User login
Alcohol-Related Hospitalizations During the Initial COVID-19 Lockdown in Massachusetts: An Interrupted Time-Series Analysis
The United States’ initial public health response to the COVID-19 pandemic included containment measures that varied by state but generally required closing or suspending schools, nonessential businesses, and travel (commonly called lockdown).1 During these periods, hospitalizations for serious and common conditions declined.2,3 In Massachusetts, a state of emergency was declared on March 10, 2020, which remained in place until May 18, 2020, when a phased reopening of businesses began.
Although the evidence on the mental health impact of containment periods has been mixed, it has been suggested that these measures could lead to increases in alcohol-related hospitalizations.4 Social isolation and increased psychosocial and financial stressors raise the risk of relapse among patients with substance use disorders.5-7 Marketing and survey data from the US and United Kingdom from the early months of the pandemic suggest that in-home alcohol consumption and sales of alcoholic beverages increased, while consumption of alcohol outside the home decreased.8-10 Other research has shown an increase in the percentage—but not necessarily the absolute number—of emergency department (ED) visits and hospitalizations for alcohol-related diagnoses during periods of containment.11,12 At least 1 study suggests that alcohol-related deaths increased beginning in the lockdown period and persisting into mid-2021.13
Because earlier studies suggest that lockdown periods are associated with increased alcohol consumption and relapse of alcohol use disorder, we hypothesized that the spring 2020 lockdown period in Massachusetts would be associated temporally with an increase in alcohol-related hospitalizations. To evaluate this hypothesis, we examined all hospitalizations in the US Department of Veterans Affairs (VA) Boston Healthcare System (VABHS) before, during, and after this lockdown period. VABHS includes a 160-bed acute care hospital and a 50-bed inpatient psychiatric facility.
Methods
We conducted an interrupted time-series analysis including all inpatient hospitalizations at VABHS from January 1, 2017, to December 31, 2020, to compare the daily number of alcohol-related hospitalizations across 3 exposure groups: prelockdown (the reference group, 1/1/2017-3/9/2020); lockdown (3/10/2020-5/18/2020); and postlockdown (5/19/2020-12/31/2020).
The VA Corporate Data Warehouse at VABHS was queried to identify all hospitalizations on the medical, psychiatry, and neurology services during the study period. Hospitalizations were considered alcohol-related if the International Statistical Classification of Diseases, Tenth Revision (ICD-10) primary diagnosis code (the main reason for hospitalization) was defined as an alcohol-related diagnosis by the VA Centralized Interactive Phenomics Resource (eAppendix 1, available online at doi:10.1278/fp.0404). This database, which has been previously used for COVID-19 research, is a catalog and knowledge-sharing platform of VA electronic health record–based phenotype algorithms, definitions, and metadata that builds on the Million Veteran Program and Cooperative Studies Program.14,15 Hospitalizations under observation status were excluded.
To examine whether alcohol-related hospitalizations could have been categorized as COVID-19 when the conditions were co-occurring, we identified 244 hospitalizations coded with a primary ICD-10 code for COVID-19 during the lockdown and postlockdown periods. At the time of admission, each hospitalization carries an initial (free text) diagnosis, of which 3 had an initial diagnosis related to alcohol use. The population at risk for alcohol-related hospitalizations was estimated as the number of patients actively engaged in care at the VABHS. This was defined as the number of patients enrolled in VA care who have previously received any VA care; patients who are enrolled but have never received VA care were excluded from the population-at-risk denominator. Population-at-risk data were available for each fiscal year (FY) of the study period (9/30-10/1); the following population-at-risk sizes were used: 38,057 for FY 2017, 38,527 for FY 2018, 39,472 for FY 2019, and 37,893 for FY 2020.
The primary outcome was the daily number of alcohol-related hospitalizations in the prelockdown, lockdown, and postlockdown periods. A sensitivity analysis was performed using an alternate definition of the primary outcome using a broader set of alcohol-related ICD-10 codes (eAppendix 2, available online at doi:10.1278/fp.0404).
Statistical Analysis
To visually examine hospitalization trends during the study period, we generated a smoothed time-series plot of the 7-day moving average of the daily number of all-cause hospitalizations and the daily number of alcohol-related hospitalizations from January 1, 2017, to December 31, 2020. We used multivariable regression to model the daily number of alcohol-related hospitalizations over prelockdown (the reference group), lockdown, and postlockdown. In addition to the exposure, we included the following covariates in our model: day of the week, calendar date (to account for secular trends), and harmonic polynomials of the day of the year (to account for seasonal variation).16
We also examined models that included the daily total number of hospitalizations to account for the reduced likelihood of hospital admission for any reason during the pandemic. We used generalized linear models with a Poisson link to generate rate ratios and corresponding 95% CIs for estimates of the daily number of alcohol-related hospitalizations. We estimated the population incidence of alcohol-related hospitalizations per 100,000 patient-months for the exposure periods using the population denominators previously described. All analyses were performed in Stata 16.1.
Results
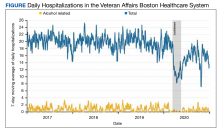
During the study period, 27,508 hospitalizations were available for analysis. The 7-day moving average of total daily hospitalizations and total daily alcohol-related hospitalizations over time for the period January 1, 2017, to December 31, 2020, are shown in the Figure.
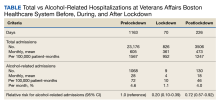
The incidence of alcohol-related hospitalizations in the population dropped from 72 per 100,000 patient-months to 10 per 100,000 patient-months during the lockdown period and increased to 46 per 100,000 patient-months during the postlockdown period (Table).
Our results were not substantially different when we ran a sensitivity analysis that excluded the total daily number of admissions from our model. Compared with the prelockdown period, the rate ratio for the number of alcohol-related hospitalizations during the lockdown period was 0.16 (95% CI, 0.08-0.30), and the rate ratio for the postlockdown period was 0.65 (95% CI, 0.52-0.82). We conducted an additional sensitivity analysis using a broader definition of the primary outcome to include all alcohol-related diagnosis codes; however, the results were unchanged.
Discussion
During the spring 2020 COVID-19 lockdown period in Massachusetts, the daily number of VABHS alcohol-related hospitalizations decreased by nearly 80% compared with the prelockdown period. During the postlockdown period, the daily number of alcohol-related hospitalizations increased but only to 72% of the prelockdown baseline by the end of December 2020. A similar trend was observed for all-cause hospitalizations for the same exposure periods.
These results differ from 2 related studies on the effect of the COVID-19 pandemic on alcohol-related hospitalizations.10,11 In a retrospective study of ED visits to 4 hospitals in New York City, Schimmel and colleagues reported that from March 1 to 31, 2020 (the initial COVID-19 peak), hospital visits for alcohol withdrawal increased while those for alcohol use decreased.10 However, these results are reported as a percentage of total ED visits rather than the total number of visits, which are vulnerable to spurious correlation because of concomitant changes in the total number of ED visits. In their study, the absolute number of alcohol-related ED visits did not increase during the initial 2020 COVID-19 peak, and the number of visits for alcohol withdrawal syndrome declined slightly (195 in 2019 and 180 in 2020). However, the percentage of visits increased from 7% to 10% because of a greater decline in total ED visits. This pattern of decline in the number of alcohol-related ED visits, accompanied by an increase in the percentage of alcohol-related ED visits, has been observed in at least 1 nationwide surveillance study.17 This apparent increase does not reflect an absolute increase in ED visits for alcohol withdrawal syndrome and represents a greater relative decline in visits for other causes during the study period.
Sharma and colleagues reported an increase in the percentage of patients who developed alcohol withdrawal syndrome while hospitalized in Delaware per 1000 hospitalizations during consecutive 2-week periods during the pandemic in 2020 compared with corresponding weeks in 2019.11 The greatest increase occurred during the last 2 weeks of the Delaware stay-at-home order. The Clinical Institute Withdrawal Assessment of Alcohol Scale, revised (CIWA-Ar) score of > 8 was used to define alcohol withdrawal syndrome. The American Society of Addiction Medicine does not recommend using CIWA-Ar to diagnose alcohol withdrawal syndrome because the scale was developed to monitor response to treatment, not to establish a diagnosis.18
Although the true population incidence of alcohol-related hospitalizations is difficult to estimate because the size of the population at risk (ie, the denominator) often is not known, the total number of hospitalizations is not a reliable surrogate.19 Individuals hospitalized for nonalcohol causes are no longer at risk for alcohol-related hospitalization.
In our study, we assume the population at risk during the study period is constant and model changes in the absolute number—rather than percentage—of alcohol-related ED visits. These absolute estimates of alcohol-related hospitalizations better reflect the true burden on the health care system and avoid the confounding effect of declining total ED visits and hospitalizations that could lead to artificially increased percentages and spurious correlation.20 The absolute percentage of alcohol-related hospitalizations also decreased during this period; therefore, our results are not sensitive to this approach.
Several factors could have contributed to the decrease in alcohol-related hospitalizations. Our findings suggest that patient likelihood to seek care and clinician threshold to admit patients for alcohol-related conditions are influenced by external factors, in this case, a public health lockdown. Although our data do not inform why hospitalizations did not return to prelockdown levels, our experience suggests that limited bed capacity and longer length of stay might have contributed. Other hypotheses include a shift to outpatient care, increased use of telehealth (a significant focus early in the pandemic), and avoiding care for less severe alcohol-related complications because of lingering concerns about exposure to COVID-19 in health care settings reported early in the pandemic. Massachusetts experienced a particularly deadly outbreak of COVID-19 in the Soldiers’ Home, a long-term care facility for veterans in Holyoke.21
Evidence suggests that in-home consumption of alcohol increased during lockdowns.8-10 Our results show that during this period hospitalizations for alcohol-related conditions decreased at VABHS, a large urban VA medical system, while alcohol-related deaths increased nationally.13 Although this observation is not evidence of causality, these outcomes could be related.
In the 2 decades before the pandemic, alcohol-related deaths increased by about 2% per year.22 From 2019 to 2020, there was a 25% increase that continued through 2021.13 Death certificate data often are inaccurate, and it is difficult to determine whether COVID-19 had a substantial contributing role to these deaths, particularly during the initial period when testing was limited or unavailable. Nonetheless, deaths due to alcohol-associated liver disease, overdoses involving alcohol, and alcohol-related traffic fatalities increased by > 10%.13,23 These trends, along with a decrease in hospitalization for alcohol-related conditions, suggest missed opportunities for intervention with patients experiencing alcohol use disorder.
Limitations
In this study, hospitalizations under observation status were excluded, which could underestimate the total number of hospitalizations related to alcohol. We reasoned that this effect was likely to be small and not substantially different by year. ICD-10 codes were used to identify alcohol-related hospitalizations as any hospitalization with an included ICD-10 code listed as the primary discharge diagnosis code. This also likely underestimated the total number of alcohol-related hospitalizations. An ICD-10 code for COVID-19 was not in widespread use during our study period, which prohibited controlling explicitly for the volume of admissions due to COVID-19. The prelockdown period only contains data from the preceding 3 years, which might not be long enough for secular trends to become apparent. We assumed the population at risk remained constant when in reality, the net movement of patients into and out of VA care during the pandemic likely was more complex but not readily quantifiable. Nonetheless, the large drop in absolute number of alcohol-related hospitalizations is not likely to be sensitive to this change. In the absence of an objective measure of care-seeking behavior, we used the total daily number of hospitalizations as a surrogate for patient propensity to seek care. The total daily number of hospitalizations also reflects changes in physician admitting behavior over time. This allowed explicit modeling of care-seeking behavior as a covariate but does not capture other important determinants such as hospital capacity.
Conclusions
In this interrupted time-series analysis, the daily number of alcohol-related hospitalizations during the initial COVID-19 pandemic–associated lockdown period at VABHS decreased by 80% and remained 28% lower in the postlockdown period compared with the prepandemic baseline. In the context of evidence suggesting that alcohol-related mortality increased during the COVID-19 pandemic, alternate strategies to reach vulnerable individuals are needed. Because of high rates of relapse, hospitalization is an important opportunity to engage patients experiencing alcohol use disorder in treatment through referral to substance use treatment programs and medication-assisted therapy. Considering the reduction in alcohol-related hospitalizations during lockdown, other strategies are needed to ensure comprehensive and longitudinal care for this vulnerable population.
1. Commonwealth of Massachussets, Executive Office of Health and Human Services, Department of Public Health. COVID-19 state of emergency. Accessed June 29, 2023. https://www.mass.gov/info-details/covid-19-state-of-emergency
2. Lange SJ, Ritchey MD, Goodman AB, et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions-United States, January-May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):795-800. doi:10.15585/mmwr.mm6925e2
3. Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood). 2020;39(11):2010-2017. doi:10.1377/hlthaff.2020.00980
4. Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021;51(2):201-211. doi:10.1017/S0033291721000015
5. Yazdi K, Fuchs-Leitner I, Rosenleitner J, Gerstgrasser NW. Impact of the COVID-19 pandemic on patients with alcohol use disorder and associated risk factors for relapse. Front Psychiatry. 2020;11:620612. doi:10.3389/fpsyt.2020.620612
6. Ornell F, Moura HF, Scherer JN, Pechansky F, Kessler FHP, von Diemen L. The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Res. 2020;289:113096. doi:10.1016/j.psychres.2020.113096
7. Kim JU, Majid A, Judge R, et al. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. Lancet Gastroenterol Hepatol. 2020;5(10):886-887. doi:10.1016/S2468-1253(20)30251-X
8. Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. doi:10.1001/jamanetworkopen.2020.22942
9. Castaldelli-Maia JM, Segura LE, Martins SS. The concerning increasing trend of alcohol beverage sales in the U.S. during the COVID-19 pandemic. Alcohol. 2021;96:37-42. doi:10.1016/j.alcohol.2021.06.004
10. Anderson P, O’Donnell A, Jané Llopis E, Kaner E. The COVID-19 alcohol paradox: British household purchases during 2020 compared with 2015-2019. PLoS One. 2022;17(1):e0261609. doi:10.1371/journal.pone.0261609
11. Schimmel J, Vargas-Torres C, Genes N, Probst MA, Manini AF. Changes in alcohol-related hospital visits during COVID-19 in New York City. Addiction. 2021;116(12):3525-3530. doi:10.1111/add.15589
12. Sharma RA, Subedi K, Gbadebo BM, Wilson B, Jurkovitz C, Horton T. Alcohol withdrawal rates in hospitalized patients during the COVID-19 pandemic. JAMA Netw Open. 2021;4(3):e210422. doi:10.1001/jamanetworkopen.2021.0422
13. White AM, Castle IP, Powell PA, Hingson RW, Koob, GF. Alcohol-related deaths during the COVID-19 pandemic. JAMA. 2022;327(17):1704-1706. doi:10.1001/jama.2022.4308
14. Dhond R, Acher R, Leatherman S, et al. Rapid implementation of a modular clinical trial informatics solution for COVID-19 research. Inform Med Unlocked. 2021;27:100788. doi:10.1016/j.imu.2021.100788
15. Cohn BA, Cirillo PM, Murphy CC, Krigbaum NY, Wallace AW. SARS-CoV-2 vaccine protection and deaths among US veterans during 2021. Science. 2022;375(6578):331-336. doi:10.1126/science.abm0620
16. Peckova M, Fahrenbruch CE, Cobb LA, Hallstrom AP. Circadian variations in the occurrence of cardiac arrests: initial and repeat episodes. Circulation. 1998;98(1):31-39. doi:10.1161/01.cir.98.1.31
17. Esser MB, Idaikkadar N, Kite-Powell A, Thomas C, Greenlund KJ. Trends in emergency department visits related to acute alcohol consumption before and during the COVID-19 pandemic in the United States, 2018-2020. Drug Alcohol Depend Rep. 2022;3:100049. doi:10.1016/j.dadr.2022.100049
18. The ASAM clinical practice guideline on alcohol withdrawal management. J Addict Med. 2020;14(3S):1-72. doi:10.1097/ADM.0000000000000668
19. Council of State and Territorial Epidemiologists. Developmental indicator: hospitalizations related to alcohol in the United States using ICD-10-CM codes. Accessed June 29, 2023. https://cste.sharefile.com/share/view/s1ee0f8d039d54031bd7ee90462416bc0
20. Kronmal RA. Spurious correlation and the fallacy of the ratio standard revisited. J R Stat Soc Ser A Stat Soc. 1993;156(3):379-392. doi:10.2307/2983064
21. Gullette MM. American eldercide. In: Sugrue TJ, Zaloom C, eds. The Long Year: A 2020 Reader. Columbia University Press; 2022: 237-244. http://www.jstor.org/stable/10.7312/sugr20452.26
22. White AM, Castle IP, Hingson RW, Powell PA. Using death certificates to explore changes in alcohol-related mortality in the United States, 1999 to 2017. Alcohol Clin Exp Res. 2020;44(1):178-187. doi:10.1111/acer.14239
23. National Highway Traffic Safety Administration. Overview of Motor Vehicle Crashes in 2020. US Department of Transportation; 2022. https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/813266
The United States’ initial public health response to the COVID-19 pandemic included containment measures that varied by state but generally required closing or suspending schools, nonessential businesses, and travel (commonly called lockdown).1 During these periods, hospitalizations for serious and common conditions declined.2,3 In Massachusetts, a state of emergency was declared on March 10, 2020, which remained in place until May 18, 2020, when a phased reopening of businesses began.
Although the evidence on the mental health impact of containment periods has been mixed, it has been suggested that these measures could lead to increases in alcohol-related hospitalizations.4 Social isolation and increased psychosocial and financial stressors raise the risk of relapse among patients with substance use disorders.5-7 Marketing and survey data from the US and United Kingdom from the early months of the pandemic suggest that in-home alcohol consumption and sales of alcoholic beverages increased, while consumption of alcohol outside the home decreased.8-10 Other research has shown an increase in the percentage—but not necessarily the absolute number—of emergency department (ED) visits and hospitalizations for alcohol-related diagnoses during periods of containment.11,12 At least 1 study suggests that alcohol-related deaths increased beginning in the lockdown period and persisting into mid-2021.13
Because earlier studies suggest that lockdown periods are associated with increased alcohol consumption and relapse of alcohol use disorder, we hypothesized that the spring 2020 lockdown period in Massachusetts would be associated temporally with an increase in alcohol-related hospitalizations. To evaluate this hypothesis, we examined all hospitalizations in the US Department of Veterans Affairs (VA) Boston Healthcare System (VABHS) before, during, and after this lockdown period. VABHS includes a 160-bed acute care hospital and a 50-bed inpatient psychiatric facility.
Methods
We conducted an interrupted time-series analysis including all inpatient hospitalizations at VABHS from January 1, 2017, to December 31, 2020, to compare the daily number of alcohol-related hospitalizations across 3 exposure groups: prelockdown (the reference group, 1/1/2017-3/9/2020); lockdown (3/10/2020-5/18/2020); and postlockdown (5/19/2020-12/31/2020).
The VA Corporate Data Warehouse at VABHS was queried to identify all hospitalizations on the medical, psychiatry, and neurology services during the study period. Hospitalizations were considered alcohol-related if the International Statistical Classification of Diseases, Tenth Revision (ICD-10) primary diagnosis code (the main reason for hospitalization) was defined as an alcohol-related diagnosis by the VA Centralized Interactive Phenomics Resource (eAppendix 1, available online at doi:10.1278/fp.0404). This database, which has been previously used for COVID-19 research, is a catalog and knowledge-sharing platform of VA electronic health record–based phenotype algorithms, definitions, and metadata that builds on the Million Veteran Program and Cooperative Studies Program.14,15 Hospitalizations under observation status were excluded.
To examine whether alcohol-related hospitalizations could have been categorized as COVID-19 when the conditions were co-occurring, we identified 244 hospitalizations coded with a primary ICD-10 code for COVID-19 during the lockdown and postlockdown periods. At the time of admission, each hospitalization carries an initial (free text) diagnosis, of which 3 had an initial diagnosis related to alcohol use. The population at risk for alcohol-related hospitalizations was estimated as the number of patients actively engaged in care at the VABHS. This was defined as the number of patients enrolled in VA care who have previously received any VA care; patients who are enrolled but have never received VA care were excluded from the population-at-risk denominator. Population-at-risk data were available for each fiscal year (FY) of the study period (9/30-10/1); the following population-at-risk sizes were used: 38,057 for FY 2017, 38,527 for FY 2018, 39,472 for FY 2019, and 37,893 for FY 2020.
The primary outcome was the daily number of alcohol-related hospitalizations in the prelockdown, lockdown, and postlockdown periods. A sensitivity analysis was performed using an alternate definition of the primary outcome using a broader set of alcohol-related ICD-10 codes (eAppendix 2, available online at doi:10.1278/fp.0404).
Statistical Analysis
To visually examine hospitalization trends during the study period, we generated a smoothed time-series plot of the 7-day moving average of the daily number of all-cause hospitalizations and the daily number of alcohol-related hospitalizations from January 1, 2017, to December 31, 2020. We used multivariable regression to model the daily number of alcohol-related hospitalizations over prelockdown (the reference group), lockdown, and postlockdown. In addition to the exposure, we included the following covariates in our model: day of the week, calendar date (to account for secular trends), and harmonic polynomials of the day of the year (to account for seasonal variation).16
We also examined models that included the daily total number of hospitalizations to account for the reduced likelihood of hospital admission for any reason during the pandemic. We used generalized linear models with a Poisson link to generate rate ratios and corresponding 95% CIs for estimates of the daily number of alcohol-related hospitalizations. We estimated the population incidence of alcohol-related hospitalizations per 100,000 patient-months for the exposure periods using the population denominators previously described. All analyses were performed in Stata 16.1.
Results
During the study period, 27,508 hospitalizations were available for analysis. The 7-day moving average of total daily hospitalizations and total daily alcohol-related hospitalizations over time for the period January 1, 2017, to December 31, 2020, are shown in the Figure.
The incidence of alcohol-related hospitalizations in the population dropped from 72 per 100,000 patient-months to 10 per 100,000 patient-months during the lockdown period and increased to 46 per 100,000 patient-months during the postlockdown period (Table).
Our results were not substantially different when we ran a sensitivity analysis that excluded the total daily number of admissions from our model. Compared with the prelockdown period, the rate ratio for the number of alcohol-related hospitalizations during the lockdown period was 0.16 (95% CI, 0.08-0.30), and the rate ratio for the postlockdown period was 0.65 (95% CI, 0.52-0.82). We conducted an additional sensitivity analysis using a broader definition of the primary outcome to include all alcohol-related diagnosis codes; however, the results were unchanged.
Discussion
During the spring 2020 COVID-19 lockdown period in Massachusetts, the daily number of VABHS alcohol-related hospitalizations decreased by nearly 80% compared with the prelockdown period. During the postlockdown period, the daily number of alcohol-related hospitalizations increased but only to 72% of the prelockdown baseline by the end of December 2020. A similar trend was observed for all-cause hospitalizations for the same exposure periods.
These results differ from 2 related studies on the effect of the COVID-19 pandemic on alcohol-related hospitalizations.10,11 In a retrospective study of ED visits to 4 hospitals in New York City, Schimmel and colleagues reported that from March 1 to 31, 2020 (the initial COVID-19 peak), hospital visits for alcohol withdrawal increased while those for alcohol use decreased.10 However, these results are reported as a percentage of total ED visits rather than the total number of visits, which are vulnerable to spurious correlation because of concomitant changes in the total number of ED visits. In their study, the absolute number of alcohol-related ED visits did not increase during the initial 2020 COVID-19 peak, and the number of visits for alcohol withdrawal syndrome declined slightly (195 in 2019 and 180 in 2020). However, the percentage of visits increased from 7% to 10% because of a greater decline in total ED visits. This pattern of decline in the number of alcohol-related ED visits, accompanied by an increase in the percentage of alcohol-related ED visits, has been observed in at least 1 nationwide surveillance study.17 This apparent increase does not reflect an absolute increase in ED visits for alcohol withdrawal syndrome and represents a greater relative decline in visits for other causes during the study period.
Sharma and colleagues reported an increase in the percentage of patients who developed alcohol withdrawal syndrome while hospitalized in Delaware per 1000 hospitalizations during consecutive 2-week periods during the pandemic in 2020 compared with corresponding weeks in 2019.11 The greatest increase occurred during the last 2 weeks of the Delaware stay-at-home order. The Clinical Institute Withdrawal Assessment of Alcohol Scale, revised (CIWA-Ar) score of > 8 was used to define alcohol withdrawal syndrome. The American Society of Addiction Medicine does not recommend using CIWA-Ar to diagnose alcohol withdrawal syndrome because the scale was developed to monitor response to treatment, not to establish a diagnosis.18
Although the true population incidence of alcohol-related hospitalizations is difficult to estimate because the size of the population at risk (ie, the denominator) often is not known, the total number of hospitalizations is not a reliable surrogate.19 Individuals hospitalized for nonalcohol causes are no longer at risk for alcohol-related hospitalization.
In our study, we assume the population at risk during the study period is constant and model changes in the absolute number—rather than percentage—of alcohol-related ED visits. These absolute estimates of alcohol-related hospitalizations better reflect the true burden on the health care system and avoid the confounding effect of declining total ED visits and hospitalizations that could lead to artificially increased percentages and spurious correlation.20 The absolute percentage of alcohol-related hospitalizations also decreased during this period; therefore, our results are not sensitive to this approach.
Several factors could have contributed to the decrease in alcohol-related hospitalizations. Our findings suggest that patient likelihood to seek care and clinician threshold to admit patients for alcohol-related conditions are influenced by external factors, in this case, a public health lockdown. Although our data do not inform why hospitalizations did not return to prelockdown levels, our experience suggests that limited bed capacity and longer length of stay might have contributed. Other hypotheses include a shift to outpatient care, increased use of telehealth (a significant focus early in the pandemic), and avoiding care for less severe alcohol-related complications because of lingering concerns about exposure to COVID-19 in health care settings reported early in the pandemic. Massachusetts experienced a particularly deadly outbreak of COVID-19 in the Soldiers’ Home, a long-term care facility for veterans in Holyoke.21
Evidence suggests that in-home consumption of alcohol increased during lockdowns.8-10 Our results show that during this period hospitalizations for alcohol-related conditions decreased at VABHS, a large urban VA medical system, while alcohol-related deaths increased nationally.13 Although this observation is not evidence of causality, these outcomes could be related.
In the 2 decades before the pandemic, alcohol-related deaths increased by about 2% per year.22 From 2019 to 2020, there was a 25% increase that continued through 2021.13 Death certificate data often are inaccurate, and it is difficult to determine whether COVID-19 had a substantial contributing role to these deaths, particularly during the initial period when testing was limited or unavailable. Nonetheless, deaths due to alcohol-associated liver disease, overdoses involving alcohol, and alcohol-related traffic fatalities increased by > 10%.13,23 These trends, along with a decrease in hospitalization for alcohol-related conditions, suggest missed opportunities for intervention with patients experiencing alcohol use disorder.
Limitations
In this study, hospitalizations under observation status were excluded, which could underestimate the total number of hospitalizations related to alcohol. We reasoned that this effect was likely to be small and not substantially different by year. ICD-10 codes were used to identify alcohol-related hospitalizations as any hospitalization with an included ICD-10 code listed as the primary discharge diagnosis code. This also likely underestimated the total number of alcohol-related hospitalizations. An ICD-10 code for COVID-19 was not in widespread use during our study period, which prohibited controlling explicitly for the volume of admissions due to COVID-19. The prelockdown period only contains data from the preceding 3 years, which might not be long enough for secular trends to become apparent. We assumed the population at risk remained constant when in reality, the net movement of patients into and out of VA care during the pandemic likely was more complex but not readily quantifiable. Nonetheless, the large drop in absolute number of alcohol-related hospitalizations is not likely to be sensitive to this change. In the absence of an objective measure of care-seeking behavior, we used the total daily number of hospitalizations as a surrogate for patient propensity to seek care. The total daily number of hospitalizations also reflects changes in physician admitting behavior over time. This allowed explicit modeling of care-seeking behavior as a covariate but does not capture other important determinants such as hospital capacity.
Conclusions
In this interrupted time-series analysis, the daily number of alcohol-related hospitalizations during the initial COVID-19 pandemic–associated lockdown period at VABHS decreased by 80% and remained 28% lower in the postlockdown period compared with the prepandemic baseline. In the context of evidence suggesting that alcohol-related mortality increased during the COVID-19 pandemic, alternate strategies to reach vulnerable individuals are needed. Because of high rates of relapse, hospitalization is an important opportunity to engage patients experiencing alcohol use disorder in treatment through referral to substance use treatment programs and medication-assisted therapy. Considering the reduction in alcohol-related hospitalizations during lockdown, other strategies are needed to ensure comprehensive and longitudinal care for this vulnerable population.
The United States’ initial public health response to the COVID-19 pandemic included containment measures that varied by state but generally required closing or suspending schools, nonessential businesses, and travel (commonly called lockdown).1 During these periods, hospitalizations for serious and common conditions declined.2,3 In Massachusetts, a state of emergency was declared on March 10, 2020, which remained in place until May 18, 2020, when a phased reopening of businesses began.
Although the evidence on the mental health impact of containment periods has been mixed, it has been suggested that these measures could lead to increases in alcohol-related hospitalizations.4 Social isolation and increased psychosocial and financial stressors raise the risk of relapse among patients with substance use disorders.5-7 Marketing and survey data from the US and United Kingdom from the early months of the pandemic suggest that in-home alcohol consumption and sales of alcoholic beverages increased, while consumption of alcohol outside the home decreased.8-10 Other research has shown an increase in the percentage—but not necessarily the absolute number—of emergency department (ED) visits and hospitalizations for alcohol-related diagnoses during periods of containment.11,12 At least 1 study suggests that alcohol-related deaths increased beginning in the lockdown period and persisting into mid-2021.13
Because earlier studies suggest that lockdown periods are associated with increased alcohol consumption and relapse of alcohol use disorder, we hypothesized that the spring 2020 lockdown period in Massachusetts would be associated temporally with an increase in alcohol-related hospitalizations. To evaluate this hypothesis, we examined all hospitalizations in the US Department of Veterans Affairs (VA) Boston Healthcare System (VABHS) before, during, and after this lockdown period. VABHS includes a 160-bed acute care hospital and a 50-bed inpatient psychiatric facility.
Methods
We conducted an interrupted time-series analysis including all inpatient hospitalizations at VABHS from January 1, 2017, to December 31, 2020, to compare the daily number of alcohol-related hospitalizations across 3 exposure groups: prelockdown (the reference group, 1/1/2017-3/9/2020); lockdown (3/10/2020-5/18/2020); and postlockdown (5/19/2020-12/31/2020).
The VA Corporate Data Warehouse at VABHS was queried to identify all hospitalizations on the medical, psychiatry, and neurology services during the study period. Hospitalizations were considered alcohol-related if the International Statistical Classification of Diseases, Tenth Revision (ICD-10) primary diagnosis code (the main reason for hospitalization) was defined as an alcohol-related diagnosis by the VA Centralized Interactive Phenomics Resource (eAppendix 1, available online at doi:10.1278/fp.0404). This database, which has been previously used for COVID-19 research, is a catalog and knowledge-sharing platform of VA electronic health record–based phenotype algorithms, definitions, and metadata that builds on the Million Veteran Program and Cooperative Studies Program.14,15 Hospitalizations under observation status were excluded.
To examine whether alcohol-related hospitalizations could have been categorized as COVID-19 when the conditions were co-occurring, we identified 244 hospitalizations coded with a primary ICD-10 code for COVID-19 during the lockdown and postlockdown periods. At the time of admission, each hospitalization carries an initial (free text) diagnosis, of which 3 had an initial diagnosis related to alcohol use. The population at risk for alcohol-related hospitalizations was estimated as the number of patients actively engaged in care at the VABHS. This was defined as the number of patients enrolled in VA care who have previously received any VA care; patients who are enrolled but have never received VA care were excluded from the population-at-risk denominator. Population-at-risk data were available for each fiscal year (FY) of the study period (9/30-10/1); the following population-at-risk sizes were used: 38,057 for FY 2017, 38,527 for FY 2018, 39,472 for FY 2019, and 37,893 for FY 2020.
The primary outcome was the daily number of alcohol-related hospitalizations in the prelockdown, lockdown, and postlockdown periods. A sensitivity analysis was performed using an alternate definition of the primary outcome using a broader set of alcohol-related ICD-10 codes (eAppendix 2, available online at doi:10.1278/fp.0404).
Statistical Analysis
To visually examine hospitalization trends during the study period, we generated a smoothed time-series plot of the 7-day moving average of the daily number of all-cause hospitalizations and the daily number of alcohol-related hospitalizations from January 1, 2017, to December 31, 2020. We used multivariable regression to model the daily number of alcohol-related hospitalizations over prelockdown (the reference group), lockdown, and postlockdown. In addition to the exposure, we included the following covariates in our model: day of the week, calendar date (to account for secular trends), and harmonic polynomials of the day of the year (to account for seasonal variation).16
We also examined models that included the daily total number of hospitalizations to account for the reduced likelihood of hospital admission for any reason during the pandemic. We used generalized linear models with a Poisson link to generate rate ratios and corresponding 95% CIs for estimates of the daily number of alcohol-related hospitalizations. We estimated the population incidence of alcohol-related hospitalizations per 100,000 patient-months for the exposure periods using the population denominators previously described. All analyses were performed in Stata 16.1.
Results
During the study period, 27,508 hospitalizations were available for analysis. The 7-day moving average of total daily hospitalizations and total daily alcohol-related hospitalizations over time for the period January 1, 2017, to December 31, 2020, are shown in the Figure.
The incidence of alcohol-related hospitalizations in the population dropped from 72 per 100,000 patient-months to 10 per 100,000 patient-months during the lockdown period and increased to 46 per 100,000 patient-months during the postlockdown period (Table).
Our results were not substantially different when we ran a sensitivity analysis that excluded the total daily number of admissions from our model. Compared with the prelockdown period, the rate ratio for the number of alcohol-related hospitalizations during the lockdown period was 0.16 (95% CI, 0.08-0.30), and the rate ratio for the postlockdown period was 0.65 (95% CI, 0.52-0.82). We conducted an additional sensitivity analysis using a broader definition of the primary outcome to include all alcohol-related diagnosis codes; however, the results were unchanged.
Discussion
During the spring 2020 COVID-19 lockdown period in Massachusetts, the daily number of VABHS alcohol-related hospitalizations decreased by nearly 80% compared with the prelockdown period. During the postlockdown period, the daily number of alcohol-related hospitalizations increased but only to 72% of the prelockdown baseline by the end of December 2020. A similar trend was observed for all-cause hospitalizations for the same exposure periods.
These results differ from 2 related studies on the effect of the COVID-19 pandemic on alcohol-related hospitalizations.10,11 In a retrospective study of ED visits to 4 hospitals in New York City, Schimmel and colleagues reported that from March 1 to 31, 2020 (the initial COVID-19 peak), hospital visits for alcohol withdrawal increased while those for alcohol use decreased.10 However, these results are reported as a percentage of total ED visits rather than the total number of visits, which are vulnerable to spurious correlation because of concomitant changes in the total number of ED visits. In their study, the absolute number of alcohol-related ED visits did not increase during the initial 2020 COVID-19 peak, and the number of visits for alcohol withdrawal syndrome declined slightly (195 in 2019 and 180 in 2020). However, the percentage of visits increased from 7% to 10% because of a greater decline in total ED visits. This pattern of decline in the number of alcohol-related ED visits, accompanied by an increase in the percentage of alcohol-related ED visits, has been observed in at least 1 nationwide surveillance study.17 This apparent increase does not reflect an absolute increase in ED visits for alcohol withdrawal syndrome and represents a greater relative decline in visits for other causes during the study period.
Sharma and colleagues reported an increase in the percentage of patients who developed alcohol withdrawal syndrome while hospitalized in Delaware per 1000 hospitalizations during consecutive 2-week periods during the pandemic in 2020 compared with corresponding weeks in 2019.11 The greatest increase occurred during the last 2 weeks of the Delaware stay-at-home order. The Clinical Institute Withdrawal Assessment of Alcohol Scale, revised (CIWA-Ar) score of > 8 was used to define alcohol withdrawal syndrome. The American Society of Addiction Medicine does not recommend using CIWA-Ar to diagnose alcohol withdrawal syndrome because the scale was developed to monitor response to treatment, not to establish a diagnosis.18
Although the true population incidence of alcohol-related hospitalizations is difficult to estimate because the size of the population at risk (ie, the denominator) often is not known, the total number of hospitalizations is not a reliable surrogate.19 Individuals hospitalized for nonalcohol causes are no longer at risk for alcohol-related hospitalization.
In our study, we assume the population at risk during the study period is constant and model changes in the absolute number—rather than percentage—of alcohol-related ED visits. These absolute estimates of alcohol-related hospitalizations better reflect the true burden on the health care system and avoid the confounding effect of declining total ED visits and hospitalizations that could lead to artificially increased percentages and spurious correlation.20 The absolute percentage of alcohol-related hospitalizations also decreased during this period; therefore, our results are not sensitive to this approach.
Several factors could have contributed to the decrease in alcohol-related hospitalizations. Our findings suggest that patient likelihood to seek care and clinician threshold to admit patients for alcohol-related conditions are influenced by external factors, in this case, a public health lockdown. Although our data do not inform why hospitalizations did not return to prelockdown levels, our experience suggests that limited bed capacity and longer length of stay might have contributed. Other hypotheses include a shift to outpatient care, increased use of telehealth (a significant focus early in the pandemic), and avoiding care for less severe alcohol-related complications because of lingering concerns about exposure to COVID-19 in health care settings reported early in the pandemic. Massachusetts experienced a particularly deadly outbreak of COVID-19 in the Soldiers’ Home, a long-term care facility for veterans in Holyoke.21
Evidence suggests that in-home consumption of alcohol increased during lockdowns.8-10 Our results show that during this period hospitalizations for alcohol-related conditions decreased at VABHS, a large urban VA medical system, while alcohol-related deaths increased nationally.13 Although this observation is not evidence of causality, these outcomes could be related.
In the 2 decades before the pandemic, alcohol-related deaths increased by about 2% per year.22 From 2019 to 2020, there was a 25% increase that continued through 2021.13 Death certificate data often are inaccurate, and it is difficult to determine whether COVID-19 had a substantial contributing role to these deaths, particularly during the initial period when testing was limited or unavailable. Nonetheless, deaths due to alcohol-associated liver disease, overdoses involving alcohol, and alcohol-related traffic fatalities increased by > 10%.13,23 These trends, along with a decrease in hospitalization for alcohol-related conditions, suggest missed opportunities for intervention with patients experiencing alcohol use disorder.
Limitations
In this study, hospitalizations under observation status were excluded, which could underestimate the total number of hospitalizations related to alcohol. We reasoned that this effect was likely to be small and not substantially different by year. ICD-10 codes were used to identify alcohol-related hospitalizations as any hospitalization with an included ICD-10 code listed as the primary discharge diagnosis code. This also likely underestimated the total number of alcohol-related hospitalizations. An ICD-10 code for COVID-19 was not in widespread use during our study period, which prohibited controlling explicitly for the volume of admissions due to COVID-19. The prelockdown period only contains data from the preceding 3 years, which might not be long enough for secular trends to become apparent. We assumed the population at risk remained constant when in reality, the net movement of patients into and out of VA care during the pandemic likely was more complex but not readily quantifiable. Nonetheless, the large drop in absolute number of alcohol-related hospitalizations is not likely to be sensitive to this change. In the absence of an objective measure of care-seeking behavior, we used the total daily number of hospitalizations as a surrogate for patient propensity to seek care. The total daily number of hospitalizations also reflects changes in physician admitting behavior over time. This allowed explicit modeling of care-seeking behavior as a covariate but does not capture other important determinants such as hospital capacity.
Conclusions
In this interrupted time-series analysis, the daily number of alcohol-related hospitalizations during the initial COVID-19 pandemic–associated lockdown period at VABHS decreased by 80% and remained 28% lower in the postlockdown period compared with the prepandemic baseline. In the context of evidence suggesting that alcohol-related mortality increased during the COVID-19 pandemic, alternate strategies to reach vulnerable individuals are needed. Because of high rates of relapse, hospitalization is an important opportunity to engage patients experiencing alcohol use disorder in treatment through referral to substance use treatment programs and medication-assisted therapy. Considering the reduction in alcohol-related hospitalizations during lockdown, other strategies are needed to ensure comprehensive and longitudinal care for this vulnerable population.
1. Commonwealth of Massachussets, Executive Office of Health and Human Services, Department of Public Health. COVID-19 state of emergency. Accessed June 29, 2023. https://www.mass.gov/info-details/covid-19-state-of-emergency
2. Lange SJ, Ritchey MD, Goodman AB, et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions-United States, January-May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):795-800. doi:10.15585/mmwr.mm6925e2
3. Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood). 2020;39(11):2010-2017. doi:10.1377/hlthaff.2020.00980
4. Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021;51(2):201-211. doi:10.1017/S0033291721000015
5. Yazdi K, Fuchs-Leitner I, Rosenleitner J, Gerstgrasser NW. Impact of the COVID-19 pandemic on patients with alcohol use disorder and associated risk factors for relapse. Front Psychiatry. 2020;11:620612. doi:10.3389/fpsyt.2020.620612
6. Ornell F, Moura HF, Scherer JN, Pechansky F, Kessler FHP, von Diemen L. The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Res. 2020;289:113096. doi:10.1016/j.psychres.2020.113096
7. Kim JU, Majid A, Judge R, et al. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. Lancet Gastroenterol Hepatol. 2020;5(10):886-887. doi:10.1016/S2468-1253(20)30251-X
8. Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. doi:10.1001/jamanetworkopen.2020.22942
9. Castaldelli-Maia JM, Segura LE, Martins SS. The concerning increasing trend of alcohol beverage sales in the U.S. during the COVID-19 pandemic. Alcohol. 2021;96:37-42. doi:10.1016/j.alcohol.2021.06.004
10. Anderson P, O’Donnell A, Jané Llopis E, Kaner E. The COVID-19 alcohol paradox: British household purchases during 2020 compared with 2015-2019. PLoS One. 2022;17(1):e0261609. doi:10.1371/journal.pone.0261609
11. Schimmel J, Vargas-Torres C, Genes N, Probst MA, Manini AF. Changes in alcohol-related hospital visits during COVID-19 in New York City. Addiction. 2021;116(12):3525-3530. doi:10.1111/add.15589
12. Sharma RA, Subedi K, Gbadebo BM, Wilson B, Jurkovitz C, Horton T. Alcohol withdrawal rates in hospitalized patients during the COVID-19 pandemic. JAMA Netw Open. 2021;4(3):e210422. doi:10.1001/jamanetworkopen.2021.0422
13. White AM, Castle IP, Powell PA, Hingson RW, Koob, GF. Alcohol-related deaths during the COVID-19 pandemic. JAMA. 2022;327(17):1704-1706. doi:10.1001/jama.2022.4308
14. Dhond R, Acher R, Leatherman S, et al. Rapid implementation of a modular clinical trial informatics solution for COVID-19 research. Inform Med Unlocked. 2021;27:100788. doi:10.1016/j.imu.2021.100788
15. Cohn BA, Cirillo PM, Murphy CC, Krigbaum NY, Wallace AW. SARS-CoV-2 vaccine protection and deaths among US veterans during 2021. Science. 2022;375(6578):331-336. doi:10.1126/science.abm0620
16. Peckova M, Fahrenbruch CE, Cobb LA, Hallstrom AP. Circadian variations in the occurrence of cardiac arrests: initial and repeat episodes. Circulation. 1998;98(1):31-39. doi:10.1161/01.cir.98.1.31
17. Esser MB, Idaikkadar N, Kite-Powell A, Thomas C, Greenlund KJ. Trends in emergency department visits related to acute alcohol consumption before and during the COVID-19 pandemic in the United States, 2018-2020. Drug Alcohol Depend Rep. 2022;3:100049. doi:10.1016/j.dadr.2022.100049
18. The ASAM clinical practice guideline on alcohol withdrawal management. J Addict Med. 2020;14(3S):1-72. doi:10.1097/ADM.0000000000000668
19. Council of State and Territorial Epidemiologists. Developmental indicator: hospitalizations related to alcohol in the United States using ICD-10-CM codes. Accessed June 29, 2023. https://cste.sharefile.com/share/view/s1ee0f8d039d54031bd7ee90462416bc0
20. Kronmal RA. Spurious correlation and the fallacy of the ratio standard revisited. J R Stat Soc Ser A Stat Soc. 1993;156(3):379-392. doi:10.2307/2983064
21. Gullette MM. American eldercide. In: Sugrue TJ, Zaloom C, eds. The Long Year: A 2020 Reader. Columbia University Press; 2022: 237-244. http://www.jstor.org/stable/10.7312/sugr20452.26
22. White AM, Castle IP, Hingson RW, Powell PA. Using death certificates to explore changes in alcohol-related mortality in the United States, 1999 to 2017. Alcohol Clin Exp Res. 2020;44(1):178-187. doi:10.1111/acer.14239
23. National Highway Traffic Safety Administration. Overview of Motor Vehicle Crashes in 2020. US Department of Transportation; 2022. https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/813266
1. Commonwealth of Massachussets, Executive Office of Health and Human Services, Department of Public Health. COVID-19 state of emergency. Accessed June 29, 2023. https://www.mass.gov/info-details/covid-19-state-of-emergency
2. Lange SJ, Ritchey MD, Goodman AB, et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions-United States, January-May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):795-800. doi:10.15585/mmwr.mm6925e2
3. Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood). 2020;39(11):2010-2017. doi:10.1377/hlthaff.2020.00980
4. Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021;51(2):201-211. doi:10.1017/S0033291721000015
5. Yazdi K, Fuchs-Leitner I, Rosenleitner J, Gerstgrasser NW. Impact of the COVID-19 pandemic on patients with alcohol use disorder and associated risk factors for relapse. Front Psychiatry. 2020;11:620612. doi:10.3389/fpsyt.2020.620612
6. Ornell F, Moura HF, Scherer JN, Pechansky F, Kessler FHP, von Diemen L. The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Res. 2020;289:113096. doi:10.1016/j.psychres.2020.113096
7. Kim JU, Majid A, Judge R, et al. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. Lancet Gastroenterol Hepatol. 2020;5(10):886-887. doi:10.1016/S2468-1253(20)30251-X
8. Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. doi:10.1001/jamanetworkopen.2020.22942
9. Castaldelli-Maia JM, Segura LE, Martins SS. The concerning increasing trend of alcohol beverage sales in the U.S. during the COVID-19 pandemic. Alcohol. 2021;96:37-42. doi:10.1016/j.alcohol.2021.06.004
10. Anderson P, O’Donnell A, Jané Llopis E, Kaner E. The COVID-19 alcohol paradox: British household purchases during 2020 compared with 2015-2019. PLoS One. 2022;17(1):e0261609. doi:10.1371/journal.pone.0261609
11. Schimmel J, Vargas-Torres C, Genes N, Probst MA, Manini AF. Changes in alcohol-related hospital visits during COVID-19 in New York City. Addiction. 2021;116(12):3525-3530. doi:10.1111/add.15589
12. Sharma RA, Subedi K, Gbadebo BM, Wilson B, Jurkovitz C, Horton T. Alcohol withdrawal rates in hospitalized patients during the COVID-19 pandemic. JAMA Netw Open. 2021;4(3):e210422. doi:10.1001/jamanetworkopen.2021.0422
13. White AM, Castle IP, Powell PA, Hingson RW, Koob, GF. Alcohol-related deaths during the COVID-19 pandemic. JAMA. 2022;327(17):1704-1706. doi:10.1001/jama.2022.4308
14. Dhond R, Acher R, Leatherman S, et al. Rapid implementation of a modular clinical trial informatics solution for COVID-19 research. Inform Med Unlocked. 2021;27:100788. doi:10.1016/j.imu.2021.100788
15. Cohn BA, Cirillo PM, Murphy CC, Krigbaum NY, Wallace AW. SARS-CoV-2 vaccine protection and deaths among US veterans during 2021. Science. 2022;375(6578):331-336. doi:10.1126/science.abm0620
16. Peckova M, Fahrenbruch CE, Cobb LA, Hallstrom AP. Circadian variations in the occurrence of cardiac arrests: initial and repeat episodes. Circulation. 1998;98(1):31-39. doi:10.1161/01.cir.98.1.31
17. Esser MB, Idaikkadar N, Kite-Powell A, Thomas C, Greenlund KJ. Trends in emergency department visits related to acute alcohol consumption before and during the COVID-19 pandemic in the United States, 2018-2020. Drug Alcohol Depend Rep. 2022;3:100049. doi:10.1016/j.dadr.2022.100049
18. The ASAM clinical practice guideline on alcohol withdrawal management. J Addict Med. 2020;14(3S):1-72. doi:10.1097/ADM.0000000000000668
19. Council of State and Territorial Epidemiologists. Developmental indicator: hospitalizations related to alcohol in the United States using ICD-10-CM codes. Accessed June 29, 2023. https://cste.sharefile.com/share/view/s1ee0f8d039d54031bd7ee90462416bc0
20. Kronmal RA. Spurious correlation and the fallacy of the ratio standard revisited. J R Stat Soc Ser A Stat Soc. 1993;156(3):379-392. doi:10.2307/2983064
21. Gullette MM. American eldercide. In: Sugrue TJ, Zaloom C, eds. The Long Year: A 2020 Reader. Columbia University Press; 2022: 237-244. http://www.jstor.org/stable/10.7312/sugr20452.26
22. White AM, Castle IP, Hingson RW, Powell PA. Using death certificates to explore changes in alcohol-related mortality in the United States, 1999 to 2017. Alcohol Clin Exp Res. 2020;44(1):178-187. doi:10.1111/acer.14239
23. National Highway Traffic Safety Administration. Overview of Motor Vehicle Crashes in 2020. US Department of Transportation; 2022. https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/813266
The Burden of Guardianship: A Matched Cohort Study
A central tenet of modern medicine is that patients must provide fully informed consent to receive or refuse medical care offered by their clinical teams.1–4 If a patient is unable to make and communicate a choice or clearly indicate an understanding of the information presented, then he or she is considered to lack the capacity to make medical decisions and the medical team must seek consent from the patient’s surrogate decision-maker.2-7 Every U.S. state recognizes a patient’s healthcare proxy (HCP) and a court-appointed guardian as a legally recognized surrogate.8,9 Most of the states also have statutes or regulations establishing a hierarchy of legally recognized surrogate decision-makers in the absence of a HCP or a court-appointed guardian, such as spouses, adult children, parents, siblings, and grandparents.8,10 In states that do not have such a statute, hospitals develop their own institutional policies for surrogate decision-making.
However, there are important limitations on the authority of these surrogate decision-makers.10 For instance, patients may not have a family member or a friend to serve as a surrogate decision-maker, often family members cannot override a patient’s objection, even when that patient lacks decision-making capacity, and certain decisions require a guardian or a HCP.8-10 In these circumstances, the hospital must petition a court to appoint a guardian as a legally recognized surrogate decision-maker. This can be an involved family member, if one exists, or an independent, typically volunteer, guardian.11 The process of guardian appointment is complex7,11 and can range from a few days to more than a month, largely dependent on court dates and finding a volunteer guardian. Much of the process occurs during the patient’s hospital stay. This prolongation of hospitalization would be expected to increase health care costs and iatrogenic complications,12–14 but data quantifying these for patients requiring guardianship are lacking. The goal of this study was to describe the characteristics of patients who undergo the process of guardianship and measure the associated burdens. These burdens include the financial costs to the medical system, the prolonged length of stay beyond medical necessity, and the costs to the patient in the form of hospital-acquired complications. Investigating the burden of guardianship is an important first step in uncovering opportunities to improve the process. We hypothesized that patients requiring guardianship would have lengths of stay and healthcare costs that were at least as large as those for patients whose conditions required similar durations of hospitalization prior to medical clearance, in part due to iatrogenic complications that would accrue while awaiting guardian appointment.
METHODS
Setting
We conducted a retrospective matched cohort study of adult inpatients at Beth Israel Deaconess Medical Center (BIDMC), a 651-bed academic, tertiary care facility in Boston, MA. The study was approved by the BIDMC Institutional Review Board as a nonhuman subject research consistent with hospital operations.
Population
For this matched cohort study, we identified case patients as those hospitalized for any reason for whom guardianship proceedings were initiated and obtained; only the first hospitalization during which the guardianship was pursued was used. Cases were identified by obtaining the data of all patients for whom the BIDMC general counsel completed the process of guardianship between October 2014 and September 2015. At BIDMC, all the guardianship proceedings are referred to the general counsel.
To determine the postclearance experience for referred patients compared with that for other patients with similar lengths of stay up to those of the referred patients’ point of clearance, we identified up to three matched controls for each case (Supplemental Figure 1). Medical clearance was defined as the date when the patient was medically stable to be discharged from the hospital, and it was determined in an iterative manner. We identified controls as hospitalized patients admitted for any cause and matched to the cases requiring guardianship on discharging service and length of stay prior to clearance. Specifically, we identified patients on the same service as the case whose length of stay was at least as long as the length of stay of the case patient until medical clearance, as defined below. We then determined the total and the excess length of stay, defined as the duration beyond clearance for each case referred for guardianship; for controls, the ‘excess’ length of stay was the number of hospitalized days beyond the corresponding time that a matched case had been provided clearance. To account for seasonal influences and the training level of house officers, we selected the three controls whose discharge date was closest (before or after) to the discharge date of their matched case.
From legal team files, we identified 61 patients hospitalized at BIDMC for whom new guardianship was pursued to completion. Of these 61 patients, 10 could not be matched to an appropriate control and were included in descriptive analyses but not in comparisons with controls.
Covariates and Outcomes
We collected the details regarding age, gender, primary language, highest level of education, marital status, insurance status, race, date of admission, date of discharge, discharge disposition, principal diagnosis, case mix index (CMI), and discharging service from our administrative and billing data. Outcomes of interest included length of stay and total hospital charges that were collected from the same databases. We used hospital charges, rather than payments, to ensure uniformity across payers.
Chart Review
Unique to cases, a team of two medical residents (JP, RP) and a hospitalist (DR) determined the date of medical clearance and hospital-associated complications by a chart review. The date of medical clearance was then used to calculate excess length of stay, ie, the duration of stay beyond the date of medical clearance, by subtracting the time to medical clearance from the total inpatient length of stay.
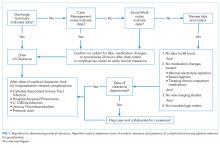
We developed a novel algorithm to determine the date of medical clearance consistently (Figure 1). We first determined whether the discharge summary indicated a clear date of medical readiness for discharge. If the discharge summary was unclear, then a case management or a social work note was used. The date of medical clearance determined by the case management or the social work note was then confirmed with clinical data. The date was confirmed if there were no significant laboratory orders and major medication changes or procedures for 24 h from the date identified. If notes were also inconclusive, then the medical clearance was determined by a review of provider order entry. Medical readiness for discharge was then defined as the first day when there were no laboratory orders for 48 h and no significant medication changes, imaging studies, or microbiologic orders.
Hospital-acquired complications were determined to be related to the guardianship process if they occurred after the date of medical stability but prior to discharge. We did not investigate hospital-acquired complications among controls. Hospital-acquired complications were defined as follows:
- Catheter-associated urinary tract infection (CAUTI): active Foley catheter order and positive urine culture that resulted in antibiotic administration.
- Hospital-acquired pneumonia (HAP): chest X-ray or computed tomography (CT) scan showing a consolidation that resulted in antibiotic administration.
- Venous thromboembolism (VTE): positive venous ultrasound or CT angiography of the chest for deep venous thrombosis (DVT) or pulmonary embolism (PE).
- Decubitus ulcer: new wound care consultation for sacral decubitus ulceration.
- Clostridium difficile (C. diff) infection: positive stool polymerase chain reaction that resulted in antibiotic administration.
The algorithm for identifying the date of clearance and the presence of complications was piloted independently by three investigators (RP, JP, DR) using a single chart review and was redesigned until a consensus was obtained. The same three investigators then independently reviewed three additional charts, including all notes, laboratory results, imaging results, and orders, with complete agreement for both date of clearance and presence of complications. Two investigators (RP, JP) then individually reviewed the remaining 57 charts. Of these, 10 were selected a priori for review by both investigators for interrater reliability, with a mean difference of 0.5 days in the estimated time to clearance and complete concordance in complications. In addition, a third investigator (DR) independently reread 5 of the 57 reviewed charts, with complete concordance in both time to clearance and presence of complications with the original readings.
Statistical Analysis
SAS 9.3 was used for all analyses (SAS Institute Inc., Cary, NC, USA).
We first examined the demographic and clinical characteristics of all 61 patients who underwent guardianship proceedings. Second, we described the primary outcomes of interest–length of stay, costs, and likelihood of complications–in this series of patients with associated 95% confidence intervals.
Third, we examined the associations between guardianship and length of stay and healthcare costs using generalized estimating equations with clustering by matched set and compound symmetry. For length of stay, we specifically assessed excess length of stay (the matching variable) to avoid immortal time bias; we also examined the total length of stay. For all regression analyses, we adjusted for the following covariates: age, gender, education, marital status, race/ethnicity, CMI, insurance status, discharging service, and principal diagnosis. To maximize normality of residuals, costs were log-transformed; length of stay beyond clearance was log-transformed after addition of 1. For both outcomes, we back-transformed the regression coefficients and presented percent change between case and control patients. All reported tests are two-sided.
RESULTS
A total of 61 guardianship cases and 118 controls were included in the analysis.
General Characteristics
The characteristics of all cases prior to matching are included in Table 1. The department of internal medicine discharged the largest proportion of cases, followed by neurosurgery and neurology departments. More than 65% of cases were insured by Medicare or Medicaid. Three-quarters of cases were discharged from the hospital to another medical facility, with about half discharged to a skilled nursing facility (SNF) or a rehabilitation center and one-quarter to a long-term acute care hospital (LTACH).
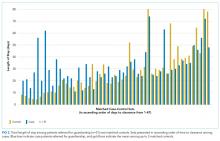
The median length of stay for patients requiring guardianship was 28 (range, 23-36) days, and the median total charges were $171,083 ($106,897-$245,281), with a total cost approximating $10.9 million for these patients. Regarding hospital-acquired complications, 10 (16%; 95% confidence interval, 8%–28%) unique cases suffered from a complication, with HAP being the most frequently (n = 5) occurring complication.
Comparison with Matched Controls
No statistically significant differences were observed between cases and controls in terms of age, primary language, highest level of education, ethnicity, insurance status, or discharging service as shown in Table 2; discharging service was a matched variable and comparable by design. However, cases tended to be less likely to be married and had a higher CMI.
When compared with control patients in terms of similar services who stayed for at least as long as their duration to clearance, the cases had significantly longer lengths of stay compared to those of controls (29 total days compared to 18 days, P < .001; Figure 2). In addition, cases incurred significantly higher median total charges ($168,666) compared to those of controls ($104,190; P = .02).
After accounting for potential confounders, including age, gender, language, education, marital status, discharging service, ethnicity, insurance status, CMI, and principal diagnosis, guardianship was associated with 58% higher excess length of stay (P = .04, 95% CI [2%-145%]). Furthermore, guardianship was associated with 23% higher total charges (P = .02, 95% CI [4%-46%]) and 37% longer total length of stay (P = .002, 95% CI [12%-67%]).
DISCUSSION
To our knowledge, this is among the first studies to investigate healthcare costs and harm to the patient in the form of hospital-associated complications as a result of guardianship proceedings. Other studies15,16 have also demonstrated excessive length of stay attributed to nonclinical factors such as guardianship, though they did not quantify the excess stay or compare guardianship cases with a matched control. One study17 demonstrated total charges of $150,000 per patient requiring guardianship, which are similar to our results. However, Chen et al. also observed an average of 27.8 medically unnecessary days, which are 16 more days than those in our study sample. This may reflect the difference in how excess days were determined, namely, statistical process control analysis in the previous study compared with a manual chart review in our study. To our knowledge, no other study has compared guardianship cases with matched controls to compare their experiences to patients with similarly prolonged stays prior to clearance.
After matching by service and the length of stay until medical clearance in each guardianship case, the subsequent length of stay was higher among cases than among controls, even after adjustment for differences in CMI and diagnosis. This suggests that the process of obtaining guardianship results in a particularly prolonged length of stay, which is presumably attributable to factors other than medical complexity or ongoing illness.
It is probable that at least two interrelated mechanisms are responsible for the particularly high costs and the long stay of patients who require guardianship. First, the process of obtaining guardianship is itself protracted in several cases, necessitating long-term admissions well beyond the point of medical stability. Second, our results suggest that longer hospital stays are apt to grow further in a feed-forward cycle due to hospital-acquired complications that develop after the date of medical clearance. Indeed, in our series, 16% of patients sustained a complication that is readily attributable to hospital care after their date of clearance, and these types of complications are likely to lengthen the stay even further.
We compared cases referred for guardianship to control patients on the same services, at similar time points, whose length of stay was at least as long as the point of medical clearance as their corresponding case patient. Because cases were hospitalized with active medical needs to at least the point of clearance, we anticipated that costs might well be lower among cases, who had no medical necessity for hospitalization at the point of clearance, compared with controls who remained hospitalized presumably for active medical needs. Counter to this hypothesis, and accounting for potentially confounding variables, undergoing a guardianship proceeding was associated with nearly 25% higher costs of patient care. This may ultimately represent a substantial burden on the healthcare system. For example, in just 1 year in our hospital, the total hospital charges reached almost $11 million for the 61 patients who underwent guardianship proceedings. Considering that 65% of the patients requiring guardianship had Medicaid or Medicare coverage, there are significant financial implications for the hospital systems and to the public.
Limitations of our study relate to its retrospective nature at a single center. Investigating guardianship cases at a single center and with a small sample size of 61 patients limits generalizability. Nevertheless, we still had enough power to detect significant differences compared with matched controls, and this study remains the largest investigation into the cost associated with guardianship to date and the only study comparing guardianship cases with matched controls. Furthermore, we did not complete chart reviews of controls, which limits direct comparisons of complications and precluded our matching on variables that required detailed review.
The retrospective design may include confounders unaccounted for in our statistical design, though we attempted to match cases with controls to account for some of these potential differences and included a broad set of covariates that included measures of comorbidity and diagnosis. To this point, we included only CMI and principal diagnosis as the measures of severity, and adjustment for CMI, which includes features of the index hospitalization itself, may represent overadjustment. However, this type of overadjustment would tend to bias toward the null hypothesis.
Investigators only completed chart reviews for cases, which limits our ability to contrast the rate of hospital-associated complications for cases with that of controls. However, the rates of CAUTI and HAP complications among our cases were notably higher than national inpatient estimates, ie, 5% and 8% compared to 0.2%18 and 0.5%-1%,19 respectively. Furthermore, we demonstrated higher total costs and total lengths of stay among guardianship patients, analyses for which the attributed date of clearance for controls was not required, and the rate of complications among the case patients was sizable despite their being formally medically cleared. In other words, regardless of whether a complication rate of 16% is “typical” for inpatients hospitalized for these durations, this suggests that persistent hospitalization after clearance does not carry a benign prognosis.
In addition, to estimate healthcare costs, we relied on total hospital charges, which are readily available and reflect, at least in part, payer costs but do not reflect true costs to the medical center. Nonetheless, charges approximately reflect costs–with some variation across cost centers–and hence provide a useful metric for comparing cases and controls. To provide context, for academic medical centers such as ours, costs are typically about half of charges.
Finally, each state has different statutes for surrogate decision-making. The results of this study reflect the Massachusetts’ experience, with no public guardianship program or hierarchy statute. That being said, while this presumably causes the need for more guardianships in Massachusetts, the mechanisms for guardianship are broadly similar nationwide and are likely to result in excessive length of stay and cost similar to those in our population, as demonstrated in studies from other states.7,15–17
Implications
At a time where medical systems are searching for opportunities to reduce the length of stay, prevent unnecessary hospitalization, and improve the quality of care, reevaluating the guardianship process is ripe with opportunity. In this single academic center, the process of guardianship was associated with 58% excess length of stay and 23% higher total hospital charges. Furthermore, one in six patients requiring guardianship suffered from hospital-associated complications.
This matched cohort study adds quantitative data demonstrating substantial burdens to the healthcare system as a result of the guardianship process and can be used as an impetus for hospital administration and legal systems to expedite the process. Potential improvements include increasing HCP form completions (which would eliminate the need to pursue guardianship for most of such patients), identifying patients who lack a legally recognized surrogate decision-maker earlier in their hospital stay (ideally upon admission), and providing resources to assist clinical teams in the completion of affidavits necessary to support the appointment of a guardian, so that paperwork can be filed with courts sooner. Further research that provides more generalizable prospective data could potentially improve the guardianship process and reduce its burden on hospitals and patients even further.
Acknowledgments
The authors express their tremendous thanks to Gail Piatkowski for her invaluable assistance in collecting administrative and billing data.
Disclosures
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article
1. O’Neill O. Autonomy and Trust in Bioethics. Cambridge: Cambridge University Press; 2002. PubMed
2. Beauchamp T, Childress J. Principles of Biomedical Ethics. 7th ed. New York: Oxford University Press; 2013.
3. McMurray RJ, Clarke OW, Barrasso JA, et al. Decisions near the end of life. J Am Med Assoc. 1992;267(16):2229-2233.
4. American Medical Association. AMA Principles of Medical Ethics: Chapter 2 - Opinions on Consent, Communication and Decision Making.; 2016.
5. Arnold RM, Kellum J. Moral justifications for surrogate decision making in the intensive care unit: Implications and limitations. Crit Care Med. 2003;31(Supplement):S347-S353. PubMed
6. Karp N, Wood E. Incapacitated and Alone: Healthcare Decision Making for Unbefriended Older People. Am Bar Assoc Hum Rights. 2003;31(2).
7. Bandy RJ, Helft PR, Bandy RW, Torke AM. Medical decision-making during the guardianship process for incapacitated, hospitalized adults: a descriptive cohort study. J Gen Intern Med. 2010;25(10):1003-1008. PubMed
8. Wynn S. Decisions by surrogates: an overview of surrogate consent laws in the United States. Bifocal. 2014;36(1):10-14.
9. Massachusetts General Laws. Chapter 201D: Health Care Proxies. https://malegislature.gov/Laws/GeneralLaws/PartII/TitleII/Chapter201D. Published 2017. Accessed March 31, 2017.
10. American Bar Association Commision on Law and Aging. Default Surrogate Consent Statutes. Am Bar Assoc. 2016:1-17.
11. Massachusetts General Laws. Chapter 190B: Massachusetts Probate Code. https://malegislature.gov/Laws/GeneralLaws/PartII/TitleII/Chapter190B. Published 2017. Accessed March 31, 2017.
12. Rosman M, Rachminov O, Segal O, Segal G. Prolonged patients’ in-hospital waiting period after discharge eligibility is associated with increased risk of infection, morbidity and mortality: a retrospective cohort analysis. BMC Health Serv Res. 2015;15:246. PubMed
13. Majeed MU, Williams DT, Pollock R, et al. Delay in discharge and its impact on unnecessary hospital bed occupancy. 2012. PubMed
14. Nobili A, Licata G, Salerno F, et al. Polypharmacy, length of hospital stay, and in-hospital mortality among elderly patients in internal medicine wards. The REPOSI study. Eur J Clin Pharmacol. 2011;67(5):507-519. PubMed
15. Chen JJ, Finn CT, Homa K, St Onge KP, Caller TA. Discharge delays for patients requiring in-hospital guardianship: A Cohort Analysis. J Healthc Qual. 2016;38(4):235-242. PubMed
16. Chen JJ, Kwon A, Stevens Y, Finn CT. Barriers beyond clinical control affecting timely hospital discharge for a patient requiring guardianship. Psychosomatics. 2015;56(2):206-209. PubMed
17. Chen JJ, Blanchard MA, Finn CT, et al. A clinical pathway for guardianship at dartmouth-hitchcock medical center. Jt Comm J Qual Patient Saf. 2014;40(9):389-397. PubMed
18. McEachern R, Campbell Jr GD. Hospital-Acquired Pneumonia: Epidemiology, Etiology, and Treatment. Infect Dis Clin North Am. 1998;12(3):761-779. PubMed
19. Zimlichman E, Henderson D, Tamir O, et al. Health care–associated infections. JAMA Intern Med. 2013;173(22):2039. PubMed
A central tenet of modern medicine is that patients must provide fully informed consent to receive or refuse medical care offered by their clinical teams.1–4 If a patient is unable to make and communicate a choice or clearly indicate an understanding of the information presented, then he or she is considered to lack the capacity to make medical decisions and the medical team must seek consent from the patient’s surrogate decision-maker.2-7 Every U.S. state recognizes a patient’s healthcare proxy (HCP) and a court-appointed guardian as a legally recognized surrogate.8,9 Most of the states also have statutes or regulations establishing a hierarchy of legally recognized surrogate decision-makers in the absence of a HCP or a court-appointed guardian, such as spouses, adult children, parents, siblings, and grandparents.8,10 In states that do not have such a statute, hospitals develop their own institutional policies for surrogate decision-making.
However, there are important limitations on the authority of these surrogate decision-makers.10 For instance, patients may not have a family member or a friend to serve as a surrogate decision-maker, often family members cannot override a patient’s objection, even when that patient lacks decision-making capacity, and certain decisions require a guardian or a HCP.8-10 In these circumstances, the hospital must petition a court to appoint a guardian as a legally recognized surrogate decision-maker. This can be an involved family member, if one exists, or an independent, typically volunteer, guardian.11 The process of guardian appointment is complex7,11 and can range from a few days to more than a month, largely dependent on court dates and finding a volunteer guardian. Much of the process occurs during the patient’s hospital stay. This prolongation of hospitalization would be expected to increase health care costs and iatrogenic complications,12–14 but data quantifying these for patients requiring guardianship are lacking. The goal of this study was to describe the characteristics of patients who undergo the process of guardianship and measure the associated burdens. These burdens include the financial costs to the medical system, the prolonged length of stay beyond medical necessity, and the costs to the patient in the form of hospital-acquired complications. Investigating the burden of guardianship is an important first step in uncovering opportunities to improve the process. We hypothesized that patients requiring guardianship would have lengths of stay and healthcare costs that were at least as large as those for patients whose conditions required similar durations of hospitalization prior to medical clearance, in part due to iatrogenic complications that would accrue while awaiting guardian appointment.
METHODS
Setting
We conducted a retrospective matched cohort study of adult inpatients at Beth Israel Deaconess Medical Center (BIDMC), a 651-bed academic, tertiary care facility in Boston, MA. The study was approved by the BIDMC Institutional Review Board as a nonhuman subject research consistent with hospital operations.
Population
For this matched cohort study, we identified case patients as those hospitalized for any reason for whom guardianship proceedings were initiated and obtained; only the first hospitalization during which the guardianship was pursued was used. Cases were identified by obtaining the data of all patients for whom the BIDMC general counsel completed the process of guardianship between October 2014 and September 2015. At BIDMC, all the guardianship proceedings are referred to the general counsel.
To determine the postclearance experience for referred patients compared with that for other patients with similar lengths of stay up to those of the referred patients’ point of clearance, we identified up to three matched controls for each case (Supplemental Figure 1). Medical clearance was defined as the date when the patient was medically stable to be discharged from the hospital, and it was determined in an iterative manner. We identified controls as hospitalized patients admitted for any cause and matched to the cases requiring guardianship on discharging service and length of stay prior to clearance. Specifically, we identified patients on the same service as the case whose length of stay was at least as long as the length of stay of the case patient until medical clearance, as defined below. We then determined the total and the excess length of stay, defined as the duration beyond clearance for each case referred for guardianship; for controls, the ‘excess’ length of stay was the number of hospitalized days beyond the corresponding time that a matched case had been provided clearance. To account for seasonal influences and the training level of house officers, we selected the three controls whose discharge date was closest (before or after) to the discharge date of their matched case.
From legal team files, we identified 61 patients hospitalized at BIDMC for whom new guardianship was pursued to completion. Of these 61 patients, 10 could not be matched to an appropriate control and were included in descriptive analyses but not in comparisons with controls.
Covariates and Outcomes
We collected the details regarding age, gender, primary language, highest level of education, marital status, insurance status, race, date of admission, date of discharge, discharge disposition, principal diagnosis, case mix index (CMI), and discharging service from our administrative and billing data. Outcomes of interest included length of stay and total hospital charges that were collected from the same databases. We used hospital charges, rather than payments, to ensure uniformity across payers.
Chart Review
Unique to cases, a team of two medical residents (JP, RP) and a hospitalist (DR) determined the date of medical clearance and hospital-associated complications by a chart review. The date of medical clearance was then used to calculate excess length of stay, ie, the duration of stay beyond the date of medical clearance, by subtracting the time to medical clearance from the total inpatient length of stay.
We developed a novel algorithm to determine the date of medical clearance consistently (Figure 1). We first determined whether the discharge summary indicated a clear date of medical readiness for discharge. If the discharge summary was unclear, then a case management or a social work note was used. The date of medical clearance determined by the case management or the social work note was then confirmed with clinical data. The date was confirmed if there were no significant laboratory orders and major medication changes or procedures for 24 h from the date identified. If notes were also inconclusive, then the medical clearance was determined by a review of provider order entry. Medical readiness for discharge was then defined as the first day when there were no laboratory orders for 48 h and no significant medication changes, imaging studies, or microbiologic orders.
Hospital-acquired complications were determined to be related to the guardianship process if they occurred after the date of medical stability but prior to discharge. We did not investigate hospital-acquired complications among controls. Hospital-acquired complications were defined as follows:
- Catheter-associated urinary tract infection (CAUTI): active Foley catheter order and positive urine culture that resulted in antibiotic administration.
- Hospital-acquired pneumonia (HAP): chest X-ray or computed tomography (CT) scan showing a consolidation that resulted in antibiotic administration.
- Venous thromboembolism (VTE): positive venous ultrasound or CT angiography of the chest for deep venous thrombosis (DVT) or pulmonary embolism (PE).
- Decubitus ulcer: new wound care consultation for sacral decubitus ulceration.
- Clostridium difficile (C. diff) infection: positive stool polymerase chain reaction that resulted in antibiotic administration.
The algorithm for identifying the date of clearance and the presence of complications was piloted independently by three investigators (RP, JP, DR) using a single chart review and was redesigned until a consensus was obtained. The same three investigators then independently reviewed three additional charts, including all notes, laboratory results, imaging results, and orders, with complete agreement for both date of clearance and presence of complications. Two investigators (RP, JP) then individually reviewed the remaining 57 charts. Of these, 10 were selected a priori for review by both investigators for interrater reliability, with a mean difference of 0.5 days in the estimated time to clearance and complete concordance in complications. In addition, a third investigator (DR) independently reread 5 of the 57 reviewed charts, with complete concordance in both time to clearance and presence of complications with the original readings.
Statistical Analysis
SAS 9.3 was used for all analyses (SAS Institute Inc., Cary, NC, USA).
We first examined the demographic and clinical characteristics of all 61 patients who underwent guardianship proceedings. Second, we described the primary outcomes of interest–length of stay, costs, and likelihood of complications–in this series of patients with associated 95% confidence intervals.
Third, we examined the associations between guardianship and length of stay and healthcare costs using generalized estimating equations with clustering by matched set and compound symmetry. For length of stay, we specifically assessed excess length of stay (the matching variable) to avoid immortal time bias; we also examined the total length of stay. For all regression analyses, we adjusted for the following covariates: age, gender, education, marital status, race/ethnicity, CMI, insurance status, discharging service, and principal diagnosis. To maximize normality of residuals, costs were log-transformed; length of stay beyond clearance was log-transformed after addition of 1. For both outcomes, we back-transformed the regression coefficients and presented percent change between case and control patients. All reported tests are two-sided.
RESULTS
A total of 61 guardianship cases and 118 controls were included in the analysis.
General Characteristics
The characteristics of all cases prior to matching are included in Table 1. The department of internal medicine discharged the largest proportion of cases, followed by neurosurgery and neurology departments. More than 65% of cases were insured by Medicare or Medicaid. Three-quarters of cases were discharged from the hospital to another medical facility, with about half discharged to a skilled nursing facility (SNF) or a rehabilitation center and one-quarter to a long-term acute care hospital (LTACH).
The median length of stay for patients requiring guardianship was 28 (range, 23-36) days, and the median total charges were $171,083 ($106,897-$245,281), with a total cost approximating $10.9 million for these patients. Regarding hospital-acquired complications, 10 (16%; 95% confidence interval, 8%–28%) unique cases suffered from a complication, with HAP being the most frequently (n = 5) occurring complication.
Comparison with Matched Controls
No statistically significant differences were observed between cases and controls in terms of age, primary language, highest level of education, ethnicity, insurance status, or discharging service as shown in Table 2; discharging service was a matched variable and comparable by design. However, cases tended to be less likely to be married and had a higher CMI.
When compared with control patients in terms of similar services who stayed for at least as long as their duration to clearance, the cases had significantly longer lengths of stay compared to those of controls (29 total days compared to 18 days, P < .001; Figure 2). In addition, cases incurred significantly higher median total charges ($168,666) compared to those of controls ($104,190; P = .02).
After accounting for potential confounders, including age, gender, language, education, marital status, discharging service, ethnicity, insurance status, CMI, and principal diagnosis, guardianship was associated with 58% higher excess length of stay (P = .04, 95% CI [2%-145%]). Furthermore, guardianship was associated with 23% higher total charges (P = .02, 95% CI [4%-46%]) and 37% longer total length of stay (P = .002, 95% CI [12%-67%]).
DISCUSSION
To our knowledge, this is among the first studies to investigate healthcare costs and harm to the patient in the form of hospital-associated complications as a result of guardianship proceedings. Other studies15,16 have also demonstrated excessive length of stay attributed to nonclinical factors such as guardianship, though they did not quantify the excess stay or compare guardianship cases with a matched control. One study17 demonstrated total charges of $150,000 per patient requiring guardianship, which are similar to our results. However, Chen et al. also observed an average of 27.8 medically unnecessary days, which are 16 more days than those in our study sample. This may reflect the difference in how excess days were determined, namely, statistical process control analysis in the previous study compared with a manual chart review in our study. To our knowledge, no other study has compared guardianship cases with matched controls to compare their experiences to patients with similarly prolonged stays prior to clearance.
After matching by service and the length of stay until medical clearance in each guardianship case, the subsequent length of stay was higher among cases than among controls, even after adjustment for differences in CMI and diagnosis. This suggests that the process of obtaining guardianship results in a particularly prolonged length of stay, which is presumably attributable to factors other than medical complexity or ongoing illness.
It is probable that at least two interrelated mechanisms are responsible for the particularly high costs and the long stay of patients who require guardianship. First, the process of obtaining guardianship is itself protracted in several cases, necessitating long-term admissions well beyond the point of medical stability. Second, our results suggest that longer hospital stays are apt to grow further in a feed-forward cycle due to hospital-acquired complications that develop after the date of medical clearance. Indeed, in our series, 16% of patients sustained a complication that is readily attributable to hospital care after their date of clearance, and these types of complications are likely to lengthen the stay even further.
We compared cases referred for guardianship to control patients on the same services, at similar time points, whose length of stay was at least as long as the point of medical clearance as their corresponding case patient. Because cases were hospitalized with active medical needs to at least the point of clearance, we anticipated that costs might well be lower among cases, who had no medical necessity for hospitalization at the point of clearance, compared with controls who remained hospitalized presumably for active medical needs. Counter to this hypothesis, and accounting for potentially confounding variables, undergoing a guardianship proceeding was associated with nearly 25% higher costs of patient care. This may ultimately represent a substantial burden on the healthcare system. For example, in just 1 year in our hospital, the total hospital charges reached almost $11 million for the 61 patients who underwent guardianship proceedings. Considering that 65% of the patients requiring guardianship had Medicaid or Medicare coverage, there are significant financial implications for the hospital systems and to the public.
Limitations of our study relate to its retrospective nature at a single center. Investigating guardianship cases at a single center and with a small sample size of 61 patients limits generalizability. Nevertheless, we still had enough power to detect significant differences compared with matched controls, and this study remains the largest investigation into the cost associated with guardianship to date and the only study comparing guardianship cases with matched controls. Furthermore, we did not complete chart reviews of controls, which limits direct comparisons of complications and precluded our matching on variables that required detailed review.
The retrospective design may include confounders unaccounted for in our statistical design, though we attempted to match cases with controls to account for some of these potential differences and included a broad set of covariates that included measures of comorbidity and diagnosis. To this point, we included only CMI and principal diagnosis as the measures of severity, and adjustment for CMI, which includes features of the index hospitalization itself, may represent overadjustment. However, this type of overadjustment would tend to bias toward the null hypothesis.
Investigators only completed chart reviews for cases, which limits our ability to contrast the rate of hospital-associated complications for cases with that of controls. However, the rates of CAUTI and HAP complications among our cases were notably higher than national inpatient estimates, ie, 5% and 8% compared to 0.2%18 and 0.5%-1%,19 respectively. Furthermore, we demonstrated higher total costs and total lengths of stay among guardianship patients, analyses for which the attributed date of clearance for controls was not required, and the rate of complications among the case patients was sizable despite their being formally medically cleared. In other words, regardless of whether a complication rate of 16% is “typical” for inpatients hospitalized for these durations, this suggests that persistent hospitalization after clearance does not carry a benign prognosis.
In addition, to estimate healthcare costs, we relied on total hospital charges, which are readily available and reflect, at least in part, payer costs but do not reflect true costs to the medical center. Nonetheless, charges approximately reflect costs–with some variation across cost centers–and hence provide a useful metric for comparing cases and controls. To provide context, for academic medical centers such as ours, costs are typically about half of charges.
Finally, each state has different statutes for surrogate decision-making. The results of this study reflect the Massachusetts’ experience, with no public guardianship program or hierarchy statute. That being said, while this presumably causes the need for more guardianships in Massachusetts, the mechanisms for guardianship are broadly similar nationwide and are likely to result in excessive length of stay and cost similar to those in our population, as demonstrated in studies from other states.7,15–17
Implications
At a time where medical systems are searching for opportunities to reduce the length of stay, prevent unnecessary hospitalization, and improve the quality of care, reevaluating the guardianship process is ripe with opportunity. In this single academic center, the process of guardianship was associated with 58% excess length of stay and 23% higher total hospital charges. Furthermore, one in six patients requiring guardianship suffered from hospital-associated complications.
This matched cohort study adds quantitative data demonstrating substantial burdens to the healthcare system as a result of the guardianship process and can be used as an impetus for hospital administration and legal systems to expedite the process. Potential improvements include increasing HCP form completions (which would eliminate the need to pursue guardianship for most of such patients), identifying patients who lack a legally recognized surrogate decision-maker earlier in their hospital stay (ideally upon admission), and providing resources to assist clinical teams in the completion of affidavits necessary to support the appointment of a guardian, so that paperwork can be filed with courts sooner. Further research that provides more generalizable prospective data could potentially improve the guardianship process and reduce its burden on hospitals and patients even further.
Acknowledgments
The authors express their tremendous thanks to Gail Piatkowski for her invaluable assistance in collecting administrative and billing data.
Disclosures
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article
A central tenet of modern medicine is that patients must provide fully informed consent to receive or refuse medical care offered by their clinical teams.1–4 If a patient is unable to make and communicate a choice or clearly indicate an understanding of the information presented, then he or she is considered to lack the capacity to make medical decisions and the medical team must seek consent from the patient’s surrogate decision-maker.2-7 Every U.S. state recognizes a patient’s healthcare proxy (HCP) and a court-appointed guardian as a legally recognized surrogate.8,9 Most of the states also have statutes or regulations establishing a hierarchy of legally recognized surrogate decision-makers in the absence of a HCP or a court-appointed guardian, such as spouses, adult children, parents, siblings, and grandparents.8,10 In states that do not have such a statute, hospitals develop their own institutional policies for surrogate decision-making.
However, there are important limitations on the authority of these surrogate decision-makers.10 For instance, patients may not have a family member or a friend to serve as a surrogate decision-maker, often family members cannot override a patient’s objection, even when that patient lacks decision-making capacity, and certain decisions require a guardian or a HCP.8-10 In these circumstances, the hospital must petition a court to appoint a guardian as a legally recognized surrogate decision-maker. This can be an involved family member, if one exists, or an independent, typically volunteer, guardian.11 The process of guardian appointment is complex7,11 and can range from a few days to more than a month, largely dependent on court dates and finding a volunteer guardian. Much of the process occurs during the patient’s hospital stay. This prolongation of hospitalization would be expected to increase health care costs and iatrogenic complications,12–14 but data quantifying these for patients requiring guardianship are lacking. The goal of this study was to describe the characteristics of patients who undergo the process of guardianship and measure the associated burdens. These burdens include the financial costs to the medical system, the prolonged length of stay beyond medical necessity, and the costs to the patient in the form of hospital-acquired complications. Investigating the burden of guardianship is an important first step in uncovering opportunities to improve the process. We hypothesized that patients requiring guardianship would have lengths of stay and healthcare costs that were at least as large as those for patients whose conditions required similar durations of hospitalization prior to medical clearance, in part due to iatrogenic complications that would accrue while awaiting guardian appointment.
METHODS
Setting
We conducted a retrospective matched cohort study of adult inpatients at Beth Israel Deaconess Medical Center (BIDMC), a 651-bed academic, tertiary care facility in Boston, MA. The study was approved by the BIDMC Institutional Review Board as a nonhuman subject research consistent with hospital operations.
Population
For this matched cohort study, we identified case patients as those hospitalized for any reason for whom guardianship proceedings were initiated and obtained; only the first hospitalization during which the guardianship was pursued was used. Cases were identified by obtaining the data of all patients for whom the BIDMC general counsel completed the process of guardianship between October 2014 and September 2015. At BIDMC, all the guardianship proceedings are referred to the general counsel.
To determine the postclearance experience for referred patients compared with that for other patients with similar lengths of stay up to those of the referred patients’ point of clearance, we identified up to three matched controls for each case (Supplemental Figure 1). Medical clearance was defined as the date when the patient was medically stable to be discharged from the hospital, and it was determined in an iterative manner. We identified controls as hospitalized patients admitted for any cause and matched to the cases requiring guardianship on discharging service and length of stay prior to clearance. Specifically, we identified patients on the same service as the case whose length of stay was at least as long as the length of stay of the case patient until medical clearance, as defined below. We then determined the total and the excess length of stay, defined as the duration beyond clearance for each case referred for guardianship; for controls, the ‘excess’ length of stay was the number of hospitalized days beyond the corresponding time that a matched case had been provided clearance. To account for seasonal influences and the training level of house officers, we selected the three controls whose discharge date was closest (before or after) to the discharge date of their matched case.
From legal team files, we identified 61 patients hospitalized at BIDMC for whom new guardianship was pursued to completion. Of these 61 patients, 10 could not be matched to an appropriate control and were included in descriptive analyses but not in comparisons with controls.
Covariates and Outcomes
We collected the details regarding age, gender, primary language, highest level of education, marital status, insurance status, race, date of admission, date of discharge, discharge disposition, principal diagnosis, case mix index (CMI), and discharging service from our administrative and billing data. Outcomes of interest included length of stay and total hospital charges that were collected from the same databases. We used hospital charges, rather than payments, to ensure uniformity across payers.
Chart Review
Unique to cases, a team of two medical residents (JP, RP) and a hospitalist (DR) determined the date of medical clearance and hospital-associated complications by a chart review. The date of medical clearance was then used to calculate excess length of stay, ie, the duration of stay beyond the date of medical clearance, by subtracting the time to medical clearance from the total inpatient length of stay.
We developed a novel algorithm to determine the date of medical clearance consistently (Figure 1). We first determined whether the discharge summary indicated a clear date of medical readiness for discharge. If the discharge summary was unclear, then a case management or a social work note was used. The date of medical clearance determined by the case management or the social work note was then confirmed with clinical data. The date was confirmed if there were no significant laboratory orders and major medication changes or procedures for 24 h from the date identified. If notes were also inconclusive, then the medical clearance was determined by a review of provider order entry. Medical readiness for discharge was then defined as the first day when there were no laboratory orders for 48 h and no significant medication changes, imaging studies, or microbiologic orders.
Hospital-acquired complications were determined to be related to the guardianship process if they occurred after the date of medical stability but prior to discharge. We did not investigate hospital-acquired complications among controls. Hospital-acquired complications were defined as follows:
- Catheter-associated urinary tract infection (CAUTI): active Foley catheter order and positive urine culture that resulted in antibiotic administration.
- Hospital-acquired pneumonia (HAP): chest X-ray or computed tomography (CT) scan showing a consolidation that resulted in antibiotic administration.
- Venous thromboembolism (VTE): positive venous ultrasound or CT angiography of the chest for deep venous thrombosis (DVT) or pulmonary embolism (PE).
- Decubitus ulcer: new wound care consultation for sacral decubitus ulceration.
- Clostridium difficile (C. diff) infection: positive stool polymerase chain reaction that resulted in antibiotic administration.
The algorithm for identifying the date of clearance and the presence of complications was piloted independently by three investigators (RP, JP, DR) using a single chart review and was redesigned until a consensus was obtained. The same three investigators then independently reviewed three additional charts, including all notes, laboratory results, imaging results, and orders, with complete agreement for both date of clearance and presence of complications. Two investigators (RP, JP) then individually reviewed the remaining 57 charts. Of these, 10 were selected a priori for review by both investigators for interrater reliability, with a mean difference of 0.5 days in the estimated time to clearance and complete concordance in complications. In addition, a third investigator (DR) independently reread 5 of the 57 reviewed charts, with complete concordance in both time to clearance and presence of complications with the original readings.
Statistical Analysis
SAS 9.3 was used for all analyses (SAS Institute Inc., Cary, NC, USA).
We first examined the demographic and clinical characteristics of all 61 patients who underwent guardianship proceedings. Second, we described the primary outcomes of interest–length of stay, costs, and likelihood of complications–in this series of patients with associated 95% confidence intervals.
Third, we examined the associations between guardianship and length of stay and healthcare costs using generalized estimating equations with clustering by matched set and compound symmetry. For length of stay, we specifically assessed excess length of stay (the matching variable) to avoid immortal time bias; we also examined the total length of stay. For all regression analyses, we adjusted for the following covariates: age, gender, education, marital status, race/ethnicity, CMI, insurance status, discharging service, and principal diagnosis. To maximize normality of residuals, costs were log-transformed; length of stay beyond clearance was log-transformed after addition of 1. For both outcomes, we back-transformed the regression coefficients and presented percent change between case and control patients. All reported tests are two-sided.
RESULTS
A total of 61 guardianship cases and 118 controls were included in the analysis.
General Characteristics
The characteristics of all cases prior to matching are included in Table 1. The department of internal medicine discharged the largest proportion of cases, followed by neurosurgery and neurology departments. More than 65% of cases were insured by Medicare or Medicaid. Three-quarters of cases were discharged from the hospital to another medical facility, with about half discharged to a skilled nursing facility (SNF) or a rehabilitation center and one-quarter to a long-term acute care hospital (LTACH).
The median length of stay for patients requiring guardianship was 28 (range, 23-36) days, and the median total charges were $171,083 ($106,897-$245,281), with a total cost approximating $10.9 million for these patients. Regarding hospital-acquired complications, 10 (16%; 95% confidence interval, 8%–28%) unique cases suffered from a complication, with HAP being the most frequently (n = 5) occurring complication.
Comparison with Matched Controls
No statistically significant differences were observed between cases and controls in terms of age, primary language, highest level of education, ethnicity, insurance status, or discharging service as shown in Table 2; discharging service was a matched variable and comparable by design. However, cases tended to be less likely to be married and had a higher CMI.
When compared with control patients in terms of similar services who stayed for at least as long as their duration to clearance, the cases had significantly longer lengths of stay compared to those of controls (29 total days compared to 18 days, P < .001; Figure 2). In addition, cases incurred significantly higher median total charges ($168,666) compared to those of controls ($104,190; P = .02).
After accounting for potential confounders, including age, gender, language, education, marital status, discharging service, ethnicity, insurance status, CMI, and principal diagnosis, guardianship was associated with 58% higher excess length of stay (P = .04, 95% CI [2%-145%]). Furthermore, guardianship was associated with 23% higher total charges (P = .02, 95% CI [4%-46%]) and 37% longer total length of stay (P = .002, 95% CI [12%-67%]).
DISCUSSION
To our knowledge, this is among the first studies to investigate healthcare costs and harm to the patient in the form of hospital-associated complications as a result of guardianship proceedings. Other studies15,16 have also demonstrated excessive length of stay attributed to nonclinical factors such as guardianship, though they did not quantify the excess stay or compare guardianship cases with a matched control. One study17 demonstrated total charges of $150,000 per patient requiring guardianship, which are similar to our results. However, Chen et al. also observed an average of 27.8 medically unnecessary days, which are 16 more days than those in our study sample. This may reflect the difference in how excess days were determined, namely, statistical process control analysis in the previous study compared with a manual chart review in our study. To our knowledge, no other study has compared guardianship cases with matched controls to compare their experiences to patients with similarly prolonged stays prior to clearance.
After matching by service and the length of stay until medical clearance in each guardianship case, the subsequent length of stay was higher among cases than among controls, even after adjustment for differences in CMI and diagnosis. This suggests that the process of obtaining guardianship results in a particularly prolonged length of stay, which is presumably attributable to factors other than medical complexity or ongoing illness.
It is probable that at least two interrelated mechanisms are responsible for the particularly high costs and the long stay of patients who require guardianship. First, the process of obtaining guardianship is itself protracted in several cases, necessitating long-term admissions well beyond the point of medical stability. Second, our results suggest that longer hospital stays are apt to grow further in a feed-forward cycle due to hospital-acquired complications that develop after the date of medical clearance. Indeed, in our series, 16% of patients sustained a complication that is readily attributable to hospital care after their date of clearance, and these types of complications are likely to lengthen the stay even further.
We compared cases referred for guardianship to control patients on the same services, at similar time points, whose length of stay was at least as long as the point of medical clearance as their corresponding case patient. Because cases were hospitalized with active medical needs to at least the point of clearance, we anticipated that costs might well be lower among cases, who had no medical necessity for hospitalization at the point of clearance, compared with controls who remained hospitalized presumably for active medical needs. Counter to this hypothesis, and accounting for potentially confounding variables, undergoing a guardianship proceeding was associated with nearly 25% higher costs of patient care. This may ultimately represent a substantial burden on the healthcare system. For example, in just 1 year in our hospital, the total hospital charges reached almost $11 million for the 61 patients who underwent guardianship proceedings. Considering that 65% of the patients requiring guardianship had Medicaid or Medicare coverage, there are significant financial implications for the hospital systems and to the public.
Limitations of our study relate to its retrospective nature at a single center. Investigating guardianship cases at a single center and with a small sample size of 61 patients limits generalizability. Nevertheless, we still had enough power to detect significant differences compared with matched controls, and this study remains the largest investigation into the cost associated with guardianship to date and the only study comparing guardianship cases with matched controls. Furthermore, we did not complete chart reviews of controls, which limits direct comparisons of complications and precluded our matching on variables that required detailed review.
The retrospective design may include confounders unaccounted for in our statistical design, though we attempted to match cases with controls to account for some of these potential differences and included a broad set of covariates that included measures of comorbidity and diagnosis. To this point, we included only CMI and principal diagnosis as the measures of severity, and adjustment for CMI, which includes features of the index hospitalization itself, may represent overadjustment. However, this type of overadjustment would tend to bias toward the null hypothesis.
Investigators only completed chart reviews for cases, which limits our ability to contrast the rate of hospital-associated complications for cases with that of controls. However, the rates of CAUTI and HAP complications among our cases were notably higher than national inpatient estimates, ie, 5% and 8% compared to 0.2%18 and 0.5%-1%,19 respectively. Furthermore, we demonstrated higher total costs and total lengths of stay among guardianship patients, analyses for which the attributed date of clearance for controls was not required, and the rate of complications among the case patients was sizable despite their being formally medically cleared. In other words, regardless of whether a complication rate of 16% is “typical” for inpatients hospitalized for these durations, this suggests that persistent hospitalization after clearance does not carry a benign prognosis.
In addition, to estimate healthcare costs, we relied on total hospital charges, which are readily available and reflect, at least in part, payer costs but do not reflect true costs to the medical center. Nonetheless, charges approximately reflect costs–with some variation across cost centers–and hence provide a useful metric for comparing cases and controls. To provide context, for academic medical centers such as ours, costs are typically about half of charges.
Finally, each state has different statutes for surrogate decision-making. The results of this study reflect the Massachusetts’ experience, with no public guardianship program or hierarchy statute. That being said, while this presumably causes the need for more guardianships in Massachusetts, the mechanisms for guardianship are broadly similar nationwide and are likely to result in excessive length of stay and cost similar to those in our population, as demonstrated in studies from other states.7,15–17
Implications
At a time where medical systems are searching for opportunities to reduce the length of stay, prevent unnecessary hospitalization, and improve the quality of care, reevaluating the guardianship process is ripe with opportunity. In this single academic center, the process of guardianship was associated with 58% excess length of stay and 23% higher total hospital charges. Furthermore, one in six patients requiring guardianship suffered from hospital-associated complications.
This matched cohort study adds quantitative data demonstrating substantial burdens to the healthcare system as a result of the guardianship process and can be used as an impetus for hospital administration and legal systems to expedite the process. Potential improvements include increasing HCP form completions (which would eliminate the need to pursue guardianship for most of such patients), identifying patients who lack a legally recognized surrogate decision-maker earlier in their hospital stay (ideally upon admission), and providing resources to assist clinical teams in the completion of affidavits necessary to support the appointment of a guardian, so that paperwork can be filed with courts sooner. Further research that provides more generalizable prospective data could potentially improve the guardianship process and reduce its burden on hospitals and patients even further.
Acknowledgments
The authors express their tremendous thanks to Gail Piatkowski for her invaluable assistance in collecting administrative and billing data.
Disclosures
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article
1. O’Neill O. Autonomy and Trust in Bioethics. Cambridge: Cambridge University Press; 2002. PubMed
2. Beauchamp T, Childress J. Principles of Biomedical Ethics. 7th ed. New York: Oxford University Press; 2013.
3. McMurray RJ, Clarke OW, Barrasso JA, et al. Decisions near the end of life. J Am Med Assoc. 1992;267(16):2229-2233.
4. American Medical Association. AMA Principles of Medical Ethics: Chapter 2 - Opinions on Consent, Communication and Decision Making.; 2016.
5. Arnold RM, Kellum J. Moral justifications for surrogate decision making in the intensive care unit: Implications and limitations. Crit Care Med. 2003;31(Supplement):S347-S353. PubMed
6. Karp N, Wood E. Incapacitated and Alone: Healthcare Decision Making for Unbefriended Older People. Am Bar Assoc Hum Rights. 2003;31(2).
7. Bandy RJ, Helft PR, Bandy RW, Torke AM. Medical decision-making during the guardianship process for incapacitated, hospitalized adults: a descriptive cohort study. J Gen Intern Med. 2010;25(10):1003-1008. PubMed
8. Wynn S. Decisions by surrogates: an overview of surrogate consent laws in the United States. Bifocal. 2014;36(1):10-14.
9. Massachusetts General Laws. Chapter 201D: Health Care Proxies. https://malegislature.gov/Laws/GeneralLaws/PartII/TitleII/Chapter201D. Published 2017. Accessed March 31, 2017.
10. American Bar Association Commision on Law and Aging. Default Surrogate Consent Statutes. Am Bar Assoc. 2016:1-17.
11. Massachusetts General Laws. Chapter 190B: Massachusetts Probate Code. https://malegislature.gov/Laws/GeneralLaws/PartII/TitleII/Chapter190B. Published 2017. Accessed March 31, 2017.
12. Rosman M, Rachminov O, Segal O, Segal G. Prolonged patients’ in-hospital waiting period after discharge eligibility is associated with increased risk of infection, morbidity and mortality: a retrospective cohort analysis. BMC Health Serv Res. 2015;15:246. PubMed
13. Majeed MU, Williams DT, Pollock R, et al. Delay in discharge and its impact on unnecessary hospital bed occupancy. 2012. PubMed
14. Nobili A, Licata G, Salerno F, et al. Polypharmacy, length of hospital stay, and in-hospital mortality among elderly patients in internal medicine wards. The REPOSI study. Eur J Clin Pharmacol. 2011;67(5):507-519. PubMed
15. Chen JJ, Finn CT, Homa K, St Onge KP, Caller TA. Discharge delays for patients requiring in-hospital guardianship: A Cohort Analysis. J Healthc Qual. 2016;38(4):235-242. PubMed
16. Chen JJ, Kwon A, Stevens Y, Finn CT. Barriers beyond clinical control affecting timely hospital discharge for a patient requiring guardianship. Psychosomatics. 2015;56(2):206-209. PubMed
17. Chen JJ, Blanchard MA, Finn CT, et al. A clinical pathway for guardianship at dartmouth-hitchcock medical center. Jt Comm J Qual Patient Saf. 2014;40(9):389-397. PubMed
18. McEachern R, Campbell Jr GD. Hospital-Acquired Pneumonia: Epidemiology, Etiology, and Treatment. Infect Dis Clin North Am. 1998;12(3):761-779. PubMed
19. Zimlichman E, Henderson D, Tamir O, et al. Health care–associated infections. JAMA Intern Med. 2013;173(22):2039. PubMed
1. O’Neill O. Autonomy and Trust in Bioethics. Cambridge: Cambridge University Press; 2002. PubMed
2. Beauchamp T, Childress J. Principles of Biomedical Ethics. 7th ed. New York: Oxford University Press; 2013.
3. McMurray RJ, Clarke OW, Barrasso JA, et al. Decisions near the end of life. J Am Med Assoc. 1992;267(16):2229-2233.
4. American Medical Association. AMA Principles of Medical Ethics: Chapter 2 - Opinions on Consent, Communication and Decision Making.; 2016.
5. Arnold RM, Kellum J. Moral justifications for surrogate decision making in the intensive care unit: Implications and limitations. Crit Care Med. 2003;31(Supplement):S347-S353. PubMed
6. Karp N, Wood E. Incapacitated and Alone: Healthcare Decision Making for Unbefriended Older People. Am Bar Assoc Hum Rights. 2003;31(2).
7. Bandy RJ, Helft PR, Bandy RW, Torke AM. Medical decision-making during the guardianship process for incapacitated, hospitalized adults: a descriptive cohort study. J Gen Intern Med. 2010;25(10):1003-1008. PubMed
8. Wynn S. Decisions by surrogates: an overview of surrogate consent laws in the United States. Bifocal. 2014;36(1):10-14.
9. Massachusetts General Laws. Chapter 201D: Health Care Proxies. https://malegislature.gov/Laws/GeneralLaws/PartII/TitleII/Chapter201D. Published 2017. Accessed March 31, 2017.
10. American Bar Association Commision on Law and Aging. Default Surrogate Consent Statutes. Am Bar Assoc. 2016:1-17.
11. Massachusetts General Laws. Chapter 190B: Massachusetts Probate Code. https://malegislature.gov/Laws/GeneralLaws/PartII/TitleII/Chapter190B. Published 2017. Accessed March 31, 2017.
12. Rosman M, Rachminov O, Segal O, Segal G. Prolonged patients’ in-hospital waiting period after discharge eligibility is associated with increased risk of infection, morbidity and mortality: a retrospective cohort analysis. BMC Health Serv Res. 2015;15:246. PubMed
13. Majeed MU, Williams DT, Pollock R, et al. Delay in discharge and its impact on unnecessary hospital bed occupancy. 2012. PubMed
14. Nobili A, Licata G, Salerno F, et al. Polypharmacy, length of hospital stay, and in-hospital mortality among elderly patients in internal medicine wards. The REPOSI study. Eur J Clin Pharmacol. 2011;67(5):507-519. PubMed
15. Chen JJ, Finn CT, Homa K, St Onge KP, Caller TA. Discharge delays for patients requiring in-hospital guardianship: A Cohort Analysis. J Healthc Qual. 2016;38(4):235-242. PubMed
16. Chen JJ, Kwon A, Stevens Y, Finn CT. Barriers beyond clinical control affecting timely hospital discharge for a patient requiring guardianship. Psychosomatics. 2015;56(2):206-209. PubMed
17. Chen JJ, Blanchard MA, Finn CT, et al. A clinical pathway for guardianship at dartmouth-hitchcock medical center. Jt Comm J Qual Patient Saf. 2014;40(9):389-397. PubMed
18. McEachern R, Campbell Jr GD. Hospital-Acquired Pneumonia: Epidemiology, Etiology, and Treatment. Infect Dis Clin North Am. 1998;12(3):761-779. PubMed
19. Zimlichman E, Henderson D, Tamir O, et al. Health care–associated infections. JAMA Intern Med. 2013;173(22):2039. PubMed
© 2018 Society of Hospital Medicine