User login
Development of a Multidisciplinary Stroke Program
Stroke is the fifth leading cause of death in the U.S. and a leading cause of long-term disability. About 15,000 military veterans are hospitalized for acute ischemic stroke each year, and $274 million was spent for their acute, postacute, and subsequent stroke-related care over the first 6 months following the stroke.1
The Durham VAMC (DVAMC) lies within the country’s “stroke belt,” an area of 8 contiguous southeastern states, and provides care to more than 200,000 veterans living in a 26-county area of central and eastern North Carolina. The stroke mortality rates in this region are up to 40% higher than that of the national average rate.2 The DVAMC sought to transform the organization of stroke care provided to hospitalized patients as an important step in optimizing their outcomes.
Background
The VHA is committed to providing high-quality, evidence-based health care and collects data reflecting its services, including care processes and outcomes. The 2009 Office of Quality and Performance report raised concerns about the delivery of stroke care within the VHA, based on an assessment of several quality indicators. This led to the 2011 VHA directive providing policies based on national standards for the management of acute ischemic stroke (AIS) in VHA medical facilities.3
The directive defined 3 types of VHA facilities: primary stroke centers, limited-hours stroke facilities, and supporting stroke facilities. The directive further required that “all VA medical facilities with inpatient acute care medical or surgical beds have a written policy guiding appropriate care to patients with AIS in place by January 1, 2012, and implemented no later than June 1, 2012,” which included “protocols or pathways for the rapid identification, evaluation, and treatment” of patients with acute stroke and monitoring of appropriate performance indicators. For many VHA facilities caring for patients with acute stroke, including the DVAMC, the directive necessitated the development of multidisciplinary teams, organized around the provision of stroke care.
DVAMC Stroke Program
A disease-specific program typically involves the coordination of multiple care components and aims to improve continuity of care. The approach is intended to reduce care fragmentation. Through an already existing program, many elements of stroke-specific care were being delivered at the DVAMC, but several gaps and no formal system existed for coordinating stroke-related care. Programmatic goals were developed to optimize adherence to national stroke-related process measures; minimize morbidity mortality, duration of hospitalization, postdischarge emergency department (ED) visits, and readmissions; and improve continuity of care.
The Team
The DVAMC is affiliated with Duke University School of Medicine and Duke University Medical Center. The Duke University Medical Center is a Joint Commission-certified Comprehensive Stroke Center, and its director also serves as the director of the Durham VAMC Stroke Program. Because of the time and clinical expertise required to develop and oversee the program, a critical initial step was to identify a dedicated stroke program coordinator (SPC) to integrate care services and manage its implementation and ongoing activities.
The specific responsibilities of the SPC vary, depending on a facility’s needs, goals, and resources. The SPC may serve primarily as the quality measure expert and data manager, have responsibilities for program implementation and maintenance, provide training for hospital staff, and help optimize communication and integration of neurologists, internal medicine teams, other consulting and treating services, and nursing and allied health providers. The SPC also may provide direct patient care, act as a case manager, and monitor longer-term outcomes.
The DVAMC SPC is a nurse practitioner (NP). The training was thought essential given an NP’s ability to work autonomously, manage all elements of care, conceptualize, collaborate, and provide medical management skills, as has been found beneficial in many other systems of care redesign.4 The DVAMC is a teaching hospital with much of the staff affiliated with Duke University Medical School and supervised by a team of expert attending physicians. The SPC’s roles at the DVAMC have been to facilitate program development, implementation, and maintenance and collect performance data and achieve quality metric goals.
Obtaining support and cooperation from all members of the health care team is necessary for success. Finding “champions”—selected staff with an interest in improving stroke care—is crucial to a multidisciplinary team approach. These staff members were identified and recruited to serve on work groups and task forces. The SPC served as the leader and as a resource for these teams.
Key Functions
The American Stroke Association’s Policy Recommendations for the Establishment of Stroke Systems of Care suggest that a stroke system should serve 3 critical functions: communication and collaboration, standardize care customized to the population, and include performance measures with a mechanism for evaluation.5
Communication/collaboration: Collaboration in the Durham VAMC occurs through multidisciplinary work groups, including all relevant disciplines. The SPC facilitated communication and integration of care. Communication with other SPCs and accessing community resources are invaluable.
Standardized care: Stroke policies and procedures ensure that care is not only evidence-based, but also consistent. Teams worked to develop policies, protocols, order sets, documentation templates, and standardized patient education materials. The SPC identified available resources, both within the hospital, as well as within the surrounding community and professional organizations to assist in developing these tools.
Performance measures and evaluation: Performance measures and program evaluations provide a means to evaluate the progress of already implemented strategies, assist in identifying further needs, and guide future plans. The DVAMC immediately began to monitor stroke care using a standardized set of metrics, and as the program developed further, additional performance measures were added, such as length of stay (LOS), postdischarge ED visits and readmissions, and stroke code treatment time goals.
Necessary Components
To ensure its comprehensiveness, the DVAMC Stroke Program was modeled after the American Heart Association (AHA) recommendations for necessary components of a stroke system: emergency medical system (EMS) response, acute in-hospital-based treatment, subacute and secondary prevention, rehabilitation, prevention and community education, and quality improvement initiatives.5 Although intended for larger community-integrated systems, the AHA model nonetheless provides a useful framework for the development of a hospital-based stroke program.
Emergency Medical Response
The establishment of collaborative networks with community partners is essential. The DVAMC staff worked closely with the local EMS providers, facilitating community collaboration. The hospital also maintains collaborative agreements with its medical affiliates for urgent and emergent treatments. The program director and program coordinator are involved in these relationships.
Acute Stroke Treatment
The first phase of system redesign for the DVAMC in response to the 2011 VHA directive included the formulation of an acute stroke medical center memorandum (MCM), or policy, which outlined the facility’s process for acute stroke evaluation and care. The DVAMC qualified as a limited-hours stroke facility (ie, a facility with the necessary personnel, infrastructure, expertise, and programs to diagnose and treat stroke patients emergently, including the administration of alteplase to appropriate candidates, limited to normal business hours).
Related: Stroke and Preventable Hospitalization: Who Is Most at Risk?
At the start of the Stroke Program, the DVAMC had only computed tomography (CT) services during daytime working hours and relied on on-call coverage during nonbusiness hours. There had been previous discussions regarding expansion of radiology CT services; however, development of the Stroke Program led to this expansion becoming a priority. Patients with symptoms of an acute stroke who might otherwise have been a candidate for treatment with IV alteplase or patients who had other symptoms warranting an emergent brain or other CT no longer needed to be transferred to another facility. Radiology Services worked with the Stroke Program, leading to the progressive expansion of CT availability to first include longer daytime coverage and in 2014, implementation of full 24/7 CT services, allowing the hospital to become a VHA primary stroke center.
In conjunction with the MCM, a stroke code team was also implemented. A stroke code facilitates the rapid evaluation and treatment of a patient with a suspected stroke who might be a candidate for acute revascularization by the neurology and critical care staff. Durham’s stroke code team consists of a neurologist, cardiac care unit resident and RN, SPC, escort services, CT technician, bed coordinator, and chaplain services. The SPC attends all stroke codes during normal working hours, collects real-time data, and obtains retrospective data from chart audits for codes occurring when the SPC is not available. By having protocols in place, the program is organized such that the SPC need not be present to facilitate care during each stroke code.
In the early stages of program development, a stroke code process was not used in the ED and was underused in the inpatient setting, making clear documentation and evaluation of acute stroke care and treatment times difficult, if not impossible. Throughout the first 15 months of the program implementation, monthly code activation use increased by 63%. The increase in stroke code team use led to improvements in acute stroke care and accurate determination of acute stroke treatment time goals.
The efforts of both the ED and radiology teams contributed to the improvements in “door-to-CT” and “door-to-CT results” times. Door-to-CT times are expected to improve further now that the facility has implemented CT services on a 24/7 basis. Currently, average door-to-CT time is 20.6 minutes, and door-to-CT results time is 42.4 minutes, both within the National Institute of Neurological Disorders and Stroke goals of < 25 minutes and < 45 minutes respectively.6 Time tracking was part of the program’s development, as this was not previously recorded. As a result, baseline door-to-CT times were not available, and a national benchmark for comparison was used. Part of the Stroke Program’s development was putting into place a process for tracking times.
Related: Does Stroke Hit Women Harder?
Standardized methods of acute stroke evaluation were implemented early in the program development and included the use of the National Institutes of Health Stroke Scale (NIHSS) and a bedside dysphagia screening process. Staff members responsible for these initial evaluations, specifically ED and intensive care unit nurses, were trained on the use of these tools, and electronic documentation templates were developed to facilitate the assessments. Comprehensive neurologic evaluation, including the essential elements of advanced stroke assessment, was also captured in standardized documentation templates for the neurology team.
The use of standardized practices and documentation templates helped the staff adhere to the requirements for the timely completion and documentation of the NIHSS to almost 100% consistently; however, it remains a challenge to consistently comply with the requirement to perform bedside dysphagia screens prior to oral intake (including medications). At the initiation of these measures, the dysphagia screen was performed for 58% of stroke patients; this rose to a fairly consistent 80% over time. Maintaining this percentage is a continual challenge that requires the SPC to work closely with the nursing staff, ED, and medicine teams.
Prior to and in the early phases of program implementation, the DVAMC effectively did not administer alteplase to patients with ischemic stroke, often because the requisite evaluations could not be completed in the required time frame. Since September of 2013, about 9 months after the program began, all 7 patients with AIS who qualified for treatment with alteplase were treated according to national guidelines. Continued work toward a goal of a < 60 minutes door-to-needle time is needed; but with notable progress, as door-to-needle time has decreased by 8% from the first alteplase administration to the most recent.
Overseen by the Simulations Department and the SPC, stroke code simulations (ie, mock stroke codes) are performed to aid in evaluating the acute stroke care process. Stroke simulation events should be an ongoing practice in any stroke program. It is an effective means to identify and address issues that may not otherwise be readily apparent.
Subacute Treatment
At DVAMC, postacute stroke care was identified as a priority. The SPC led a multidisciplinary team that was tasked with developing a postacute stroke care map, or integrated care pathway. Consistent care practices, a comprehensive tool to be used as a guide, can assist in improving outcomes, especially in a teaching facility with constantly changing medical and other clinical staff. The tool was developed using best practice guidelines from all disciplines. Staff members are encouraged to reference the pathway when caring for stroke patients, with necessary elements of care or performance measures in boldface to highlight their importance. Overall, DVAMC’s Best Care score (the percentage of patients whose care met all performance measures during the admission) rose from 57.1% to 78.6% over the course of the first year of the program.
Another key element of subacute stroke care is the provision of standardized patient stroke education. Before program initiation, stroke education at the DVAMC lacked consistency in both content and frequency. Secondary prevention should start at diagnosis, and education should be a continual process from admission to discharge. A patient booklet was developed that incorporated all required elements of stroke education per AHA guidelines: stroke risk factors, recognizing signs and symptoms, emergency activation, medications, and follow-up needs as well as other information, such as stroke pathophysiology, diet and activity, and managing lifestyle changes.7
Patient education templates were designed to facilitate documentation. Achieving this performance measure is a challenge not only for the DVAMC, but also for acute facilities nationwide. It requires involvement of the SPC as well as continual staff feedback and improvement challenges. Adherence to the patient education performance measure at the DVAMC improved from 0% meeting all 5 required elements at baseline to an average of 80% of patients.
A team of stroke champions representing each discipline involved in stroke care was recruited to be part of a postacute stroke team, led by the SPC. The team, consisting of neurologists, nurses, physical therapists, occupational therapists, speech therapists, nutritionists, social workers, and case managers, meets weekly for rounding on stroke patients, discussing patient care issues, assessing the effectiveness of the program, and addressing any system issues. This regular meeting facilitates collaboration and overall team building.
Rehabilitation and Follow-up
Routine physical, occupational, and speech therapy assessments are necessary to guide discharge planning. Although providing rehabilitation services is a priority, payer source can be a barrier to ideal rehabilitative care for DVAMC veterans. VA-based rehabilitation facilities are limited; therefore, community rehabilitation options, paid for by either VA funds or the patient’s insurance (if available), are used for the majority of stroke patients requiring these services. Efforts to increase access to stroke-specific rehabilitation options were undertaken by dedicated stroke champions at DVAMC; however, obtaining satisfactory payment agreements remains challenging.
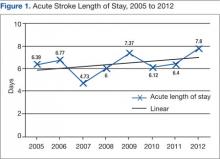
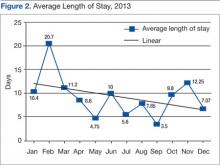
Timely discharge is an element of care that the SPC also continually assesses. Discharge planning should begin on admission, and the SPC helps ensure that patient and caregiver needs are met and that all necessary follow-up and consultation visits have been scheduled. The LOS for stroke patients at the DVAMC had been on a steady upward trend from 6.39 days in 2005 to nearly 8 days in 2012. Over the course of 2013, the first year of the Stroke Program, stroke LOS decreased to just over 7 days (Figures 1 and 2).
Readmission rates are lower in high-risk populations when patients are seen for follow-up in the first 1 to 2 weeks postdischarge.8 Scheduling early visits can be challenging, especially in the current environment of an overburdened health care system. The DVAMC adopted the practice of Stroke Program follow-up phone calls, performed 7 to 10 days postdischarge. A standardized checklist of questions and dialogue was implemented that addressed common poststroke issues and education. Readmissions decreased from 21% in the first quarter of 2013, to 5% in the fourth quarter of 2013 after the implementation of this checklist follow-up. It is likely still too early to determine with any certainty whether the efforts aimed at improved patient education and early intervention are responsible for this decline.
Prevention and Education
Secondary prevention starts with stroke diagnosis and should include the patient and family/caregiver, when applicable. Inpatient stroke education was a priority early in the program. As the acute and postacute program developed, attention turned to community education and prevention.
Community education should emphasize early intervention. As elsewhere, the DVAMC found that the majority of patients present for care well outside the treatment window for alteplase administration. Based on national guidelines, IV alteplase must be initiated in selected patients within 4.5 hours of symptom onset. Many surveys confirm that patients are not able to accurately identify stroke symptoms or are not aware that stroke is a medical emergency. Challenges in stroke care lie in community education.9,10 The SPC met with primary care providers (PCPs) to coordinate educational and preventative efforts, recruiting them in primary and secondary prevention strategies and educating them on high-risk patients.
The SPC also collaborated with one of the outpatient clinic Patient Aligned Care Teams (PACT, or primary care team) on the development of a primary prevention program. The PACT initiated a risk reduction educational program after noting that many of their patients had suboptimal stroke risk factor management.
The project is still in the pilot stage but is showing promise regarding patient interest and participation. It is focused on addressing 4 major risk factors: hypertension, diabetes, hyperlipidemia, and tobacco use. Through a PACT report, patients were identified as having stroke risk factors that were not optimally controlled. The project aims to reduce the risk of stroke through education, goal setting, and lifestyle modification and saw a 25% rate of participation among those patients identified as candidates for the program. Of these participants, 100% completed all 4 sessions and rated the program highly favorable.
Quality Improvement Measures
Tracking performance measures should begin at program inception. “Measures improve fastest when they are being used. …Measurement and reporting with currently available data should begin immediately. …The implied message is this: since data will be impossible to ignore, we might as well make them better.”8 The VHA has a system for monitoring various quality measures, which include specific aspects of acute stroke care set forth by the VHA Stroke Directive: timely administration of alteplase, timely performance of NIHSS, and performance of a dysphagia screen prior to oral intake.
The DVAMC SPC began more comprehensive assessments of acute stroke care and evaluated elements of postacute stroke care, based on a nationally recognized set of performance measures. A system of tracking stroke performance data was initiated in the first month of the program and is based on the 10 stroke performance measures defined by the AHA and the Joint Commission. Data are currently analyzed independent of a national data management system that does not allow for national benchmarking; however, the analysis was a starting point to track facility progress and emphasized the need for consistent care. Along with collecting data on the 10 stroke-specific elements, the SPC began a system to follow duration of hospitalization, postdischarge ED visits, readmissions, and mortality rates, as well as stroke code and door-to-needle-time data. The data are shared with the DVAMC Critical Care Committee via monthly reports, program leadership via quarterly reports, facility leadership via annual reports, and facility staff through periodic e-mails and the all-employee share drive.
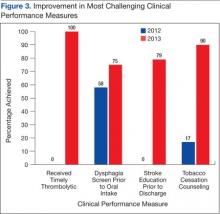
The first year of the program was associated with improvements in quality metrics across most areas of stroke care. Notably, 11 quality indicators that assess direct patient care measures have improved significantly from prior to program initiation in 2012 to after implementation of a comprehensive stroke care program at the conclusion of 2013. Those measures that were not already at goal of ≥ 85% achievement showed the most dramatic improvements (Figure 3).
Goals and Future Planning
The work of the DVAMC Stroke Program is far from over. Progress made is easily lost without continual monitoring and feedback. Challenges continue as well. Goals moving forward include improving door-to-needle times for IV alteplase therapy, more consistently performing swallow screens prior to oral intake, more consistently providing patient education, and increasing engagement with PCPs and the veteran community in providing stroke education and risk reduction.
A larger goal for future planning for the DVAMC is the need for a designated stroke care unit. Currently, stroke patients are admitted to the Critical Care Unit (CCU) for initial monitoring and treatment and when stable are moved to general medical wards. In some instances, this necessitates that the less acute patients occupy a CCU bed due to ward nursing limitations (ie, neuro checks every 2-hours is too great of a time demand for the ward nurses) or that the more neurologic acute patients are transferred to general medical wards when they would benefit from a more neurology-focused therapeutic environment. Stroke unit care has been associated with improved patient outcomes compared with care on general medical wards.11 The development of a designated stroke care unit is a long-range goal of the program.
Conclusion
The development of the Stroke Program, including an SPC, has improved the care of veterans with stroke at the DVAMC. The achievements of the DVAMC Stroke Program are the result of coordinated efforts of a team of dedicated health care professionals from all disciplines who sought to improve stroke care for veterans. The DVAMC continues to strive toward ever-improving outcomes, working with community partners and challenging itself to achieve a higher level of excellence. The lessons learned at the DVAMC may serve as a model for other VHA hospitals seeking to improve their stroke-related care programs.
Acknowledgements
The authors thank the executive leadership team and the chief of medicine of the DVAMC who recognized the need and potential for better stroke coordination and who have been fully supportive of the authors’ efforts to improve coordination, education, and care of their patients with strokes.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. QUERI—Quality Enhancement Research Initiative. Stroke QUERI. QUERI Website. http://www .queri.research.va.gov/str/default.cfm. Updated/Reviewed June 19, 2014. Accessed January 22, 2015.
2. Howard G, Evans GW, Pearce K, et al. Is the stroke belt disappearing? An analysis of racial, temporal, and age effects. Stroke. 1995;26(7):1153-1158.
3. Veterans Health Administration, U.S. Department of Veterans Affairs. Treatment of Acute Ischemic Stroke (AIS). VHA Directive 2011-038. U.S. Department of Veterans Affairs Website. http://www .va.gov/vhapublications/ViewPublication.asp?pub _ID=2458. Published November 2, 2011. Accessed January 22, 2015.
4. Green T, Newcommon N. Advancing nursing practice: The role of the nurse practitioner in an acute stroke program. J Neurosci Nurs. 2006;38(4 suppl):328-330.
5. Schwamm LH, Pancioli A, Acker JE III, et al; American Stroke Association’s Task Force on the Development of Stroke Systems. Recommendations for the establishment of stroke systems of care: Recommendations from the American Stroke Association’s Task Force on the Development of Stroke Systems. Stroke. 2005;36(3):690-703.
6. Bock BF. Response system for patients presenting with acute stroke. Paper presented at: Proceedings of a National Symposium on Rapid Identification and Treatment of Acute Stroke; December 12-13, 1996; Bethesda, MD. http://www.ninds.nih.gov/news_and _events/proceedings/stroke_proceedings/bock.htm.Published. Updated May 17, 2011. Accessed January 22, 2015.
7. American Heart Association, American Stroke Association. Stroke fact sheet. American Heart Association Website. http://www.heart.org/idc/groups/heart-public/@wcm/@private/@hcm/@gwtg/documents /downloadable/ucm_310976.pdf. Published April 2014. Accessed January 22, 2015.
8. Lee TH. Care redesign—A path forward for providers. N Engl J Med. 2012;367(5):466-472.
9. Kleindorfer D, Khoury J, Broderick JP, et al. Temporal trends in public awareness of stroke: Warning signs, risk factors, and treatment. Stroke. 2009;40(7):2502-2506.
10. Jauch EC, Saver JL, Adams HP Jr, et al; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Perripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947.
11. How do stroke units improve patient outcomes? A collaborative systematic review of the randomized trials. Stroke Unit Trialists Collaboration. Stroke. 1997;28(11):2139-2144.
Stroke is the fifth leading cause of death in the U.S. and a leading cause of long-term disability. About 15,000 military veterans are hospitalized for acute ischemic stroke each year, and $274 million was spent for their acute, postacute, and subsequent stroke-related care over the first 6 months following the stroke.1
The Durham VAMC (DVAMC) lies within the country’s “stroke belt,” an area of 8 contiguous southeastern states, and provides care to more than 200,000 veterans living in a 26-county area of central and eastern North Carolina. The stroke mortality rates in this region are up to 40% higher than that of the national average rate.2 The DVAMC sought to transform the organization of stroke care provided to hospitalized patients as an important step in optimizing their outcomes.
Background
The VHA is committed to providing high-quality, evidence-based health care and collects data reflecting its services, including care processes and outcomes. The 2009 Office of Quality and Performance report raised concerns about the delivery of stroke care within the VHA, based on an assessment of several quality indicators. This led to the 2011 VHA directive providing policies based on national standards for the management of acute ischemic stroke (AIS) in VHA medical facilities.3
The directive defined 3 types of VHA facilities: primary stroke centers, limited-hours stroke facilities, and supporting stroke facilities. The directive further required that “all VA medical facilities with inpatient acute care medical or surgical beds have a written policy guiding appropriate care to patients with AIS in place by January 1, 2012, and implemented no later than June 1, 2012,” which included “protocols or pathways for the rapid identification, evaluation, and treatment” of patients with acute stroke and monitoring of appropriate performance indicators. For many VHA facilities caring for patients with acute stroke, including the DVAMC, the directive necessitated the development of multidisciplinary teams, organized around the provision of stroke care.
DVAMC Stroke Program
A disease-specific program typically involves the coordination of multiple care components and aims to improve continuity of care. The approach is intended to reduce care fragmentation. Through an already existing program, many elements of stroke-specific care were being delivered at the DVAMC, but several gaps and no formal system existed for coordinating stroke-related care. Programmatic goals were developed to optimize adherence to national stroke-related process measures; minimize morbidity mortality, duration of hospitalization, postdischarge emergency department (ED) visits, and readmissions; and improve continuity of care.
The Team
The DVAMC is affiliated with Duke University School of Medicine and Duke University Medical Center. The Duke University Medical Center is a Joint Commission-certified Comprehensive Stroke Center, and its director also serves as the director of the Durham VAMC Stroke Program. Because of the time and clinical expertise required to develop and oversee the program, a critical initial step was to identify a dedicated stroke program coordinator (SPC) to integrate care services and manage its implementation and ongoing activities.
The specific responsibilities of the SPC vary, depending on a facility’s needs, goals, and resources. The SPC may serve primarily as the quality measure expert and data manager, have responsibilities for program implementation and maintenance, provide training for hospital staff, and help optimize communication and integration of neurologists, internal medicine teams, other consulting and treating services, and nursing and allied health providers. The SPC also may provide direct patient care, act as a case manager, and monitor longer-term outcomes.
The DVAMC SPC is a nurse practitioner (NP). The training was thought essential given an NP’s ability to work autonomously, manage all elements of care, conceptualize, collaborate, and provide medical management skills, as has been found beneficial in many other systems of care redesign.4 The DVAMC is a teaching hospital with much of the staff affiliated with Duke University Medical School and supervised by a team of expert attending physicians. The SPC’s roles at the DVAMC have been to facilitate program development, implementation, and maintenance and collect performance data and achieve quality metric goals.
Obtaining support and cooperation from all members of the health care team is necessary for success. Finding “champions”—selected staff with an interest in improving stroke care—is crucial to a multidisciplinary team approach. These staff members were identified and recruited to serve on work groups and task forces. The SPC served as the leader and as a resource for these teams.
Key Functions
The American Stroke Association’s Policy Recommendations for the Establishment of Stroke Systems of Care suggest that a stroke system should serve 3 critical functions: communication and collaboration, standardize care customized to the population, and include performance measures with a mechanism for evaluation.5
Communication/collaboration: Collaboration in the Durham VAMC occurs through multidisciplinary work groups, including all relevant disciplines. The SPC facilitated communication and integration of care. Communication with other SPCs and accessing community resources are invaluable.
Standardized care: Stroke policies and procedures ensure that care is not only evidence-based, but also consistent. Teams worked to develop policies, protocols, order sets, documentation templates, and standardized patient education materials. The SPC identified available resources, both within the hospital, as well as within the surrounding community and professional organizations to assist in developing these tools.
Performance measures and evaluation: Performance measures and program evaluations provide a means to evaluate the progress of already implemented strategies, assist in identifying further needs, and guide future plans. The DVAMC immediately began to monitor stroke care using a standardized set of metrics, and as the program developed further, additional performance measures were added, such as length of stay (LOS), postdischarge ED visits and readmissions, and stroke code treatment time goals.
Necessary Components
To ensure its comprehensiveness, the DVAMC Stroke Program was modeled after the American Heart Association (AHA) recommendations for necessary components of a stroke system: emergency medical system (EMS) response, acute in-hospital-based treatment, subacute and secondary prevention, rehabilitation, prevention and community education, and quality improvement initiatives.5 Although intended for larger community-integrated systems, the AHA model nonetheless provides a useful framework for the development of a hospital-based stroke program.
Emergency Medical Response
The establishment of collaborative networks with community partners is essential. The DVAMC staff worked closely with the local EMS providers, facilitating community collaboration. The hospital also maintains collaborative agreements with its medical affiliates for urgent and emergent treatments. The program director and program coordinator are involved in these relationships.
Acute Stroke Treatment
The first phase of system redesign for the DVAMC in response to the 2011 VHA directive included the formulation of an acute stroke medical center memorandum (MCM), or policy, which outlined the facility’s process for acute stroke evaluation and care. The DVAMC qualified as a limited-hours stroke facility (ie, a facility with the necessary personnel, infrastructure, expertise, and programs to diagnose and treat stroke patients emergently, including the administration of alteplase to appropriate candidates, limited to normal business hours).
Related: Stroke and Preventable Hospitalization: Who Is Most at Risk?
At the start of the Stroke Program, the DVAMC had only computed tomography (CT) services during daytime working hours and relied on on-call coverage during nonbusiness hours. There had been previous discussions regarding expansion of radiology CT services; however, development of the Stroke Program led to this expansion becoming a priority. Patients with symptoms of an acute stroke who might otherwise have been a candidate for treatment with IV alteplase or patients who had other symptoms warranting an emergent brain or other CT no longer needed to be transferred to another facility. Radiology Services worked with the Stroke Program, leading to the progressive expansion of CT availability to first include longer daytime coverage and in 2014, implementation of full 24/7 CT services, allowing the hospital to become a VHA primary stroke center.
In conjunction with the MCM, a stroke code team was also implemented. A stroke code facilitates the rapid evaluation and treatment of a patient with a suspected stroke who might be a candidate for acute revascularization by the neurology and critical care staff. Durham’s stroke code team consists of a neurologist, cardiac care unit resident and RN, SPC, escort services, CT technician, bed coordinator, and chaplain services. The SPC attends all stroke codes during normal working hours, collects real-time data, and obtains retrospective data from chart audits for codes occurring when the SPC is not available. By having protocols in place, the program is organized such that the SPC need not be present to facilitate care during each stroke code.
In the early stages of program development, a stroke code process was not used in the ED and was underused in the inpatient setting, making clear documentation and evaluation of acute stroke care and treatment times difficult, if not impossible. Throughout the first 15 months of the program implementation, monthly code activation use increased by 63%. The increase in stroke code team use led to improvements in acute stroke care and accurate determination of acute stroke treatment time goals.
The efforts of both the ED and radiology teams contributed to the improvements in “door-to-CT” and “door-to-CT results” times. Door-to-CT times are expected to improve further now that the facility has implemented CT services on a 24/7 basis. Currently, average door-to-CT time is 20.6 minutes, and door-to-CT results time is 42.4 minutes, both within the National Institute of Neurological Disorders and Stroke goals of < 25 minutes and < 45 minutes respectively.6 Time tracking was part of the program’s development, as this was not previously recorded. As a result, baseline door-to-CT times were not available, and a national benchmark for comparison was used. Part of the Stroke Program’s development was putting into place a process for tracking times.
Related: Does Stroke Hit Women Harder?
Standardized methods of acute stroke evaluation were implemented early in the program development and included the use of the National Institutes of Health Stroke Scale (NIHSS) and a bedside dysphagia screening process. Staff members responsible for these initial evaluations, specifically ED and intensive care unit nurses, were trained on the use of these tools, and electronic documentation templates were developed to facilitate the assessments. Comprehensive neurologic evaluation, including the essential elements of advanced stroke assessment, was also captured in standardized documentation templates for the neurology team.
The use of standardized practices and documentation templates helped the staff adhere to the requirements for the timely completion and documentation of the NIHSS to almost 100% consistently; however, it remains a challenge to consistently comply with the requirement to perform bedside dysphagia screens prior to oral intake (including medications). At the initiation of these measures, the dysphagia screen was performed for 58% of stroke patients; this rose to a fairly consistent 80% over time. Maintaining this percentage is a continual challenge that requires the SPC to work closely with the nursing staff, ED, and medicine teams.
Prior to and in the early phases of program implementation, the DVAMC effectively did not administer alteplase to patients with ischemic stroke, often because the requisite evaluations could not be completed in the required time frame. Since September of 2013, about 9 months after the program began, all 7 patients with AIS who qualified for treatment with alteplase were treated according to national guidelines. Continued work toward a goal of a < 60 minutes door-to-needle time is needed; but with notable progress, as door-to-needle time has decreased by 8% from the first alteplase administration to the most recent.
Overseen by the Simulations Department and the SPC, stroke code simulations (ie, mock stroke codes) are performed to aid in evaluating the acute stroke care process. Stroke simulation events should be an ongoing practice in any stroke program. It is an effective means to identify and address issues that may not otherwise be readily apparent.
Subacute Treatment
At DVAMC, postacute stroke care was identified as a priority. The SPC led a multidisciplinary team that was tasked with developing a postacute stroke care map, or integrated care pathway. Consistent care practices, a comprehensive tool to be used as a guide, can assist in improving outcomes, especially in a teaching facility with constantly changing medical and other clinical staff. The tool was developed using best practice guidelines from all disciplines. Staff members are encouraged to reference the pathway when caring for stroke patients, with necessary elements of care or performance measures in boldface to highlight their importance. Overall, DVAMC’s Best Care score (the percentage of patients whose care met all performance measures during the admission) rose from 57.1% to 78.6% over the course of the first year of the program.
Another key element of subacute stroke care is the provision of standardized patient stroke education. Before program initiation, stroke education at the DVAMC lacked consistency in both content and frequency. Secondary prevention should start at diagnosis, and education should be a continual process from admission to discharge. A patient booklet was developed that incorporated all required elements of stroke education per AHA guidelines: stroke risk factors, recognizing signs and symptoms, emergency activation, medications, and follow-up needs as well as other information, such as stroke pathophysiology, diet and activity, and managing lifestyle changes.7
Patient education templates were designed to facilitate documentation. Achieving this performance measure is a challenge not only for the DVAMC, but also for acute facilities nationwide. It requires involvement of the SPC as well as continual staff feedback and improvement challenges. Adherence to the patient education performance measure at the DVAMC improved from 0% meeting all 5 required elements at baseline to an average of 80% of patients.
A team of stroke champions representing each discipline involved in stroke care was recruited to be part of a postacute stroke team, led by the SPC. The team, consisting of neurologists, nurses, physical therapists, occupational therapists, speech therapists, nutritionists, social workers, and case managers, meets weekly for rounding on stroke patients, discussing patient care issues, assessing the effectiveness of the program, and addressing any system issues. This regular meeting facilitates collaboration and overall team building.
Rehabilitation and Follow-up
Routine physical, occupational, and speech therapy assessments are necessary to guide discharge planning. Although providing rehabilitation services is a priority, payer source can be a barrier to ideal rehabilitative care for DVAMC veterans. VA-based rehabilitation facilities are limited; therefore, community rehabilitation options, paid for by either VA funds or the patient’s insurance (if available), are used for the majority of stroke patients requiring these services. Efforts to increase access to stroke-specific rehabilitation options were undertaken by dedicated stroke champions at DVAMC; however, obtaining satisfactory payment agreements remains challenging.
Timely discharge is an element of care that the SPC also continually assesses. Discharge planning should begin on admission, and the SPC helps ensure that patient and caregiver needs are met and that all necessary follow-up and consultation visits have been scheduled. The LOS for stroke patients at the DVAMC had been on a steady upward trend from 6.39 days in 2005 to nearly 8 days in 2012. Over the course of 2013, the first year of the Stroke Program, stroke LOS decreased to just over 7 days (Figures 1 and 2).
Readmission rates are lower in high-risk populations when patients are seen for follow-up in the first 1 to 2 weeks postdischarge.8 Scheduling early visits can be challenging, especially in the current environment of an overburdened health care system. The DVAMC adopted the practice of Stroke Program follow-up phone calls, performed 7 to 10 days postdischarge. A standardized checklist of questions and dialogue was implemented that addressed common poststroke issues and education. Readmissions decreased from 21% in the first quarter of 2013, to 5% in the fourth quarter of 2013 after the implementation of this checklist follow-up. It is likely still too early to determine with any certainty whether the efforts aimed at improved patient education and early intervention are responsible for this decline.
Prevention and Education
Secondary prevention starts with stroke diagnosis and should include the patient and family/caregiver, when applicable. Inpatient stroke education was a priority early in the program. As the acute and postacute program developed, attention turned to community education and prevention.
Community education should emphasize early intervention. As elsewhere, the DVAMC found that the majority of patients present for care well outside the treatment window for alteplase administration. Based on national guidelines, IV alteplase must be initiated in selected patients within 4.5 hours of symptom onset. Many surveys confirm that patients are not able to accurately identify stroke symptoms or are not aware that stroke is a medical emergency. Challenges in stroke care lie in community education.9,10 The SPC met with primary care providers (PCPs) to coordinate educational and preventative efforts, recruiting them in primary and secondary prevention strategies and educating them on high-risk patients.
The SPC also collaborated with one of the outpatient clinic Patient Aligned Care Teams (PACT, or primary care team) on the development of a primary prevention program. The PACT initiated a risk reduction educational program after noting that many of their patients had suboptimal stroke risk factor management.
The project is still in the pilot stage but is showing promise regarding patient interest and participation. It is focused on addressing 4 major risk factors: hypertension, diabetes, hyperlipidemia, and tobacco use. Through a PACT report, patients were identified as having stroke risk factors that were not optimally controlled. The project aims to reduce the risk of stroke through education, goal setting, and lifestyle modification and saw a 25% rate of participation among those patients identified as candidates for the program. Of these participants, 100% completed all 4 sessions and rated the program highly favorable.
Quality Improvement Measures
Tracking performance measures should begin at program inception. “Measures improve fastest when they are being used. …Measurement and reporting with currently available data should begin immediately. …The implied message is this: since data will be impossible to ignore, we might as well make them better.”8 The VHA has a system for monitoring various quality measures, which include specific aspects of acute stroke care set forth by the VHA Stroke Directive: timely administration of alteplase, timely performance of NIHSS, and performance of a dysphagia screen prior to oral intake.
The DVAMC SPC began more comprehensive assessments of acute stroke care and evaluated elements of postacute stroke care, based on a nationally recognized set of performance measures. A system of tracking stroke performance data was initiated in the first month of the program and is based on the 10 stroke performance measures defined by the AHA and the Joint Commission. Data are currently analyzed independent of a national data management system that does not allow for national benchmarking; however, the analysis was a starting point to track facility progress and emphasized the need for consistent care. Along with collecting data on the 10 stroke-specific elements, the SPC began a system to follow duration of hospitalization, postdischarge ED visits, readmissions, and mortality rates, as well as stroke code and door-to-needle-time data. The data are shared with the DVAMC Critical Care Committee via monthly reports, program leadership via quarterly reports, facility leadership via annual reports, and facility staff through periodic e-mails and the all-employee share drive.
The first year of the program was associated with improvements in quality metrics across most areas of stroke care. Notably, 11 quality indicators that assess direct patient care measures have improved significantly from prior to program initiation in 2012 to after implementation of a comprehensive stroke care program at the conclusion of 2013. Those measures that were not already at goal of ≥ 85% achievement showed the most dramatic improvements (Figure 3).
Goals and Future Planning
The work of the DVAMC Stroke Program is far from over. Progress made is easily lost without continual monitoring and feedback. Challenges continue as well. Goals moving forward include improving door-to-needle times for IV alteplase therapy, more consistently performing swallow screens prior to oral intake, more consistently providing patient education, and increasing engagement with PCPs and the veteran community in providing stroke education and risk reduction.
A larger goal for future planning for the DVAMC is the need for a designated stroke care unit. Currently, stroke patients are admitted to the Critical Care Unit (CCU) for initial monitoring and treatment and when stable are moved to general medical wards. In some instances, this necessitates that the less acute patients occupy a CCU bed due to ward nursing limitations (ie, neuro checks every 2-hours is too great of a time demand for the ward nurses) or that the more neurologic acute patients are transferred to general medical wards when they would benefit from a more neurology-focused therapeutic environment. Stroke unit care has been associated with improved patient outcomes compared with care on general medical wards.11 The development of a designated stroke care unit is a long-range goal of the program.
Conclusion
The development of the Stroke Program, including an SPC, has improved the care of veterans with stroke at the DVAMC. The achievements of the DVAMC Stroke Program are the result of coordinated efforts of a team of dedicated health care professionals from all disciplines who sought to improve stroke care for veterans. The DVAMC continues to strive toward ever-improving outcomes, working with community partners and challenging itself to achieve a higher level of excellence. The lessons learned at the DVAMC may serve as a model for other VHA hospitals seeking to improve their stroke-related care programs.
Acknowledgements
The authors thank the executive leadership team and the chief of medicine of the DVAMC who recognized the need and potential for better stroke coordination and who have been fully supportive of the authors’ efforts to improve coordination, education, and care of their patients with strokes.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Stroke is the fifth leading cause of death in the U.S. and a leading cause of long-term disability. About 15,000 military veterans are hospitalized for acute ischemic stroke each year, and $274 million was spent for their acute, postacute, and subsequent stroke-related care over the first 6 months following the stroke.1
The Durham VAMC (DVAMC) lies within the country’s “stroke belt,” an area of 8 contiguous southeastern states, and provides care to more than 200,000 veterans living in a 26-county area of central and eastern North Carolina. The stroke mortality rates in this region are up to 40% higher than that of the national average rate.2 The DVAMC sought to transform the organization of stroke care provided to hospitalized patients as an important step in optimizing their outcomes.
Background
The VHA is committed to providing high-quality, evidence-based health care and collects data reflecting its services, including care processes and outcomes. The 2009 Office of Quality and Performance report raised concerns about the delivery of stroke care within the VHA, based on an assessment of several quality indicators. This led to the 2011 VHA directive providing policies based on national standards for the management of acute ischemic stroke (AIS) in VHA medical facilities.3
The directive defined 3 types of VHA facilities: primary stroke centers, limited-hours stroke facilities, and supporting stroke facilities. The directive further required that “all VA medical facilities with inpatient acute care medical or surgical beds have a written policy guiding appropriate care to patients with AIS in place by January 1, 2012, and implemented no later than June 1, 2012,” which included “protocols or pathways for the rapid identification, evaluation, and treatment” of patients with acute stroke and monitoring of appropriate performance indicators. For many VHA facilities caring for patients with acute stroke, including the DVAMC, the directive necessitated the development of multidisciplinary teams, organized around the provision of stroke care.
DVAMC Stroke Program
A disease-specific program typically involves the coordination of multiple care components and aims to improve continuity of care. The approach is intended to reduce care fragmentation. Through an already existing program, many elements of stroke-specific care were being delivered at the DVAMC, but several gaps and no formal system existed for coordinating stroke-related care. Programmatic goals were developed to optimize adherence to national stroke-related process measures; minimize morbidity mortality, duration of hospitalization, postdischarge emergency department (ED) visits, and readmissions; and improve continuity of care.
The Team
The DVAMC is affiliated with Duke University School of Medicine and Duke University Medical Center. The Duke University Medical Center is a Joint Commission-certified Comprehensive Stroke Center, and its director also serves as the director of the Durham VAMC Stroke Program. Because of the time and clinical expertise required to develop and oversee the program, a critical initial step was to identify a dedicated stroke program coordinator (SPC) to integrate care services and manage its implementation and ongoing activities.
The specific responsibilities of the SPC vary, depending on a facility’s needs, goals, and resources. The SPC may serve primarily as the quality measure expert and data manager, have responsibilities for program implementation and maintenance, provide training for hospital staff, and help optimize communication and integration of neurologists, internal medicine teams, other consulting and treating services, and nursing and allied health providers. The SPC also may provide direct patient care, act as a case manager, and monitor longer-term outcomes.
The DVAMC SPC is a nurse practitioner (NP). The training was thought essential given an NP’s ability to work autonomously, manage all elements of care, conceptualize, collaborate, and provide medical management skills, as has been found beneficial in many other systems of care redesign.4 The DVAMC is a teaching hospital with much of the staff affiliated with Duke University Medical School and supervised by a team of expert attending physicians. The SPC’s roles at the DVAMC have been to facilitate program development, implementation, and maintenance and collect performance data and achieve quality metric goals.
Obtaining support and cooperation from all members of the health care team is necessary for success. Finding “champions”—selected staff with an interest in improving stroke care—is crucial to a multidisciplinary team approach. These staff members were identified and recruited to serve on work groups and task forces. The SPC served as the leader and as a resource for these teams.
Key Functions
The American Stroke Association’s Policy Recommendations for the Establishment of Stroke Systems of Care suggest that a stroke system should serve 3 critical functions: communication and collaboration, standardize care customized to the population, and include performance measures with a mechanism for evaluation.5
Communication/collaboration: Collaboration in the Durham VAMC occurs through multidisciplinary work groups, including all relevant disciplines. The SPC facilitated communication and integration of care. Communication with other SPCs and accessing community resources are invaluable.
Standardized care: Stroke policies and procedures ensure that care is not only evidence-based, but also consistent. Teams worked to develop policies, protocols, order sets, documentation templates, and standardized patient education materials. The SPC identified available resources, both within the hospital, as well as within the surrounding community and professional organizations to assist in developing these tools.
Performance measures and evaluation: Performance measures and program evaluations provide a means to evaluate the progress of already implemented strategies, assist in identifying further needs, and guide future plans. The DVAMC immediately began to monitor stroke care using a standardized set of metrics, and as the program developed further, additional performance measures were added, such as length of stay (LOS), postdischarge ED visits and readmissions, and stroke code treatment time goals.
Necessary Components
To ensure its comprehensiveness, the DVAMC Stroke Program was modeled after the American Heart Association (AHA) recommendations for necessary components of a stroke system: emergency medical system (EMS) response, acute in-hospital-based treatment, subacute and secondary prevention, rehabilitation, prevention and community education, and quality improvement initiatives.5 Although intended for larger community-integrated systems, the AHA model nonetheless provides a useful framework for the development of a hospital-based stroke program.
Emergency Medical Response
The establishment of collaborative networks with community partners is essential. The DVAMC staff worked closely with the local EMS providers, facilitating community collaboration. The hospital also maintains collaborative agreements with its medical affiliates for urgent and emergent treatments. The program director and program coordinator are involved in these relationships.
Acute Stroke Treatment
The first phase of system redesign for the DVAMC in response to the 2011 VHA directive included the formulation of an acute stroke medical center memorandum (MCM), or policy, which outlined the facility’s process for acute stroke evaluation and care. The DVAMC qualified as a limited-hours stroke facility (ie, a facility with the necessary personnel, infrastructure, expertise, and programs to diagnose and treat stroke patients emergently, including the administration of alteplase to appropriate candidates, limited to normal business hours).
Related: Stroke and Preventable Hospitalization: Who Is Most at Risk?
At the start of the Stroke Program, the DVAMC had only computed tomography (CT) services during daytime working hours and relied on on-call coverage during nonbusiness hours. There had been previous discussions regarding expansion of radiology CT services; however, development of the Stroke Program led to this expansion becoming a priority. Patients with symptoms of an acute stroke who might otherwise have been a candidate for treatment with IV alteplase or patients who had other symptoms warranting an emergent brain or other CT no longer needed to be transferred to another facility. Radiology Services worked with the Stroke Program, leading to the progressive expansion of CT availability to first include longer daytime coverage and in 2014, implementation of full 24/7 CT services, allowing the hospital to become a VHA primary stroke center.
In conjunction with the MCM, a stroke code team was also implemented. A stroke code facilitates the rapid evaluation and treatment of a patient with a suspected stroke who might be a candidate for acute revascularization by the neurology and critical care staff. Durham’s stroke code team consists of a neurologist, cardiac care unit resident and RN, SPC, escort services, CT technician, bed coordinator, and chaplain services. The SPC attends all stroke codes during normal working hours, collects real-time data, and obtains retrospective data from chart audits for codes occurring when the SPC is not available. By having protocols in place, the program is organized such that the SPC need not be present to facilitate care during each stroke code.
In the early stages of program development, a stroke code process was not used in the ED and was underused in the inpatient setting, making clear documentation and evaluation of acute stroke care and treatment times difficult, if not impossible. Throughout the first 15 months of the program implementation, monthly code activation use increased by 63%. The increase in stroke code team use led to improvements in acute stroke care and accurate determination of acute stroke treatment time goals.
The efforts of both the ED and radiology teams contributed to the improvements in “door-to-CT” and “door-to-CT results” times. Door-to-CT times are expected to improve further now that the facility has implemented CT services on a 24/7 basis. Currently, average door-to-CT time is 20.6 minutes, and door-to-CT results time is 42.4 minutes, both within the National Institute of Neurological Disorders and Stroke goals of < 25 minutes and < 45 minutes respectively.6 Time tracking was part of the program’s development, as this was not previously recorded. As a result, baseline door-to-CT times were not available, and a national benchmark for comparison was used. Part of the Stroke Program’s development was putting into place a process for tracking times.
Related: Does Stroke Hit Women Harder?
Standardized methods of acute stroke evaluation were implemented early in the program development and included the use of the National Institutes of Health Stroke Scale (NIHSS) and a bedside dysphagia screening process. Staff members responsible for these initial evaluations, specifically ED and intensive care unit nurses, were trained on the use of these tools, and electronic documentation templates were developed to facilitate the assessments. Comprehensive neurologic evaluation, including the essential elements of advanced stroke assessment, was also captured in standardized documentation templates for the neurology team.
The use of standardized practices and documentation templates helped the staff adhere to the requirements for the timely completion and documentation of the NIHSS to almost 100% consistently; however, it remains a challenge to consistently comply with the requirement to perform bedside dysphagia screens prior to oral intake (including medications). At the initiation of these measures, the dysphagia screen was performed for 58% of stroke patients; this rose to a fairly consistent 80% over time. Maintaining this percentage is a continual challenge that requires the SPC to work closely with the nursing staff, ED, and medicine teams.
Prior to and in the early phases of program implementation, the DVAMC effectively did not administer alteplase to patients with ischemic stroke, often because the requisite evaluations could not be completed in the required time frame. Since September of 2013, about 9 months after the program began, all 7 patients with AIS who qualified for treatment with alteplase were treated according to national guidelines. Continued work toward a goal of a < 60 minutes door-to-needle time is needed; but with notable progress, as door-to-needle time has decreased by 8% from the first alteplase administration to the most recent.
Overseen by the Simulations Department and the SPC, stroke code simulations (ie, mock stroke codes) are performed to aid in evaluating the acute stroke care process. Stroke simulation events should be an ongoing practice in any stroke program. It is an effective means to identify and address issues that may not otherwise be readily apparent.
Subacute Treatment
At DVAMC, postacute stroke care was identified as a priority. The SPC led a multidisciplinary team that was tasked with developing a postacute stroke care map, or integrated care pathway. Consistent care practices, a comprehensive tool to be used as a guide, can assist in improving outcomes, especially in a teaching facility with constantly changing medical and other clinical staff. The tool was developed using best practice guidelines from all disciplines. Staff members are encouraged to reference the pathway when caring for stroke patients, with necessary elements of care or performance measures in boldface to highlight their importance. Overall, DVAMC’s Best Care score (the percentage of patients whose care met all performance measures during the admission) rose from 57.1% to 78.6% over the course of the first year of the program.
Another key element of subacute stroke care is the provision of standardized patient stroke education. Before program initiation, stroke education at the DVAMC lacked consistency in both content and frequency. Secondary prevention should start at diagnosis, and education should be a continual process from admission to discharge. A patient booklet was developed that incorporated all required elements of stroke education per AHA guidelines: stroke risk factors, recognizing signs and symptoms, emergency activation, medications, and follow-up needs as well as other information, such as stroke pathophysiology, diet and activity, and managing lifestyle changes.7
Patient education templates were designed to facilitate documentation. Achieving this performance measure is a challenge not only for the DVAMC, but also for acute facilities nationwide. It requires involvement of the SPC as well as continual staff feedback and improvement challenges. Adherence to the patient education performance measure at the DVAMC improved from 0% meeting all 5 required elements at baseline to an average of 80% of patients.
A team of stroke champions representing each discipline involved in stroke care was recruited to be part of a postacute stroke team, led by the SPC. The team, consisting of neurologists, nurses, physical therapists, occupational therapists, speech therapists, nutritionists, social workers, and case managers, meets weekly for rounding on stroke patients, discussing patient care issues, assessing the effectiveness of the program, and addressing any system issues. This regular meeting facilitates collaboration and overall team building.
Rehabilitation and Follow-up
Routine physical, occupational, and speech therapy assessments are necessary to guide discharge planning. Although providing rehabilitation services is a priority, payer source can be a barrier to ideal rehabilitative care for DVAMC veterans. VA-based rehabilitation facilities are limited; therefore, community rehabilitation options, paid for by either VA funds or the patient’s insurance (if available), are used for the majority of stroke patients requiring these services. Efforts to increase access to stroke-specific rehabilitation options were undertaken by dedicated stroke champions at DVAMC; however, obtaining satisfactory payment agreements remains challenging.
Timely discharge is an element of care that the SPC also continually assesses. Discharge planning should begin on admission, and the SPC helps ensure that patient and caregiver needs are met and that all necessary follow-up and consultation visits have been scheduled. The LOS for stroke patients at the DVAMC had been on a steady upward trend from 6.39 days in 2005 to nearly 8 days in 2012. Over the course of 2013, the first year of the Stroke Program, stroke LOS decreased to just over 7 days (Figures 1 and 2).
Readmission rates are lower in high-risk populations when patients are seen for follow-up in the first 1 to 2 weeks postdischarge.8 Scheduling early visits can be challenging, especially in the current environment of an overburdened health care system. The DVAMC adopted the practice of Stroke Program follow-up phone calls, performed 7 to 10 days postdischarge. A standardized checklist of questions and dialogue was implemented that addressed common poststroke issues and education. Readmissions decreased from 21% in the first quarter of 2013, to 5% in the fourth quarter of 2013 after the implementation of this checklist follow-up. It is likely still too early to determine with any certainty whether the efforts aimed at improved patient education and early intervention are responsible for this decline.
Prevention and Education
Secondary prevention starts with stroke diagnosis and should include the patient and family/caregiver, when applicable. Inpatient stroke education was a priority early in the program. As the acute and postacute program developed, attention turned to community education and prevention.
Community education should emphasize early intervention. As elsewhere, the DVAMC found that the majority of patients present for care well outside the treatment window for alteplase administration. Based on national guidelines, IV alteplase must be initiated in selected patients within 4.5 hours of symptom onset. Many surveys confirm that patients are not able to accurately identify stroke symptoms or are not aware that stroke is a medical emergency. Challenges in stroke care lie in community education.9,10 The SPC met with primary care providers (PCPs) to coordinate educational and preventative efforts, recruiting them in primary and secondary prevention strategies and educating them on high-risk patients.
The SPC also collaborated with one of the outpatient clinic Patient Aligned Care Teams (PACT, or primary care team) on the development of a primary prevention program. The PACT initiated a risk reduction educational program after noting that many of their patients had suboptimal stroke risk factor management.
The project is still in the pilot stage but is showing promise regarding patient interest and participation. It is focused on addressing 4 major risk factors: hypertension, diabetes, hyperlipidemia, and tobacco use. Through a PACT report, patients were identified as having stroke risk factors that were not optimally controlled. The project aims to reduce the risk of stroke through education, goal setting, and lifestyle modification and saw a 25% rate of participation among those patients identified as candidates for the program. Of these participants, 100% completed all 4 sessions and rated the program highly favorable.
Quality Improvement Measures
Tracking performance measures should begin at program inception. “Measures improve fastest when they are being used. …Measurement and reporting with currently available data should begin immediately. …The implied message is this: since data will be impossible to ignore, we might as well make them better.”8 The VHA has a system for monitoring various quality measures, which include specific aspects of acute stroke care set forth by the VHA Stroke Directive: timely administration of alteplase, timely performance of NIHSS, and performance of a dysphagia screen prior to oral intake.
The DVAMC SPC began more comprehensive assessments of acute stroke care and evaluated elements of postacute stroke care, based on a nationally recognized set of performance measures. A system of tracking stroke performance data was initiated in the first month of the program and is based on the 10 stroke performance measures defined by the AHA and the Joint Commission. Data are currently analyzed independent of a national data management system that does not allow for national benchmarking; however, the analysis was a starting point to track facility progress and emphasized the need for consistent care. Along with collecting data on the 10 stroke-specific elements, the SPC began a system to follow duration of hospitalization, postdischarge ED visits, readmissions, and mortality rates, as well as stroke code and door-to-needle-time data. The data are shared with the DVAMC Critical Care Committee via monthly reports, program leadership via quarterly reports, facility leadership via annual reports, and facility staff through periodic e-mails and the all-employee share drive.
The first year of the program was associated with improvements in quality metrics across most areas of stroke care. Notably, 11 quality indicators that assess direct patient care measures have improved significantly from prior to program initiation in 2012 to after implementation of a comprehensive stroke care program at the conclusion of 2013. Those measures that were not already at goal of ≥ 85% achievement showed the most dramatic improvements (Figure 3).
Goals and Future Planning
The work of the DVAMC Stroke Program is far from over. Progress made is easily lost without continual monitoring and feedback. Challenges continue as well. Goals moving forward include improving door-to-needle times for IV alteplase therapy, more consistently performing swallow screens prior to oral intake, more consistently providing patient education, and increasing engagement with PCPs and the veteran community in providing stroke education and risk reduction.
A larger goal for future planning for the DVAMC is the need for a designated stroke care unit. Currently, stroke patients are admitted to the Critical Care Unit (CCU) for initial monitoring and treatment and when stable are moved to general medical wards. In some instances, this necessitates that the less acute patients occupy a CCU bed due to ward nursing limitations (ie, neuro checks every 2-hours is too great of a time demand for the ward nurses) or that the more neurologic acute patients are transferred to general medical wards when they would benefit from a more neurology-focused therapeutic environment. Stroke unit care has been associated with improved patient outcomes compared with care on general medical wards.11 The development of a designated stroke care unit is a long-range goal of the program.
Conclusion
The development of the Stroke Program, including an SPC, has improved the care of veterans with stroke at the DVAMC. The achievements of the DVAMC Stroke Program are the result of coordinated efforts of a team of dedicated health care professionals from all disciplines who sought to improve stroke care for veterans. The DVAMC continues to strive toward ever-improving outcomes, working with community partners and challenging itself to achieve a higher level of excellence. The lessons learned at the DVAMC may serve as a model for other VHA hospitals seeking to improve their stroke-related care programs.
Acknowledgements
The authors thank the executive leadership team and the chief of medicine of the DVAMC who recognized the need and potential for better stroke coordination and who have been fully supportive of the authors’ efforts to improve coordination, education, and care of their patients with strokes.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. QUERI—Quality Enhancement Research Initiative. Stroke QUERI. QUERI Website. http://www .queri.research.va.gov/str/default.cfm. Updated/Reviewed June 19, 2014. Accessed January 22, 2015.
2. Howard G, Evans GW, Pearce K, et al. Is the stroke belt disappearing? An analysis of racial, temporal, and age effects. Stroke. 1995;26(7):1153-1158.
3. Veterans Health Administration, U.S. Department of Veterans Affairs. Treatment of Acute Ischemic Stroke (AIS). VHA Directive 2011-038. U.S. Department of Veterans Affairs Website. http://www .va.gov/vhapublications/ViewPublication.asp?pub _ID=2458. Published November 2, 2011. Accessed January 22, 2015.
4. Green T, Newcommon N. Advancing nursing practice: The role of the nurse practitioner in an acute stroke program. J Neurosci Nurs. 2006;38(4 suppl):328-330.
5. Schwamm LH, Pancioli A, Acker JE III, et al; American Stroke Association’s Task Force on the Development of Stroke Systems. Recommendations for the establishment of stroke systems of care: Recommendations from the American Stroke Association’s Task Force on the Development of Stroke Systems. Stroke. 2005;36(3):690-703.
6. Bock BF. Response system for patients presenting with acute stroke. Paper presented at: Proceedings of a National Symposium on Rapid Identification and Treatment of Acute Stroke; December 12-13, 1996; Bethesda, MD. http://www.ninds.nih.gov/news_and _events/proceedings/stroke_proceedings/bock.htm.Published. Updated May 17, 2011. Accessed January 22, 2015.
7. American Heart Association, American Stroke Association. Stroke fact sheet. American Heart Association Website. http://www.heart.org/idc/groups/heart-public/@wcm/@private/@hcm/@gwtg/documents /downloadable/ucm_310976.pdf. Published April 2014. Accessed January 22, 2015.
8. Lee TH. Care redesign—A path forward for providers. N Engl J Med. 2012;367(5):466-472.
9. Kleindorfer D, Khoury J, Broderick JP, et al. Temporal trends in public awareness of stroke: Warning signs, risk factors, and treatment. Stroke. 2009;40(7):2502-2506.
10. Jauch EC, Saver JL, Adams HP Jr, et al; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Perripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947.
11. How do stroke units improve patient outcomes? A collaborative systematic review of the randomized trials. Stroke Unit Trialists Collaboration. Stroke. 1997;28(11):2139-2144.
1. QUERI—Quality Enhancement Research Initiative. Stroke QUERI. QUERI Website. http://www .queri.research.va.gov/str/default.cfm. Updated/Reviewed June 19, 2014. Accessed January 22, 2015.
2. Howard G, Evans GW, Pearce K, et al. Is the stroke belt disappearing? An analysis of racial, temporal, and age effects. Stroke. 1995;26(7):1153-1158.
3. Veterans Health Administration, U.S. Department of Veterans Affairs. Treatment of Acute Ischemic Stroke (AIS). VHA Directive 2011-038. U.S. Department of Veterans Affairs Website. http://www .va.gov/vhapublications/ViewPublication.asp?pub _ID=2458. Published November 2, 2011. Accessed January 22, 2015.
4. Green T, Newcommon N. Advancing nursing practice: The role of the nurse practitioner in an acute stroke program. J Neurosci Nurs. 2006;38(4 suppl):328-330.
5. Schwamm LH, Pancioli A, Acker JE III, et al; American Stroke Association’s Task Force on the Development of Stroke Systems. Recommendations for the establishment of stroke systems of care: Recommendations from the American Stroke Association’s Task Force on the Development of Stroke Systems. Stroke. 2005;36(3):690-703.
6. Bock BF. Response system for patients presenting with acute stroke. Paper presented at: Proceedings of a National Symposium on Rapid Identification and Treatment of Acute Stroke; December 12-13, 1996; Bethesda, MD. http://www.ninds.nih.gov/news_and _events/proceedings/stroke_proceedings/bock.htm.Published. Updated May 17, 2011. Accessed January 22, 2015.
7. American Heart Association, American Stroke Association. Stroke fact sheet. American Heart Association Website. http://www.heart.org/idc/groups/heart-public/@wcm/@private/@hcm/@gwtg/documents /downloadable/ucm_310976.pdf. Published April 2014. Accessed January 22, 2015.
8. Lee TH. Care redesign—A path forward for providers. N Engl J Med. 2012;367(5):466-472.
9. Kleindorfer D, Khoury J, Broderick JP, et al. Temporal trends in public awareness of stroke: Warning signs, risk factors, and treatment. Stroke. 2009;40(7):2502-2506.
10. Jauch EC, Saver JL, Adams HP Jr, et al; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Perripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947.
11. How do stroke units improve patient outcomes? A collaborative systematic review of the randomized trials. Stroke Unit Trialists Collaboration. Stroke. 1997;28(11):2139-2144.