User login
By now the upheaval of changing to the new International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) diagnostic coding system has settled. The code freeze that was initiated in 2012 has ended, and the new and revised codes that will go into effect on October 1, 2016, are being revealed. Good documentation will lead to more accurate diagnostic coding, which in turn assists decision makers in their quest to report the health of our population and to make good decisions for resource allocation. You are in the unique position to assist in this process, so keep up the good work.
In this article, I focus on ICD-10 diagnostic coding for obstetric services. I will cover diagnostic coding for gynecologic services in the September issue of OBG Management.
Code revisions for uterine scar and more changes to note
With the upcoming edition of ICD-10, the code Z3A, Weeks’ gestation, will be changed from mandatory reporting to reporting if known. This means that if the patient is no longer pregnant, a Z3A code no longer needs to be reported, and if at the time of service the provider does not know the weeks’ gestation, Z3A would not be required. However, this information should be readily available during the antepartum period and should still be considered important to record and report. And it would still be reported for hospitalization for delivery.
If the code O09.81, Supervision of pregnancy resulting from assisted reproductive technology, is reported, the code Z33.3, Gestational carrier status, may be reported in addition for informational purposes.
When the code O34.29, Maternal care due to uterine scar from other previous surgery, is reported, the tabular index clarifies that this refers to a uterine scar from a transmural uterine incision other than that used for cesarean delivery. This would include incision into the uterine wall to remove fibroids.
The O42 code category, relating to Premature rupture of membranes, should now be interpreted to mean rupture of membranes at or after 37 completed weeks of gestation, rather than after 37 completed weeks.
The code category O99.6, Diseases of the digestive system complicating pregnancy, childbirth, and the puerperium, has been clarified: it does not include hemorrhoids in pregnancy. Therefore, a code from O22.4_ (a final digit of 0 [unspecified], 1, 2, or 3 is required for the trimester) also can be reported if hemorrhoids are present.
A note now clarifies that O99.82, Streptococcus B carrier state complicating pregnancy, childbirth, and the puerperium, cannot be reported with Z22.330, Carrier of streptococcus group B (GBS) in a nonpregnant woman.
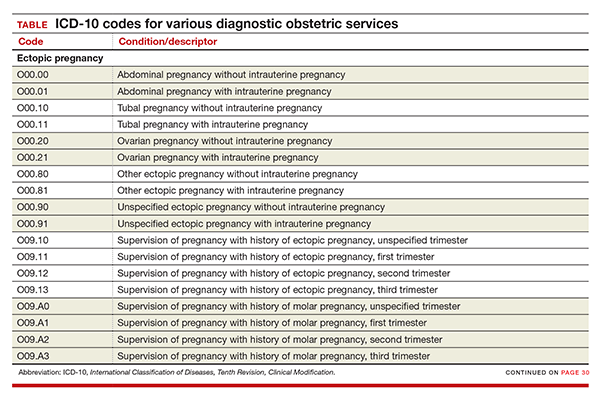
New codes for specifying types of ectopic pregnancy
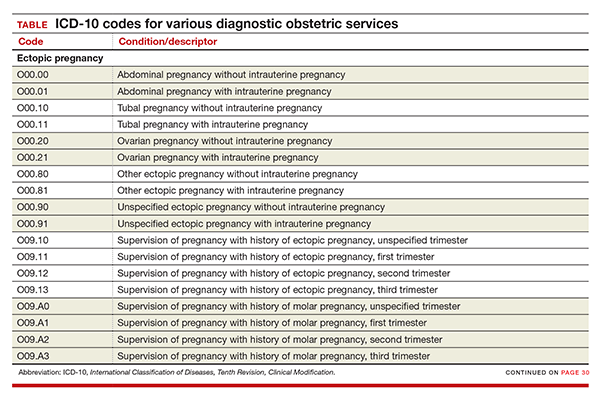
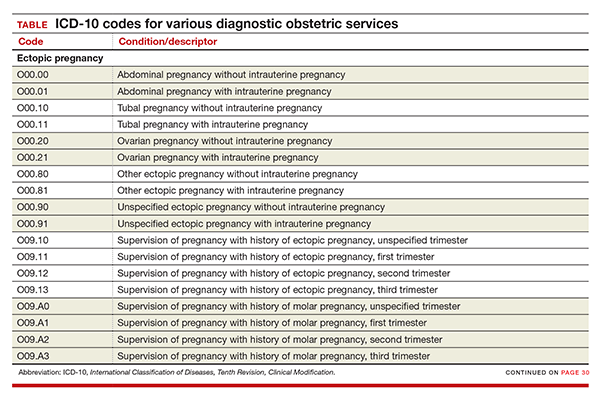
ICD-10 did not initially recognize ectopic pregnancy with and without intrauterine pregnancy, as was the case in ICD-9, but starting in October it will do so. In addition, a history of ectopic or molar pregnancy during a current pregnancy is now reported separately. Each of these codes will require a final digit to indicate the trimester (TABLE).
Codes added for complicating conditions of childbirth and the puerperium
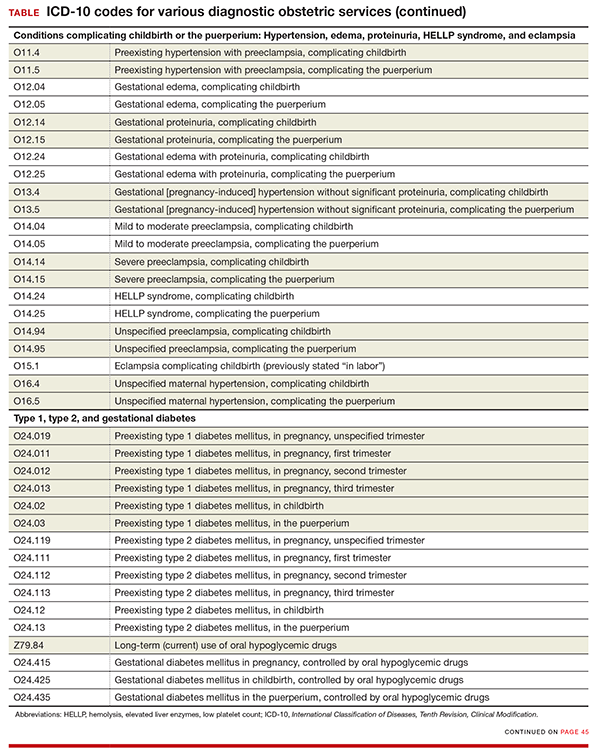
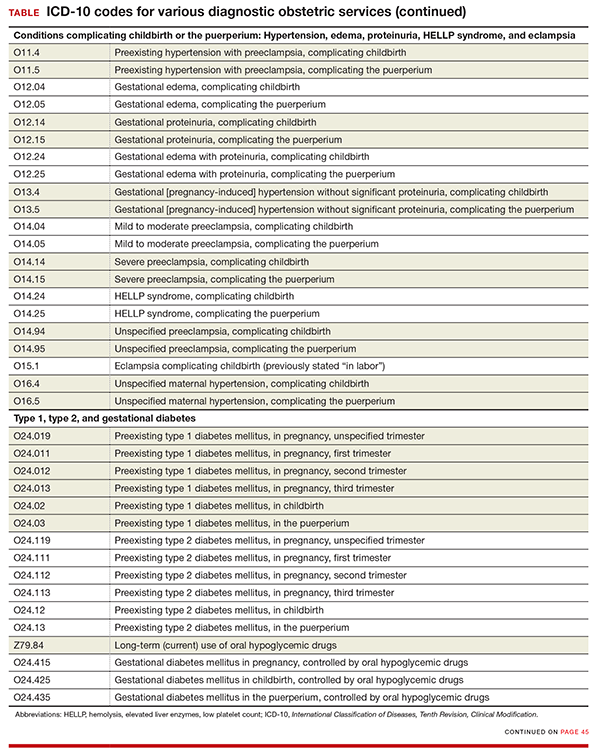
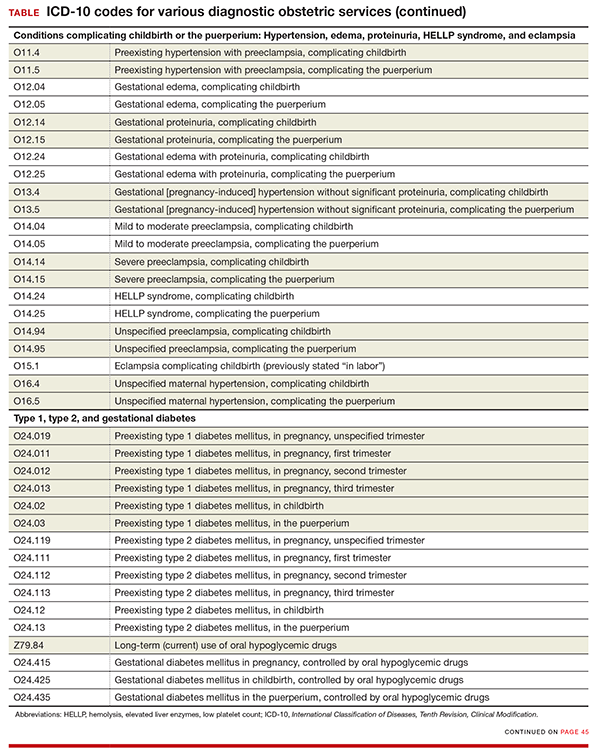
Missing from the ICD-10 lineup last year were codes for conditions related to hypertension, edema, proteinuria, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and eclampsia that were complicating the pregnancy at the time of delivery or after delivery (TABLE).
Note that the “childbirth” code is reported only when a patient delivers at the current episode of care. Once a patient delivers and is discharged, the “puerperium” code should be selected.
Revised descriptions, new reporting instruction for diabetes
The code descriptions for preexisting type 1 and type 2 diabetes were revised, but this change does not impact reporting the codes. However, for type 2 diabetes, the instruction for reporting an additional code has changed. Now, in addition to reporting the code for current use of insulin (Z79.4), when appropriate, report the new added code for use of hypoglycemic agents (Z79.84), such as glyburide or metformin.
For gestational diabetes, new codes have been added for the use of hypoglycemic agents; therefore, no additional code is reported (TABLE).
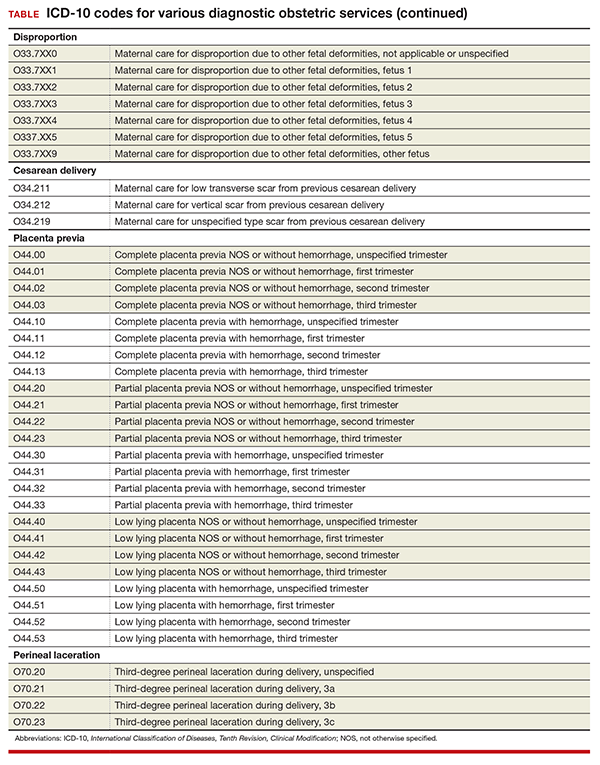
Disproportion code includes numeric specifier for fetus
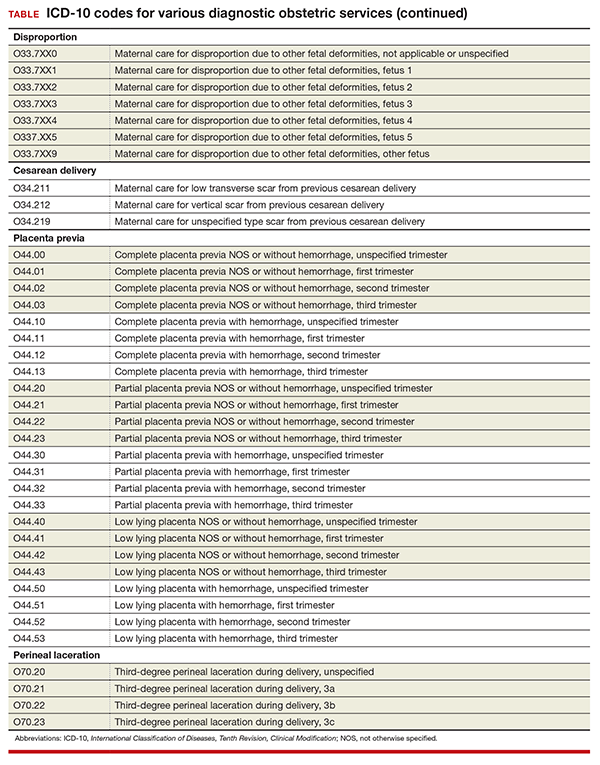
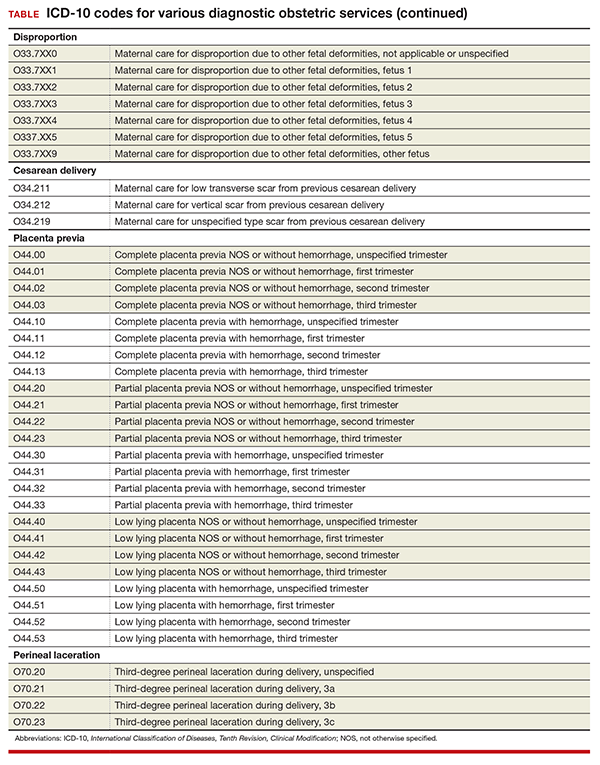
The disproportion code category was expanded to include a final digit for the fetus with the deformity (TABLE). The final digit of the code number denotes which fetus; for example, “0” means a singleton pregnancy, “1” means fetus 1 (number range from 1 to 5), and “9” denotes any fetus after the fifth.
Cesarean delivery scar codes expanded
The code for maternal care for a scar from a previous cesarean delivery has been expanded to 3 different codes (TABLE). Clinicians should make every effort to document and report the location of the previous cesarean as low transverse or vertical. From a coding standpoint, a vertical scar can also be referred to as a classical scar.
Changes to placenta previa codes
The code category for placenta previa has been expanded to capture the degree of previa as complete, partial, or low lying and with or without hemorrhage (TABLE). Going forward, it will be important to carefully document the circumstances so that the most specific code can be reported and tracked. Trimester specification is required as the final digit.
New subclassifications for perineal laceration
The code category for perineal laceration has been expanded with new codes to capture subclassifications for a third-degree laceration that can involve the external and internal anal sphincter (TABLE). Through its collaborative hub, the Women’s Health Registry Alliance (reVITALize) initiative, the American Congress of Obstetricians and Gynecologists (ACOG) worked on the current classification of third- and fourth-degree perineal lacerations, which has been adopted by the Royal College of Obstetricians and Gynaecologists.1
Under this subclassification, a 3a laceration would involve a tear of less than 50% of the external anal sphincter (EAS); 3b would involve a tear of more than 50% of the EAS; and 3c would mean that both the external and internal anal sphincter are torn. ACOG and its collaborative group encourage clinicians to use these subclassifications in documentation to allow for more robust data collection and complete repair information. From a payment standpoint, such information may go a long way to substantiating the severity of a tear, which may require more physician work.
Z code additions
Finally, the ever-popular diagnostic code for Rho(D) immunization is back, and 2 codes have been added for a gestational carrier and 1 for a family history of sudden infant death syndrome. The codes are:
- Z29.13 Encounter for prophylactic Rho(D) immune globulin
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z33.3 Pregnant state, gestational carrier
- Z84.82 Family history of sudden infant death syndrome.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee meeting: diagnosis agenda. September 23-24, 2014;38, 39. http://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed July 5, 2016.
By now the upheaval of changing to the new International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) diagnostic coding system has settled. The code freeze that was initiated in 2012 has ended, and the new and revised codes that will go into effect on October 1, 2016, are being revealed. Good documentation will lead to more accurate diagnostic coding, which in turn assists decision makers in their quest to report the health of our population and to make good decisions for resource allocation. You are in the unique position to assist in this process, so keep up the good work.
In this article, I focus on ICD-10 diagnostic coding for obstetric services. I will cover diagnostic coding for gynecologic services in the September issue of OBG Management.
Code revisions for uterine scar and more changes to note
With the upcoming edition of ICD-10, the code Z3A, Weeks’ gestation, will be changed from mandatory reporting to reporting if known. This means that if the patient is no longer pregnant, a Z3A code no longer needs to be reported, and if at the time of service the provider does not know the weeks’ gestation, Z3A would not be required. However, this information should be readily available during the antepartum period and should still be considered important to record and report. And it would still be reported for hospitalization for delivery.
If the code O09.81, Supervision of pregnancy resulting from assisted reproductive technology, is reported, the code Z33.3, Gestational carrier status, may be reported in addition for informational purposes.
When the code O34.29, Maternal care due to uterine scar from other previous surgery, is reported, the tabular index clarifies that this refers to a uterine scar from a transmural uterine incision other than that used for cesarean delivery. This would include incision into the uterine wall to remove fibroids.
The O42 code category, relating to Premature rupture of membranes, should now be interpreted to mean rupture of membranes at or after 37 completed weeks of gestation, rather than after 37 completed weeks.
The code category O99.6, Diseases of the digestive system complicating pregnancy, childbirth, and the puerperium, has been clarified: it does not include hemorrhoids in pregnancy. Therefore, a code from O22.4_ (a final digit of 0 [unspecified], 1, 2, or 3 is required for the trimester) also can be reported if hemorrhoids are present.
A note now clarifies that O99.82, Streptococcus B carrier state complicating pregnancy, childbirth, and the puerperium, cannot be reported with Z22.330, Carrier of streptococcus group B (GBS) in a nonpregnant woman.
New codes for specifying types of ectopic pregnancy
ICD-10 did not initially recognize ectopic pregnancy with and without intrauterine pregnancy, as was the case in ICD-9, but starting in October it will do so. In addition, a history of ectopic or molar pregnancy during a current pregnancy is now reported separately. Each of these codes will require a final digit to indicate the trimester (TABLE).
Codes added for complicating conditions of childbirth and the puerperium
Missing from the ICD-10 lineup last year were codes for conditions related to hypertension, edema, proteinuria, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and eclampsia that were complicating the pregnancy at the time of delivery or after delivery (TABLE).
Note that the “childbirth” code is reported only when a patient delivers at the current episode of care. Once a patient delivers and is discharged, the “puerperium” code should be selected.
Revised descriptions, new reporting instruction for diabetes
The code descriptions for preexisting type 1 and type 2 diabetes were revised, but this change does not impact reporting the codes. However, for type 2 diabetes, the instruction for reporting an additional code has changed. Now, in addition to reporting the code for current use of insulin (Z79.4), when appropriate, report the new added code for use of hypoglycemic agents (Z79.84), such as glyburide or metformin.
For gestational diabetes, new codes have been added for the use of hypoglycemic agents; therefore, no additional code is reported (TABLE).
Disproportion code includes numeric specifier for fetus
The disproportion code category was expanded to include a final digit for the fetus with the deformity (TABLE). The final digit of the code number denotes which fetus; for example, “0” means a singleton pregnancy, “1” means fetus 1 (number range from 1 to 5), and “9” denotes any fetus after the fifth.
Cesarean delivery scar codes expanded
The code for maternal care for a scar from a previous cesarean delivery has been expanded to 3 different codes (TABLE). Clinicians should make every effort to document and report the location of the previous cesarean as low transverse or vertical. From a coding standpoint, a vertical scar can also be referred to as a classical scar.
Changes to placenta previa codes
The code category for placenta previa has been expanded to capture the degree of previa as complete, partial, or low lying and with or without hemorrhage (TABLE). Going forward, it will be important to carefully document the circumstances so that the most specific code can be reported and tracked. Trimester specification is required as the final digit.
New subclassifications for perineal laceration
The code category for perineal laceration has been expanded with new codes to capture subclassifications for a third-degree laceration that can involve the external and internal anal sphincter (TABLE). Through its collaborative hub, the Women’s Health Registry Alliance (reVITALize) initiative, the American Congress of Obstetricians and Gynecologists (ACOG) worked on the current classification of third- and fourth-degree perineal lacerations, which has been adopted by the Royal College of Obstetricians and Gynaecologists.1
Under this subclassification, a 3a laceration would involve a tear of less than 50% of the external anal sphincter (EAS); 3b would involve a tear of more than 50% of the EAS; and 3c would mean that both the external and internal anal sphincter are torn. ACOG and its collaborative group encourage clinicians to use these subclassifications in documentation to allow for more robust data collection and complete repair information. From a payment standpoint, such information may go a long way to substantiating the severity of a tear, which may require more physician work.
Z code additions
Finally, the ever-popular diagnostic code for Rho(D) immunization is back, and 2 codes have been added for a gestational carrier and 1 for a family history of sudden infant death syndrome. The codes are:
- Z29.13 Encounter for prophylactic Rho(D) immune globulin
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z33.3 Pregnant state, gestational carrier
- Z84.82 Family history of sudden infant death syndrome.
By now the upheaval of changing to the new International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) diagnostic coding system has settled. The code freeze that was initiated in 2012 has ended, and the new and revised codes that will go into effect on October 1, 2016, are being revealed. Good documentation will lead to more accurate diagnostic coding, which in turn assists decision makers in their quest to report the health of our population and to make good decisions for resource allocation. You are in the unique position to assist in this process, so keep up the good work.
In this article, I focus on ICD-10 diagnostic coding for obstetric services. I will cover diagnostic coding for gynecologic services in the September issue of OBG Management.
Code revisions for uterine scar and more changes to note
With the upcoming edition of ICD-10, the code Z3A, Weeks’ gestation, will be changed from mandatory reporting to reporting if known. This means that if the patient is no longer pregnant, a Z3A code no longer needs to be reported, and if at the time of service the provider does not know the weeks’ gestation, Z3A would not be required. However, this information should be readily available during the antepartum period and should still be considered important to record and report. And it would still be reported for hospitalization for delivery.
If the code O09.81, Supervision of pregnancy resulting from assisted reproductive technology, is reported, the code Z33.3, Gestational carrier status, may be reported in addition for informational purposes.
When the code O34.29, Maternal care due to uterine scar from other previous surgery, is reported, the tabular index clarifies that this refers to a uterine scar from a transmural uterine incision other than that used for cesarean delivery. This would include incision into the uterine wall to remove fibroids.
The O42 code category, relating to Premature rupture of membranes, should now be interpreted to mean rupture of membranes at or after 37 completed weeks of gestation, rather than after 37 completed weeks.
The code category O99.6, Diseases of the digestive system complicating pregnancy, childbirth, and the puerperium, has been clarified: it does not include hemorrhoids in pregnancy. Therefore, a code from O22.4_ (a final digit of 0 [unspecified], 1, 2, or 3 is required for the trimester) also can be reported if hemorrhoids are present.
A note now clarifies that O99.82, Streptococcus B carrier state complicating pregnancy, childbirth, and the puerperium, cannot be reported with Z22.330, Carrier of streptococcus group B (GBS) in a nonpregnant woman.
New codes for specifying types of ectopic pregnancy
ICD-10 did not initially recognize ectopic pregnancy with and without intrauterine pregnancy, as was the case in ICD-9, but starting in October it will do so. In addition, a history of ectopic or molar pregnancy during a current pregnancy is now reported separately. Each of these codes will require a final digit to indicate the trimester (TABLE).
Codes added for complicating conditions of childbirth and the puerperium
Missing from the ICD-10 lineup last year were codes for conditions related to hypertension, edema, proteinuria, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and eclampsia that were complicating the pregnancy at the time of delivery or after delivery (TABLE).
Note that the “childbirth” code is reported only when a patient delivers at the current episode of care. Once a patient delivers and is discharged, the “puerperium” code should be selected.
Revised descriptions, new reporting instruction for diabetes
The code descriptions for preexisting type 1 and type 2 diabetes were revised, but this change does not impact reporting the codes. However, for type 2 diabetes, the instruction for reporting an additional code has changed. Now, in addition to reporting the code for current use of insulin (Z79.4), when appropriate, report the new added code for use of hypoglycemic agents (Z79.84), such as glyburide or metformin.
For gestational diabetes, new codes have been added for the use of hypoglycemic agents; therefore, no additional code is reported (TABLE).
Disproportion code includes numeric specifier for fetus
The disproportion code category was expanded to include a final digit for the fetus with the deformity (TABLE). The final digit of the code number denotes which fetus; for example, “0” means a singleton pregnancy, “1” means fetus 1 (number range from 1 to 5), and “9” denotes any fetus after the fifth.
Cesarean delivery scar codes expanded
The code for maternal care for a scar from a previous cesarean delivery has been expanded to 3 different codes (TABLE). Clinicians should make every effort to document and report the location of the previous cesarean as low transverse or vertical. From a coding standpoint, a vertical scar can also be referred to as a classical scar.
Changes to placenta previa codes
The code category for placenta previa has been expanded to capture the degree of previa as complete, partial, or low lying and with or without hemorrhage (TABLE). Going forward, it will be important to carefully document the circumstances so that the most specific code can be reported and tracked. Trimester specification is required as the final digit.
New subclassifications for perineal laceration
The code category for perineal laceration has been expanded with new codes to capture subclassifications for a third-degree laceration that can involve the external and internal anal sphincter (TABLE). Through its collaborative hub, the Women’s Health Registry Alliance (reVITALize) initiative, the American Congress of Obstetricians and Gynecologists (ACOG) worked on the current classification of third- and fourth-degree perineal lacerations, which has been adopted by the Royal College of Obstetricians and Gynaecologists.1
Under this subclassification, a 3a laceration would involve a tear of less than 50% of the external anal sphincter (EAS); 3b would involve a tear of more than 50% of the EAS; and 3c would mean that both the external and internal anal sphincter are torn. ACOG and its collaborative group encourage clinicians to use these subclassifications in documentation to allow for more robust data collection and complete repair information. From a payment standpoint, such information may go a long way to substantiating the severity of a tear, which may require more physician work.
Z code additions
Finally, the ever-popular diagnostic code for Rho(D) immunization is back, and 2 codes have been added for a gestational carrier and 1 for a family history of sudden infant death syndrome. The codes are:
- Z29.13 Encounter for prophylactic Rho(D) immune globulin
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z33.3 Pregnant state, gestational carrier
- Z84.82 Family history of sudden infant death syndrome.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee meeting: diagnosis agenda. September 23-24, 2014;38, 39. http://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed July 5, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee meeting: diagnosis agenda. September 23-24, 2014;38, 39. http://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed July 5, 2016.
In this Article
- New and expanded codes
- Z code additions
- Table of codes