User login
Palliative Medicine in the ED
Overview
Palliative medicine in the ED represents a paradigm shift for the emergency physician (EP)—from identifying and stabilizing acute medical and surgical conditions to providing symptomatic comfort care to a dying patient. When the ED became the “safety net” for patients who have serious, life-limiting illnesses,1-3 it also became the most frequent place where such care is initially sought4—although not considered an ideal place to begin such care.
In one study, approximately 40% of dying patients presented to the ED during their final 2 weeks of life.5 With the ED becoming more recognized as a location for palliative care, the EP plays a key role in the care of these patients. The 2013 Model of the Clinical Practice of Emergency Medicine explicitly lists palliative medicine within the EP’s scope of practice.6 Further support for providing palliative care in emergency medicine includes the cosponsorship of Hospice and Palliative Medicine subspecialty board certification by the American Board of Emergency Medicine in 2008. Finally, palliative care medicine principles have been endorsed in the “Choosing Wisely” initiative of the American College of Emergency Physicians.
Essential Palliative Care Skills
Quest et al7 have identified the following 12 primary palliative care skills in which every EP should be competent:
- Assessment of illness trajectory;
- Determination of prognosis;
- Communication of bad news;
- Interpretation and formation of an advance care plan;
- Allowance of family presence during resuscitation;
- Symptom management (both pain and nonpain);
- Withholding and withdrawal of life-sustaining treatments;
- Management of imminently dying patients;
- Identification and implementation of hospice and palliative care plans;
- Understanding of ethical and legal issues pertinent to end-of-life care;
- Display of spiritual and cultural competency; and
- Management of the dying child.
Although all of the above are important skills, this paper focuses on the symptom management of pain and nonpain (skill 6) in patients presenting to the ED with a life-limiting illness. The evidence base for these treatments is limited due to the many methodological challenges faced when studying symptoms in patients who are at end of life.
Pharmacologic Management of Symptoms
Recent research has found that symptom burden is high at end of life. Despite the increase in attention to these patients and their needs, symptoms including pain, depression, and delirium have repeatedly increased between 1998 and 2010.8 A 2013 study recommended that a minimum of four classes of medications be considered for patients who are at end of life: opioid (for pain); benzodiazepine (for anxiety); antipsychotic (for delirium and nausea); and antimuscarinic (for excessive secretions).9 The role and indications for each of these drug classes will be discussed.
Palliative Care Intervention
Though EPs frequently request specialty and subspecialty consultation for ED patients, they usually do not consider a palliative care medicine consult for the dying patient. Palliative care medicine utilizes an interdisciplinary, collaborative, team-based approach to decrease the pain and suffering of patients with advanced illness.10
Benefits from early palliative care intervention in the ED include improved symptom management, improved patient and family satisfaction, improved outcomes, decreased length of stay, less use of intensive care units, and less costs.4
Pain Management
Pain is one of the most devastating symptoms that a patient can experience, and its management is an integral component of palliative care medicine. Initial evaluation must include appropriate assessment of the pain and its impact on a patient’s function and quality of life.
The general approach to pain management follows the World Health Organization pain ladder. For mild to moderate pain, step 1 begins with acetaminophen or a nonsteroidal anti-inflammatory drug (NSAID), with or without an adjuvant such as an antidepressant or anticonvulsant. If pain persists, step 2 involves the addition of an opioid. For moderate to severe pain, step 3 involves the addition of stronger opioids, such as hydromorphone, morphine, and oxycodone. Typically, a patient with a serious, life-limiting illness who presents to the ED for help will likely require treatment with strong opioids (step 3).
Opioids
In patients requiring step 3 management, opioids are the primary medication used to manage pain. An initial equivalent dose of morphine 5 mg intravenously (IV) is appropriate in an opioid-naïve patient. The adage of “starting low and going slow” is important to follow; however, an important corollary is “…and use enough.” If a patient’s pain is not controlled with initial dosages, additional bolus doses of 50% to 100% increments will be necessary. Because opioids do not have a ceiling effect, it is important to understand that dosages may seem very high for some patients compared to others. In this population, ensuring baseline pain control, with either an oral long-acting formulation or a continuous IV infusion, is important.11
Difficulties clinicians have in determining opioids for the management of pain are multifactorial. One consideration may be the growing public concern for prescription opioid abuse, potentially creating resistance to appropriate use of opioids by clinicians who fear legal or regulatory push back.
General principles in managing severe pain in the opioid-tolerant patient include the following: (1) calculating the morphine equivalent as a daily 24-hour dose; (2) determining the breakthrough dose, which is usually 10% to 15% of the calculated daily dose; (3) titrating doses upward if pain is not controlled, or if more than three breakthrough doses are being required daily; and (4) reducing the calculated conversion dose of a new opioid 25% to 50% when converting to a different opioid.12
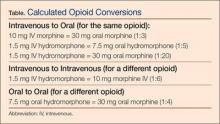
The EP is frequently required to convert a patient’s oral opioid analgesic to an equivalent IV dose, and hydromorphone and morphine are the two most commonly used. The Table provides an approximation for this conversion.
Equianalgesic Dosing
Equianalgesic dosing is an important concept in pain management, especially for those patients already receiving opioids. There is great variation in the analgesic potency of the different opioids. The dose at which two opioids provide equivalent pain relief is the equianalgesic dose. Usually, this is standardized to 10 mg of parenteral morphine.13 Unfortunately, it is not uncommon for patients to be undertreated when switched to another opioid.
Nonpain Symptom Management
Nonpain symptoms that all EPs must know how to manage include constipation, dyspnea, nausea/vomiting, the so-called death rattle, and terminal delirium. In one study of reasons for ED visits by palliative care patients, the most common were dyspnea (26%), nausea/vomiting/constipation (17%), and uncontrolled pain (15%).14
Constipation
The most important adverse effect of opioids—one that does not improve or change during treatment—is constipation. Constipation in general—not just associated with opioids—has been ranked as one of the 10 most bothersome symptoms in the palliative care population, leading to discomfort, decreased quality of life, and potential small bowel obstruction or perforation.15 Unless contraindicated, a gastrointestinal stimulant such as senna, or an osmotic laxative such as lactulose, must be prescribed whenever an opioid is initiated. As the author (Galicia-Castillo) often notes, “The hand that writes the prescription for an opioid should be the hand that writes an Rx for a bowel regimen, or it becomes the hand that disimpacts the patient.”
The most recent Cochrane Review for the management of constipation in the palliative care population did not show any differences in the effectiveness among three commonly used laxatives: senna, docusate, and lactulose. This review did not evaluate polyethylene glycol, which is also commonly used.16 The addition of stool softeners, bisacodyl and nightly prune juice can also be helpful.10
Dyspnea
Dyspnea, the subjective feeling of breathing discomfort, is a common end-of-life complaint. Similar to pain, self-report is required for adequate assessment of dyspnea. Treatment recommendations include opioids, anxiolytics, and oxygen therapy.18 Opioids are the most widely studied treatment for dyspnea, demonstrating reduction in breathlessness in patients who have a variety of conditions, such as advanced chronic obstructive pulmonary disease, interstitial lung disease, cancer, and chronic heart failure.19
While many of the benefits of opioids are widely recognized and understood, the manner in which they improve symptoms of dyspnea is less well known. In addition, the evidence of effectiveness is limited to oral or parenteral morphine and fentanyl, and nebulized opioids have not been well studied. Oxygen treatments have been shown to reduce dyspnea in patients who suffer from hypoxemia; however, no benefit was found for patients who had only mild or no hypoxemia. A majority of dying patients did not experience a change in respiratory comfort after their supplemental oxygen was withdrawn. In these cases, when administration of oxygen is unnecessary, it may potentially introduce further discomfort to end-of-life patients by causing nasal dryness and impaired mobility.20
The use of benzodiazepines as the primary medication to manage dyspnea is unfounded, but may provide some benefit when used in conjunction with opioids.11 When indicated, a longer-acting agent (eg, clonazepam, with an initial starting does of 0.25 mg orally every 12 hours) may be used.4
Nausea and Vomiting
Nausea and vomiting have been reported by 16% to 68% of patients who had life-limiting illness, such as cancer, heart failure, renal failure, or acquired immunodeficiency syndrome.21 The etiology of nausea and vomiting is multifactorial in a dying patient. Assessment and treatment has been based on understanding how neurotransmitters are involved in the “emetic pathway,”22 but other pathways, such as a cytokine-mediated model of cancer symptoms, may also be important.23
Nonpharmacologic methods to utilize include avoidance of environmental stimuli, such as fatty, spicy, and salted foods; use of relaxation and distraction; and massage.22 Several medication classes have been utilized to treat nausea and vomiting: prokinetic agents (metoclopramide 10 mg three to four times a day, 30 minutes prior to meals and bedtime); dopamine receptor antagonists (haloperidol 1.5-5 mg two to three times a day); antihistaminic agents (promethazine 25 mg orally or IV every 4-6 hours, with a maximum dose of 100 mg/d); and selective 5 hydroxytryptamine-3 receptor antagonists (ondansetron 4-8 mg once or twice a day). Other agents that have been utilized include corticosteroids, benzodiazepines, octreotide, and cannabinoids.22
Procedures such as percutaneous endoscopic gastrostomy placement, nasogastric tube placement, and stenting may be necessary for patients who have advanced disease caused by a mechanical obstruction.22
Death Rattle
The death rattle occurs when secretions accumulate in the pharynx and/or airways when swallowing and cough mechanisms are no longer intact.24 This phenomenon occurs in 23% to 92% of dying patients.25 Generally, death occurs within 48 hours for about 75% of such patients.26 The noise that results from this process is usually more disturbing for those visiting the patients than to the patient themselves. Conservative measures to employ include placing patients on their sides to facilitate secretion drainage and to minimize upper airway sounds, gentle oral and pharyngeal suctioning, and limiting fluid input.11
One recent study reviewing the use of the anticholinergics atropine, scopolamine, and hyoscine demonstrated similar efficacy among the three drugs. Dosages used in this study included atropine 0.5 mg as a subcutaneous bolus, followed by 3 mg every 24 hours subcutaneously; scopolamine as a 0.25 mg subcutaneous bolus, followed by 1.5 mg every 24 hours IV or by subcutaneous infusion; and hyoscine 20 mg as a subcutaneous bolus followed by 60 mg every 24 hours IV or subcutaneous infusion. Glycopyrrolate is often used in the cognitively intact patient, as it does not cross the blood-brain barrier; however, supply concerns at the time of the study prevented a review of its efficiency.27 All of these medications are also available in oral and transdermal formulations.
Terminal Delirium
Delirium is a common complication for patients nearing the end of life, affecting as many as 88% of dying patients.28 It is characterized by an acute onset of cognitive impairment that may manifest as either a hyperactive or hypoactive state. Causes for terminal delirium are multifactorial. Initially, management should include prevention strategies, such as frequently orientating the patient, maintenance of day-night cycles, provision of adequate sleep, and minimization of sensory overload.11 When pharmacological therapy is required to improve quality of life, a neuroleptic medication, namely haloperidol, should be used initially. The addition of a benzodiazepine may help if the initial treatments are ineffective, or if sedation is desired.28
Summary
Emergency physicians have a unique opportunity to improve the quality of life for patients suffering serious illness, especially those who are actively dying. The management of pain and nonpain symptoms in patients who are at end of life, is a particularly important skill for every EP. If available, a consultation with a palliative care medicine consultant may improve both short- and long-term patient care.
Dr Galicia-Castillo is the Sue Faulkner Scribner professor of geriatrics at the Eastern Virginia Medical School Glennan Center for Geriatrics and Gerontology, and Medical Director for Palliative Care Medicine at Sentara Norfolk General Hospital. Dr Counselman is the distinguished professor and chairman of the department of emergency medicine at Eastern Virginia Medical School, Norfolk; and a physician at Emergency Physicians of Tidewater, Norfolk, Virginia. He is also the associate editor in chief of EMERGENCY MEDICINE editorial board.
- Alsirafy SA, Raheem AA, Al-Zahrani AS, et al. Emergency department visits at the end of life of patients with terminal cancer: pattern, causes, and avoidability. Am J Hosp Palliat Care. 2015:1049909115581819. [Epub ahead of print].
- Grudzen CR, Richardson LD, Morrison M, Cho E, Morrison RS. Palliative care needs of seriously ill, older adults presenting to the emergency department. Acad Emerg Med. 2010;17(11):1253-1257.
- Smith AK, Schonberg MA, Fisher J, et al. Emergency department experiences of acutely symptomatic patients with terminal illness and their family caregivers. J Pain Symptom Manage. 2010;39(6):972-981.
- Mierendorf S, Gidvani V. Palliative care in the emergency department. Perm J. 2014;18(2):77-85.
- Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? CMAJ. 2010;182(6): 563-568.
- Counselman FL, Borenstein MA, Chisholm CD, et al; EM Model Review Task Force; American Board of Emergency Medicine. The 2013 Model of the Clinical Practice of Emergency Medicine. Acad Emerg Med. 2014;21(5):574-598.
- Quest TE, Marco CA, Derse AR. Hospice and palliative medicine: new subspecialty, new opportunities. Ann Emerg Med. 2009;54(1):94-102.
- Singer AE, Meeker D, Teno JM, Lynn J, Lunney JR, Lorenz KA. Symptom trends in the last year of life from 1998 to 2010: a cohort study. Ann Intern Med. 2015;162(3):175-183.
- Lindqvist O, Lundquist G, Dickman A, et al; OPCARE9. Four essential drugs needed for quality care of the dying: a Delphi-study based international expert consensus opinion. J Palliat Med. 2013;16(1):38-43.
- Kandarian B, Morrison RS, Richardson LD, Ortiz J, Grudzen CR. Emergency department-initiated palliative care for advanced cancer patients: protocol for a pilot randomized controlled trial. Trials. 2014;15:251.
- Campbell ML. Caring for dying patients in the intensive care unit: managing pain, dyspnea, anxiety, delirium, and death rattle. AACN Adv Crit Care. 2015;26(2):110-120.
- Lamba S, Quest TE. Hospice care and the emergency department: rules, regulations, and referrals. Ann Emerg Med. 2011;57(3):282-290.
- Shaheen PE, Walsh D, Lasheen W, Davis MP, Lagman RL. Opioid equianalgesic tables: are they all equally dangerous? J Pain Symptom Manage.2009;38(3):409-417.
- Wallace EM, Cooney MC, Walsh J, Conroy M, Twomey F. Why do palliative care patients present to the emergency department? Avoidable or unavoidable? Am J Hosp Palliat Care. 2013;30(3):253-253.
- Erichsén E, Milberg A, Jaarsma T, Friedrichsen MJ. Constipation in specialized palliative care: prevalence, definition, and patient-perceived symptom distress. J Palliat Med. 2015;18(7):585-592.
- Candy B, Jones L, Larkin PJ, Vickerstaff V, Tookman A, Stone P. Laxatives for the management of constipation in people receiving palliative care. Cochrane Database Syst Rev. 2015;5:CD003448.
- Parshall MB, Schwartzstein RM, Adams L, et al; American Thoracic Society Committee on Dyspnea. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4):435-452.
- LeGrand SB, Khawam EA, Walsh D, Rivera NI. Opioids, respiratory function, and dyspnea. Am J Hosp Palliat Care. 2003;20(1):57-61.
- Meek PM, Schwartzstein R, Adams L, el al. Dyspnea. Mechanisms, assessment, and management: a consensus statement. American Thoracic Society. Am J Respir Crit Care Med. 1999;159(1):321-340.
- Campbell ML, Yarandi H, Dove-Medows E. Oxygen is nonbeneficial for most patients who are near death. J Pain Symptom Manage. 2013;45(3):517-523.
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31(1):58-69.
- Glare P, Miller J, Nikolova T, Tickoo R. Treating nausea and vomiting in palliative care: a review. Clin Interv Aging. 2011;6:243-259.
- Cleeland CS, Bennett GJ, Dantzer R, et al. Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism? A cytokine-immunologic model of cancer symptoms. Cancer. 2003;97(11):2919-2925.
- Bennett M, Lucas V, Brennan M, Hughes A, O’Donnell V, Wee B; Association for Palliative Medicine’s Science Committee. Using anti-muscarinic drugs in the management of death rattle: evidence-based guidelines for palliative care. Palliat Med. 2002;16(5):369-374.
- Mercadamte S. Death rattle: critical review and research agenda. Support Care Cancer. 2014;22(2):
- 571-575.
- Wildiers H, Menten J. Death rattle: prevalence, prevention and treatment. J Pain Symptom Manage. 2002;23(4):310-317.
- Wildiers H, Dhaenekint C, Demeulenaere P, et al; Flemish Federation of Palliative Care. Atropine, hyoscine butylbromide, or scopolamine are equally effective for the treatment of death rattle in terminal care. J Pain Symptom Manage. 2009;38(1):124-133.
- Kehl KA. Treatment of terminal restlessness: a review of the evidence. J Pain Palliat Care Pharmacother. 2004;18(1):5-30.
Overview
Palliative medicine in the ED represents a paradigm shift for the emergency physician (EP)—from identifying and stabilizing acute medical and surgical conditions to providing symptomatic comfort care to a dying patient. When the ED became the “safety net” for patients who have serious, life-limiting illnesses,1-3 it also became the most frequent place where such care is initially sought4—although not considered an ideal place to begin such care.
In one study, approximately 40% of dying patients presented to the ED during their final 2 weeks of life.5 With the ED becoming more recognized as a location for palliative care, the EP plays a key role in the care of these patients. The 2013 Model of the Clinical Practice of Emergency Medicine explicitly lists palliative medicine within the EP’s scope of practice.6 Further support for providing palliative care in emergency medicine includes the cosponsorship of Hospice and Palliative Medicine subspecialty board certification by the American Board of Emergency Medicine in 2008. Finally, palliative care medicine principles have been endorsed in the “Choosing Wisely” initiative of the American College of Emergency Physicians.
Essential Palliative Care Skills
Quest et al7 have identified the following 12 primary palliative care skills in which every EP should be competent:
- Assessment of illness trajectory;
- Determination of prognosis;
- Communication of bad news;
- Interpretation and formation of an advance care plan;
- Allowance of family presence during resuscitation;
- Symptom management (both pain and nonpain);
- Withholding and withdrawal of life-sustaining treatments;
- Management of imminently dying patients;
- Identification and implementation of hospice and palliative care plans;
- Understanding of ethical and legal issues pertinent to end-of-life care;
- Display of spiritual and cultural competency; and
- Management of the dying child.
Although all of the above are important skills, this paper focuses on the symptom management of pain and nonpain (skill 6) in patients presenting to the ED with a life-limiting illness. The evidence base for these treatments is limited due to the many methodological challenges faced when studying symptoms in patients who are at end of life.
Pharmacologic Management of Symptoms
Recent research has found that symptom burden is high at end of life. Despite the increase in attention to these patients and their needs, symptoms including pain, depression, and delirium have repeatedly increased between 1998 and 2010.8 A 2013 study recommended that a minimum of four classes of medications be considered for patients who are at end of life: opioid (for pain); benzodiazepine (for anxiety); antipsychotic (for delirium and nausea); and antimuscarinic (for excessive secretions).9 The role and indications for each of these drug classes will be discussed.
Palliative Care Intervention
Though EPs frequently request specialty and subspecialty consultation for ED patients, they usually do not consider a palliative care medicine consult for the dying patient. Palliative care medicine utilizes an interdisciplinary, collaborative, team-based approach to decrease the pain and suffering of patients with advanced illness.10
Benefits from early palliative care intervention in the ED include improved symptom management, improved patient and family satisfaction, improved outcomes, decreased length of stay, less use of intensive care units, and less costs.4
Pain Management
Pain is one of the most devastating symptoms that a patient can experience, and its management is an integral component of palliative care medicine. Initial evaluation must include appropriate assessment of the pain and its impact on a patient’s function and quality of life.
The general approach to pain management follows the World Health Organization pain ladder. For mild to moderate pain, step 1 begins with acetaminophen or a nonsteroidal anti-inflammatory drug (NSAID), with or without an adjuvant such as an antidepressant or anticonvulsant. If pain persists, step 2 involves the addition of an opioid. For moderate to severe pain, step 3 involves the addition of stronger opioids, such as hydromorphone, morphine, and oxycodone. Typically, a patient with a serious, life-limiting illness who presents to the ED for help will likely require treatment with strong opioids (step 3).
Opioids
In patients requiring step 3 management, opioids are the primary medication used to manage pain. An initial equivalent dose of morphine 5 mg intravenously (IV) is appropriate in an opioid-naïve patient. The adage of “starting low and going slow” is important to follow; however, an important corollary is “…and use enough.” If a patient’s pain is not controlled with initial dosages, additional bolus doses of 50% to 100% increments will be necessary. Because opioids do not have a ceiling effect, it is important to understand that dosages may seem very high for some patients compared to others. In this population, ensuring baseline pain control, with either an oral long-acting formulation or a continuous IV infusion, is important.11
Difficulties clinicians have in determining opioids for the management of pain are multifactorial. One consideration may be the growing public concern for prescription opioid abuse, potentially creating resistance to appropriate use of opioids by clinicians who fear legal or regulatory push back.
General principles in managing severe pain in the opioid-tolerant patient include the following: (1) calculating the morphine equivalent as a daily 24-hour dose; (2) determining the breakthrough dose, which is usually 10% to 15% of the calculated daily dose; (3) titrating doses upward if pain is not controlled, or if more than three breakthrough doses are being required daily; and (4) reducing the calculated conversion dose of a new opioid 25% to 50% when converting to a different opioid.12
The EP is frequently required to convert a patient’s oral opioid analgesic to an equivalent IV dose, and hydromorphone and morphine are the two most commonly used. The Table provides an approximation for this conversion.
Equianalgesic Dosing
Equianalgesic dosing is an important concept in pain management, especially for those patients already receiving opioids. There is great variation in the analgesic potency of the different opioids. The dose at which two opioids provide equivalent pain relief is the equianalgesic dose. Usually, this is standardized to 10 mg of parenteral morphine.13 Unfortunately, it is not uncommon for patients to be undertreated when switched to another opioid.
Nonpain Symptom Management
Nonpain symptoms that all EPs must know how to manage include constipation, dyspnea, nausea/vomiting, the so-called death rattle, and terminal delirium. In one study of reasons for ED visits by palliative care patients, the most common were dyspnea (26%), nausea/vomiting/constipation (17%), and uncontrolled pain (15%).14
Constipation
The most important adverse effect of opioids—one that does not improve or change during treatment—is constipation. Constipation in general—not just associated with opioids—has been ranked as one of the 10 most bothersome symptoms in the palliative care population, leading to discomfort, decreased quality of life, and potential small bowel obstruction or perforation.15 Unless contraindicated, a gastrointestinal stimulant such as senna, or an osmotic laxative such as lactulose, must be prescribed whenever an opioid is initiated. As the author (Galicia-Castillo) often notes, “The hand that writes the prescription for an opioid should be the hand that writes an Rx for a bowel regimen, or it becomes the hand that disimpacts the patient.”
The most recent Cochrane Review for the management of constipation in the palliative care population did not show any differences in the effectiveness among three commonly used laxatives: senna, docusate, and lactulose. This review did not evaluate polyethylene glycol, which is also commonly used.16 The addition of stool softeners, bisacodyl and nightly prune juice can also be helpful.10
Dyspnea
Dyspnea, the subjective feeling of breathing discomfort, is a common end-of-life complaint. Similar to pain, self-report is required for adequate assessment of dyspnea. Treatment recommendations include opioids, anxiolytics, and oxygen therapy.18 Opioids are the most widely studied treatment for dyspnea, demonstrating reduction in breathlessness in patients who have a variety of conditions, such as advanced chronic obstructive pulmonary disease, interstitial lung disease, cancer, and chronic heart failure.19
While many of the benefits of opioids are widely recognized and understood, the manner in which they improve symptoms of dyspnea is less well known. In addition, the evidence of effectiveness is limited to oral or parenteral morphine and fentanyl, and nebulized opioids have not been well studied. Oxygen treatments have been shown to reduce dyspnea in patients who suffer from hypoxemia; however, no benefit was found for patients who had only mild or no hypoxemia. A majority of dying patients did not experience a change in respiratory comfort after their supplemental oxygen was withdrawn. In these cases, when administration of oxygen is unnecessary, it may potentially introduce further discomfort to end-of-life patients by causing nasal dryness and impaired mobility.20
The use of benzodiazepines as the primary medication to manage dyspnea is unfounded, but may provide some benefit when used in conjunction with opioids.11 When indicated, a longer-acting agent (eg, clonazepam, with an initial starting does of 0.25 mg orally every 12 hours) may be used.4
Nausea and Vomiting
Nausea and vomiting have been reported by 16% to 68% of patients who had life-limiting illness, such as cancer, heart failure, renal failure, or acquired immunodeficiency syndrome.21 The etiology of nausea and vomiting is multifactorial in a dying patient. Assessment and treatment has been based on understanding how neurotransmitters are involved in the “emetic pathway,”22 but other pathways, such as a cytokine-mediated model of cancer symptoms, may also be important.23
Nonpharmacologic methods to utilize include avoidance of environmental stimuli, such as fatty, spicy, and salted foods; use of relaxation and distraction; and massage.22 Several medication classes have been utilized to treat nausea and vomiting: prokinetic agents (metoclopramide 10 mg three to four times a day, 30 minutes prior to meals and bedtime); dopamine receptor antagonists (haloperidol 1.5-5 mg two to three times a day); antihistaminic agents (promethazine 25 mg orally or IV every 4-6 hours, with a maximum dose of 100 mg/d); and selective 5 hydroxytryptamine-3 receptor antagonists (ondansetron 4-8 mg once or twice a day). Other agents that have been utilized include corticosteroids, benzodiazepines, octreotide, and cannabinoids.22
Procedures such as percutaneous endoscopic gastrostomy placement, nasogastric tube placement, and stenting may be necessary for patients who have advanced disease caused by a mechanical obstruction.22
Death Rattle
The death rattle occurs when secretions accumulate in the pharynx and/or airways when swallowing and cough mechanisms are no longer intact.24 This phenomenon occurs in 23% to 92% of dying patients.25 Generally, death occurs within 48 hours for about 75% of such patients.26 The noise that results from this process is usually more disturbing for those visiting the patients than to the patient themselves. Conservative measures to employ include placing patients on their sides to facilitate secretion drainage and to minimize upper airway sounds, gentle oral and pharyngeal suctioning, and limiting fluid input.11
One recent study reviewing the use of the anticholinergics atropine, scopolamine, and hyoscine demonstrated similar efficacy among the three drugs. Dosages used in this study included atropine 0.5 mg as a subcutaneous bolus, followed by 3 mg every 24 hours subcutaneously; scopolamine as a 0.25 mg subcutaneous bolus, followed by 1.5 mg every 24 hours IV or by subcutaneous infusion; and hyoscine 20 mg as a subcutaneous bolus followed by 60 mg every 24 hours IV or subcutaneous infusion. Glycopyrrolate is often used in the cognitively intact patient, as it does not cross the blood-brain barrier; however, supply concerns at the time of the study prevented a review of its efficiency.27 All of these medications are also available in oral and transdermal formulations.
Terminal Delirium
Delirium is a common complication for patients nearing the end of life, affecting as many as 88% of dying patients.28 It is characterized by an acute onset of cognitive impairment that may manifest as either a hyperactive or hypoactive state. Causes for terminal delirium are multifactorial. Initially, management should include prevention strategies, such as frequently orientating the patient, maintenance of day-night cycles, provision of adequate sleep, and minimization of sensory overload.11 When pharmacological therapy is required to improve quality of life, a neuroleptic medication, namely haloperidol, should be used initially. The addition of a benzodiazepine may help if the initial treatments are ineffective, or if sedation is desired.28
Summary
Emergency physicians have a unique opportunity to improve the quality of life for patients suffering serious illness, especially those who are actively dying. The management of pain and nonpain symptoms in patients who are at end of life, is a particularly important skill for every EP. If available, a consultation with a palliative care medicine consultant may improve both short- and long-term patient care.
Dr Galicia-Castillo is the Sue Faulkner Scribner professor of geriatrics at the Eastern Virginia Medical School Glennan Center for Geriatrics and Gerontology, and Medical Director for Palliative Care Medicine at Sentara Norfolk General Hospital. Dr Counselman is the distinguished professor and chairman of the department of emergency medicine at Eastern Virginia Medical School, Norfolk; and a physician at Emergency Physicians of Tidewater, Norfolk, Virginia. He is also the associate editor in chief of EMERGENCY MEDICINE editorial board.
Overview
Palliative medicine in the ED represents a paradigm shift for the emergency physician (EP)—from identifying and stabilizing acute medical and surgical conditions to providing symptomatic comfort care to a dying patient. When the ED became the “safety net” for patients who have serious, life-limiting illnesses,1-3 it also became the most frequent place where such care is initially sought4—although not considered an ideal place to begin such care.
In one study, approximately 40% of dying patients presented to the ED during their final 2 weeks of life.5 With the ED becoming more recognized as a location for palliative care, the EP plays a key role in the care of these patients. The 2013 Model of the Clinical Practice of Emergency Medicine explicitly lists palliative medicine within the EP’s scope of practice.6 Further support for providing palliative care in emergency medicine includes the cosponsorship of Hospice and Palliative Medicine subspecialty board certification by the American Board of Emergency Medicine in 2008. Finally, palliative care medicine principles have been endorsed in the “Choosing Wisely” initiative of the American College of Emergency Physicians.
Essential Palliative Care Skills
Quest et al7 have identified the following 12 primary palliative care skills in which every EP should be competent:
- Assessment of illness trajectory;
- Determination of prognosis;
- Communication of bad news;
- Interpretation and formation of an advance care plan;
- Allowance of family presence during resuscitation;
- Symptom management (both pain and nonpain);
- Withholding and withdrawal of life-sustaining treatments;
- Management of imminently dying patients;
- Identification and implementation of hospice and palliative care plans;
- Understanding of ethical and legal issues pertinent to end-of-life care;
- Display of spiritual and cultural competency; and
- Management of the dying child.
Although all of the above are important skills, this paper focuses on the symptom management of pain and nonpain (skill 6) in patients presenting to the ED with a life-limiting illness. The evidence base for these treatments is limited due to the many methodological challenges faced when studying symptoms in patients who are at end of life.
Pharmacologic Management of Symptoms
Recent research has found that symptom burden is high at end of life. Despite the increase in attention to these patients and their needs, symptoms including pain, depression, and delirium have repeatedly increased between 1998 and 2010.8 A 2013 study recommended that a minimum of four classes of medications be considered for patients who are at end of life: opioid (for pain); benzodiazepine (for anxiety); antipsychotic (for delirium and nausea); and antimuscarinic (for excessive secretions).9 The role and indications for each of these drug classes will be discussed.
Palliative Care Intervention
Though EPs frequently request specialty and subspecialty consultation for ED patients, they usually do not consider a palliative care medicine consult for the dying patient. Palliative care medicine utilizes an interdisciplinary, collaborative, team-based approach to decrease the pain and suffering of patients with advanced illness.10
Benefits from early palliative care intervention in the ED include improved symptom management, improved patient and family satisfaction, improved outcomes, decreased length of stay, less use of intensive care units, and less costs.4
Pain Management
Pain is one of the most devastating symptoms that a patient can experience, and its management is an integral component of palliative care medicine. Initial evaluation must include appropriate assessment of the pain and its impact on a patient’s function and quality of life.
The general approach to pain management follows the World Health Organization pain ladder. For mild to moderate pain, step 1 begins with acetaminophen or a nonsteroidal anti-inflammatory drug (NSAID), with or without an adjuvant such as an antidepressant or anticonvulsant. If pain persists, step 2 involves the addition of an opioid. For moderate to severe pain, step 3 involves the addition of stronger opioids, such as hydromorphone, morphine, and oxycodone. Typically, a patient with a serious, life-limiting illness who presents to the ED for help will likely require treatment with strong opioids (step 3).
Opioids
In patients requiring step 3 management, opioids are the primary medication used to manage pain. An initial equivalent dose of morphine 5 mg intravenously (IV) is appropriate in an opioid-naïve patient. The adage of “starting low and going slow” is important to follow; however, an important corollary is “…and use enough.” If a patient’s pain is not controlled with initial dosages, additional bolus doses of 50% to 100% increments will be necessary. Because opioids do not have a ceiling effect, it is important to understand that dosages may seem very high for some patients compared to others. In this population, ensuring baseline pain control, with either an oral long-acting formulation or a continuous IV infusion, is important.11
Difficulties clinicians have in determining opioids for the management of pain are multifactorial. One consideration may be the growing public concern for prescription opioid abuse, potentially creating resistance to appropriate use of opioids by clinicians who fear legal or regulatory push back.
General principles in managing severe pain in the opioid-tolerant patient include the following: (1) calculating the morphine equivalent as a daily 24-hour dose; (2) determining the breakthrough dose, which is usually 10% to 15% of the calculated daily dose; (3) titrating doses upward if pain is not controlled, or if more than three breakthrough doses are being required daily; and (4) reducing the calculated conversion dose of a new opioid 25% to 50% when converting to a different opioid.12
The EP is frequently required to convert a patient’s oral opioid analgesic to an equivalent IV dose, and hydromorphone and morphine are the two most commonly used. The Table provides an approximation for this conversion.
Equianalgesic Dosing
Equianalgesic dosing is an important concept in pain management, especially for those patients already receiving opioids. There is great variation in the analgesic potency of the different opioids. The dose at which two opioids provide equivalent pain relief is the equianalgesic dose. Usually, this is standardized to 10 mg of parenteral morphine.13 Unfortunately, it is not uncommon for patients to be undertreated when switched to another opioid.
Nonpain Symptom Management
Nonpain symptoms that all EPs must know how to manage include constipation, dyspnea, nausea/vomiting, the so-called death rattle, and terminal delirium. In one study of reasons for ED visits by palliative care patients, the most common were dyspnea (26%), nausea/vomiting/constipation (17%), and uncontrolled pain (15%).14
Constipation
The most important adverse effect of opioids—one that does not improve or change during treatment—is constipation. Constipation in general—not just associated with opioids—has been ranked as one of the 10 most bothersome symptoms in the palliative care population, leading to discomfort, decreased quality of life, and potential small bowel obstruction or perforation.15 Unless contraindicated, a gastrointestinal stimulant such as senna, or an osmotic laxative such as lactulose, must be prescribed whenever an opioid is initiated. As the author (Galicia-Castillo) often notes, “The hand that writes the prescription for an opioid should be the hand that writes an Rx for a bowel regimen, or it becomes the hand that disimpacts the patient.”
The most recent Cochrane Review for the management of constipation in the palliative care population did not show any differences in the effectiveness among three commonly used laxatives: senna, docusate, and lactulose. This review did not evaluate polyethylene glycol, which is also commonly used.16 The addition of stool softeners, bisacodyl and nightly prune juice can also be helpful.10
Dyspnea
Dyspnea, the subjective feeling of breathing discomfort, is a common end-of-life complaint. Similar to pain, self-report is required for adequate assessment of dyspnea. Treatment recommendations include opioids, anxiolytics, and oxygen therapy.18 Opioids are the most widely studied treatment for dyspnea, demonstrating reduction in breathlessness in patients who have a variety of conditions, such as advanced chronic obstructive pulmonary disease, interstitial lung disease, cancer, and chronic heart failure.19
While many of the benefits of opioids are widely recognized and understood, the manner in which they improve symptoms of dyspnea is less well known. In addition, the evidence of effectiveness is limited to oral or parenteral morphine and fentanyl, and nebulized opioids have not been well studied. Oxygen treatments have been shown to reduce dyspnea in patients who suffer from hypoxemia; however, no benefit was found for patients who had only mild or no hypoxemia. A majority of dying patients did not experience a change in respiratory comfort after their supplemental oxygen was withdrawn. In these cases, when administration of oxygen is unnecessary, it may potentially introduce further discomfort to end-of-life patients by causing nasal dryness and impaired mobility.20
The use of benzodiazepines as the primary medication to manage dyspnea is unfounded, but may provide some benefit when used in conjunction with opioids.11 When indicated, a longer-acting agent (eg, clonazepam, with an initial starting does of 0.25 mg orally every 12 hours) may be used.4
Nausea and Vomiting
Nausea and vomiting have been reported by 16% to 68% of patients who had life-limiting illness, such as cancer, heart failure, renal failure, or acquired immunodeficiency syndrome.21 The etiology of nausea and vomiting is multifactorial in a dying patient. Assessment and treatment has been based on understanding how neurotransmitters are involved in the “emetic pathway,”22 but other pathways, such as a cytokine-mediated model of cancer symptoms, may also be important.23
Nonpharmacologic methods to utilize include avoidance of environmental stimuli, such as fatty, spicy, and salted foods; use of relaxation and distraction; and massage.22 Several medication classes have been utilized to treat nausea and vomiting: prokinetic agents (metoclopramide 10 mg three to four times a day, 30 minutes prior to meals and bedtime); dopamine receptor antagonists (haloperidol 1.5-5 mg two to three times a day); antihistaminic agents (promethazine 25 mg orally or IV every 4-6 hours, with a maximum dose of 100 mg/d); and selective 5 hydroxytryptamine-3 receptor antagonists (ondansetron 4-8 mg once or twice a day). Other agents that have been utilized include corticosteroids, benzodiazepines, octreotide, and cannabinoids.22
Procedures such as percutaneous endoscopic gastrostomy placement, nasogastric tube placement, and stenting may be necessary for patients who have advanced disease caused by a mechanical obstruction.22
Death Rattle
The death rattle occurs when secretions accumulate in the pharynx and/or airways when swallowing and cough mechanisms are no longer intact.24 This phenomenon occurs in 23% to 92% of dying patients.25 Generally, death occurs within 48 hours for about 75% of such patients.26 The noise that results from this process is usually more disturbing for those visiting the patients than to the patient themselves. Conservative measures to employ include placing patients on their sides to facilitate secretion drainage and to minimize upper airway sounds, gentle oral and pharyngeal suctioning, and limiting fluid input.11
One recent study reviewing the use of the anticholinergics atropine, scopolamine, and hyoscine demonstrated similar efficacy among the three drugs. Dosages used in this study included atropine 0.5 mg as a subcutaneous bolus, followed by 3 mg every 24 hours subcutaneously; scopolamine as a 0.25 mg subcutaneous bolus, followed by 1.5 mg every 24 hours IV or by subcutaneous infusion; and hyoscine 20 mg as a subcutaneous bolus followed by 60 mg every 24 hours IV or subcutaneous infusion. Glycopyrrolate is often used in the cognitively intact patient, as it does not cross the blood-brain barrier; however, supply concerns at the time of the study prevented a review of its efficiency.27 All of these medications are also available in oral and transdermal formulations.
Terminal Delirium
Delirium is a common complication for patients nearing the end of life, affecting as many as 88% of dying patients.28 It is characterized by an acute onset of cognitive impairment that may manifest as either a hyperactive or hypoactive state. Causes for terminal delirium are multifactorial. Initially, management should include prevention strategies, such as frequently orientating the patient, maintenance of day-night cycles, provision of adequate sleep, and minimization of sensory overload.11 When pharmacological therapy is required to improve quality of life, a neuroleptic medication, namely haloperidol, should be used initially. The addition of a benzodiazepine may help if the initial treatments are ineffective, or if sedation is desired.28
Summary
Emergency physicians have a unique opportunity to improve the quality of life for patients suffering serious illness, especially those who are actively dying. The management of pain and nonpain symptoms in patients who are at end of life, is a particularly important skill for every EP. If available, a consultation with a palliative care medicine consultant may improve both short- and long-term patient care.
Dr Galicia-Castillo is the Sue Faulkner Scribner professor of geriatrics at the Eastern Virginia Medical School Glennan Center for Geriatrics and Gerontology, and Medical Director for Palliative Care Medicine at Sentara Norfolk General Hospital. Dr Counselman is the distinguished professor and chairman of the department of emergency medicine at Eastern Virginia Medical School, Norfolk; and a physician at Emergency Physicians of Tidewater, Norfolk, Virginia. He is also the associate editor in chief of EMERGENCY MEDICINE editorial board.
- Alsirafy SA, Raheem AA, Al-Zahrani AS, et al. Emergency department visits at the end of life of patients with terminal cancer: pattern, causes, and avoidability. Am J Hosp Palliat Care. 2015:1049909115581819. [Epub ahead of print].
- Grudzen CR, Richardson LD, Morrison M, Cho E, Morrison RS. Palliative care needs of seriously ill, older adults presenting to the emergency department. Acad Emerg Med. 2010;17(11):1253-1257.
- Smith AK, Schonberg MA, Fisher J, et al. Emergency department experiences of acutely symptomatic patients with terminal illness and their family caregivers. J Pain Symptom Manage. 2010;39(6):972-981.
- Mierendorf S, Gidvani V. Palliative care in the emergency department. Perm J. 2014;18(2):77-85.
- Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? CMAJ. 2010;182(6): 563-568.
- Counselman FL, Borenstein MA, Chisholm CD, et al; EM Model Review Task Force; American Board of Emergency Medicine. The 2013 Model of the Clinical Practice of Emergency Medicine. Acad Emerg Med. 2014;21(5):574-598.
- Quest TE, Marco CA, Derse AR. Hospice and palliative medicine: new subspecialty, new opportunities. Ann Emerg Med. 2009;54(1):94-102.
- Singer AE, Meeker D, Teno JM, Lynn J, Lunney JR, Lorenz KA. Symptom trends in the last year of life from 1998 to 2010: a cohort study. Ann Intern Med. 2015;162(3):175-183.
- Lindqvist O, Lundquist G, Dickman A, et al; OPCARE9. Four essential drugs needed for quality care of the dying: a Delphi-study based international expert consensus opinion. J Palliat Med. 2013;16(1):38-43.
- Kandarian B, Morrison RS, Richardson LD, Ortiz J, Grudzen CR. Emergency department-initiated palliative care for advanced cancer patients: protocol for a pilot randomized controlled trial. Trials. 2014;15:251.
- Campbell ML. Caring for dying patients in the intensive care unit: managing pain, dyspnea, anxiety, delirium, and death rattle. AACN Adv Crit Care. 2015;26(2):110-120.
- Lamba S, Quest TE. Hospice care and the emergency department: rules, regulations, and referrals. Ann Emerg Med. 2011;57(3):282-290.
- Shaheen PE, Walsh D, Lasheen W, Davis MP, Lagman RL. Opioid equianalgesic tables: are they all equally dangerous? J Pain Symptom Manage.2009;38(3):409-417.
- Wallace EM, Cooney MC, Walsh J, Conroy M, Twomey F. Why do palliative care patients present to the emergency department? Avoidable or unavoidable? Am J Hosp Palliat Care. 2013;30(3):253-253.
- Erichsén E, Milberg A, Jaarsma T, Friedrichsen MJ. Constipation in specialized palliative care: prevalence, definition, and patient-perceived symptom distress. J Palliat Med. 2015;18(7):585-592.
- Candy B, Jones L, Larkin PJ, Vickerstaff V, Tookman A, Stone P. Laxatives for the management of constipation in people receiving palliative care. Cochrane Database Syst Rev. 2015;5:CD003448.
- Parshall MB, Schwartzstein RM, Adams L, et al; American Thoracic Society Committee on Dyspnea. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4):435-452.
- LeGrand SB, Khawam EA, Walsh D, Rivera NI. Opioids, respiratory function, and dyspnea. Am J Hosp Palliat Care. 2003;20(1):57-61.
- Meek PM, Schwartzstein R, Adams L, el al. Dyspnea. Mechanisms, assessment, and management: a consensus statement. American Thoracic Society. Am J Respir Crit Care Med. 1999;159(1):321-340.
- Campbell ML, Yarandi H, Dove-Medows E. Oxygen is nonbeneficial for most patients who are near death. J Pain Symptom Manage. 2013;45(3):517-523.
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31(1):58-69.
- Glare P, Miller J, Nikolova T, Tickoo R. Treating nausea and vomiting in palliative care: a review. Clin Interv Aging. 2011;6:243-259.
- Cleeland CS, Bennett GJ, Dantzer R, et al. Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism? A cytokine-immunologic model of cancer symptoms. Cancer. 2003;97(11):2919-2925.
- Bennett M, Lucas V, Brennan M, Hughes A, O’Donnell V, Wee B; Association for Palliative Medicine’s Science Committee. Using anti-muscarinic drugs in the management of death rattle: evidence-based guidelines for palliative care. Palliat Med. 2002;16(5):369-374.
- Mercadamte S. Death rattle: critical review and research agenda. Support Care Cancer. 2014;22(2):
- 571-575.
- Wildiers H, Menten J. Death rattle: prevalence, prevention and treatment. J Pain Symptom Manage. 2002;23(4):310-317.
- Wildiers H, Dhaenekint C, Demeulenaere P, et al; Flemish Federation of Palliative Care. Atropine, hyoscine butylbromide, or scopolamine are equally effective for the treatment of death rattle in terminal care. J Pain Symptom Manage. 2009;38(1):124-133.
- Kehl KA. Treatment of terminal restlessness: a review of the evidence. J Pain Palliat Care Pharmacother. 2004;18(1):5-30.
- Alsirafy SA, Raheem AA, Al-Zahrani AS, et al. Emergency department visits at the end of life of patients with terminal cancer: pattern, causes, and avoidability. Am J Hosp Palliat Care. 2015:1049909115581819. [Epub ahead of print].
- Grudzen CR, Richardson LD, Morrison M, Cho E, Morrison RS. Palliative care needs of seriously ill, older adults presenting to the emergency department. Acad Emerg Med. 2010;17(11):1253-1257.
- Smith AK, Schonberg MA, Fisher J, et al. Emergency department experiences of acutely symptomatic patients with terminal illness and their family caregivers. J Pain Symptom Manage. 2010;39(6):972-981.
- Mierendorf S, Gidvani V. Palliative care in the emergency department. Perm J. 2014;18(2):77-85.
- Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? CMAJ. 2010;182(6): 563-568.
- Counselman FL, Borenstein MA, Chisholm CD, et al; EM Model Review Task Force; American Board of Emergency Medicine. The 2013 Model of the Clinical Practice of Emergency Medicine. Acad Emerg Med. 2014;21(5):574-598.
- Quest TE, Marco CA, Derse AR. Hospice and palliative medicine: new subspecialty, new opportunities. Ann Emerg Med. 2009;54(1):94-102.
- Singer AE, Meeker D, Teno JM, Lynn J, Lunney JR, Lorenz KA. Symptom trends in the last year of life from 1998 to 2010: a cohort study. Ann Intern Med. 2015;162(3):175-183.
- Lindqvist O, Lundquist G, Dickman A, et al; OPCARE9. Four essential drugs needed for quality care of the dying: a Delphi-study based international expert consensus opinion. J Palliat Med. 2013;16(1):38-43.
- Kandarian B, Morrison RS, Richardson LD, Ortiz J, Grudzen CR. Emergency department-initiated palliative care for advanced cancer patients: protocol for a pilot randomized controlled trial. Trials. 2014;15:251.
- Campbell ML. Caring for dying patients in the intensive care unit: managing pain, dyspnea, anxiety, delirium, and death rattle. AACN Adv Crit Care. 2015;26(2):110-120.
- Lamba S, Quest TE. Hospice care and the emergency department: rules, regulations, and referrals. Ann Emerg Med. 2011;57(3):282-290.
- Shaheen PE, Walsh D, Lasheen W, Davis MP, Lagman RL. Opioid equianalgesic tables: are they all equally dangerous? J Pain Symptom Manage.2009;38(3):409-417.
- Wallace EM, Cooney MC, Walsh J, Conroy M, Twomey F. Why do palliative care patients present to the emergency department? Avoidable or unavoidable? Am J Hosp Palliat Care. 2013;30(3):253-253.
- Erichsén E, Milberg A, Jaarsma T, Friedrichsen MJ. Constipation in specialized palliative care: prevalence, definition, and patient-perceived symptom distress. J Palliat Med. 2015;18(7):585-592.
- Candy B, Jones L, Larkin PJ, Vickerstaff V, Tookman A, Stone P. Laxatives for the management of constipation in people receiving palliative care. Cochrane Database Syst Rev. 2015;5:CD003448.
- Parshall MB, Schwartzstein RM, Adams L, et al; American Thoracic Society Committee on Dyspnea. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4):435-452.
- LeGrand SB, Khawam EA, Walsh D, Rivera NI. Opioids, respiratory function, and dyspnea. Am J Hosp Palliat Care. 2003;20(1):57-61.
- Meek PM, Schwartzstein R, Adams L, el al. Dyspnea. Mechanisms, assessment, and management: a consensus statement. American Thoracic Society. Am J Respir Crit Care Med. 1999;159(1):321-340.
- Campbell ML, Yarandi H, Dove-Medows E. Oxygen is nonbeneficial for most patients who are near death. J Pain Symptom Manage. 2013;45(3):517-523.
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31(1):58-69.
- Glare P, Miller J, Nikolova T, Tickoo R. Treating nausea and vomiting in palliative care: a review. Clin Interv Aging. 2011;6:243-259.
- Cleeland CS, Bennett GJ, Dantzer R, et al. Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism? A cytokine-immunologic model of cancer symptoms. Cancer. 2003;97(11):2919-2925.
- Bennett M, Lucas V, Brennan M, Hughes A, O’Donnell V, Wee B; Association for Palliative Medicine’s Science Committee. Using anti-muscarinic drugs in the management of death rattle: evidence-based guidelines for palliative care. Palliat Med. 2002;16(5):369-374.
- Mercadamte S. Death rattle: critical review and research agenda. Support Care Cancer. 2014;22(2):
- 571-575.
- Wildiers H, Menten J. Death rattle: prevalence, prevention and treatment. J Pain Symptom Manage. 2002;23(4):310-317.
- Wildiers H, Dhaenekint C, Demeulenaere P, et al; Flemish Federation of Palliative Care. Atropine, hyoscine butylbromide, or scopolamine are equally effective for the treatment of death rattle in terminal care. J Pain Symptom Manage. 2009;38(1):124-133.
- Kehl KA. Treatment of terminal restlessness: a review of the evidence. J Pain Palliat Care Pharmacother. 2004;18(1):5-30.