User login
Does provider self-reporting of etiquette behaviors improve patient experience? A randomized controlled trial
Physicians have historically had limited adoption of strategies to improve patient experience and often cite suboptimal data and lack of evidence-driven strategies. 1,2 However, public reporting of hospital-level physician domain Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) experience scores, and more recent linking of payments to performance on patient experience metrics, have been associated with significant increases in physician domain scores for most of the hospitals. 3 Hospitals and healthcare organizations have deployed a broad range of strategies to engage physicians. These include emphasizing the relationship between patient experience and patient compliance, complaints, and malpractice lawsuits; appealing to physicians’ sense of competitiveness by publishing individual provider experience scores; educating physicians on HCAHPS and providing them with regularly updated data; and development of specific techniques for improving patient-physician interaction. 4-8
Studies show that educational curricula on improving etiquette and communication skills for physicians lead to improvement in patient experience, and many such training programs are available to hospitals for a significant cost.9-15 Other studies that have focused on providing timely and individual feedback to physicians using tools other than HCAHPS have shown improvement in experience in some instances. 16,17 However, these strategies are resource intensive, require the presence of an independent observer in each patient room, and may not be practical in many settings. Further, long-term sustainability may be problematic.
Since the goal of any educational intervention targeting physicians is routinizing best practices, and since resource-intensive strategies of continuous assessment and feedback may not be practical, we sought to test the impact of periodic physician self-reporting of their etiquette-based behavior on their patient experience scores.
METHODS
Subjects
Hospitalists from 4 hospitals (2 community and 2 academic) that are part of the same healthcare system were the study subjects. Hospitalists who had at least 15 unique patients responding to the routinely administered Press Ganey experience survey during the baseline period were considered eligible. Eligible hospitalists were invited to enroll in the study if their site director confirmed that the provider was likely to stay with the group for the subsequent 12-month study period.
Randomization, Intervention and Control Group
Hospitalists were randomized to the study arm or control arm (1:1 randomization). Study arm participants received biweekly etiquette behavior (EB) surveys and were asked to report how frequently they performed 7 best-practice bedside etiquette behaviors during the previous 2-week period (Table 1). These behaviors were pre-defined by a consensus group of investigators as being amenable to self-report and commonly considered best practice as described in detail below. Control-arm participants received similarly worded survey on quality improvement behaviors (QIB) that would not be expected to impact patient experience (such as reviewing medications to ensure that antithrombotic prophylaxis was prescribed, Table 1).
Baseline and Study Periods
A 12-month period prior to the enrollment of each hospitalist was considered the baseline period for that individual. Hospitalist eligibility was assessed based on number of unique patients for each hospitalist who responded to the survey during this baseline period. Once enrolled, baseline provider-level patient experience scores were calculated based on the survey responses during this 12-month baseline period. Baseline etiquette behavior performance of the study was calculated from the first survey. After the initial survey, hospitalists received biweekly surveys (EB or QIB) for the 12-month study period for a total of 26 surveys (including the initial survey).
Survey Development, Nature of Survey, Survey Distribution Methods
The EB and QIB physician self-report surveys were developed through an iterative process by the study team. The EB survey included elements from an etiquette-based medicine checklist for hospitalized patients described by Kahn et al. 18 We conducted a review of literature to identify evidence-based practices.19-22 Research team members contributed items on best practices in etiquette-based medicine from their experience. Specifically, behaviors were selected if they met the following 4 criteria: 1) performing the behavior did not lead to significant increase in workload and was relatively easy to incorporate in the work flow; 2) occurrence of the behavior would be easy to note for any outside observer or the providers themselves; 3) the practice was considered to be either an evidence-based or consensus-based best-practice; 4) there was consensus among study team members on including the item. The survey was tested for understandability by hospitalists who were not eligible for the study.
The EB survey contained 7 items related to behaviors that were expected to impact patient experience. The QIB survey contained 4 items related to behaviors that were expected to improve quality (Table 1). The initial survey also included questions about demographic characteristics of the participants.
Survey questionnaires were sent via email every 2 weeks for a period of 12 months. The survey questionnaire became available every other week, between Friday morning and Tuesday midnight, during the study period. Hospitalists received daily email reminders on each of these days with a link to the survey website if they did not complete the survey. They had the opportunity to report that they were not on service in the prior week and opt out of the survey for the specific 2-week period. The survey questions were available online as well as on a mobile device format.
Provider Level Patient Experience Scores
Provider-level patient experience scores were calculated from the physician domain Press Ganey survey items, which included the time that the physician spent with patients, the physician addressed questions/worries, the physician kept patients informed, the friendliness/courtesy of physician, and the skill of physician. Press Ganey responses were scored from 1 to 5 based on the Likert scale responses on the survey such that a response “very good” was scored 5 and a response “very poor” was scored 1. Additionally, physician domain HCAHPS item (doctors treat with courtesy/respect, doctors listen carefully, doctors explain in way patients understand) responses were utilized to calculate another set of HCAHPS provider level experience scores. The responses were scored as 1 for “always” response and “0” for any other response, consistent with CMS dichotomization of these results for public reporting. Weighted scores were calculated for individual hospitalists based on the proportion of days each hospitalist billed for the hospitalization so that experience scores of patients who were cared for by multiple providers were assigned to each provider in proportion to the percent of care delivered.23 Separate composite physician scores were generated from the 5 Press Ganey and for the 3 HCAHPS physician items. Each item was weighted equally, with the maximum possible for Press Ganey composite score of 25 (sum of the maximum possible score of 5 on each of the 5 Press Ganey items) and the HCAHPS possible total was 3 (sum of the maximum possible score of 1 on each of the 3 HCAHPS items).
ANALYSIS AND STATISTICAL METHODS
We analyzed the data to assess for changes in frequency of self-reported behavior over the study period, changes in provider-level patient experience between baseline and study period, and the association between the these 2 outcomes. The self-reported etiquette-based behavior responses were scored as 1 for the lowest response (never) to 4 as the highest (always). With 7 questions, the maximum attainable score was 28. The maximum score was normalized to 100 for ease of interpretation (corresponding to percentage of time etiquette behaviors were employed, by self-report). Similarly, the maximum attainable self-reported QIB-related behavior score on the 4 questions was 16. This was also converted to 0-100 scale for ease of comparison.
Two additional sets of analyses were performed to evaluate changes in patient experience during the study period. First, the mean 12-month provider level patient experience composite score in the baseline period was compared with the 12-month composite score during the 12-month study period for the study group and the control group. These were assessed with and without adjusting for age, sex, race, and U.S. medical school graduate (USMG) status. In the second set of unadjusted and adjusted analyses, changes in biweekly composite scores during the study period were compared between the intervention and the control groups while accounting for correlation between observations from the same physician using mixed linear models. Linear mixed models were used to accommodate correlations among multiple observations made on the same physician by including random effects within each regression model. Furthermore, these models allowed us to account for unbalanced design in our data when not all physicians had an equal number of observations and data elements were collected asynchronously.24 Analyses were performed in R version 3.2.2 (The R Project for Statistical Computing, Vienna, Austria); linear mixed models were performed using the ‘nlme’ package.25
We hypothesized that self-reporting on biweekly surveys would result in increases in the frequency of the reported behavior in each arm. We also hypothesized that, because of biweekly reflection and self-reporting on etiquette-based bedside behavior, patient experience scores would increase in the study arm.
RESULTS
Of the 80 hospitalists approached to participate in the study, 64 elected to participate (80% participation rate). The mean response rate to the survey was 57.4% for the intervention arm and 85.7% for the control arm. Higher response rates were not associated with improved patient experience scores. Of the respondents, 43.1% were younger than 35 years of age, 51.5% practiced in academic settings, and 53.1% were female. There was no statistical difference between hospitalists’ baseline composite experience scores based on gender, age, academic hospitalist status, USMG status, and English as a second language status. Similarly, there were no differences in poststudy composite experience scores based on physician characteristics.
Physicians reported high rates of etiquette-based behavior at baseline (mean score, 83.9+/-3.3), and this showed moderate improvement over the study period (5.6 % [3.9%-7.3%, P < 0.0001]). Similarly, there was a moderate increase in frequency of self-reported behavior in the control arm (6.8% [3.5%-10.1%, P < 0.0001]). Hospitalists reported on 80.7% (77.6%-83.4%) of the biweekly surveys that they “almost always” wrapped up by asking, “Do you have any other questions or concerns” or something similar. In contrast, hospitalists reported on only 27.9% (24.7%-31.3%) of the biweekly survey that they “almost always” sat down in the patient room.
The composite physician domain Press Ganey experience scores were no different for the intervention arm and the control arm during the 12-month baseline period (21.8 vs. 21.7; P = 0.90) and the 12-month intervention period (21.6 vs. 21.5; P = 0.75). Baseline self-reported behaviors were not associated with baseline experience scores. Similarly, there were no differences between the arms on composite physician domain HCAHPS experience scores during baseline (2.1 vs. 2.3; P = 0.13) and intervention periods (2.2 vs. 2.1; P = 0.33).
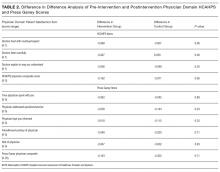
The difference in difference analysis of the baseline and postintervention composite between the intervention arm and the control arm was not statistically significant for Press Ganey composite physician experience scores (-0.163 vs. -0.322; P = 0.71) or HCAHPS composite physician scores (-0.162 vs. -0.071; P = 0.06). The results did not change when controlled for survey response rate (percentage biweekly surveys completed by the hospitalist), age, gender, USMG status, English as a second language status, or percent clinical effort. The difference in difference analysis of the individual Press Ganey and HCAHPS physician domain items that were used to calculate the composite score was also not statistically significant (Table 2).
Changes in self-reported etiquette-based behavior were not associated with any changes in composite Press Ganey and HCAHPS experience score or individual items of the composite experience scores between baseline and intervention period. Similarly, biweekly self-reported etiquette behaviors were not associated with composite and individual item experience scores derived from responses of the patients discharged during the same 2-week reporting period. The intra-class correlation between observations from the same physician was only 0.02%, suggesting that most of the variation in scores was likely due to patient factors and did not result from differences between physicians.
DISCUSSION
This 12-month randomized multicenter study of hospitalists showed that repeated self-reporting of etiquette-based behavior results in modest reported increases in performance of these behaviors. However, there was no associated increase in provider level patient experience scores at the end of the study period when compared to baseline scores of the same physicians or when compared to the scores of the control group. The study demonstrated feasibility of self-reporting of behaviors by physicians with high participation when provided modest incentives.
Educational and feedback strategies used to improve patient experience are very resource intensive. Training sessions provided at some hospitals may take hours, and sustained effects are unproved. The presence of an independent observer in patient rooms to generate feedback for providers is not scalable and sustainable outside of a research study environment.9-11,15,17,26-29 We attempted to use physician repeated self-reporting to reinforce the important and easy to adopt components of etiquette-based behavior to develop a more easily sustainable strategy. This may have failed for several reasons.
When combining “always” and “usually” responses, the physicians in our study reported a high level of etiquette behavior at baseline. If physicians believe that they are performing well at baseline, they would not consider this to be an area in need of improvement. Bigger changes in behavior may have been possible had the physicians rated themselves less favorably at baseline. Inflated or high baseline self-assessment of performance might also have led to limited success of other types of educational interventions had they been employed.
Studies published since the rollout of our study have shown that physicians significantly overestimate how frequently they perform these etiquette behaviors.30,31 It is likely that was the case in our study subjects. This may, at best, indicate that a much higher change in the level of self-reported performance would be needed to result in meaningful actual changes, or worse, may render self-reported etiquette behavior entirely unreliable. Interventions designed to improve etiquette-based behavior might need to provide feedback about performance.
A program that provides education on the importance of etiquette-based behaviors, obtains objective measures of performance of these behaviors, and offers individualized feedback may be more likely to increase the desired behaviors. This is a limitation of our study. However, we aimed to test a method that required limited resources. Additionally, our method for attributing HCAHPS scores to an individual physician, based on weighted scores that were calculated according to the proportion of days each hospitalist billed for the hospitalization, may be inaccurate. It is possible that each interaction does not contribute equally to the overall score. A team-based intervention and experience measurements could overcome this limitation.
CONCLUSION
This randomized trial demonstrated the feasibility of self-assessment of bedside etiquette behaviors by hospitalists but failed to demonstrate a meaningful impact on patient experience through self-report. These findings suggest that more intensive interventions, perhaps involving direct observation, peer-to-peer mentoring, or other techniques may be required to impact significantly physician etiquette behaviors.
Disclosure
Johns Hopkins Hospitalist Scholars Program provided funding support. Dr. Qayyum is a consultant for Sunovion. The other authors have nothing to report.
1. Blumenthal D, Kilo CM. A report card on continuous quality improvement. Milbank Q. 1998;76(4):625-648. PubMed
2. Shortell SM, Bennett CL, Byck GR. Assessing the impact of continuous quality improvement on clinical practice: What it will take to accelerate progress. Milbank Q. 1998;76(4):593-624. PubMed
3. Mann RK, Siddiqui Z, Kurbanova N, Qayyum R. Effect of HCAHPS reporting on patient satisfaction with physician communication. J Hosp Med. 2015;11(2):105-110. PubMed
4. Rivers PA, Glover SH. Health care competition, strategic mission, and patient satisfaction: research model and propositions. J Health Organ Manag. 2008;22(6):627-641. PubMed
5. Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27(3):237-251. PubMed
6. Stelfox HT, Gandhi TK, Orav EJ, Gustafson ML. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133. PubMed
7. Rodriguez HP, Rodday AM, Marshall RE, Nelson KL, Rogers WH, Safran DG. Relation of patients’ experiences with individual physicians to malpractice risk. Int J Qual Health Care. 2008;20(1):5-12. PubMed
8. Cydulka RK, Tamayo-Sarver J, Gage A, Bagnoli D. Association of patient satisfaction with complaints and risk management among emergency physicians. J Emerg Med. 2011;41(4):405-411. PubMed
9. Windover AK, Boissy A, Rice TW, Gilligan T, Velez VJ, Merlino J. The REDE model of healthcare communication: Optimizing relationship as a therapeutic agent. Journal of Patient Experience. 2014;1(1):8-13.
10. Chou CL, Hirschmann K, Fortin AH 6th, Lichstein PR. The impact of a faculty learning community on professional and personal development: the facilitator training program of the American Academy on Communication in Healthcare. Acad Med. 2014;89(7):1051-1056. PubMed
11. Kennedy M, Denise M, Fasolino M, John P, Gullen M, David J. Improving the patient experience through provider communication skills building. Patient Experience Journal. 2014;1(1):56-60.
12. Braverman AM, Kunkel EJ, Katz L, et al. Do I buy it? How AIDET™ training changes residents’ values about patient care. Journal of Patient Experience. 2015;2(1):13-20.
13. Riess H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27(10):1280-1286. PubMed
14. Rothberg MB, Steele JR, Wheeler J, Arora A, Priya A, Lindenauer PK. The relationship between time spent communicating and communication outcomes on a hospital medicine service. J Gen Internl Med. 2012;27(2):185-189. PubMed
15. O’Leary KJ, Cyrus RM. Improving patient satisfaction: timely feedback to specific physicians is essential for success. J Hosp Med. 2015;10(8):555-556. PubMed
16. Indovina K, Keniston A, Reid M, et al. Real‐time patient experience surveys of hospitalized medical patients. J Hosp Med. 2016;10(8):497-502. PubMed
17. Banka G, Edgington S, Kyulo N, et al. Improving patient satisfaction through physician education, feedback, and incentives. J Hosp Med. 2015;10(8):497-502. PubMed
18. Kahn MW. Etiquette-based medicine. N Engl J Med. 2008;358(19):1988-1989. PubMed
19. Arora V, Gangireddy S, Mehrotra A, Ginde R, Tormey M, Meltzer D. Ability of hospitalized patients to identify their in-hospital physicians. Arch Intern Med. 2009;169(2):199-201. PubMed
20. Francis JJ, Pankratz VS, Huddleston JM. Patient satisfaction associated with correct identification of physicians’ photographs. Mayo Clin Proc. 2001;76(6):604-608. PubMed
21. Strasser F, Palmer JL, Willey J, et al. Impact of physician sitting versus standing during inpatient oncology consultations: patients’ preference and perception of compassion and duration. A randomized controlled trial. J Pain Symptom Manage. 2005;29(5):489-497. PubMed
22. Dudas RA, Lemerman H, Barone M, Serwint JR. PHACES (Photographs of Academic Clinicians and Their Educational Status): a tool to improve delivery of family-centered care. Acad Pediatr. 2010;10(2):138-145. PubMed
23. Herzke C, Michtalik H, Durkin N, et al. A method for attributing patient-level metrics to rotating providers in an inpatient setting. J Hosp Med. Under revision.
24. Holden JE, Kelley K, Agarwal R. Analyzing change: a primer on multilevel models with applications to nephrology. Am J Nephrol. 2008;28(5):792-801. PubMed
25. Pinheiro J, Bates D, DebRoy S, Sarkar D. Linear and nonlinear mixed effects models. R package version. 2007;3:57.
26. Braverman AM, Kunkel EJ, Katz L, et al. Do I buy it? How AIDET™ training changes residents’ values about patient care. Journal of Patient Experience. 2015;2(1):13-20.
27. Riess H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: A randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27(10):1280-1286. PubMed
28. Raper SE, Gupta M, Okusanya O, Morris JB. Improving communication skills: A course for academic medical center surgery residents and faculty. J Surg Educ. 2015;72(6):e202-e211. PubMed
29. Indovina K, Keniston A, Reid M, et al. Real‐time patient experience surveys of hospitalized medical patients. J Hosp Med. 2016;11(4):251-256. PubMed
30. Block L, Hutzler L, Habicht R, et al. Do internal medicine interns practice etiquette‐based communication? A critical look at the inpatient encounter. J Hosp Med. 2013;8(11):631-634. PubMed
31. Tackett S, Tad-y D, Rios R, Kisuule F, Wright S. Appraising the practice of etiquette-based medicine in the inpatient setting. J Gen Intern Med. 2013;28(7):908-913. PubMed
Physicians have historically had limited adoption of strategies to improve patient experience and often cite suboptimal data and lack of evidence-driven strategies. 1,2 However, public reporting of hospital-level physician domain Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) experience scores, and more recent linking of payments to performance on patient experience metrics, have been associated with significant increases in physician domain scores for most of the hospitals. 3 Hospitals and healthcare organizations have deployed a broad range of strategies to engage physicians. These include emphasizing the relationship between patient experience and patient compliance, complaints, and malpractice lawsuits; appealing to physicians’ sense of competitiveness by publishing individual provider experience scores; educating physicians on HCAHPS and providing them with regularly updated data; and development of specific techniques for improving patient-physician interaction. 4-8
Studies show that educational curricula on improving etiquette and communication skills for physicians lead to improvement in patient experience, and many such training programs are available to hospitals for a significant cost.9-15 Other studies that have focused on providing timely and individual feedback to physicians using tools other than HCAHPS have shown improvement in experience in some instances. 16,17 However, these strategies are resource intensive, require the presence of an independent observer in each patient room, and may not be practical in many settings. Further, long-term sustainability may be problematic.
Since the goal of any educational intervention targeting physicians is routinizing best practices, and since resource-intensive strategies of continuous assessment and feedback may not be practical, we sought to test the impact of periodic physician self-reporting of their etiquette-based behavior on their patient experience scores.
METHODS
Subjects
Hospitalists from 4 hospitals (2 community and 2 academic) that are part of the same healthcare system were the study subjects. Hospitalists who had at least 15 unique patients responding to the routinely administered Press Ganey experience survey during the baseline period were considered eligible. Eligible hospitalists were invited to enroll in the study if their site director confirmed that the provider was likely to stay with the group for the subsequent 12-month study period.
Randomization, Intervention and Control Group
Hospitalists were randomized to the study arm or control arm (1:1 randomization). Study arm participants received biweekly etiquette behavior (EB) surveys and were asked to report how frequently they performed 7 best-practice bedside etiquette behaviors during the previous 2-week period (Table 1). These behaviors were pre-defined by a consensus group of investigators as being amenable to self-report and commonly considered best practice as described in detail below. Control-arm participants received similarly worded survey on quality improvement behaviors (QIB) that would not be expected to impact patient experience (such as reviewing medications to ensure that antithrombotic prophylaxis was prescribed, Table 1).
Baseline and Study Periods
A 12-month period prior to the enrollment of each hospitalist was considered the baseline period for that individual. Hospitalist eligibility was assessed based on number of unique patients for each hospitalist who responded to the survey during this baseline period. Once enrolled, baseline provider-level patient experience scores were calculated based on the survey responses during this 12-month baseline period. Baseline etiquette behavior performance of the study was calculated from the first survey. After the initial survey, hospitalists received biweekly surveys (EB or QIB) for the 12-month study period for a total of 26 surveys (including the initial survey).
Survey Development, Nature of Survey, Survey Distribution Methods
The EB and QIB physician self-report surveys were developed through an iterative process by the study team. The EB survey included elements from an etiquette-based medicine checklist for hospitalized patients described by Kahn et al. 18 We conducted a review of literature to identify evidence-based practices.19-22 Research team members contributed items on best practices in etiquette-based medicine from their experience. Specifically, behaviors were selected if they met the following 4 criteria: 1) performing the behavior did not lead to significant increase in workload and was relatively easy to incorporate in the work flow; 2) occurrence of the behavior would be easy to note for any outside observer or the providers themselves; 3) the practice was considered to be either an evidence-based or consensus-based best-practice; 4) there was consensus among study team members on including the item. The survey was tested for understandability by hospitalists who were not eligible for the study.
The EB survey contained 7 items related to behaviors that were expected to impact patient experience. The QIB survey contained 4 items related to behaviors that were expected to improve quality (Table 1). The initial survey also included questions about demographic characteristics of the participants.
Survey questionnaires were sent via email every 2 weeks for a period of 12 months. The survey questionnaire became available every other week, between Friday morning and Tuesday midnight, during the study period. Hospitalists received daily email reminders on each of these days with a link to the survey website if they did not complete the survey. They had the opportunity to report that they were not on service in the prior week and opt out of the survey for the specific 2-week period. The survey questions were available online as well as on a mobile device format.
Provider Level Patient Experience Scores
Provider-level patient experience scores were calculated from the physician domain Press Ganey survey items, which included the time that the physician spent with patients, the physician addressed questions/worries, the physician kept patients informed, the friendliness/courtesy of physician, and the skill of physician. Press Ganey responses were scored from 1 to 5 based on the Likert scale responses on the survey such that a response “very good” was scored 5 and a response “very poor” was scored 1. Additionally, physician domain HCAHPS item (doctors treat with courtesy/respect, doctors listen carefully, doctors explain in way patients understand) responses were utilized to calculate another set of HCAHPS provider level experience scores. The responses were scored as 1 for “always” response and “0” for any other response, consistent with CMS dichotomization of these results for public reporting. Weighted scores were calculated for individual hospitalists based on the proportion of days each hospitalist billed for the hospitalization so that experience scores of patients who were cared for by multiple providers were assigned to each provider in proportion to the percent of care delivered.23 Separate composite physician scores were generated from the 5 Press Ganey and for the 3 HCAHPS physician items. Each item was weighted equally, with the maximum possible for Press Ganey composite score of 25 (sum of the maximum possible score of 5 on each of the 5 Press Ganey items) and the HCAHPS possible total was 3 (sum of the maximum possible score of 1 on each of the 3 HCAHPS items).
ANALYSIS AND STATISTICAL METHODS
We analyzed the data to assess for changes in frequency of self-reported behavior over the study period, changes in provider-level patient experience between baseline and study period, and the association between the these 2 outcomes. The self-reported etiquette-based behavior responses were scored as 1 for the lowest response (never) to 4 as the highest (always). With 7 questions, the maximum attainable score was 28. The maximum score was normalized to 100 for ease of interpretation (corresponding to percentage of time etiquette behaviors were employed, by self-report). Similarly, the maximum attainable self-reported QIB-related behavior score on the 4 questions was 16. This was also converted to 0-100 scale for ease of comparison.
Two additional sets of analyses were performed to evaluate changes in patient experience during the study period. First, the mean 12-month provider level patient experience composite score in the baseline period was compared with the 12-month composite score during the 12-month study period for the study group and the control group. These were assessed with and without adjusting for age, sex, race, and U.S. medical school graduate (USMG) status. In the second set of unadjusted and adjusted analyses, changes in biweekly composite scores during the study period were compared between the intervention and the control groups while accounting for correlation between observations from the same physician using mixed linear models. Linear mixed models were used to accommodate correlations among multiple observations made on the same physician by including random effects within each regression model. Furthermore, these models allowed us to account for unbalanced design in our data when not all physicians had an equal number of observations and data elements were collected asynchronously.24 Analyses were performed in R version 3.2.2 (The R Project for Statistical Computing, Vienna, Austria); linear mixed models were performed using the ‘nlme’ package.25
We hypothesized that self-reporting on biweekly surveys would result in increases in the frequency of the reported behavior in each arm. We also hypothesized that, because of biweekly reflection and self-reporting on etiquette-based bedside behavior, patient experience scores would increase in the study arm.
RESULTS
Of the 80 hospitalists approached to participate in the study, 64 elected to participate (80% participation rate). The mean response rate to the survey was 57.4% for the intervention arm and 85.7% for the control arm. Higher response rates were not associated with improved patient experience scores. Of the respondents, 43.1% were younger than 35 years of age, 51.5% practiced in academic settings, and 53.1% were female. There was no statistical difference between hospitalists’ baseline composite experience scores based on gender, age, academic hospitalist status, USMG status, and English as a second language status. Similarly, there were no differences in poststudy composite experience scores based on physician characteristics.
Physicians reported high rates of etiquette-based behavior at baseline (mean score, 83.9+/-3.3), and this showed moderate improvement over the study period (5.6 % [3.9%-7.3%, P < 0.0001]). Similarly, there was a moderate increase in frequency of self-reported behavior in the control arm (6.8% [3.5%-10.1%, P < 0.0001]). Hospitalists reported on 80.7% (77.6%-83.4%) of the biweekly surveys that they “almost always” wrapped up by asking, “Do you have any other questions or concerns” or something similar. In contrast, hospitalists reported on only 27.9% (24.7%-31.3%) of the biweekly survey that they “almost always” sat down in the patient room.
The composite physician domain Press Ganey experience scores were no different for the intervention arm and the control arm during the 12-month baseline period (21.8 vs. 21.7; P = 0.90) and the 12-month intervention period (21.6 vs. 21.5; P = 0.75). Baseline self-reported behaviors were not associated with baseline experience scores. Similarly, there were no differences between the arms on composite physician domain HCAHPS experience scores during baseline (2.1 vs. 2.3; P = 0.13) and intervention periods (2.2 vs. 2.1; P = 0.33).
The difference in difference analysis of the baseline and postintervention composite between the intervention arm and the control arm was not statistically significant for Press Ganey composite physician experience scores (-0.163 vs. -0.322; P = 0.71) or HCAHPS composite physician scores (-0.162 vs. -0.071; P = 0.06). The results did not change when controlled for survey response rate (percentage biweekly surveys completed by the hospitalist), age, gender, USMG status, English as a second language status, or percent clinical effort. The difference in difference analysis of the individual Press Ganey and HCAHPS physician domain items that were used to calculate the composite score was also not statistically significant (Table 2).
Changes in self-reported etiquette-based behavior were not associated with any changes in composite Press Ganey and HCAHPS experience score or individual items of the composite experience scores between baseline and intervention period. Similarly, biweekly self-reported etiquette behaviors were not associated with composite and individual item experience scores derived from responses of the patients discharged during the same 2-week reporting period. The intra-class correlation between observations from the same physician was only 0.02%, suggesting that most of the variation in scores was likely due to patient factors and did not result from differences between physicians.
DISCUSSION
This 12-month randomized multicenter study of hospitalists showed that repeated self-reporting of etiquette-based behavior results in modest reported increases in performance of these behaviors. However, there was no associated increase in provider level patient experience scores at the end of the study period when compared to baseline scores of the same physicians or when compared to the scores of the control group. The study demonstrated feasibility of self-reporting of behaviors by physicians with high participation when provided modest incentives.
Educational and feedback strategies used to improve patient experience are very resource intensive. Training sessions provided at some hospitals may take hours, and sustained effects are unproved. The presence of an independent observer in patient rooms to generate feedback for providers is not scalable and sustainable outside of a research study environment.9-11,15,17,26-29 We attempted to use physician repeated self-reporting to reinforce the important and easy to adopt components of etiquette-based behavior to develop a more easily sustainable strategy. This may have failed for several reasons.
When combining “always” and “usually” responses, the physicians in our study reported a high level of etiquette behavior at baseline. If physicians believe that they are performing well at baseline, they would not consider this to be an area in need of improvement. Bigger changes in behavior may have been possible had the physicians rated themselves less favorably at baseline. Inflated or high baseline self-assessment of performance might also have led to limited success of other types of educational interventions had they been employed.
Studies published since the rollout of our study have shown that physicians significantly overestimate how frequently they perform these etiquette behaviors.30,31 It is likely that was the case in our study subjects. This may, at best, indicate that a much higher change in the level of self-reported performance would be needed to result in meaningful actual changes, or worse, may render self-reported etiquette behavior entirely unreliable. Interventions designed to improve etiquette-based behavior might need to provide feedback about performance.
A program that provides education on the importance of etiquette-based behaviors, obtains objective measures of performance of these behaviors, and offers individualized feedback may be more likely to increase the desired behaviors. This is a limitation of our study. However, we aimed to test a method that required limited resources. Additionally, our method for attributing HCAHPS scores to an individual physician, based on weighted scores that were calculated according to the proportion of days each hospitalist billed for the hospitalization, may be inaccurate. It is possible that each interaction does not contribute equally to the overall score. A team-based intervention and experience measurements could overcome this limitation.
CONCLUSION
This randomized trial demonstrated the feasibility of self-assessment of bedside etiquette behaviors by hospitalists but failed to demonstrate a meaningful impact on patient experience through self-report. These findings suggest that more intensive interventions, perhaps involving direct observation, peer-to-peer mentoring, or other techniques may be required to impact significantly physician etiquette behaviors.
Disclosure
Johns Hopkins Hospitalist Scholars Program provided funding support. Dr. Qayyum is a consultant for Sunovion. The other authors have nothing to report.
Physicians have historically had limited adoption of strategies to improve patient experience and often cite suboptimal data and lack of evidence-driven strategies. 1,2 However, public reporting of hospital-level physician domain Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) experience scores, and more recent linking of payments to performance on patient experience metrics, have been associated with significant increases in physician domain scores for most of the hospitals. 3 Hospitals and healthcare organizations have deployed a broad range of strategies to engage physicians. These include emphasizing the relationship between patient experience and patient compliance, complaints, and malpractice lawsuits; appealing to physicians’ sense of competitiveness by publishing individual provider experience scores; educating physicians on HCAHPS and providing them with regularly updated data; and development of specific techniques for improving patient-physician interaction. 4-8
Studies show that educational curricula on improving etiquette and communication skills for physicians lead to improvement in patient experience, and many such training programs are available to hospitals for a significant cost.9-15 Other studies that have focused on providing timely and individual feedback to physicians using tools other than HCAHPS have shown improvement in experience in some instances. 16,17 However, these strategies are resource intensive, require the presence of an independent observer in each patient room, and may not be practical in many settings. Further, long-term sustainability may be problematic.
Since the goal of any educational intervention targeting physicians is routinizing best practices, and since resource-intensive strategies of continuous assessment and feedback may not be practical, we sought to test the impact of periodic physician self-reporting of their etiquette-based behavior on their patient experience scores.
METHODS
Subjects
Hospitalists from 4 hospitals (2 community and 2 academic) that are part of the same healthcare system were the study subjects. Hospitalists who had at least 15 unique patients responding to the routinely administered Press Ganey experience survey during the baseline period were considered eligible. Eligible hospitalists were invited to enroll in the study if their site director confirmed that the provider was likely to stay with the group for the subsequent 12-month study period.
Randomization, Intervention and Control Group
Hospitalists were randomized to the study arm or control arm (1:1 randomization). Study arm participants received biweekly etiquette behavior (EB) surveys and were asked to report how frequently they performed 7 best-practice bedside etiquette behaviors during the previous 2-week period (Table 1). These behaviors were pre-defined by a consensus group of investigators as being amenable to self-report and commonly considered best practice as described in detail below. Control-arm participants received similarly worded survey on quality improvement behaviors (QIB) that would not be expected to impact patient experience (such as reviewing medications to ensure that antithrombotic prophylaxis was prescribed, Table 1).
Baseline and Study Periods
A 12-month period prior to the enrollment of each hospitalist was considered the baseline period for that individual. Hospitalist eligibility was assessed based on number of unique patients for each hospitalist who responded to the survey during this baseline period. Once enrolled, baseline provider-level patient experience scores were calculated based on the survey responses during this 12-month baseline period. Baseline etiquette behavior performance of the study was calculated from the first survey. After the initial survey, hospitalists received biweekly surveys (EB or QIB) for the 12-month study period for a total of 26 surveys (including the initial survey).
Survey Development, Nature of Survey, Survey Distribution Methods
The EB and QIB physician self-report surveys were developed through an iterative process by the study team. The EB survey included elements from an etiquette-based medicine checklist for hospitalized patients described by Kahn et al. 18 We conducted a review of literature to identify evidence-based practices.19-22 Research team members contributed items on best practices in etiquette-based medicine from their experience. Specifically, behaviors were selected if they met the following 4 criteria: 1) performing the behavior did not lead to significant increase in workload and was relatively easy to incorporate in the work flow; 2) occurrence of the behavior would be easy to note for any outside observer or the providers themselves; 3) the practice was considered to be either an evidence-based or consensus-based best-practice; 4) there was consensus among study team members on including the item. The survey was tested for understandability by hospitalists who were not eligible for the study.
The EB survey contained 7 items related to behaviors that were expected to impact patient experience. The QIB survey contained 4 items related to behaviors that were expected to improve quality (Table 1). The initial survey also included questions about demographic characteristics of the participants.
Survey questionnaires were sent via email every 2 weeks for a period of 12 months. The survey questionnaire became available every other week, between Friday morning and Tuesday midnight, during the study period. Hospitalists received daily email reminders on each of these days with a link to the survey website if they did not complete the survey. They had the opportunity to report that they were not on service in the prior week and opt out of the survey for the specific 2-week period. The survey questions were available online as well as on a mobile device format.
Provider Level Patient Experience Scores
Provider-level patient experience scores were calculated from the physician domain Press Ganey survey items, which included the time that the physician spent with patients, the physician addressed questions/worries, the physician kept patients informed, the friendliness/courtesy of physician, and the skill of physician. Press Ganey responses were scored from 1 to 5 based on the Likert scale responses on the survey such that a response “very good” was scored 5 and a response “very poor” was scored 1. Additionally, physician domain HCAHPS item (doctors treat with courtesy/respect, doctors listen carefully, doctors explain in way patients understand) responses were utilized to calculate another set of HCAHPS provider level experience scores. The responses were scored as 1 for “always” response and “0” for any other response, consistent with CMS dichotomization of these results for public reporting. Weighted scores were calculated for individual hospitalists based on the proportion of days each hospitalist billed for the hospitalization so that experience scores of patients who were cared for by multiple providers were assigned to each provider in proportion to the percent of care delivered.23 Separate composite physician scores were generated from the 5 Press Ganey and for the 3 HCAHPS physician items. Each item was weighted equally, with the maximum possible for Press Ganey composite score of 25 (sum of the maximum possible score of 5 on each of the 5 Press Ganey items) and the HCAHPS possible total was 3 (sum of the maximum possible score of 1 on each of the 3 HCAHPS items).
ANALYSIS AND STATISTICAL METHODS
We analyzed the data to assess for changes in frequency of self-reported behavior over the study period, changes in provider-level patient experience between baseline and study period, and the association between the these 2 outcomes. The self-reported etiquette-based behavior responses were scored as 1 for the lowest response (never) to 4 as the highest (always). With 7 questions, the maximum attainable score was 28. The maximum score was normalized to 100 for ease of interpretation (corresponding to percentage of time etiquette behaviors were employed, by self-report). Similarly, the maximum attainable self-reported QIB-related behavior score on the 4 questions was 16. This was also converted to 0-100 scale for ease of comparison.
Two additional sets of analyses were performed to evaluate changes in patient experience during the study period. First, the mean 12-month provider level patient experience composite score in the baseline period was compared with the 12-month composite score during the 12-month study period for the study group and the control group. These were assessed with and without adjusting for age, sex, race, and U.S. medical school graduate (USMG) status. In the second set of unadjusted and adjusted analyses, changes in biweekly composite scores during the study period were compared between the intervention and the control groups while accounting for correlation between observations from the same physician using mixed linear models. Linear mixed models were used to accommodate correlations among multiple observations made on the same physician by including random effects within each regression model. Furthermore, these models allowed us to account for unbalanced design in our data when not all physicians had an equal number of observations and data elements were collected asynchronously.24 Analyses were performed in R version 3.2.2 (The R Project for Statistical Computing, Vienna, Austria); linear mixed models were performed using the ‘nlme’ package.25
We hypothesized that self-reporting on biweekly surveys would result in increases in the frequency of the reported behavior in each arm. We also hypothesized that, because of biweekly reflection and self-reporting on etiquette-based bedside behavior, patient experience scores would increase in the study arm.
RESULTS
Of the 80 hospitalists approached to participate in the study, 64 elected to participate (80% participation rate). The mean response rate to the survey was 57.4% for the intervention arm and 85.7% for the control arm. Higher response rates were not associated with improved patient experience scores. Of the respondents, 43.1% were younger than 35 years of age, 51.5% practiced in academic settings, and 53.1% were female. There was no statistical difference between hospitalists’ baseline composite experience scores based on gender, age, academic hospitalist status, USMG status, and English as a second language status. Similarly, there were no differences in poststudy composite experience scores based on physician characteristics.
Physicians reported high rates of etiquette-based behavior at baseline (mean score, 83.9+/-3.3), and this showed moderate improvement over the study period (5.6 % [3.9%-7.3%, P < 0.0001]). Similarly, there was a moderate increase in frequency of self-reported behavior in the control arm (6.8% [3.5%-10.1%, P < 0.0001]). Hospitalists reported on 80.7% (77.6%-83.4%) of the biweekly surveys that they “almost always” wrapped up by asking, “Do you have any other questions or concerns” or something similar. In contrast, hospitalists reported on only 27.9% (24.7%-31.3%) of the biweekly survey that they “almost always” sat down in the patient room.
The composite physician domain Press Ganey experience scores were no different for the intervention arm and the control arm during the 12-month baseline period (21.8 vs. 21.7; P = 0.90) and the 12-month intervention period (21.6 vs. 21.5; P = 0.75). Baseline self-reported behaviors were not associated with baseline experience scores. Similarly, there were no differences between the arms on composite physician domain HCAHPS experience scores during baseline (2.1 vs. 2.3; P = 0.13) and intervention periods (2.2 vs. 2.1; P = 0.33).
The difference in difference analysis of the baseline and postintervention composite between the intervention arm and the control arm was not statistically significant for Press Ganey composite physician experience scores (-0.163 vs. -0.322; P = 0.71) or HCAHPS composite physician scores (-0.162 vs. -0.071; P = 0.06). The results did not change when controlled for survey response rate (percentage biweekly surveys completed by the hospitalist), age, gender, USMG status, English as a second language status, or percent clinical effort. The difference in difference analysis of the individual Press Ganey and HCAHPS physician domain items that were used to calculate the composite score was also not statistically significant (Table 2).
Changes in self-reported etiquette-based behavior were not associated with any changes in composite Press Ganey and HCAHPS experience score or individual items of the composite experience scores between baseline and intervention period. Similarly, biweekly self-reported etiquette behaviors were not associated with composite and individual item experience scores derived from responses of the patients discharged during the same 2-week reporting period. The intra-class correlation between observations from the same physician was only 0.02%, suggesting that most of the variation in scores was likely due to patient factors and did not result from differences between physicians.
DISCUSSION
This 12-month randomized multicenter study of hospitalists showed that repeated self-reporting of etiquette-based behavior results in modest reported increases in performance of these behaviors. However, there was no associated increase in provider level patient experience scores at the end of the study period when compared to baseline scores of the same physicians or when compared to the scores of the control group. The study demonstrated feasibility of self-reporting of behaviors by physicians with high participation when provided modest incentives.
Educational and feedback strategies used to improve patient experience are very resource intensive. Training sessions provided at some hospitals may take hours, and sustained effects are unproved. The presence of an independent observer in patient rooms to generate feedback for providers is not scalable and sustainable outside of a research study environment.9-11,15,17,26-29 We attempted to use physician repeated self-reporting to reinforce the important and easy to adopt components of etiquette-based behavior to develop a more easily sustainable strategy. This may have failed for several reasons.
When combining “always” and “usually” responses, the physicians in our study reported a high level of etiquette behavior at baseline. If physicians believe that they are performing well at baseline, they would not consider this to be an area in need of improvement. Bigger changes in behavior may have been possible had the physicians rated themselves less favorably at baseline. Inflated or high baseline self-assessment of performance might also have led to limited success of other types of educational interventions had they been employed.
Studies published since the rollout of our study have shown that physicians significantly overestimate how frequently they perform these etiquette behaviors.30,31 It is likely that was the case in our study subjects. This may, at best, indicate that a much higher change in the level of self-reported performance would be needed to result in meaningful actual changes, or worse, may render self-reported etiquette behavior entirely unreliable. Interventions designed to improve etiquette-based behavior might need to provide feedback about performance.
A program that provides education on the importance of etiquette-based behaviors, obtains objective measures of performance of these behaviors, and offers individualized feedback may be more likely to increase the desired behaviors. This is a limitation of our study. However, we aimed to test a method that required limited resources. Additionally, our method for attributing HCAHPS scores to an individual physician, based on weighted scores that were calculated according to the proportion of days each hospitalist billed for the hospitalization, may be inaccurate. It is possible that each interaction does not contribute equally to the overall score. A team-based intervention and experience measurements could overcome this limitation.
CONCLUSION
This randomized trial demonstrated the feasibility of self-assessment of bedside etiquette behaviors by hospitalists but failed to demonstrate a meaningful impact on patient experience through self-report. These findings suggest that more intensive interventions, perhaps involving direct observation, peer-to-peer mentoring, or other techniques may be required to impact significantly physician etiquette behaviors.
Disclosure
Johns Hopkins Hospitalist Scholars Program provided funding support. Dr. Qayyum is a consultant for Sunovion. The other authors have nothing to report.
1. Blumenthal D, Kilo CM. A report card on continuous quality improvement. Milbank Q. 1998;76(4):625-648. PubMed
2. Shortell SM, Bennett CL, Byck GR. Assessing the impact of continuous quality improvement on clinical practice: What it will take to accelerate progress. Milbank Q. 1998;76(4):593-624. PubMed
3. Mann RK, Siddiqui Z, Kurbanova N, Qayyum R. Effect of HCAHPS reporting on patient satisfaction with physician communication. J Hosp Med. 2015;11(2):105-110. PubMed
4. Rivers PA, Glover SH. Health care competition, strategic mission, and patient satisfaction: research model and propositions. J Health Organ Manag. 2008;22(6):627-641. PubMed
5. Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27(3):237-251. PubMed
6. Stelfox HT, Gandhi TK, Orav EJ, Gustafson ML. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133. PubMed
7. Rodriguez HP, Rodday AM, Marshall RE, Nelson KL, Rogers WH, Safran DG. Relation of patients’ experiences with individual physicians to malpractice risk. Int J Qual Health Care. 2008;20(1):5-12. PubMed
8. Cydulka RK, Tamayo-Sarver J, Gage A, Bagnoli D. Association of patient satisfaction with complaints and risk management among emergency physicians. J Emerg Med. 2011;41(4):405-411. PubMed
9. Windover AK, Boissy A, Rice TW, Gilligan T, Velez VJ, Merlino J. The REDE model of healthcare communication: Optimizing relationship as a therapeutic agent. Journal of Patient Experience. 2014;1(1):8-13.
10. Chou CL, Hirschmann K, Fortin AH 6th, Lichstein PR. The impact of a faculty learning community on professional and personal development: the facilitator training program of the American Academy on Communication in Healthcare. Acad Med. 2014;89(7):1051-1056. PubMed
11. Kennedy M, Denise M, Fasolino M, John P, Gullen M, David J. Improving the patient experience through provider communication skills building. Patient Experience Journal. 2014;1(1):56-60.
12. Braverman AM, Kunkel EJ, Katz L, et al. Do I buy it? How AIDET™ training changes residents’ values about patient care. Journal of Patient Experience. 2015;2(1):13-20.
13. Riess H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27(10):1280-1286. PubMed
14. Rothberg MB, Steele JR, Wheeler J, Arora A, Priya A, Lindenauer PK. The relationship between time spent communicating and communication outcomes on a hospital medicine service. J Gen Internl Med. 2012;27(2):185-189. PubMed
15. O’Leary KJ, Cyrus RM. Improving patient satisfaction: timely feedback to specific physicians is essential for success. J Hosp Med. 2015;10(8):555-556. PubMed
16. Indovina K, Keniston A, Reid M, et al. Real‐time patient experience surveys of hospitalized medical patients. J Hosp Med. 2016;10(8):497-502. PubMed
17. Banka G, Edgington S, Kyulo N, et al. Improving patient satisfaction through physician education, feedback, and incentives. J Hosp Med. 2015;10(8):497-502. PubMed
18. Kahn MW. Etiquette-based medicine. N Engl J Med. 2008;358(19):1988-1989. PubMed
19. Arora V, Gangireddy S, Mehrotra A, Ginde R, Tormey M, Meltzer D. Ability of hospitalized patients to identify their in-hospital physicians. Arch Intern Med. 2009;169(2):199-201. PubMed
20. Francis JJ, Pankratz VS, Huddleston JM. Patient satisfaction associated with correct identification of physicians’ photographs. Mayo Clin Proc. 2001;76(6):604-608. PubMed
21. Strasser F, Palmer JL, Willey J, et al. Impact of physician sitting versus standing during inpatient oncology consultations: patients’ preference and perception of compassion and duration. A randomized controlled trial. J Pain Symptom Manage. 2005;29(5):489-497. PubMed
22. Dudas RA, Lemerman H, Barone M, Serwint JR. PHACES (Photographs of Academic Clinicians and Their Educational Status): a tool to improve delivery of family-centered care. Acad Pediatr. 2010;10(2):138-145. PubMed
23. Herzke C, Michtalik H, Durkin N, et al. A method for attributing patient-level metrics to rotating providers in an inpatient setting. J Hosp Med. Under revision.
24. Holden JE, Kelley K, Agarwal R. Analyzing change: a primer on multilevel models with applications to nephrology. Am J Nephrol. 2008;28(5):792-801. PubMed
25. Pinheiro J, Bates D, DebRoy S, Sarkar D. Linear and nonlinear mixed effects models. R package version. 2007;3:57.
26. Braverman AM, Kunkel EJ, Katz L, et al. Do I buy it? How AIDET™ training changes residents’ values about patient care. Journal of Patient Experience. 2015;2(1):13-20.
27. Riess H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: A randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27(10):1280-1286. PubMed
28. Raper SE, Gupta M, Okusanya O, Morris JB. Improving communication skills: A course for academic medical center surgery residents and faculty. J Surg Educ. 2015;72(6):e202-e211. PubMed
29. Indovina K, Keniston A, Reid M, et al. Real‐time patient experience surveys of hospitalized medical patients. J Hosp Med. 2016;11(4):251-256. PubMed
30. Block L, Hutzler L, Habicht R, et al. Do internal medicine interns practice etiquette‐based communication? A critical look at the inpatient encounter. J Hosp Med. 2013;8(11):631-634. PubMed
31. Tackett S, Tad-y D, Rios R, Kisuule F, Wright S. Appraising the practice of etiquette-based medicine in the inpatient setting. J Gen Intern Med. 2013;28(7):908-913. PubMed
1. Blumenthal D, Kilo CM. A report card on continuous quality improvement. Milbank Q. 1998;76(4):625-648. PubMed
2. Shortell SM, Bennett CL, Byck GR. Assessing the impact of continuous quality improvement on clinical practice: What it will take to accelerate progress. Milbank Q. 1998;76(4):593-624. PubMed
3. Mann RK, Siddiqui Z, Kurbanova N, Qayyum R. Effect of HCAHPS reporting on patient satisfaction with physician communication. J Hosp Med. 2015;11(2):105-110. PubMed
4. Rivers PA, Glover SH. Health care competition, strategic mission, and patient satisfaction: research model and propositions. J Health Organ Manag. 2008;22(6):627-641. PubMed
5. Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27(3):237-251. PubMed
6. Stelfox HT, Gandhi TK, Orav EJ, Gustafson ML. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133. PubMed
7. Rodriguez HP, Rodday AM, Marshall RE, Nelson KL, Rogers WH, Safran DG. Relation of patients’ experiences with individual physicians to malpractice risk. Int J Qual Health Care. 2008;20(1):5-12. PubMed
8. Cydulka RK, Tamayo-Sarver J, Gage A, Bagnoli D. Association of patient satisfaction with complaints and risk management among emergency physicians. J Emerg Med. 2011;41(4):405-411. PubMed
9. Windover AK, Boissy A, Rice TW, Gilligan T, Velez VJ, Merlino J. The REDE model of healthcare communication: Optimizing relationship as a therapeutic agent. Journal of Patient Experience. 2014;1(1):8-13.
10. Chou CL, Hirschmann K, Fortin AH 6th, Lichstein PR. The impact of a faculty learning community on professional and personal development: the facilitator training program of the American Academy on Communication in Healthcare. Acad Med. 2014;89(7):1051-1056. PubMed
11. Kennedy M, Denise M, Fasolino M, John P, Gullen M, David J. Improving the patient experience through provider communication skills building. Patient Experience Journal. 2014;1(1):56-60.
12. Braverman AM, Kunkel EJ, Katz L, et al. Do I buy it? How AIDET™ training changes residents’ values about patient care. Journal of Patient Experience. 2015;2(1):13-20.
13. Riess H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27(10):1280-1286. PubMed
14. Rothberg MB, Steele JR, Wheeler J, Arora A, Priya A, Lindenauer PK. The relationship between time spent communicating and communication outcomes on a hospital medicine service. J Gen Internl Med. 2012;27(2):185-189. PubMed
15. O’Leary KJ, Cyrus RM. Improving patient satisfaction: timely feedback to specific physicians is essential for success. J Hosp Med. 2015;10(8):555-556. PubMed
16. Indovina K, Keniston A, Reid M, et al. Real‐time patient experience surveys of hospitalized medical patients. J Hosp Med. 2016;10(8):497-502. PubMed
17. Banka G, Edgington S, Kyulo N, et al. Improving patient satisfaction through physician education, feedback, and incentives. J Hosp Med. 2015;10(8):497-502. PubMed
18. Kahn MW. Etiquette-based medicine. N Engl J Med. 2008;358(19):1988-1989. PubMed
19. Arora V, Gangireddy S, Mehrotra A, Ginde R, Tormey M, Meltzer D. Ability of hospitalized patients to identify their in-hospital physicians. Arch Intern Med. 2009;169(2):199-201. PubMed
20. Francis JJ, Pankratz VS, Huddleston JM. Patient satisfaction associated with correct identification of physicians’ photographs. Mayo Clin Proc. 2001;76(6):604-608. PubMed
21. Strasser F, Palmer JL, Willey J, et al. Impact of physician sitting versus standing during inpatient oncology consultations: patients’ preference and perception of compassion and duration. A randomized controlled trial. J Pain Symptom Manage. 2005;29(5):489-497. PubMed
22. Dudas RA, Lemerman H, Barone M, Serwint JR. PHACES (Photographs of Academic Clinicians and Their Educational Status): a tool to improve delivery of family-centered care. Acad Pediatr. 2010;10(2):138-145. PubMed
23. Herzke C, Michtalik H, Durkin N, et al. A method for attributing patient-level metrics to rotating providers in an inpatient setting. J Hosp Med. Under revision.
24. Holden JE, Kelley K, Agarwal R. Analyzing change: a primer on multilevel models with applications to nephrology. Am J Nephrol. 2008;28(5):792-801. PubMed
25. Pinheiro J, Bates D, DebRoy S, Sarkar D. Linear and nonlinear mixed effects models. R package version. 2007;3:57.
26. Braverman AM, Kunkel EJ, Katz L, et al. Do I buy it? How AIDET™ training changes residents’ values about patient care. Journal of Patient Experience. 2015;2(1):13-20.
27. Riess H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: A randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27(10):1280-1286. PubMed
28. Raper SE, Gupta M, Okusanya O, Morris JB. Improving communication skills: A course for academic medical center surgery residents and faculty. J Surg Educ. 2015;72(6):e202-e211. PubMed
29. Indovina K, Keniston A, Reid M, et al. Real‐time patient experience surveys of hospitalized medical patients. J Hosp Med. 2016;11(4):251-256. PubMed
30. Block L, Hutzler L, Habicht R, et al. Do internal medicine interns practice etiquette‐based communication? A critical look at the inpatient encounter. J Hosp Med. 2013;8(11):631-634. PubMed
31. Tackett S, Tad-y D, Rios R, Kisuule F, Wright S. Appraising the practice of etiquette-based medicine in the inpatient setting. J Gen Intern Med. 2013;28(7):908-913. PubMed
© 2017 Society of Hospital Medicine
In the Literature: HM-Related Research You Need to Know
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk of infection with arterial and central venous catheters
- Rifaximin and prevention of hepatic encephalopathy
- Tracheotomy to prevent ventilator-associated pneumonia
- Coagulopathy and risk of VTE in patients with cirrhosis
- Use of age-adjusted D-dimer for PE diagnosis
- Continuation of anti-hypertensive medications after stroke
- Number of lumen cultures and detection of CRBSIs
- Timing of anticoagulation and outcomes in PE
Arterial and Central Venous Catheters Have Similar Rates of Colonization and Blood Stream Infections
Clinical question: Are arterial catheters (ACs) safer than central venous catheters (CVCs) in terms of colonization and catheter-related infections?
Background: Unlike CVCs, only a few studies have addressed blood-stream infections (BSI) related to AC usage, probably due to the traditional perception that ACs pose a lesser risk of colonization and BSI than CVC.
Study design: Randomized, controlled trial.
Setting: Three university hospitals and two general hospitals in France.
Synopsis: The study included 3,532 catheters (1,915 CVC and 1,617 AC) with 27,541 catheter-days from seven ICU settings. The same standard procedures were followed for catheter insertion and site dressing change at the various centers. Catheters were removed when they no longer were needed or when catheter-related infection (CRI) was suspected.
Colonization and CRI rates were similar in both arterial and venous catheters: 7.9% vs. 9.6% and 0.68% vs. 0.94%, respectively. The daily risk of colonization over time was stable for CVC, but appeared to increase for AC.
One important limitation to this study is that many patients had both arterial and venous catheters, leading to difficulty attributing infection to either one. Hospitalists caring for ICU patients should weigh the risks and benefits of prolonged use of AC due to similar rates of colonization and CRI as CVC.
Bottom line: Arterial and central venous catheters are equally prone to colonization and cause similar rates of CRI, but AC daily risk tends to increase with time; thus, AC should receive the same precautions as CVC.
Citation: Lucet JC, Bouadma L, Zahar JR, et. al. Infectious risk associated with arterial catheters compared with central venous catheters. Crit Care Med. 2010;38(4):1030-1005.
Rifaximin Prevents Recurrence of Hepatic Encephalopathy Episodes and Reduces Associated Risk for Hospitalization
Clinical question: What is the efficacy of rifaximin for the prevention of hepatic encephalopathy?
Background: Hepatic encephalopathy is a chronic, debilitating complication of liver cirrhosis. The efficacy of treatment of acute episodes with rifaximin is well documented in the literature; however, prevention of such episodes using rifaximin is poorly studied.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Seventy centers in the U.S., Canada, and Russia.
Synopsis: A total of 299 chronic liver disease patients, in remission from recurrent hepatic encephalopathy, randomly were assigned to receive either oral rifaximin (140 patients) or placebo (159 patients) for six months.
When compared to placebo, rifaximin reduced the risk of breakthrough episodes of hepatic encephalopathy over a six-month treatment period (22.1% vs 45.9%, HR 0.42; 95% confidence interval, 0.28-0.64, P<0.001), as well as risk of hospitalization involving hepatic encephalopathy (13.6% vs 22.6%, HR 0.50; 95% CI, 0.29-0.87, P=0.01).
The incidence of adverse effects was similar in both groups. More than 90% of patients received concomitant lactulose therapy.
Bottom line: Rifaximin treatment delays the first breakthrough episode of hepatic encephalopathy during a six-month period; moreover, it significantly reduces the associated risk for hospitalization.
Citation: Bass NM, Mullen KD, Sanyal A, et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362:1071-1081.
Early Tracheotomy Does Not Decrease the Incidence of Ventilator-Associated Pneumonia in ICU Patients
Clinical question: Does early tracheotomy decrease the incidence of ventilator-associated pneumonia (VAP) in mechanically ventilated adult ICU patients without existing lung infection?
Background: There is considerable variation in timing and incidence of tracheotomy across ICUs. Observational studies have reported that tracheotomy performed earlier might be associated with quicker weaning from mechanical ventilation; however, randomized, controlled trials have failed to confirm this finding.
Study design: Multicenter randomized controlled trial.
Setting: Adult ICU in Italy.
Synopsis: Between 2004 and 2008, 600 mechanically ventilated patients without lung infection were enrolled from 12 adult ICUs in Italy. Of these patients, 419 were randomized to early tracheotomy performed six to eight days after intubation (N=209) or to late tracheotomy performed 13-15 days after intubation (N=210).
VAP was diagnosed in 14% of patients in the early tracheotomy group, compared with 21% in the late tracheotomy group (P=0.07). Although the number of ventilator-free and ICU-free days was higher in the early tracheotomy group, long-term outcomes did not differ between the two groups.
Only 69% of patients in the early tracheotomy group and 57% of patients in the late tracheotomy group received tracheotomy, but all the patients were included in the final analysis due to the intention-to-treat design of the study, which might have diluted the effect of the intervention. In addition, the smaller sample size may have prevented the study from reaching statistical significance.
Bottom line: Early tracheotomy does not significantly decrease the incidence of VAP as compared to late tracheotomy.
Citation: Terragni PP, Antonelli M, Fumagalli R, et al. Early vs. late tracheotomy for prevention of pneumonia in mechanically ventilated adult ICU patients. JAMA. 2010;303(15): 1483-1489.
Coagulopathy in Cirrhotic Patients Is Not Protective against VTE
Clinical question: Does the degree of INR elevation affect the incidence of VTE in hospitalized patients with cirrhosis?
Background: Chronic liver disease (CLD) and subsequent development of cirrhosis renders patients coagulopathic. Historically, this has provided a sense of security to clinicians that these patients inherently possess a decreased VTE risk.
Study design: Retrospective cohort study.
Setting: University of Missouri Medical Center in Columbia.
Synopsis: Chart review of patients admitted with CLD and cirrhosis from Jan. 1, 2000, and Jan. 31, 2007, demonstrated an incidence rate of VTE of 6.3%, which is much higher than previous reports.
Most patients with CLD received no thrombosis prophylaxis; notably, there was no difference in VTE incidence between subgroups who received prophylaxis and those who did not. Five percent of VTE cases occurred in patients with an INR exceeding 1.6, with Child-Pugh class C patients having the highest thromboembolism incidence.
This retrospective chart review was limited by information and reporting bias and the inability to control confounding variables. Less than half of the patients were screened for VTE, which means that the true incidence of thrombus could actually be higher. Further studies are needed to provide proper risk assessment.
Bottom line: Patients with CLD and cirrhosis are at risk for VTE, even in the setting of coagulopathy, and might require VTE prophylaxis.
Citation: Dabbagh O, Oza A, Prakash S, Sunna R, Saettele TM. Coagulopathy does not protect against venous thromboembolism in hospitalized patients with chronic liver disease. Chest. 2010;137(5):1145-1149.
Pulmonary Embolism Can Be Safely Excluded Using Age-Adjusted D-dimer Cut-off Value
Clinical question: Does the new age-adjusted D-dimer cutoff value in older patients safely exclude pulmonary embolism (PE)?
Background: D-dimer is a useful blood test to exclude PE; however, D-dimer concentration increases with age, and hence the current cutoff of 500µg/l used in excluding a PE becomes less specific in older patients.
Study design: Retrospective multicenter cohort study.
Setting: General and teaching hospitals in Belgium, Switzerland, France, and Netherlands.
Synopsis: The study included 5,132 consecutive patients with clinically suspected PE. Patients were distributed into a derivation set (N=1,331) and two independent validation sets (N1=2,151 and N2=1,643). For patients older than 50, the use of the new age-adjusted D-dimer cutoff (patient age multiplied by 10µg/l) resulted in a combined 11% increase in the number of patients with negative results. This increase was more prominent in patients aged older than 70 (13% to 16%).
The new age-adjusted D-dimer cutoff point failed to detect PE in 0.2% of cases in the derivation set and in 0.6% and 0.3% of cases in the two validation sets, respectively. However, despite external validation, prospective studies are needed before implementing such criteria into clinical practice.
Bottom line: The age-adjusted D-dimer combined with clinical probability greatly increases the proportion of older patients in whom PE can be safely excluded.
Citation: Douma RA, Le Gal G, Söhne M, et al. Potential of an age adjusted D-dimer cut-off value to improve the exclusion of pulmonary embolism in older patients: a retrospective analysis of three large cohorts. BMJ. 2010;340:c1475.
Antihypertensive Drugs After Stroke Does Not Impact Cardiovascular Event Rate or Mortality at Six Months
Clinical question: Should antihypertensive medications be continued during the immediate post-stroke period in patients who previously were on such therapy?
Background: More than 50% of patients suffering from acute stroke are on antihypertensive therapy prior to admission. However, efficacy of such therapy in reducing cardiovascular event rates and mortality in the immediate post-stroke period is not well studied.
Study design: Prospective, randomized, open-blinded-endpoint trial.
Setting: Forty-nine UK National Institute for Health Research Stroke Centers.
Synopsis: From January 2003 and March 2009, 763 patients with pre-existing hypertension and diagnosis of mild to moderate acute stroke were recruited and assigned to continue or stop antihypertension drugs. The time limit for inclusion into the study was within 48 hours of the stroke and the endpoint was death or dependency (modified Rankin Scale >3) at the end of two weeks.
There was a statistically significant difference in the two groups at two weeks in both systolic and diastolic pressures, 13 mmHg and 8mmHg, respectively (P<0.0001). Seventy-two of 379 patients in the continuation group and 82 of 384 patients in the stop group reached the primary endpoint (P=0.3). The latter point is a major limitation to this trial, since it was underpowered because of early termination to detect differences in outcomes.
Bottom line: Antihypertensive therapy during the immediate post-stroke period did not reduce two-week death or dependency, cardiovascular event rate, or mortality at six months.
Citation: Robinson TG, Potter JF, Ford GA, et al. Effects of antihypertensive treatment after acute stroke in the continue or stop post-stroke antihypertensives collaborative study (COSSACS): a prospective, randomized, open, blinded-endpoint trial. Lancet Neurol. 2010;9:767-775.
All Lumens from Multi-Lumen Catheters Should Be Cultured to Diagnose Catheter-Related Bloodstream Infections
Clinical question: Do all lumens from multi-lumen catheters need to be cultured to best diagnose catheter-related bloodstream infections (CRBSIs)?
Background: The recent Infectious Diseases Society of America’s “Clinical Practice Guidelines for the Diagnosis and Management of Intravascular Catheter-Related Infections” has not conclusively established the number of lumens to culture from multi-lumen catheters when attempting to diagnose CRBSIs.
Study design: Retrospective cohort study.
Setting: Large teaching institution in Spain.
Synopsis: From January 2003 until May 2009, 154 patients, mostly men, with a mean age of 58.1 years, were recruited to participate in the study. Of these, 171 episodes of proven CRBSIs were detected in 154 subjects. Of the 171 tested catheters (112 double lumen and 59 triple lumen), testing only one lumen from double catheters would have led to 27.2% of missed cases for CRBSIs. Additionally, testing only two or one lumen from triple lumen catheters would have led to 15.8% and 37.3% of missed cases for CRBSIs, respectively.
The study was limited by being conducted at a single test site and the need to withdraw catheters to perform endoluminal brushing and semi-quantitative techniques. Though diagnostic yield might significantly improve by culturing all multi-lumen sites, hospitalists should consider the time and cost expenditure for testing from more than one lumen.
Bottom line: Culturing all lumens from multi-lumen catheters could greatly increase diagnostic yield in CRBSIs.
Citation: Guembe M, Rodríguez-Créixems M, Sánchez-Carrillo C, Pérez-Parra A, Martín-Rabadán P, Bouza E. How many lumens should be cultured in the conservative diagnosis of catheter-related bloodstream infections? CID. 2010;50(12):1575-1579.
Early Anticoagulation Improves Survival after Acute PE
Clinical question: Does the timing of initial heparinization reduce mortality in patients with acute symptomatic PE?
Background: Acute PE is rapidly fatal if not diagnosed and treated. Studies have shown that intravenous heparin improves overall survival for patients with PE, and therapeutic anticoagulation reduces rates of recurrent VTE. However, studies investigating the relation between time to achieve therapeutic anticoagulation and mortality or PE recurrence are limited.
Study design: Retrospective cohort study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: From June 2002 and September 2005, 400 patients were identified with PE using retrospective data from Mayo Clinic’s electronic medical records. Patients who received heparin in the ED had lower in-hospital mortality (OR 0.20, 95% CI, 0.06-0.69) and 30-day mortality (OR 0.25, 95% CI, 0.12-0.55) compared with patients who received heparin after admission. Similarly, patients who achieved a therapeutic aPTT within 24 hours also had lower 30-day mortality (OR 0.34, 95% CI, 0.14-0.84). Patients with COPD and malignancies had higher in-hospital and 30-day mortality, respectively.
Bottom line: It is difficult to draw a causal relationship from a retrospective review, but hospitalists should start immediate anticoagulation therapy when a PE is suspected.
Citation: Smith SB, Geske JB, Maguire JM, Zane NA, Carter RE, Morgenthaler TI. Early anticoagulation is associated with reduced mortality for acute pulmonary embolism. Chest. 2010;137(6): 1382-1390. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk of infection with arterial and central venous catheters
- Rifaximin and prevention of hepatic encephalopathy
- Tracheotomy to prevent ventilator-associated pneumonia
- Coagulopathy and risk of VTE in patients with cirrhosis
- Use of age-adjusted D-dimer for PE diagnosis
- Continuation of anti-hypertensive medications after stroke
- Number of lumen cultures and detection of CRBSIs
- Timing of anticoagulation and outcomes in PE
Arterial and Central Venous Catheters Have Similar Rates of Colonization and Blood Stream Infections
Clinical question: Are arterial catheters (ACs) safer than central venous catheters (CVCs) in terms of colonization and catheter-related infections?
Background: Unlike CVCs, only a few studies have addressed blood-stream infections (BSI) related to AC usage, probably due to the traditional perception that ACs pose a lesser risk of colonization and BSI than CVC.
Study design: Randomized, controlled trial.
Setting: Three university hospitals and two general hospitals in France.
Synopsis: The study included 3,532 catheters (1,915 CVC and 1,617 AC) with 27,541 catheter-days from seven ICU settings. The same standard procedures were followed for catheter insertion and site dressing change at the various centers. Catheters were removed when they no longer were needed or when catheter-related infection (CRI) was suspected.
Colonization and CRI rates were similar in both arterial and venous catheters: 7.9% vs. 9.6% and 0.68% vs. 0.94%, respectively. The daily risk of colonization over time was stable for CVC, but appeared to increase for AC.
One important limitation to this study is that many patients had both arterial and venous catheters, leading to difficulty attributing infection to either one. Hospitalists caring for ICU patients should weigh the risks and benefits of prolonged use of AC due to similar rates of colonization and CRI as CVC.
Bottom line: Arterial and central venous catheters are equally prone to colonization and cause similar rates of CRI, but AC daily risk tends to increase with time; thus, AC should receive the same precautions as CVC.
Citation: Lucet JC, Bouadma L, Zahar JR, et. al. Infectious risk associated with arterial catheters compared with central venous catheters. Crit Care Med. 2010;38(4):1030-1005.
Rifaximin Prevents Recurrence of Hepatic Encephalopathy Episodes and Reduces Associated Risk for Hospitalization
Clinical question: What is the efficacy of rifaximin for the prevention of hepatic encephalopathy?
Background: Hepatic encephalopathy is a chronic, debilitating complication of liver cirrhosis. The efficacy of treatment of acute episodes with rifaximin is well documented in the literature; however, prevention of such episodes using rifaximin is poorly studied.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Seventy centers in the U.S., Canada, and Russia.
Synopsis: A total of 299 chronic liver disease patients, in remission from recurrent hepatic encephalopathy, randomly were assigned to receive either oral rifaximin (140 patients) or placebo (159 patients) for six months.
When compared to placebo, rifaximin reduced the risk of breakthrough episodes of hepatic encephalopathy over a six-month treatment period (22.1% vs 45.9%, HR 0.42; 95% confidence interval, 0.28-0.64, P<0.001), as well as risk of hospitalization involving hepatic encephalopathy (13.6% vs 22.6%, HR 0.50; 95% CI, 0.29-0.87, P=0.01).
The incidence of adverse effects was similar in both groups. More than 90% of patients received concomitant lactulose therapy.
Bottom line: Rifaximin treatment delays the first breakthrough episode of hepatic encephalopathy during a six-month period; moreover, it significantly reduces the associated risk for hospitalization.
Citation: Bass NM, Mullen KD, Sanyal A, et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362:1071-1081.
Early Tracheotomy Does Not Decrease the Incidence of Ventilator-Associated Pneumonia in ICU Patients
Clinical question: Does early tracheotomy decrease the incidence of ventilator-associated pneumonia (VAP) in mechanically ventilated adult ICU patients without existing lung infection?
Background: There is considerable variation in timing and incidence of tracheotomy across ICUs. Observational studies have reported that tracheotomy performed earlier might be associated with quicker weaning from mechanical ventilation; however, randomized, controlled trials have failed to confirm this finding.
Study design: Multicenter randomized controlled trial.
Setting: Adult ICU in Italy.
Synopsis: Between 2004 and 2008, 600 mechanically ventilated patients without lung infection were enrolled from 12 adult ICUs in Italy. Of these patients, 419 were randomized to early tracheotomy performed six to eight days after intubation (N=209) or to late tracheotomy performed 13-15 days after intubation (N=210).
VAP was diagnosed in 14% of patients in the early tracheotomy group, compared with 21% in the late tracheotomy group (P=0.07). Although the number of ventilator-free and ICU-free days was higher in the early tracheotomy group, long-term outcomes did not differ between the two groups.
Only 69% of patients in the early tracheotomy group and 57% of patients in the late tracheotomy group received tracheotomy, but all the patients were included in the final analysis due to the intention-to-treat design of the study, which might have diluted the effect of the intervention. In addition, the smaller sample size may have prevented the study from reaching statistical significance.
Bottom line: Early tracheotomy does not significantly decrease the incidence of VAP as compared to late tracheotomy.
Citation: Terragni PP, Antonelli M, Fumagalli R, et al. Early vs. late tracheotomy for prevention of pneumonia in mechanically ventilated adult ICU patients. JAMA. 2010;303(15): 1483-1489.
Coagulopathy in Cirrhotic Patients Is Not Protective against VTE
Clinical question: Does the degree of INR elevation affect the incidence of VTE in hospitalized patients with cirrhosis?
Background: Chronic liver disease (CLD) and subsequent development of cirrhosis renders patients coagulopathic. Historically, this has provided a sense of security to clinicians that these patients inherently possess a decreased VTE risk.
Study design: Retrospective cohort study.
Setting: University of Missouri Medical Center in Columbia.
Synopsis: Chart review of patients admitted with CLD and cirrhosis from Jan. 1, 2000, and Jan. 31, 2007, demonstrated an incidence rate of VTE of 6.3%, which is much higher than previous reports.
Most patients with CLD received no thrombosis prophylaxis; notably, there was no difference in VTE incidence between subgroups who received prophylaxis and those who did not. Five percent of VTE cases occurred in patients with an INR exceeding 1.6, with Child-Pugh class C patients having the highest thromboembolism incidence.
This retrospective chart review was limited by information and reporting bias and the inability to control confounding variables. Less than half of the patients were screened for VTE, which means that the true incidence of thrombus could actually be higher. Further studies are needed to provide proper risk assessment.
Bottom line: Patients with CLD and cirrhosis are at risk for VTE, even in the setting of coagulopathy, and might require VTE prophylaxis.
Citation: Dabbagh O, Oza A, Prakash S, Sunna R, Saettele TM. Coagulopathy does not protect against venous thromboembolism in hospitalized patients with chronic liver disease. Chest. 2010;137(5):1145-1149.
Pulmonary Embolism Can Be Safely Excluded Using Age-Adjusted D-dimer Cut-off Value
Clinical question: Does the new age-adjusted D-dimer cutoff value in older patients safely exclude pulmonary embolism (PE)?
Background: D-dimer is a useful blood test to exclude PE; however, D-dimer concentration increases with age, and hence the current cutoff of 500µg/l used in excluding a PE becomes less specific in older patients.
Study design: Retrospective multicenter cohort study.
Setting: General and teaching hospitals in Belgium, Switzerland, France, and Netherlands.
Synopsis: The study included 5,132 consecutive patients with clinically suspected PE. Patients were distributed into a derivation set (N=1,331) and two independent validation sets (N1=2,151 and N2=1,643). For patients older than 50, the use of the new age-adjusted D-dimer cutoff (patient age multiplied by 10µg/l) resulted in a combined 11% increase in the number of patients with negative results. This increase was more prominent in patients aged older than 70 (13% to 16%).
The new age-adjusted D-dimer cutoff point failed to detect PE in 0.2% of cases in the derivation set and in 0.6% and 0.3% of cases in the two validation sets, respectively. However, despite external validation, prospective studies are needed before implementing such criteria into clinical practice.
Bottom line: The age-adjusted D-dimer combined with clinical probability greatly increases the proportion of older patients in whom PE can be safely excluded.
Citation: Douma RA, Le Gal G, Söhne M, et al. Potential of an age adjusted D-dimer cut-off value to improve the exclusion of pulmonary embolism in older patients: a retrospective analysis of three large cohorts. BMJ. 2010;340:c1475.
Antihypertensive Drugs After Stroke Does Not Impact Cardiovascular Event Rate or Mortality at Six Months
Clinical question: Should antihypertensive medications be continued during the immediate post-stroke period in patients who previously were on such therapy?
Background: More than 50% of patients suffering from acute stroke are on antihypertensive therapy prior to admission. However, efficacy of such therapy in reducing cardiovascular event rates and mortality in the immediate post-stroke period is not well studied.
Study design: Prospective, randomized, open-blinded-endpoint trial.
Setting: Forty-nine UK National Institute for Health Research Stroke Centers.
Synopsis: From January 2003 and March 2009, 763 patients with pre-existing hypertension and diagnosis of mild to moderate acute stroke were recruited and assigned to continue or stop antihypertension drugs. The time limit for inclusion into the study was within 48 hours of the stroke and the endpoint was death or dependency (modified Rankin Scale >3) at the end of two weeks.
There was a statistically significant difference in the two groups at two weeks in both systolic and diastolic pressures, 13 mmHg and 8mmHg, respectively (P<0.0001). Seventy-two of 379 patients in the continuation group and 82 of 384 patients in the stop group reached the primary endpoint (P=0.3). The latter point is a major limitation to this trial, since it was underpowered because of early termination to detect differences in outcomes.
Bottom line: Antihypertensive therapy during the immediate post-stroke period did not reduce two-week death or dependency, cardiovascular event rate, or mortality at six months.
Citation: Robinson TG, Potter JF, Ford GA, et al. Effects of antihypertensive treatment after acute stroke in the continue or stop post-stroke antihypertensives collaborative study (COSSACS): a prospective, randomized, open, blinded-endpoint trial. Lancet Neurol. 2010;9:767-775.
All Lumens from Multi-Lumen Catheters Should Be Cultured to Diagnose Catheter-Related Bloodstream Infections
Clinical question: Do all lumens from multi-lumen catheters need to be cultured to best diagnose catheter-related bloodstream infections (CRBSIs)?
Background: The recent Infectious Diseases Society of America’s “Clinical Practice Guidelines for the Diagnosis and Management of Intravascular Catheter-Related Infections” has not conclusively established the number of lumens to culture from multi-lumen catheters when attempting to diagnose CRBSIs.
Study design: Retrospective cohort study.
Setting: Large teaching institution in Spain.
Synopsis: From January 2003 until May 2009, 154 patients, mostly men, with a mean age of 58.1 years, were recruited to participate in the study. Of these, 171 episodes of proven CRBSIs were detected in 154 subjects. Of the 171 tested catheters (112 double lumen and 59 triple lumen), testing only one lumen from double catheters would have led to 27.2% of missed cases for CRBSIs. Additionally, testing only two or one lumen from triple lumen catheters would have led to 15.8% and 37.3% of missed cases for CRBSIs, respectively.
The study was limited by being conducted at a single test site and the need to withdraw catheters to perform endoluminal brushing and semi-quantitative techniques. Though diagnostic yield might significantly improve by culturing all multi-lumen sites, hospitalists should consider the time and cost expenditure for testing from more than one lumen.
Bottom line: Culturing all lumens from multi-lumen catheters could greatly increase diagnostic yield in CRBSIs.
Citation: Guembe M, Rodríguez-Créixems M, Sánchez-Carrillo C, Pérez-Parra A, Martín-Rabadán P, Bouza E. How many lumens should be cultured in the conservative diagnosis of catheter-related bloodstream infections? CID. 2010;50(12):1575-1579.
Early Anticoagulation Improves Survival after Acute PE
Clinical question: Does the timing of initial heparinization reduce mortality in patients with acute symptomatic PE?
Background: Acute PE is rapidly fatal if not diagnosed and treated. Studies have shown that intravenous heparin improves overall survival for patients with PE, and therapeutic anticoagulation reduces rates of recurrent VTE. However, studies investigating the relation between time to achieve therapeutic anticoagulation and mortality or PE recurrence are limited.
Study design: Retrospective cohort study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: From June 2002 and September 2005, 400 patients were identified with PE using retrospective data from Mayo Clinic’s electronic medical records. Patients who received heparin in the ED had lower in-hospital mortality (OR 0.20, 95% CI, 0.06-0.69) and 30-day mortality (OR 0.25, 95% CI, 0.12-0.55) compared with patients who received heparin after admission. Similarly, patients who achieved a therapeutic aPTT within 24 hours also had lower 30-day mortality (OR 0.34, 95% CI, 0.14-0.84). Patients with COPD and malignancies had higher in-hospital and 30-day mortality, respectively.
Bottom line: It is difficult to draw a causal relationship from a retrospective review, but hospitalists should start immediate anticoagulation therapy when a PE is suspected.
Citation: Smith SB, Geske JB, Maguire JM, Zane NA, Carter RE, Morgenthaler TI. Early anticoagulation is associated with reduced mortality for acute pulmonary embolism. Chest. 2010;137(6): 1382-1390. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk of infection with arterial and central venous catheters
- Rifaximin and prevention of hepatic encephalopathy
- Tracheotomy to prevent ventilator-associated pneumonia
- Coagulopathy and risk of VTE in patients with cirrhosis
- Use of age-adjusted D-dimer for PE diagnosis
- Continuation of anti-hypertensive medications after stroke
- Number of lumen cultures and detection of CRBSIs
- Timing of anticoagulation and outcomes in PE
Arterial and Central Venous Catheters Have Similar Rates of Colonization and Blood Stream Infections
Clinical question: Are arterial catheters (ACs) safer than central venous catheters (CVCs) in terms of colonization and catheter-related infections?
Background: Unlike CVCs, only a few studies have addressed blood-stream infections (BSI) related to AC usage, probably due to the traditional perception that ACs pose a lesser risk of colonization and BSI than CVC.
Study design: Randomized, controlled trial.
Setting: Three university hospitals and two general hospitals in France.
Synopsis: The study included 3,532 catheters (1,915 CVC and 1,617 AC) with 27,541 catheter-days from seven ICU settings. The same standard procedures were followed for catheter insertion and site dressing change at the various centers. Catheters were removed when they no longer were needed or when catheter-related infection (CRI) was suspected.
Colonization and CRI rates were similar in both arterial and venous catheters: 7.9% vs. 9.6% and 0.68% vs. 0.94%, respectively. The daily risk of colonization over time was stable for CVC, but appeared to increase for AC.
One important limitation to this study is that many patients had both arterial and venous catheters, leading to difficulty attributing infection to either one. Hospitalists caring for ICU patients should weigh the risks and benefits of prolonged use of AC due to similar rates of colonization and CRI as CVC.
Bottom line: Arterial and central venous catheters are equally prone to colonization and cause similar rates of CRI, but AC daily risk tends to increase with time; thus, AC should receive the same precautions as CVC.
Citation: Lucet JC, Bouadma L, Zahar JR, et. al. Infectious risk associated with arterial catheters compared with central venous catheters. Crit Care Med. 2010;38(4):1030-1005.
Rifaximin Prevents Recurrence of Hepatic Encephalopathy Episodes and Reduces Associated Risk for Hospitalization
Clinical question: What is the efficacy of rifaximin for the prevention of hepatic encephalopathy?
Background: Hepatic encephalopathy is a chronic, debilitating complication of liver cirrhosis. The efficacy of treatment of acute episodes with rifaximin is well documented in the literature; however, prevention of such episodes using rifaximin is poorly studied.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Seventy centers in the U.S., Canada, and Russia.
Synopsis: A total of 299 chronic liver disease patients, in remission from recurrent hepatic encephalopathy, randomly were assigned to receive either oral rifaximin (140 patients) or placebo (159 patients) for six months.
When compared to placebo, rifaximin reduced the risk of breakthrough episodes of hepatic encephalopathy over a six-month treatment period (22.1% vs 45.9%, HR 0.42; 95% confidence interval, 0.28-0.64, P<0.001), as well as risk of hospitalization involving hepatic encephalopathy (13.6% vs 22.6%, HR 0.50; 95% CI, 0.29-0.87, P=0.01).
The incidence of adverse effects was similar in both groups. More than 90% of patients received concomitant lactulose therapy.
Bottom line: Rifaximin treatment delays the first breakthrough episode of hepatic encephalopathy during a six-month period; moreover, it significantly reduces the associated risk for hospitalization.
Citation: Bass NM, Mullen KD, Sanyal A, et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362:1071-1081.
Early Tracheotomy Does Not Decrease the Incidence of Ventilator-Associated Pneumonia in ICU Patients
Clinical question: Does early tracheotomy decrease the incidence of ventilator-associated pneumonia (VAP) in mechanically ventilated adult ICU patients without existing lung infection?
Background: There is considerable variation in timing and incidence of tracheotomy across ICUs. Observational studies have reported that tracheotomy performed earlier might be associated with quicker weaning from mechanical ventilation; however, randomized, controlled trials have failed to confirm this finding.
Study design: Multicenter randomized controlled trial.
Setting: Adult ICU in Italy.
Synopsis: Between 2004 and 2008, 600 mechanically ventilated patients without lung infection were enrolled from 12 adult ICUs in Italy. Of these patients, 419 were randomized to early tracheotomy performed six to eight days after intubation (N=209) or to late tracheotomy performed 13-15 days after intubation (N=210).
VAP was diagnosed in 14% of patients in the early tracheotomy group, compared with 21% in the late tracheotomy group (P=0.07). Although the number of ventilator-free and ICU-free days was higher in the early tracheotomy group, long-term outcomes did not differ between the two groups.
Only 69% of patients in the early tracheotomy group and 57% of patients in the late tracheotomy group received tracheotomy, but all the patients were included in the final analysis due to the intention-to-treat design of the study, which might have diluted the effect of the intervention. In addition, the smaller sample size may have prevented the study from reaching statistical significance.
Bottom line: Early tracheotomy does not significantly decrease the incidence of VAP as compared to late tracheotomy.
Citation: Terragni PP, Antonelli M, Fumagalli R, et al. Early vs. late tracheotomy for prevention of pneumonia in mechanically ventilated adult ICU patients. JAMA. 2010;303(15): 1483-1489.
Coagulopathy in Cirrhotic Patients Is Not Protective against VTE
Clinical question: Does the degree of INR elevation affect the incidence of VTE in hospitalized patients with cirrhosis?
Background: Chronic liver disease (CLD) and subsequent development of cirrhosis renders patients coagulopathic. Historically, this has provided a sense of security to clinicians that these patients inherently possess a decreased VTE risk.
Study design: Retrospective cohort study.
Setting: University of Missouri Medical Center in Columbia.
Synopsis: Chart review of patients admitted with CLD and cirrhosis from Jan. 1, 2000, and Jan. 31, 2007, demonstrated an incidence rate of VTE of 6.3%, which is much higher than previous reports.
Most patients with CLD received no thrombosis prophylaxis; notably, there was no difference in VTE incidence between subgroups who received prophylaxis and those who did not. Five percent of VTE cases occurred in patients with an INR exceeding 1.6, with Child-Pugh class C patients having the highest thromboembolism incidence.
This retrospective chart review was limited by information and reporting bias and the inability to control confounding variables. Less than half of the patients were screened for VTE, which means that the true incidence of thrombus could actually be higher. Further studies are needed to provide proper risk assessment.
Bottom line: Patients with CLD and cirrhosis are at risk for VTE, even in the setting of coagulopathy, and might require VTE prophylaxis.
Citation: Dabbagh O, Oza A, Prakash S, Sunna R, Saettele TM. Coagulopathy does not protect against venous thromboembolism in hospitalized patients with chronic liver disease. Chest. 2010;137(5):1145-1149.
Pulmonary Embolism Can Be Safely Excluded Using Age-Adjusted D-dimer Cut-off Value
Clinical question: Does the new age-adjusted D-dimer cutoff value in older patients safely exclude pulmonary embolism (PE)?
Background: D-dimer is a useful blood test to exclude PE; however, D-dimer concentration increases with age, and hence the current cutoff of 500µg/l used in excluding a PE becomes less specific in older patients.
Study design: Retrospective multicenter cohort study.
Setting: General and teaching hospitals in Belgium, Switzerland, France, and Netherlands.
Synopsis: The study included 5,132 consecutive patients with clinically suspected PE. Patients were distributed into a derivation set (N=1,331) and two independent validation sets (N1=2,151 and N2=1,643). For patients older than 50, the use of the new age-adjusted D-dimer cutoff (patient age multiplied by 10µg/l) resulted in a combined 11% increase in the number of patients with negative results. This increase was more prominent in patients aged older than 70 (13% to 16%).
The new age-adjusted D-dimer cutoff point failed to detect PE in 0.2% of cases in the derivation set and in 0.6% and 0.3% of cases in the two validation sets, respectively. However, despite external validation, prospective studies are needed before implementing such criteria into clinical practice.
Bottom line: The age-adjusted D-dimer combined with clinical probability greatly increases the proportion of older patients in whom PE can be safely excluded.
Citation: Douma RA, Le Gal G, Söhne M, et al. Potential of an age adjusted D-dimer cut-off value to improve the exclusion of pulmonary embolism in older patients: a retrospective analysis of three large cohorts. BMJ. 2010;340:c1475.
Antihypertensive Drugs After Stroke Does Not Impact Cardiovascular Event Rate or Mortality at Six Months
Clinical question: Should antihypertensive medications be continued during the immediate post-stroke period in patients who previously were on such therapy?
Background: More than 50% of patients suffering from acute stroke are on antihypertensive therapy prior to admission. However, efficacy of such therapy in reducing cardiovascular event rates and mortality in the immediate post-stroke period is not well studied.
Study design: Prospective, randomized, open-blinded-endpoint trial.
Setting: Forty-nine UK National Institute for Health Research Stroke Centers.
Synopsis: From January 2003 and March 2009, 763 patients with pre-existing hypertension and diagnosis of mild to moderate acute stroke were recruited and assigned to continue or stop antihypertension drugs. The time limit for inclusion into the study was within 48 hours of the stroke and the endpoint was death or dependency (modified Rankin Scale >3) at the end of two weeks.
There was a statistically significant difference in the two groups at two weeks in both systolic and diastolic pressures, 13 mmHg and 8mmHg, respectively (P<0.0001). Seventy-two of 379 patients in the continuation group and 82 of 384 patients in the stop group reached the primary endpoint (P=0.3). The latter point is a major limitation to this trial, since it was underpowered because of early termination to detect differences in outcomes.
Bottom line: Antihypertensive therapy during the immediate post-stroke period did not reduce two-week death or dependency, cardiovascular event rate, or mortality at six months.
Citation: Robinson TG, Potter JF, Ford GA, et al. Effects of antihypertensive treatment after acute stroke in the continue or stop post-stroke antihypertensives collaborative study (COSSACS): a prospective, randomized, open, blinded-endpoint trial. Lancet Neurol. 2010;9:767-775.
All Lumens from Multi-Lumen Catheters Should Be Cultured to Diagnose Catheter-Related Bloodstream Infections
Clinical question: Do all lumens from multi-lumen catheters need to be cultured to best diagnose catheter-related bloodstream infections (CRBSIs)?
Background: The recent Infectious Diseases Society of America’s “Clinical Practice Guidelines for the Diagnosis and Management of Intravascular Catheter-Related Infections” has not conclusively established the number of lumens to culture from multi-lumen catheters when attempting to diagnose CRBSIs.
Study design: Retrospective cohort study.
Setting: Large teaching institution in Spain.
Synopsis: From January 2003 until May 2009, 154 patients, mostly men, with a mean age of 58.1 years, were recruited to participate in the study. Of these, 171 episodes of proven CRBSIs were detected in 154 subjects. Of the 171 tested catheters (112 double lumen and 59 triple lumen), testing only one lumen from double catheters would have led to 27.2% of missed cases for CRBSIs. Additionally, testing only two or one lumen from triple lumen catheters would have led to 15.8% and 37.3% of missed cases for CRBSIs, respectively.
The study was limited by being conducted at a single test site and the need to withdraw catheters to perform endoluminal brushing and semi-quantitative techniques. Though diagnostic yield might significantly improve by culturing all multi-lumen sites, hospitalists should consider the time and cost expenditure for testing from more than one lumen.
Bottom line: Culturing all lumens from multi-lumen catheters could greatly increase diagnostic yield in CRBSIs.
Citation: Guembe M, Rodríguez-Créixems M, Sánchez-Carrillo C, Pérez-Parra A, Martín-Rabadán P, Bouza E. How many lumens should be cultured in the conservative diagnosis of catheter-related bloodstream infections? CID. 2010;50(12):1575-1579.
Early Anticoagulation Improves Survival after Acute PE
Clinical question: Does the timing of initial heparinization reduce mortality in patients with acute symptomatic PE?
Background: Acute PE is rapidly fatal if not diagnosed and treated. Studies have shown that intravenous heparin improves overall survival for patients with PE, and therapeutic anticoagulation reduces rates of recurrent VTE. However, studies investigating the relation between time to achieve therapeutic anticoagulation and mortality or PE recurrence are limited.
Study design: Retrospective cohort study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: From June 2002 and September 2005, 400 patients were identified with PE using retrospective data from Mayo Clinic’s electronic medical records. Patients who received heparin in the ED had lower in-hospital mortality (OR 0.20, 95% CI, 0.06-0.69) and 30-day mortality (OR 0.25, 95% CI, 0.12-0.55) compared with patients who received heparin after admission. Similarly, patients who achieved a therapeutic aPTT within 24 hours also had lower 30-day mortality (OR 0.34, 95% CI, 0.14-0.84). Patients with COPD and malignancies had higher in-hospital and 30-day mortality, respectively.
Bottom line: It is difficult to draw a causal relationship from a retrospective review, but hospitalists should start immediate anticoagulation therapy when a PE is suspected.
Citation: Smith SB, Geske JB, Maguire JM, Zane NA, Carter RE, Morgenthaler TI. Early anticoagulation is associated with reduced mortality for acute pulmonary embolism. Chest. 2010;137(6): 1382-1390. TH