User login
Coding and reimbursement 101: How to maximize your payments
While reimbursement for ObGyn services seemingly should be a simple matter of putting codes on a claim form, the reality is that it is complex, and it requires a team approach to accomplish timely filing to receive fair and accurate reimbursement.
Reimbursement occurs over the length of the revenue cycle for a patient encounter and involves many steps. It starts when the patient makes an appointment for services and ends when the practice receives payment. Along the way, there must be good clinician documentation and sound knowledge about the billing process (including the Current Procedural Terminology [CPT] or Healthcare Common Procedure Coding System [HCPCS] codes for services), the International Classification of Diseases, Tenth Revision, Clinical Modification [ICD-10-CM] codes that establish medical necessity, the modifiers that alter the meaning of the codes, and, of course, the bundling issues that now accompany many coding situations.
In addition, ObGyn practices must contend with a multitude of payers—from federal to commercial—and must understand and adhere to each payer’s rules and policies to maximize and retain reimbursement.
In this article, I detail stumbling blocks to maximizing reimbursement and how to avoid them.
Coding considerations for office services
Good documentation before, during, and after a patient’s office visit is essential, along with accurate codes, modifiers, and order of services on the claims you submit.
Prep paperwork before the patient encounter
Once a patient makes an appointment, the front-end staff can handle some of the tasks in the cycle. This includes ensuring that the patient’s insurance coverage information is current, informing the patient of any additional information to bring at the time of the visit (such as a patient history form for a new patient visit or a list of current prescriptions), or, if an established patient will be having a procedure, making sure that prior authorization is complete. This streamlines the process, assists the clinician with documentation housekeeping, and ensures that incorrect or missing information does not cause a claim to be denied or not be filed in a timely manner (many payers require submission of an initial claim 30 days from the date of service).
Continue to: Document details of the clinician-patient interaction
Document details of the clinician-patient interaction
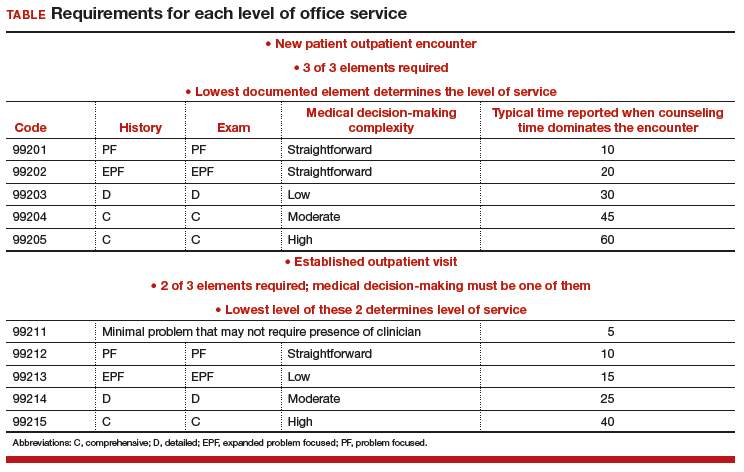
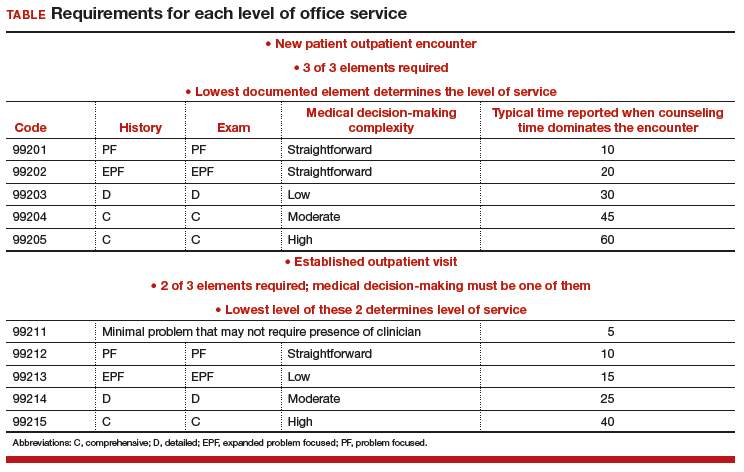
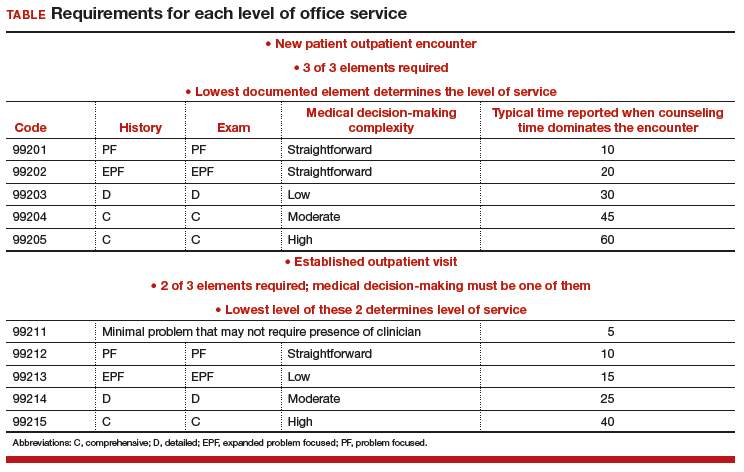
At the time of the encounter, you are responsible for documenting your contact with the patient in enough detail to support billing a CPT evaluation and management (E/M) code at the level selected and/or any procedures or other services performed. The TABLE provides an overview of the requirements for each level of office service.
If both an E/M and a procedure are performed on the same date of service, the E/M must be documented to show it was separate from the procedure and that the work was significantly more than would be required to accomplish the procedure. Documentation of the procedure should include the indication, steps performed, findings, the patient’s condition afterward, and instructions for aftercare or follow-up.
If you use an electronic health record for reporting, you may be the one responsible for selecting both the CPT code for services performed and an ICD-10-CM code(s) to establish the medical need for them. Select the most accurate CPT codes, and clearly link them to a supporting diagnosis for each service that will be billed. If more than one diagnosis is applicable, the first one linked to any given service should represent the most important justification, as not all payers will accept more than one diagnosis code on the claim per service billed.
If the billing staff is assigned the task of selecting the CPT and/or ICD-10-CM diagnostic codes based on your documentation, they should be well versed in the services, procedures, and diagnoses reported for their ObGyn practice.
The actual code selection may end up being a joint venture between the clinician and the staff to ensure that accurate information will be entered on the claim. Good and frequent clinician-staff communication on billing of services can transform average reimbursement into maximized reimbursement.
Be aware of bundles
Sometimes more than one service or procedure is listed on a claim on the same date of service. However, it is important to identify all potential bundles before billing to ensure correct payment. For instance, payers like to bundle an E/M service and a procedure, or you may be in the global period (defined below) of a surgery but need to report an unrelated service.
You and your staff must work together to ensure the claim is submitted with the correct modifiers; on the other hand, you may decide that a better method of coding is in order. Some payers, for example, will not reimburse both an insertion and a removal of an intrauterine device (IUD) on the same date of service. If that does happen, a modifier on the removal code might save the day, rather than billing 2 codes.
Continue to: Manage the modifiers
Manage the modifiers
Sometimes the code billed requires a modifier to ensure payment. Typical modifiers used in an ObGyn office setting include the following:
- 22, Increased procedural services (the clinician must assign a fee that is higher than the usual fee for the procedure and be able to document CPT equivalents to the work involved)
- 24, Unrelated E/M during the postoperative period (note that this modifier does not apply during the antepartum period for pregnancy)
- 25, Significant and separate E/M on the same date as another service or minor procedure
- 52, Reduced services (generally, the payer will expect an explanation of the reduced service and will determine payment accordingly)
- 57, Decision to perform major surgery the day of or the day before the surgery
- 59, Distinct procedural service (used when 2 procedures are bundled and a modifier is allowed). Note that payment reductions for multiple procedures will still apply.
- 79, Unrelated procedure during the postoperative period (usually paid at the full allowable).
Organize the order of services on the claim
For an outpatient claim that includes both an E/M service and procedures, the order of the services—not the order in which they were performed—may be important to obtaining maximum reimbursement. In general, payers will pay in full for a supported E/M service no matter where it appears on the claim, but they apply reductions only for multiple procedures.
For instance, if you insert levonorgestrel implants on the same date as you remove a large polyp from the cervix, you would want to report the code with the highest relative value unit (RVU) first. In this case, it would be 11981 (4.05 RVUs), 57500 (3.61 RVUs).
In the IUD case mentioned earlier (removal and insertion of IUDs on the same date), the order of the codes, assuming the payer reimburses for both, will be even more important since removal usually has a higher payment: 58301 (2.70 RUVs), 58300 (1.54 RVUs).
Coding considerations for surgical services
Surgical services performed in a hospital or ambulatory surgical center present another set of must-dos to ensure timely and fair reimbursement.
Grasp the ‘global package’ concept
Understanding this concept can be crucial to getting paid for additional services during this time period and correct billing for any E/M services performed prior to surgery. In general, the routine history and physical examination performed prior to a major surgery is considered included in the work and should not be billed separately. Surgical clearance for a patient’s condition, such as hypertension, a heart condition, or lung issues, can be billed separately, but these generally are performed by someone other than the operating surgeon.
Procedures performed in the hospital setting generally will have a 10- or 90-day global period. During this time, any related E/M service should not be billed separately, and the use of modifiers becomes even more important than with office services.
Applicable modifiers for use with hospital surgery can include all those for outpatient services plus:
- 50, Bilateral procedure (for which you may be paid up to 150% of the allowable)
- 58, Staged or related procedure during the postoperative period (this may be paid at the full allowable)
- 62, Co-surgeons (both surgeons bill the same CPT code and both document their involvement in the surgery). Medicare will reimburse each surgeon 62.5% of the allowable.
- 78, Return to the operating room for an unplanned related procedure (the full allowable may be reduced by some payers owing to their belief that this is soon after the original procedure so intraoperative time only is considered).
Be savvy about surgical bundles
Here, it is important to understand all published bundling edits for multiple procedures performed by the same surgeon at the same surgical session. If a code combination is never allowed but the surgery is more intense due to additional work required, a modifier -22 may be your only option. Again, clear, concise documentation of the additional work is imperative to receive the additional payment.
When a modifier is allowed, it generally will be one that denotes a procedure done on bilateral organs (such as the ovaries) when there is no extensive code to cover all of the work or when the additional procedure is “distinct” and meets the criteria for using a modifier 59.
Medicare has expanded the modifier -59 into additional modifiers to further explain the situation. These additional modifiers are:
- XE, A service that is distinct because it occurred during a separate encounter on the same date of service
- XS, A service that is distinct because it was performed on a separate organ/structure
- XP, A service that is distinct because it was performed by a different practitioner
- XU, The use of a service that is distinct because it does not overlap usual components of the main service.
Standards of care: Some steps are inherent to the surgery
Expect to receive claim denials if you bill separately for adhesiolysis during a surgical procedure. Every payer considers this procedure related to access to the surgical site and will deny separate coding. If the lysis was truly significant in terms of work, try reporting the modifier 22 and provide adequate documentation.
Other procedures at the time of surgery that generally are not paid for include 1) examination under anesthesia, 2) any procedure done to check the surgeon’s work (for example, cystoscopy, especially when done after urinary or pelvic reconstruction procedures, or chromotubation following extensive ovariolysis), 3) placement of catheters, and 4) placement of devices to alleviate postsurgical pain.
Bottom line
Maximizing reimbursement involves good documentation, correct CPT codes linked to specific and accurate medical indications, the use of appropriate modifiers, and listing codes in order of their relative values from highest to lowest.
Should a denial or unfair reduction in payment come your way, analyze the rejection to determine the cause and make billing and reporting changes as needed to improve your future reimbursements.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
While reimbursement for ObGyn services seemingly should be a simple matter of putting codes on a claim form, the reality is that it is complex, and it requires a team approach to accomplish timely filing to receive fair and accurate reimbursement.
Reimbursement occurs over the length of the revenue cycle for a patient encounter and involves many steps. It starts when the patient makes an appointment for services and ends when the practice receives payment. Along the way, there must be good clinician documentation and sound knowledge about the billing process (including the Current Procedural Terminology [CPT] or Healthcare Common Procedure Coding System [HCPCS] codes for services), the International Classification of Diseases, Tenth Revision, Clinical Modification [ICD-10-CM] codes that establish medical necessity, the modifiers that alter the meaning of the codes, and, of course, the bundling issues that now accompany many coding situations.
In addition, ObGyn practices must contend with a multitude of payers—from federal to commercial—and must understand and adhere to each payer’s rules and policies to maximize and retain reimbursement.
In this article, I detail stumbling blocks to maximizing reimbursement and how to avoid them.
Coding considerations for office services
Good documentation before, during, and after a patient’s office visit is essential, along with accurate codes, modifiers, and order of services on the claims you submit.
Prep paperwork before the patient encounter
Once a patient makes an appointment, the front-end staff can handle some of the tasks in the cycle. This includes ensuring that the patient’s insurance coverage information is current, informing the patient of any additional information to bring at the time of the visit (such as a patient history form for a new patient visit or a list of current prescriptions), or, if an established patient will be having a procedure, making sure that prior authorization is complete. This streamlines the process, assists the clinician with documentation housekeeping, and ensures that incorrect or missing information does not cause a claim to be denied or not be filed in a timely manner (many payers require submission of an initial claim 30 days from the date of service).
Continue to: Document details of the clinician-patient interaction
Document details of the clinician-patient interaction
At the time of the encounter, you are responsible for documenting your contact with the patient in enough detail to support billing a CPT evaluation and management (E/M) code at the level selected and/or any procedures or other services performed. The TABLE provides an overview of the requirements for each level of office service.
If both an E/M and a procedure are performed on the same date of service, the E/M must be documented to show it was separate from the procedure and that the work was significantly more than would be required to accomplish the procedure. Documentation of the procedure should include the indication, steps performed, findings, the patient’s condition afterward, and instructions for aftercare or follow-up.
If you use an electronic health record for reporting, you may be the one responsible for selecting both the CPT code for services performed and an ICD-10-CM code(s) to establish the medical need for them. Select the most accurate CPT codes, and clearly link them to a supporting diagnosis for each service that will be billed. If more than one diagnosis is applicable, the first one linked to any given service should represent the most important justification, as not all payers will accept more than one diagnosis code on the claim per service billed.
If the billing staff is assigned the task of selecting the CPT and/or ICD-10-CM diagnostic codes based on your documentation, they should be well versed in the services, procedures, and diagnoses reported for their ObGyn practice.
The actual code selection may end up being a joint venture between the clinician and the staff to ensure that accurate information will be entered on the claim. Good and frequent clinician-staff communication on billing of services can transform average reimbursement into maximized reimbursement.
Be aware of bundles
Sometimes more than one service or procedure is listed on a claim on the same date of service. However, it is important to identify all potential bundles before billing to ensure correct payment. For instance, payers like to bundle an E/M service and a procedure, or you may be in the global period (defined below) of a surgery but need to report an unrelated service.
You and your staff must work together to ensure the claim is submitted with the correct modifiers; on the other hand, you may decide that a better method of coding is in order. Some payers, for example, will not reimburse both an insertion and a removal of an intrauterine device (IUD) on the same date of service. If that does happen, a modifier on the removal code might save the day, rather than billing 2 codes.
Continue to: Manage the modifiers
Manage the modifiers
Sometimes the code billed requires a modifier to ensure payment. Typical modifiers used in an ObGyn office setting include the following:
- 22, Increased procedural services (the clinician must assign a fee that is higher than the usual fee for the procedure and be able to document CPT equivalents to the work involved)
- 24, Unrelated E/M during the postoperative period (note that this modifier does not apply during the antepartum period for pregnancy)
- 25, Significant and separate E/M on the same date as another service or minor procedure
- 52, Reduced services (generally, the payer will expect an explanation of the reduced service and will determine payment accordingly)
- 57, Decision to perform major surgery the day of or the day before the surgery
- 59, Distinct procedural service (used when 2 procedures are bundled and a modifier is allowed). Note that payment reductions for multiple procedures will still apply.
- 79, Unrelated procedure during the postoperative period (usually paid at the full allowable).
Organize the order of services on the claim
For an outpatient claim that includes both an E/M service and procedures, the order of the services—not the order in which they were performed—may be important to obtaining maximum reimbursement. In general, payers will pay in full for a supported E/M service no matter where it appears on the claim, but they apply reductions only for multiple procedures.
For instance, if you insert levonorgestrel implants on the same date as you remove a large polyp from the cervix, you would want to report the code with the highest relative value unit (RVU) first. In this case, it would be 11981 (4.05 RVUs), 57500 (3.61 RVUs).
In the IUD case mentioned earlier (removal and insertion of IUDs on the same date), the order of the codes, assuming the payer reimburses for both, will be even more important since removal usually has a higher payment: 58301 (2.70 RUVs), 58300 (1.54 RVUs).
Coding considerations for surgical services
Surgical services performed in a hospital or ambulatory surgical center present another set of must-dos to ensure timely and fair reimbursement.
Grasp the ‘global package’ concept
Understanding this concept can be crucial to getting paid for additional services during this time period and correct billing for any E/M services performed prior to surgery. In general, the routine history and physical examination performed prior to a major surgery is considered included in the work and should not be billed separately. Surgical clearance for a patient’s condition, such as hypertension, a heart condition, or lung issues, can be billed separately, but these generally are performed by someone other than the operating surgeon.
Procedures performed in the hospital setting generally will have a 10- or 90-day global period. During this time, any related E/M service should not be billed separately, and the use of modifiers becomes even more important than with office services.
Applicable modifiers for use with hospital surgery can include all those for outpatient services plus:
- 50, Bilateral procedure (for which you may be paid up to 150% of the allowable)
- 58, Staged or related procedure during the postoperative period (this may be paid at the full allowable)
- 62, Co-surgeons (both surgeons bill the same CPT code and both document their involvement in the surgery). Medicare will reimburse each surgeon 62.5% of the allowable.
- 78, Return to the operating room for an unplanned related procedure (the full allowable may be reduced by some payers owing to their belief that this is soon after the original procedure so intraoperative time only is considered).
Be savvy about surgical bundles
Here, it is important to understand all published bundling edits for multiple procedures performed by the same surgeon at the same surgical session. If a code combination is never allowed but the surgery is more intense due to additional work required, a modifier -22 may be your only option. Again, clear, concise documentation of the additional work is imperative to receive the additional payment.
When a modifier is allowed, it generally will be one that denotes a procedure done on bilateral organs (such as the ovaries) when there is no extensive code to cover all of the work or when the additional procedure is “distinct” and meets the criteria for using a modifier 59.
Medicare has expanded the modifier -59 into additional modifiers to further explain the situation. These additional modifiers are:
- XE, A service that is distinct because it occurred during a separate encounter on the same date of service
- XS, A service that is distinct because it was performed on a separate organ/structure
- XP, A service that is distinct because it was performed by a different practitioner
- XU, The use of a service that is distinct because it does not overlap usual components of the main service.
Standards of care: Some steps are inherent to the surgery
Expect to receive claim denials if you bill separately for adhesiolysis during a surgical procedure. Every payer considers this procedure related to access to the surgical site and will deny separate coding. If the lysis was truly significant in terms of work, try reporting the modifier 22 and provide adequate documentation.
Other procedures at the time of surgery that generally are not paid for include 1) examination under anesthesia, 2) any procedure done to check the surgeon’s work (for example, cystoscopy, especially when done after urinary or pelvic reconstruction procedures, or chromotubation following extensive ovariolysis), 3) placement of catheters, and 4) placement of devices to alleviate postsurgical pain.
Bottom line
Maximizing reimbursement involves good documentation, correct CPT codes linked to specific and accurate medical indications, the use of appropriate modifiers, and listing codes in order of their relative values from highest to lowest.
Should a denial or unfair reduction in payment come your way, analyze the rejection to determine the cause and make billing and reporting changes as needed to improve your future reimbursements.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
While reimbursement for ObGyn services seemingly should be a simple matter of putting codes on a claim form, the reality is that it is complex, and it requires a team approach to accomplish timely filing to receive fair and accurate reimbursement.
Reimbursement occurs over the length of the revenue cycle for a patient encounter and involves many steps. It starts when the patient makes an appointment for services and ends when the practice receives payment. Along the way, there must be good clinician documentation and sound knowledge about the billing process (including the Current Procedural Terminology [CPT] or Healthcare Common Procedure Coding System [HCPCS] codes for services), the International Classification of Diseases, Tenth Revision, Clinical Modification [ICD-10-CM] codes that establish medical necessity, the modifiers that alter the meaning of the codes, and, of course, the bundling issues that now accompany many coding situations.
In addition, ObGyn practices must contend with a multitude of payers—from federal to commercial—and must understand and adhere to each payer’s rules and policies to maximize and retain reimbursement.
In this article, I detail stumbling blocks to maximizing reimbursement and how to avoid them.
Coding considerations for office services
Good documentation before, during, and after a patient’s office visit is essential, along with accurate codes, modifiers, and order of services on the claims you submit.
Prep paperwork before the patient encounter
Once a patient makes an appointment, the front-end staff can handle some of the tasks in the cycle. This includes ensuring that the patient’s insurance coverage information is current, informing the patient of any additional information to bring at the time of the visit (such as a patient history form for a new patient visit or a list of current prescriptions), or, if an established patient will be having a procedure, making sure that prior authorization is complete. This streamlines the process, assists the clinician with documentation housekeeping, and ensures that incorrect or missing information does not cause a claim to be denied or not be filed in a timely manner (many payers require submission of an initial claim 30 days from the date of service).
Continue to: Document details of the clinician-patient interaction
Document details of the clinician-patient interaction
At the time of the encounter, you are responsible for documenting your contact with the patient in enough detail to support billing a CPT evaluation and management (E/M) code at the level selected and/or any procedures or other services performed. The TABLE provides an overview of the requirements for each level of office service.
If both an E/M and a procedure are performed on the same date of service, the E/M must be documented to show it was separate from the procedure and that the work was significantly more than would be required to accomplish the procedure. Documentation of the procedure should include the indication, steps performed, findings, the patient’s condition afterward, and instructions for aftercare or follow-up.
If you use an electronic health record for reporting, you may be the one responsible for selecting both the CPT code for services performed and an ICD-10-CM code(s) to establish the medical need for them. Select the most accurate CPT codes, and clearly link them to a supporting diagnosis for each service that will be billed. If more than one diagnosis is applicable, the first one linked to any given service should represent the most important justification, as not all payers will accept more than one diagnosis code on the claim per service billed.
If the billing staff is assigned the task of selecting the CPT and/or ICD-10-CM diagnostic codes based on your documentation, they should be well versed in the services, procedures, and diagnoses reported for their ObGyn practice.
The actual code selection may end up being a joint venture between the clinician and the staff to ensure that accurate information will be entered on the claim. Good and frequent clinician-staff communication on billing of services can transform average reimbursement into maximized reimbursement.
Be aware of bundles
Sometimes more than one service or procedure is listed on a claim on the same date of service. However, it is important to identify all potential bundles before billing to ensure correct payment. For instance, payers like to bundle an E/M service and a procedure, or you may be in the global period (defined below) of a surgery but need to report an unrelated service.
You and your staff must work together to ensure the claim is submitted with the correct modifiers; on the other hand, you may decide that a better method of coding is in order. Some payers, for example, will not reimburse both an insertion and a removal of an intrauterine device (IUD) on the same date of service. If that does happen, a modifier on the removal code might save the day, rather than billing 2 codes.
Continue to: Manage the modifiers
Manage the modifiers
Sometimes the code billed requires a modifier to ensure payment. Typical modifiers used in an ObGyn office setting include the following:
- 22, Increased procedural services (the clinician must assign a fee that is higher than the usual fee for the procedure and be able to document CPT equivalents to the work involved)
- 24, Unrelated E/M during the postoperative period (note that this modifier does not apply during the antepartum period for pregnancy)
- 25, Significant and separate E/M on the same date as another service or minor procedure
- 52, Reduced services (generally, the payer will expect an explanation of the reduced service and will determine payment accordingly)
- 57, Decision to perform major surgery the day of or the day before the surgery
- 59, Distinct procedural service (used when 2 procedures are bundled and a modifier is allowed). Note that payment reductions for multiple procedures will still apply.
- 79, Unrelated procedure during the postoperative period (usually paid at the full allowable).
Organize the order of services on the claim
For an outpatient claim that includes both an E/M service and procedures, the order of the services—not the order in which they were performed—may be important to obtaining maximum reimbursement. In general, payers will pay in full for a supported E/M service no matter where it appears on the claim, but they apply reductions only for multiple procedures.
For instance, if you insert levonorgestrel implants on the same date as you remove a large polyp from the cervix, you would want to report the code with the highest relative value unit (RVU) first. In this case, it would be 11981 (4.05 RVUs), 57500 (3.61 RVUs).
In the IUD case mentioned earlier (removal and insertion of IUDs on the same date), the order of the codes, assuming the payer reimburses for both, will be even more important since removal usually has a higher payment: 58301 (2.70 RUVs), 58300 (1.54 RVUs).
Coding considerations for surgical services
Surgical services performed in a hospital or ambulatory surgical center present another set of must-dos to ensure timely and fair reimbursement.
Grasp the ‘global package’ concept
Understanding this concept can be crucial to getting paid for additional services during this time period and correct billing for any E/M services performed prior to surgery. In general, the routine history and physical examination performed prior to a major surgery is considered included in the work and should not be billed separately. Surgical clearance for a patient’s condition, such as hypertension, a heart condition, or lung issues, can be billed separately, but these generally are performed by someone other than the operating surgeon.
Procedures performed in the hospital setting generally will have a 10- or 90-day global period. During this time, any related E/M service should not be billed separately, and the use of modifiers becomes even more important than with office services.
Applicable modifiers for use with hospital surgery can include all those for outpatient services plus:
- 50, Bilateral procedure (for which you may be paid up to 150% of the allowable)
- 58, Staged or related procedure during the postoperative period (this may be paid at the full allowable)
- 62, Co-surgeons (both surgeons bill the same CPT code and both document their involvement in the surgery). Medicare will reimburse each surgeon 62.5% of the allowable.
- 78, Return to the operating room for an unplanned related procedure (the full allowable may be reduced by some payers owing to their belief that this is soon after the original procedure so intraoperative time only is considered).
Be savvy about surgical bundles
Here, it is important to understand all published bundling edits for multiple procedures performed by the same surgeon at the same surgical session. If a code combination is never allowed but the surgery is more intense due to additional work required, a modifier -22 may be your only option. Again, clear, concise documentation of the additional work is imperative to receive the additional payment.
When a modifier is allowed, it generally will be one that denotes a procedure done on bilateral organs (such as the ovaries) when there is no extensive code to cover all of the work or when the additional procedure is “distinct” and meets the criteria for using a modifier 59.
Medicare has expanded the modifier -59 into additional modifiers to further explain the situation. These additional modifiers are:
- XE, A service that is distinct because it occurred during a separate encounter on the same date of service
- XS, A service that is distinct because it was performed on a separate organ/structure
- XP, A service that is distinct because it was performed by a different practitioner
- XU, The use of a service that is distinct because it does not overlap usual components of the main service.
Standards of care: Some steps are inherent to the surgery
Expect to receive claim denials if you bill separately for adhesiolysis during a surgical procedure. Every payer considers this procedure related to access to the surgical site and will deny separate coding. If the lysis was truly significant in terms of work, try reporting the modifier 22 and provide adequate documentation.
Other procedures at the time of surgery that generally are not paid for include 1) examination under anesthesia, 2) any procedure done to check the surgeon’s work (for example, cystoscopy, especially when done after urinary or pelvic reconstruction procedures, or chromotubation following extensive ovariolysis), 3) placement of catheters, and 4) placement of devices to alleviate postsurgical pain.
Bottom line
Maximizing reimbursement involves good documentation, correct CPT codes linked to specific and accurate medical indications, the use of appropriate modifiers, and listing codes in order of their relative values from highest to lowest.
Should a denial or unfair reduction in payment come your way, analyze the rejection to determine the cause and make billing and reporting changes as needed to improve your future reimbursements.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Coding considerations in investigating chronic pelvic pain
Nonsurgical interventions for chronic pelvic pain may include evaluation and management visits for managing medications, trigger point injections, or pelvic floor physical therapy. However, while these management options can be coded, some of them may have limitations imposed by payers on the frequency of care and by whom the care may be rendered.
For encounters that involve the management of pain medications, it is important that documentation for each of these visits clearly spells out the progress the patient is making in setting goals for pain management. Frequent office visits may send a flag to the payer for overutilization; complete documentation will go a long way to support the medical necessity of each visit at the level billed.
Who renders treatment?
Sometimes, chronic pelvic pain management involves pelvic floor physical therapy, such as teaching pelvic floor exercises or using biofeedback to control certain aspects of the pain. The majority of payers have strict guidelines dictating who can render these services by way of licensure and training if performed by someone other than the physician, and at what frequency. Typically, the person performing the therapy must be, at minimum, a licensed physical therapist.
Frequency
Frequency is often limited to 1 to 2 times a week in increments of 4 weeks before additional authorization is granted. Again, careful and detailed documentation of the patient’s progress will be crucial to continued therapy.
The TABLE shows typical Current Procedural Terminology (CPT) codes that might be authorized by the payer for this type of management.
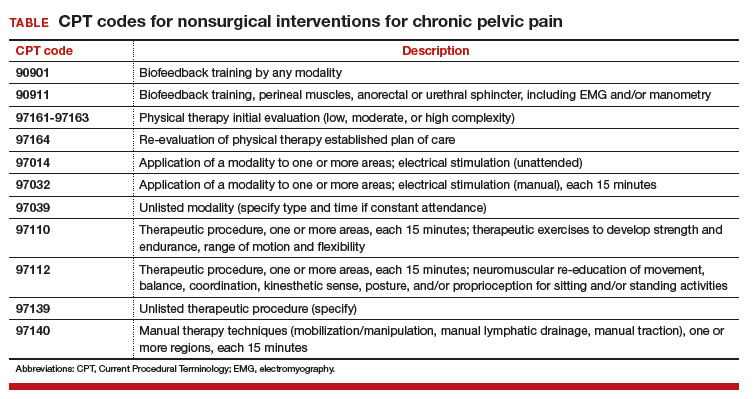
Timed codes
Keep in mind that the “timed” codes listed above are based on the provider’s time spent one-on-one in direct contact with the patient. The time must have been used to provide skilled services and includes pre-, intra-, and posttreatment. CPT also has clarified that if “less than 15 minutes of service is provided, then the reduced services modifier -52 should be appended to the code to identify the reduction of service.” It will therefore be important that the provider accurately document the time involved in the therapy session for these codes.
Trigger point injections
Another treatment option is the use of trigger point injections to control pelvic pain. CPT provides 2 codes to report these:
- 20552, Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s)
- 20553, Injection(s); single or multiple trigger point(s), 3 or more muscles.
Notice that the choice of code depends on the number of muscles the anesthetic is injected into, not the number of injections given at that muscle site.
The relative values units assigned to these codes are based on the injection procedure alone. Normally, the anesthetic used (lidocaine or bupivacaine) can be billed in addition; however, there are no specific Healthcare Common Procedure Coding System (HCPCS) “J” codes for either. Code J2001, Injection, lidocaine HCl, can only be reported for an intravenous infusion, not intramuscular, and the only current code for bupivacaine is an “S” code that is only recognized by some Blue Cross/Blue Shield payers (S0020, Injection, bupivacaine HCl, 30 ml).
Some physicians also inject sodium bicarbonate, but this, too, has no specific “J” code. Because of this, the only correct J code to report these drugs will be J3490, Unclassified drugs. Be sure to include the National Drug Code (NDC) number (usually found on the package insert) for each drug, and an invoice showing your cost with the claim.
ICD-10-CM codes needed for support
Billing for services will not be complete without a supporting diagnostic code. For pelvic pain in particular, 1 or more of the following ICD-10-CM codes may provide the medical justification for the provided nonsurgical services so long as there are no identified psychological factors:
- G89.0, Central pain syndrome
- G89.29, Other chronic pain
- N94.10, Unspecified dyspareunia
- N94.11, Superficial (introital) dyspareunia
- N94.12, Deep dyspareunia
- N94.19, Other specified dyspareunia
- N94.2, Vaginismus
- N94.4, Primary dysmenorrhea
- N94.5, Secondary dysmenorrhea
- N94.6, Dysmenorrhea, unspecified
- N94.810, Vulvar vestibulitis
- N94.818, Other vulvodynia
- N94.819, Vulvodynia, unspecified
- R10.2, Pelvic and perineal pain.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Nonsurgical interventions for chronic pelvic pain may include evaluation and management visits for managing medications, trigger point injections, or pelvic floor physical therapy. However, while these management options can be coded, some of them may have limitations imposed by payers on the frequency of care and by whom the care may be rendered.
For encounters that involve the management of pain medications, it is important that documentation for each of these visits clearly spells out the progress the patient is making in setting goals for pain management. Frequent office visits may send a flag to the payer for overutilization; complete documentation will go a long way to support the medical necessity of each visit at the level billed.
Who renders treatment?
Sometimes, chronic pelvic pain management involves pelvic floor physical therapy, such as teaching pelvic floor exercises or using biofeedback to control certain aspects of the pain. The majority of payers have strict guidelines dictating who can render these services by way of licensure and training if performed by someone other than the physician, and at what frequency. Typically, the person performing the therapy must be, at minimum, a licensed physical therapist.
Frequency
Frequency is often limited to 1 to 2 times a week in increments of 4 weeks before additional authorization is granted. Again, careful and detailed documentation of the patient’s progress will be crucial to continued therapy.
The TABLE shows typical Current Procedural Terminology (CPT) codes that might be authorized by the payer for this type of management.
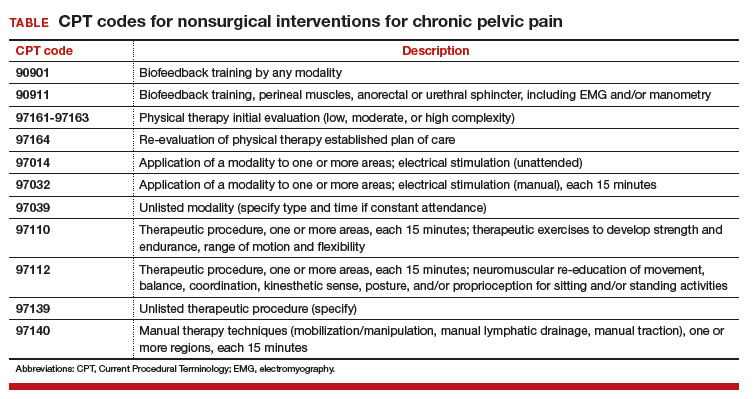
Timed codes
Keep in mind that the “timed” codes listed above are based on the provider’s time spent one-on-one in direct contact with the patient. The time must have been used to provide skilled services and includes pre-, intra-, and posttreatment. CPT also has clarified that if “less than 15 minutes of service is provided, then the reduced services modifier -52 should be appended to the code to identify the reduction of service.” It will therefore be important that the provider accurately document the time involved in the therapy session for these codes.
Trigger point injections
Another treatment option is the use of trigger point injections to control pelvic pain. CPT provides 2 codes to report these:
- 20552, Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s)
- 20553, Injection(s); single or multiple trigger point(s), 3 or more muscles.
Notice that the choice of code depends on the number of muscles the anesthetic is injected into, not the number of injections given at that muscle site.
The relative values units assigned to these codes are based on the injection procedure alone. Normally, the anesthetic used (lidocaine or bupivacaine) can be billed in addition; however, there are no specific Healthcare Common Procedure Coding System (HCPCS) “J” codes for either. Code J2001, Injection, lidocaine HCl, can only be reported for an intravenous infusion, not intramuscular, and the only current code for bupivacaine is an “S” code that is only recognized by some Blue Cross/Blue Shield payers (S0020, Injection, bupivacaine HCl, 30 ml).
Some physicians also inject sodium bicarbonate, but this, too, has no specific “J” code. Because of this, the only correct J code to report these drugs will be J3490, Unclassified drugs. Be sure to include the National Drug Code (NDC) number (usually found on the package insert) for each drug, and an invoice showing your cost with the claim.
ICD-10-CM codes needed for support
Billing for services will not be complete without a supporting diagnostic code. For pelvic pain in particular, 1 or more of the following ICD-10-CM codes may provide the medical justification for the provided nonsurgical services so long as there are no identified psychological factors:
- G89.0, Central pain syndrome
- G89.29, Other chronic pain
- N94.10, Unspecified dyspareunia
- N94.11, Superficial (introital) dyspareunia
- N94.12, Deep dyspareunia
- N94.19, Other specified dyspareunia
- N94.2, Vaginismus
- N94.4, Primary dysmenorrhea
- N94.5, Secondary dysmenorrhea
- N94.6, Dysmenorrhea, unspecified
- N94.810, Vulvar vestibulitis
- N94.818, Other vulvodynia
- N94.819, Vulvodynia, unspecified
- R10.2, Pelvic and perineal pain.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Nonsurgical interventions for chronic pelvic pain may include evaluation and management visits for managing medications, trigger point injections, or pelvic floor physical therapy. However, while these management options can be coded, some of them may have limitations imposed by payers on the frequency of care and by whom the care may be rendered.
For encounters that involve the management of pain medications, it is important that documentation for each of these visits clearly spells out the progress the patient is making in setting goals for pain management. Frequent office visits may send a flag to the payer for overutilization; complete documentation will go a long way to support the medical necessity of each visit at the level billed.
Who renders treatment?
Sometimes, chronic pelvic pain management involves pelvic floor physical therapy, such as teaching pelvic floor exercises or using biofeedback to control certain aspects of the pain. The majority of payers have strict guidelines dictating who can render these services by way of licensure and training if performed by someone other than the physician, and at what frequency. Typically, the person performing the therapy must be, at minimum, a licensed physical therapist.
Frequency
Frequency is often limited to 1 to 2 times a week in increments of 4 weeks before additional authorization is granted. Again, careful and detailed documentation of the patient’s progress will be crucial to continued therapy.
The TABLE shows typical Current Procedural Terminology (CPT) codes that might be authorized by the payer for this type of management.
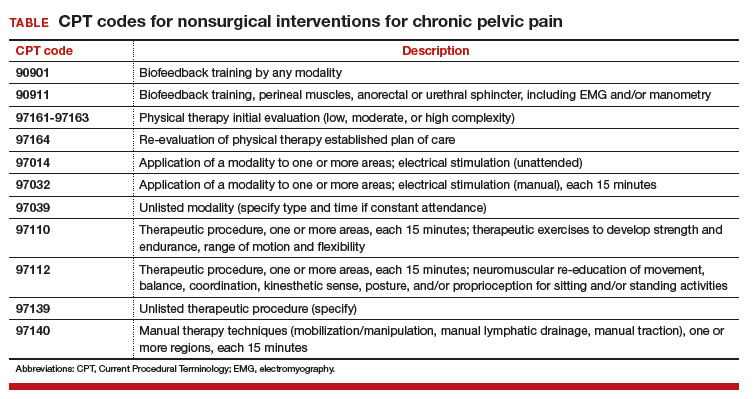
Timed codes
Keep in mind that the “timed” codes listed above are based on the provider’s time spent one-on-one in direct contact with the patient. The time must have been used to provide skilled services and includes pre-, intra-, and posttreatment. CPT also has clarified that if “less than 15 minutes of service is provided, then the reduced services modifier -52 should be appended to the code to identify the reduction of service.” It will therefore be important that the provider accurately document the time involved in the therapy session for these codes.
Trigger point injections
Another treatment option is the use of trigger point injections to control pelvic pain. CPT provides 2 codes to report these:
- 20552, Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s)
- 20553, Injection(s); single or multiple trigger point(s), 3 or more muscles.
Notice that the choice of code depends on the number of muscles the anesthetic is injected into, not the number of injections given at that muscle site.
The relative values units assigned to these codes are based on the injection procedure alone. Normally, the anesthetic used (lidocaine or bupivacaine) can be billed in addition; however, there are no specific Healthcare Common Procedure Coding System (HCPCS) “J” codes for either. Code J2001, Injection, lidocaine HCl, can only be reported for an intravenous infusion, not intramuscular, and the only current code for bupivacaine is an “S” code that is only recognized by some Blue Cross/Blue Shield payers (S0020, Injection, bupivacaine HCl, 30 ml).
Some physicians also inject sodium bicarbonate, but this, too, has no specific “J” code. Because of this, the only correct J code to report these drugs will be J3490, Unclassified drugs. Be sure to include the National Drug Code (NDC) number (usually found on the package insert) for each drug, and an invoice showing your cost with the claim.
ICD-10-CM codes needed for support
Billing for services will not be complete without a supporting diagnostic code. For pelvic pain in particular, 1 or more of the following ICD-10-CM codes may provide the medical justification for the provided nonsurgical services so long as there are no identified psychological factors:
- G89.0, Central pain syndrome
- G89.29, Other chronic pain
- N94.10, Unspecified dyspareunia
- N94.11, Superficial (introital) dyspareunia
- N94.12, Deep dyspareunia
- N94.19, Other specified dyspareunia
- N94.2, Vaginismus
- N94.4, Primary dysmenorrhea
- N94.5, Secondary dysmenorrhea
- N94.6, Dysmenorrhea, unspecified
- N94.810, Vulvar vestibulitis
- N94.818, Other vulvodynia
- N94.819, Vulvodynia, unspecified
- R10.2, Pelvic and perineal pain.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CPT and relative value changes that may affect reimbursement to your ObGyn practice
Another year brings changes to Current Procedural Terminology (CPT) codes (which are developed and copyrighted by the American Medical Association) in the form of additions and revisions, and payments related to resource-based relative value scale (RBRVS) revisions for selected services. As of January 1, 2018, 2 new Category I codes pertain to laparoscopic treatments for gynecologic cancer, and the 4 existing codes for colporrhaphy have been revised to include cystourethroscopy. New Category III codes include 4 for fetal magnetocardiography and 1 for transvaginal tactile imaging. Medicare also has reevaluated certain relative value units (RVUs) in outpatient and facility settings.
New and revised Category I codes
Laparoscopic treatments for gynecologic cancer. Technologic advances in performing laparoscopic procedures have allowed for more extensive laparoscopic surgery for various gynecologic cancers and, to this end, 2 new codes have been added.
First, a new code was added to capture comprehensive laparoscopic surgical staging for gynecologic cancer. This new code, 38573, Laparoscopy, surgical; with bilateral total pelvic lymphadenectomy and peri-aortic lymph node sampling, peritoneal washings, peritoneal biopsy(ies), omentectomy, and diaphragmatic washings, including diaphragmatic and other serosal biopsy(ies), when performed, may not be reported with any other code that includes lymphadenectomy, omentectomy, or hysterectomy. It is intended primarily for a stand-alone staging procedure after an initial biopsy shows a gynecologic malignancy such as ovarian cancer. This new code has been valued at 33.59 RVUs.
Second, a new code was added to capture laparoscopic debulking in conjunction with hysterectomy. The new code, 58575, Laparoscopy, surgical, total hysterectomy for resection of malignancy (tumor debulking), with omentectomy including salpingo-oophorectomy, unilateral or bilateral, when performed, has been valued at 53.62 RVUs. The open equivalent to this new code is 58953, Bilateral salpingo-oophorectomy with omentectomy, total abdominal hysterectomy and radical dissection for debulking.
Cystourethroscopy. The revisions involve no longer permitting separate reporting of 52000, Cystourethroscopy (separate procedure), with the colporrhaphy codes 57240−57265. The rationale behind this change was that surgeons were routinely performing cystoscopy at the time of these procedures and therefore it should become part of the surgical procedure. Currently the Medicare National Correct Coding Initiative (NCCI) bundles 52000 with these 4 codes, but only code 57250 allows for the use of a modifier -59 to bypass the edit if the purpose of the cystoscopy was evaluation of a distinct complaint or problem (such as evaluating patient-expressed urinary symptoms prior to the surgery that were investigated at the time of the prolapse surgery). When codes 57240, 57260, or 57265 are billed along with 52000, the cystoscopy will be denied and a modifier -59 cannot be reported to bypass this edit.
New Category III codes
The new Category III codes represent emerging technology, and it is important to report them, rather than an unlisted code, if the procedures described are performed so that data can be collected for later consideration to make these Category I CPT codes. Since these codes are not assigned relative values, the provider will need to let the payer know which existing CPT Category I code most closely represents the work involved.
Fetal magnetocardiography. The new Category III codes for fetal magnetocardiography describe essentially a fetal electrocardiogram (ECG) that would be performed to assess fetal arrhythmias by placing up to 3 leads on the mother’s abdomen. Possible comparison codes for physician work might include 59050, fetal monitoring by consultant during labor; 93000−93010, 12-lead ECG, or 93040−93042, rhythm strip up to 3 leads. However, because the equipment is very expensive, these codes would not capture practice expense and the physician would have to negotiate a reasonable reimbursement level with the payer, if the magnetocardiography was a covered service. The new codes are as follows:
- 0475T, Recording of fetal magnetic cardiac signal using at least 3 channels; patient recording and storage, data scanning with signal extraction, technical analysis and result, as well as supervision, review, and interpretation of report by a physician or other qualified health care professional
- 0476T, Recording of fetal magnetic cardiac signal using at least 3 channels; patient recording, data scanning, with raw electronic signal transfer of data and storage
- 0477T, Recording of fetal magnetic cardiac signal using at least 3 channels; signal extraction, technical analysis, and result.
Transvaginal tactile imaging. The new Category III code, 0487T, Biomechanical mapping, transvaginal, with report, describes the use of a pressure sensor probe inserted into the vaginal canal to measure and collect data on pelvic muscle strength, elasticity, tissue integrity, and tone. These data produce images in real time that are mapped to produce a report for physician review, interpretation, and report. The data allow quantification of pelvic floor dysfunction and may be useful in determining the most appropriate treatment (whether surgical or medical) for this gynecologic condition. The procedure uses a transvaginal probe like an ultrasound, so using 76830, transvaginal ultrasound, would not be unreasonable as a comparison code as a start.
Medicare relative value changes
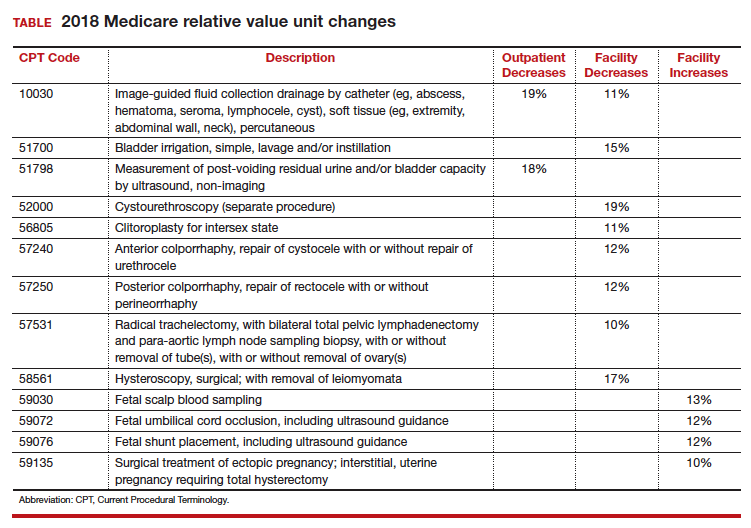
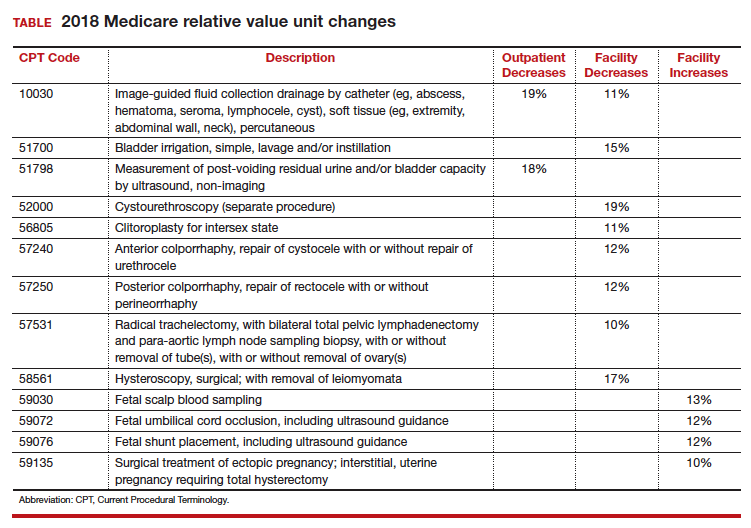
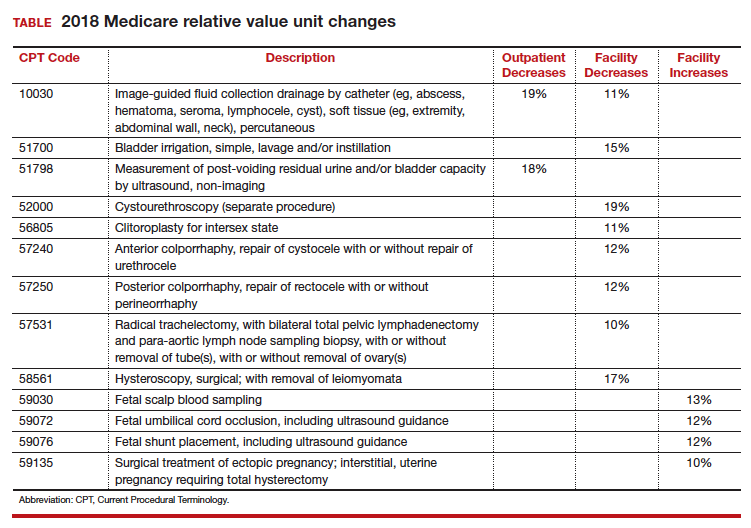
Every year, Medicare reevaluates potentially misvalued CPT codes and this year was no exception. The TABLE represents the winners and losers for codes in the outpatient and facility settings that have increased or decreased RVUs by more than 10%.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Another year brings changes to Current Procedural Terminology (CPT) codes (which are developed and copyrighted by the American Medical Association) in the form of additions and revisions, and payments related to resource-based relative value scale (RBRVS) revisions for selected services. As of January 1, 2018, 2 new Category I codes pertain to laparoscopic treatments for gynecologic cancer, and the 4 existing codes for colporrhaphy have been revised to include cystourethroscopy. New Category III codes include 4 for fetal magnetocardiography and 1 for transvaginal tactile imaging. Medicare also has reevaluated certain relative value units (RVUs) in outpatient and facility settings.
New and revised Category I codes
Laparoscopic treatments for gynecologic cancer. Technologic advances in performing laparoscopic procedures have allowed for more extensive laparoscopic surgery for various gynecologic cancers and, to this end, 2 new codes have been added.
First, a new code was added to capture comprehensive laparoscopic surgical staging for gynecologic cancer. This new code, 38573, Laparoscopy, surgical; with bilateral total pelvic lymphadenectomy and peri-aortic lymph node sampling, peritoneal washings, peritoneal biopsy(ies), omentectomy, and diaphragmatic washings, including diaphragmatic and other serosal biopsy(ies), when performed, may not be reported with any other code that includes lymphadenectomy, omentectomy, or hysterectomy. It is intended primarily for a stand-alone staging procedure after an initial biopsy shows a gynecologic malignancy such as ovarian cancer. This new code has been valued at 33.59 RVUs.
Second, a new code was added to capture laparoscopic debulking in conjunction with hysterectomy. The new code, 58575, Laparoscopy, surgical, total hysterectomy for resection of malignancy (tumor debulking), with omentectomy including salpingo-oophorectomy, unilateral or bilateral, when performed, has been valued at 53.62 RVUs. The open equivalent to this new code is 58953, Bilateral salpingo-oophorectomy with omentectomy, total abdominal hysterectomy and radical dissection for debulking.
Cystourethroscopy. The revisions involve no longer permitting separate reporting of 52000, Cystourethroscopy (separate procedure), with the colporrhaphy codes 57240−57265. The rationale behind this change was that surgeons were routinely performing cystoscopy at the time of these procedures and therefore it should become part of the surgical procedure. Currently the Medicare National Correct Coding Initiative (NCCI) bundles 52000 with these 4 codes, but only code 57250 allows for the use of a modifier -59 to bypass the edit if the purpose of the cystoscopy was evaluation of a distinct complaint or problem (such as evaluating patient-expressed urinary symptoms prior to the surgery that were investigated at the time of the prolapse surgery). When codes 57240, 57260, or 57265 are billed along with 52000, the cystoscopy will be denied and a modifier -59 cannot be reported to bypass this edit.
New Category III codes
The new Category III codes represent emerging technology, and it is important to report them, rather than an unlisted code, if the procedures described are performed so that data can be collected for later consideration to make these Category I CPT codes. Since these codes are not assigned relative values, the provider will need to let the payer know which existing CPT Category I code most closely represents the work involved.
Fetal magnetocardiography. The new Category III codes for fetal magnetocardiography describe essentially a fetal electrocardiogram (ECG) that would be performed to assess fetal arrhythmias by placing up to 3 leads on the mother’s abdomen. Possible comparison codes for physician work might include 59050, fetal monitoring by consultant during labor; 93000−93010, 12-lead ECG, or 93040−93042, rhythm strip up to 3 leads. However, because the equipment is very expensive, these codes would not capture practice expense and the physician would have to negotiate a reasonable reimbursement level with the payer, if the magnetocardiography was a covered service. The new codes are as follows:
- 0475T, Recording of fetal magnetic cardiac signal using at least 3 channels; patient recording and storage, data scanning with signal extraction, technical analysis and result, as well as supervision, review, and interpretation of report by a physician or other qualified health care professional
- 0476T, Recording of fetal magnetic cardiac signal using at least 3 channels; patient recording, data scanning, with raw electronic signal transfer of data and storage
- 0477T, Recording of fetal magnetic cardiac signal using at least 3 channels; signal extraction, technical analysis, and result.
Transvaginal tactile imaging. The new Category III code, 0487T, Biomechanical mapping, transvaginal, with report, describes the use of a pressure sensor probe inserted into the vaginal canal to measure and collect data on pelvic muscle strength, elasticity, tissue integrity, and tone. These data produce images in real time that are mapped to produce a report for physician review, interpretation, and report. The data allow quantification of pelvic floor dysfunction and may be useful in determining the most appropriate treatment (whether surgical or medical) for this gynecologic condition. The procedure uses a transvaginal probe like an ultrasound, so using 76830, transvaginal ultrasound, would not be unreasonable as a comparison code as a start.
Medicare relative value changes
Every year, Medicare reevaluates potentially misvalued CPT codes and this year was no exception. The TABLE represents the winners and losers for codes in the outpatient and facility settings that have increased or decreased RVUs by more than 10%.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Another year brings changes to Current Procedural Terminology (CPT) codes (which are developed and copyrighted by the American Medical Association) in the form of additions and revisions, and payments related to resource-based relative value scale (RBRVS) revisions for selected services. As of January 1, 2018, 2 new Category I codes pertain to laparoscopic treatments for gynecologic cancer, and the 4 existing codes for colporrhaphy have been revised to include cystourethroscopy. New Category III codes include 4 for fetal magnetocardiography and 1 for transvaginal tactile imaging. Medicare also has reevaluated certain relative value units (RVUs) in outpatient and facility settings.
New and revised Category I codes
Laparoscopic treatments for gynecologic cancer. Technologic advances in performing laparoscopic procedures have allowed for more extensive laparoscopic surgery for various gynecologic cancers and, to this end, 2 new codes have been added.
First, a new code was added to capture comprehensive laparoscopic surgical staging for gynecologic cancer. This new code, 38573, Laparoscopy, surgical; with bilateral total pelvic lymphadenectomy and peri-aortic lymph node sampling, peritoneal washings, peritoneal biopsy(ies), omentectomy, and diaphragmatic washings, including diaphragmatic and other serosal biopsy(ies), when performed, may not be reported with any other code that includes lymphadenectomy, omentectomy, or hysterectomy. It is intended primarily for a stand-alone staging procedure after an initial biopsy shows a gynecologic malignancy such as ovarian cancer. This new code has been valued at 33.59 RVUs.
Second, a new code was added to capture laparoscopic debulking in conjunction with hysterectomy. The new code, 58575, Laparoscopy, surgical, total hysterectomy for resection of malignancy (tumor debulking), with omentectomy including salpingo-oophorectomy, unilateral or bilateral, when performed, has been valued at 53.62 RVUs. The open equivalent to this new code is 58953, Bilateral salpingo-oophorectomy with omentectomy, total abdominal hysterectomy and radical dissection for debulking.
Cystourethroscopy. The revisions involve no longer permitting separate reporting of 52000, Cystourethroscopy (separate procedure), with the colporrhaphy codes 57240−57265. The rationale behind this change was that surgeons were routinely performing cystoscopy at the time of these procedures and therefore it should become part of the surgical procedure. Currently the Medicare National Correct Coding Initiative (NCCI) bundles 52000 with these 4 codes, but only code 57250 allows for the use of a modifier -59 to bypass the edit if the purpose of the cystoscopy was evaluation of a distinct complaint or problem (such as evaluating patient-expressed urinary symptoms prior to the surgery that were investigated at the time of the prolapse surgery). When codes 57240, 57260, or 57265 are billed along with 52000, the cystoscopy will be denied and a modifier -59 cannot be reported to bypass this edit.
New Category III codes
The new Category III codes represent emerging technology, and it is important to report them, rather than an unlisted code, if the procedures described are performed so that data can be collected for later consideration to make these Category I CPT codes. Since these codes are not assigned relative values, the provider will need to let the payer know which existing CPT Category I code most closely represents the work involved.
Fetal magnetocardiography. The new Category III codes for fetal magnetocardiography describe essentially a fetal electrocardiogram (ECG) that would be performed to assess fetal arrhythmias by placing up to 3 leads on the mother’s abdomen. Possible comparison codes for physician work might include 59050, fetal monitoring by consultant during labor; 93000−93010, 12-lead ECG, or 93040−93042, rhythm strip up to 3 leads. However, because the equipment is very expensive, these codes would not capture practice expense and the physician would have to negotiate a reasonable reimbursement level with the payer, if the magnetocardiography was a covered service. The new codes are as follows:
- 0475T, Recording of fetal magnetic cardiac signal using at least 3 channels; patient recording and storage, data scanning with signal extraction, technical analysis and result, as well as supervision, review, and interpretation of report by a physician or other qualified health care professional
- 0476T, Recording of fetal magnetic cardiac signal using at least 3 channels; patient recording, data scanning, with raw electronic signal transfer of data and storage
- 0477T, Recording of fetal magnetic cardiac signal using at least 3 channels; signal extraction, technical analysis, and result.
Transvaginal tactile imaging. The new Category III code, 0487T, Biomechanical mapping, transvaginal, with report, describes the use of a pressure sensor probe inserted into the vaginal canal to measure and collect data on pelvic muscle strength, elasticity, tissue integrity, and tone. These data produce images in real time that are mapped to produce a report for physician review, interpretation, and report. The data allow quantification of pelvic floor dysfunction and may be useful in determining the most appropriate treatment (whether surgical or medical) for this gynecologic condition. The procedure uses a transvaginal probe like an ultrasound, so using 76830, transvaginal ultrasound, would not be unreasonable as a comparison code as a start.
Medicare relative value changes
Every year, Medicare reevaluates potentially misvalued CPT codes and this year was no exception. The TABLE represents the winners and losers for codes in the outpatient and facility settings that have increased or decreased RVUs by more than 10%.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
ICD-10-CM code changes: What's new for 2018
The list of new and revised International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes has been published, with changes becoming effective on October 1, 2017. This year, you can look forward to minimal code changes for gynecologic conditions. The biggest change in this category is the addition of codes that describe a lump in the breast according to which breast and the location on the breast, as well as the addition of a code for prophylactic removal of the fallopian tubes. The codes related to obstetrics will have more extensive changes. You will find revisions to the codes for ectopic pregnancy, a new set of codes for addressing an abnormal fetal heart rate during the antepartum period, and, most welcome of all, an expansion of the single code for antenatal testing to 17 very specific codes.
Gynecologic code changes
The single code N63, Unspecified lump in breast, has been expanded to include codes for both the right and the left breast. Code N63 therefore will be considered invalid after October 1, 2018. Expanded codes include:
- N63.0, Unspecified lump in unspecified breast
- N63.1, Unspecified lump in the right breast
- N63.10, Unspecified lump in the right breast, unspecified quadrant
- N63.11, Unspecified lump in the right breast, upper outer quadrant
- N63.12, Unspecified lump in the right breast, upper inner quadrant
- N63.13, Unspecified lump in the right breast, lower outer quadrant
- N63.14, Unspecified lump in the right breast, lower inner quadrant
- N63.2, Unspecified lump in the left breast
- N63.20, Unspecified lump in the left breast, unspecified quadrant
- N63.21, Unspecified lump in the left breast, upper outer quadrant
- N63.22, Unspecified lump in the left breast, upper inner quadrant
- N63.23, Unspecified lump in the left breast, lower outer quadrant
- N63.24, Unspecified lump in the left breast, lower inner quadrant
- N63.3, Unspecified lump in axillary tail
- N63.31, Unspecified lump in axillary tail of the right breast
- N63.32, Unspecified lump in axillary tail of the left breast
- N63.4, Unspecified lump in breast, subareolar
- N63.41, Unspecified lump in right breast, subareolar
- N63.42, Unspecified lump in left breast, subareolar
Other changes to gynecologic codes
There has been a minor change to the description for code Z31.5, Encounter for genetic counseling. It now is described as "Encounter for procreative genetic counseling."
The code Z40.02, Encounter for prophylactic removal of ovary(s), now refers to one or more ovaries without distinction of right or left, and a new code has been added for removal of the fallopian tube(s), Z40.03, Encounter for prophylactic removal of fallopian tube(s).
The inclusion term "endometriosis of the thorax" has been added to code N80.8, Other endometriosis.
The inclusion term "premenstrual dysphoric disorder" has been deleted from code N94.3, Premenstrual tension syndrome. If the patient has been diagnosed with this condition, the code F32.81, Premenstrual dysphoric disorder, should be reported, as this is considered a mental health issue.
The "excludes 1" note under code Z87.41, Personal history of dysplasia of the female genital tract, has been revised. The codes for personal history of intraepithelial neoplasia III that may not be reported with this code are Z86.001 and Z86.008.
Obstetric code changes
The ectopic pregnancy codes have been revised to include references to the right or left structure affected, which means the codes change from 5 digits to 6 digits in length, and the codes O00.10, O00.11, O00.20, and O00.21 will no longer be valid.
- O00.1, Tubal pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.101, Right tubal pregnancy without intrauterine pregnancy
- O00.102, Left tubal pregnancy without intrauterine pregnancy
- O00.109, Unspecified tubal pregnancy without intrauterine pregnancy
- O00.11, Tubal pregnancy with intrauterine pregnancy
- O00.111, Right tubal pregnancy with intrauterine pregnancy
- O00.112, Left tubal pregnancy with intrauterine pregnancy
- O00.119, Unspecified tubal pregnancy with intrauterine pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.2, Ovarian pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
- O00.201, Right ovarian pregnancy without intrauterine pregnancy
- O00.202, Left ovarian pregnancy without intrauterine pregnancy
- O00.209, Unspecified ovarian pregnancy without intrauterine pregnancy
- O00.21, Ovarian pregnancy with intrauterine pregnancy
- O00.211, Right ovarian pregnancy with intrauterine pregnancy
- O00.212, Left ovarian pregnancy with intrauterine pregnancy
- O00.219, Unspecified ovarian pregnancy with intrauterine pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
New codes for fetal heart rate abnormalities
New codes have been added to report a fetal heart rate or rhythm abnormality during the antepartum period. Until now, there only has been a code that addresses this issue during labor and delivery, O76, Abnormality in fetal heart rate and rhythm complicating labor and delivery.
- O36.83, Maternal care for abnormalities of the fetal heart rate or rhythm
- O36.831, Maternal care for abnormalities of the fetal heart rate or rhythm, first trimester
- O36.832, Maternal care for abnormalities of the fetal heart rate or rhythm, second trimester
- O36.833, Maternal care for abnormalities of the fetal heart rate or rhythm, third trimester
- O36.839, Maternal care for abnormalities of the fetal heart rate or rhythm, unspecified trimester
Several codes redefined
ICD-10 has corrected an "excludes" note error for the code O99.1, Other diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism complicating pregnancy, childbirth, and the puerperium. In 2017, any hemorrhage with coagulation defects defined in code category O45.- or codes O46.0-, O67.0, or O72.3 could be reported with O99.1. This set of codes has now been redefined as an "excludes 1" note, which means that they may not be reported with O99.1 since they are considered inclusive.
More specific codes added for antenatal screening
Great news for those awaiting a more specific code for antenatal screening: The code Z36 has been expanded to more closely match the codes that were available in ICD-9-CM, but it goes beyond the basic list in that codes have been added for things like nonvisualization of anatomic structures on a previous scan and screening for cervical length and fetal lung maturity. Be sure to pay attention to the excludes notes and other inclusive terms.
- Z36, Encounter for antenatal screening of mother (Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease.)
Includes: Encounter for placental sample (taken vaginally)
Excludes 2: O28.-, Abnormal findings on antenatal screening of mother
- Z36.5, Encounter for antenatal screening for isoimmunization
- Z36.4, Encounter for antenatal screening for fetal growth retardation
Intrauterine growth restriction (IUGR)/small-for-dates - Z36.3, Encounter for antenatal screening for malformations
Screening for a suspected anomaly - Z36.2, Encounter for other antenatal screening follow-up
Nonvisualized anatomy on a previous scan - Z36.1, Encounter for antenatal screening for raised alpha-fetoprotein level
Encounter for antenatal screening for elevated maternal serum alpha-fetoprotein level - Z36.0, Encounter for antenatal screening for chromosomal anomalies
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.8A, Encounter for antenatal screening for other genetic defects
- Z36.89, Encounter for other specified antenatal screening
- Z36.88, Encounter for antenatal screening for fetal macrosomia
Screening for large-for-dates - Z36.87, Encounter for antenatal screening for uncertain dates
- Z36.86, Encounter for antenatal screening for cervical length
Screening for risk of preterm labor - Z36.85, Encounter for antenatal screening for Streptococcus B
- Z36.84, Encounter for antenatal screening for fetal lung maturity
- Z36.83, Encounter for fetal screening for congenital cardiac abnormalities
- Z36.82, Encounter for antenatal screening for nuchal translucency
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.9, Encounter for antenatal screening, unspecified
Code changes for abortion and complications
The code range for use with Z3A, weeks of gestation, has changed from O00-O9A to O09-O9A to reflect the guideline change last year to remove the requirement to use this code with any code that describes pregnancy with an abortive outcome (codes O00-O08).
In addition, if a patient has retained products of conception (POC) after either a spontaneous or elective abortion, report the "without complication" code for the retained POC (O03.4, Incomplete spontaneous abortion without complication, or O07.4, Failed attempted termination of pregnancy without complication). If any other complication occurred in addition to the retained POC, use the code for that particular complication and not O03.4 or O07.4.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The list of new and revised International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes has been published, with changes becoming effective on October 1, 2017. This year, you can look forward to minimal code changes for gynecologic conditions. The biggest change in this category is the addition of codes that describe a lump in the breast according to which breast and the location on the breast, as well as the addition of a code for prophylactic removal of the fallopian tubes. The codes related to obstetrics will have more extensive changes. You will find revisions to the codes for ectopic pregnancy, a new set of codes for addressing an abnormal fetal heart rate during the antepartum period, and, most welcome of all, an expansion of the single code for antenatal testing to 17 very specific codes.
Gynecologic code changes
The single code N63, Unspecified lump in breast, has been expanded to include codes for both the right and the left breast. Code N63 therefore will be considered invalid after October 1, 2018. Expanded codes include:
- N63.0, Unspecified lump in unspecified breast
- N63.1, Unspecified lump in the right breast
- N63.10, Unspecified lump in the right breast, unspecified quadrant
- N63.11, Unspecified lump in the right breast, upper outer quadrant
- N63.12, Unspecified lump in the right breast, upper inner quadrant
- N63.13, Unspecified lump in the right breast, lower outer quadrant
- N63.14, Unspecified lump in the right breast, lower inner quadrant
- N63.2, Unspecified lump in the left breast
- N63.20, Unspecified lump in the left breast, unspecified quadrant
- N63.21, Unspecified lump in the left breast, upper outer quadrant
- N63.22, Unspecified lump in the left breast, upper inner quadrant
- N63.23, Unspecified lump in the left breast, lower outer quadrant
- N63.24, Unspecified lump in the left breast, lower inner quadrant
- N63.3, Unspecified lump in axillary tail
- N63.31, Unspecified lump in axillary tail of the right breast
- N63.32, Unspecified lump in axillary tail of the left breast
- N63.4, Unspecified lump in breast, subareolar
- N63.41, Unspecified lump in right breast, subareolar
- N63.42, Unspecified lump in left breast, subareolar
Other changes to gynecologic codes
There has been a minor change to the description for code Z31.5, Encounter for genetic counseling. It now is described as "Encounter for procreative genetic counseling."
The code Z40.02, Encounter for prophylactic removal of ovary(s), now refers to one or more ovaries without distinction of right or left, and a new code has been added for removal of the fallopian tube(s), Z40.03, Encounter for prophylactic removal of fallopian tube(s).
The inclusion term "endometriosis of the thorax" has been added to code N80.8, Other endometriosis.
The inclusion term "premenstrual dysphoric disorder" has been deleted from code N94.3, Premenstrual tension syndrome. If the patient has been diagnosed with this condition, the code F32.81, Premenstrual dysphoric disorder, should be reported, as this is considered a mental health issue.
The "excludes 1" note under code Z87.41, Personal history of dysplasia of the female genital tract, has been revised. The codes for personal history of intraepithelial neoplasia III that may not be reported with this code are Z86.001 and Z86.008.
Obstetric code changes
The ectopic pregnancy codes have been revised to include references to the right or left structure affected, which means the codes change from 5 digits to 6 digits in length, and the codes O00.10, O00.11, O00.20, and O00.21 will no longer be valid.
- O00.1, Tubal pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.101, Right tubal pregnancy without intrauterine pregnancy
- O00.102, Left tubal pregnancy without intrauterine pregnancy
- O00.109, Unspecified tubal pregnancy without intrauterine pregnancy
- O00.11, Tubal pregnancy with intrauterine pregnancy
- O00.111, Right tubal pregnancy with intrauterine pregnancy
- O00.112, Left tubal pregnancy with intrauterine pregnancy
- O00.119, Unspecified tubal pregnancy with intrauterine pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.2, Ovarian pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
- O00.201, Right ovarian pregnancy without intrauterine pregnancy
- O00.202, Left ovarian pregnancy without intrauterine pregnancy
- O00.209, Unspecified ovarian pregnancy without intrauterine pregnancy
- O00.21, Ovarian pregnancy with intrauterine pregnancy
- O00.211, Right ovarian pregnancy with intrauterine pregnancy
- O00.212, Left ovarian pregnancy with intrauterine pregnancy
- O00.219, Unspecified ovarian pregnancy with intrauterine pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
New codes for fetal heart rate abnormalities
New codes have been added to report a fetal heart rate or rhythm abnormality during the antepartum period. Until now, there only has been a code that addresses this issue during labor and delivery, O76, Abnormality in fetal heart rate and rhythm complicating labor and delivery.
- O36.83, Maternal care for abnormalities of the fetal heart rate or rhythm
- O36.831, Maternal care for abnormalities of the fetal heart rate or rhythm, first trimester
- O36.832, Maternal care for abnormalities of the fetal heart rate or rhythm, second trimester
- O36.833, Maternal care for abnormalities of the fetal heart rate or rhythm, third trimester
- O36.839, Maternal care for abnormalities of the fetal heart rate or rhythm, unspecified trimester
Several codes redefined
ICD-10 has corrected an "excludes" note error for the code O99.1, Other diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism complicating pregnancy, childbirth, and the puerperium. In 2017, any hemorrhage with coagulation defects defined in code category O45.- or codes O46.0-, O67.0, or O72.3 could be reported with O99.1. This set of codes has now been redefined as an "excludes 1" note, which means that they may not be reported with O99.1 since they are considered inclusive.
More specific codes added for antenatal screening
Great news for those awaiting a more specific code for antenatal screening: The code Z36 has been expanded to more closely match the codes that were available in ICD-9-CM, but it goes beyond the basic list in that codes have been added for things like nonvisualization of anatomic structures on a previous scan and screening for cervical length and fetal lung maturity. Be sure to pay attention to the excludes notes and other inclusive terms.
- Z36, Encounter for antenatal screening of mother (Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease.)
Includes: Encounter for placental sample (taken vaginally)
Excludes 2: O28.-, Abnormal findings on antenatal screening of mother
- Z36.5, Encounter for antenatal screening for isoimmunization
- Z36.4, Encounter for antenatal screening for fetal growth retardation
Intrauterine growth restriction (IUGR)/small-for-dates - Z36.3, Encounter for antenatal screening for malformations
Screening for a suspected anomaly - Z36.2, Encounter for other antenatal screening follow-up
Nonvisualized anatomy on a previous scan - Z36.1, Encounter for antenatal screening for raised alpha-fetoprotein level
Encounter for antenatal screening for elevated maternal serum alpha-fetoprotein level - Z36.0, Encounter for antenatal screening for chromosomal anomalies
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.8A, Encounter for antenatal screening for other genetic defects
- Z36.89, Encounter for other specified antenatal screening
- Z36.88, Encounter for antenatal screening for fetal macrosomia
Screening for large-for-dates - Z36.87, Encounter for antenatal screening for uncertain dates
- Z36.86, Encounter for antenatal screening for cervical length
Screening for risk of preterm labor - Z36.85, Encounter for antenatal screening for Streptococcus B
- Z36.84, Encounter for antenatal screening for fetal lung maturity
- Z36.83, Encounter for fetal screening for congenital cardiac abnormalities
- Z36.82, Encounter for antenatal screening for nuchal translucency
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.9, Encounter for antenatal screening, unspecified
Code changes for abortion and complications
The code range for use with Z3A, weeks of gestation, has changed from O00-O9A to O09-O9A to reflect the guideline change last year to remove the requirement to use this code with any code that describes pregnancy with an abortive outcome (codes O00-O08).
In addition, if a patient has retained products of conception (POC) after either a spontaneous or elective abortion, report the "without complication" code for the retained POC (O03.4, Incomplete spontaneous abortion without complication, or O07.4, Failed attempted termination of pregnancy without complication). If any other complication occurred in addition to the retained POC, use the code for that particular complication and not O03.4 or O07.4.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The list of new and revised International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes has been published, with changes becoming effective on October 1, 2017. This year, you can look forward to minimal code changes for gynecologic conditions. The biggest change in this category is the addition of codes that describe a lump in the breast according to which breast and the location on the breast, as well as the addition of a code for prophylactic removal of the fallopian tubes. The codes related to obstetrics will have more extensive changes. You will find revisions to the codes for ectopic pregnancy, a new set of codes for addressing an abnormal fetal heart rate during the antepartum period, and, most welcome of all, an expansion of the single code for antenatal testing to 17 very specific codes.
Gynecologic code changes
The single code N63, Unspecified lump in breast, has been expanded to include codes for both the right and the left breast. Code N63 therefore will be considered invalid after October 1, 2018. Expanded codes include:
- N63.0, Unspecified lump in unspecified breast
- N63.1, Unspecified lump in the right breast
- N63.10, Unspecified lump in the right breast, unspecified quadrant
- N63.11, Unspecified lump in the right breast, upper outer quadrant
- N63.12, Unspecified lump in the right breast, upper inner quadrant
- N63.13, Unspecified lump in the right breast, lower outer quadrant
- N63.14, Unspecified lump in the right breast, lower inner quadrant
- N63.2, Unspecified lump in the left breast
- N63.20, Unspecified lump in the left breast, unspecified quadrant
- N63.21, Unspecified lump in the left breast, upper outer quadrant
- N63.22, Unspecified lump in the left breast, upper inner quadrant
- N63.23, Unspecified lump in the left breast, lower outer quadrant
- N63.24, Unspecified lump in the left breast, lower inner quadrant
- N63.3, Unspecified lump in axillary tail
- N63.31, Unspecified lump in axillary tail of the right breast
- N63.32, Unspecified lump in axillary tail of the left breast
- N63.4, Unspecified lump in breast, subareolar
- N63.41, Unspecified lump in right breast, subareolar
- N63.42, Unspecified lump in left breast, subareolar
Other changes to gynecologic codes
There has been a minor change to the description for code Z31.5, Encounter for genetic counseling. It now is described as "Encounter for procreative genetic counseling."
The code Z40.02, Encounter for prophylactic removal of ovary(s), now refers to one or more ovaries without distinction of right or left, and a new code has been added for removal of the fallopian tube(s), Z40.03, Encounter for prophylactic removal of fallopian tube(s).
The inclusion term "endometriosis of the thorax" has been added to code N80.8, Other endometriosis.
The inclusion term "premenstrual dysphoric disorder" has been deleted from code N94.3, Premenstrual tension syndrome. If the patient has been diagnosed with this condition, the code F32.81, Premenstrual dysphoric disorder, should be reported, as this is considered a mental health issue.
The "excludes 1" note under code Z87.41, Personal history of dysplasia of the female genital tract, has been revised. The codes for personal history of intraepithelial neoplasia III that may not be reported with this code are Z86.001 and Z86.008.
Obstetric code changes
The ectopic pregnancy codes have been revised to include references to the right or left structure affected, which means the codes change from 5 digits to 6 digits in length, and the codes O00.10, O00.11, O00.20, and O00.21 will no longer be valid.
- O00.1, Tubal pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.101, Right tubal pregnancy without intrauterine pregnancy
- O00.102, Left tubal pregnancy without intrauterine pregnancy
- O00.109, Unspecified tubal pregnancy without intrauterine pregnancy
- O00.11, Tubal pregnancy with intrauterine pregnancy
- O00.111, Right tubal pregnancy with intrauterine pregnancy
- O00.112, Left tubal pregnancy with intrauterine pregnancy
- O00.119, Unspecified tubal pregnancy with intrauterine pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.2, Ovarian pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
- O00.201, Right ovarian pregnancy without intrauterine pregnancy
- O00.202, Left ovarian pregnancy without intrauterine pregnancy
- O00.209, Unspecified ovarian pregnancy without intrauterine pregnancy
- O00.21, Ovarian pregnancy with intrauterine pregnancy
- O00.211, Right ovarian pregnancy with intrauterine pregnancy
- O00.212, Left ovarian pregnancy with intrauterine pregnancy
- O00.219, Unspecified ovarian pregnancy with intrauterine pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
New codes for fetal heart rate abnormalities
New codes have been added to report a fetal heart rate or rhythm abnormality during the antepartum period. Until now, there only has been a code that addresses this issue during labor and delivery, O76, Abnormality in fetal heart rate and rhythm complicating labor and delivery.
- O36.83, Maternal care for abnormalities of the fetal heart rate or rhythm
- O36.831, Maternal care for abnormalities of the fetal heart rate or rhythm, first trimester
- O36.832, Maternal care for abnormalities of the fetal heart rate or rhythm, second trimester
- O36.833, Maternal care for abnormalities of the fetal heart rate or rhythm, third trimester
- O36.839, Maternal care for abnormalities of the fetal heart rate or rhythm, unspecified trimester
Several codes redefined
ICD-10 has corrected an "excludes" note error for the code O99.1, Other diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism complicating pregnancy, childbirth, and the puerperium. In 2017, any hemorrhage with coagulation defects defined in code category O45.- or codes O46.0-, O67.0, or O72.3 could be reported with O99.1. This set of codes has now been redefined as an "excludes 1" note, which means that they may not be reported with O99.1 since they are considered inclusive.
More specific codes added for antenatal screening
Great news for those awaiting a more specific code for antenatal screening: The code Z36 has been expanded to more closely match the codes that were available in ICD-9-CM, but it goes beyond the basic list in that codes have been added for things like nonvisualization of anatomic structures on a previous scan and screening for cervical length and fetal lung maturity. Be sure to pay attention to the excludes notes and other inclusive terms.
- Z36, Encounter for antenatal screening of mother (Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease.)
Includes: Encounter for placental sample (taken vaginally)
Excludes 2: O28.-, Abnormal findings on antenatal screening of mother
- Z36.5, Encounter for antenatal screening for isoimmunization
- Z36.4, Encounter for antenatal screening for fetal growth retardation
Intrauterine growth restriction (IUGR)/small-for-dates - Z36.3, Encounter for antenatal screening for malformations
Screening for a suspected anomaly - Z36.2, Encounter for other antenatal screening follow-up
Nonvisualized anatomy on a previous scan - Z36.1, Encounter for antenatal screening for raised alpha-fetoprotein level
Encounter for antenatal screening for elevated maternal serum alpha-fetoprotein level - Z36.0, Encounter for antenatal screening for chromosomal anomalies
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.8A, Encounter for antenatal screening for other genetic defects
- Z36.89, Encounter for other specified antenatal screening
- Z36.88, Encounter for antenatal screening for fetal macrosomia
Screening for large-for-dates - Z36.87, Encounter for antenatal screening for uncertain dates
- Z36.86, Encounter for antenatal screening for cervical length
Screening for risk of preterm labor - Z36.85, Encounter for antenatal screening for Streptococcus B
- Z36.84, Encounter for antenatal screening for fetal lung maturity
- Z36.83, Encounter for fetal screening for congenital cardiac abnormalities
- Z36.82, Encounter for antenatal screening for nuchal translucency
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.9, Encounter for antenatal screening, unspecified
Code changes for abortion and complications
The code range for use with Z3A, weeks of gestation, has changed from O00-O9A to O09-O9A to reflect the guideline change last year to remove the requirement to use this code with any code that describes pregnancy with an abortive outcome (codes O00-O08).
In addition, if a patient has retained products of conception (POC) after either a spontaneous or elective abortion, report the "without complication" code for the retained POC (O03.4, Incomplete spontaneous abortion without complication, or O07.4, Failed attempted termination of pregnancy without complication). If any other complication occurred in addition to the retained POC, use the code for that particular complication and not O03.4 or O07.4.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In-office hysteroscopy procedures: Reimbursement jumps 237%
As it does annually, the Centers for Medicare & Medicaid Services (CMS) has announced changes to the resource-based relative value scale (RBRVS) physician payment system. This system is not static, and each year the CMS identifies codes to review that appear to be either overvalued or undervalued. While the CMS leads this process, the American Medical Association (AMA), working in conjunction with national medical specialty societies, provides annual recommended updates and changes to the CMS via its AMA/Specialty Society RVS Update Committee (RUC).
RVUs defined
Relative value units (RVUs), assigned to most codes found in the AMA’s Current Procedural Terminology (CPT) book, are calculated based on 3 elements: physician work, practice expense, and malpractice cost. For Medicare reimbursement purposes, these elements are adjusted by the current geographic index, and this adjusted RVU is then multiplied by the Medicare calculated annual conversion factor (in fiscal year 2017, that amount is $35.8887) to determine the final allowable for any given provider.
Commercial payers who use the RBRVS system for reimbursement usually calculate their own conversion factors, which they may or may not publish. Such calculation can be based on a percentage increase over the Medicare rate or other factors.
In-office hysteroscopy procedure reimbursement increases
This year, some notable increases and decreases in the practice expense element will impact payment to ObGyn practices. The best news is that for practices in which clinicians have been removing polyps or performing endometrial sampling or a full dilation and curettage (D & C) using a hysteroscope in the office, practice expense reimbursement now will improve dramatically. The practice expense RVU for CPT code 58558, Hysteroscopy, surgical; with sampling (biopsy) of endometrium and/or polypectomy, with or without D & C, has been increased more than 450% in this setting, with an increase from 6.11 in 2016 to 33.82 as of January 2, 2017, which reduces to a 237% increase when the change to the total RVU is calculated.
More new-found income. The only other procedure showing at least a 10% increase in reimbursement in the office setting is the professional component for the ultrasonic guidance for aspiration of ova.
When your reimbursements will decrease
Unfortunately, reimbursement has also been decreased for some CPT code procedures. The urodynamic study code 51784, Electromyography studies (EMG) of anal or urethral sphincter, other than needle, any technique, has decreased in RVU value by about 64%. This is due to cutting by half the physician work, practice expense, and malpractice cost RVU elements. Although hit with a somewhat smaller decrease, code 58562, Hysteroscopy, surgical; with removal of impacted foreign body, also suffered a decrease in all 3 RVU elements in the office setting, amounting to about a 19% decrease.
In the facility setting, the RVU for the code for vaginoplasty has been increased by 10%, but 11 procedures have lost between 11% and 19% of their previous RVU levels in this setting, and more than half are for hysteroscopic procedures. The complete list of codes that have incurred at least a 10% RVU change in 2017 are listed in TABLES 1 and 2 according to place of service.
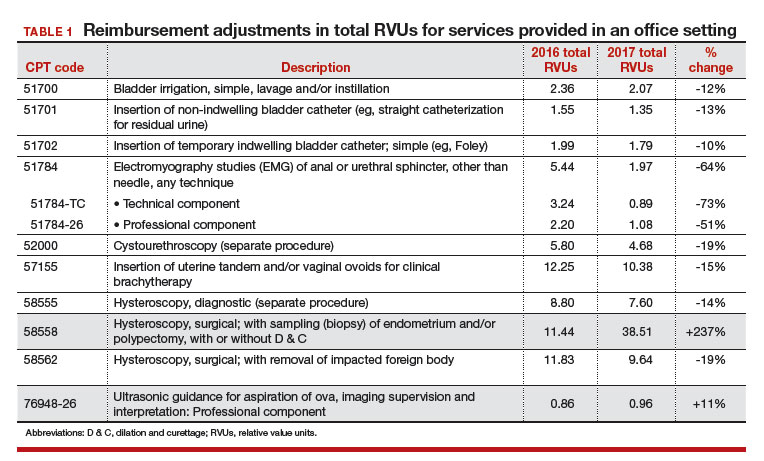
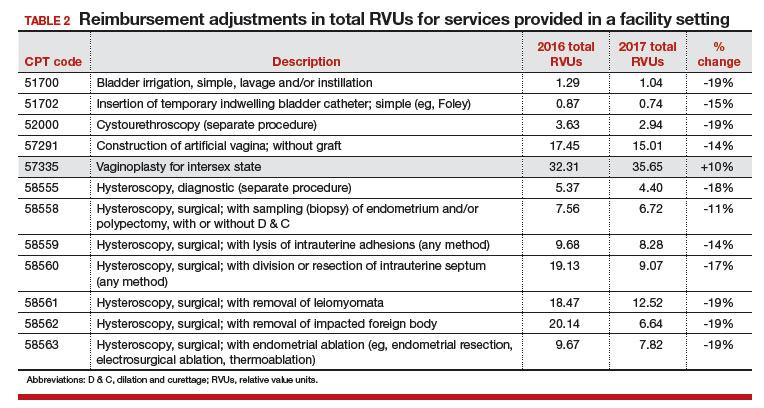
Related article:
GYN coding changes to note for your maximized reimbursement
What’s up next for review and possible adjustment
Finally, as a reminder to all providers, the CMS has identified 3 procedure codes that are potentially misvalued due to their being reported more than 50% of the time with an evaluation and management (E/M) service. These codes represent 0-day procedures and will be evaluated during 2017:
- 57150, Irrigation of vagina and/or application of medicament for treatment of bacterial, parasitic, or fungoid disease
- 57160, Fitting and insertion of pessary or other intravaginal support device
- 58100, Endometrial sampling (biopsy) with or without endocervical sampling (biopsy), without cervical dilation, any method (separate procedure).
The CMS has made it clear that all 0-day procedure codes include evaluation services on the date of service, including the decision to do the procedure. If the CMS examination of data finds that the documentation does not support a separate and significant E/M service at the time of the procedure, the agency will consider adjusting the physician work component. All providers should therefore examine their reporting of an E/M service with 0-day procedures to ensure that the documentation clearly supports doing so.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
As it does annually, the Centers for Medicare & Medicaid Services (CMS) has announced changes to the resource-based relative value scale (RBRVS) physician payment system. This system is not static, and each year the CMS identifies codes to review that appear to be either overvalued or undervalued. While the CMS leads this process, the American Medical Association (AMA), working in conjunction with national medical specialty societies, provides annual recommended updates and changes to the CMS via its AMA/Specialty Society RVS Update Committee (RUC).
RVUs defined
Relative value units (RVUs), assigned to most codes found in the AMA’s Current Procedural Terminology (CPT) book, are calculated based on 3 elements: physician work, practice expense, and malpractice cost. For Medicare reimbursement purposes, these elements are adjusted by the current geographic index, and this adjusted RVU is then multiplied by the Medicare calculated annual conversion factor (in fiscal year 2017, that amount is $35.8887) to determine the final allowable for any given provider.
Commercial payers who use the RBRVS system for reimbursement usually calculate their own conversion factors, which they may or may not publish. Such calculation can be based on a percentage increase over the Medicare rate or other factors.
In-office hysteroscopy procedure reimbursement increases
This year, some notable increases and decreases in the practice expense element will impact payment to ObGyn practices. The best news is that for practices in which clinicians have been removing polyps or performing endometrial sampling or a full dilation and curettage (D & C) using a hysteroscope in the office, practice expense reimbursement now will improve dramatically. The practice expense RVU for CPT code 58558, Hysteroscopy, surgical; with sampling (biopsy) of endometrium and/or polypectomy, with or without D & C, has been increased more than 450% in this setting, with an increase from 6.11 in 2016 to 33.82 as of January 2, 2017, which reduces to a 237% increase when the change to the total RVU is calculated.
More new-found income. The only other procedure showing at least a 10% increase in reimbursement in the office setting is the professional component for the ultrasonic guidance for aspiration of ova.
When your reimbursements will decrease
Unfortunately, reimbursement has also been decreased for some CPT code procedures. The urodynamic study code 51784, Electromyography studies (EMG) of anal or urethral sphincter, other than needle, any technique, has decreased in RVU value by about 64%. This is due to cutting by half the physician work, practice expense, and malpractice cost RVU elements. Although hit with a somewhat smaller decrease, code 58562, Hysteroscopy, surgical; with removal of impacted foreign body, also suffered a decrease in all 3 RVU elements in the office setting, amounting to about a 19% decrease.
In the facility setting, the RVU for the code for vaginoplasty has been increased by 10%, but 11 procedures have lost between 11% and 19% of their previous RVU levels in this setting, and more than half are for hysteroscopic procedures. The complete list of codes that have incurred at least a 10% RVU change in 2017 are listed in TABLES 1 and 2 according to place of service.
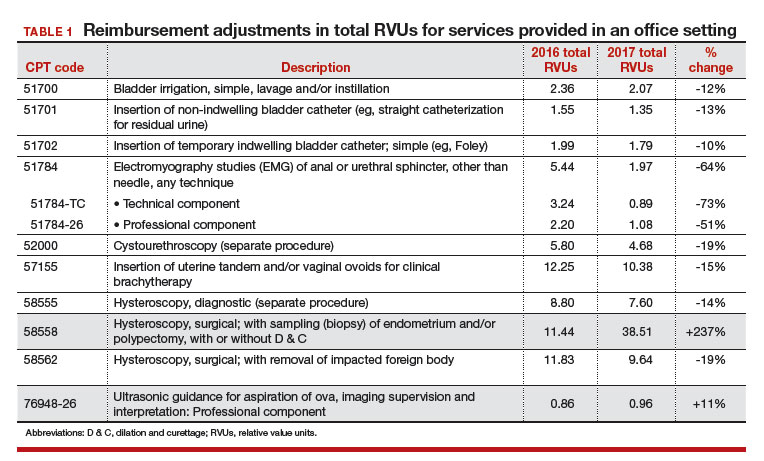
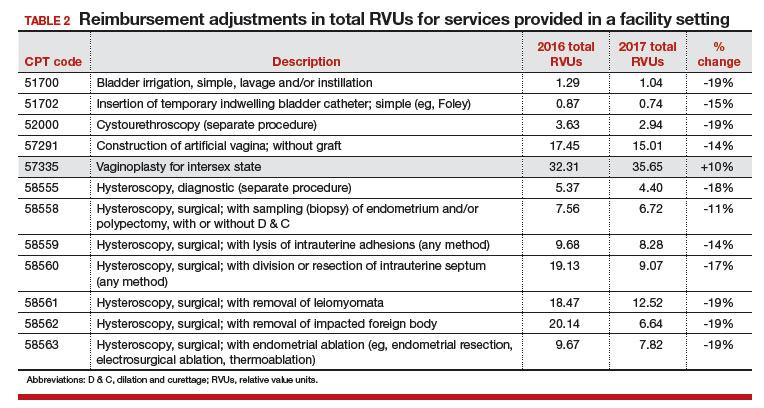
Related article:
GYN coding changes to note for your maximized reimbursement
What’s up next for review and possible adjustment
Finally, as a reminder to all providers, the CMS has identified 3 procedure codes that are potentially misvalued due to their being reported more than 50% of the time with an evaluation and management (E/M) service. These codes represent 0-day procedures and will be evaluated during 2017:
- 57150, Irrigation of vagina and/or application of medicament for treatment of bacterial, parasitic, or fungoid disease
- 57160, Fitting and insertion of pessary or other intravaginal support device
- 58100, Endometrial sampling (biopsy) with or without endocervical sampling (biopsy), without cervical dilation, any method (separate procedure).
The CMS has made it clear that all 0-day procedure codes include evaluation services on the date of service, including the decision to do the procedure. If the CMS examination of data finds that the documentation does not support a separate and significant E/M service at the time of the procedure, the agency will consider adjusting the physician work component. All providers should therefore examine their reporting of an E/M service with 0-day procedures to ensure that the documentation clearly supports doing so.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
As it does annually, the Centers for Medicare & Medicaid Services (CMS) has announced changes to the resource-based relative value scale (RBRVS) physician payment system. This system is not static, and each year the CMS identifies codes to review that appear to be either overvalued or undervalued. While the CMS leads this process, the American Medical Association (AMA), working in conjunction with national medical specialty societies, provides annual recommended updates and changes to the CMS via its AMA/Specialty Society RVS Update Committee (RUC).
RVUs defined
Relative value units (RVUs), assigned to most codes found in the AMA’s Current Procedural Terminology (CPT) book, are calculated based on 3 elements: physician work, practice expense, and malpractice cost. For Medicare reimbursement purposes, these elements are adjusted by the current geographic index, and this adjusted RVU is then multiplied by the Medicare calculated annual conversion factor (in fiscal year 2017, that amount is $35.8887) to determine the final allowable for any given provider.
Commercial payers who use the RBRVS system for reimbursement usually calculate their own conversion factors, which they may or may not publish. Such calculation can be based on a percentage increase over the Medicare rate or other factors.
In-office hysteroscopy procedure reimbursement increases
This year, some notable increases and decreases in the practice expense element will impact payment to ObGyn practices. The best news is that for practices in which clinicians have been removing polyps or performing endometrial sampling or a full dilation and curettage (D & C) using a hysteroscope in the office, practice expense reimbursement now will improve dramatically. The practice expense RVU for CPT code 58558, Hysteroscopy, surgical; with sampling (biopsy) of endometrium and/or polypectomy, with or without D & C, has been increased more than 450% in this setting, with an increase from 6.11 in 2016 to 33.82 as of January 2, 2017, which reduces to a 237% increase when the change to the total RVU is calculated.
More new-found income. The only other procedure showing at least a 10% increase in reimbursement in the office setting is the professional component for the ultrasonic guidance for aspiration of ova.
When your reimbursements will decrease
Unfortunately, reimbursement has also been decreased for some CPT code procedures. The urodynamic study code 51784, Electromyography studies (EMG) of anal or urethral sphincter, other than needle, any technique, has decreased in RVU value by about 64%. This is due to cutting by half the physician work, practice expense, and malpractice cost RVU elements. Although hit with a somewhat smaller decrease, code 58562, Hysteroscopy, surgical; with removal of impacted foreign body, also suffered a decrease in all 3 RVU elements in the office setting, amounting to about a 19% decrease.
In the facility setting, the RVU for the code for vaginoplasty has been increased by 10%, but 11 procedures have lost between 11% and 19% of their previous RVU levels in this setting, and more than half are for hysteroscopic procedures. The complete list of codes that have incurred at least a 10% RVU change in 2017 are listed in TABLES 1 and 2 according to place of service.
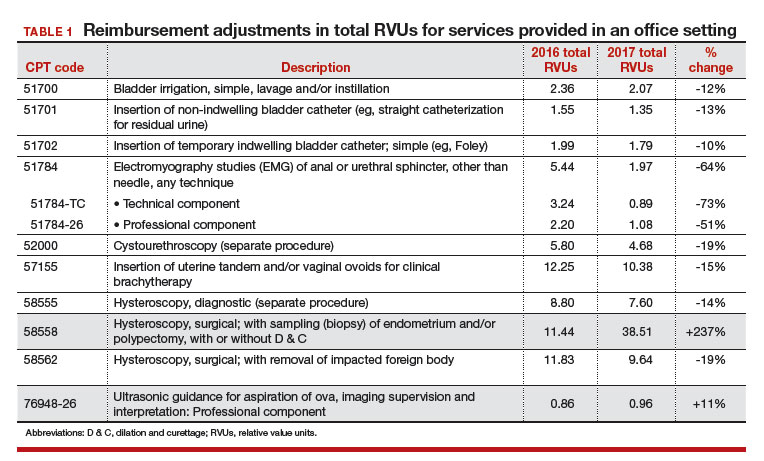
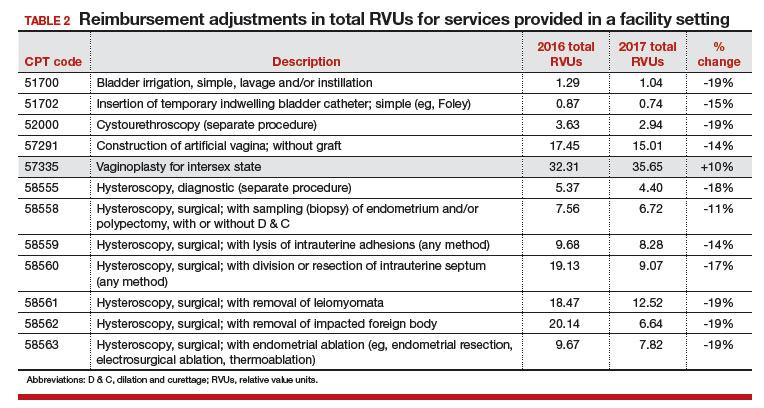
Related article:
GYN coding changes to note for your maximized reimbursement
What’s up next for review and possible adjustment
Finally, as a reminder to all providers, the CMS has identified 3 procedure codes that are potentially misvalued due to their being reported more than 50% of the time with an evaluation and management (E/M) service. These codes represent 0-day procedures and will be evaluated during 2017:
- 57150, Irrigation of vagina and/or application of medicament for treatment of bacterial, parasitic, or fungoid disease
- 57160, Fitting and insertion of pessary or other intravaginal support device
- 58100, Endometrial sampling (biopsy) with or without endocervical sampling (biopsy), without cervical dilation, any method (separate procedure).
The CMS has made it clear that all 0-day procedure codes include evaluation services on the date of service, including the decision to do the procedure. If the CMS examination of data finds that the documentation does not support a separate and significant E/M service at the time of the procedure, the agency will consider adjusting the physician work component. All providers should therefore examine their reporting of an E/M service with 0-day procedures to ensure that the documentation clearly supports doing so.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
IN THIS ARTICLE
- Relative value scale changes
- In-office servicesreimbursement
- In-facility servicesreimbursement
2016 GYN coding changes to note for your maximized reimbursement
In the August 2016 issue of OBG
Urogynecology diagnostic codes
Urogynecologists will find a large number of changes to codes they can select on October 1, 2016. While some codes improve reporting for conditions or symptoms related to urinary issues, many more concern postoperative complications following surgery for devices and grafts applied to the genitourinary system.
The American Urological Association requested new codes to align with a 2009 joint report on the terminology for female pelvic floor dysfunction.1 These codes, along with others, are listed in TABLE 1.
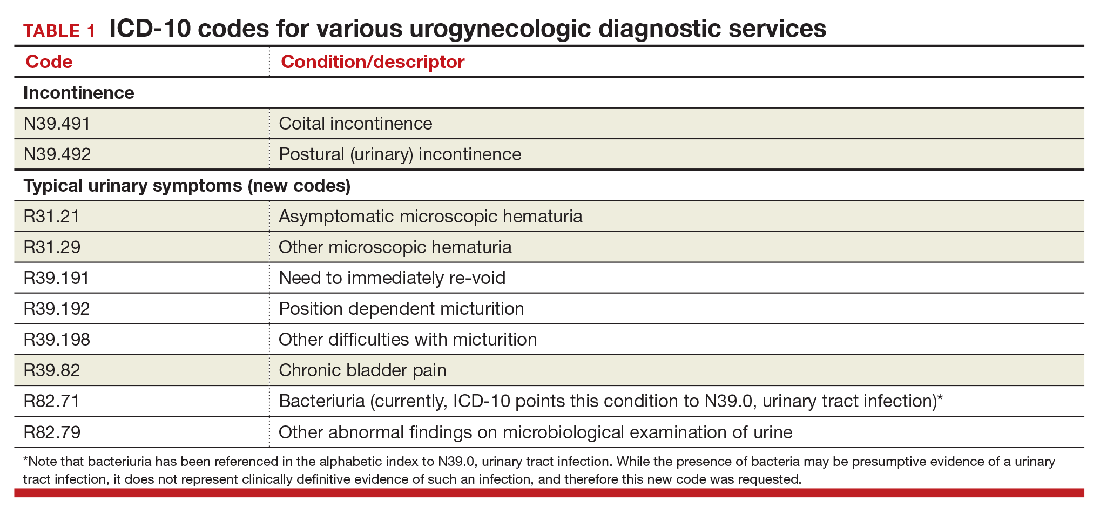
Urinary procedure complication codes
Not every urogynecologist will have an issue after surgery for incontinence, but if they do, there are tons of new and revised codes to address every possible complication the patient may have (TABLE 2). Each of these codes is reported based on whether the complication is being actively treated (initial encounter: final character is A), is being followed up after treatment (subsequent encounter: final character is D), or is caused by another condition (sequela: final character is S).
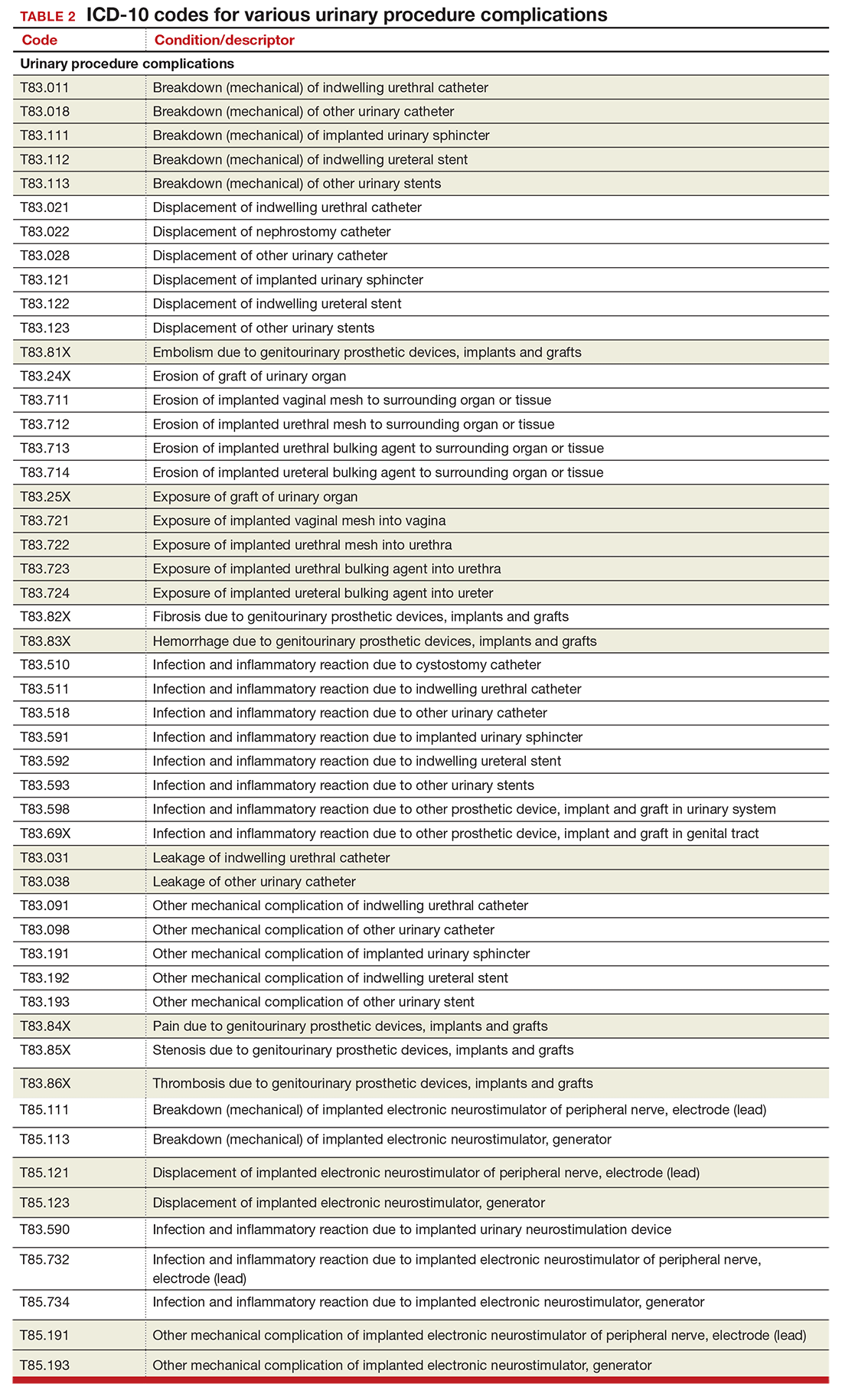
Gynecology-related diagnostic codes
Laterality
If there are 2 organs in the genitourinary system, the chances are good that there is now a right and a left designation code in ICD-10. Documentation should be clear, of course, and if the condition exists on both the right and the left side (even if only one side is being treated actively), list both codes, as there is no bilateral designation in the codes (TABLE 3). And while there is a code for “unspecified side,” providers normally do know which side, so use of this code should be avoided, if possible.
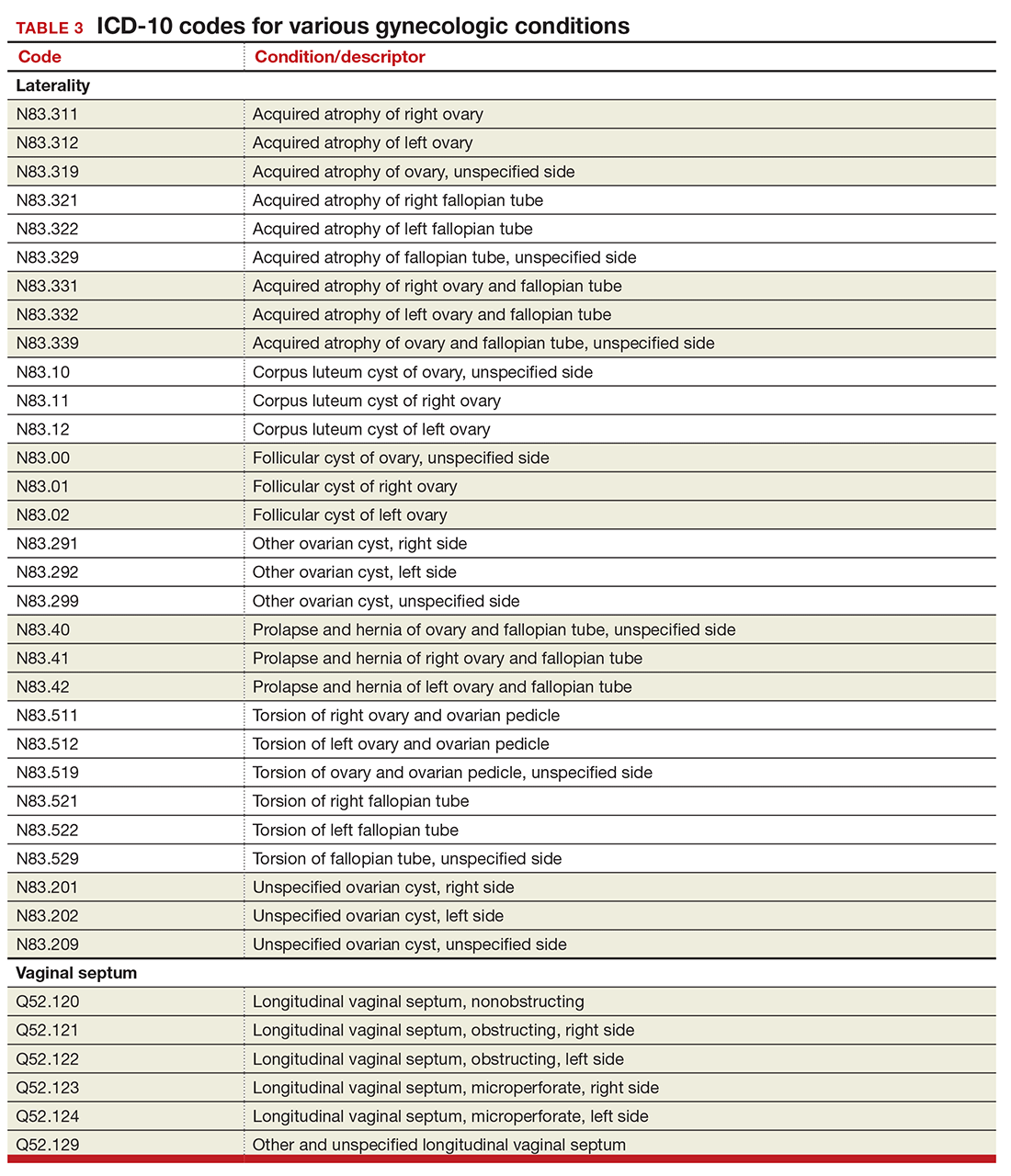
Vaginal septum
The right and left designations extend to the congenital codes for vaginal septum, but they go one step further. The American Congress of Obstetricians and Gynecologists (ACOG) requested that the codes for longitudinal vaginal septum be expanded to differentiate a nonobstructing vaginal septum from an obstructing vaginal septum, in addition to adding laterality to these codes (TABLE 3).2
Mastitis
There are now 2 new codes for inflammation of the breast; one describes mastitis without abscess, while the other code includes an abscess of the breast and nipple (TABLE 4). Once again, documentation will lead to the most specific code to describe the findings.
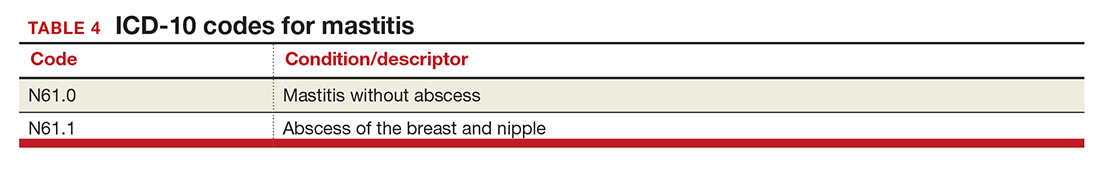
Childhood and prepubertal concerns
The single code for hypertrophy of the vulva has been expanded to include asymmetric labium majus enlargement. This code was requested by ACOG because this is a known clinical diagnosis and the currently available vulvar codes are inadequate for capturing this condition. The vulvar enlargement appears to be in response to hormonal surges during prepuberty and early puberty. Adult hypertrophy, either congenital or acquired from childbirth or as a late result of an old injury, would be reported by the “other specified” code (TABLE 5).
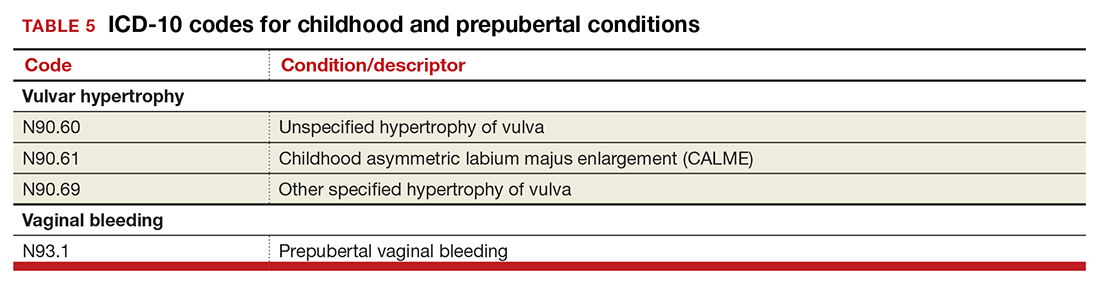
The causes of prepubertal bleeding vary and include the presence of a foreign object, tumors, or fluctuations in hormones, but prepubertal bleeding differs from the bleeding associated with normal menstruation. For that reason, ACOG requested a code that better captures the nature of the condition before a thorough work-up has pinpointed the cause (TABLE 5). Once the cause of the bleeding is known, a more specific diagnosis would then be reported (eg, D28.1, Benign neoplasm of vagina, or T19.2XXA, Foreign body in vulva and vagina, initial encounter).
Dypareunia
Additional documentation for dyspareunia will now be required to ensure that the most specific code is reported. In this case, the clinician should identify whether the pain is superficial or deep to better report on female pelvic floor dysfunction and to support the different treatments based on the location of the pain (TABLE 6). Deep dyspareunia would be felt in the mid or upper vagina.
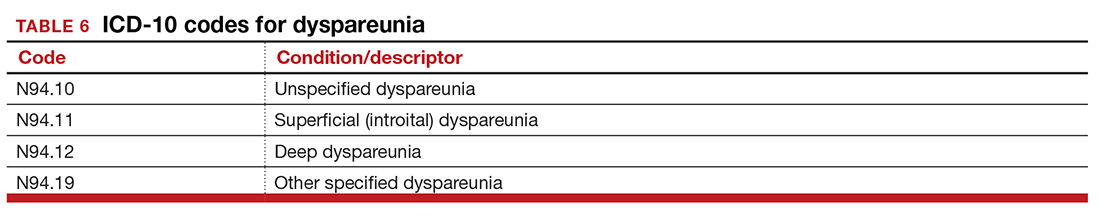
Postoperative hemorrhage and hematoma
The codes for postprocedural hemorrhage and hematomas have received a face-lift: the single codes for these 2 complications will be split so that each can be reported separately (TABLE 7). Note that the new codes require that the condition be found following the initial surgery, and the code selected depends on whether the surgery involved the genitourinary system or another system.
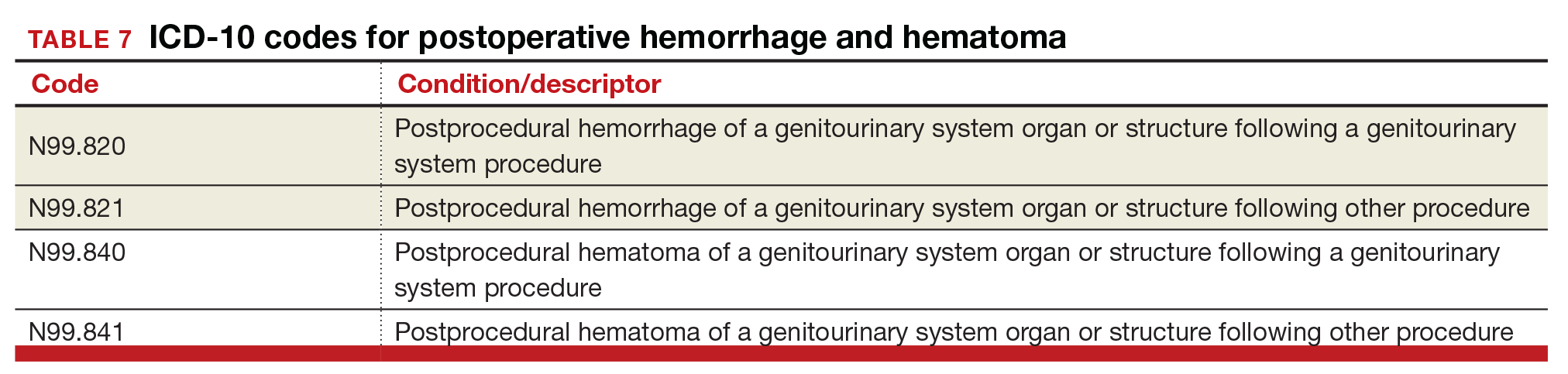
Hormone malignancy status
The new Z19 codes will augment information known about a patient’s neoplasm (TABLE 8). The ICD-10 rule states that the type and location of the neoplasm are always coded first, followed by one of the new Z19 codes, if known.
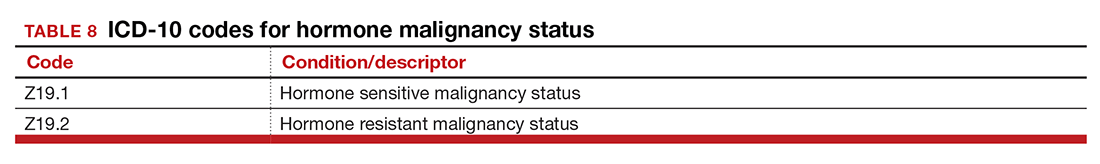
Viral hepatitis carrier
The more specific code for type of viral hepatitis the patient is a carrier of has been bundled into a single code for viral hepatitis (TABLE 9). Carrier status in ICD-10 is defined as a person who harbors the specific organisms of a disease, does not currently have any symptoms, but is capable of transmitting the infection.
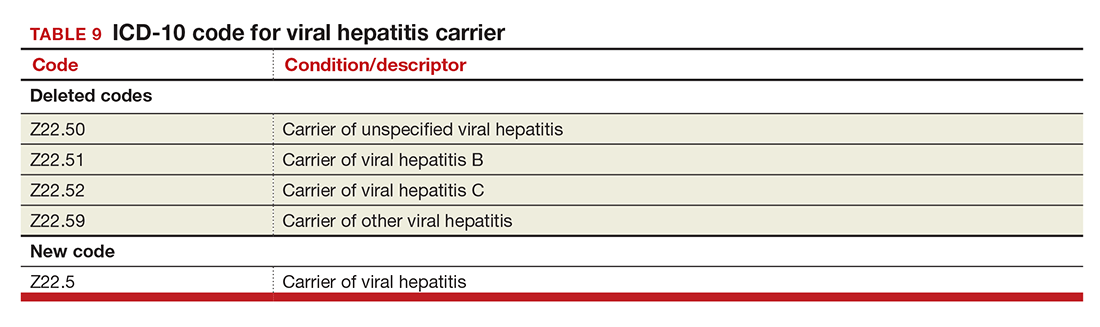
Contraception
The good news is that the ICD-9 code for contraceptive subdermal implants has been added to ICD-10 coding. In addition, the codes for contraceptive methods have been expanded to also include vaginal rings and transdermal patches (TABLE 10).
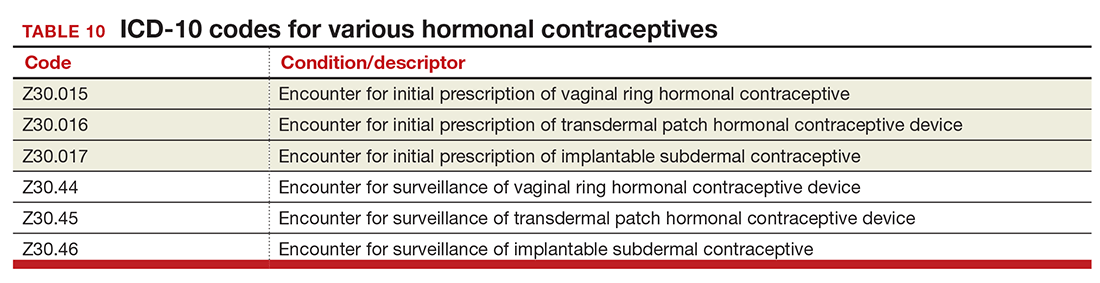
Miscellaneous code changes
Counseling a patient prior to pregnancy just got easier with the addition of a code for gestational carriers. Also, the old ICD-9 code that let a payer know that a procedure was converted from a laparoscopic to an open abdominal procedure is back (TABLE 11).
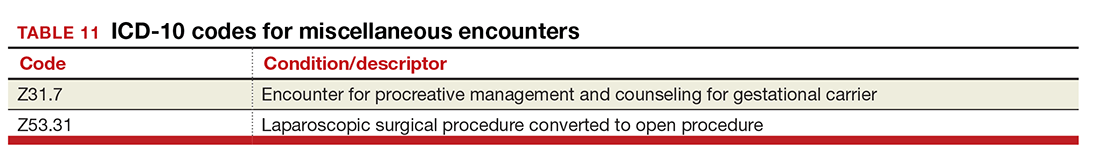
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. September 23–24, 2014;28–29. https://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed August 30, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. March 18–19, 2015. http://www.cdc.gov/nchs/data/icd/Tentative_Agenda_March%202015_Final.pdf. Accessed August 30, 2016.
In the August 2016 issue of OBG
Urogynecology diagnostic codes
Urogynecologists will find a large number of changes to codes they can select on October 1, 2016. While some codes improve reporting for conditions or symptoms related to urinary issues, many more concern postoperative complications following surgery for devices and grafts applied to the genitourinary system.
The American Urological Association requested new codes to align with a 2009 joint report on the terminology for female pelvic floor dysfunction.1 These codes, along with others, are listed in TABLE 1.
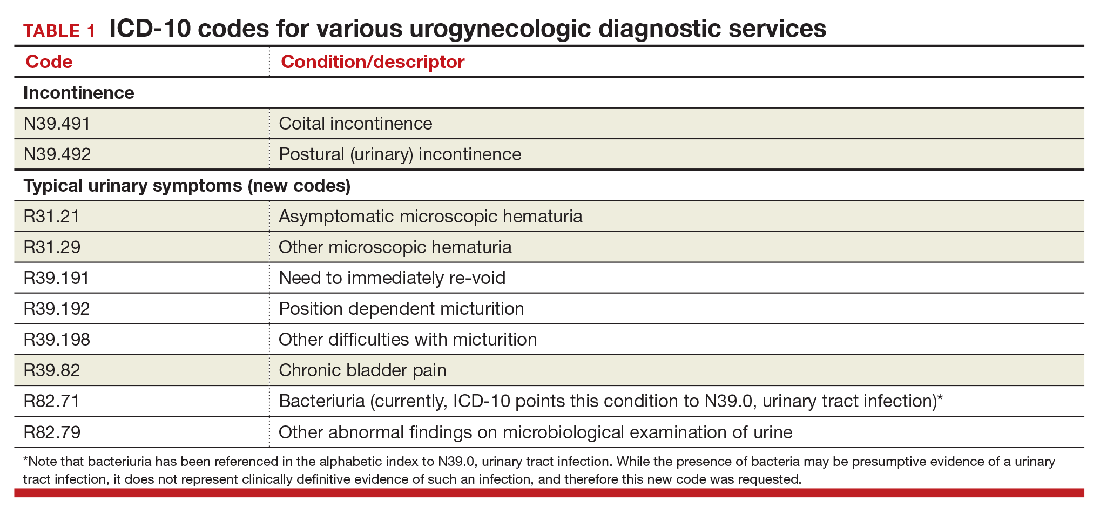
Urinary procedure complication codes
Not every urogynecologist will have an issue after surgery for incontinence, but if they do, there are tons of new and revised codes to address every possible complication the patient may have (TABLE 2). Each of these codes is reported based on whether the complication is being actively treated (initial encounter: final character is A), is being followed up after treatment (subsequent encounter: final character is D), or is caused by another condition (sequela: final character is S).
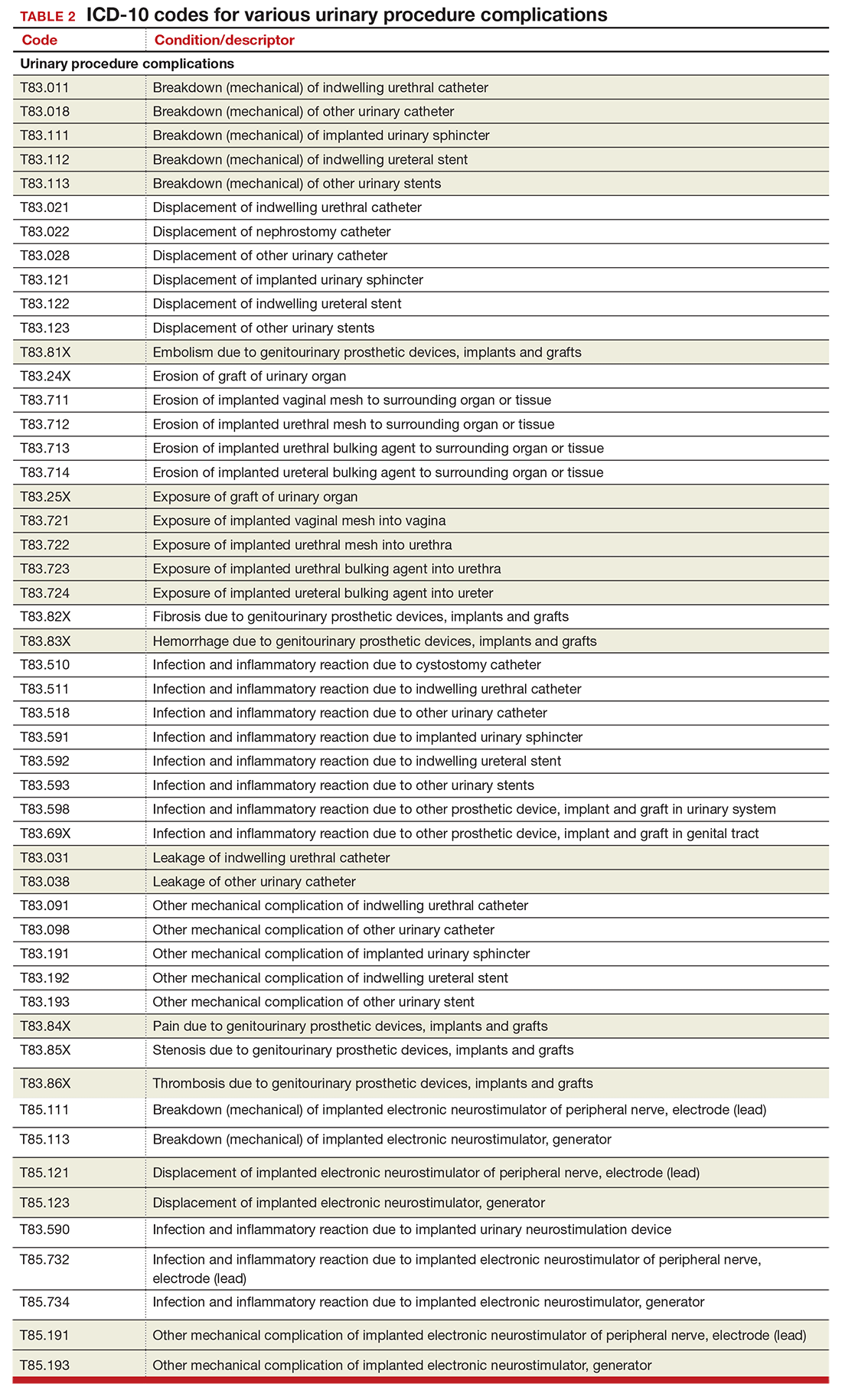
Gynecology-related diagnostic codes
Laterality
If there are 2 organs in the genitourinary system, the chances are good that there is now a right and a left designation code in ICD-10. Documentation should be clear, of course, and if the condition exists on both the right and the left side (even if only one side is being treated actively), list both codes, as there is no bilateral designation in the codes (TABLE 3). And while there is a code for “unspecified side,” providers normally do know which side, so use of this code should be avoided, if possible.
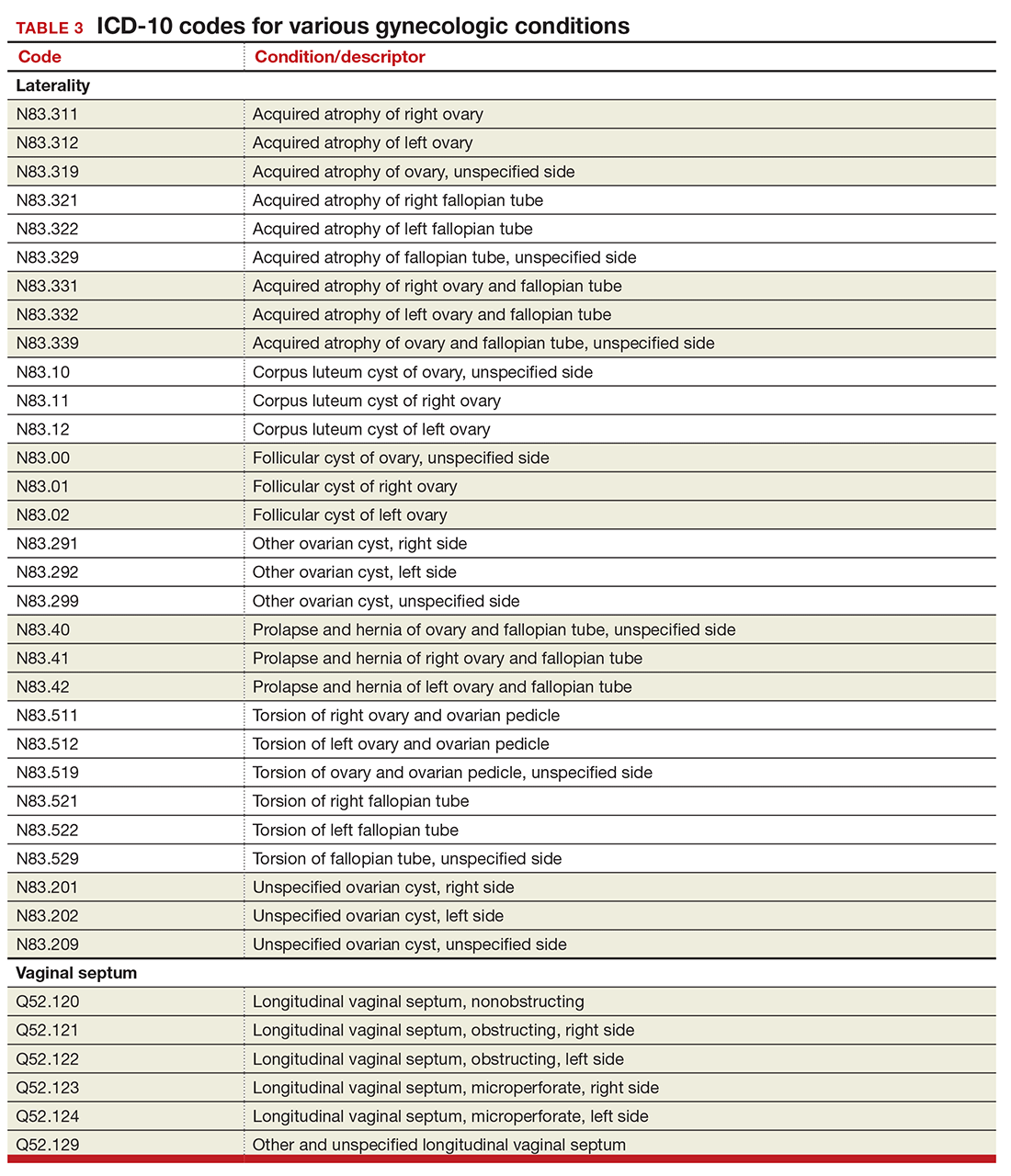
Vaginal septum
The right and left designations extend to the congenital codes for vaginal septum, but they go one step further. The American Congress of Obstetricians and Gynecologists (ACOG) requested that the codes for longitudinal vaginal septum be expanded to differentiate a nonobstructing vaginal septum from an obstructing vaginal septum, in addition to adding laterality to these codes (TABLE 3).2
Mastitis
There are now 2 new codes for inflammation of the breast; one describes mastitis without abscess, while the other code includes an abscess of the breast and nipple (TABLE 4). Once again, documentation will lead to the most specific code to describe the findings.
Childhood and prepubertal concerns
The single code for hypertrophy of the vulva has been expanded to include asymmetric labium majus enlargement. This code was requested by ACOG because this is a known clinical diagnosis and the currently available vulvar codes are inadequate for capturing this condition. The vulvar enlargement appears to be in response to hormonal surges during prepuberty and early puberty. Adult hypertrophy, either congenital or acquired from childbirth or as a late result of an old injury, would be reported by the “other specified” code (TABLE 5).
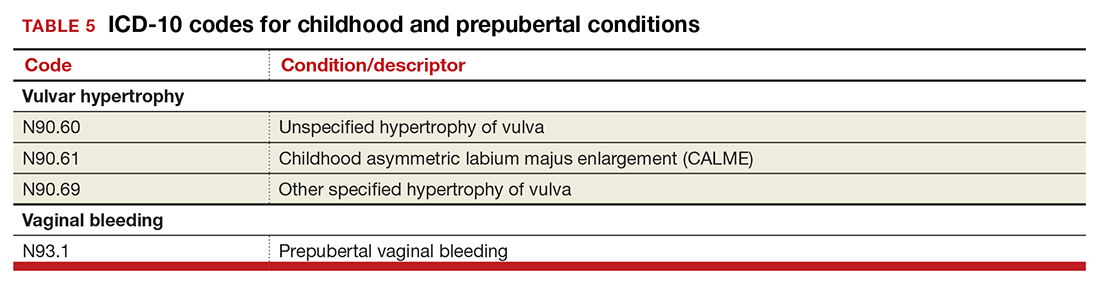
The causes of prepubertal bleeding vary and include the presence of a foreign object, tumors, or fluctuations in hormones, but prepubertal bleeding differs from the bleeding associated with normal menstruation. For that reason, ACOG requested a code that better captures the nature of the condition before a thorough work-up has pinpointed the cause (TABLE 5). Once the cause of the bleeding is known, a more specific diagnosis would then be reported (eg, D28.1, Benign neoplasm of vagina, or T19.2XXA, Foreign body in vulva and vagina, initial encounter).
Dypareunia
Additional documentation for dyspareunia will now be required to ensure that the most specific code is reported. In this case, the clinician should identify whether the pain is superficial or deep to better report on female pelvic floor dysfunction and to support the different treatments based on the location of the pain (TABLE 6). Deep dyspareunia would be felt in the mid or upper vagina.
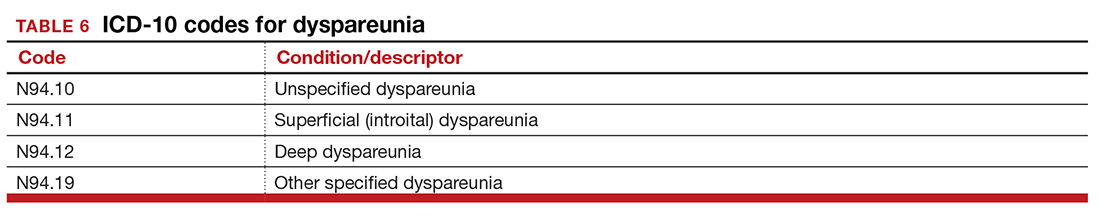
Postoperative hemorrhage and hematoma
The codes for postprocedural hemorrhage and hematomas have received a face-lift: the single codes for these 2 complications will be split so that each can be reported separately (TABLE 7). Note that the new codes require that the condition be found following the initial surgery, and the code selected depends on whether the surgery involved the genitourinary system or another system.
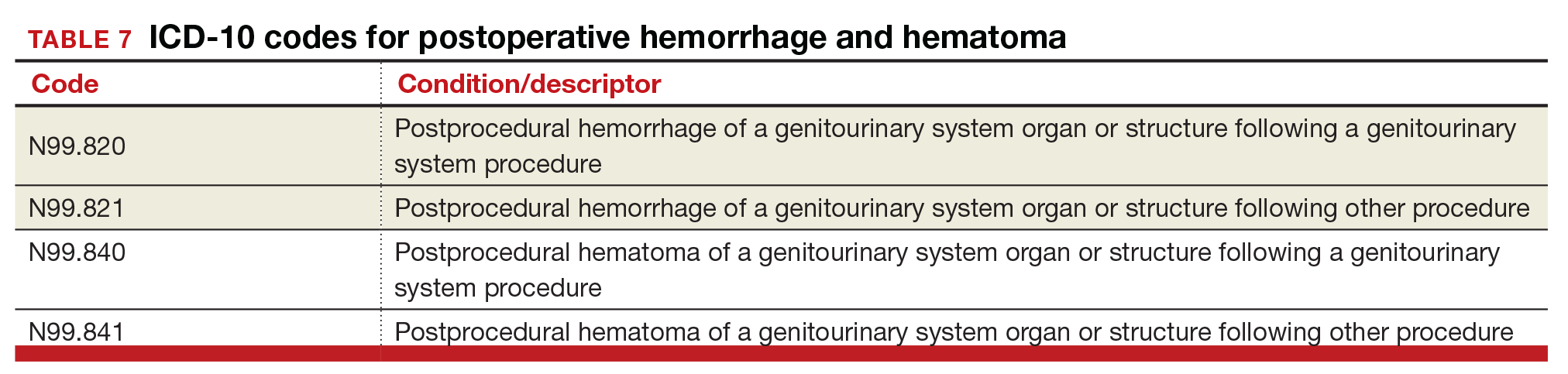
Hormone malignancy status
The new Z19 codes will augment information known about a patient’s neoplasm (TABLE 8). The ICD-10 rule states that the type and location of the neoplasm are always coded first, followed by one of the new Z19 codes, if known.
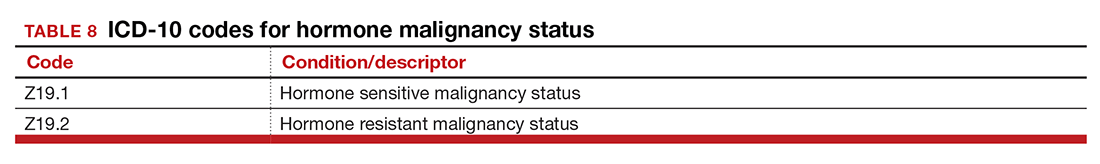
Viral hepatitis carrier
The more specific code for type of viral hepatitis the patient is a carrier of has been bundled into a single code for viral hepatitis (TABLE 9). Carrier status in ICD-10 is defined as a person who harbors the specific organisms of a disease, does not currently have any symptoms, but is capable of transmitting the infection.
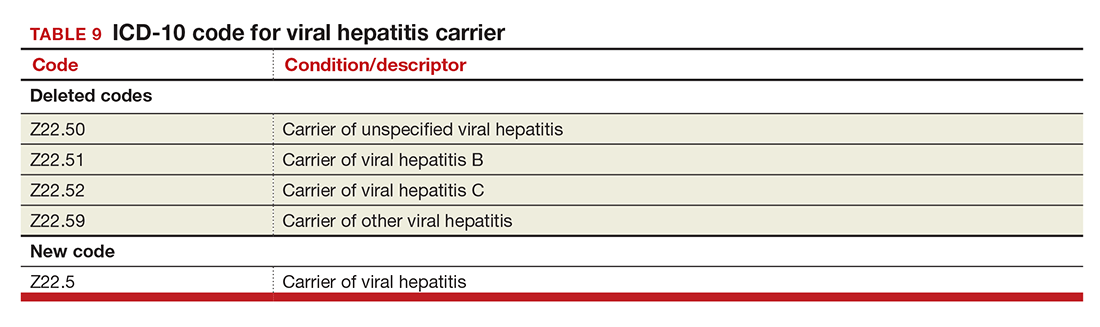
Contraception
The good news is that the ICD-9 code for contraceptive subdermal implants has been added to ICD-10 coding. In addition, the codes for contraceptive methods have been expanded to also include vaginal rings and transdermal patches (TABLE 10).
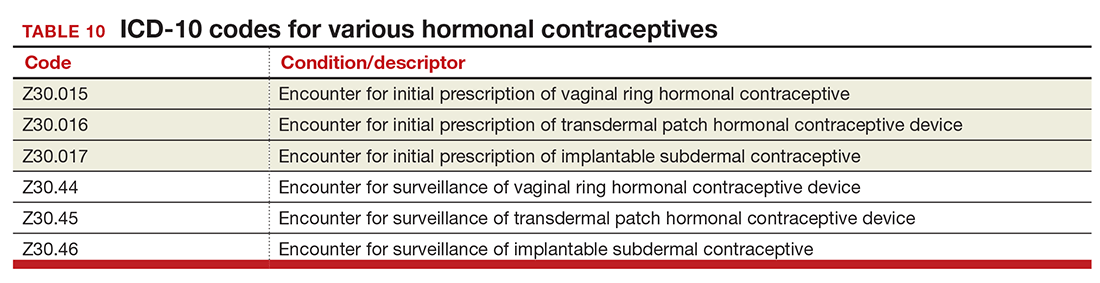
Miscellaneous code changes
Counseling a patient prior to pregnancy just got easier with the addition of a code for gestational carriers. Also, the old ICD-9 code that let a payer know that a procedure was converted from a laparoscopic to an open abdominal procedure is back (TABLE 11).
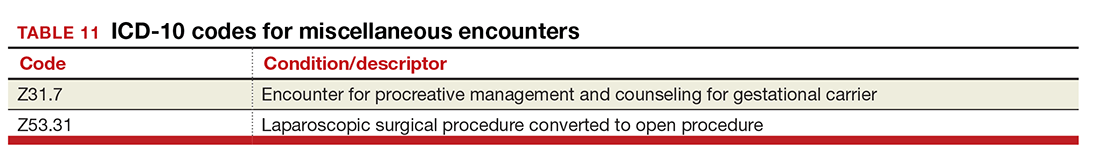
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In the August 2016 issue of OBG
Urogynecology diagnostic codes
Urogynecologists will find a large number of changes to codes they can select on October 1, 2016. While some codes improve reporting for conditions or symptoms related to urinary issues, many more concern postoperative complications following surgery for devices and grafts applied to the genitourinary system.
The American Urological Association requested new codes to align with a 2009 joint report on the terminology for female pelvic floor dysfunction.1 These codes, along with others, are listed in TABLE 1.
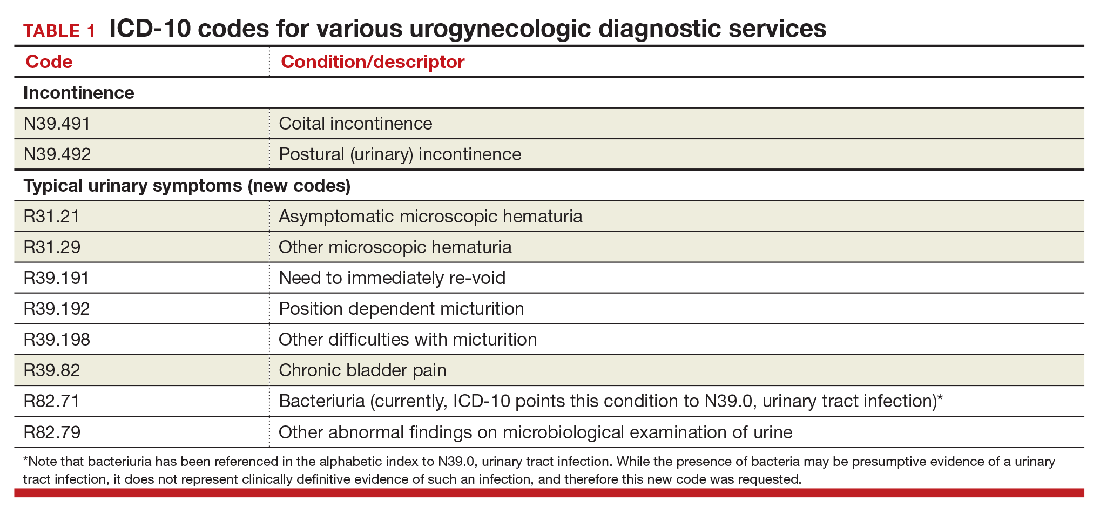
Urinary procedure complication codes
Not every urogynecologist will have an issue after surgery for incontinence, but if they do, there are tons of new and revised codes to address every possible complication the patient may have (TABLE 2). Each of these codes is reported based on whether the complication is being actively treated (initial encounter: final character is A), is being followed up after treatment (subsequent encounter: final character is D), or is caused by another condition (sequela: final character is S).
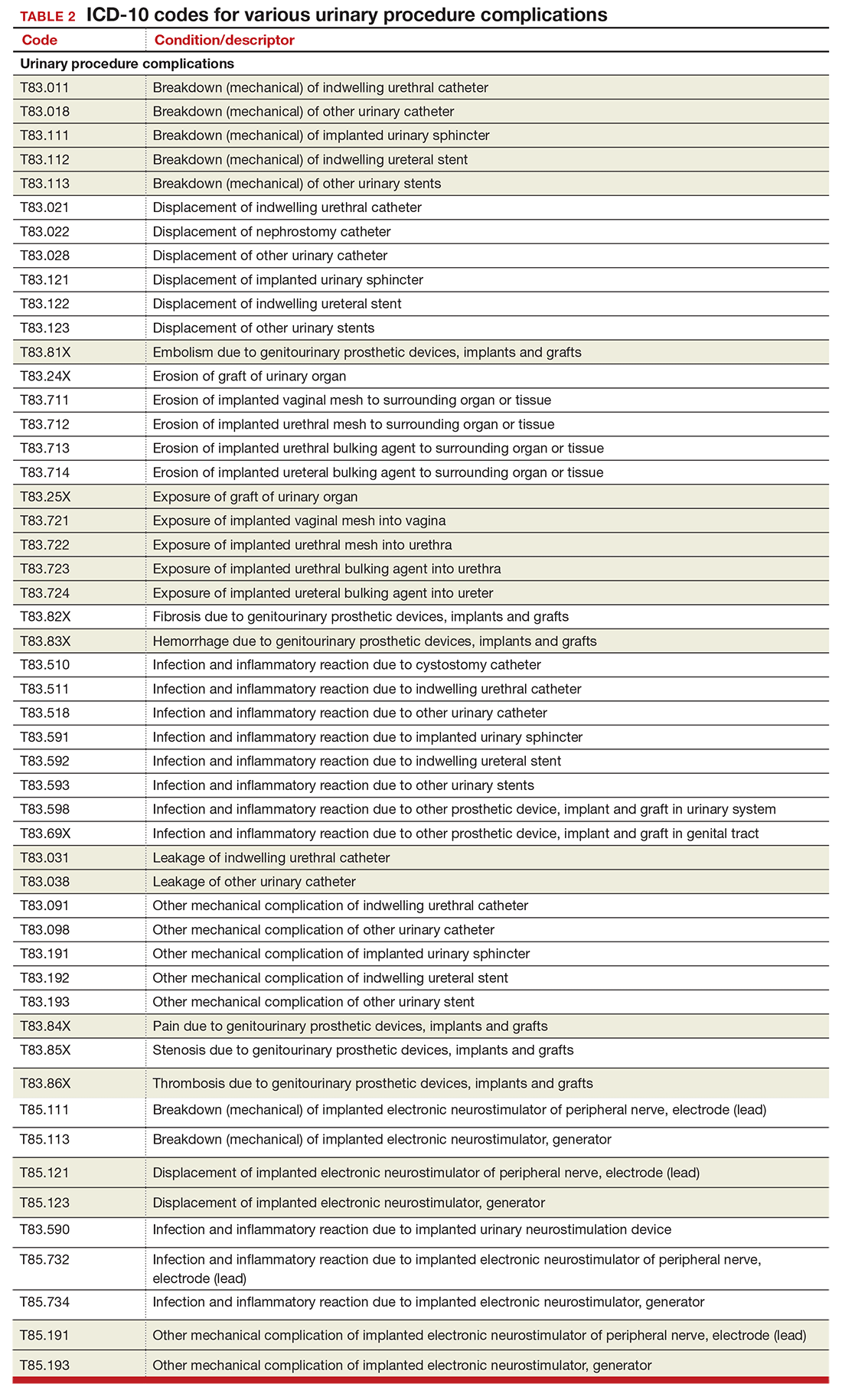
Gynecology-related diagnostic codes
Laterality
If there are 2 organs in the genitourinary system, the chances are good that there is now a right and a left designation code in ICD-10. Documentation should be clear, of course, and if the condition exists on both the right and the left side (even if only one side is being treated actively), list both codes, as there is no bilateral designation in the codes (TABLE 3). And while there is a code for “unspecified side,” providers normally do know which side, so use of this code should be avoided, if possible.
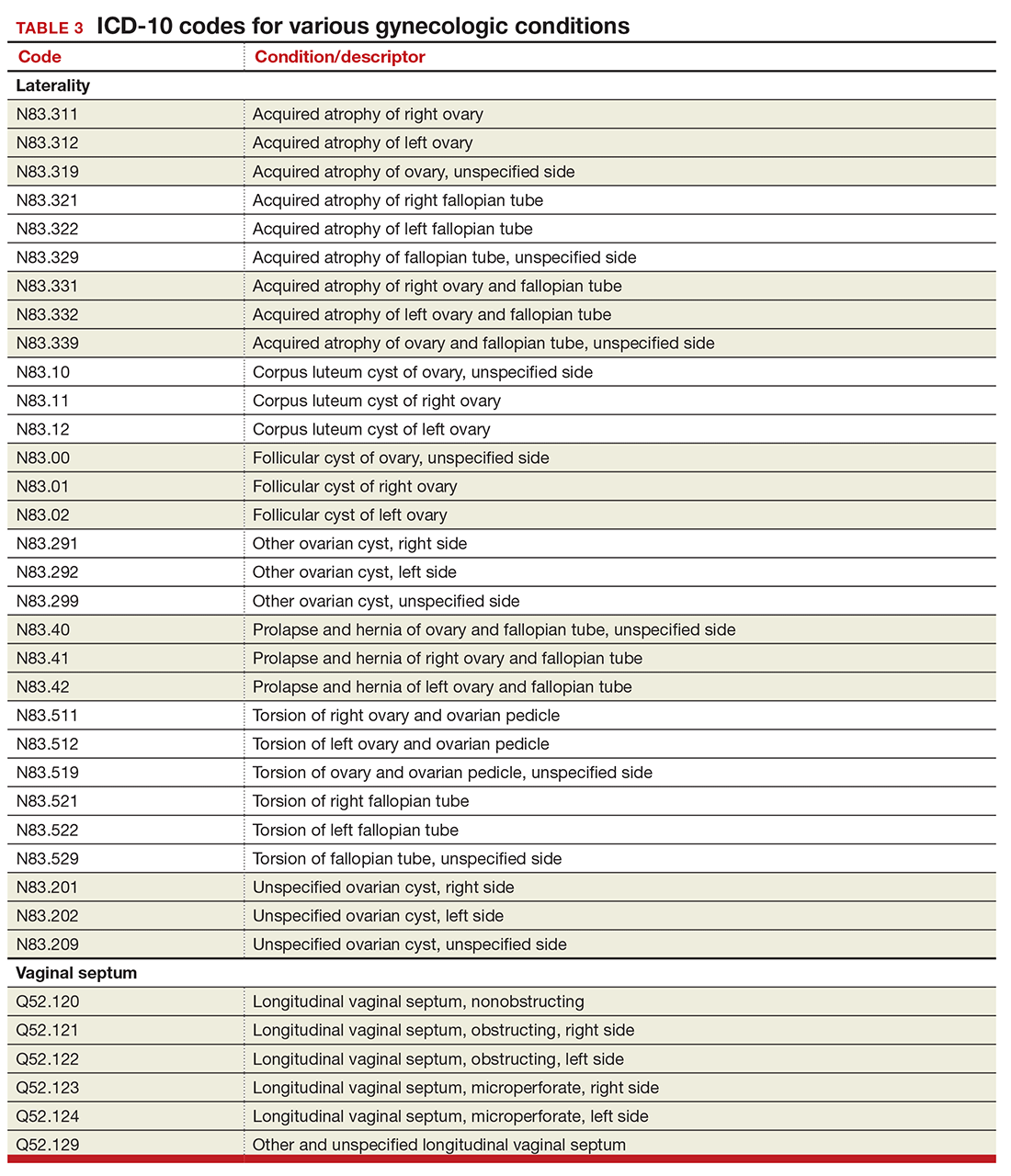
Vaginal septum
The right and left designations extend to the congenital codes for vaginal septum, but they go one step further. The American Congress of Obstetricians and Gynecologists (ACOG) requested that the codes for longitudinal vaginal septum be expanded to differentiate a nonobstructing vaginal septum from an obstructing vaginal septum, in addition to adding laterality to these codes (TABLE 3).2
Mastitis
There are now 2 new codes for inflammation of the breast; one describes mastitis without abscess, while the other code includes an abscess of the breast and nipple (TABLE 4). Once again, documentation will lead to the most specific code to describe the findings.
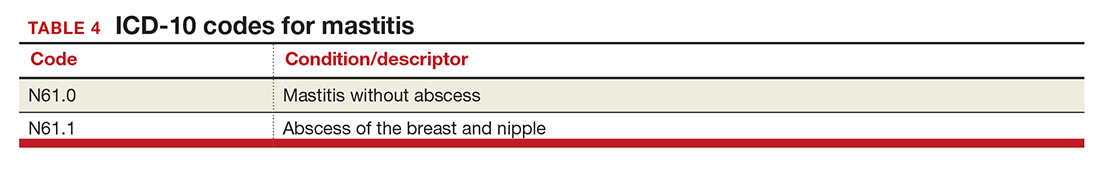
Childhood and prepubertal concerns
The single code for hypertrophy of the vulva has been expanded to include asymmetric labium majus enlargement. This code was requested by ACOG because this is a known clinical diagnosis and the currently available vulvar codes are inadequate for capturing this condition. The vulvar enlargement appears to be in response to hormonal surges during prepuberty and early puberty. Adult hypertrophy, either congenital or acquired from childbirth or as a late result of an old injury, would be reported by the “other specified” code (TABLE 5).
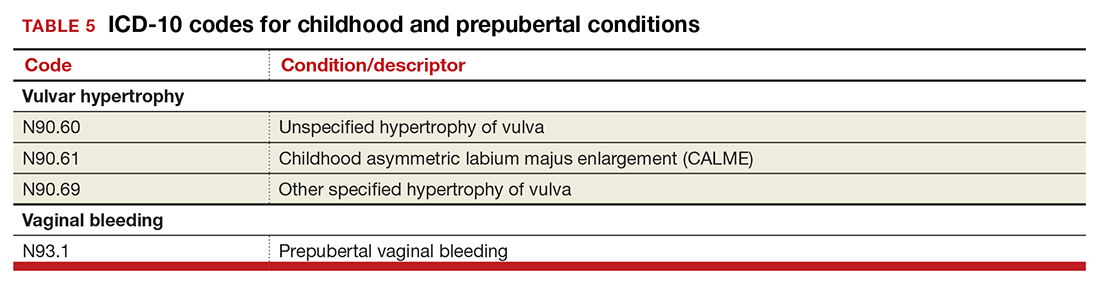
The causes of prepubertal bleeding vary and include the presence of a foreign object, tumors, or fluctuations in hormones, but prepubertal bleeding differs from the bleeding associated with normal menstruation. For that reason, ACOG requested a code that better captures the nature of the condition before a thorough work-up has pinpointed the cause (TABLE 5). Once the cause of the bleeding is known, a more specific diagnosis would then be reported (eg, D28.1, Benign neoplasm of vagina, or T19.2XXA, Foreign body in vulva and vagina, initial encounter).
Dypareunia
Additional documentation for dyspareunia will now be required to ensure that the most specific code is reported. In this case, the clinician should identify whether the pain is superficial or deep to better report on female pelvic floor dysfunction and to support the different treatments based on the location of the pain (TABLE 6). Deep dyspareunia would be felt in the mid or upper vagina.
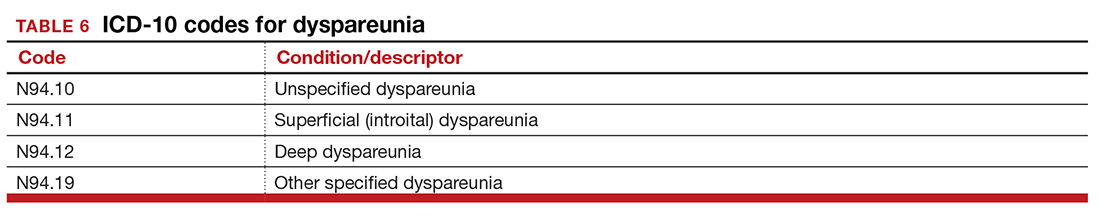
Postoperative hemorrhage and hematoma
The codes for postprocedural hemorrhage and hematomas have received a face-lift: the single codes for these 2 complications will be split so that each can be reported separately (TABLE 7). Note that the new codes require that the condition be found following the initial surgery, and the code selected depends on whether the surgery involved the genitourinary system or another system.
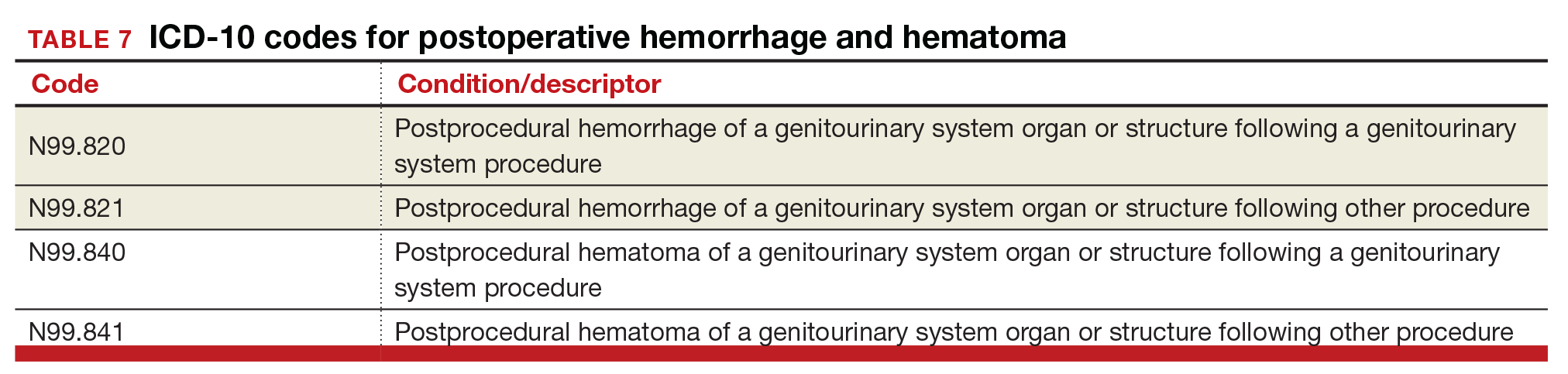
Hormone malignancy status
The new Z19 codes will augment information known about a patient’s neoplasm (TABLE 8). The ICD-10 rule states that the type and location of the neoplasm are always coded first, followed by one of the new Z19 codes, if known.
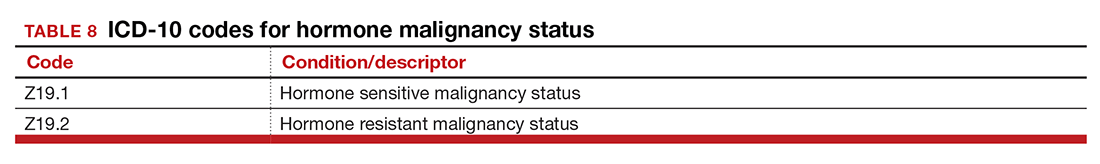
Viral hepatitis carrier
The more specific code for type of viral hepatitis the patient is a carrier of has been bundled into a single code for viral hepatitis (TABLE 9). Carrier status in ICD-10 is defined as a person who harbors the specific organisms of a disease, does not currently have any symptoms, but is capable of transmitting the infection.
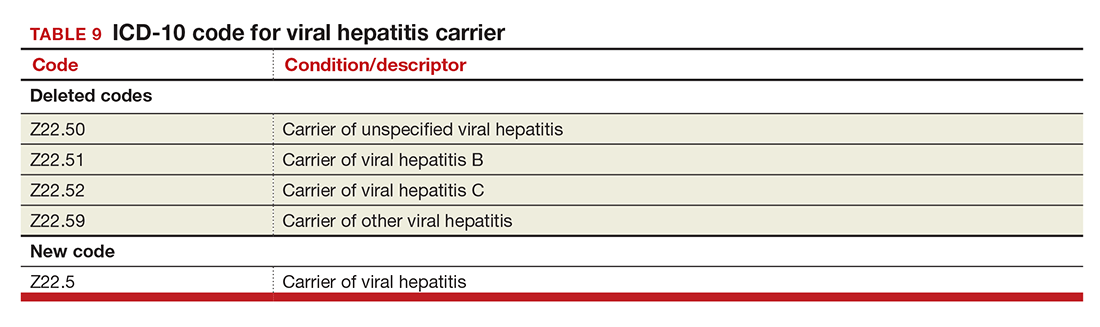
Contraception
The good news is that the ICD-9 code for contraceptive subdermal implants has been added to ICD-10 coding. In addition, the codes for contraceptive methods have been expanded to also include vaginal rings and transdermal patches (TABLE 10).
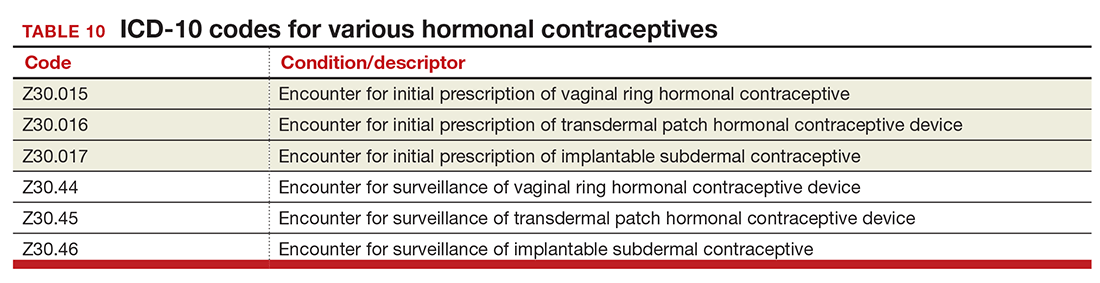
Miscellaneous code changes
Counseling a patient prior to pregnancy just got easier with the addition of a code for gestational carriers. Also, the old ICD-9 code that let a payer know that a procedure was converted from a laparoscopic to an open abdominal procedure is back (TABLE 11).
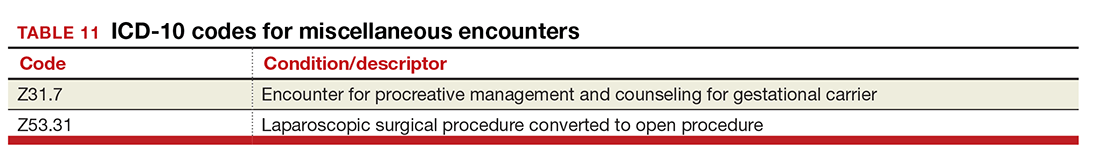
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. September 23–24, 2014;28–29. https://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed August 30, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. March 18–19, 2015. http://www.cdc.gov/nchs/data/icd/Tentative_Agenda_March%202015_Final.pdf. Accessed August 30, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. September 23–24, 2014;28–29. https://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed August 30, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. March 18–19, 2015. http://www.cdc.gov/nchs/data/icd/Tentative_Agenda_March%202015_Final.pdf. Accessed August 30, 2016.
In this Article
- Urogynecology dx codes
- Gynecology dx codes
- Codes for hormonal contraceptives
2016 Obstetric code changes that could affect your reimbursement (very soon)
By now the upheaval of changing to the new International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) diagnostic coding system has settled. The code freeze that was initiated in 2012 has ended, and the new and revised codes that will go into effect on October 1, 2016, are being revealed. Good documentation will lead to more accurate diagnostic coding, which in turn assists decision makers in their quest to report the health of our population and to make good decisions for resource allocation. You are in the unique position to assist in this process, so keep up the good work.
In this article, I focus on ICD-10 diagnostic coding for obstetric services. I will cover diagnostic coding for gynecologic services in the September issue of OBG Management.
Code revisions for uterine scar and more changes to note
With the upcoming edition of ICD-10, the code Z3A, Weeks’ gestation, will be changed from mandatory reporting to reporting if known. This means that if the patient is no longer pregnant, a Z3A code no longer needs to be reported, and if at the time of service the provider does not know the weeks’ gestation, Z3A would not be required. However, this information should be readily available during the antepartum period and should still be considered important to record and report. And it would still be reported for hospitalization for delivery.
If the code O09.81, Supervision of pregnancy resulting from assisted reproductive technology, is reported, the code Z33.3, Gestational carrier status, may be reported in addition for informational purposes.
When the code O34.29, Maternal care due to uterine scar from other previous surgery, is reported, the tabular index clarifies that this refers to a uterine scar from a transmural uterine incision other than that used for cesarean delivery. This would include incision into the uterine wall to remove fibroids.
The O42 code category, relating to Premature rupture of membranes, should now be interpreted to mean rupture of membranes at or after 37 completed weeks of gestation, rather than after 37 completed weeks.
The code category O99.6, Diseases of the digestive system complicating pregnancy, childbirth, and the puerperium, has been clarified: it does not include hemorrhoids in pregnancy. Therefore, a code from O22.4_ (a final digit of 0 [unspecified], 1, 2, or 3 is required for the trimester) also can be reported if hemorrhoids are present.
A note now clarifies that O99.82, Streptococcus B carrier state complicating pregnancy, childbirth, and the puerperium, cannot be reported with Z22.330, Carrier of streptococcus group B (GBS) in a nonpregnant woman.
New codes for specifying types of ectopic pregnancy
ICD-10 did not initially recognize ectopic pregnancy with and without intrauterine pregnancy, as was the case in ICD-9, but starting in October it will do so. In addition, a history of ectopic or molar pregnancy during a current pregnancy is now reported separately. Each of these codes will require a final digit to indicate the trimester (TABLE).
Codes added for complicating conditions of childbirth and the puerperium
Missing from the ICD-10 lineup last year were codes for conditions related to hypertension, edema, proteinuria, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and eclampsia that were complicating the pregnancy at the time of delivery or after delivery (TABLE).
Note that the “childbirth” code is reported only when a patient delivers at the current episode of care. Once a patient delivers and is discharged, the “puerperium” code should be selected.
Revised descriptions, new reporting instruction for diabetes
The code descriptions for preexisting type 1 and type 2 diabetes were revised, but this change does not impact reporting the codes. However, for type 2 diabetes, the instruction for reporting an additional code has changed. Now, in addition to reporting the code for current use of insulin (Z79.4), when appropriate, report the new added code for use of hypoglycemic agents (Z79.84), such as glyburide or metformin.
For gestational diabetes, new codes have been added for the use of hypoglycemic agents; therefore, no additional code is reported (TABLE).
Disproportion code includes numeric specifier for fetus
The disproportion code category was expanded to include a final digit for the fetus with the deformity (TABLE). The final digit of the code number denotes which fetus; for example, “0” means a singleton pregnancy, “1” means fetus 1 (number range from 1 to 5), and “9” denotes any fetus after the fifth.
Cesarean delivery scar codes expanded
The code for maternal care for a scar from a previous cesarean delivery has been expanded to 3 different codes (TABLE). Clinicians should make every effort to document and report the location of the previous cesarean as low transverse or vertical. From a coding standpoint, a vertical scar can also be referred to as a classical scar.
Changes to placenta previa codes
The code category for placenta previa has been expanded to capture the degree of previa as complete, partial, or low lying and with or without hemorrhage (TABLE). Going forward, it will be important to carefully document the circumstances so that the most specific code can be reported and tracked. Trimester specification is required as the final digit.
New subclassifications for perineal laceration
The code category for perineal laceration has been expanded with new codes to capture subclassifications for a third-degree laceration that can involve the external and internal anal sphincter (TABLE). Through its collaborative hub, the Women’s Health Registry Alliance (reVITALize) initiative, the American Congress of Obstetricians and Gynecologists (ACOG) worked on the current classification of third- and fourth-degree perineal lacerations, which has been adopted by the Royal College of Obstetricians and Gynaecologists.1
Under this subclassification, a 3a laceration would involve a tear of less than 50% of the external anal sphincter (EAS); 3b would involve a tear of more than 50% of the EAS; and 3c would mean that both the external and internal anal sphincter are torn. ACOG and its collaborative group encourage clinicians to use these subclassifications in documentation to allow for more robust data collection and complete repair information. From a payment standpoint, such information may go a long way to substantiating the severity of a tear, which may require more physician work.
Z code additions
Finally, the ever-popular diagnostic code for Rho(D) immunization is back, and 2 codes have been added for a gestational carrier and 1 for a family history of sudden infant death syndrome. The codes are:
- Z29.13 Encounter for prophylactic Rho(D) immune globulin
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z33.3 Pregnant state, gestational carrier
- Z84.82 Family history of sudden infant death syndrome.
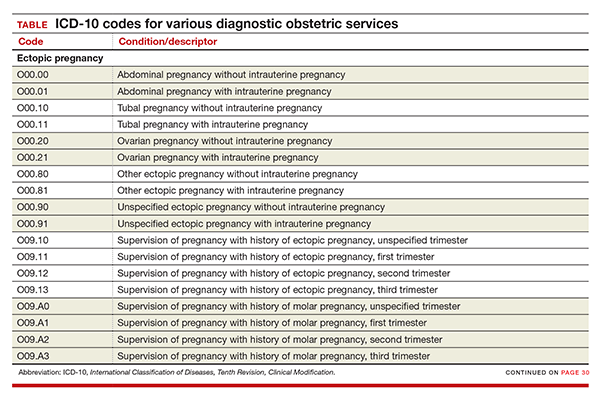
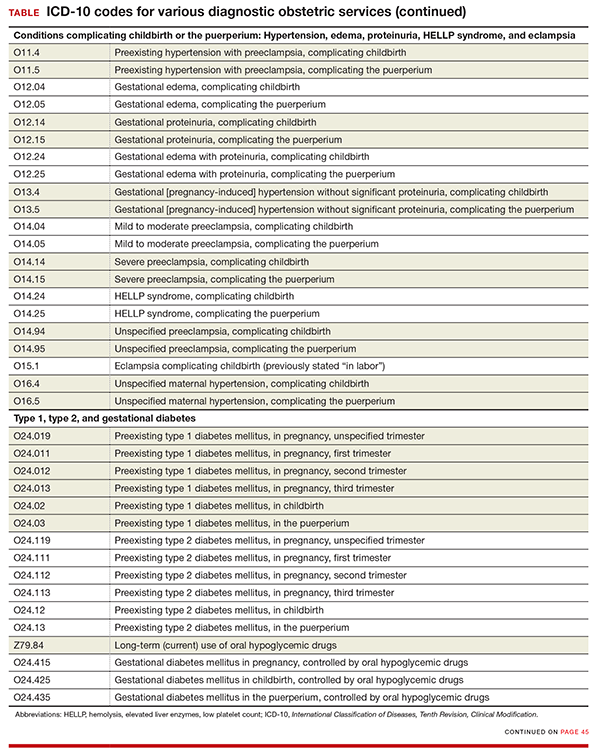
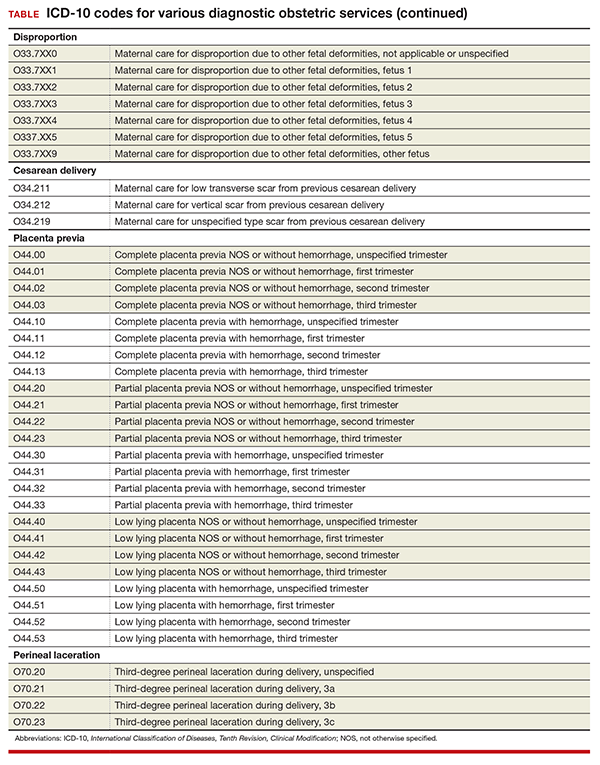
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee meeting: diagnosis agenda. September 23-24, 2014;38, 39. http://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed July 5, 2016.
By now the upheaval of changing to the new International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) diagnostic coding system has settled. The code freeze that was initiated in 2012 has ended, and the new and revised codes that will go into effect on October 1, 2016, are being revealed. Good documentation will lead to more accurate diagnostic coding, which in turn assists decision makers in their quest to report the health of our population and to make good decisions for resource allocation. You are in the unique position to assist in this process, so keep up the good work.
In this article, I focus on ICD-10 diagnostic coding for obstetric services. I will cover diagnostic coding for gynecologic services in the September issue of OBG Management.
Code revisions for uterine scar and more changes to note
With the upcoming edition of ICD-10, the code Z3A, Weeks’ gestation, will be changed from mandatory reporting to reporting if known. This means that if the patient is no longer pregnant, a Z3A code no longer needs to be reported, and if at the time of service the provider does not know the weeks’ gestation, Z3A would not be required. However, this information should be readily available during the antepartum period and should still be considered important to record and report. And it would still be reported for hospitalization for delivery.
If the code O09.81, Supervision of pregnancy resulting from assisted reproductive technology, is reported, the code Z33.3, Gestational carrier status, may be reported in addition for informational purposes.
When the code O34.29, Maternal care due to uterine scar from other previous surgery, is reported, the tabular index clarifies that this refers to a uterine scar from a transmural uterine incision other than that used for cesarean delivery. This would include incision into the uterine wall to remove fibroids.
The O42 code category, relating to Premature rupture of membranes, should now be interpreted to mean rupture of membranes at or after 37 completed weeks of gestation, rather than after 37 completed weeks.
The code category O99.6, Diseases of the digestive system complicating pregnancy, childbirth, and the puerperium, has been clarified: it does not include hemorrhoids in pregnancy. Therefore, a code from O22.4_ (a final digit of 0 [unspecified], 1, 2, or 3 is required for the trimester) also can be reported if hemorrhoids are present.
A note now clarifies that O99.82, Streptococcus B carrier state complicating pregnancy, childbirth, and the puerperium, cannot be reported with Z22.330, Carrier of streptococcus group B (GBS) in a nonpregnant woman.
New codes for specifying types of ectopic pregnancy
ICD-10 did not initially recognize ectopic pregnancy with and without intrauterine pregnancy, as was the case in ICD-9, but starting in October it will do so. In addition, a history of ectopic or molar pregnancy during a current pregnancy is now reported separately. Each of these codes will require a final digit to indicate the trimester (TABLE).
Codes added for complicating conditions of childbirth and the puerperium
Missing from the ICD-10 lineup last year were codes for conditions related to hypertension, edema, proteinuria, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and eclampsia that were complicating the pregnancy at the time of delivery or after delivery (TABLE).
Note that the “childbirth” code is reported only when a patient delivers at the current episode of care. Once a patient delivers and is discharged, the “puerperium” code should be selected.
Revised descriptions, new reporting instruction for diabetes
The code descriptions for preexisting type 1 and type 2 diabetes were revised, but this change does not impact reporting the codes. However, for type 2 diabetes, the instruction for reporting an additional code has changed. Now, in addition to reporting the code for current use of insulin (Z79.4), when appropriate, report the new added code for use of hypoglycemic agents (Z79.84), such as glyburide or metformin.
For gestational diabetes, new codes have been added for the use of hypoglycemic agents; therefore, no additional code is reported (TABLE).
Disproportion code includes numeric specifier for fetus
The disproportion code category was expanded to include a final digit for the fetus with the deformity (TABLE). The final digit of the code number denotes which fetus; for example, “0” means a singleton pregnancy, “1” means fetus 1 (number range from 1 to 5), and “9” denotes any fetus after the fifth.
Cesarean delivery scar codes expanded
The code for maternal care for a scar from a previous cesarean delivery has been expanded to 3 different codes (TABLE). Clinicians should make every effort to document and report the location of the previous cesarean as low transverse or vertical. From a coding standpoint, a vertical scar can also be referred to as a classical scar.
Changes to placenta previa codes
The code category for placenta previa has been expanded to capture the degree of previa as complete, partial, or low lying and with or without hemorrhage (TABLE). Going forward, it will be important to carefully document the circumstances so that the most specific code can be reported and tracked. Trimester specification is required as the final digit.
New subclassifications for perineal laceration
The code category for perineal laceration has been expanded with new codes to capture subclassifications for a third-degree laceration that can involve the external and internal anal sphincter (TABLE). Through its collaborative hub, the Women’s Health Registry Alliance (reVITALize) initiative, the American Congress of Obstetricians and Gynecologists (ACOG) worked on the current classification of third- and fourth-degree perineal lacerations, which has been adopted by the Royal College of Obstetricians and Gynaecologists.1
Under this subclassification, a 3a laceration would involve a tear of less than 50% of the external anal sphincter (EAS); 3b would involve a tear of more than 50% of the EAS; and 3c would mean that both the external and internal anal sphincter are torn. ACOG and its collaborative group encourage clinicians to use these subclassifications in documentation to allow for more robust data collection and complete repair information. From a payment standpoint, such information may go a long way to substantiating the severity of a tear, which may require more physician work.
Z code additions
Finally, the ever-popular diagnostic code for Rho(D) immunization is back, and 2 codes have been added for a gestational carrier and 1 for a family history of sudden infant death syndrome. The codes are:
- Z29.13 Encounter for prophylactic Rho(D) immune globulin
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z33.3 Pregnant state, gestational carrier
- Z84.82 Family history of sudden infant death syndrome.
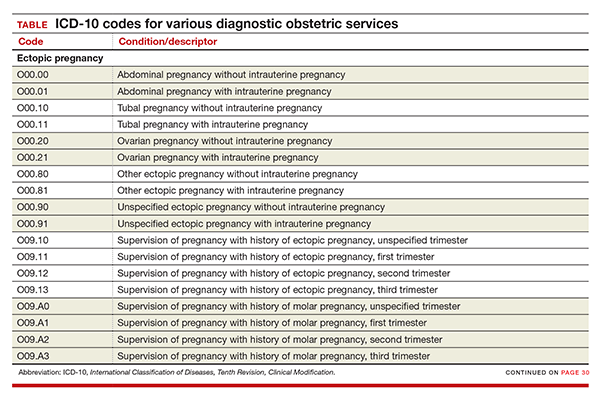
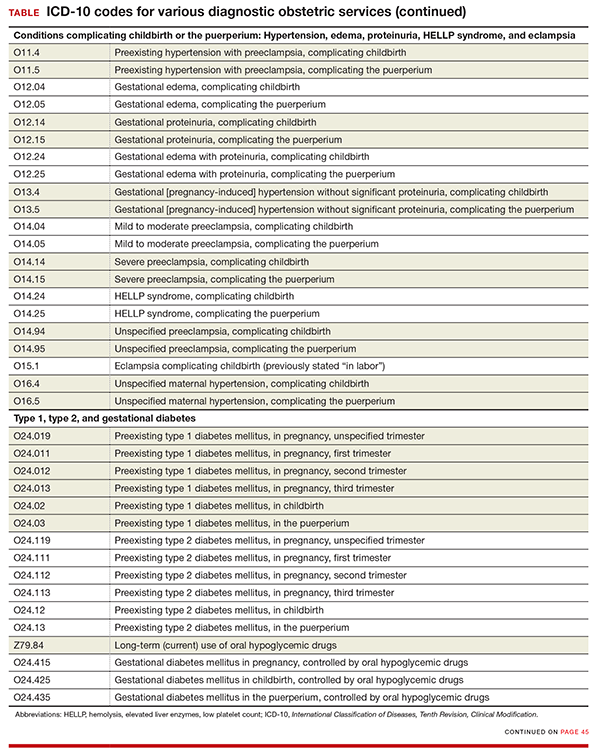
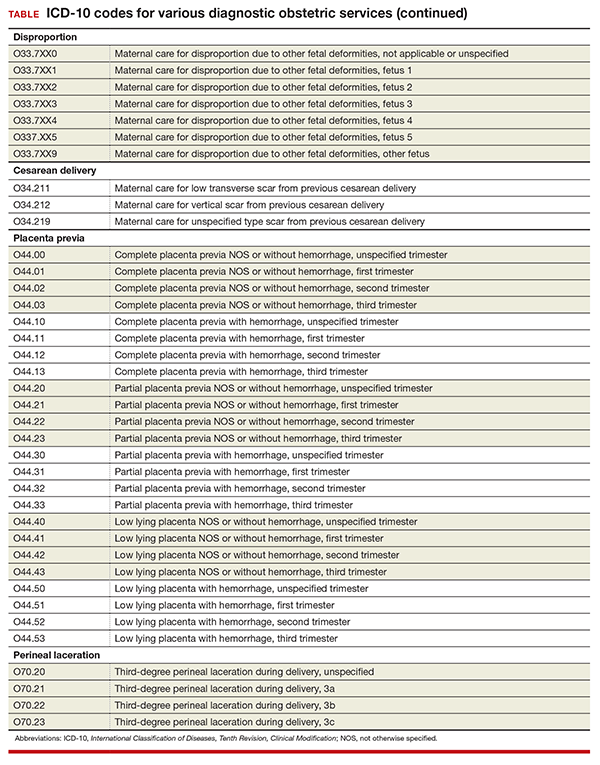
By now the upheaval of changing to the new International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) diagnostic coding system has settled. The code freeze that was initiated in 2012 has ended, and the new and revised codes that will go into effect on October 1, 2016, are being revealed. Good documentation will lead to more accurate diagnostic coding, which in turn assists decision makers in their quest to report the health of our population and to make good decisions for resource allocation. You are in the unique position to assist in this process, so keep up the good work.
In this article, I focus on ICD-10 diagnostic coding for obstetric services. I will cover diagnostic coding for gynecologic services in the September issue of OBG Management.
Code revisions for uterine scar and more changes to note
With the upcoming edition of ICD-10, the code Z3A, Weeks’ gestation, will be changed from mandatory reporting to reporting if known. This means that if the patient is no longer pregnant, a Z3A code no longer needs to be reported, and if at the time of service the provider does not know the weeks’ gestation, Z3A would not be required. However, this information should be readily available during the antepartum period and should still be considered important to record and report. And it would still be reported for hospitalization for delivery.
If the code O09.81, Supervision of pregnancy resulting from assisted reproductive technology, is reported, the code Z33.3, Gestational carrier status, may be reported in addition for informational purposes.
When the code O34.29, Maternal care due to uterine scar from other previous surgery, is reported, the tabular index clarifies that this refers to a uterine scar from a transmural uterine incision other than that used for cesarean delivery. This would include incision into the uterine wall to remove fibroids.
The O42 code category, relating to Premature rupture of membranes, should now be interpreted to mean rupture of membranes at or after 37 completed weeks of gestation, rather than after 37 completed weeks.
The code category O99.6, Diseases of the digestive system complicating pregnancy, childbirth, and the puerperium, has been clarified: it does not include hemorrhoids in pregnancy. Therefore, a code from O22.4_ (a final digit of 0 [unspecified], 1, 2, or 3 is required for the trimester) also can be reported if hemorrhoids are present.
A note now clarifies that O99.82, Streptococcus B carrier state complicating pregnancy, childbirth, and the puerperium, cannot be reported with Z22.330, Carrier of streptococcus group B (GBS) in a nonpregnant woman.
New codes for specifying types of ectopic pregnancy
ICD-10 did not initially recognize ectopic pregnancy with and without intrauterine pregnancy, as was the case in ICD-9, but starting in October it will do so. In addition, a history of ectopic or molar pregnancy during a current pregnancy is now reported separately. Each of these codes will require a final digit to indicate the trimester (TABLE).
Codes added for complicating conditions of childbirth and the puerperium
Missing from the ICD-10 lineup last year were codes for conditions related to hypertension, edema, proteinuria, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and eclampsia that were complicating the pregnancy at the time of delivery or after delivery (TABLE).
Note that the “childbirth” code is reported only when a patient delivers at the current episode of care. Once a patient delivers and is discharged, the “puerperium” code should be selected.
Revised descriptions, new reporting instruction for diabetes
The code descriptions for preexisting type 1 and type 2 diabetes were revised, but this change does not impact reporting the codes. However, for type 2 diabetes, the instruction for reporting an additional code has changed. Now, in addition to reporting the code for current use of insulin (Z79.4), when appropriate, report the new added code for use of hypoglycemic agents (Z79.84), such as glyburide or metformin.
For gestational diabetes, new codes have been added for the use of hypoglycemic agents; therefore, no additional code is reported (TABLE).
Disproportion code includes numeric specifier for fetus
The disproportion code category was expanded to include a final digit for the fetus with the deformity (TABLE). The final digit of the code number denotes which fetus; for example, “0” means a singleton pregnancy, “1” means fetus 1 (number range from 1 to 5), and “9” denotes any fetus after the fifth.
Cesarean delivery scar codes expanded
The code for maternal care for a scar from a previous cesarean delivery has been expanded to 3 different codes (TABLE). Clinicians should make every effort to document and report the location of the previous cesarean as low transverse or vertical. From a coding standpoint, a vertical scar can also be referred to as a classical scar.
Changes to placenta previa codes
The code category for placenta previa has been expanded to capture the degree of previa as complete, partial, or low lying and with or without hemorrhage (TABLE). Going forward, it will be important to carefully document the circumstances so that the most specific code can be reported and tracked. Trimester specification is required as the final digit.
New subclassifications for perineal laceration
The code category for perineal laceration has been expanded with new codes to capture subclassifications for a third-degree laceration that can involve the external and internal anal sphincter (TABLE). Through its collaborative hub, the Women’s Health Registry Alliance (reVITALize) initiative, the American Congress of Obstetricians and Gynecologists (ACOG) worked on the current classification of third- and fourth-degree perineal lacerations, which has been adopted by the Royal College of Obstetricians and Gynaecologists.1
Under this subclassification, a 3a laceration would involve a tear of less than 50% of the external anal sphincter (EAS); 3b would involve a tear of more than 50% of the EAS; and 3c would mean that both the external and internal anal sphincter are torn. ACOG and its collaborative group encourage clinicians to use these subclassifications in documentation to allow for more robust data collection and complete repair information. From a payment standpoint, such information may go a long way to substantiating the severity of a tear, which may require more physician work.
Z code additions
Finally, the ever-popular diagnostic code for Rho(D) immunization is back, and 2 codes have been added for a gestational carrier and 1 for a family history of sudden infant death syndrome. The codes are:
- Z29.13 Encounter for prophylactic Rho(D) immune globulin
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z33.3 Pregnant state, gestational carrier
- Z84.82 Family history of sudden infant death syndrome.
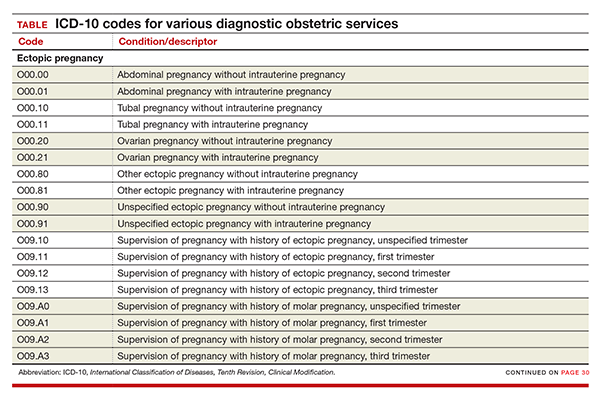
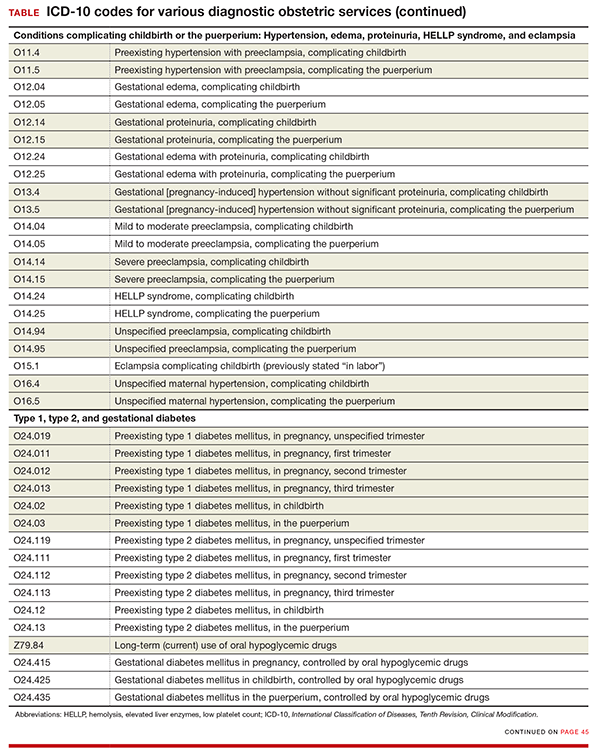
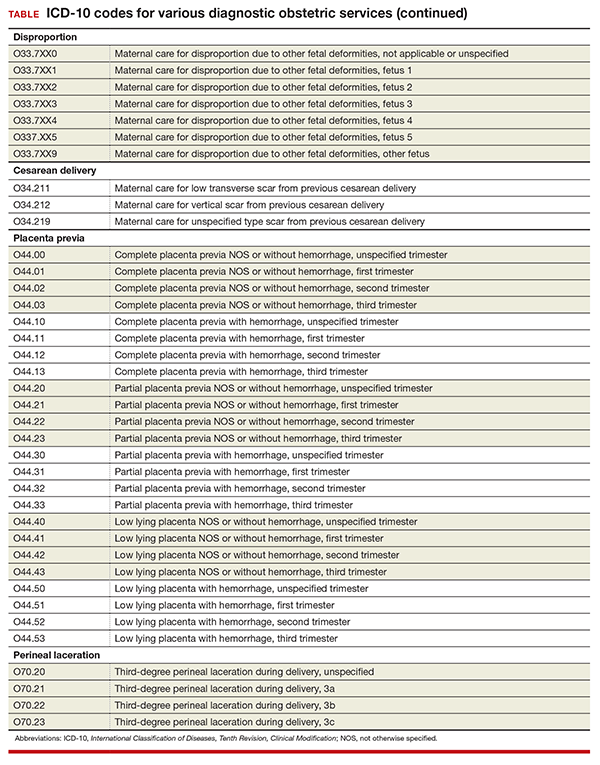
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee meeting: diagnosis agenda. September 23-24, 2014;38, 39. http://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed July 5, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee meeting: diagnosis agenda. September 23-24, 2014;38, 39. http://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed July 5, 2016.
In this Article
- New and expanded codes
- Z code additions
- Table of codes