User login
Communicating Discharge Instructions
Discharge from the hospital is a vulnerable time for patients. Nearly 1 in 5 patients experiences an adverse event during this transition, with a third of these being likely preventable.1, 2 Comprehensive discharge instructions are necessary to ensure a smooth transition from hospital to home, as the responsibility for care shifts from providers to the patient and caregivers. Unfortunately, patients often go home without understanding critical information about their hospital stay, such as their discharge diagnosis or medication changes,3, 4 leaving them both dissatisfied with their discharge instructions5 and at risk for hospital readmission.
Efforts to improve discharge education have focused on increasing communication between care provider and patient. The use of designated discharge coordinators,6, 7 implementation of teach‐back techniques to assess and confirm understanding,8 and adoption of patient‐centered educational materials all offer tools to improve communication with patients. However, guidelines for communication between providers and their shared role in patient discharge education, particularly between nurses and physicians, are scarce. Daily interdisciplinary rounds9 and shared electronic health records are potential ways to foster such communication, but the methods and frequency with which providers communicate about discharge instructions with each other is poorly understood. Furthermore, despite a common set of goals for discharge instructions,10, 11 it is unclear where the responsibility to provide these elements lies: with nurses, physicians, neither, or both.
Understanding perceptions and communication practices of providers in their delivery of discharge instructions is an important first step in defining responsibilities and improving accountability for discharge education. In this study, we surveyed nurses and physicians about their discharge education practices to better understand how each group sees their own role in discharge teaching, and how these findings may generate recommendations to improve future practices.
METHODS
Setting and Subjects
University of California, San Francisco Medical Center (UCSFMC) is a 600‐bed tertiary care academic teaching hospital. We surveyed interns, hospitalists on a teaching service, and day‐shift nurses from the inpatient medical service, based on care they provided at UCSFMC from July 2010 to February 2011. The 3 groups are the primary providers at our institution who deliver discharge education. The study was approved by our Institutional Review Board (IRB), the Committee on Human Research.
Survey Development
We developed a survey tool based on a literature review and expert input from local institutional leaders in nursing, residency training, and hospital medicine. The aims of the survey tool were to: 1) assess perceptions and practice of the nurse and physician role in patient discharge education; 2) describe the current practice of physiciannurse communication at discharge; and 3) assess openness to new communication tools.
Specific elements of discharge education assessed in the survey were established from the existing literature,10, 11 and our local best practices (see Supporting Information, Text Box, in the online version of this article). Prior to survey administration, we conducted informal focus groups of interns, hospitalists, and day‐shift nurses, and piloted the survey to assure clarity in the questions and proposed responses.
The survey asked respondents to assign responsibility for the discharge education elements to the physician, nurse, both, or neither, and then to describe their current practice in patient education and in physiciannurse communication. The frequency that respondents provide discharge education to patients and the frequency of nursephysician communication around the elements of discharge education were assessed using Likert scales (1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = always). Finally, the survey asked respondents about their interest in tools to improve provider communication at discharge.
Survey Administration
Surveys were administered on paper and electronically, the latter using a commercial online survey tool. Paper surveys were circulated at nurse staff meetings on the 2 units in January and February 2011, with links to an electronic survey sent by e‐mail for those unable to attend. Electronic surveys were distributed via e‐mail to all interns and hospitalists in January 2011. The mid‐year time period was selected to ensure that all interns had provided clinical care at this hospital site. Two reminder e‐mails were sent to non‐respondents.
Data Analysis
Paper‐based surveys were subsequently entered into the online survey tool. Student t tests were used to compare Likert scale means between 2 provider groups, while analysis of variance (ANOVA) was used to compare differences between nurses, interns, and hospitalists. Chi‐squared analysis was used to compare dichotomous variables of agreement and disagreement.
Likert scales of education to patients were dichotomized into frequent education (that provided often or always) versus infrequent education (that provided never, rarely, or sometimes). Likert scales of communication between nurses were similarly dichotomized. Correlation between frequent education to patients (often or always) and the frequency of communication between nurses and physicians (often or always) was assessed using Pearson's r.
RESULTS
One hundred twenty‐nine providers responded to the survey with an overall survey response rate of 129/184 (70%). Forty‐five (64%) nurses, 56 (71%) interns, and 28 (78%) hospitalists participated. We organized the results into 4 sections based on the survey's question domains. First, we analyzed providers' (defined as nurses, interns, and hospitalists) perceived responsibility for the elements of patient discharge education (see Supporting Information, Text Box, in the online version of this article). Second, we examined how providers' responsibility compared to their reported practice. Third, we looked at the communication between nurses and physicians on the care team around these shared elements of discharge education. Lastly, we looked at providers' willingness to adopt tools to improve nursephysician communication around the time of discharge.
Perceived Responsibility for Discharge Education
Providers felt that most elements of discharge education were a shared responsibility, accounting for 58% of the responses to all the questions. Nurses, however, were the most likely to respond that the elements of discharge education were a shared responsibility, with 64% of all nursing responses indicating that the discharge education elements were a shared responsibility, compared to 54% of intern's responses and 55% of hospitalist's responses (P < 0.005). Correspondingly, nurses also responded least often that items were primarily a nursing responsibility (10% of all responses), compared to interns (12% of all responses) and hospitalists (18% of all responses) (nurses vs hospitalists, P < 0.001). No single elements were responsible for these differences, instead Table 1 demonstrates this trend across most elements. Hospitalists, despite their increased experience in discharging patients, were less likely than interns to respond that elements of discharge education were a physician's responsibility (21% vs 32% of all responses, P < 0.001).
| Nursing Responsibility (%) | Combined (%) | Physician Responsibility (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | |
| |||||||||
| Medication teaching and schedule | 33 | 29 | 33 | 55 | 58 | 52 | 0 | 0 | 0 |
| Contact information for postdischarge questions | 28 | 45 | 33 | 60 | 44 | 59 | 12 | 9 | 4 |
| Instructions for self‐care (eg, diet, activity, wound care) | 23 | 30 | 43 | 77 | 62 | 57 | 0 | 7 | 0 |
| Follow‐up appointment dates and times | 9 | 20 | 46 | 86 | 82 | 50 | 5 | 0 | 0 |
| Signs and symptoms that may develop and when to seek care (eg, call physician, 911) | 18 | 11 | 19 | 82 | 67 | 70 | 0 | 20 | 11 |
| Symptom management at home (eg, pain, SOB, nausea) | 11 | 2 | 21 | 89 | 69 | 75 | 0 | 29 | 4 |
| Home health services ordered | 5 | 9 | 21 | 79 | 65 | 54 | 14 | 22 | 0 |
| Reason for follow‐up appointments | 2 | 4 | 11 | 77 | 67 | 68 | 20 | 29 | 21 |
| Changes to medication regimen made during hospitalization | 2 | 2 | 4 | 66 | 53 | 79 | 30 | 43 | 18 |
| Discharge medical diagnoses | 0 | 0 | 0 | 60 | 56 | 61 | 40 | 45 | 39 |
| Explanation of diagnosis in lay terms | 0 | 0 | 0 | 69 | 45 | 64 | 31 | 55 | 36 |
| Summary of hospital findings and treatments (eg, CT scan results, response to antibiotics) | 0 | 0 | 0 | 18 | 11 | 18 | 82 | 88 | 71 |
| Pending results from studies during hospitalization | 0 | 2 | 0 | 12 | 27 | 29 | 88 | 66 | 68 |
The majority of providers were in agreement that 9 of the 13 elements were a shared nursephysician responsibility, with varying degrees of consensus. All groups also agreed that 2 of the elements, summary of hospital findings and pending results from studies during hospitalization, should be primarily the physician's responsibility. However, there was disagreement on the remaining 2 items. The majority of interns viewed the explanation of the diagnosis in lay terms as a physician responsibility (55%), compared to a minority of nurses (31%) and hospitalists (36%) (P < 0.05). Interns were also more likely than others to view providing contact information for questions after discharge as a uniquely nursing responsibility (45%), compared to nurses (28%) and hospitalists (33%) who viewed this as shared responsibility; this difference was not statistically significant.
Discharge Education by Providers on the Care Team
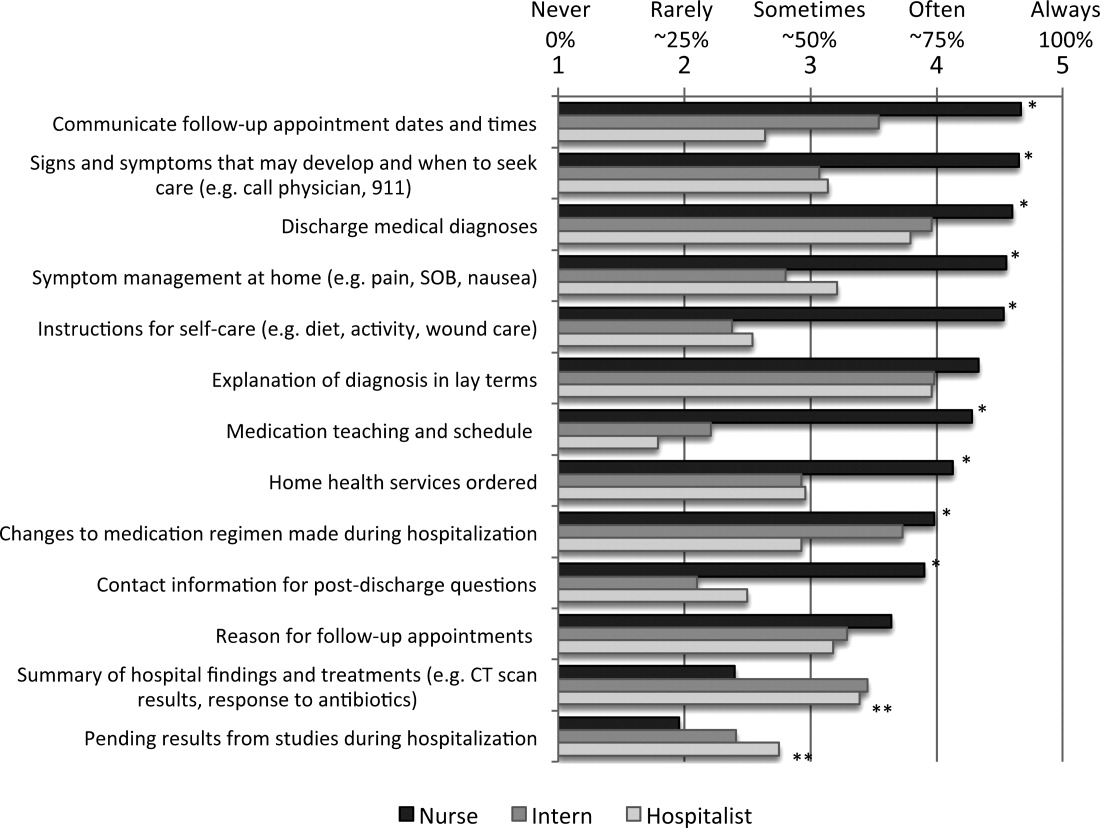
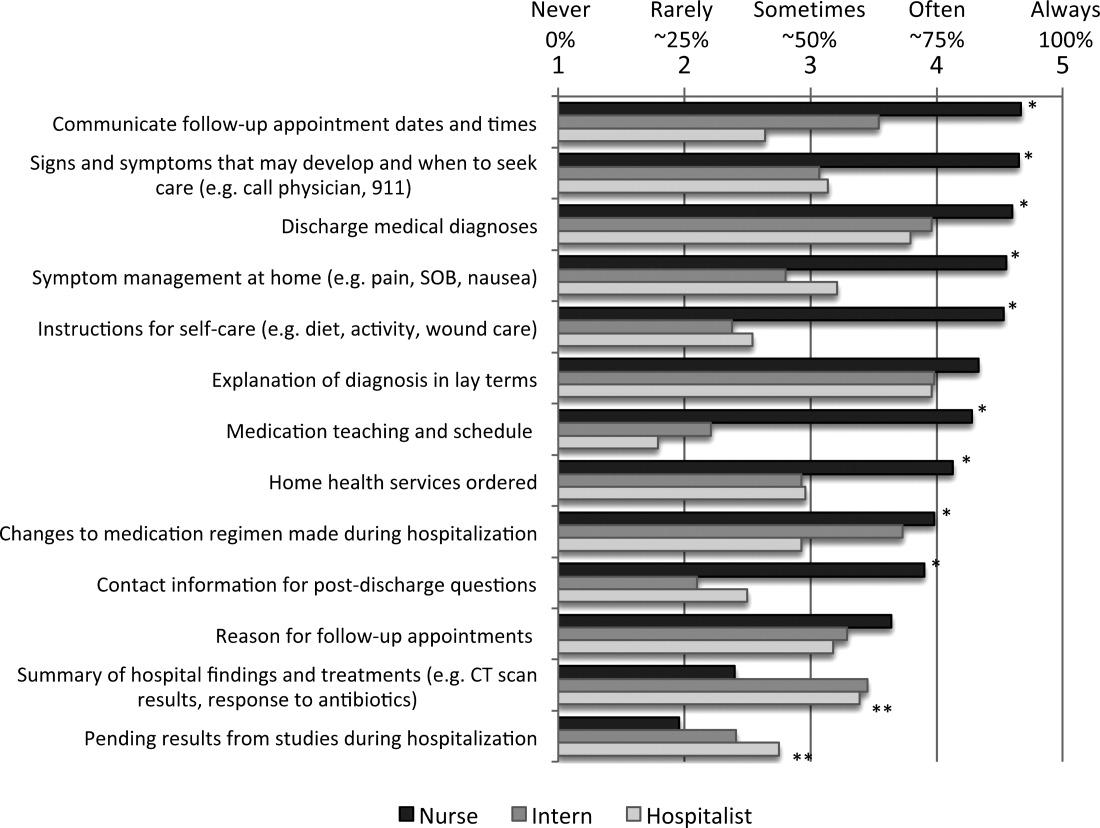
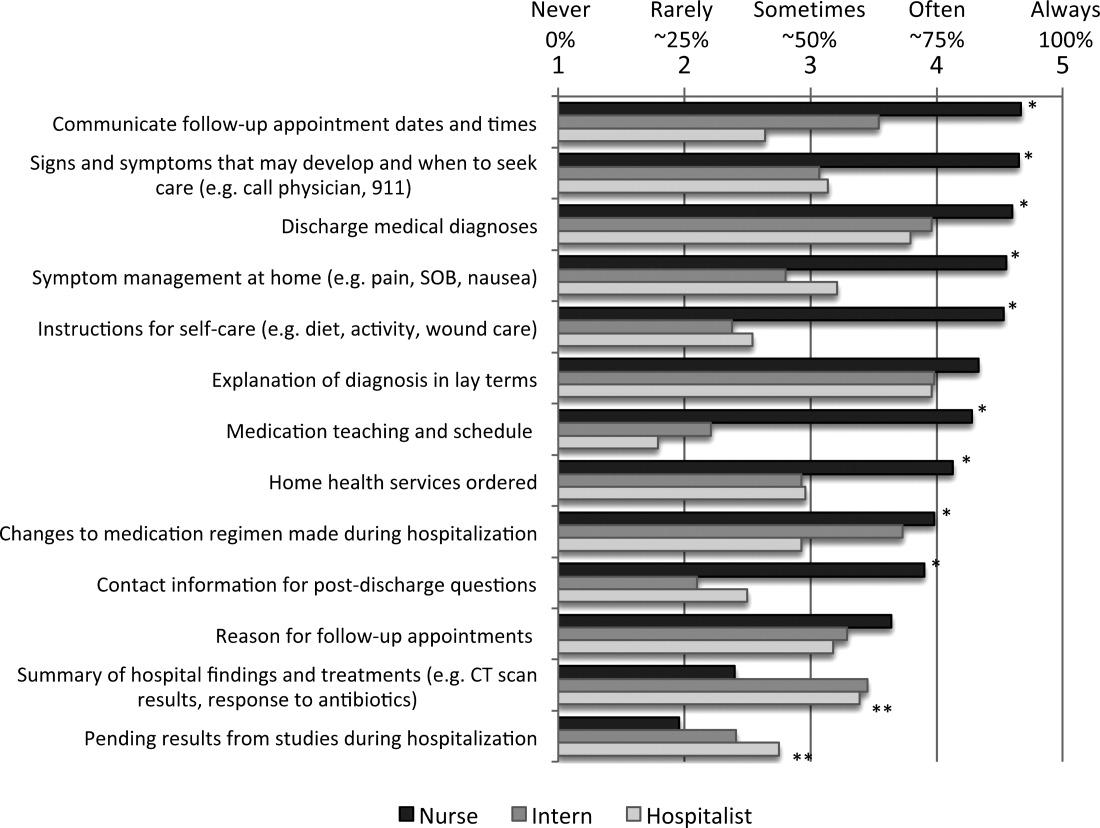
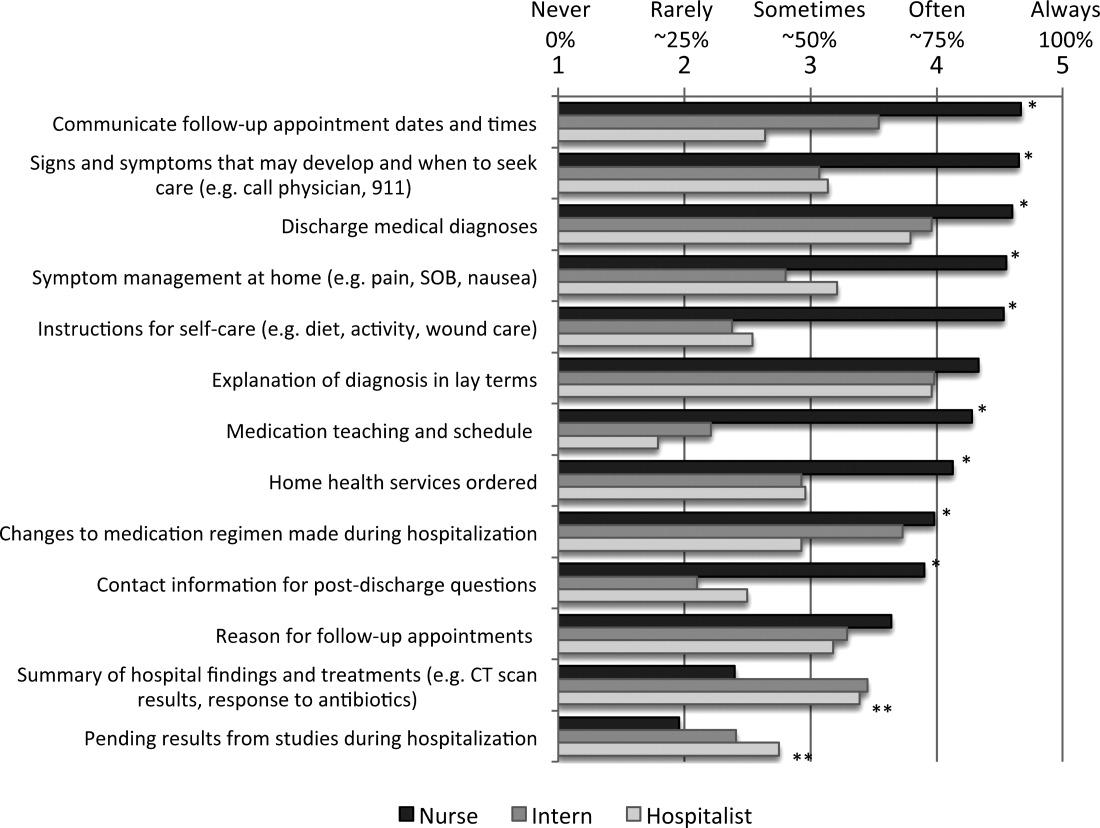
Despite nurses' reluctance to claim sole responsibility for elements of discharge education, nurses on the whole reported providing discharge education more often than either interns or hospitalists (P < 0.05). Figure 1 illustrates each group's reported practice of communicating specific discharge education on a Likert scale. For the 9 elements viewed as a shared responsibility and the 2 elements where there was disagreement, nurses reported communicating most items significantly more often than both interns and hospitalists (P < 0.001 for all elements except reason for follow‐up appointments, explanation of diagnosis in lay terms, and changes to medication regimen made during hospitalization). Items that were reported to be a physician responsibility were communicated more often by interns and hospitalists than nurses (P < 0.005), but were the items least often communicated by any care provider. Hospitalists did not report communicating any items significantly more than interns.
Communication Between Nurses and Physicians
Overall, communication between nurses and physicians was infrequent, with the 64% of nurses, 64% of interns, and 70% of hospitalists reporting that they never or rarely communicate with the other around any discharge education elements. Hospitalists were not more likely than interns to report communicating with nurses on any items, instead reported communicating with nurses around follow‐up appointments and home health services significantly less often (P < 0.05). There was a statistically significant increase in communication by all providers around items of shared responsibility, compared to items viewed as the responsibility of the physicians (14% vs 5.0% increase in communicated often or always; P < 0.001). Elements on which nurses and physicians communicated often or always were also discharge education elements reported as more often provided to patients (r = 0.577).
Potential Solutions for Sharing Discharge Information
Overall, both nurses, interns, and hospitalists were very open to proposed methods of enhancing their communication at discharge. Compared to interns and hospitalists, nurses were more likely to support communication tools, and significantly more in favor of verbal communication, discharge summary availability at the time of discharge, and access to a physician handoff tool. Only 1 solution, a standardized checklist, was favored more by interns and hospitalists, but the difference was not statistically significant. Verbal communication with the other group on the day of discharge was supported most strongly, with 100% of nurses, and 81% of interns and hospitalists reporting being likely or very likely to use this strategy. The least supported item by all groups was using white boards to communicate discharge information (Table 2).
| Likelihood of Using the Proposed Strategies | ||||
|---|---|---|---|---|
| Nurse | Intern | Hospitalist | P (ANOVA) | |
| ||||
| Verbal communication between providers on day of discharge | 4.8 | 4.2 | 4.1 | <0.001 |
| Discharge summary available at time of discharge | 4.7 | 3.8 | 4.4 | <0.001 |
| Discharge information in physician sign‐out tool | 4.3 | 3.8 | 3.2 | <0.001 |
| Nurse participation in daily physician rounds on the floor | 4.2 | 4.1 | 4.6 | 0.057 |
| Standardized checklist for discharges | 3.6 | 4.0 | 4.2 | 0.122 |
| Discharge information on white boards | 3.4 | 3.0 | 3.3 | 0.259 |
DISCUSSION
Our study demonstrated that nurses, interns, and hospitalists all feel that they play a pivotal role in discharge education. Compared to both interns and hospitalists, nurses were more likely to view discharge education as a shared responsibility, but nurses also reported providing more discharge education to patients. The elements of discharge education deemed a physician responsibility were reported as the least often provided to patients. Despite the majority of responses indicating that discharge education is a shared nursephysician responsibility, reported provider communication about discharge education was infrequent. Arguing for more communication, elements for which nurses and physicians perceived communicating more frequently were also more often reportedly conveyed to patients. The summative findings suggest that inconsistent discharge education and communication between providers may be leading to patients who are not regularly receiving complete discharge information. Nurses, interns, and hospitalists, however, were all very engaged in potential solutions to improve discharge communication, providing opportunities for immediate impact.
The question becomes where to start. Poor discharge instructions are associated with increased hospital readmission,10 and comprehensive discharge education is a suggested strategy to reduce preventable readmissions.12 Academic hospitalists, despite likely having witnessed the negative impact of poor discharge education, were not more likely than interns to report educating patients, nor did they report communicating more often with nurses. In teaching institutions, specifically, discharge education is being provided by multiple physicians: interns, residents, and hospitalists who may not have clearly defined roles in providing discharge education.13 Thus, providing comprehensive discharge instructions may require a hardwired system to ensure all elements of discharge education are addressed.
Further, our increasing dependence on technology may paradoxically necessitate more formal structures for in‐person communication, as the ability to enter discharge orders remotely leads to less frequent direct communication. Fortunately, as institutions move to computerized systems for discharge orders and instructions, there are increasing opportunities for a standardized approach to the elements of discharge education. While these results may suggest that one individual should be solely responsible for discharge education, trials using teams of nurse practitioners to facilitate transitions of care found no difference in patient length of stay or 30‐day readmission rates.14, 15
Formal systems that increase communication in high‐risk circumstances remain a focus in patient safety, and have been implemented successfully in procedural settings and with handoffs in patient care.1618 A prominent example is operating room time‐outs, which implemented a structured tool and shared process to increase nursephysician communication and reduce mortality.19 Since elements of discharge education with more frequent communication between nurses and physicians were more often conveyed to patients, our results suggest that a discharge time‐out might offer similar benefit. Fortunately, nurses and physicians rated verbal communication as the most desirable solution to share discharge education information. While not formally evaluated, one solution may be adoption of the previously described critical conversation, a structured format and a consistent time for communication that ensures both nurses and physicians understand what education needs to be provided to patients and by whom.20 The 13 discharge elements outlined in our study now provide a starting point for defining specific discussion points at discharge, delineation of who should communicate each element, and the basis for developing an operational discharge time‐out.
There are several limitations to our study. First, the survey instrument was not previously used or validated. However, we did seek formal and structured input while developing our survey, and conducted pilot testing to ensure clarity and comprehension with representatives of all study groups. Second, the 13 discharge education elements we included do not represent a comprehensive list, and were chosen based on our literature review and best practices at our institution. Third, our cross‐sectional study only captures perceptions and practices during a single time point, and may not adequately capture the greater continuum of true practice. Finally, our results may not be generalizable outside UCSFMC or other academic medical centers, particularly if other institutions have employed specific structures for discharge, such as a dedicated discharge coordinator.
CONCLUSION
Discharging patients is a complex process and one in which multiple providers and poor systems contribute to the redesign challenges. Providing high‐quality discharge education instructions to patients is an important step in making a complex process safer. Poor communication between nurses and physicians, complicated by ambiguous perceptions of responsibility for specific information, offers an opportunity for improvement efforts. We should not let well thought out treatment plans fail due to poor patient education on discharge. Our findings argue for a more systematic approach to the discharge education provided by nurses, interns, and hospitalists.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138(3):161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.Can Med Assoc J.2004;170(3):345–349.
- ,.Patients' understanding of their treatment plans and diagnosis at discharge.Mayo Clin Proc.2005;80(8):991–994.
- ,,.Functional health literacy and understanding of medications at discharge.Mayo Clin Proc.2008;83(5):554–558.
- ,,,.Patients' perception of hospital care in the United States.N Engl J Med.2008;359(18):1921–1931.
- ,,, et al.Comprehensive discharge planning and home follow‐up of hospitalized elders: a randomized clinical trial.JAMA.1999;281(7):613–620.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,, et al.Closing the loop: physician communication with diabetic patients who have low health literacy.Arch Intern Med.2003;163(1):83–90.
- ,,, et al.Structured interdisciplinary rounds in a medical teaching unit: improving patient safety.Arch Intern Med.2011;171(7):678–684.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1(6):354–360.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,,.Redefining readmission risk factors for general medicine patients.J Hosp Med.2011;6(2):54–60.
- ,,,,.“Out of sight, out of mind”: housestaff perceptions of quality‐limiting factors in discharge care at teaching hospitals.J Hosp Med.2012;7:376–381.
- ,,,,.To the hospital and back home again: a nurse practitioner‐based transitional care program for hospitalized homebound people.J Am Geriatr Soc.2011;59(3):544–551.
- ,,, et al.Improving the discharge process by embedding a discharge facilitator in a resident team.J Hosp Med.2011;6(9):494–500.
- ,,,,,.The potential for improved teamwork to reduce medical errors in the emergency department. The MedTeams Research Consortium.Ann Emerg Med.1999;34(3):373–383.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- ,,,,.Risk‐adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions.J Am Coll Surg.2007;205(6):778–784.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- ,,,,,.Critical conversations: a call for a nonprocedural “time out.”J Hosp Med.2011;6(4):225–230.
Discharge from the hospital is a vulnerable time for patients. Nearly 1 in 5 patients experiences an adverse event during this transition, with a third of these being likely preventable.1, 2 Comprehensive discharge instructions are necessary to ensure a smooth transition from hospital to home, as the responsibility for care shifts from providers to the patient and caregivers. Unfortunately, patients often go home without understanding critical information about their hospital stay, such as their discharge diagnosis or medication changes,3, 4 leaving them both dissatisfied with their discharge instructions5 and at risk for hospital readmission.
Efforts to improve discharge education have focused on increasing communication between care provider and patient. The use of designated discharge coordinators,6, 7 implementation of teach‐back techniques to assess and confirm understanding,8 and adoption of patient‐centered educational materials all offer tools to improve communication with patients. However, guidelines for communication between providers and their shared role in patient discharge education, particularly between nurses and physicians, are scarce. Daily interdisciplinary rounds9 and shared electronic health records are potential ways to foster such communication, but the methods and frequency with which providers communicate about discharge instructions with each other is poorly understood. Furthermore, despite a common set of goals for discharge instructions,10, 11 it is unclear where the responsibility to provide these elements lies: with nurses, physicians, neither, or both.
Understanding perceptions and communication practices of providers in their delivery of discharge instructions is an important first step in defining responsibilities and improving accountability for discharge education. In this study, we surveyed nurses and physicians about their discharge education practices to better understand how each group sees their own role in discharge teaching, and how these findings may generate recommendations to improve future practices.
METHODS
Setting and Subjects
University of California, San Francisco Medical Center (UCSFMC) is a 600‐bed tertiary care academic teaching hospital. We surveyed interns, hospitalists on a teaching service, and day‐shift nurses from the inpatient medical service, based on care they provided at UCSFMC from July 2010 to February 2011. The 3 groups are the primary providers at our institution who deliver discharge education. The study was approved by our Institutional Review Board (IRB), the Committee on Human Research.
Survey Development
We developed a survey tool based on a literature review and expert input from local institutional leaders in nursing, residency training, and hospital medicine. The aims of the survey tool were to: 1) assess perceptions and practice of the nurse and physician role in patient discharge education; 2) describe the current practice of physiciannurse communication at discharge; and 3) assess openness to new communication tools.
Specific elements of discharge education assessed in the survey were established from the existing literature,10, 11 and our local best practices (see Supporting Information, Text Box, in the online version of this article). Prior to survey administration, we conducted informal focus groups of interns, hospitalists, and day‐shift nurses, and piloted the survey to assure clarity in the questions and proposed responses.
The survey asked respondents to assign responsibility for the discharge education elements to the physician, nurse, both, or neither, and then to describe their current practice in patient education and in physiciannurse communication. The frequency that respondents provide discharge education to patients and the frequency of nursephysician communication around the elements of discharge education were assessed using Likert scales (1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = always). Finally, the survey asked respondents about their interest in tools to improve provider communication at discharge.
Survey Administration
Surveys were administered on paper and electronically, the latter using a commercial online survey tool. Paper surveys were circulated at nurse staff meetings on the 2 units in January and February 2011, with links to an electronic survey sent by e‐mail for those unable to attend. Electronic surveys were distributed via e‐mail to all interns and hospitalists in January 2011. The mid‐year time period was selected to ensure that all interns had provided clinical care at this hospital site. Two reminder e‐mails were sent to non‐respondents.
Data Analysis
Paper‐based surveys were subsequently entered into the online survey tool. Student t tests were used to compare Likert scale means between 2 provider groups, while analysis of variance (ANOVA) was used to compare differences between nurses, interns, and hospitalists. Chi‐squared analysis was used to compare dichotomous variables of agreement and disagreement.
Likert scales of education to patients were dichotomized into frequent education (that provided often or always) versus infrequent education (that provided never, rarely, or sometimes). Likert scales of communication between nurses were similarly dichotomized. Correlation between frequent education to patients (often or always) and the frequency of communication between nurses and physicians (often or always) was assessed using Pearson's r.
RESULTS
One hundred twenty‐nine providers responded to the survey with an overall survey response rate of 129/184 (70%). Forty‐five (64%) nurses, 56 (71%) interns, and 28 (78%) hospitalists participated. We organized the results into 4 sections based on the survey's question domains. First, we analyzed providers' (defined as nurses, interns, and hospitalists) perceived responsibility for the elements of patient discharge education (see Supporting Information, Text Box, in the online version of this article). Second, we examined how providers' responsibility compared to their reported practice. Third, we looked at the communication between nurses and physicians on the care team around these shared elements of discharge education. Lastly, we looked at providers' willingness to adopt tools to improve nursephysician communication around the time of discharge.
Perceived Responsibility for Discharge Education
Providers felt that most elements of discharge education were a shared responsibility, accounting for 58% of the responses to all the questions. Nurses, however, were the most likely to respond that the elements of discharge education were a shared responsibility, with 64% of all nursing responses indicating that the discharge education elements were a shared responsibility, compared to 54% of intern's responses and 55% of hospitalist's responses (P < 0.005). Correspondingly, nurses also responded least often that items were primarily a nursing responsibility (10% of all responses), compared to interns (12% of all responses) and hospitalists (18% of all responses) (nurses vs hospitalists, P < 0.001). No single elements were responsible for these differences, instead Table 1 demonstrates this trend across most elements. Hospitalists, despite their increased experience in discharging patients, were less likely than interns to respond that elements of discharge education were a physician's responsibility (21% vs 32% of all responses, P < 0.001).
| Nursing Responsibility (%) | Combined (%) | Physician Responsibility (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | |
| |||||||||
| Medication teaching and schedule | 33 | 29 | 33 | 55 | 58 | 52 | 0 | 0 | 0 |
| Contact information for postdischarge questions | 28 | 45 | 33 | 60 | 44 | 59 | 12 | 9 | 4 |
| Instructions for self‐care (eg, diet, activity, wound care) | 23 | 30 | 43 | 77 | 62 | 57 | 0 | 7 | 0 |
| Follow‐up appointment dates and times | 9 | 20 | 46 | 86 | 82 | 50 | 5 | 0 | 0 |
| Signs and symptoms that may develop and when to seek care (eg, call physician, 911) | 18 | 11 | 19 | 82 | 67 | 70 | 0 | 20 | 11 |
| Symptom management at home (eg, pain, SOB, nausea) | 11 | 2 | 21 | 89 | 69 | 75 | 0 | 29 | 4 |
| Home health services ordered | 5 | 9 | 21 | 79 | 65 | 54 | 14 | 22 | 0 |
| Reason for follow‐up appointments | 2 | 4 | 11 | 77 | 67 | 68 | 20 | 29 | 21 |
| Changes to medication regimen made during hospitalization | 2 | 2 | 4 | 66 | 53 | 79 | 30 | 43 | 18 |
| Discharge medical diagnoses | 0 | 0 | 0 | 60 | 56 | 61 | 40 | 45 | 39 |
| Explanation of diagnosis in lay terms | 0 | 0 | 0 | 69 | 45 | 64 | 31 | 55 | 36 |
| Summary of hospital findings and treatments (eg, CT scan results, response to antibiotics) | 0 | 0 | 0 | 18 | 11 | 18 | 82 | 88 | 71 |
| Pending results from studies during hospitalization | 0 | 2 | 0 | 12 | 27 | 29 | 88 | 66 | 68 |
The majority of providers were in agreement that 9 of the 13 elements were a shared nursephysician responsibility, with varying degrees of consensus. All groups also agreed that 2 of the elements, summary of hospital findings and pending results from studies during hospitalization, should be primarily the physician's responsibility. However, there was disagreement on the remaining 2 items. The majority of interns viewed the explanation of the diagnosis in lay terms as a physician responsibility (55%), compared to a minority of nurses (31%) and hospitalists (36%) (P < 0.05). Interns were also more likely than others to view providing contact information for questions after discharge as a uniquely nursing responsibility (45%), compared to nurses (28%) and hospitalists (33%) who viewed this as shared responsibility; this difference was not statistically significant.
Discharge Education by Providers on the Care Team
Despite nurses' reluctance to claim sole responsibility for elements of discharge education, nurses on the whole reported providing discharge education more often than either interns or hospitalists (P < 0.05). Figure 1 illustrates each group's reported practice of communicating specific discharge education on a Likert scale. For the 9 elements viewed as a shared responsibility and the 2 elements where there was disagreement, nurses reported communicating most items significantly more often than both interns and hospitalists (P < 0.001 for all elements except reason for follow‐up appointments, explanation of diagnosis in lay terms, and changes to medication regimen made during hospitalization). Items that were reported to be a physician responsibility were communicated more often by interns and hospitalists than nurses (P < 0.005), but were the items least often communicated by any care provider. Hospitalists did not report communicating any items significantly more than interns.
Communication Between Nurses and Physicians
Overall, communication between nurses and physicians was infrequent, with the 64% of nurses, 64% of interns, and 70% of hospitalists reporting that they never or rarely communicate with the other around any discharge education elements. Hospitalists were not more likely than interns to report communicating with nurses on any items, instead reported communicating with nurses around follow‐up appointments and home health services significantly less often (P < 0.05). There was a statistically significant increase in communication by all providers around items of shared responsibility, compared to items viewed as the responsibility of the physicians (14% vs 5.0% increase in communicated often or always; P < 0.001). Elements on which nurses and physicians communicated often or always were also discharge education elements reported as more often provided to patients (r = 0.577).
Potential Solutions for Sharing Discharge Information
Overall, both nurses, interns, and hospitalists were very open to proposed methods of enhancing their communication at discharge. Compared to interns and hospitalists, nurses were more likely to support communication tools, and significantly more in favor of verbal communication, discharge summary availability at the time of discharge, and access to a physician handoff tool. Only 1 solution, a standardized checklist, was favored more by interns and hospitalists, but the difference was not statistically significant. Verbal communication with the other group on the day of discharge was supported most strongly, with 100% of nurses, and 81% of interns and hospitalists reporting being likely or very likely to use this strategy. The least supported item by all groups was using white boards to communicate discharge information (Table 2).
| Likelihood of Using the Proposed Strategies | ||||
|---|---|---|---|---|
| Nurse | Intern | Hospitalist | P (ANOVA) | |
| ||||
| Verbal communication between providers on day of discharge | 4.8 | 4.2 | 4.1 | <0.001 |
| Discharge summary available at time of discharge | 4.7 | 3.8 | 4.4 | <0.001 |
| Discharge information in physician sign‐out tool | 4.3 | 3.8 | 3.2 | <0.001 |
| Nurse participation in daily physician rounds on the floor | 4.2 | 4.1 | 4.6 | 0.057 |
| Standardized checklist for discharges | 3.6 | 4.0 | 4.2 | 0.122 |
| Discharge information on white boards | 3.4 | 3.0 | 3.3 | 0.259 |
DISCUSSION
Our study demonstrated that nurses, interns, and hospitalists all feel that they play a pivotal role in discharge education. Compared to both interns and hospitalists, nurses were more likely to view discharge education as a shared responsibility, but nurses also reported providing more discharge education to patients. The elements of discharge education deemed a physician responsibility were reported as the least often provided to patients. Despite the majority of responses indicating that discharge education is a shared nursephysician responsibility, reported provider communication about discharge education was infrequent. Arguing for more communication, elements for which nurses and physicians perceived communicating more frequently were also more often reportedly conveyed to patients. The summative findings suggest that inconsistent discharge education and communication between providers may be leading to patients who are not regularly receiving complete discharge information. Nurses, interns, and hospitalists, however, were all very engaged in potential solutions to improve discharge communication, providing opportunities for immediate impact.
The question becomes where to start. Poor discharge instructions are associated with increased hospital readmission,10 and comprehensive discharge education is a suggested strategy to reduce preventable readmissions.12 Academic hospitalists, despite likely having witnessed the negative impact of poor discharge education, were not more likely than interns to report educating patients, nor did they report communicating more often with nurses. In teaching institutions, specifically, discharge education is being provided by multiple physicians: interns, residents, and hospitalists who may not have clearly defined roles in providing discharge education.13 Thus, providing comprehensive discharge instructions may require a hardwired system to ensure all elements of discharge education are addressed.
Further, our increasing dependence on technology may paradoxically necessitate more formal structures for in‐person communication, as the ability to enter discharge orders remotely leads to less frequent direct communication. Fortunately, as institutions move to computerized systems for discharge orders and instructions, there are increasing opportunities for a standardized approach to the elements of discharge education. While these results may suggest that one individual should be solely responsible for discharge education, trials using teams of nurse practitioners to facilitate transitions of care found no difference in patient length of stay or 30‐day readmission rates.14, 15
Formal systems that increase communication in high‐risk circumstances remain a focus in patient safety, and have been implemented successfully in procedural settings and with handoffs in patient care.1618 A prominent example is operating room time‐outs, which implemented a structured tool and shared process to increase nursephysician communication and reduce mortality.19 Since elements of discharge education with more frequent communication between nurses and physicians were more often conveyed to patients, our results suggest that a discharge time‐out might offer similar benefit. Fortunately, nurses and physicians rated verbal communication as the most desirable solution to share discharge education information. While not formally evaluated, one solution may be adoption of the previously described critical conversation, a structured format and a consistent time for communication that ensures both nurses and physicians understand what education needs to be provided to patients and by whom.20 The 13 discharge elements outlined in our study now provide a starting point for defining specific discussion points at discharge, delineation of who should communicate each element, and the basis for developing an operational discharge time‐out.
There are several limitations to our study. First, the survey instrument was not previously used or validated. However, we did seek formal and structured input while developing our survey, and conducted pilot testing to ensure clarity and comprehension with representatives of all study groups. Second, the 13 discharge education elements we included do not represent a comprehensive list, and were chosen based on our literature review and best practices at our institution. Third, our cross‐sectional study only captures perceptions and practices during a single time point, and may not adequately capture the greater continuum of true practice. Finally, our results may not be generalizable outside UCSFMC or other academic medical centers, particularly if other institutions have employed specific structures for discharge, such as a dedicated discharge coordinator.
CONCLUSION
Discharging patients is a complex process and one in which multiple providers and poor systems contribute to the redesign challenges. Providing high‐quality discharge education instructions to patients is an important step in making a complex process safer. Poor communication between nurses and physicians, complicated by ambiguous perceptions of responsibility for specific information, offers an opportunity for improvement efforts. We should not let well thought out treatment plans fail due to poor patient education on discharge. Our findings argue for a more systematic approach to the discharge education provided by nurses, interns, and hospitalists.
Discharge from the hospital is a vulnerable time for patients. Nearly 1 in 5 patients experiences an adverse event during this transition, with a third of these being likely preventable.1, 2 Comprehensive discharge instructions are necessary to ensure a smooth transition from hospital to home, as the responsibility for care shifts from providers to the patient and caregivers. Unfortunately, patients often go home without understanding critical information about their hospital stay, such as their discharge diagnosis or medication changes,3, 4 leaving them both dissatisfied with their discharge instructions5 and at risk for hospital readmission.
Efforts to improve discharge education have focused on increasing communication between care provider and patient. The use of designated discharge coordinators,6, 7 implementation of teach‐back techniques to assess and confirm understanding,8 and adoption of patient‐centered educational materials all offer tools to improve communication with patients. However, guidelines for communication between providers and their shared role in patient discharge education, particularly between nurses and physicians, are scarce. Daily interdisciplinary rounds9 and shared electronic health records are potential ways to foster such communication, but the methods and frequency with which providers communicate about discharge instructions with each other is poorly understood. Furthermore, despite a common set of goals for discharge instructions,10, 11 it is unclear where the responsibility to provide these elements lies: with nurses, physicians, neither, or both.
Understanding perceptions and communication practices of providers in their delivery of discharge instructions is an important first step in defining responsibilities and improving accountability for discharge education. In this study, we surveyed nurses and physicians about their discharge education practices to better understand how each group sees their own role in discharge teaching, and how these findings may generate recommendations to improve future practices.
METHODS
Setting and Subjects
University of California, San Francisco Medical Center (UCSFMC) is a 600‐bed tertiary care academic teaching hospital. We surveyed interns, hospitalists on a teaching service, and day‐shift nurses from the inpatient medical service, based on care they provided at UCSFMC from July 2010 to February 2011. The 3 groups are the primary providers at our institution who deliver discharge education. The study was approved by our Institutional Review Board (IRB), the Committee on Human Research.
Survey Development
We developed a survey tool based on a literature review and expert input from local institutional leaders in nursing, residency training, and hospital medicine. The aims of the survey tool were to: 1) assess perceptions and practice of the nurse and physician role in patient discharge education; 2) describe the current practice of physiciannurse communication at discharge; and 3) assess openness to new communication tools.
Specific elements of discharge education assessed in the survey were established from the existing literature,10, 11 and our local best practices (see Supporting Information, Text Box, in the online version of this article). Prior to survey administration, we conducted informal focus groups of interns, hospitalists, and day‐shift nurses, and piloted the survey to assure clarity in the questions and proposed responses.
The survey asked respondents to assign responsibility for the discharge education elements to the physician, nurse, both, or neither, and then to describe their current practice in patient education and in physiciannurse communication. The frequency that respondents provide discharge education to patients and the frequency of nursephysician communication around the elements of discharge education were assessed using Likert scales (1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = always). Finally, the survey asked respondents about their interest in tools to improve provider communication at discharge.
Survey Administration
Surveys were administered on paper and electronically, the latter using a commercial online survey tool. Paper surveys were circulated at nurse staff meetings on the 2 units in January and February 2011, with links to an electronic survey sent by e‐mail for those unable to attend. Electronic surveys were distributed via e‐mail to all interns and hospitalists in January 2011. The mid‐year time period was selected to ensure that all interns had provided clinical care at this hospital site. Two reminder e‐mails were sent to non‐respondents.
Data Analysis
Paper‐based surveys were subsequently entered into the online survey tool. Student t tests were used to compare Likert scale means between 2 provider groups, while analysis of variance (ANOVA) was used to compare differences between nurses, interns, and hospitalists. Chi‐squared analysis was used to compare dichotomous variables of agreement and disagreement.
Likert scales of education to patients were dichotomized into frequent education (that provided often or always) versus infrequent education (that provided never, rarely, or sometimes). Likert scales of communication between nurses were similarly dichotomized. Correlation between frequent education to patients (often or always) and the frequency of communication between nurses and physicians (often or always) was assessed using Pearson's r.
RESULTS
One hundred twenty‐nine providers responded to the survey with an overall survey response rate of 129/184 (70%). Forty‐five (64%) nurses, 56 (71%) interns, and 28 (78%) hospitalists participated. We organized the results into 4 sections based on the survey's question domains. First, we analyzed providers' (defined as nurses, interns, and hospitalists) perceived responsibility for the elements of patient discharge education (see Supporting Information, Text Box, in the online version of this article). Second, we examined how providers' responsibility compared to their reported practice. Third, we looked at the communication between nurses and physicians on the care team around these shared elements of discharge education. Lastly, we looked at providers' willingness to adopt tools to improve nursephysician communication around the time of discharge.
Perceived Responsibility for Discharge Education
Providers felt that most elements of discharge education were a shared responsibility, accounting for 58% of the responses to all the questions. Nurses, however, were the most likely to respond that the elements of discharge education were a shared responsibility, with 64% of all nursing responses indicating that the discharge education elements were a shared responsibility, compared to 54% of intern's responses and 55% of hospitalist's responses (P < 0.005). Correspondingly, nurses also responded least often that items were primarily a nursing responsibility (10% of all responses), compared to interns (12% of all responses) and hospitalists (18% of all responses) (nurses vs hospitalists, P < 0.001). No single elements were responsible for these differences, instead Table 1 demonstrates this trend across most elements. Hospitalists, despite their increased experience in discharging patients, were less likely than interns to respond that elements of discharge education were a physician's responsibility (21% vs 32% of all responses, P < 0.001).
| Nursing Responsibility (%) | Combined (%) | Physician Responsibility (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | |
| |||||||||
| Medication teaching and schedule | 33 | 29 | 33 | 55 | 58 | 52 | 0 | 0 | 0 |
| Contact information for postdischarge questions | 28 | 45 | 33 | 60 | 44 | 59 | 12 | 9 | 4 |
| Instructions for self‐care (eg, diet, activity, wound care) | 23 | 30 | 43 | 77 | 62 | 57 | 0 | 7 | 0 |
| Follow‐up appointment dates and times | 9 | 20 | 46 | 86 | 82 | 50 | 5 | 0 | 0 |
| Signs and symptoms that may develop and when to seek care (eg, call physician, 911) | 18 | 11 | 19 | 82 | 67 | 70 | 0 | 20 | 11 |
| Symptom management at home (eg, pain, SOB, nausea) | 11 | 2 | 21 | 89 | 69 | 75 | 0 | 29 | 4 |
| Home health services ordered | 5 | 9 | 21 | 79 | 65 | 54 | 14 | 22 | 0 |
| Reason for follow‐up appointments | 2 | 4 | 11 | 77 | 67 | 68 | 20 | 29 | 21 |
| Changes to medication regimen made during hospitalization | 2 | 2 | 4 | 66 | 53 | 79 | 30 | 43 | 18 |
| Discharge medical diagnoses | 0 | 0 | 0 | 60 | 56 | 61 | 40 | 45 | 39 |
| Explanation of diagnosis in lay terms | 0 | 0 | 0 | 69 | 45 | 64 | 31 | 55 | 36 |
| Summary of hospital findings and treatments (eg, CT scan results, response to antibiotics) | 0 | 0 | 0 | 18 | 11 | 18 | 82 | 88 | 71 |
| Pending results from studies during hospitalization | 0 | 2 | 0 | 12 | 27 | 29 | 88 | 66 | 68 |
The majority of providers were in agreement that 9 of the 13 elements were a shared nursephysician responsibility, with varying degrees of consensus. All groups also agreed that 2 of the elements, summary of hospital findings and pending results from studies during hospitalization, should be primarily the physician's responsibility. However, there was disagreement on the remaining 2 items. The majority of interns viewed the explanation of the diagnosis in lay terms as a physician responsibility (55%), compared to a minority of nurses (31%) and hospitalists (36%) (P < 0.05). Interns were also more likely than others to view providing contact information for questions after discharge as a uniquely nursing responsibility (45%), compared to nurses (28%) and hospitalists (33%) who viewed this as shared responsibility; this difference was not statistically significant.
Discharge Education by Providers on the Care Team
Despite nurses' reluctance to claim sole responsibility for elements of discharge education, nurses on the whole reported providing discharge education more often than either interns or hospitalists (P < 0.05). Figure 1 illustrates each group's reported practice of communicating specific discharge education on a Likert scale. For the 9 elements viewed as a shared responsibility and the 2 elements where there was disagreement, nurses reported communicating most items significantly more often than both interns and hospitalists (P < 0.001 for all elements except reason for follow‐up appointments, explanation of diagnosis in lay terms, and changes to medication regimen made during hospitalization). Items that were reported to be a physician responsibility were communicated more often by interns and hospitalists than nurses (P < 0.005), but were the items least often communicated by any care provider. Hospitalists did not report communicating any items significantly more than interns.
Communication Between Nurses and Physicians
Overall, communication between nurses and physicians was infrequent, with the 64% of nurses, 64% of interns, and 70% of hospitalists reporting that they never or rarely communicate with the other around any discharge education elements. Hospitalists were not more likely than interns to report communicating with nurses on any items, instead reported communicating with nurses around follow‐up appointments and home health services significantly less often (P < 0.05). There was a statistically significant increase in communication by all providers around items of shared responsibility, compared to items viewed as the responsibility of the physicians (14% vs 5.0% increase in communicated often or always; P < 0.001). Elements on which nurses and physicians communicated often or always were also discharge education elements reported as more often provided to patients (r = 0.577).
Potential Solutions for Sharing Discharge Information
Overall, both nurses, interns, and hospitalists were very open to proposed methods of enhancing their communication at discharge. Compared to interns and hospitalists, nurses were more likely to support communication tools, and significantly more in favor of verbal communication, discharge summary availability at the time of discharge, and access to a physician handoff tool. Only 1 solution, a standardized checklist, was favored more by interns and hospitalists, but the difference was not statistically significant. Verbal communication with the other group on the day of discharge was supported most strongly, with 100% of nurses, and 81% of interns and hospitalists reporting being likely or very likely to use this strategy. The least supported item by all groups was using white boards to communicate discharge information (Table 2).
| Likelihood of Using the Proposed Strategies | ||||
|---|---|---|---|---|
| Nurse | Intern | Hospitalist | P (ANOVA) | |
| ||||
| Verbal communication between providers on day of discharge | 4.8 | 4.2 | 4.1 | <0.001 |
| Discharge summary available at time of discharge | 4.7 | 3.8 | 4.4 | <0.001 |
| Discharge information in physician sign‐out tool | 4.3 | 3.8 | 3.2 | <0.001 |
| Nurse participation in daily physician rounds on the floor | 4.2 | 4.1 | 4.6 | 0.057 |
| Standardized checklist for discharges | 3.6 | 4.0 | 4.2 | 0.122 |
| Discharge information on white boards | 3.4 | 3.0 | 3.3 | 0.259 |
DISCUSSION
Our study demonstrated that nurses, interns, and hospitalists all feel that they play a pivotal role in discharge education. Compared to both interns and hospitalists, nurses were more likely to view discharge education as a shared responsibility, but nurses also reported providing more discharge education to patients. The elements of discharge education deemed a physician responsibility were reported as the least often provided to patients. Despite the majority of responses indicating that discharge education is a shared nursephysician responsibility, reported provider communication about discharge education was infrequent. Arguing for more communication, elements for which nurses and physicians perceived communicating more frequently were also more often reportedly conveyed to patients. The summative findings suggest that inconsistent discharge education and communication between providers may be leading to patients who are not regularly receiving complete discharge information. Nurses, interns, and hospitalists, however, were all very engaged in potential solutions to improve discharge communication, providing opportunities for immediate impact.
The question becomes where to start. Poor discharge instructions are associated with increased hospital readmission,10 and comprehensive discharge education is a suggested strategy to reduce preventable readmissions.12 Academic hospitalists, despite likely having witnessed the negative impact of poor discharge education, were not more likely than interns to report educating patients, nor did they report communicating more often with nurses. In teaching institutions, specifically, discharge education is being provided by multiple physicians: interns, residents, and hospitalists who may not have clearly defined roles in providing discharge education.13 Thus, providing comprehensive discharge instructions may require a hardwired system to ensure all elements of discharge education are addressed.
Further, our increasing dependence on technology may paradoxically necessitate more formal structures for in‐person communication, as the ability to enter discharge orders remotely leads to less frequent direct communication. Fortunately, as institutions move to computerized systems for discharge orders and instructions, there are increasing opportunities for a standardized approach to the elements of discharge education. While these results may suggest that one individual should be solely responsible for discharge education, trials using teams of nurse practitioners to facilitate transitions of care found no difference in patient length of stay or 30‐day readmission rates.14, 15
Formal systems that increase communication in high‐risk circumstances remain a focus in patient safety, and have been implemented successfully in procedural settings and with handoffs in patient care.1618 A prominent example is operating room time‐outs, which implemented a structured tool and shared process to increase nursephysician communication and reduce mortality.19 Since elements of discharge education with more frequent communication between nurses and physicians were more often conveyed to patients, our results suggest that a discharge time‐out might offer similar benefit. Fortunately, nurses and physicians rated verbal communication as the most desirable solution to share discharge education information. While not formally evaluated, one solution may be adoption of the previously described critical conversation, a structured format and a consistent time for communication that ensures both nurses and physicians understand what education needs to be provided to patients and by whom.20 The 13 discharge elements outlined in our study now provide a starting point for defining specific discussion points at discharge, delineation of who should communicate each element, and the basis for developing an operational discharge time‐out.
There are several limitations to our study. First, the survey instrument was not previously used or validated. However, we did seek formal and structured input while developing our survey, and conducted pilot testing to ensure clarity and comprehension with representatives of all study groups. Second, the 13 discharge education elements we included do not represent a comprehensive list, and were chosen based on our literature review and best practices at our institution. Third, our cross‐sectional study only captures perceptions and practices during a single time point, and may not adequately capture the greater continuum of true practice. Finally, our results may not be generalizable outside UCSFMC or other academic medical centers, particularly if other institutions have employed specific structures for discharge, such as a dedicated discharge coordinator.
CONCLUSION
Discharging patients is a complex process and one in which multiple providers and poor systems contribute to the redesign challenges. Providing high‐quality discharge education instructions to patients is an important step in making a complex process safer. Poor communication between nurses and physicians, complicated by ambiguous perceptions of responsibility for specific information, offers an opportunity for improvement efforts. We should not let well thought out treatment plans fail due to poor patient education on discharge. Our findings argue for a more systematic approach to the discharge education provided by nurses, interns, and hospitalists.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138(3):161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.Can Med Assoc J.2004;170(3):345–349.
- ,.Patients' understanding of their treatment plans and diagnosis at discharge.Mayo Clin Proc.2005;80(8):991–994.
- ,,.Functional health literacy and understanding of medications at discharge.Mayo Clin Proc.2008;83(5):554–558.
- ,,,.Patients' perception of hospital care in the United States.N Engl J Med.2008;359(18):1921–1931.
- ,,, et al.Comprehensive discharge planning and home follow‐up of hospitalized elders: a randomized clinical trial.JAMA.1999;281(7):613–620.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,, et al.Closing the loop: physician communication with diabetic patients who have low health literacy.Arch Intern Med.2003;163(1):83–90.
- ,,, et al.Structured interdisciplinary rounds in a medical teaching unit: improving patient safety.Arch Intern Med.2011;171(7):678–684.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1(6):354–360.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,,.Redefining readmission risk factors for general medicine patients.J Hosp Med.2011;6(2):54–60.
- ,,,,.“Out of sight, out of mind”: housestaff perceptions of quality‐limiting factors in discharge care at teaching hospitals.J Hosp Med.2012;7:376–381.
- ,,,,.To the hospital and back home again: a nurse practitioner‐based transitional care program for hospitalized homebound people.J Am Geriatr Soc.2011;59(3):544–551.
- ,,, et al.Improving the discharge process by embedding a discharge facilitator in a resident team.J Hosp Med.2011;6(9):494–500.
- ,,,,,.The potential for improved teamwork to reduce medical errors in the emergency department. The MedTeams Research Consortium.Ann Emerg Med.1999;34(3):373–383.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- ,,,,.Risk‐adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions.J Am Coll Surg.2007;205(6):778–784.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- ,,,,,.Critical conversations: a call for a nonprocedural “time out.”J Hosp Med.2011;6(4):225–230.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138(3):161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.Can Med Assoc J.2004;170(3):345–349.
- ,.Patients' understanding of their treatment plans and diagnosis at discharge.Mayo Clin Proc.2005;80(8):991–994.
- ,,.Functional health literacy and understanding of medications at discharge.Mayo Clin Proc.2008;83(5):554–558.
- ,,,.Patients' perception of hospital care in the United States.N Engl J Med.2008;359(18):1921–1931.
- ,,, et al.Comprehensive discharge planning and home follow‐up of hospitalized elders: a randomized clinical trial.JAMA.1999;281(7):613–620.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,, et al.Closing the loop: physician communication with diabetic patients who have low health literacy.Arch Intern Med.2003;163(1):83–90.
- ,,, et al.Structured interdisciplinary rounds in a medical teaching unit: improving patient safety.Arch Intern Med.2011;171(7):678–684.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1(6):354–360.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,,.Redefining readmission risk factors for general medicine patients.J Hosp Med.2011;6(2):54–60.
- ,,,,.“Out of sight, out of mind”: housestaff perceptions of quality‐limiting factors in discharge care at teaching hospitals.J Hosp Med.2012;7:376–381.
- ,,,,.To the hospital and back home again: a nurse practitioner‐based transitional care program for hospitalized homebound people.J Am Geriatr Soc.2011;59(3):544–551.
- ,,, et al.Improving the discharge process by embedding a discharge facilitator in a resident team.J Hosp Med.2011;6(9):494–500.
- ,,,,,.The potential for improved teamwork to reduce medical errors in the emergency department. The MedTeams Research Consortium.Ann Emerg Med.1999;34(3):373–383.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- ,,,,.Risk‐adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions.J Am Coll Surg.2007;205(6):778–784.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- ,,,,,.Critical conversations: a call for a nonprocedural “time out.”J Hosp Med.2011;6(4):225–230.
Copyright © 2012 Society of Hospital Medicine