User login
Update in Hospital Palliative Care
Seriously ill patients frequently receive care in hospitals,[1, 2, 3] and palliative care is a core competency for hospitalists.[4, 5] The goal of this update was to summarize and critique recently published research that has the highest potential to impact the clinical practice of palliative care in the hospital. We reviewed articles published between January 2012 and May 2013. To identify articles, we hand‐searched 22 leading journals (see Appendix) and the Cochrane Database of Systematic Reviews, and performed a PubMed keyword search using the terms hospice and palliative care. We evaluated identified articles based on scientific rigor and relevance to hospital practice. In this review, we summarize 9 articles that were collectively selected as having the highest impact on the clinical practice of hospital palliative care. We summarize each article and its findings and note cautions and implications for practice.
SYMPTOM MANAGEMENT
Indwelling Pleural Catheters and Talc Pleurodesis Provide Similar Dyspnea Relief in Patients With Malignant Pleural Effusions
Davies HE, Mishra EK, Kahan BC, et al. Effect of an indwelling pleural catheter vs chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion. JAMA. 2012;307:23832389.
Background
Expert guidelines recommend chest‐tube insertion and talc pleurodesis as a first‐line therapy for symptomatic malignant pleural effusions, but indwelling pleural catheters are gaining in popularity.[6] The optimal management is unknown.
Findings
A total of 106 patients with newly diagnosed symptomatic malignant pleural effusion were randomized to undergo talc pleurodesis or placement of an indwelling pleural catheter. Most patients had metastatic breast or lung cancer. Overall, there were no differences in relief of dyspnea at 42 days between patients who received indwelling catheters and pleurodesis; importantly, more than 75% of patients in both groups reported improved shortness of breath. The initial hospitalization was much shorter in the indwelling catheter group (0 days vs 4 days). There was no difference in quality of life, but in surviving patients, dyspnea at 6 months was better with the indwelling catheter. In the talc group, 22% of patients required further pleural procedures compared with 6% in the indwelling catheter group. Patients in the talc group had a higher frequency of adverse events than in the catheter group (40% vs 13%). In the catheter group, the most common adverse events were pleural infection, cellulitis, and catheter obstruction.
Cautions
The study was small and unblinded, and the primary outcome was subjective dyspnea. The study occurred at 7 hospitals, and the impact of institutional or provider experience was not taken into account. Last, overall costs of care, which could impact the choice of intervention, were not calculated.
Implications
This was a small but well‐done study showing that indwelling catheters and talc pleurodesis provide similar relief of dyspnea 42 days postintervention. Given these results, both interventions seem to be acceptable options. Clinicians and patients could select the best option based on local procedural expertise and patient factors such as preference, ability to manage a catheter, and life expectancy.
Most Dying Patients Do Not Experience Increased Respiratory Distress When Oxygen is Withdrawn
Campbell ML, Yarandi H, Dove‐Medows E. Oxygen is nonbeneficial for most patients who are near death. J Pain Symptom Manage. 2013;45(3):517523.
Background
Oxygen is frequently administered to patients at the end of life, yet there is limited evidence evaluating whether oxygen reduces respiratory distress in dying patients.
Findings
In this double‐blind, repeated‐measure study, patients served as their own controls as the investigators evaluated respiratory distress with and without oxygen therapy. The study included 32 patients who were enrolled in hospice or seen in palliative care consultation and had a diagnosis such as lung cancer or heart failure that might cause dyspnea. Medical air (nasal cannula with air flow), supplemental oxygen, and no flow were randomly alternated every 10 minutes for 1 hour. Blinded research assistants used a validated observation scale to compare respiratory distress under each condition. At baseline, 27 of 32 (84%) patients were on oxygen. Three patients, all of whom were conscious and on oxygen at baseline, experienced increased respiratory distress without oxygen; reapplication of supplemental oxygen relieved their distress. The other 29 patients had no change in respiratory distress under the oxygen, medical air, and no flow conditions.
Cautions
All patients in this study were near death as measured by the Palliative Performance Scale, which assesses prognosis based on functional status and level of consciousness. Patients were excluded if they were receiving high‐flow oxygen by face mask or were experiencing respiratory distress at the time of initial evaluation. Some patients experienced increased discomfort after withdrawal of oxygen. Close observation is needed to determine which patients will experience distress.
Implications
The majority of patients who were receiving oxygen at baseline experienced no change in respiratory comfort when oxygen was withdrawn, supporting previous evidence that oxygen provides little benefit in nonhypoxemic patients. Oxygen may be an unnecessary intervention near death and has the potential to add to discomfort through nasal dryness and decreased mobility.
Sennosides Performed Similarly to Docusate Plus Sennosides in Managing Opioid‐Induced Constipation in Seriously Ill Patients
Tarumi Y, Wilson MP, Szafran O, Spooner GR. Randomized, double‐blind, placebo‐controlled trial of oral docusate in the management of constipation in hospice patients. J Pain Symptom Manage. 2013;45:213.
Background
Seriously ill patients frequently suffer from constipation, often as a result of opioid analgesics. Hospital clinicians should seek to optimize bowel regimens to prevent opioid‐induced constipation. A combination of the stimulant laxative sennoside and the stool softener docusate is often recommended to treat and prevent constipation. Docusate may not have additional benefit to sennoside, and may have significant burdens, including disturbing the absorption of other medications, adding to patients' pill burden and increasing nurse workload.[7]
Findings
In this double‐blinded trial, 74 patients in 3 inpatient hospices in Canada were randomized to receive sennoside plus either docusate 100 mg, or placebo tablets twice daily, or sennoside plus placebo for 10 days. Most patients had cancer as a life‐limiting diagnosis and received opioids during the study period. All were able to tolerate pills and food or sips of fluid. There was no significant difference between the 2 groups in stool frequency, volume, consistency, or patients' perceptions of difficulty with defecation. The percentage of patients who had a bowel movement at least every 3 days was 71% in the docusate plus sennoside group and 81% in the sennoside only group (P=0.45). There was also no significant difference between the groups in sennoside dose (which ranged between 13, 8.6 mg tablets daily), mean morphine equivalent daily dosage, or other bowel interventions.
Cautions
The trial was small, though it was adequately powered to detect a clinically meaningful difference between the 2 groups of 0.5 in the average number of bowel movements per day. The consent rate was low (26%); the authors do not detail reasons patients were not randomized. Patients who did not participate might have had different responses.
Implications
Consistent with previous work,[7] these results indicate that docusate is probably not needed for routine management of opioid‐induced constipation in seriously ill patients.
Sublingual Atropine Performed Similarly to Placebo in Reducing Noise Associated With Respiratory Rattle Near Death
Heisler M, Hamilton G, Abbott A, et al. Randomized double‐blind trial of sublingual atropine vs. placebo for the management of death rattle. J Pain Symptom Manage. 2012;45(1):1422.
Background
Increased respiratory tract secretions in patients near death can cause noisy breathing, often referred to as a death rattle. Antimuscarinic medications, such as atropine, are frequently used to decrease audible respirations and family distress, though little evidence exists to support this practice.
Findings
In this double‐blind, placebo‐controlled, parallel group trial at 3 inpatient hospices, 177 terminally ill patients with audible respiratory secretions were randomized to 2 drops of sublingual atropine 1% solution or placebo drops. Bedside nurses rated patients' respiratory secretions at enrollment, and 2 and 4 hours after receiving atropine or placebo. There were no differences in noise score between subjects treated with atropine and placebo at 2 hours (37.8% vs. 41.3%, P=0.24) or at 4 hours (39.7% and 51.7%, P=0.21). There were no differences in the safety end point of change in heart rate (P=0.47).
Cautions
Previous studies comparing different anticholinergic medications and routes of administration to manage audible respiratory secretions had variable response rates but suggested a benefit to antimuscarinic medications. However, these trials had significant methodological limitations including lack of randomization and blinding. The improvement in death rattle over time in other studies may suggest a favorable natural course for respiratory secretions rather than a treatment effect.
Implications
Although generalizability to other antimuscarinic medications and routes of administration is limited, in a randomized, double‐blind, placebo‐controlled trial, sublingual atropine did not reduce the noise from respiratory secretions when compared to placebo.
PATIENT AND FAMILY OUTCOMES AFTER CARDIOPULMONARY RESUSCITATION
Over Half of Older Adult Survivors of In‐Hospital Cardiopulmonary Resuscitation Were Alive At 1 Year
Chan PS, Krumholz HM, Spertus JA, et al. Long‐term outcomes in elderly survivors of in‐hospital cardiac arrest. N Engl J Med. 2013;368:10191026.
Background
Studies of cardiopulmonary resuscitation (CPR) outcomes have focused on survival to hospital discharge. Little is known about long‐term outcomes following in‐hospital cardiac arrest in older adults.
Findings
The authors analyzed data from the Get With the GuidelinesResuscitation registry from 2000 to 2008 and Medicare inpatient files from 2000 to 2010. The cohort included 6972 patients at 401 hospitals who were discharged after surviving in‐hospital arrest. Outcomes were survival and freedom from hospital readmission at 1 year after discharge. At discharge, 48% of patients had either no or mild neurologic disability at discharge; the remainder had moderate to severe neurologic disability. Overall, 58% of patients who were discharged were still alive at 1 year. Survival rates were lowest for patients who were discharged in coma or vegetative state (8% at 1 year), and highest for those discharged with mild or no disability (73% at 1 year). Older patients had lower survival rates than younger patients, as did men compared with women and blacks compared with whites. At 1 year, 34.4% of the patients had not been readmitted. Predictors of readmission were similar to those for lower survival rates.
Cautions
This study only analyzed survival data from patients who survived to hospital discharge after receiving in‐hospital CPR, not all patients who had a cardiac arrest. Thus, the survival rates reported here do not include patients who died during the original arrest, or who survived the arrest but died during their hospitalization. The 1‐year survival rate for people aged 65 years and above following a cardiac arrest is not reported but is likely to be about 10%, based on data from this registry.[8] Data were not available for health status, neurologic status, or quality of life of the survivors at 1 year.
Implications
Older patients who receive in‐hospital CPR and have a good neurologic status at hospital discharge have good long‐term outcomes. In counseling patients about CPR, it is important to note that most patients who receive CPR do not survive to hospital discharge.
Families Who Were Present During CPR Had Decreased Post‐traumatic Stress Symptoms
Jabre P, Belpomme V, Azoulay E, et al. Family presence during cardiopulmonary resuscitation. N Engl J Med. 2013;368:10081018.
Background
Family members who watch their loved ones undergo (CPR) might have increased emotional distress. Alternatively, observing CPR may allow for appreciation of the efforts taken for their loved one and provide comfort at a challenging time. The right balance of benefit and harm is unclear.
Findings
Between 2009 and 2011, 15 prehospital emergency medical service units in France were randomized to offer adult family members the opportunity to observe CPR or follow their usual practice. A total of 570 relatives were enrolled. In the intervention group, 79% of relatives observed CPR, compared to 43% in the control group. There was no difference in the effectiveness of CPR between the 2 groups. At 90 days, post‐traumatic stress symptoms were more common in the control group (adjusted odds ratio [OR]: 1.7; 95% confidence interval [CI]: 1.2‐2.5). At 90 days, those who were present for the resuscitation also had fewer symptoms of anxiety and fewer symptoms of depression (P0.009 for both). Stress of the medical teams involved in the CPR was not different between the 2 groups. No malpractice claims were filed in either group.
Cautions
The study was conducted only in France, so the results may not be generalizable outside of France. In addition, the observed resuscitation was for patients who suffered a cardiac arrest in the home; it is unclear if the same results would be found in the emergency department or hospital.
Implications
This is the highest quality study to date in this area that argues for actively inviting family members to be present for resuscitation efforts in the home. Further studies are needed to determine if hospitals should implement standard protocols. In the meantime, providers who perform CPR should consider inviting families to observe, as it may result in less emotional distress for family members.
COMMUNICATION AND DECISION MAKING
Surrogate Decision Makers Interpreted Prognostic Information Optimistically
Zier LS, Sottile PD, Hong SY, et al. Surrogate decision makers' interpretation of prognostic information: a mixed‐methods study. Ann Intern Med. 2012;156:360366.
Background
Surrogates of critically ill patients often have beliefs about prognosis that are discordant from what is told to them by providers. Little is known about why this is the case.
Findings
Eighty surrogates of patients in intensive care units (ICUs) were given questionnaires with hypothetical prognostic statements and asked to identify a survival probability associated with each statement on a 0% to 100% scale. Interviewers examined the questionnaires to identify responses that were not concordant with the given prognostic statements. They then interviewed participants to determine why the answers were discordant. The researchers found that surrogates were more likely to offer an overoptimistic interpretation of statements communicating a high risk of death, compared to statements communicating a low risk of death. The qualitative interviews revealed that surrogates felt they needed to express ongoing optimism and that patient factors not known to the medical team would lead to better outcomes.
Cautions
The participants were surrogates who were present in the ICU at the time when study investigators were there, and thus the results may not be generalizable to all surrogates. Only a subset of participants completed qualitative interviews. Prognostic statements were hypothetical. Written prognostic statements may be interpreted differently than spoken statements.
Implications
Surrogate decision makers may interpret prognostic statements optimistically, especially when a high risk of death is estimated. Inaccurate interpretation may be related to personal beliefs about the patients' strengths and a need to hold onto hope for a positive outcome. When communicating with surrogates of critically ill patients, providers should be aware that, beyond the actual information shared, many other factors influence surrogates' beliefs about prognosis.
A Majority of Patients With Metastatic Cancer Felt That Chemotherapy Might Cure Their Disease
Weeks JC, Catalano PJ, Chronin A, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367:16161625.
Background
Chemotherapy for advanced cancer is not curative, and many cancer patients overestimate their prognosis. Little is known about patients' understanding of the goals of chemotherapy when cancer is advanced.
Findings
Participants were part of the Cancer Care Outcomes Research and Surveillance study. Patients with stage IV lung or colon cancer who opted to receive chemotherapy (n=1193) were asked how likely they thought it was that the chemotherapy would cure their cancer. A majority (69% of lung cancer patients and 81% of colon cancer patients) felt that chemotherapy might cure their disease. Those who rated their physicians very favorably in satisfaction surveys were more likely to feel that that chemotherapy might be curative, compared to those who rated their physician less favorably (OR: 1.90; 95% CI: 1.33‐2.72).
Cautions
The study did not include patients who died soon after diagnosis and thus does not provide information about those who opted for chemotherapy but did not survive to the interview. It is possible that responses were influenced by participants' need to express optimism (social desirability bias). It is not clear how or whether prognostic disclosure by physicians caused the lower satisfaction ratings.
Implications
Despite the fact that stage IV lung and colon cancer are not curable with chemotherapy, a majority of patients reported believing that chemotherapy might cure their disease. Hospital clinicians should be aware that many patients who they view as terminally ill believe their illness may be cured.
Older Patients Who Viewed a Goals‐of‐Care Video at Admission to a Skilled Nursing Facility Were More Likely to Prefer Comfort Care
Volandes AE, Brandeis GH, Davis AD, et al. A randomized controlled trial of a goals‐of‐care video for elderly patients admitted to skilled nursing facilities. J Palliat Med. 2012;15:805811.
Background
Seriously ill older patients are frequently discharged from hospitals to skilled nursing facilities (SNFs). It is important to clarify and document patients' goals for care at the time of admission to SNFs, to ensure that care provided there is consistent with patients' preferences. Previous work has shown promise using videos to assist patients in advance‐care planning, providing realistic and standardized portrayals of different treatment options.[9, 10]
Findings
English‐speaking patients at least 65 years of age who did not have altered mental status were randomized to hear a verbal description (n=51) or view a 6‐minute video (n=50) that presented the same information accompanied by pictures of patients of 3 possible goals of medical care: life‐prolonging care, limited medical care, and comfort care. After the video or narrative, patients were asked what their care preference would be if they became more ill while at the SNF. Patients who viewed the video were more likely to report a preference for comfort care, compared to patients who received the narrative, 80% vs 57%, P=0.02. In a review of medical records, only 31% of patients who reported a preference for comfort care had a do not resuscitate order at the SNF.
Cautions
The study was conducted at 2 nursing homes located in the Boston, Massachusetts area, which may limit generalizability. Assessors were not blinded to whether the patient saw the video or received the narrative, which may have introduced bias. The authors note that the video aimed to present the different care options without valuing one over the other, though it may have inadvertently presented one option in a more favorable light.
Implications
Videos may be powerful tools for helping nursing home patients to clarify goals of care, and might be applied in the hospital setting prior to transferring patients to nursing homes. There is a significant opportunity to improve concordance of care with preferences through better documentation and implementation of code status orders when transferring patients to SNFs.
Acknowledgments
Disclosures: Drs. Anderson and Johnson and Mr. Horton received an honorarium and support for travel to present findings resulting from the literature review at the Annual Assembly of the American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association on March 16, 2013 in New Orleans, Louisiana. Dr. Anderson was funded by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF‐CTSI grant number KL2TR000143. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The authors report no conflicts of interest.
APPENDIX
Journals That Were Hand Searched to Identify Articles, By Topic Area
General:
- British Medical Journal
- Journal of the American Medical Association
- Lancet
- New England Journal of Medicine
Internal medicine:
- Annals Internal Medicine
- Archives Internal Medicine
- Journal of General Internal Medicine
- Journal of Hospital Medicine
Palliative care and symptom management:
- Journal Pain and Symptom Management
- Journal of Palliative Care
- Journal of Palliative Medicine
- Palliative Medicine
- Pain
Oncology:
- Journal of Clinical Oncology
- Supportive Care in Cancer
Critical care:
- American Journal of Respiratory and Critical Care Medicine
- Critical Care Medicine
Pediatrics:
- Pediatrics
Geriatrics:
- Journal of the American Geriatrics Society
Education:
- Academic Medicine
Nursing:
- Journal of Hospice and Palliative Nursing
- Oncology Nursing Forum
- The Dartmouth Atlas of Health Care. Percent of Medicare decedents hospitalized at least once during the last six months of life 2007. Available at: http://www.dartmouthatlas.org/data/table.aspx?ind=133. Accessed October 30, 2013.
- , , , et al. Change in end‐of‐life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309(5):470–477.
- , , , et al. End‐of‐life care for lung cancer patients in the United States and Ontario. J Natl Cancer Inst. 2011;103(11):853–862.
- , , , , . Core competencies in hospital medicine: development and methodology. J Hosp Med. 2006;1(suppl 1):48–56.
- Society of Hospital Medicine; 2008.The core competencies in hospital medicine. http://www.hospitalmedicine.org/Content/NavigationMenu/Education/CoreCurriculum/Core_Competencies.htm. Accessed October 30, 2013.
- , , , , . Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline. Thorax. 2010;65:ii32–ii40.
- , . A comparison of sennosides‐based bowel protocols with and without docusate in hospitalized patients with cancer. J Palliat Med. 2008;11(4):575–581.
- , , , , , . Trends in survival after In‐hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920.
- , , , et al. Use of video to facilitate end‐of‐life discussions with patients with cancer: a randomized controlled trial. J Clin Oncol. 2010;28(2):305–310.
- , , , et al. Augmenting advance care planning in poor prognosis cancer with a video decision aid: a preintervention‐postintervention study. Cancer. 2012;118(17):4331–4338.
Seriously ill patients frequently receive care in hospitals,[1, 2, 3] and palliative care is a core competency for hospitalists.[4, 5] The goal of this update was to summarize and critique recently published research that has the highest potential to impact the clinical practice of palliative care in the hospital. We reviewed articles published between January 2012 and May 2013. To identify articles, we hand‐searched 22 leading journals (see Appendix) and the Cochrane Database of Systematic Reviews, and performed a PubMed keyword search using the terms hospice and palliative care. We evaluated identified articles based on scientific rigor and relevance to hospital practice. In this review, we summarize 9 articles that were collectively selected as having the highest impact on the clinical practice of hospital palliative care. We summarize each article and its findings and note cautions and implications for practice.
SYMPTOM MANAGEMENT
Indwelling Pleural Catheters and Talc Pleurodesis Provide Similar Dyspnea Relief in Patients With Malignant Pleural Effusions
Davies HE, Mishra EK, Kahan BC, et al. Effect of an indwelling pleural catheter vs chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion. JAMA. 2012;307:23832389.
Background
Expert guidelines recommend chest‐tube insertion and talc pleurodesis as a first‐line therapy for symptomatic malignant pleural effusions, but indwelling pleural catheters are gaining in popularity.[6] The optimal management is unknown.
Findings
A total of 106 patients with newly diagnosed symptomatic malignant pleural effusion were randomized to undergo talc pleurodesis or placement of an indwelling pleural catheter. Most patients had metastatic breast or lung cancer. Overall, there were no differences in relief of dyspnea at 42 days between patients who received indwelling catheters and pleurodesis; importantly, more than 75% of patients in both groups reported improved shortness of breath. The initial hospitalization was much shorter in the indwelling catheter group (0 days vs 4 days). There was no difference in quality of life, but in surviving patients, dyspnea at 6 months was better with the indwelling catheter. In the talc group, 22% of patients required further pleural procedures compared with 6% in the indwelling catheter group. Patients in the talc group had a higher frequency of adverse events than in the catheter group (40% vs 13%). In the catheter group, the most common adverse events were pleural infection, cellulitis, and catheter obstruction.
Cautions
The study was small and unblinded, and the primary outcome was subjective dyspnea. The study occurred at 7 hospitals, and the impact of institutional or provider experience was not taken into account. Last, overall costs of care, which could impact the choice of intervention, were not calculated.
Implications
This was a small but well‐done study showing that indwelling catheters and talc pleurodesis provide similar relief of dyspnea 42 days postintervention. Given these results, both interventions seem to be acceptable options. Clinicians and patients could select the best option based on local procedural expertise and patient factors such as preference, ability to manage a catheter, and life expectancy.
Most Dying Patients Do Not Experience Increased Respiratory Distress When Oxygen is Withdrawn
Campbell ML, Yarandi H, Dove‐Medows E. Oxygen is nonbeneficial for most patients who are near death. J Pain Symptom Manage. 2013;45(3):517523.
Background
Oxygen is frequently administered to patients at the end of life, yet there is limited evidence evaluating whether oxygen reduces respiratory distress in dying patients.
Findings
In this double‐blind, repeated‐measure study, patients served as their own controls as the investigators evaluated respiratory distress with and without oxygen therapy. The study included 32 patients who were enrolled in hospice or seen in palliative care consultation and had a diagnosis such as lung cancer or heart failure that might cause dyspnea. Medical air (nasal cannula with air flow), supplemental oxygen, and no flow were randomly alternated every 10 minutes for 1 hour. Blinded research assistants used a validated observation scale to compare respiratory distress under each condition. At baseline, 27 of 32 (84%) patients were on oxygen. Three patients, all of whom were conscious and on oxygen at baseline, experienced increased respiratory distress without oxygen; reapplication of supplemental oxygen relieved their distress. The other 29 patients had no change in respiratory distress under the oxygen, medical air, and no flow conditions.
Cautions
All patients in this study were near death as measured by the Palliative Performance Scale, which assesses prognosis based on functional status and level of consciousness. Patients were excluded if they were receiving high‐flow oxygen by face mask or were experiencing respiratory distress at the time of initial evaluation. Some patients experienced increased discomfort after withdrawal of oxygen. Close observation is needed to determine which patients will experience distress.
Implications
The majority of patients who were receiving oxygen at baseline experienced no change in respiratory comfort when oxygen was withdrawn, supporting previous evidence that oxygen provides little benefit in nonhypoxemic patients. Oxygen may be an unnecessary intervention near death and has the potential to add to discomfort through nasal dryness and decreased mobility.
Sennosides Performed Similarly to Docusate Plus Sennosides in Managing Opioid‐Induced Constipation in Seriously Ill Patients
Tarumi Y, Wilson MP, Szafran O, Spooner GR. Randomized, double‐blind, placebo‐controlled trial of oral docusate in the management of constipation in hospice patients. J Pain Symptom Manage. 2013;45:213.
Background
Seriously ill patients frequently suffer from constipation, often as a result of opioid analgesics. Hospital clinicians should seek to optimize bowel regimens to prevent opioid‐induced constipation. A combination of the stimulant laxative sennoside and the stool softener docusate is often recommended to treat and prevent constipation. Docusate may not have additional benefit to sennoside, and may have significant burdens, including disturbing the absorption of other medications, adding to patients' pill burden and increasing nurse workload.[7]
Findings
In this double‐blinded trial, 74 patients in 3 inpatient hospices in Canada were randomized to receive sennoside plus either docusate 100 mg, or placebo tablets twice daily, or sennoside plus placebo for 10 days. Most patients had cancer as a life‐limiting diagnosis and received opioids during the study period. All were able to tolerate pills and food or sips of fluid. There was no significant difference between the 2 groups in stool frequency, volume, consistency, or patients' perceptions of difficulty with defecation. The percentage of patients who had a bowel movement at least every 3 days was 71% in the docusate plus sennoside group and 81% in the sennoside only group (P=0.45). There was also no significant difference between the groups in sennoside dose (which ranged between 13, 8.6 mg tablets daily), mean morphine equivalent daily dosage, or other bowel interventions.
Cautions
The trial was small, though it was adequately powered to detect a clinically meaningful difference between the 2 groups of 0.5 in the average number of bowel movements per day. The consent rate was low (26%); the authors do not detail reasons patients were not randomized. Patients who did not participate might have had different responses.
Implications
Consistent with previous work,[7] these results indicate that docusate is probably not needed for routine management of opioid‐induced constipation in seriously ill patients.
Sublingual Atropine Performed Similarly to Placebo in Reducing Noise Associated With Respiratory Rattle Near Death
Heisler M, Hamilton G, Abbott A, et al. Randomized double‐blind trial of sublingual atropine vs. placebo for the management of death rattle. J Pain Symptom Manage. 2012;45(1):1422.
Background
Increased respiratory tract secretions in patients near death can cause noisy breathing, often referred to as a death rattle. Antimuscarinic medications, such as atropine, are frequently used to decrease audible respirations and family distress, though little evidence exists to support this practice.
Findings
In this double‐blind, placebo‐controlled, parallel group trial at 3 inpatient hospices, 177 terminally ill patients with audible respiratory secretions were randomized to 2 drops of sublingual atropine 1% solution or placebo drops. Bedside nurses rated patients' respiratory secretions at enrollment, and 2 and 4 hours after receiving atropine or placebo. There were no differences in noise score between subjects treated with atropine and placebo at 2 hours (37.8% vs. 41.3%, P=0.24) or at 4 hours (39.7% and 51.7%, P=0.21). There were no differences in the safety end point of change in heart rate (P=0.47).
Cautions
Previous studies comparing different anticholinergic medications and routes of administration to manage audible respiratory secretions had variable response rates but suggested a benefit to antimuscarinic medications. However, these trials had significant methodological limitations including lack of randomization and blinding. The improvement in death rattle over time in other studies may suggest a favorable natural course for respiratory secretions rather than a treatment effect.
Implications
Although generalizability to other antimuscarinic medications and routes of administration is limited, in a randomized, double‐blind, placebo‐controlled trial, sublingual atropine did not reduce the noise from respiratory secretions when compared to placebo.
PATIENT AND FAMILY OUTCOMES AFTER CARDIOPULMONARY RESUSCITATION
Over Half of Older Adult Survivors of In‐Hospital Cardiopulmonary Resuscitation Were Alive At 1 Year
Chan PS, Krumholz HM, Spertus JA, et al. Long‐term outcomes in elderly survivors of in‐hospital cardiac arrest. N Engl J Med. 2013;368:10191026.
Background
Studies of cardiopulmonary resuscitation (CPR) outcomes have focused on survival to hospital discharge. Little is known about long‐term outcomes following in‐hospital cardiac arrest in older adults.
Findings
The authors analyzed data from the Get With the GuidelinesResuscitation registry from 2000 to 2008 and Medicare inpatient files from 2000 to 2010. The cohort included 6972 patients at 401 hospitals who were discharged after surviving in‐hospital arrest. Outcomes were survival and freedom from hospital readmission at 1 year after discharge. At discharge, 48% of patients had either no or mild neurologic disability at discharge; the remainder had moderate to severe neurologic disability. Overall, 58% of patients who were discharged were still alive at 1 year. Survival rates were lowest for patients who were discharged in coma or vegetative state (8% at 1 year), and highest for those discharged with mild or no disability (73% at 1 year). Older patients had lower survival rates than younger patients, as did men compared with women and blacks compared with whites. At 1 year, 34.4% of the patients had not been readmitted. Predictors of readmission were similar to those for lower survival rates.
Cautions
This study only analyzed survival data from patients who survived to hospital discharge after receiving in‐hospital CPR, not all patients who had a cardiac arrest. Thus, the survival rates reported here do not include patients who died during the original arrest, or who survived the arrest but died during their hospitalization. The 1‐year survival rate for people aged 65 years and above following a cardiac arrest is not reported but is likely to be about 10%, based on data from this registry.[8] Data were not available for health status, neurologic status, or quality of life of the survivors at 1 year.
Implications
Older patients who receive in‐hospital CPR and have a good neurologic status at hospital discharge have good long‐term outcomes. In counseling patients about CPR, it is important to note that most patients who receive CPR do not survive to hospital discharge.
Families Who Were Present During CPR Had Decreased Post‐traumatic Stress Symptoms
Jabre P, Belpomme V, Azoulay E, et al. Family presence during cardiopulmonary resuscitation. N Engl J Med. 2013;368:10081018.
Background
Family members who watch their loved ones undergo (CPR) might have increased emotional distress. Alternatively, observing CPR may allow for appreciation of the efforts taken for their loved one and provide comfort at a challenging time. The right balance of benefit and harm is unclear.
Findings
Between 2009 and 2011, 15 prehospital emergency medical service units in France were randomized to offer adult family members the opportunity to observe CPR or follow their usual practice. A total of 570 relatives were enrolled. In the intervention group, 79% of relatives observed CPR, compared to 43% in the control group. There was no difference in the effectiveness of CPR between the 2 groups. At 90 days, post‐traumatic stress symptoms were more common in the control group (adjusted odds ratio [OR]: 1.7; 95% confidence interval [CI]: 1.2‐2.5). At 90 days, those who were present for the resuscitation also had fewer symptoms of anxiety and fewer symptoms of depression (P0.009 for both). Stress of the medical teams involved in the CPR was not different between the 2 groups. No malpractice claims were filed in either group.
Cautions
The study was conducted only in France, so the results may not be generalizable outside of France. In addition, the observed resuscitation was for patients who suffered a cardiac arrest in the home; it is unclear if the same results would be found in the emergency department or hospital.
Implications
This is the highest quality study to date in this area that argues for actively inviting family members to be present for resuscitation efforts in the home. Further studies are needed to determine if hospitals should implement standard protocols. In the meantime, providers who perform CPR should consider inviting families to observe, as it may result in less emotional distress for family members.
COMMUNICATION AND DECISION MAKING
Surrogate Decision Makers Interpreted Prognostic Information Optimistically
Zier LS, Sottile PD, Hong SY, et al. Surrogate decision makers' interpretation of prognostic information: a mixed‐methods study. Ann Intern Med. 2012;156:360366.
Background
Surrogates of critically ill patients often have beliefs about prognosis that are discordant from what is told to them by providers. Little is known about why this is the case.
Findings
Eighty surrogates of patients in intensive care units (ICUs) were given questionnaires with hypothetical prognostic statements and asked to identify a survival probability associated with each statement on a 0% to 100% scale. Interviewers examined the questionnaires to identify responses that were not concordant with the given prognostic statements. They then interviewed participants to determine why the answers were discordant. The researchers found that surrogates were more likely to offer an overoptimistic interpretation of statements communicating a high risk of death, compared to statements communicating a low risk of death. The qualitative interviews revealed that surrogates felt they needed to express ongoing optimism and that patient factors not known to the medical team would lead to better outcomes.
Cautions
The participants were surrogates who were present in the ICU at the time when study investigators were there, and thus the results may not be generalizable to all surrogates. Only a subset of participants completed qualitative interviews. Prognostic statements were hypothetical. Written prognostic statements may be interpreted differently than spoken statements.
Implications
Surrogate decision makers may interpret prognostic statements optimistically, especially when a high risk of death is estimated. Inaccurate interpretation may be related to personal beliefs about the patients' strengths and a need to hold onto hope for a positive outcome. When communicating with surrogates of critically ill patients, providers should be aware that, beyond the actual information shared, many other factors influence surrogates' beliefs about prognosis.
A Majority of Patients With Metastatic Cancer Felt That Chemotherapy Might Cure Their Disease
Weeks JC, Catalano PJ, Chronin A, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367:16161625.
Background
Chemotherapy for advanced cancer is not curative, and many cancer patients overestimate their prognosis. Little is known about patients' understanding of the goals of chemotherapy when cancer is advanced.
Findings
Participants were part of the Cancer Care Outcomes Research and Surveillance study. Patients with stage IV lung or colon cancer who opted to receive chemotherapy (n=1193) were asked how likely they thought it was that the chemotherapy would cure their cancer. A majority (69% of lung cancer patients and 81% of colon cancer patients) felt that chemotherapy might cure their disease. Those who rated their physicians very favorably in satisfaction surveys were more likely to feel that that chemotherapy might be curative, compared to those who rated their physician less favorably (OR: 1.90; 95% CI: 1.33‐2.72).
Cautions
The study did not include patients who died soon after diagnosis and thus does not provide information about those who opted for chemotherapy but did not survive to the interview. It is possible that responses were influenced by participants' need to express optimism (social desirability bias). It is not clear how or whether prognostic disclosure by physicians caused the lower satisfaction ratings.
Implications
Despite the fact that stage IV lung and colon cancer are not curable with chemotherapy, a majority of patients reported believing that chemotherapy might cure their disease. Hospital clinicians should be aware that many patients who they view as terminally ill believe their illness may be cured.
Older Patients Who Viewed a Goals‐of‐Care Video at Admission to a Skilled Nursing Facility Were More Likely to Prefer Comfort Care
Volandes AE, Brandeis GH, Davis AD, et al. A randomized controlled trial of a goals‐of‐care video for elderly patients admitted to skilled nursing facilities. J Palliat Med. 2012;15:805811.
Background
Seriously ill older patients are frequently discharged from hospitals to skilled nursing facilities (SNFs). It is important to clarify and document patients' goals for care at the time of admission to SNFs, to ensure that care provided there is consistent with patients' preferences. Previous work has shown promise using videos to assist patients in advance‐care planning, providing realistic and standardized portrayals of different treatment options.[9, 10]
Findings
English‐speaking patients at least 65 years of age who did not have altered mental status were randomized to hear a verbal description (n=51) or view a 6‐minute video (n=50) that presented the same information accompanied by pictures of patients of 3 possible goals of medical care: life‐prolonging care, limited medical care, and comfort care. After the video or narrative, patients were asked what their care preference would be if they became more ill while at the SNF. Patients who viewed the video were more likely to report a preference for comfort care, compared to patients who received the narrative, 80% vs 57%, P=0.02. In a review of medical records, only 31% of patients who reported a preference for comfort care had a do not resuscitate order at the SNF.
Cautions
The study was conducted at 2 nursing homes located in the Boston, Massachusetts area, which may limit generalizability. Assessors were not blinded to whether the patient saw the video or received the narrative, which may have introduced bias. The authors note that the video aimed to present the different care options without valuing one over the other, though it may have inadvertently presented one option in a more favorable light.
Implications
Videos may be powerful tools for helping nursing home patients to clarify goals of care, and might be applied in the hospital setting prior to transferring patients to nursing homes. There is a significant opportunity to improve concordance of care with preferences through better documentation and implementation of code status orders when transferring patients to SNFs.
Acknowledgments
Disclosures: Drs. Anderson and Johnson and Mr. Horton received an honorarium and support for travel to present findings resulting from the literature review at the Annual Assembly of the American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association on March 16, 2013 in New Orleans, Louisiana. Dr. Anderson was funded by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF‐CTSI grant number KL2TR000143. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The authors report no conflicts of interest.
APPENDIX
Journals That Were Hand Searched to Identify Articles, By Topic Area
General:
- British Medical Journal
- Journal of the American Medical Association
- Lancet
- New England Journal of Medicine
Internal medicine:
- Annals Internal Medicine
- Archives Internal Medicine
- Journal of General Internal Medicine
- Journal of Hospital Medicine
Palliative care and symptom management:
- Journal Pain and Symptom Management
- Journal of Palliative Care
- Journal of Palliative Medicine
- Palliative Medicine
- Pain
Oncology:
- Journal of Clinical Oncology
- Supportive Care in Cancer
Critical care:
- American Journal of Respiratory and Critical Care Medicine
- Critical Care Medicine
Pediatrics:
- Pediatrics
Geriatrics:
- Journal of the American Geriatrics Society
Education:
- Academic Medicine
Nursing:
- Journal of Hospice and Palliative Nursing
- Oncology Nursing Forum
Seriously ill patients frequently receive care in hospitals,[1, 2, 3] and palliative care is a core competency for hospitalists.[4, 5] The goal of this update was to summarize and critique recently published research that has the highest potential to impact the clinical practice of palliative care in the hospital. We reviewed articles published between January 2012 and May 2013. To identify articles, we hand‐searched 22 leading journals (see Appendix) and the Cochrane Database of Systematic Reviews, and performed a PubMed keyword search using the terms hospice and palliative care. We evaluated identified articles based on scientific rigor and relevance to hospital practice. In this review, we summarize 9 articles that were collectively selected as having the highest impact on the clinical practice of hospital palliative care. We summarize each article and its findings and note cautions and implications for practice.
SYMPTOM MANAGEMENT
Indwelling Pleural Catheters and Talc Pleurodesis Provide Similar Dyspnea Relief in Patients With Malignant Pleural Effusions
Davies HE, Mishra EK, Kahan BC, et al. Effect of an indwelling pleural catheter vs chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion. JAMA. 2012;307:23832389.
Background
Expert guidelines recommend chest‐tube insertion and talc pleurodesis as a first‐line therapy for symptomatic malignant pleural effusions, but indwelling pleural catheters are gaining in popularity.[6] The optimal management is unknown.
Findings
A total of 106 patients with newly diagnosed symptomatic malignant pleural effusion were randomized to undergo talc pleurodesis or placement of an indwelling pleural catheter. Most patients had metastatic breast or lung cancer. Overall, there were no differences in relief of dyspnea at 42 days between patients who received indwelling catheters and pleurodesis; importantly, more than 75% of patients in both groups reported improved shortness of breath. The initial hospitalization was much shorter in the indwelling catheter group (0 days vs 4 days). There was no difference in quality of life, but in surviving patients, dyspnea at 6 months was better with the indwelling catheter. In the talc group, 22% of patients required further pleural procedures compared with 6% in the indwelling catheter group. Patients in the talc group had a higher frequency of adverse events than in the catheter group (40% vs 13%). In the catheter group, the most common adverse events were pleural infection, cellulitis, and catheter obstruction.
Cautions
The study was small and unblinded, and the primary outcome was subjective dyspnea. The study occurred at 7 hospitals, and the impact of institutional or provider experience was not taken into account. Last, overall costs of care, which could impact the choice of intervention, were not calculated.
Implications
This was a small but well‐done study showing that indwelling catheters and talc pleurodesis provide similar relief of dyspnea 42 days postintervention. Given these results, both interventions seem to be acceptable options. Clinicians and patients could select the best option based on local procedural expertise and patient factors such as preference, ability to manage a catheter, and life expectancy.
Most Dying Patients Do Not Experience Increased Respiratory Distress When Oxygen is Withdrawn
Campbell ML, Yarandi H, Dove‐Medows E. Oxygen is nonbeneficial for most patients who are near death. J Pain Symptom Manage. 2013;45(3):517523.
Background
Oxygen is frequently administered to patients at the end of life, yet there is limited evidence evaluating whether oxygen reduces respiratory distress in dying patients.
Findings
In this double‐blind, repeated‐measure study, patients served as their own controls as the investigators evaluated respiratory distress with and without oxygen therapy. The study included 32 patients who were enrolled in hospice or seen in palliative care consultation and had a diagnosis such as lung cancer or heart failure that might cause dyspnea. Medical air (nasal cannula with air flow), supplemental oxygen, and no flow were randomly alternated every 10 minutes for 1 hour. Blinded research assistants used a validated observation scale to compare respiratory distress under each condition. At baseline, 27 of 32 (84%) patients were on oxygen. Three patients, all of whom were conscious and on oxygen at baseline, experienced increased respiratory distress without oxygen; reapplication of supplemental oxygen relieved their distress. The other 29 patients had no change in respiratory distress under the oxygen, medical air, and no flow conditions.
Cautions
All patients in this study were near death as measured by the Palliative Performance Scale, which assesses prognosis based on functional status and level of consciousness. Patients were excluded if they were receiving high‐flow oxygen by face mask or were experiencing respiratory distress at the time of initial evaluation. Some patients experienced increased discomfort after withdrawal of oxygen. Close observation is needed to determine which patients will experience distress.
Implications
The majority of patients who were receiving oxygen at baseline experienced no change in respiratory comfort when oxygen was withdrawn, supporting previous evidence that oxygen provides little benefit in nonhypoxemic patients. Oxygen may be an unnecessary intervention near death and has the potential to add to discomfort through nasal dryness and decreased mobility.
Sennosides Performed Similarly to Docusate Plus Sennosides in Managing Opioid‐Induced Constipation in Seriously Ill Patients
Tarumi Y, Wilson MP, Szafran O, Spooner GR. Randomized, double‐blind, placebo‐controlled trial of oral docusate in the management of constipation in hospice patients. J Pain Symptom Manage. 2013;45:213.
Background
Seriously ill patients frequently suffer from constipation, often as a result of opioid analgesics. Hospital clinicians should seek to optimize bowel regimens to prevent opioid‐induced constipation. A combination of the stimulant laxative sennoside and the stool softener docusate is often recommended to treat and prevent constipation. Docusate may not have additional benefit to sennoside, and may have significant burdens, including disturbing the absorption of other medications, adding to patients' pill burden and increasing nurse workload.[7]
Findings
In this double‐blinded trial, 74 patients in 3 inpatient hospices in Canada were randomized to receive sennoside plus either docusate 100 mg, or placebo tablets twice daily, or sennoside plus placebo for 10 days. Most patients had cancer as a life‐limiting diagnosis and received opioids during the study period. All were able to tolerate pills and food or sips of fluid. There was no significant difference between the 2 groups in stool frequency, volume, consistency, or patients' perceptions of difficulty with defecation. The percentage of patients who had a bowel movement at least every 3 days was 71% in the docusate plus sennoside group and 81% in the sennoside only group (P=0.45). There was also no significant difference between the groups in sennoside dose (which ranged between 13, 8.6 mg tablets daily), mean morphine equivalent daily dosage, or other bowel interventions.
Cautions
The trial was small, though it was adequately powered to detect a clinically meaningful difference between the 2 groups of 0.5 in the average number of bowel movements per day. The consent rate was low (26%); the authors do not detail reasons patients were not randomized. Patients who did not participate might have had different responses.
Implications
Consistent with previous work,[7] these results indicate that docusate is probably not needed for routine management of opioid‐induced constipation in seriously ill patients.
Sublingual Atropine Performed Similarly to Placebo in Reducing Noise Associated With Respiratory Rattle Near Death
Heisler M, Hamilton G, Abbott A, et al. Randomized double‐blind trial of sublingual atropine vs. placebo for the management of death rattle. J Pain Symptom Manage. 2012;45(1):1422.
Background
Increased respiratory tract secretions in patients near death can cause noisy breathing, often referred to as a death rattle. Antimuscarinic medications, such as atropine, are frequently used to decrease audible respirations and family distress, though little evidence exists to support this practice.
Findings
In this double‐blind, placebo‐controlled, parallel group trial at 3 inpatient hospices, 177 terminally ill patients with audible respiratory secretions were randomized to 2 drops of sublingual atropine 1% solution or placebo drops. Bedside nurses rated patients' respiratory secretions at enrollment, and 2 and 4 hours after receiving atropine or placebo. There were no differences in noise score between subjects treated with atropine and placebo at 2 hours (37.8% vs. 41.3%, P=0.24) or at 4 hours (39.7% and 51.7%, P=0.21). There were no differences in the safety end point of change in heart rate (P=0.47).
Cautions
Previous studies comparing different anticholinergic medications and routes of administration to manage audible respiratory secretions had variable response rates but suggested a benefit to antimuscarinic medications. However, these trials had significant methodological limitations including lack of randomization and blinding. The improvement in death rattle over time in other studies may suggest a favorable natural course for respiratory secretions rather than a treatment effect.
Implications
Although generalizability to other antimuscarinic medications and routes of administration is limited, in a randomized, double‐blind, placebo‐controlled trial, sublingual atropine did not reduce the noise from respiratory secretions when compared to placebo.
PATIENT AND FAMILY OUTCOMES AFTER CARDIOPULMONARY RESUSCITATION
Over Half of Older Adult Survivors of In‐Hospital Cardiopulmonary Resuscitation Were Alive At 1 Year
Chan PS, Krumholz HM, Spertus JA, et al. Long‐term outcomes in elderly survivors of in‐hospital cardiac arrest. N Engl J Med. 2013;368:10191026.
Background
Studies of cardiopulmonary resuscitation (CPR) outcomes have focused on survival to hospital discharge. Little is known about long‐term outcomes following in‐hospital cardiac arrest in older adults.
Findings
The authors analyzed data from the Get With the GuidelinesResuscitation registry from 2000 to 2008 and Medicare inpatient files from 2000 to 2010. The cohort included 6972 patients at 401 hospitals who were discharged after surviving in‐hospital arrest. Outcomes were survival and freedom from hospital readmission at 1 year after discharge. At discharge, 48% of patients had either no or mild neurologic disability at discharge; the remainder had moderate to severe neurologic disability. Overall, 58% of patients who were discharged were still alive at 1 year. Survival rates were lowest for patients who were discharged in coma or vegetative state (8% at 1 year), and highest for those discharged with mild or no disability (73% at 1 year). Older patients had lower survival rates than younger patients, as did men compared with women and blacks compared with whites. At 1 year, 34.4% of the patients had not been readmitted. Predictors of readmission were similar to those for lower survival rates.
Cautions
This study only analyzed survival data from patients who survived to hospital discharge after receiving in‐hospital CPR, not all patients who had a cardiac arrest. Thus, the survival rates reported here do not include patients who died during the original arrest, or who survived the arrest but died during their hospitalization. The 1‐year survival rate for people aged 65 years and above following a cardiac arrest is not reported but is likely to be about 10%, based on data from this registry.[8] Data were not available for health status, neurologic status, or quality of life of the survivors at 1 year.
Implications
Older patients who receive in‐hospital CPR and have a good neurologic status at hospital discharge have good long‐term outcomes. In counseling patients about CPR, it is important to note that most patients who receive CPR do not survive to hospital discharge.
Families Who Were Present During CPR Had Decreased Post‐traumatic Stress Symptoms
Jabre P, Belpomme V, Azoulay E, et al. Family presence during cardiopulmonary resuscitation. N Engl J Med. 2013;368:10081018.
Background
Family members who watch their loved ones undergo (CPR) might have increased emotional distress. Alternatively, observing CPR may allow for appreciation of the efforts taken for their loved one and provide comfort at a challenging time. The right balance of benefit and harm is unclear.
Findings
Between 2009 and 2011, 15 prehospital emergency medical service units in France were randomized to offer adult family members the opportunity to observe CPR or follow their usual practice. A total of 570 relatives were enrolled. In the intervention group, 79% of relatives observed CPR, compared to 43% in the control group. There was no difference in the effectiveness of CPR between the 2 groups. At 90 days, post‐traumatic stress symptoms were more common in the control group (adjusted odds ratio [OR]: 1.7; 95% confidence interval [CI]: 1.2‐2.5). At 90 days, those who were present for the resuscitation also had fewer symptoms of anxiety and fewer symptoms of depression (P0.009 for both). Stress of the medical teams involved in the CPR was not different between the 2 groups. No malpractice claims were filed in either group.
Cautions
The study was conducted only in France, so the results may not be generalizable outside of France. In addition, the observed resuscitation was for patients who suffered a cardiac arrest in the home; it is unclear if the same results would be found in the emergency department or hospital.
Implications
This is the highest quality study to date in this area that argues for actively inviting family members to be present for resuscitation efforts in the home. Further studies are needed to determine if hospitals should implement standard protocols. In the meantime, providers who perform CPR should consider inviting families to observe, as it may result in less emotional distress for family members.
COMMUNICATION AND DECISION MAKING
Surrogate Decision Makers Interpreted Prognostic Information Optimistically
Zier LS, Sottile PD, Hong SY, et al. Surrogate decision makers' interpretation of prognostic information: a mixed‐methods study. Ann Intern Med. 2012;156:360366.
Background
Surrogates of critically ill patients often have beliefs about prognosis that are discordant from what is told to them by providers. Little is known about why this is the case.
Findings
Eighty surrogates of patients in intensive care units (ICUs) were given questionnaires with hypothetical prognostic statements and asked to identify a survival probability associated with each statement on a 0% to 100% scale. Interviewers examined the questionnaires to identify responses that were not concordant with the given prognostic statements. They then interviewed participants to determine why the answers were discordant. The researchers found that surrogates were more likely to offer an overoptimistic interpretation of statements communicating a high risk of death, compared to statements communicating a low risk of death. The qualitative interviews revealed that surrogates felt they needed to express ongoing optimism and that patient factors not known to the medical team would lead to better outcomes.
Cautions
The participants were surrogates who were present in the ICU at the time when study investigators were there, and thus the results may not be generalizable to all surrogates. Only a subset of participants completed qualitative interviews. Prognostic statements were hypothetical. Written prognostic statements may be interpreted differently than spoken statements.
Implications
Surrogate decision makers may interpret prognostic statements optimistically, especially when a high risk of death is estimated. Inaccurate interpretation may be related to personal beliefs about the patients' strengths and a need to hold onto hope for a positive outcome. When communicating with surrogates of critically ill patients, providers should be aware that, beyond the actual information shared, many other factors influence surrogates' beliefs about prognosis.
A Majority of Patients With Metastatic Cancer Felt That Chemotherapy Might Cure Their Disease
Weeks JC, Catalano PJ, Chronin A, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367:16161625.
Background
Chemotherapy for advanced cancer is not curative, and many cancer patients overestimate their prognosis. Little is known about patients' understanding of the goals of chemotherapy when cancer is advanced.
Findings
Participants were part of the Cancer Care Outcomes Research and Surveillance study. Patients with stage IV lung or colon cancer who opted to receive chemotherapy (n=1193) were asked how likely they thought it was that the chemotherapy would cure their cancer. A majority (69% of lung cancer patients and 81% of colon cancer patients) felt that chemotherapy might cure their disease. Those who rated their physicians very favorably in satisfaction surveys were more likely to feel that that chemotherapy might be curative, compared to those who rated their physician less favorably (OR: 1.90; 95% CI: 1.33‐2.72).
Cautions
The study did not include patients who died soon after diagnosis and thus does not provide information about those who opted for chemotherapy but did not survive to the interview. It is possible that responses were influenced by participants' need to express optimism (social desirability bias). It is not clear how or whether prognostic disclosure by physicians caused the lower satisfaction ratings.
Implications
Despite the fact that stage IV lung and colon cancer are not curable with chemotherapy, a majority of patients reported believing that chemotherapy might cure their disease. Hospital clinicians should be aware that many patients who they view as terminally ill believe their illness may be cured.
Older Patients Who Viewed a Goals‐of‐Care Video at Admission to a Skilled Nursing Facility Were More Likely to Prefer Comfort Care
Volandes AE, Brandeis GH, Davis AD, et al. A randomized controlled trial of a goals‐of‐care video for elderly patients admitted to skilled nursing facilities. J Palliat Med. 2012;15:805811.
Background
Seriously ill older patients are frequently discharged from hospitals to skilled nursing facilities (SNFs). It is important to clarify and document patients' goals for care at the time of admission to SNFs, to ensure that care provided there is consistent with patients' preferences. Previous work has shown promise using videos to assist patients in advance‐care planning, providing realistic and standardized portrayals of different treatment options.[9, 10]
Findings
English‐speaking patients at least 65 years of age who did not have altered mental status were randomized to hear a verbal description (n=51) or view a 6‐minute video (n=50) that presented the same information accompanied by pictures of patients of 3 possible goals of medical care: life‐prolonging care, limited medical care, and comfort care. After the video or narrative, patients were asked what their care preference would be if they became more ill while at the SNF. Patients who viewed the video were more likely to report a preference for comfort care, compared to patients who received the narrative, 80% vs 57%, P=0.02. In a review of medical records, only 31% of patients who reported a preference for comfort care had a do not resuscitate order at the SNF.
Cautions
The study was conducted at 2 nursing homes located in the Boston, Massachusetts area, which may limit generalizability. Assessors were not blinded to whether the patient saw the video or received the narrative, which may have introduced bias. The authors note that the video aimed to present the different care options without valuing one over the other, though it may have inadvertently presented one option in a more favorable light.
Implications
Videos may be powerful tools for helping nursing home patients to clarify goals of care, and might be applied in the hospital setting prior to transferring patients to nursing homes. There is a significant opportunity to improve concordance of care with preferences through better documentation and implementation of code status orders when transferring patients to SNFs.
Acknowledgments
Disclosures: Drs. Anderson and Johnson and Mr. Horton received an honorarium and support for travel to present findings resulting from the literature review at the Annual Assembly of the American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association on March 16, 2013 in New Orleans, Louisiana. Dr. Anderson was funded by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF‐CTSI grant number KL2TR000143. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The authors report no conflicts of interest.
APPENDIX
Journals That Were Hand Searched to Identify Articles, By Topic Area
General:
- British Medical Journal
- Journal of the American Medical Association
- Lancet
- New England Journal of Medicine
Internal medicine:
- Annals Internal Medicine
- Archives Internal Medicine
- Journal of General Internal Medicine
- Journal of Hospital Medicine
Palliative care and symptom management:
- Journal Pain and Symptom Management
- Journal of Palliative Care
- Journal of Palliative Medicine
- Palliative Medicine
- Pain
Oncology:
- Journal of Clinical Oncology
- Supportive Care in Cancer
Critical care:
- American Journal of Respiratory and Critical Care Medicine
- Critical Care Medicine
Pediatrics:
- Pediatrics
Geriatrics:
- Journal of the American Geriatrics Society
Education:
- Academic Medicine
Nursing:
- Journal of Hospice and Palliative Nursing
- Oncology Nursing Forum
- The Dartmouth Atlas of Health Care. Percent of Medicare decedents hospitalized at least once during the last six months of life 2007. Available at: http://www.dartmouthatlas.org/data/table.aspx?ind=133. Accessed October 30, 2013.
- , , , et al. Change in end‐of‐life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309(5):470–477.
- , , , et al. End‐of‐life care for lung cancer patients in the United States and Ontario. J Natl Cancer Inst. 2011;103(11):853–862.
- , , , , . Core competencies in hospital medicine: development and methodology. J Hosp Med. 2006;1(suppl 1):48–56.
- Society of Hospital Medicine; 2008.The core competencies in hospital medicine. http://www.hospitalmedicine.org/Content/NavigationMenu/Education/CoreCurriculum/Core_Competencies.htm. Accessed October 30, 2013.
- , , , , . Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline. Thorax. 2010;65:ii32–ii40.
- , . A comparison of sennosides‐based bowel protocols with and without docusate in hospitalized patients with cancer. J Palliat Med. 2008;11(4):575–581.
- , , , , , . Trends in survival after In‐hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920.
- , , , et al. Use of video to facilitate end‐of‐life discussions with patients with cancer: a randomized controlled trial. J Clin Oncol. 2010;28(2):305–310.
- , , , et al. Augmenting advance care planning in poor prognosis cancer with a video decision aid: a preintervention‐postintervention study. Cancer. 2012;118(17):4331–4338.
- The Dartmouth Atlas of Health Care. Percent of Medicare decedents hospitalized at least once during the last six months of life 2007. Available at: http://www.dartmouthatlas.org/data/table.aspx?ind=133. Accessed October 30, 2013.
- , , , et al. Change in end‐of‐life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309(5):470–477.
- , , , et al. End‐of‐life care for lung cancer patients in the United States and Ontario. J Natl Cancer Inst. 2011;103(11):853–862.
- , , , , . Core competencies in hospital medicine: development and methodology. J Hosp Med. 2006;1(suppl 1):48–56.
- Society of Hospital Medicine; 2008.The core competencies in hospital medicine. http://www.hospitalmedicine.org/Content/NavigationMenu/Education/CoreCurriculum/Core_Competencies.htm. Accessed October 30, 2013.
- , , , , . Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline. Thorax. 2010;65:ii32–ii40.
- , . A comparison of sennosides‐based bowel protocols with and without docusate in hospitalized patients with cancer. J Palliat Med. 2008;11(4):575–581.
- , , , , , . Trends in survival after In‐hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920.
- , , , et al. Use of video to facilitate end‐of‐life discussions with patients with cancer: a randomized controlled trial. J Clin Oncol. 2010;28(2):305–310.
- , , , et al. Augmenting advance care planning in poor prognosis cancer with a video decision aid: a preintervention‐postintervention study. Cancer. 2012;118(17):4331–4338.
Communicating Discharge Instructions
Discharge from the hospital is a vulnerable time for patients. Nearly 1 in 5 patients experiences an adverse event during this transition, with a third of these being likely preventable.1, 2 Comprehensive discharge instructions are necessary to ensure a smooth transition from hospital to home, as the responsibility for care shifts from providers to the patient and caregivers. Unfortunately, patients often go home without understanding critical information about their hospital stay, such as their discharge diagnosis or medication changes,3, 4 leaving them both dissatisfied with their discharge instructions5 and at risk for hospital readmission.
Efforts to improve discharge education have focused on increasing communication between care provider and patient. The use of designated discharge coordinators,6, 7 implementation of teach‐back techniques to assess and confirm understanding,8 and adoption of patient‐centered educational materials all offer tools to improve communication with patients. However, guidelines for communication between providers and their shared role in patient discharge education, particularly between nurses and physicians, are scarce. Daily interdisciplinary rounds9 and shared electronic health records are potential ways to foster such communication, but the methods and frequency with which providers communicate about discharge instructions with each other is poorly understood. Furthermore, despite a common set of goals for discharge instructions,10, 11 it is unclear where the responsibility to provide these elements lies: with nurses, physicians, neither, or both.
Understanding perceptions and communication practices of providers in their delivery of discharge instructions is an important first step in defining responsibilities and improving accountability for discharge education. In this study, we surveyed nurses and physicians about their discharge education practices to better understand how each group sees their own role in discharge teaching, and how these findings may generate recommendations to improve future practices.
METHODS
Setting and Subjects
University of California, San Francisco Medical Center (UCSFMC) is a 600‐bed tertiary care academic teaching hospital. We surveyed interns, hospitalists on a teaching service, and day‐shift nurses from the inpatient medical service, based on care they provided at UCSFMC from July 2010 to February 2011. The 3 groups are the primary providers at our institution who deliver discharge education. The study was approved by our Institutional Review Board (IRB), the Committee on Human Research.
Survey Development
We developed a survey tool based on a literature review and expert input from local institutional leaders in nursing, residency training, and hospital medicine. The aims of the survey tool were to: 1) assess perceptions and practice of the nurse and physician role in patient discharge education; 2) describe the current practice of physiciannurse communication at discharge; and 3) assess openness to new communication tools.
Specific elements of discharge education assessed in the survey were established from the existing literature,10, 11 and our local best practices (see Supporting Information, Text Box, in the online version of this article). Prior to survey administration, we conducted informal focus groups of interns, hospitalists, and day‐shift nurses, and piloted the survey to assure clarity in the questions and proposed responses.
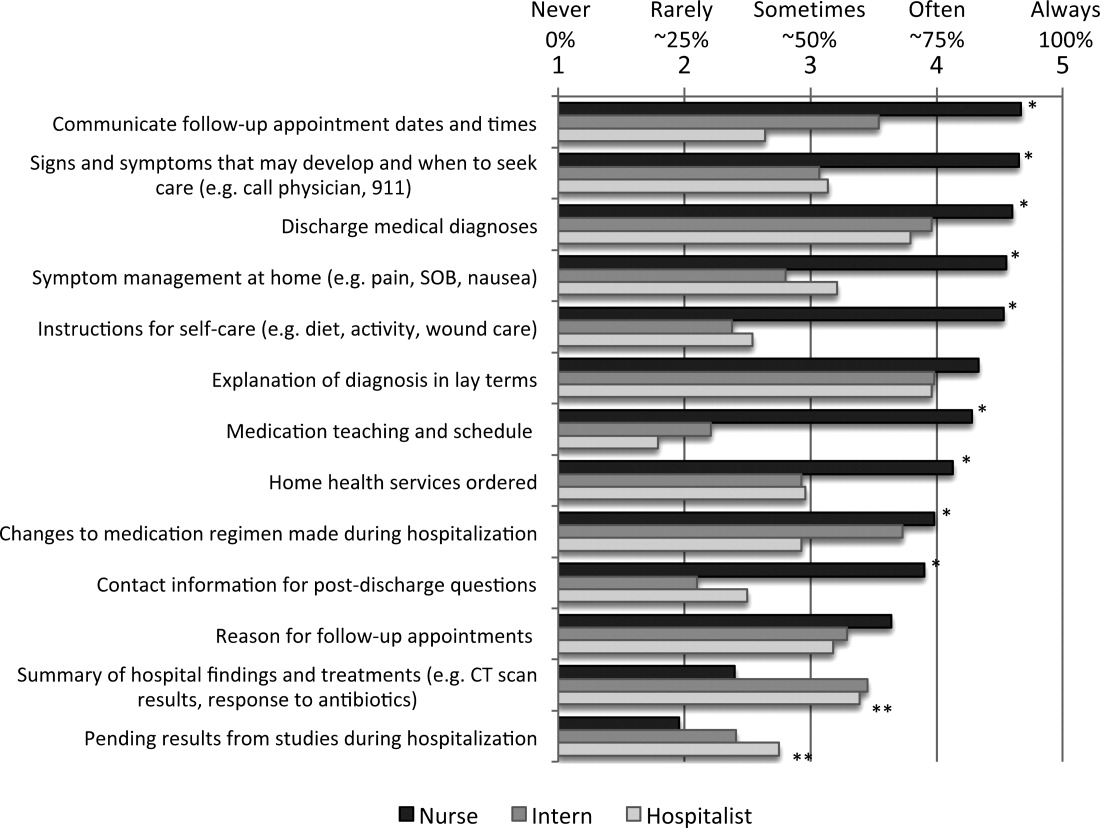
The survey asked respondents to assign responsibility for the discharge education elements to the physician, nurse, both, or neither, and then to describe their current practice in patient education and in physiciannurse communication. The frequency that respondents provide discharge education to patients and the frequency of nursephysician communication around the elements of discharge education were assessed using Likert scales (1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = always). Finally, the survey asked respondents about their interest in tools to improve provider communication at discharge.
Survey Administration
Surveys were administered on paper and electronically, the latter using a commercial online survey tool. Paper surveys were circulated at nurse staff meetings on the 2 units in January and February 2011, with links to an electronic survey sent by e‐mail for those unable to attend. Electronic surveys were distributed via e‐mail to all interns and hospitalists in January 2011. The mid‐year time period was selected to ensure that all interns had provided clinical care at this hospital site. Two reminder e‐mails were sent to non‐respondents.
Data Analysis
Paper‐based surveys were subsequently entered into the online survey tool. Student t tests were used to compare Likert scale means between 2 provider groups, while analysis of variance (ANOVA) was used to compare differences between nurses, interns, and hospitalists. Chi‐squared analysis was used to compare dichotomous variables of agreement and disagreement.
Likert scales of education to patients were dichotomized into frequent education (that provided often or always) versus infrequent education (that provided never, rarely, or sometimes). Likert scales of communication between nurses were similarly dichotomized. Correlation between frequent education to patients (often or always) and the frequency of communication between nurses and physicians (often or always) was assessed using Pearson's r.
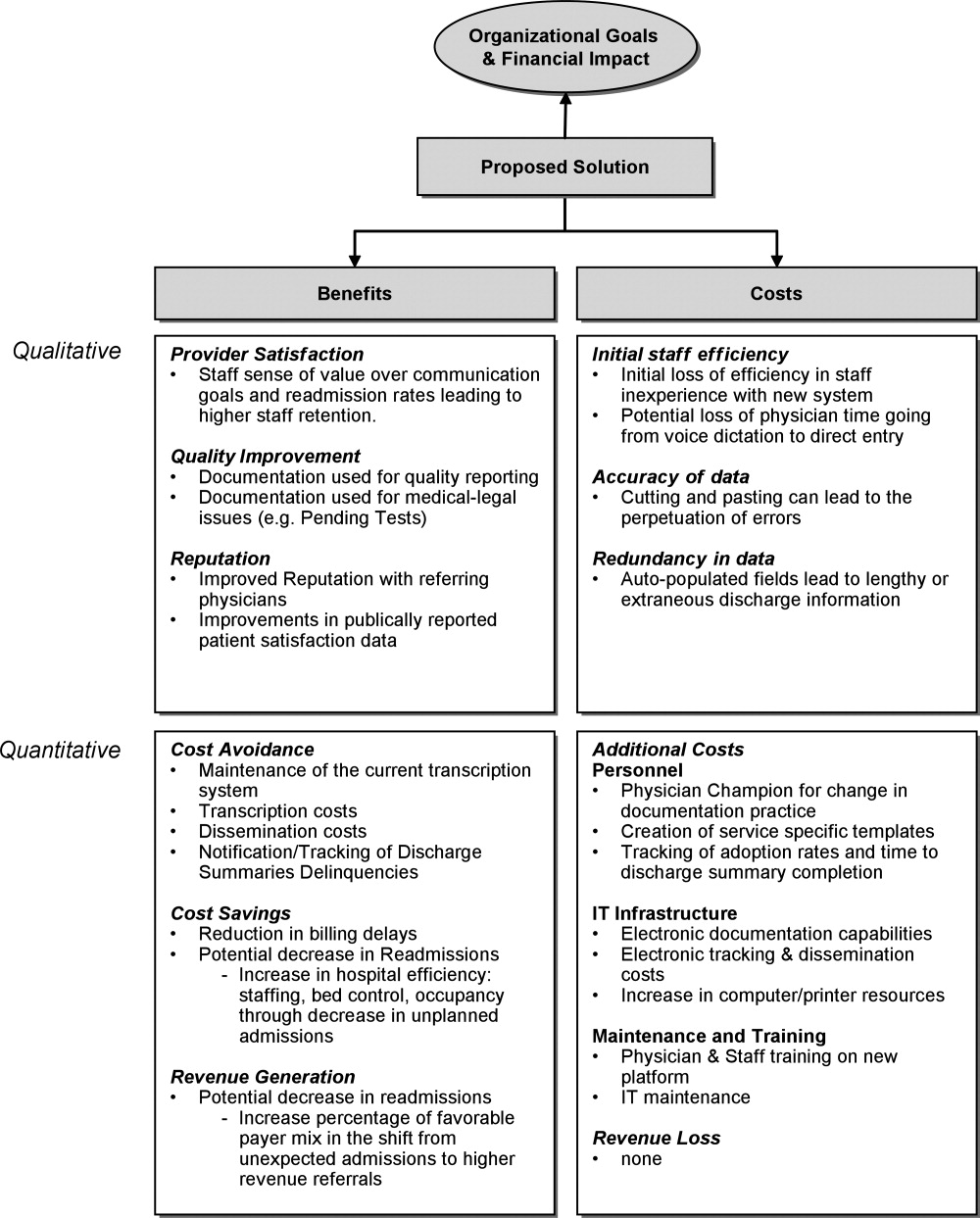
RESULTS
One hundred twenty‐nine providers responded to the survey with an overall survey response rate of 129/184 (70%). Forty‐five (64%) nurses, 56 (71%) interns, and 28 (78%) hospitalists participated. We organized the results into 4 sections based on the survey's question domains. First, we analyzed providers' (defined as nurses, interns, and hospitalists) perceived responsibility for the elements of patient discharge education (see Supporting Information, Text Box, in the online version of this article). Second, we examined how providers' responsibility compared to their reported practice. Third, we looked at the communication between nurses and physicians on the care team around these shared elements of discharge education. Lastly, we looked at providers' willingness to adopt tools to improve nursephysician communication around the time of discharge.
Perceived Responsibility for Discharge Education
Providers felt that most elements of discharge education were a shared responsibility, accounting for 58% of the responses to all the questions. Nurses, however, were the most likely to respond that the elements of discharge education were a shared responsibility, with 64% of all nursing responses indicating that the discharge education elements were a shared responsibility, compared to 54% of intern's responses and 55% of hospitalist's responses (P < 0.005). Correspondingly, nurses also responded least often that items were primarily a nursing responsibility (10% of all responses), compared to interns (12% of all responses) and hospitalists (18% of all responses) (nurses vs hospitalists, P < 0.001). No single elements were responsible for these differences, instead Table 1 demonstrates this trend across most elements. Hospitalists, despite their increased experience in discharging patients, were less likely than interns to respond that elements of discharge education were a physician's responsibility (21% vs 32% of all responses, P < 0.001).
| Nursing Responsibility (%) | Combined (%) | Physician Responsibility (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | |
| |||||||||
| Medication teaching and schedule | 33 | 29 | 33 | 55 | 58 | 52 | 0 | 0 | 0 |
| Contact information for postdischarge questions | 28 | 45 | 33 | 60 | 44 | 59 | 12 | 9 | 4 |
| Instructions for self‐care (eg, diet, activity, wound care) | 23 | 30 | 43 | 77 | 62 | 57 | 0 | 7 | 0 |
| Follow‐up appointment dates and times | 9 | 20 | 46 | 86 | 82 | 50 | 5 | 0 | 0 |
| Signs and symptoms that may develop and when to seek care (eg, call physician, 911) | 18 | 11 | 19 | 82 | 67 | 70 | 0 | 20 | 11 |
| Symptom management at home (eg, pain, SOB, nausea) | 11 | 2 | 21 | 89 | 69 | 75 | 0 | 29 | 4 |
| Home health services ordered | 5 | 9 | 21 | 79 | 65 | 54 | 14 | 22 | 0 |
| Reason for follow‐up appointments | 2 | 4 | 11 | 77 | 67 | 68 | 20 | 29 | 21 |
| Changes to medication regimen made during hospitalization | 2 | 2 | 4 | 66 | 53 | 79 | 30 | 43 | 18 |
| Discharge medical diagnoses | 0 | 0 | 0 | 60 | 56 | 61 | 40 | 45 | 39 |
| Explanation of diagnosis in lay terms | 0 | 0 | 0 | 69 | 45 | 64 | 31 | 55 | 36 |
| Summary of hospital findings and treatments (eg, CT scan results, response to antibiotics) | 0 | 0 | 0 | 18 | 11 | 18 | 82 | 88 | 71 |
| Pending results from studies during hospitalization | 0 | 2 | 0 | 12 | 27 | 29 | 88 | 66 | 68 |
The majority of providers were in agreement that 9 of the 13 elements were a shared nursephysician responsibility, with varying degrees of consensus. All groups also agreed that 2 of the elements, summary of hospital findings and pending results from studies during hospitalization, should be primarily the physician's responsibility. However, there was disagreement on the remaining 2 items. The majority of interns viewed the explanation of the diagnosis in lay terms as a physician responsibility (55%), compared to a minority of nurses (31%) and hospitalists (36%) (P < 0.05). Interns were also more likely than others to view providing contact information for questions after discharge as a uniquely nursing responsibility (45%), compared to nurses (28%) and hospitalists (33%) who viewed this as shared responsibility; this difference was not statistically significant.
Discharge Education by Providers on the Care Team
Despite nurses' reluctance to claim sole responsibility for elements of discharge education, nurses on the whole reported providing discharge education more often than either interns or hospitalists (P < 0.05). Figure 1 illustrates each group's reported practice of communicating specific discharge education on a Likert scale. For the 9 elements viewed as a shared responsibility and the 2 elements where there was disagreement, nurses reported communicating most items significantly more often than both interns and hospitalists (P < 0.001 for all elements except reason for follow‐up appointments, explanation of diagnosis in lay terms, and changes to medication regimen made during hospitalization). Items that were reported to be a physician responsibility were communicated more often by interns and hospitalists than nurses (P < 0.005), but were the items least often communicated by any care provider. Hospitalists did not report communicating any items significantly more than interns.
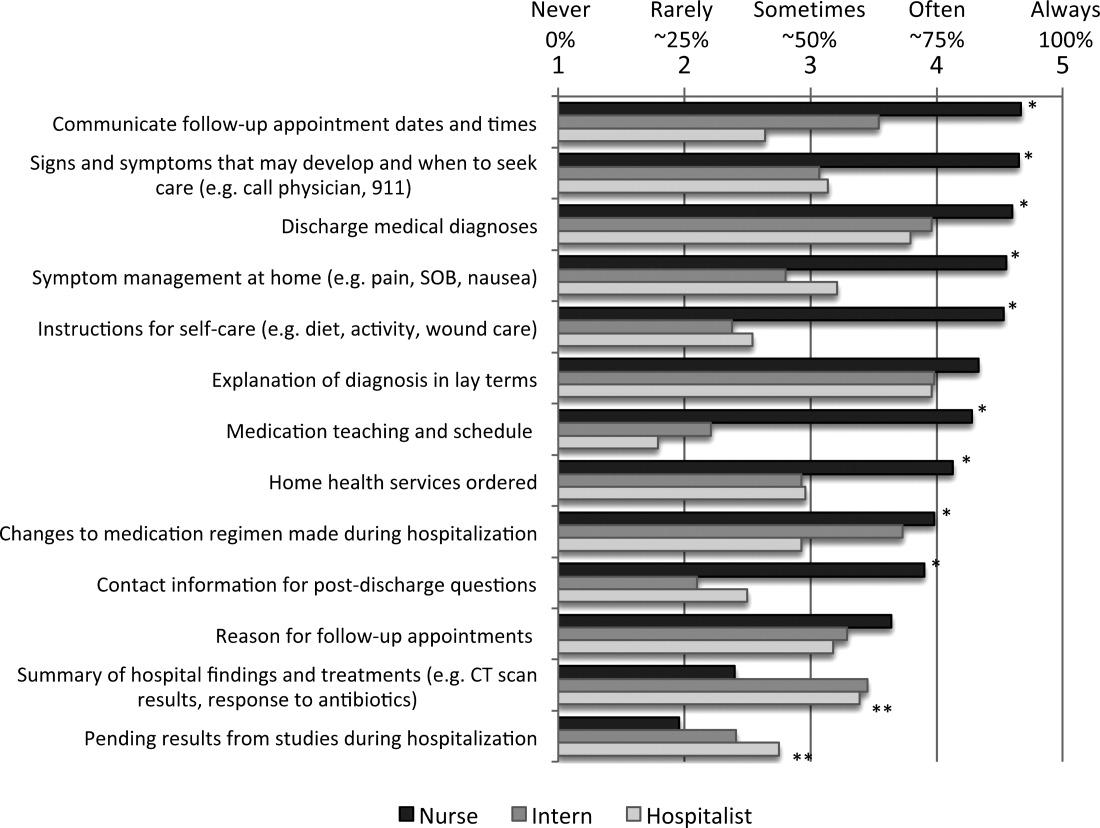
Communication Between Nurses and Physicians
Overall, communication between nurses and physicians was infrequent, with the 64% of nurses, 64% of interns, and 70% of hospitalists reporting that they never or rarely communicate with the other around any discharge education elements. Hospitalists were not more likely than interns to report communicating with nurses on any items, instead reported communicating with nurses around follow‐up appointments and home health services significantly less often (P < 0.05). There was a statistically significant increase in communication by all providers around items of shared responsibility, compared to items viewed as the responsibility of the physicians (14% vs 5.0% increase in communicated often or always; P < 0.001). Elements on which nurses and physicians communicated often or always were also discharge education elements reported as more often provided to patients (r = 0.577).
Potential Solutions for Sharing Discharge Information
Overall, both nurses, interns, and hospitalists were very open to proposed methods of enhancing their communication at discharge. Compared to interns and hospitalists, nurses were more likely to support communication tools, and significantly more in favor of verbal communication, discharge summary availability at the time of discharge, and access to a physician handoff tool. Only 1 solution, a standardized checklist, was favored more by interns and hospitalists, but the difference was not statistically significant. Verbal communication with the other group on the day of discharge was supported most strongly, with 100% of nurses, and 81% of interns and hospitalists reporting being likely or very likely to use this strategy. The least supported item by all groups was using white boards to communicate discharge information (Table 2).
| Likelihood of Using the Proposed Strategies | ||||
|---|---|---|---|---|
| Nurse | Intern | Hospitalist | P (ANOVA) | |
| ||||
| Verbal communication between providers on day of discharge | 4.8 | 4.2 | 4.1 | <0.001 |
| Discharge summary available at time of discharge | 4.7 | 3.8 | 4.4 | <0.001 |
| Discharge information in physician sign‐out tool | 4.3 | 3.8 | 3.2 | <0.001 |
| Nurse participation in daily physician rounds on the floor | 4.2 | 4.1 | 4.6 | 0.057 |
| Standardized checklist for discharges | 3.6 | 4.0 | 4.2 | 0.122 |
| Discharge information on white boards | 3.4 | 3.0 | 3.3 | 0.259 |
DISCUSSION
Our study demonstrated that nurses, interns, and hospitalists all feel that they play a pivotal role in discharge education. Compared to both interns and hospitalists, nurses were more likely to view discharge education as a shared responsibility, but nurses also reported providing more discharge education to patients. The elements of discharge education deemed a physician responsibility were reported as the least often provided to patients. Despite the majority of responses indicating that discharge education is a shared nursephysician responsibility, reported provider communication about discharge education was infrequent. Arguing for more communication, elements for which nurses and physicians perceived communicating more frequently were also more often reportedly conveyed to patients. The summative findings suggest that inconsistent discharge education and communication between providers may be leading to patients who are not regularly receiving complete discharge information. Nurses, interns, and hospitalists, however, were all very engaged in potential solutions to improve discharge communication, providing opportunities for immediate impact.
The question becomes where to start. Poor discharge instructions are associated with increased hospital readmission,10 and comprehensive discharge education is a suggested strategy to reduce preventable readmissions.12 Academic hospitalists, despite likely having witnessed the negative impact of poor discharge education, were not more likely than interns to report educating patients, nor did they report communicating more often with nurses. In teaching institutions, specifically, discharge education is being provided by multiple physicians: interns, residents, and hospitalists who may not have clearly defined roles in providing discharge education.13 Thus, providing comprehensive discharge instructions may require a hardwired system to ensure all elements of discharge education are addressed.
Further, our increasing dependence on technology may paradoxically necessitate more formal structures for in‐person communication, as the ability to enter discharge orders remotely leads to less frequent direct communication. Fortunately, as institutions move to computerized systems for discharge orders and instructions, there are increasing opportunities for a standardized approach to the elements of discharge education. While these results may suggest that one individual should be solely responsible for discharge education, trials using teams of nurse practitioners to facilitate transitions of care found no difference in patient length of stay or 30‐day readmission rates.14, 15
Formal systems that increase communication in high‐risk circumstances remain a focus in patient safety, and have been implemented successfully in procedural settings and with handoffs in patient care.1618 A prominent example is operating room time‐outs, which implemented a structured tool and shared process to increase nursephysician communication and reduce mortality.19 Since elements of discharge education with more frequent communication between nurses and physicians were more often conveyed to patients, our results suggest that a discharge time‐out might offer similar benefit. Fortunately, nurses and physicians rated verbal communication as the most desirable solution to share discharge education information. While not formally evaluated, one solution may be adoption of the previously described critical conversation, a structured format and a consistent time for communication that ensures both nurses and physicians understand what education needs to be provided to patients and by whom.20 The 13 discharge elements outlined in our study now provide a starting point for defining specific discussion points at discharge, delineation of who should communicate each element, and the basis for developing an operational discharge time‐out.
There are several limitations to our study. First, the survey instrument was not previously used or validated. However, we did seek formal and structured input while developing our survey, and conducted pilot testing to ensure clarity and comprehension with representatives of all study groups. Second, the 13 discharge education elements we included do not represent a comprehensive list, and were chosen based on our literature review and best practices at our institution. Third, our cross‐sectional study only captures perceptions and practices during a single time point, and may not adequately capture the greater continuum of true practice. Finally, our results may not be generalizable outside UCSFMC or other academic medical centers, particularly if other institutions have employed specific structures for discharge, such as a dedicated discharge coordinator.
CONCLUSION
Discharging patients is a complex process and one in which multiple providers and poor systems contribute to the redesign challenges. Providing high‐quality discharge education instructions to patients is an important step in making a complex process safer. Poor communication between nurses and physicians, complicated by ambiguous perceptions of responsibility for specific information, offers an opportunity for improvement efforts. We should not let well thought out treatment plans fail due to poor patient education on discharge. Our findings argue for a more systematic approach to the discharge education provided by nurses, interns, and hospitalists.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138(3):161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.Can Med Assoc J.2004;170(3):345–349.
- ,.Patients' understanding of their treatment plans and diagnosis at discharge.Mayo Clin Proc.2005;80(8):991–994.
- ,,.Functional health literacy and understanding of medications at discharge.Mayo Clin Proc.2008;83(5):554–558.
- ,,,.Patients' perception of hospital care in the United States.N Engl J Med.2008;359(18):1921–1931.
- ,,, et al.Comprehensive discharge planning and home follow‐up of hospitalized elders: a randomized clinical trial.JAMA.1999;281(7):613–620.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,, et al.Closing the loop: physician communication with diabetic patients who have low health literacy.Arch Intern Med.2003;163(1):83–90.
- ,,, et al.Structured interdisciplinary rounds in a medical teaching unit: improving patient safety.Arch Intern Med.2011;171(7):678–684.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1(6):354–360.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,,.Redefining readmission risk factors for general medicine patients.J Hosp Med.2011;6(2):54–60.
- ,,,,.“Out of sight, out of mind”: housestaff perceptions of quality‐limiting factors in discharge care at teaching hospitals.J Hosp Med.2012;7:376–381.
- ,,,,.To the hospital and back home again: a nurse practitioner‐based transitional care program for hospitalized homebound people.J Am Geriatr Soc.2011;59(3):544–551.
- ,,, et al.Improving the discharge process by embedding a discharge facilitator in a resident team.J Hosp Med.2011;6(9):494–500.
- ,,,,,.The potential for improved teamwork to reduce medical errors in the emergency department. The MedTeams Research Consortium.Ann Emerg Med.1999;34(3):373–383.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- ,,,,.Risk‐adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions.J Am Coll Surg.2007;205(6):778–784.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- ,,,,,.Critical conversations: a call for a nonprocedural “time out.”J Hosp Med.2011;6(4):225–230.
Discharge from the hospital is a vulnerable time for patients. Nearly 1 in 5 patients experiences an adverse event during this transition, with a third of these being likely preventable.1, 2 Comprehensive discharge instructions are necessary to ensure a smooth transition from hospital to home, as the responsibility for care shifts from providers to the patient and caregivers. Unfortunately, patients often go home without understanding critical information about their hospital stay, such as their discharge diagnosis or medication changes,3, 4 leaving them both dissatisfied with their discharge instructions5 and at risk for hospital readmission.
Efforts to improve discharge education have focused on increasing communication between care provider and patient. The use of designated discharge coordinators,6, 7 implementation of teach‐back techniques to assess and confirm understanding,8 and adoption of patient‐centered educational materials all offer tools to improve communication with patients. However, guidelines for communication between providers and their shared role in patient discharge education, particularly between nurses and physicians, are scarce. Daily interdisciplinary rounds9 and shared electronic health records are potential ways to foster such communication, but the methods and frequency with which providers communicate about discharge instructions with each other is poorly understood. Furthermore, despite a common set of goals for discharge instructions,10, 11 it is unclear where the responsibility to provide these elements lies: with nurses, physicians, neither, or both.
Understanding perceptions and communication practices of providers in their delivery of discharge instructions is an important first step in defining responsibilities and improving accountability for discharge education. In this study, we surveyed nurses and physicians about their discharge education practices to better understand how each group sees their own role in discharge teaching, and how these findings may generate recommendations to improve future practices.
METHODS
Setting and Subjects
University of California, San Francisco Medical Center (UCSFMC) is a 600‐bed tertiary care academic teaching hospital. We surveyed interns, hospitalists on a teaching service, and day‐shift nurses from the inpatient medical service, based on care they provided at UCSFMC from July 2010 to February 2011. The 3 groups are the primary providers at our institution who deliver discharge education. The study was approved by our Institutional Review Board (IRB), the Committee on Human Research.
Survey Development
We developed a survey tool based on a literature review and expert input from local institutional leaders in nursing, residency training, and hospital medicine. The aims of the survey tool were to: 1) assess perceptions and practice of the nurse and physician role in patient discharge education; 2) describe the current practice of physiciannurse communication at discharge; and 3) assess openness to new communication tools.
Specific elements of discharge education assessed in the survey were established from the existing literature,10, 11 and our local best practices (see Supporting Information, Text Box, in the online version of this article). Prior to survey administration, we conducted informal focus groups of interns, hospitalists, and day‐shift nurses, and piloted the survey to assure clarity in the questions and proposed responses.
The survey asked respondents to assign responsibility for the discharge education elements to the physician, nurse, both, or neither, and then to describe their current practice in patient education and in physiciannurse communication. The frequency that respondents provide discharge education to patients and the frequency of nursephysician communication around the elements of discharge education were assessed using Likert scales (1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = always). Finally, the survey asked respondents about their interest in tools to improve provider communication at discharge.
Survey Administration
Surveys were administered on paper and electronically, the latter using a commercial online survey tool. Paper surveys were circulated at nurse staff meetings on the 2 units in January and February 2011, with links to an electronic survey sent by e‐mail for those unable to attend. Electronic surveys were distributed via e‐mail to all interns and hospitalists in January 2011. The mid‐year time period was selected to ensure that all interns had provided clinical care at this hospital site. Two reminder e‐mails were sent to non‐respondents.
Data Analysis
Paper‐based surveys were subsequently entered into the online survey tool. Student t tests were used to compare Likert scale means between 2 provider groups, while analysis of variance (ANOVA) was used to compare differences between nurses, interns, and hospitalists. Chi‐squared analysis was used to compare dichotomous variables of agreement and disagreement.
Likert scales of education to patients were dichotomized into frequent education (that provided often or always) versus infrequent education (that provided never, rarely, or sometimes). Likert scales of communication between nurses were similarly dichotomized. Correlation between frequent education to patients (often or always) and the frequency of communication between nurses and physicians (often or always) was assessed using Pearson's r.
RESULTS
One hundred twenty‐nine providers responded to the survey with an overall survey response rate of 129/184 (70%). Forty‐five (64%) nurses, 56 (71%) interns, and 28 (78%) hospitalists participated. We organized the results into 4 sections based on the survey's question domains. First, we analyzed providers' (defined as nurses, interns, and hospitalists) perceived responsibility for the elements of patient discharge education (see Supporting Information, Text Box, in the online version of this article). Second, we examined how providers' responsibility compared to their reported practice. Third, we looked at the communication between nurses and physicians on the care team around these shared elements of discharge education. Lastly, we looked at providers' willingness to adopt tools to improve nursephysician communication around the time of discharge.
Perceived Responsibility for Discharge Education
Providers felt that most elements of discharge education were a shared responsibility, accounting for 58% of the responses to all the questions. Nurses, however, were the most likely to respond that the elements of discharge education were a shared responsibility, with 64% of all nursing responses indicating that the discharge education elements were a shared responsibility, compared to 54% of intern's responses and 55% of hospitalist's responses (P < 0.005). Correspondingly, nurses also responded least often that items were primarily a nursing responsibility (10% of all responses), compared to interns (12% of all responses) and hospitalists (18% of all responses) (nurses vs hospitalists, P < 0.001). No single elements were responsible for these differences, instead Table 1 demonstrates this trend across most elements. Hospitalists, despite their increased experience in discharging patients, were less likely than interns to respond that elements of discharge education were a physician's responsibility (21% vs 32% of all responses, P < 0.001).
| Nursing Responsibility (%) | Combined (%) | Physician Responsibility (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | |
| |||||||||
| Medication teaching and schedule | 33 | 29 | 33 | 55 | 58 | 52 | 0 | 0 | 0 |
| Contact information for postdischarge questions | 28 | 45 | 33 | 60 | 44 | 59 | 12 | 9 | 4 |
| Instructions for self‐care (eg, diet, activity, wound care) | 23 | 30 | 43 | 77 | 62 | 57 | 0 | 7 | 0 |
| Follow‐up appointment dates and times | 9 | 20 | 46 | 86 | 82 | 50 | 5 | 0 | 0 |
| Signs and symptoms that may develop and when to seek care (eg, call physician, 911) | 18 | 11 | 19 | 82 | 67 | 70 | 0 | 20 | 11 |
| Symptom management at home (eg, pain, SOB, nausea) | 11 | 2 | 21 | 89 | 69 | 75 | 0 | 29 | 4 |
| Home health services ordered | 5 | 9 | 21 | 79 | 65 | 54 | 14 | 22 | 0 |
| Reason for follow‐up appointments | 2 | 4 | 11 | 77 | 67 | 68 | 20 | 29 | 21 |
| Changes to medication regimen made during hospitalization | 2 | 2 | 4 | 66 | 53 | 79 | 30 | 43 | 18 |
| Discharge medical diagnoses | 0 | 0 | 0 | 60 | 56 | 61 | 40 | 45 | 39 |
| Explanation of diagnosis in lay terms | 0 | 0 | 0 | 69 | 45 | 64 | 31 | 55 | 36 |
| Summary of hospital findings and treatments (eg, CT scan results, response to antibiotics) | 0 | 0 | 0 | 18 | 11 | 18 | 82 | 88 | 71 |
| Pending results from studies during hospitalization | 0 | 2 | 0 | 12 | 27 | 29 | 88 | 66 | 68 |
The majority of providers were in agreement that 9 of the 13 elements were a shared nursephysician responsibility, with varying degrees of consensus. All groups also agreed that 2 of the elements, summary of hospital findings and pending results from studies during hospitalization, should be primarily the physician's responsibility. However, there was disagreement on the remaining 2 items. The majority of interns viewed the explanation of the diagnosis in lay terms as a physician responsibility (55%), compared to a minority of nurses (31%) and hospitalists (36%) (P < 0.05). Interns were also more likely than others to view providing contact information for questions after discharge as a uniquely nursing responsibility (45%), compared to nurses (28%) and hospitalists (33%) who viewed this as shared responsibility; this difference was not statistically significant.
Discharge Education by Providers on the Care Team
Despite nurses' reluctance to claim sole responsibility for elements of discharge education, nurses on the whole reported providing discharge education more often than either interns or hospitalists (P < 0.05). Figure 1 illustrates each group's reported practice of communicating specific discharge education on a Likert scale. For the 9 elements viewed as a shared responsibility and the 2 elements where there was disagreement, nurses reported communicating most items significantly more often than both interns and hospitalists (P < 0.001 for all elements except reason for follow‐up appointments, explanation of diagnosis in lay terms, and changes to medication regimen made during hospitalization). Items that were reported to be a physician responsibility were communicated more often by interns and hospitalists than nurses (P < 0.005), but were the items least often communicated by any care provider. Hospitalists did not report communicating any items significantly more than interns.
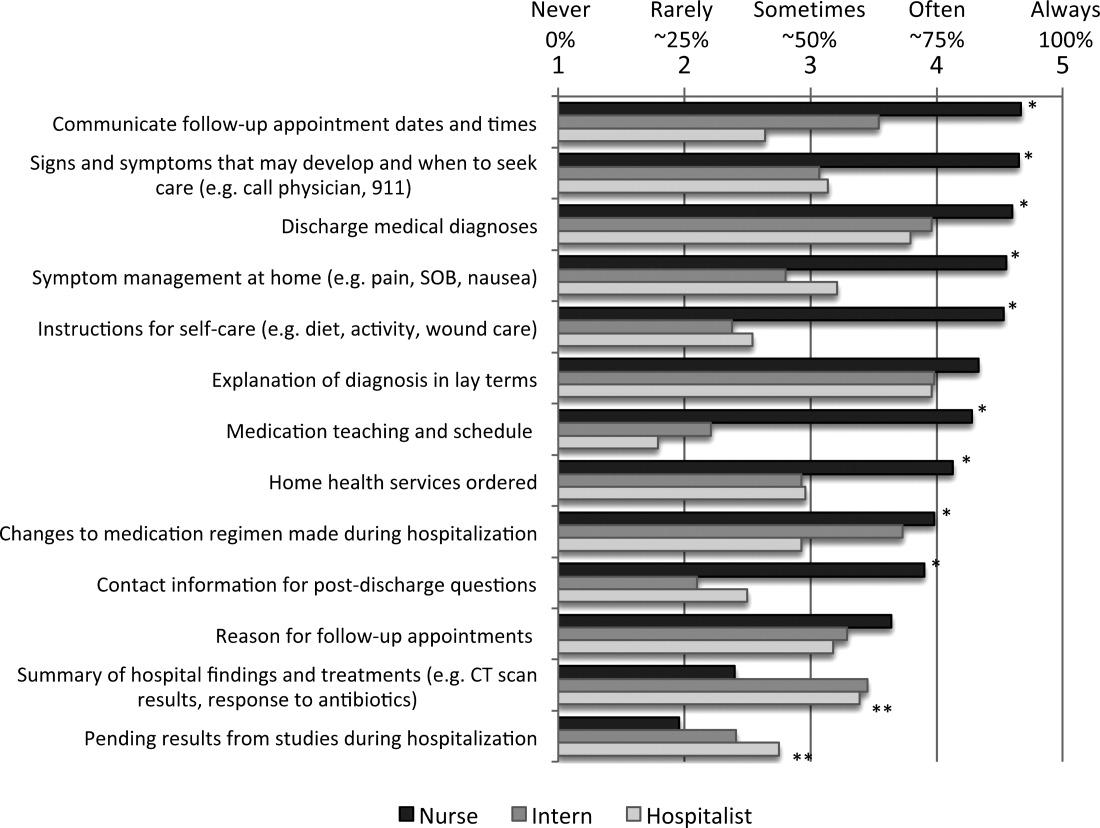
Communication Between Nurses and Physicians
Overall, communication between nurses and physicians was infrequent, with the 64% of nurses, 64% of interns, and 70% of hospitalists reporting that they never or rarely communicate with the other around any discharge education elements. Hospitalists were not more likely than interns to report communicating with nurses on any items, instead reported communicating with nurses around follow‐up appointments and home health services significantly less often (P < 0.05). There was a statistically significant increase in communication by all providers around items of shared responsibility, compared to items viewed as the responsibility of the physicians (14% vs 5.0% increase in communicated often or always; P < 0.001). Elements on which nurses and physicians communicated often or always were also discharge education elements reported as more often provided to patients (r = 0.577).
Potential Solutions for Sharing Discharge Information
Overall, both nurses, interns, and hospitalists were very open to proposed methods of enhancing their communication at discharge. Compared to interns and hospitalists, nurses were more likely to support communication tools, and significantly more in favor of verbal communication, discharge summary availability at the time of discharge, and access to a physician handoff tool. Only 1 solution, a standardized checklist, was favored more by interns and hospitalists, but the difference was not statistically significant. Verbal communication with the other group on the day of discharge was supported most strongly, with 100% of nurses, and 81% of interns and hospitalists reporting being likely or very likely to use this strategy. The least supported item by all groups was using white boards to communicate discharge information (Table 2).
| Likelihood of Using the Proposed Strategies | ||||
|---|---|---|---|---|
| Nurse | Intern | Hospitalist | P (ANOVA) | |
| ||||
| Verbal communication between providers on day of discharge | 4.8 | 4.2 | 4.1 | <0.001 |
| Discharge summary available at time of discharge | 4.7 | 3.8 | 4.4 | <0.001 |
| Discharge information in physician sign‐out tool | 4.3 | 3.8 | 3.2 | <0.001 |
| Nurse participation in daily physician rounds on the floor | 4.2 | 4.1 | 4.6 | 0.057 |
| Standardized checklist for discharges | 3.6 | 4.0 | 4.2 | 0.122 |
| Discharge information on white boards | 3.4 | 3.0 | 3.3 | 0.259 |
DISCUSSION
Our study demonstrated that nurses, interns, and hospitalists all feel that they play a pivotal role in discharge education. Compared to both interns and hospitalists, nurses were more likely to view discharge education as a shared responsibility, but nurses also reported providing more discharge education to patients. The elements of discharge education deemed a physician responsibility were reported as the least often provided to patients. Despite the majority of responses indicating that discharge education is a shared nursephysician responsibility, reported provider communication about discharge education was infrequent. Arguing for more communication, elements for which nurses and physicians perceived communicating more frequently were also more often reportedly conveyed to patients. The summative findings suggest that inconsistent discharge education and communication between providers may be leading to patients who are not regularly receiving complete discharge information. Nurses, interns, and hospitalists, however, were all very engaged in potential solutions to improve discharge communication, providing opportunities for immediate impact.
The question becomes where to start. Poor discharge instructions are associated with increased hospital readmission,10 and comprehensive discharge education is a suggested strategy to reduce preventable readmissions.12 Academic hospitalists, despite likely having witnessed the negative impact of poor discharge education, were not more likely than interns to report educating patients, nor did they report communicating more often with nurses. In teaching institutions, specifically, discharge education is being provided by multiple physicians: interns, residents, and hospitalists who may not have clearly defined roles in providing discharge education.13 Thus, providing comprehensive discharge instructions may require a hardwired system to ensure all elements of discharge education are addressed.
Further, our increasing dependence on technology may paradoxically necessitate more formal structures for in‐person communication, as the ability to enter discharge orders remotely leads to less frequent direct communication. Fortunately, as institutions move to computerized systems for discharge orders and instructions, there are increasing opportunities for a standardized approach to the elements of discharge education. While these results may suggest that one individual should be solely responsible for discharge education, trials using teams of nurse practitioners to facilitate transitions of care found no difference in patient length of stay or 30‐day readmission rates.14, 15
Formal systems that increase communication in high‐risk circumstances remain a focus in patient safety, and have been implemented successfully in procedural settings and with handoffs in patient care.1618 A prominent example is operating room time‐outs, which implemented a structured tool and shared process to increase nursephysician communication and reduce mortality.19 Since elements of discharge education with more frequent communication between nurses and physicians were more often conveyed to patients, our results suggest that a discharge time‐out might offer similar benefit. Fortunately, nurses and physicians rated verbal communication as the most desirable solution to share discharge education information. While not formally evaluated, one solution may be adoption of the previously described critical conversation, a structured format and a consistent time for communication that ensures both nurses and physicians understand what education needs to be provided to patients and by whom.20 The 13 discharge elements outlined in our study now provide a starting point for defining specific discussion points at discharge, delineation of who should communicate each element, and the basis for developing an operational discharge time‐out.
There are several limitations to our study. First, the survey instrument was not previously used or validated. However, we did seek formal and structured input while developing our survey, and conducted pilot testing to ensure clarity and comprehension with representatives of all study groups. Second, the 13 discharge education elements we included do not represent a comprehensive list, and were chosen based on our literature review and best practices at our institution. Third, our cross‐sectional study only captures perceptions and practices during a single time point, and may not adequately capture the greater continuum of true practice. Finally, our results may not be generalizable outside UCSFMC or other academic medical centers, particularly if other institutions have employed specific structures for discharge, such as a dedicated discharge coordinator.
CONCLUSION
Discharging patients is a complex process and one in which multiple providers and poor systems contribute to the redesign challenges. Providing high‐quality discharge education instructions to patients is an important step in making a complex process safer. Poor communication between nurses and physicians, complicated by ambiguous perceptions of responsibility for specific information, offers an opportunity for improvement efforts. We should not let well thought out treatment plans fail due to poor patient education on discharge. Our findings argue for a more systematic approach to the discharge education provided by nurses, interns, and hospitalists.
Discharge from the hospital is a vulnerable time for patients. Nearly 1 in 5 patients experiences an adverse event during this transition, with a third of these being likely preventable.1, 2 Comprehensive discharge instructions are necessary to ensure a smooth transition from hospital to home, as the responsibility for care shifts from providers to the patient and caregivers. Unfortunately, patients often go home without understanding critical information about their hospital stay, such as their discharge diagnosis or medication changes,3, 4 leaving them both dissatisfied with their discharge instructions5 and at risk for hospital readmission.
Efforts to improve discharge education have focused on increasing communication between care provider and patient. The use of designated discharge coordinators,6, 7 implementation of teach‐back techniques to assess and confirm understanding,8 and adoption of patient‐centered educational materials all offer tools to improve communication with patients. However, guidelines for communication between providers and their shared role in patient discharge education, particularly between nurses and physicians, are scarce. Daily interdisciplinary rounds9 and shared electronic health records are potential ways to foster such communication, but the methods and frequency with which providers communicate about discharge instructions with each other is poorly understood. Furthermore, despite a common set of goals for discharge instructions,10, 11 it is unclear where the responsibility to provide these elements lies: with nurses, physicians, neither, or both.
Understanding perceptions and communication practices of providers in their delivery of discharge instructions is an important first step in defining responsibilities and improving accountability for discharge education. In this study, we surveyed nurses and physicians about their discharge education practices to better understand how each group sees their own role in discharge teaching, and how these findings may generate recommendations to improve future practices.
METHODS
Setting and Subjects
University of California, San Francisco Medical Center (UCSFMC) is a 600‐bed tertiary care academic teaching hospital. We surveyed interns, hospitalists on a teaching service, and day‐shift nurses from the inpatient medical service, based on care they provided at UCSFMC from July 2010 to February 2011. The 3 groups are the primary providers at our institution who deliver discharge education. The study was approved by our Institutional Review Board (IRB), the Committee on Human Research.
Survey Development
We developed a survey tool based on a literature review and expert input from local institutional leaders in nursing, residency training, and hospital medicine. The aims of the survey tool were to: 1) assess perceptions and practice of the nurse and physician role in patient discharge education; 2) describe the current practice of physiciannurse communication at discharge; and 3) assess openness to new communication tools.
Specific elements of discharge education assessed in the survey were established from the existing literature,10, 11 and our local best practices (see Supporting Information, Text Box, in the online version of this article). Prior to survey administration, we conducted informal focus groups of interns, hospitalists, and day‐shift nurses, and piloted the survey to assure clarity in the questions and proposed responses.
The survey asked respondents to assign responsibility for the discharge education elements to the physician, nurse, both, or neither, and then to describe their current practice in patient education and in physiciannurse communication. The frequency that respondents provide discharge education to patients and the frequency of nursephysician communication around the elements of discharge education were assessed using Likert scales (1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = always). Finally, the survey asked respondents about their interest in tools to improve provider communication at discharge.
Survey Administration
Surveys were administered on paper and electronically, the latter using a commercial online survey tool. Paper surveys were circulated at nurse staff meetings on the 2 units in January and February 2011, with links to an electronic survey sent by e‐mail for those unable to attend. Electronic surveys were distributed via e‐mail to all interns and hospitalists in January 2011. The mid‐year time period was selected to ensure that all interns had provided clinical care at this hospital site. Two reminder e‐mails were sent to non‐respondents.
Data Analysis
Paper‐based surveys were subsequently entered into the online survey tool. Student t tests were used to compare Likert scale means between 2 provider groups, while analysis of variance (ANOVA) was used to compare differences between nurses, interns, and hospitalists. Chi‐squared analysis was used to compare dichotomous variables of agreement and disagreement.
Likert scales of education to patients were dichotomized into frequent education (that provided often or always) versus infrequent education (that provided never, rarely, or sometimes). Likert scales of communication between nurses were similarly dichotomized. Correlation between frequent education to patients (often or always) and the frequency of communication between nurses and physicians (often or always) was assessed using Pearson's r.
RESULTS
One hundred twenty‐nine providers responded to the survey with an overall survey response rate of 129/184 (70%). Forty‐five (64%) nurses, 56 (71%) interns, and 28 (78%) hospitalists participated. We organized the results into 4 sections based on the survey's question domains. First, we analyzed providers' (defined as nurses, interns, and hospitalists) perceived responsibility for the elements of patient discharge education (see Supporting Information, Text Box, in the online version of this article). Second, we examined how providers' responsibility compared to their reported practice. Third, we looked at the communication between nurses and physicians on the care team around these shared elements of discharge education. Lastly, we looked at providers' willingness to adopt tools to improve nursephysician communication around the time of discharge.
Perceived Responsibility for Discharge Education
Providers felt that most elements of discharge education were a shared responsibility, accounting for 58% of the responses to all the questions. Nurses, however, were the most likely to respond that the elements of discharge education were a shared responsibility, with 64% of all nursing responses indicating that the discharge education elements were a shared responsibility, compared to 54% of intern's responses and 55% of hospitalist's responses (P < 0.005). Correspondingly, nurses also responded least often that items were primarily a nursing responsibility (10% of all responses), compared to interns (12% of all responses) and hospitalists (18% of all responses) (nurses vs hospitalists, P < 0.001). No single elements were responsible for these differences, instead Table 1 demonstrates this trend across most elements. Hospitalists, despite their increased experience in discharging patients, were less likely than interns to respond that elements of discharge education were a physician's responsibility (21% vs 32% of all responses, P < 0.001).
| Nursing Responsibility (%) | Combined (%) | Physician Responsibility (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | Nurse N = 45 | Intern N = 56 | Hospitalist N = 28 | |
| |||||||||
| Medication teaching and schedule | 33 | 29 | 33 | 55 | 58 | 52 | 0 | 0 | 0 |
| Contact information for postdischarge questions | 28 | 45 | 33 | 60 | 44 | 59 | 12 | 9 | 4 |
| Instructions for self‐care (eg, diet, activity, wound care) | 23 | 30 | 43 | 77 | 62 | 57 | 0 | 7 | 0 |
| Follow‐up appointment dates and times | 9 | 20 | 46 | 86 | 82 | 50 | 5 | 0 | 0 |
| Signs and symptoms that may develop and when to seek care (eg, call physician, 911) | 18 | 11 | 19 | 82 | 67 | 70 | 0 | 20 | 11 |
| Symptom management at home (eg, pain, SOB, nausea) | 11 | 2 | 21 | 89 | 69 | 75 | 0 | 29 | 4 |
| Home health services ordered | 5 | 9 | 21 | 79 | 65 | 54 | 14 | 22 | 0 |
| Reason for follow‐up appointments | 2 | 4 | 11 | 77 | 67 | 68 | 20 | 29 | 21 |
| Changes to medication regimen made during hospitalization | 2 | 2 | 4 | 66 | 53 | 79 | 30 | 43 | 18 |
| Discharge medical diagnoses | 0 | 0 | 0 | 60 | 56 | 61 | 40 | 45 | 39 |
| Explanation of diagnosis in lay terms | 0 | 0 | 0 | 69 | 45 | 64 | 31 | 55 | 36 |
| Summary of hospital findings and treatments (eg, CT scan results, response to antibiotics) | 0 | 0 | 0 | 18 | 11 | 18 | 82 | 88 | 71 |
| Pending results from studies during hospitalization | 0 | 2 | 0 | 12 | 27 | 29 | 88 | 66 | 68 |
The majority of providers were in agreement that 9 of the 13 elements were a shared nursephysician responsibility, with varying degrees of consensus. All groups also agreed that 2 of the elements, summary of hospital findings and pending results from studies during hospitalization, should be primarily the physician's responsibility. However, there was disagreement on the remaining 2 items. The majority of interns viewed the explanation of the diagnosis in lay terms as a physician responsibility (55%), compared to a minority of nurses (31%) and hospitalists (36%) (P < 0.05). Interns were also more likely than others to view providing contact information for questions after discharge as a uniquely nursing responsibility (45%), compared to nurses (28%) and hospitalists (33%) who viewed this as shared responsibility; this difference was not statistically significant.
Discharge Education by Providers on the Care Team
Despite nurses' reluctance to claim sole responsibility for elements of discharge education, nurses on the whole reported providing discharge education more often than either interns or hospitalists (P < 0.05). Figure 1 illustrates each group's reported practice of communicating specific discharge education on a Likert scale. For the 9 elements viewed as a shared responsibility and the 2 elements where there was disagreement, nurses reported communicating most items significantly more often than both interns and hospitalists (P < 0.001 for all elements except reason for follow‐up appointments, explanation of diagnosis in lay terms, and changes to medication regimen made during hospitalization). Items that were reported to be a physician responsibility were communicated more often by interns and hospitalists than nurses (P < 0.005), but were the items least often communicated by any care provider. Hospitalists did not report communicating any items significantly more than interns.
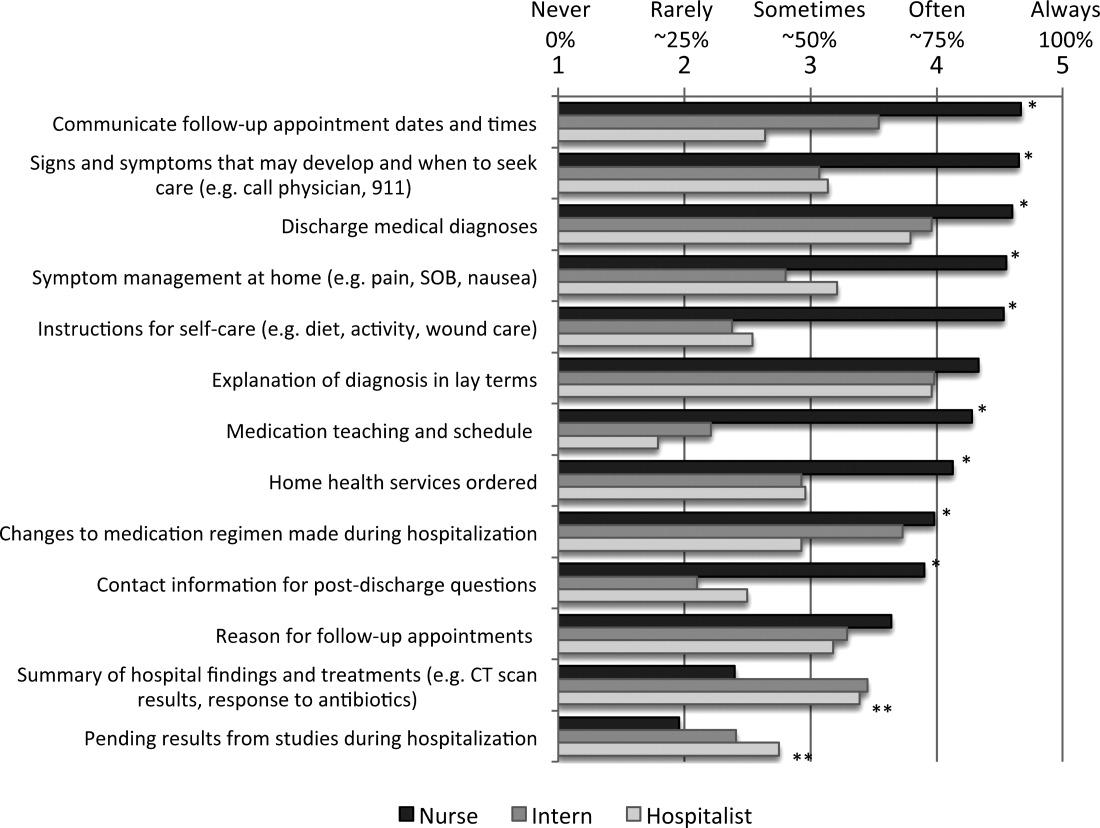
Communication Between Nurses and Physicians
Overall, communication between nurses and physicians was infrequent, with the 64% of nurses, 64% of interns, and 70% of hospitalists reporting that they never or rarely communicate with the other around any discharge education elements. Hospitalists were not more likely than interns to report communicating with nurses on any items, instead reported communicating with nurses around follow‐up appointments and home health services significantly less often (P < 0.05). There was a statistically significant increase in communication by all providers around items of shared responsibility, compared to items viewed as the responsibility of the physicians (14% vs 5.0% increase in communicated often or always; P < 0.001). Elements on which nurses and physicians communicated often or always were also discharge education elements reported as more often provided to patients (r = 0.577).
Potential Solutions for Sharing Discharge Information
Overall, both nurses, interns, and hospitalists were very open to proposed methods of enhancing their communication at discharge. Compared to interns and hospitalists, nurses were more likely to support communication tools, and significantly more in favor of verbal communication, discharge summary availability at the time of discharge, and access to a physician handoff tool. Only 1 solution, a standardized checklist, was favored more by interns and hospitalists, but the difference was not statistically significant. Verbal communication with the other group on the day of discharge was supported most strongly, with 100% of nurses, and 81% of interns and hospitalists reporting being likely or very likely to use this strategy. The least supported item by all groups was using white boards to communicate discharge information (Table 2).
| Likelihood of Using the Proposed Strategies | ||||
|---|---|---|---|---|
| Nurse | Intern | Hospitalist | P (ANOVA) | |
| ||||
| Verbal communication between providers on day of discharge | 4.8 | 4.2 | 4.1 | <0.001 |
| Discharge summary available at time of discharge | 4.7 | 3.8 | 4.4 | <0.001 |
| Discharge information in physician sign‐out tool | 4.3 | 3.8 | 3.2 | <0.001 |
| Nurse participation in daily physician rounds on the floor | 4.2 | 4.1 | 4.6 | 0.057 |
| Standardized checklist for discharges | 3.6 | 4.0 | 4.2 | 0.122 |
| Discharge information on white boards | 3.4 | 3.0 | 3.3 | 0.259 |
DISCUSSION
Our study demonstrated that nurses, interns, and hospitalists all feel that they play a pivotal role in discharge education. Compared to both interns and hospitalists, nurses were more likely to view discharge education as a shared responsibility, but nurses also reported providing more discharge education to patients. The elements of discharge education deemed a physician responsibility were reported as the least often provided to patients. Despite the majority of responses indicating that discharge education is a shared nursephysician responsibility, reported provider communication about discharge education was infrequent. Arguing for more communication, elements for which nurses and physicians perceived communicating more frequently were also more often reportedly conveyed to patients. The summative findings suggest that inconsistent discharge education and communication between providers may be leading to patients who are not regularly receiving complete discharge information. Nurses, interns, and hospitalists, however, were all very engaged in potential solutions to improve discharge communication, providing opportunities for immediate impact.
The question becomes where to start. Poor discharge instructions are associated with increased hospital readmission,10 and comprehensive discharge education is a suggested strategy to reduce preventable readmissions.12 Academic hospitalists, despite likely having witnessed the negative impact of poor discharge education, were not more likely than interns to report educating patients, nor did they report communicating more often with nurses. In teaching institutions, specifically, discharge education is being provided by multiple physicians: interns, residents, and hospitalists who may not have clearly defined roles in providing discharge education.13 Thus, providing comprehensive discharge instructions may require a hardwired system to ensure all elements of discharge education are addressed.
Further, our increasing dependence on technology may paradoxically necessitate more formal structures for in‐person communication, as the ability to enter discharge orders remotely leads to less frequent direct communication. Fortunately, as institutions move to computerized systems for discharge orders and instructions, there are increasing opportunities for a standardized approach to the elements of discharge education. While these results may suggest that one individual should be solely responsible for discharge education, trials using teams of nurse practitioners to facilitate transitions of care found no difference in patient length of stay or 30‐day readmission rates.14, 15
Formal systems that increase communication in high‐risk circumstances remain a focus in patient safety, and have been implemented successfully in procedural settings and with handoffs in patient care.1618 A prominent example is operating room time‐outs, which implemented a structured tool and shared process to increase nursephysician communication and reduce mortality.19 Since elements of discharge education with more frequent communication between nurses and physicians were more often conveyed to patients, our results suggest that a discharge time‐out might offer similar benefit. Fortunately, nurses and physicians rated verbal communication as the most desirable solution to share discharge education information. While not formally evaluated, one solution may be adoption of the previously described critical conversation, a structured format and a consistent time for communication that ensures both nurses and physicians understand what education needs to be provided to patients and by whom.20 The 13 discharge elements outlined in our study now provide a starting point for defining specific discussion points at discharge, delineation of who should communicate each element, and the basis for developing an operational discharge time‐out.
There are several limitations to our study. First, the survey instrument was not previously used or validated. However, we did seek formal and structured input while developing our survey, and conducted pilot testing to ensure clarity and comprehension with representatives of all study groups. Second, the 13 discharge education elements we included do not represent a comprehensive list, and were chosen based on our literature review and best practices at our institution. Third, our cross‐sectional study only captures perceptions and practices during a single time point, and may not adequately capture the greater continuum of true practice. Finally, our results may not be generalizable outside UCSFMC or other academic medical centers, particularly if other institutions have employed specific structures for discharge, such as a dedicated discharge coordinator.
CONCLUSION
Discharging patients is a complex process and one in which multiple providers and poor systems contribute to the redesign challenges. Providing high‐quality discharge education instructions to patients is an important step in making a complex process safer. Poor communication between nurses and physicians, complicated by ambiguous perceptions of responsibility for specific information, offers an opportunity for improvement efforts. We should not let well thought out treatment plans fail due to poor patient education on discharge. Our findings argue for a more systematic approach to the discharge education provided by nurses, interns, and hospitalists.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138(3):161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.Can Med Assoc J.2004;170(3):345–349.
- ,.Patients' understanding of their treatment plans and diagnosis at discharge.Mayo Clin Proc.2005;80(8):991–994.
- ,,.Functional health literacy and understanding of medications at discharge.Mayo Clin Proc.2008;83(5):554–558.
- ,,,.Patients' perception of hospital care in the United States.N Engl J Med.2008;359(18):1921–1931.
- ,,, et al.Comprehensive discharge planning and home follow‐up of hospitalized elders: a randomized clinical trial.JAMA.1999;281(7):613–620.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,, et al.Closing the loop: physician communication with diabetic patients who have low health literacy.Arch Intern Med.2003;163(1):83–90.
- ,,, et al.Structured interdisciplinary rounds in a medical teaching unit: improving patient safety.Arch Intern Med.2011;171(7):678–684.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1(6):354–360.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,,.Redefining readmission risk factors for general medicine patients.J Hosp Med.2011;6(2):54–60.
- ,,,,.“Out of sight, out of mind”: housestaff perceptions of quality‐limiting factors in discharge care at teaching hospitals.J Hosp Med.2012;7:376–381.
- ,,,,.To the hospital and back home again: a nurse practitioner‐based transitional care program for hospitalized homebound people.J Am Geriatr Soc.2011;59(3):544–551.
- ,,, et al.Improving the discharge process by embedding a discharge facilitator in a resident team.J Hosp Med.2011;6(9):494–500.
- ,,,,,.The potential for improved teamwork to reduce medical errors in the emergency department. The MedTeams Research Consortium.Ann Emerg Med.1999;34(3):373–383.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- ,,,,.Risk‐adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions.J Am Coll Surg.2007;205(6):778–784.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- ,,,,,.Critical conversations: a call for a nonprocedural “time out.”J Hosp Med.2011;6(4):225–230.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138(3):161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.Can Med Assoc J.2004;170(3):345–349.
- ,.Patients' understanding of their treatment plans and diagnosis at discharge.Mayo Clin Proc.2005;80(8):991–994.
- ,,.Functional health literacy and understanding of medications at discharge.Mayo Clin Proc.2008;83(5):554–558.
- ,,,.Patients' perception of hospital care in the United States.N Engl J Med.2008;359(18):1921–1931.
- ,,, et al.Comprehensive discharge planning and home follow‐up of hospitalized elders: a randomized clinical trial.JAMA.1999;281(7):613–620.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,, et al.Closing the loop: physician communication with diabetic patients who have low health literacy.Arch Intern Med.2003;163(1):83–90.
- ,,, et al.Structured interdisciplinary rounds in a medical teaching unit: improving patient safety.Arch Intern Med.2011;171(7):678–684.
- ,,, et al.Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists.J Hosp Med.2006;1(6):354–360.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,,.Redefining readmission risk factors for general medicine patients.J Hosp Med.2011;6(2):54–60.
- ,,,,.“Out of sight, out of mind”: housestaff perceptions of quality‐limiting factors in discharge care at teaching hospitals.J Hosp Med.2012;7:376–381.
- ,,,,.To the hospital and back home again: a nurse practitioner‐based transitional care program for hospitalized homebound people.J Am Geriatr Soc.2011;59(3):544–551.
- ,,, et al.Improving the discharge process by embedding a discharge facilitator in a resident team.J Hosp Med.2011;6(9):494–500.
- ,,,,,.The potential for improved teamwork to reduce medical errors in the emergency department. The MedTeams Research Consortium.Ann Emerg Med.1999;34(3):373–383.
- ,,, et al.Association between nurse‐physician collaboration and patient outcomes in three intensive care units.Crit Care Med.1999;27(9):1991–1998.
- ,,,,.Risk‐adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions.J Am Coll Surg.2007;205(6):778–784.
- ,,, et al.A surgical safety checklist to reduce morbidity and mortality in a global population.N Engl J Med.2009;360(5):491–499.
- ,,,,,.Critical conversations: a call for a nonprocedural “time out.”J Hosp Med.2011;6(4):225–230.
Copyright © 2012 Society of Hospital Medicine
Patient Satisfaction With Procedural Care
In order to improve resident supervision and timeliness of invasive bedside procedures such as paracentesis, thoracentesis, and lumbar puncture, some academic medical centers have implemented procedure services that focus on providing high‐quality procedural care.1, 2
Procedure services have the potential to affect patient satisfaction, a key indicator in quality of care measurment.3 Having senior physicians present increases patient comfort during outpatient case presentations4 and improves patient satisfaction with explanations of tests and medications.5 However, we had concerns that teaching during a procedure may heighten patient anxiety. Patients are reluctant to be the first patient of a resident or medical student for a procedure,68 and patients are more likely to refuse consent to have a resident perform complex procedures.8 In previous studies, patient satisfaction with gynecological exams and flexible sigmoidoscopy performed by residents was comparable to satisfaction with those performed by staff physicians,9, 10 though in the case of flexible sigmoidoscopy, procedure duration was slightly longer.10 Few, if any, data describe bedside teaching or patient impressions of physician communication during procedures.
We carried out a prospective study of patient perceptions of the University of California San Francisco (UCSF) Hospitalist Procedure Service (HPS). Our study had the primary goal of understanding how our modelwhich involves bedside procedural teaching and feedback in real time (eg, as the procedure is performed)is perceived by patients.
Patients and Methods
Site
Our survey was carried out at UCSF Moffitt‐Long Hospital, a 560‐bed university teaching hospital and the primary university hospital for the University of California San Francisco. This study was reviewed and approved by the Committee on Human Research at UCSF.
Procedure Service
The HPS is composed of two interns who rotate for 2 weeks on a mandatory rotation performing the majority of the procedures done by the service. Every procedure is supervised by an attending hospitalist who has received extended training from interventional radiologists and emergency department ultrasound faculty. Patients are referred to the service by their primary admitting team. Interns receive procedure‐specific didactics, demonstration, and practice with procedure kits, supplemental readings, computer‐based procedure modules, and evidence‐based summaries of procedure‐related considerations. All interns also attend a half‐day procedure simulation session to review procedural and ultrasound techniques.
While interns obtain informed consent and prepare the patient for the procedure, the attending and intern team communicate the following points with each patient: 1) identification as the dedicated procedure team, separate from the primary team caring for the patient; 2) attending self‐identification as the supervisor; 3) attention to stepwise communication with the patient during the procedure; 4) attention to patient comfort throughout the procedure; 5) emphasis on patient safety through the use of time‐outs, sterile technique, and ultrasound when appropriate; and 6) the intention to discuss best practice and teach during the procedure.
All paracentesis and thoracentesis sites are marked by using bedside ultrasound (S‐Cath, SonoSite, Bothell, WA) guidance prior to and, if needed, during the procedure. Ultrasound is occasionally used for marking joint aspiration and lumbar puncture.11 Interns are responsible for making an initial site marking, which is then confirmed by the attending physician. Although not systematized, our service encourages the intern and attending to communicate about proper technique during the procedure itself. For example, attendings ask questions about technique based on evidence in the literature (eg, Why do you replace the stylet in a lumbar puncture needle prior to removal?) or about trouble shooting (eg, What would you do if the flow of ascites stops during this paracentesis?) and also correct any errors in technique (Recall the angle you intended to use based on the ultrasound view).
Patients
Patients are referred to the procedure service by their primary team; referrals are accepted for patients on all services at all levels of care, including the emergency department (ED) and the intensive care unit (ICU). Participants in this study were referred for one of our target procedures (paracentesis, thoracentesis, or lumbar puncture) between November 2008 and July 2009. Patients gave written consent for the supplemental survey independent of consent for the procedure. All consents and procedures were performed in a patient's hospital room and one family member was allowed to stay in the room if desired by the patient. After the completion of the procedure, the attending on the procedure service at the time, which included study authors D.S. and M.M., approached consecutive patients who spoke and read English and were deemed to have capacity to consent for their own procedure to be surveyed. Patients were considered to have capacity to consent based on commonly accepted criteria described in the literature.12, 13 Patients were also excluded if their procedure was performed by the attending alone, if they had repeated procedures done by the service, or if they were too altered or critically ill to participate in the survey.
Survey
Our survey was developed through identification of items reported in the literature,1421 as well as items newly developed for purposes of examining our primary aims. Newly developed questions focused on patients' satisfaction with major aspects of procedure performance as well as the quality and impact of communication with the patient and between members of the team. Two open‐text questions were included to allow patients to share what went well with the procedure as well as areas for improvement. The research team developed a pool of question items for potential inclusion in a patient satisfaction questionnaire. These items were then shown to a group of research‐oriented health professionals, who meet regularly to review academic research protocols. The group provided their opinions about the content and comprehension of the questions, and the written survey employed was a result of their revisions (see Appendix in Supporting Information online).
Written surveys were distributed to patients by the hospitalist attending on service following the procedure as permitted by patients' severity of illness and availability. Surveys were anonymous and self‐administered by the patient or a family member who was in the room for the procedure; all questions were voluntary. A nurse was made responsible for collecting the survey when possible. Survey results were entered into a database without identifiers, with limited demographic information; patient gender, age, and procedure type were included by the attending hospitalist at the end of the survey. A separate and more detailed procedure database was kept of all procedures performed and was used to record patient consent or reason for not consenting as well as documented receipt of a completed survey. This non‐anonymous database contained detailed supplemental information including patient age, level of care, referring service, presence of bloody fluid at any point during the procedure, and physician‐reported immediate complications at the bedside in free text.
Analysis
Reported immediate complications were classified into major and minor based on reported definitions in the literature.2226 Similar to previous studies, major immediate complications were defined as those requiring further procedural intervention, medical therapy, or both.27 Major complications were defined as: bleeding requiring transfusion, pneumothorax requiring a chest tube, respiratory failure, bowel perforation, cerebral herniation or shock, cerebrospinal fluid (CSF) leak requiring intervention, and transfer to a higher level of care. For patients receiving a thoracentesis, chart review was performed to determine the presence of a follow‐up chest x‐ray, the presence of a pneumothorax, or clinical evidence for re‐expansion pulmonary edema. We analyzed differences between respondents and non‐respondents using Chi‐square tests for categorical variables (gender, level of care, referring service, procedure type, bloody fluid, and immediate reported complications) and independent t tests for continuous variables (age).
After review of the open‐ended fields, responses were classified into the following categories: pain control, physician skill, professionalism, communication, symptom relief, procedure duration, and miscellaneous comments. Responses regarding patient perceptions of physician communication were dichotomized into positive (1 = Strongly Agree, 2 = Agree) and negative (3 = Neutral, 4 = Disagree, and 5 = Strongly Disagree), and independent t tests were used to determine the contribution of factors, such as age, while Chi‐square tests were used for the contribution of gender and procedure type. All statistical tests were performed by using the SAS statistical application program (version 9.2).
Results
Respondent Characteristics
Of 324 procedures performed by the HPS during the study period, 95 (29%) were eligible for consent. Of the 229 patients not eligible for consent, 32 (10%) were excluded because the procedure was performed by the attending alone, 76 (23%) lacked English proficiency or literacy, 66 (20%) had altered mental status, 32 (10%) were intubated and/or had severe illness precluding consent, and 23 (7%) were repeat procedures on patients who had previously completed the survey. Only two patients specifically requested an attending to perform the procedure after an introduction to the service. Of the 95 patients eligible for consent, 89 were consented for the survey, and 65 (68%) completed the survey. Of the six eligible, non‐consented patients, all were leaving the floor immediately following the procedure, and time did not allow for consent and survey distribution. There were no differences between eligible responders and nonresponders in age, gender, procedure, requesting service, presence of bloody fluid, or physician‐reported immediate complications (Table 1).
| Demographics | Respondera (n = 65) | Nonresponder (n = 24) |
|---|---|---|
| ||
| Age, y [mean (SD)] | 55.4 (15.7) | 50.4 (17.4) |
| Male gender, n (%) male | 41 (63.1) | 11 (45.8) |
| Procedure, n (%) | ||
| Paracentesis | 31 (47.7) | 10 (41.7) |
| Thoracentesis | 17 (25.8) | 6 (25.0) |
| Lumbar puncture | 15 (22.7) | 7 (29.2) |
| Arthrocentesis | 2 (3.0) | 1 (4.2) |
| Patient location, n (%) | ||
| Floor | 47 (72.3) | 19 (79.2) |
| Step down/telemetry | 17 (26.1) | 3 (12.5) |
| Intensive care unit | 1 (1.5) | 2 (8.3) |
| Service requesting, n (%) | ||
| Medicine | 29 (44.6) | 10 (41.7) |
| Cardiology | 6 (9.1) | 3 (12.5) |
| Liver transplant | 20 (30.3) | 7 (29.2) |
| Bone marrow transplant | 7 (10.6) | 1 (4.2) |
| Surgery | 0 | 1 (4.2) |
| Neurosurgery | 1 (1.5) | 1 (4.2) |
| Other | 2 (3.0) | 1 (4.2) |
| Reported presence of bloody fluid at any point in the procedure, n (%) | 9 (13.6) | 4 (16.7) |
| Other reported immediate complications | ||
| Equipment malfunction | 2 (3.0) | 1 (4.2) |
| Significant cough/pleuritic pain | 1 (1.5) | 1 (4.2) |
| Transient oxygen desaturation | 1 (1.5) | 0 |
| Ascites leak | 0 | 0 |
| Hematoma | 0 | 0 |
| Persistent bleeding | 0 | 0 |
| Transfer to a higher level of care | 0 | 0 |
Complications
As complications would likely play a role in procedure satisfaction, we describe immediate complications for the study population. Of the 324 procedures performed during the study period, no patient had predefined major immediate complications. Upon further chart review of the 96 patients that had a thoracentesis performed, all had a follow‐up chest x‐ray and none suffered an iatrogenic pneumothorax or re‐expansion pulmonary edema. Minor immediate complications for the 324 procedures were reported as follows: postprocedure pain in four patients (1.2%), cough in nine patients (2.8%), five equipment malfunctions (1.5%), four ascites leaks (1.2%), and one incisional bleed requiring a suture for hemostasis (0.3%). There was no significant difference in complications between those consented for the survey and the total study population.
Procedure Satisfaction
More than 90% of patients were satisfied or very satisfied with most aspects of the procedure, including the informed consent process, pain control, expertise, and courtesy of physicians (Table 2). The percentage of patients satisfied with the duration of procedure (88%) was lower than for other measures of satisfaction. Of the 38 patients receiving therapeutic procedures, 34 (89%) were satisfied or highly satisfied with the improvement in symptoms following the procedure.
| Very Satisfied and Satisfied No. (%) | Neutral No. (%) | Dissatisfied and Very Dissatisfied No. (%) | N/A No. (%) | |
|---|---|---|---|---|
| Your overall procedure experience | 65 (100) | 0 (0) | 0 (0) | 0 (0) |
| Explanation of the procedure, risks, and benefits before the procedure | 64 (99) | 1 (2) | 0 (0) | 0 (0) |
| Pain control during the procedure | 60 (92) | 5 (8) | 0 (0) | 0 (0) |
| Expertise/skill of the physicians performing your procedure | 62 (95) | 3 (5) | 0 (0) | 0 (0) |
| Courtesy and bedside manner of the physicians performing your procedure | 65 (100) | 0 (0) | 0 (0) | 0 (0) |
| The time it took to perform your procedure | 57 (88) | 6 (9) | 0 (0) | 2 (3) |
| Improvement in your symptoms following this procedure, if applicable | 34 (52) | 7 (11) | 0 (0) | 24 (37) |
When asked what went well with the procedure, 59 (91%) respondents provided additional comments and feedback. Each response was classified as described in the Methods section. Of the free text responses, 8 of the 59 patients (14%) commented on the attention to pain control (eg, The caring and attention to my pain was most important to me), 5 (8%) on the skills of the operators (Great examination of the entire stomach region with the ultrasound to ensure the best position of the catheter), 6 (10%) on the courtesy and professionalism of the team (eg, Courteous, team‐feeling, addressed my concerns), 9 (15%) on their communication with the team (eg, The doctors made me feel very comfortable before the procedure by laying out the plan and explaining each part of the procedure), and 8 (14%) on relief of their symptoms (eg, There was an almost immediate and significant improvement in my breathing, bloating, and pain). Twenty‐three of the 59 comments (39%) were categorized as miscellaneous (eg, All went great. I fell asleep).
When asked areas for improvement, 55 (85%) patients responded. Thirty‐three patients (60%) reported that nothing could be improved or they instructed the team to just keep doing what you are doing, while 22 (40%) patients expressed a concern. Responses were categorized in a similar fashion to the positive responses. Five of the 22 negative comments (23%) reported that the procedure took too long (eg, Procedure could have been shorter. I got tired sitting up), 4 (18%) commented on pain control (eg, The poke for marking my skin hurt more than the anesthetic. I was surprised), 6 (27%) felt communication was a problem (eg, Discuss the steps with the patient audibly, no whispering, speak clearly), and 7 (32%) had miscellaneous concerns (eg, Try not to do this procedure right after another one).
Physician Communication
Sixty‐four patients (98%) reported that the physicians performing their procedure communicated with each other during the procedure (Table 3). Although one patient did not feel that the physicians communicated with each other, he or she still answered the follow‐up questions regarding perceptions of physician communication. We excluded this patient from our analysis as his or her answers may not be reliable. The majority of patients (84%) reported this communication as reassuring and felt it was a normal part of procedure performance (94%). Those that did not agree that physician communication was reassuring did not differ in average age (P = 0.307), gender (P = 0.511), or procedure type (P = 0.562).
| Strongly Agree and Agree No. (%) | Neutral No. (%) | Disagree, and Strongly Disagree No. (%) | |
|---|---|---|---|
| I felt that the physicians talking to each other about my procedure was reassuring to me | 54 (84) | 10 (16) | 0 (0) |
| Physicians talking to each other while doing a procedure is a normal part of doing a procedure | 60 (94) | 4 (6) | 0 (0) |
Of all positive and negative comments, five specifically addressed communication between physicians. Most (four) reflected satisfaction with bedside teaching (eg, They discussed the procedure in a professional manner and eased my mind at all times) and with having an expert in the room (eg, [The team] discussed things like needle placement, which was nice because there was a second opinion right there in the room). Patients also felt that it was good to experience the teaching, with one patient reporting that the best part of the procedure was watching doctors learn from each other. Patients did not express specific reservations about bedside teaching, resident technique, or fear of complications in free text.
Discussion
Even though novice interns performed procedures and simultaneous bedside teaching, patient satisfaction with a teaching procedure service was high, and reported complication rates were low. In addition, a majority of patients found discussions related to teaching activities reassuring and potentially important to their perception of care quality. Analogous studies examining patient satisfaction with endoscopic care found similar rates of patient satisfaction with endoscopists' bedside manner, technical skills, and pain control, but these studies included sedated patients.21 Our results are unique, as we evaluated awake patients with attention to perception of bedside teaching with novice interns.
Our findings offer an alternative strategy for bedside procedural teaching that employs transparency in the use of an expert and a trainee to introduce patients to bedside teaching by experts, which is not common at many academic medical centers.28 Patients may have been reassured by a clear explanation of the role of the service and the providers involved as well as an assurance of expertise and attention to patient comfort and safety. In addition to patient satisfaction, this model has the potential to impact both the safety of bedside procedures and housestaff education around procedure performance. For example, pneumothorax rates using our procedure service model are lower than those published (0% vs. 4% for ultrasound‐guided thoracentesis and 8.5% for thoracentesis by less experienced clinicians).29
Providers may be reluctant to teach at the bedside of awake patients for fear of heightening patient anxiety over trainee inexperience. In the 1960s similar fears were raised over the concern for patient anxiety with bedside rounding,30 but later studies revealed these concerns to be largely unfounded. Instead, bedside rounds have been shown to positively influence patients' feelings about their hospital experience and their relationships with their physicians compared with patients whose case presentations were made in a conference room.31, 32 Given the opportunity to comment on areas for improvement, patients in our study specifically elaborated regarding pain control, communication, and efficiency problems. Although 16% of patients did not find the communication of physicians reassuring, none of the negative comments reflected problems with bedside teaching, but rather concepts such as desiring a better explanation of steps throughout the procedure. Specifically, patients desire better communication for unanticipated pain.
There are several limitations to this study. Lack of patient satisfaction data from a control group of patients whose procedures were performed by attendings or housestaff alone limits our ability to draw conclusions about our satisfaction scores. The scarce applicable literature offers only imperfect comparison data. Because hospitalists were not blinded to the survey, attending behavior may have been subject to a Hawthorne effect.33 Consenting patients after the procedure could have provided hospitalists with an opportunity to exclude patients who appeared less satisfied with their procedure; however, attempts were made to prevent this behavior by requiring strict accounting of why a patient was not consented for the study. Use of alternative personnel for consent such as nurses was explored, but was found not to be feasible due to limited resources. These data are only applicable to English‐speaking patients who are literate and well enough to complete a survey. It is not clear whether the experience for other patients would reflect the same outcomes. It is plausible that non‐English‐speaking patients might have more concerns about incomprehensible conversations taking place during their procedure. Although the surveys were anonymous and patients were told that the proceduralists would not see individual responses, responses may have been biased out of patient concern that their response might affect their care. Hospitalists obtaining consent, however, were careful to stress anonymity and the distinction between the primary team and the procedure team.
Academic hospitals are struggling with providing quality procedural care while balancing housestaff education and experience.28 With hospitalists playing an increasingly prominent role in housestaff education and patient satisfaction initiatives, the supervision of housestaff by trained hospitalist faculty may help meet both aims in the performance of invasive bedside procedures, particularly at institutions where simulation training resources are limited. Although concern may exist for potential patient anxiety with bedside teaching, our data demonstrate high levels of patient satisfaction with a hospitalist procedure service despite novice procedure performers and an emphasis on teaching during the procedure.
- ,,, et al.Creation of an innovative inpatient medical procedure service and a method to evaluate house staff competency.J Gen Intern Med.2004;19(5 Pt 2):510–513.
- ,,, et al.Impact of a bedside procedure service on general medicine inpatients: A firm‐based trial.J Hosp Med.2007;2(3):143–149.
- Hospital Care Quality Information from the Consumer Perspective (HCAHPS).Quality Assurance Guidelines.Baltimore, MD:Centers for Medicare 113(8):657–662.
- ,,,,.The effect of bedside case presentations on patients' perceptions of their medical care.N Engl J Med.1997;336(16):1150–1155.
- ,,,.‘Sorry, it's my first time!’ Will patients consent to medical students learning procedures?Med Educ.2005;39(4):365–369.
- ,.Ethical considerations surrounding first time procedures: a study and analysis of patient attitudes toward spinal taps by students.Kennedy Inst Ethics J.1992;2(3):217–231.
- ,,,.Patients' willingness to allow residents to learn to practice medical procedures.Acad Med.2004;79(2):144–147.
- ,,.Patient satisfaction with gynecologic care provided by family practice resident physicians.Fam Pract Res J.1991;11(4):421–428.
- ,,.Resident participation in flexible sigmoidoscopy does not affect patient satisfaction.Am J Gastroenterol.2000;95(6):1563–1566.
- ,.Bedside ultrasound for difficult lumbar puncture.J Emerg Med.2005;28(2):197–200.
- ,.Conducting the Assessment. In:Assessing Competence to Consent to Treatment: A Guide for Physicians and Other Health Professionals.First Edition ed.New York, NY:Oxford University Press;1998:80–91.
- ,.Care of Ill, Socially Complicated Patients. In:Medical Management of Vulnerable 2007:407–418.
- ,,,,.Interventional radiologic procedures: patient anxiety, perception of pain, understanding of procedure, and satisfaction with medication‐‐a prospective study.Radiology.2000;215(3):684–688.
- ,,,,.Improving the assessment of (in)patients' satisfaction with hospital care.Med Care.2001;39(3):270–283.
- ,,,.Factors determining inpatient satisfaction with care.Soc Sci Med.2002;54(4):493–504.
- ,,,.Reliability and validity of the Satisfaction with Hospital Care Questionnaire.Int J Qual Health Care.2002;14(6):471–482.
- ,,,,.A randomized trial of four patient satisfaction questionnaires.Med Care.2003;41(12):1343–1352.
- ,,, et al.Development and validation of an in‐patient satisfaction questionnaire.Int J Qual Health Care.2005;17(6):465–472.
- ,,,.Central venous port catheters: evaluation of patients' satisfaction with implantation under local anesthesia.J Vasc Access.2009;10(1):27–32.
- ,,,.Factors influencing patient satisfaction when undergoing endoscopic procedures.Gastrointest Endosc.2009;69(4):883–91, quiz 891.e1.
- ,,, et al.Complications associated with thoracentesis. A prospective, randomized study comparing three different methods.Arch Intern Med.1990;150(4):873–877.
- ,,, et al.Risk of complications after abdominal paracentesis in cirrhotic patients: a prospective study.Clin Gastroenterol Hepatol.2009;7(8):906–909.
- ,,, et al.Performance standards for therapeutic abdominal paracentesis.Hepatology.2004;40(2):484–488.
- ,,,,.Lumbar puncture: its indications, contraindications, complications and technique.Rev Neurol.2007;45(7):433–436.
- .How to perform a lumbar puncture with the patient in the seated position.Br J Hosp Med (Lond).2006;67(3):M46–7.
- ,,.Are commonly used resident measurements associated with procedural skills in internal medicine residency training?J Gen Intern Med.2007;22(3):357–361.
- ,,,MERN Group,.Supervising the Supervisors‐Procedural Training and Supervision in Internal Medicine Residency.J Gen Intern Med.2010.
- ,,,.Pneumothorax following thoracentesis: a systematic review and meta‐analysis.Arch Intern Med.2010;170(4):332–339.
- ,,.The emotional impact of ward rounds.J Mt Sinai Hosp NY.1956;23(6):782–803.
- ,,,.The physiologic and psychological effects of the bedside presentation.N Engl J Med.1989;321(18):1273–1275.
- ,,,,.The effect of bedside case presentations on patients' perceptions of their medical care.N Engl J Med.1997;336(16):1150–1155.
- .Hawthorne effects and research into professional practice.J Eval Clin Pract.2001;7(1):65–70.
In order to improve resident supervision and timeliness of invasive bedside procedures such as paracentesis, thoracentesis, and lumbar puncture, some academic medical centers have implemented procedure services that focus on providing high‐quality procedural care.1, 2
Procedure services have the potential to affect patient satisfaction, a key indicator in quality of care measurment.3 Having senior physicians present increases patient comfort during outpatient case presentations4 and improves patient satisfaction with explanations of tests and medications.5 However, we had concerns that teaching during a procedure may heighten patient anxiety. Patients are reluctant to be the first patient of a resident or medical student for a procedure,68 and patients are more likely to refuse consent to have a resident perform complex procedures.8 In previous studies, patient satisfaction with gynecological exams and flexible sigmoidoscopy performed by residents was comparable to satisfaction with those performed by staff physicians,9, 10 though in the case of flexible sigmoidoscopy, procedure duration was slightly longer.10 Few, if any, data describe bedside teaching or patient impressions of physician communication during procedures.
We carried out a prospective study of patient perceptions of the University of California San Francisco (UCSF) Hospitalist Procedure Service (HPS). Our study had the primary goal of understanding how our modelwhich involves bedside procedural teaching and feedback in real time (eg, as the procedure is performed)is perceived by patients.
Patients and Methods
Site
Our survey was carried out at UCSF Moffitt‐Long Hospital, a 560‐bed university teaching hospital and the primary university hospital for the University of California San Francisco. This study was reviewed and approved by the Committee on Human Research at UCSF.
Procedure Service
The HPS is composed of two interns who rotate for 2 weeks on a mandatory rotation performing the majority of the procedures done by the service. Every procedure is supervised by an attending hospitalist who has received extended training from interventional radiologists and emergency department ultrasound faculty. Patients are referred to the service by their primary admitting team. Interns receive procedure‐specific didactics, demonstration, and practice with procedure kits, supplemental readings, computer‐based procedure modules, and evidence‐based summaries of procedure‐related considerations. All interns also attend a half‐day procedure simulation session to review procedural and ultrasound techniques.
While interns obtain informed consent and prepare the patient for the procedure, the attending and intern team communicate the following points with each patient: 1) identification as the dedicated procedure team, separate from the primary team caring for the patient; 2) attending self‐identification as the supervisor; 3) attention to stepwise communication with the patient during the procedure; 4) attention to patient comfort throughout the procedure; 5) emphasis on patient safety through the use of time‐outs, sterile technique, and ultrasound when appropriate; and 6) the intention to discuss best practice and teach during the procedure.
All paracentesis and thoracentesis sites are marked by using bedside ultrasound (S‐Cath, SonoSite, Bothell, WA) guidance prior to and, if needed, during the procedure. Ultrasound is occasionally used for marking joint aspiration and lumbar puncture.11 Interns are responsible for making an initial site marking, which is then confirmed by the attending physician. Although not systematized, our service encourages the intern and attending to communicate about proper technique during the procedure itself. For example, attendings ask questions about technique based on evidence in the literature (eg, Why do you replace the stylet in a lumbar puncture needle prior to removal?) or about trouble shooting (eg, What would you do if the flow of ascites stops during this paracentesis?) and also correct any errors in technique (Recall the angle you intended to use based on the ultrasound view).
Patients
Patients are referred to the procedure service by their primary team; referrals are accepted for patients on all services at all levels of care, including the emergency department (ED) and the intensive care unit (ICU). Participants in this study were referred for one of our target procedures (paracentesis, thoracentesis, or lumbar puncture) between November 2008 and July 2009. Patients gave written consent for the supplemental survey independent of consent for the procedure. All consents and procedures were performed in a patient's hospital room and one family member was allowed to stay in the room if desired by the patient. After the completion of the procedure, the attending on the procedure service at the time, which included study authors D.S. and M.M., approached consecutive patients who spoke and read English and were deemed to have capacity to consent for their own procedure to be surveyed. Patients were considered to have capacity to consent based on commonly accepted criteria described in the literature.12, 13 Patients were also excluded if their procedure was performed by the attending alone, if they had repeated procedures done by the service, or if they were too altered or critically ill to participate in the survey.
Survey
Our survey was developed through identification of items reported in the literature,1421 as well as items newly developed for purposes of examining our primary aims. Newly developed questions focused on patients' satisfaction with major aspects of procedure performance as well as the quality and impact of communication with the patient and between members of the team. Two open‐text questions were included to allow patients to share what went well with the procedure as well as areas for improvement. The research team developed a pool of question items for potential inclusion in a patient satisfaction questionnaire. These items were then shown to a group of research‐oriented health professionals, who meet regularly to review academic research protocols. The group provided their opinions about the content and comprehension of the questions, and the written survey employed was a result of their revisions (see Appendix in Supporting Information online).
Written surveys were distributed to patients by the hospitalist attending on service following the procedure as permitted by patients' severity of illness and availability. Surveys were anonymous and self‐administered by the patient or a family member who was in the room for the procedure; all questions were voluntary. A nurse was made responsible for collecting the survey when possible. Survey results were entered into a database without identifiers, with limited demographic information; patient gender, age, and procedure type were included by the attending hospitalist at the end of the survey. A separate and more detailed procedure database was kept of all procedures performed and was used to record patient consent or reason for not consenting as well as documented receipt of a completed survey. This non‐anonymous database contained detailed supplemental information including patient age, level of care, referring service, presence of bloody fluid at any point during the procedure, and physician‐reported immediate complications at the bedside in free text.
Analysis
Reported immediate complications were classified into major and minor based on reported definitions in the literature.2226 Similar to previous studies, major immediate complications were defined as those requiring further procedural intervention, medical therapy, or both.27 Major complications were defined as: bleeding requiring transfusion, pneumothorax requiring a chest tube, respiratory failure, bowel perforation, cerebral herniation or shock, cerebrospinal fluid (CSF) leak requiring intervention, and transfer to a higher level of care. For patients receiving a thoracentesis, chart review was performed to determine the presence of a follow‐up chest x‐ray, the presence of a pneumothorax, or clinical evidence for re‐expansion pulmonary edema. We analyzed differences between respondents and non‐respondents using Chi‐square tests for categorical variables (gender, level of care, referring service, procedure type, bloody fluid, and immediate reported complications) and independent t tests for continuous variables (age).
After review of the open‐ended fields, responses were classified into the following categories: pain control, physician skill, professionalism, communication, symptom relief, procedure duration, and miscellaneous comments. Responses regarding patient perceptions of physician communication were dichotomized into positive (1 = Strongly Agree, 2 = Agree) and negative (3 = Neutral, 4 = Disagree, and 5 = Strongly Disagree), and independent t tests were used to determine the contribution of factors, such as age, while Chi‐square tests were used for the contribution of gender and procedure type. All statistical tests were performed by using the SAS statistical application program (version 9.2).
Results
Respondent Characteristics
Of 324 procedures performed by the HPS during the study period, 95 (29%) were eligible for consent. Of the 229 patients not eligible for consent, 32 (10%) were excluded because the procedure was performed by the attending alone, 76 (23%) lacked English proficiency or literacy, 66 (20%) had altered mental status, 32 (10%) were intubated and/or had severe illness precluding consent, and 23 (7%) were repeat procedures on patients who had previously completed the survey. Only two patients specifically requested an attending to perform the procedure after an introduction to the service. Of the 95 patients eligible for consent, 89 were consented for the survey, and 65 (68%) completed the survey. Of the six eligible, non‐consented patients, all were leaving the floor immediately following the procedure, and time did not allow for consent and survey distribution. There were no differences between eligible responders and nonresponders in age, gender, procedure, requesting service, presence of bloody fluid, or physician‐reported immediate complications (Table 1).
| Demographics | Respondera (n = 65) | Nonresponder (n = 24) |
|---|---|---|
| ||
| Age, y [mean (SD)] | 55.4 (15.7) | 50.4 (17.4) |
| Male gender, n (%) male | 41 (63.1) | 11 (45.8) |
| Procedure, n (%) | ||
| Paracentesis | 31 (47.7) | 10 (41.7) |
| Thoracentesis | 17 (25.8) | 6 (25.0) |
| Lumbar puncture | 15 (22.7) | 7 (29.2) |
| Arthrocentesis | 2 (3.0) | 1 (4.2) |
| Patient location, n (%) | ||
| Floor | 47 (72.3) | 19 (79.2) |
| Step down/telemetry | 17 (26.1) | 3 (12.5) |
| Intensive care unit | 1 (1.5) | 2 (8.3) |
| Service requesting, n (%) | ||
| Medicine | 29 (44.6) | 10 (41.7) |
| Cardiology | 6 (9.1) | 3 (12.5) |
| Liver transplant | 20 (30.3) | 7 (29.2) |
| Bone marrow transplant | 7 (10.6) | 1 (4.2) |
| Surgery | 0 | 1 (4.2) |
| Neurosurgery | 1 (1.5) | 1 (4.2) |
| Other | 2 (3.0) | 1 (4.2) |
| Reported presence of bloody fluid at any point in the procedure, n (%) | 9 (13.6) | 4 (16.7) |
| Other reported immediate complications | ||
| Equipment malfunction | 2 (3.0) | 1 (4.2) |
| Significant cough/pleuritic pain | 1 (1.5) | 1 (4.2) |
| Transient oxygen desaturation | 1 (1.5) | 0 |
| Ascites leak | 0 | 0 |
| Hematoma | 0 | 0 |
| Persistent bleeding | 0 | 0 |
| Transfer to a higher level of care | 0 | 0 |
Complications
As complications would likely play a role in procedure satisfaction, we describe immediate complications for the study population. Of the 324 procedures performed during the study period, no patient had predefined major immediate complications. Upon further chart review of the 96 patients that had a thoracentesis performed, all had a follow‐up chest x‐ray and none suffered an iatrogenic pneumothorax or re‐expansion pulmonary edema. Minor immediate complications for the 324 procedures were reported as follows: postprocedure pain in four patients (1.2%), cough in nine patients (2.8%), five equipment malfunctions (1.5%), four ascites leaks (1.2%), and one incisional bleed requiring a suture for hemostasis (0.3%). There was no significant difference in complications between those consented for the survey and the total study population.
Procedure Satisfaction
More than 90% of patients were satisfied or very satisfied with most aspects of the procedure, including the informed consent process, pain control, expertise, and courtesy of physicians (Table 2). The percentage of patients satisfied with the duration of procedure (88%) was lower than for other measures of satisfaction. Of the 38 patients receiving therapeutic procedures, 34 (89%) were satisfied or highly satisfied with the improvement in symptoms following the procedure.
| Very Satisfied and Satisfied No. (%) | Neutral No. (%) | Dissatisfied and Very Dissatisfied No. (%) | N/A No. (%) | |
|---|---|---|---|---|
| Your overall procedure experience | 65 (100) | 0 (0) | 0 (0) | 0 (0) |
| Explanation of the procedure, risks, and benefits before the procedure | 64 (99) | 1 (2) | 0 (0) | 0 (0) |
| Pain control during the procedure | 60 (92) | 5 (8) | 0 (0) | 0 (0) |
| Expertise/skill of the physicians performing your procedure | 62 (95) | 3 (5) | 0 (0) | 0 (0) |
| Courtesy and bedside manner of the physicians performing your procedure | 65 (100) | 0 (0) | 0 (0) | 0 (0) |
| The time it took to perform your procedure | 57 (88) | 6 (9) | 0 (0) | 2 (3) |
| Improvement in your symptoms following this procedure, if applicable | 34 (52) | 7 (11) | 0 (0) | 24 (37) |
When asked what went well with the procedure, 59 (91%) respondents provided additional comments and feedback. Each response was classified as described in the Methods section. Of the free text responses, 8 of the 59 patients (14%) commented on the attention to pain control (eg, The caring and attention to my pain was most important to me), 5 (8%) on the skills of the operators (Great examination of the entire stomach region with the ultrasound to ensure the best position of the catheter), 6 (10%) on the courtesy and professionalism of the team (eg, Courteous, team‐feeling, addressed my concerns), 9 (15%) on their communication with the team (eg, The doctors made me feel very comfortable before the procedure by laying out the plan and explaining each part of the procedure), and 8 (14%) on relief of their symptoms (eg, There was an almost immediate and significant improvement in my breathing, bloating, and pain). Twenty‐three of the 59 comments (39%) were categorized as miscellaneous (eg, All went great. I fell asleep).
When asked areas for improvement, 55 (85%) patients responded. Thirty‐three patients (60%) reported that nothing could be improved or they instructed the team to just keep doing what you are doing, while 22 (40%) patients expressed a concern. Responses were categorized in a similar fashion to the positive responses. Five of the 22 negative comments (23%) reported that the procedure took too long (eg, Procedure could have been shorter. I got tired sitting up), 4 (18%) commented on pain control (eg, The poke for marking my skin hurt more than the anesthetic. I was surprised), 6 (27%) felt communication was a problem (eg, Discuss the steps with the patient audibly, no whispering, speak clearly), and 7 (32%) had miscellaneous concerns (eg, Try not to do this procedure right after another one).
Physician Communication
Sixty‐four patients (98%) reported that the physicians performing their procedure communicated with each other during the procedure (Table 3). Although one patient did not feel that the physicians communicated with each other, he or she still answered the follow‐up questions regarding perceptions of physician communication. We excluded this patient from our analysis as his or her answers may not be reliable. The majority of patients (84%) reported this communication as reassuring and felt it was a normal part of procedure performance (94%). Those that did not agree that physician communication was reassuring did not differ in average age (P = 0.307), gender (P = 0.511), or procedure type (P = 0.562).
| Strongly Agree and Agree No. (%) | Neutral No. (%) | Disagree, and Strongly Disagree No. (%) | |
|---|---|---|---|
| I felt that the physicians talking to each other about my procedure was reassuring to me | 54 (84) | 10 (16) | 0 (0) |
| Physicians talking to each other while doing a procedure is a normal part of doing a procedure | 60 (94) | 4 (6) | 0 (0) |
Of all positive and negative comments, five specifically addressed communication between physicians. Most (four) reflected satisfaction with bedside teaching (eg, They discussed the procedure in a professional manner and eased my mind at all times) and with having an expert in the room (eg, [The team] discussed things like needle placement, which was nice because there was a second opinion right there in the room). Patients also felt that it was good to experience the teaching, with one patient reporting that the best part of the procedure was watching doctors learn from each other. Patients did not express specific reservations about bedside teaching, resident technique, or fear of complications in free text.
Discussion
Even though novice interns performed procedures and simultaneous bedside teaching, patient satisfaction with a teaching procedure service was high, and reported complication rates were low. In addition, a majority of patients found discussions related to teaching activities reassuring and potentially important to their perception of care quality. Analogous studies examining patient satisfaction with endoscopic care found similar rates of patient satisfaction with endoscopists' bedside manner, technical skills, and pain control, but these studies included sedated patients.21 Our results are unique, as we evaluated awake patients with attention to perception of bedside teaching with novice interns.
Our findings offer an alternative strategy for bedside procedural teaching that employs transparency in the use of an expert and a trainee to introduce patients to bedside teaching by experts, which is not common at many academic medical centers.28 Patients may have been reassured by a clear explanation of the role of the service and the providers involved as well as an assurance of expertise and attention to patient comfort and safety. In addition to patient satisfaction, this model has the potential to impact both the safety of bedside procedures and housestaff education around procedure performance. For example, pneumothorax rates using our procedure service model are lower than those published (0% vs. 4% for ultrasound‐guided thoracentesis and 8.5% for thoracentesis by less experienced clinicians).29
Providers may be reluctant to teach at the bedside of awake patients for fear of heightening patient anxiety over trainee inexperience. In the 1960s similar fears were raised over the concern for patient anxiety with bedside rounding,30 but later studies revealed these concerns to be largely unfounded. Instead, bedside rounds have been shown to positively influence patients' feelings about their hospital experience and their relationships with their physicians compared with patients whose case presentations were made in a conference room.31, 32 Given the opportunity to comment on areas for improvement, patients in our study specifically elaborated regarding pain control, communication, and efficiency problems. Although 16% of patients did not find the communication of physicians reassuring, none of the negative comments reflected problems with bedside teaching, but rather concepts such as desiring a better explanation of steps throughout the procedure. Specifically, patients desire better communication for unanticipated pain.
There are several limitations to this study. Lack of patient satisfaction data from a control group of patients whose procedures were performed by attendings or housestaff alone limits our ability to draw conclusions about our satisfaction scores. The scarce applicable literature offers only imperfect comparison data. Because hospitalists were not blinded to the survey, attending behavior may have been subject to a Hawthorne effect.33 Consenting patients after the procedure could have provided hospitalists with an opportunity to exclude patients who appeared less satisfied with their procedure; however, attempts were made to prevent this behavior by requiring strict accounting of why a patient was not consented for the study. Use of alternative personnel for consent such as nurses was explored, but was found not to be feasible due to limited resources. These data are only applicable to English‐speaking patients who are literate and well enough to complete a survey. It is not clear whether the experience for other patients would reflect the same outcomes. It is plausible that non‐English‐speaking patients might have more concerns about incomprehensible conversations taking place during their procedure. Although the surveys were anonymous and patients were told that the proceduralists would not see individual responses, responses may have been biased out of patient concern that their response might affect their care. Hospitalists obtaining consent, however, were careful to stress anonymity and the distinction between the primary team and the procedure team.
Academic hospitals are struggling with providing quality procedural care while balancing housestaff education and experience.28 With hospitalists playing an increasingly prominent role in housestaff education and patient satisfaction initiatives, the supervision of housestaff by trained hospitalist faculty may help meet both aims in the performance of invasive bedside procedures, particularly at institutions where simulation training resources are limited. Although concern may exist for potential patient anxiety with bedside teaching, our data demonstrate high levels of patient satisfaction with a hospitalist procedure service despite novice procedure performers and an emphasis on teaching during the procedure.
In order to improve resident supervision and timeliness of invasive bedside procedures such as paracentesis, thoracentesis, and lumbar puncture, some academic medical centers have implemented procedure services that focus on providing high‐quality procedural care.1, 2
Procedure services have the potential to affect patient satisfaction, a key indicator in quality of care measurment.3 Having senior physicians present increases patient comfort during outpatient case presentations4 and improves patient satisfaction with explanations of tests and medications.5 However, we had concerns that teaching during a procedure may heighten patient anxiety. Patients are reluctant to be the first patient of a resident or medical student for a procedure,68 and patients are more likely to refuse consent to have a resident perform complex procedures.8 In previous studies, patient satisfaction with gynecological exams and flexible sigmoidoscopy performed by residents was comparable to satisfaction with those performed by staff physicians,9, 10 though in the case of flexible sigmoidoscopy, procedure duration was slightly longer.10 Few, if any, data describe bedside teaching or patient impressions of physician communication during procedures.
We carried out a prospective study of patient perceptions of the University of California San Francisco (UCSF) Hospitalist Procedure Service (HPS). Our study had the primary goal of understanding how our modelwhich involves bedside procedural teaching and feedback in real time (eg, as the procedure is performed)is perceived by patients.
Patients and Methods
Site
Our survey was carried out at UCSF Moffitt‐Long Hospital, a 560‐bed university teaching hospital and the primary university hospital for the University of California San Francisco. This study was reviewed and approved by the Committee on Human Research at UCSF.
Procedure Service
The HPS is composed of two interns who rotate for 2 weeks on a mandatory rotation performing the majority of the procedures done by the service. Every procedure is supervised by an attending hospitalist who has received extended training from interventional radiologists and emergency department ultrasound faculty. Patients are referred to the service by their primary admitting team. Interns receive procedure‐specific didactics, demonstration, and practice with procedure kits, supplemental readings, computer‐based procedure modules, and evidence‐based summaries of procedure‐related considerations. All interns also attend a half‐day procedure simulation session to review procedural and ultrasound techniques.
While interns obtain informed consent and prepare the patient for the procedure, the attending and intern team communicate the following points with each patient: 1) identification as the dedicated procedure team, separate from the primary team caring for the patient; 2) attending self‐identification as the supervisor; 3) attention to stepwise communication with the patient during the procedure; 4) attention to patient comfort throughout the procedure; 5) emphasis on patient safety through the use of time‐outs, sterile technique, and ultrasound when appropriate; and 6) the intention to discuss best practice and teach during the procedure.
All paracentesis and thoracentesis sites are marked by using bedside ultrasound (S‐Cath, SonoSite, Bothell, WA) guidance prior to and, if needed, during the procedure. Ultrasound is occasionally used for marking joint aspiration and lumbar puncture.11 Interns are responsible for making an initial site marking, which is then confirmed by the attending physician. Although not systematized, our service encourages the intern and attending to communicate about proper technique during the procedure itself. For example, attendings ask questions about technique based on evidence in the literature (eg, Why do you replace the stylet in a lumbar puncture needle prior to removal?) or about trouble shooting (eg, What would you do if the flow of ascites stops during this paracentesis?) and also correct any errors in technique (Recall the angle you intended to use based on the ultrasound view).
Patients
Patients are referred to the procedure service by their primary team; referrals are accepted for patients on all services at all levels of care, including the emergency department (ED) and the intensive care unit (ICU). Participants in this study were referred for one of our target procedures (paracentesis, thoracentesis, or lumbar puncture) between November 2008 and July 2009. Patients gave written consent for the supplemental survey independent of consent for the procedure. All consents and procedures were performed in a patient's hospital room and one family member was allowed to stay in the room if desired by the patient. After the completion of the procedure, the attending on the procedure service at the time, which included study authors D.S. and M.M., approached consecutive patients who spoke and read English and were deemed to have capacity to consent for their own procedure to be surveyed. Patients were considered to have capacity to consent based on commonly accepted criteria described in the literature.12, 13 Patients were also excluded if their procedure was performed by the attending alone, if they had repeated procedures done by the service, or if they were too altered or critically ill to participate in the survey.
Survey
Our survey was developed through identification of items reported in the literature,1421 as well as items newly developed for purposes of examining our primary aims. Newly developed questions focused on patients' satisfaction with major aspects of procedure performance as well as the quality and impact of communication with the patient and between members of the team. Two open‐text questions were included to allow patients to share what went well with the procedure as well as areas for improvement. The research team developed a pool of question items for potential inclusion in a patient satisfaction questionnaire. These items were then shown to a group of research‐oriented health professionals, who meet regularly to review academic research protocols. The group provided their opinions about the content and comprehension of the questions, and the written survey employed was a result of their revisions (see Appendix in Supporting Information online).
Written surveys were distributed to patients by the hospitalist attending on service following the procedure as permitted by patients' severity of illness and availability. Surveys were anonymous and self‐administered by the patient or a family member who was in the room for the procedure; all questions were voluntary. A nurse was made responsible for collecting the survey when possible. Survey results were entered into a database without identifiers, with limited demographic information; patient gender, age, and procedure type were included by the attending hospitalist at the end of the survey. A separate and more detailed procedure database was kept of all procedures performed and was used to record patient consent or reason for not consenting as well as documented receipt of a completed survey. This non‐anonymous database contained detailed supplemental information including patient age, level of care, referring service, presence of bloody fluid at any point during the procedure, and physician‐reported immediate complications at the bedside in free text.
Analysis
Reported immediate complications were classified into major and minor based on reported definitions in the literature.2226 Similar to previous studies, major immediate complications were defined as those requiring further procedural intervention, medical therapy, or both.27 Major complications were defined as: bleeding requiring transfusion, pneumothorax requiring a chest tube, respiratory failure, bowel perforation, cerebral herniation or shock, cerebrospinal fluid (CSF) leak requiring intervention, and transfer to a higher level of care. For patients receiving a thoracentesis, chart review was performed to determine the presence of a follow‐up chest x‐ray, the presence of a pneumothorax, or clinical evidence for re‐expansion pulmonary edema. We analyzed differences between respondents and non‐respondents using Chi‐square tests for categorical variables (gender, level of care, referring service, procedure type, bloody fluid, and immediate reported complications) and independent t tests for continuous variables (age).
After review of the open‐ended fields, responses were classified into the following categories: pain control, physician skill, professionalism, communication, symptom relief, procedure duration, and miscellaneous comments. Responses regarding patient perceptions of physician communication were dichotomized into positive (1 = Strongly Agree, 2 = Agree) and negative (3 = Neutral, 4 = Disagree, and 5 = Strongly Disagree), and independent t tests were used to determine the contribution of factors, such as age, while Chi‐square tests were used for the contribution of gender and procedure type. All statistical tests were performed by using the SAS statistical application program (version 9.2).
Results
Respondent Characteristics
Of 324 procedures performed by the HPS during the study period, 95 (29%) were eligible for consent. Of the 229 patients not eligible for consent, 32 (10%) were excluded because the procedure was performed by the attending alone, 76 (23%) lacked English proficiency or literacy, 66 (20%) had altered mental status, 32 (10%) were intubated and/or had severe illness precluding consent, and 23 (7%) were repeat procedures on patients who had previously completed the survey. Only two patients specifically requested an attending to perform the procedure after an introduction to the service. Of the 95 patients eligible for consent, 89 were consented for the survey, and 65 (68%) completed the survey. Of the six eligible, non‐consented patients, all were leaving the floor immediately following the procedure, and time did not allow for consent and survey distribution. There were no differences between eligible responders and nonresponders in age, gender, procedure, requesting service, presence of bloody fluid, or physician‐reported immediate complications (Table 1).
| Demographics | Respondera (n = 65) | Nonresponder (n = 24) |
|---|---|---|
| ||
| Age, y [mean (SD)] | 55.4 (15.7) | 50.4 (17.4) |
| Male gender, n (%) male | 41 (63.1) | 11 (45.8) |
| Procedure, n (%) | ||
| Paracentesis | 31 (47.7) | 10 (41.7) |
| Thoracentesis | 17 (25.8) | 6 (25.0) |
| Lumbar puncture | 15 (22.7) | 7 (29.2) |
| Arthrocentesis | 2 (3.0) | 1 (4.2) |
| Patient location, n (%) | ||
| Floor | 47 (72.3) | 19 (79.2) |
| Step down/telemetry | 17 (26.1) | 3 (12.5) |
| Intensive care unit | 1 (1.5) | 2 (8.3) |
| Service requesting, n (%) | ||
| Medicine | 29 (44.6) | 10 (41.7) |
| Cardiology | 6 (9.1) | 3 (12.5) |
| Liver transplant | 20 (30.3) | 7 (29.2) |
| Bone marrow transplant | 7 (10.6) | 1 (4.2) |
| Surgery | 0 | 1 (4.2) |
| Neurosurgery | 1 (1.5) | 1 (4.2) |
| Other | 2 (3.0) | 1 (4.2) |
| Reported presence of bloody fluid at any point in the procedure, n (%) | 9 (13.6) | 4 (16.7) |
| Other reported immediate complications | ||
| Equipment malfunction | 2 (3.0) | 1 (4.2) |
| Significant cough/pleuritic pain | 1 (1.5) | 1 (4.2) |
| Transient oxygen desaturation | 1 (1.5) | 0 |
| Ascites leak | 0 | 0 |
| Hematoma | 0 | 0 |
| Persistent bleeding | 0 | 0 |
| Transfer to a higher level of care | 0 | 0 |
Complications
As complications would likely play a role in procedure satisfaction, we describe immediate complications for the study population. Of the 324 procedures performed during the study period, no patient had predefined major immediate complications. Upon further chart review of the 96 patients that had a thoracentesis performed, all had a follow‐up chest x‐ray and none suffered an iatrogenic pneumothorax or re‐expansion pulmonary edema. Minor immediate complications for the 324 procedures were reported as follows: postprocedure pain in four patients (1.2%), cough in nine patients (2.8%), five equipment malfunctions (1.5%), four ascites leaks (1.2%), and one incisional bleed requiring a suture for hemostasis (0.3%). There was no significant difference in complications between those consented for the survey and the total study population.
Procedure Satisfaction
More than 90% of patients were satisfied or very satisfied with most aspects of the procedure, including the informed consent process, pain control, expertise, and courtesy of physicians (Table 2). The percentage of patients satisfied with the duration of procedure (88%) was lower than for other measures of satisfaction. Of the 38 patients receiving therapeutic procedures, 34 (89%) were satisfied or highly satisfied with the improvement in symptoms following the procedure.
| Very Satisfied and Satisfied No. (%) | Neutral No. (%) | Dissatisfied and Very Dissatisfied No. (%) | N/A No. (%) | |
|---|---|---|---|---|
| Your overall procedure experience | 65 (100) | 0 (0) | 0 (0) | 0 (0) |
| Explanation of the procedure, risks, and benefits before the procedure | 64 (99) | 1 (2) | 0 (0) | 0 (0) |
| Pain control during the procedure | 60 (92) | 5 (8) | 0 (0) | 0 (0) |
| Expertise/skill of the physicians performing your procedure | 62 (95) | 3 (5) | 0 (0) | 0 (0) |
| Courtesy and bedside manner of the physicians performing your procedure | 65 (100) | 0 (0) | 0 (0) | 0 (0) |
| The time it took to perform your procedure | 57 (88) | 6 (9) | 0 (0) | 2 (3) |
| Improvement in your symptoms following this procedure, if applicable | 34 (52) | 7 (11) | 0 (0) | 24 (37) |
When asked what went well with the procedure, 59 (91%) respondents provided additional comments and feedback. Each response was classified as described in the Methods section. Of the free text responses, 8 of the 59 patients (14%) commented on the attention to pain control (eg, The caring and attention to my pain was most important to me), 5 (8%) on the skills of the operators (Great examination of the entire stomach region with the ultrasound to ensure the best position of the catheter), 6 (10%) on the courtesy and professionalism of the team (eg, Courteous, team‐feeling, addressed my concerns), 9 (15%) on their communication with the team (eg, The doctors made me feel very comfortable before the procedure by laying out the plan and explaining each part of the procedure), and 8 (14%) on relief of their symptoms (eg, There was an almost immediate and significant improvement in my breathing, bloating, and pain). Twenty‐three of the 59 comments (39%) were categorized as miscellaneous (eg, All went great. I fell asleep).
When asked areas for improvement, 55 (85%) patients responded. Thirty‐three patients (60%) reported that nothing could be improved or they instructed the team to just keep doing what you are doing, while 22 (40%) patients expressed a concern. Responses were categorized in a similar fashion to the positive responses. Five of the 22 negative comments (23%) reported that the procedure took too long (eg, Procedure could have been shorter. I got tired sitting up), 4 (18%) commented on pain control (eg, The poke for marking my skin hurt more than the anesthetic. I was surprised), 6 (27%) felt communication was a problem (eg, Discuss the steps with the patient audibly, no whispering, speak clearly), and 7 (32%) had miscellaneous concerns (eg, Try not to do this procedure right after another one).
Physician Communication
Sixty‐four patients (98%) reported that the physicians performing their procedure communicated with each other during the procedure (Table 3). Although one patient did not feel that the physicians communicated with each other, he or she still answered the follow‐up questions regarding perceptions of physician communication. We excluded this patient from our analysis as his or her answers may not be reliable. The majority of patients (84%) reported this communication as reassuring and felt it was a normal part of procedure performance (94%). Those that did not agree that physician communication was reassuring did not differ in average age (P = 0.307), gender (P = 0.511), or procedure type (P = 0.562).
| Strongly Agree and Agree No. (%) | Neutral No. (%) | Disagree, and Strongly Disagree No. (%) | |
|---|---|---|---|
| I felt that the physicians talking to each other about my procedure was reassuring to me | 54 (84) | 10 (16) | 0 (0) |
| Physicians talking to each other while doing a procedure is a normal part of doing a procedure | 60 (94) | 4 (6) | 0 (0) |
Of all positive and negative comments, five specifically addressed communication between physicians. Most (four) reflected satisfaction with bedside teaching (eg, They discussed the procedure in a professional manner and eased my mind at all times) and with having an expert in the room (eg, [The team] discussed things like needle placement, which was nice because there was a second opinion right there in the room). Patients also felt that it was good to experience the teaching, with one patient reporting that the best part of the procedure was watching doctors learn from each other. Patients did not express specific reservations about bedside teaching, resident technique, or fear of complications in free text.
Discussion
Even though novice interns performed procedures and simultaneous bedside teaching, patient satisfaction with a teaching procedure service was high, and reported complication rates were low. In addition, a majority of patients found discussions related to teaching activities reassuring and potentially important to their perception of care quality. Analogous studies examining patient satisfaction with endoscopic care found similar rates of patient satisfaction with endoscopists' bedside manner, technical skills, and pain control, but these studies included sedated patients.21 Our results are unique, as we evaluated awake patients with attention to perception of bedside teaching with novice interns.
Our findings offer an alternative strategy for bedside procedural teaching that employs transparency in the use of an expert and a trainee to introduce patients to bedside teaching by experts, which is not common at many academic medical centers.28 Patients may have been reassured by a clear explanation of the role of the service and the providers involved as well as an assurance of expertise and attention to patient comfort and safety. In addition to patient satisfaction, this model has the potential to impact both the safety of bedside procedures and housestaff education around procedure performance. For example, pneumothorax rates using our procedure service model are lower than those published (0% vs. 4% for ultrasound‐guided thoracentesis and 8.5% for thoracentesis by less experienced clinicians).29
Providers may be reluctant to teach at the bedside of awake patients for fear of heightening patient anxiety over trainee inexperience. In the 1960s similar fears were raised over the concern for patient anxiety with bedside rounding,30 but later studies revealed these concerns to be largely unfounded. Instead, bedside rounds have been shown to positively influence patients' feelings about their hospital experience and their relationships with their physicians compared with patients whose case presentations were made in a conference room.31, 32 Given the opportunity to comment on areas for improvement, patients in our study specifically elaborated regarding pain control, communication, and efficiency problems. Although 16% of patients did not find the communication of physicians reassuring, none of the negative comments reflected problems with bedside teaching, but rather concepts such as desiring a better explanation of steps throughout the procedure. Specifically, patients desire better communication for unanticipated pain.
There are several limitations to this study. Lack of patient satisfaction data from a control group of patients whose procedures were performed by attendings or housestaff alone limits our ability to draw conclusions about our satisfaction scores. The scarce applicable literature offers only imperfect comparison data. Because hospitalists were not blinded to the survey, attending behavior may have been subject to a Hawthorne effect.33 Consenting patients after the procedure could have provided hospitalists with an opportunity to exclude patients who appeared less satisfied with their procedure; however, attempts were made to prevent this behavior by requiring strict accounting of why a patient was not consented for the study. Use of alternative personnel for consent such as nurses was explored, but was found not to be feasible due to limited resources. These data are only applicable to English‐speaking patients who are literate and well enough to complete a survey. It is not clear whether the experience for other patients would reflect the same outcomes. It is plausible that non‐English‐speaking patients might have more concerns about incomprehensible conversations taking place during their procedure. Although the surveys were anonymous and patients were told that the proceduralists would not see individual responses, responses may have been biased out of patient concern that their response might affect their care. Hospitalists obtaining consent, however, were careful to stress anonymity and the distinction between the primary team and the procedure team.
Academic hospitals are struggling with providing quality procedural care while balancing housestaff education and experience.28 With hospitalists playing an increasingly prominent role in housestaff education and patient satisfaction initiatives, the supervision of housestaff by trained hospitalist faculty may help meet both aims in the performance of invasive bedside procedures, particularly at institutions where simulation training resources are limited. Although concern may exist for potential patient anxiety with bedside teaching, our data demonstrate high levels of patient satisfaction with a hospitalist procedure service despite novice procedure performers and an emphasis on teaching during the procedure.
- ,,, et al.Creation of an innovative inpatient medical procedure service and a method to evaluate house staff competency.J Gen Intern Med.2004;19(5 Pt 2):510–513.
- ,,, et al.Impact of a bedside procedure service on general medicine inpatients: A firm‐based trial.J Hosp Med.2007;2(3):143–149.
- Hospital Care Quality Information from the Consumer Perspective (HCAHPS).Quality Assurance Guidelines.Baltimore, MD:Centers for Medicare 113(8):657–662.
- ,,,,.The effect of bedside case presentations on patients' perceptions of their medical care.N Engl J Med.1997;336(16):1150–1155.
- ,,,.‘Sorry, it's my first time!’ Will patients consent to medical students learning procedures?Med Educ.2005;39(4):365–369.
- ,.Ethical considerations surrounding first time procedures: a study and analysis of patient attitudes toward spinal taps by students.Kennedy Inst Ethics J.1992;2(3):217–231.
- ,,,.Patients' willingness to allow residents to learn to practice medical procedures.Acad Med.2004;79(2):144–147.
- ,,.Patient satisfaction with gynecologic care provided by family practice resident physicians.Fam Pract Res J.1991;11(4):421–428.
- ,,.Resident participation in flexible sigmoidoscopy does not affect patient satisfaction.Am J Gastroenterol.2000;95(6):1563–1566.
- ,.Bedside ultrasound for difficult lumbar puncture.J Emerg Med.2005;28(2):197–200.
- ,.Conducting the Assessment. In:Assessing Competence to Consent to Treatment: A Guide for Physicians and Other Health Professionals.First Edition ed.New York, NY:Oxford University Press;1998:80–91.
- ,.Care of Ill, Socially Complicated Patients. In:Medical Management of Vulnerable 2007:407–418.
- ,,,,.Interventional radiologic procedures: patient anxiety, perception of pain, understanding of procedure, and satisfaction with medication‐‐a prospective study.Radiology.2000;215(3):684–688.
- ,,,,.Improving the assessment of (in)patients' satisfaction with hospital care.Med Care.2001;39(3):270–283.
- ,,,.Factors determining inpatient satisfaction with care.Soc Sci Med.2002;54(4):493–504.
- ,,,.Reliability and validity of the Satisfaction with Hospital Care Questionnaire.Int J Qual Health Care.2002;14(6):471–482.
- ,,,,.A randomized trial of four patient satisfaction questionnaires.Med Care.2003;41(12):1343–1352.
- ,,, et al.Development and validation of an in‐patient satisfaction questionnaire.Int J Qual Health Care.2005;17(6):465–472.
- ,,,.Central venous port catheters: evaluation of patients' satisfaction with implantation under local anesthesia.J Vasc Access.2009;10(1):27–32.
- ,,,.Factors influencing patient satisfaction when undergoing endoscopic procedures.Gastrointest Endosc.2009;69(4):883–91, quiz 891.e1.
- ,,, et al.Complications associated with thoracentesis. A prospective, randomized study comparing three different methods.Arch Intern Med.1990;150(4):873–877.
- ,,, et al.Risk of complications after abdominal paracentesis in cirrhotic patients: a prospective study.Clin Gastroenterol Hepatol.2009;7(8):906–909.
- ,,, et al.Performance standards for therapeutic abdominal paracentesis.Hepatology.2004;40(2):484–488.
- ,,,,.Lumbar puncture: its indications, contraindications, complications and technique.Rev Neurol.2007;45(7):433–436.
- .How to perform a lumbar puncture with the patient in the seated position.Br J Hosp Med (Lond).2006;67(3):M46–7.
- ,,.Are commonly used resident measurements associated with procedural skills in internal medicine residency training?J Gen Intern Med.2007;22(3):357–361.
- ,,,MERN Group,.Supervising the Supervisors‐Procedural Training and Supervision in Internal Medicine Residency.J Gen Intern Med.2010.
- ,,,.Pneumothorax following thoracentesis: a systematic review and meta‐analysis.Arch Intern Med.2010;170(4):332–339.
- ,,.The emotional impact of ward rounds.J Mt Sinai Hosp NY.1956;23(6):782–803.
- ,,,.The physiologic and psychological effects of the bedside presentation.N Engl J Med.1989;321(18):1273–1275.
- ,,,,.The effect of bedside case presentations on patients' perceptions of their medical care.N Engl J Med.1997;336(16):1150–1155.
- .Hawthorne effects and research into professional practice.J Eval Clin Pract.2001;7(1):65–70.
- ,,, et al.Creation of an innovative inpatient medical procedure service and a method to evaluate house staff competency.J Gen Intern Med.2004;19(5 Pt 2):510–513.
- ,,, et al.Impact of a bedside procedure service on general medicine inpatients: A firm‐based trial.J Hosp Med.2007;2(3):143–149.
- Hospital Care Quality Information from the Consumer Perspective (HCAHPS).Quality Assurance Guidelines.Baltimore, MD:Centers for Medicare 113(8):657–662.
- ,,,,.The effect of bedside case presentations on patients' perceptions of their medical care.N Engl J Med.1997;336(16):1150–1155.
- ,,,.‘Sorry, it's my first time!’ Will patients consent to medical students learning procedures?Med Educ.2005;39(4):365–369.
- ,.Ethical considerations surrounding first time procedures: a study and analysis of patient attitudes toward spinal taps by students.Kennedy Inst Ethics J.1992;2(3):217–231.
- ,,,.Patients' willingness to allow residents to learn to practice medical procedures.Acad Med.2004;79(2):144–147.
- ,,.Patient satisfaction with gynecologic care provided by family practice resident physicians.Fam Pract Res J.1991;11(4):421–428.
- ,,.Resident participation in flexible sigmoidoscopy does not affect patient satisfaction.Am J Gastroenterol.2000;95(6):1563–1566.
- ,.Bedside ultrasound for difficult lumbar puncture.J Emerg Med.2005;28(2):197–200.
- ,.Conducting the Assessment. In:Assessing Competence to Consent to Treatment: A Guide for Physicians and Other Health Professionals.First Edition ed.New York, NY:Oxford University Press;1998:80–91.
- ,.Care of Ill, Socially Complicated Patients. In:Medical Management of Vulnerable 2007:407–418.
- ,,,,.Interventional radiologic procedures: patient anxiety, perception of pain, understanding of procedure, and satisfaction with medication‐‐a prospective study.Radiology.2000;215(3):684–688.
- ,,,,.Improving the assessment of (in)patients' satisfaction with hospital care.Med Care.2001;39(3):270–283.
- ,,,.Factors determining inpatient satisfaction with care.Soc Sci Med.2002;54(4):493–504.
- ,,,.Reliability and validity of the Satisfaction with Hospital Care Questionnaire.Int J Qual Health Care.2002;14(6):471–482.
- ,,,,.A randomized trial of four patient satisfaction questionnaires.Med Care.2003;41(12):1343–1352.
- ,,, et al.Development and validation of an in‐patient satisfaction questionnaire.Int J Qual Health Care.2005;17(6):465–472.
- ,,,.Central venous port catheters: evaluation of patients' satisfaction with implantation under local anesthesia.J Vasc Access.2009;10(1):27–32.
- ,,,.Factors influencing patient satisfaction when undergoing endoscopic procedures.Gastrointest Endosc.2009;69(4):883–91, quiz 891.e1.
- ,,, et al.Complications associated with thoracentesis. A prospective, randomized study comparing three different methods.Arch Intern Med.1990;150(4):873–877.
- ,,, et al.Risk of complications after abdominal paracentesis in cirrhotic patients: a prospective study.Clin Gastroenterol Hepatol.2009;7(8):906–909.
- ,,, et al.Performance standards for therapeutic abdominal paracentesis.Hepatology.2004;40(2):484–488.
- ,,,,.Lumbar puncture: its indications, contraindications, complications and technique.Rev Neurol.2007;45(7):433–436.
- .How to perform a lumbar puncture with the patient in the seated position.Br J Hosp Med (Lond).2006;67(3):M46–7.
- ,,.Are commonly used resident measurements associated with procedural skills in internal medicine residency training?J Gen Intern Med.2007;22(3):357–361.
- ,,,MERN Group,.Supervising the Supervisors‐Procedural Training and Supervision in Internal Medicine Residency.J Gen Intern Med.2010.
- ,,,.Pneumothorax following thoracentesis: a systematic review and meta‐analysis.Arch Intern Med.2010;170(4):332–339.
- ,,.The emotional impact of ward rounds.J Mt Sinai Hosp NY.1956;23(6):782–803.
- ,,,.The physiologic and psychological effects of the bedside presentation.N Engl J Med.1989;321(18):1273–1275.
- ,,,,.The effect of bedside case presentations on patients' perceptions of their medical care.N Engl J Med.1997;336(16):1150–1155.
- .Hawthorne effects and research into professional practice.J Eval Clin Pract.2001;7(1):65–70.
Copyright © 2011 Society of Hospital Medicine
Business Case for an Electronic Discharge Summary
Delivering the highest possible quality of care is among the top priorities of all medical centers. That said, any quality innovation must be seen as adding value from a variety of perspectives. Especially in the current economic climate, a sound business case is paramount to the advancement of any quality innovation. Given the nature of their work, hospitalists are ideally suited to undertake system improvement innovations. To assist hospitalists in successfully implementing quality and safety initiatives, we have designed a framework of elements required for a business case. We describe our experience developing and implementing an electronic discharge summary and utilize a structured framework to articulate the business case for its implementation.
Defining a Business Case Framework
A business case is a structured proposal outlining the qualitative and quantitative factors that justify a course of action. An effective business case for a quality improvement initiative articulates how both factors are aligned with preexisting organizational goals. In modeling the business case framework for the electronic discharge summary, Figure 1 outlines the qualitative and quantitative costs and benefits that can affect institutional decision making.
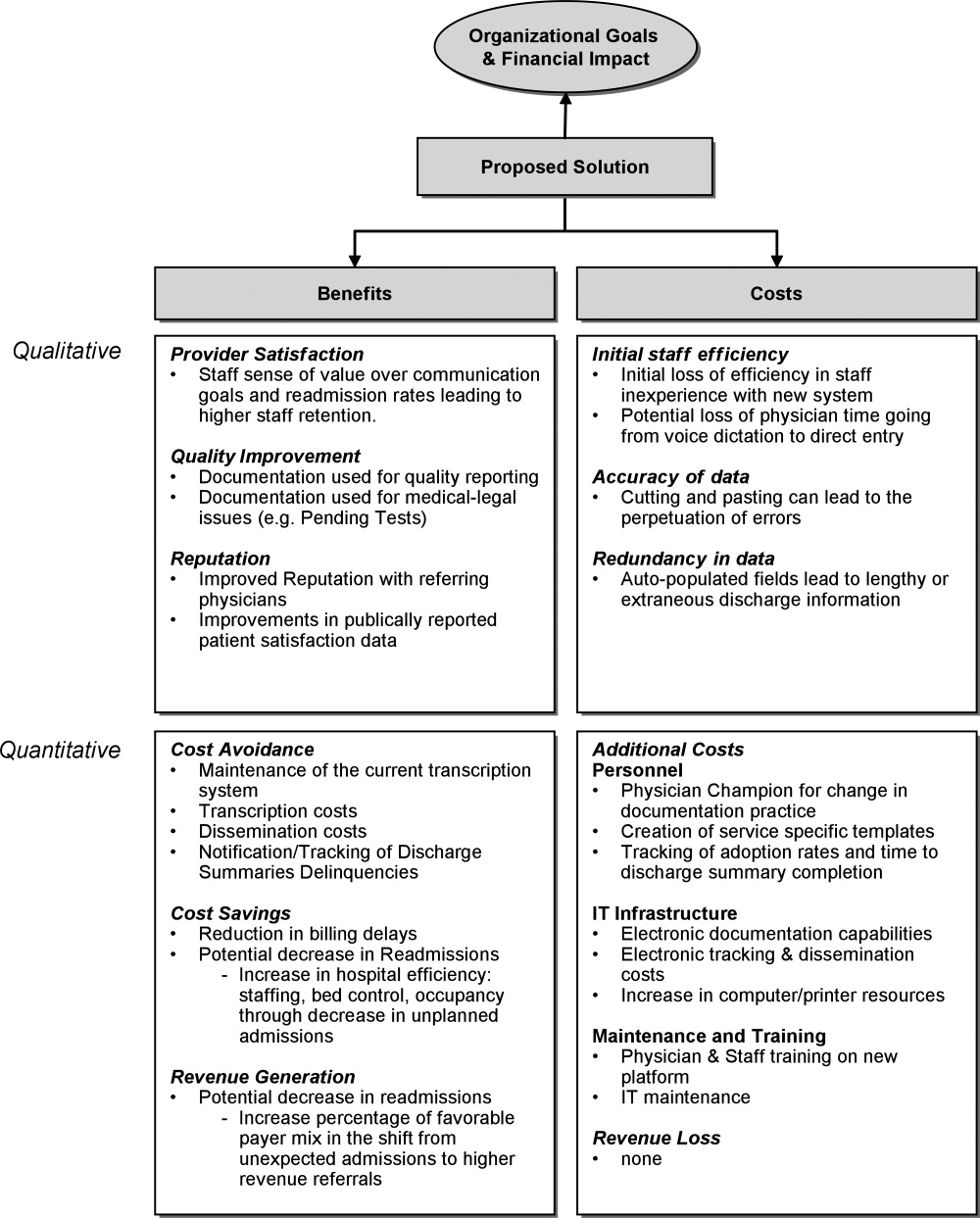
Organizational Aims and Financial Impact: Determining Costs and Benefits
Organizational goals drive decision making and resource allocation at all levels. As priorities change with time, understanding which predominate in an organization will be essential to building a business case. Institutions may be more willing to adopt expensive innovations if they are justified by progress toward the qualitative organizational goals. Figure 1 demonstrates several institutional goals both qualitative (provider satisfaction, quality improvement, and institutional reputation) and quantitative (cost avoidance, cost savings, and revenue generation) that could drive the decision making for an electronic discharge summary. After examining how an initiative aligns with institutional aims, the next step is to weigh the benefits against the potential costs. Costs in our example include not only the quantitative financial investment in information technology (IT) infrastructure, personnel and maintenance, but also may include qualitative costs such as loss of staff efficiency and redundant documentation. Costs and savings will be geographically variable and depend on the institutional framework, eg, the existing system for medical records, institutional patient payer mix, type of payment structure (global vs. utilization based*), and reimbursement rates. While it may be impractical to account for every cost and savings resulting from the project implementation, every effort should be made to account for the key variables that make up the cost‐benefit calculation.
The Business Case for an Electronic Discharge Summary at University of California San Francisco (UCSF)
Current State of Discharge Documentation a UCSF
UCSF Medical Center is a 600‐bed quaternary care academic institution that discharges approximately 100 patients per day. Our hospital discharge summary is used to document a patient's hospital course and post discharge plan, information necessary for continued care in the outpatient setting. Literature supports the potential for timely and relevant discharge summaries to improve care transitions, clinician satisfaction, and resource use.1 In 2008, however, the majority of our discharge summaries were completed greater than 14 days post discharge, in accordance with national practice.2 Despite Centers for Medicare & Medicaid Services (CMS) and the Joint Commission discharge summary standards regarding content,3, 4 most discharge summaries are composed using freeform dictation.2 Consequently, discharge summaries often lack critical information,57 and may not reach the correct outpatient provider in a timely manner.5, 811
Our Proposed Solution: E‐Discharge
As hospitals are increasingly implementing electronic medical records (EMR),12 there is a growing opportunity to efficiently and reliably incorporate information from the medical record into electronic or database assisted discharge materials. At UCSF the need to develop a system to document and communicate tests pending at discharge fueled the development of an electronic discharge summary. UCSF's vendor‐supplied EMR lacks the ability to integrate electronic patient data into a progress note or discharge summary in a manner usable for physicians. Instead physicians are required to use a telephone voice dictation system, which is subsequently transcribed to text within 1 to 3 days. A separate software platform tracks attending signature of the transcribed text and automatically triggers dissemination through computerized fax and campus mail. The turnaround time for a discharge summary can be as long as 3 weeks. With the time involved and high cost of implementing new or more sophisticated versions of EMR, we chose to design a solution that would improve care for our patients in a more immediate and cost neutral fashion. Our goal was to create an affordable, electronic, systematized solution to produce both timely and relevant discharge summaries, in the hopes of improving communications with providers and thus patient outcomes.
In earlier work, UCSF developed UCSF Note Writer, a template‐based documentation tool that uses web service to import data from the underlying database for provider documentation.13 As a standardized template has been shown to improve quality of communication to both patients and referring providers,1, 14, 15 we developed a template in UCSF Note Writer with both free text and auto‐populated fields for a discharge summary based on current guidelines.1619 We encouraged the documentation of medication changes, changes in functional status and pending tests.
The adoption of such an electronic format has also been shown to improve the efficiency of discharge documentation over conventional dictation and transcription.1, 2022 While this change may be institution dependent, we employed strategies such as allowing the discharge summary to be initiated and updated throughout the hospital admission and unifying the discharge summary with the last day's progress note to facilitate timeliness. To promote efficiency, we allowed providers to import pertinent labs, microbiology, and in the future, the importation of pending tests. While the electronic format in itself does not promote timeliness, it incorporates the discharge summary into physician daily workflow and enables efficiency in data gathering and transfer. For outpatient providers who can access the EMR, any delay or potential fault in the delivery of the discharge materials is eliminated, while outside providers can receive copies through other rapid and reliable modes of electronic delivery (eg, EMR inbox notification) with an appropriate infrastructure.
Application of the Business Framework to the Case for an Electronic Discharge
Considering the potential improvements in care delivery, the argument for an electronic discharge summary may seem self‐evident. To realize its implementation, however, it is necessary to consider other aspects of organizational decision making. We employed the following structure to articulate a robust and sound business case for e‐discharge.
Qualitative Benefits
Quality and Safety
Publically reported data are often derived from hospital chart abstraction and may impact accreditation, reputation, and pay for performance programs.18, 23, 24 The discharge summary is a readily available source of information regarding discharge medications, patient instruction, and communication regarding pending tests. As such, its quality should be a priority for hospital decision makers. Electronic discharge summaries have the potential to reduce adverse events in the high‐risk post‐hospitalization period.1, 25 As such they may improve outpatient physicians' ability to deliver relevant care, reduce preventable readmissions26 and reduce malpractice vulnerability27all key drivers in organizational decision making.
Patient Satisfaction
Patients want to feel prepared for discharge by understanding the continuity of their care from the hospital to the outpatient setting. Discharge preparedness, commonly queried and reported in national patient satisfaction surveys, is low.28 Many electronic discharge summary platforms allow for translation into tailored patient instructions available to the patient in real time, helping to ensure that patients receive quality discharge education.29
Referring Physician Satisfaction
Poor discharge communication reduces referring physicians' satisfaction, which may discourage them from referring patients to the hospital or organization, having broader financial implications.25, 30 Even for medical centers with a busy emergency department, outpatient physician referrals and recommendations make up over 50% of an institution's admissions.31 An electronic discharge summary available in the EMR at the time of discharge, electronically transmitted to referring providers can impact the referral patterns of community physicians.
Readmission
Now publicly reported, readmission rates are another benchmark by which to judge hospital care.32 Patients with discharge summaries that are unavailable to outpatient providers, a very common occurance,2 have a higher trend toward readmission.26 Improved quality of care at the time of discharge resulting in fewer readmissions will better position hospitals to contend with potential Medicare reforms.
Quantitative Benefits
IT Infrastructure: Transcription, Deficiency Tracking, Dissemination
Hospitals, including UCSF, use internal or external transcriptionists to transcribe dictated recordings into typed text at a substantial cost to large medical centers. Medical records staff also track both discharge summary completion and their dissemination to referring providers in compliance with regulatory mandates.4, 33 The use of electronic documentation that relies on physician‐direct entry and that automates dissemination and tracking of discharge documentation provides a potential cost savings to offset the costs of a new system. UCSF Medical Center discharges 100 patients per day and could conservatively avoid almost $500,000 in transcription costs annually (Text Box 1).34
Text Box 1
UCSF Transcription costs:
Average cost/line for transcribed text: $0.17
Average Lines in a discharge summary: 80
# pts discharged/day: 100
Yearly costs = $496,400
Billing
Delays in completion of discharge summaries result in billing delays when critical information required for coding is in the discharge summary. Deferred payment on long admissions can reach tens of thousands of dollars, representing a significant strain on medical center finances. Comprehensive electronic discharge materials may simplify coding through careful documentation and improve billing efficiency through rapid completion.
At our medical center, approximately 20% of billing is delayed due to incomplete discharge documentation. For a hospital that generates over $1.4 billion dollars in billing revenue per year, this can translate into significant financial losses. Hospitals may have to borrow money or draw from existing resources to cover operative deficits created by a delay in the receipt of large payment. Lenders charge approximately 1% to 2% annual interest rate, which translates into 0.2% to 0.4% in billed costs that the hospital gives away to their lenders. Hospitals would be well served by eliminating delays in billing to improve revenue flow (Text Box 2).
Text Box 2
UCSF Annual revenue: $1.4 Billion
Billing that requires discharge summary completion: 20%
Lender's interest rate: 12%
Lenders interest rate (12%) on delayed billing (20%) = 0.20.4% of total revenue
Assuming a 14 day delay in billing: 0.20.4% of total revenue ($1,400,000,000) for 14/365 days = $107,000$215,000
Qualitative Costs
Efficiency and Physician Time
Implementation of any new system is likely to result in initial diminished efficiency. If patient volume is stable, this may not translate into loss of revenue, but rather cause staff to change their workflow. For example, given the new inefficiency in charting, staff may spend less time on direct patient care tasks (Intravenous Catheter placement, FT placement, patient education, discharge instructions), thus increasing the qualitative costs to implementing the system.
To minimize these costs, we used a step wise phased role out starting with one pilot team, with a plan to expand to multiple teams prior to implementation on the entire medicine service. This allowed for the creation of one central and several ancillary physician champions to troubleshoot the new system to help minimize productivity losses. One of the largest concerns in the switch from voice dictation to physician‐direct entry into an electronic summary is the cost of physician time. System adjustments through several pilots helped ensure that the time investment of a novice user was not significantly greater than time previously spent dictating.
Quality of Documentation
Unanticipated consequences from a switch to an electronic platform must be considered, such as the possibility of longer more redundant discharge summaries. The amount of information available for automated import will vary by institutional preference, but the recipient's access to the EMR, primary physician preference, and technologic capabilities should be considered. At UCSF we made an effort to distill the information most important to subsequent care, disabling the importation of multiple days of radiology data and instead working to create a system for discharge medication importation. As with any electronic document, the medium also lends itself to cutting and pasting, which may lead to anachronistic information carried forward from hospital progress notes earlier in the stay.35, 36 The largest experience with this unintended consequence can be found in the Veteran's Affairs Health System EMR, which found that 9% of progress notes studied contained copied or duplicated text.37 The authors recommended that clear policies, programs to raise practitioner awareness, and the development of monitoring procedure be implemented coincident with electronic note‐writing capabilities.
Quantitative Costs
Quantitative Costs will be highly variable across institutions, geographical areas, and software platforms as the infrastructure of existing EMRs are highly variable. The cost of implementation depends heavily on whether inpatient documentation (and thus discharge documentation) is a feature of an institutional EMR, or whether a stand‐alone discharge documentation infrastructure is needed. An explanation of the differences between these types of EMRs and the importance to the cost of infrastructure implementation is further described in the following section. Rather than providing a direct accounting of costs, we have provided a tabular summary of costs that should be considered with the adoption of an electronic discharge summary based on the type of institutional EMR (Table 1).
| Voice Dictation | E‐Discharge in an EMR With Inpatient Documentation Abilities | E‐Discharge in an EMR Without Inpatient Documentation Abilities | |
|---|---|---|---|
| |||
| Infrastructure | |||
| Software | + | ||
| Hardware (sufficient computers and printers) | + | + | |
| Network connectivity | + | + | |
| Server capacity for system backup | + | + | |
| Interface with current EMR | + | ||
| Personnel | |||
| Physician champion | + | + | |
| Physician training | + | + | |
| Computer programmer | + | + | |
| Transcription | + | ||
| Deficiency tracking | + | ||
| Dissemination | + | ||
| Maintenance | |||
| Computer/printer maintenance | + | + | |
| Network maintenance | + | + | |
| Software add‐ons and updates | + | + | + |
Infrastructure
For most health care organizations, the transition to an EMR includes adoption of results reporting systems and computerized provider order entry; only a more select group of hospitals with a complete EMR electronically document inpatient care (eg, progress notes) through physician direct entry. While there is substantial literature regarding the benefits and pitfalls of adopting computerized order entry (CPOE),38, 39 there is less attention devoted to the costs of implementing large‐scale electronic documentation, including an electronic discharge summary, as opposed to paper notes or dictation.4042 Institutions using an EMR with electronic care documentation capability have already invested in the infrastructure to implement electronic discharge documentation, and can employ it at a modest cost. For these institutions, the infrastructure cost of the transition from paper charting or dictation to direct entry by physicians lies in ensuring sufficient computers and connectivity to handle the increased computer use. On the other hand, for those institutions where the EMR lacks this capability there are few freestanding documentation platforms available for purchase. The cost of implementing such a system is high, both for the purchase of additional software and the integration of that software in to the EMR supplied by the primary vendor. Other notable infrastructure costs to consider are ensuring sufficient network connectivity, computers and printers to accommodate increased use that will come with electronic note writing as well as server support for system backups.
Personnel
Engaging the right personnel will smooth the implementation of an electronic discharge summary. In addition to dedicated user training sessions, a physician champion who can promote and monitor user training on the new platform will facilitate prompt implementation. An IT support programmer should work with the physician champion to address concerns and troubleshoot problems. Additional personnel may also be needed to track progress in discharge summary adoption, quality and efficiency. Ideally these personnel can be funneled from those who work transcribing, disseminating and tracking completion of discharge summaries, positions that will be needed in a reduced capacity.
Maintenance
Increased IT infrastructure also means increased IT maintenance and upgrades of servers, network connectivity, computers and printers. Discussions with vendors regarding costs of maintenance, upgrades and add‐on features should be considered when adopting an electronic discharge summary platform.
Conclusion
While many QI initiatives have the potential to improve clinical care, resource limitations and competing priorities necessitate that hospital decision makers see the value of hospitalist driven improvements. A sound business case is the key to successfully influencing decision making and furthering necessary innovations. We have detailed the elements of a business case and applied them to a proposed innovationthe electronic discharge summary. While the cost of multifunctional EMR with full electronic care documentation may be impossible to implement given high initial costs and competing priorities, investing in an e‐discharge solution has real‐time benefits in the impact on patients, system improvements, qualitative benefits, and return on investment. Being able to articulate key qualitative and quantitative elements creates a sound business case that can be applied to QI initiatives in general, and assist hospitalists in garnering support and resources to continue to improve care.
Acknowledgements
The authors acknowledge Kathleen Kerr and the members of the BOOST collaborative for helping with background research and in creating the impetus for this work.
Global payments are fixed‐dollar payments for the care that patients may receive in a given time period, such as a month or year, whereas utilization based payments are payments based on the use of diagnostic and treatment modalities (eg, CT scans and blood cultures).
- ,,, et al.Creating a better discharge summary: Improvement in quality and timeliness using an electronic discharge summary.J Hosp Med.2009;4(4):219–225.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- Standard IM.6.10Hospital Accredidation Standards. In: Oakbrook Terrace,IL:Joint Commission Resources;2006:338–340.
- .Medical Record Services, Section 482.24. In: MacDonald I, ed.The CMS Hospital Conditions of Participation.First edition.United States:Hc Pro Inc.;2005:24–25.
- .Hospital discharge and death communications.Br J Hosp Med.1989;42(1):59–61.
- ,,,.Hospital discharge reports: content and design.Br Med J.1975;4(5994):443–446.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143(2):121–128.
- .Delayed communication between hospitals and general practitioners: where does the problem lie?BMJ.1988;297(6640):28–29.
- .Study of “discharge communications” from hospital.Br Med J (Clin Res Ed).1986;293(6557):1283–1284.
- ,.Quality assessment of a discharge summary system.CMAJ.1995;152(9):1437–1442.
- ,,,.General practitioner‐hospital communications: a review of discharge summaries.J Qual Clin Pract.2001;21(4):104–108.
- .Stimulus bill spurs plans for rapid IT progress.Manag Care.2009;18(2):5–6.
- ,,, et al. UCSF Notewriter. Copyright Regents of the University of California.2006–year="2010"2010.
- ,,,,.Assessing quality and efficiency of discharge summaries.Am J Med Qual.2005;20(6):337–343.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,.What is necessary for high‐quality discharge summaries?Am J Med Qual.1999;14(4):160–169.
- ,,,,.Outpatient physicians' satisfaction with discharge summaries and perceived need for an electronic discharge summary.J Hosp Med.2006;1(5):317–320.
- ,.Are general practitioners satisfied with electronic discharge summaries?HIM J.2007;36(1):7–12.
- ,,,.Dictated versus database‐generated discharge summaries: a randomized clinical trial.CMAJ.1999;160(3):319–326.
- ,,,.Evaluation of computer generated neonatal discharge summaries.Arch Dis Child.1991;66(4 Spec No):433–436.
- ,,,,,.Evaluation of a computer‐generated discharge summary for patients with acute coronary syndromes.Br J Gen Pract.1998;48(429):1163–1164.
- The Common Wealth Fund. Why not the best org. Available at: http/www.whynotthebest.org. Updated 2009. Accessed May2010.
- ,.Pay for performance: an overview of the literature.Am J Med Qual.2009;24(2):140–163.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170(3):345–349.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17(3):186–192.
- ,,, et al.Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims.Ann Intern Med.2006;145(7):488–496.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43(3):246–255.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20(4):317–323.
- ,,.Referring physician satisfaction: toward a better understanding of hospital referrals.J Hosp Mark.1998;12(2):95–111.
- U.S. Department of Health 7(3):269–272.
- .IT vulnerabilities highlighted by errors, malfunctions at veterans' medical centers.JAMA.2009;301(9):919–920.
- ,.Copy and paste: a remediable hazard of electronic health records.Am J Med.2009;122(6):495–496.
- ,,,.Are electronic medical records trustworthy? Observations on copying, pasting and duplication.AMIA Annu Symp Proc.2003:269–273.
- ,,, et al.Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review.JAMA.2005;293(10):1223–1238.
- ,,, et al.Role of computerized physician order entry systems in facilitating medication errors.JAMA.2005;293(10):1197–1203.
- ,,.The elements of electronic note style.J AHIMA.2003;74(2):68,70.
- ,,,,,.Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians.J Am Med Inform Assoc.2004;11(4):300–309.
- ,,,.The transition to electronic documentation on a teaching hospital medical service.AMIA Annu Symp Proc.2006:629–633.
Delivering the highest possible quality of care is among the top priorities of all medical centers. That said, any quality innovation must be seen as adding value from a variety of perspectives. Especially in the current economic climate, a sound business case is paramount to the advancement of any quality innovation. Given the nature of their work, hospitalists are ideally suited to undertake system improvement innovations. To assist hospitalists in successfully implementing quality and safety initiatives, we have designed a framework of elements required for a business case. We describe our experience developing and implementing an electronic discharge summary and utilize a structured framework to articulate the business case for its implementation.
Defining a Business Case Framework
A business case is a structured proposal outlining the qualitative and quantitative factors that justify a course of action. An effective business case for a quality improvement initiative articulates how both factors are aligned with preexisting organizational goals. In modeling the business case framework for the electronic discharge summary, Figure 1 outlines the qualitative and quantitative costs and benefits that can affect institutional decision making.
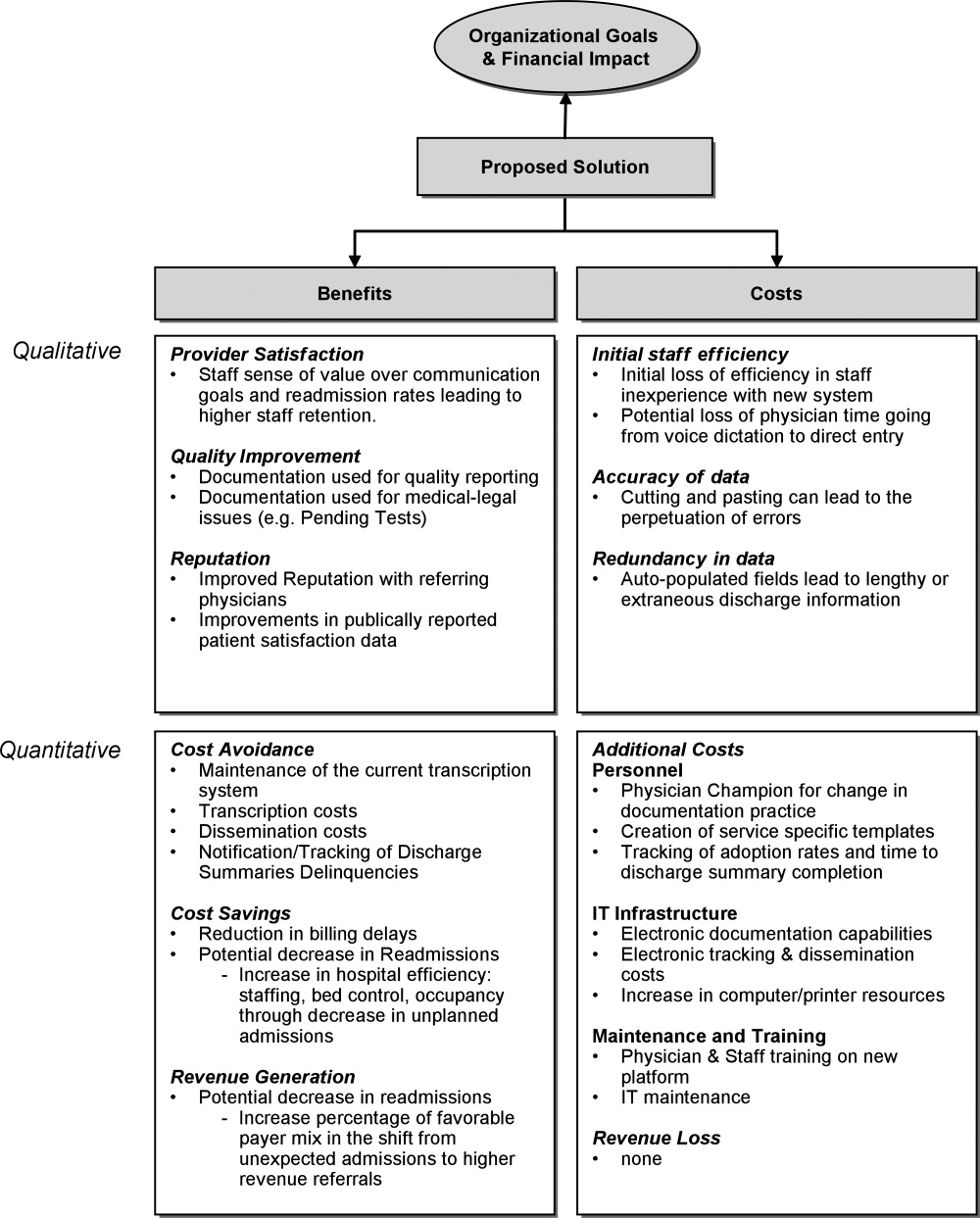
Organizational Aims and Financial Impact: Determining Costs and Benefits
Organizational goals drive decision making and resource allocation at all levels. As priorities change with time, understanding which predominate in an organization will be essential to building a business case. Institutions may be more willing to adopt expensive innovations if they are justified by progress toward the qualitative organizational goals. Figure 1 demonstrates several institutional goals both qualitative (provider satisfaction, quality improvement, and institutional reputation) and quantitative (cost avoidance, cost savings, and revenue generation) that could drive the decision making for an electronic discharge summary. After examining how an initiative aligns with institutional aims, the next step is to weigh the benefits against the potential costs. Costs in our example include not only the quantitative financial investment in information technology (IT) infrastructure, personnel and maintenance, but also may include qualitative costs such as loss of staff efficiency and redundant documentation. Costs and savings will be geographically variable and depend on the institutional framework, eg, the existing system for medical records, institutional patient payer mix, type of payment structure (global vs. utilization based*), and reimbursement rates. While it may be impractical to account for every cost and savings resulting from the project implementation, every effort should be made to account for the key variables that make up the cost‐benefit calculation.
The Business Case for an Electronic Discharge Summary at University of California San Francisco (UCSF)
Current State of Discharge Documentation a UCSF
UCSF Medical Center is a 600‐bed quaternary care academic institution that discharges approximately 100 patients per day. Our hospital discharge summary is used to document a patient's hospital course and post discharge plan, information necessary for continued care in the outpatient setting. Literature supports the potential for timely and relevant discharge summaries to improve care transitions, clinician satisfaction, and resource use.1 In 2008, however, the majority of our discharge summaries were completed greater than 14 days post discharge, in accordance with national practice.2 Despite Centers for Medicare & Medicaid Services (CMS) and the Joint Commission discharge summary standards regarding content,3, 4 most discharge summaries are composed using freeform dictation.2 Consequently, discharge summaries often lack critical information,57 and may not reach the correct outpatient provider in a timely manner.5, 811
Our Proposed Solution: E‐Discharge
As hospitals are increasingly implementing electronic medical records (EMR),12 there is a growing opportunity to efficiently and reliably incorporate information from the medical record into electronic or database assisted discharge materials. At UCSF the need to develop a system to document and communicate tests pending at discharge fueled the development of an electronic discharge summary. UCSF's vendor‐supplied EMR lacks the ability to integrate electronic patient data into a progress note or discharge summary in a manner usable for physicians. Instead physicians are required to use a telephone voice dictation system, which is subsequently transcribed to text within 1 to 3 days. A separate software platform tracks attending signature of the transcribed text and automatically triggers dissemination through computerized fax and campus mail. The turnaround time for a discharge summary can be as long as 3 weeks. With the time involved and high cost of implementing new or more sophisticated versions of EMR, we chose to design a solution that would improve care for our patients in a more immediate and cost neutral fashion. Our goal was to create an affordable, electronic, systematized solution to produce both timely and relevant discharge summaries, in the hopes of improving communications with providers and thus patient outcomes.
In earlier work, UCSF developed UCSF Note Writer, a template‐based documentation tool that uses web service to import data from the underlying database for provider documentation.13 As a standardized template has been shown to improve quality of communication to both patients and referring providers,1, 14, 15 we developed a template in UCSF Note Writer with both free text and auto‐populated fields for a discharge summary based on current guidelines.1619 We encouraged the documentation of medication changes, changes in functional status and pending tests.
The adoption of such an electronic format has also been shown to improve the efficiency of discharge documentation over conventional dictation and transcription.1, 2022 While this change may be institution dependent, we employed strategies such as allowing the discharge summary to be initiated and updated throughout the hospital admission and unifying the discharge summary with the last day's progress note to facilitate timeliness. To promote efficiency, we allowed providers to import pertinent labs, microbiology, and in the future, the importation of pending tests. While the electronic format in itself does not promote timeliness, it incorporates the discharge summary into physician daily workflow and enables efficiency in data gathering and transfer. For outpatient providers who can access the EMR, any delay or potential fault in the delivery of the discharge materials is eliminated, while outside providers can receive copies through other rapid and reliable modes of electronic delivery (eg, EMR inbox notification) with an appropriate infrastructure.
Application of the Business Framework to the Case for an Electronic Discharge
Considering the potential improvements in care delivery, the argument for an electronic discharge summary may seem self‐evident. To realize its implementation, however, it is necessary to consider other aspects of organizational decision making. We employed the following structure to articulate a robust and sound business case for e‐discharge.
Qualitative Benefits
Quality and Safety
Publically reported data are often derived from hospital chart abstraction and may impact accreditation, reputation, and pay for performance programs.18, 23, 24 The discharge summary is a readily available source of information regarding discharge medications, patient instruction, and communication regarding pending tests. As such, its quality should be a priority for hospital decision makers. Electronic discharge summaries have the potential to reduce adverse events in the high‐risk post‐hospitalization period.1, 25 As such they may improve outpatient physicians' ability to deliver relevant care, reduce preventable readmissions26 and reduce malpractice vulnerability27all key drivers in organizational decision making.
Patient Satisfaction
Patients want to feel prepared for discharge by understanding the continuity of their care from the hospital to the outpatient setting. Discharge preparedness, commonly queried and reported in national patient satisfaction surveys, is low.28 Many electronic discharge summary platforms allow for translation into tailored patient instructions available to the patient in real time, helping to ensure that patients receive quality discharge education.29
Referring Physician Satisfaction
Poor discharge communication reduces referring physicians' satisfaction, which may discourage them from referring patients to the hospital or organization, having broader financial implications.25, 30 Even for medical centers with a busy emergency department, outpatient physician referrals and recommendations make up over 50% of an institution's admissions.31 An electronic discharge summary available in the EMR at the time of discharge, electronically transmitted to referring providers can impact the referral patterns of community physicians.
Readmission
Now publicly reported, readmission rates are another benchmark by which to judge hospital care.32 Patients with discharge summaries that are unavailable to outpatient providers, a very common occurance,2 have a higher trend toward readmission.26 Improved quality of care at the time of discharge resulting in fewer readmissions will better position hospitals to contend with potential Medicare reforms.
Quantitative Benefits
IT Infrastructure: Transcription, Deficiency Tracking, Dissemination
Hospitals, including UCSF, use internal or external transcriptionists to transcribe dictated recordings into typed text at a substantial cost to large medical centers. Medical records staff also track both discharge summary completion and their dissemination to referring providers in compliance with regulatory mandates.4, 33 The use of electronic documentation that relies on physician‐direct entry and that automates dissemination and tracking of discharge documentation provides a potential cost savings to offset the costs of a new system. UCSF Medical Center discharges 100 patients per day and could conservatively avoid almost $500,000 in transcription costs annually (Text Box 1).34
Text Box 1
UCSF Transcription costs:
Average cost/line for transcribed text: $0.17
Average Lines in a discharge summary: 80
# pts discharged/day: 100
Yearly costs = $496,400
Billing
Delays in completion of discharge summaries result in billing delays when critical information required for coding is in the discharge summary. Deferred payment on long admissions can reach tens of thousands of dollars, representing a significant strain on medical center finances. Comprehensive electronic discharge materials may simplify coding through careful documentation and improve billing efficiency through rapid completion.
At our medical center, approximately 20% of billing is delayed due to incomplete discharge documentation. For a hospital that generates over $1.4 billion dollars in billing revenue per year, this can translate into significant financial losses. Hospitals may have to borrow money or draw from existing resources to cover operative deficits created by a delay in the receipt of large payment. Lenders charge approximately 1% to 2% annual interest rate, which translates into 0.2% to 0.4% in billed costs that the hospital gives away to their lenders. Hospitals would be well served by eliminating delays in billing to improve revenue flow (Text Box 2).
Text Box 2
UCSF Annual revenue: $1.4 Billion
Billing that requires discharge summary completion: 20%
Lender's interest rate: 12%
Lenders interest rate (12%) on delayed billing (20%) = 0.20.4% of total revenue
Assuming a 14 day delay in billing: 0.20.4% of total revenue ($1,400,000,000) for 14/365 days = $107,000$215,000
Qualitative Costs
Efficiency and Physician Time
Implementation of any new system is likely to result in initial diminished efficiency. If patient volume is stable, this may not translate into loss of revenue, but rather cause staff to change their workflow. For example, given the new inefficiency in charting, staff may spend less time on direct patient care tasks (Intravenous Catheter placement, FT placement, patient education, discharge instructions), thus increasing the qualitative costs to implementing the system.
To minimize these costs, we used a step wise phased role out starting with one pilot team, with a plan to expand to multiple teams prior to implementation on the entire medicine service. This allowed for the creation of one central and several ancillary physician champions to troubleshoot the new system to help minimize productivity losses. One of the largest concerns in the switch from voice dictation to physician‐direct entry into an electronic summary is the cost of physician time. System adjustments through several pilots helped ensure that the time investment of a novice user was not significantly greater than time previously spent dictating.
Quality of Documentation
Unanticipated consequences from a switch to an electronic platform must be considered, such as the possibility of longer more redundant discharge summaries. The amount of information available for automated import will vary by institutional preference, but the recipient's access to the EMR, primary physician preference, and technologic capabilities should be considered. At UCSF we made an effort to distill the information most important to subsequent care, disabling the importation of multiple days of radiology data and instead working to create a system for discharge medication importation. As with any electronic document, the medium also lends itself to cutting and pasting, which may lead to anachronistic information carried forward from hospital progress notes earlier in the stay.35, 36 The largest experience with this unintended consequence can be found in the Veteran's Affairs Health System EMR, which found that 9% of progress notes studied contained copied or duplicated text.37 The authors recommended that clear policies, programs to raise practitioner awareness, and the development of monitoring procedure be implemented coincident with electronic note‐writing capabilities.
Quantitative Costs
Quantitative Costs will be highly variable across institutions, geographical areas, and software platforms as the infrastructure of existing EMRs are highly variable. The cost of implementation depends heavily on whether inpatient documentation (and thus discharge documentation) is a feature of an institutional EMR, or whether a stand‐alone discharge documentation infrastructure is needed. An explanation of the differences between these types of EMRs and the importance to the cost of infrastructure implementation is further described in the following section. Rather than providing a direct accounting of costs, we have provided a tabular summary of costs that should be considered with the adoption of an electronic discharge summary based on the type of institutional EMR (Table 1).
| Voice Dictation | E‐Discharge in an EMR With Inpatient Documentation Abilities | E‐Discharge in an EMR Without Inpatient Documentation Abilities | |
|---|---|---|---|
| |||
| Infrastructure | |||
| Software | + | ||
| Hardware (sufficient computers and printers) | + | + | |
| Network connectivity | + | + | |
| Server capacity for system backup | + | + | |
| Interface with current EMR | + | ||
| Personnel | |||
| Physician champion | + | + | |
| Physician training | + | + | |
| Computer programmer | + | + | |
| Transcription | + | ||
| Deficiency tracking | + | ||
| Dissemination | + | ||
| Maintenance | |||
| Computer/printer maintenance | + | + | |
| Network maintenance | + | + | |
| Software add‐ons and updates | + | + | + |
Infrastructure
For most health care organizations, the transition to an EMR includes adoption of results reporting systems and computerized provider order entry; only a more select group of hospitals with a complete EMR electronically document inpatient care (eg, progress notes) through physician direct entry. While there is substantial literature regarding the benefits and pitfalls of adopting computerized order entry (CPOE),38, 39 there is less attention devoted to the costs of implementing large‐scale electronic documentation, including an electronic discharge summary, as opposed to paper notes or dictation.4042 Institutions using an EMR with electronic care documentation capability have already invested in the infrastructure to implement electronic discharge documentation, and can employ it at a modest cost. For these institutions, the infrastructure cost of the transition from paper charting or dictation to direct entry by physicians lies in ensuring sufficient computers and connectivity to handle the increased computer use. On the other hand, for those institutions where the EMR lacks this capability there are few freestanding documentation platforms available for purchase. The cost of implementing such a system is high, both for the purchase of additional software and the integration of that software in to the EMR supplied by the primary vendor. Other notable infrastructure costs to consider are ensuring sufficient network connectivity, computers and printers to accommodate increased use that will come with electronic note writing as well as server support for system backups.
Personnel
Engaging the right personnel will smooth the implementation of an electronic discharge summary. In addition to dedicated user training sessions, a physician champion who can promote and monitor user training on the new platform will facilitate prompt implementation. An IT support programmer should work with the physician champion to address concerns and troubleshoot problems. Additional personnel may also be needed to track progress in discharge summary adoption, quality and efficiency. Ideally these personnel can be funneled from those who work transcribing, disseminating and tracking completion of discharge summaries, positions that will be needed in a reduced capacity.
Maintenance
Increased IT infrastructure also means increased IT maintenance and upgrades of servers, network connectivity, computers and printers. Discussions with vendors regarding costs of maintenance, upgrades and add‐on features should be considered when adopting an electronic discharge summary platform.
Conclusion
While many QI initiatives have the potential to improve clinical care, resource limitations and competing priorities necessitate that hospital decision makers see the value of hospitalist driven improvements. A sound business case is the key to successfully influencing decision making and furthering necessary innovations. We have detailed the elements of a business case and applied them to a proposed innovationthe electronic discharge summary. While the cost of multifunctional EMR with full electronic care documentation may be impossible to implement given high initial costs and competing priorities, investing in an e‐discharge solution has real‐time benefits in the impact on patients, system improvements, qualitative benefits, and return on investment. Being able to articulate key qualitative and quantitative elements creates a sound business case that can be applied to QI initiatives in general, and assist hospitalists in garnering support and resources to continue to improve care.
Acknowledgements
The authors acknowledge Kathleen Kerr and the members of the BOOST collaborative for helping with background research and in creating the impetus for this work.
Global payments are fixed‐dollar payments for the care that patients may receive in a given time period, such as a month or year, whereas utilization based payments are payments based on the use of diagnostic and treatment modalities (eg, CT scans and blood cultures).
Delivering the highest possible quality of care is among the top priorities of all medical centers. That said, any quality innovation must be seen as adding value from a variety of perspectives. Especially in the current economic climate, a sound business case is paramount to the advancement of any quality innovation. Given the nature of their work, hospitalists are ideally suited to undertake system improvement innovations. To assist hospitalists in successfully implementing quality and safety initiatives, we have designed a framework of elements required for a business case. We describe our experience developing and implementing an electronic discharge summary and utilize a structured framework to articulate the business case for its implementation.
Defining a Business Case Framework
A business case is a structured proposal outlining the qualitative and quantitative factors that justify a course of action. An effective business case for a quality improvement initiative articulates how both factors are aligned with preexisting organizational goals. In modeling the business case framework for the electronic discharge summary, Figure 1 outlines the qualitative and quantitative costs and benefits that can affect institutional decision making.
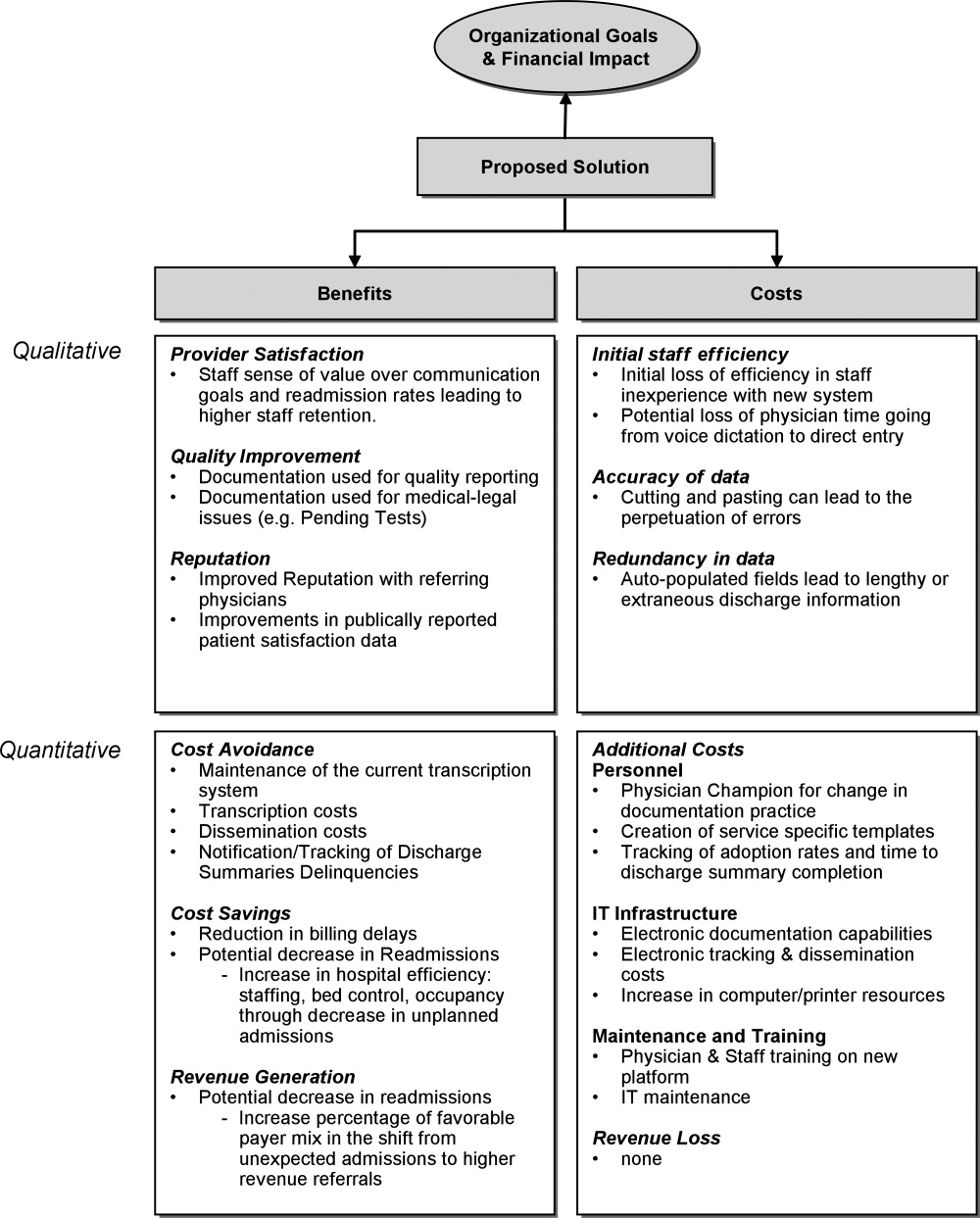
Organizational Aims and Financial Impact: Determining Costs and Benefits
Organizational goals drive decision making and resource allocation at all levels. As priorities change with time, understanding which predominate in an organization will be essential to building a business case. Institutions may be more willing to adopt expensive innovations if they are justified by progress toward the qualitative organizational goals. Figure 1 demonstrates several institutional goals both qualitative (provider satisfaction, quality improvement, and institutional reputation) and quantitative (cost avoidance, cost savings, and revenue generation) that could drive the decision making for an electronic discharge summary. After examining how an initiative aligns with institutional aims, the next step is to weigh the benefits against the potential costs. Costs in our example include not only the quantitative financial investment in information technology (IT) infrastructure, personnel and maintenance, but also may include qualitative costs such as loss of staff efficiency and redundant documentation. Costs and savings will be geographically variable and depend on the institutional framework, eg, the existing system for medical records, institutional patient payer mix, type of payment structure (global vs. utilization based*), and reimbursement rates. While it may be impractical to account for every cost and savings resulting from the project implementation, every effort should be made to account for the key variables that make up the cost‐benefit calculation.
The Business Case for an Electronic Discharge Summary at University of California San Francisco (UCSF)
Current State of Discharge Documentation a UCSF
UCSF Medical Center is a 600‐bed quaternary care academic institution that discharges approximately 100 patients per day. Our hospital discharge summary is used to document a patient's hospital course and post discharge plan, information necessary for continued care in the outpatient setting. Literature supports the potential for timely and relevant discharge summaries to improve care transitions, clinician satisfaction, and resource use.1 In 2008, however, the majority of our discharge summaries were completed greater than 14 days post discharge, in accordance with national practice.2 Despite Centers for Medicare & Medicaid Services (CMS) and the Joint Commission discharge summary standards regarding content,3, 4 most discharge summaries are composed using freeform dictation.2 Consequently, discharge summaries often lack critical information,57 and may not reach the correct outpatient provider in a timely manner.5, 811
Our Proposed Solution: E‐Discharge
As hospitals are increasingly implementing electronic medical records (EMR),12 there is a growing opportunity to efficiently and reliably incorporate information from the medical record into electronic or database assisted discharge materials. At UCSF the need to develop a system to document and communicate tests pending at discharge fueled the development of an electronic discharge summary. UCSF's vendor‐supplied EMR lacks the ability to integrate electronic patient data into a progress note or discharge summary in a manner usable for physicians. Instead physicians are required to use a telephone voice dictation system, which is subsequently transcribed to text within 1 to 3 days. A separate software platform tracks attending signature of the transcribed text and automatically triggers dissemination through computerized fax and campus mail. The turnaround time for a discharge summary can be as long as 3 weeks. With the time involved and high cost of implementing new or more sophisticated versions of EMR, we chose to design a solution that would improve care for our patients in a more immediate and cost neutral fashion. Our goal was to create an affordable, electronic, systematized solution to produce both timely and relevant discharge summaries, in the hopes of improving communications with providers and thus patient outcomes.
In earlier work, UCSF developed UCSF Note Writer, a template‐based documentation tool that uses web service to import data from the underlying database for provider documentation.13 As a standardized template has been shown to improve quality of communication to both patients and referring providers,1, 14, 15 we developed a template in UCSF Note Writer with both free text and auto‐populated fields for a discharge summary based on current guidelines.1619 We encouraged the documentation of medication changes, changes in functional status and pending tests.
The adoption of such an electronic format has also been shown to improve the efficiency of discharge documentation over conventional dictation and transcription.1, 2022 While this change may be institution dependent, we employed strategies such as allowing the discharge summary to be initiated and updated throughout the hospital admission and unifying the discharge summary with the last day's progress note to facilitate timeliness. To promote efficiency, we allowed providers to import pertinent labs, microbiology, and in the future, the importation of pending tests. While the electronic format in itself does not promote timeliness, it incorporates the discharge summary into physician daily workflow and enables efficiency in data gathering and transfer. For outpatient providers who can access the EMR, any delay or potential fault in the delivery of the discharge materials is eliminated, while outside providers can receive copies through other rapid and reliable modes of electronic delivery (eg, EMR inbox notification) with an appropriate infrastructure.
Application of the Business Framework to the Case for an Electronic Discharge
Considering the potential improvements in care delivery, the argument for an electronic discharge summary may seem self‐evident. To realize its implementation, however, it is necessary to consider other aspects of organizational decision making. We employed the following structure to articulate a robust and sound business case for e‐discharge.
Qualitative Benefits
Quality and Safety
Publically reported data are often derived from hospital chart abstraction and may impact accreditation, reputation, and pay for performance programs.18, 23, 24 The discharge summary is a readily available source of information regarding discharge medications, patient instruction, and communication regarding pending tests. As such, its quality should be a priority for hospital decision makers. Electronic discharge summaries have the potential to reduce adverse events in the high‐risk post‐hospitalization period.1, 25 As such they may improve outpatient physicians' ability to deliver relevant care, reduce preventable readmissions26 and reduce malpractice vulnerability27all key drivers in organizational decision making.
Patient Satisfaction
Patients want to feel prepared for discharge by understanding the continuity of their care from the hospital to the outpatient setting. Discharge preparedness, commonly queried and reported in national patient satisfaction surveys, is low.28 Many electronic discharge summary platforms allow for translation into tailored patient instructions available to the patient in real time, helping to ensure that patients receive quality discharge education.29
Referring Physician Satisfaction
Poor discharge communication reduces referring physicians' satisfaction, which may discourage them from referring patients to the hospital or organization, having broader financial implications.25, 30 Even for medical centers with a busy emergency department, outpatient physician referrals and recommendations make up over 50% of an institution's admissions.31 An electronic discharge summary available in the EMR at the time of discharge, electronically transmitted to referring providers can impact the referral patterns of community physicians.
Readmission
Now publicly reported, readmission rates are another benchmark by which to judge hospital care.32 Patients with discharge summaries that are unavailable to outpatient providers, a very common occurance,2 have a higher trend toward readmission.26 Improved quality of care at the time of discharge resulting in fewer readmissions will better position hospitals to contend with potential Medicare reforms.
Quantitative Benefits
IT Infrastructure: Transcription, Deficiency Tracking, Dissemination
Hospitals, including UCSF, use internal or external transcriptionists to transcribe dictated recordings into typed text at a substantial cost to large medical centers. Medical records staff also track both discharge summary completion and their dissemination to referring providers in compliance with regulatory mandates.4, 33 The use of electronic documentation that relies on physician‐direct entry and that automates dissemination and tracking of discharge documentation provides a potential cost savings to offset the costs of a new system. UCSF Medical Center discharges 100 patients per day and could conservatively avoid almost $500,000 in transcription costs annually (Text Box 1).34
Text Box 1
UCSF Transcription costs:
Average cost/line for transcribed text: $0.17
Average Lines in a discharge summary: 80
# pts discharged/day: 100
Yearly costs = $496,400
Billing
Delays in completion of discharge summaries result in billing delays when critical information required for coding is in the discharge summary. Deferred payment on long admissions can reach tens of thousands of dollars, representing a significant strain on medical center finances. Comprehensive electronic discharge materials may simplify coding through careful documentation and improve billing efficiency through rapid completion.
At our medical center, approximately 20% of billing is delayed due to incomplete discharge documentation. For a hospital that generates over $1.4 billion dollars in billing revenue per year, this can translate into significant financial losses. Hospitals may have to borrow money or draw from existing resources to cover operative deficits created by a delay in the receipt of large payment. Lenders charge approximately 1% to 2% annual interest rate, which translates into 0.2% to 0.4% in billed costs that the hospital gives away to their lenders. Hospitals would be well served by eliminating delays in billing to improve revenue flow (Text Box 2).
Text Box 2
UCSF Annual revenue: $1.4 Billion
Billing that requires discharge summary completion: 20%
Lender's interest rate: 12%
Lenders interest rate (12%) on delayed billing (20%) = 0.20.4% of total revenue
Assuming a 14 day delay in billing: 0.20.4% of total revenue ($1,400,000,000) for 14/365 days = $107,000$215,000
Qualitative Costs
Efficiency and Physician Time
Implementation of any new system is likely to result in initial diminished efficiency. If patient volume is stable, this may not translate into loss of revenue, but rather cause staff to change their workflow. For example, given the new inefficiency in charting, staff may spend less time on direct patient care tasks (Intravenous Catheter placement, FT placement, patient education, discharge instructions), thus increasing the qualitative costs to implementing the system.
To minimize these costs, we used a step wise phased role out starting with one pilot team, with a plan to expand to multiple teams prior to implementation on the entire medicine service. This allowed for the creation of one central and several ancillary physician champions to troubleshoot the new system to help minimize productivity losses. One of the largest concerns in the switch from voice dictation to physician‐direct entry into an electronic summary is the cost of physician time. System adjustments through several pilots helped ensure that the time investment of a novice user was not significantly greater than time previously spent dictating.
Quality of Documentation
Unanticipated consequences from a switch to an electronic platform must be considered, such as the possibility of longer more redundant discharge summaries. The amount of information available for automated import will vary by institutional preference, but the recipient's access to the EMR, primary physician preference, and technologic capabilities should be considered. At UCSF we made an effort to distill the information most important to subsequent care, disabling the importation of multiple days of radiology data and instead working to create a system for discharge medication importation. As with any electronic document, the medium also lends itself to cutting and pasting, which may lead to anachronistic information carried forward from hospital progress notes earlier in the stay.35, 36 The largest experience with this unintended consequence can be found in the Veteran's Affairs Health System EMR, which found that 9% of progress notes studied contained copied or duplicated text.37 The authors recommended that clear policies, programs to raise practitioner awareness, and the development of monitoring procedure be implemented coincident with electronic note‐writing capabilities.
Quantitative Costs
Quantitative Costs will be highly variable across institutions, geographical areas, and software platforms as the infrastructure of existing EMRs are highly variable. The cost of implementation depends heavily on whether inpatient documentation (and thus discharge documentation) is a feature of an institutional EMR, or whether a stand‐alone discharge documentation infrastructure is needed. An explanation of the differences between these types of EMRs and the importance to the cost of infrastructure implementation is further described in the following section. Rather than providing a direct accounting of costs, we have provided a tabular summary of costs that should be considered with the adoption of an electronic discharge summary based on the type of institutional EMR (Table 1).
| Voice Dictation | E‐Discharge in an EMR With Inpatient Documentation Abilities | E‐Discharge in an EMR Without Inpatient Documentation Abilities | |
|---|---|---|---|
| |||
| Infrastructure | |||
| Software | + | ||
| Hardware (sufficient computers and printers) | + | + | |
| Network connectivity | + | + | |
| Server capacity for system backup | + | + | |
| Interface with current EMR | + | ||
| Personnel | |||
| Physician champion | + | + | |
| Physician training | + | + | |
| Computer programmer | + | + | |
| Transcription | + | ||
| Deficiency tracking | + | ||
| Dissemination | + | ||
| Maintenance | |||
| Computer/printer maintenance | + | + | |
| Network maintenance | + | + | |
| Software add‐ons and updates | + | + | + |
Infrastructure
For most health care organizations, the transition to an EMR includes adoption of results reporting systems and computerized provider order entry; only a more select group of hospitals with a complete EMR electronically document inpatient care (eg, progress notes) through physician direct entry. While there is substantial literature regarding the benefits and pitfalls of adopting computerized order entry (CPOE),38, 39 there is less attention devoted to the costs of implementing large‐scale electronic documentation, including an electronic discharge summary, as opposed to paper notes or dictation.4042 Institutions using an EMR with electronic care documentation capability have already invested in the infrastructure to implement electronic discharge documentation, and can employ it at a modest cost. For these institutions, the infrastructure cost of the transition from paper charting or dictation to direct entry by physicians lies in ensuring sufficient computers and connectivity to handle the increased computer use. On the other hand, for those institutions where the EMR lacks this capability there are few freestanding documentation platforms available for purchase. The cost of implementing such a system is high, both for the purchase of additional software and the integration of that software in to the EMR supplied by the primary vendor. Other notable infrastructure costs to consider are ensuring sufficient network connectivity, computers and printers to accommodate increased use that will come with electronic note writing as well as server support for system backups.
Personnel
Engaging the right personnel will smooth the implementation of an electronic discharge summary. In addition to dedicated user training sessions, a physician champion who can promote and monitor user training on the new platform will facilitate prompt implementation. An IT support programmer should work with the physician champion to address concerns and troubleshoot problems. Additional personnel may also be needed to track progress in discharge summary adoption, quality and efficiency. Ideally these personnel can be funneled from those who work transcribing, disseminating and tracking completion of discharge summaries, positions that will be needed in a reduced capacity.
Maintenance
Increased IT infrastructure also means increased IT maintenance and upgrades of servers, network connectivity, computers and printers. Discussions with vendors regarding costs of maintenance, upgrades and add‐on features should be considered when adopting an electronic discharge summary platform.
Conclusion
While many QI initiatives have the potential to improve clinical care, resource limitations and competing priorities necessitate that hospital decision makers see the value of hospitalist driven improvements. A sound business case is the key to successfully influencing decision making and furthering necessary innovations. We have detailed the elements of a business case and applied them to a proposed innovationthe electronic discharge summary. While the cost of multifunctional EMR with full electronic care documentation may be impossible to implement given high initial costs and competing priorities, investing in an e‐discharge solution has real‐time benefits in the impact on patients, system improvements, qualitative benefits, and return on investment. Being able to articulate key qualitative and quantitative elements creates a sound business case that can be applied to QI initiatives in general, and assist hospitalists in garnering support and resources to continue to improve care.
Acknowledgements
The authors acknowledge Kathleen Kerr and the members of the BOOST collaborative for helping with background research and in creating the impetus for this work.
Global payments are fixed‐dollar payments for the care that patients may receive in a given time period, such as a month or year, whereas utilization based payments are payments based on the use of diagnostic and treatment modalities (eg, CT scans and blood cultures).
- ,,, et al.Creating a better discharge summary: Improvement in quality and timeliness using an electronic discharge summary.J Hosp Med.2009;4(4):219–225.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- Standard IM.6.10Hospital Accredidation Standards. In: Oakbrook Terrace,IL:Joint Commission Resources;2006:338–340.
- .Medical Record Services, Section 482.24. In: MacDonald I, ed.The CMS Hospital Conditions of Participation.First edition.United States:Hc Pro Inc.;2005:24–25.
- .Hospital discharge and death communications.Br J Hosp Med.1989;42(1):59–61.
- ,,,.Hospital discharge reports: content and design.Br Med J.1975;4(5994):443–446.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143(2):121–128.
- .Delayed communication between hospitals and general practitioners: where does the problem lie?BMJ.1988;297(6640):28–29.
- .Study of “discharge communications” from hospital.Br Med J (Clin Res Ed).1986;293(6557):1283–1284.
- ,.Quality assessment of a discharge summary system.CMAJ.1995;152(9):1437–1442.
- ,,,.General practitioner‐hospital communications: a review of discharge summaries.J Qual Clin Pract.2001;21(4):104–108.
- .Stimulus bill spurs plans for rapid IT progress.Manag Care.2009;18(2):5–6.
- ,,, et al. UCSF Notewriter. Copyright Regents of the University of California.2006–year="2010"2010.
- ,,,,.Assessing quality and efficiency of discharge summaries.Am J Med Qual.2005;20(6):337–343.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,.What is necessary for high‐quality discharge summaries?Am J Med Qual.1999;14(4):160–169.
- ,,,,.Outpatient physicians' satisfaction with discharge summaries and perceived need for an electronic discharge summary.J Hosp Med.2006;1(5):317–320.
- ,.Are general practitioners satisfied with electronic discharge summaries?HIM J.2007;36(1):7–12.
- ,,,.Dictated versus database‐generated discharge summaries: a randomized clinical trial.CMAJ.1999;160(3):319–326.
- ,,,.Evaluation of computer generated neonatal discharge summaries.Arch Dis Child.1991;66(4 Spec No):433–436.
- ,,,,,.Evaluation of a computer‐generated discharge summary for patients with acute coronary syndromes.Br J Gen Pract.1998;48(429):1163–1164.
- The Common Wealth Fund. Why not the best org. Available at: http/www.whynotthebest.org. Updated 2009. Accessed May2010.
- ,.Pay for performance: an overview of the literature.Am J Med Qual.2009;24(2):140–163.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170(3):345–349.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17(3):186–192.
- ,,, et al.Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims.Ann Intern Med.2006;145(7):488–496.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43(3):246–255.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20(4):317–323.
- ,,.Referring physician satisfaction: toward a better understanding of hospital referrals.J Hosp Mark.1998;12(2):95–111.
- U.S. Department of Health 7(3):269–272.
- .IT vulnerabilities highlighted by errors, malfunctions at veterans' medical centers.JAMA.2009;301(9):919–920.
- ,.Copy and paste: a remediable hazard of electronic health records.Am J Med.2009;122(6):495–496.
- ,,,.Are electronic medical records trustworthy? Observations on copying, pasting and duplication.AMIA Annu Symp Proc.2003:269–273.
- ,,, et al.Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review.JAMA.2005;293(10):1223–1238.
- ,,, et al.Role of computerized physician order entry systems in facilitating medication errors.JAMA.2005;293(10):1197–1203.
- ,,.The elements of electronic note style.J AHIMA.2003;74(2):68,70.
- ,,,,,.Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians.J Am Med Inform Assoc.2004;11(4):300–309.
- ,,,.The transition to electronic documentation on a teaching hospital medical service.AMIA Annu Symp Proc.2006:629–633.
- ,,, et al.Creating a better discharge summary: Improvement in quality and timeliness using an electronic discharge summary.J Hosp Med.2009;4(4):219–225.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- Standard IM.6.10Hospital Accredidation Standards. In: Oakbrook Terrace,IL:Joint Commission Resources;2006:338–340.
- .Medical Record Services, Section 482.24. In: MacDonald I, ed.The CMS Hospital Conditions of Participation.First edition.United States:Hc Pro Inc.;2005:24–25.
- .Hospital discharge and death communications.Br J Hosp Med.1989;42(1):59–61.
- ,,,.Hospital discharge reports: content and design.Br Med J.1975;4(5994):443–446.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143(2):121–128.
- .Delayed communication between hospitals and general practitioners: where does the problem lie?BMJ.1988;297(6640):28–29.
- .Study of “discharge communications” from hospital.Br Med J (Clin Res Ed).1986;293(6557):1283–1284.
- ,.Quality assessment of a discharge summary system.CMAJ.1995;152(9):1437–1442.
- ,,,.General practitioner‐hospital communications: a review of discharge summaries.J Qual Clin Pract.2001;21(4):104–108.
- .Stimulus bill spurs plans for rapid IT progress.Manag Care.2009;18(2):5–6.
- ,,, et al. UCSF Notewriter. Copyright Regents of the University of California.2006–year="2010"2010.
- ,,,,.Assessing quality and efficiency of discharge summaries.Am J Med Qual.2005;20(6):337–343.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,.What is necessary for high‐quality discharge summaries?Am J Med Qual.1999;14(4):160–169.
- ,,,,.Outpatient physicians' satisfaction with discharge summaries and perceived need for an electronic discharge summary.J Hosp Med.2006;1(5):317–320.
- ,.Are general practitioners satisfied with electronic discharge summaries?HIM J.2007;36(1):7–12.
- ,,,.Dictated versus database‐generated discharge summaries: a randomized clinical trial.CMAJ.1999;160(3):319–326.
- ,,,.Evaluation of computer generated neonatal discharge summaries.Arch Dis Child.1991;66(4 Spec No):433–436.
- ,,,,,.Evaluation of a computer‐generated discharge summary for patients with acute coronary syndromes.Br J Gen Pract.1998;48(429):1163–1164.
- The Common Wealth Fund. Why not the best org. Available at: http/www.whynotthebest.org. Updated 2009. Accessed May2010.
- ,.Pay for performance: an overview of the literature.Am J Med Qual.2009;24(2):140–163.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170(3):345–349.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17(3):186–192.
- ,,, et al.Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims.Ann Intern Med.2006;145(7):488–496.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43(3):246–255.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20(4):317–323.
- ,,.Referring physician satisfaction: toward a better understanding of hospital referrals.J Hosp Mark.1998;12(2):95–111.
- U.S. Department of Health 7(3):269–272.
- .IT vulnerabilities highlighted by errors, malfunctions at veterans' medical centers.JAMA.2009;301(9):919–920.
- ,.Copy and paste: a remediable hazard of electronic health records.Am J Med.2009;122(6):495–496.
- ,,,.Are electronic medical records trustworthy? Observations on copying, pasting and duplication.AMIA Annu Symp Proc.2003:269–273.
- ,,, et al.Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review.JAMA.2005;293(10):1223–1238.
- ,,, et al.Role of computerized physician order entry systems in facilitating medication errors.JAMA.2005;293(10):1197–1203.
- ,,.The elements of electronic note style.J AHIMA.2003;74(2):68,70.
- ,,,,,.Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians.J Am Med Inform Assoc.2004;11(4):300–309.
- ,,,.The transition to electronic documentation on a teaching hospital medical service.AMIA Annu Symp Proc.2006:629–633.