User login
Introducing the Hospitalist Morale Index
Explosive growth in hospital medicine has led to hospitalists having the option to change jobs easily. Annual turnover for all physicians is 6.8%, whereas that of hospitalists exceeds 14.8%.[1] Losing a single physician has significant financial and operational implications, with estimates of $20,000 to $120,000 in recruiting costs, and up to $500,000 in lost revenue that may take years to recoup due to the time required for new physician assimilation.[2, 3] In 2006, the Society of Hospital Medicine (SHM) appointed a career task force to develop retention recommendations, 1 of which includes monitoring hospitalists' job satisfaction.[4]
Studies examining physician satisfaction have demonstrated that high physician job satisfaction is associated with lower physician turnover.[5] However, surveys of hospitalists, including SHM's Hospital Medicine Physician Worklife Survey (HMPWS), have reported high job satisfaction among hospitalists,[6, 7, 8, 9, 10] suggesting that high job satisfaction may not be enough to overcome forces that pull hospitalists toward other opportunities.
Morale, a more complex construct related to an individual's contentment and happiness, might provide insight into reducing hospitalist turnover. Morale has been defined as the emotional or mental condition with respect to cheerfulness, confidence, or zeal and is especially relevant in the face of opposition or hardship.[11] Job satisfaction is 1 element that contributes to morale, but alone does not equate morale.[12] Morale, more than satisfaction, relates to how people see themselves within the group and may be closely tied to the concept of esprit de corps. To illustrate, workers may feel satisfied with the content of their job, but frustration with the organization may result in low morale.[13] Efforts focused on assessing provider morale may provide deeper understanding of hospitalists' professional needs and garner insight for retention strategies.
The construct of hospitalist morale and its underlying drivers has not been explored in the literature. Using literature within and outside of healthcare,[1, 12, 14, 15, 16, 17, 18, 19, 20, 21, 22] and our own prior work,[23] we sought to characterize elements that contribute to hospitalist morale and develop a metric to measure it. The HMPWS found that job satisfaction factors vary across hospitalist groups.[9] We suspected that the same would hold true for factors important to morale at the individual level. This study describes the development and validation of the Hospitalist Morale Index (HMI), and explores the relationship between morale and intent to leave due to unhappiness.
METHODS
2009 Pilot Survey
To establish content validity, after reviewing employee morale literature, and examining qualitative comments from our 2007 and 2008 morale surveys, our expert panel, consisting of practicing hospitalists, hospitalist leaders, and administrative staff, identified 46 potential drivers of hospitalist morale. In May 2009, all hospitalists, including physicians, nurse practitioners (NPs), and physician assistants (PAs) from a single hospitalist group received invitations to complete the pilot survey. We asked hospitalists to assess on 5‐point Likert scales the importance of (not at all to tremendously) and contentment with (extremely discontent to extremely content) each of the 46 items as it relates to their work morale. Also included were demographic questions and general morale questions (including rating participants' own morale), investment, long‐term career plans, and intent to leave due to unhappiness.
Data Collection
To maintain anonymity and limit social desirability bias, a database manager, working outside the Division of Hospital Medicine and otherwise not associated with the research team, used Survey Monkey to coordinate survey distribution and data collection. Each respondent had a unique identifier code that was unrelated to the respondent's name and email address. Personal identifiers were maintained in a secure database accessible only to the database manager.
Establishing Internal Structure Validity Evidence
Response frequency to each question was examined for irregularities in distribution. For continuous variables, descriptive statistics were examined for evidence of skewness, outliers, and non‐normality to ensure appropriate use of parametric statistical tests. Upon ranking importance ratings by mode, 15 of 46 items were judged to be of low importance by almost all participants and removed from further consideration.
Stata 13.1 (StataCorp, College Station, TX) was used for exploratory factor analysis (EFA) of the importance responses for all 31 remaining items by principal components factoring. Eigenvalues >1 were designated as a cutoff point for inclusion in varimax rotation. Factor loading of 0.50 was the threshold for inclusion in a factor.
The 31 items loaded across 10 factors; however, 3 factors included 1 item each. After reviewing the scree plot and considering their face value, these items/factors were omitted. Repeating the factor analysis resulted in a 28‐item, 7‐factor solution that accounted for 75% variance. All items were considered informative as demonstrated by low uniqueness scores (0.050.38). Using standard validation procedures, all 7 factors were found to have acceptable factor loadings (0.460.98) and face validity. Cronbach's quantified internal reliability of the 7 factors with scores ranging from 0.68 to 0.92. We named the resultant solution the Hospitalist Morale Index (HMI).
Establishing Response Process Validity Evidence
In developing the HMI, we asked respondents to rate the importance of and their contentment with each variable as related to their work morale. From pilot testing, which included discussions with respondents immediately after completing the survey, we learned that the 2‐part consideration of each variable resulted in thoughtful reflection about their morale. Further, by multiplying the contentment score for each item (scaled from 15) by the corresponding importance score (scaled 01), we quantified the relative contribution and contentment of each item for each hospitalist. Scaling importance scores from 0 to 1 insured that items that were not considered important to the respondent did not affect the respondent's personal morale score. Averaging resultant item scores that were greater than 0 resulted in a personal morale score for each hospitalist. Averaging item scores >0 that constituted each factor resulted in factor scores.
May 2011 Survey
The refined survey was distributed in May 2011 to a convenience sample of 5 hospitalist programs at separate hospitals (3 community hospitals, 2 academic hospitals) encompassing 108 hospitalists in 3 different states. Responses to the 2011 survey were used to complete confirmatory factor analyses (CFA) and establish further validity and reliability evidence.
Based on the 28‐item, 7‐factor solution developed from the pilot study, we developed the theoretical model of factors constituting hospitalist morale. We used the structural equation modeling command in Stata 13 to perform CFA. Factor loading of 0.50 was the threshold for inclusion of an item in a factor. To measure internal consistency, we considered Cronbach's score of 0.60 acceptable. Iterative models were reviewed to find the optimal solution for the data. Four items did not fit into any of the 5 resulting factors and were evaluated in terms of mean importance score and face value. Three items were considered important enough to warrant being stand‐alone items, whereas 1 was omitted. Two additional items had borderline factor loadings (0.48, 0.49) and were included in the model as stand‐alone items due to their overall relevance. The resultant solution was a 5‐factor model with 5 additional stand‐alone items (Table 1).
| Factor | Cronbach's | |||||
|---|---|---|---|---|---|---|
| Clinical | Workload | Leadership | Appreciation and Acknowledgement | Material Rewards | ||
| How much does the following item contribute to your morale? | ||||||
| Paperwork | 0.72 | 0.89 | ||||
| Relationship with patients | 0.69 | 0.90 | ||||
| Electronic medical system | 0.60 | 0.90 | ||||
| Intellectual stimulation | 0.59 | 0.90 | ||||
| Variety of cases | 0.58 | 0.90 | ||||
| Relationship with consultants | 0.51 | 0.89 | ||||
| No. of night shifts | 0.74 | 0.89 | ||||
| Patient census | 0.61 | 0.90 | ||||
| No. of shifts | 0.52 | 0.90 | ||||
| Fairness of leadership | 0.82 | 0.89 | ||||
| Effectiveness of leadership | 0.82 | 0.89 | ||||
| Leadership's receptiveness to my thoughts and suggestions | 0.78 | 0.89 | ||||
| Leadership as advocate for my needs | 0.77 | 0.89 | ||||
| Approachability of leadership | 0.77 | 0.89 | ||||
| Accessibility of leadership | 0.69 | 0.89 | ||||
| Alignment of the group's goals with my goals | 0.50 | 0.89 | ||||
| Recognition within the group | 0.82 | 0.89 | ||||
| Feeling valued within the institution | 0.73 | 0.89 | ||||
| Feeling valued within the group | 0.73 | 0.89 | ||||
| Feedback | 0.52 | 0.89 | ||||
| Pay | 0.99 | 0.90 | ||||
| Benefits | 0.56 | 0.89 | ||||
| Cronbach's | 0.78 | 0.65 | 0.89 | 0.78 | 0.71 | |
| How much does the following item contribute to your morale? | Single item indicators | |||||
| Family time | 0.90 | |||||
| Job security | 0.90 | |||||
| Institutional climate | 0.89 | |||||
| Opportunities for professional growth | 0.90 | |||||
| Autonomy | 0.89 | |||||
| Cronbach's | 0.90 | |||||
Establishing Convergent, Concurrent, and Discriminant Validity Evidence
To establish convergent, concurrent, and discriminant validity, linear and logistic regression models were examined for continuous and categorical data accordingly.
Self‐perceived overall work morale and perceived group morale, as assessed by 6‐point Likert questions with response options from terrible to excellent, were modeled as predictors for personal morale as calculated by the HMI.
Personal morale scores were modeled as predictors of professional growth, stress, investment in the group, and intent to leave due to unhappiness. While completing the HMI, hospitalists simultaneously completed a validated professional growth scale[24] and Cohen stress scale.[25] We hypothesized that those with higher morale would have more professional growth. Stress, although an important issue in the workplace, is a distinct construct from morale, and we did not expect a significant relationship between personal morale and stress. We used Pearson's r to assess the strength of association between the HMI and these scales. Participants' level of investment in their group was assessed on a 5‐point Likert scale. To simplify presentation, highly invested represents those claiming to be very or tremendously invested in the success of their current hospitalist group. Intent to leave due to unhappiness was assessed on a 5‐point Likert scale, I have had serious thoughts about leaving my current hospitalist group because I am unhappy, with responses from strongly disagree (1) to strongly agree (5). To simplify presentation, responses higher than 2 are considered to be consistent with intending to leave due to unhappiness.
Our institutional review board approved the study.
RESULTS
Respondents
In May 2009, 30 of the 33 (91%) invited hospitalists completed the original pilot morale survey; 19 (63%) were women. Eleven hospitalists (37%) had been part of the group 1 year or less, whereas 4 (13%) had been with the group for more than 5 years.
In May 2011, 93 of the 108 (86%) hospitalists from 5 hospitals completed the demographic and global parts of the survey. Fifty (53%) were from community hospitals; 47 (51%) were women. Thirty‐seven (40%) physicians and 6 (60%) NPs/PAs were from academic hospitals. Thirty‐nine hospitalists (42%) had been with their current group 1 year or less. Ten hospitalists (11%) had been with their current group over 5 years. Sixty‐three respondents (68%) considered themselves career hospitalists, whereas 5 (5%) did not; the rest were undecided.
Internal Structure Validity Evidence
The final CFA from the 2011 survey resulted in a 5‐factor plus 5stand‐alone‐items HMI. The solution with item‐level and factor‐level Cronbach's scores (range, 0.890.90 and range, 0.650.89, respectively) are shown in Table 1.
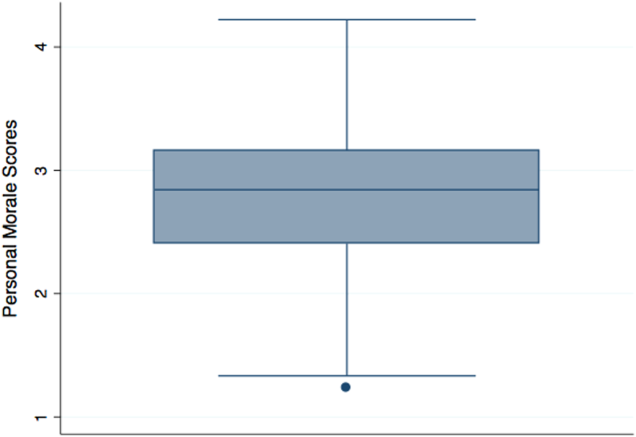
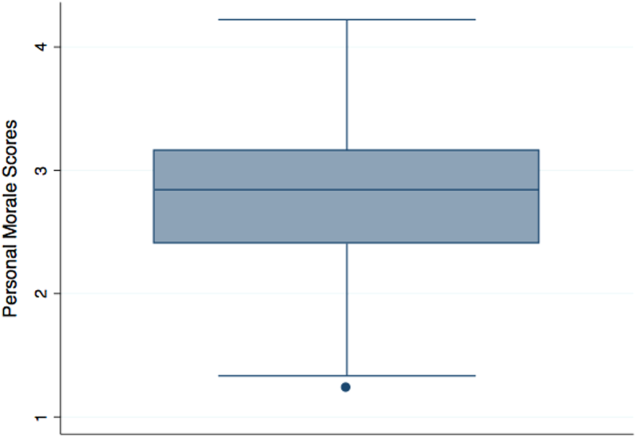
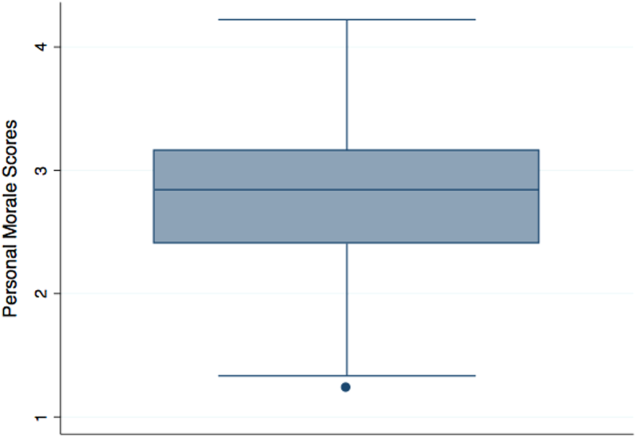
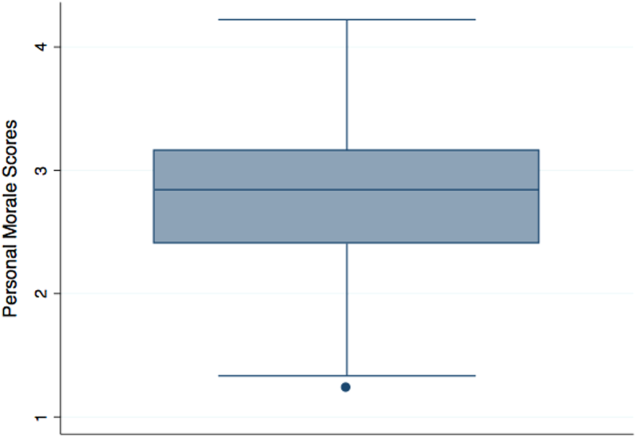
Personal Morale Scores and Factor Scores
Personal morale scores were normally distributed (mean = 2.79; standard deviation [SD] = 0.58), ranging from 1.23 to 4.22, with a theoretical low of 0 and high of 5 (Figure 1). Mean personal morale scores across hospitalist groups ranged from 2.70 to 2.99 (P > 0.05). Personal morale scores, factor sores and item scores for NPs and PAs did not significantly differ from those of physicians (P > 0.05 for all analyses). Personal morale scores were lower for those in their first 3 years with their current group, compared to those with greater institutional longevity. For every categorical increase in a participant's response to seeing oneself as a career hospitalist, the personal morale score rose 0.23 points (P < 0.001).
Factor scores for material reward and mean item scores for professional growth were significantly different across the 5 hospitalist groups (P = 0.03 and P < 0.001, respectively). Community hospitalists had significantly higher factor scores, despite having similar importance scores, for material rewards than academic hospitalists (diff. = 0.44, P = 0.02). Academic hospitalists had significantly higher scores for professional growth (diff. = 0.94, P < 0.001) (Table 2). Professional growth had the highest importance score for academic hospitalists (mean = 0.87, SD = 0.18) and the lowest importance score for community hospitalists (mean = 0.65, SD = 0.24, P < 0.001).
| Personal Morale Score | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical | Workload | Leadership | Appreciation and Acknowledgement | Material Rewards | Family Time | Institutional Climate | Job Security | Autonomy | Professional Growth | |||
| ||||||||||||
| All participants | Mean | 2.79 | 2.54 | 2.78 | 3.18 | 2.58 | 2.48 | 3.05 | 2.67 | 2.92 | 3.00 | 2.76 |
| SD | 0.58 | 0.63 | 0.70 | 0.95 | 0.86 | 0.85 | 1.15 | 0.97 | 1.11 | 1.10 | 1.21 | |
| Academic A | Mean | 2.77 | 2.43 | 2.92 | 3.10 | 2.54 | 2.28 | 3.16 | 2.70 | 3.06 | 3.20 | 3.08 |
| SD | 0.57 | 0.62 | 0.64 | 0.92 | 0.84 | 0.77 | 1.19 | 0.95 | 1.08 | 1.12 | 1.24 | |
| Academic B | Mean | 2.99 | 2.58 | 2.99 | 3.88 | 2.69 | 2.00 | 2.58 | 2.13 | 1.65 | 3.29 | 4.33 |
| SD | 0.36 | 0.70 | 0.80 | 0.29 | 0.80 | 0.35 | 0.92 | 0.88 | 0.78 | 1.01 | 0.82 | |
| Community A | Mean | 2.86 | 2.61 | 2.51 | 3.23 | 2.73 | 3.03 | 2.88 | 2.84 | 2.95 | 3.23 | 2.66 |
| SD | 0.75 | 0.79 | 0.68 | 1.21 | 1.11 | 1.14 | 1.37 | 1.17 | 0.98 | 1.24 | 1.15 | |
| Community B | Mean | 2.86 | 2.74 | 2.97 | 3.37 | 2.67 | 2.44 | 3.28 | 2.35 | 2.70 | 2.50 | 2.25 |
| SD | 0.67 | 0.55 | 0.86 | 1.04 | 0.94 | 0.87 | 1.00 | 1.15 | 1.40 | 0.72 | 1.26 | |
| Community C | Mean | 2.70 | 2.56 | 2.64 | 2.99 | 2.47 | 2.53 | 3.03 | 2.79 | 3.07 | 2.68 | 2.15 |
| SD | 0.49 | 0.53 | 0.67 | 0.85 | 0.73 | 0.64 | 1.08 | 0.76 | 1.05 | 1.07 | 0.71 | |
| Academic combined | Mean | 2.80 | 2.45 | 2.93 | 3.22 | 2.56 | 2.24 | 3.07 | 2.62 | 2.88 | 3.21 | 3.28 |
| SD | 0.54 | 0.63 | 0.66 | 0.89 | 0.82 | 0.72 | 1.16 | 0.95 | 1.14 | 1.10 | 1.26 | |
| Community combined | Mean | 2.79 | 2.61 | 2.66 | 3.14 | 2.60 | 2.68 | 3.03 | 2.72 | 2.95 | 2.82 | 2.34 |
| SD | 0.62 | 0.62 | 0.72 | 1.01 | 0.90 | 0.90 | 1.15 | 0.99 | 1.09 | 1.09 | 1.00 | |
| P value | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | 0.02 | >0.05 | >0.05 | >0.05 | >0.05 | <0.001 | |
Convergent, Concurrent, and Discriminant Validity Evidence
For every categorical increase on the question assessing overall morale, the personal morale score was 0.23 points higher (P < 0.001). For every categorical increase in a participant's perception of the group's morale, the personal morale score was 0.29 points higher (P < 0.001).
For every 1‐point increase in personal morale score, the odds of being highly invested in the group increased by 5 times (odds ratio [OR]: 5.23, 95% confidence interval [CI]: 1.91‐14.35, P = 0.001). The mean personal morale score for highly invested hospitalists was 2.92, whereas that of those less invested was 2.43 (diff. = 0.49, P < 0.001) (Table 3). Highly invested hospitalists had significantly higher importance factor scores for leadership (diff. = 0.08, P = 0.03) as well as appreciation and acknowledgement (diff. = 0.08, P = 0.02).
| Personal Morale Score | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical | Workload | Leadership | Appreciation and Acknowledgement | Material Rewards | Family Time | Institutional Climate | Job Security | Autonomy | Professional Growth | ||
| |||||||||||
| Highly invested in success of current hospitalist group | |||||||||||
| Mean | 2.92 | 2.61 | 2.89 | 3.38 | 2.78 | 2.45 | 3.21 | 2.78 | 2.86 | 3.10 | 2.95 |
| SD | 0.55 | 0.59 | 0.68 | 0.92 | 0.88 | 0.77 | 1.11 | 1.00 | 1.09 | 1.06 | 1.25 |
| Less invested in success of current hospitalist group | |||||||||||
| Mean | 2.43 | 2.34 | 2.48 | 2.60 | 2.02 | 2.57 | 2.60 | 2.38 | 3.08 | 2.69 | 2.24 |
| SD | 0.52 | 0.69 | 0.69 | 0.81 | 0.49 | 1.04 | 1.17 | 0.83 | 1.18 | 1.19 | 0.94 |
| P value | <0.001 | >0.05 | 0.02 | 0.001 | <0.001 | >0.05 | 0.03 | >0.05 | >0.05 | >0.05 | 0.02 |
| Not intending to leave because unhappy | |||||||||||
| Mean | 2.97 | 2.67 | 2.89 | 3.48 | 2.77 | 2.52 | 3.24 | 2.85 | 3.05 | 3.06 | 3.01 |
| SD | 0.51 | 0.54 | 0.61 | 0.91 | 0.89 | 0.78 | 1.03 | 0.99 | 1.10 | 1.07 | 1.25 |
| Intending to leave current group because unhappy | |||||||||||
| Mean | 2.45 | 2.30 | 2.59 | 2.59 | 2.21 | 2.40 | 2.68 | 2.33 | 2.67 | 2.88 | 2.28 |
| SD | 0.56 | 0.72 | 0.82 | 0.74 | 0.68 | 0.97 | 1.29 | 0.83 | 1.11 | 1.17 | 0.97 |
| P value | <0.001 | 0.01 | >0.05 | <0.001 | 0.003 | >0.05 | 0.03 | 0.01 | >0.05 | >0.05 | 0.01 |
Every 1‐point increase in personal morale was associated with a rise of 2.27 on the professional growth scale (P = 0.01). The correlation between these 2 scales was 0.26 (P = 0.01). Every 1‐point increase in personal morale was associated with a 2.21 point decrease on the Cohen stress scale (P > 0.05). The correlation between these 2 scales was 0.21 (P > 0.05).
Morale and Intent to Leave Due to Unhappiness
Sixteen (37%) academic and 18 (36%) community hospitalists reported having thoughts of leaving their current hospitalist program due to unhappiness. The mean personal morale score for hospitalists with no intent to leave their current group was 2.97, whereas that of those with intent to leave was 2.45 (diff. = 0.53, P < 0.001). Each 1‐point increase in the personal morale score was associated with an 85% decrease (OR: 0.15, 95% CI: 0.05‐0.41, P < 0.001) in the odds of leaving because of unhappiness. Holding self‐perception of being a career hospitalist constant, each 1‐point increase in the personal morale score was associated with an 83% decrease (OR: 0.17, 95% CI: 0.05‐0.51, P = 0.002) in the odds of leaving because of unhappiness. Hospitalists who reported intent to leave had significantly lower factor scores for all factors and items except workload, material reward, and autonomy than those who did not report intent to leave (Table 3). Within the academic groups, those who reported intent to leave had significantly lower scores for professional growth (diff. = 1.08, P = 0.01). For community groups, those who reported intent to leave had significantly lower scores for clinical work (diff. = 0.54, P = 0.003), workload (diff. = 0.50, P = 0.02), leadership (diff. = 1.19, P < 0.001), feeling appreciated and acknowledged (diff. = 0.68, P = 0.01), job security (diff. = 0.70, P = 0.03), and institutional climate (diff. = 0.67, P = 0.02) than those who did not report intent to leave.
DISCUSSION
The HMI is a validated tool that objectively measures and quantifies hospitalist morale. The HMI's capacity to comprehensively assess morale comes from its breadth and depth in uncovering work‐related areas that may be sources of contentment or displeasure. Furthermore, the fact that HMI scores varied among groups of individuals, including those who are thinking about leaving their hospitalist group because they are unhappy and those who are highly invested in their hospitalist group, speaks to its ability to highlight and account for what is most important to hospitalist providers.
Low employee morale has been associated with decreased productivity, increased absenteeism, increased turnover, and decreased patient satisfaction.[2, 26, 27, 28] A few frustrated workers can breed group discontentment and lower the entire group's morale.[28] In addition to its financial impact, departures due to low morale can be sudden and devastating, leading to loss of team cohesiveness, increased work burden on the remaining workforce, burnout, and cascades of more turnover.[2] In contrast, when morale is high, workers more commonly go the extra mile, are more committed to the organization's mission, and are more supportive of their coworkers.[28]
While we asked the informants about plans to leave their job, there are many factors that drive an individual's intent and ultimate decision to make changes in his or her employment. Some factors are outside the control of the employer or practice leaders, such as change in an individual's family life or desire and opportunity to pursue fellowship training. Others variables, however, are more directly tied to the job or practice environment. In a specialty where providers are relatively mobile and turnover is high, it is important for hospitalist practices to cultivate a climate in which the sacrifices associated with leaving outweigh the promised benefits.[29]
Results from the HMPWS suggested the need to address climate and fairness issues in hospitalist programs to improve satisfaction and retention.[9] Two large healthcare systems achieved success by investing in multipronged physician retention strategies including recruiting advisors, sign‐on bonuses, extensive onboarding, family support, and the promotion of ongoing effective communication.[3, 30]
Our findings suggest that morale for hospitalists is a complex amalgam of contentment and importance, and that there may not be a one size fits all solution to improving morale for all. While we did not find a difference in personal morale scores across individual hospitalist groups, or even between academic and community groups, each group had a unique profile with variability in the dynamics between importance and contentment of different factors. If practice group leaders review HMI data for their providers and use the information to facilitate meaningful dialogue with them about the factors influencing their morale, such leaders will have great insight into allocating resources for the best return on investment.
While we believe that the HMI is providing unique perspective compared to other commonly used metrics, it may be best to employ HMI data as complementary measures alongside that of some of the benchmarked scales that explore job satisfaction, job fit, and burnout among hospitalists.[6, 9, 10, 31, 32, 33, 34, 35] Aggregate HMI data at the group level may allow for the identification of factors that are highly important to morale but scored low in contentment. Such factors deserve priority and attention such that the subgroups within a practice can collaborate to come to consensus on strategies for amelioration. Because the HMI generates a score and profile for each provider, we can imagine effective leaders using the HMI with individuals as part of an annual review to facilitate discussion about maximizing contentment at work. Being fully transparent and sharing an honest nonanonymous version of the HMI with a superior would require a special relationship founded on trust and mutual respect.
Several limitations of this study should be considered. First, the initial item reduction and EFA were based on a single‐site survey, and our overall sample size was relatively small. We plan on expanding our sample size in the future for further validation of our exploratory findings. Second, the data were collected at 2 specific times several years ago. In continuing to analyze the data from subsequent years, validity and reliability results remain stable, thereby minimizing the likelihood of significant historical bias. Third, there may have been some recall bias, in that respondents may have overlooked the good and perseverated over variables that disappointed them. Fourth, although intention to leave does not necessarily equate actual employee turnover, intention has been found to be a strong predictor of quitting a job.[36, 37] Finally, while we had high response rates, response bias may have existed wherein those with lower morale may have elected not to complete the survey or became apathetic in their responses.
The HMI is a validated instrument that evaluates hospitalist morale by incorporating each provider's characterization of the importance of and contentment with 27 variables. By accounting for the multidimensional and dynamic nature of morale, the HMI may help program leaders tailor retention and engagement strategies specific to their own group. Future studies may explore trends in contributors to morale and examine whether interventions to augment low morale can result in improved morale and hospitalist retention.
Acknowledgements
The authors are indebted to the hospitalists who were willing to share their perspectives about their work, and grateful to Ms. Lisa Roberts, Ms. Barbara Brigade, and Ms. Regina Landis for insuring confidentiality in managing the survey database.
Disclosures: Dr. Chandra had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Wright is a Miller‐Coulson Family Scholar through the Johns Hopkins Center for Innovative Medicine. Ethical approval has been granted for studies involving human subjects by a Johns Hopkins University School of Medicine institutional review board. The authors report no conflicts of interest.
- 2014 State of Hospital Medicine Report. Philadelphia, PA: Society of Hospital Medicine; 2014.
- , , . A review of physician turnover: rates, causes, and consequences. Am J Med Qual. 2004;19(2):56–66.
- . Physician retention plans help reduce costs and optimize revenues. Healthc Financ Manage. 1998;52(1):75–77.
- SHM Career Satisfaction Task Force. A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction.; 2006. Available at: www.hospitalmedicine.org. Accessed February 28, 2009.
- , . Outcomes of physician job satisfaction: a narrative review, implications, and directions for future research. Health Care Manage Rev. 2003;28(2):119–139.
- , , , , . Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851–858.
- . Doing the same and earning less: male and female physicians in a new medical specialty. Inquiry. 2004;41(3):301–315.
- . Physician satisfaction and communication. National findings and best practices. Available at: http://www.pressganey.com/files/clark_cox_acpe_apr06.pdf. Accessed October 10, 2010.
- , , , , . Worklife and satisfaction of hospitalists: toward flourishing careers. J Gen Intern Med. 2012;27(1):28–36.
- , , , , ; Society of Hospital Medicine Career Satisfaction Task Force. Job characteristics, satisfaction, and burnout across hospitalist practice models. J Hosp Med. 2012;7(5):402–410.
- Morale | Define Morale at Dictionary.com. Morale | Define Morale at Dictionary.com. Morale | Define Morale at Dictionary.com. Available at: http://dictionary.reference.com/browse/morale. Accessed June 5, 2014.
- . Morale and satisfaction: a study in past‐future time perspective. Adm Sci Q. 1958:195–209.
- . Men and Women of the Corporation. 2nd ed. New York, NY: Basic Books; 1993.
- . The relation of morale to turnover among teachers. Am Educ Res J. 1965:163–173.
- . Structural and individual determinants of organization morale and satisfaction. Soc Forces. 1982;61:1088.
- , , . Morale matters: midlevel administrators and their intent to leave. J Higher Educ. 2000:34–59.
- . Factors influencing employee morale. Harv Bus Rev. 1950;28(1):61–73.
- . Dimensions of teacher morale. Am Educ Res J. 1970;7(2):221.
- , . The definition and measurement of employee morale. Adm Sci Q. 1958:157–184.
- , , , et al. Measuring physician job satisfaction in a changing workplace and a challenging environment. SGIM Career Satisfaction Study Group. Society of General Internal Medicine. Med Care. 1999;37(11):1174–1182.
- . Structural and individual determinants of organization morale and satisfaction. Soc Forces. 1983;61(4):1088–1108.
- . Morale and its measurement. Am J Sociol. 1941;47(3):406–414.
- , , , . Following morale over time within an academic hospitalist division. J Clin Outcomes Manag. 2011;18(1):21–26.
- , , , et al. Personal growth and its correlates during residency training. Med Educ. 2006;40(8):737–745.
- , , . A global measure of perceived stress. J Health Soc Behav. 1983:385–396.
- , , . Morale matters: midlevel administrators and their intent to leave. J Higher Educ. 2000;71(1):34–59.
- , . Faculty members' morale and their intention to leave: a multilevel explanation. J Higher Educ. 2002;73(4):518–542.
- , . Employee Morale. New York, NY: Palgrave Macmillan; 2009.
- , , , , . Silence Kills. Silence Kills: The Seven Crucial Conversations® for Healthcare. VitalSmarts™ in association with the American Association of Critical Care Nurses, USA. 2005. Accessed October 10, 2014.
- , , . The lifelong iterative process of physician retention. J Healthc Manag. 2009;54(4):220–226.
- . Physicians' burnout. Rev Prat. 2004;54(7):753–754.
- , , , , , . Work stress and health in primary health care physicians and hospital physicians. Occup Environ Med. 2008;65(5):364–366.
- , , , et al. Understanding physicians' intentions to withdraw from practice: the role of job satisfaction, job stress, mental and physical health. 2001. Health Care Manage Rev. 2010;35(2):105–115.
- , , , , , . Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358–1367.
- , . Burnout and Hospitalists: Etiology and Prevention. In: What Exactly Does A Hospitalist Do? Best of the Best Hospital Medicine 2005: Strategies for Success. Society of Hospital Medicine; 2005:5.
- , . Using job involvement and organizational commitment interactively to predict turnover. J Manage. 1989;15(1):115–127.
- , , , et al. Nurse turnover: a literature review. Int J Nurs Stud. 2006;43(2):237–263.
Explosive growth in hospital medicine has led to hospitalists having the option to change jobs easily. Annual turnover for all physicians is 6.8%, whereas that of hospitalists exceeds 14.8%.[1] Losing a single physician has significant financial and operational implications, with estimates of $20,000 to $120,000 in recruiting costs, and up to $500,000 in lost revenue that may take years to recoup due to the time required for new physician assimilation.[2, 3] In 2006, the Society of Hospital Medicine (SHM) appointed a career task force to develop retention recommendations, 1 of which includes monitoring hospitalists' job satisfaction.[4]
Studies examining physician satisfaction have demonstrated that high physician job satisfaction is associated with lower physician turnover.[5] However, surveys of hospitalists, including SHM's Hospital Medicine Physician Worklife Survey (HMPWS), have reported high job satisfaction among hospitalists,[6, 7, 8, 9, 10] suggesting that high job satisfaction may not be enough to overcome forces that pull hospitalists toward other opportunities.
Morale, a more complex construct related to an individual's contentment and happiness, might provide insight into reducing hospitalist turnover. Morale has been defined as the emotional or mental condition with respect to cheerfulness, confidence, or zeal and is especially relevant in the face of opposition or hardship.[11] Job satisfaction is 1 element that contributes to morale, but alone does not equate morale.[12] Morale, more than satisfaction, relates to how people see themselves within the group and may be closely tied to the concept of esprit de corps. To illustrate, workers may feel satisfied with the content of their job, but frustration with the organization may result in low morale.[13] Efforts focused on assessing provider morale may provide deeper understanding of hospitalists' professional needs and garner insight for retention strategies.
The construct of hospitalist morale and its underlying drivers has not been explored in the literature. Using literature within and outside of healthcare,[1, 12, 14, 15, 16, 17, 18, 19, 20, 21, 22] and our own prior work,[23] we sought to characterize elements that contribute to hospitalist morale and develop a metric to measure it. The HMPWS found that job satisfaction factors vary across hospitalist groups.[9] We suspected that the same would hold true for factors important to morale at the individual level. This study describes the development and validation of the Hospitalist Morale Index (HMI), and explores the relationship between morale and intent to leave due to unhappiness.
METHODS
2009 Pilot Survey
To establish content validity, after reviewing employee morale literature, and examining qualitative comments from our 2007 and 2008 morale surveys, our expert panel, consisting of practicing hospitalists, hospitalist leaders, and administrative staff, identified 46 potential drivers of hospitalist morale. In May 2009, all hospitalists, including physicians, nurse practitioners (NPs), and physician assistants (PAs) from a single hospitalist group received invitations to complete the pilot survey. We asked hospitalists to assess on 5‐point Likert scales the importance of (not at all to tremendously) and contentment with (extremely discontent to extremely content) each of the 46 items as it relates to their work morale. Also included were demographic questions and general morale questions (including rating participants' own morale), investment, long‐term career plans, and intent to leave due to unhappiness.
Data Collection
To maintain anonymity and limit social desirability bias, a database manager, working outside the Division of Hospital Medicine and otherwise not associated with the research team, used Survey Monkey to coordinate survey distribution and data collection. Each respondent had a unique identifier code that was unrelated to the respondent's name and email address. Personal identifiers were maintained in a secure database accessible only to the database manager.
Establishing Internal Structure Validity Evidence
Response frequency to each question was examined for irregularities in distribution. For continuous variables, descriptive statistics were examined for evidence of skewness, outliers, and non‐normality to ensure appropriate use of parametric statistical tests. Upon ranking importance ratings by mode, 15 of 46 items were judged to be of low importance by almost all participants and removed from further consideration.
Stata 13.1 (StataCorp, College Station, TX) was used for exploratory factor analysis (EFA) of the importance responses for all 31 remaining items by principal components factoring. Eigenvalues >1 were designated as a cutoff point for inclusion in varimax rotation. Factor loading of 0.50 was the threshold for inclusion in a factor.
The 31 items loaded across 10 factors; however, 3 factors included 1 item each. After reviewing the scree plot and considering their face value, these items/factors were omitted. Repeating the factor analysis resulted in a 28‐item, 7‐factor solution that accounted for 75% variance. All items were considered informative as demonstrated by low uniqueness scores (0.050.38). Using standard validation procedures, all 7 factors were found to have acceptable factor loadings (0.460.98) and face validity. Cronbach's quantified internal reliability of the 7 factors with scores ranging from 0.68 to 0.92. We named the resultant solution the Hospitalist Morale Index (HMI).
Establishing Response Process Validity Evidence
In developing the HMI, we asked respondents to rate the importance of and their contentment with each variable as related to their work morale. From pilot testing, which included discussions with respondents immediately after completing the survey, we learned that the 2‐part consideration of each variable resulted in thoughtful reflection about their morale. Further, by multiplying the contentment score for each item (scaled from 15) by the corresponding importance score (scaled 01), we quantified the relative contribution and contentment of each item for each hospitalist. Scaling importance scores from 0 to 1 insured that items that were not considered important to the respondent did not affect the respondent's personal morale score. Averaging resultant item scores that were greater than 0 resulted in a personal morale score for each hospitalist. Averaging item scores >0 that constituted each factor resulted in factor scores.
May 2011 Survey
The refined survey was distributed in May 2011 to a convenience sample of 5 hospitalist programs at separate hospitals (3 community hospitals, 2 academic hospitals) encompassing 108 hospitalists in 3 different states. Responses to the 2011 survey were used to complete confirmatory factor analyses (CFA) and establish further validity and reliability evidence.
Based on the 28‐item, 7‐factor solution developed from the pilot study, we developed the theoretical model of factors constituting hospitalist morale. We used the structural equation modeling command in Stata 13 to perform CFA. Factor loading of 0.50 was the threshold for inclusion of an item in a factor. To measure internal consistency, we considered Cronbach's score of 0.60 acceptable. Iterative models were reviewed to find the optimal solution for the data. Four items did not fit into any of the 5 resulting factors and were evaluated in terms of mean importance score and face value. Three items were considered important enough to warrant being stand‐alone items, whereas 1 was omitted. Two additional items had borderline factor loadings (0.48, 0.49) and were included in the model as stand‐alone items due to their overall relevance. The resultant solution was a 5‐factor model with 5 additional stand‐alone items (Table 1).
| Factor | Cronbach's | |||||
|---|---|---|---|---|---|---|
| Clinical | Workload | Leadership | Appreciation and Acknowledgement | Material Rewards | ||
| How much does the following item contribute to your morale? | ||||||
| Paperwork | 0.72 | 0.89 | ||||
| Relationship with patients | 0.69 | 0.90 | ||||
| Electronic medical system | 0.60 | 0.90 | ||||
| Intellectual stimulation | 0.59 | 0.90 | ||||
| Variety of cases | 0.58 | 0.90 | ||||
| Relationship with consultants | 0.51 | 0.89 | ||||
| No. of night shifts | 0.74 | 0.89 | ||||
| Patient census | 0.61 | 0.90 | ||||
| No. of shifts | 0.52 | 0.90 | ||||
| Fairness of leadership | 0.82 | 0.89 | ||||
| Effectiveness of leadership | 0.82 | 0.89 | ||||
| Leadership's receptiveness to my thoughts and suggestions | 0.78 | 0.89 | ||||
| Leadership as advocate for my needs | 0.77 | 0.89 | ||||
| Approachability of leadership | 0.77 | 0.89 | ||||
| Accessibility of leadership | 0.69 | 0.89 | ||||
| Alignment of the group's goals with my goals | 0.50 | 0.89 | ||||
| Recognition within the group | 0.82 | 0.89 | ||||
| Feeling valued within the institution | 0.73 | 0.89 | ||||
| Feeling valued within the group | 0.73 | 0.89 | ||||
| Feedback | 0.52 | 0.89 | ||||
| Pay | 0.99 | 0.90 | ||||
| Benefits | 0.56 | 0.89 | ||||
| Cronbach's | 0.78 | 0.65 | 0.89 | 0.78 | 0.71 | |
| How much does the following item contribute to your morale? | Single item indicators | |||||
| Family time | 0.90 | |||||
| Job security | 0.90 | |||||
| Institutional climate | 0.89 | |||||
| Opportunities for professional growth | 0.90 | |||||
| Autonomy | 0.89 | |||||
| Cronbach's | 0.90 | |||||
Establishing Convergent, Concurrent, and Discriminant Validity Evidence
To establish convergent, concurrent, and discriminant validity, linear and logistic regression models were examined for continuous and categorical data accordingly.
Self‐perceived overall work morale and perceived group morale, as assessed by 6‐point Likert questions with response options from terrible to excellent, were modeled as predictors for personal morale as calculated by the HMI.
Personal morale scores were modeled as predictors of professional growth, stress, investment in the group, and intent to leave due to unhappiness. While completing the HMI, hospitalists simultaneously completed a validated professional growth scale[24] and Cohen stress scale.[25] We hypothesized that those with higher morale would have more professional growth. Stress, although an important issue in the workplace, is a distinct construct from morale, and we did not expect a significant relationship between personal morale and stress. We used Pearson's r to assess the strength of association between the HMI and these scales. Participants' level of investment in their group was assessed on a 5‐point Likert scale. To simplify presentation, highly invested represents those claiming to be very or tremendously invested in the success of their current hospitalist group. Intent to leave due to unhappiness was assessed on a 5‐point Likert scale, I have had serious thoughts about leaving my current hospitalist group because I am unhappy, with responses from strongly disagree (1) to strongly agree (5). To simplify presentation, responses higher than 2 are considered to be consistent with intending to leave due to unhappiness.
Our institutional review board approved the study.
RESULTS
Respondents
In May 2009, 30 of the 33 (91%) invited hospitalists completed the original pilot morale survey; 19 (63%) were women. Eleven hospitalists (37%) had been part of the group 1 year or less, whereas 4 (13%) had been with the group for more than 5 years.
In May 2011, 93 of the 108 (86%) hospitalists from 5 hospitals completed the demographic and global parts of the survey. Fifty (53%) were from community hospitals; 47 (51%) were women. Thirty‐seven (40%) physicians and 6 (60%) NPs/PAs were from academic hospitals. Thirty‐nine hospitalists (42%) had been with their current group 1 year or less. Ten hospitalists (11%) had been with their current group over 5 years. Sixty‐three respondents (68%) considered themselves career hospitalists, whereas 5 (5%) did not; the rest were undecided.
Internal Structure Validity Evidence
The final CFA from the 2011 survey resulted in a 5‐factor plus 5stand‐alone‐items HMI. The solution with item‐level and factor‐level Cronbach's scores (range, 0.890.90 and range, 0.650.89, respectively) are shown in Table 1.
Personal Morale Scores and Factor Scores
Personal morale scores were normally distributed (mean = 2.79; standard deviation [SD] = 0.58), ranging from 1.23 to 4.22, with a theoretical low of 0 and high of 5 (Figure 1). Mean personal morale scores across hospitalist groups ranged from 2.70 to 2.99 (P > 0.05). Personal morale scores, factor sores and item scores for NPs and PAs did not significantly differ from those of physicians (P > 0.05 for all analyses). Personal morale scores were lower for those in their first 3 years with their current group, compared to those with greater institutional longevity. For every categorical increase in a participant's response to seeing oneself as a career hospitalist, the personal morale score rose 0.23 points (P < 0.001).
Factor scores for material reward and mean item scores for professional growth were significantly different across the 5 hospitalist groups (P = 0.03 and P < 0.001, respectively). Community hospitalists had significantly higher factor scores, despite having similar importance scores, for material rewards than academic hospitalists (diff. = 0.44, P = 0.02). Academic hospitalists had significantly higher scores for professional growth (diff. = 0.94, P < 0.001) (Table 2). Professional growth had the highest importance score for academic hospitalists (mean = 0.87, SD = 0.18) and the lowest importance score for community hospitalists (mean = 0.65, SD = 0.24, P < 0.001).
| Personal Morale Score | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical | Workload | Leadership | Appreciation and Acknowledgement | Material Rewards | Family Time | Institutional Climate | Job Security | Autonomy | Professional Growth | |||
| ||||||||||||
| All participants | Mean | 2.79 | 2.54 | 2.78 | 3.18 | 2.58 | 2.48 | 3.05 | 2.67 | 2.92 | 3.00 | 2.76 |
| SD | 0.58 | 0.63 | 0.70 | 0.95 | 0.86 | 0.85 | 1.15 | 0.97 | 1.11 | 1.10 | 1.21 | |
| Academic A | Mean | 2.77 | 2.43 | 2.92 | 3.10 | 2.54 | 2.28 | 3.16 | 2.70 | 3.06 | 3.20 | 3.08 |
| SD | 0.57 | 0.62 | 0.64 | 0.92 | 0.84 | 0.77 | 1.19 | 0.95 | 1.08 | 1.12 | 1.24 | |
| Academic B | Mean | 2.99 | 2.58 | 2.99 | 3.88 | 2.69 | 2.00 | 2.58 | 2.13 | 1.65 | 3.29 | 4.33 |
| SD | 0.36 | 0.70 | 0.80 | 0.29 | 0.80 | 0.35 | 0.92 | 0.88 | 0.78 | 1.01 | 0.82 | |
| Community A | Mean | 2.86 | 2.61 | 2.51 | 3.23 | 2.73 | 3.03 | 2.88 | 2.84 | 2.95 | 3.23 | 2.66 |
| SD | 0.75 | 0.79 | 0.68 | 1.21 | 1.11 | 1.14 | 1.37 | 1.17 | 0.98 | 1.24 | 1.15 | |
| Community B | Mean | 2.86 | 2.74 | 2.97 | 3.37 | 2.67 | 2.44 | 3.28 | 2.35 | 2.70 | 2.50 | 2.25 |
| SD | 0.67 | 0.55 | 0.86 | 1.04 | 0.94 | 0.87 | 1.00 | 1.15 | 1.40 | 0.72 | 1.26 | |
| Community C | Mean | 2.70 | 2.56 | 2.64 | 2.99 | 2.47 | 2.53 | 3.03 | 2.79 | 3.07 | 2.68 | 2.15 |
| SD | 0.49 | 0.53 | 0.67 | 0.85 | 0.73 | 0.64 | 1.08 | 0.76 | 1.05 | 1.07 | 0.71 | |
| Academic combined | Mean | 2.80 | 2.45 | 2.93 | 3.22 | 2.56 | 2.24 | 3.07 | 2.62 | 2.88 | 3.21 | 3.28 |
| SD | 0.54 | 0.63 | 0.66 | 0.89 | 0.82 | 0.72 | 1.16 | 0.95 | 1.14 | 1.10 | 1.26 | |
| Community combined | Mean | 2.79 | 2.61 | 2.66 | 3.14 | 2.60 | 2.68 | 3.03 | 2.72 | 2.95 | 2.82 | 2.34 |
| SD | 0.62 | 0.62 | 0.72 | 1.01 | 0.90 | 0.90 | 1.15 | 0.99 | 1.09 | 1.09 | 1.00 | |
| P value | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | 0.02 | >0.05 | >0.05 | >0.05 | >0.05 | <0.001 | |
Convergent, Concurrent, and Discriminant Validity Evidence
For every categorical increase on the question assessing overall morale, the personal morale score was 0.23 points higher (P < 0.001). For every categorical increase in a participant's perception of the group's morale, the personal morale score was 0.29 points higher (P < 0.001).
For every 1‐point increase in personal morale score, the odds of being highly invested in the group increased by 5 times (odds ratio [OR]: 5.23, 95% confidence interval [CI]: 1.91‐14.35, P = 0.001). The mean personal morale score for highly invested hospitalists was 2.92, whereas that of those less invested was 2.43 (diff. = 0.49, P < 0.001) (Table 3). Highly invested hospitalists had significantly higher importance factor scores for leadership (diff. = 0.08, P = 0.03) as well as appreciation and acknowledgement (diff. = 0.08, P = 0.02).
| Personal Morale Score | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical | Workload | Leadership | Appreciation and Acknowledgement | Material Rewards | Family Time | Institutional Climate | Job Security | Autonomy | Professional Growth | ||
| |||||||||||
| Highly invested in success of current hospitalist group | |||||||||||
| Mean | 2.92 | 2.61 | 2.89 | 3.38 | 2.78 | 2.45 | 3.21 | 2.78 | 2.86 | 3.10 | 2.95 |
| SD | 0.55 | 0.59 | 0.68 | 0.92 | 0.88 | 0.77 | 1.11 | 1.00 | 1.09 | 1.06 | 1.25 |
| Less invested in success of current hospitalist group | |||||||||||
| Mean | 2.43 | 2.34 | 2.48 | 2.60 | 2.02 | 2.57 | 2.60 | 2.38 | 3.08 | 2.69 | 2.24 |
| SD | 0.52 | 0.69 | 0.69 | 0.81 | 0.49 | 1.04 | 1.17 | 0.83 | 1.18 | 1.19 | 0.94 |
| P value | <0.001 | >0.05 | 0.02 | 0.001 | <0.001 | >0.05 | 0.03 | >0.05 | >0.05 | >0.05 | 0.02 |
| Not intending to leave because unhappy | |||||||||||
| Mean | 2.97 | 2.67 | 2.89 | 3.48 | 2.77 | 2.52 | 3.24 | 2.85 | 3.05 | 3.06 | 3.01 |
| SD | 0.51 | 0.54 | 0.61 | 0.91 | 0.89 | 0.78 | 1.03 | 0.99 | 1.10 | 1.07 | 1.25 |
| Intending to leave current group because unhappy | |||||||||||
| Mean | 2.45 | 2.30 | 2.59 | 2.59 | 2.21 | 2.40 | 2.68 | 2.33 | 2.67 | 2.88 | 2.28 |
| SD | 0.56 | 0.72 | 0.82 | 0.74 | 0.68 | 0.97 | 1.29 | 0.83 | 1.11 | 1.17 | 0.97 |
| P value | <0.001 | 0.01 | >0.05 | <0.001 | 0.003 | >0.05 | 0.03 | 0.01 | >0.05 | >0.05 | 0.01 |
Every 1‐point increase in personal morale was associated with a rise of 2.27 on the professional growth scale (P = 0.01). The correlation between these 2 scales was 0.26 (P = 0.01). Every 1‐point increase in personal morale was associated with a 2.21 point decrease on the Cohen stress scale (P > 0.05). The correlation between these 2 scales was 0.21 (P > 0.05).
Morale and Intent to Leave Due to Unhappiness
Sixteen (37%) academic and 18 (36%) community hospitalists reported having thoughts of leaving their current hospitalist program due to unhappiness. The mean personal morale score for hospitalists with no intent to leave their current group was 2.97, whereas that of those with intent to leave was 2.45 (diff. = 0.53, P < 0.001). Each 1‐point increase in the personal morale score was associated with an 85% decrease (OR: 0.15, 95% CI: 0.05‐0.41, P < 0.001) in the odds of leaving because of unhappiness. Holding self‐perception of being a career hospitalist constant, each 1‐point increase in the personal morale score was associated with an 83% decrease (OR: 0.17, 95% CI: 0.05‐0.51, P = 0.002) in the odds of leaving because of unhappiness. Hospitalists who reported intent to leave had significantly lower factor scores for all factors and items except workload, material reward, and autonomy than those who did not report intent to leave (Table 3). Within the academic groups, those who reported intent to leave had significantly lower scores for professional growth (diff. = 1.08, P = 0.01). For community groups, those who reported intent to leave had significantly lower scores for clinical work (diff. = 0.54, P = 0.003), workload (diff. = 0.50, P = 0.02), leadership (diff. = 1.19, P < 0.001), feeling appreciated and acknowledged (diff. = 0.68, P = 0.01), job security (diff. = 0.70, P = 0.03), and institutional climate (diff. = 0.67, P = 0.02) than those who did not report intent to leave.
DISCUSSION
The HMI is a validated tool that objectively measures and quantifies hospitalist morale. The HMI's capacity to comprehensively assess morale comes from its breadth and depth in uncovering work‐related areas that may be sources of contentment or displeasure. Furthermore, the fact that HMI scores varied among groups of individuals, including those who are thinking about leaving their hospitalist group because they are unhappy and those who are highly invested in their hospitalist group, speaks to its ability to highlight and account for what is most important to hospitalist providers.
Low employee morale has been associated with decreased productivity, increased absenteeism, increased turnover, and decreased patient satisfaction.[2, 26, 27, 28] A few frustrated workers can breed group discontentment and lower the entire group's morale.[28] In addition to its financial impact, departures due to low morale can be sudden and devastating, leading to loss of team cohesiveness, increased work burden on the remaining workforce, burnout, and cascades of more turnover.[2] In contrast, when morale is high, workers more commonly go the extra mile, are more committed to the organization's mission, and are more supportive of their coworkers.[28]
While we asked the informants about plans to leave their job, there are many factors that drive an individual's intent and ultimate decision to make changes in his or her employment. Some factors are outside the control of the employer or practice leaders, such as change in an individual's family life or desire and opportunity to pursue fellowship training. Others variables, however, are more directly tied to the job or practice environment. In a specialty where providers are relatively mobile and turnover is high, it is important for hospitalist practices to cultivate a climate in which the sacrifices associated with leaving outweigh the promised benefits.[29]
Results from the HMPWS suggested the need to address climate and fairness issues in hospitalist programs to improve satisfaction and retention.[9] Two large healthcare systems achieved success by investing in multipronged physician retention strategies including recruiting advisors, sign‐on bonuses, extensive onboarding, family support, and the promotion of ongoing effective communication.[3, 30]
Our findings suggest that morale for hospitalists is a complex amalgam of contentment and importance, and that there may not be a one size fits all solution to improving morale for all. While we did not find a difference in personal morale scores across individual hospitalist groups, or even between academic and community groups, each group had a unique profile with variability in the dynamics between importance and contentment of different factors. If practice group leaders review HMI data for their providers and use the information to facilitate meaningful dialogue with them about the factors influencing their morale, such leaders will have great insight into allocating resources for the best return on investment.
While we believe that the HMI is providing unique perspective compared to other commonly used metrics, it may be best to employ HMI data as complementary measures alongside that of some of the benchmarked scales that explore job satisfaction, job fit, and burnout among hospitalists.[6, 9, 10, 31, 32, 33, 34, 35] Aggregate HMI data at the group level may allow for the identification of factors that are highly important to morale but scored low in contentment. Such factors deserve priority and attention such that the subgroups within a practice can collaborate to come to consensus on strategies for amelioration. Because the HMI generates a score and profile for each provider, we can imagine effective leaders using the HMI with individuals as part of an annual review to facilitate discussion about maximizing contentment at work. Being fully transparent and sharing an honest nonanonymous version of the HMI with a superior would require a special relationship founded on trust and mutual respect.
Several limitations of this study should be considered. First, the initial item reduction and EFA were based on a single‐site survey, and our overall sample size was relatively small. We plan on expanding our sample size in the future for further validation of our exploratory findings. Second, the data were collected at 2 specific times several years ago. In continuing to analyze the data from subsequent years, validity and reliability results remain stable, thereby minimizing the likelihood of significant historical bias. Third, there may have been some recall bias, in that respondents may have overlooked the good and perseverated over variables that disappointed them. Fourth, although intention to leave does not necessarily equate actual employee turnover, intention has been found to be a strong predictor of quitting a job.[36, 37] Finally, while we had high response rates, response bias may have existed wherein those with lower morale may have elected not to complete the survey or became apathetic in their responses.
The HMI is a validated instrument that evaluates hospitalist morale by incorporating each provider's characterization of the importance of and contentment with 27 variables. By accounting for the multidimensional and dynamic nature of morale, the HMI may help program leaders tailor retention and engagement strategies specific to their own group. Future studies may explore trends in contributors to morale and examine whether interventions to augment low morale can result in improved morale and hospitalist retention.
Acknowledgements
The authors are indebted to the hospitalists who were willing to share their perspectives about their work, and grateful to Ms. Lisa Roberts, Ms. Barbara Brigade, and Ms. Regina Landis for insuring confidentiality in managing the survey database.
Disclosures: Dr. Chandra had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Wright is a Miller‐Coulson Family Scholar through the Johns Hopkins Center for Innovative Medicine. Ethical approval has been granted for studies involving human subjects by a Johns Hopkins University School of Medicine institutional review board. The authors report no conflicts of interest.
Explosive growth in hospital medicine has led to hospitalists having the option to change jobs easily. Annual turnover for all physicians is 6.8%, whereas that of hospitalists exceeds 14.8%.[1] Losing a single physician has significant financial and operational implications, with estimates of $20,000 to $120,000 in recruiting costs, and up to $500,000 in lost revenue that may take years to recoup due to the time required for new physician assimilation.[2, 3] In 2006, the Society of Hospital Medicine (SHM) appointed a career task force to develop retention recommendations, 1 of which includes monitoring hospitalists' job satisfaction.[4]
Studies examining physician satisfaction have demonstrated that high physician job satisfaction is associated with lower physician turnover.[5] However, surveys of hospitalists, including SHM's Hospital Medicine Physician Worklife Survey (HMPWS), have reported high job satisfaction among hospitalists,[6, 7, 8, 9, 10] suggesting that high job satisfaction may not be enough to overcome forces that pull hospitalists toward other opportunities.
Morale, a more complex construct related to an individual's contentment and happiness, might provide insight into reducing hospitalist turnover. Morale has been defined as the emotional or mental condition with respect to cheerfulness, confidence, or zeal and is especially relevant in the face of opposition or hardship.[11] Job satisfaction is 1 element that contributes to morale, but alone does not equate morale.[12] Morale, more than satisfaction, relates to how people see themselves within the group and may be closely tied to the concept of esprit de corps. To illustrate, workers may feel satisfied with the content of their job, but frustration with the organization may result in low morale.[13] Efforts focused on assessing provider morale may provide deeper understanding of hospitalists' professional needs and garner insight for retention strategies.
The construct of hospitalist morale and its underlying drivers has not been explored in the literature. Using literature within and outside of healthcare,[1, 12, 14, 15, 16, 17, 18, 19, 20, 21, 22] and our own prior work,[23] we sought to characterize elements that contribute to hospitalist morale and develop a metric to measure it. The HMPWS found that job satisfaction factors vary across hospitalist groups.[9] We suspected that the same would hold true for factors important to morale at the individual level. This study describes the development and validation of the Hospitalist Morale Index (HMI), and explores the relationship between morale and intent to leave due to unhappiness.
METHODS
2009 Pilot Survey
To establish content validity, after reviewing employee morale literature, and examining qualitative comments from our 2007 and 2008 morale surveys, our expert panel, consisting of practicing hospitalists, hospitalist leaders, and administrative staff, identified 46 potential drivers of hospitalist morale. In May 2009, all hospitalists, including physicians, nurse practitioners (NPs), and physician assistants (PAs) from a single hospitalist group received invitations to complete the pilot survey. We asked hospitalists to assess on 5‐point Likert scales the importance of (not at all to tremendously) and contentment with (extremely discontent to extremely content) each of the 46 items as it relates to their work morale. Also included were demographic questions and general morale questions (including rating participants' own morale), investment, long‐term career plans, and intent to leave due to unhappiness.
Data Collection
To maintain anonymity and limit social desirability bias, a database manager, working outside the Division of Hospital Medicine and otherwise not associated with the research team, used Survey Monkey to coordinate survey distribution and data collection. Each respondent had a unique identifier code that was unrelated to the respondent's name and email address. Personal identifiers were maintained in a secure database accessible only to the database manager.
Establishing Internal Structure Validity Evidence
Response frequency to each question was examined for irregularities in distribution. For continuous variables, descriptive statistics were examined for evidence of skewness, outliers, and non‐normality to ensure appropriate use of parametric statistical tests. Upon ranking importance ratings by mode, 15 of 46 items were judged to be of low importance by almost all participants and removed from further consideration.
Stata 13.1 (StataCorp, College Station, TX) was used for exploratory factor analysis (EFA) of the importance responses for all 31 remaining items by principal components factoring. Eigenvalues >1 were designated as a cutoff point for inclusion in varimax rotation. Factor loading of 0.50 was the threshold for inclusion in a factor.
The 31 items loaded across 10 factors; however, 3 factors included 1 item each. After reviewing the scree plot and considering their face value, these items/factors were omitted. Repeating the factor analysis resulted in a 28‐item, 7‐factor solution that accounted for 75% variance. All items were considered informative as demonstrated by low uniqueness scores (0.050.38). Using standard validation procedures, all 7 factors were found to have acceptable factor loadings (0.460.98) and face validity. Cronbach's quantified internal reliability of the 7 factors with scores ranging from 0.68 to 0.92. We named the resultant solution the Hospitalist Morale Index (HMI).
Establishing Response Process Validity Evidence
In developing the HMI, we asked respondents to rate the importance of and their contentment with each variable as related to their work morale. From pilot testing, which included discussions with respondents immediately after completing the survey, we learned that the 2‐part consideration of each variable resulted in thoughtful reflection about their morale. Further, by multiplying the contentment score for each item (scaled from 15) by the corresponding importance score (scaled 01), we quantified the relative contribution and contentment of each item for each hospitalist. Scaling importance scores from 0 to 1 insured that items that were not considered important to the respondent did not affect the respondent's personal morale score. Averaging resultant item scores that were greater than 0 resulted in a personal morale score for each hospitalist. Averaging item scores >0 that constituted each factor resulted in factor scores.
May 2011 Survey
The refined survey was distributed in May 2011 to a convenience sample of 5 hospitalist programs at separate hospitals (3 community hospitals, 2 academic hospitals) encompassing 108 hospitalists in 3 different states. Responses to the 2011 survey were used to complete confirmatory factor analyses (CFA) and establish further validity and reliability evidence.
Based on the 28‐item, 7‐factor solution developed from the pilot study, we developed the theoretical model of factors constituting hospitalist morale. We used the structural equation modeling command in Stata 13 to perform CFA. Factor loading of 0.50 was the threshold for inclusion of an item in a factor. To measure internal consistency, we considered Cronbach's score of 0.60 acceptable. Iterative models were reviewed to find the optimal solution for the data. Four items did not fit into any of the 5 resulting factors and were evaluated in terms of mean importance score and face value. Three items were considered important enough to warrant being stand‐alone items, whereas 1 was omitted. Two additional items had borderline factor loadings (0.48, 0.49) and were included in the model as stand‐alone items due to their overall relevance. The resultant solution was a 5‐factor model with 5 additional stand‐alone items (Table 1).
| Factor | Cronbach's | |||||
|---|---|---|---|---|---|---|
| Clinical | Workload | Leadership | Appreciation and Acknowledgement | Material Rewards | ||
| How much does the following item contribute to your morale? | ||||||
| Paperwork | 0.72 | 0.89 | ||||
| Relationship with patients | 0.69 | 0.90 | ||||
| Electronic medical system | 0.60 | 0.90 | ||||
| Intellectual stimulation | 0.59 | 0.90 | ||||
| Variety of cases | 0.58 | 0.90 | ||||
| Relationship with consultants | 0.51 | 0.89 | ||||
| No. of night shifts | 0.74 | 0.89 | ||||
| Patient census | 0.61 | 0.90 | ||||
| No. of shifts | 0.52 | 0.90 | ||||
| Fairness of leadership | 0.82 | 0.89 | ||||
| Effectiveness of leadership | 0.82 | 0.89 | ||||
| Leadership's receptiveness to my thoughts and suggestions | 0.78 | 0.89 | ||||
| Leadership as advocate for my needs | 0.77 | 0.89 | ||||
| Approachability of leadership | 0.77 | 0.89 | ||||
| Accessibility of leadership | 0.69 | 0.89 | ||||
| Alignment of the group's goals with my goals | 0.50 | 0.89 | ||||
| Recognition within the group | 0.82 | 0.89 | ||||
| Feeling valued within the institution | 0.73 | 0.89 | ||||
| Feeling valued within the group | 0.73 | 0.89 | ||||
| Feedback | 0.52 | 0.89 | ||||
| Pay | 0.99 | 0.90 | ||||
| Benefits | 0.56 | 0.89 | ||||
| Cronbach's | 0.78 | 0.65 | 0.89 | 0.78 | 0.71 | |
| How much does the following item contribute to your morale? | Single item indicators | |||||
| Family time | 0.90 | |||||
| Job security | 0.90 | |||||
| Institutional climate | 0.89 | |||||
| Opportunities for professional growth | 0.90 | |||||
| Autonomy | 0.89 | |||||
| Cronbach's | 0.90 | |||||
Establishing Convergent, Concurrent, and Discriminant Validity Evidence
To establish convergent, concurrent, and discriminant validity, linear and logistic regression models were examined for continuous and categorical data accordingly.
Self‐perceived overall work morale and perceived group morale, as assessed by 6‐point Likert questions with response options from terrible to excellent, were modeled as predictors for personal morale as calculated by the HMI.
Personal morale scores were modeled as predictors of professional growth, stress, investment in the group, and intent to leave due to unhappiness. While completing the HMI, hospitalists simultaneously completed a validated professional growth scale[24] and Cohen stress scale.[25] We hypothesized that those with higher morale would have more professional growth. Stress, although an important issue in the workplace, is a distinct construct from morale, and we did not expect a significant relationship between personal morale and stress. We used Pearson's r to assess the strength of association between the HMI and these scales. Participants' level of investment in their group was assessed on a 5‐point Likert scale. To simplify presentation, highly invested represents those claiming to be very or tremendously invested in the success of their current hospitalist group. Intent to leave due to unhappiness was assessed on a 5‐point Likert scale, I have had serious thoughts about leaving my current hospitalist group because I am unhappy, with responses from strongly disagree (1) to strongly agree (5). To simplify presentation, responses higher than 2 are considered to be consistent with intending to leave due to unhappiness.
Our institutional review board approved the study.
RESULTS
Respondents
In May 2009, 30 of the 33 (91%) invited hospitalists completed the original pilot morale survey; 19 (63%) were women. Eleven hospitalists (37%) had been part of the group 1 year or less, whereas 4 (13%) had been with the group for more than 5 years.
In May 2011, 93 of the 108 (86%) hospitalists from 5 hospitals completed the demographic and global parts of the survey. Fifty (53%) were from community hospitals; 47 (51%) were women. Thirty‐seven (40%) physicians and 6 (60%) NPs/PAs were from academic hospitals. Thirty‐nine hospitalists (42%) had been with their current group 1 year or less. Ten hospitalists (11%) had been with their current group over 5 years. Sixty‐three respondents (68%) considered themselves career hospitalists, whereas 5 (5%) did not; the rest were undecided.
Internal Structure Validity Evidence
The final CFA from the 2011 survey resulted in a 5‐factor plus 5stand‐alone‐items HMI. The solution with item‐level and factor‐level Cronbach's scores (range, 0.890.90 and range, 0.650.89, respectively) are shown in Table 1.
Personal Morale Scores and Factor Scores
Personal morale scores were normally distributed (mean = 2.79; standard deviation [SD] = 0.58), ranging from 1.23 to 4.22, with a theoretical low of 0 and high of 5 (Figure 1). Mean personal morale scores across hospitalist groups ranged from 2.70 to 2.99 (P > 0.05). Personal morale scores, factor sores and item scores for NPs and PAs did not significantly differ from those of physicians (P > 0.05 for all analyses). Personal morale scores were lower for those in their first 3 years with their current group, compared to those with greater institutional longevity. For every categorical increase in a participant's response to seeing oneself as a career hospitalist, the personal morale score rose 0.23 points (P < 0.001).
Factor scores for material reward and mean item scores for professional growth were significantly different across the 5 hospitalist groups (P = 0.03 and P < 0.001, respectively). Community hospitalists had significantly higher factor scores, despite having similar importance scores, for material rewards than academic hospitalists (diff. = 0.44, P = 0.02). Academic hospitalists had significantly higher scores for professional growth (diff. = 0.94, P < 0.001) (Table 2). Professional growth had the highest importance score for academic hospitalists (mean = 0.87, SD = 0.18) and the lowest importance score for community hospitalists (mean = 0.65, SD = 0.24, P < 0.001).
| Personal Morale Score | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical | Workload | Leadership | Appreciation and Acknowledgement | Material Rewards | Family Time | Institutional Climate | Job Security | Autonomy | Professional Growth | |||
| ||||||||||||
| All participants | Mean | 2.79 | 2.54 | 2.78 | 3.18 | 2.58 | 2.48 | 3.05 | 2.67 | 2.92 | 3.00 | 2.76 |
| SD | 0.58 | 0.63 | 0.70 | 0.95 | 0.86 | 0.85 | 1.15 | 0.97 | 1.11 | 1.10 | 1.21 | |
| Academic A | Mean | 2.77 | 2.43 | 2.92 | 3.10 | 2.54 | 2.28 | 3.16 | 2.70 | 3.06 | 3.20 | 3.08 |
| SD | 0.57 | 0.62 | 0.64 | 0.92 | 0.84 | 0.77 | 1.19 | 0.95 | 1.08 | 1.12 | 1.24 | |
| Academic B | Mean | 2.99 | 2.58 | 2.99 | 3.88 | 2.69 | 2.00 | 2.58 | 2.13 | 1.65 | 3.29 | 4.33 |
| SD | 0.36 | 0.70 | 0.80 | 0.29 | 0.80 | 0.35 | 0.92 | 0.88 | 0.78 | 1.01 | 0.82 | |
| Community A | Mean | 2.86 | 2.61 | 2.51 | 3.23 | 2.73 | 3.03 | 2.88 | 2.84 | 2.95 | 3.23 | 2.66 |
| SD | 0.75 | 0.79 | 0.68 | 1.21 | 1.11 | 1.14 | 1.37 | 1.17 | 0.98 | 1.24 | 1.15 | |
| Community B | Mean | 2.86 | 2.74 | 2.97 | 3.37 | 2.67 | 2.44 | 3.28 | 2.35 | 2.70 | 2.50 | 2.25 |
| SD | 0.67 | 0.55 | 0.86 | 1.04 | 0.94 | 0.87 | 1.00 | 1.15 | 1.40 | 0.72 | 1.26 | |
| Community C | Mean | 2.70 | 2.56 | 2.64 | 2.99 | 2.47 | 2.53 | 3.03 | 2.79 | 3.07 | 2.68 | 2.15 |
| SD | 0.49 | 0.53 | 0.67 | 0.85 | 0.73 | 0.64 | 1.08 | 0.76 | 1.05 | 1.07 | 0.71 | |
| Academic combined | Mean | 2.80 | 2.45 | 2.93 | 3.22 | 2.56 | 2.24 | 3.07 | 2.62 | 2.88 | 3.21 | 3.28 |
| SD | 0.54 | 0.63 | 0.66 | 0.89 | 0.82 | 0.72 | 1.16 | 0.95 | 1.14 | 1.10 | 1.26 | |
| Community combined | Mean | 2.79 | 2.61 | 2.66 | 3.14 | 2.60 | 2.68 | 3.03 | 2.72 | 2.95 | 2.82 | 2.34 |
| SD | 0.62 | 0.62 | 0.72 | 1.01 | 0.90 | 0.90 | 1.15 | 0.99 | 1.09 | 1.09 | 1.00 | |
| P value | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | 0.02 | >0.05 | >0.05 | >0.05 | >0.05 | <0.001 | |
Convergent, Concurrent, and Discriminant Validity Evidence
For every categorical increase on the question assessing overall morale, the personal morale score was 0.23 points higher (P < 0.001). For every categorical increase in a participant's perception of the group's morale, the personal morale score was 0.29 points higher (P < 0.001).
For every 1‐point increase in personal morale score, the odds of being highly invested in the group increased by 5 times (odds ratio [OR]: 5.23, 95% confidence interval [CI]: 1.91‐14.35, P = 0.001). The mean personal morale score for highly invested hospitalists was 2.92, whereas that of those less invested was 2.43 (diff. = 0.49, P < 0.001) (Table 3). Highly invested hospitalists had significantly higher importance factor scores for leadership (diff. = 0.08, P = 0.03) as well as appreciation and acknowledgement (diff. = 0.08, P = 0.02).
| Personal Morale Score | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical | Workload | Leadership | Appreciation and Acknowledgement | Material Rewards | Family Time | Institutional Climate | Job Security | Autonomy | Professional Growth | ||
| |||||||||||
| Highly invested in success of current hospitalist group | |||||||||||
| Mean | 2.92 | 2.61 | 2.89 | 3.38 | 2.78 | 2.45 | 3.21 | 2.78 | 2.86 | 3.10 | 2.95 |
| SD | 0.55 | 0.59 | 0.68 | 0.92 | 0.88 | 0.77 | 1.11 | 1.00 | 1.09 | 1.06 | 1.25 |
| Less invested in success of current hospitalist group | |||||||||||
| Mean | 2.43 | 2.34 | 2.48 | 2.60 | 2.02 | 2.57 | 2.60 | 2.38 | 3.08 | 2.69 | 2.24 |
| SD | 0.52 | 0.69 | 0.69 | 0.81 | 0.49 | 1.04 | 1.17 | 0.83 | 1.18 | 1.19 | 0.94 |
| P value | <0.001 | >0.05 | 0.02 | 0.001 | <0.001 | >0.05 | 0.03 | >0.05 | >0.05 | >0.05 | 0.02 |
| Not intending to leave because unhappy | |||||||||||
| Mean | 2.97 | 2.67 | 2.89 | 3.48 | 2.77 | 2.52 | 3.24 | 2.85 | 3.05 | 3.06 | 3.01 |
| SD | 0.51 | 0.54 | 0.61 | 0.91 | 0.89 | 0.78 | 1.03 | 0.99 | 1.10 | 1.07 | 1.25 |
| Intending to leave current group because unhappy | |||||||||||
| Mean | 2.45 | 2.30 | 2.59 | 2.59 | 2.21 | 2.40 | 2.68 | 2.33 | 2.67 | 2.88 | 2.28 |
| SD | 0.56 | 0.72 | 0.82 | 0.74 | 0.68 | 0.97 | 1.29 | 0.83 | 1.11 | 1.17 | 0.97 |
| P value | <0.001 | 0.01 | >0.05 | <0.001 | 0.003 | >0.05 | 0.03 | 0.01 | >0.05 | >0.05 | 0.01 |
Every 1‐point increase in personal morale was associated with a rise of 2.27 on the professional growth scale (P = 0.01). The correlation between these 2 scales was 0.26 (P = 0.01). Every 1‐point increase in personal morale was associated with a 2.21 point decrease on the Cohen stress scale (P > 0.05). The correlation between these 2 scales was 0.21 (P > 0.05).
Morale and Intent to Leave Due to Unhappiness
Sixteen (37%) academic and 18 (36%) community hospitalists reported having thoughts of leaving their current hospitalist program due to unhappiness. The mean personal morale score for hospitalists with no intent to leave their current group was 2.97, whereas that of those with intent to leave was 2.45 (diff. = 0.53, P < 0.001). Each 1‐point increase in the personal morale score was associated with an 85% decrease (OR: 0.15, 95% CI: 0.05‐0.41, P < 0.001) in the odds of leaving because of unhappiness. Holding self‐perception of being a career hospitalist constant, each 1‐point increase in the personal morale score was associated with an 83% decrease (OR: 0.17, 95% CI: 0.05‐0.51, P = 0.002) in the odds of leaving because of unhappiness. Hospitalists who reported intent to leave had significantly lower factor scores for all factors and items except workload, material reward, and autonomy than those who did not report intent to leave (Table 3). Within the academic groups, those who reported intent to leave had significantly lower scores for professional growth (diff. = 1.08, P = 0.01). For community groups, those who reported intent to leave had significantly lower scores for clinical work (diff. = 0.54, P = 0.003), workload (diff. = 0.50, P = 0.02), leadership (diff. = 1.19, P < 0.001), feeling appreciated and acknowledged (diff. = 0.68, P = 0.01), job security (diff. = 0.70, P = 0.03), and institutional climate (diff. = 0.67, P = 0.02) than those who did not report intent to leave.
DISCUSSION
The HMI is a validated tool that objectively measures and quantifies hospitalist morale. The HMI's capacity to comprehensively assess morale comes from its breadth and depth in uncovering work‐related areas that may be sources of contentment or displeasure. Furthermore, the fact that HMI scores varied among groups of individuals, including those who are thinking about leaving their hospitalist group because they are unhappy and those who are highly invested in their hospitalist group, speaks to its ability to highlight and account for what is most important to hospitalist providers.
Low employee morale has been associated with decreased productivity, increased absenteeism, increased turnover, and decreased patient satisfaction.[2, 26, 27, 28] A few frustrated workers can breed group discontentment and lower the entire group's morale.[28] In addition to its financial impact, departures due to low morale can be sudden and devastating, leading to loss of team cohesiveness, increased work burden on the remaining workforce, burnout, and cascades of more turnover.[2] In contrast, when morale is high, workers more commonly go the extra mile, are more committed to the organization's mission, and are more supportive of their coworkers.[28]
While we asked the informants about plans to leave their job, there are many factors that drive an individual's intent and ultimate decision to make changes in his or her employment. Some factors are outside the control of the employer or practice leaders, such as change in an individual's family life or desire and opportunity to pursue fellowship training. Others variables, however, are more directly tied to the job or practice environment. In a specialty where providers are relatively mobile and turnover is high, it is important for hospitalist practices to cultivate a climate in which the sacrifices associated with leaving outweigh the promised benefits.[29]
Results from the HMPWS suggested the need to address climate and fairness issues in hospitalist programs to improve satisfaction and retention.[9] Two large healthcare systems achieved success by investing in multipronged physician retention strategies including recruiting advisors, sign‐on bonuses, extensive onboarding, family support, and the promotion of ongoing effective communication.[3, 30]
Our findings suggest that morale for hospitalists is a complex amalgam of contentment and importance, and that there may not be a one size fits all solution to improving morale for all. While we did not find a difference in personal morale scores across individual hospitalist groups, or even between academic and community groups, each group had a unique profile with variability in the dynamics between importance and contentment of different factors. If practice group leaders review HMI data for their providers and use the information to facilitate meaningful dialogue with them about the factors influencing their morale, such leaders will have great insight into allocating resources for the best return on investment.
While we believe that the HMI is providing unique perspective compared to other commonly used metrics, it may be best to employ HMI data as complementary measures alongside that of some of the benchmarked scales that explore job satisfaction, job fit, and burnout among hospitalists.[6, 9, 10, 31, 32, 33, 34, 35] Aggregate HMI data at the group level may allow for the identification of factors that are highly important to morale but scored low in contentment. Such factors deserve priority and attention such that the subgroups within a practice can collaborate to come to consensus on strategies for amelioration. Because the HMI generates a score and profile for each provider, we can imagine effective leaders using the HMI with individuals as part of an annual review to facilitate discussion about maximizing contentment at work. Being fully transparent and sharing an honest nonanonymous version of the HMI with a superior would require a special relationship founded on trust and mutual respect.
Several limitations of this study should be considered. First, the initial item reduction and EFA were based on a single‐site survey, and our overall sample size was relatively small. We plan on expanding our sample size in the future for further validation of our exploratory findings. Second, the data were collected at 2 specific times several years ago. In continuing to analyze the data from subsequent years, validity and reliability results remain stable, thereby minimizing the likelihood of significant historical bias. Third, there may have been some recall bias, in that respondents may have overlooked the good and perseverated over variables that disappointed them. Fourth, although intention to leave does not necessarily equate actual employee turnover, intention has been found to be a strong predictor of quitting a job.[36, 37] Finally, while we had high response rates, response bias may have existed wherein those with lower morale may have elected not to complete the survey or became apathetic in their responses.
The HMI is a validated instrument that evaluates hospitalist morale by incorporating each provider's characterization of the importance of and contentment with 27 variables. By accounting for the multidimensional and dynamic nature of morale, the HMI may help program leaders tailor retention and engagement strategies specific to their own group. Future studies may explore trends in contributors to morale and examine whether interventions to augment low morale can result in improved morale and hospitalist retention.
Acknowledgements
The authors are indebted to the hospitalists who were willing to share their perspectives about their work, and grateful to Ms. Lisa Roberts, Ms. Barbara Brigade, and Ms. Regina Landis for insuring confidentiality in managing the survey database.
Disclosures: Dr. Chandra had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Wright is a Miller‐Coulson Family Scholar through the Johns Hopkins Center for Innovative Medicine. Ethical approval has been granted for studies involving human subjects by a Johns Hopkins University School of Medicine institutional review board. The authors report no conflicts of interest.
- 2014 State of Hospital Medicine Report. Philadelphia, PA: Society of Hospital Medicine; 2014.
- , , . A review of physician turnover: rates, causes, and consequences. Am J Med Qual. 2004;19(2):56–66.
- . Physician retention plans help reduce costs and optimize revenues. Healthc Financ Manage. 1998;52(1):75–77.
- SHM Career Satisfaction Task Force. A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction.; 2006. Available at: www.hospitalmedicine.org. Accessed February 28, 2009.
- , . Outcomes of physician job satisfaction: a narrative review, implications, and directions for future research. Health Care Manage Rev. 2003;28(2):119–139.
- , , , , . Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851–858.
- . Doing the same and earning less: male and female physicians in a new medical specialty. Inquiry. 2004;41(3):301–315.
- . Physician satisfaction and communication. National findings and best practices. Available at: http://www.pressganey.com/files/clark_cox_acpe_apr06.pdf. Accessed October 10, 2010.
- , , , , . Worklife and satisfaction of hospitalists: toward flourishing careers. J Gen Intern Med. 2012;27(1):28–36.
- , , , , ; Society of Hospital Medicine Career Satisfaction Task Force. Job characteristics, satisfaction, and burnout across hospitalist practice models. J Hosp Med. 2012;7(5):402–410.
- Morale | Define Morale at Dictionary.com. Morale | Define Morale at Dictionary.com. Morale | Define Morale at Dictionary.com. Available at: http://dictionary.reference.com/browse/morale. Accessed June 5, 2014.
- . Morale and satisfaction: a study in past‐future time perspective. Adm Sci Q. 1958:195–209.
- . Men and Women of the Corporation. 2nd ed. New York, NY: Basic Books; 1993.
- . The relation of morale to turnover among teachers. Am Educ Res J. 1965:163–173.
- . Structural and individual determinants of organization morale and satisfaction. Soc Forces. 1982;61:1088.
- , , . Morale matters: midlevel administrators and their intent to leave. J Higher Educ. 2000:34–59.
- . Factors influencing employee morale. Harv Bus Rev. 1950;28(1):61–73.
- . Dimensions of teacher morale. Am Educ Res J. 1970;7(2):221.
- , . The definition and measurement of employee morale. Adm Sci Q. 1958:157–184.
- , , , et al. Measuring physician job satisfaction in a changing workplace and a challenging environment. SGIM Career Satisfaction Study Group. Society of General Internal Medicine. Med Care. 1999;37(11):1174–1182.
- . Structural and individual determinants of organization morale and satisfaction. Soc Forces. 1983;61(4):1088–1108.
- . Morale and its measurement. Am J Sociol. 1941;47(3):406–414.
- , , , . Following morale over time within an academic hospitalist division. J Clin Outcomes Manag. 2011;18(1):21–26.
- , , , et al. Personal growth and its correlates during residency training. Med Educ. 2006;40(8):737–745.
- , , . A global measure of perceived stress. J Health Soc Behav. 1983:385–396.
- , , . Morale matters: midlevel administrators and their intent to leave. J Higher Educ. 2000;71(1):34–59.
- , . Faculty members' morale and their intention to leave: a multilevel explanation. J Higher Educ. 2002;73(4):518–542.
- , . Employee Morale. New York, NY: Palgrave Macmillan; 2009.
- , , , , . Silence Kills. Silence Kills: The Seven Crucial Conversations® for Healthcare. VitalSmarts™ in association with the American Association of Critical Care Nurses, USA. 2005. Accessed October 10, 2014.
- , , . The lifelong iterative process of physician retention. J Healthc Manag. 2009;54(4):220–226.
- . Physicians' burnout. Rev Prat. 2004;54(7):753–754.
- , , , , , . Work stress and health in primary health care physicians and hospital physicians. Occup Environ Med. 2008;65(5):364–366.
- , , , et al. Understanding physicians' intentions to withdraw from practice: the role of job satisfaction, job stress, mental and physical health. 2001. Health Care Manage Rev. 2010;35(2):105–115.
- , , , , , . Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358–1367.
- , . Burnout and Hospitalists: Etiology and Prevention. In: What Exactly Does A Hospitalist Do? Best of the Best Hospital Medicine 2005: Strategies for Success. Society of Hospital Medicine; 2005:5.
- , . Using job involvement and organizational commitment interactively to predict turnover. J Manage. 1989;15(1):115–127.
- , , , et al. Nurse turnover: a literature review. Int J Nurs Stud. 2006;43(2):237–263.
- 2014 State of Hospital Medicine Report. Philadelphia, PA: Society of Hospital Medicine; 2014.
- , , . A review of physician turnover: rates, causes, and consequences. Am J Med Qual. 2004;19(2):56–66.
- . Physician retention plans help reduce costs and optimize revenues. Healthc Financ Manage. 1998;52(1):75–77.
- SHM Career Satisfaction Task Force. A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction.; 2006. Available at: www.hospitalmedicine.org. Accessed February 28, 2009.
- , . Outcomes of physician job satisfaction: a narrative review, implications, and directions for future research. Health Care Manage Rev. 2003;28(2):119–139.
- , , , , . Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851–858.
- . Doing the same and earning less: male and female physicians in a new medical specialty. Inquiry. 2004;41(3):301–315.
- . Physician satisfaction and communication. National findings and best practices. Available at: http://www.pressganey.com/files/clark_cox_acpe_apr06.pdf. Accessed October 10, 2010.
- , , , , . Worklife and satisfaction of hospitalists: toward flourishing careers. J Gen Intern Med. 2012;27(1):28–36.
- , , , , ; Society of Hospital Medicine Career Satisfaction Task Force. Job characteristics, satisfaction, and burnout across hospitalist practice models. J Hosp Med. 2012;7(5):402–410.
- Morale | Define Morale at Dictionary.com. Morale | Define Morale at Dictionary.com. Morale | Define Morale at Dictionary.com. Available at: http://dictionary.reference.com/browse/morale. Accessed June 5, 2014.
- . Morale and satisfaction: a study in past‐future time perspective. Adm Sci Q. 1958:195–209.
- . Men and Women of the Corporation. 2nd ed. New York, NY: Basic Books; 1993.
- . The relation of morale to turnover among teachers. Am Educ Res J. 1965:163–173.
- . Structural and individual determinants of organization morale and satisfaction. Soc Forces. 1982;61:1088.
- , , . Morale matters: midlevel administrators and their intent to leave. J Higher Educ. 2000:34–59.
- . Factors influencing employee morale. Harv Bus Rev. 1950;28(1):61–73.
- . Dimensions of teacher morale. Am Educ Res J. 1970;7(2):221.
- , . The definition and measurement of employee morale. Adm Sci Q. 1958:157–184.
- , , , et al. Measuring physician job satisfaction in a changing workplace and a challenging environment. SGIM Career Satisfaction Study Group. Society of General Internal Medicine. Med Care. 1999;37(11):1174–1182.
- . Structural and individual determinants of organization morale and satisfaction. Soc Forces. 1983;61(4):1088–1108.
- . Morale and its measurement. Am J Sociol. 1941;47(3):406–414.
- , , , . Following morale over time within an academic hospitalist division. J Clin Outcomes Manag. 2011;18(1):21–26.
- , , , et al. Personal growth and its correlates during residency training. Med Educ. 2006;40(8):737–745.
- , , . A global measure of perceived stress. J Health Soc Behav. 1983:385–396.
- , , . Morale matters: midlevel administrators and their intent to leave. J Higher Educ. 2000;71(1):34–59.
- , . Faculty members' morale and their intention to leave: a multilevel explanation. J Higher Educ. 2002;73(4):518–542.
- , . Employee Morale. New York, NY: Palgrave Macmillan; 2009.
- , , , , . Silence Kills. Silence Kills: The Seven Crucial Conversations® for Healthcare. VitalSmarts™ in association with the American Association of Critical Care Nurses, USA. 2005. Accessed October 10, 2014.
- , , . The lifelong iterative process of physician retention. J Healthc Manag. 2009;54(4):220–226.
- . Physicians' burnout. Rev Prat. 2004;54(7):753–754.
- , , , , , . Work stress and health in primary health care physicians and hospital physicians. Occup Environ Med. 2008;65(5):364–366.
- , , , et al. Understanding physicians' intentions to withdraw from practice: the role of job satisfaction, job stress, mental and physical health. 2001. Health Care Manage Rev. 2010;35(2):105–115.
- , , , , , . Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358–1367.
- , . Burnout and Hospitalists: Etiology and Prevention. In: What Exactly Does A Hospitalist Do? Best of the Best Hospital Medicine 2005: Strategies for Success. Society of Hospital Medicine; 2005:5.
- , . Using job involvement and organizational commitment interactively to predict turnover. J Manage. 1989;15(1):115–127.
- , , , et al. Nurse turnover: a literature review. Int J Nurs Stud. 2006;43(2):237–263.
© 2016 Society of Hospital Medicine
Inpatient Mammography
Testing for breast cancer is traditionally offered in outpatient settings, and screening mammography rates have plateaued since 2000.[1] Current data suggest that the mammography utilization gap by race has narrowed; however, disparity remains among low‐income, uninsured, and underinsured populations.[2, 3] The lowest compliance with screening mammography recommendations have been reported among women with low income (63.2%), uninsured (50.4%), and those without a usual source of healthcare (43.6%).[4] Although socioeconomic status, access to the healthcare system, and awareness about screening benefits can all influence women's willingness to have screening, the most common reason that women report for not having mammograms were that no one recommended the test.[5, 6] These findings support previous reports that physicians' recommendations about the need for screening mammography is an influential factor in determining women's decisions related to compliance.[7] Hence, the role of healthcare providers in all clinical care settings is pivotal in reducing mammography utilization disparities.
A recent study evaluating the breast cancer screening adherence among the hospitalized women aged 50 to 75 years noted that many (60%) were low income (annual household income <$20,000), 39% were nonadherent, and 35% were at high risk of developing breast cancer.[8] Further, a majority of these hospitalized women were amenable to inpatient screening mammography if due and offered during the hospital stay.[8] As a follow‐up, the purpose of the current study was to explore how hospitalists feel about getting involved in breast cancer screening and ordering screening mammograms for hospitalized women. We hypothesized that a greater proportion of hospitalists would order mammography for hospitalized women who were both overdue for screening and at high risk for developing breast cancer if they fundamentally believe that they have a role in breast cancer screening. This study also explored anticipated barriers that may be of concern to hospitalists when ordering inpatient screening mammography.
METHODS
Study Design and Sample
All hospitalist providers within 4 groups affiliated with Johns Hopkins Medical Institution (Johns Hopkins Hospital, Johns Hopkins Bayview Medical Center, Howard County General Hospital, and Suburban Hospital) were approached for participation in this‐cross sectional study. The hospitalists included physicians, nurse practitioners, and physician assistants. All hospitalists were eligible to participate in the study, and there was no monetary incentive attached to the study participation. A total of 110 hospitalists were approached for study participation. Of these, 4 hospitalists (3.5%) declined to participate, leaving a study population of 106 hospitalists.
Data Collection and Measures
Participants were sent the survey via email using SurveyMonkey. The survey included questions regarding demographic information such as age, gender, race, and clinical experience in hospital medicine. To evaluate for potential personal sources of bias related to mammography, study participants were asked if they have had a family member diagnosed with breast cancer.
A central question asked whether respondents agreed with the following: I believe that hospitalists should be involved in breast cancer screening. The questionnaire also evaluated hospitalists' practical approaches to 2 clinical scenarios by soliciting decision about whether they would order an inpatient screening mammogram. These clinical scenarios were designed using the Gail risk prediction score for probability of developing breast cancer within the next 5 years according to the National Cancer Institute Breast Cancer Risk Tool.[9] Study participants were not provided with the Gail scores and had to infer the risk from the clinical information provided in scenarios. One case described a woman at high risk, and the other with a lower‐risk profile. The first question was: Would you order screening mammography for a 65‐year‐old African American female with obesity and family history for breast cancer admitted to the hospital for cellulitis? She has never had a mammogram and is willing to have it while in hospital. Based on the information provided in the scenario, the 5‐year risk prediction for developing breast cancer using the Gail risk model was high (2.1%). The second scenario asked: Would you order a screening mammography for a 62‐year‐old healthy Hispanic female admitted for presyncope? Patient is uninsured and requests a screening mammogram while in hospital [assume that personal and family histories for breast cancer are negative]. Based on the information provided in the scenario, the 5‐year risk prediction for developing breast cancer using the Gail risk model was low (0.6%).
Several questions regarding potential barriers to inpatient screening mammography were also asked. Some of these questions were based on barriers mentioned in our earlier study of patients,[8] whereas others emerged from a review of the literature and during focus group discussions with hospitalist providers. Pilot testing of the survey was conducted on hospitalists outside the study sample to enhance question clarity. This study was approved by our institutional review board.
Statistical Methods
Respondent characteristics are presented as proportions and means. Unpaired t tests and [2] tests were used to look for associations between demographic characteristics and responses to the question about whether they believe that they should be involved in breast cancer screening. The survey data were analyzed using the Stata statistical software package version 12.1 (StataCorp, College Station, TX).
RESULTS
Out of 106 study subjects willing to participate, 8 did not respond, yielding a response rate of 92%. The mean age of the study participants was 37.6 years, and 55% were female. Almost two‐thirds of study participants (59%) were faculty physicians at an academic hospital, and the average clinical experience as a hospitalist was 4.6 years. Study participants were diverse with respect to ethnicity, and only 30% reported having a family member with breast cancer (Table 1). Because breast cancer is a disease that affects primarily women, stratified analysis by gender showed that most of these characteristic were similar across genders, except fewer women were full time (76% vs 93%, P=0.04) and on the faculty (44% vs 77%, P=0.003).
| Characteristics* | All Participants (n=98) |
|---|---|
| |
| Age, y, mean (SD) | 37.6 (5.5) |
| Female, n (%) | 54 (55) |
| Race, n (%) | |
| Caucasian | 35 (36) |
| African American | 12 (12) |
| Asian | 32 (33) |
| Other | 13 (13) |
| Hospitalist experience, y, mean (SD) | 4.6 (3.5) |
| Full time, n (%) | 82 (84) |
| Family history of breast cancer, n (%) | 30 (30) |
| Faculty physician, n (%) | 58 (59) |
| Believe that hospitalists should be involved in breast cancer screening, n (%) | 35 (38) |
Only 38% believed that hospitalists should be involved with breast cancer screening. The most commonly cited concern related to ordering an inpatient screening mammography was follow‐up of the results of the mammography, followed by the test may not be covered by patient's insurance. As shown in Table 2, these concerns were not perceived differently among providers who believed that hospitalists should be involved in breast cancer screening as compared to those who do not. Demographic variables from Table 1 failed to discern any significant associations related to believing that hospitalists should be involved with breast cancer screening or with concerns about the barriers to screening presented in Table 2 (data not shown). As shown in Table 2, overall, 32% hospitalists were willing to order a screening mammography during a hospital stay for the scenario of the woman at high risk for developing breast cancer (5‐year risk prediction using Gail model 2.1%) and 33% for the low‐risk scenario (5‐year risk prediction using Gail model 0.6%).
| Concern About Screening* | Believe That Hospitalists Should Be Involved in Breast Cancer Screening (n=35) | Do Not Believe That Hospitalists Should Be Involved in Breast Cancer Screening (n=58) | P Value |
|---|---|---|---|
| |||
| Result follow‐up, agree/strongly agree, n (%) | 34 (97) | 51 (88) | 0.25 |
| Interference with patient care, agree/strongly agree, n (%) | 23 (67) | 27 (47) | 0.07 |
| Cost, agree/strongly agree, n (%) | 23 (66) | 28 (48) | 0.10 |
| Concern that the test will not be covered by patient's insurance, agree/strongly agree, n (%) | 23 (66) | 34 (59) | 0.50 |
| Not my responsibility to do cancer prevention, agree/strongly agree, n (%) | 7 (20) | 16 (28) | 0.57 |
| Response to clinical scenarios | |||
| Would order a screening mammogram in the hospital for a high‐risk woman [scenario 1: Gail risk model: 2.1%], n (%) | 23 (66) | 6 (10) | 0.0001 |
| Would order a screening mammography in the hospital for a low‐risk woman [scenario 2: Gail risk model: 0.6%], n (%) | 18 (51) | 13 (22) | 0.004 |
DISCUSSION
Our study suggests that most hospitalists do not believe that they should be involved in breast cancer screening for their hospitalized patients. This perspective was not influenced by either the physician gender, family history for breast cancer, or by the patient's level of risk for developing breast cancer. When patients are in the hospital, both the setting and the acute illness are known to promote reflection and consideration of self‐care.[10] With major healthcare system changes on the horizon and the passing of the Affordable Care Act, we are becoming teams of providers who are collectively responsible for optimal care delivery. It may be possible to increase breast cancer screening rates by educating our patients and offering inpatient screening mammography while they are in the hospital, particularly to those who are at high risk of developing breast cancer.
Physician recommendations for preventive health and screening have consistently been found to be among the strongest predictors of screening utilization.[11] This is the first study to our knowledge that has attempted to understand hospitalists' views and concerns about ordering screening tests to detect occult malignancy. Although addressing preventive care during a hospitalization may seem complex and difficult, helping these women understand their personal risk profile (eg, family history of breast cancer, use of estrogen, race, age, and genetic risk factors) may be what is needed for beginning to influence perspective that might ultimately translate into a willingness to undergo screening.[12, 13, 14] Such delivery of patient‐centered care is built on a foundation of shared decision‐making, which takes into account the patient's preferences, values, and wishes.[15]
Ordering screening mammography for hospitalized patients will require a deeper understanding of hospitalists' attitudes, because the way that these physicians feel about the tests utility will dramatically influence the way that this opportunity is presented to patients, and ultimately the patients' preference to have or forego testing. Our study results are consistent with another publication that highlighted incongruence between physicians' views and patients' preferences for screening practices.[8, 11] Concerns cited, such as interference with patient's acute care, deserve attention, because it may be possible to carry out the screening in ways and at times that do not interfere with treatment or prolong length of stay. Exploring this with a feasibility study will be necessary. Such an approach has been advocated by Trimble et al. for inpatient cervical cancer screening as an efficient strategy to target high‐risk, nonadherent women.[16]
The inpatient setting allows for the elimination of major barriers to screening (like transportation and remembering to get to screening appointments),[8] thereby actively facilitating this needed service. Costs associated with inpatient screening mammography may deter both hospitalists and patients from screening; however, some insurers and Medicare pay for the full cost of screening tests, irrespective of the clinical setting.[17] Further, as hospitals or accountable care organizations become responsible for total cost per beneficiary, screening costs will be preferable when compared with the expenses associated with later detection of pathology and caring for advanced disease states.
One might question whether the mortality benefit of screening mammography is comparable among hospitalized women (who are theoretically sicker and with shorter life expectancy) and those cared for in outpatient practices. Unfortunately, we do not yet know the answer to this question, because data for inpatient screening mammography are nonexistent, and currently this is not considered as a standard of care. However, one can expect the benefits to be similar, if not greater, when performed in the outpatient setting, if preliminary efforts are directed at those who are both nonadherent and at high risk for breast cancer. According to 1 study, increasing mammography utilization by 5% in our country would prevent 560 deaths from breast cancer each year.[18]
Several limitations of this study should be considered. First, this cross‐sectional study was conducted at hospitals associated with a single institution and the results may not be generalizable. Second, although physicians' concerns were explored in this study, we did not solicit input about the potential impact of prevention and screening on the nursing staff. Third, there may be concerns about the hypothetical nature of anchoring and possible framing effects with the 2 clinical scenarios. Finally, it is possible that the hospitalists' response may have been subject to social desirability bias. That said, the response to the key question Do you think hospitalists should be involved in breast cancer screening? do not support a socially desirable bias.
Given the current policy emphasis on reducing disparities in cancer screening, it may be reasonable to expand the role of all healthcare providers and healthcare facilities in screening high‐risk populations. Screening tests that may seem difficult to coordinate in hospitals currently may become easier as our hospitals evolve to become more patient centered. Future studies are needed to evaluate the feasibility and potential barriers to inpatient screening mammography.
Disclosure
Disclosures: Dr. Wright is a Miller‐Coulson Family Scholar, and this support comes from Hopkins Center for Innovative Medicine. This work was made possible in part by the Maryland Cigarette Restitution Fund Research Grant at Johns Hopkins. The authors report no conflicts of interest.
- Centers for Disease Control and Prevention (CDC). Vital signs: breast cancer screening among women aged 50–74 years—United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(26):813–816.
- American Cancer Society. Breast Cancer Facts 2013.
- , , , et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control. 2009;20:417–435.
- , , , ; Centers for Disease Control and Prevention. Breast cancer screening among adult women—behavioral risk factor surveillance system, United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61(suppl):46–50.
- , . Disparities in breast cancer. Curr Probl Cancer. 2007;31(3):134–156.
- , , . Factors associated with mammography utilization: a systematic quantitative review of the literature. J Womens Health (Larchmt). 2008;17:1477–1498.
- , , , et al. Processes of care in cervical and breast cancer screening and follow‐up: the importance of communication. Prev Med. 2004;39:81–90.
- , , , . Breast cancer screening preferences among hospitalized women. J Womens Health (Larchmt). 2013;22(7):637–642.
- , , , et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;8:1879–1886.
- , , , . Expanding the roles of hospitalist physicians to include public health. J Hosp Med. 2007;2:93–101.
- , , , et al. Colorectal cancer screening: conjoint analysis of consumer preferences and physicians' perceived consumer preferences in the US and Canada. Paper presented at: 27th Annual Meeting of the Society for Medical Decision Making; October 21–24, 2005; San Francisco, CA.
- , , . Family history of breast cancer: impact on the disease experience. Cancer Pract. 2000;8:135–142.
- , , , . Breast cancer knowledge and attitudes toward mammography as predictors of breast cancer preventive behavior in Kazakh, Korean, and Russian women in Kazakhstan. Int J Public Health. 2008;53:123–130.
- , , , , . The relation between projected breast cancer risk, perceived cancer risk, and mammography use. Results from the National Health Interview Survey. J Gen Intern Med. 2006;21:158–164.
- , . Patient‐centered communication in cancer care: promoting healing and reducing suffering. NIH publication no. 07‐6225. Bethesda, MD: National Cancer Institute, 2007.
- , , , , , . Effectiveness of screening for cervical cancer in an inpatient hospital setting. Obstet Gynecol. 2004;103(2):310–316.
- Centers for Medicare 38:600–609.
Testing for breast cancer is traditionally offered in outpatient settings, and screening mammography rates have plateaued since 2000.[1] Current data suggest that the mammography utilization gap by race has narrowed; however, disparity remains among low‐income, uninsured, and underinsured populations.[2, 3] The lowest compliance with screening mammography recommendations have been reported among women with low income (63.2%), uninsured (50.4%), and those without a usual source of healthcare (43.6%).[4] Although socioeconomic status, access to the healthcare system, and awareness about screening benefits can all influence women's willingness to have screening, the most common reason that women report for not having mammograms were that no one recommended the test.[5, 6] These findings support previous reports that physicians' recommendations about the need for screening mammography is an influential factor in determining women's decisions related to compliance.[7] Hence, the role of healthcare providers in all clinical care settings is pivotal in reducing mammography utilization disparities.
A recent study evaluating the breast cancer screening adherence among the hospitalized women aged 50 to 75 years noted that many (60%) were low income (annual household income <$20,000), 39% were nonadherent, and 35% were at high risk of developing breast cancer.[8] Further, a majority of these hospitalized women were amenable to inpatient screening mammography if due and offered during the hospital stay.[8] As a follow‐up, the purpose of the current study was to explore how hospitalists feel about getting involved in breast cancer screening and ordering screening mammograms for hospitalized women. We hypothesized that a greater proportion of hospitalists would order mammography for hospitalized women who were both overdue for screening and at high risk for developing breast cancer if they fundamentally believe that they have a role in breast cancer screening. This study also explored anticipated barriers that may be of concern to hospitalists when ordering inpatient screening mammography.
METHODS
Study Design and Sample
All hospitalist providers within 4 groups affiliated with Johns Hopkins Medical Institution (Johns Hopkins Hospital, Johns Hopkins Bayview Medical Center, Howard County General Hospital, and Suburban Hospital) were approached for participation in this‐cross sectional study. The hospitalists included physicians, nurse practitioners, and physician assistants. All hospitalists were eligible to participate in the study, and there was no monetary incentive attached to the study participation. A total of 110 hospitalists were approached for study participation. Of these, 4 hospitalists (3.5%) declined to participate, leaving a study population of 106 hospitalists.
Data Collection and Measures
Participants were sent the survey via email using SurveyMonkey. The survey included questions regarding demographic information such as age, gender, race, and clinical experience in hospital medicine. To evaluate for potential personal sources of bias related to mammography, study participants were asked if they have had a family member diagnosed with breast cancer.
A central question asked whether respondents agreed with the following: I believe that hospitalists should be involved in breast cancer screening. The questionnaire also evaluated hospitalists' practical approaches to 2 clinical scenarios by soliciting decision about whether they would order an inpatient screening mammogram. These clinical scenarios were designed using the Gail risk prediction score for probability of developing breast cancer within the next 5 years according to the National Cancer Institute Breast Cancer Risk Tool.[9] Study participants were not provided with the Gail scores and had to infer the risk from the clinical information provided in scenarios. One case described a woman at high risk, and the other with a lower‐risk profile. The first question was: Would you order screening mammography for a 65‐year‐old African American female with obesity and family history for breast cancer admitted to the hospital for cellulitis? She has never had a mammogram and is willing to have it while in hospital. Based on the information provided in the scenario, the 5‐year risk prediction for developing breast cancer using the Gail risk model was high (2.1%). The second scenario asked: Would you order a screening mammography for a 62‐year‐old healthy Hispanic female admitted for presyncope? Patient is uninsured and requests a screening mammogram while in hospital [assume that personal and family histories for breast cancer are negative]. Based on the information provided in the scenario, the 5‐year risk prediction for developing breast cancer using the Gail risk model was low (0.6%).
Several questions regarding potential barriers to inpatient screening mammography were also asked. Some of these questions were based on barriers mentioned in our earlier study of patients,[8] whereas others emerged from a review of the literature and during focus group discussions with hospitalist providers. Pilot testing of the survey was conducted on hospitalists outside the study sample to enhance question clarity. This study was approved by our institutional review board.
Statistical Methods
Respondent characteristics are presented as proportions and means. Unpaired t tests and [2] tests were used to look for associations between demographic characteristics and responses to the question about whether they believe that they should be involved in breast cancer screening. The survey data were analyzed using the Stata statistical software package version 12.1 (StataCorp, College Station, TX).
RESULTS
Out of 106 study subjects willing to participate, 8 did not respond, yielding a response rate of 92%. The mean age of the study participants was 37.6 years, and 55% were female. Almost two‐thirds of study participants (59%) were faculty physicians at an academic hospital, and the average clinical experience as a hospitalist was 4.6 years. Study participants were diverse with respect to ethnicity, and only 30% reported having a family member with breast cancer (Table 1). Because breast cancer is a disease that affects primarily women, stratified analysis by gender showed that most of these characteristic were similar across genders, except fewer women were full time (76% vs 93%, P=0.04) and on the faculty (44% vs 77%, P=0.003).
| Characteristics* | All Participants (n=98) |
|---|---|
| |
| Age, y, mean (SD) | 37.6 (5.5) |
| Female, n (%) | 54 (55) |
| Race, n (%) | |
| Caucasian | 35 (36) |
| African American | 12 (12) |
| Asian | 32 (33) |
| Other | 13 (13) |
| Hospitalist experience, y, mean (SD) | 4.6 (3.5) |
| Full time, n (%) | 82 (84) |
| Family history of breast cancer, n (%) | 30 (30) |
| Faculty physician, n (%) | 58 (59) |
| Believe that hospitalists should be involved in breast cancer screening, n (%) | 35 (38) |
Only 38% believed that hospitalists should be involved with breast cancer screening. The most commonly cited concern related to ordering an inpatient screening mammography was follow‐up of the results of the mammography, followed by the test may not be covered by patient's insurance. As shown in Table 2, these concerns were not perceived differently among providers who believed that hospitalists should be involved in breast cancer screening as compared to those who do not. Demographic variables from Table 1 failed to discern any significant associations related to believing that hospitalists should be involved with breast cancer screening or with concerns about the barriers to screening presented in Table 2 (data not shown). As shown in Table 2, overall, 32% hospitalists were willing to order a screening mammography during a hospital stay for the scenario of the woman at high risk for developing breast cancer (5‐year risk prediction using Gail model 2.1%) and 33% for the low‐risk scenario (5‐year risk prediction using Gail model 0.6%).
| Concern About Screening* | Believe That Hospitalists Should Be Involved in Breast Cancer Screening (n=35) | Do Not Believe That Hospitalists Should Be Involved in Breast Cancer Screening (n=58) | P Value |
|---|---|---|---|
| |||
| Result follow‐up, agree/strongly agree, n (%) | 34 (97) | 51 (88) | 0.25 |
| Interference with patient care, agree/strongly agree, n (%) | 23 (67) | 27 (47) | 0.07 |
| Cost, agree/strongly agree, n (%) | 23 (66) | 28 (48) | 0.10 |
| Concern that the test will not be covered by patient's insurance, agree/strongly agree, n (%) | 23 (66) | 34 (59) | 0.50 |
| Not my responsibility to do cancer prevention, agree/strongly agree, n (%) | 7 (20) | 16 (28) | 0.57 |
| Response to clinical scenarios | |||
| Would order a screening mammogram in the hospital for a high‐risk woman [scenario 1: Gail risk model: 2.1%], n (%) | 23 (66) | 6 (10) | 0.0001 |
| Would order a screening mammography in the hospital for a low‐risk woman [scenario 2: Gail risk model: 0.6%], n (%) | 18 (51) | 13 (22) | 0.004 |
DISCUSSION
Our study suggests that most hospitalists do not believe that they should be involved in breast cancer screening for their hospitalized patients. This perspective was not influenced by either the physician gender, family history for breast cancer, or by the patient's level of risk for developing breast cancer. When patients are in the hospital, both the setting and the acute illness are known to promote reflection and consideration of self‐care.[10] With major healthcare system changes on the horizon and the passing of the Affordable Care Act, we are becoming teams of providers who are collectively responsible for optimal care delivery. It may be possible to increase breast cancer screening rates by educating our patients and offering inpatient screening mammography while they are in the hospital, particularly to those who are at high risk of developing breast cancer.
Physician recommendations for preventive health and screening have consistently been found to be among the strongest predictors of screening utilization.[11] This is the first study to our knowledge that has attempted to understand hospitalists' views and concerns about ordering screening tests to detect occult malignancy. Although addressing preventive care during a hospitalization may seem complex and difficult, helping these women understand their personal risk profile (eg, family history of breast cancer, use of estrogen, race, age, and genetic risk factors) may be what is needed for beginning to influence perspective that might ultimately translate into a willingness to undergo screening.[12, 13, 14] Such delivery of patient‐centered care is built on a foundation of shared decision‐making, which takes into account the patient's preferences, values, and wishes.[15]
Ordering screening mammography for hospitalized patients will require a deeper understanding of hospitalists' attitudes, because the way that these physicians feel about the tests utility will dramatically influence the way that this opportunity is presented to patients, and ultimately the patients' preference to have or forego testing. Our study results are consistent with another publication that highlighted incongruence between physicians' views and patients' preferences for screening practices.[8, 11] Concerns cited, such as interference with patient's acute care, deserve attention, because it may be possible to carry out the screening in ways and at times that do not interfere with treatment or prolong length of stay. Exploring this with a feasibility study will be necessary. Such an approach has been advocated by Trimble et al. for inpatient cervical cancer screening as an efficient strategy to target high‐risk, nonadherent women.[16]
The inpatient setting allows for the elimination of major barriers to screening (like transportation and remembering to get to screening appointments),[8] thereby actively facilitating this needed service. Costs associated with inpatient screening mammography may deter both hospitalists and patients from screening; however, some insurers and Medicare pay for the full cost of screening tests, irrespective of the clinical setting.[17] Further, as hospitals or accountable care organizations become responsible for total cost per beneficiary, screening costs will be preferable when compared with the expenses associated with later detection of pathology and caring for advanced disease states.
One might question whether the mortality benefit of screening mammography is comparable among hospitalized women (who are theoretically sicker and with shorter life expectancy) and those cared for in outpatient practices. Unfortunately, we do not yet know the answer to this question, because data for inpatient screening mammography are nonexistent, and currently this is not considered as a standard of care. However, one can expect the benefits to be similar, if not greater, when performed in the outpatient setting, if preliminary efforts are directed at those who are both nonadherent and at high risk for breast cancer. According to 1 study, increasing mammography utilization by 5% in our country would prevent 560 deaths from breast cancer each year.[18]
Several limitations of this study should be considered. First, this cross‐sectional study was conducted at hospitals associated with a single institution and the results may not be generalizable. Second, although physicians' concerns were explored in this study, we did not solicit input about the potential impact of prevention and screening on the nursing staff. Third, there may be concerns about the hypothetical nature of anchoring and possible framing effects with the 2 clinical scenarios. Finally, it is possible that the hospitalists' response may have been subject to social desirability bias. That said, the response to the key question Do you think hospitalists should be involved in breast cancer screening? do not support a socially desirable bias.
Given the current policy emphasis on reducing disparities in cancer screening, it may be reasonable to expand the role of all healthcare providers and healthcare facilities in screening high‐risk populations. Screening tests that may seem difficult to coordinate in hospitals currently may become easier as our hospitals evolve to become more patient centered. Future studies are needed to evaluate the feasibility and potential barriers to inpatient screening mammography.
Disclosure
Disclosures: Dr. Wright is a Miller‐Coulson Family Scholar, and this support comes from Hopkins Center for Innovative Medicine. This work was made possible in part by the Maryland Cigarette Restitution Fund Research Grant at Johns Hopkins. The authors report no conflicts of interest.
Testing for breast cancer is traditionally offered in outpatient settings, and screening mammography rates have plateaued since 2000.[1] Current data suggest that the mammography utilization gap by race has narrowed; however, disparity remains among low‐income, uninsured, and underinsured populations.[2, 3] The lowest compliance with screening mammography recommendations have been reported among women with low income (63.2%), uninsured (50.4%), and those without a usual source of healthcare (43.6%).[4] Although socioeconomic status, access to the healthcare system, and awareness about screening benefits can all influence women's willingness to have screening, the most common reason that women report for not having mammograms were that no one recommended the test.[5, 6] These findings support previous reports that physicians' recommendations about the need for screening mammography is an influential factor in determining women's decisions related to compliance.[7] Hence, the role of healthcare providers in all clinical care settings is pivotal in reducing mammography utilization disparities.
A recent study evaluating the breast cancer screening adherence among the hospitalized women aged 50 to 75 years noted that many (60%) were low income (annual household income <$20,000), 39% were nonadherent, and 35% were at high risk of developing breast cancer.[8] Further, a majority of these hospitalized women were amenable to inpatient screening mammography if due and offered during the hospital stay.[8] As a follow‐up, the purpose of the current study was to explore how hospitalists feel about getting involved in breast cancer screening and ordering screening mammograms for hospitalized women. We hypothesized that a greater proportion of hospitalists would order mammography for hospitalized women who were both overdue for screening and at high risk for developing breast cancer if they fundamentally believe that they have a role in breast cancer screening. This study also explored anticipated barriers that may be of concern to hospitalists when ordering inpatient screening mammography.
METHODS
Study Design and Sample
All hospitalist providers within 4 groups affiliated with Johns Hopkins Medical Institution (Johns Hopkins Hospital, Johns Hopkins Bayview Medical Center, Howard County General Hospital, and Suburban Hospital) were approached for participation in this‐cross sectional study. The hospitalists included physicians, nurse practitioners, and physician assistants. All hospitalists were eligible to participate in the study, and there was no monetary incentive attached to the study participation. A total of 110 hospitalists were approached for study participation. Of these, 4 hospitalists (3.5%) declined to participate, leaving a study population of 106 hospitalists.
Data Collection and Measures
Participants were sent the survey via email using SurveyMonkey. The survey included questions regarding demographic information such as age, gender, race, and clinical experience in hospital medicine. To evaluate for potential personal sources of bias related to mammography, study participants were asked if they have had a family member diagnosed with breast cancer.
A central question asked whether respondents agreed with the following: I believe that hospitalists should be involved in breast cancer screening. The questionnaire also evaluated hospitalists' practical approaches to 2 clinical scenarios by soliciting decision about whether they would order an inpatient screening mammogram. These clinical scenarios were designed using the Gail risk prediction score for probability of developing breast cancer within the next 5 years according to the National Cancer Institute Breast Cancer Risk Tool.[9] Study participants were not provided with the Gail scores and had to infer the risk from the clinical information provided in scenarios. One case described a woman at high risk, and the other with a lower‐risk profile. The first question was: Would you order screening mammography for a 65‐year‐old African American female with obesity and family history for breast cancer admitted to the hospital for cellulitis? She has never had a mammogram and is willing to have it while in hospital. Based on the information provided in the scenario, the 5‐year risk prediction for developing breast cancer using the Gail risk model was high (2.1%). The second scenario asked: Would you order a screening mammography for a 62‐year‐old healthy Hispanic female admitted for presyncope? Patient is uninsured and requests a screening mammogram while in hospital [assume that personal and family histories for breast cancer are negative]. Based on the information provided in the scenario, the 5‐year risk prediction for developing breast cancer using the Gail risk model was low (0.6%).
Several questions regarding potential barriers to inpatient screening mammography were also asked. Some of these questions were based on barriers mentioned in our earlier study of patients,[8] whereas others emerged from a review of the literature and during focus group discussions with hospitalist providers. Pilot testing of the survey was conducted on hospitalists outside the study sample to enhance question clarity. This study was approved by our institutional review board.
Statistical Methods
Respondent characteristics are presented as proportions and means. Unpaired t tests and [2] tests were used to look for associations between demographic characteristics and responses to the question about whether they believe that they should be involved in breast cancer screening. The survey data were analyzed using the Stata statistical software package version 12.1 (StataCorp, College Station, TX).
RESULTS
Out of 106 study subjects willing to participate, 8 did not respond, yielding a response rate of 92%. The mean age of the study participants was 37.6 years, and 55% were female. Almost two‐thirds of study participants (59%) were faculty physicians at an academic hospital, and the average clinical experience as a hospitalist was 4.6 years. Study participants were diverse with respect to ethnicity, and only 30% reported having a family member with breast cancer (Table 1). Because breast cancer is a disease that affects primarily women, stratified analysis by gender showed that most of these characteristic were similar across genders, except fewer women were full time (76% vs 93%, P=0.04) and on the faculty (44% vs 77%, P=0.003).
| Characteristics* | All Participants (n=98) |
|---|---|
| |
| Age, y, mean (SD) | 37.6 (5.5) |
| Female, n (%) | 54 (55) |
| Race, n (%) | |
| Caucasian | 35 (36) |
| African American | 12 (12) |
| Asian | 32 (33) |
| Other | 13 (13) |
| Hospitalist experience, y, mean (SD) | 4.6 (3.5) |
| Full time, n (%) | 82 (84) |
| Family history of breast cancer, n (%) | 30 (30) |
| Faculty physician, n (%) | 58 (59) |
| Believe that hospitalists should be involved in breast cancer screening, n (%) | 35 (38) |
Only 38% believed that hospitalists should be involved with breast cancer screening. The most commonly cited concern related to ordering an inpatient screening mammography was follow‐up of the results of the mammography, followed by the test may not be covered by patient's insurance. As shown in Table 2, these concerns were not perceived differently among providers who believed that hospitalists should be involved in breast cancer screening as compared to those who do not. Demographic variables from Table 1 failed to discern any significant associations related to believing that hospitalists should be involved with breast cancer screening or with concerns about the barriers to screening presented in Table 2 (data not shown). As shown in Table 2, overall, 32% hospitalists were willing to order a screening mammography during a hospital stay for the scenario of the woman at high risk for developing breast cancer (5‐year risk prediction using Gail model 2.1%) and 33% for the low‐risk scenario (5‐year risk prediction using Gail model 0.6%).
| Concern About Screening* | Believe That Hospitalists Should Be Involved in Breast Cancer Screening (n=35) | Do Not Believe That Hospitalists Should Be Involved in Breast Cancer Screening (n=58) | P Value |
|---|---|---|---|
| |||
| Result follow‐up, agree/strongly agree, n (%) | 34 (97) | 51 (88) | 0.25 |
| Interference with patient care, agree/strongly agree, n (%) | 23 (67) | 27 (47) | 0.07 |
| Cost, agree/strongly agree, n (%) | 23 (66) | 28 (48) | 0.10 |
| Concern that the test will not be covered by patient's insurance, agree/strongly agree, n (%) | 23 (66) | 34 (59) | 0.50 |
| Not my responsibility to do cancer prevention, agree/strongly agree, n (%) | 7 (20) | 16 (28) | 0.57 |
| Response to clinical scenarios | |||
| Would order a screening mammogram in the hospital for a high‐risk woman [scenario 1: Gail risk model: 2.1%], n (%) | 23 (66) | 6 (10) | 0.0001 |
| Would order a screening mammography in the hospital for a low‐risk woman [scenario 2: Gail risk model: 0.6%], n (%) | 18 (51) | 13 (22) | 0.004 |
DISCUSSION
Our study suggests that most hospitalists do not believe that they should be involved in breast cancer screening for their hospitalized patients. This perspective was not influenced by either the physician gender, family history for breast cancer, or by the patient's level of risk for developing breast cancer. When patients are in the hospital, both the setting and the acute illness are known to promote reflection and consideration of self‐care.[10] With major healthcare system changes on the horizon and the passing of the Affordable Care Act, we are becoming teams of providers who are collectively responsible for optimal care delivery. It may be possible to increase breast cancer screening rates by educating our patients and offering inpatient screening mammography while they are in the hospital, particularly to those who are at high risk of developing breast cancer.
Physician recommendations for preventive health and screening have consistently been found to be among the strongest predictors of screening utilization.[11] This is the first study to our knowledge that has attempted to understand hospitalists' views and concerns about ordering screening tests to detect occult malignancy. Although addressing preventive care during a hospitalization may seem complex and difficult, helping these women understand their personal risk profile (eg, family history of breast cancer, use of estrogen, race, age, and genetic risk factors) may be what is needed for beginning to influence perspective that might ultimately translate into a willingness to undergo screening.[12, 13, 14] Such delivery of patient‐centered care is built on a foundation of shared decision‐making, which takes into account the patient's preferences, values, and wishes.[15]
Ordering screening mammography for hospitalized patients will require a deeper understanding of hospitalists' attitudes, because the way that these physicians feel about the tests utility will dramatically influence the way that this opportunity is presented to patients, and ultimately the patients' preference to have or forego testing. Our study results are consistent with another publication that highlighted incongruence between physicians' views and patients' preferences for screening practices.[8, 11] Concerns cited, such as interference with patient's acute care, deserve attention, because it may be possible to carry out the screening in ways and at times that do not interfere with treatment or prolong length of stay. Exploring this with a feasibility study will be necessary. Such an approach has been advocated by Trimble et al. for inpatient cervical cancer screening as an efficient strategy to target high‐risk, nonadherent women.[16]
The inpatient setting allows for the elimination of major barriers to screening (like transportation and remembering to get to screening appointments),[8] thereby actively facilitating this needed service. Costs associated with inpatient screening mammography may deter both hospitalists and patients from screening; however, some insurers and Medicare pay for the full cost of screening tests, irrespective of the clinical setting.[17] Further, as hospitals or accountable care organizations become responsible for total cost per beneficiary, screening costs will be preferable when compared with the expenses associated with later detection of pathology and caring for advanced disease states.
One might question whether the mortality benefit of screening mammography is comparable among hospitalized women (who are theoretically sicker and with shorter life expectancy) and those cared for in outpatient practices. Unfortunately, we do not yet know the answer to this question, because data for inpatient screening mammography are nonexistent, and currently this is not considered as a standard of care. However, one can expect the benefits to be similar, if not greater, when performed in the outpatient setting, if preliminary efforts are directed at those who are both nonadherent and at high risk for breast cancer. According to 1 study, increasing mammography utilization by 5% in our country would prevent 560 deaths from breast cancer each year.[18]
Several limitations of this study should be considered. First, this cross‐sectional study was conducted at hospitals associated with a single institution and the results may not be generalizable. Second, although physicians' concerns were explored in this study, we did not solicit input about the potential impact of prevention and screening on the nursing staff. Third, there may be concerns about the hypothetical nature of anchoring and possible framing effects with the 2 clinical scenarios. Finally, it is possible that the hospitalists' response may have been subject to social desirability bias. That said, the response to the key question Do you think hospitalists should be involved in breast cancer screening? do not support a socially desirable bias.
Given the current policy emphasis on reducing disparities in cancer screening, it may be reasonable to expand the role of all healthcare providers and healthcare facilities in screening high‐risk populations. Screening tests that may seem difficult to coordinate in hospitals currently may become easier as our hospitals evolve to become more patient centered. Future studies are needed to evaluate the feasibility and potential barriers to inpatient screening mammography.
Disclosure
Disclosures: Dr. Wright is a Miller‐Coulson Family Scholar, and this support comes from Hopkins Center for Innovative Medicine. This work was made possible in part by the Maryland Cigarette Restitution Fund Research Grant at Johns Hopkins. The authors report no conflicts of interest.
- Centers for Disease Control and Prevention (CDC). Vital signs: breast cancer screening among women aged 50–74 years—United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(26):813–816.
- American Cancer Society. Breast Cancer Facts 2013.
- , , , et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control. 2009;20:417–435.
- , , , ; Centers for Disease Control and Prevention. Breast cancer screening among adult women—behavioral risk factor surveillance system, United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61(suppl):46–50.
- , . Disparities in breast cancer. Curr Probl Cancer. 2007;31(3):134–156.
- , , . Factors associated with mammography utilization: a systematic quantitative review of the literature. J Womens Health (Larchmt). 2008;17:1477–1498.
- , , , et al. Processes of care in cervical and breast cancer screening and follow‐up: the importance of communication. Prev Med. 2004;39:81–90.
- , , , . Breast cancer screening preferences among hospitalized women. J Womens Health (Larchmt). 2013;22(7):637–642.
- , , , et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;8:1879–1886.
- , , , . Expanding the roles of hospitalist physicians to include public health. J Hosp Med. 2007;2:93–101.
- , , , et al. Colorectal cancer screening: conjoint analysis of consumer preferences and physicians' perceived consumer preferences in the US and Canada. Paper presented at: 27th Annual Meeting of the Society for Medical Decision Making; October 21–24, 2005; San Francisco, CA.
- , , . Family history of breast cancer: impact on the disease experience. Cancer Pract. 2000;8:135–142.
- , , , . Breast cancer knowledge and attitudes toward mammography as predictors of breast cancer preventive behavior in Kazakh, Korean, and Russian women in Kazakhstan. Int J Public Health. 2008;53:123–130.
- , , , , . The relation between projected breast cancer risk, perceived cancer risk, and mammography use. Results from the National Health Interview Survey. J Gen Intern Med. 2006;21:158–164.
- , . Patient‐centered communication in cancer care: promoting healing and reducing suffering. NIH publication no. 07‐6225. Bethesda, MD: National Cancer Institute, 2007.
- , , , , , . Effectiveness of screening for cervical cancer in an inpatient hospital setting. Obstet Gynecol. 2004;103(2):310–316.
- Centers for Medicare 38:600–609.
- Centers for Disease Control and Prevention (CDC). Vital signs: breast cancer screening among women aged 50–74 years—United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(26):813–816.
- American Cancer Society. Breast Cancer Facts 2013.
- , , , et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control. 2009;20:417–435.
- , , , ; Centers for Disease Control and Prevention. Breast cancer screening among adult women—behavioral risk factor surveillance system, United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61(suppl):46–50.
- , . Disparities in breast cancer. Curr Probl Cancer. 2007;31(3):134–156.
- , , . Factors associated with mammography utilization: a systematic quantitative review of the literature. J Womens Health (Larchmt). 2008;17:1477–1498.
- , , , et al. Processes of care in cervical and breast cancer screening and follow‐up: the importance of communication. Prev Med. 2004;39:81–90.
- , , , . Breast cancer screening preferences among hospitalized women. J Womens Health (Larchmt). 2013;22(7):637–642.
- , , , et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;8:1879–1886.
- , , , . Expanding the roles of hospitalist physicians to include public health. J Hosp Med. 2007;2:93–101.
- , , , et al. Colorectal cancer screening: conjoint analysis of consumer preferences and physicians' perceived consumer preferences in the US and Canada. Paper presented at: 27th Annual Meeting of the Society for Medical Decision Making; October 21–24, 2005; San Francisco, CA.
- , , . Family history of breast cancer: impact on the disease experience. Cancer Pract. 2000;8:135–142.
- , , , . Breast cancer knowledge and attitudes toward mammography as predictors of breast cancer preventive behavior in Kazakh, Korean, and Russian women in Kazakhstan. Int J Public Health. 2008;53:123–130.
- , , , , . The relation between projected breast cancer risk, perceived cancer risk, and mammography use. Results from the National Health Interview Survey. J Gen Intern Med. 2006;21:158–164.
- , . Patient‐centered communication in cancer care: promoting healing and reducing suffering. NIH publication no. 07‐6225. Bethesda, MD: National Cancer Institute, 2007.
- , , , , , . Effectiveness of screening for cervical cancer in an inpatient hospital setting. Obstet Gynecol. 2004;103(2):310–316.
- Centers for Medicare 38:600–609.
© 2015 Society of Hospital Medicine
RIP Conference Provides Peer Mentoring
The research‐in‐progress (RIP) conference is commonplace in academia, but there are no studies that objectively characterize its value. Bringing faculty together away from revenue‐generating activities carries a significant cost. As such, measuring the success of such gatherings is necessary.
Mentors are an invaluable influence on the careers of junior faculty members, helping them to produce high‐quality research.13 Unfortunately, some divisions lack mentorship to support the academic needs of less experienced faculty.1 Peer mentorship may be a solution. RIP sessions represent an opportunity to intentionally formalize peer mentoring. Further, these sessions can facilitate collaborations as individuals become aware of colleagues' interests. The goal of this study was to assess the value of the research‐in‐progress conference initiated within the hospitalist division at our institution.
Methods
Study Design
This cohort study was conducted to evaluate the value of the RIP conference among hospitalists in our division and the academic outcomes of the projects.
Setting and Participants
The study took place at Johns Hopkins Bayview Medical Center (JHBMC), a 335‐bed university‐affiliated medical center in Baltimore, Maryland. The hospitalist division consists of faculty physicians, nurse practitioners, and physician assistants (20.06 FTE physicians and 7.41 FTE midlevel providers). Twelve (54%) of our faculty members are female, and the mean age of providers is 35.7 years. The providers have been practicing hospitalist medicine for 3.0 years on average; 2 (9%) are clinical associates, 16 (73%) are instructors, and 3 (14%) are assistant professors.
All faculty members presenting at the RIP session were members of the division. A senior faculty member (a professor in the Division of General Internal Medicine) helps to coordinate the conference. The group's research assistant was present at the sessions and was charged with data collection and collation.
The Johns Hopkins University institutional review board approved the study.
The Research in Progress Conference
During the 2009 academic year, our division held 15 RIP sessions. At each session, 1 faculty member presented a research proposal. The goal of each session was to provide a forum where faculty members could share their research ideas (specific aims, hypotheses, planned design, outcome measures, analytic plans, and preliminary results [if applicable]) in order to receive feedback. The senior faculty member met with the presenter prior to each session in order to: (1) ensure that half the RIP time was reserved for discussion and (2) review the presenter's goals so these would be made explicit to peers. The coordinator of the RIP conference facilitated the discussion, solicited input from all attendees, and encouraged constructive criticism.
Evaluation, Data Collection, and Analysis
At the end of each session, attendees (who were exclusively members of the hospitalist division) were asked to complete an anonymous survey. The 1‐page instrument was designed (1) with input from curriculum development experts4 and (2) after a review of the literature about RIP conferences. These steps conferred content validity to the instrument, which assessed perceptions about the session's quality and what was learned. Five‐point Likert scales were used to characterize the conference's success in several areas, including being intellectually/professionally stimulating and keeping them apprised of their colleagues' interests. The survey also assessed the participatory nature of the conference (balance of presentation vs discussion), its climate (extremely critical vs extremely supportive), and how the conference assisted the presenter. The presenters completed a distinct survey related to how helpful the conference was in improving/enhancing their projects. A final open‐ended section invited additional comments. The instrument was piloted and iteratively revised before its use in this study.
For the projects presented, we assessed the percentage that resulted in a peer‐reviewed publication or a presentation at a national meeting.
Results
The mean number of attendees at the RIP sessions was 9.6 persons. A total of 143 evaluations were completed. All 15 presenters (100%) completed their assessments. The research ideas presented spanned a breadth of topics in clinical research, quality improvement, policy, and professional development (Table 1).
| Session | Date | Presenter | Topic | Evaluations Completed |
|---|---|---|---|---|
| 1 | 7/2008 | Dr. CS | Hospital medicine in Canada versus the United States | 7 |
| 2 | 7/2008 | Dr. RT | Procedures by hospitalists | 9 |
| 3 | 8/2008 | Dr. MA | Clostridium difficile treatment in the hospital | 11 |
| 4 | 8/2008 | Dr. EH | Active bed management | 6 |
| 5 | 9/2008 | Dr. AS | Medication reconciliation for geriatric inpatients | 10 |
| 6 | 9/2008 | Dr. DT | Time‐motion study of hospitalists | 10 |
| 7 | 10/2008 | Dr. KV | e‐Triage pilot | 16 |
| 8 | 11/2008 | Dr. EH | Assessing clinical performance of hospitalists | 7 |
| 9 | 12/2008 | Dr. SC | Trends and implications of hospitalists' morale | 8 |
| 10 | 1/2009 | Dr. TB | Lessons learned: tracking urinary catheter use at Bayview | 11 |
| 11 | 2/2009 | Dr. FK | Utilizing audit and feedback to improve performance in tobacco dependence counseling | 12 |
| 12 | 3/2009 | Dr. MK | Survivorship care plans | 7 |
| 13 | 4/2009 | Dr. DK | Outpatient provider preference for discharge summary format/style/length | 7 |
| 14 | 5/2009 | Dr. RW | Comparing preoperative consults done by hospitalists and cardiologists | 11 |
| 15 | 6/2009 | Dr. AK | Development of Web‐based messaging tool for providers | 12 |
Presenter Perspective
All 15 presenters (100%) felt a lot or tremendously supported during their sessions. Thirteen physicians (86%) believed that the sessions were a lot or tremendously helpful in advancing their projects. The presenters believed that the guidance and discussions related to their research ideas, aims, hypotheses, and plans were most helpful for advancing their projects (Table 2).
| Not at All, n (%) | A Little, n (%) | Some, n (%) | A Lot, n (%) | Tremendously, n (%) | |
|---|---|---|---|---|---|
| General questions: | |||||
| Intellectually/professionally stimulating | 0 (0) | 0 (0) | 0 (0) | 5 (33) | 10 (66) |
| Feeling supported by your colleagues in your scholarly pursuits | 0 (0) | 0 (0) | 0 (0) | 4 (27) | 11 (73) |
| Session helpful in the following areas: | |||||
| Advancing your project | 0 (0) | 0 (0) | 2 (13) | 5 (33) | 8 (53) |
| Generated new hypotheses | 1 (6) | 3 (20) | 5 (33) | 5 (33) | 1 (6) |
| Clarification of research questions | 0 (0) | 2 (13) | 4 (27) | 7 (47) | 2 (13) |
| Ideas for alternate methods | 1 (6) | 1 (6) | 2 (13) | 7 (47) | 4 (27) |
| New outcomes suggested | 1 (6) | 2 (13) | 2 (13) | 5 (33) | 5 (33) |
| Strategies to improve or enhance data collection | 0 (0) | 2 (13) | 0 (0) | 8 (53) | 5 (33) |
| Suggestions for alternate analyses or analytical strategies | 1 (1) | 1 (6) | 4 (27) | 5 (33) | 4 (27) |
| Input into what is most novel/emnteresting about this work | 0 (0) | 2 (13) | 3 (20) | 6 (40) | 4 (27) |
| Guidance about the implications of the work | 1 (6) | 2 (13) | 1 (6) | 7 (47) | 4 (27) |
| Ideas about next steps or future direction/studies | 0 (0) | 0 (0) | 3 (21) | 8 (57) | 3 (21) |
Examples of the written comments are:
I was overwhelmed by how engaged people were in my project.
The process of preparing for the session and then the discussion both helped my thinking. Colleagues were very supportive.
I am so glad I heard these comments and received this feedback now, rather than from peer reviewers selected by a journal to review my study. It would have been a much more difficult situation to fix at that later time.
Attendee Perspective
The majority of attendees (123 of 143, 86%) found the sessions to be a lot or extremely stimulating, and almost all (96%) were a lot or extremely satisfied with how the RIP sessions kept them abreast of their colleagues' academic interests. In addition, 92% judged the session's climate to be a lot or extremely supportive, and 88% deemed the balance of presentation to discussion to be just right. Attendees believed that they were most helpful to the presenter in terms of conceiving ideas for alternative methods to be used to answer the research question and in providing strategies to improve data collection (Table 3).
| Insight Offered | n (%) |
|---|---|
| Ideas for alternate methods | 92 (64%) |
| Strategies to improve data collection | 85 (59.4%) |
| New hypotheses generated | 84 (58.7%) |
| Ideas for next steps/future direction/studies | 83 (58%) |
| New outcomes suggested that should be considered | 69 (48%) |
| Clarification of the research questions | 61 (43%) |
| Input about what is most novel/emnteresting about the work | 60 (42%) |
| Guidance about the real implications of the work | 59 (41%) |
| Suggestions for alternate analyses or analytical strategies | 51 (36%) |
The free text comments primarily addressed how the presenters' research ideas were helped by the session:
There were great ideas for improvementincluding practical approaches for recruitment.
The session made me think of the daily routine things that we do that could be studied.
There were some great ideas to help Dr. A make the study more simple, doable, and practical. There were also some good ideas regarding potential sources of funding.
Academic Success
Of the 15 projects, 6 have been published in peer‐reviewed journals as first‐ or senior‐authored publications.510 Of these, 3 were presented at national meetings prior to publication. Four additional projects have been presented at a national society's annual meeting, all of which are being prepared for publication. Of the remaining 5 presentations, 4 were terminated because of the low likelihood of academic success. The remaining project is ongoing.
Comparatively, scholarly output in the prior year by the 24 physicians in the hospitalist group was 4 first‐ or senior‐authored publications in peer‐reviewed journals and 3 presentations at national meetings.
Discussion
In this article, we report our experience with the RIP conference. The sessions were perceived to be intellectually stimulating and supportive, whereas the discussions proved helpful in advancing project ideas. Ample discussion time and good attendance were thought to be critical to the success.
To our knowledge, this is the first article gathering feedback from attendees and presenters at a RIP conference and to track academic outcomes. Several types of meetings have been established within faculty and trainee groups to support and encourage scholarly activities.11, 12 The benefits of peer collaboration and peer mentoring have been described in the literature.13, 14 For example, Edwards described the success of shortstop meetings among small groups of faculty members every 4‐6 weeks in which discussions of research projects and mutual feedback would occur.15 Santucci described peer‐mentored research development meetings, with increased research productivity.12
Mentoring is critically important for academic success in medicine.1619 When divisions have limited senior mentors available, peer mentoring has proven to be indispensable as a mechanism to support faculty members.2022 The RIP conference provided a forum for peer mentoring and provided a partial solution to the limited resource of experienced research mentors in the division. The RIP sessions appear to have helped to bring the majority of presented ideas to academic fruition. Perhaps even more important, the sessions were able to terminate studies judged to have low academic promise before the faculty had invested significant time.
Several limitations of our study should be considered. First, this study involved a research‐in‐progress conference coordinated for a group of hospitalist physicians at 1 institution, and the results may not be generalizable. Second, although attendance was good at each conference, some faculty members did not come to many sessions. It is possible that those not attending may have rated the sessions differently. Session evaluations were anonymous, and we do not know whether specific attendees rated all sessions highly, thereby resulting in some degree of clustering. Third, this study did not compare the effectiveness of the RIP conference with other peer‐mentorship models. Finally, our study was uncontrolled. Although it would not be possible to restrict specific faculty from presenting at or attending the RIP conference, we intend to more carefully collect attendance data to see whether there might be a dose‐response effect with respect to participation in this conference and academic success.
In conclusion, our RIP conference was perceived as valuable by our group and was associated with academic success. In our division, the RIP conference serves as a way to operationalize peer mentoring. Our findings may help other groups to refine either the focus or format of their RIP sessions and those wishing to initiate such a conference.
- ,,, et al.Junior faculty members' mentoring relationships and their professional development in US medical schools.Acad Med.1998;73:318–323.
- ,.Mentors, Advisors and Role Models in Graduate and Professional Education.Washington, DC:Association of Academic Health Centers;1996.
- ,.Characteristics of the successful researcher and implications for faculty development.J Med Educ.1986;61:22–31.
- ,,.Curriculum Development for Medical Education: A Six‐Step Approach.2nd ed.Baltimore, MD:The Johns Hopkins University Press;2009.
- ,,, et al.Characteristics of hospitalists and hospitalist programs in the United States and Canada.J Clin Outcomes Meas.2009;16:69–74
- ,,, et al.Procedures performed by hospitalist and non‐hospitalist general internists.J Gen Intern Med.2010;25:448–452.
- ,,, et al.Intravenous immunoglobulin for the treatment of severe Clostridium difficile colitis: an observational study and review of the literature [review].J Hosp Med.2010;5:E1–E9.
- ,,, et al.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–811.
- ,,, et al.Transitioning to breast cancer survivorship: perspectives of patients, cancer specialists, and primary care providers.J Gen Intern Med.2009;24(Suppl 2):S459–S466.
- ,,, et al.Utilizing audit and feedback to improve hospitalists' performance in tobacco dependence counseling.Nicotine Tob Res.2010;12:797–800.
- ,,, et al.An internal medicine interest group research program can improve scholarly productivity of medical students and foster mentoring relationships with internists.Teach Learn Med.2008;20:163–167.
- ,,, et al.Peer‐mentored research development meeting: a model for successful peer mentoring among junior level researchers.Acad Psychiatry.2008;32:493–497.
- ,,, et al.Mentoring junior faculty in geriatric oncology: report from the cancer and aging research group.J Clin Oncol.2008;26:3125–3127.
- ,,the Canadian Critical Care Trials Group.Investigator‐led clinical research consortia: the Canadian Critical Care Trials Group.Crit Care Med.2009;37(1):S165–S172.
- .“Short stops”: peer support of scholarly activity.Acad Med.2002;77:939.
- ,,,,,,.Mentorship in academic general internal medicine. Results of a survey of mentors.J Gen Intern Med.2005;20:1014–1018.
- ,,, et al.Making the most of mentors: a guide for mentees.Acad Med.2009;84:140–144.
- ,,.Mentoring in academic medicine: a systematic review.JAMA.2006;296:1103–1115.
- ,,, et al.Assessing the role of influential mentors in the research development of primary care fellows.Acad Med.2004;79:865–872.
- ,,.Peer group mentoring of junior faculty.Acad Psychiatry.2008;32:230–235.
- ,,,.Facilitated peer mentorship: a pilot program for academic advancement of female medical faculty.J Womens Health.2008;17:1009–1015.
- ,Mentoring faculty in academic medicine. A new paradigm?J Gen Intern Med.2005;20:866–870.
The research‐in‐progress (RIP) conference is commonplace in academia, but there are no studies that objectively characterize its value. Bringing faculty together away from revenue‐generating activities carries a significant cost. As such, measuring the success of such gatherings is necessary.
Mentors are an invaluable influence on the careers of junior faculty members, helping them to produce high‐quality research.13 Unfortunately, some divisions lack mentorship to support the academic needs of less experienced faculty.1 Peer mentorship may be a solution. RIP sessions represent an opportunity to intentionally formalize peer mentoring. Further, these sessions can facilitate collaborations as individuals become aware of colleagues' interests. The goal of this study was to assess the value of the research‐in‐progress conference initiated within the hospitalist division at our institution.
Methods
Study Design
This cohort study was conducted to evaluate the value of the RIP conference among hospitalists in our division and the academic outcomes of the projects.
Setting and Participants
The study took place at Johns Hopkins Bayview Medical Center (JHBMC), a 335‐bed university‐affiliated medical center in Baltimore, Maryland. The hospitalist division consists of faculty physicians, nurse practitioners, and physician assistants (20.06 FTE physicians and 7.41 FTE midlevel providers). Twelve (54%) of our faculty members are female, and the mean age of providers is 35.7 years. The providers have been practicing hospitalist medicine for 3.0 years on average; 2 (9%) are clinical associates, 16 (73%) are instructors, and 3 (14%) are assistant professors.
All faculty members presenting at the RIP session were members of the division. A senior faculty member (a professor in the Division of General Internal Medicine) helps to coordinate the conference. The group's research assistant was present at the sessions and was charged with data collection and collation.
The Johns Hopkins University institutional review board approved the study.
The Research in Progress Conference
During the 2009 academic year, our division held 15 RIP sessions. At each session, 1 faculty member presented a research proposal. The goal of each session was to provide a forum where faculty members could share their research ideas (specific aims, hypotheses, planned design, outcome measures, analytic plans, and preliminary results [if applicable]) in order to receive feedback. The senior faculty member met with the presenter prior to each session in order to: (1) ensure that half the RIP time was reserved for discussion and (2) review the presenter's goals so these would be made explicit to peers. The coordinator of the RIP conference facilitated the discussion, solicited input from all attendees, and encouraged constructive criticism.
Evaluation, Data Collection, and Analysis
At the end of each session, attendees (who were exclusively members of the hospitalist division) were asked to complete an anonymous survey. The 1‐page instrument was designed (1) with input from curriculum development experts4 and (2) after a review of the literature about RIP conferences. These steps conferred content validity to the instrument, which assessed perceptions about the session's quality and what was learned. Five‐point Likert scales were used to characterize the conference's success in several areas, including being intellectually/professionally stimulating and keeping them apprised of their colleagues' interests. The survey also assessed the participatory nature of the conference (balance of presentation vs discussion), its climate (extremely critical vs extremely supportive), and how the conference assisted the presenter. The presenters completed a distinct survey related to how helpful the conference was in improving/enhancing their projects. A final open‐ended section invited additional comments. The instrument was piloted and iteratively revised before its use in this study.
For the projects presented, we assessed the percentage that resulted in a peer‐reviewed publication or a presentation at a national meeting.
Results
The mean number of attendees at the RIP sessions was 9.6 persons. A total of 143 evaluations were completed. All 15 presenters (100%) completed their assessments. The research ideas presented spanned a breadth of topics in clinical research, quality improvement, policy, and professional development (Table 1).
| Session | Date | Presenter | Topic | Evaluations Completed |
|---|---|---|---|---|
| 1 | 7/2008 | Dr. CS | Hospital medicine in Canada versus the United States | 7 |
| 2 | 7/2008 | Dr. RT | Procedures by hospitalists | 9 |
| 3 | 8/2008 | Dr. MA | Clostridium difficile treatment in the hospital | 11 |
| 4 | 8/2008 | Dr. EH | Active bed management | 6 |
| 5 | 9/2008 | Dr. AS | Medication reconciliation for geriatric inpatients | 10 |
| 6 | 9/2008 | Dr. DT | Time‐motion study of hospitalists | 10 |
| 7 | 10/2008 | Dr. KV | e‐Triage pilot | 16 |
| 8 | 11/2008 | Dr. EH | Assessing clinical performance of hospitalists | 7 |
| 9 | 12/2008 | Dr. SC | Trends and implications of hospitalists' morale | 8 |
| 10 | 1/2009 | Dr. TB | Lessons learned: tracking urinary catheter use at Bayview | 11 |
| 11 | 2/2009 | Dr. FK | Utilizing audit and feedback to improve performance in tobacco dependence counseling | 12 |
| 12 | 3/2009 | Dr. MK | Survivorship care plans | 7 |
| 13 | 4/2009 | Dr. DK | Outpatient provider preference for discharge summary format/style/length | 7 |
| 14 | 5/2009 | Dr. RW | Comparing preoperative consults done by hospitalists and cardiologists | 11 |
| 15 | 6/2009 | Dr. AK | Development of Web‐based messaging tool for providers | 12 |
Presenter Perspective
All 15 presenters (100%) felt a lot or tremendously supported during their sessions. Thirteen physicians (86%) believed that the sessions were a lot or tremendously helpful in advancing their projects. The presenters believed that the guidance and discussions related to their research ideas, aims, hypotheses, and plans were most helpful for advancing their projects (Table 2).
| Not at All, n (%) | A Little, n (%) | Some, n (%) | A Lot, n (%) | Tremendously, n (%) | |
|---|---|---|---|---|---|
| General questions: | |||||
| Intellectually/professionally stimulating | 0 (0) | 0 (0) | 0 (0) | 5 (33) | 10 (66) |
| Feeling supported by your colleagues in your scholarly pursuits | 0 (0) | 0 (0) | 0 (0) | 4 (27) | 11 (73) |
| Session helpful in the following areas: | |||||
| Advancing your project | 0 (0) | 0 (0) | 2 (13) | 5 (33) | 8 (53) |
| Generated new hypotheses | 1 (6) | 3 (20) | 5 (33) | 5 (33) | 1 (6) |
| Clarification of research questions | 0 (0) | 2 (13) | 4 (27) | 7 (47) | 2 (13) |
| Ideas for alternate methods | 1 (6) | 1 (6) | 2 (13) | 7 (47) | 4 (27) |
| New outcomes suggested | 1 (6) | 2 (13) | 2 (13) | 5 (33) | 5 (33) |
| Strategies to improve or enhance data collection | 0 (0) | 2 (13) | 0 (0) | 8 (53) | 5 (33) |
| Suggestions for alternate analyses or analytical strategies | 1 (1) | 1 (6) | 4 (27) | 5 (33) | 4 (27) |
| Input into what is most novel/emnteresting about this work | 0 (0) | 2 (13) | 3 (20) | 6 (40) | 4 (27) |
| Guidance about the implications of the work | 1 (6) | 2 (13) | 1 (6) | 7 (47) | 4 (27) |
| Ideas about next steps or future direction/studies | 0 (0) | 0 (0) | 3 (21) | 8 (57) | 3 (21) |
Examples of the written comments are:
I was overwhelmed by how engaged people were in my project.
The process of preparing for the session and then the discussion both helped my thinking. Colleagues were very supportive.
I am so glad I heard these comments and received this feedback now, rather than from peer reviewers selected by a journal to review my study. It would have been a much more difficult situation to fix at that later time.
Attendee Perspective
The majority of attendees (123 of 143, 86%) found the sessions to be a lot or extremely stimulating, and almost all (96%) were a lot or extremely satisfied with how the RIP sessions kept them abreast of their colleagues' academic interests. In addition, 92% judged the session's climate to be a lot or extremely supportive, and 88% deemed the balance of presentation to discussion to be just right. Attendees believed that they were most helpful to the presenter in terms of conceiving ideas for alternative methods to be used to answer the research question and in providing strategies to improve data collection (Table 3).
| Insight Offered | n (%) |
|---|---|
| Ideas for alternate methods | 92 (64%) |
| Strategies to improve data collection | 85 (59.4%) |
| New hypotheses generated | 84 (58.7%) |
| Ideas for next steps/future direction/studies | 83 (58%) |
| New outcomes suggested that should be considered | 69 (48%) |
| Clarification of the research questions | 61 (43%) |
| Input about what is most novel/emnteresting about the work | 60 (42%) |
| Guidance about the real implications of the work | 59 (41%) |
| Suggestions for alternate analyses or analytical strategies | 51 (36%) |
The free text comments primarily addressed how the presenters' research ideas were helped by the session:
There were great ideas for improvementincluding practical approaches for recruitment.
The session made me think of the daily routine things that we do that could be studied.
There were some great ideas to help Dr. A make the study more simple, doable, and practical. There were also some good ideas regarding potential sources of funding.
Academic Success
Of the 15 projects, 6 have been published in peer‐reviewed journals as first‐ or senior‐authored publications.510 Of these, 3 were presented at national meetings prior to publication. Four additional projects have been presented at a national society's annual meeting, all of which are being prepared for publication. Of the remaining 5 presentations, 4 were terminated because of the low likelihood of academic success. The remaining project is ongoing.
Comparatively, scholarly output in the prior year by the 24 physicians in the hospitalist group was 4 first‐ or senior‐authored publications in peer‐reviewed journals and 3 presentations at national meetings.
Discussion
In this article, we report our experience with the RIP conference. The sessions were perceived to be intellectually stimulating and supportive, whereas the discussions proved helpful in advancing project ideas. Ample discussion time and good attendance were thought to be critical to the success.
To our knowledge, this is the first article gathering feedback from attendees and presenters at a RIP conference and to track academic outcomes. Several types of meetings have been established within faculty and trainee groups to support and encourage scholarly activities.11, 12 The benefits of peer collaboration and peer mentoring have been described in the literature.13, 14 For example, Edwards described the success of shortstop meetings among small groups of faculty members every 4‐6 weeks in which discussions of research projects and mutual feedback would occur.15 Santucci described peer‐mentored research development meetings, with increased research productivity.12
Mentoring is critically important for academic success in medicine.1619 When divisions have limited senior mentors available, peer mentoring has proven to be indispensable as a mechanism to support faculty members.2022 The RIP conference provided a forum for peer mentoring and provided a partial solution to the limited resource of experienced research mentors in the division. The RIP sessions appear to have helped to bring the majority of presented ideas to academic fruition. Perhaps even more important, the sessions were able to terminate studies judged to have low academic promise before the faculty had invested significant time.
Several limitations of our study should be considered. First, this study involved a research‐in‐progress conference coordinated for a group of hospitalist physicians at 1 institution, and the results may not be generalizable. Second, although attendance was good at each conference, some faculty members did not come to many sessions. It is possible that those not attending may have rated the sessions differently. Session evaluations were anonymous, and we do not know whether specific attendees rated all sessions highly, thereby resulting in some degree of clustering. Third, this study did not compare the effectiveness of the RIP conference with other peer‐mentorship models. Finally, our study was uncontrolled. Although it would not be possible to restrict specific faculty from presenting at or attending the RIP conference, we intend to more carefully collect attendance data to see whether there might be a dose‐response effect with respect to participation in this conference and academic success.
In conclusion, our RIP conference was perceived as valuable by our group and was associated with academic success. In our division, the RIP conference serves as a way to operationalize peer mentoring. Our findings may help other groups to refine either the focus or format of their RIP sessions and those wishing to initiate such a conference.
The research‐in‐progress (RIP) conference is commonplace in academia, but there are no studies that objectively characterize its value. Bringing faculty together away from revenue‐generating activities carries a significant cost. As such, measuring the success of such gatherings is necessary.
Mentors are an invaluable influence on the careers of junior faculty members, helping them to produce high‐quality research.13 Unfortunately, some divisions lack mentorship to support the academic needs of less experienced faculty.1 Peer mentorship may be a solution. RIP sessions represent an opportunity to intentionally formalize peer mentoring. Further, these sessions can facilitate collaborations as individuals become aware of colleagues' interests. The goal of this study was to assess the value of the research‐in‐progress conference initiated within the hospitalist division at our institution.
Methods
Study Design
This cohort study was conducted to evaluate the value of the RIP conference among hospitalists in our division and the academic outcomes of the projects.
Setting and Participants
The study took place at Johns Hopkins Bayview Medical Center (JHBMC), a 335‐bed university‐affiliated medical center in Baltimore, Maryland. The hospitalist division consists of faculty physicians, nurse practitioners, and physician assistants (20.06 FTE physicians and 7.41 FTE midlevel providers). Twelve (54%) of our faculty members are female, and the mean age of providers is 35.7 years. The providers have been practicing hospitalist medicine for 3.0 years on average; 2 (9%) are clinical associates, 16 (73%) are instructors, and 3 (14%) are assistant professors.
All faculty members presenting at the RIP session were members of the division. A senior faculty member (a professor in the Division of General Internal Medicine) helps to coordinate the conference. The group's research assistant was present at the sessions and was charged with data collection and collation.
The Johns Hopkins University institutional review board approved the study.
The Research in Progress Conference
During the 2009 academic year, our division held 15 RIP sessions. At each session, 1 faculty member presented a research proposal. The goal of each session was to provide a forum where faculty members could share their research ideas (specific aims, hypotheses, planned design, outcome measures, analytic plans, and preliminary results [if applicable]) in order to receive feedback. The senior faculty member met with the presenter prior to each session in order to: (1) ensure that half the RIP time was reserved for discussion and (2) review the presenter's goals so these would be made explicit to peers. The coordinator of the RIP conference facilitated the discussion, solicited input from all attendees, and encouraged constructive criticism.
Evaluation, Data Collection, and Analysis
At the end of each session, attendees (who were exclusively members of the hospitalist division) were asked to complete an anonymous survey. The 1‐page instrument was designed (1) with input from curriculum development experts4 and (2) after a review of the literature about RIP conferences. These steps conferred content validity to the instrument, which assessed perceptions about the session's quality and what was learned. Five‐point Likert scales were used to characterize the conference's success in several areas, including being intellectually/professionally stimulating and keeping them apprised of their colleagues' interests. The survey also assessed the participatory nature of the conference (balance of presentation vs discussion), its climate (extremely critical vs extremely supportive), and how the conference assisted the presenter. The presenters completed a distinct survey related to how helpful the conference was in improving/enhancing their projects. A final open‐ended section invited additional comments. The instrument was piloted and iteratively revised before its use in this study.
For the projects presented, we assessed the percentage that resulted in a peer‐reviewed publication or a presentation at a national meeting.
Results
The mean number of attendees at the RIP sessions was 9.6 persons. A total of 143 evaluations were completed. All 15 presenters (100%) completed their assessments. The research ideas presented spanned a breadth of topics in clinical research, quality improvement, policy, and professional development (Table 1).
| Session | Date | Presenter | Topic | Evaluations Completed |
|---|---|---|---|---|
| 1 | 7/2008 | Dr. CS | Hospital medicine in Canada versus the United States | 7 |
| 2 | 7/2008 | Dr. RT | Procedures by hospitalists | 9 |
| 3 | 8/2008 | Dr. MA | Clostridium difficile treatment in the hospital | 11 |
| 4 | 8/2008 | Dr. EH | Active bed management | 6 |
| 5 | 9/2008 | Dr. AS | Medication reconciliation for geriatric inpatients | 10 |
| 6 | 9/2008 | Dr. DT | Time‐motion study of hospitalists | 10 |
| 7 | 10/2008 | Dr. KV | e‐Triage pilot | 16 |
| 8 | 11/2008 | Dr. EH | Assessing clinical performance of hospitalists | 7 |
| 9 | 12/2008 | Dr. SC | Trends and implications of hospitalists' morale | 8 |
| 10 | 1/2009 | Dr. TB | Lessons learned: tracking urinary catheter use at Bayview | 11 |
| 11 | 2/2009 | Dr. FK | Utilizing audit and feedback to improve performance in tobacco dependence counseling | 12 |
| 12 | 3/2009 | Dr. MK | Survivorship care plans | 7 |
| 13 | 4/2009 | Dr. DK | Outpatient provider preference for discharge summary format/style/length | 7 |
| 14 | 5/2009 | Dr. RW | Comparing preoperative consults done by hospitalists and cardiologists | 11 |
| 15 | 6/2009 | Dr. AK | Development of Web‐based messaging tool for providers | 12 |
Presenter Perspective
All 15 presenters (100%) felt a lot or tremendously supported during their sessions. Thirteen physicians (86%) believed that the sessions were a lot or tremendously helpful in advancing their projects. The presenters believed that the guidance and discussions related to their research ideas, aims, hypotheses, and plans were most helpful for advancing their projects (Table 2).
| Not at All, n (%) | A Little, n (%) | Some, n (%) | A Lot, n (%) | Tremendously, n (%) | |
|---|---|---|---|---|---|
| General questions: | |||||
| Intellectually/professionally stimulating | 0 (0) | 0 (0) | 0 (0) | 5 (33) | 10 (66) |
| Feeling supported by your colleagues in your scholarly pursuits | 0 (0) | 0 (0) | 0 (0) | 4 (27) | 11 (73) |
| Session helpful in the following areas: | |||||
| Advancing your project | 0 (0) | 0 (0) | 2 (13) | 5 (33) | 8 (53) |
| Generated new hypotheses | 1 (6) | 3 (20) | 5 (33) | 5 (33) | 1 (6) |
| Clarification of research questions | 0 (0) | 2 (13) | 4 (27) | 7 (47) | 2 (13) |
| Ideas for alternate methods | 1 (6) | 1 (6) | 2 (13) | 7 (47) | 4 (27) |
| New outcomes suggested | 1 (6) | 2 (13) | 2 (13) | 5 (33) | 5 (33) |
| Strategies to improve or enhance data collection | 0 (0) | 2 (13) | 0 (0) | 8 (53) | 5 (33) |
| Suggestions for alternate analyses or analytical strategies | 1 (1) | 1 (6) | 4 (27) | 5 (33) | 4 (27) |
| Input into what is most novel/emnteresting about this work | 0 (0) | 2 (13) | 3 (20) | 6 (40) | 4 (27) |
| Guidance about the implications of the work | 1 (6) | 2 (13) | 1 (6) | 7 (47) | 4 (27) |
| Ideas about next steps or future direction/studies | 0 (0) | 0 (0) | 3 (21) | 8 (57) | 3 (21) |
Examples of the written comments are:
I was overwhelmed by how engaged people were in my project.
The process of preparing for the session and then the discussion both helped my thinking. Colleagues were very supportive.
I am so glad I heard these comments and received this feedback now, rather than from peer reviewers selected by a journal to review my study. It would have been a much more difficult situation to fix at that later time.
Attendee Perspective
The majority of attendees (123 of 143, 86%) found the sessions to be a lot or extremely stimulating, and almost all (96%) were a lot or extremely satisfied with how the RIP sessions kept them abreast of their colleagues' academic interests. In addition, 92% judged the session's climate to be a lot or extremely supportive, and 88% deemed the balance of presentation to discussion to be just right. Attendees believed that they were most helpful to the presenter in terms of conceiving ideas for alternative methods to be used to answer the research question and in providing strategies to improve data collection (Table 3).
| Insight Offered | n (%) |
|---|---|
| Ideas for alternate methods | 92 (64%) |
| Strategies to improve data collection | 85 (59.4%) |
| New hypotheses generated | 84 (58.7%) |
| Ideas for next steps/future direction/studies | 83 (58%) |
| New outcomes suggested that should be considered | 69 (48%) |
| Clarification of the research questions | 61 (43%) |
| Input about what is most novel/emnteresting about the work | 60 (42%) |
| Guidance about the real implications of the work | 59 (41%) |
| Suggestions for alternate analyses or analytical strategies | 51 (36%) |
The free text comments primarily addressed how the presenters' research ideas were helped by the session:
There were great ideas for improvementincluding practical approaches for recruitment.
The session made me think of the daily routine things that we do that could be studied.
There were some great ideas to help Dr. A make the study more simple, doable, and practical. There were also some good ideas regarding potential sources of funding.
Academic Success
Of the 15 projects, 6 have been published in peer‐reviewed journals as first‐ or senior‐authored publications.510 Of these, 3 were presented at national meetings prior to publication. Four additional projects have been presented at a national society's annual meeting, all of which are being prepared for publication. Of the remaining 5 presentations, 4 were terminated because of the low likelihood of academic success. The remaining project is ongoing.
Comparatively, scholarly output in the prior year by the 24 physicians in the hospitalist group was 4 first‐ or senior‐authored publications in peer‐reviewed journals and 3 presentations at national meetings.
Discussion
In this article, we report our experience with the RIP conference. The sessions were perceived to be intellectually stimulating and supportive, whereas the discussions proved helpful in advancing project ideas. Ample discussion time and good attendance were thought to be critical to the success.
To our knowledge, this is the first article gathering feedback from attendees and presenters at a RIP conference and to track academic outcomes. Several types of meetings have been established within faculty and trainee groups to support and encourage scholarly activities.11, 12 The benefits of peer collaboration and peer mentoring have been described in the literature.13, 14 For example, Edwards described the success of shortstop meetings among small groups of faculty members every 4‐6 weeks in which discussions of research projects and mutual feedback would occur.15 Santucci described peer‐mentored research development meetings, with increased research productivity.12
Mentoring is critically important for academic success in medicine.1619 When divisions have limited senior mentors available, peer mentoring has proven to be indispensable as a mechanism to support faculty members.2022 The RIP conference provided a forum for peer mentoring and provided a partial solution to the limited resource of experienced research mentors in the division. The RIP sessions appear to have helped to bring the majority of presented ideas to academic fruition. Perhaps even more important, the sessions were able to terminate studies judged to have low academic promise before the faculty had invested significant time.
Several limitations of our study should be considered. First, this study involved a research‐in‐progress conference coordinated for a group of hospitalist physicians at 1 institution, and the results may not be generalizable. Second, although attendance was good at each conference, some faculty members did not come to many sessions. It is possible that those not attending may have rated the sessions differently. Session evaluations were anonymous, and we do not know whether specific attendees rated all sessions highly, thereby resulting in some degree of clustering. Third, this study did not compare the effectiveness of the RIP conference with other peer‐mentorship models. Finally, our study was uncontrolled. Although it would not be possible to restrict specific faculty from presenting at or attending the RIP conference, we intend to more carefully collect attendance data to see whether there might be a dose‐response effect with respect to participation in this conference and academic success.
In conclusion, our RIP conference was perceived as valuable by our group and was associated with academic success. In our division, the RIP conference serves as a way to operationalize peer mentoring. Our findings may help other groups to refine either the focus or format of their RIP sessions and those wishing to initiate such a conference.
- ,,, et al.Junior faculty members' mentoring relationships and their professional development in US medical schools.Acad Med.1998;73:318–323.
- ,.Mentors, Advisors and Role Models in Graduate and Professional Education.Washington, DC:Association of Academic Health Centers;1996.
- ,.Characteristics of the successful researcher and implications for faculty development.J Med Educ.1986;61:22–31.
- ,,.Curriculum Development for Medical Education: A Six‐Step Approach.2nd ed.Baltimore, MD:The Johns Hopkins University Press;2009.
- ,,, et al.Characteristics of hospitalists and hospitalist programs in the United States and Canada.J Clin Outcomes Meas.2009;16:69–74
- ,,, et al.Procedures performed by hospitalist and non‐hospitalist general internists.J Gen Intern Med.2010;25:448–452.
- ,,, et al.Intravenous immunoglobulin for the treatment of severe Clostridium difficile colitis: an observational study and review of the literature [review].J Hosp Med.2010;5:E1–E9.
- ,,, et al.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–811.
- ,,, et al.Transitioning to breast cancer survivorship: perspectives of patients, cancer specialists, and primary care providers.J Gen Intern Med.2009;24(Suppl 2):S459–S466.
- ,,, et al.Utilizing audit and feedback to improve hospitalists' performance in tobacco dependence counseling.Nicotine Tob Res.2010;12:797–800.
- ,,, et al.An internal medicine interest group research program can improve scholarly productivity of medical students and foster mentoring relationships with internists.Teach Learn Med.2008;20:163–167.
- ,,, et al.Peer‐mentored research development meeting: a model for successful peer mentoring among junior level researchers.Acad Psychiatry.2008;32:493–497.
- ,,, et al.Mentoring junior faculty in geriatric oncology: report from the cancer and aging research group.J Clin Oncol.2008;26:3125–3127.
- ,,the Canadian Critical Care Trials Group.Investigator‐led clinical research consortia: the Canadian Critical Care Trials Group.Crit Care Med.2009;37(1):S165–S172.
- .“Short stops”: peer support of scholarly activity.Acad Med.2002;77:939.
- ,,,,,,.Mentorship in academic general internal medicine. Results of a survey of mentors.J Gen Intern Med.2005;20:1014–1018.
- ,,, et al.Making the most of mentors: a guide for mentees.Acad Med.2009;84:140–144.
- ,,.Mentoring in academic medicine: a systematic review.JAMA.2006;296:1103–1115.
- ,,, et al.Assessing the role of influential mentors in the research development of primary care fellows.Acad Med.2004;79:865–872.
- ,,.Peer group mentoring of junior faculty.Acad Psychiatry.2008;32:230–235.
- ,,,.Facilitated peer mentorship: a pilot program for academic advancement of female medical faculty.J Womens Health.2008;17:1009–1015.
- ,Mentoring faculty in academic medicine. A new paradigm?J Gen Intern Med.2005;20:866–870.
- ,,, et al.Junior faculty members' mentoring relationships and their professional development in US medical schools.Acad Med.1998;73:318–323.
- ,.Mentors, Advisors and Role Models in Graduate and Professional Education.Washington, DC:Association of Academic Health Centers;1996.
- ,.Characteristics of the successful researcher and implications for faculty development.J Med Educ.1986;61:22–31.
- ,,.Curriculum Development for Medical Education: A Six‐Step Approach.2nd ed.Baltimore, MD:The Johns Hopkins University Press;2009.
- ,,, et al.Characteristics of hospitalists and hospitalist programs in the United States and Canada.J Clin Outcomes Meas.2009;16:69–74
- ,,, et al.Procedures performed by hospitalist and non‐hospitalist general internists.J Gen Intern Med.2010;25:448–452.
- ,,, et al.Intravenous immunoglobulin for the treatment of severe Clostridium difficile colitis: an observational study and review of the literature [review].J Hosp Med.2010;5:E1–E9.
- ,,, et al.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–811.
- ,,, et al.Transitioning to breast cancer survivorship: perspectives of patients, cancer specialists, and primary care providers.J Gen Intern Med.2009;24(Suppl 2):S459–S466.
- ,,, et al.Utilizing audit and feedback to improve hospitalists' performance in tobacco dependence counseling.Nicotine Tob Res.2010;12:797–800.
- ,,, et al.An internal medicine interest group research program can improve scholarly productivity of medical students and foster mentoring relationships with internists.Teach Learn Med.2008;20:163–167.
- ,,, et al.Peer‐mentored research development meeting: a model for successful peer mentoring among junior level researchers.Acad Psychiatry.2008;32:493–497.
- ,,, et al.Mentoring junior faculty in geriatric oncology: report from the cancer and aging research group.J Clin Oncol.2008;26:3125–3127.
- ,,the Canadian Critical Care Trials Group.Investigator‐led clinical research consortia: the Canadian Critical Care Trials Group.Crit Care Med.2009;37(1):S165–S172.
- .“Short stops”: peer support of scholarly activity.Acad Med.2002;77:939.
- ,,,,,,.Mentorship in academic general internal medicine. Results of a survey of mentors.J Gen Intern Med.2005;20:1014–1018.
- ,,, et al.Making the most of mentors: a guide for mentees.Acad Med.2009;84:140–144.
- ,,.Mentoring in academic medicine: a systematic review.JAMA.2006;296:1103–1115.
- ,,, et al.Assessing the role of influential mentors in the research development of primary care fellows.Acad Med.2004;79:865–872.
- ,,.Peer group mentoring of junior faculty.Acad Psychiatry.2008;32:230–235.
- ,,,.Facilitated peer mentorship: a pilot program for academic advancement of female medical faculty.J Womens Health.2008;17:1009–1015.
- ,Mentoring faculty in academic medicine. A new paradigm?J Gen Intern Med.2005;20:866–870.
Copyright © 2011 Society of Hospital Medicine
Hospitalist Physician Leadership Skills
Physicians assume myriad leadership roles within medical institutions. Clinically‐oriented leadership roles can range from managing a small group of providers, to leading entire health systems, to heading up national quality improvement initiatives. While often competent in the practice of medicine, many physicians have not pursued structured management or administrative training. In a survey of Medicine Department Chairs at academic medical centers, none had advanced management degrees despite spending an average of 55% of their time on administrative duties. It is not uncommon for physicians to attend leadership development programs or management seminars, as evidenced by the increasing demand for education.1 Various methods for skill enhancement have been described24; however, the most effective approaches have yet to be determined.
Miller and Dollard5 and Bandura6, 7 have explained that behavioral contracts have evolved from social cognitive theory principles. These contracts are formal written agreements, often negotiated between 2 individuals, to facilitate behavior change. Typically, they involve a clear definition of expected behaviors with specific consequences (usually positive reinforcement).810 Their use in modifying physician behavior, particularly those related to leadership, has not been studied.
Hospitalist physicians represent the fastest growing specialty in the United States.11, 12 Among other responsibilities, they have taken on roles as leaders in hospital administration, education, quality improvement, and public health.1315 The Society of Hospital Medicine (SHM), the largest US organization committed to the practice of hospital medicine,16 has established Leadership Academies to prepare hospitalists for these duties. The goal of this study was to assess how hospitalist physicians' commitment to grow as leaders was expressed using behavioral contacts as a vehicle to clarify their intentions and whether behavioral change occurred over time.
Methods
Study Design
A qualitative study design was selected to explore how current and future hospitalist leaders planned to modify their behaviors after participating in a hospitalist leadership training course. Participants were encouraged to complete a behavioral contract highlighting their personal goals.
Approximately 12 months later, follow‐up data were collected. Participants were sent copies of their behavioral contracts and surveyed about the extent to which they have realized their personal goals.
Subjects
Hospitalist leaders participating in the 4‐day level I or II leadership courses of the SHM Leadership Academy were studied.
Data Collection
In the final sessions of the 2007‐2008 Leadership Academy courses, participants completed an optional behavioral contract exercise in which they partnered with a colleague and were asked to identify 4 action plans they intended to implement upon their return home. These were written down and signed. Selected demographic information was also collected.
Follow‐up surveys were sent by mail and electronically to a subset of participants with completed behavioral contracts. A 5‐point Likert scale (strongly agree . . . strongly disagree) was used to assess the extent of adherence to the goals listed in the behavioral contracts.
Data Analysis
Transcripts were analyzed using an editing organizing style, a qualitative analysis technique to find meaningful units or segments of text that both stand on their own and relate to the purpose of the study.12 With this method, the coding template emerges from the data. Two investigators independently analyzed the transcripts and created a coding template based on common themes identified among the participants. In cases of discrepant coding, the 2 investigators had discussions to reach consensus. The authors agreed on representative quotes for each theme. Triangulation was established through sharing results of the analysis with a subset of participants.
Follow‐up survey data was summarized descriptively showing proportion data.
Results
Response Rate and Participant Demographics
Out of 264 people who completed the course, 120 decided to participate in the optional behavioral contract exercise. The median age of participants was 38 years (Table 1). The majority were male (84; 70.0%), and hospitalist leaders (76; 63.3%). The median time in practice as a hospitalist was 4 years. Fewer than one‐half held an academic appointment (40; 33.3%) with most being at the rank of Assistant Professor (14; 11.7%). Most of the participants worked in a private hospital (80; 66.7%).
| Characteristic | |
|---|---|
| |
| Age in years [median (SD)] | 38 (8) |
| Male [n (%)] | 84 (70.0) |
| Years in practice as hospitalist [median (SD)] | 4 (13) |
| Leader of hospitalist program [n (%)] | 76 (63.3) |
| Academic affiliation [n (%)] | 40 (33.3) |
| Academic rank [n (%)] | |
| Instructor | 9 (7.5) |
| Assistant professor | 14 (11.7) |
| Associate professor | 13 (10.8) |
| Hospital type [n (%)] | |
| Private | 80 (66.7) |
| University | 15 (12.5) |
| Government | 2 (1.7) |
| Veterans administration | 0 (0.0) |
| Other | 1 (0.1) |
Results of Qualitative Analysis of Behavioral Contracts
From the analyses of the behavioral contracts, themes emerged related to ways in which participants hoped to develop and improve. The themes and the frequencies with which they were recorded in the behavioral contracts are shown in Table 2.
| Theme | Total Number of Times Theme Mentioned in All Behavioral Contracts | Number of Respondents Referring to Theme [n (%)] |
|---|---|---|
| ||
| Improving communication and interpersonal skills | 132 | 70 (58.3) |
| Refinement of vision, goals, and strategic planning | 115 | 62 (51.7) |
| Improve intrapersonal development | 65 | 36 (30.0) |
| Enhance negotiation skills | 65 | 44 (36.7) |
| Commit to organizational change | 53 | 32 (26.7) |
| Understanding business drivers | 38 | 28 (23.3) |
| Setting performance and clinical metrics | 34 | 26 (21.7) |
| Strengthen interdepartmental relations | 32 | 26 (21.7) |
Improving Communication and Interpersonal Skills
A desire to improve communication and listening skills, particularly in the context of conflict resolution, was mentioned repeatedly. Heightened awareness about different personality types to allow for improved interpersonal relationships was another concept that was emphasized.
One female Instructor from an academic medical center described her intentions:
I will try to do a better job at assessing the behavioral tendencies of my partners and adjust my own style for more effective communication.
Refinement of Vision, Goals, and Strategic Planning
Physicians were committed to returning to their home institutions and embarking on initiatives to advance vision and goals of their groups within the context of strategic planning. Participants were interested in creating hospitalist‐specific mission statements, developing specific goals that take advantage of strengths and opportunities while minimizing internal weaknesses and considering external threats. They described wanting to align the interests of members of their hospitalist groups around a common goal.
A female hospitalist leader in private practice wished to:
Clearly define a group vision and commit to re‐evaluation on a regular basis to ensure we are on track . . . and conduct a SWOT (Strengths, Weaknesses, Opportunities, Threats) analysis to set future goals.
Improve Intrapersonal Development
Participants expressed desire to improve their leadership skills. Proposed goals included: (1) recognizing their weaknesses and soliciting feedback from colleagues, (2) minimizing emotional response to stress, (3) sharing their knowledge and skills for the benefit of peers, (4) delegating work more effectively to others, (5) reading suggested books on leadership, (6) serving as a positive role model and mentor, and (7) managing meetings and difficult coworkers more skillfully.
One female Assistant Professor from an academic medical center outlined:
I want to be able to: (1) manage up better and effectively negotiate with the administration on behalf of my group; (2) become better at leadership skills by using the tools offered at the Academy; and (3) effectively support my group members to develop their skills to become successful in their chosen niches. I will . . . improve the poor morale in my group.
Enhance Negotiation Skills
Many physician leaders identified negotiation principles and techniques as foundations for improvement for interactions within their own groups, as well as with the hospital administration.
A male private hospitalist leader working for 4 years as a hospitalist described plans to utilize negotiation skills within and outside the group:
Negotiate with my team of hospitalists to make them more compliant with the rules and regulations of the group, and negotiate an excellent contract with hospital administration. . . .
Commit to Organizational Change
The hospitalist respondents described their ability to influence organizational change given their unique position at the interface between patient care delivery and hospital administration. To realize organizational change, commonly cited ideas included recruitment and retention of clinically excellent practitioners, and developing standard protocols to facilitate quality improvement initiatives.
A male Instructor of Medicine listed select areas in which to become more involved:
Participation with the Chief Executive Officer of the company in quality improvement projects, calls to the primary care practitioners upon discharge, and the handoff process.
Other Themes
The final 3 themes included are: understanding business drivers; the establishment of better metrics to assess performance; and the strengthening of interdepartmental relations.
Follow‐up Data About Adherence to Plans Delineated in Behavioral Contracts
Out of 65 completed behavioral contracts from the 2007 Level I participants, 32 returned a follow‐up survey (response rate 49.3%). Figure 1 shows the extent to which respondents believed that they were compliant with their proposed plans for change or improvement. Degree of adherence was displayed as a proportion of total goals. Out of those who returned a follow‐up survey, all but 1 respondent either strongly agreed or agreed that they adhered to at least one of their goals (96.9%).

Select representative comments that illustrate the physicians' appreciation of using behavioral contracts include:
my approach to problems is a bit more analytical.
simple changes in how I approach people and interact with them has greatly improved my skills as a leader and allowed me to accomplish my goals with much less effort.
Discussion
Through the qualitative analysis of the behavioral contracts completed by participants of a Leadership Academy for hospitalists, we characterized the ways that hospitalist practitioners hoped to evolve as leaders. The major themes that emerged relate not only to their own growth and development but also their pledge to advance the success of the group or division. The level of commitment and impact of the behavioral contracts appear to be reinforced by an overwhelmingly positive response to adherence to personal goals one year after course participation. Communication and interpersonal development were most frequently cited in the behavioral contracts as areas for which the hospitalist leaders acknowledged a desire to grow. In a study of academic department of medicine chairs, communication skills were identified as being vital for effective leadership.3 The Chairs also recognized other proficiencies required for leading that were consistent with those outlined in the behavioral contracts: strategic planning, change management, team building, personnel management, and systems thinking. McDade et al.17 examined the effects of participation in an executive leadership program developed for female academic faculty in medical and dental schools in the United States and Canada. They noted increased self‐assessed leadership capabilities at 18 months after attending the program, across 10 leadership constructs taught in the classes. These leadership constructs resonate with the themes found in the plans for change described by our informants.
Hospitalists are assuming leadership roles in an increasing number and with greater scope; however, until now their perspectives on what skill sets are required to be successful have not been well documented. Significant time, effort, and money are invested into the development of hospitalists as leaders.4 The behavioral contract appears to be a tool acceptable to hospitalist physicians; perhaps it can be used as part annual reviews with hospitalists aspiring to be leaders.
Several limitations of the study shall be considered. First, not all participants attending the Leadership Academy opted to fill out the behavioral contracts. Second, this qualitative study is limited to those practitioners who are genuinely interested in growing as leaders as evidenced by their willingness to invest in going to the course. Third, follow‐up surveys relied on self‐assessment and it is not known whether actual realization of these goals occurred or the extent to which behavioral contracts were responsible. Further, follow‐up data were only completed by 49% percent of those targeted. However, hospitalists may be fairly resistant to being surveyed as evidenced by the fact that SHM's 2005‐2006 membership survey yielded a response rate of only 26%.18 Finally, many of the thematic goals were described by fewer than 50% of informants. However, it is important to note that the elements included on each person's behavioral contract emerged spontaneously. If subjects were specifically asked about each theme, the number of comments related to each would certainly be much higher. Qualitative analysis does not really allow us to know whether one theme is more important than another merely because it was mentioned more frequently.
Hospitalist leaders appear to be committed to professional growth and they have reported realization of goals delineated in their behavioral contracts. While varied methods are being used as part of physician leadership training programs, behavioral contracts may enhance promise for change.
Acknowledgements
The authors thank Regina Hess for assistance in data preparation and Laurence Wellikson, MD, FHM, Russell Holman, MD and Erica Pearson (all from the SHM) for data collection.
Physicians assume myriad leadership roles within medical institutions. Clinically‐oriented leadership roles can range from managing a small group of providers, to leading entire health systems, to heading up national quality improvement initiatives. While often competent in the practice of medicine, many physicians have not pursued structured management or administrative training. In a survey of Medicine Department Chairs at academic medical centers, none had advanced management degrees despite spending an average of 55% of their time on administrative duties. It is not uncommon for physicians to attend leadership development programs or management seminars, as evidenced by the increasing demand for education.1 Various methods for skill enhancement have been described24; however, the most effective approaches have yet to be determined.
Miller and Dollard5 and Bandura6, 7 have explained that behavioral contracts have evolved from social cognitive theory principles. These contracts are formal written agreements, often negotiated between 2 individuals, to facilitate behavior change. Typically, they involve a clear definition of expected behaviors with specific consequences (usually positive reinforcement).810 Their use in modifying physician behavior, particularly those related to leadership, has not been studied.
Hospitalist physicians represent the fastest growing specialty in the United States.11, 12 Among other responsibilities, they have taken on roles as leaders in hospital administration, education, quality improvement, and public health.1315 The Society of Hospital Medicine (SHM), the largest US organization committed to the practice of hospital medicine,16 has established Leadership Academies to prepare hospitalists for these duties. The goal of this study was to assess how hospitalist physicians' commitment to grow as leaders was expressed using behavioral contacts as a vehicle to clarify their intentions and whether behavioral change occurred over time.
Methods
Study Design
A qualitative study design was selected to explore how current and future hospitalist leaders planned to modify their behaviors after participating in a hospitalist leadership training course. Participants were encouraged to complete a behavioral contract highlighting their personal goals.
Approximately 12 months later, follow‐up data were collected. Participants were sent copies of their behavioral contracts and surveyed about the extent to which they have realized their personal goals.
Subjects
Hospitalist leaders participating in the 4‐day level I or II leadership courses of the SHM Leadership Academy were studied.
Data Collection
In the final sessions of the 2007‐2008 Leadership Academy courses, participants completed an optional behavioral contract exercise in which they partnered with a colleague and were asked to identify 4 action plans they intended to implement upon their return home. These were written down and signed. Selected demographic information was also collected.
Follow‐up surveys were sent by mail and electronically to a subset of participants with completed behavioral contracts. A 5‐point Likert scale (strongly agree . . . strongly disagree) was used to assess the extent of adherence to the goals listed in the behavioral contracts.
Data Analysis
Transcripts were analyzed using an editing organizing style, a qualitative analysis technique to find meaningful units or segments of text that both stand on their own and relate to the purpose of the study.12 With this method, the coding template emerges from the data. Two investigators independently analyzed the transcripts and created a coding template based on common themes identified among the participants. In cases of discrepant coding, the 2 investigators had discussions to reach consensus. The authors agreed on representative quotes for each theme. Triangulation was established through sharing results of the analysis with a subset of participants.
Follow‐up survey data was summarized descriptively showing proportion data.
Results
Response Rate and Participant Demographics
Out of 264 people who completed the course, 120 decided to participate in the optional behavioral contract exercise. The median age of participants was 38 years (Table 1). The majority were male (84; 70.0%), and hospitalist leaders (76; 63.3%). The median time in practice as a hospitalist was 4 years. Fewer than one‐half held an academic appointment (40; 33.3%) with most being at the rank of Assistant Professor (14; 11.7%). Most of the participants worked in a private hospital (80; 66.7%).
| Characteristic | |
|---|---|
| |
| Age in years [median (SD)] | 38 (8) |
| Male [n (%)] | 84 (70.0) |
| Years in practice as hospitalist [median (SD)] | 4 (13) |
| Leader of hospitalist program [n (%)] | 76 (63.3) |
| Academic affiliation [n (%)] | 40 (33.3) |
| Academic rank [n (%)] | |
| Instructor | 9 (7.5) |
| Assistant professor | 14 (11.7) |
| Associate professor | 13 (10.8) |
| Hospital type [n (%)] | |
| Private | 80 (66.7) |
| University | 15 (12.5) |
| Government | 2 (1.7) |
| Veterans administration | 0 (0.0) |
| Other | 1 (0.1) |
Results of Qualitative Analysis of Behavioral Contracts
From the analyses of the behavioral contracts, themes emerged related to ways in which participants hoped to develop and improve. The themes and the frequencies with which they were recorded in the behavioral contracts are shown in Table 2.
| Theme | Total Number of Times Theme Mentioned in All Behavioral Contracts | Number of Respondents Referring to Theme [n (%)] |
|---|---|---|
| ||
| Improving communication and interpersonal skills | 132 | 70 (58.3) |
| Refinement of vision, goals, and strategic planning | 115 | 62 (51.7) |
| Improve intrapersonal development | 65 | 36 (30.0) |
| Enhance negotiation skills | 65 | 44 (36.7) |
| Commit to organizational change | 53 | 32 (26.7) |
| Understanding business drivers | 38 | 28 (23.3) |
| Setting performance and clinical metrics | 34 | 26 (21.7) |
| Strengthen interdepartmental relations | 32 | 26 (21.7) |
Improving Communication and Interpersonal Skills
A desire to improve communication and listening skills, particularly in the context of conflict resolution, was mentioned repeatedly. Heightened awareness about different personality types to allow for improved interpersonal relationships was another concept that was emphasized.
One female Instructor from an academic medical center described her intentions:
I will try to do a better job at assessing the behavioral tendencies of my partners and adjust my own style for more effective communication.
Refinement of Vision, Goals, and Strategic Planning
Physicians were committed to returning to their home institutions and embarking on initiatives to advance vision and goals of their groups within the context of strategic planning. Participants were interested in creating hospitalist‐specific mission statements, developing specific goals that take advantage of strengths and opportunities while minimizing internal weaknesses and considering external threats. They described wanting to align the interests of members of their hospitalist groups around a common goal.
A female hospitalist leader in private practice wished to:
Clearly define a group vision and commit to re‐evaluation on a regular basis to ensure we are on track . . . and conduct a SWOT (Strengths, Weaknesses, Opportunities, Threats) analysis to set future goals.
Improve Intrapersonal Development
Participants expressed desire to improve their leadership skills. Proposed goals included: (1) recognizing their weaknesses and soliciting feedback from colleagues, (2) minimizing emotional response to stress, (3) sharing their knowledge and skills for the benefit of peers, (4) delegating work more effectively to others, (5) reading suggested books on leadership, (6) serving as a positive role model and mentor, and (7) managing meetings and difficult coworkers more skillfully.
One female Assistant Professor from an academic medical center outlined:
I want to be able to: (1) manage up better and effectively negotiate with the administration on behalf of my group; (2) become better at leadership skills by using the tools offered at the Academy; and (3) effectively support my group members to develop their skills to become successful in their chosen niches. I will . . . improve the poor morale in my group.
Enhance Negotiation Skills
Many physician leaders identified negotiation principles and techniques as foundations for improvement for interactions within their own groups, as well as with the hospital administration.
A male private hospitalist leader working for 4 years as a hospitalist described plans to utilize negotiation skills within and outside the group:
Negotiate with my team of hospitalists to make them more compliant with the rules and regulations of the group, and negotiate an excellent contract with hospital administration. . . .
Commit to Organizational Change
The hospitalist respondents described their ability to influence organizational change given their unique position at the interface between patient care delivery and hospital administration. To realize organizational change, commonly cited ideas included recruitment and retention of clinically excellent practitioners, and developing standard protocols to facilitate quality improvement initiatives.
A male Instructor of Medicine listed select areas in which to become more involved:
Participation with the Chief Executive Officer of the company in quality improvement projects, calls to the primary care practitioners upon discharge, and the handoff process.
Other Themes
The final 3 themes included are: understanding business drivers; the establishment of better metrics to assess performance; and the strengthening of interdepartmental relations.
Follow‐up Data About Adherence to Plans Delineated in Behavioral Contracts
Out of 65 completed behavioral contracts from the 2007 Level I participants, 32 returned a follow‐up survey (response rate 49.3%). Figure 1 shows the extent to which respondents believed that they were compliant with their proposed plans for change or improvement. Degree of adherence was displayed as a proportion of total goals. Out of those who returned a follow‐up survey, all but 1 respondent either strongly agreed or agreed that they adhered to at least one of their goals (96.9%).

Select representative comments that illustrate the physicians' appreciation of using behavioral contracts include:
my approach to problems is a bit more analytical.
simple changes in how I approach people and interact with them has greatly improved my skills as a leader and allowed me to accomplish my goals with much less effort.
Discussion
Through the qualitative analysis of the behavioral contracts completed by participants of a Leadership Academy for hospitalists, we characterized the ways that hospitalist practitioners hoped to evolve as leaders. The major themes that emerged relate not only to their own growth and development but also their pledge to advance the success of the group or division. The level of commitment and impact of the behavioral contracts appear to be reinforced by an overwhelmingly positive response to adherence to personal goals one year after course participation. Communication and interpersonal development were most frequently cited in the behavioral contracts as areas for which the hospitalist leaders acknowledged a desire to grow. In a study of academic department of medicine chairs, communication skills were identified as being vital for effective leadership.3 The Chairs also recognized other proficiencies required for leading that were consistent with those outlined in the behavioral contracts: strategic planning, change management, team building, personnel management, and systems thinking. McDade et al.17 examined the effects of participation in an executive leadership program developed for female academic faculty in medical and dental schools in the United States and Canada. They noted increased self‐assessed leadership capabilities at 18 months after attending the program, across 10 leadership constructs taught in the classes. These leadership constructs resonate with the themes found in the plans for change described by our informants.
Hospitalists are assuming leadership roles in an increasing number and with greater scope; however, until now their perspectives on what skill sets are required to be successful have not been well documented. Significant time, effort, and money are invested into the development of hospitalists as leaders.4 The behavioral contract appears to be a tool acceptable to hospitalist physicians; perhaps it can be used as part annual reviews with hospitalists aspiring to be leaders.
Several limitations of the study shall be considered. First, not all participants attending the Leadership Academy opted to fill out the behavioral contracts. Second, this qualitative study is limited to those practitioners who are genuinely interested in growing as leaders as evidenced by their willingness to invest in going to the course. Third, follow‐up surveys relied on self‐assessment and it is not known whether actual realization of these goals occurred or the extent to which behavioral contracts were responsible. Further, follow‐up data were only completed by 49% percent of those targeted. However, hospitalists may be fairly resistant to being surveyed as evidenced by the fact that SHM's 2005‐2006 membership survey yielded a response rate of only 26%.18 Finally, many of the thematic goals were described by fewer than 50% of informants. However, it is important to note that the elements included on each person's behavioral contract emerged spontaneously. If subjects were specifically asked about each theme, the number of comments related to each would certainly be much higher. Qualitative analysis does not really allow us to know whether one theme is more important than another merely because it was mentioned more frequently.
Hospitalist leaders appear to be committed to professional growth and they have reported realization of goals delineated in their behavioral contracts. While varied methods are being used as part of physician leadership training programs, behavioral contracts may enhance promise for change.
Acknowledgements
The authors thank Regina Hess for assistance in data preparation and Laurence Wellikson, MD, FHM, Russell Holman, MD and Erica Pearson (all from the SHM) for data collection.
Physicians assume myriad leadership roles within medical institutions. Clinically‐oriented leadership roles can range from managing a small group of providers, to leading entire health systems, to heading up national quality improvement initiatives. While often competent in the practice of medicine, many physicians have not pursued structured management or administrative training. In a survey of Medicine Department Chairs at academic medical centers, none had advanced management degrees despite spending an average of 55% of their time on administrative duties. It is not uncommon for physicians to attend leadership development programs or management seminars, as evidenced by the increasing demand for education.1 Various methods for skill enhancement have been described24; however, the most effective approaches have yet to be determined.
Miller and Dollard5 and Bandura6, 7 have explained that behavioral contracts have evolved from social cognitive theory principles. These contracts are formal written agreements, often negotiated between 2 individuals, to facilitate behavior change. Typically, they involve a clear definition of expected behaviors with specific consequences (usually positive reinforcement).810 Their use in modifying physician behavior, particularly those related to leadership, has not been studied.
Hospitalist physicians represent the fastest growing specialty in the United States.11, 12 Among other responsibilities, they have taken on roles as leaders in hospital administration, education, quality improvement, and public health.1315 The Society of Hospital Medicine (SHM), the largest US organization committed to the practice of hospital medicine,16 has established Leadership Academies to prepare hospitalists for these duties. The goal of this study was to assess how hospitalist physicians' commitment to grow as leaders was expressed using behavioral contacts as a vehicle to clarify their intentions and whether behavioral change occurred over time.
Methods
Study Design
A qualitative study design was selected to explore how current and future hospitalist leaders planned to modify their behaviors after participating in a hospitalist leadership training course. Participants were encouraged to complete a behavioral contract highlighting their personal goals.
Approximately 12 months later, follow‐up data were collected. Participants were sent copies of their behavioral contracts and surveyed about the extent to which they have realized their personal goals.
Subjects
Hospitalist leaders participating in the 4‐day level I or II leadership courses of the SHM Leadership Academy were studied.
Data Collection
In the final sessions of the 2007‐2008 Leadership Academy courses, participants completed an optional behavioral contract exercise in which they partnered with a colleague and were asked to identify 4 action plans they intended to implement upon their return home. These were written down and signed. Selected demographic information was also collected.
Follow‐up surveys were sent by mail and electronically to a subset of participants with completed behavioral contracts. A 5‐point Likert scale (strongly agree . . . strongly disagree) was used to assess the extent of adherence to the goals listed in the behavioral contracts.
Data Analysis
Transcripts were analyzed using an editing organizing style, a qualitative analysis technique to find meaningful units or segments of text that both stand on their own and relate to the purpose of the study.12 With this method, the coding template emerges from the data. Two investigators independently analyzed the transcripts and created a coding template based on common themes identified among the participants. In cases of discrepant coding, the 2 investigators had discussions to reach consensus. The authors agreed on representative quotes for each theme. Triangulation was established through sharing results of the analysis with a subset of participants.
Follow‐up survey data was summarized descriptively showing proportion data.
Results
Response Rate and Participant Demographics
Out of 264 people who completed the course, 120 decided to participate in the optional behavioral contract exercise. The median age of participants was 38 years (Table 1). The majority were male (84; 70.0%), and hospitalist leaders (76; 63.3%). The median time in practice as a hospitalist was 4 years. Fewer than one‐half held an academic appointment (40; 33.3%) with most being at the rank of Assistant Professor (14; 11.7%). Most of the participants worked in a private hospital (80; 66.7%).
| Characteristic | |
|---|---|
| |
| Age in years [median (SD)] | 38 (8) |
| Male [n (%)] | 84 (70.0) |
| Years in practice as hospitalist [median (SD)] | 4 (13) |
| Leader of hospitalist program [n (%)] | 76 (63.3) |
| Academic affiliation [n (%)] | 40 (33.3) |
| Academic rank [n (%)] | |
| Instructor | 9 (7.5) |
| Assistant professor | 14 (11.7) |
| Associate professor | 13 (10.8) |
| Hospital type [n (%)] | |
| Private | 80 (66.7) |
| University | 15 (12.5) |
| Government | 2 (1.7) |
| Veterans administration | 0 (0.0) |
| Other | 1 (0.1) |
Results of Qualitative Analysis of Behavioral Contracts
From the analyses of the behavioral contracts, themes emerged related to ways in which participants hoped to develop and improve. The themes and the frequencies with which they were recorded in the behavioral contracts are shown in Table 2.
| Theme | Total Number of Times Theme Mentioned in All Behavioral Contracts | Number of Respondents Referring to Theme [n (%)] |
|---|---|---|
| ||
| Improving communication and interpersonal skills | 132 | 70 (58.3) |
| Refinement of vision, goals, and strategic planning | 115 | 62 (51.7) |
| Improve intrapersonal development | 65 | 36 (30.0) |
| Enhance negotiation skills | 65 | 44 (36.7) |
| Commit to organizational change | 53 | 32 (26.7) |
| Understanding business drivers | 38 | 28 (23.3) |
| Setting performance and clinical metrics | 34 | 26 (21.7) |
| Strengthen interdepartmental relations | 32 | 26 (21.7) |
Improving Communication and Interpersonal Skills
A desire to improve communication and listening skills, particularly in the context of conflict resolution, was mentioned repeatedly. Heightened awareness about different personality types to allow for improved interpersonal relationships was another concept that was emphasized.
One female Instructor from an academic medical center described her intentions:
I will try to do a better job at assessing the behavioral tendencies of my partners and adjust my own style for more effective communication.
Refinement of Vision, Goals, and Strategic Planning
Physicians were committed to returning to their home institutions and embarking on initiatives to advance vision and goals of their groups within the context of strategic planning. Participants were interested in creating hospitalist‐specific mission statements, developing specific goals that take advantage of strengths and opportunities while minimizing internal weaknesses and considering external threats. They described wanting to align the interests of members of their hospitalist groups around a common goal.
A female hospitalist leader in private practice wished to:
Clearly define a group vision and commit to re‐evaluation on a regular basis to ensure we are on track . . . and conduct a SWOT (Strengths, Weaknesses, Opportunities, Threats) analysis to set future goals.
Improve Intrapersonal Development
Participants expressed desire to improve their leadership skills. Proposed goals included: (1) recognizing their weaknesses and soliciting feedback from colleagues, (2) minimizing emotional response to stress, (3) sharing their knowledge and skills for the benefit of peers, (4) delegating work more effectively to others, (5) reading suggested books on leadership, (6) serving as a positive role model and mentor, and (7) managing meetings and difficult coworkers more skillfully.
One female Assistant Professor from an academic medical center outlined:
I want to be able to: (1) manage up better and effectively negotiate with the administration on behalf of my group; (2) become better at leadership skills by using the tools offered at the Academy; and (3) effectively support my group members to develop their skills to become successful in their chosen niches. I will . . . improve the poor morale in my group.
Enhance Negotiation Skills
Many physician leaders identified negotiation principles and techniques as foundations for improvement for interactions within their own groups, as well as with the hospital administration.
A male private hospitalist leader working for 4 years as a hospitalist described plans to utilize negotiation skills within and outside the group:
Negotiate with my team of hospitalists to make them more compliant with the rules and regulations of the group, and negotiate an excellent contract with hospital administration. . . .
Commit to Organizational Change
The hospitalist respondents described their ability to influence organizational change given their unique position at the interface between patient care delivery and hospital administration. To realize organizational change, commonly cited ideas included recruitment and retention of clinically excellent practitioners, and developing standard protocols to facilitate quality improvement initiatives.
A male Instructor of Medicine listed select areas in which to become more involved:
Participation with the Chief Executive Officer of the company in quality improvement projects, calls to the primary care practitioners upon discharge, and the handoff process.
Other Themes
The final 3 themes included are: understanding business drivers; the establishment of better metrics to assess performance; and the strengthening of interdepartmental relations.
Follow‐up Data About Adherence to Plans Delineated in Behavioral Contracts
Out of 65 completed behavioral contracts from the 2007 Level I participants, 32 returned a follow‐up survey (response rate 49.3%). Figure 1 shows the extent to which respondents believed that they were compliant with their proposed plans for change or improvement. Degree of adherence was displayed as a proportion of total goals. Out of those who returned a follow‐up survey, all but 1 respondent either strongly agreed or agreed that they adhered to at least one of their goals (96.9%).

Select representative comments that illustrate the physicians' appreciation of using behavioral contracts include:
my approach to problems is a bit more analytical.
simple changes in how I approach people and interact with them has greatly improved my skills as a leader and allowed me to accomplish my goals with much less effort.
Discussion
Through the qualitative analysis of the behavioral contracts completed by participants of a Leadership Academy for hospitalists, we characterized the ways that hospitalist practitioners hoped to evolve as leaders. The major themes that emerged relate not only to their own growth and development but also their pledge to advance the success of the group or division. The level of commitment and impact of the behavioral contracts appear to be reinforced by an overwhelmingly positive response to adherence to personal goals one year after course participation. Communication and interpersonal development were most frequently cited in the behavioral contracts as areas for which the hospitalist leaders acknowledged a desire to grow. In a study of academic department of medicine chairs, communication skills were identified as being vital for effective leadership.3 The Chairs also recognized other proficiencies required for leading that were consistent with those outlined in the behavioral contracts: strategic planning, change management, team building, personnel management, and systems thinking. McDade et al.17 examined the effects of participation in an executive leadership program developed for female academic faculty in medical and dental schools in the United States and Canada. They noted increased self‐assessed leadership capabilities at 18 months after attending the program, across 10 leadership constructs taught in the classes. These leadership constructs resonate with the themes found in the plans for change described by our informants.
Hospitalists are assuming leadership roles in an increasing number and with greater scope; however, until now their perspectives on what skill sets are required to be successful have not been well documented. Significant time, effort, and money are invested into the development of hospitalists as leaders.4 The behavioral contract appears to be a tool acceptable to hospitalist physicians; perhaps it can be used as part annual reviews with hospitalists aspiring to be leaders.
Several limitations of the study shall be considered. First, not all participants attending the Leadership Academy opted to fill out the behavioral contracts. Second, this qualitative study is limited to those practitioners who are genuinely interested in growing as leaders as evidenced by their willingness to invest in going to the course. Third, follow‐up surveys relied on self‐assessment and it is not known whether actual realization of these goals occurred or the extent to which behavioral contracts were responsible. Further, follow‐up data were only completed by 49% percent of those targeted. However, hospitalists may be fairly resistant to being surveyed as evidenced by the fact that SHM's 2005‐2006 membership survey yielded a response rate of only 26%.18 Finally, many of the thematic goals were described by fewer than 50% of informants. However, it is important to note that the elements included on each person's behavioral contract emerged spontaneously. If subjects were specifically asked about each theme, the number of comments related to each would certainly be much higher. Qualitative analysis does not really allow us to know whether one theme is more important than another merely because it was mentioned more frequently.
Hospitalist leaders appear to be committed to professional growth and they have reported realization of goals delineated in their behavioral contracts. While varied methods are being used as part of physician leadership training programs, behavioral contracts may enhance promise for change.
Acknowledgements
The authors thank Regina Hess for assistance in data preparation and Laurence Wellikson, MD, FHM, Russell Holman, MD and Erica Pearson (all from the SHM) for data collection.
Copyright © 2010 Society of Hospital Medicine
Academic Suppport
Promotion through the ranks is the hallmark of success in academia. The support and infrastructure necessary to develop junior faculty members at academic medical centers may be inadequate.1, 2 Academic hospitalists are particularly vulnerable and at high risk for failure because of their heavy clinical commitment and limited time to pursue scholarly interests. Further, relatively few have pursued fellowship training, which means that many hospitalists must learn research‐related skills and the nuances of academia after joining the faculty.
Top‐notch mentors are believed to be integral to the success of the academic physician.36 Among other responsibilities, mentors (1) direct mentees toward promising opportunities, (2) serve as advocates for mentees, and (3) lend expertise to mentees' studies and scholarship. In general, there is concern that the cadre of talented, committed, and capable mentors is dwindling such that they are insufficient in number to satisfy and support the needs of the faculty.7, 8 In hospital medicine, experienced mentorship is particularly in short supply because the field is relatively new and there has been tremendous growth in the number of academic hospitalists, producing a large demand.
Like many hospitalist groups, our hospitalist division, the Collaborative Inpatient Medicine Service (CIMS), has experienced significant growth. It became apparent that the faculty needed and deserved a well‐designed academic support program to foster the development of skills necessary for academic success. The remainder of this article discusses our approach toward fulfilling these needs and the results to date.
DEVELOPING THE HOSPITALIST ACADEMIC SUPPORT PROGRAM
Problem Identification
Johns Hopkins Bayview Medical Center (JHBMC) is a 700‐bed urban university‐affiliated hospital. The CIMS hospital group is a distinct division separate from the hospitalist group at Johns Hopkins Hospital. All faculty are employed by the Johns Hopkins University School of Medicine (JHUSOM), and there is a single promotion track for the faculty. Specific requirements for promotion may be found in the Johns Hopkins University School of Medicine silver book at
CIMS had been growing in numbers from 4 full‐time equivalent (FTE) physicians in fiscal year (FY) 01 to 11.8 FTE physicians in FY06.
Most had limited training in research.
The physicians had little protected time for skill development and for working on scholarly projects.
Attempts to recruit a professor‐/associate professorlevel hospitalist from another institution to mentor our faculty members had been unsuccessful.
The hospitalists in our group had diverse interests such that we needed to find a flexible mentor who was willing and able to work across a breadth of content areas and methodologies.
Preliminary attempts to link up our hospitalists with clinician‐investigators at our institution were not fruitful.
Needs Assessment
In soliciting input from the hospitalists themselves and other stakeholders (including institutional leadership and leaders in hospital medicine), the following needs were identified:
Each CIMS faculty member must have a body of scholarship to support promotion and long‐term academic success.
Each CIMS faculty member needs appropriate mentorship.
Each CIMS faculty member needs protected time for scholarly work.
The CIMS faculty members need to support one another and be collaborative in their scholarly work.
The scholarly activities of the CIMS faculty need to support the mission of the division.
The mission of our division had been established to value and encourage the diverse interests and talents within the group:
The Collaborative Inpatient Medical Service (CIMS) is dedicated to serving the public trust by advancing the field of Hospital Medicine through the realization of excellence in patient care, education, research, leadership, and systems‐improvement.
Objectives
The objectives of the academic support program were organized into those for the CIMS Division as well as specific individual faculty goals and are outlined below:
Objectives for the division:
To increase the number and quality of peer‐reviewed publications produced by CIMS faculty.
To increase the amount of scholarly time available to CIMS faculty. In addition to external funding sources, we were committed to exploring nontraditional funding sources such as hospital administration and partnerships with other divisions or departments (including information technology) in need of clinically savvy physicians to help with projects.
To augment the leadership roles of the CIMS faculty with our institution and on a national level.
To support the CIMS faculty members such that they can be promoted at Johns Hopkins University School of Medicine (JHUSOM) and thereby retained.
Goals for individuals:
Each CIMS faculty member will advance his or her skill set to be moving toward producing scholarly work independently.
Each faculty member will lead at least 1 scholarly project at all times and will be involved as a team‐member in others.
Each faculty member will understand the criteria for promotion at our institution and will reflect on plans and strategies to realize success.
Strategies for Achieving the Objectives and Goals
Establish a Strong Mentoring System for the CIMS
The CIMS identified a primary mentor for the group, a faculty member within the Division of General Internal Medicine who was an experienced mentor with formidable management skills and an excellent track record in publishing scholarly work. Twenty‐percent of the mentor's time was set aside so he would have sufficient time to spend with CIMS faculty members in developing scholarly activities.
The mentor meets individually with each CIMS faculty member at the beginning of each academic year to identify career objectives; review current activities, interests, and skills; identify career development needs that require additional training or resources; set priorities for scholarly work; identify opportunities for collaboration internally and externally; and identify additional potential mentors to support specific projects. Regular follow‐up meetings are arranged, as needed to review progress and encourage advancing the work. The mentor uses resources to stay abreast of relevant funding opportunities and shares them with the group. The mentor reports regularly to the director of the CIMS regarding progress. The process as outlined remains ongoing.
Investing the Requisite Resources
A major decision was made that CIMS hospitalists would have 30% of their time protected for academic work, without the need for external funding. The expectation that the faculty had to use this time to effectively advance their career goals, which in turn would support the mission of CIMS, was clearly and explicitly expressed. The faculty would also be permitted to decrease their clinical time further on obtaining external funding. Additionally, in conjunction with a specific grant, the group hired a research assistant to permanently support the scholarly work of the faculty.
Leaders in both hospital administration and the Department of Medicine agreed that the only way to maintain a stable group of mature hospitalists who could serve as champions for change and help develop functional quality improvement projects was to support them in their academic efforts, including protected academic time irrespective of external funding.
The funding to protect the scholarly commitment (the mentor, the protected time of CIMS faculty, and the research assistant) has come primarily from divisional funds, although the CIMS budget is subsidized by the Department of Medicine and the medical center.
Recruit Faculty with Fellowship Training
It is our goal to reach a critical mass of hospitalists with experience and advanced training in scholarship. Fellowship‐trained faculty members are best positioned to realize academic success and can impart their knowledge and skills to others. Fellowship‐trained faculty members hired to date have come from either general internal medicine (n = 1) or geriatric (n = 2) fellowship programs, and none have been trained in a hospitalist fellowship program. It is hoped that these fellowship‐trained faculty and some of the other more experienced members of the group will be able to share in the mentoring responsibilities so that mentoring outsourcing can ultimately be replaced by CIMS faculty members.
EVALUATION DATA
In the 2 years since implementation of the scholarly support program, individual faculty in the CIMS have been meeting the above‐mentioned goals. Specifically, with respect to acquiring knowledge and skills, 2 faculty members have completed their master's degrees, and 6 others have made use of select courses to augment their knowledge and skills. All faculty members (100%) have a scholarly project they are leading, and most have reached out to a colleague in the CIMS to assist them, such that nearly all are team members on at least 1 other scholarly project. Through informal mentoring sessions and a once‐yearly formal meeting related to academic promotion, all members (100%) of the faculty are aware of the expectations and requirements for promotion.
Table 1 shows the accomplishment of the 5 faculty members in the academic track who have been division members for 3 years or more. Among the 5 faculty in the academic track, publications and extramural funding are improving. In the 5 years before the initiative, CIMS faculty averaged approximately 0.5 publications per person per year; in the first 2 years of this initiative, that number has increased to 1.3 publications per person per year. The 1 physician who has not yet been published has completed projects and has several article in process. External funding (largely in the form of 3 extramural grants from private foundations) has increased dramatically from an average of 4% per FTE before the intervention to approximately 15% per FTE afterward. In addition, all faculty members have secured a source of additional funding to reduce their clinical efforts since the implementation of this program. One foundation funded project that involved all division members, whose goal was to develop mechanisms to improve the discharge process of elderly patients to their homes, won the award at the SGIM 2007 National Meeting for the best clinical innovation. As illustrated in Table 1, 1 of the founding CIMS members transferred out of the academic track in 2003 in alignment with this physician's personal and professional goals and preferences. Two faculty members have moved up an academic rank, and several others are poised to do so.
| Dr. A* | Dr. B | Dr. C | Dr. D | Dr. E | Dr. F | |
|---|---|---|---|---|---|---|
| ||||||
| Years on faculty | 7 | 7 | 7 | 5 | 3 | 3 |
| Clinical % FTE before ASP | 70% | 60% | 60% | 70% | 70% | 70% |
| Clinical % FTE after ASP | Not applicable | 30% | 60% | 60% | 50% | 45% |
| Number of publications per year before ASP | Not applicable | 0.75 | 0.75 | 0 | 0 | 0 |
| Number of publications per year after ASP | Not applicable | 2.5 | 2 | 1 | 1 | 0 |
| Leadership role and title before ASP: | Not applicable | |||||
| a. within institution | Yes | No | No | No | No | |
| b. national level | No | No | No | No | No | |
| Leadership role and title after ASP: | Not applicable | |||||
| a. within institution | Yes | Yes | Yes | Yes | No | |
| b. national level | Yes | No | No | No | Yes | |
Thus, the divisional objectives (increasing number of publications, securing funding to increase the time devoted to scholarship, new leadership roles, and progression toward promotion) are being met as well.
CONCLUSIONS
Our rapidly growing hospitalist division recognized that several factors threatened the ability of the division and individuals to succeed academically. Divisional, departmental, and medical center leadership was committed to creating a supportive structure that would be available to all hospitalists as opposed to expecting each individual to unearth the necessary resources on their own. The innovative approach to foster individual, and therefore divisional, academic and scholarly success was designed around the following strategies: retention of an expert mentor (who is a not a hospitalist) and securing 20% of his time, investing in scholarship by protecting 30% nonclinical time for academic pursuits, and attempting to seek out fellowship‐trained hospitalists when hiring.
Although quality mentorship, protected time, and recruiting the best‐available talent to fill needs may not seem all that innovative, we believe the systematic approach to the problem and our steadfast application of the strategic plan is unique, innovative, and may present a model to be emulated by other divisions. Some may contend that it is impossible to protect 30% FTE of academic hospitalists indefinitely. Our group has made substantial investment in supporting the academic pursuits of our physicians, and we believe this is essential to maintaining their satisfaction and commitment to scholarship. This amount of protected time is offered to the entire physician faculty and continues even as our division has almost tripled in size. This initiative represents a carefully calculated investment that has influenced our ability to recruit and retain excellent people. Ongoing prospective study of this intervention over time will provide additional perspective on its value and shortcomings. Nonetheless, early data suggest that the plan is indeed working and that our group is satisfied with the return on investment to date.
- ,,,.2001.Status of clinical research in academic health centers: views from the research leadership.JAMA.286:800–806.
- ,,,.Contemporary (post‐Wills) survey of the views of Australian medical researchers: importance of funding, infrastructure and motivators for a research career.Med J Aust.2005;183:604–605.
- ,.Mentors, Advisors, and Role Models in Graduate and Professional Education.Washington DC:Association of Academic Health Centers;1996.
- ,.Characteristics of the successful researcher and implications for faculty development.J Med Educ.1986;61:22–31.
- .On mentoring.J R Soc Med.1997;90:347–349.
- ,,, et al.Junior faculty members' mentoring relationships and their professional development in U.S. medical schools.Acad Med.1998;73:318–323.
- AAMC (Association of American Medical Colleges).For the Health of the Public: Ensuring the Future of Clinical Research.Washington, DC:AAMC;1999.
- .2002.Clinical research career development: the individual perspective.Acad Med.77:1084–1088.
Promotion through the ranks is the hallmark of success in academia. The support and infrastructure necessary to develop junior faculty members at academic medical centers may be inadequate.1, 2 Academic hospitalists are particularly vulnerable and at high risk for failure because of their heavy clinical commitment and limited time to pursue scholarly interests. Further, relatively few have pursued fellowship training, which means that many hospitalists must learn research‐related skills and the nuances of academia after joining the faculty.
Top‐notch mentors are believed to be integral to the success of the academic physician.36 Among other responsibilities, mentors (1) direct mentees toward promising opportunities, (2) serve as advocates for mentees, and (3) lend expertise to mentees' studies and scholarship. In general, there is concern that the cadre of talented, committed, and capable mentors is dwindling such that they are insufficient in number to satisfy and support the needs of the faculty.7, 8 In hospital medicine, experienced mentorship is particularly in short supply because the field is relatively new and there has been tremendous growth in the number of academic hospitalists, producing a large demand.
Like many hospitalist groups, our hospitalist division, the Collaborative Inpatient Medicine Service (CIMS), has experienced significant growth. It became apparent that the faculty needed and deserved a well‐designed academic support program to foster the development of skills necessary for academic success. The remainder of this article discusses our approach toward fulfilling these needs and the results to date.
DEVELOPING THE HOSPITALIST ACADEMIC SUPPORT PROGRAM
Problem Identification
Johns Hopkins Bayview Medical Center (JHBMC) is a 700‐bed urban university‐affiliated hospital. The CIMS hospital group is a distinct division separate from the hospitalist group at Johns Hopkins Hospital. All faculty are employed by the Johns Hopkins University School of Medicine (JHUSOM), and there is a single promotion track for the faculty. Specific requirements for promotion may be found in the Johns Hopkins University School of Medicine silver book at
CIMS had been growing in numbers from 4 full‐time equivalent (FTE) physicians in fiscal year (FY) 01 to 11.8 FTE physicians in FY06.
Most had limited training in research.
The physicians had little protected time for skill development and for working on scholarly projects.
Attempts to recruit a professor‐/associate professorlevel hospitalist from another institution to mentor our faculty members had been unsuccessful.
The hospitalists in our group had diverse interests such that we needed to find a flexible mentor who was willing and able to work across a breadth of content areas and methodologies.
Preliminary attempts to link up our hospitalists with clinician‐investigators at our institution were not fruitful.
Needs Assessment
In soliciting input from the hospitalists themselves and other stakeholders (including institutional leadership and leaders in hospital medicine), the following needs were identified:
Each CIMS faculty member must have a body of scholarship to support promotion and long‐term academic success.
Each CIMS faculty member needs appropriate mentorship.
Each CIMS faculty member needs protected time for scholarly work.
The CIMS faculty members need to support one another and be collaborative in their scholarly work.
The scholarly activities of the CIMS faculty need to support the mission of the division.
The mission of our division had been established to value and encourage the diverse interests and talents within the group:
The Collaborative Inpatient Medical Service (CIMS) is dedicated to serving the public trust by advancing the field of Hospital Medicine through the realization of excellence in patient care, education, research, leadership, and systems‐improvement.
Objectives
The objectives of the academic support program were organized into those for the CIMS Division as well as specific individual faculty goals and are outlined below:
Objectives for the division:
To increase the number and quality of peer‐reviewed publications produced by CIMS faculty.
To increase the amount of scholarly time available to CIMS faculty. In addition to external funding sources, we were committed to exploring nontraditional funding sources such as hospital administration and partnerships with other divisions or departments (including information technology) in need of clinically savvy physicians to help with projects.
To augment the leadership roles of the CIMS faculty with our institution and on a national level.
To support the CIMS faculty members such that they can be promoted at Johns Hopkins University School of Medicine (JHUSOM) and thereby retained.
Goals for individuals:
Each CIMS faculty member will advance his or her skill set to be moving toward producing scholarly work independently.
Each faculty member will lead at least 1 scholarly project at all times and will be involved as a team‐member in others.
Each faculty member will understand the criteria for promotion at our institution and will reflect on plans and strategies to realize success.
Strategies for Achieving the Objectives and Goals
Establish a Strong Mentoring System for the CIMS
The CIMS identified a primary mentor for the group, a faculty member within the Division of General Internal Medicine who was an experienced mentor with formidable management skills and an excellent track record in publishing scholarly work. Twenty‐percent of the mentor's time was set aside so he would have sufficient time to spend with CIMS faculty members in developing scholarly activities.
The mentor meets individually with each CIMS faculty member at the beginning of each academic year to identify career objectives; review current activities, interests, and skills; identify career development needs that require additional training or resources; set priorities for scholarly work; identify opportunities for collaboration internally and externally; and identify additional potential mentors to support specific projects. Regular follow‐up meetings are arranged, as needed to review progress and encourage advancing the work. The mentor uses resources to stay abreast of relevant funding opportunities and shares them with the group. The mentor reports regularly to the director of the CIMS regarding progress. The process as outlined remains ongoing.
Investing the Requisite Resources
A major decision was made that CIMS hospitalists would have 30% of their time protected for academic work, without the need for external funding. The expectation that the faculty had to use this time to effectively advance their career goals, which in turn would support the mission of CIMS, was clearly and explicitly expressed. The faculty would also be permitted to decrease their clinical time further on obtaining external funding. Additionally, in conjunction with a specific grant, the group hired a research assistant to permanently support the scholarly work of the faculty.
Leaders in both hospital administration and the Department of Medicine agreed that the only way to maintain a stable group of mature hospitalists who could serve as champions for change and help develop functional quality improvement projects was to support them in their academic efforts, including protected academic time irrespective of external funding.
The funding to protect the scholarly commitment (the mentor, the protected time of CIMS faculty, and the research assistant) has come primarily from divisional funds, although the CIMS budget is subsidized by the Department of Medicine and the medical center.
Recruit Faculty with Fellowship Training
It is our goal to reach a critical mass of hospitalists with experience and advanced training in scholarship. Fellowship‐trained faculty members are best positioned to realize academic success and can impart their knowledge and skills to others. Fellowship‐trained faculty members hired to date have come from either general internal medicine (n = 1) or geriatric (n = 2) fellowship programs, and none have been trained in a hospitalist fellowship program. It is hoped that these fellowship‐trained faculty and some of the other more experienced members of the group will be able to share in the mentoring responsibilities so that mentoring outsourcing can ultimately be replaced by CIMS faculty members.
EVALUATION DATA
In the 2 years since implementation of the scholarly support program, individual faculty in the CIMS have been meeting the above‐mentioned goals. Specifically, with respect to acquiring knowledge and skills, 2 faculty members have completed their master's degrees, and 6 others have made use of select courses to augment their knowledge and skills. All faculty members (100%) have a scholarly project they are leading, and most have reached out to a colleague in the CIMS to assist them, such that nearly all are team members on at least 1 other scholarly project. Through informal mentoring sessions and a once‐yearly formal meeting related to academic promotion, all members (100%) of the faculty are aware of the expectations and requirements for promotion.
Table 1 shows the accomplishment of the 5 faculty members in the academic track who have been division members for 3 years or more. Among the 5 faculty in the academic track, publications and extramural funding are improving. In the 5 years before the initiative, CIMS faculty averaged approximately 0.5 publications per person per year; in the first 2 years of this initiative, that number has increased to 1.3 publications per person per year. The 1 physician who has not yet been published has completed projects and has several article in process. External funding (largely in the form of 3 extramural grants from private foundations) has increased dramatically from an average of 4% per FTE before the intervention to approximately 15% per FTE afterward. In addition, all faculty members have secured a source of additional funding to reduce their clinical efforts since the implementation of this program. One foundation funded project that involved all division members, whose goal was to develop mechanisms to improve the discharge process of elderly patients to their homes, won the award at the SGIM 2007 National Meeting for the best clinical innovation. As illustrated in Table 1, 1 of the founding CIMS members transferred out of the academic track in 2003 in alignment with this physician's personal and professional goals and preferences. Two faculty members have moved up an academic rank, and several others are poised to do so.
| Dr. A* | Dr. B | Dr. C | Dr. D | Dr. E | Dr. F | |
|---|---|---|---|---|---|---|
| ||||||
| Years on faculty | 7 | 7 | 7 | 5 | 3 | 3 |
| Clinical % FTE before ASP | 70% | 60% | 60% | 70% | 70% | 70% |
| Clinical % FTE after ASP | Not applicable | 30% | 60% | 60% | 50% | 45% |
| Number of publications per year before ASP | Not applicable | 0.75 | 0.75 | 0 | 0 | 0 |
| Number of publications per year after ASP | Not applicable | 2.5 | 2 | 1 | 1 | 0 |
| Leadership role and title before ASP: | Not applicable | |||||
| a. within institution | Yes | No | No | No | No | |
| b. national level | No | No | No | No | No | |
| Leadership role and title after ASP: | Not applicable | |||||
| a. within institution | Yes | Yes | Yes | Yes | No | |
| b. national level | Yes | No | No | No | Yes | |
Thus, the divisional objectives (increasing number of publications, securing funding to increase the time devoted to scholarship, new leadership roles, and progression toward promotion) are being met as well.
CONCLUSIONS
Our rapidly growing hospitalist division recognized that several factors threatened the ability of the division and individuals to succeed academically. Divisional, departmental, and medical center leadership was committed to creating a supportive structure that would be available to all hospitalists as opposed to expecting each individual to unearth the necessary resources on their own. The innovative approach to foster individual, and therefore divisional, academic and scholarly success was designed around the following strategies: retention of an expert mentor (who is a not a hospitalist) and securing 20% of his time, investing in scholarship by protecting 30% nonclinical time for academic pursuits, and attempting to seek out fellowship‐trained hospitalists when hiring.
Although quality mentorship, protected time, and recruiting the best‐available talent to fill needs may not seem all that innovative, we believe the systematic approach to the problem and our steadfast application of the strategic plan is unique, innovative, and may present a model to be emulated by other divisions. Some may contend that it is impossible to protect 30% FTE of academic hospitalists indefinitely. Our group has made substantial investment in supporting the academic pursuits of our physicians, and we believe this is essential to maintaining their satisfaction and commitment to scholarship. This amount of protected time is offered to the entire physician faculty and continues even as our division has almost tripled in size. This initiative represents a carefully calculated investment that has influenced our ability to recruit and retain excellent people. Ongoing prospective study of this intervention over time will provide additional perspective on its value and shortcomings. Nonetheless, early data suggest that the plan is indeed working and that our group is satisfied with the return on investment to date.
Promotion through the ranks is the hallmark of success in academia. The support and infrastructure necessary to develop junior faculty members at academic medical centers may be inadequate.1, 2 Academic hospitalists are particularly vulnerable and at high risk for failure because of their heavy clinical commitment and limited time to pursue scholarly interests. Further, relatively few have pursued fellowship training, which means that many hospitalists must learn research‐related skills and the nuances of academia after joining the faculty.
Top‐notch mentors are believed to be integral to the success of the academic physician.36 Among other responsibilities, mentors (1) direct mentees toward promising opportunities, (2) serve as advocates for mentees, and (3) lend expertise to mentees' studies and scholarship. In general, there is concern that the cadre of talented, committed, and capable mentors is dwindling such that they are insufficient in number to satisfy and support the needs of the faculty.7, 8 In hospital medicine, experienced mentorship is particularly in short supply because the field is relatively new and there has been tremendous growth in the number of academic hospitalists, producing a large demand.
Like many hospitalist groups, our hospitalist division, the Collaborative Inpatient Medicine Service (CIMS), has experienced significant growth. It became apparent that the faculty needed and deserved a well‐designed academic support program to foster the development of skills necessary for academic success. The remainder of this article discusses our approach toward fulfilling these needs and the results to date.
DEVELOPING THE HOSPITALIST ACADEMIC SUPPORT PROGRAM
Problem Identification
Johns Hopkins Bayview Medical Center (JHBMC) is a 700‐bed urban university‐affiliated hospital. The CIMS hospital group is a distinct division separate from the hospitalist group at Johns Hopkins Hospital. All faculty are employed by the Johns Hopkins University School of Medicine (JHUSOM), and there is a single promotion track for the faculty. Specific requirements for promotion may be found in the Johns Hopkins University School of Medicine silver book at
CIMS had been growing in numbers from 4 full‐time equivalent (FTE) physicians in fiscal year (FY) 01 to 11.8 FTE physicians in FY06.
Most had limited training in research.
The physicians had little protected time for skill development and for working on scholarly projects.
Attempts to recruit a professor‐/associate professorlevel hospitalist from another institution to mentor our faculty members had been unsuccessful.
The hospitalists in our group had diverse interests such that we needed to find a flexible mentor who was willing and able to work across a breadth of content areas and methodologies.
Preliminary attempts to link up our hospitalists with clinician‐investigators at our institution were not fruitful.
Needs Assessment
In soliciting input from the hospitalists themselves and other stakeholders (including institutional leadership and leaders in hospital medicine), the following needs were identified:
Each CIMS faculty member must have a body of scholarship to support promotion and long‐term academic success.
Each CIMS faculty member needs appropriate mentorship.
Each CIMS faculty member needs protected time for scholarly work.
The CIMS faculty members need to support one another and be collaborative in their scholarly work.
The scholarly activities of the CIMS faculty need to support the mission of the division.
The mission of our division had been established to value and encourage the diverse interests and talents within the group:
The Collaborative Inpatient Medical Service (CIMS) is dedicated to serving the public trust by advancing the field of Hospital Medicine through the realization of excellence in patient care, education, research, leadership, and systems‐improvement.
Objectives
The objectives of the academic support program were organized into those for the CIMS Division as well as specific individual faculty goals and are outlined below:
Objectives for the division:
To increase the number and quality of peer‐reviewed publications produced by CIMS faculty.
To increase the amount of scholarly time available to CIMS faculty. In addition to external funding sources, we were committed to exploring nontraditional funding sources such as hospital administration and partnerships with other divisions or departments (including information technology) in need of clinically savvy physicians to help with projects.
To augment the leadership roles of the CIMS faculty with our institution and on a national level.
To support the CIMS faculty members such that they can be promoted at Johns Hopkins University School of Medicine (JHUSOM) and thereby retained.
Goals for individuals:
Each CIMS faculty member will advance his or her skill set to be moving toward producing scholarly work independently.
Each faculty member will lead at least 1 scholarly project at all times and will be involved as a team‐member in others.
Each faculty member will understand the criteria for promotion at our institution and will reflect on plans and strategies to realize success.
Strategies for Achieving the Objectives and Goals
Establish a Strong Mentoring System for the CIMS
The CIMS identified a primary mentor for the group, a faculty member within the Division of General Internal Medicine who was an experienced mentor with formidable management skills and an excellent track record in publishing scholarly work. Twenty‐percent of the mentor's time was set aside so he would have sufficient time to spend with CIMS faculty members in developing scholarly activities.
The mentor meets individually with each CIMS faculty member at the beginning of each academic year to identify career objectives; review current activities, interests, and skills; identify career development needs that require additional training or resources; set priorities for scholarly work; identify opportunities for collaboration internally and externally; and identify additional potential mentors to support specific projects. Regular follow‐up meetings are arranged, as needed to review progress and encourage advancing the work. The mentor uses resources to stay abreast of relevant funding opportunities and shares them with the group. The mentor reports regularly to the director of the CIMS regarding progress. The process as outlined remains ongoing.
Investing the Requisite Resources
A major decision was made that CIMS hospitalists would have 30% of their time protected for academic work, without the need for external funding. The expectation that the faculty had to use this time to effectively advance their career goals, which in turn would support the mission of CIMS, was clearly and explicitly expressed. The faculty would also be permitted to decrease their clinical time further on obtaining external funding. Additionally, in conjunction with a specific grant, the group hired a research assistant to permanently support the scholarly work of the faculty.
Leaders in both hospital administration and the Department of Medicine agreed that the only way to maintain a stable group of mature hospitalists who could serve as champions for change and help develop functional quality improvement projects was to support them in their academic efforts, including protected academic time irrespective of external funding.
The funding to protect the scholarly commitment (the mentor, the protected time of CIMS faculty, and the research assistant) has come primarily from divisional funds, although the CIMS budget is subsidized by the Department of Medicine and the medical center.
Recruit Faculty with Fellowship Training
It is our goal to reach a critical mass of hospitalists with experience and advanced training in scholarship. Fellowship‐trained faculty members are best positioned to realize academic success and can impart their knowledge and skills to others. Fellowship‐trained faculty members hired to date have come from either general internal medicine (n = 1) or geriatric (n = 2) fellowship programs, and none have been trained in a hospitalist fellowship program. It is hoped that these fellowship‐trained faculty and some of the other more experienced members of the group will be able to share in the mentoring responsibilities so that mentoring outsourcing can ultimately be replaced by CIMS faculty members.
EVALUATION DATA
In the 2 years since implementation of the scholarly support program, individual faculty in the CIMS have been meeting the above‐mentioned goals. Specifically, with respect to acquiring knowledge and skills, 2 faculty members have completed their master's degrees, and 6 others have made use of select courses to augment their knowledge and skills. All faculty members (100%) have a scholarly project they are leading, and most have reached out to a colleague in the CIMS to assist them, such that nearly all are team members on at least 1 other scholarly project. Through informal mentoring sessions and a once‐yearly formal meeting related to academic promotion, all members (100%) of the faculty are aware of the expectations and requirements for promotion.
Table 1 shows the accomplishment of the 5 faculty members in the academic track who have been division members for 3 years or more. Among the 5 faculty in the academic track, publications and extramural funding are improving. In the 5 years before the initiative, CIMS faculty averaged approximately 0.5 publications per person per year; in the first 2 years of this initiative, that number has increased to 1.3 publications per person per year. The 1 physician who has not yet been published has completed projects and has several article in process. External funding (largely in the form of 3 extramural grants from private foundations) has increased dramatically from an average of 4% per FTE before the intervention to approximately 15% per FTE afterward. In addition, all faculty members have secured a source of additional funding to reduce their clinical efforts since the implementation of this program. One foundation funded project that involved all division members, whose goal was to develop mechanisms to improve the discharge process of elderly patients to their homes, won the award at the SGIM 2007 National Meeting for the best clinical innovation. As illustrated in Table 1, 1 of the founding CIMS members transferred out of the academic track in 2003 in alignment with this physician's personal and professional goals and preferences. Two faculty members have moved up an academic rank, and several others are poised to do so.
| Dr. A* | Dr. B | Dr. C | Dr. D | Dr. E | Dr. F | |
|---|---|---|---|---|---|---|
| ||||||
| Years on faculty | 7 | 7 | 7 | 5 | 3 | 3 |
| Clinical % FTE before ASP | 70% | 60% | 60% | 70% | 70% | 70% |
| Clinical % FTE after ASP | Not applicable | 30% | 60% | 60% | 50% | 45% |
| Number of publications per year before ASP | Not applicable | 0.75 | 0.75 | 0 | 0 | 0 |
| Number of publications per year after ASP | Not applicable | 2.5 | 2 | 1 | 1 | 0 |
| Leadership role and title before ASP: | Not applicable | |||||
| a. within institution | Yes | No | No | No | No | |
| b. national level | No | No | No | No | No | |
| Leadership role and title after ASP: | Not applicable | |||||
| a. within institution | Yes | Yes | Yes | Yes | No | |
| b. national level | Yes | No | No | No | Yes | |
Thus, the divisional objectives (increasing number of publications, securing funding to increase the time devoted to scholarship, new leadership roles, and progression toward promotion) are being met as well.
CONCLUSIONS
Our rapidly growing hospitalist division recognized that several factors threatened the ability of the division and individuals to succeed academically. Divisional, departmental, and medical center leadership was committed to creating a supportive structure that would be available to all hospitalists as opposed to expecting each individual to unearth the necessary resources on their own. The innovative approach to foster individual, and therefore divisional, academic and scholarly success was designed around the following strategies: retention of an expert mentor (who is a not a hospitalist) and securing 20% of his time, investing in scholarship by protecting 30% nonclinical time for academic pursuits, and attempting to seek out fellowship‐trained hospitalists when hiring.
Although quality mentorship, protected time, and recruiting the best‐available talent to fill needs may not seem all that innovative, we believe the systematic approach to the problem and our steadfast application of the strategic plan is unique, innovative, and may present a model to be emulated by other divisions. Some may contend that it is impossible to protect 30% FTE of academic hospitalists indefinitely. Our group has made substantial investment in supporting the academic pursuits of our physicians, and we believe this is essential to maintaining their satisfaction and commitment to scholarship. This amount of protected time is offered to the entire physician faculty and continues even as our division has almost tripled in size. This initiative represents a carefully calculated investment that has influenced our ability to recruit and retain excellent people. Ongoing prospective study of this intervention over time will provide additional perspective on its value and shortcomings. Nonetheless, early data suggest that the plan is indeed working and that our group is satisfied with the return on investment to date.
- ,,,.2001.Status of clinical research in academic health centers: views from the research leadership.JAMA.286:800–806.
- ,,,.Contemporary (post‐Wills) survey of the views of Australian medical researchers: importance of funding, infrastructure and motivators for a research career.Med J Aust.2005;183:604–605.
- ,.Mentors, Advisors, and Role Models in Graduate and Professional Education.Washington DC:Association of Academic Health Centers;1996.
- ,.Characteristics of the successful researcher and implications for faculty development.J Med Educ.1986;61:22–31.
- .On mentoring.J R Soc Med.1997;90:347–349.
- ,,, et al.Junior faculty members' mentoring relationships and their professional development in U.S. medical schools.Acad Med.1998;73:318–323.
- AAMC (Association of American Medical Colleges).For the Health of the Public: Ensuring the Future of Clinical Research.Washington, DC:AAMC;1999.
- .2002.Clinical research career development: the individual perspective.Acad Med.77:1084–1088.
- ,,,.2001.Status of clinical research in academic health centers: views from the research leadership.JAMA.286:800–806.
- ,,,.Contemporary (post‐Wills) survey of the views of Australian medical researchers: importance of funding, infrastructure and motivators for a research career.Med J Aust.2005;183:604–605.
- ,.Mentors, Advisors, and Role Models in Graduate and Professional Education.Washington DC:Association of Academic Health Centers;1996.
- ,.Characteristics of the successful researcher and implications for faculty development.J Med Educ.1986;61:22–31.
- .On mentoring.J R Soc Med.1997;90:347–349.
- ,,, et al.Junior faculty members' mentoring relationships and their professional development in U.S. medical schools.Acad Med.1998;73:318–323.
- AAMC (Association of American Medical Colleges).For the Health of the Public: Ensuring the Future of Clinical Research.Washington, DC:AAMC;1999.
- .2002.Clinical research career development: the individual perspective.Acad Med.77:1084–1088.
Copyright © 2008 Society of Hospital Medicine
Expanding Hospitalist Roles to Public Health
The field of hospital medicine came into being in response to numerous factors involving physicians, patients, and hospitals themselves1 Now, years later, hospital medicine is a specialty that is growing, both in size and sophistication such that the role of the hospitalist is constantly evolving.2 A compelling function that has not yet been clearly articulated is the opportunity for hospitalists to serve as public health practitioners in their unique clinical environment. There is precedence for the power of collaboration between medicine and public health as has been seen with emergency medicine's willingness to embrace opportunities to advance public health.35
In public health, the programs, services, and institutions involved emphasize the prevention of disease and the health needs of the population as a whole. Public health activities vary with changing technology and social values, but the goals remain the same: to reduce the amount of disease, premature death, and disease‐associated discomfort and disability in the population.6 The authors of a leading textbook of public health, Scutchfield and Keck, contend that the most important skill for public health practice is the capacity to visualize the potential for health that exists in a community.6
Hospitalists care for a distinct subset of the general populationinpatients, only a small percentage of society in a given year. Yet over time hospitalists affect a substantial subset of the larger population that uses considerable health care resources.79 Furthermore, hospitalization can be a sentinel event with public health implications (eg, newly diagnosed HIV infection or acute myocardial infarction in a patient with an extended family of cigarette smokers). This presents an opportunity to educate and counsel both the patient and the patient's social network. One model of public health practice by hospitalists is to influence the patient, his or her family, and the community by touching and inspiring the hospitalized patient.
Hospitalists are already involved in many of the core functions of public health (assessment, assurance, and policy development; Fig. 1).10 Achieving ongoing success in this arena means developing hospitalists who are consciously in tune with their roles as public health practitioners.
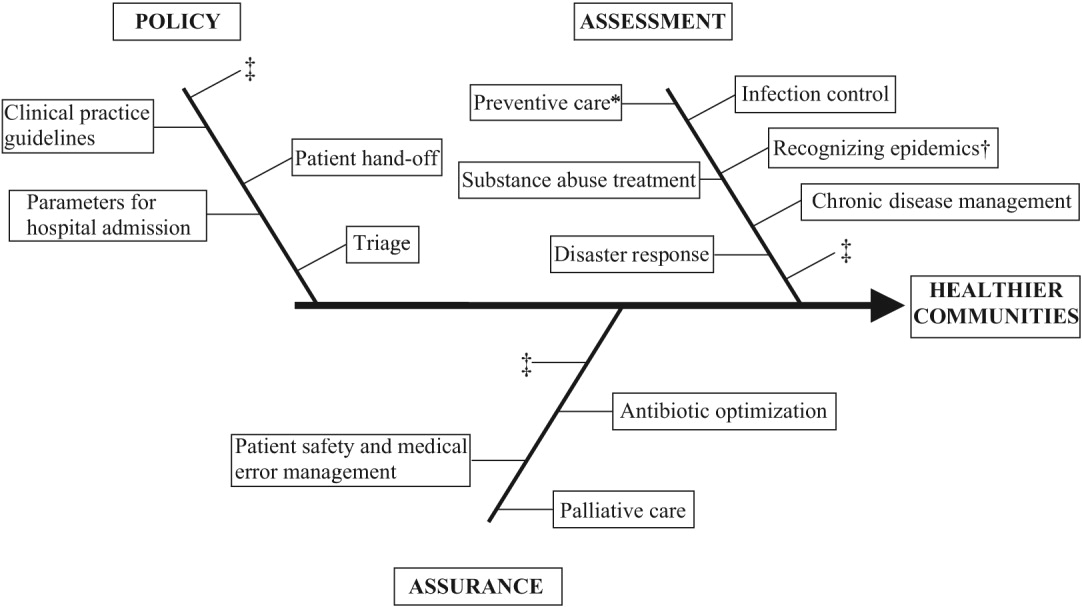
In this article we define the specific public health contributions that hospitalists have made and describe the possibilities for further innovative advances. To this end, we outline specific public health roles under the broad categories of assessment, assurance, and policy. We point to advances in public health accomplished by hospitalists as well as those being performed by nonhospitalists in the hospital setting. We conclude by describing some of the barriers to and implications of hospitalists taking on public health roles.
ASSESSMENT
Assessment is the systematic collection, analysis, and dissemination of health status information.10 These activities include disease surveillance and investigation of acute outbreaks or changes in the epidemiology of chronic diseases. Assessment also involves understanding the health of a population and the key determinants of a population's health from a variety of perspectives: physical, biological, behavioral, social, cultural, and spiritual.6 Human health has been defined as a state characterized by anatomic integrity; ability to perform personally valued family work and community roles; ability to deal with physical, biologic, and social stress; a feeling of well‐being; and freedom from the risk of disease and untimely death.6 Hospitalists interact with individuals at times of stress and acute illness and thus have a unique opportunity to assess the strength, viability, and resources available to individuals. Key roles that may fall within the auspices of assessment in hospital medicine are infection control, epidemic recognition, disaster response, preventive care, substance abuse treatment, and chronic disease management.
Infection Control
Physicians caring for inpatients have a crucial stake in controlling hospital infection as exemplified by the work of Flanders et al. on preventing nosocomial infections, especially nosocomial pneumonia.11 They describe specific strategies to prevent iatrogenic spread such as washing hands before and after patient contact, establishing guidelines against the use of artificial fingernails, using indwelling devices such as catheters only when absolutely necessary, and using sterile barriers.11 Hospitalists such as Sanjay Saint have led the way in studying methods to reduce bladder catheterization, which has been associated with urinary tract infections12; others have collaborated on work to prevent infections in nursing homes.13 Given the importance of this field, there is room for further hospitalist involvement. Novel methods for infection control in hospitals have been studied by nonhospitalists such as Wisnivesky, who prospectively validated a clinical decision rule to predict the need for respiratory isolation of inpatients with suspected tuberculosis (TB). This prediction rule, which is based on clinical and chest radiographic findings, was able to accurately identify patients at low risk for TB from among inpatients with suspected active pulmonary TB isolated on admission to the hospital.14 Retrospective application of the prediction rule showed respiratory precautions were inappropriately implemented for a third of patients.14 These studies are examples of empiric public health research performed in the inpatient setting. In the infection control domain, candidate issues for further study could include interventions aimed at reducing rates of Clostridium difficile, developing programs for standardized surveillance of hospital infection, validating electronic markers for nosocomial infection, and taking innovative approaches to improving hand‐washing practices in the hospital.15, 16
Recognizing Epidemics
An excellent example of the importance of hospitalists embracing public health and remembering their patients are part of a community was the severe acute respiratory syndrome (SARS) outbreak in Toronto, Ontario, Canada. The outbreak is thought to have begun with a single traveler. With the transfer of patients and the movement of visitors and health care workers among facilities, SARS quickly spread through Toronto, making it the largest SARS‐affected area outside Asia.17 Approximately a month after the outbreak was recognized in Toronto, it was thought to be over, and the World Health Organization (WHO) removed Toronto from its SARS‐affected list.17 Unfortunately, patients with unrecognized SARS remained in health care institutions, including a patient transferred to a rehabilitation center. Infection quickly spread again, resulting in a second phase of the outbreak.17
The SARS outbreak served as a reminder that a global public health system is essential and taught many lessons17 germane to pandemics that recur annually (eg, influenza viruses) as well those that episodically threaten the health of the population (eg, avian flu). Proposed actions to prevent a repeat of the scenario that occurred with SARS in Toronto include assessing the current facilities (eg, isolation rooms and respiratory masks) at each institution, identifying health care workers willing to serve as an outbreak team, and the hiring staff to train hospital personnel in personal protective equipment (PPE) and infection control policies.18 The Centers for Disease Control and Prevention (CDC) contends that planning for the possibility of a virulent pandemic at the local, national, and global levels is critical to limiting the mortality and morbidity should such occur.19, 20 In a previous article, Pile and Gordon declared hospitalists are key players in institutional efforts to prepare for a viral pandemic such as influenza and should be aware of lessons that may be applied from responses to pandemics such as SARS.19 Well placed to recognize clinical trends that may herald epidemics, hospitalists can fulfill some of the necessary public health responsibilities delineated above.
Disaster Response
Natural disasters and terrorism are in the forefront of the popular press and are also high priorities in health care and public health.21 Terrorism and natural disasters cause significant injury, illness, and death.22 Hospital‐based health care providers fulfill a variety of roles when terrorist acts and disasters occur, including reporting, diagnosing, and managing illness, providing preventive measures (eg, vaccines and preparedness kits), preventing the secondary spread of disease, assisting in the investigation of the causes of disease outbreaks, participating in preparedness planning, and evaluating preparedness policies and programs.22 The experience gained in the aftermaths of Hurricanes Katrina and Rita with their unprecedented death, injury, destruction, and displacement should help to guide future response and recovery activities.23 Hospitalists were at the forefront of delivering care, living in their hospitals for days after Hurricane Katrina. Without question, hospitalists will be called on again to serve those affected by disasters.
Preventive Care
For many patients admitted to the hospital, meeting a hospitalist is their first encounter with a physician in years.24, 25 In these instances, hospitalists must ensure that patients' immunizations are up‐to‐date and arrange appropriate follow‐up care with primary care providers. Greenwald described an important role that hospitalists could play in HIV prevention by promoting HIV testing in the hospital.26 The CDC recently confirmed the wisdom of this approach and estimates that the 250,000 to 1.2 million people in the United States with HIV infection who do not know their serostatus play a significant role in HIV transmission.26, 27 In an effort to promote testing, the CDC has initiated a program aimed at incorporating HIV testing into routine medical care, as recommended by others.28 More than a quarter of patients with HIV in the United States are diagnosed in the hospital, and for many other patients, hospitalization is their only real opportunity to be tested.26, 29 Similarly, when hospitalists find elevated cholesterol or triglycerides in routine evaluations of patients who present with chest pain, they have to decide whether to initiate lipid‐lowering medications.30 The hospitalist is sometimes the only physician that patients repeatedly admitted, may see over prolonged periods. It follows that if hospitalists are remiss in delivering preventive care to such patients, they lose the opportunity to positively affect their long‐term health. In practice, hospitalists perform myriad preventive‐care functions, although there is scant literature supporting this role. Hospitalists have an opportunity to collaborate in research projects of hospital‐initiated preventive care that measure outcomes at the community level.
Substance Abuse
In the Unites States, 25%‐40% of hospital admissions are related to substance abuse and its sequelae.31 These patients frequently are admitted to general medicine services for detoxification or treatment of substance‐abuse‐related morbidity, although some American hospitals have specialized treatment and detoxification centers. There is a pressing need for more models of comprehensive care that address the complex issues of addiction, including the biological, social, cultural, spiritual, and developmental needs of patients.32
Hospitalists routinely counsel their patients with substance abuse problems and often consult a chemical dependency counselor, who provides patients with additional information about outpatient or inpatient facilities that may help them after their hospitalization. Unfortunately, because of the natural history of substance abuse, many of these patients are rehospitalized with the same problems even after going through rehabilitation. The adoption of a public health philosophy and approach by hospitalists may assist patients who have addictions through innovative multidisciplinary interventions while these patient are being detoxified. Traditionally, these responsibilities have fallen to primary care providers and psychologists in substance abuse medicine; but, as mentioned previously, many such patients are rehospitalized before they make it to their follow‐up appointments.
In a study examining smoking cessation practices among Norwegian hospital physicians, 98% of the doctors stated they ask their patients about their smoking habits, but fewer than 7% of these physicians regularly offer smoking‐cessation counseling, hand out materials, or give patients other advice about smoking cessation.33 That study illustrates that hospital doctors often ask about problems but can certainly improve in terms of intervention and follow‐up. Other works by nonhospitalist physicians have examined the real potential of inpatient interventions for smoking cessation. Most of this work involves a multidisciplinary approach that relies heavily on nurses. For example, Davies et al. evaluated the effectiveness of a hospital‐based intervention for smoking cessation among low‐income smokers using public health methodologies. The intervention was effective and promising as a way to affect smokers in underserved communities.34
Chronic Disease Management
Public health roles involving chronic disease management include surveillance, intervention design, and implementation of control programs.6 Given their access to data on hospitalized patients, hospitalists can carry out surveillance and empirical population‐based research about hospitalized patients with chronic illnesses. Thoughtfully designed protocols can measure the success of interventions initiated in patients while hospitalized, with further data collection and follow‐up after patients have returned to the community.35 Such endeavors can improve the likelihood that patients with chronic conditions are effectively referred to programs that will maintain their health and functional status.36 If hospitalists consider themselves public health providers, encounters with these hospitalized patients will go beyond noting that their chronic conditions are stable and instead will lay the groundwork to prospectively control these conditions. This approach would have the potential to reduce the number of future hospitalizations and lead to healthier communities.37 To truly carry this out effectively, coordinated collaboration between primary care providers and hospitalists will be necessary.
ASSURANCE
Assurance is the provision of access to necessary health services. It entails efforts to solve problems that threaten the health of populations and empowers individuals to maintain their own health. This is accomplished by either encouraging action, delegating to other entities (private or public sector), mandating specific requirements through regulation, or providing services directly.10 Hospitalist teams aim to ensure that the high‐quality services needed to protect the health of their community (hospitalized patients) are available and that this population receives proper consideration in the allocation of resources. The few studies to date that have directly examined the quality of care that hospitalists provide38 have done so using evidence‐based measures believed to correlate with improved health care outcomes.38 The ambiguities in assessing quality may in part limit such studies.39 Specific hospitalist roles that fall under the assurance umbrella include antibiotic optimization, palliative care, patient safety, and medical error management.
Antibiotic Optimization
Inappropriate use of antimicrobial treatment for infectious diseases has cost and public health implications.40 These inappropriate uses include giving antibiotics when not indicated, overusing broad‐spectrum antibiotics, making mismatches between microbes and medicines when cultures and information on test sensitivity are available, and using intravenous formulations when oral therapy would suffice.41 The public health impact goes way beyond increasing selective pressure for antimicrobial resistance to include safety, adverse events, and increased costs to both patient and hospitals.40 At our institution, the hospital medicine service and infectious disease division have jointly developed and implemented an intervention to reduce inappropriate antibiotic use. At other institutions, hospitalist teams have developed protocols for treating infectious diseases commonly encountered in the hospitalized patient.42 The recommendations of both Amin and Reddy for management of community‐ and hospital‐acquired pneumonia acknowledged that through establishment of clinical care pathways, variation in prescribing patterns among hospitalists can be decreased while optimizing outcomes.42 The work of Williams and colleagues is another example of advances by hospitalists. They reviewed the literature to determine that the use of combination antibiotics as empiric therapy for community‐acquired pneumonia is superior to the use of a single effective antibiotic in treating bacteremic patients with pneumococcal community‐acquired pneumonia.43
Palliative Care
Mortality is a vital outcome measure of public health research and interventions. Not surprisingly, many people are hospitalized in the final months of their life and often die in a hospital. Pantilat showed that hospitalists can respond to these circumstances and have the opportunity to improve care of the dying.4446 Muir et al. evaluated the convergence of the fields of palliative care medicine and hospital medicine and reviewed the opportunities for mutual education and improved patient care.47 They described how the confluence of the changing nature and site of death in the United States coupled with the reorganization of hospital care provides a strategic opportunity to improve end‐of‐life care.47 Hospitalists can ensure that care of the dying is delivered with skill, compassion, and expertise. And so it is imperative they be trained to accomplish this objective.47, 49
Fortunately, hospitalists already appear to enhance patientphysician communication. Auerbach looked at communication, care patterns, and outcomes of dying patients, comparing patients being cared for by hospitalists with those being care for by community‐based physicians. Hospitalists had discussions with patients or their families about care more often than did nonhospitalist physicians (91% versus 73%, respectively, P = .006).49 Because the delivery of high‐quality palliative care is time consuming and complex, alternative models for billing or the use of physician extenders or consultants may be necessary at some institutions.
Patient Safety and Medical Error Management
Hospitalists have been in the forefront of promoting a culture of patient safety.50 Their continuous presence in the hospital and their interactions with members of health care teams from multiple disciplines who share this goal make them important facilitators. Hospitalists have increasing involvement in systems‐based efforts aimed at reducing medical errors.50 Hospitalists are being asked to lead committees that adopt multidisciplinary approaches to reduce adverse events, morbidity, and mortality.50 These committees often have representation from pharmacy, nursing, and other key hospital stakeholders including from the administration.51 Quality assurance activities assess locally collected data and compare results with local and national benchmarks. There are several published examples of hospitalists engaged in patient safety and medical error management. For example, Shojania et al compiled evidence based safety practices in an effort to promote patient safety.52, 53 Schnipper studied the role of pharmacist counseling in preventing adverse drug events (ADEs) after hospitalization and found that pharmacist medication review, patient counseling, and telephone follow‐up were associated with a lower rate of preventable ADEs 30 days after hospital discharge.54 Moreover, Syed paired hospitalists and pharmacists to collaboratively prescribe medications appropriately. In one study there were fewer medication errors and adverse drug reactions in patients treated by a team led by hospitalists than in those treated by the control group, made up of nonhospitalist attendings.55
POLICY
Policy development defines health control goals and objectives and develops implementation plans for those goals.10 By necessity, it operates at the intersection of legislative, political, and regulatory processes.10 At many institutions, hospitalists have been involved in the development of policies ensuring that the core functions of assessment and assurance are addressed and maintained. In fact, hospitalists report that development of quality assurance and practice guidelines accounts for most of their nonclinical time.56 This role of hospitalists is supported by anecdotal reports rather than published empiric evidence.57 For example, at Johns Hopkins Bayview Medical Center, hospitalist‐led teams have developed triage and patient handoff policies designed to improve patient safety. Parameters for admission to the general medicine ward have been elaborated and are periodically refined by the hospitalist team.
Another area that falls within the genre of policy is development of clinical practice guidelines. Guidelines for the treatment of pneumonia, congestive heart failure, deep‐vein thrombosis prophylaxis, alcohol and drug withdrawal, pain management, delirium, and chronic obstructive pulmonary disease have been developed by nonhospitalists.58, 59 These areas are considered core competencies in hospital medicine, and as such, hospitalists have an obligation to review and refine these guidelines to ensure the best provision of care to our patients.59
Hospitalists have been engaged in upholding guidelines that affect community practice. For example, in a study comparing treatment of patients admitted with congestive heart failure by hospitalists compared with that by nonhospitalists, hospitalists were found to be more likely to document left ventricular function, a core measure of quality as defined by JCAHO.39, 60 Knowledge about cardiac function can direct future care for patients when they return to the community and into the care of their primary care providers. In another example, Rifkin found that patients with community‐acquired pneumonia treated by hospitalists were more rapidly converted to oral antibiotics from intravenous antibiotics, facilitating a shorter length of stay,61 which reduced the opportunity for nosocomial infections to propagate. Because hospitalists are skilled at following guidelines,59 it follows that they should seize the opportunity to develop more of them.
As the hospitalist movement continues to grow, hospitalists will likely be engaged in implementing citywide, statewide, and even national policies that ensure optimal care of the hospitalized patient.
BARRIERS TO HOSPITALISTS FOCUSING ON PUBLIC HEALTH
Hospitalists are involved in public health activities even though they may not recognize the extent of this involvement. However, there may be some drawbacks to hospitalists viewing each patient encounter as an opportunity for a public health intervention. First, in viewing a patient as part of a cohort, the individual needs of the patient may be overlooked. There is inherent tension between population‐based and individual‐based care, which is a challenge. Second, hospitalists are busy clinicians who may be most highly valued because of their focus on efficiency and cost savings in the acute care setting. This factor alone may prevent substantive involvement by hospitalists in public health practice. Moving beyond the management of an acute illness may interfere with this efficiency and cost effectiveness from the hospital's perspective. However, interventions that promote health and prevent or reduce rehospitalizations may be cost effective to society in the long run. Third, current billing systems do not adequately reward or reimburse providers for the extra time that may be necessary to engage in public health practice. Fourth, hospitalists may not have the awareness, interest, training, or commitment to engage in public health practice. Finally, there may not be effective collaboration and communication systems between primary care providers and hospitalists. This barrier limits or hinders many possibilities for the effective execution of several public health initiatives.
CONCLUSIONS AND IMPLICATIONS
Hospitalists and the specialty of hospital medicine materialized because of myriad economic forces and the need to provide safe, high‐quality care to hospitalized patients. In this article we have described the ways in which hospitalists can be explicitly involved in public health practice. Traditionally, physicians caring for hospitalized patients have collected information through histories and physical examinations, interpreted laboratory data and tests, and formulated assessments and plans of care. To become public health practitioners, hospitalists have to go beyond these tasks and consider public health thought processes, such as problem‐solving paradigms and theories of behavior change. In adopting this public health perspective, hospitalists may begin to think of a patient in the context of the larger community in order to define the problems facing the community, not just the patient, determine the magnitude of such problems, identify key stakeholders, create intervention/prevention strategies, set priorities and recommend interventions, and implement and evaluate those interventions. This approach forces providers to move beyond the physicianpatient model and draw on public health models to invoke change. Hopefully, future research will further convince hospitalists of the benefits of this approach. Although it may be easier to defer care and management decisions to an outpatient physician, data suggest that intervening when patients are in the hospital may be most effective.62, 63 For example, is it possible that patients are more likely to quit smoking when they are sick in the hospital than when they are in their usual state of health on a routine visit at their primary care provider's office?64 Further, although deferring care to a primary care provider (PCP) may be easier, it is not always possible given these barriers: (1) some patients are routinely rehospitalized, precluding primary care visits, (2) some recommendations may not be received by PCPs, and (3) PCPpatient encounters are brief and the agendas full, and there are limited resources to address recommendations from the hospital.
As hospitalists become more involved in public health practice, their collaboration with physicians and researchers in other fields, nurses, policymakers, and administrators will expand. Succeeding in this arena requires integrity, motivation, capacity, understanding, knowledge, and experience.65 It is hoped that hospitalists will embrace the opportunity and master the requisite skill set necessary to practice in and advance this field. As hospitalist fellowship programs are developed, public health practice skills could be incorporated into the curriculum. Currently 6 of 16 fellowship programs offer either a master of public health degree or public health courses.66 Public health skills can also be taught at Society of Hospital Medicine meetings and other continuing medical education events.
With the evolution of hospital medicine, hospitalists have to be malleable in order to optimally meet the needs of the population they serve. The possibilities are endless.
- ,.The Hospitalist movement 5 years later.JAMA.2002;287:487–494.
- Hospitals and Health Networks. Hospitalists: a specialty coming into its own. Available at: http://www.hhmag.com. Accessed February 27,2006.
- ,,.Emergency medicine and public health: new steps in old directions.Ann Emerg Med.2001;38:675–683.
- ,, et al.A public health approach to emergency medicine: preparing for the twenty‐first century.Acad Emerg Med.1994;1:277–286.
- ,.Emergency medicine in population‐based systems of care.Ann Emerg Med.1997;30:800–803.
- ,.Principles of Public Health Practice.Albany, NY:Delmar Publishing;1997.
- Centers for Medicare and Medicaid. Health care spending and growth rate continue to decline in 2004. Available at: http://www.cms.hhs.gov. Accessed October 31,2006.
- ,,, et al.National health expenditures, 2002.Health Care Financ Rev. Summer2004;25:4.
- ,,, et al.Health spending Projections Through 2015: Changes on the Horizon.Health Affairs2006;25:w61–w73.
- Institute of Medicine.Recommendations from the Future of Public Health. InThe Future of the Public's Health.Washington, DC:National Academic Press;2003:411–420.
- ,,.Nosocomial pneumonia: state of the science.Am J Infect Control.2006;34:84–93.
- ,,,,.A reminder reduces urinary catheterization in hospitalized patients.Jt Comm J Qual Patient Saf.2005;31:455–462.
- ,,,.Preventing infections in nursing homes: A survey of infection control practices in southeast Michigan.Am J Infect Control.2005;33:489–492.
- ,,,.Prospective validation of a prediction model for isolating inpatients with suspected pulmonary tuberculosis.Arch Intern Med.2005;165:453–457.
- ,.The Hospital Infection Standardised Surveillance (HISS) programme: analysis of a two‐year pilot.J Hosp Infect.2003;53:259–267.
- ,,,.A Laboratory‐Based, Hospital‐Wide, Electronic Marker for Nosocomial Infection.Am J Clin Pathol.2006;125:34–39.
- ,,.Severe acute respiratory syndrome.Arch Pathol Lab Med.2004;128:1346–1350.
- ,,.Severe acute respiratory syndrome: responses of the healthcare system to a global epidemic.Curr Opin Otolaryngol Head Neck Surg.2005;13:161–164.
- ,.Pandemic influenza and the hospitalist: apocalypse when?J Hosp Med.2006;1:118–123.
- Center for Disease Control and Prevention. Pandemic Influenza information for Health Professionals. Available at: http://www.cdc.gov/flu/pandemic/. Accessed October 31,2006.
- .US health policy in the aftermath of Hurricane Katrina.JAMA.2006;295:437–40
- Levy B,Sidel V, eds.Terrorism and Public Health.New York:Oxford University Press;2003.
- Centers for Disease Control and Prevention (CDC).Public health response to Hurricanes Katrina and Rita—United States 2005.MMWR Morb Mortal Wkly Rep.2006;55:229–231.
- ,,,,,.Racial and ethnic disparities in health: a view from the South Bronx.J Health Care Poor Underserved.2006;17:116–127.
- ,.Williams E. Health Seeking behaviors of African Americans: implications for health administration.J Health Hum Serv Adm.2005;28(1):68–95.
- .Routine rapid HIV testing in hospitals: another opportunity for hospitalists to improve care.J Hosp Med.2006;1:106–112.
- Centers for Disease Control and Prevention.Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003.MMWR Morb Mortal Wkly Rep.2003;52:329–332.
- ,,, et al.Expanded screening for HIV in the United States—an analysis of cost‐effectiveness.N Engl J Med.2005;352:586–595.
- ,,,.Identifying undiagnosed human immunodeficiency virus: the yield for routine, voluntary, inpatient testing.Arch Intern Med.2002;162:887–892.
- ,,,,.Insufficient treatment of hypercholestrolemia among patients hospitalized with chest pain.Clin Cardiol.2006;29:259–262.
- .Medical management of alcoholic patients. In:Kissen B,Besleiter H, eds.Treatment and Rehabilitation of the Chronic Alcoholic.New York:Plenum Publishing Co.;1997.
- ,,.An integral approach to substance abuse.J Psychoactive Drugs.2005;37:363–371.
- ,,, et al.Smoking cessation practice among Norwegian hospital physicians.Tiddskr Nor laegeforen.2000;120:1629–1632.
- ,, et al.Evaluation of an intervention for hospitalized African American smokers.Am J Health Behav.2005;29:228–239.
- .Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs [review].J Am Geriatr Soc.2003;51:549–555.
- ,,,,.Advances in hospital medicine: a review of key articles from the literature.Med Clin N Am.2002;86:797–823.
- ,,,,,.Comprehensive discharge planning with post discharge support for older patients with congestive heart failure.JAMA.2004;291:1358–1367.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis.Med Care Res Rev.2005;62:379–406.
- ,,,,,Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists.Arch Intern Med.2002;162:1251–1256.
- ,,,.Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) colloquim, 2002.Lancet Infect Dis.2004;4:44–53.
- ,,, et al.Systematic review of antimicrobial drug prescribing in hospitals.Emerg Infect Dis.2006;12:211–216.
- ,,,,,,.Recommendations for management of community and hospital acquired pneumonia‐the hospitalist perspective.Curr Opin Pulm Med.2004;10(suppl 1):S23–S27.
- ,,,,.Advances in hospital medicine: a review of key articles from the literature.Med Clin N Am.2002;86:797–823.
- .End‐of‐life care for the hospitalized patient.Med Clin N Am.2002;86:749–770.
- ,.Palliative care for patients with heart failure.JAMA.2004;291:2476–2482.
- ,.Prevalence and structure of palliative care services in California hospitals.Arch Intern Med.2003;163:1084–1088.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.J Med.2001;111:10S–14S.
- .Palliative care in hospitals.J Hosp Med.2006;1:21–28.
- ,.End‐of‐life care in a voluntary hospitalist model: effects on communication, process of care, and patient symptoms.Am J Med.2004;116:669–675.
- ,,,Understanding medical error and improving patient safety in the inpatient setting,Med Clin N Am2002;86:847–867.
- , The hospitalist movement: ten issues to consider, hospital practice. Available at: http://www.hosppract.com/issues/1999/02/wachter.htm. Accessed March 14,2006.
- Shojania KG,Duncan BW,McDonald KM,Wachter RM, eds.Making health care safer: a critical analysis of patient safety practices. Evidence Report/Technology Assessment No. 43 from the Agency for Healthcare Research and Quality: AHRQ Publication No. 01‐E058;2001. Available at: http://www.ahrq.gov/clinic/ptsafety/.
- ,,,.Safe but sound: patient safety meets evidence‐based medicine.JAMA.2002;288:508–513.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- Hospitalists, pharmacists partner to cut errors: shorter lengths of stay, lower med costs result. HealthCare Benchmarks and Quality Improvement.American Health Consultants, Inc.,2005.
- ,,,.Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians.Ann Intern Med.1999;130:343–349.
- ,,,,.Core competencies in hospital medicine: Development and methodology.J Hosp Med.2006;1:48–56.
- National guideline clearing house. Available at: http://www.guideline.gov. Accessed June 26,2006.
- ,,,,, eds.The core competencies in hospital medicine.J Hosp Med.2006;1(suppl 1).
- Joint Commission on Accreditation of Healthcare Organizations. Core Measures overview. Available at: http://www.jcaho.org/perfeas/coremeas/cm.ovrvw.html. Accessed February 1,2006.
- ,,,.,Comparison of processes and outcomes of pneumonia care between hospitalists and community‐based primary care physicians.Mayo Clin Proc.2002;77:1053–1058.
- ,.The effectiveness of a nursing inpatient smoking cessation program in individuals with cardiovascular disease.Nurs Res.2005;54:243–254.
- ,,,,,.Evaluation of an intervention for hospitalized African American smokers.Am J Health Behav.2005;29:228–239.
- .Smoking cessation: the case for hospital‐based interventions.Prof Nurse.2003;19(3):145–148..
- . Dee Hock's management principles, in his own words. Fast Company.1996;5:79. Available at: http://www.fastcompany.com/magazine/05/dee2.html.
- ,,,.Hospital Medicine Fellowships: Works in progress.Am J Med.2006;119(1):72.e1–e7.
The field of hospital medicine came into being in response to numerous factors involving physicians, patients, and hospitals themselves1 Now, years later, hospital medicine is a specialty that is growing, both in size and sophistication such that the role of the hospitalist is constantly evolving.2 A compelling function that has not yet been clearly articulated is the opportunity for hospitalists to serve as public health practitioners in their unique clinical environment. There is precedence for the power of collaboration between medicine and public health as has been seen with emergency medicine's willingness to embrace opportunities to advance public health.35
In public health, the programs, services, and institutions involved emphasize the prevention of disease and the health needs of the population as a whole. Public health activities vary with changing technology and social values, but the goals remain the same: to reduce the amount of disease, premature death, and disease‐associated discomfort and disability in the population.6 The authors of a leading textbook of public health, Scutchfield and Keck, contend that the most important skill for public health practice is the capacity to visualize the potential for health that exists in a community.6
Hospitalists care for a distinct subset of the general populationinpatients, only a small percentage of society in a given year. Yet over time hospitalists affect a substantial subset of the larger population that uses considerable health care resources.79 Furthermore, hospitalization can be a sentinel event with public health implications (eg, newly diagnosed HIV infection or acute myocardial infarction in a patient with an extended family of cigarette smokers). This presents an opportunity to educate and counsel both the patient and the patient's social network. One model of public health practice by hospitalists is to influence the patient, his or her family, and the community by touching and inspiring the hospitalized patient.
Hospitalists are already involved in many of the core functions of public health (assessment, assurance, and policy development; Fig. 1).10 Achieving ongoing success in this arena means developing hospitalists who are consciously in tune with their roles as public health practitioners.
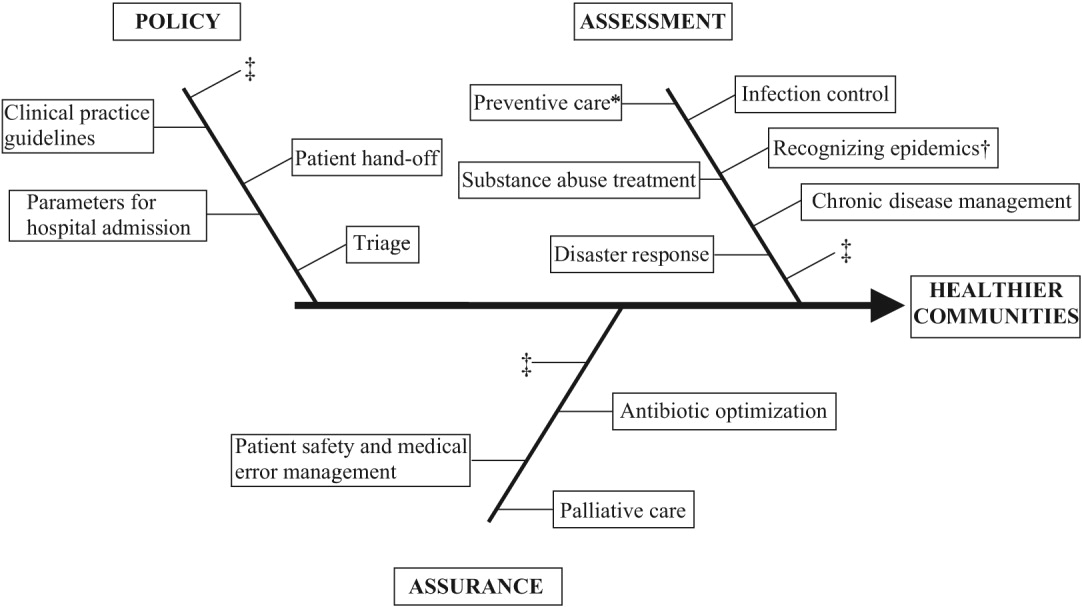
In this article we define the specific public health contributions that hospitalists have made and describe the possibilities for further innovative advances. To this end, we outline specific public health roles under the broad categories of assessment, assurance, and policy. We point to advances in public health accomplished by hospitalists as well as those being performed by nonhospitalists in the hospital setting. We conclude by describing some of the barriers to and implications of hospitalists taking on public health roles.
ASSESSMENT
Assessment is the systematic collection, analysis, and dissemination of health status information.10 These activities include disease surveillance and investigation of acute outbreaks or changes in the epidemiology of chronic diseases. Assessment also involves understanding the health of a population and the key determinants of a population's health from a variety of perspectives: physical, biological, behavioral, social, cultural, and spiritual.6 Human health has been defined as a state characterized by anatomic integrity; ability to perform personally valued family work and community roles; ability to deal with physical, biologic, and social stress; a feeling of well‐being; and freedom from the risk of disease and untimely death.6 Hospitalists interact with individuals at times of stress and acute illness and thus have a unique opportunity to assess the strength, viability, and resources available to individuals. Key roles that may fall within the auspices of assessment in hospital medicine are infection control, epidemic recognition, disaster response, preventive care, substance abuse treatment, and chronic disease management.
Infection Control
Physicians caring for inpatients have a crucial stake in controlling hospital infection as exemplified by the work of Flanders et al. on preventing nosocomial infections, especially nosocomial pneumonia.11 They describe specific strategies to prevent iatrogenic spread such as washing hands before and after patient contact, establishing guidelines against the use of artificial fingernails, using indwelling devices such as catheters only when absolutely necessary, and using sterile barriers.11 Hospitalists such as Sanjay Saint have led the way in studying methods to reduce bladder catheterization, which has been associated with urinary tract infections12; others have collaborated on work to prevent infections in nursing homes.13 Given the importance of this field, there is room for further hospitalist involvement. Novel methods for infection control in hospitals have been studied by nonhospitalists such as Wisnivesky, who prospectively validated a clinical decision rule to predict the need for respiratory isolation of inpatients with suspected tuberculosis (TB). This prediction rule, which is based on clinical and chest radiographic findings, was able to accurately identify patients at low risk for TB from among inpatients with suspected active pulmonary TB isolated on admission to the hospital.14 Retrospective application of the prediction rule showed respiratory precautions were inappropriately implemented for a third of patients.14 These studies are examples of empiric public health research performed in the inpatient setting. In the infection control domain, candidate issues for further study could include interventions aimed at reducing rates of Clostridium difficile, developing programs for standardized surveillance of hospital infection, validating electronic markers for nosocomial infection, and taking innovative approaches to improving hand‐washing practices in the hospital.15, 16
Recognizing Epidemics
An excellent example of the importance of hospitalists embracing public health and remembering their patients are part of a community was the severe acute respiratory syndrome (SARS) outbreak in Toronto, Ontario, Canada. The outbreak is thought to have begun with a single traveler. With the transfer of patients and the movement of visitors and health care workers among facilities, SARS quickly spread through Toronto, making it the largest SARS‐affected area outside Asia.17 Approximately a month after the outbreak was recognized in Toronto, it was thought to be over, and the World Health Organization (WHO) removed Toronto from its SARS‐affected list.17 Unfortunately, patients with unrecognized SARS remained in health care institutions, including a patient transferred to a rehabilitation center. Infection quickly spread again, resulting in a second phase of the outbreak.17
The SARS outbreak served as a reminder that a global public health system is essential and taught many lessons17 germane to pandemics that recur annually (eg, influenza viruses) as well those that episodically threaten the health of the population (eg, avian flu). Proposed actions to prevent a repeat of the scenario that occurred with SARS in Toronto include assessing the current facilities (eg, isolation rooms and respiratory masks) at each institution, identifying health care workers willing to serve as an outbreak team, and the hiring staff to train hospital personnel in personal protective equipment (PPE) and infection control policies.18 The Centers for Disease Control and Prevention (CDC) contends that planning for the possibility of a virulent pandemic at the local, national, and global levels is critical to limiting the mortality and morbidity should such occur.19, 20 In a previous article, Pile and Gordon declared hospitalists are key players in institutional efforts to prepare for a viral pandemic such as influenza and should be aware of lessons that may be applied from responses to pandemics such as SARS.19 Well placed to recognize clinical trends that may herald epidemics, hospitalists can fulfill some of the necessary public health responsibilities delineated above.
Disaster Response
Natural disasters and terrorism are in the forefront of the popular press and are also high priorities in health care and public health.21 Terrorism and natural disasters cause significant injury, illness, and death.22 Hospital‐based health care providers fulfill a variety of roles when terrorist acts and disasters occur, including reporting, diagnosing, and managing illness, providing preventive measures (eg, vaccines and preparedness kits), preventing the secondary spread of disease, assisting in the investigation of the causes of disease outbreaks, participating in preparedness planning, and evaluating preparedness policies and programs.22 The experience gained in the aftermaths of Hurricanes Katrina and Rita with their unprecedented death, injury, destruction, and displacement should help to guide future response and recovery activities.23 Hospitalists were at the forefront of delivering care, living in their hospitals for days after Hurricane Katrina. Without question, hospitalists will be called on again to serve those affected by disasters.
Preventive Care
For many patients admitted to the hospital, meeting a hospitalist is their first encounter with a physician in years.24, 25 In these instances, hospitalists must ensure that patients' immunizations are up‐to‐date and arrange appropriate follow‐up care with primary care providers. Greenwald described an important role that hospitalists could play in HIV prevention by promoting HIV testing in the hospital.26 The CDC recently confirmed the wisdom of this approach and estimates that the 250,000 to 1.2 million people in the United States with HIV infection who do not know their serostatus play a significant role in HIV transmission.26, 27 In an effort to promote testing, the CDC has initiated a program aimed at incorporating HIV testing into routine medical care, as recommended by others.28 More than a quarter of patients with HIV in the United States are diagnosed in the hospital, and for many other patients, hospitalization is their only real opportunity to be tested.26, 29 Similarly, when hospitalists find elevated cholesterol or triglycerides in routine evaluations of patients who present with chest pain, they have to decide whether to initiate lipid‐lowering medications.30 The hospitalist is sometimes the only physician that patients repeatedly admitted, may see over prolonged periods. It follows that if hospitalists are remiss in delivering preventive care to such patients, they lose the opportunity to positively affect their long‐term health. In practice, hospitalists perform myriad preventive‐care functions, although there is scant literature supporting this role. Hospitalists have an opportunity to collaborate in research projects of hospital‐initiated preventive care that measure outcomes at the community level.
Substance Abuse
In the Unites States, 25%‐40% of hospital admissions are related to substance abuse and its sequelae.31 These patients frequently are admitted to general medicine services for detoxification or treatment of substance‐abuse‐related morbidity, although some American hospitals have specialized treatment and detoxification centers. There is a pressing need for more models of comprehensive care that address the complex issues of addiction, including the biological, social, cultural, spiritual, and developmental needs of patients.32
Hospitalists routinely counsel their patients with substance abuse problems and often consult a chemical dependency counselor, who provides patients with additional information about outpatient or inpatient facilities that may help them after their hospitalization. Unfortunately, because of the natural history of substance abuse, many of these patients are rehospitalized with the same problems even after going through rehabilitation. The adoption of a public health philosophy and approach by hospitalists may assist patients who have addictions through innovative multidisciplinary interventions while these patient are being detoxified. Traditionally, these responsibilities have fallen to primary care providers and psychologists in substance abuse medicine; but, as mentioned previously, many such patients are rehospitalized before they make it to their follow‐up appointments.
In a study examining smoking cessation practices among Norwegian hospital physicians, 98% of the doctors stated they ask their patients about their smoking habits, but fewer than 7% of these physicians regularly offer smoking‐cessation counseling, hand out materials, or give patients other advice about smoking cessation.33 That study illustrates that hospital doctors often ask about problems but can certainly improve in terms of intervention and follow‐up. Other works by nonhospitalist physicians have examined the real potential of inpatient interventions for smoking cessation. Most of this work involves a multidisciplinary approach that relies heavily on nurses. For example, Davies et al. evaluated the effectiveness of a hospital‐based intervention for smoking cessation among low‐income smokers using public health methodologies. The intervention was effective and promising as a way to affect smokers in underserved communities.34
Chronic Disease Management
Public health roles involving chronic disease management include surveillance, intervention design, and implementation of control programs.6 Given their access to data on hospitalized patients, hospitalists can carry out surveillance and empirical population‐based research about hospitalized patients with chronic illnesses. Thoughtfully designed protocols can measure the success of interventions initiated in patients while hospitalized, with further data collection and follow‐up after patients have returned to the community.35 Such endeavors can improve the likelihood that patients with chronic conditions are effectively referred to programs that will maintain their health and functional status.36 If hospitalists consider themselves public health providers, encounters with these hospitalized patients will go beyond noting that their chronic conditions are stable and instead will lay the groundwork to prospectively control these conditions. This approach would have the potential to reduce the number of future hospitalizations and lead to healthier communities.37 To truly carry this out effectively, coordinated collaboration between primary care providers and hospitalists will be necessary.
ASSURANCE
Assurance is the provision of access to necessary health services. It entails efforts to solve problems that threaten the health of populations and empowers individuals to maintain their own health. This is accomplished by either encouraging action, delegating to other entities (private or public sector), mandating specific requirements through regulation, or providing services directly.10 Hospitalist teams aim to ensure that the high‐quality services needed to protect the health of their community (hospitalized patients) are available and that this population receives proper consideration in the allocation of resources. The few studies to date that have directly examined the quality of care that hospitalists provide38 have done so using evidence‐based measures believed to correlate with improved health care outcomes.38 The ambiguities in assessing quality may in part limit such studies.39 Specific hospitalist roles that fall under the assurance umbrella include antibiotic optimization, palliative care, patient safety, and medical error management.
Antibiotic Optimization
Inappropriate use of antimicrobial treatment for infectious diseases has cost and public health implications.40 These inappropriate uses include giving antibiotics when not indicated, overusing broad‐spectrum antibiotics, making mismatches between microbes and medicines when cultures and information on test sensitivity are available, and using intravenous formulations when oral therapy would suffice.41 The public health impact goes way beyond increasing selective pressure for antimicrobial resistance to include safety, adverse events, and increased costs to both patient and hospitals.40 At our institution, the hospital medicine service and infectious disease division have jointly developed and implemented an intervention to reduce inappropriate antibiotic use. At other institutions, hospitalist teams have developed protocols for treating infectious diseases commonly encountered in the hospitalized patient.42 The recommendations of both Amin and Reddy for management of community‐ and hospital‐acquired pneumonia acknowledged that through establishment of clinical care pathways, variation in prescribing patterns among hospitalists can be decreased while optimizing outcomes.42 The work of Williams and colleagues is another example of advances by hospitalists. They reviewed the literature to determine that the use of combination antibiotics as empiric therapy for community‐acquired pneumonia is superior to the use of a single effective antibiotic in treating bacteremic patients with pneumococcal community‐acquired pneumonia.43
Palliative Care
Mortality is a vital outcome measure of public health research and interventions. Not surprisingly, many people are hospitalized in the final months of their life and often die in a hospital. Pantilat showed that hospitalists can respond to these circumstances and have the opportunity to improve care of the dying.4446 Muir et al. evaluated the convergence of the fields of palliative care medicine and hospital medicine and reviewed the opportunities for mutual education and improved patient care.47 They described how the confluence of the changing nature and site of death in the United States coupled with the reorganization of hospital care provides a strategic opportunity to improve end‐of‐life care.47 Hospitalists can ensure that care of the dying is delivered with skill, compassion, and expertise. And so it is imperative they be trained to accomplish this objective.47, 49
Fortunately, hospitalists already appear to enhance patientphysician communication. Auerbach looked at communication, care patterns, and outcomes of dying patients, comparing patients being cared for by hospitalists with those being care for by community‐based physicians. Hospitalists had discussions with patients or their families about care more often than did nonhospitalist physicians (91% versus 73%, respectively, P = .006).49 Because the delivery of high‐quality palliative care is time consuming and complex, alternative models for billing or the use of physician extenders or consultants may be necessary at some institutions.
Patient Safety and Medical Error Management
Hospitalists have been in the forefront of promoting a culture of patient safety.50 Their continuous presence in the hospital and their interactions with members of health care teams from multiple disciplines who share this goal make them important facilitators. Hospitalists have increasing involvement in systems‐based efforts aimed at reducing medical errors.50 Hospitalists are being asked to lead committees that adopt multidisciplinary approaches to reduce adverse events, morbidity, and mortality.50 These committees often have representation from pharmacy, nursing, and other key hospital stakeholders including from the administration.51 Quality assurance activities assess locally collected data and compare results with local and national benchmarks. There are several published examples of hospitalists engaged in patient safety and medical error management. For example, Shojania et al compiled evidence based safety practices in an effort to promote patient safety.52, 53 Schnipper studied the role of pharmacist counseling in preventing adverse drug events (ADEs) after hospitalization and found that pharmacist medication review, patient counseling, and telephone follow‐up were associated with a lower rate of preventable ADEs 30 days after hospital discharge.54 Moreover, Syed paired hospitalists and pharmacists to collaboratively prescribe medications appropriately. In one study there were fewer medication errors and adverse drug reactions in patients treated by a team led by hospitalists than in those treated by the control group, made up of nonhospitalist attendings.55
POLICY
Policy development defines health control goals and objectives and develops implementation plans for those goals.10 By necessity, it operates at the intersection of legislative, political, and regulatory processes.10 At many institutions, hospitalists have been involved in the development of policies ensuring that the core functions of assessment and assurance are addressed and maintained. In fact, hospitalists report that development of quality assurance and practice guidelines accounts for most of their nonclinical time.56 This role of hospitalists is supported by anecdotal reports rather than published empiric evidence.57 For example, at Johns Hopkins Bayview Medical Center, hospitalist‐led teams have developed triage and patient handoff policies designed to improve patient safety. Parameters for admission to the general medicine ward have been elaborated and are periodically refined by the hospitalist team.
Another area that falls within the genre of policy is development of clinical practice guidelines. Guidelines for the treatment of pneumonia, congestive heart failure, deep‐vein thrombosis prophylaxis, alcohol and drug withdrawal, pain management, delirium, and chronic obstructive pulmonary disease have been developed by nonhospitalists.58, 59 These areas are considered core competencies in hospital medicine, and as such, hospitalists have an obligation to review and refine these guidelines to ensure the best provision of care to our patients.59
Hospitalists have been engaged in upholding guidelines that affect community practice. For example, in a study comparing treatment of patients admitted with congestive heart failure by hospitalists compared with that by nonhospitalists, hospitalists were found to be more likely to document left ventricular function, a core measure of quality as defined by JCAHO.39, 60 Knowledge about cardiac function can direct future care for patients when they return to the community and into the care of their primary care providers. In another example, Rifkin found that patients with community‐acquired pneumonia treated by hospitalists were more rapidly converted to oral antibiotics from intravenous antibiotics, facilitating a shorter length of stay,61 which reduced the opportunity for nosocomial infections to propagate. Because hospitalists are skilled at following guidelines,59 it follows that they should seize the opportunity to develop more of them.
As the hospitalist movement continues to grow, hospitalists will likely be engaged in implementing citywide, statewide, and even national policies that ensure optimal care of the hospitalized patient.
BARRIERS TO HOSPITALISTS FOCUSING ON PUBLIC HEALTH
Hospitalists are involved in public health activities even though they may not recognize the extent of this involvement. However, there may be some drawbacks to hospitalists viewing each patient encounter as an opportunity for a public health intervention. First, in viewing a patient as part of a cohort, the individual needs of the patient may be overlooked. There is inherent tension between population‐based and individual‐based care, which is a challenge. Second, hospitalists are busy clinicians who may be most highly valued because of their focus on efficiency and cost savings in the acute care setting. This factor alone may prevent substantive involvement by hospitalists in public health practice. Moving beyond the management of an acute illness may interfere with this efficiency and cost effectiveness from the hospital's perspective. However, interventions that promote health and prevent or reduce rehospitalizations may be cost effective to society in the long run. Third, current billing systems do not adequately reward or reimburse providers for the extra time that may be necessary to engage in public health practice. Fourth, hospitalists may not have the awareness, interest, training, or commitment to engage in public health practice. Finally, there may not be effective collaboration and communication systems between primary care providers and hospitalists. This barrier limits or hinders many possibilities for the effective execution of several public health initiatives.
CONCLUSIONS AND IMPLICATIONS
Hospitalists and the specialty of hospital medicine materialized because of myriad economic forces and the need to provide safe, high‐quality care to hospitalized patients. In this article we have described the ways in which hospitalists can be explicitly involved in public health practice. Traditionally, physicians caring for hospitalized patients have collected information through histories and physical examinations, interpreted laboratory data and tests, and formulated assessments and plans of care. To become public health practitioners, hospitalists have to go beyond these tasks and consider public health thought processes, such as problem‐solving paradigms and theories of behavior change. In adopting this public health perspective, hospitalists may begin to think of a patient in the context of the larger community in order to define the problems facing the community, not just the patient, determine the magnitude of such problems, identify key stakeholders, create intervention/prevention strategies, set priorities and recommend interventions, and implement and evaluate those interventions. This approach forces providers to move beyond the physicianpatient model and draw on public health models to invoke change. Hopefully, future research will further convince hospitalists of the benefits of this approach. Although it may be easier to defer care and management decisions to an outpatient physician, data suggest that intervening when patients are in the hospital may be most effective.62, 63 For example, is it possible that patients are more likely to quit smoking when they are sick in the hospital than when they are in their usual state of health on a routine visit at their primary care provider's office?64 Further, although deferring care to a primary care provider (PCP) may be easier, it is not always possible given these barriers: (1) some patients are routinely rehospitalized, precluding primary care visits, (2) some recommendations may not be received by PCPs, and (3) PCPpatient encounters are brief and the agendas full, and there are limited resources to address recommendations from the hospital.
As hospitalists become more involved in public health practice, their collaboration with physicians and researchers in other fields, nurses, policymakers, and administrators will expand. Succeeding in this arena requires integrity, motivation, capacity, understanding, knowledge, and experience.65 It is hoped that hospitalists will embrace the opportunity and master the requisite skill set necessary to practice in and advance this field. As hospitalist fellowship programs are developed, public health practice skills could be incorporated into the curriculum. Currently 6 of 16 fellowship programs offer either a master of public health degree or public health courses.66 Public health skills can also be taught at Society of Hospital Medicine meetings and other continuing medical education events.
With the evolution of hospital medicine, hospitalists have to be malleable in order to optimally meet the needs of the population they serve. The possibilities are endless.
The field of hospital medicine came into being in response to numerous factors involving physicians, patients, and hospitals themselves1 Now, years later, hospital medicine is a specialty that is growing, both in size and sophistication such that the role of the hospitalist is constantly evolving.2 A compelling function that has not yet been clearly articulated is the opportunity for hospitalists to serve as public health practitioners in their unique clinical environment. There is precedence for the power of collaboration between medicine and public health as has been seen with emergency medicine's willingness to embrace opportunities to advance public health.35
In public health, the programs, services, and institutions involved emphasize the prevention of disease and the health needs of the population as a whole. Public health activities vary with changing technology and social values, but the goals remain the same: to reduce the amount of disease, premature death, and disease‐associated discomfort and disability in the population.6 The authors of a leading textbook of public health, Scutchfield and Keck, contend that the most important skill for public health practice is the capacity to visualize the potential for health that exists in a community.6
Hospitalists care for a distinct subset of the general populationinpatients, only a small percentage of society in a given year. Yet over time hospitalists affect a substantial subset of the larger population that uses considerable health care resources.79 Furthermore, hospitalization can be a sentinel event with public health implications (eg, newly diagnosed HIV infection or acute myocardial infarction in a patient with an extended family of cigarette smokers). This presents an opportunity to educate and counsel both the patient and the patient's social network. One model of public health practice by hospitalists is to influence the patient, his or her family, and the community by touching and inspiring the hospitalized patient.
Hospitalists are already involved in many of the core functions of public health (assessment, assurance, and policy development; Fig. 1).10 Achieving ongoing success in this arena means developing hospitalists who are consciously in tune with their roles as public health practitioners.
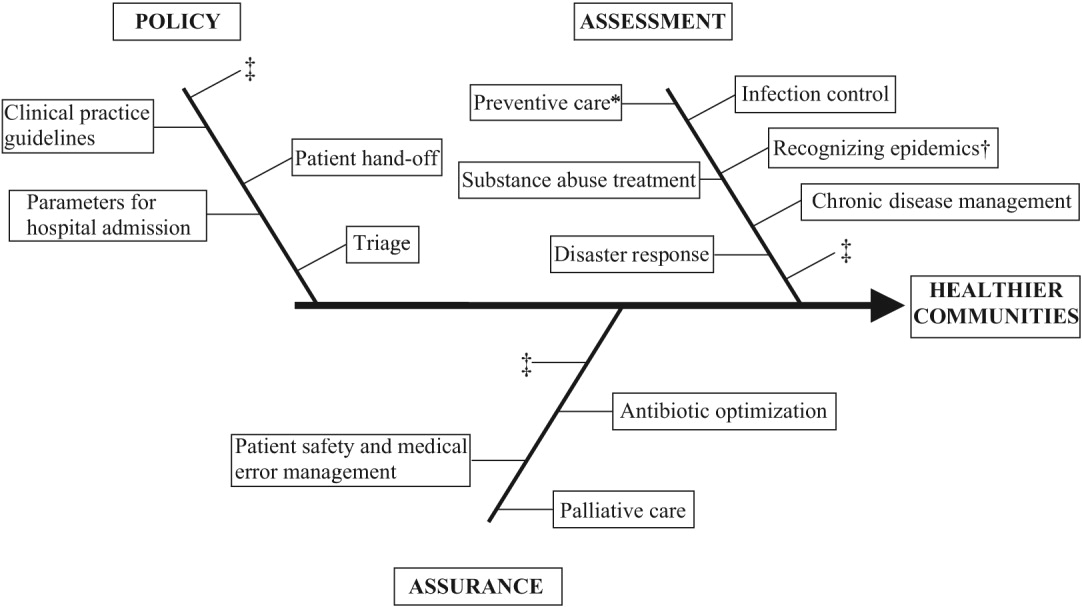
In this article we define the specific public health contributions that hospitalists have made and describe the possibilities for further innovative advances. To this end, we outline specific public health roles under the broad categories of assessment, assurance, and policy. We point to advances in public health accomplished by hospitalists as well as those being performed by nonhospitalists in the hospital setting. We conclude by describing some of the barriers to and implications of hospitalists taking on public health roles.
ASSESSMENT
Assessment is the systematic collection, analysis, and dissemination of health status information.10 These activities include disease surveillance and investigation of acute outbreaks or changes in the epidemiology of chronic diseases. Assessment also involves understanding the health of a population and the key determinants of a population's health from a variety of perspectives: physical, biological, behavioral, social, cultural, and spiritual.6 Human health has been defined as a state characterized by anatomic integrity; ability to perform personally valued family work and community roles; ability to deal with physical, biologic, and social stress; a feeling of well‐being; and freedom from the risk of disease and untimely death.6 Hospitalists interact with individuals at times of stress and acute illness and thus have a unique opportunity to assess the strength, viability, and resources available to individuals. Key roles that may fall within the auspices of assessment in hospital medicine are infection control, epidemic recognition, disaster response, preventive care, substance abuse treatment, and chronic disease management.
Infection Control
Physicians caring for inpatients have a crucial stake in controlling hospital infection as exemplified by the work of Flanders et al. on preventing nosocomial infections, especially nosocomial pneumonia.11 They describe specific strategies to prevent iatrogenic spread such as washing hands before and after patient contact, establishing guidelines against the use of artificial fingernails, using indwelling devices such as catheters only when absolutely necessary, and using sterile barriers.11 Hospitalists such as Sanjay Saint have led the way in studying methods to reduce bladder catheterization, which has been associated with urinary tract infections12; others have collaborated on work to prevent infections in nursing homes.13 Given the importance of this field, there is room for further hospitalist involvement. Novel methods for infection control in hospitals have been studied by nonhospitalists such as Wisnivesky, who prospectively validated a clinical decision rule to predict the need for respiratory isolation of inpatients with suspected tuberculosis (TB). This prediction rule, which is based on clinical and chest radiographic findings, was able to accurately identify patients at low risk for TB from among inpatients with suspected active pulmonary TB isolated on admission to the hospital.14 Retrospective application of the prediction rule showed respiratory precautions were inappropriately implemented for a third of patients.14 These studies are examples of empiric public health research performed in the inpatient setting. In the infection control domain, candidate issues for further study could include interventions aimed at reducing rates of Clostridium difficile, developing programs for standardized surveillance of hospital infection, validating electronic markers for nosocomial infection, and taking innovative approaches to improving hand‐washing practices in the hospital.15, 16
Recognizing Epidemics
An excellent example of the importance of hospitalists embracing public health and remembering their patients are part of a community was the severe acute respiratory syndrome (SARS) outbreak in Toronto, Ontario, Canada. The outbreak is thought to have begun with a single traveler. With the transfer of patients and the movement of visitors and health care workers among facilities, SARS quickly spread through Toronto, making it the largest SARS‐affected area outside Asia.17 Approximately a month after the outbreak was recognized in Toronto, it was thought to be over, and the World Health Organization (WHO) removed Toronto from its SARS‐affected list.17 Unfortunately, patients with unrecognized SARS remained in health care institutions, including a patient transferred to a rehabilitation center. Infection quickly spread again, resulting in a second phase of the outbreak.17
The SARS outbreak served as a reminder that a global public health system is essential and taught many lessons17 germane to pandemics that recur annually (eg, influenza viruses) as well those that episodically threaten the health of the population (eg, avian flu). Proposed actions to prevent a repeat of the scenario that occurred with SARS in Toronto include assessing the current facilities (eg, isolation rooms and respiratory masks) at each institution, identifying health care workers willing to serve as an outbreak team, and the hiring staff to train hospital personnel in personal protective equipment (PPE) and infection control policies.18 The Centers for Disease Control and Prevention (CDC) contends that planning for the possibility of a virulent pandemic at the local, national, and global levels is critical to limiting the mortality and morbidity should such occur.19, 20 In a previous article, Pile and Gordon declared hospitalists are key players in institutional efforts to prepare for a viral pandemic such as influenza and should be aware of lessons that may be applied from responses to pandemics such as SARS.19 Well placed to recognize clinical trends that may herald epidemics, hospitalists can fulfill some of the necessary public health responsibilities delineated above.
Disaster Response
Natural disasters and terrorism are in the forefront of the popular press and are also high priorities in health care and public health.21 Terrorism and natural disasters cause significant injury, illness, and death.22 Hospital‐based health care providers fulfill a variety of roles when terrorist acts and disasters occur, including reporting, diagnosing, and managing illness, providing preventive measures (eg, vaccines and preparedness kits), preventing the secondary spread of disease, assisting in the investigation of the causes of disease outbreaks, participating in preparedness planning, and evaluating preparedness policies and programs.22 The experience gained in the aftermaths of Hurricanes Katrina and Rita with their unprecedented death, injury, destruction, and displacement should help to guide future response and recovery activities.23 Hospitalists were at the forefront of delivering care, living in their hospitals for days after Hurricane Katrina. Without question, hospitalists will be called on again to serve those affected by disasters.
Preventive Care
For many patients admitted to the hospital, meeting a hospitalist is their first encounter with a physician in years.24, 25 In these instances, hospitalists must ensure that patients' immunizations are up‐to‐date and arrange appropriate follow‐up care with primary care providers. Greenwald described an important role that hospitalists could play in HIV prevention by promoting HIV testing in the hospital.26 The CDC recently confirmed the wisdom of this approach and estimates that the 250,000 to 1.2 million people in the United States with HIV infection who do not know their serostatus play a significant role in HIV transmission.26, 27 In an effort to promote testing, the CDC has initiated a program aimed at incorporating HIV testing into routine medical care, as recommended by others.28 More than a quarter of patients with HIV in the United States are diagnosed in the hospital, and for many other patients, hospitalization is their only real opportunity to be tested.26, 29 Similarly, when hospitalists find elevated cholesterol or triglycerides in routine evaluations of patients who present with chest pain, they have to decide whether to initiate lipid‐lowering medications.30 The hospitalist is sometimes the only physician that patients repeatedly admitted, may see over prolonged periods. It follows that if hospitalists are remiss in delivering preventive care to such patients, they lose the opportunity to positively affect their long‐term health. In practice, hospitalists perform myriad preventive‐care functions, although there is scant literature supporting this role. Hospitalists have an opportunity to collaborate in research projects of hospital‐initiated preventive care that measure outcomes at the community level.
Substance Abuse
In the Unites States, 25%‐40% of hospital admissions are related to substance abuse and its sequelae.31 These patients frequently are admitted to general medicine services for detoxification or treatment of substance‐abuse‐related morbidity, although some American hospitals have specialized treatment and detoxification centers. There is a pressing need for more models of comprehensive care that address the complex issues of addiction, including the biological, social, cultural, spiritual, and developmental needs of patients.32
Hospitalists routinely counsel their patients with substance abuse problems and often consult a chemical dependency counselor, who provides patients with additional information about outpatient or inpatient facilities that may help them after their hospitalization. Unfortunately, because of the natural history of substance abuse, many of these patients are rehospitalized with the same problems even after going through rehabilitation. The adoption of a public health philosophy and approach by hospitalists may assist patients who have addictions through innovative multidisciplinary interventions while these patient are being detoxified. Traditionally, these responsibilities have fallen to primary care providers and psychologists in substance abuse medicine; but, as mentioned previously, many such patients are rehospitalized before they make it to their follow‐up appointments.
In a study examining smoking cessation practices among Norwegian hospital physicians, 98% of the doctors stated they ask their patients about their smoking habits, but fewer than 7% of these physicians regularly offer smoking‐cessation counseling, hand out materials, or give patients other advice about smoking cessation.33 That study illustrates that hospital doctors often ask about problems but can certainly improve in terms of intervention and follow‐up. Other works by nonhospitalist physicians have examined the real potential of inpatient interventions for smoking cessation. Most of this work involves a multidisciplinary approach that relies heavily on nurses. For example, Davies et al. evaluated the effectiveness of a hospital‐based intervention for smoking cessation among low‐income smokers using public health methodologies. The intervention was effective and promising as a way to affect smokers in underserved communities.34
Chronic Disease Management
Public health roles involving chronic disease management include surveillance, intervention design, and implementation of control programs.6 Given their access to data on hospitalized patients, hospitalists can carry out surveillance and empirical population‐based research about hospitalized patients with chronic illnesses. Thoughtfully designed protocols can measure the success of interventions initiated in patients while hospitalized, with further data collection and follow‐up after patients have returned to the community.35 Such endeavors can improve the likelihood that patients with chronic conditions are effectively referred to programs that will maintain their health and functional status.36 If hospitalists consider themselves public health providers, encounters with these hospitalized patients will go beyond noting that their chronic conditions are stable and instead will lay the groundwork to prospectively control these conditions. This approach would have the potential to reduce the number of future hospitalizations and lead to healthier communities.37 To truly carry this out effectively, coordinated collaboration between primary care providers and hospitalists will be necessary.
ASSURANCE
Assurance is the provision of access to necessary health services. It entails efforts to solve problems that threaten the health of populations and empowers individuals to maintain their own health. This is accomplished by either encouraging action, delegating to other entities (private or public sector), mandating specific requirements through regulation, or providing services directly.10 Hospitalist teams aim to ensure that the high‐quality services needed to protect the health of their community (hospitalized patients) are available and that this population receives proper consideration in the allocation of resources. The few studies to date that have directly examined the quality of care that hospitalists provide38 have done so using evidence‐based measures believed to correlate with improved health care outcomes.38 The ambiguities in assessing quality may in part limit such studies.39 Specific hospitalist roles that fall under the assurance umbrella include antibiotic optimization, palliative care, patient safety, and medical error management.
Antibiotic Optimization
Inappropriate use of antimicrobial treatment for infectious diseases has cost and public health implications.40 These inappropriate uses include giving antibiotics when not indicated, overusing broad‐spectrum antibiotics, making mismatches between microbes and medicines when cultures and information on test sensitivity are available, and using intravenous formulations when oral therapy would suffice.41 The public health impact goes way beyond increasing selective pressure for antimicrobial resistance to include safety, adverse events, and increased costs to both patient and hospitals.40 At our institution, the hospital medicine service and infectious disease division have jointly developed and implemented an intervention to reduce inappropriate antibiotic use. At other institutions, hospitalist teams have developed protocols for treating infectious diseases commonly encountered in the hospitalized patient.42 The recommendations of both Amin and Reddy for management of community‐ and hospital‐acquired pneumonia acknowledged that through establishment of clinical care pathways, variation in prescribing patterns among hospitalists can be decreased while optimizing outcomes.42 The work of Williams and colleagues is another example of advances by hospitalists. They reviewed the literature to determine that the use of combination antibiotics as empiric therapy for community‐acquired pneumonia is superior to the use of a single effective antibiotic in treating bacteremic patients with pneumococcal community‐acquired pneumonia.43
Palliative Care
Mortality is a vital outcome measure of public health research and interventions. Not surprisingly, many people are hospitalized in the final months of their life and often die in a hospital. Pantilat showed that hospitalists can respond to these circumstances and have the opportunity to improve care of the dying.4446 Muir et al. evaluated the convergence of the fields of palliative care medicine and hospital medicine and reviewed the opportunities for mutual education and improved patient care.47 They described how the confluence of the changing nature and site of death in the United States coupled with the reorganization of hospital care provides a strategic opportunity to improve end‐of‐life care.47 Hospitalists can ensure that care of the dying is delivered with skill, compassion, and expertise. And so it is imperative they be trained to accomplish this objective.47, 49
Fortunately, hospitalists already appear to enhance patientphysician communication. Auerbach looked at communication, care patterns, and outcomes of dying patients, comparing patients being cared for by hospitalists with those being care for by community‐based physicians. Hospitalists had discussions with patients or their families about care more often than did nonhospitalist physicians (91% versus 73%, respectively, P = .006).49 Because the delivery of high‐quality palliative care is time consuming and complex, alternative models for billing or the use of physician extenders or consultants may be necessary at some institutions.
Patient Safety and Medical Error Management
Hospitalists have been in the forefront of promoting a culture of patient safety.50 Their continuous presence in the hospital and their interactions with members of health care teams from multiple disciplines who share this goal make them important facilitators. Hospitalists have increasing involvement in systems‐based efforts aimed at reducing medical errors.50 Hospitalists are being asked to lead committees that adopt multidisciplinary approaches to reduce adverse events, morbidity, and mortality.50 These committees often have representation from pharmacy, nursing, and other key hospital stakeholders including from the administration.51 Quality assurance activities assess locally collected data and compare results with local and national benchmarks. There are several published examples of hospitalists engaged in patient safety and medical error management. For example, Shojania et al compiled evidence based safety practices in an effort to promote patient safety.52, 53 Schnipper studied the role of pharmacist counseling in preventing adverse drug events (ADEs) after hospitalization and found that pharmacist medication review, patient counseling, and telephone follow‐up were associated with a lower rate of preventable ADEs 30 days after hospital discharge.54 Moreover, Syed paired hospitalists and pharmacists to collaboratively prescribe medications appropriately. In one study there were fewer medication errors and adverse drug reactions in patients treated by a team led by hospitalists than in those treated by the control group, made up of nonhospitalist attendings.55
POLICY
Policy development defines health control goals and objectives and develops implementation plans for those goals.10 By necessity, it operates at the intersection of legislative, political, and regulatory processes.10 At many institutions, hospitalists have been involved in the development of policies ensuring that the core functions of assessment and assurance are addressed and maintained. In fact, hospitalists report that development of quality assurance and practice guidelines accounts for most of their nonclinical time.56 This role of hospitalists is supported by anecdotal reports rather than published empiric evidence.57 For example, at Johns Hopkins Bayview Medical Center, hospitalist‐led teams have developed triage and patient handoff policies designed to improve patient safety. Parameters for admission to the general medicine ward have been elaborated and are periodically refined by the hospitalist team.
Another area that falls within the genre of policy is development of clinical practice guidelines. Guidelines for the treatment of pneumonia, congestive heart failure, deep‐vein thrombosis prophylaxis, alcohol and drug withdrawal, pain management, delirium, and chronic obstructive pulmonary disease have been developed by nonhospitalists.58, 59 These areas are considered core competencies in hospital medicine, and as such, hospitalists have an obligation to review and refine these guidelines to ensure the best provision of care to our patients.59
Hospitalists have been engaged in upholding guidelines that affect community practice. For example, in a study comparing treatment of patients admitted with congestive heart failure by hospitalists compared with that by nonhospitalists, hospitalists were found to be more likely to document left ventricular function, a core measure of quality as defined by JCAHO.39, 60 Knowledge about cardiac function can direct future care for patients when they return to the community and into the care of their primary care providers. In another example, Rifkin found that patients with community‐acquired pneumonia treated by hospitalists were more rapidly converted to oral antibiotics from intravenous antibiotics, facilitating a shorter length of stay,61 which reduced the opportunity for nosocomial infections to propagate. Because hospitalists are skilled at following guidelines,59 it follows that they should seize the opportunity to develop more of them.
As the hospitalist movement continues to grow, hospitalists will likely be engaged in implementing citywide, statewide, and even national policies that ensure optimal care of the hospitalized patient.
BARRIERS TO HOSPITALISTS FOCUSING ON PUBLIC HEALTH
Hospitalists are involved in public health activities even though they may not recognize the extent of this involvement. However, there may be some drawbacks to hospitalists viewing each patient encounter as an opportunity for a public health intervention. First, in viewing a patient as part of a cohort, the individual needs of the patient may be overlooked. There is inherent tension between population‐based and individual‐based care, which is a challenge. Second, hospitalists are busy clinicians who may be most highly valued because of their focus on efficiency and cost savings in the acute care setting. This factor alone may prevent substantive involvement by hospitalists in public health practice. Moving beyond the management of an acute illness may interfere with this efficiency and cost effectiveness from the hospital's perspective. However, interventions that promote health and prevent or reduce rehospitalizations may be cost effective to society in the long run. Third, current billing systems do not adequately reward or reimburse providers for the extra time that may be necessary to engage in public health practice. Fourth, hospitalists may not have the awareness, interest, training, or commitment to engage in public health practice. Finally, there may not be effective collaboration and communication systems between primary care providers and hospitalists. This barrier limits or hinders many possibilities for the effective execution of several public health initiatives.
CONCLUSIONS AND IMPLICATIONS
Hospitalists and the specialty of hospital medicine materialized because of myriad economic forces and the need to provide safe, high‐quality care to hospitalized patients. In this article we have described the ways in which hospitalists can be explicitly involved in public health practice. Traditionally, physicians caring for hospitalized patients have collected information through histories and physical examinations, interpreted laboratory data and tests, and formulated assessments and plans of care. To become public health practitioners, hospitalists have to go beyond these tasks and consider public health thought processes, such as problem‐solving paradigms and theories of behavior change. In adopting this public health perspective, hospitalists may begin to think of a patient in the context of the larger community in order to define the problems facing the community, not just the patient, determine the magnitude of such problems, identify key stakeholders, create intervention/prevention strategies, set priorities and recommend interventions, and implement and evaluate those interventions. This approach forces providers to move beyond the physicianpatient model and draw on public health models to invoke change. Hopefully, future research will further convince hospitalists of the benefits of this approach. Although it may be easier to defer care and management decisions to an outpatient physician, data suggest that intervening when patients are in the hospital may be most effective.62, 63 For example, is it possible that patients are more likely to quit smoking when they are sick in the hospital than when they are in their usual state of health on a routine visit at their primary care provider's office?64 Further, although deferring care to a primary care provider (PCP) may be easier, it is not always possible given these barriers: (1) some patients are routinely rehospitalized, precluding primary care visits, (2) some recommendations may not be received by PCPs, and (3) PCPpatient encounters are brief and the agendas full, and there are limited resources to address recommendations from the hospital.
As hospitalists become more involved in public health practice, their collaboration with physicians and researchers in other fields, nurses, policymakers, and administrators will expand. Succeeding in this arena requires integrity, motivation, capacity, understanding, knowledge, and experience.65 It is hoped that hospitalists will embrace the opportunity and master the requisite skill set necessary to practice in and advance this field. As hospitalist fellowship programs are developed, public health practice skills could be incorporated into the curriculum. Currently 6 of 16 fellowship programs offer either a master of public health degree or public health courses.66 Public health skills can also be taught at Society of Hospital Medicine meetings and other continuing medical education events.
With the evolution of hospital medicine, hospitalists have to be malleable in order to optimally meet the needs of the population they serve. The possibilities are endless.
- ,.The Hospitalist movement 5 years later.JAMA.2002;287:487–494.
- Hospitals and Health Networks. Hospitalists: a specialty coming into its own. Available at: http://www.hhmag.com. Accessed February 27,2006.
- ,,.Emergency medicine and public health: new steps in old directions.Ann Emerg Med.2001;38:675–683.
- ,, et al.A public health approach to emergency medicine: preparing for the twenty‐first century.Acad Emerg Med.1994;1:277–286.
- ,.Emergency medicine in population‐based systems of care.Ann Emerg Med.1997;30:800–803.
- ,.Principles of Public Health Practice.Albany, NY:Delmar Publishing;1997.
- Centers for Medicare and Medicaid. Health care spending and growth rate continue to decline in 2004. Available at: http://www.cms.hhs.gov. Accessed October 31,2006.
- ,,, et al.National health expenditures, 2002.Health Care Financ Rev. Summer2004;25:4.
- ,,, et al.Health spending Projections Through 2015: Changes on the Horizon.Health Affairs2006;25:w61–w73.
- Institute of Medicine.Recommendations from the Future of Public Health. InThe Future of the Public's Health.Washington, DC:National Academic Press;2003:411–420.
- ,,.Nosocomial pneumonia: state of the science.Am J Infect Control.2006;34:84–93.
- ,,,,.A reminder reduces urinary catheterization in hospitalized patients.Jt Comm J Qual Patient Saf.2005;31:455–462.
- ,,,.Preventing infections in nursing homes: A survey of infection control practices in southeast Michigan.Am J Infect Control.2005;33:489–492.
- ,,,.Prospective validation of a prediction model for isolating inpatients with suspected pulmonary tuberculosis.Arch Intern Med.2005;165:453–457.
- ,.The Hospital Infection Standardised Surveillance (HISS) programme: analysis of a two‐year pilot.J Hosp Infect.2003;53:259–267.
- ,,,.A Laboratory‐Based, Hospital‐Wide, Electronic Marker for Nosocomial Infection.Am J Clin Pathol.2006;125:34–39.
- ,,.Severe acute respiratory syndrome.Arch Pathol Lab Med.2004;128:1346–1350.
- ,,.Severe acute respiratory syndrome: responses of the healthcare system to a global epidemic.Curr Opin Otolaryngol Head Neck Surg.2005;13:161–164.
- ,.Pandemic influenza and the hospitalist: apocalypse when?J Hosp Med.2006;1:118–123.
- Center for Disease Control and Prevention. Pandemic Influenza information for Health Professionals. Available at: http://www.cdc.gov/flu/pandemic/. Accessed October 31,2006.
- .US health policy in the aftermath of Hurricane Katrina.JAMA.2006;295:437–40
- Levy B,Sidel V, eds.Terrorism and Public Health.New York:Oxford University Press;2003.
- Centers for Disease Control and Prevention (CDC).Public health response to Hurricanes Katrina and Rita—United States 2005.MMWR Morb Mortal Wkly Rep.2006;55:229–231.
- ,,,,,.Racial and ethnic disparities in health: a view from the South Bronx.J Health Care Poor Underserved.2006;17:116–127.
- ,.Williams E. Health Seeking behaviors of African Americans: implications for health administration.J Health Hum Serv Adm.2005;28(1):68–95.
- .Routine rapid HIV testing in hospitals: another opportunity for hospitalists to improve care.J Hosp Med.2006;1:106–112.
- Centers for Disease Control and Prevention.Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003.MMWR Morb Mortal Wkly Rep.2003;52:329–332.
- ,,, et al.Expanded screening for HIV in the United States—an analysis of cost‐effectiveness.N Engl J Med.2005;352:586–595.
- ,,,.Identifying undiagnosed human immunodeficiency virus: the yield for routine, voluntary, inpatient testing.Arch Intern Med.2002;162:887–892.
- ,,,,.Insufficient treatment of hypercholestrolemia among patients hospitalized with chest pain.Clin Cardiol.2006;29:259–262.
- .Medical management of alcoholic patients. In:Kissen B,Besleiter H, eds.Treatment and Rehabilitation of the Chronic Alcoholic.New York:Plenum Publishing Co.;1997.
- ,,.An integral approach to substance abuse.J Psychoactive Drugs.2005;37:363–371.
- ,,, et al.Smoking cessation practice among Norwegian hospital physicians.Tiddskr Nor laegeforen.2000;120:1629–1632.
- ,, et al.Evaluation of an intervention for hospitalized African American smokers.Am J Health Behav.2005;29:228–239.
- .Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs [review].J Am Geriatr Soc.2003;51:549–555.
- ,,,,.Advances in hospital medicine: a review of key articles from the literature.Med Clin N Am.2002;86:797–823.
- ,,,,,.Comprehensive discharge planning with post discharge support for older patients with congestive heart failure.JAMA.2004;291:1358–1367.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis.Med Care Res Rev.2005;62:379–406.
- ,,,,,Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists.Arch Intern Med.2002;162:1251–1256.
- ,,,.Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) colloquim, 2002.Lancet Infect Dis.2004;4:44–53.
- ,,, et al.Systematic review of antimicrobial drug prescribing in hospitals.Emerg Infect Dis.2006;12:211–216.
- ,,,,,,.Recommendations for management of community and hospital acquired pneumonia‐the hospitalist perspective.Curr Opin Pulm Med.2004;10(suppl 1):S23–S27.
- ,,,,.Advances in hospital medicine: a review of key articles from the literature.Med Clin N Am.2002;86:797–823.
- .End‐of‐life care for the hospitalized patient.Med Clin N Am.2002;86:749–770.
- ,.Palliative care for patients with heart failure.JAMA.2004;291:2476–2482.
- ,.Prevalence and structure of palliative care services in California hospitals.Arch Intern Med.2003;163:1084–1088.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.J Med.2001;111:10S–14S.
- .Palliative care in hospitals.J Hosp Med.2006;1:21–28.
- ,.End‐of‐life care in a voluntary hospitalist model: effects on communication, process of care, and patient symptoms.Am J Med.2004;116:669–675.
- ,,,Understanding medical error and improving patient safety in the inpatient setting,Med Clin N Am2002;86:847–867.
- , The hospitalist movement: ten issues to consider, hospital practice. Available at: http://www.hosppract.com/issues/1999/02/wachter.htm. Accessed March 14,2006.
- Shojania KG,Duncan BW,McDonald KM,Wachter RM, eds.Making health care safer: a critical analysis of patient safety practices. Evidence Report/Technology Assessment No. 43 from the Agency for Healthcare Research and Quality: AHRQ Publication No. 01‐E058;2001. Available at: http://www.ahrq.gov/clinic/ptsafety/.
- ,,,.Safe but sound: patient safety meets evidence‐based medicine.JAMA.2002;288:508–513.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- Hospitalists, pharmacists partner to cut errors: shorter lengths of stay, lower med costs result. HealthCare Benchmarks and Quality Improvement.American Health Consultants, Inc.,2005.
- ,,,.Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians.Ann Intern Med.1999;130:343–349.
- ,,,,.Core competencies in hospital medicine: Development and methodology.J Hosp Med.2006;1:48–56.
- National guideline clearing house. Available at: http://www.guideline.gov. Accessed June 26,2006.
- ,,,,, eds.The core competencies in hospital medicine.J Hosp Med.2006;1(suppl 1).
- Joint Commission on Accreditation of Healthcare Organizations. Core Measures overview. Available at: http://www.jcaho.org/perfeas/coremeas/cm.ovrvw.html. Accessed February 1,2006.
- ,,,.,Comparison of processes and outcomes of pneumonia care between hospitalists and community‐based primary care physicians.Mayo Clin Proc.2002;77:1053–1058.
- ,.The effectiveness of a nursing inpatient smoking cessation program in individuals with cardiovascular disease.Nurs Res.2005;54:243–254.
- ,,,,,.Evaluation of an intervention for hospitalized African American smokers.Am J Health Behav.2005;29:228–239.
- .Smoking cessation: the case for hospital‐based interventions.Prof Nurse.2003;19(3):145–148..
- . Dee Hock's management principles, in his own words. Fast Company.1996;5:79. Available at: http://www.fastcompany.com/magazine/05/dee2.html.
- ,,,.Hospital Medicine Fellowships: Works in progress.Am J Med.2006;119(1):72.e1–e7.
- ,.The Hospitalist movement 5 years later.JAMA.2002;287:487–494.
- Hospitals and Health Networks. Hospitalists: a specialty coming into its own. Available at: http://www.hhmag.com. Accessed February 27,2006.
- ,,.Emergency medicine and public health: new steps in old directions.Ann Emerg Med.2001;38:675–683.
- ,, et al.A public health approach to emergency medicine: preparing for the twenty‐first century.Acad Emerg Med.1994;1:277–286.
- ,.Emergency medicine in population‐based systems of care.Ann Emerg Med.1997;30:800–803.
- ,.Principles of Public Health Practice.Albany, NY:Delmar Publishing;1997.
- Centers for Medicare and Medicaid. Health care spending and growth rate continue to decline in 2004. Available at: http://www.cms.hhs.gov. Accessed October 31,2006.
- ,,, et al.National health expenditures, 2002.Health Care Financ Rev. Summer2004;25:4.
- ,,, et al.Health spending Projections Through 2015: Changes on the Horizon.Health Affairs2006;25:w61–w73.
- Institute of Medicine.Recommendations from the Future of Public Health. InThe Future of the Public's Health.Washington, DC:National Academic Press;2003:411–420.
- ,,.Nosocomial pneumonia: state of the science.Am J Infect Control.2006;34:84–93.
- ,,,,.A reminder reduces urinary catheterization in hospitalized patients.Jt Comm J Qual Patient Saf.2005;31:455–462.
- ,,,.Preventing infections in nursing homes: A survey of infection control practices in southeast Michigan.Am J Infect Control.2005;33:489–492.
- ,,,.Prospective validation of a prediction model for isolating inpatients with suspected pulmonary tuberculosis.Arch Intern Med.2005;165:453–457.
- ,.The Hospital Infection Standardised Surveillance (HISS) programme: analysis of a two‐year pilot.J Hosp Infect.2003;53:259–267.
- ,,,.A Laboratory‐Based, Hospital‐Wide, Electronic Marker for Nosocomial Infection.Am J Clin Pathol.2006;125:34–39.
- ,,.Severe acute respiratory syndrome.Arch Pathol Lab Med.2004;128:1346–1350.
- ,,.Severe acute respiratory syndrome: responses of the healthcare system to a global epidemic.Curr Opin Otolaryngol Head Neck Surg.2005;13:161–164.
- ,.Pandemic influenza and the hospitalist: apocalypse when?J Hosp Med.2006;1:118–123.
- Center for Disease Control and Prevention. Pandemic Influenza information for Health Professionals. Available at: http://www.cdc.gov/flu/pandemic/. Accessed October 31,2006.
- .US health policy in the aftermath of Hurricane Katrina.JAMA.2006;295:437–40
- Levy B,Sidel V, eds.Terrorism and Public Health.New York:Oxford University Press;2003.
- Centers for Disease Control and Prevention (CDC).Public health response to Hurricanes Katrina and Rita—United States 2005.MMWR Morb Mortal Wkly Rep.2006;55:229–231.
- ,,,,,.Racial and ethnic disparities in health: a view from the South Bronx.J Health Care Poor Underserved.2006;17:116–127.
- ,.Williams E. Health Seeking behaviors of African Americans: implications for health administration.J Health Hum Serv Adm.2005;28(1):68–95.
- .Routine rapid HIV testing in hospitals: another opportunity for hospitalists to improve care.J Hosp Med.2006;1:106–112.
- Centers for Disease Control and Prevention.Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003.MMWR Morb Mortal Wkly Rep.2003;52:329–332.
- ,,, et al.Expanded screening for HIV in the United States—an analysis of cost‐effectiveness.N Engl J Med.2005;352:586–595.
- ,,,.Identifying undiagnosed human immunodeficiency virus: the yield for routine, voluntary, inpatient testing.Arch Intern Med.2002;162:887–892.
- ,,,,.Insufficient treatment of hypercholestrolemia among patients hospitalized with chest pain.Clin Cardiol.2006;29:259–262.
- .Medical management of alcoholic patients. In:Kissen B,Besleiter H, eds.Treatment and Rehabilitation of the Chronic Alcoholic.New York:Plenum Publishing Co.;1997.
- ,,.An integral approach to substance abuse.J Psychoactive Drugs.2005;37:363–371.
- ,,, et al.Smoking cessation practice among Norwegian hospital physicians.Tiddskr Nor laegeforen.2000;120:1629–1632.
- ,, et al.Evaluation of an intervention for hospitalized African American smokers.Am J Health Behav.2005;29:228–239.
- .Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs [review].J Am Geriatr Soc.2003;51:549–555.
- ,,,,.Advances in hospital medicine: a review of key articles from the literature.Med Clin N Am.2002;86:797–823.
- ,,,,,.Comprehensive discharge planning with post discharge support for older patients with congestive heart failure.JAMA.2004;291:1358–1367.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the United States: a research synthesis.Med Care Res Rev.2005;62:379–406.
- ,,,,,Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists.Arch Intern Med.2002;162:1251–1256.
- ,,,.Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) colloquim, 2002.Lancet Infect Dis.2004;4:44–53.
- ,,, et al.Systematic review of antimicrobial drug prescribing in hospitals.Emerg Infect Dis.2006;12:211–216.
- ,,,,,,.Recommendations for management of community and hospital acquired pneumonia‐the hospitalist perspective.Curr Opin Pulm Med.2004;10(suppl 1):S23–S27.
- ,,,,.Advances in hospital medicine: a review of key articles from the literature.Med Clin N Am.2002;86:797–823.
- .End‐of‐life care for the hospitalized patient.Med Clin N Am.2002;86:749–770.
- ,.Palliative care for patients with heart failure.JAMA.2004;291:2476–2482.
- ,.Prevalence and structure of palliative care services in California hospitals.Arch Intern Med.2003;163:1084–1088.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.J Med.2001;111:10S–14S.
- .Palliative care in hospitals.J Hosp Med.2006;1:21–28.
- ,.End‐of‐life care in a voluntary hospitalist model: effects on communication, process of care, and patient symptoms.Am J Med.2004;116:669–675.
- ,,,Understanding medical error and improving patient safety in the inpatient setting,Med Clin N Am2002;86:847–867.
- , The hospitalist movement: ten issues to consider, hospital practice. Available at: http://www.hosppract.com/issues/1999/02/wachter.htm. Accessed March 14,2006.
- Shojania KG,Duncan BW,McDonald KM,Wachter RM, eds.Making health care safer: a critical analysis of patient safety practices. Evidence Report/Technology Assessment No. 43 from the Agency for Healthcare Research and Quality: AHRQ Publication No. 01‐E058;2001. Available at: http://www.ahrq.gov/clinic/ptsafety/.
- ,,,.Safe but sound: patient safety meets evidence‐based medicine.JAMA.2002;288:508–513.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- Hospitalists, pharmacists partner to cut errors: shorter lengths of stay, lower med costs result. HealthCare Benchmarks and Quality Improvement.American Health Consultants, Inc.,2005.
- ,,,.Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians.Ann Intern Med.1999;130:343–349.
- ,,,,.Core competencies in hospital medicine: Development and methodology.J Hosp Med.2006;1:48–56.
- National guideline clearing house. Available at: http://www.guideline.gov. Accessed June 26,2006.
- ,,,,, eds.The core competencies in hospital medicine.J Hosp Med.2006;1(suppl 1).
- Joint Commission on Accreditation of Healthcare Organizations. Core Measures overview. Available at: http://www.jcaho.org/perfeas/coremeas/cm.ovrvw.html. Accessed February 1,2006.
- ,,,.,Comparison of processes and outcomes of pneumonia care between hospitalists and community‐based primary care physicians.Mayo Clin Proc.2002;77:1053–1058.
- ,.The effectiveness of a nursing inpatient smoking cessation program in individuals with cardiovascular disease.Nurs Res.2005;54:243–254.
- ,,,,,.Evaluation of an intervention for hospitalized African American smokers.Am J Health Behav.2005;29:228–239.
- .Smoking cessation: the case for hospital‐based interventions.Prof Nurse.2003;19(3):145–148..
- . Dee Hock's management principles, in his own words. Fast Company.1996;5:79. Available at: http://www.fastcompany.com/magazine/05/dee2.html.
- ,,,.Hospital Medicine Fellowships: Works in progress.Am J Med.2006;119(1):72.e1–e7.
Copyright © 2007 Society of Hospital Medicine