MMWR Morb Mortal Wkly Rep.2003;52:329–332.
- ,,, et al.Expanded screening for HIV in the United States—an analysis of cost‐effectiveness.N Engl J Med.2005;352:586–595.
- ,,,.Identifying undiagnosed human immunodeficiency virus: the yield for routine, voluntary, inpatient testing.Arch Intern Med.2002;162:887–892.
- ,,,,.Insufficient treatment of hypercholestrolemia among patients hospitalized with chest pain.Clin Cardiol.2006;29:259–262.
- .Medical management of alcoholic patients. In:Kissen B,Besleiter H, eds.Treatment and Rehabilitation of the Chronic Alcoholic.New York:Plenum Publishing Co.;1997.
- ,,.An integral approach to substance abuse.J Psychoactive Drugs.2005;37:363–371.
- ,,, et al.Smoking cessation practice among Norwegian hospital physicians.Tiddskr Nor laegeforen.2000;120:1629–1632.
- ,, et al.Evaluation of an intervention for hospitalized African American smokers.Am J Health Behav.2005;29:228–239.
- .Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs [review].J Am Geriatr Soc.2003;51:549–555.
- ,,,,.Advances in hospital medicine: a review of key articles from the literature.Med Clin N Am.2002;86:797–823.
- ,,,,,.Comprehensive discharge planning with post discharge support for older patients with congestive heart failure.JAMA.2004;291:1358–1367.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis.Med Care Res Rev.2005;62:379–406.
- ,,,,,Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists.Arch Intern Med.2002;162:1251–1256.
- ,,,.Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) colloquim, 2002.Lancet Infect Dis.2004;4:44–53.
- ,,, et al.Systematic review of antimicrobial drug prescribing in hospitals.Emerg Infect Dis.2006;12:211–216.
- ,,,,,,.Recommendations for management of community and hospital acquired pneumonia‐the hospitalist perspective.Curr Opin Pulm Med.2004;10(suppl 1):S23–S27.
- ,,,,.Advances in hospital medicine: a review of key articles from the literature.Med Clin N Am.2002;86:797–823.
- .End‐of‐life care for the hospitalized patient.Med Clin N Am.2002;86:749–770.
- ,.Palliative care for patients with heart failure.JAMA.2004;291:2476–2482.
- ,.Prevalence and structure of palliative care services in California hospitals.Arch Intern Med.2003;163:1084–1088.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.J Med.2001;111:10S–14S.
- .Palliative care in hospitals.J Hosp Med.2006;1:21–28.
- ,.End‐of‐life care in a voluntary hospitalist model: effects on communication, process of care, and patient symptoms.Am J Med.2004;116:669–675.
- ,,,Understanding medical error and improving patient safety in the inpatient setting,Med Clin N Am2002;86:847–867.
- , The hospitalist movement: ten issues to consider, hospital practice. Available at: http://www.hosppract.com/issues/1999/02/wachter.htm. Accessed March 14,2006.
- Shojania KG,Duncan BW,McDonald KM,Wachter RM, eds.Making health care safer: a critical analysis of patient safety practices. Evidence Report/Technology Assessment No. 43 from the Agency for Healthcare Research and Quality: AHRQ Publication No. 01‐E058;2001. Available at: http://www.ahrq.gov/clinic/ptsafety/.
- ,,,.Safe but sound: patient safety meets evidence‐based medicine.JAMA.2002;288:508–513.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- Hospitalists, pharmacists partner to cut errors: shorter lengths of stay, lower med costs result. HealthCare Benchmarks and Quality Improvement.American Health Consultants, Inc.,2005.
- ,,,.Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians.Ann Intern Med.1999;130:343–349.
- ,,,,.Core competencies in hospital medicine: Development and methodology.J Hosp Med.2006;1:48–56.
- National guideline clearing house. Available at: http://www.guideline.gov. Accessed June 26,2006.
- ,,,,, eds.The core competencies in hospital medicine.J Hosp Med.2006;1(suppl 1).
- Joint Commission on Accreditation of Healthcare Organizations. Core Measures overview. Available at: http://www.jcaho.org/perfeas/coremeas/cm.ovrvw.html. Accessed February 1,2006.
- ,,,.,Comparison of processes and outcomes of pneumonia care between hospitalists and community‐based primary care physicians.Mayo Clin Proc.2002;77:1053–1058.
- ,.The effectiveness of a nursing inpatient smoking cessation program in individuals with cardiovascular disease.Nurs Res.2005;54:243–254.
- ,,,,,.Evaluation of an intervention for hospitalized African American smokers.Am J Health Behav.2005;29:228–239.
- .Smoking cessation: the case for hospital‐based interventions.Prof Nurse.2003;19(3):145–148..
- . Dee Hock's management principles, in his own words. Fast Company.1996;5:79. Available at: http://www.fastcompany.com/magazine/05/dee2.html.
- ,,,.Hospital Medicine Fellowships: Works in progress.Am J Med.2006;119(1):72.e1–e7.
Copyright © 2007 Society of Hospital Medicine